
RESPIRATORY DISTRESS IN
NEWBORN: TREATED WITH
VENTILATION IN A LEVEL II
NURSERY
A.K. Malhotra
R. Nagpal
R.K. Gupta
D.S. Chhajta
R.K. Arora
ABSTRACT
Fifty consecutive neonates with respiratory
distress persisting beyond 6 h of age were
studied during a 18 month period (total delive-
ries 2000/y). Twenty two neonates were mana-
ged with oxygen hood with increasing oxygen
concentration, 28 with continuous positive air-
way pressure (CPAP) ventilation using a nasal
cannula. Of these babies on CPAP, 10 were
shifted to intermittent positive pressure ventila-
tion (IPPV) on a pressure limited, time cycled
ventilator (Neovent, Vickers). Babies were
monitored with continuous hemoglobin oxygen
saturation (SaO
2
), hourly blood pressure and
vital charting. Radial arterial blood gas analysis
(ABG) was done when feasible and especially on
clinical deterioration. Oxygen (FiO
2
0.95) from
an oxygen concentrator was used as a source of
continuous supply of oxygen. Commonest cause
of respiratory distress was hyaline membrane
disease (18%), followed by wet lung syndromes
(14%), meconium aspiration (12%), asphyxia
(12%) and septicemia (8%). In 8 babies, a lung
biopsy (postmortem) was done to confirm the
diagnosis. Nineteen of the 50 babies with respi-
ratory distress died, there was a survival of 50%
on CPAP and 30% on IPPV. No case of oxygen
toxicity or other major complications was
encountered. Even with moderate resources,
neonatal ventilation in a Level II nursery is a
Respiratory distress is the most com-
mon problem in neonatal nurseries. It
results from a variety of causes and an
urgent work up is essential. Yet for
hypoxemia some form of assisted venti-
lation is immediately warranted. The
outlook of babies with respiratory dis-
tress syndrome has changed after the
first use of continuous positive airway
pressure (CPAP) by Gregory et al.(l). It
is now an established modality for neo-
nates for many years.
In India, a survival of 100% in babies
more than 1.5 Kg on CPAP mode is
reported(2). It is also recommended that
neonatal ventilation should be ventured
in centres where basic facilities for Level
II care already exist. Ours is a well
equipped nursery recognized by the
National Neonatology Forum (NNF).
We treated 50 babies with respiratory
distress, of which 31 survived.
Material and Methods
In a prospective study, we analyzed
the causes of respiratory distress and
indications for ventilation in newborns
during a 18 month period (Jan '92-June
'93). There were a total of 2931 booked
deliveries during this period in our hos-
pital which caters to a mixed Indian
challenging task. Babies less than 1000g require
aggressive measures which is not very economi-
cal in a special care baby unit (SCBU).
Key words: Neonatal ventilation, Respiratory
distress.
From the Neonatal Unit, Department of Pediat-
rics, Command Hospital, Pune All 040.
Reprint requests: Lt. Col. A.K. Malhotra, 174,
Military Hospital C/o 56 A.P.O.
Received for publication: October 2,1993;
Accepted: June 8,1994

MALHOTRA ET AL.
population. For the diagnosis of respira-
tory distress, the important signs are
respiratory rate more than 60 per
minute, grunt and sub-costal recessions.
These signs being non-specific, we con-
sider two out of three of these as
confirmative of respiratory distress(3).
Rarely, apneic attacks may present as a
sole manifestation of ventilatory failure.
As the spectrum of respiratory dis-
tress in newborns is large, we start a
workup at four hours of age and give a
provisional diagnosis at 6 hours of post
natal life. The initial workup included a
gastric aspirate shake test, chest X-ray
and an arterial blood gas (ABG) analy-
sis. Blood pressure and vital signs were
recorded. Oxygen saturation (SaO
2
) and
heart rate were monitored using a pulse
oximeter (Ohmeda Biox 3760). Oxygen
from a oxygen concentrator (Air Sep
Forlife) with FiO
2
0.95 was used to sup-
ply oxygen. Intravenous fluids were
started at the rate of 60 ml per kg body
weight of 10% dextrose solution. If clini-
cal condition warranted antibiotics,
blood cultures were taken prior in 10 ml
culture bottles. Downes RDS Score(4)
was recorded and babies with a score of
six or more were put on CPAP with a
nasal cannula (Argyle). Babies with a
score of five or less were managed with
oxygen hood with increasing FiO
2
con-
centrations.
The indication for giving CPAP were
(i) Downes score of 6 or more; (ii) inabi-
lity to maintain a SaO
2
of 87% with oxy-
gen hood; (iii) PaO
2
of less than 50 mm
Hg; and (iv) radiological evidence of
severe hyaline membrane disease
(HMD) with a negative shake test.
CPAP is considered a failure if a baby
has (i) inability to maintain a SaO
2
of
208
VENTILATION FOR RDS
87% with CPAP of 12 cm H
2
O and FiO
2
of 0.9; (ii) PaO
2
<50 mm Hg with FiO
2
0.9; (iii) pH <7.25, PaCO
2
>60 mm Hg;
and (iv) recurrent (more than 3) apneic
attacks as a manifestation of respiratory
failure. CPAP failures were shifted to
intermittent positive pressure ventila-
tion (IPPV) mode on a time cycled, pres-
sure limited continuous flow neonatal
ventilator (Neovent, Vickers). We use
minimal ventilatory settings depending
on the lung pathology to achieve a SaO
2
of 90±3% or PaO
2
60-80 mm Hg. Subse-
quent ABG was done through repeated
radial arterial punctures at 6-12 hourly
intervals. The definitions suggested by
NNF Group on Neonatal Nomencla-
ture(3) were accepted. Babies delivered
with a thick meconium stained liquor
were intubated prior to first breath. Sep-
ticemia was diagnosed if the blood cul-
ture grew pathogenic organisms. Imma-
turity was labelled when a baby less
than 1000 g had no other primary cause
of death.
Results
Out of the 50 babies enrolled in the
study, 26 were males and 24 females.
There were 40 babies with low birth
weight; of these 10 babies were less than
1000g. Mean birth weight was 1823 g
(range 740-3900 g) and mean gestational.
age 33 wk (range 26-42 wk). The smal-
lest baby a non survivor was 740 g with
a gestational age of 26 weeks. Table I de-
picts the modes of oxygenation. Twenty
two babies were managed with oxygen
hood and 28 required CPAP ventilation.
Of these 10 babies had a failure of CPAP
ventilation and were shifted to IPPV
mode. The mean duration of CPAP
mode was 53 h (range 11-156 h) and
IPPV mode 46 h (range 7-74 h).

INDIAN PEDIATRICS
Hyaline membrane disease (18%)
was the commonest cause of respiratory
distress, followed by wet lung syn-
dromes (14%), meconium aspiration
syndrome (12%), asphyxia (12%) and
VOLUME 32-FEBRUARY 1995
septicemia (8%) (Table II). There was one
baby 1000 g who developed chronic pul-
monary insufficiency of prematurity
(CPIP) and was discharged with a
weight of 1750g. In 8 cases (birth weight
MALHOTRAETAL.
900-2000g) with a clinical diagnosis of
HMD, the cause of death was confirmed
by a postmortem lung biopsy. In all
these cases, the histopathological fea-
tures were consistent with hyaline
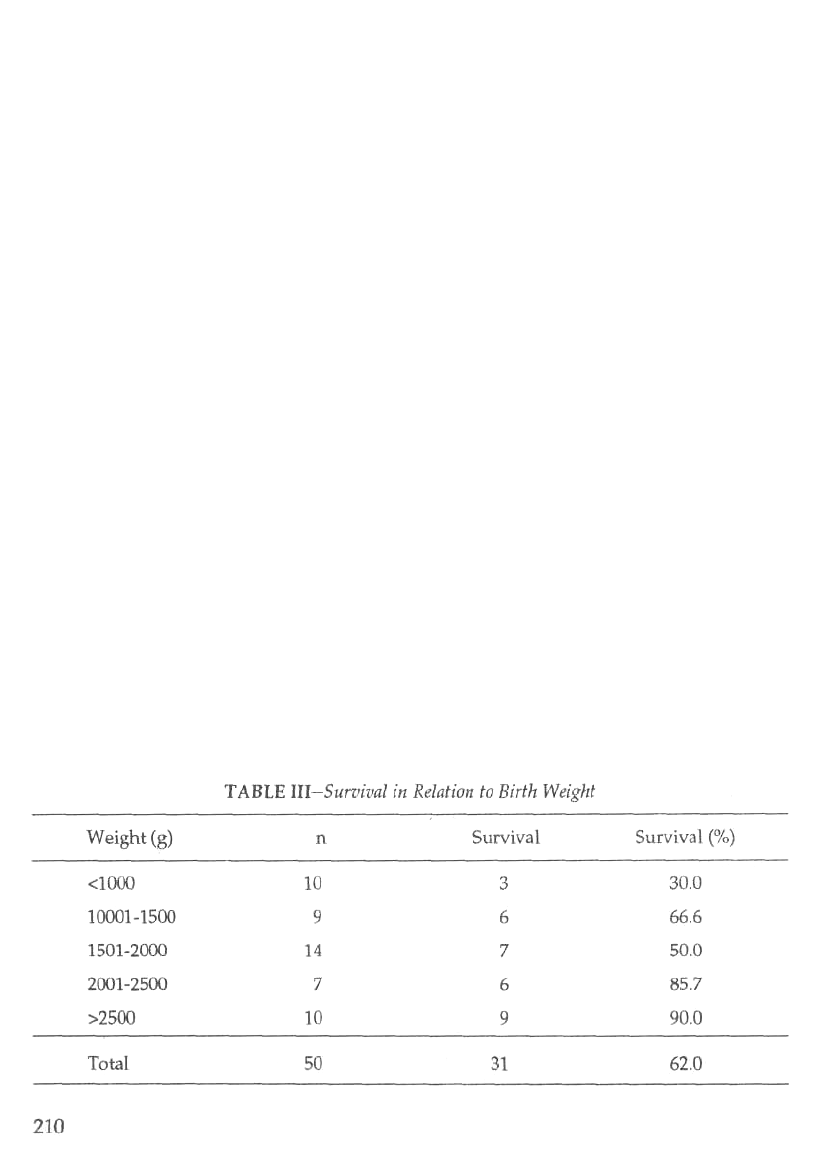
membrane disease. Table III depicts the
survival in relation to the birth weight
and mode of ventilation. There was a
50% survival on CPAP and 30% on IPPV
mode. Survival of babies less than 1000g
was 30%. Three babies had a symptom-
atic ductus arteriosus (PDA) and were
managed on standard lines. No baby
developed pneumofhorax or other
major complications of ventilation or
oxygen therapy.
Discussion
Majority of the medical colleges in
our country lack the basic infrastructure
to ventilate babies(2). Ventilation has
only been reported from tertiary centres
and experience from Level II nurseries
is lacking. We have the expertise but the
resources are limited. At the same time,
IPPV and aggressive monitoring results
in a significant iatrogenic morbidity.
Within the frame work of the physics of
ventilation every nursery evolves its
protocols and settings for ventilation.
VENTILATION FOR RDS
As oxygen is a drug, we choose a mid-
line path whereby the complications are
minimum. The CPAP mode with nasal
cannula is an easy way to improve oxy-
genation. This makes the routine endo-
tracheal intubation of infants requiring
only continuous airway distending
pressures no longer justifiable(5).
Once oxygenation is adequate and
signs of respiratory distress decrease, an
optimal CPAP is achieved. CPAP failu-
res appear to have an omnious progno-
sis regardless of the birth weight(5). In
our series, we had 10 babies less than
1000g and the mortality in them was
70%. CPAP is not an ideal treatment for
them and they may require IPPV at the
outset(2). Chronic pulmonary insuffi-
ciency of prematurity is a distinct entity
as these babies are less than 1000g and
have a normal chest X-ray at birth but
are oxygen dependent at 3-4 weeks of
age. We agree with Singh et al. in
considering a cut off of immaturity at
750 g(2). In a review of literature(5) the
incidence of pneumothoraces was 0 to
14%. We had no case of pneumofhorax
or other major complications of oxygen
toxicity.

INDIAN PEDIATRICS
Pulse oximetry is a reliable tech-
nique for monitoring of oxygenation in
newborns(6,7). It is a handy tool in a
Level II nursery as apart from SaO
2
it
displays the heart rate. It obviates the
use of an electrocardiograph and apnea
monitors. In managing cases of respira-
tory distress, it has few limitations and
the artifacts are avoidable. Fanconi et
al.(8) constructed oxygen dissociation
curves with pulse oximeter SaO
2
, mea-
sured SaO
2
and calculated SaO
2
; they
were all similar. A pulse oximeter read-
ing of 85% to 90% is a clinically safe tar-
get. We maintain a SaO
2
level of 90±3%
and titrate FiO
2
to that level. On clinical
deterioration and failure to maintain
saturation, an ABG helps in correcting
the acid base defect. As oxygen is
always at a premium in a Level II nur-
sery, oxygen (FiO
2
0.95) from an oxygen
concentrator is a useful equipment to
supply oxygen.
Getting a neonatal autopsy in India
is a difficult task. We have found a lung
biopsy done immediately after death an
easy method to come to a diagnosis. In 8
of our babies, biopsy showed features
suggesting HMD. Considering babies
more than 1000g, we have a survival of
70% and only 30% in less than 1000g.
These babies require aggressive mea-
sures which is not very economical in a
Level II nursery.
Acknowledgement
The authors are grateful to Director
General, Armed Forces Medical Ser-
vices, New Delhi for financial assistance
as part of AFMRC Project No 1912/92.
VOLUME 32-FEBRUARY 1995
REFERENCES
1. Gregory JZA, Kitterman JA, Phibbs
RH, et al. Treatment of idiopathic res-
piratory distress syndrome with con-
tinuous positive airway pressure. N
Engl J Med 1971, 284:1333-1341.
2. Singh M, Deorari AK, Paul VK, et al.
Three year experience with neonatal
ventilation from a tertiary care hospi-
tal in Delhi. Indian Pediatr 1993, 30:
783-789.
3. Singh M, Paul VK, Bhakoo ON. Neo-
natal Nomenclature and Data Collec-
tion. New Delhi, National Neonato-
logy Forum, 1989.
4. Downes JJ, Vidyasagar D, Morrow
GM, et al. Respiratory distress syn-
drome of infants I. New clinical sco-
ring system (RDS Score) with acid-
base and blood-gas correlction. Clin
Pediatr 1970, 9: 325.
5. Boros SJ, Reynolds JW. Hyaline mem-
brane disease treated with early nasal
and expiratory pressure: One year's
experience. Pediatrics 1975, 56:' 218-
223.
6. Jennis MS, Peabody JL. Pulse
oximetry: An alternative method of
assessment of oxygenation in newborn
infants. Pediatrics 1987, 79: 524-527.
7. Ramnathan R, Durand M, Larrazabal
C. Pulse oximetry in very low birth
weight infants with acute and chronic
lung disease. Pediatrics 1978, 79: 612-
616.
8. Fanconi S, Doherty P, Edmonds JF, et
al. Pulse oximetry in pediatric inten-
sive care: Comparison with measured
saturations and transcutaneous oxy-
gen tension. J Pediatr 1985, 107: 362-
366.
211
