1
Washington - Health Care Benefit Manager (HCBM) Disclosure
Washington law, under Rule 21-02-034/WAC 284-180-325, requires carriers to post on their website
information that identifies each HCBM contracted with them and identify the services provided by
the HCBM.
Health Care Benefits Manager means a person or entity providing services to, or acting on behalf of,
a health carrier or employee benefits programs, that directly or indirectly impacts the determination or
utilization of benefits for, or patient access to, health care services, drugs, and supplies including, but
not limited to:
• Prior authorization or preauthorization of benefits or care
• Certification of benefits or care
• Medical necessity determinations
• Utilization review
• Benefit determinations
• Claims processing and repricing for services and procedures
• Outcome management
• Provider credentialing and recredentialing
• Payment or authorization of payment to providers and facilities for services or procedures
• Dispute resolution, grievances, or appeals relating to determinations or utilization of benefits
• Provider network management or
• Disease management
Health Care Benefit Manager also includes, but is not limited to, HCBMs that specialize in specific types
of health care benefit management such as pharmacy benefit managers, radiology benefit managers,
laboratory benefit managers and mental health benefit managers.
Below is a listing of the HCBMs we contract with, carriers and the services they provide.
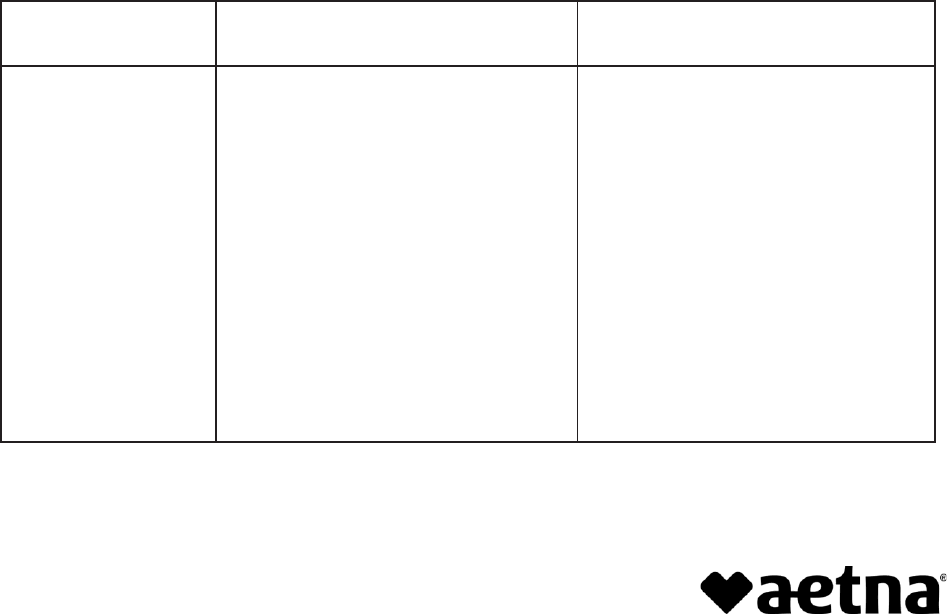
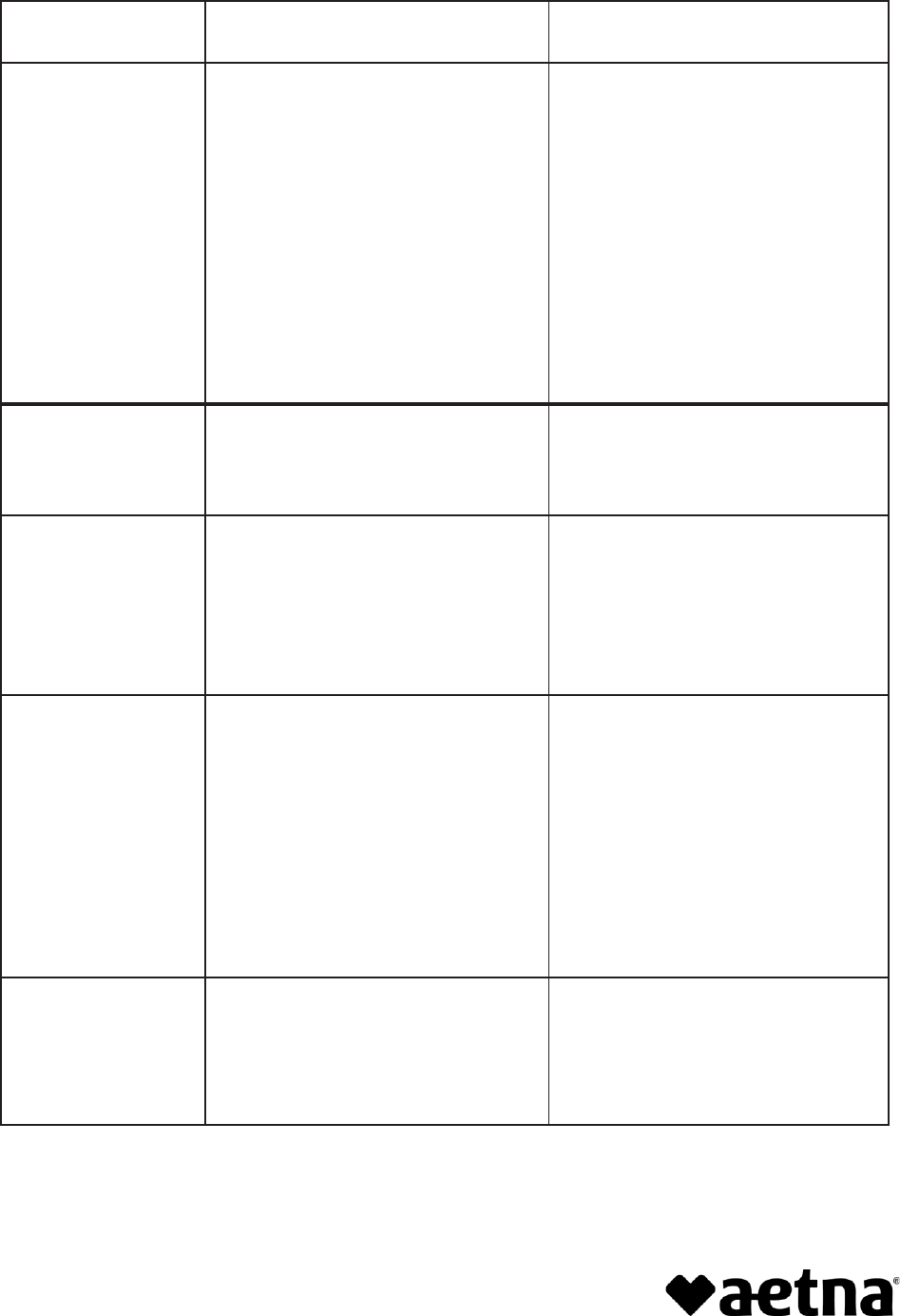
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
Aetna Health
Management
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company (ALIC)
• First Health Life & Health Insurance
Company
• Benefit determinations
• Claims processing or repricing
• Credentialing
• Disease management
• Dispute resolution, grievance,
appeals (related to benefits)
• Outcome management
• Payment/authorization of payment
to providers
• Provider network management
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
Health insurance plans are offered, underwritten and/or administered by Aetna Life Insurance
Company (Aetna).
912116-01-01 (1/22)
2
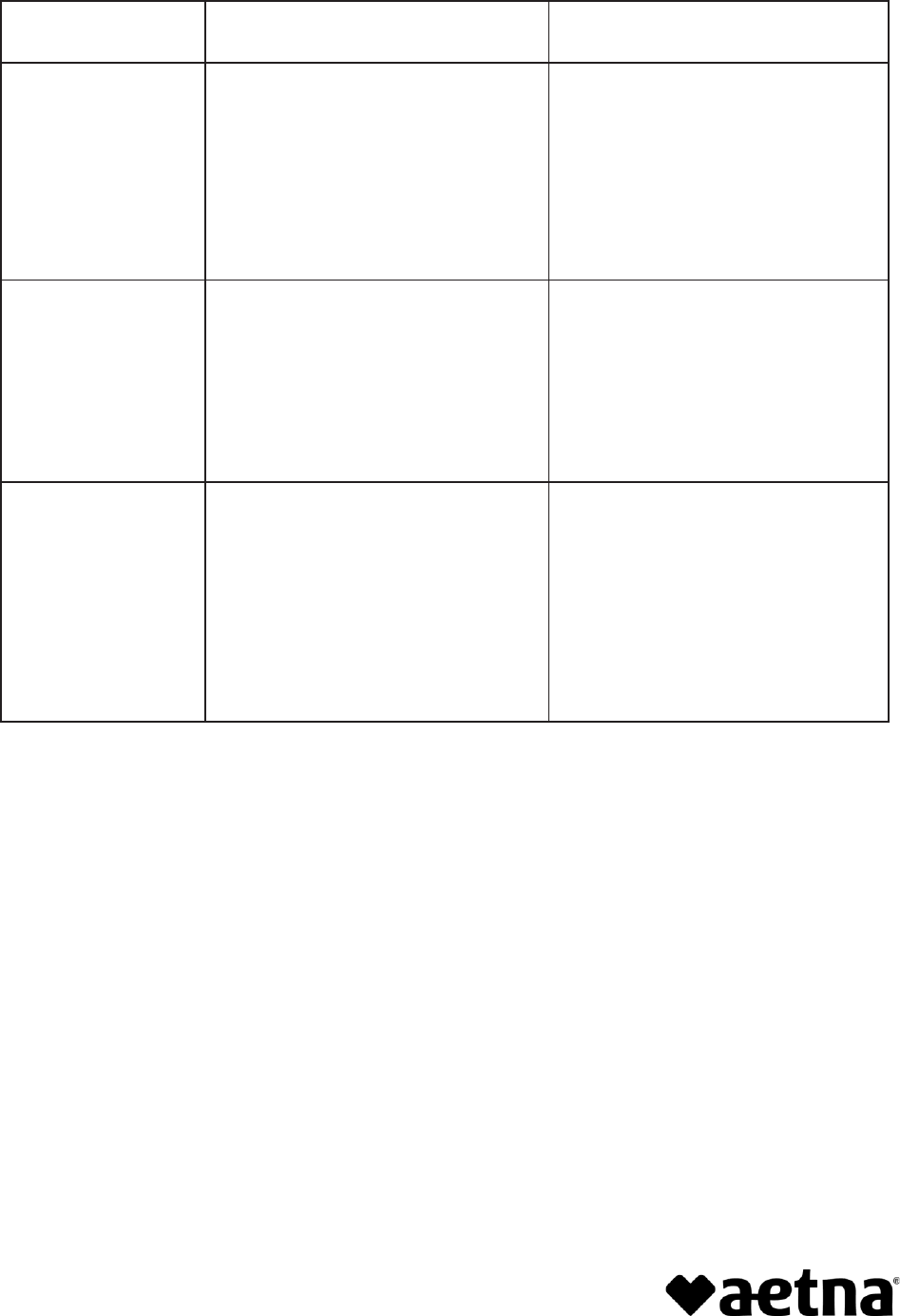
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
Aetna Network
Services
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company (ALIC)
• First Health Life & Health Insurance
Company
• Provider network management
American Health
Holding
• Continental Life Insurance Company
of Brentwood, Tennessee
• Disease management
• Dispute resolution, grievance,
appeals (related to benefits)
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
American Specialty
Health Network
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company (ALIC)
• First Health Life & Health Insurance
Company
• Claims processing or repricing
• Credentialing
• Payment/authorization of payment
to providers
• Provider network management
services
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
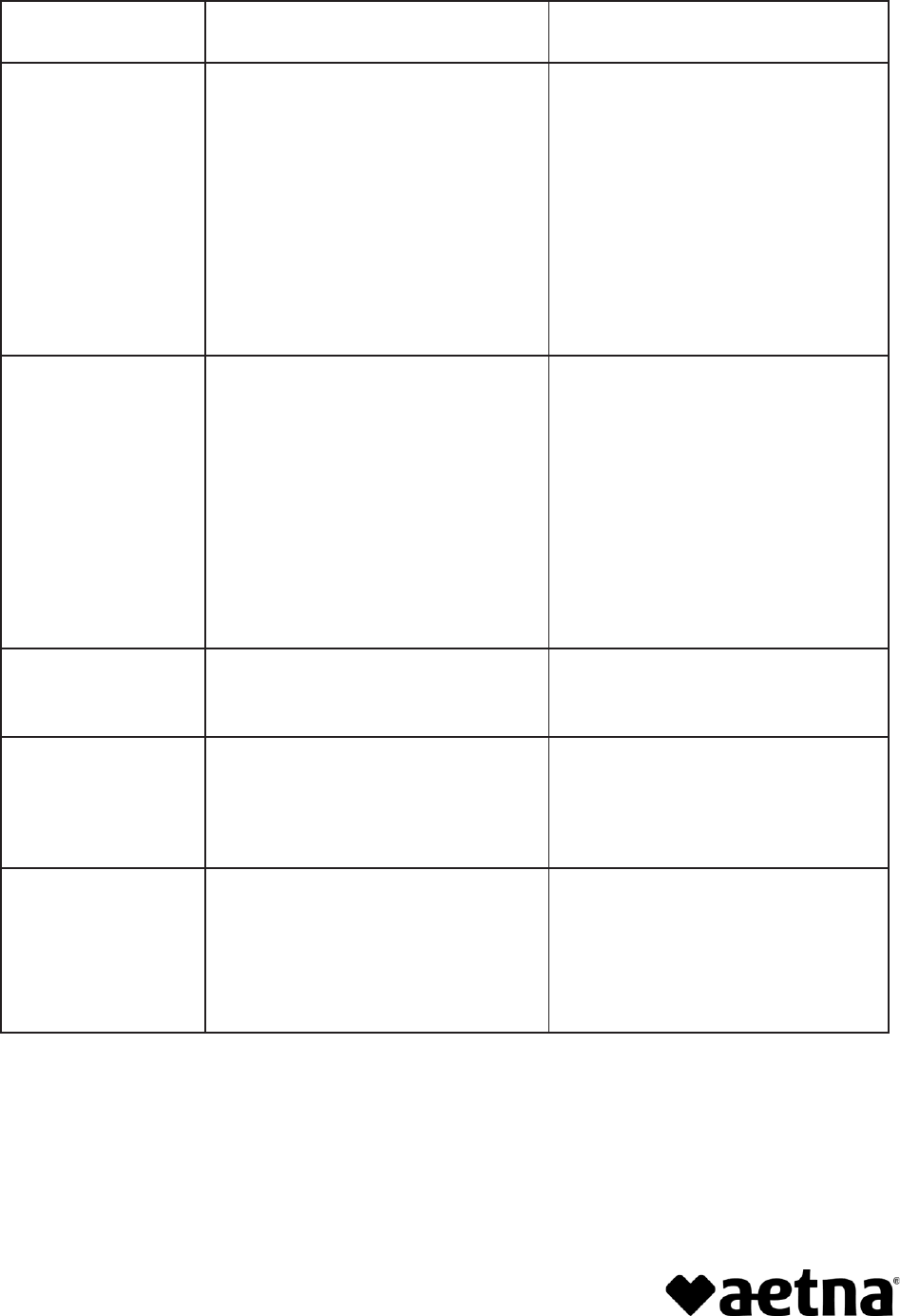
3
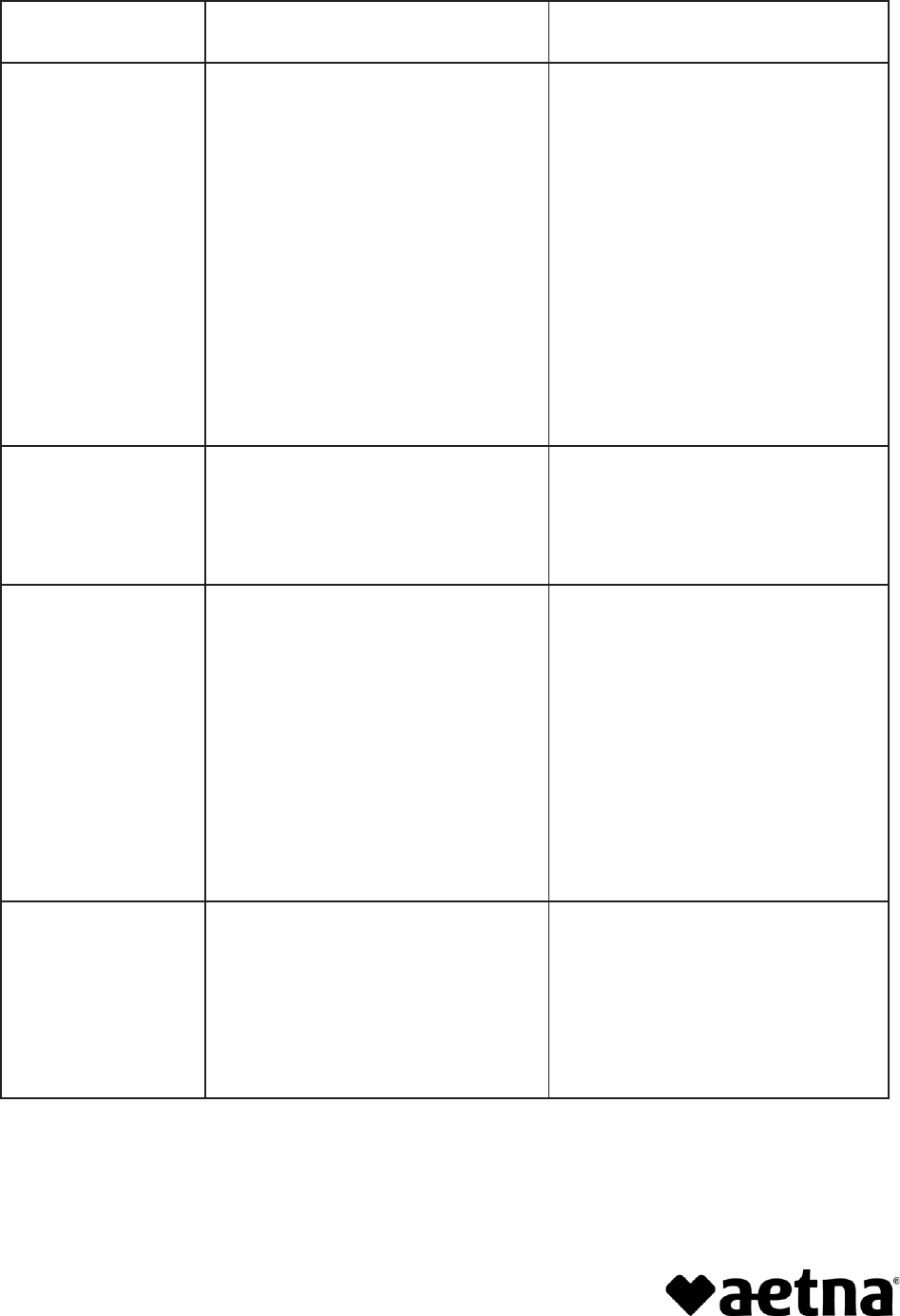
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
Amplifon
• Accendo Insurance Company
• Aetna Better Health of Washington
(ABH)
• Aetna Health and Life Insurance
Company
• Aetna Health Inc. (AHI)
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company (ALIC)
• Continental Life Insurance Company
of Brentwood, Tennessee
• First Health Life & Health Insurance
Company
• Claims processing or repricing
Careington
International
Corp
• Aetna Life Insurance Company (ALIC)
• Provider network management
service
• Provider credentialing and
recredentialing
Caremark PCS
Health LLC
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company (ALIC)
• First Health Life & Health Insurance
Company
• Benefit determinations
• Claims processing or repricing
• Credentialing
• Dispute resolution, grievance,
appeals (related to benefits)
• Payment/authorization of payment
to providers
• Provider network management
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
Concentrix Daksh
Services India Private
Limited
• Aetna Life Insurance Company
(ALIC)
• Claims processing or repricing
• Dispute resolution, grievance,
appeals (related to benefits)
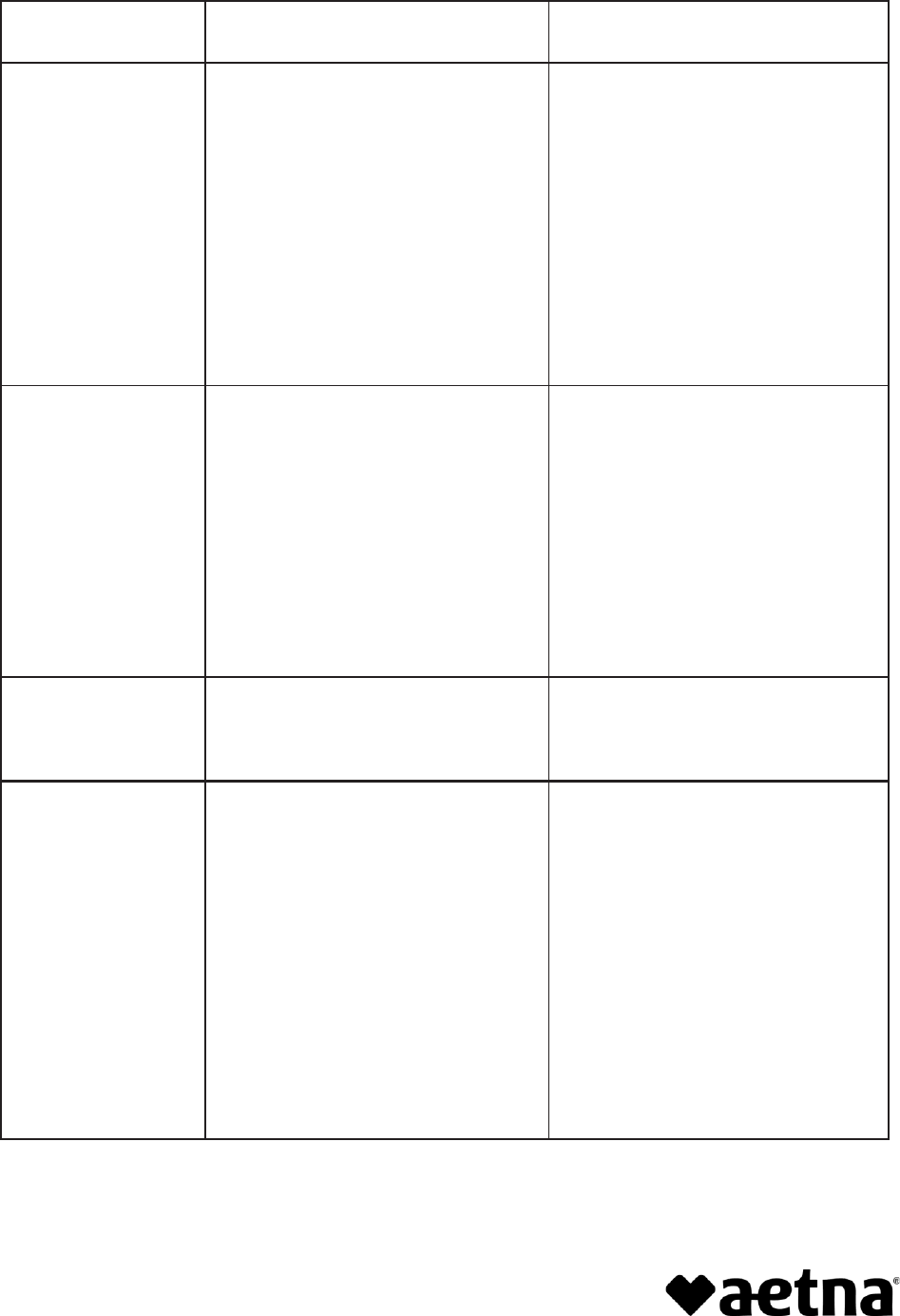
4
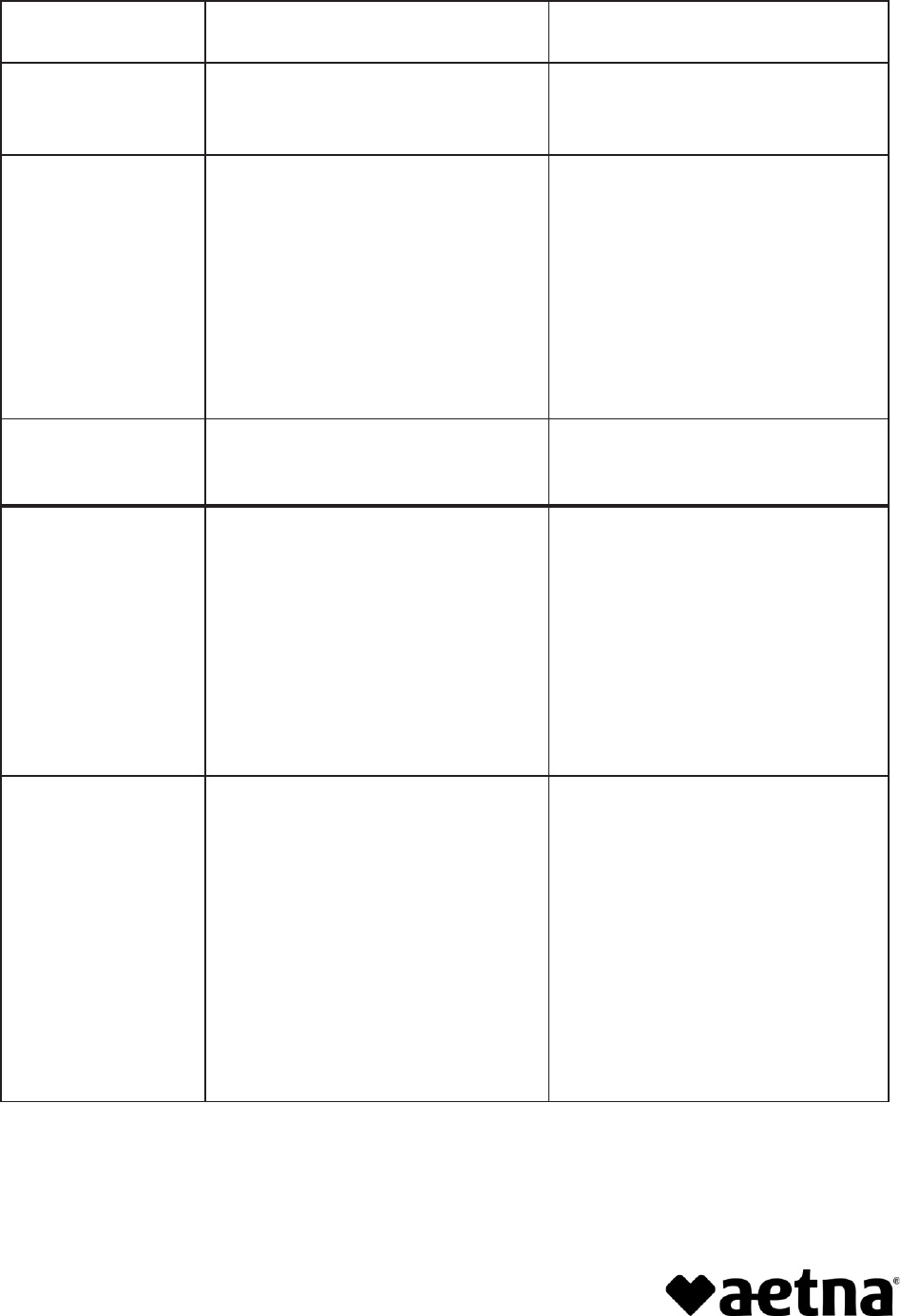
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
Cotiviti, Inc.
• Aetna Life Insurance Company (ALIC)
• Coordination of benefits/benefit
determinations
CVS Health Solutions
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Disease management
• Payment/authorization of payment
to providers
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
Dental Health
Alliance LLC
• Aetna Life Insurance Company
(ALIC)
• Credentialing for dental
• Provider network management
Eleanor Health
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Credentialling for Behavioral Health
• Disease management
EviCore
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Utilization management (prior
authorization, certification of
benefits or care, medical
necessity determinations)
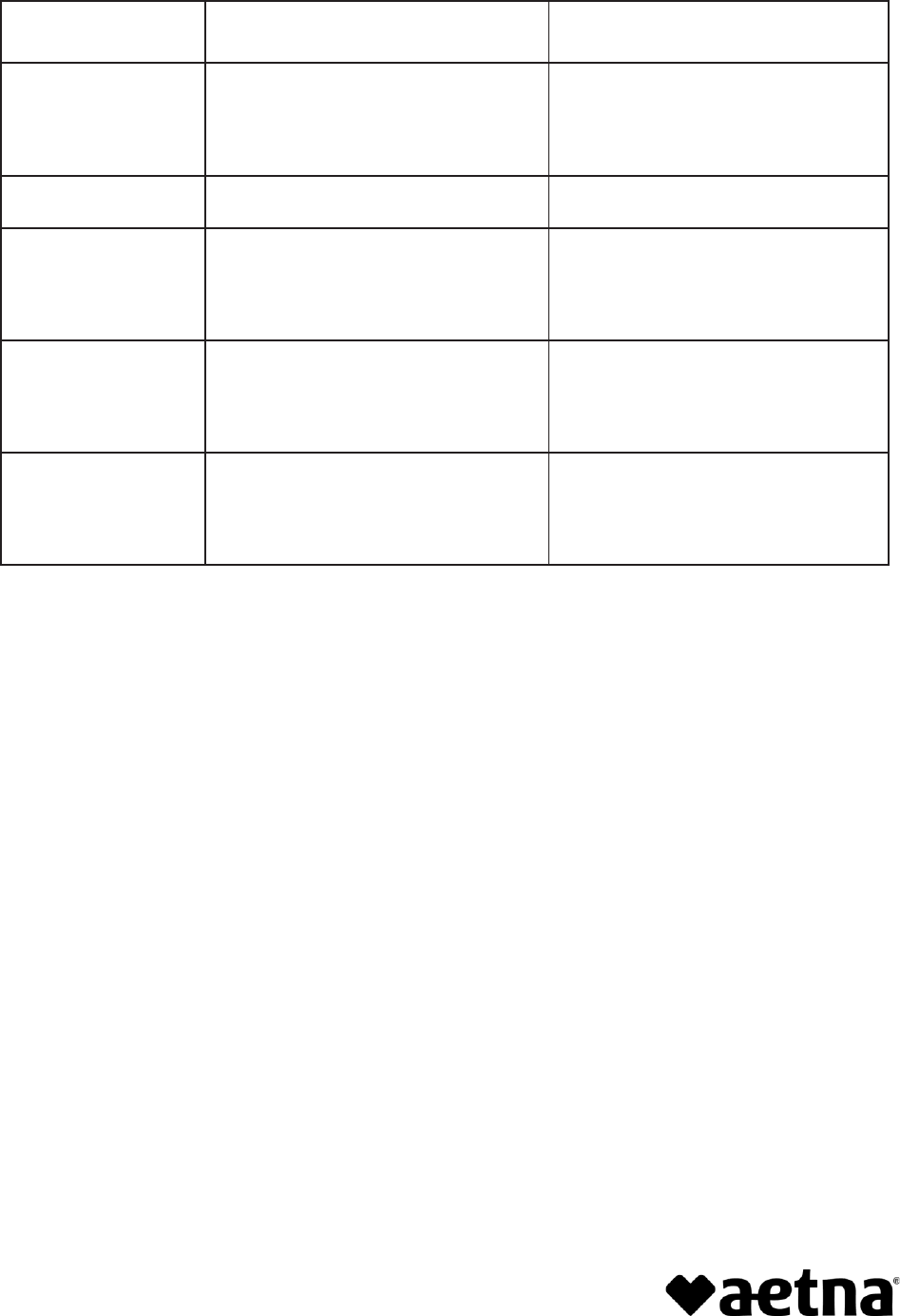
5
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
ExlService
Philippines, Inc.
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• Aetna Health & Life Insurance
Company
• Accendo Insurance Company
• Continental Life Insurance Company
of Brentwood, Tennessee
• First Health Life & Health Insurance
Company
• Benefit determinations
• Claims processing or repricing
• Dispute resolution, grievance,
appeals (related to benefits)
• Outcome management
• Payment/authorization of payment
to providers
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
EyeMed
• Aetna Health Inc. (AHI)
• Aetna Life Insurance Company
(ALIC)
• Claims processing or repricing
• Credentialing for network
• Provider network management
First American
Administrators
• Aetna Health Inc. (AHI)
• Aetna Life Insurance Company
(ALIC)
• Claims processing or repricing
First Health Group
Corp
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Claims processing or repricing
• Provider network management
Government
Employees Health
Association, Inc.
(GEHA)
• Aetna Life Insurance Company
(ALIC)
• Provider network management
service
• Provider credentialing and
recredentialing
6
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
HealthHelp, LLC
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• Continental Life Insurance Company
of Brentwood, Tennessee
• First Health Life & Health Insurance
Company
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
• Claims processing or repricing
Hearing Care
Solutions
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Life Insurance Company
(ALIC)
• AHIC (Aetna Health Insurance
Company)
• Continental Life Insurance Company
of Brentwood, Tennessee
• First Health Life & Health Insurance
Company
• Claims processing or repricing for
network
HGS Healthcare, LLC
• Aetna Life Insurance Company
(ALIC)
• Claims processing or repricing
• Dispute resolution, grievance,
appeals (related to benefits)
Infosys
• Aetna Life Insurance Company
(ALIC)
• Dispute resolution, grievance,
appeals (related to benefits)
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
Medical Review
Institute of America,
LLC
• Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• UM (prior authorization, certification
of benefits or care, medical
necessity determinations)
• Dispute resolution, grievance,
appeals (related to benefits)
7
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
MediCall d.b.a.
Cognizant Technology
Solutions
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• Continental Life Insurance Company
of Brentwood, Tennessee
• First Health Life & Health Insurance
Company
• Claims processing or repricing
• Payment/authorization of payment
to providers
• UM (prior authorization,
certification of benefits or care,
medical necessity determinations)
Multi-Plan
• Accendo Insurance Company
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Claims processing or repricing
• Provider network management
OptumInsight, Inc.
• Aetna Life Insurance Company
(ALIC)
• Coordination of benefits/benefit
determinations
Sprata Behavioral
Services
• Accendo Insurance Company
• Aetna Behavioral Health of
Washington (ABH)
• Aetna Health and Life Insurance
Company
• Aetna Health Insurance Company
(AHIC)
• Aetna Life Insurance Company
(ALIC)
• First Health Life & Health Insurance
Company
• Credentialling for Behavioral Health
network
8
Health Care Benefit
Manager (HCBM)
Carrier/Insurer
Services the HCBM
Provides
Talkspace Network
• Aetna Health Inc. (AHI)
• Aetna Life Insurance Company (ALIC)
• Aetna Behavioral Health of
Washington (ABH)
• Credentialling for Behavioral Health
network
Teladoc
• Aetna Life Insurance Company
(ALIC)
• Credentialling
The Rawlings
Company, LLC
• Aetna Life Insurance Company (ALIC)
• Coordination of benefits/benefit
determinations
Tivity Health
DBA Healthways
WholeHealth
Networks, Inc.
• Aetna Health Inc. (AHI)
• Aetna Life Insurance Company (ALIC)
• Aetna Behavioral Health of
Washington (ABH)
• Credentialling for network
• Provider network management
Zelis
Healthcare, LLC
• Aetna Life Insurance Company (ALIC)
• Provider credentialling
• Provider network management

9
Aetna complies with applicable federal civil rights laws and does not unlawfully discriminate, exclude or
treat people differently based on their race, color, national origin, sex, age, or disability.
We provide free aids/services to people with disabilities and to people who need language assistance.
If you need a qualified interpreter, written information in other formats, translation or other services, call
the number on your ID card.
If you believe we have failed to provide these services or otherwise discriminated based on a protected
class noted above, you can also file a grievance with the Civil Rights Coordinator by contacting:
Civil Rights Coordinator,
P.O. Box 14462, Lexington, KY 40512 (CA HMO customers: PO Box 24030 Fresno, CA 93779),
1-800-648-7817, TTY: 711,
Fax: 859-425-3379 (CA HMO customers: 860-262-7705).
You can also file a civil rights complaint with the U.S. Department of Health and Human Services,
Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or at:
U.S. Department of Health and Human Services, 200 Independence Avenue SW., Room 509F,
HHH Building, Washington, DC 20201, or at 1-800-368-1019, 800-537-7697 (TDD).

10
TTY: 711
To access language services at no cost to you, call
1-888-982-3862
.
Para acceder a los servicios de idiomas sin costo, llame al 1-888-982-3862. (Spanish)
如欲使用免費語言服務,請致電
1-888-982-3862
。(Chinese)
Afin d'accéder aux services langagiers sans frais, composez le
1-888-982-3862
. (French)
Para ma-access ang mga serbisyo sa wika nang wala kayong babayaran, tumawag sa 1-888-982-3862 .
(Tagalog)
Um auf für Sie kostenlose Sprachdienstleistungen zuzugreifen, rufen Sie 1-888-982-3862 an. (German)
3862-982-888-1
.(Arabic)
Pou jwenn sèvis lang gratis, rele 1-888-982-3862 . (French Creole-Haitian)
Per accedere ai servizi linguistici, senza alcun costo per lei, chiami il numero 1-888-982-3862 . (Italian)
言語サービスを無料でご利用いただくには、1-888-982-3862
までお電話ください。(Japanese)
무료 언어 서비스를 이용하려면
1-888-982-3862
번으로 전화해 주십시오. (Korean)
3862-982-888-1
.
)
Farsi
-
Persian
(
Aby uzyskać dostęp do bezpłatnych usług językowych proszę zadzwonoć
1-888-982-3862
. (Polish)
Para acessar os serviços de idiomas sem custo para você, ligue para
1-888-982-3862
. (Portuguese)
Для того чтобы бесплатно получить помощь переводчика, позвоните по телефону
1-888-982-3862
.
(Russian)
Nếu quý vị muốn sử dụng miễn phí các dịch vụ ngôn ngữ, hãy gọi tới số
1-888-982-3862
. (Vietnamese)
©2022 Aetna Inc.
912116-01-01 (1/22)
