
ABA Provider Orientation

We will cover…
• Introduction to Amerigroup
• Overview of Amerigroup Services
• How to become an Amerigroup Provider
• Expectations for Credentialing

Introduction to Amerigroup

Our Beginning and Mission

Our Members by Market
Ohio
New Jersey
Louisiana
Florida Maryland Georgia
Nevada
New York
Texas
Tennessee
New Mexico
Washington
Kansas

Overview of Amerigroup Services

providers.amerigroup.com
The provider website is
available to all
providers, regardless of
participation status.
The tools on the site
allow you to perform
key transactions.
8
Translation Services
24 hours a day
7 days a week
Over 170 languages

9
Member Enrollment
New York
New Jersey
Maryland
Ohio
Virginia
Tennessee
Georgia
Florida
Texas
New Mexico
Nevada
Louisiana
Washington

Nevada Member ID Card

Our Service Partners
Please refer to the provider
manual/handbook for a list of
service partners, contact
information and more information
about member benefits.
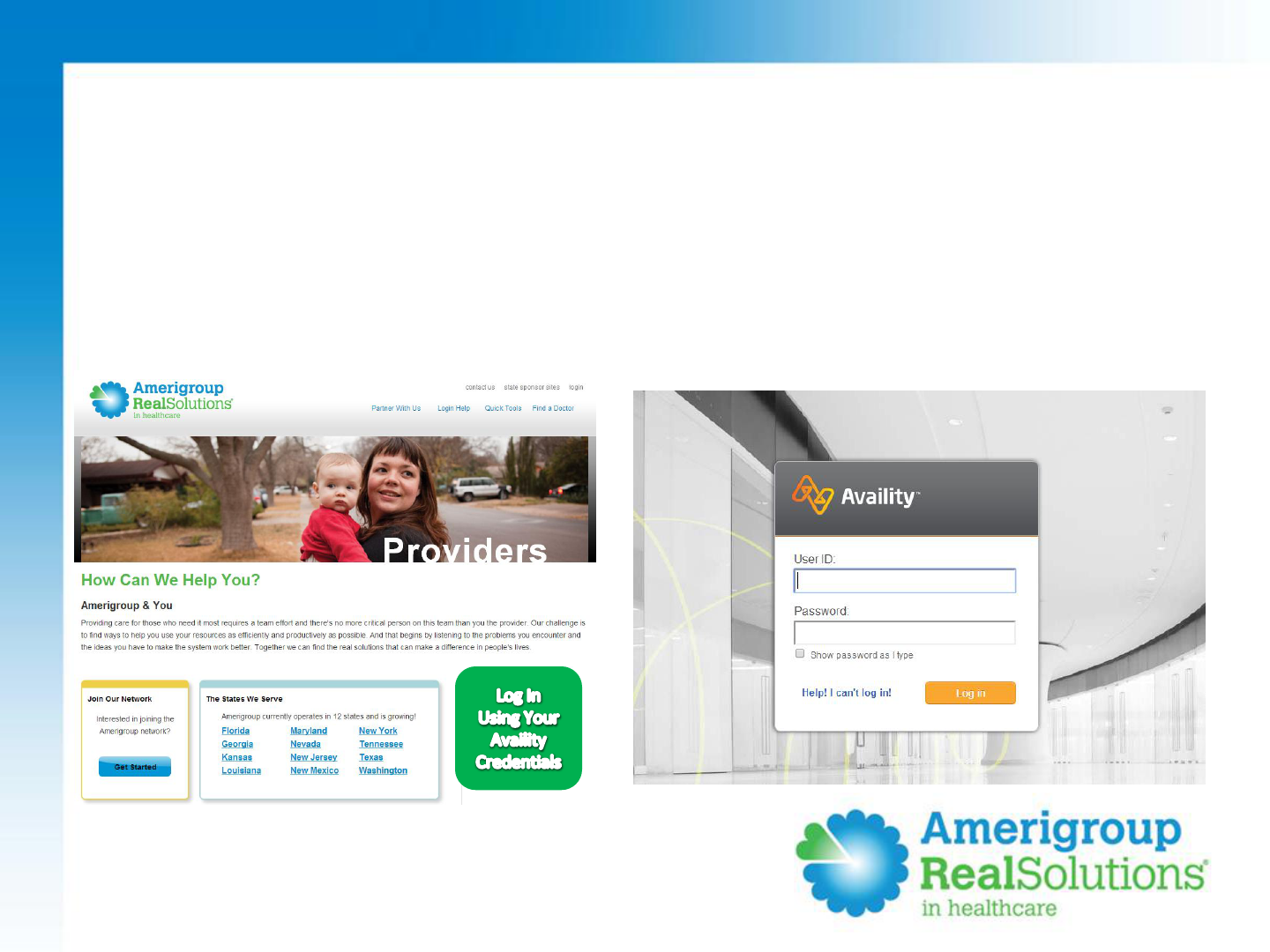
Availity
• Providers can access secure functionality in two ways:
Providers.Amerigroup.com
www.Availity.com

14
Electronic Payment Services
If you sign up for ERA/EFT, you can:
• Start receiving ERAs and import the
information directly into your
patient management or patient
accounting system
• Route EFTs to the bank account of
your choice
• Create your own custom reports
within your office
• Access reports 24 hours a day, 7 days
a week

15
Your Support System
Provider Relations
Medical Management
Provider Services
Patient 360

• Asthma
• Bipolar disorder
• Congestive heart failure
• COPD
• Diabetes
• HIV/AIDS
• Major depressive disorder
• Obesity
• Schizophrenia
• Transplants
• And more!
We offer programs for
members living with:
Disease Management

Quality Management
Our Quality
Management team
continually analyzes
provider performance
and member outcomes
for improvement
opportunities.
If your provider group would like
training in HEDIS measures, please call:
Candice Speers
702-228-1308

How to become an Amerigroup
Provider

Contracting
Contracting
• Submit a letter of intent
• Submit a copy of your current W9
For new providers, Contracting and Credentialing
occurs simultaneously.
E:mail
nv1provsvcs@amerigroup.com
Facsimile
1-866-495-8711

Contracting
Contracting
• Submit a letter of intent
• Where is the practice located
• How long has the organization been in business
• Indicate your approved Nevada Medicaid Provider Type
• Describe your Quality Management Program
• What services are provided
• Submit a copy of your current W9
For new providers, Contracting and Credentialing
occurs simultaneously.

Contracting
For new providers, Contracting and Credentialing
occurs simultaneously.
Contracting
• Submit a letter of intent
• Submit a copy of your current W9
• Assure the W9 is completed correctly
• Name as shown on your Income Tax Return
• d/b/a
• Signed and Dated

Complete Sections 1-6
Complete Part 1
Sign and Date Part 2

Contracting
Contract
• Review agreement to ensure your legal name and d/b/a
are listed correctly
Credentialing Documents
• Ensure Credentialing Documents are completed in their
entirety
• Ensure that a Disclosure of Ownership Form is
included for the Group/Facility/Practitioner
Contracting Specialist will send a configured agreement
along with the required credentialing documents

Contracting
Contract
• Return the signed contract in its entirety to the Contracting
Specialist
Credentialing Documents
• Return the completed credentialing documents in their
entirety to the Contracting Specialist
Contracting Specialist will send a configured agreement
along with the required credentialing documents

Question and Answers

Expectations for Credentialing
ABA providers
The below providers will submit a NV Standard application:
• Licensed Board Certified Behavior Analysts (BCBA)
• Licensed Psychologists
• Licensed and Board Certified Assistant Behavior Analysts
(BCaBA)
The below providers will be submitted on a roster:
• Certified Autism Behavior Interventionists (CABI)*
• Registered Behavior Technicians (RBT)*
* Must be supervised by a qualified licensed practitioner. The
licensed practitioner must be fully credentialed.

Credentialing Updates
Notify Amerigroup’s Local Credentialing Team when:
• Adding a new provider to your practice
• A provider has left your practice
• Your practice changes TIN
NVCredentialing@Amerigroup.com

Re-Credentialing
• Providers are re-credentialed every three years (36 months).
• Amerigroup begins the re-credentialing process eight
months in advance of the provider’s 36-month re-
credentialing due date.
• To avoid termination, providers must return all requested
materials within 120 days of their re-credentialing due date.

Disclosure of Ownership (DOO)
In order to be initially credentialed or re-credentialed,
providers must ensure a completed DOO is on file with
Amerigroup.
The DOO must be signed within the last three years.
• Entity DOO – is completed for the group
• Provider Person DOO – is completed for providers in a
private practice

Ongoing Credentialing
Please notify us if you
have any changes in
licensure, demographics
or participation status.
NVCredentialing@
Amerigroup.com

Claim Submission Tips
COMPANY CONFIDENTIAL | FOR INTERNAL USE ONLY | DO NOT COPY

The individual providers name must be billed in field 31 of the CMS 1500
The individual providers NPI must be on the claim form in field 24J
COMPANY CONFIDENTIAL | FOR INTERNAL USE ONLY | DO NOT COPY
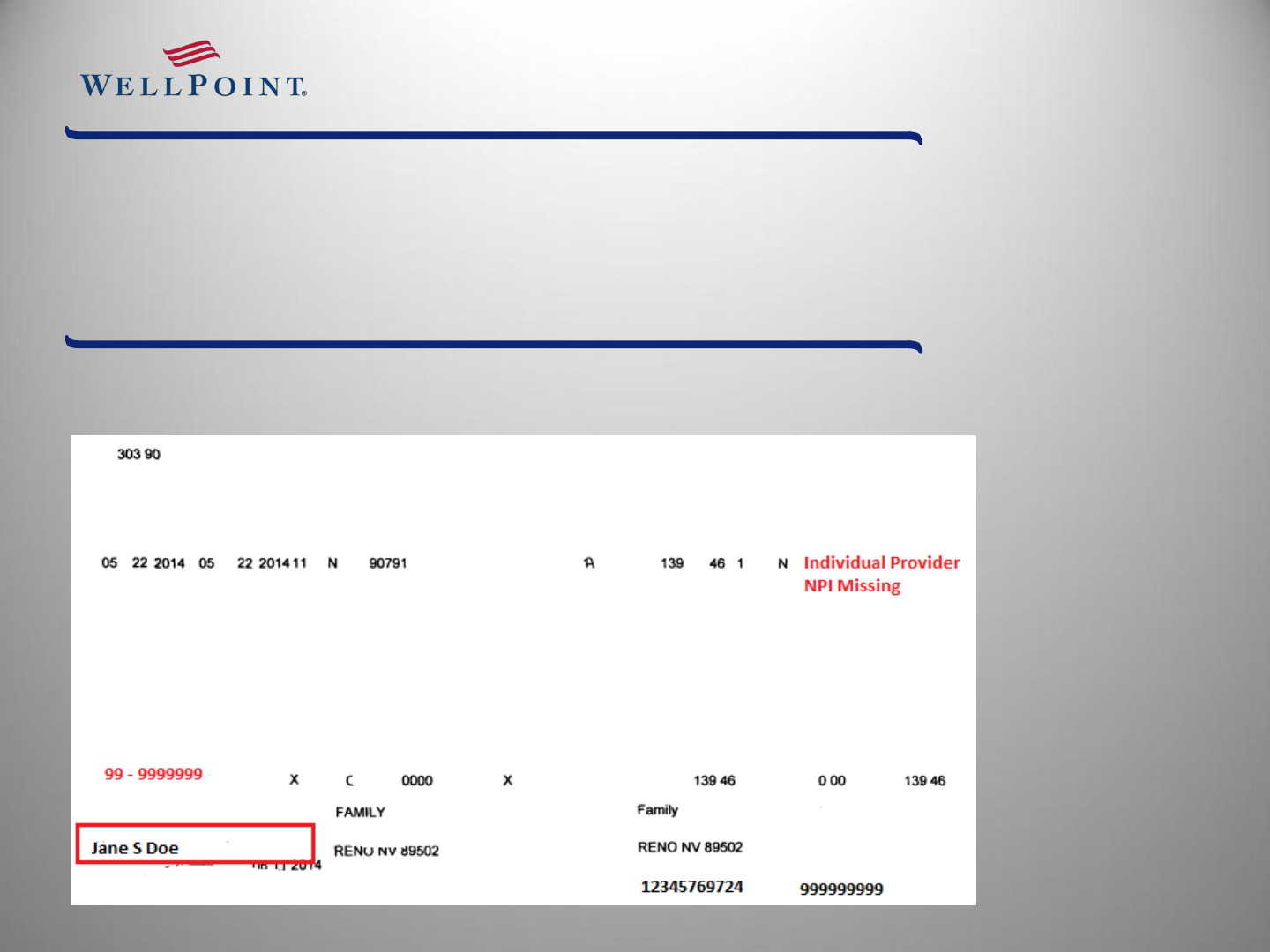
Even if the individual providers name has been billed in field 31 of the CMS
1500 the NPI for the individual provider must still be on the claim form in
field 24J
COMPANY CONFIDENTIAL | FOR INTERNAL USE ONLY | DO NOT COPY
Exp: Providers name is Jane S Doe but we do not have her NPI

Corrected Claims must be marked “Corrected Claim”
COMPANY CONFIDENTIAL | FOR INTERNAL USE ONLY | DO NOT COPY
• Exp: Corrected Claim can be stamped or handwritten on the claim. If
it’s not included on the claim, the claim could be denied as a duplicate.
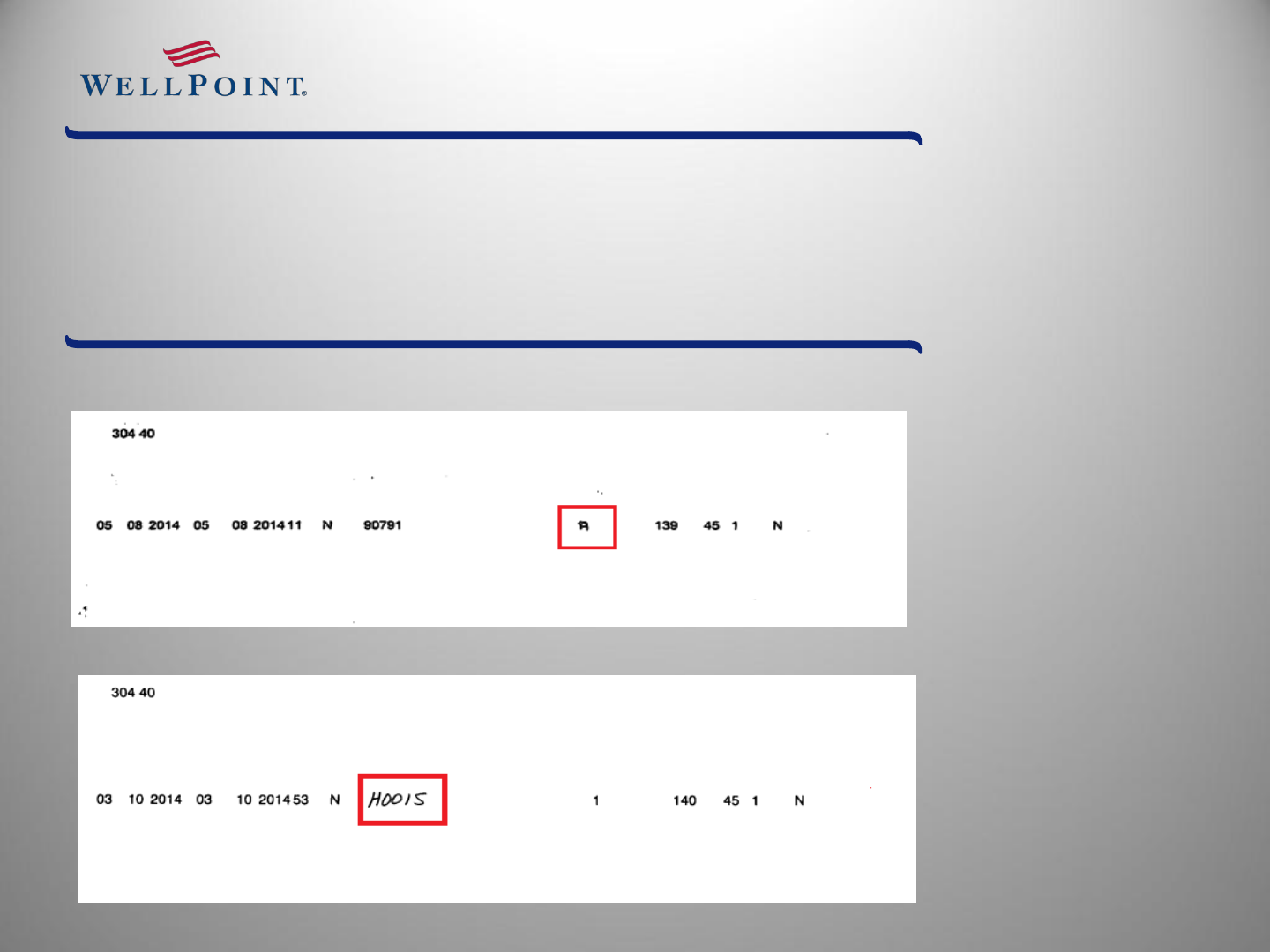
Claims that have been altered will not be processed. If the claim is typed then
the entire claim must be typed. We can’t accept a typed claim with a
handwritten unalterable field.
COMPANY CONFIDENTIAL | FOR INTERNAL USE ONLY | DO NOT COPY
• Exp: The claim below was typed but the diagnosis pointer was handwritten.
• Exp: The claim below was typed but the HCPCS Code was handwritten.

Closing

Contact Information
Contracting Manager:
TJ Dahna
702-228-1308
nv1provsvcs@amerigroup.com
Credentialing Specialists:
Krystl Sloan & Michele Loyd
702-228-1308
nvcredentialing@amerigroup.com
Provider Relations Team:
nv1provsvcs@amerigroup.com
Facsimile: 1-866-495-8711
Provider Relations Manager:
Jaime Collins
Jaime.Colli[email protected]

Thank you for partnering with



