
Cover Image
This report provides data and analysis on Covered California’s efforts to improve the performance of
California’s health care system and to ensure that its members receive affordable, high-quality care.
The people featured on the cover are individuals who have benefited from these efforts. Their stories —
and those of others told here: https://www.coveredca.com/real-stories/ — go beyond the data to provide
personal perspectives on what Covered California has achieved over the past five years.
This document is in the public domain and may be copied or reproduced without permission.
Suggested citation: Covered California. (2019). Covered California Holding Health Plans Accountable
for Quality and Delivery System Reform.

Foreword
The Affordable Care Act opened the door to quality care for millions of Americans who had previously
been shut out of our health care system. A companion to this report, “Covered California’s First Five
Years: Improving Access, Affordability and Accountability”, provides an overview of how California —
the state government, Covered California, and other stakeholders — are working together to use the
tools provided by the Affordable Care Act to lower costs for consumers and provide meaningful choice
and coverage that truly meets consumers’ needs. The state is now building on and going beyond the
Affordable Care Act on the path toward universal coverage.
This report details how for more than five years, Covered California has held itself accountable as a
public entity charged with assuring consumers get the right care at the right time, while we hold the 11
health insurance companies we have chosen to contract with accountable for making sure that
consumers receive high-quality care and that both insurers and providers are implementing the delivery
system reforms needed to improve care for all Californians.
For Covered California, accountability means making sure health plans are meeting consumers’ needs
today and seeing that they are taking concerted and deliberate action to improve how health care is
paid for, organized and delivered in California. The goal of this accountability is to have a health care
system that truly addresses the triple aim of improving health, delivering better-quality care and
lowering costs.
This report focuses on how contracted health insurers are held accountable for assuring quality care
and for promoting delivery system reform. Chapter 1 describes the framework that now guides this
work. Chapters 2 through 6 describe how Covered California holds insurers accountable for assuring
quality care, including not only the specific measures used to track performance, but also the progress
that has been made overall and by individual insurers on these measures. Chapters 8 through 11 then
summarize the approaches to holding each health insurer accountable for advancing health care
delivery reform.
We share this report not because we believe our work is done, but rather because it is just beginning.
Improving health care quality and lowering underlying health costs is long-term pursuit. That pursuit is
central to Covered California’s mission, and this report identifies progress made and areas of needed
attention as we move forward.
Peter V. Lee
Executive Director
Covered California Holding Health Plans Accountable for Quality
and Delivery System Reform
Table of Contents
Chapter 1: Covered California’s Framework for Assuring Quality Care and Promoting
Delivery System Reform ................................................................................................................. 1
ASSURING QUALITY CARE ......................................................................................................... 6
Chapter 2: Individualized, Equitable Care — Best Possible Care for All ....................................... 6
Chapter 3: Health Promotion and Prevention .............................................................................. 25
Chapter 4: Mental Health and Substance Use Disorder Treatment ............................................ 34
Chapter 5: Acute, Chronic and Other Conditions ......................................................................... 43
Chapter 6: Complex Care ............................................................................................................. 52
EFFECTIVE CARE DELIVERY .................................................................................................... 59
Chapter 7: Promotion of Effective Primary Care .......................................................................... 59
Chapter 8: Promotion of Integrated Delivery Systems and Accountable Care Organizations .... 66
Chapter 9: Networks Based on Value .......................................................................................... 73
Chapter 10: Appropriate Interventions ......................................................................................... 79
Chapter 11: Sites and Expanded Approaches to Care Delivery .................................................. 89
Chapter 12: Summary and Implications for the Future .............................................................. 102
APPENDICES ............................................................................................................................. 103
Appendix 1: Limitations and Major Caveats about Health Disparities Data .............................. 104
Appendix 2: Additional Health Plan Measures Reported to Quality Rating System ................. 105
Appendix 3: 2019 Marketplace Quality Rating System Measure Set ........................................ 139
Appendix 4: Additional Publicly Reported Hospital Quality and Safety Data ............................ 141
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
CHAPTER 1
COVERED CALIFORNIA 1
Chapter 1: Covered California’s Framework for Assuring Quality Care and
Promoting Delivery System Reform
Covered California’s current contract requirements with qualified health plan (QHP) issuers (also
referred to as “health insurance companies”, “insurers” or “health plans” in this report)
1
are laid out in
Attachment 7: Quality, Network Management, Delivery System Standards and Improvement Strategy of
the QHP issuer contract. The contract is designed to hold insurers accountable for ensuring that people
get the right care at the right time and that care is individualized for their specific needs, while seeking
to improve how care is delivered and promoting care that is increasingly high-quality, equitable and
cost-effective.
2
The current Attachment 7 is composed of nine articles; each article has a distinct focus, including
ensuring networks are based on value and reducing health disparities. In addition, multiple articles have
elements related to quality improvement, network management and delivery system reform
requirements. Attachment 7 includes a number of initiatives that require concerted, multi-year efforts of
health insurance companies across the California delivery system. Insurers report annually and as part
of quarterly review meetings with Covered California on their Attachment 7 performance. Covered
California staff review and assess the information submitted for both contract compliance purposes and
to assess the success of the Attachment 7 initiatives in achieving the priority outcomes of quality care
and effectively delivering that care.
Covered California is working to update its health insurance company contract terms for the 2022-2024
plan years and is seeking to refresh its requirements for the future that continue to address the “Triple
Aim” of lowering costs, improving quality and improving health outcomes, with a focus on reducing
health disparities. This update will include a revised framework for Attachment 7 that is organized and
composed of two main strategies: Assuring Quality Care and Effective Care Delivery. This report
describes the progress Covered California contracted health insurance companies have made between
2014 and 2019
3
in implementing the requirements within the current Attachment 7 organized by the
revised framework described in Figure 1. Covered California’s Framework for Holding Plans
Accountable for Quality Care and Delivery Reform Framework.
Assuring Quality Care
Covered California is committed to ensuring that care is individualized and equitable for not only those
people currently needing or receiving treatment, but for those who are working to stay healthy. The
1
The term “health insurance companies” or “insurers” refers to the organizations providing health coverage and “health plan” refers to the
health coverage products they provide, such as an HMO plan vs. a PPO plan.
2
Beginning with the inaugural 2014 plan year and updated in 2017, Covered California set forth standards and strategies for quality
improvement and delivery system reform in its QHP issuer contract, specifically in the section of the contract titled “Attachment 7: Quality,
Network Management, Delivery System Standards and Improvement Strategy”. See more: https://hbex.coveredca.com/insurance-
companies/PDFs/Attachment-7_2020_Clean_Final-Model.pdf.
3
This report does not include data for plan year or measurement year 2014; rather it describes the progress Covered California contracted
health insurance companies have made since 2014 on Attachment 7 requirements with the first year of data representing plan year or
measurement year 2015 for most requirements.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
CHAPTER 1
COVERED CALIFORNIA 2
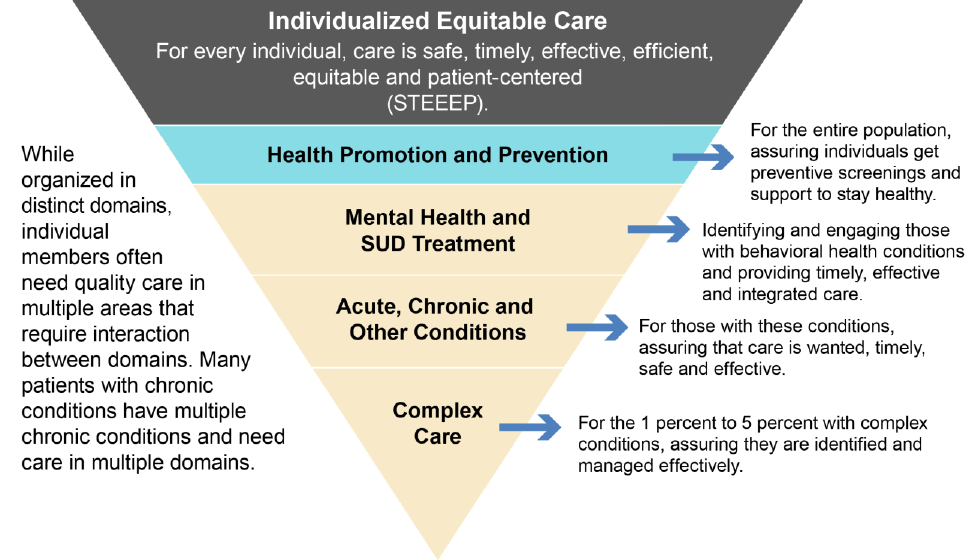
Figure 1. Covered California’s Framework for Holding Plans Accountable for Quality Care and Delivery
Reform Framework
concept of individualized, equitable care
4
means regardless of one’s circumstances, race, gender,
where one lives or other socioeconomic factors — and for some decisions where more than one
evidence-based treatment is available, based on one’s values and preferences — every individual
deserves the best possible care that is personalized for them and delivered in the right setting at the
right time, does not cause harm and is the most cost-effective possible. These goals are consistent with
the six domains of health care quality identified by the Institute of Medicine:
5
safe, timely, effective,
efficient, equitable and patient-centered (STEEEP). In addition to assuring quality care for those
insured through the marketplace, Covered California will continue its efforts to identify and reduce racial
and ethnic health disparities for the entire population.
What follows are the organizing domains for assuring quality care beyond the cross-cutting concept that
all care should be individualized and equitable:
• Health promotion and prevention: Everyone is encouraged to receive preventive care
services and health screenings and use support tools that promote a healthy lifestyle. This
includes everything from regular checkups to smoking cessation and dietary programs.
• Mental health and substance use disorder treatment: Identifying, engaging and supporting
through treatment people with mental health conditions and substance use disorders and
ensuring that they are provided with timely and effective care that is integrated with their other
health care needs.
4
In the current contract, Covered California focused health equity efforts on reduction of health disparities. While inclusive of health
disparities reduction, the revised framework of Individualized, Equitable Care is intended to capture the broad goal of care that is
individualized to address an individual’s health needs.
5
Committee on Quality Health Care in America, Institute of Medicine. (2001). Crossing the quality chasm: a new health system for the 21st
century. Washington, D.C.: National Academy Press.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
CHAPTER 1
COVERED CALIFORNIA 3
• Acute, chronic and other conditions: Actively managing care for people with acute
conditions, which are defined as illnesses or diseases that are short term and last typically a few
days to weeks, such as an infection or an injury; chronic conditions, which typically develop
slowly over time and last months to years, such as diabetes, most cancers, cardiovascular
disease, and infectious diseases like Human Immunodeficiency Virus (HIV); and other
conditions that are temporary, such as pregnancy or gestational diabetes.
• Complex care: Effectively managing very complex conditions for individuals that require a
multitude of specialty, high-cost treatments — such as cancer or transplants — or require end of
life care. These are individuals who need to be managed effectively or seen in very specialized
settings by providers who know how to manage their condition well and can provide coordinated
interventions.
The concept of individualized, equitable care as it applies to the specific care domains is illustrated in
Figure 2. Covered California’s Domains for Assuring Contracted Health Plans Deliver Quality Care,
recognizing that some members with mental health, substance use disorders or multiple chronic
conditions need care in multiple domains.
Figure 2. Covered California’s Domains for Assuring Contracted Health Plans Deliver Quality Care
Effective Care Delivery
In addition to addressing various populations and the care they receive, Covered California also
focuses on effective care delivery strategies and its contractual requirements promote improving the
way care is delivered for our enrollees and all Californians, whether it is provided by a primary care
physician, hospital, clinic or other provider. What follows are the organizing strategies for effective care
delivery:

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
CHAPTER 1
COVERED CALIFORNIA 4
• Effective primary care: The foundation of providing appropriate and equitable care is built on
team-based, data-driven primary care that is well integrated, coordinated and continuous. While
many consumers benefit from an ongoing continuous relationship with a single physician, there
is strong evidence that primary care through well-integrated sites of care or delivery systems are
more effective.
• Promotion of integrated delivery systems and accountable care organizations: Effectively
caring for and managing a person’s health requires an integrated care system that can
coordinate across providers, sites and time for a variety of conditions while delivering good
outcomes and quality at an affordable cost.
• Networks based on value: All clinicians, providers, hospitals and sites of care are selected and
regularly assessed based on how those individuals or institutions provide care that is safe,
timely, effective, efficient, equitable, and patient-centered. Ideally, every network is composed of
integrated systems, effective primary care and designed considering the value it provides.
Regardless of the organizing strategies — whether focused on primary care, an integrated delivery
system or the overall network — Covered California aims to ensure the interventions that patients
receive are both appropriate and delivered through sites and services that meet their needs:
• Appropriate interventions: The use of clinical interventions, such as prescriptions,
procedures, diagnostic tests and devices that are rooted in the STEEEP domains and based on
strong evidence and shared decision-making.
• Sites and expanded approaches to care delivery: Covered California supports patients in
getting health interventions and treatments in the most appropriate setting. That means assuring
quality care is delivered not only in hospitals, whether on an in-patient or outpatient basis, but in
ambulatory settings such as a doctor’s office, urgent care facilities, retail facilities such as drop-
in clinics, at home, or through telehealth. Expanded approaches to care delivery also include
who provides care in addition to physicians, such as registered nurses, pharmacists, midwives
or other non-licensed providers like community health workers.
Key Drivers of Quality Care and Effective Delivery
Covered California recognizes that moving health reform forward in an impactful way within a delivery
system shared among many purchasers and health insurance companies will require aligning with
other purchasers and working with all relevant payers in a way that reduces the burden on providers.
When considering the key drivers of quality care and effective delivery, Covered California has looked
to the National Quality Strategy
6
and mirrored many of the same levers initially noted in 2011.
Many of these levers or drivers are specifically articulated as expectations of health insurers in
Attachment 7 as ways to assure individuals get the right care. Insurers are working to improve the
delivery system over time. However, some of the “community drivers” that are identified may be outside
of the scope of an individual insurer’s responsibility or Covered California’s contract. Nevertheless, it is
important to recognize these drivers are a part of the context within which health care is delivered and
the quality of health that consumers experience. Examples of community drivers are detailed after the
roster of drivers specific to health insurer’s work. Key drivers include:
6
Agency for Healthcare Research and Quality. (2011) 2011 Report to Congress: National Strategy for Quality Improvement in Health Care.
Retrieved from https://www.ahrq.gov/workingforquality/reports/2011-annual-report.html
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
CHAPTER 1
COVERED CALIFORNIA 5
1. Benefit design: Helping consumers make informed decisions by standardizing benefit designs,
so they are easier to understand and compare, and incentivize access to the right care at the
right time. Benefit design may include incentives to encourage patients to use particular
providers or particular sites of care or formulary and other designs to encourage providers to
select particular interventions as appropriate.
2. Measurement for improvement, choice and accountability: Providing meaningful and
actionable performance feedback to providers, insurers and the public to improve care and
compare treatment results, cost and patient experiences for consumers.
3. Payment: Rewarding and incentivizing delivery of high-quality, patient-centered care that
promotes better health, quality improvement and value while also fostering innovation,
improving efficiency and adopting evidence-based practices.
4. Patient-centered social needs: Identifying, and, as needed, addressing patient-centered
support for non-medical services, recognizing that many people may face barriers that prevent
them from staying healthy and receiving the right care at the right time, such as food insecurity,
housing insecurity and lack of transportation to their doctor.
5. Patient and consumer engagement: Increasing support for and the level of participation by
patients and consumers in managing their health and making their personal health care
decisions.
6. Data sharing: Making patient data available and accessible to support clinical care and
coordination, decrease health care costs, reduce paperwork, improve outcomes and give
patients more control over their health care.
7. Data analytics: Inspecting, transforming and modeling data to discover timely and reliable
information that will aid in a patient or provider’s decision-making processes.
8. Administrative simplification and provider burden reduction: Implementing system
changes to maximize the time providers spend with patients and minimize unnecessary
administrative burden.
9. Certification, accreditation and regulation: Employing existing regulatory and accreditation
processes and work with other agencies and departments to ensure approaches meet safety
and quality standards. For example, California’s Departments of Insurance and Managed Health
Care enforce the regulatory standards that Covered California relies on for network adequacy.
The National Committee for Quality Assurance (NCQA), among others, conducts health plan
accreditation.
10. Quality improvement and technical assistance: Promoting initiatives that will lead to better
patient outcomes and better care delivery approaches, strengthening the evidence base to
inform better decision-making and fostering learning environments that offer training, resources,
tools and guidance to help organizations achieve quality improvement goals.
Beyond the drivers of more effective care and healthier populations that relate to what an individual
insurer can do or be held accountable for, Covered California recognizes and seeks to better
understand the impact of broader social and structural issues on health status, care and care delivery.
Community health drivers include:
• Workforce: Investing in people to prepare the next generation of health care professionals and
support lifelong learning for providers.
• Community-wide social determinants: Addressing structural social and economic influences
that impact individual and group differences in health.
• Population and public health: Increasing the health of a community through broad
interventions that address public health, homelessness or food insecurity.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 6
ASSURING QUALITY CARE
Chapter 2: Individualized, Equitable
Care — Best Possible Care for All
Covered California’s overarching goal is to
ensure that everyone receives the best possible
health care. This goal entails striving to ensure
that care is personalized, does not cause harm,
is delivered in the right setting at the right time,
and is as cost effective as possible. For
decisions where more than one evidence-based
treatment is available, the goal is to support
individuals in choosing treatment based on their
values and preferences. In the framework
proposed by the Institute of Medicine 20 years
ago, everyone should receive care that is safe,
timely, effective, efficient, equitable, and patient-
centered (often captured by the acronym
“STEEEP”).
7
Unfortunately, the quality of care
delivered in the United States varies
dramatically.
Of the elements related to the Institute of
Medicine’s framework, the domain that has too
often not been given central focus is the charge
to ensure that care is equitable. Addressing
health equity and disparities in health care has
been integral to Covered California’s mission.
Given that focus, after reviewing some important
overall indicators of how health plans are
generally meeting consumers’ needs, much of
this chapter specifically addresses Covered
California’s focus on the issue of equity. The
other domains of the STEEEP framework are
addressed throughout the report and are integral
to Covered California’s approach. The Quality
Rating System (QRS), which includes
performance measures based both on clinical
measures and on patients’ reported experience
of getting care, provides a global picture of how
Covered California’s health plans are doing at
providing the best possible care. In this chapter,
the Global and Summary Components of the
7
Committee on Quality Health Care in America, Institute of Medicine. (2001). Crossing the quality chasm: a new health system for the 21st
century. Washington, D.C.: National Academy Press.
• Covered California enrollees are generally
very satisfied with their experience with
their health plans and their health care,
with the vast majority enrolled in plans that
score above the 50
th
percentile for enrollee
satisfaction with their health care and plan.
• Global Quality Ratings have improved
since their launch in 2016, but a dip in 2019
has generated further scrutiny.
• Covered California has launched a long-
term initiative to reduce health disparities.
In response to contractual requirements, 93
percent of enrollees are in plans that were
at or above the 80 percent requirement for
enrollee self-identification of race/ethnicity.
• All 11 insurers are analyzing disparities in
care for patients with diabetes,
hypertension, asthma and depression for
all of their lines of business, not just
Covered California, and planning targeted
interventions.
• Gaps in quality by race/ethnicity were
found for all insurers — but were not
consistent (e.g., for some insurers African
Americans warranted targeted
interventions for diabetes, and Latinos in
others).
• Racial and ethnic disparities are generally
smaller than the differences in quality
across plans: enrollment in Sharp Health
Plan or Kaiser Permanente is a better
predictor of receiving good care than race
or ethnicity is.
• Nevertheless, all insurers have identified a
disparity where a targeted intervention can
improve help reduce disparities and
improve health.
Highlights
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 7
health plan quality ratings are presented, along with two measures that relate to enrollee satisfaction
with their health plan and their care.
Social, economic and geographic disparities in health and health care pose a particularly serious
challenge to the goal of ensuring the best possible care for all. Because social and environmental
factors are powerful determinants not only of the care individuals receive but also of their underlying
health, reducing disparities requires efforts within the health care delivery system and in the broader
community. Covered California recognizes that meaningful progress will require multi-pronged and
multi-year efforts.
Covered California is working to reduce disparities and promote health equity. To this end, Covered
California has hired a new health equity officer who plans, implements and integrates Covered
California’s health equity agenda with Covered California’s quality improvement and delivery system
reform efforts. The health equity officer leads the work of the new Population Care Unit within the Plan
Management Division, which is composed of staff positions dedicated to quality improvement, health
equity and social determinants of health.
Covered California is working with health plans to reduce health disparities and promote health equity
by: (1) identifying the race/ethnicity of all enrollees; (2) collecting data on diabetes, hypertension,
asthma and depression to measure how quality varies by race/ethnicity; (3) conducting population
health-improvement activities and interventions to narrow observed disparities in care; and (4)
promoting community health initiatives that foster better health, healthier environments, and promote
healthy behaviors. This chapter describes how Covered California has moved forward in each of these
areas.
This chapter on individualized, equitable care is organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Health Plan-Reported Measures for Health Disparities
Section 3. Implications for the Future
Section 1. Qualified Health Plan Experience
Health Plan Measures Reported to the Quality Rating System
This section presents performance data reported by health insurance companies for contract
requirements and includes assessments and observations by Covered California. One key mechanism
used by Covered California for health plan oversight and accountability is public reporting of global and
individual health plan quality-performance measures to the Centers for Medicare and Medicaid
Services’ Marketplace Quality Rating System (QRS). In the current contract requirements, health plans
are required to:
1. Annually collect and report to Covered California for each product type the measure numerator,
denominator and rates for its QRS data, including Healthcare Effectiveness Data and
Information Set (HEDIS) measures, Consumer Assessment of Healthcare Providers and
Systems (CAHPS) survey data and other performance data.
2. Submit HEDIS and CAHPS scores to include the measure numerator, denominator and rate for
the required measures set reported to NCQA Quality Compass and the Department of Health
Care Services (DHCS), for each product type for which it has data in California.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 8
Global and Summary Component Health Plan Quality Ratings
The Marketplace QRS global quality ratings show how health plans compare on helping members get
the right medical care and on member-reported experiences of care and service. Covered California
displays each health plan’s QRS rating to enrollees through the plan shopping experience and on
coveredca.com.
Plans are rated on a scale of one to five stars. To assign the star rating, each health plan’s results are
compared to about 200 marketplace health plans nationwide. A five-star plan means that health plan
scored among the top plans nationwide; a one-star rating means the plan’s score was among the
lowest.
QRS is composed of a global quality ratings and summary component ratings for three major aspects
of health plan performance.
8
Each health plan’s product (HMO, PPO, EPO) receives a separate QRS
rating.
Global quality rating: The global quality rating is a roll-up of three summary components per the
following weighting:
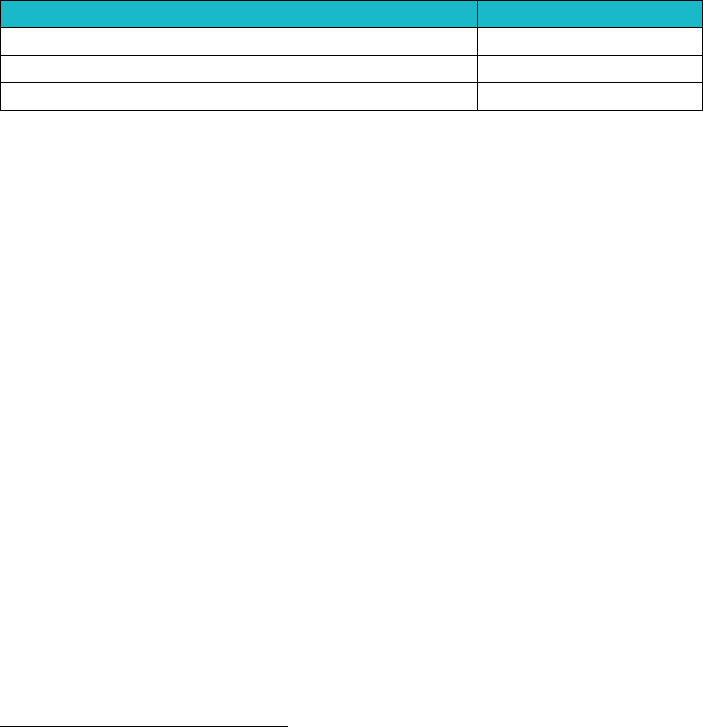
Summary Components
Weights
Getting Right Care (HEDIS)
66%
Members’ Care Experience (CAHPS)
17%
Plan Services (HEDIS and CAHPS)
17%
A global quality rating is constructed for each health plan that has at least two of the three component
scores, and one of the scores must be for the “Getting the right care” component:
• Getting the right care: Each year, a sample of members from each health plan is selected, and
their records are checked to compare their medical care with national standards for care and
evidence-based treatments. More than 30 HEDIS measures are tracked using medical charts
and billing records sent by providers and hospitals. These quality measures include how well
the health plan and its providers care for enrollees, such as controlling high blood pressure,
lowering cholesterol and getting the right medications.
• Members’ care experience: Members’ experiences with their doctor and care are based on the
CAHPS survey that asks about members’ recent experiences when visiting the doctor and
getting medical care. About one of every five people who receive a survey in the mail or by
phone provides a response, with about 250 members from each plan completing surveys.
CAHPS surveys are currently only available in English or Spanish, but insurers are encouraged
to translate the surveys into other languages that reflect their patient population. Translation
guidelines are readily available from CMS.
• Plan services for members: A sample of plan members’ records is checked to see if patients
got unnecessary care — services that could be harmful and wasteful. The CAHPS member
survey is also used to report on members’ experiences in getting help and information from the
insurer’s customer service staff.
8
See the Appendix 2 for the complete list of measures used to determine each summary component rating of QRS.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 9
The QRS ratings of Covered California health plans have generally improved over time, but there was a
downward trend in 2019.
9
For the 2019 reporting year, which represents the 2018 measurement year,
the overall trend is lower star ratings compared to 2018: for the global rating, only one plan has a 5-star
rating and one plan has a 4-star rating while most have 2 and 3-star ratings (see Table 1. Global
Quality Ratings by Reportable Products for Individual and CCSB Markets, 2016-2019).
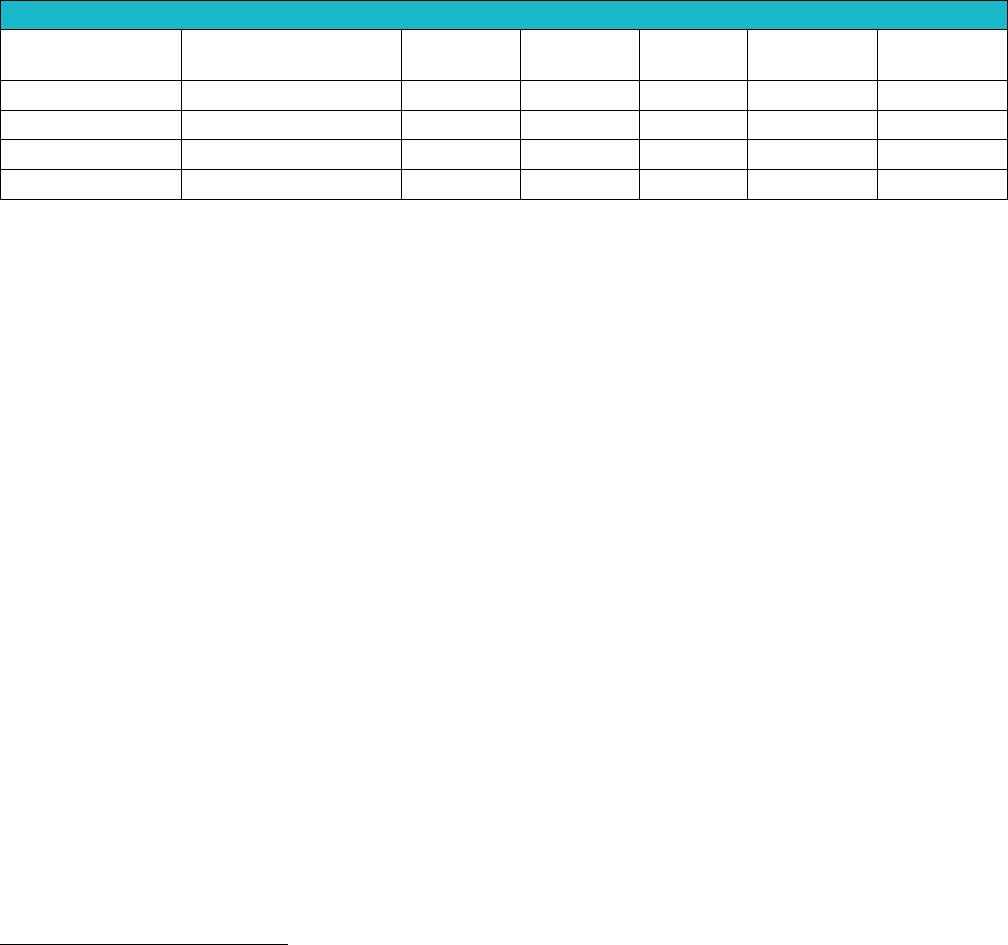
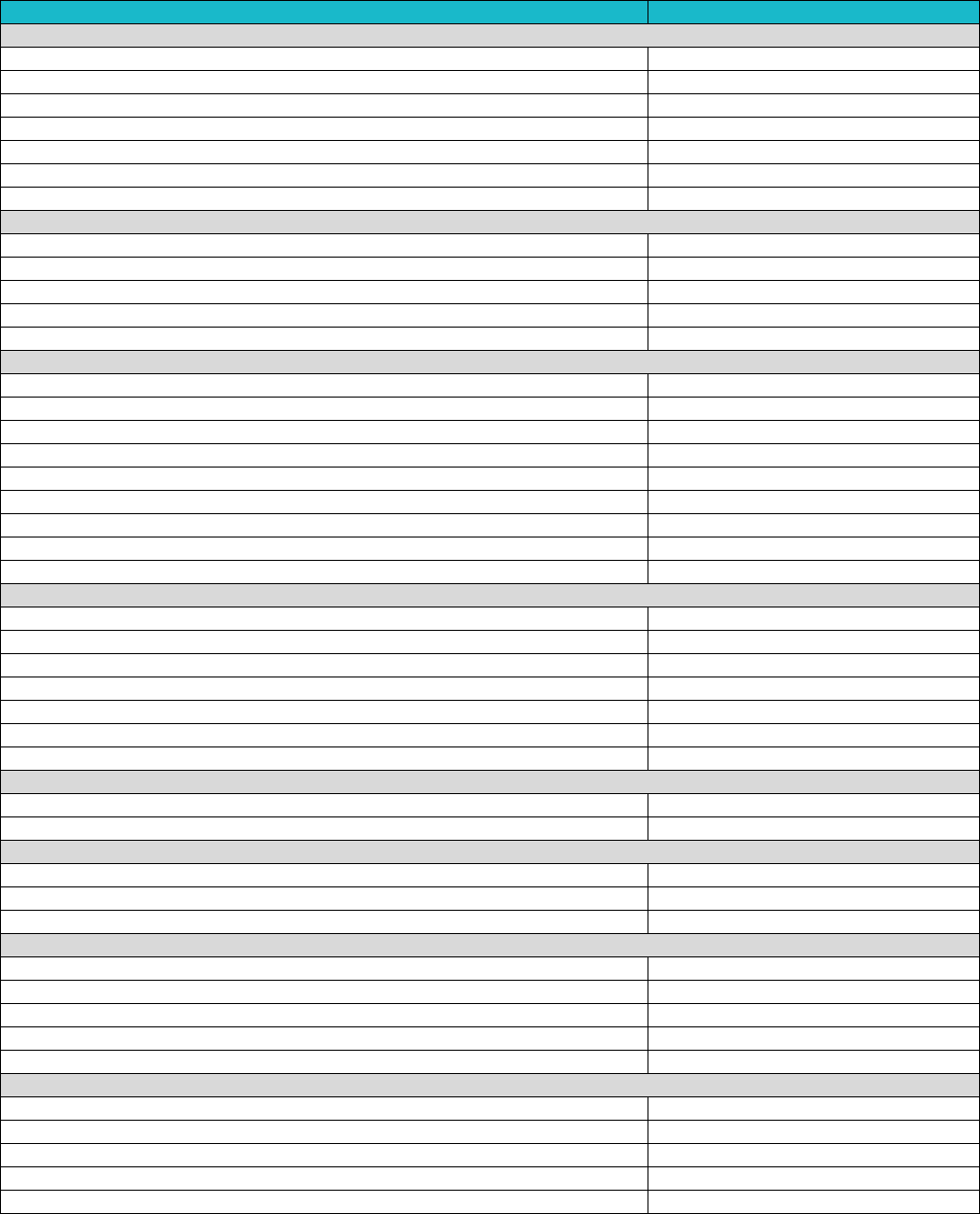
Table 1. Global Quality Ratings by Reportable Products for
Individual and Covered California for Small Business (CCSB) Markets, 2016-2019
Overall Quality Ratings by Reportable Products for Individual and CCSB Markets
# Products with
No Global Rating
1 Star
★
2 Star
★★
3 Star
★★★
4 Star
★★★★
5 Star
★★★★★
2019 QRS
3*
0
5
5
1
1
2018 QRS
3*
0
0
6
4
2
2017 QRS
4*
0
3
6
1
1
2016 QRS
5*
1
7
2
1
1
*No global rating if a newer product and not eligible for reporting or insufficient sample sizes to report results for at least 2 of the 3 summary
component categories.
Source: Covered California Health Plan QRS Reporting
Table 2 lists the global rating and the three summary component ratings for each Covered California
health plan for 2019. Covered California health plans generally performed well on the Plan Services for
Members component rating, with all plans receiving a 3-star rating or above on this component.
9
The 2018 reporting year, which represented the 2017 measurement year, was impacted by a federal statistical methodology that appears
to have inflated star ratings for that year. Covered California is working with CMS to achieve a more stable methodology that will allow
better year-to-year comparisons of star ratings based on changes in performance. This affected only the star rating, not the underlying
measure scores reported below.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 10
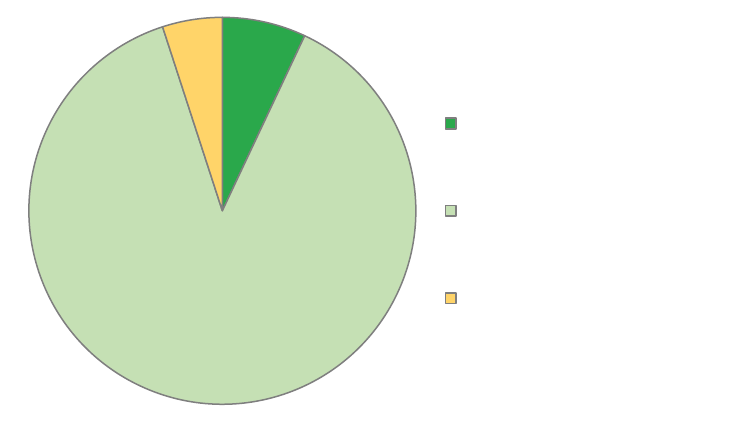
Table 2. Covered California Health Plan QRS Global and Summary Component Ratings, 2019
Health Plan
Product
Type
Global Rating
Getting the
Right Care
Members’ Care
Experiences
Plan Services
for Members
Anthem
EPO
★★
★★
★★
★★★
Blue Shield
PPO
★★★
★★
★★★
★★★
Blue Shield
HMO
★★★
★★
★★★
★★★
CCHP
HMO
★★★
★★★
★★
★★★★★
Health Net
HMO
★★
★★★
★
★★★
Health Net
EPO
One Quality
Rating Available
★★
Not
Reportable**
Not
Reportable**
Health Net
PPO
Quality Rating
in Future*
Quality Rating
in Future*
Quality Rating in
Future*
Quality Rating
in Future*
Kaiser
HMO
★★★★★
★★★★★
★★★★
★★★★★
LA Care
HMO
★★★
★★★
★★
★★★
Molina
HMO
★★
★★
★★
★★★
Oscar
EPO
★★
★★
★★★
★★★★★
Sharp
HMO
★★★★
★★★★
★★★
★★★★
Valley
HMO
★★★
★★★★
★
★★★
WHA
HMO
★★
★★
★★★
★★★★
Blue Shield
HMO/CCSB
★★★
★★
★★★
★★★
Health Net
PPO/CCSB
Quality Rating
in Future*
Quality Rating
in Future*
Quality Rating in
Future*
Quality Rating
in Future*
*Quality ratings are reported for a health plan product after its first two years with Covered California.
**Not enough data to calculate a score according to the quality rating methodology.
Source: Covered California Health Plan QRS Reporting
Enrollee Satisfaction With Their Health Care and Health Plan
Assuring that care is patient-centered requires assessment of a range of elements, including the extent
to which patients receive the right care, at the right time, and in the most appropriate setting. As
discussed in Chapter 10: Appropriate Interventions, it also means that care provided is informed and
based on the patient’s preferences and their understanding of the implications of their choices. At a
high level, however, a starting point of making sure care is patient-centered is considering patient
voices in assessing health plans’ performance.
Among the health plan measures reported to the Marketplace Quality Rating System are Consumer
Assessment of Healthcare Providers and Systems (CAHPS) measures that reflect consumers’
perspectives and their reported experience with care received. These Marketplace Quality Rating
System (QRS) standard performance measures are a key mechanism used by Covered California for
health plan oversight and accountability. To more sharply focus health plan accountability efforts,
Covered California examined over 40 measures used by QRS and is proposing to prioritize a subset of
13 measures that were selected based on the following criteria: (1) health impact; (2) extent of health
plan variation; (3) performance improvement opportunity; (4) alignment with other California
accountability programs; and (5) balance across domains of care, such as prevention, chronic illness
care and behavioral health. Three of the 13 measures overlap with the measures currently collected by
race/ethnicity for health disparities reduction interventions as discussed in Section 2 of this chapter.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 11
The following tables display the priority measures for individualized, equitable care in the QRS measure
set and include the Covered California weighted average, the highest- and lowest-performing plans,
plan-specific performance and national percentiles for all marketplace plans:
1. Rating of Health Plan (Table 3).
2. Rating of All Health Care (Table 4).
These two CAHPS questions the reflect consumers’ overall satisfaction with their health plan and the
care they received. As evident from each of these measures, there is generally high satisfaction among
Covered California enrollees with their health plans (with 95 percent of enrollees reporting satisfaction
that is above the 50
th
percentile nationally) and with their care (75 percent of enrollees reporting
satisfaction that is above the 50
th
percentile nationally). (See Figure 3. Covered California Enrollment in
Health Plans by Consumer Rating of Health Plan — 95 Percent of Enrollees in Plans Scoring Above
the 50
th
Percentile Nationally, and All Enrollees in Plans Above the 25
th
Percentile, 2019.)
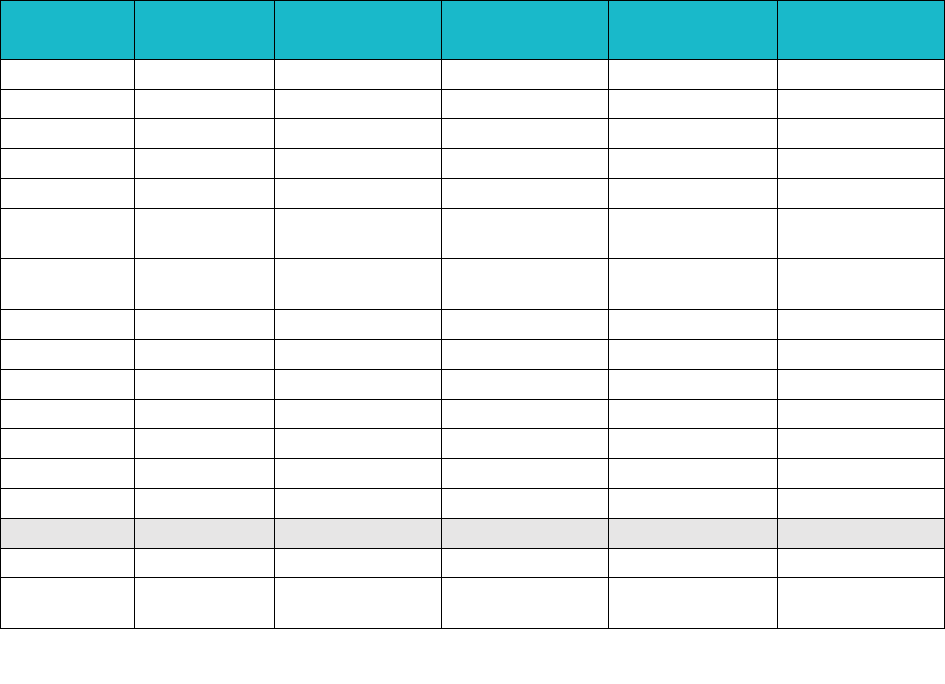
Figure 3: Covered California Enrollment in Health Plans by Consumer Rating of Health Plan — 95 Percent
of Enrollees in Plans Scoring Above the 50
th
Percentile Nationally, and All Enrollees in Plans Above the
25
th
Percentile, 2019
7%
88%
5%
Enrollees in Plans at 90th
Percentile and Above
Enrollees in Plans at 50th to
90th Percentile
Enrollees in Plans at 25th to
50th Percentile

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 12
Rating of Health Plan
The Rating of Health Plan measure indicates enrollee experience related to the rating of health plan
QHP Enrollee Survey question.
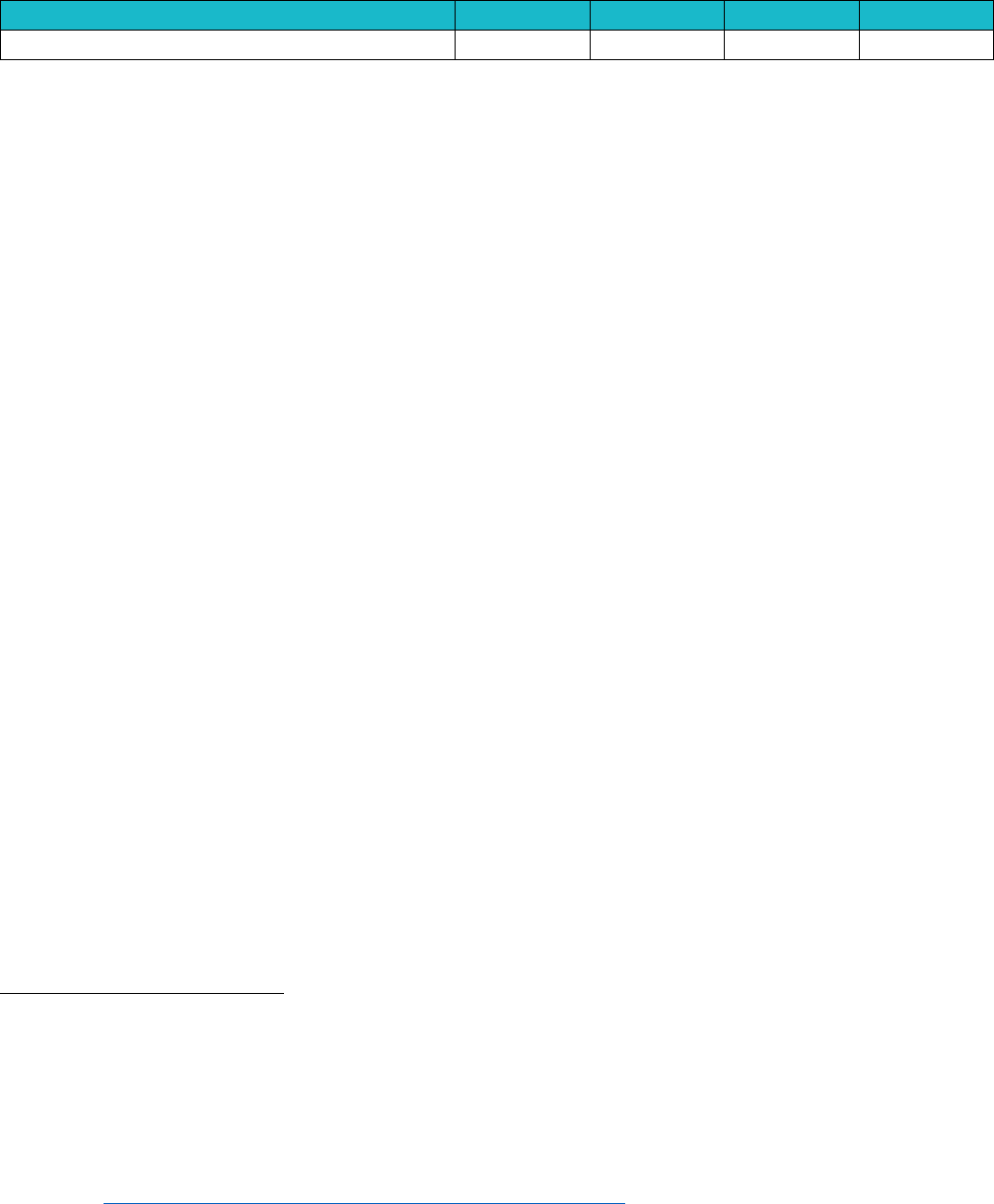
Table 3: Covered California Enrollees Rating of Health Plan (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
78 +
78 +
79 +
75 +
7%
93,322
1
Plans at 50th to 90th
Percentile
72 to 78
72 to 78
73 to 79
69 to 75
88%
1,187,877
10
Plans at 25th to 50th
Percentile
67 to 72
68 to 72
69 to 73
64 to 69
5%
64,031
1
Plans Below 25th Percentile
Below 67
Below 68
Below 69
Below 64
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest
Performer
79
80
82
76
Covered CA Weighted
Average
73
76
78
73
Covered CA Lowest
Performer
66
69
65
69
Covered California Plan-Specific Performance
Anthem HMO
71
74
Anthem PPO
67
70
Anthem EPO
67
69
5%
64,031
Blue Shield HMO
70
75
76
7%
93,322
Blue Shield PPO
75
75
78
71
25%
335,176
CCHP HMO
74
76
78
73
1%
10,013
Health Net HMO
70
75
73
70
11%
145,183
Health Net EPO
69
65
Health Net PPO
Kaiser Permanente HMO
79
80
82
74
36%
477,683
LA Care HMO
68
77
73
73
6%
84,750
Molina Healthcare HMO
66
72
69
71
4%
56,023
Oscar Health Plan EPO
80
71
3%
35,962
Sharp Health Plan HMO
77
80
78
75
1%
17,335
Valley Health Plan HMO
70
76
78
75
1%
16,366
Western Health Advantage
HMO
77
77
78
72
1%
9,386
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 13
Rating of All Health Care
The “Rating of all health care” measure is an overall indicator of enrollees’ satisfaction (0-10 scale) with
their health care based on the QHP Enrollee Survey.
Table 4: Covered California Enrollees’ Rating of All Health Care (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
85 +
86 +
86 +
82 +
0%
-
0
Plans at 50th to 90th Percentile
82 to 85
83 to 86
83 to 86
78 to 82
75%
1,008,266
5
Plans at 25th to 50th Percentile
80 to 82
81 to 83
81 to 83
75 to 78
25%
336,964
7
Plans Below 25th Percentile
Below 80
Below 81
Below 81
Below 75
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
84
88
86
80
Covered CA Weighted
Average
80
81
83
78
Covered CA Lowest Performer
69
75
74
75
Covered California Plan-Specific Performance
Anthem HMO
78
79
Anthem PPO
76
82
Anthem EPO
76
5%
64,031
Blue Shield HMO
80
7%
93,322
Blue Shield PPO
83
82
85
78
25%
335,176
CCHP HMO
80
80
81
77
1%
10,013
Health Net HMO
74
78
78
75
11%
145,183
Health Net EPO
81
Health Net PPO
Kaiser Permanente HMO
84
84
86
80
36%
477,683
LA Care HMO
80
83
76
78
6%
84,750
Molina Healthcare HMO
69
75
74
76
4%
56,023
Oscar Health Plan EPO
82
76
3%
35,962
Sharp Health Plan HMO
83
88
85
80
1%
17,335
Valley Health Plan HMO
76
80
81
77
1%
16,366
Western Health Advantage
HMO
83
85
84
76
1%
9,386

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 14
Covered California’s Attention to Equity and Health Disparities
Covered California has prioritized initiatives to narrow health care and coverage disparities and ensure
health equity for all. Reducing health disparities is part of Covered California’s vision and mission
statement and has the potential to benefit all Californians (with over 4 million consumers served to date
through Covered California
10
) and because the populations measured and targeted for improvement by
health insurance companies include all of their enrollees under age 65 across all lines of business.
While disparities are influenced by social
and economic factors beyond the control
of the health care delivery system, there
is agreement and evidence that health
care disparities can be narrowed through
quality improvement activities tailored to
the needs of specific populations and
targeting select measures at the health
plan level. To this end, Covered
California has laid out a health
disparities and health equity agenda
centered on four requirements:
1. Promoting community health initiatives that foster better health, healthier environments and
healthy behaviors.
2. Identifying the race or ethnicity of all enrollees through self-identification or imputed
methodology.
3. Collecting data by race/ethnicity for disease control and management measures for asthma,
depression, diabetes and hypertension — conditions with especially high levels of morbidity and
mortality experienced by disadvantaged populations.
4. Conducting population-health improvement activities and interventions to narrow observed
disparities in care.
See Section 2 for information on health plan progress in conducting interventions to narrow observed
disparities in care and collecting data by race/ethnicity for disease control and management measures
for asthma, depression, diabetes and hypertension.
Promoting Community Health Initiatives That Foster Better Health, Healthier
Environments, and Promotion of Healthy Behaviors
Under contract requirements, Covered California included requirements for engagement and promotion
of community-wide initiatives that foster better health, healthier environments, and the promotion of
healthy behaviors across the community. Covered California specifically encouraged community health
initiatives that have undergone or are being piloted through systematic review to determine
10
This figure only includes on-exchange enrollment since 2014. The figure is higher if off-exchange mirrored plan enrollment is included.
Covered California’s Mission and Vision
Covered California’s vision is to improve the health of
all Californians by assuring their access to affordable,
high quality care.
Covered California’s mission is to increase the number
of insured Californians, improve health care quality,
lower costs, and reduce health disparities through an
innovative, competitive marketplace that empowers
consumers to choose the health plan and providers that
give them the best value.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 15
effectiveness in promoting health and preventing disease, injury or disability and have been
recommended by the Community Preventive Services Task Force. Such programs may include:
1. Partnerships with local, state, or federal public health departments such as Let’s Get Healthy
California.
2. CMS Accountable Health Communities.
3. Organizations that operate preventive and other health programs, such as Cal Fresh.
4. Hospital activities undertaken under the Community Health Needs Assessment required every
three years under the Affordable Care Act.
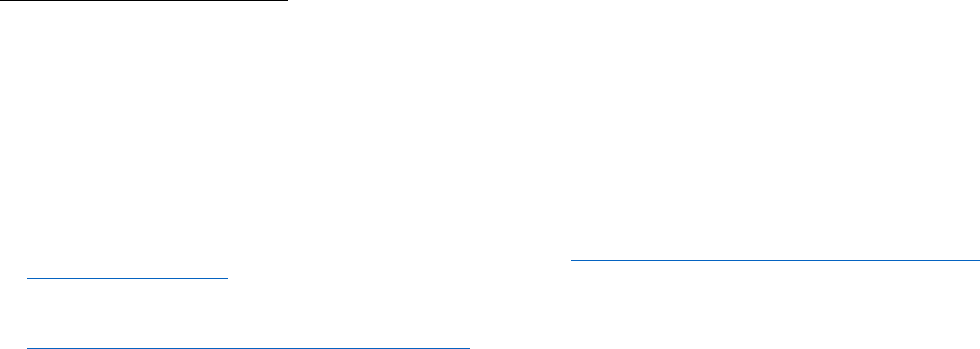
Table 5. Covered California Insurer Activities to Improve Community Health, 2018 shows health insurer
reported initiatives, programs and projects that improve community health apart from the health delivery
system. Health insurance company involvement in external-facing activities is used by Covered
California to identify potential disparity-reduction opportunities.
Identifying the Race or Ethnicity of All Enrollees
Understanding disparities in care requires data collection on demographics and other social
determinants of health. Health insurance companies vary in the degree to which demographic data is
collected and integrated into member records. While state law requires health insurance companies to
collect race, ethnicity, and language data, insurers use different methods to obtain this information and
have different rates for the percentage of membership self-identifying race/ethnicity (i.e. race/ethnicity
self-identification rates).
11
Before the initiatives described below, no purchaser or state agency in
California monitored the success of collecting self-identification rates and there had been no broad
attempt to use the data to evaluate disparities in care.
To achieve high self-identification rates across all health insurance companies, Covered California set a
goal for all insurers to achieve identification of at least 80 percent of all Covered California membership
by year-end 2019 and encouraged use of various data collection methods beyond the membership
enrollment application to identify race/ethnicity. Starting with the 2018 plan year, insurers were
assessed on a contract performance standard for the self-identification rate and received financial
penalties or credits based on whether they achieved the target. Insurers proposed intermediate
milestones for the performance standard for the 2018 plan year and will be assessed on whether they
achieved a target of 80 percent in 2019.
Based on analysis of data gathered for this performance standard, eight insurers have achieved the 80
percent target as of 2018 and some have exceeded 95 percent. Insurers have attributed the increased
identification rates to improved data collection and incorporation of best practices for asking enrollees
for race/ethnicity information.
11
Senate Bill 853, Chapter 717, Statutes of 2009.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 16
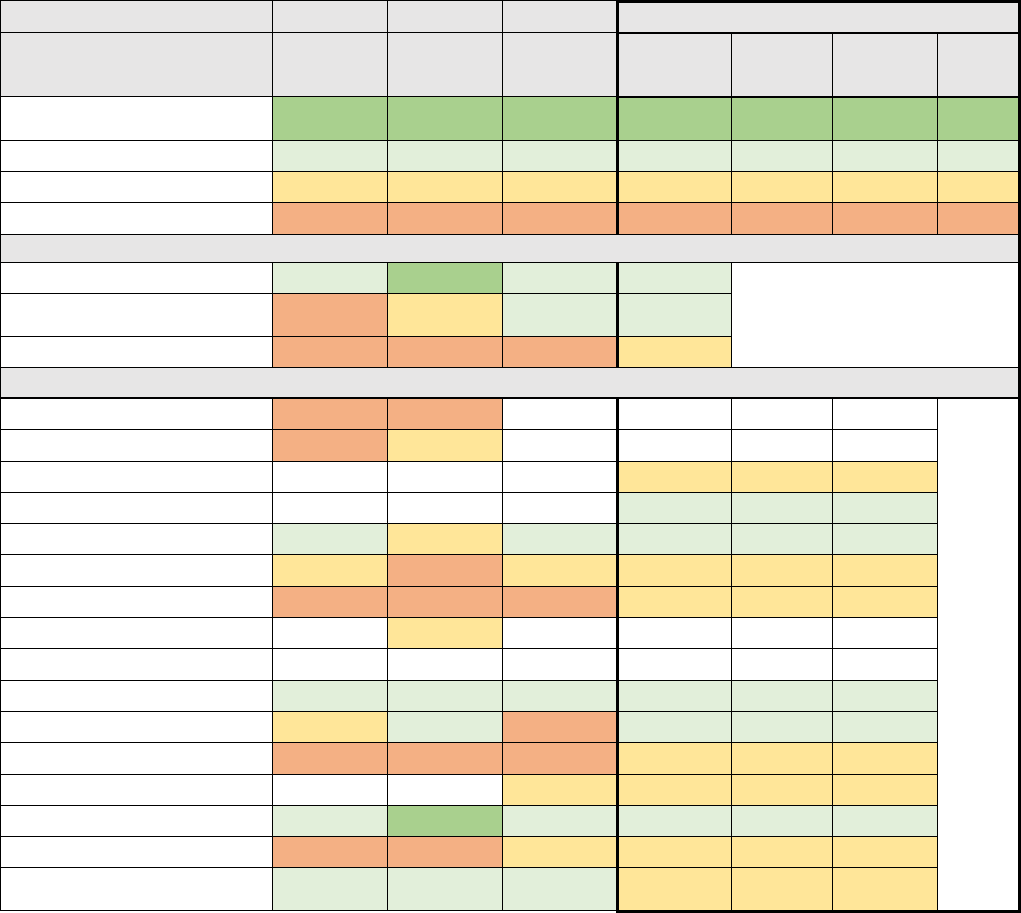
Table 5. Covered California Insurer Activities to Improve Community Health, 2018
Number of Health Plans
Internal facing, member related efforts
Health education portal
3
Quality collaboratives
1
Member outreach
2
Lifestyle or disease-specific workshops and classes
8
Educational materials
5
Incentive programs
2
Connections to outside orgs and programs
2
Internal facing, member related efforts non-health-related
Philanthropy
1
Non-health classes
1
Health insurance education
6
Financial counseling/decision-making support
2
Interpreting services availability education
1
External or community facing activities, health-related
Health fairs (starred if funded)
7
Screening events (starred if funded)
2
Enrollment fairs
1
Public health conferences
1
Statewide or community collaboratives and taskforces
5
Community workshops/classes or peer to peer support
3
Health promotors program
2
Financial support of community health programs
4
Educational materials
2
External facing, non-health-related
Employee volunteers
1
Ads and newsletters
2
Community events
3
Financial support of community non-health programs
2
Education support
2
Non-health coalitions (e.g. homelessness)
2
Health plan option education
1
Engaged with health systems for community risk assessments identifying high priority needs
Through providers
3
Health plan activities
5
Community health effort
School programs
1
In-home assessments
1
Educational campaign
2
Health plan-funded community health programs based on needs assessments or other activity
Grant programs
4
Health fairs
2
Health resource center(s)
2
Community clinics
2
Screening events
2
Participated in geographic disaster relief efforts
Safety policies
1
Member services in affected areas
1
Disaster relief as part of government
1
Disaster preparedness programs
2
Community partner support around disaster relief
2
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 17
Table 6. Number of Insurers Meeting the 80 Percent Target for Identification of Race/Ethnicity
2015
2016
2017
2018
Number of Insurers
5
4
5
8
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Challenges in Data Collection
Health insurance companies can collect self-identification data from several sources. The race/ethnicity
question in the Covered California enrollment application is voluntary and is included in the enrollment
file sent to insurers. Beyond enrollment data, insurers have reported receiving data from providers,
customer service, health risk assessments and website registration. Methods for data collection vary by
insurer, resulting in considerable variation during 2015-18 in how well each insurer met Covered
California’s goals for ensuring race/ethnicity identification for quality improvement purposes.
12
While all insurers have demonstrated improvement towards the 2019 target, it is important to note that
these rates represent Covered California membership only. As discussed in Section 2. Health Plan-
Reported Measures for Health Disparities, an objective of the health equity agenda is to track and trend
a select set disparities measures that include a health insurance company’s full book of business
excluding Medicare. Larger numbers are necessary to be able to accurately measure performance,
especially for relatively small minority populations. Identification of member race/ethnicity when
reporting health disparities measures is similarly challenging. For this reason, Covered California has
encouraged insurers to supplement self-reported identification with a proxy methodology based on
surname and census track. Covered California will continue to work with insurers to improve and
validate self-identification of race and ethnicity.
Section 2. Health Plan Reported Measures and Efforts to Narrow Health
Disparities
Many of Covered California’s contracted health insurance companies have been actively engaged in
efforts to understand and address health care disparities for many years. These efforts are reflected in
a range of activities. Four of Covered California’s health insurance companies, Health Net, Kaiser
Foundation Health Plan of Southern California, L.A. Care and Molina Healthcare, representing 36
percent (503,220 out of 1,384,030) of enrollment in 2018 earned the National Committee for Quality
Assurance’s (NCQA) Distinction in Multicultural Health Care (MHC), a program that recognizes
organizations that provide culturally and linguistically sensitive services and work to reduce disparities
in health and health care.
13
In 2017, Covered California began an initiative to measure and seek improvement in health equity
across all contracted insurers. In collaboration with health insurance companies and consumer
12
In 2018, Covered California examined current self-identification rates in the Covered California enrollment file to compare to insurer
reported rates. Covered California’s self-identification rate in 2017 was 75.5 percent across all insurers. In theory, insurer reported rates
should be equal to or higher than the rate provided in the enrollment file, assuming all data is transferred to the insurer and the insurer’s
other avenues of data collection supplement the race/ethnicity field in its membership file. In practice, some insurers have reported
considerably lower rates and are currently evaluating internal data collection to understand the discrepancies. Covered California is also
aware of some errors in the 834 data transmission related to race/ethnicity categorization and is actively working on a system change
request to appropriately identify membership answering this question in the enrollment application.
13
See more: https://www.ncqa.org/programs/health-plans/multicultural-health-care-mhc/.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 18
stakeholders, Covered California targeted four conditions that affect large numbers of consumers, have
serious potentially avoidable complications, and for which there is strong evidence of racial or ethnic
disparities:
• Asthma: Although asthma affects all populations, the burden of this disease falls
disproportionately on minority populations: the prevalence of childhood asthma is 12.7 percent
among non-Hispanic blacks compared to 8 percent among non-Hispanic whites and 6.4 percent
among Hispanics. Even more striking, the asthma mortality rate among non-Hispanic black
children is nearly eight times that of non-Hispanic whites.
14
• Depression: National surveys indicate that nearly one in six Americans has experienced a
major depressive episode, with many experiencing multiple episodes. Depression is a leading
cause of disability and death, largely related to the nearly tenfold higher risk of suicide among
those with depression.
15
Depression is undertreated in all populations, but more so among
minorities. Although 40 percent of non-Latino whites with depression failed to receive treatment,
64 percent of Latinos, 69 percent of Asians, and 59 percent of African Americans failed to
receive any treatment.
16
• Diabetes: While diabetes affects almost 10 percent of the U.S. population overall, the
prevalence in Hispanics (11.9 percent) and African Americans (13.4 percent) is much higher
than it is in non-Hispanic Whites. Diabetes is the seventh leading cause of death and
contributes to an increased risk of heart attacks, stroke, amputation and kidney disease.
17
• Hypertension: Almost one third of adults have hypertension (high blood pressure), a major risk
factor for heart attacks (the leading cause of death in the U.S.) and strokes (the seventh leading
cause of death). The prevalence of hypertension among non-Hispanic blacks (41 percent) is
substantially higher than among whites (29 percent) or Hispanics (28 percent). Among those
with hypertension, the proportion who were well controlled differed dramatically: whites at 53
percent, non-Hispanic blacks at 43 percent and Hispanics at 30 percent.
18
Because of the public health importance of these conditions and the serious disparities in health and
health care that have been documented and the potential for targeted interventions to reduce morbidity
and mortality, Covered California selected 14 measures related to these conditions to track, of which
five are National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and
Information Set (HEDIS) measures and nine are based on Agency for Healthcare Research and Quality
(AHRQ) Prevention Quality Indicators (PQI). Importantly, these measures are now being reported by
insurers annually not only for Covered California’s enrollees, but also for all non-Medicare commercial
14
Forno, E., and Celedón, J. C. (2012). Health disparities in asthma. American journal of respiratory and critical care medicine, 185(10),
1033–1035. doi:10.1164/rccm.201202-0350ED
15
McLaughlin K. A. (2011). The public health impact of major depression: a call for interdisciplinary prevention efforts. Prevention science:
the official journal of the Society for Prevention Research, 12(4), 361–371. doi:10.1007/s11121-011-0231-8
16
Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C. N., Takeuchi, D., … Meng, X. L. (2008). Disparity in depression treatment among
racial and ethnic minority populations in the United States. Psychiatric services (Washington, D.C.), 59(11), 1264–1272.
doi:10.1176/appi.ps.59.11.1264
17
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and
Prevention, U.S. Dept of Health and Human Services; 2017. Retrieved from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-
diabetes-statistics-report.pdf.
18
Centers for Disease Control and Prevention. Prevalence of Hypertension and Controlled Hypertension — United States, 2007–2010.
Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2013. Retrieved from:
https://www.cdc.gov/mmwr/preview/mmwrhtml/su6203a24.htm.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 19
and Medi-Cal lives, with rates supplied by race/ethnicity (see Table 7. Covered California Insurer “All-
Plan” Reported Measures for Health Disparities).
Data for the full non-Medicare population was required for the following principal reasons: (1) narrowing
disparities requires quality improvement interventions regardless of coverage type; (2) the larger
population size makes measurement of disparities more accurate; and (3) high turnover in the
individual market results in consumers transitioning to other sources of coverage, such as employer-
based coverage or Medi-Cal. These markets are served by the same health insurance companies that
participate in Covered California.
During the first year of reporting for plan year 2015, insurers reported on 10 measures, and an
additional four measures were phased in for plan year 2016. Insurers will continue reporting the data for
all 14 measures through plan year 2020 as Covered California continues to evaluate insurer’s data and
the progress of planned interventions.
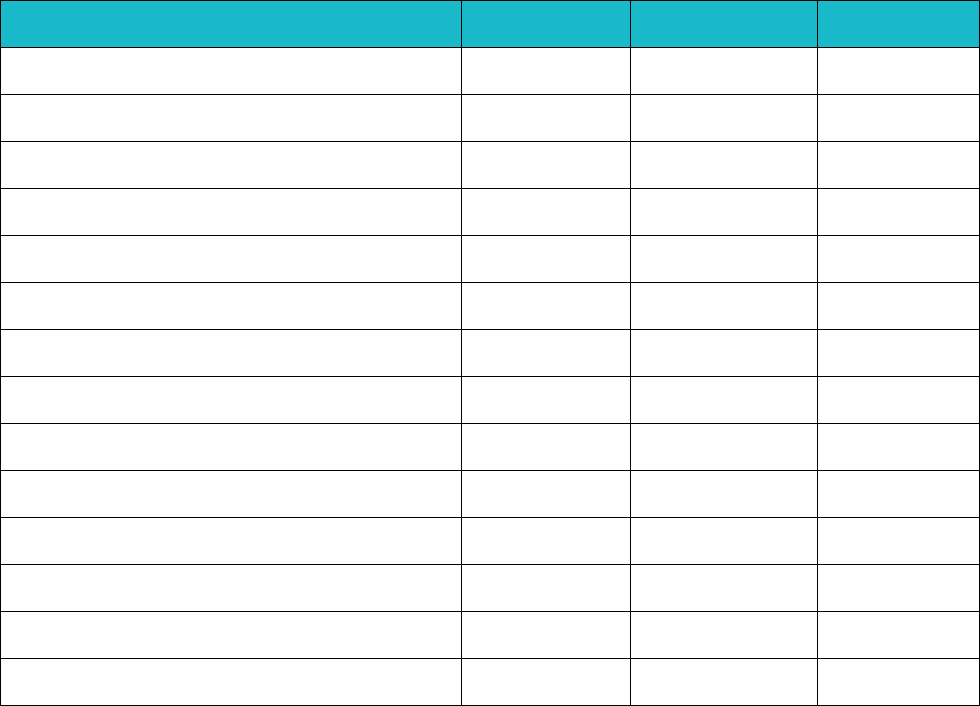
Table 7. Covered California Insurer “All-Plan” Reported Measures for Health Disparities
Measure
Measure
Steward
Years Reported
Condition
AMR - Asthma Medication Ratio Ages 5-85
NCQA
MY 2015, 2016,
2017
Asthma
Admissions for Asthma among Older Adults with
Asthma
AHRQ PQI
MY 2015, 2016,
2017
Asthma
Admissions for Bacterial Pneumonia among
Members with Asthma
AHRQ PQI
MY 2016, 2017
Asthma
Admissions for Asthma among Children and
Younger Adults with Asthma
AHRQ PQI
MY 2015, 2016,
2017
Asthma
Antidepressant Medication Management
(Effective Acute Phase Treatment)
NCQA
MY 2015, 2016,
2017
Depression
Antidepressant Medication Management
(Effective Continuation Phase Treatment)
NCQA
MY 2015, 2016,
2017
Depression
Diabetes Care: HbA1c Control < 8.0% (NQF
0575)
NCQA
MY 2015, 2016,
2017
Diabetes
Admissions for Diabetes Short-term
Complications among Members with Diabetes
AHRQ PQI
MY 2015, 2016,
2017
Diabetes
Admissions for Diabetes Long-Term
Complications among Members with Diabetes
AHRQ PQI
MY 2015, 2016,
2017
Diabetes
Admissions for Uncontrolled Diabetes among
Members with Diabetes
AHRQ PQI
MY 2016, 2017
Diabetes
Admissions for Lower-Extremity Amputation
among Members with Diabetes
AHRQ PQI
MY 2016, 2017
Diabetes
Controlling High Blood Pressure (NQF 0018)
NCQA
MY 2015, 2016,
2017
Hypertension
Admissions for Hypertension among Members
with Hypertension
AHRQ PQI
MY 2015, 2016,
2017
Hypertension
Admissions for Heart Failure among Members
with Hypertension
AHRQ PQI
MY 2016, 2017
Hypertension
Opportunities for Intervention
The dataset used to evaluate insurer populations for disparities is unique in that it aggregates data for
enrollees under 65 across all lines of business. In addition to serving different geographies with known
variations among them, each insurer has a very different mix of population served ranging from
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 20
predominantly employer-based commercial enrollees to predominantly Medi-Cal enrollees. Insurers
also have varying quality of data, most aggregating 400-person HEDIS samples for each line of
business but some having access to robust clinical data from electronic health records. For these
reasons and more as detailed in Appendix 1: Limitations and Major Caveats about Health Disparities
Data, Covered California has determined that the results cannot be used to compare performance
across plans.
However, Covered California and each insurer found actionable differences in measures across
race/ethnicity groups that justify interventions. In addition, one of the key observations was that the
apparent disparities based on race/ethnicity were in almost all cases far smaller than the differences in
care or treatment across health plans — with enrollment in Kaiser Permanente or Sharp Health Plan
being a far better predictor of receiving good care than race/ethnicity. This observation was consistent
with Covered California’s findings regarding the generally superior care provided by integrated delivery
systems (see Chapter 3 and Chapter 4).
The following sections present high-level summaries of key trends based on preliminary analysis of
insurer-reported data and examples of disparity reduction proposals.
Conducting Population Health Improvement Activities and Interventions to Narrow
Observed Disparities in Care
After collection and submission of three years of baseline data for the indicators of potential gaps in
care related to the four conditions, Covered California has worked with each insurer to select a quality
improvement project aimed at narrowing a health care disparity found in the baseline data related to the
four target conditions. Covered California has met with each insurer to discuss opportunities for
conducting quality improvement activities and interventions to narrow each health insurer’s specific
observed health care disparities. In 2020, each Covered California insurer will implement a quality
improvement project aimed at narrowing a health care disparity and will periodically report their
progress. Covered California will hold insurers accountable for narrowing the selected disparity while
maintaining or improving outcomes for targeted enrollees, which in most cases encompasses more
than just Covered California members — sometimes including all commercial enrollees and other
enrollees in the individual market or all Medi-Cal enrollees.
In addition to data reporting and analysis, insurers are reporting progress on infrastructure and staffing
enhancements needed to develop their health care disparity reduction project, as well as related and
aligned activities to support this Covered California initiative. These activities range in scope and scale:
some represent the next phase of multi-year efforts while others are starting by proposing time-limited
or smaller scale projects. The following are examples of activities reported by insurers:
• Enhanced member education, messaging, incentives and self-management tools.
• Enhanced provider education and clinical guidance reminders.
• Streamlined data collection processes to increase reporting and monitoring quality.
• Focused partnerships with community stakeholders.
• Disease registry development and sharing between providers and insurers.
• Outreach events and mobile care in at-risk communities.
• Enhanced care team support for affected populations.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 21
These important efforts are building the foundation for increasingly effective interventions to improve
care for all while reducing disparities in both health and health care.
The tables below document four representative examples of the target populations, measurement gaps
and interventions proposed to be undertaken by health insurance companies.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 22
Table 8. Health Net’s Proposed Interventions for Improved Diabetes and Hypertension Management
Rationale and Target Population(s) for Intervention
Summary of Select Interventions
Health Net proposes to target African American and Latino
members for improved diabetes and hypertension management
across Medi-Cal and individual market (Covered California and
off-exchange) lines of business.
Rationale and Target Population(s) for Intervention
• Rates for HbA1c control for African American members are 14
percent lower than white members with diabetes.
• Rates for blood pressure control for African American
members are 32 percent lower than white members with
hypertension.
• Rates for blood pressure control for Latino members are 28
percent lower than white members with hypertension.
Community, Member and Provider
Interventions
• Focus on the social determinants
of health (SDOH), social
marketing, and community
coalition and advisory group.
• Collection of member-level SDOH
data, one-stop clinics, medication
adherence bundle protocols;
nutrition and food insecurity pilot.
• Partnership with select clinic and
hospital; modified workflow;
motivational interviewing training.
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Table 9. LA Care’s Proposed Interventions for Improved Diabetes Management
Rationale and Target Population(s) for Intervention
Summary of Select Interventions
L.A. Care proposes to target African American and American
Indian/Alaskan Native members for improved diabetes
management for the Covered California line of business.
Rationale and Target Population(s) for Intervention
• The prevalence of diabetes among African Americans is 40
percent higher compared to the overall Los Angeles County
population.
• The prevalence of diabetes among American Indian/Alaskan
Natives is more than 50 percent higher compared to the
overall Los Angeles County population.
• Rates of HbA1c control for African American members are 8
percent lower than the total diabetes population.
• Rates of HbA1c control for American Indian/Alaskan Native
members are 12 percent lower than the total diabetes
population.
Member, Provider and Administrative
Interventions
• Online member portal diabetes
education course.
• Provider feedback, education and
reminders of guideline therapies
for members with diabetes control
below target.
• Systematic data collection process
improvements to improve the
accuracy and timeliness of HbA1c
laboratory data.
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 23
Table 10. Kaiser Permanente’s Proposed Interventions for Improved Diabetes and Hypertension
Management
Rationale and Target Population(s) for Intervention
Summary of Select Interventions
Kaiser Permanente proposes to target African American and
Latino members for improved diabetes and hypertension
management across Commercial lines of business (employer-
based and individual market, for both Covered California and off-
exchange enrollment).
Rationale and Target Population(s) for Intervention
• Mortality due to diabetes is 50 percent higher in
Hispanic/Latino than in White members.
• Mortality due to hypertension is 4-5 times higher in African
Americans than in white members.
• Rates of HbA1c control among Hispanic/Latino members are
12 percent lower than the overall Commercial diabetes
population.
• Rates of blood pressure control for Black/African American
members are 7 percent lower than for the overall Commercial
hypertensive population.
Member, Provider, and Administrative
Interventions
• Forums across sites for sharing
best practices
• Ongoing review of patient-facing
materials for culturally responsive
messaging
• Language concordant care for
Latino diabetics
• Innovative approaches to
community outreach (e.g. Mobile
Health Vehicle to churches, blood
pressure checks in barber shops)
• Specialty blood pressure clinic for
Black/African American members
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Table 11. Anthem’s Proposed Interventions for Improved Depression Medication Management
Rationale and Target Population(s) for Intervention
Summary of Select Interventions
Anthem proposes to target Hispanic/Latino members for improved
depression medication management for the Covered California
line of business.
Rationale and Target Population(s) for Intervention
• Rates for the Antidepressant Medication Management
(Effective Acute Phase Treatment) for Hispanic/Latino
members are 40 percent lower than White Covered California
members.
• Rates for the Antidepressant Medication Management
(Effective Continuation Phase Treatment) for Hispanic/Latino
members are 32 percent lower than White Covered California
members.
Member, Provider, and Policy
Interventions
• Member outreach and coaching
through mail and telephone;
telehealth initiatives for psychology
and psychiatry services; pilot for
prescribing providers and
members
• Review of provider education
materials communications and
implement changes, as
appropriate, with aim to reduce
care gaps
• Updated evaluation of HEDIS
specifications for potential
advocacy
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 2
COVERED CALIFORNIA 24
Section 3: Implications for the Future
Satisfaction surveys (CAHPS) demonstrate that Covered California enrollees rate their health plans
highly on two comprehensive measures. The Covered California initiative to promote health equity
through individualized, equitable care for all is just beginning. As described in this chapter, finding
appropriate data to use as a baseline for building strategies has been and will continue to be a
challenge until all insurers have more complete clinical data. Despite these challenges, insurers have
found actionable disparities and early initiatives are underway. As with other efforts to improve the
performance of the health care system, addressing disparities in health and health care can best be
accomplished by using data and evidence to understand the underlying causes of poor performance
and by working with all involved to develop, test and spread successful interventions.
Even accounting for differences in measurement and populations, the findings regarding disparities in
care suggest that on some measures, the more integrated health insurance companies report better
quality scores for all groups – to levels that are among the best in the country. While some of these
insurers have long invested in and hired staff to support culturally competent care, these findings
suggest that integrated and coordinated approaches to care delivery may reduce racial or ethnic
disparities on some measures of quality.
Covered California is evaluating progress and identifying opportunities for expansion of its health equity
program in the future, including potentially analyzing health outcomes based on other demographic
categories such as: (1) income; (2) disability status; (3) sexual orientation; (4) gender identity; and (5)
limited English proficiency (LEP). Since the data is collected across all lines of business, Covered
California will seek collaboration with other purchasers, especially the Department of Health Care
Services (DHCS), which oversees California’s Medi-Cal program that serves over approximately one
third of the entire California population. Covered California is also considering encouraging all insurers
to acquire the National Committee for Quality Assurance’s (NCQA) Distinction in Multicultural Health
Care (MHC) as this program recognizes organizations that provide culturally and linguistically sensitive
services and that work to reduce disparities in health and health care.
In the current contract, Covered California requires its insurers to engage in and report on efforts to
impact the health of populations beyond their enrollees. Both the data provided by the insurers and
research conducted by Health Management Associates (HMA) did not find evidence of the efficacy of
such interventions.
19
There is, however, evidence of the impact of health insurance companies focusing
on specific social determinants of health for enrolled populations — such as providing transportation or
food assistance for insured individuals with particular needs. Given these findings, Covered California is
reassessing the contractual expectations of its insurers for addressing social determinants of health.
Covered California has a potentially critical role to play in promoting broad engagement among public
and private purchasers to address health equity. In work commissioned by Covered California,
PricewaterhouseCoopers found that while focusing on health equity and disparities was a priority for
public purchasers, very few private purchasers consider this issue a priority.
20
19
The most current best evidence is documented in Chapter 1, Health Equity: Reducing Disparities, of a companion Covered California
report, Current Best Evidence and Performance Measures for Improving Quality of Care and Delivery System Reform.
20
“Health Purchaser Strategies for Improving Quality of Care and Delivery System Reform.” Review conducted for Covered California by
PricewaterhouseCoopers. Available at: https://hbex.coveredca.com/stakeholders/plan-
management/library/coveredca_health_purchaser_strategies_07-19.pdf.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 25
Chapter 3: Health Promotion and
Prevention
Health Promotion and Prevention relates to health
insurance company activities to encourage all
enrollees to receive preventive care services and
health screenings and use tools that promote a
healthy lifestyle. This includes everything from
regular checkups to smoking cessation and dietary
programs.
This chapter on Health Promotion and Prevention is
organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Health Plan Measures Reported to the
Marketplace Quality Rating System
Section 3. Implications for the Future
Section 1. Qualified Health Plan
Experience
Qualified Health Plan Experience presents
performance data reported by health insurance
companies for contract requirements and includes
assessments and observations by Covered
California. Prevention and wellness are key
components of high-value health care. Research
shows that treating those who are sick is often far
costlier and less effective than preventing disease
from occurring and keeping populations healthy.
Prevention occurs at three levels, each of which is
important in promoting enrollee health and wellness
and each of which is represented in Covered
California’s prevention reporting and requirements.
• Primary Prevention: Primary prevention
focuses on intervening before a health event
occurs. Promotion of healthy behaviors and
vaccinations are forms of primary prevention
that insurers play a role in promoting.
Intervening on risk factors for disease, like
obesity or smoking status, is also a form of
primary prevention.
• Secondary Prevention: Secondary
prevention includes screening for diseases to
identify diseases at an early stage. The
positive impact of timely screening for
• Kaiser Permanente frequently
performed at or above the 90
th
percentile nationally on preventive
screening measures while most other
plans performed in the 25
th
to 90
th
percentile.
• For the three HEDIS preventive care
measures Covered California identified
as priority measures — breast,
cervical, and colorectal cancer
screening — not only was there wide
variation observed among plans over
the past four years, but from two to six
health plans reported performance
below the 25
th
percentile nationally —
highlighting both the need and
opportunity for improvement.
• Across insurers, there exist robust
health communication processes to
inform enrollees about health and
wellness benefits. Insurers offered
information about free preventive
services, offered a 24/7 telephonic
nurse line, inbound and outbound
telephonic coaching, as well as
member reminders.
• Contract requirements call for reporting
on tobacco cessation and obesity
management programs, but this data
was incomplete due to the lack of
access to clinical data for most
insurers. Covered California is looking
at the feasibility of (1) better collection
of clinical data to improve enrollee
identification or requiring insurers to do
so and (2) better tracking of program
availability and participation rates.
• Covered California is assessing what
factors contribute to better
performance among some providers in
non-Kaiser Permanente insurers and
how Kaiser Permanente’s performance
can be replicated across California.
Highlights

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 26
cancer, for example, is well documented. This screening helps providers identify and treat
cancers early, before symptoms appear.
• Tertiary Prevention: Tertiary prevention focuses on managing diseases after a diagnosis to
help slow or stop disease progression and prevent debilitating or other negative impacts of
disease.
Covered California’s prevention and wellness requirements are centered on identifying enrollees who
are eligible for certain preventive and wellness benefits, notifying enrollees about the availability of these
services, and making sure those eligible receive appropriate services. Proactively identifying and
notifying enrollees eligible for prevention and wellness benefits, monitoring health status and making
appropriate referrals, and ensuring at-risk enrollees receive proactive coordinated care all center around
making sure people get the right preventive care when they need it at all three levels of prevention,
instead of waiting until more serious and costly manifestations of disease prompt care. Covered
California has identified several priority disease areas for reporting, including those with significant
evidence around the importance of prevention. Under contract requirements, insurers are required to
report the following:
1. Utilization of tobacco cessation intervention services;
2. Utilization of obesity management services;
3. Processes for communicating health and wellness benefits to enrollees and providers and the
way they incorporate and use of enrollee-specific health and wellness information; and
4. Utilization of necessary preventive services through the following select HEDIS measures:
breast cancer screening, cervical cancer screening, colorectal cancer screening, and chlamydia
screening for women.
Tobacco Cessation
Covered California health insurance companies reported significant data challenges in reporting both
the number of tobacco dependent enrollees and participation rates in smoking cessation programs.
Integrated delivery systems, such as Kaiser Permanente and Sharp Health Plan, reported the most
consistent data year-over-year, likely due to having access to clinical data that confirms a diagnosis of
tobacco dependency. Other insurers were hampered by data challenges that include a lack of access
to clinical data, inability to track physician referrals to tobacco cessation programs or educational
classes offered by medical groups that are not documented or billed on a claim, reliance on enrollee
provided data in health risk assessments that are not universally administered, and inability to track by
lines of business, such as Covered California membership. Given this set of challenges, the available
data reported for both Covered California enrollees and members in all lines of business (inclusive of
Covered California) ranged between less than 1 percent to as high as 70 percent.
21
Covered California
cautions these figures are likely incomplete. Future requirements in this area will need to consider the
feasibility of (1) collecting clinical data to improve identification of tobacco dependent members and (2)
better tracking of program availability and participation rates.
21
Health plans reporting participation rates on the high end of the range generally had a far smaller number of enrollees identified as
tobacco dependent. Covered California did not calculate a weighted average participation rate due to incomplete reporting and data
collection challenges.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 27
Obesity Management
Covered California health insurance companies experienced a similar set of challenges for tracking
obese members; the most important of which is the lack of access to clinical data that documents a
diagnosis of obesity. Some insurers also reported they do not track specific lines of business, such as
Covered California membership, for participation in weight management programs. Some insurers
relied on data through health risk assessments, wellness portals, and self-referrals by enrollees. Given
this set of challenges, the available 2018 data reported for Covered California enrollees ranged
between less than 1 percent to roughly 40 percent. For members in all lines of business (inclusive of
Covered California),
22
the 2018 data ranged between roughly 1 percent to nearly 20 percent. Again,
Covered California cautions these figures are likely incomplete. Future requirements in this area will
need to consider the feasibility of (1) collecting clinical data to improve identification of obese members
and (2) better tracking of program availability and participation rates.
Processes for Communicating Health and Wellness Benefits
Through annual reporting, health insurance companies reported the methods used to communicate
health and wellness benefits to enrollees using pre-defined categories, such as customized printed
materials about free preventive services or 24/7 telephonic nurse lines. Table 12. Processes for
Communicating Health and Wellness Benefits for Commercial and Covered California Enrollees, 2016
summarizes this data which reflects insurers’ activities in 2016 as this information was not required in
later reporting.
Health communication processes offered to enrollees are relatively consistent across health insurance
companies. Most or all insurers offered information, both template and customized, about free
preventive services, offered a 24/7 telephonic nurse line, inbound and outbound telephonic coaching,
as well as member care service reminders. While not universally used, most health insurance
companies reported using nurse lines for specific populations (i.e., complex conditions or oncology
patients) as well as interactive voice response (IVR) member care/service reminders (offered by 7 out
of 12 insurers).
22
Health plans reporting participation rates on the high end of the range generally had a far smaller number of enrollees identified as
tobacco dependent. Covered California did not calculate a weighted average participation rate due to incomplete reporting and data
collection challenges.
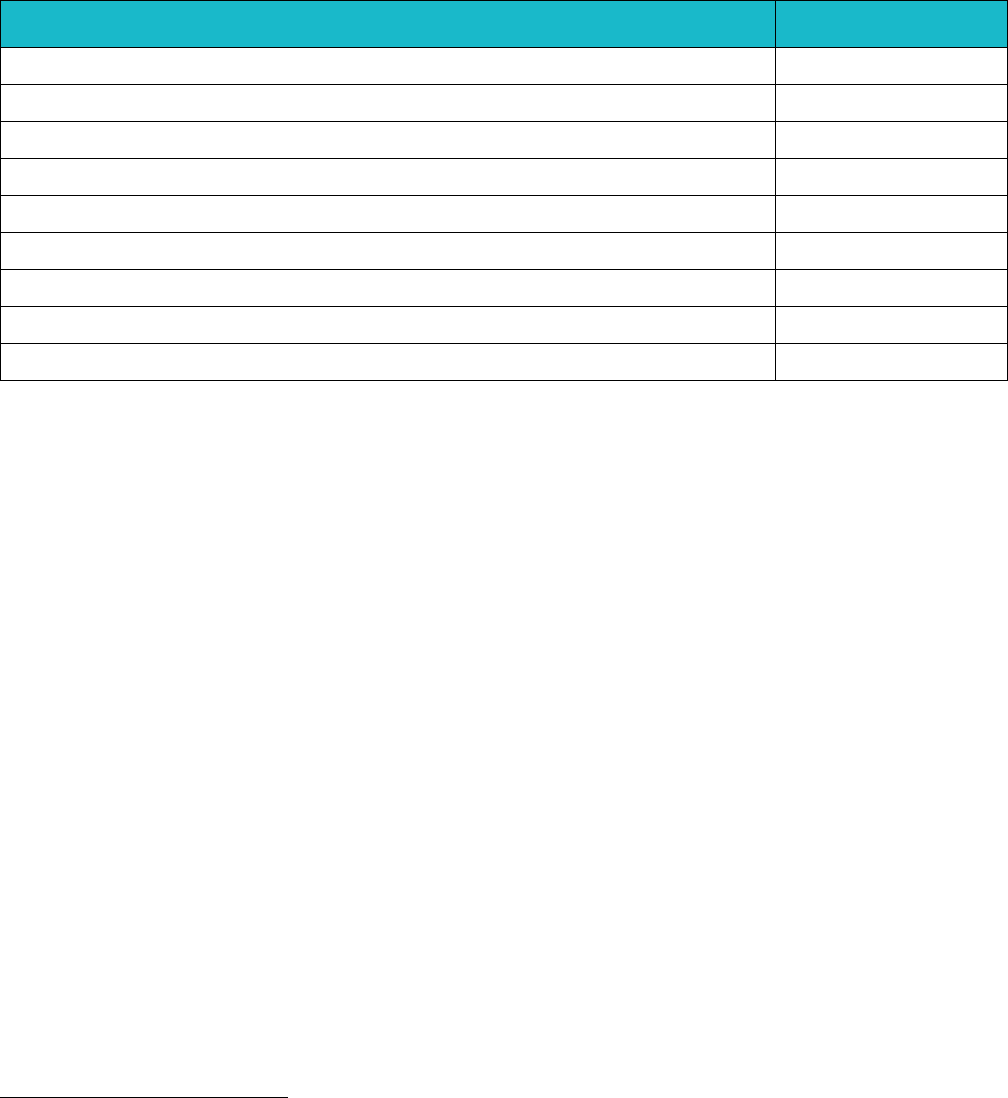
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 28
Table 12. Processes for Communicating Health and Wellness Benefits for Commercial and Covered
California Enrollees, 2016
23
Processes for Communicating Health and Wellness Benefits
Number of
Health Plans
Template newsletter articles/printed materials about free preventive services
12
Customized printed materials about free preventive services
11
24/7 Telephonic Nurse Line
11
24/7 Nurse Navigator for complex conditions
4
24/7 Nurse Navigator for oncology management
3
Inbound telephonic health coaching
12
Outbound telephone health coaching
10
Member care/service reminders (IVR)
7
Member care/service reminders (Paper)
11
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Section 2. Health Plan Measures Reported to the Marketplace Quality
Rating System
Health Plan Measures Reported to the Marketplace Quality Rating System details health plan
performance on Healthcare Effectiveness Data Information Set (HEDIS) and Consumer Assessment of
Healthcare Providers and Systems (CAHPS) measures reported to the Centers for Medicaid and
Medicare Services’ Quality Rating System (QRS). These standard performance measures are a key
mechanism used by Covered California for health plan oversight and accountability. To more sharply
focus health plan accountability efforts, Covered California examined over 40 measures used by QRS
and is proposing to prioritize a subset of 13 measures that were selected based on the following
criteria: (1) health impact; (2) extent of health plan variation; (3) performance improvement opportunity;
(4) alignment with other California accountability programs; and (5) balance across domains of care,
such as prevention, chronic illness care and behavioral health. Three of the 13 measures also overlap
with the measures currently collected by race/ethnicity for health disparities reduction interventions as
discussed in Chapter 2.
The following tables display the three measures for Health Promotion and Prevention in the QRS
measure set that Covered California has identified as priority measures (with eight additional measures
detailed in Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System).
23
The 11 health insurance companies in Covered California are: Anthem Blue Cross, Blue Shield of California, Chinese Community Health
Plan, Health Net, Kaiser Permanente, L.A. Care, Molina Healthcare, Oscar Health, Sharp Health Plan, Valley Health Plan, and Western
Health Advantage. In this table, Health Net is counted twice because its reports data separately for Health Net Life (PPO/EPO products)
and Health Net of California (HMO/HSP products).
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 29
The tables include the Covered California weighted average, highest and lowest performing plans,
plan-specific performance, as well as national percentiles for all Marketplace plans. The priority
measures are:
1. Breast Cancer Screening (Table 13)
2. Cervical Cancer Screening (Table 14
3. Colorectal Cancer Screening (Table 15)
See Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System, for eight
additional QRS measures that pertain to Health Promotion and Prevention:
4. Chlamydia Screening in Women (Table A1)
5. Adult BMI Assessment (Table A2)
6. Childhood Immunizations (Combination 3) (Table A3)
7. Immunizations for Adolescents (Combination 2) (Table A4)
8. Flu Vaccinations for Adults Ages 18-64 (Table A5)
9. Medical Assistance with Smoking and Tobacco Use Cessation (Table A6)
10. Weight Assessment and Counseling for Nutrition and Physical Activity for Children and
Adolescents (Table A7)
11. Annual Dental Visit (Table A8)
Appendix 2 also describes how to interpret the display of the measures.
Performance on other measures included in the QRS measure set are presented in relevant subject
chapters, but most are covered in Chapter 5: Acute, Chronic and Other Conditions.
For the Health Promotion and Prevention measures, some of the overall observations include:
• Kaiser Permanente frequently performed at or above the 90
th
percentile nationally on preventive
screening measures while most other plans performed in the 25
th
to 90
th
percentile.
• For the three HEDIS preventive care measures Covered California identified as priority
measures — breast, cervical, and colorectal cancer screening — not only was there wide
variation observed among plans over the past four years, but from two to six health plans
reported performance below the 25th percentile nationally — highlighting both the need and
opportunity for improvement.
• The variation in performance, with some health plans performing below the 25
th
percentile
nationally is reflected in the eight measures reported in Appendix 2.
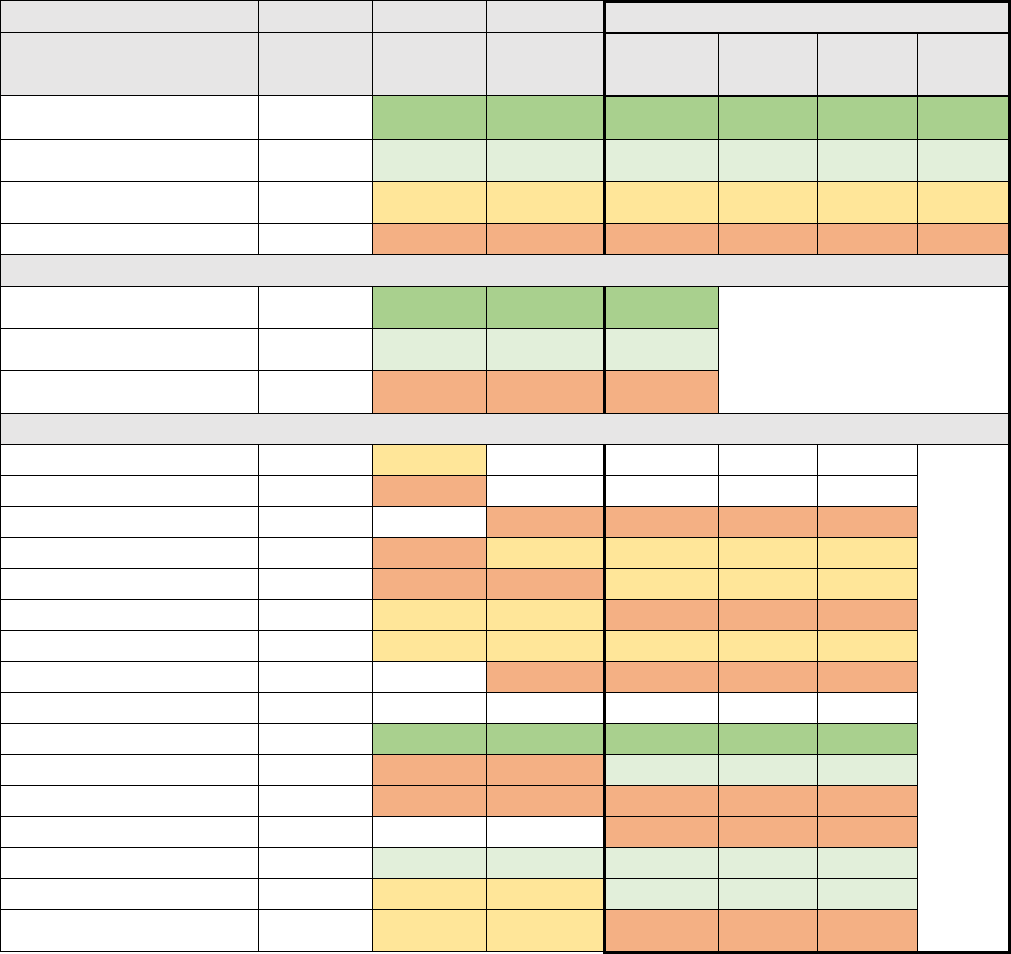
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 30
Breast Cancer Screening
The Breast Cancer Screening measure is the percentage of women 50-74 years of age who have
received a mammogram to screen for breast cancer.
Table 13. Breast Cancer Screening for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
79 +
79 +
79 +
35%
477,683
1
Plans at 50th to 90th
Percentile
MN-S
70 to 79
70 to 79
70 to 79
9%
118,451
3
Plans at 25th to 50th
Percentile
MN-S
65 to 70
65 to 70
65 to 70
43%
573,681
3
Plans Below 25th Percentile
MN-S
Below 65
Below 65
Below 65
13%
176,811
6
Covered California High/Average/Low Performers
Covered CA Highest
Performer
89
86
84
84
Covered CA Weighted
Average
74
70
72
72
Covered CA Lowest
Performer
67
52
58
47
Covered California Plan-Specific Performance
Anthem HMO
70
67
Anthem PPO
68
61
Anthem EPO
58
57
5%
64,031
Blue Shield HMO
63
65
69
7%
93,322
Blue Shield PPO
67
61
65
65
25%
335,176
CCHP HMO
87
65
68
64
1%
10,013
Health Net HMO
71
66
69
69
11%
145,183
Health Net EPO
62
58
0%
1,396
Health Net PPO
Kaiser Permanente HMO
89
86
84
84
35%
477,683
LA Care HMO
52
65
73
6%
84,750
Molina Healthcare HMO
59
61
47
4%
56,023
Oscar Health Plan EPO
51
3%
35,962
Sharp Health Plan HMO
82
76
74
72
1%
17,335
Valley Health Plan HMO
69
67
71
1%
16,366
Western Health Advantage
HMO
75
69
65
64
1%
9,386
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
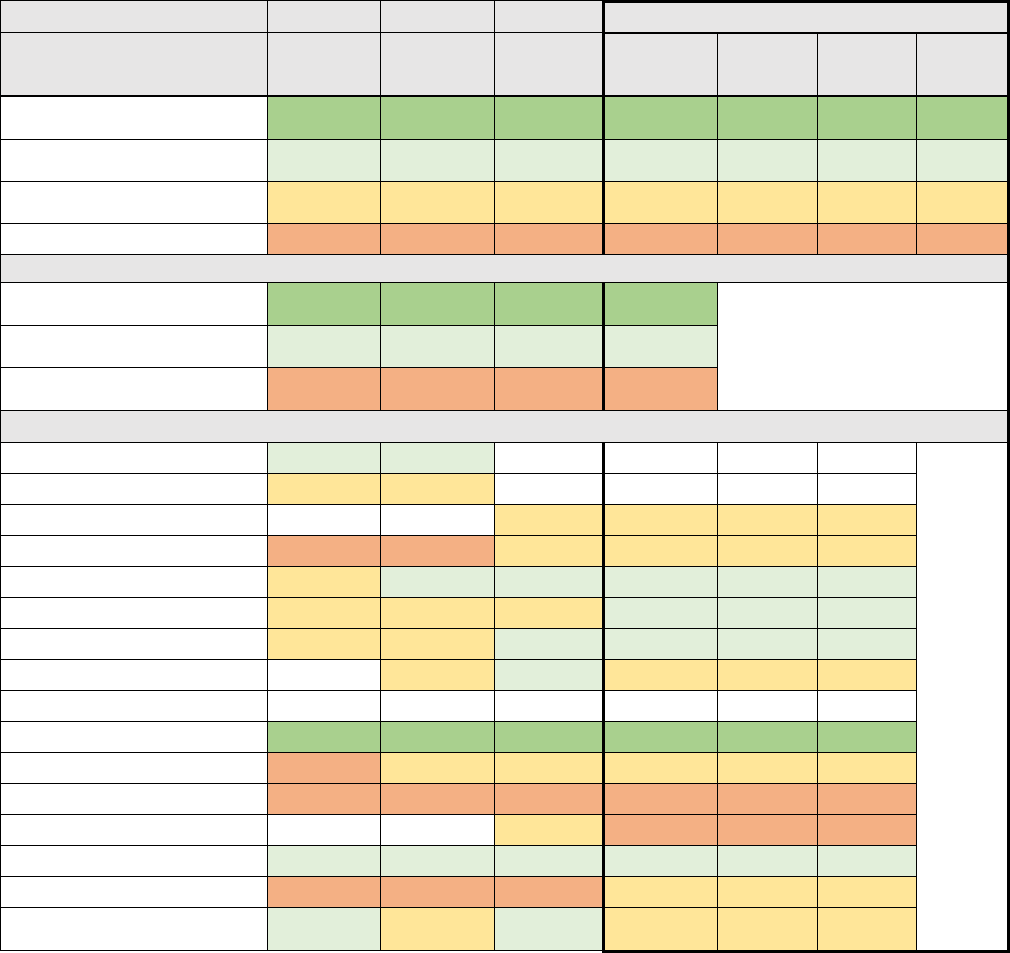
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 31
Cervical Cancer Screening
The Cervical Cancer Screening measure is the percentage of women 21-64 years of age who were
screened for cervical cancer.
Table 14. Cervical Cancer Screening for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
72 +
71 +
74 +
73 +
35%
477,683
1
Plans at 50th to 90th
Percentile
55 to 72
56 to 71
56 to 74
56 to 73
38%
507,707
4
Plans at 25th to 50th
Percentile
46 to 55
47 to 56
48 to 56
48 to 56
20%
269,251
6
Plans Below 25th Percentile
Below 46
Below 47
Below 48
Below 48
7%
91,985
2
Covered California High/Average/Low Performers
Covered CA Highest
Performer
81
82
80
79
Covered CA Weighted
Average
59
62
65
64
Covered CA Lowest
Performer
35
33
41
42
Covered California Plan-Specific Performance
Anthem HMO
59
62
Anthem PPO
55
53
Anthem EPO
55
53
5%
64,031
Blue Shield HMO
41
45
49
48
7%
93,322
Blue Shield PPO
52
59
63
60
25%
335,176
CCHP HMO
50
53
56
57
1%
10,013
Health Net HMO
50
55
60
56
11%
145,183
Health Net EPO
53
59
53
0%
1,396
Health Net PPO
Kaiser Permanente HMO
81
82
80
79
35%
477,683
LA Care HMO
35
54
51
54
6%
84,750
Molina Healthcare HMO
40
33
41
42
4%
56,023
Oscar Health Plan EPO
50
45
3%
35,962
Sharp Health Plan HMO
56
61
62
64
1%
17,335
Valley Health Plan HMO
38
46
43
50
1%
16,366
Western Health Advantage
HMO
59
55
62
54
1%
9,386
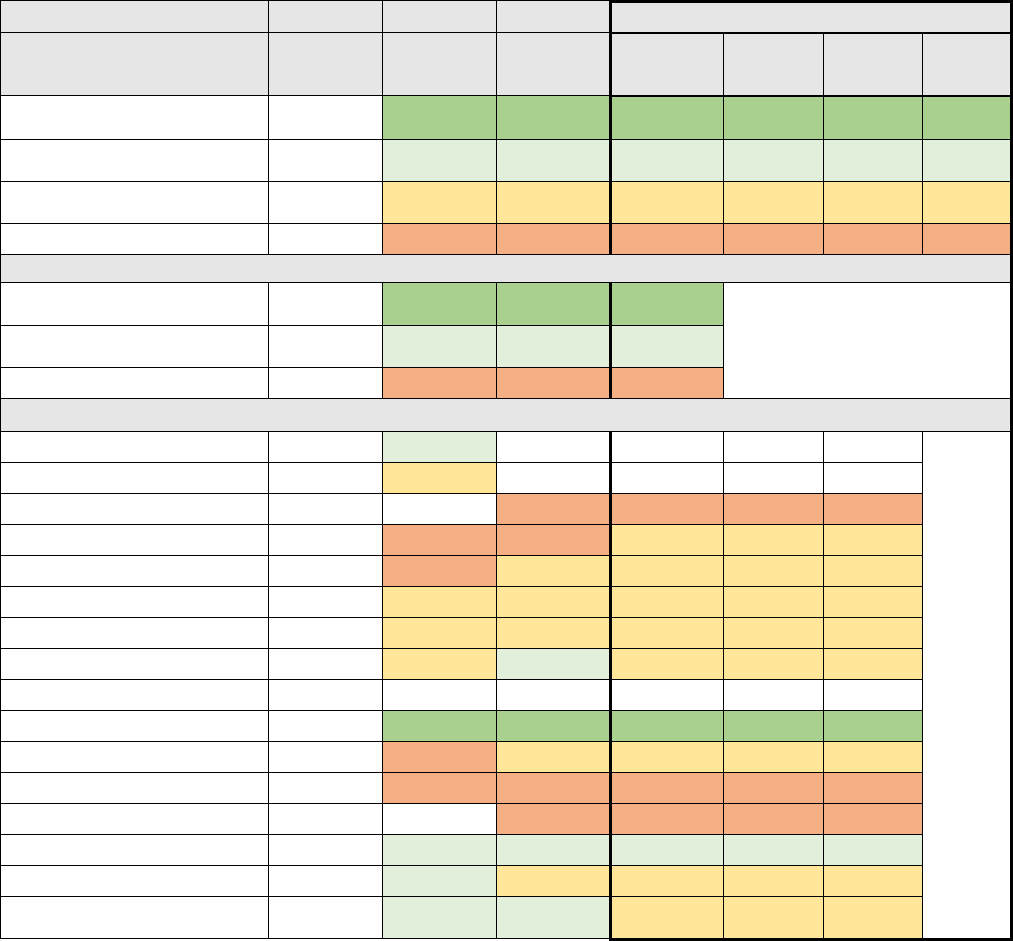
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 32
Colorectal Cancer Screening
The Colorectal Cancer Screening measure is the percentage of adults 50-75 years of age who had
appropriate screening for colorectal cancer.
Table 15. Colorectal Cancer Screening for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
67 +
68 +
69 +
35%
477,683
1
Plans at 50th to 90th
Percentile
MN-S
52 to 67
54 to 68
55 to 69
1%
17,335
1
Plans at 25th to 50th
Percentile
MN-S
44 to 52
45 to 54
47 to 55
52%
695,592
8
Plans Below 25th Percentile
MN-S
Below 44
Below 45
Below 47
12%
156,016
3
Covered California High/Average/Low Performers
Covered CA Highest
Performer
82
80
78
76
Covered CA Weighted
Average
51
55
58
58
Covered CA Lowest Performer
28
35
34
27
Covered California Plan-Specific Performance
Anthem HMO
46
53
Anthem PPO
44
47
Anthem EPO
42
40
5%
64,031
Blue Shield HMO
38
36
39
51
7%
93,322
Blue Shield PPO
41
42
51
49
25%
335,176
CCHP HMO
46
49
53
53
1%
10,013
Health Net HMO
41
47
51
51
11%
145,183
Health Net EPO
48
54
49
0%
1,396
Health Net PPO
Kaiser Permanente HMO
82
80
78
76
35%
477,683
LA Care HMO
29
38
49
54
6%
84,750
Molina Healthcare HMO
28
35
34
27
4%
56,023
Oscar Health Plan EPO
37
36
3%
35,962
Sharp Health Plan HMO
62
55
66
57
1%
17,335
Valley Health Plan HMO
54
52
50
54
1%
16,366
Western Health Advantage
HMO
62
53
57
52
1%
9,386
*M-NS: This measure was not used in determining the overall QRS rating in 2016.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 3
COVERED CALIFORNIA 33
Section 3. Implications for the Future
Covered California included reporting requirements related to smoking cessation and obesity
management programs because substantial evidence shows that effective interventions can improve
health outcomes and reduce health care costs.
24
Based on the inability of insurers to provide
information on program participation in a consistent manner, Covered California is considering other
ways to promote these services including exploring the feasibility of (1) collecting clinical data to
improve enrollee identification or (2) better tracking of program availability and participation rates and
perhaps using large databases that predict public health risks by census track. Covered California is
working with insurers to ensure these health promotion and prevention programs are offered in the
languages spoken by their enrollees and further promote the availability of translation services.
In the major areas related to health plan measures of screening, the main observation from the
reporting over the past four years is that there is wide variation among the plans. Kaiser Permanente
and Sharp Health Plan frequently report screening rate scores that are in the top 90
th
percentile in the
nation; while other most of the other plans have lower scores – ranging from the 25
th
to just above the
50
th
percentile. The fact that several health plans performed below the 25
th
percentile nationally on
cancer screenings and on other preventive care measures detailed in Appendix 2 — in particular, six
health plans had a breast cancer screening rate score below the 25
th
percentile — is concerning and
warrants concerted efforts from both Covered California and the health plans to address. Low
screening rates could be partially attributed to poor data collection techniques and lack of patient
education and engagement. Covered California is engaging with its contracted health plans to develop
strategies to improve their screening rates.
The ability of integrated systems, such as Kaiser Permanente and Sharp Health Plan, to achieve such
positive results is a clear indicator of what is possible with well-coordinated and integrated care. In
future years, Covered California should assess what factors can contribute to better performance
among non-integrated plans and how the performance of integrated systems can be replicated across
California. Covered California will seek to foster national benchmark performance across all plans.
24
The most current best evidence is documented in Chapter 2, Health Promotion and Prevention, of a companion Covered California report,
Current Best Evidence and Performance Measures for Improving Quality of Care and Delivery System Reform.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 34
Chapter 4: Mental Health and
Substance Use Disorder Treatment
Mental Health and Substance Use Disorder
Treatment includes health insurance company
activities to identify, engage and provide treatment to
those with mental health conditions and substance
use disorders, and ensure that they are provided with
timely and effective care that is integrated with their
general health care needs.
This chapter on Mental Health and Substance Use
Disorder Treatment is organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Health Plan Measures Reported to the
Marketplace Quality Rating System
Section 3. Implications for the Future
Section 1. Qualified Health Plan
Experience
Qualified Health Plan Experience presents
performance data reported by insurers for contract
requirements and includes assessments and
observations by Covered California. Covered
California recognizes the critical importance of
mental health and substance use disorder treatment,
collectively “behavioral health services,” in improving
health outcomes and reducing costs. Consistent with
the ACA’s expansion of mental health and substance
use disorder services and promotion of integrating
these services into mainstream health care, Covered
California requires insurers to report progress on:
1. Making behavioral health services available
to enrollees;
2. Integrating behavioral health services with
medical services; and
3. Reporting the percent of enrollees cared for
in an integrated behavioral health model.
In the absence of an established best practice for
integrating medical and behavioral health services in
2016, the current contract requirements largely focus
on gathering qualitative information about health
insurance company strategies. Covered California
has summarized strategies reported by insurers but
• For the adult behavioral health
measures, there is wide variation in
performance among the plans over the
past four years with most health plans
performing poorly. For two of three
priority measures in 2019, six or more
plans performed below the 25
th
percentile. For each of the three
measures, only one plan performed at
or above the 90
th
percentile nationally.
Covered California is actively engaging
with insurers on how to improve in
these areas.
• To promote access to and availability
of behavioral health services, insurers
report a range of activities, including
increasing provider capacity,
implementing telehealth services, and
adopting new CPT codes that support
care collaboration.
• Insurers are pursuing a broad
spectrum of behavioral health
integration efforts, including co-location
of services, increased coordination
with carve-out vendors, and embedded
behavioral health staff in primary care
clinics.
• The percent of enrollees cared for
under an integrated behavioral health
model appears to have increased
between 2015 and 2018.
Requirements for future reporting are
being revised to better support tracking
and trending of behavioral health
integration.
• Covered California is exploring how
best to use patient-reported outcome
measures to track improvement in
behavioral health care. Monitoring
outcomes for behavioral health is a
major gap in assessing performance of
insurers and the delivery system.
Highlights

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 35
notes that these qualitative descriptions will benefit from standardized definitions to better quantify
adoption in future reporting.
Promoting Availability of Behavioral Health Services, 2015, 2017 and 2018
25
The following are strategies one or more health insurance companies adopted to promote the
availability of behavioral health services during 2015, 2017 and 2018:
• Added a full-time Behavioral Health Medical Director to the physician leadership team; added
mental health providers, psychiatrists (including with bilingual skills), and medical social workers
to the provider network;
• Increased access in the following ways:
o Offered more appointments through expanded hours and expanded and improved
facilities where mental health and wellness care is provided;
o Allow enrollees to self-refer to behavioral health providers instead of requiring prior
authorization;
o Provided open access to free-standing network for professional and facility behavioral
health providers;
o Offered a telehealth program, with some offering a 24/7 program for behavioral health
services, including programs to improve psychiatry access;
o Annually monitored access through provider-to-member ratios, provider surveys,
member experience surveys, grievances and appeals and HEDIS results;
o Required underperforming providers to implement a corrective action plan;
o Offered classes on behavioral health; and
o Provided online patient portals.
• Adopted Psychiatric Care Collaborative Current Procedural Terminology (CPT) codes to
Physician Fee schedules and removed prior authorization requirements for behavioral health
outpatient services;
• Expanded opioid treatment and implemented a disease management program for depression;
• Carve-out or subcontracted vendors educated primary care physicians about behavioral health
services via hotlines, online toolkits, and provided access to Behavioral Health Integration
specialists and Community Transition coordinators some of whom were also on the medical
staff of physician organizations; and
• Deployed an electronic care management program that provides virtual psychiatric support and
financial incentives to improve care for patients with behavioral health issues, including
screenings and online consultations.
25
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 36
Integrating Behavioral Health Services with Primary Care, 2015, 2017 and 2018
26
The following are strategies one or more health insurance companies engaged in to integrate
behavioral health services with primary care during 2015, 2017 and 2018:
• Developed a universal consent form to allow data sharing between primary care and behavioral
health providers;
• Primary care physicians and behavioral health providers coordinated care through the same
medical record or through an e-management model that facilitated communication and
electronic data sharing. Leveraged an integrated data warehouse (medical, behavioral health,
pharmacy, etc.) to identify gaps in care and at-risk members for interventions by case
managers;
• Primary care physicians referred directly to behavioral health case management programs for
assistance with complex care patients; case management departments at the plan level helped
facilitate referrals to medical groups or providers; outpatient behavioral health departments that
were in the same physical location as primary care, pharmacy, and specialty services helped
facilitated primary care physician referrals and team-based care;
• Implemented a “Feedback-Informed Care” model which involves soliciting an enrollee’s
feedback about the therapy process and allowing them to direct their care;
• Implemented a pay-for-performance program that connected primary care physicians with
behavioral health providers to coordinate on referrals and care coordination;
• Integrated behavioral health with providers participating in Accountable Care Organization
(ACO) models;
• Worked with a health system to integrate psychiatrists within primary care clinics;
• Provided care management following discharge from an inpatient setting;
• Implemented a co-management strategy that involves integrated clinical rounds between
medical and behavioral health teams; and
• Managed behavioral health needs through carve-out vendors or delegated providers as follows:
o Enhanced coordination of behavioral and physical health care through housing carve-out
vendors onsite, monthly joint clinical rounds or weekly integration meetings with co-
located providers.
o Carve-out vendors monitored outcomes, such as case management volume and
engagement, utilization management trends, and quality of care issues.
o Shared data with carve-out vendors to monitor drug interactions and compliance.
o Held periodic meetings with delegated behavioral health providers to focus on a variety
of topics, including data, best practices, communication and collaboration, referral
processes, HEDIS measures performance, and CAHPS Experience of Care and Health
Outcomes (ECHO) survey results.
26
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 37
Enrollees Cared for in an Integrated Behavioral Health Model, 2015 and 2018
27
Health insurance companies reported the percent of enrollees cared for in an integrated behavioral
health model (IBHM) based on their respective definitions as current contract requirements do not
include standard reporting on best practices implemented (e.g., use of unified care plans or patient
registries). It is important to note that this measure also does not capture the range of health insurance
company activities for behavioral health integration. As the percent of enrollees cared for in an IBHM is
a quantitative measure, the following numbers should be viewed with caution since (1) there has not
been a standard definition for an IBHM and (2) insurers reported incomplete data and Covered
California observed year-to-year inconsistencies.
In 2015, 2 percent of Covered California enrollees were cared for in an IBHM; with individual insurers
ranging from 0 to 6 percent.
28
Based on incomplete numbers for 2018, enrollees cared for in an IBHM
model appears to have increased to 11 percent, with reporting insurers ranging from 0 to 34 percent.
Given the challenges observed to date, requirements for future reporting will be based on standardized
best practices to support tracking and trending adoption of behavioral health integration.
Section 2. Health Plan Measures Reported to the Marketplace Quality
Rating System
Health Plan Measures Reported to the Marketplace Quality Rating System detail health plan
performance on Healthcare Effectiveness Data Information Set (HEDIS) and Consumer Assessment of
Healthcare Providers and Systems (CAHPS) measures reported to the Centers for Medicaid and
Medicare Services’ Quality Rating System (QRS). These standard performance measures are a key
mechanism used by Covered California for health plan oversight and accountability. To more sharply
focus health plan accountability efforts, Covered California examined over 40 measures used by QRS
and is proposing to prioritize a subset of 13 measures.
The following tables display the priority measures for Mental Health and Substance Use Disorder
Treatment in the QRS measure set (with one additional measure detailed in Appendix 2: Additional
Health Plan Measures Reported to the Quality Rating System) and include the Covered California
weighted average, highest and lowest performing plans, plan-specific performance, as well as national
percentiles for all Marketplace plans:
1. Antidepressant Medication Management (Table 16)
2. Follow Up After Hospitalization for Mental Illness (Table 17)
3. Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (Table
18)
See Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System, for one
additional QRS measure that pertains to Mental Health and Substance Use Disorder Treatment: Follow
Up Care for Children Prescribed ADHD Medication (ADD) (Table A9). Covered California is evaluating
27
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.
28
Data only available for plan years 2015 and 2018. Covered California waived data collection for plan year 2016 and 2017.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 38
available behavioral health measures for children as part of its work in finding the right measures for
subpopulations.
Appendix 2 also describes how to interpret the display of the measures.
For the priority adult behavioral health measures, there is wide variation in performance among the
health plans over the past four years with most plans performing poorly. For two of three priority
measures in 2019 (Antidepressant Medication Management and Initiation and Engagement of Alcohol
and Other Drug Abuse or Dependence Treatment), six or more plans performed below the 25
th
percentile. For each of the three measures, only one plan performed at or above the 90
th
percentile
nationally.
Covered California recognizes that there are additional behavioral health measures, such as Utilization
of the Patient Health Questionnaire-9 to Monitor Depression Symptoms for Adolescents and Adults,
that use clinical data to monitor patients at the time of diagnosis and outcomes over time and therefore
better represent the quality of care for depression. However, slow progress has been made in California
in collecting clinical or patient reported outcome measures through 2018. Until most health insurance
companies are collecting clinical data-based measures, Covered California must rely on the existing
behavioral health measures.
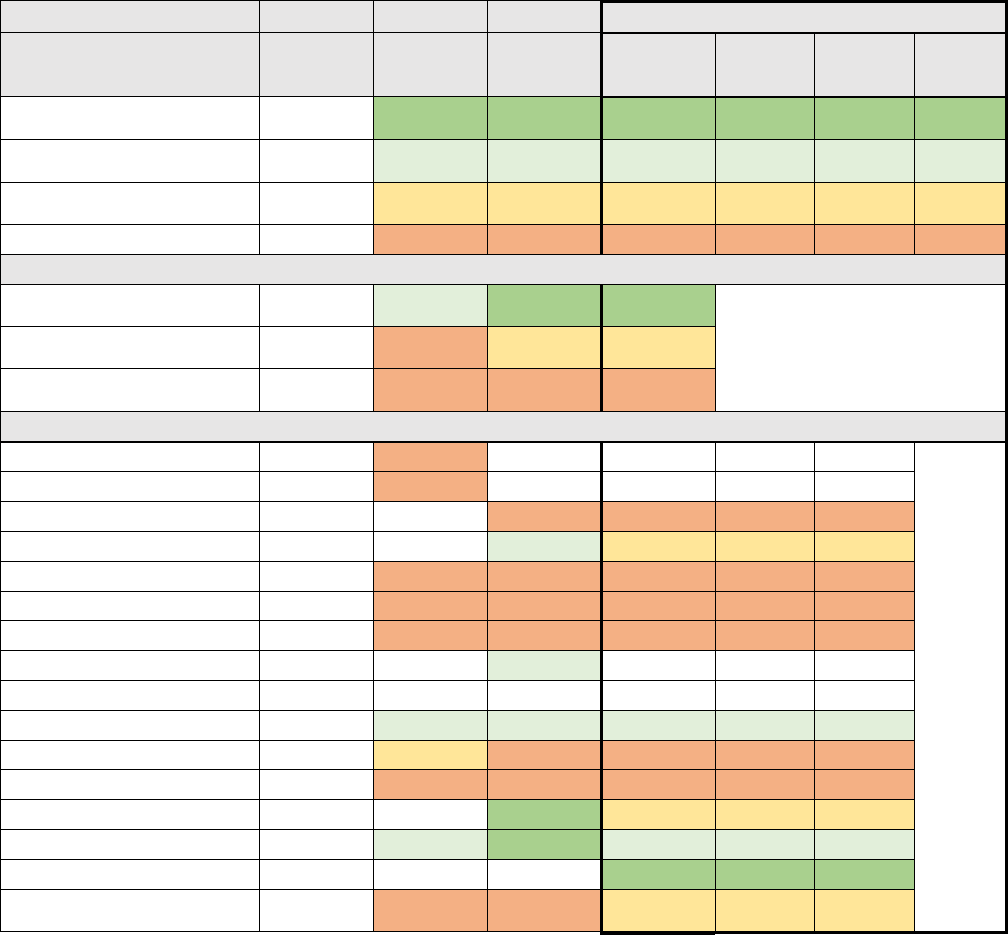
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 39
Antidepressant Medication Management
The Antidepressant Medication Management measure is the percentage of members 18 years of age
and older who were treated with antidepressant medication, had a diagnosis of major depression and
who remained on an antidepressant medication treatment.
1. Effective Acute Phase Treatment: The percentage of members who remained on an
antidepressant medication for at least 84 days (12 weeks).
2. Effective Continuation Phase Treatment: The percentage of members who remained on an
antidepressant medication for at least 180 days (6 months).
Table 16. Antidepressant Medication Management for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
72 +
73 +
73 +
1%
16,366
1
Plans at 50th to 90th
Percentile
MN-S
63 to 72
63 to 73
64 to 73
37%
495,018
2
Plans at 25th to 50th
Percentile
MN-S
58 to 63
57 to 63
59 to 64
10%
138,670
3
Plans Below 25th Percentile
MN-S
Below 58
Below 57
Below 59
52%
695,176
6
Covered California High/Average/Low Performers
Covered CA Highest
Performer
68
78
84
Covered CA Weighted
Average
57
60
61
Covered CA Lowest
Performer
43
36
43
Covered California Plan-Specific Performance
Anthem HMO
50
Anthem PPO
52
Anthem EPO
53
52
5%
64,031
Blue Shield HMO
66
60
7%
93,322
Blue Shield PPO
53
53
56
25%
335,176
CCHP HMO
56
36
43
1%
10,013
Health Net HMO
51
55
53
11%
145,183
Health Net EPO
65
Health Net PPO
Kaiser Permanente HMO
68
69
69
36%
477,683
LA Care HMO
61
54
56
6%
84,750
Molina Healthcare HMO
43
45
51
4%
56,023
Oscar Health Plan EPO
78
62
3%
35,962
Sharp Health Plan HMO
67
77
67
1%
17,335
Valley Health Plan HMO
84
1%
16,366
Western Health Advantage
HMO
57
46
61
1%
9,386
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
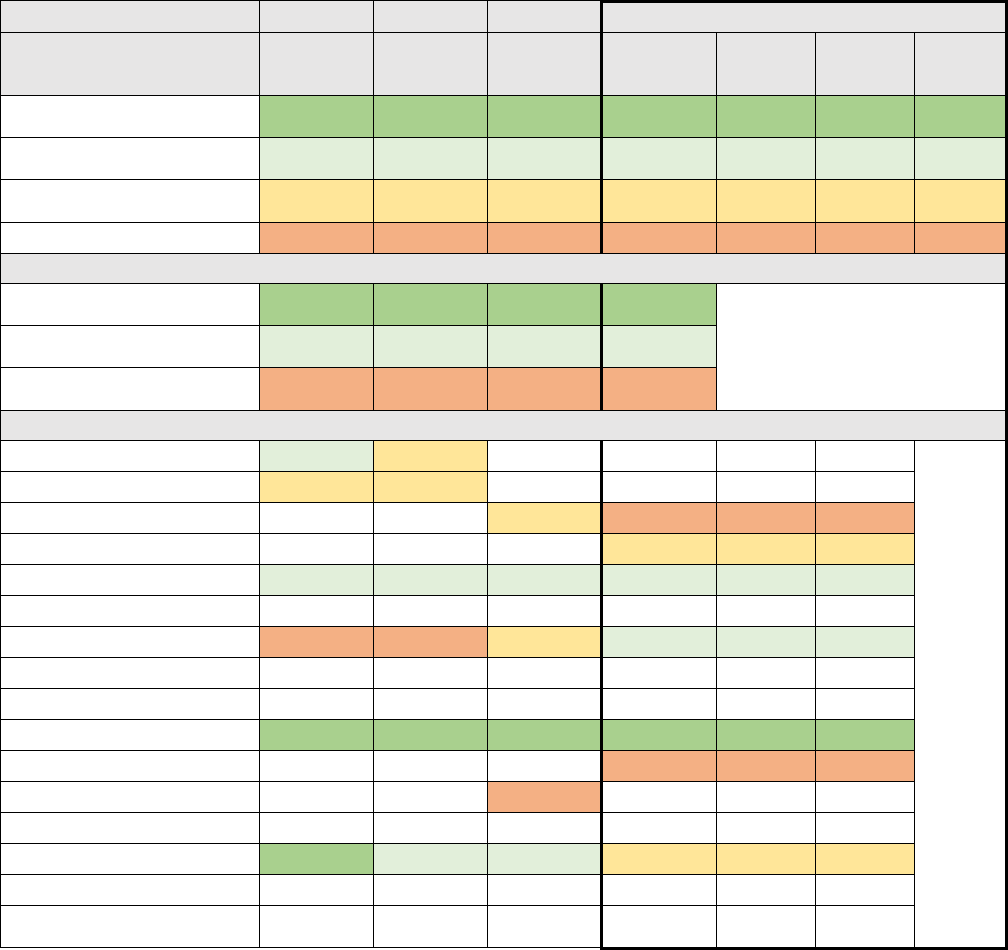
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 40
Follow Up After Hospitalization for Mental Illness
The Follow Up After Hospitalization for Mental Illness measure is the percentage of discharges for
members 6 years of age and older who were hospitalized for treatment of selected mental illness and
who had a follow-up visit with a mental health practitioner within 7 days after discharge.
Table 17. Follow Up After Hospitalization for Mental Illness for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
67 +
67 +
64 +
59 +
39%
477,683
1
Plans at 50th to 90th
Percentile
48 to 67
48 to 67
41 to 64
38 to 59
39%
480,359
2
Plans at 25th to 50th
Percentile
38 to 48
38 to 48
31 to 41
29 to 38
9%
110,657
2
Plans Below 25th Percentile
Below 38
Below 38
Below 31
Below 29
12%
148,781
2
Covered California High/Average/Low Performers
Covered CA Highest
Performer
75
79
73
72
Covered CA Weighted
Average
56
60
53
50
Covered CA Lowest
Performer
38
30
28
26
Covered California Plan-Specific Performance
Anthem HMO
51
48
Anthem PPO
43
44
Anthem EPO
39
27
5%
64,031
Blue Shield HMO
30
8%
93,322
Blue Shield PPO
56
55
42
38
28%
335,176
CCHP HMO
Health Net HMO
38
30
35
40
12%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
75
79
73
72
39%
477,683
LA Care HMO
26
7%
84,750
Molina Healthcare HMO
28
Oscar Health Plan EPO
Sharp Health Plan HMO
70
65
57
35
1%
17,335
Valley Health Plan HMO
Western Health Advantage
HMO
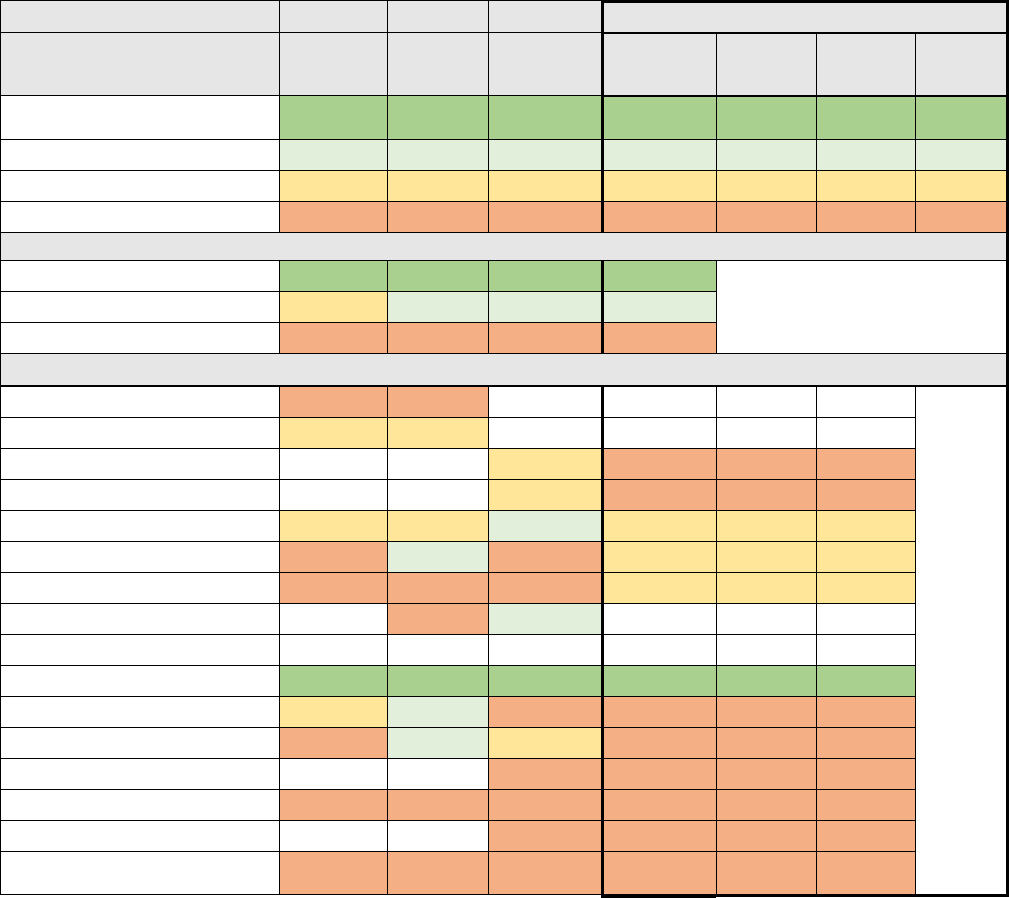
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 41
Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment
The Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (IET)
measure is the percentage of adolescent and adult members with a new episode of alcohol or other
drug (AOD) dependence who received the following:
1. Initiation of AOD Treatment: The percentage of members who initiate treatment through an
inpatient AOD admission, outpatient visit, intensive outpatient encounter or partial
hospitalization, telehealth or medication treatment within 14 days of the diagnosis.
2. Engagement of AOD Treatment: The percentage of members who initiated treatment and who
had two or more additional AOD services or medication treatment within 34 days of the initiation
visit.
Table 18. Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment for
Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number of
Plans
Plans at 90th Percentile and
Above
28 +
30 +
31 +
32 +
36%
477,683
1
Plans at 50th to 90th Percentile
21 to 28
21 to 30
23 to 31
24 to 32
0%
-
0
Plans at 25th to 50th Percentile
18 to 21
18 to 21
19 to 23
19 to 24
36%
490,372
3
Plans Below 25th Percentile
Below 18
Below 18
Below 19
Below 19
28%
377,175
8
Covered California High/Average/Low Performers
Covered CA Highest Performer
33
33
33
34
Covered CA Weighted Average
21
23
26
25
Covered CA Lowest Performer
12
6
12
16
Covered California Plan-Specific Performance
Anthem HMO
17
18
Anthem PPO
19
20
Anthem EPO
20
18
5%
64,031
Blue Shield HMO
21
18
7%
93,322
Blue Shield PPO
19
19
29
23
25%
335,176
CCHP HMO
14
21
17
22
1%
10,013
Health Net HMO
12
14
14
20
11%
145,183
Health Net EPO
12
23
Health Net PPO
Kaiser Permanente HMO
33
33
33
34
36%
477,683
LA Care HMO
20
24
12
19
6%
84,750
Molina Healthcare HMO
13
24
21
17
4%
56,023
Oscar Health Plan EPO
18
18
3%
35,962
Sharp Health Plan HMO
12
17
18
17
1%
17,335
Valley Health Plan HMO
19
18
1%
16,366
Western Health Advantage
HMO
14
6
15
16
1%
9,386

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 4
COVERED CALIFORNIA 42
Section 3. Implications for the Future
Covered California included reporting requirements related to mental health and substance use
disorder treatment services because of the significant unmet needs of enrollees and the increasing
evidence that integrating primary care and behavioral health services improves health outcomes and
delivers a return on investment by reducing downstream health care costs. Several models including
collaborative care, co-location and telehealth have demonstrated success.
29
While insurers report a wide array of approaches to promoting the availability of behavioral health
services and the integration of behavioral health services with primary care, it is difficult to measure if
these efforts are translating to better behavioral health care or outcomes for consumers. Covered
California is determining how to promote better measurement and accountability in this area which may
involve standardized definitions and use of best practices to support tracking and trending of available
services and adoption of behavioral health integration.
For measures of behavioral health quality, the main observation from the reporting over the past four
years is that there is wide variation among the plans and while some scores reflect high percentile
ranking, for many measures there are multiple health plans that are performing poorly compared to
national benchmark data. For the priority adult behavioral health measures, there is wide variation in
performance among the health plans over the past four years with most plans performing poorly. For
two of three priority measures in 2019 (Antidepressant Medication Management and Initiation and
Engagement of Alcohol and Other Drug Abuse or Dependence Treatment), six or more plans
performed below the 25
th
percentile. For each of the three measures, only one plan performed at or
above the 90
th
percentile nationally. This is concerning and warrants further concerted efforts from both
Covered California and its contracted health plans to address. Covered California is engaging with
health plans on adopting best practices for behavioral health care and developing strategies to improve
their performance on these behavioral health measures.
Covered California is also seeking to improve behavioral health measurement. The current HEDIS
behavioral health measures in the QRS measure set should be replaced or updated. None assess
behavioral health status or outcomes making performance assessment of health insurance companies
and the delivery system difficult. Covered California is exploring how best to use patient-reported
outcome measures for behavioral health. One promising measure is the use of the Patient Health
Questionnaire-9 (PHQ-9) because it can be used to both identify patients with depression symptoms
and monitor their outcomes over time. However, slow progress has been made in California because
this measure relies on collecting clinical data.
There is significant opportunity for collaboration on spreading integrated behavioral health models and
collecting clinical data through statewide collaboratives including the Integrated Healthcare Association
and California Quality Collaborative.
29
The most current best evidence is documented in Chapter 3, Mental Health and Substance Use Disorder Treatment, of a companion
Covered California report, Current Best Evidence and Performance Measures for Improving Quality of Care and Delivery System Reform.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 43
Chapter 5: Acute, Chronic and Other
Conditions
Acute, Chronic and Other Conditions entails
health insurance companies actively managing
care for enrollees with acute conditions, which is
defined as an illness or disease that is short-term
and lasts typically a few days to weeks (such as
an infection, an injury or the misuse of
medications), chronic conditions, which typically
develop slowly over time and last months to years
(such as diabetes, most cancers, cardiovascular
disease, and infectious diseases like Human
Immunodeficiency Virus) and other conditions
that are temporary, such as pregnancy or
gestational diabetes.
In addition, this chapter, Acute, Chronic and
Other Conditions, encompasses subpopulations
covered in subject chapters of this report:
Chapter 4: Mental Health and Substance Use
Disorder Treatment; Chapter 6: Complex Care;
Chapter 7: Promotion of Effective Primary Care;
and Chapter 10: Appropriate Interventions.
This chapter on Acute, Chronic, and Other
Conditions is organized as follows:
Section 1. Health Plan Measures Reported to the
Marketplace Quality Rating System
Section 2. Implications for the Future
Section 1. Health Plan Measures
Reported to the Marketplace Quality
Rating System
As described in previous chapters, one key mechanism used by Covered California for health
insurance company oversight and accountability is public reporting of global and individual health plan
quality performance measures to the Centers for Medicaid and Medicare Services’ Marketplace Quality
Rating System (QRS). To more sharply focus health plan accountability efforts, Covered California
examined over 40 measures used by QRS and is proposing to prioritize a subset of 13 measures.
The following tables display the priority measures for Acute, Chronic and Other Condition measures in
the QRS measure set (with 11 additional measures detailed in Appendix 2: Additional Health Plan
Measures Reported to the Quality Rating System) and include the Covered California weighted
average, highest and lowest performing plans, plan-specific performance, as well as national
percentiles for all Marketplace plans:
1. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%) (Table 19)
• For the measures related to care for
chronic conditions, there is wide variation
among plans, with Kaiser Permanente and
Sharp Health Plan being among the 90
th
percentile nationally, while other plans
have a range of scores. The ability of
these integrated delivery systems to
achieve such positive results is a clear
indicator of what is possible with well-
coordinated and integrated care. Covered
California is assessing what factors
contribute to better performance among
non-integrated systems and how this
performance can be replicated across
California.
• Enrollee satisfaction with their health plan
and care is comparable to nationwide
results for most Covered California plans.
However, compared to the nation,
enrollees report less favorably about their
access to care and how well their care is
coordinated. For these two priority CAHPS
Measures, Access to Care and Care
Coordination, most plans’ scores cluster
around the national 50
th
percentile or
below the 25
th
percentile. CAHPS results
for marketplace plans nationwide are
highly compressed with only a few points
difference among percentile and all results
are relatively high compared to other
measures.
Highlights

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 44
2. Controlling High Blood Pressure (Table 20)
3. Plan All-Cause Readmissions (Table 21)
4. Access to Care (Table 22)
5. Care Coordination (Table 23)
See Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System, for the 11
additional QRS measures that pertain to Acute, Chronic and Other Conditions:
6. Proportion of Days Covered (RAS Antagonists) (Table A10)
7. Proportion of Days Covered (Statins) (Table A11)
8. Proportion of Day Covered (Diabetes All Class) (Table A12)
9. Comprehensive Diabetes Care: Eye Exam (Retinal) Performed (Table A13)
10. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Testing (Table A14)
11. Comprehensive Diabetes Care: Medical Attention for Nephropathy (Table A15)
12. Medication Management for People with Asthma (75% of Treatment Period) (Table A16)
13. Prenatal and Postpartum Care (Postpartum Care) (Table A17)
14. Prenatal and Postpartum Care (Timeliness of Prenatal Care) (Table A18)
15. Well-Child Visits in the First 15 Months of Life (6 or More Visits) (Table A19)
16. Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life (Table A20)
Appendix 2 also describes how to interpret the display of the measures.
For the measures related to care for chronic conditions, there is wide variation among plans, with
Kaiser Permanente and Sharp Health Plan being among the 90
th
percentile nationally, while other plans
have a range of scores. The ability of these integrated delivery systems to achieve such positive results
is a clear indicator of what is possible with well-coordinated and integrated care. Covered California is
assessing what factors contribute to better performance among non-integrated systems and how this
performance can be replicated across California.
The wide variation in performance is particularly meaningful for measures related to managing diabetes
and hypertension that target the opportunities to improve the morbidity and mortality attributable to
these conditions. Better performance on these indicators means there would be fewer adverse events
and more lives saved. A 1 percent reduction in HbA1c reduces diabetes-related deaths by 21 percent
and myocardial infarctions (heart attacks) by 14 percent.
30
For every 10 percent reduction in
HbA1c (e.g., 10 to 9 or 9 to 8) the risk of progression to blindness fell 44 percent, progression to kidney
failure fell 25 percent, and loss of sensation in the feet by 30 percent.
31
Another study estimated the
effect of having all health plans nationally achieve the 90
th
percentile on measures focused on diabetes
and cardiovascular disease found it would result in 2.3 million fewer heart attacks (a reduction of 22
percent), 800,000 fewer strokes (a reduction of 12 percent) as well as reduced incidence of several
30
Stratton, I. M., Adler, A. I., Neil, H. A., Matthews, D. R., Manley, S. E., Cull, C. A., … Holman, R. R. (2000). Association of glycaemia with
macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ (Clinical research
ed.), 321(7258), 405–412. doi:10.1136/bmj.321.7258.405
31
Nathan, D. M., Bayless, M., Cleary, P., Genuth, S., Gubitosi-Klug, R., Lachin, J. M., … DCCT/EDIC Research Group (2013). Diabetes
control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: advances and
contributions. Diabetes, 62(12), 3976–3986. doi:10.2337/db13-1093

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 45
other less common complications over a ten year period.
32
The researchers estimated approximately
4.9 million years of life would have been saved during this same period.
Covered California health insurers generally have worse scores than the rest of the nation on the
Access to Care and Care Coordination measures, with the majority of insurers below the 25
th
percentile
and none above the 50
th
. It is important to note that the CAHPS results for marketplace plans
nationwide are highly compressed with only a few points difference among each percentile and all
results are relatively high compared to other measures. Also, California’s demographic diversity
includes greater numbers of people in race/ethnicity groups who tend to give plans lower scores. This
suggests insurers may not meet the needs of all groups equally. Covered California sees these
enrollee-experience scores as reason for both concern and future research. Covered California is
working with its health insurance companies to assure improvement in these areas and is seeking to
expand the number and sources of measures that can best assess consumers’ experience in access to
care, care coordination and other important quality domains.
32
Note these estimates are from a 2008 study based on the Archimedes simulation model. At the time, impacts were modeled for the U.S.
population of 210 million adults ages 18-85 over a ten-year period, 1995-2005: Eddy, D. M., Pawlson, L. G., Schaaf, D.
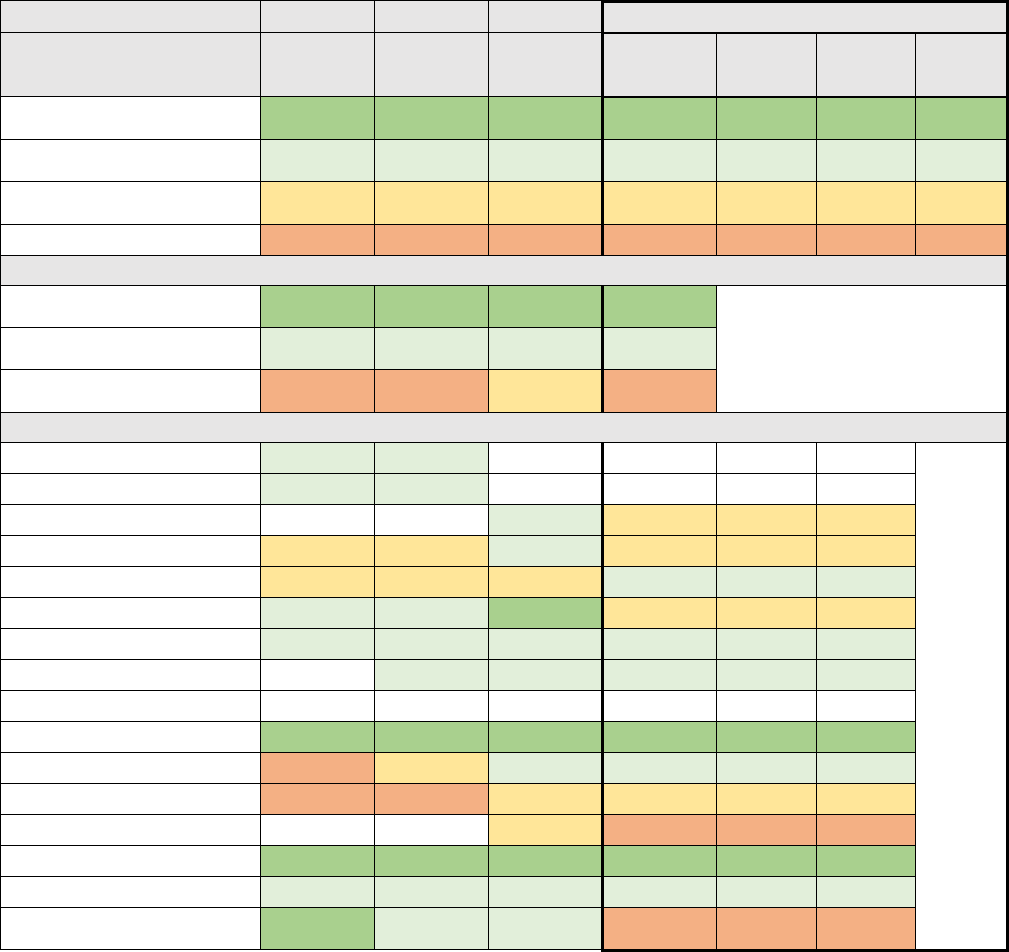
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 46
Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%)
The Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control measure is the percentage of
members 18–75 years of age with diabetes (type 1 and type 2) whose most recent HbA1c level was
less than 8 percent.
Table 19. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%) for Covered California
Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
67 +
67 +
69 +
68 +
37%
495,018
2
Plans at 50th to 90th
Percentile
56 to 67
58 to 67
59 to 69
58 to 68
43%
582,871
5
Plans at 25th to 50th
Percentile
46 to 56
48 to 58
50 to 59
52 to 58
17%
223,389
4
Plans Below 25th Percentile
Below 46
Below 48
Below 50
Below 52
3%
45,348
2
Covered California High/Average/Low Performers
Covered CA Highest
Performer
75
70
73
72
Covered CA Weighted
Average
58
60
63
64
Covered CA Lowest
Performer
38
47
52
49
Covered California Plan-Specific Performance
Anthem HMO
61
60
Anthem PPO
56
61
Anthem EPO
62
57
5%
64,031
Blue Shield HMO
47
48
59
56
7%
93,322
Blue Shield PPO
53
55
56
64
25%
335,176
CCHP HMO
65
60
73
57
1%
10,013
Health Net HMO
63
58
65
58
11%
145,183
Health Net EPO
62
68
63
0%
1,396
Health Net PPO
Kaiser Permanente HMO
68
70
71
70
35%
477,683
LA Care HMO
39
54
62
62
6%
84,750
Molina Healthcare HMO
38
47
52
58
4%
56,023
Oscar Health Plan EPO
57
50
3%
35,962
Sharp Health Plan HMO
75
70
71
72
1%
17,335
Valley Health Plan HMO
60
58
59
60
1%
16,366
Western Health Advantage
HMO
69
61
64
49
1%
9,386
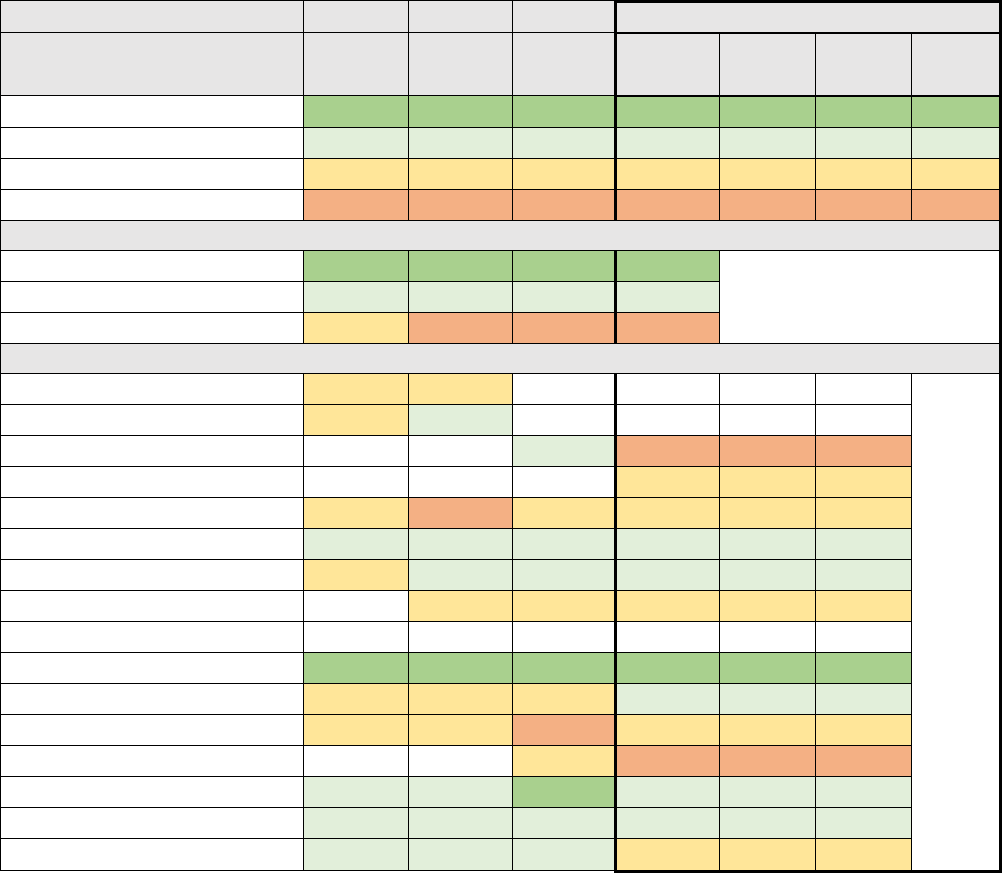
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 47
Controlling High Blood Pressure
The Controlling High Blood Pressure measure is the percentage of members 18–85 years of age who
had a diagnosis of hypertension and whose blood pressure was adequately controlled.
Table 20. Controlling High Blood Pressure for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and Above
76 +
76 +
77 +
75 +
35%
477,683
1
Plans at 50th to 90th Percentile
58 to 76
59 to 76
61 to 77
62 to 75
20%
273,647
5
Plans at 25th to 50th Percentile
49 to 58
47 to 59
49 to 61
54 to 62
37%
495,303
5
Plans Below 25th Percentile
Below 49
Below 47
Below 49
Below 54
7%
99,993
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
85
86
82
81
Covered CA Weighted Average
63
63
66
66
Covered CA Lowest Performer
49
43
43
44
Covered California Plan-Specific Performance
Anthem HMO
51
56
Anthem PPO
55
61
Anthem EPO
62
45
5%
64,031
Blue Shield HMO
61
7%
93,322
Blue Shield PPO
57
43
52
56
25%
335,176
CCHP HMO
72
73
62
68
1%
10,013
Health Net HMO
57
61
63
63
11%
145,183
Health Net EPO
49
54
59
0%
1,396
Health Net PPO
Kaiser Permanente HMO
85
86
82
81
35%
477,683
LA Care HMO
50
59
56
68
6%
84,750
Molina Healthcare HMO
49
51
43
58
4%
56,023
Oscar Health Plan EPO
54
44
3%
35,962
Sharp Health Plan HMO
75
72
81
74
1%
17,335
Valley Health Plan HMO
59
64
68
64
1%
16,366
Western Health Advantage HMO
61
64
66
58
1%
9,386
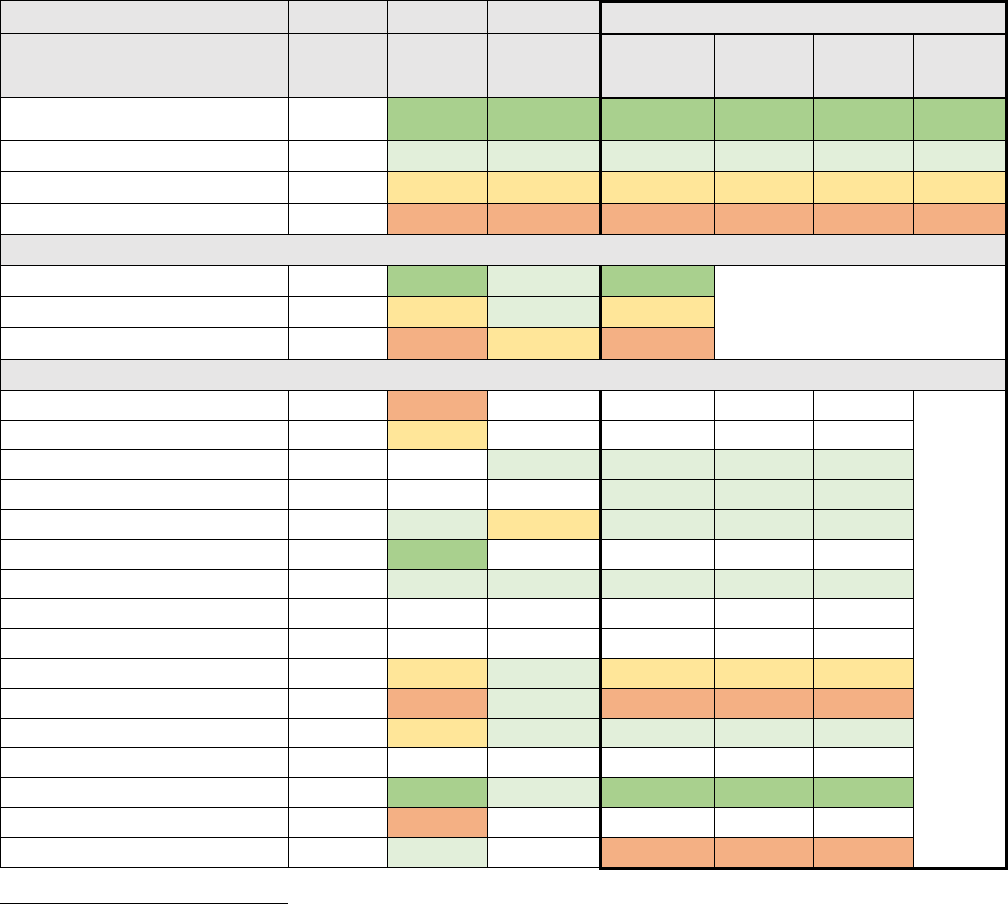
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 48
Plan All-Cause Readmissions
The Plan All-Cause Readmissions measure is a ratio that compares the number of acute inpatient
stays for members 18–64 years of age that were followed by an unplanned acute readmission for any
diagnosis within 30 days to the predicted number of acute readmissions.
33
This measure compares the
actual readmission rate of a health plan to the expected admission rate. If the actual readmission rate is
lower than the expected readmission rate, the plan is performing better at reducing readmissions than
expected and the plan would have a measure value less than 100. A plan can have a measure value
above 100 if their observed rate was greater than their expected rate meaning their performance was
worse than expected. A lower rate indicates better performance.
Table 21. Plan All-Cause Readmissions for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number of
Plans
Plans at 90th Percentile and
Above
M-NS
<= 58
<= 53
<= 52
1%
17,335
1
Plans at 50th to 90th Percentile
M-NS
78 to 58
76 to 53
71 to 52
54%
693,735
5
Plans at 25th to 50th Percentile
M-NS
88 to 78
86 to 76
77 to 71
37%
477,683
1
Plans Below 25th Percentile
M-NS
Above 88
Above 86
Above 77
7%
94,136
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
59
17
66
52
Covered CA Weighted Average
86
80
74
71
Covered CA Lowest Performer
163
119
86
95
Covered California Plan-Specific Performance
Anthem HMO
95
91
Anthem PPO
82
80
Anthem EPO
74
71
5%
64,031
Blue Shield HMO
68
7%
93,322
Blue Shield PPO
94
76
86
70
26%
335,176
CCHP HMO
163
17
Health Net HMO
74
77
71
71
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
88
84
68
73
37%
477,683
LA Care HMO
59
119
72
80
7%
84,750
Molina Healthcare HMO
65
82
66
55
4%
56,023
Oscar Health Plan EPO
Sharp Health Plan HMO
75
56
67
52
1%
17,335
Valley Health Plan HMO
115
Western Health Advantage HMO
103
76
95
1%
9,386
33
The observed to expected readmission rates are multiplied by 100 to convert to whole numbers.
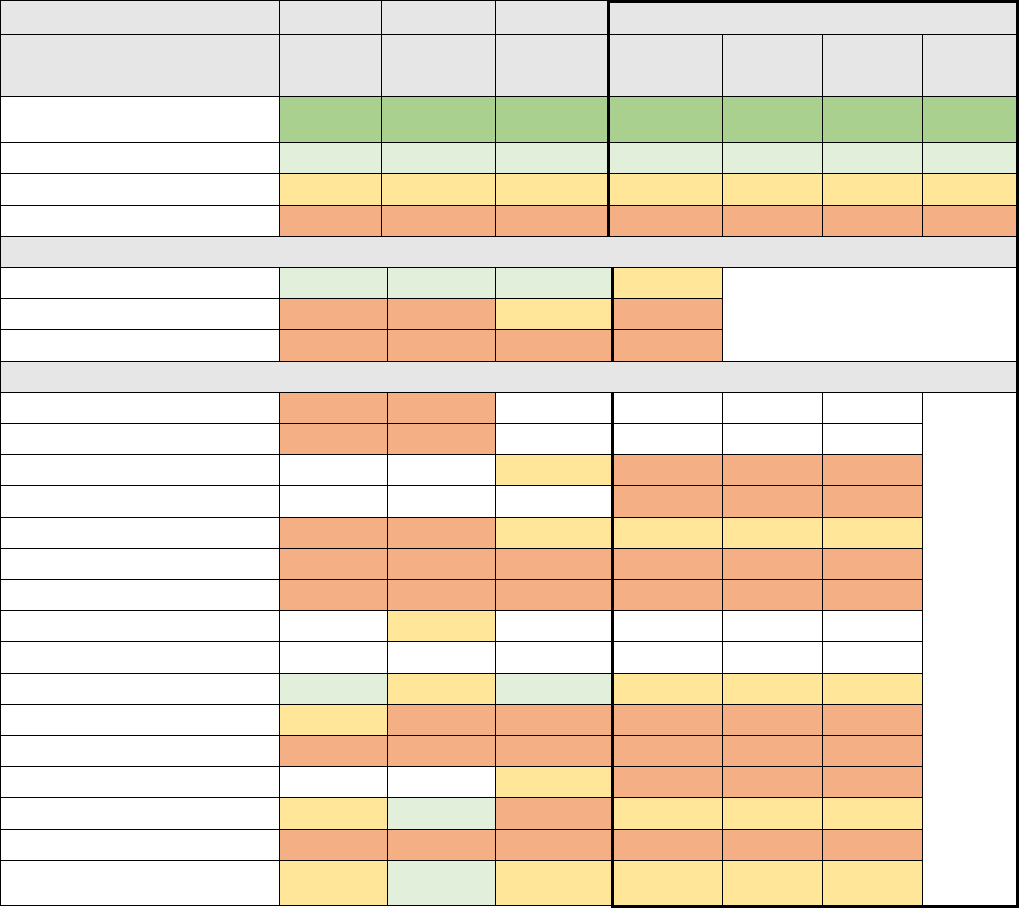
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 49
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
Access to Care
The Access to Care measure is based on four 2019 QHP Enrollee Survey questions about enrollee’s
experience of receiving care:
1. In the last 6 months, when you needed care right away, in an emergency room, doctor’s office, or
clinic, how often did you get care as soon as you needed?
2. In the last 6 months, how often did you get an appointment for a check-up or routine care at a
doctor’s office or clinic as soon as you needed?
3. In the last 6 months, how often was it easy to get the care, tests, or treatment you needed?
4. In the last 6 months, how often did you get an appointment to see a specialist as soon as you
needed?
Table 22. Access to Care for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number of
Plans
Plans at 90th Percentile and
Above
81 +
82 +
84 +
80 +
0%
-
0
Plans at 50th to 90th Percentile
76 to 81
77 to 82
80 to 84
75 to 80
0%
-
0
Plans at 25th to 50th Percentile
72 to 76
74 to 77
77 to 80
72 to 75
62%
839,580
4
Plans Below 25th Percentile
Below 72
Below 74
Below 77
Below 72
38%
505,650
8
Covered California High/Average/Low Performers
Covered CA Highest Performer
78
79
81
75
Covered CA Weighted Average
70
71
77
72
Covered CA Lowest Performer
56
60
67
57
Covered California Plan-Specific Performance
Anthem HMO
62
61
Anthem PPO
66
72
Anthem EPO
77
69
5%
64,031
Blue Shield HMO
71
7%
93,322
Blue Shield PPO
70
71
79
73
25%
335,176
CCHP HMO
62
65
67
67
1%
10,013
Health Net HMO
65
65
69
66
11%
145,183
Health Net EPO
74
Health Net PPO
Kaiser Permanente HMO
78
77
81
75
36%
477,683
LA Care HMO
73
72
67
67
6%
84,750
Molina Healthcare HMO
59
60
69
68
4%
56,023
Oscar Health Plan EPO
77
71
3%
35,962
Sharp Health Plan HMO
76
79
74
73
1%
17,335
Valley Health Plan HMO
56
65
70
57
1%
16,366
Western Health Advantage
HMO
74
79
79
73
1%
9,386
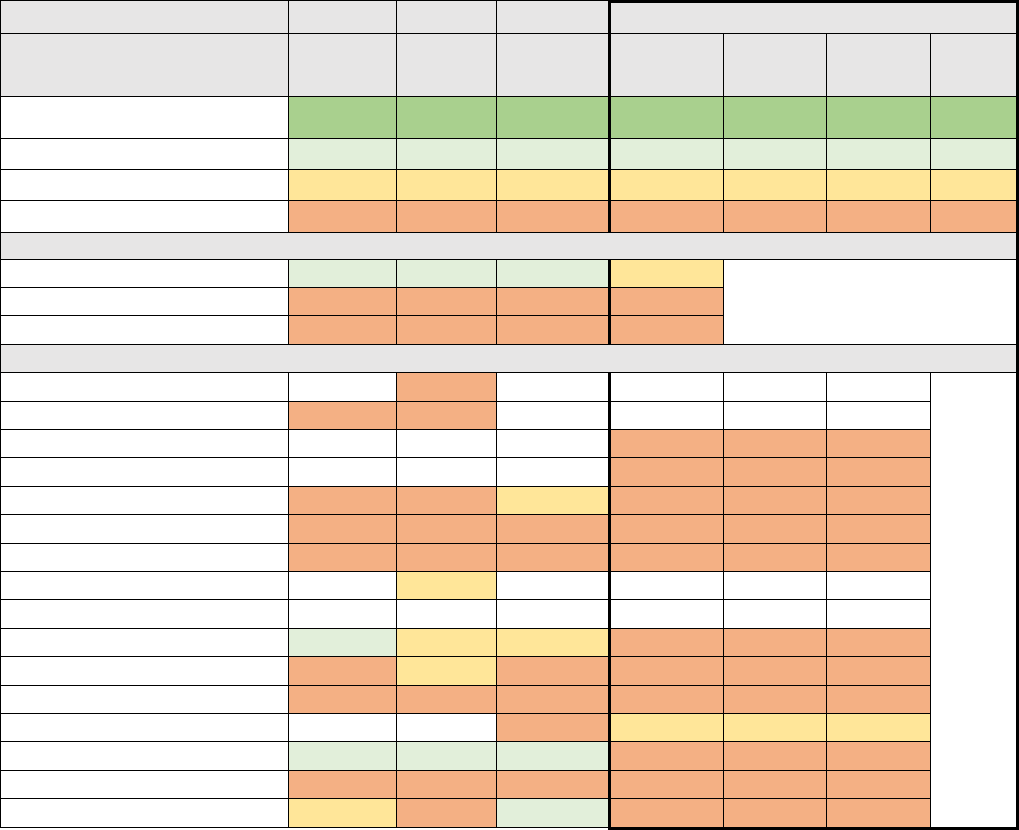
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 50
Care Coordination
The Care Coordination measure is based on six 2019 QHP Enrollee Survey questions about enrollee’s
experience of receiving care:
1. When you visited your personal doctor for a scheduled appointment in the last 6 months, how often
did he or she have your medical records or other information about your care?
2. In the last 6 months, when your personal doctor ordered a blood test, x-ray, or other test for you,
how often did someone from your personal doctor’s office follow up to give you those results?
3. In the last 6 months, when your personal doctor ordered a blood test, x-ray, or other test for you,
how often did you get those results as soon as you needed them?
4. In the last 6 months, how often did your personal doctor seem informed and up-to-date about the
care you got from specialists?
5. In the last 6 months, how often did you and your personal doctor talk about all the prescription
medicines you were taking?
6. In the last 6 months, did you get the help that you needed from your personal doctor’s office to
manage your care among these different providers and services?
Table 23. Care Coordination for Covered California Enrollees
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
88 +
89 +
88 +
87 +
0%
-
0
Plans at 50th to 90th Percentile
84 to 88
85 to 89
85 to 88
83 to 87
0%
-
0
Plans at 25th to 50th Percentile
82 to 84
82 to 85
83 to 85
81 to 83
3%
35,962
1
Plans Below 25th Percentile
Below 82
Below 82
Below 83
Below 81
97%
1,309,268
11
Covered California High/Average/Low Performers
Covered CA Highest Performer
85
88
86
83
Covered CA Weighted Average
81
81
83
79
Covered CA Lowest Performer
74
76
74
73
Covered California Plan-Specific Performance
Anthem HMO
76
Anthem PPO
81
81
Anthem EPO
79
5%
64,031
Blue Shield HMO
81
7%
93,322
Blue Shield PPO
81
82
84
81
25%
335,176
CCHP HMO
76
77
77
80
1%
10,013
Health Net HMO
76
78
79
76
11%
145,183
Health Net EPO
84
Health Net PPO
Kaiser Permanente HMO
85
83
85
80
36%
477,683
LA Care HMO
81
83
78
77
6%
84,750
Molina Healthcare HMO
74
77
74
78
4%
56,023
Oscar Health Plan EPO
80
83
3%
35,962
Sharp Health Plan HMO
84
88
85
79
1%
17,335
Valley Health Plan HMO
79
79
79
73
1%
16,366
Western Health Advantage HMO
84
81
86
81
1%
9,386
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 5
COVERED CALIFORNIA 51
Section 2. Implications for the Future
For these health plan measures for addressing chronic illnesses, the main observation from the
reporting over the past four years is that there is wide variation among the plans. Kaiser Permanente
and Sharp Health Plan frequently report providing services or getting results that are in the top 90
th
percentile in the nation, while other plans have lower scores – ranging from the 25
th
to just above the
50
th
percentile. The wide variation in performance is particularly meaningful for measures related to
managing diabetes and hypertension that do a remarkable job of targeting the opportunities to improve
the morbidity and mortality attributable to those conditions. Improvement in performance across all
California plans would be potentially life-saving and clinically meaningful for hundreds of thousands of
Californians.
The ability of integrated delivery systems to achieve such positive results is a clear indicator of what is
possible with well-coordinated and integrated care. Covered California is assessing what factors
contribute to better performance among non-integrated systems and how this performance can be
replicated across California.
Covered California identified four priority CAHPS measures. For two of these measures — overall
satisfaction with care and with their health plan — most Covered California health plans perform above
the 50
th
percentile compared to national marketplace plans (see Chapter 2: Individualized, Equitable
Care). It is concerning that 8 health plans score below the 25
th
percentile on members' Access to Care
and that 11 health plans score below the 25
th
percentile for Care Coordination. It is important to note
that the CAHPS results for marketplace plans nationwide are highly compressed with only a few points
difference among each percentile and all results are relatively high compared to other measures.
Covered California sees these enrollee-experience scores as reason for both concern and future
research and is working with its health insurance companies to assure improvement in these areas.
Covered California is also seeking to expand the number and sources of measures that can best
assess consumers’ experience in access to care, care coordination and other important quality
domains.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 52
Chapter 6: Complex Care
Complex Care involves effectively managing very
complex conditions for individuals that require a
multitude of specialty, high-cost treatments – such
as rare cancers or transplants – or require end of life
care. These individuals need to be managed
effectively, provided well-coordinated care, or be
seen in very specialized settings.
This chapter on Complex Care presents
performance data reported by health insurance
companies for contract requirements and includes
assessments and observations by Covered
California. This chapter is organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Implications for the Future
Section 1: Qualified Health Plan
Experience
Qualified Health Plan Experience presents
performance data reported by health insurance
companies for contract requirements and includes
assessments and observations by Covered
California. The current contract requirements for
Complex Care largely focus on health plan
processes for effectively managing at-risk enrollees
with complex conditions, defined as: “clinical
conditions that are of a complex nature that typically
involve ongoing case management support from
appropriately trained clinical staff. Frequently,
individuals have multiple chronic clinical conditions
that complicate management (“polychronic”) or may
have a complex, infrequent specialty condition that
requires specialized expertise for optimal
management.”
34
It has been shown that when high-risk enrollees are
identified early, they are most likely to benefit from
34
See Glossary of Key Terms for Attachment 7 to Covered California 2017 Qualified Health Plan Contract: Quality, Network Management,
and Delivery System Standards, and Improvement Strategy: https://hbex.coveredca.com/insurance-companies/PDFs/Attachment-7-
Amended-for-2019.pdf.
• All insurers leverage medical and
pharmacy claims as well as
demographic information to identify
high-cost or high-risk patients for
various care and case management
support, but there is no consistent
measurement of the efficacy of their
efforts, primarily due to the lack of
standard population identification or
quality measures for complex care.
• All insurers contracted with Centers of
Excellence (COE), with the most
common treatments being cancer care
and bariatric surgery. Identification and
performance measurement for COEs is
not standardized.
• Only one insurer had a formal steerage
program for transplants while most
insurers promote their COEs by relying
on member interactions with the
service center or care management
team.
• Most health plans offered Health Risk
Assessments (HRAs) to determine
enrollee health status on a voluntary
basis, but completion rates are very
low.
• A large-scale effort to support at-risk
enrollees in effective coverage
transitions coordinated by Covered
California and insurers occurred when
Anthem exited multiple rating regions
in 2018, affecting nearly 137,000
consumers.
Highlights
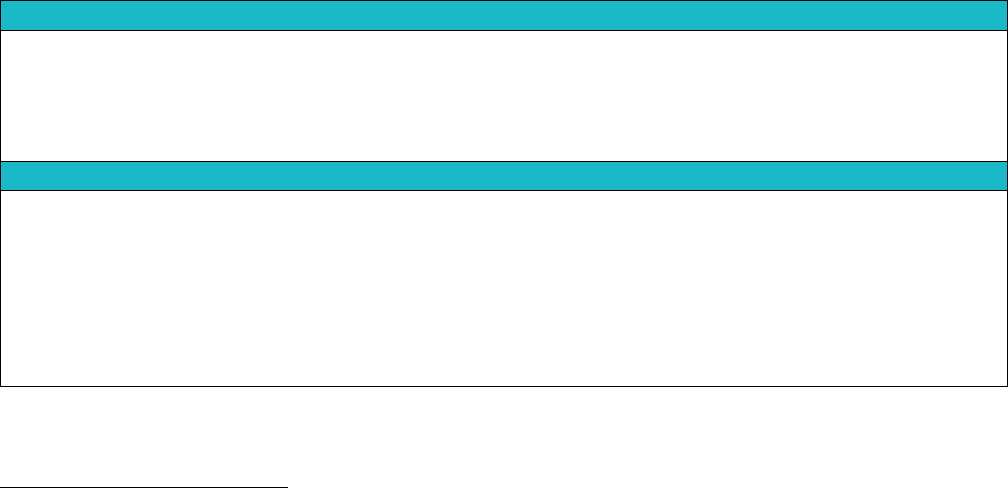
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 53
well-coordinated care. As such, Covered California has the following requirements for health plans to
address complex care:
1. Coordinating treatment for enrollees with conditions that required high specialized management,
such as transplant patients, and the use of Centers of Excellence (COEs) for these enrollees;
2. Collecting information to monitor enrollee health status;
3. Tracking changes in health status and the use of health risk assessments;
4. Supporting at-risk enrollees requiring transition; and
5. Identification and services for at-risk enrollees.
Centers of Excellence
Health insurance companies are required to report on how enrollees with conditions that require highly
specialized management, like transplant patients and burn patients, are managed by providers with
documented special experience and proficiency based on volume and outcome data, such as Centers
of Excellence (COEs). Centers of Excellence allow for complex care patients to be seen in very
specialized settings, such as National Cancer Institute designated cancer centers.
Although there are no standards for identifying COEs, described below are common themes discussed
by insurers about the process for use and promotion of COEs to enrollees with specialized conditions,
as well as the strategy for including COEs in each insurer’s network (see Table 24. Covered California
Insurer Processes and Strategies for Use of Centers of Excellence, 2015, 2017 and 2018). All insurers
contract with COEs but only one insurer has a formal steerage program to direct enrollees to COEs for
transplants. Most health insurance companies promote COEs through enrollee interactions with their
service centers or care management teams. Other insurers simply note that COEs are available in their
Evidence of Coverage documents.
Table 24. Covered California Insurer Processes and Strategies for Use of Centers of Excellence, 2015,
2017 and 2018
35
Process: Promotion of Centers of Excellence
• Steered all members to transplant COEs and encouraged use of COEs for other conditions
• Member services or concierge teams assisted members in locating designated facilities and managing
benefit requirements and limitations
• Care managers and medical directors drove appropriate use of these facilities
• Did not actively promote or steer members; identified COEs in coverage documents
Strategy: Basis for Inclusion in Network
• Must meet or exceed a specific level of volume and outcomes while demonstrating adherence to industry
standards; inclusion in network reviewed yearly
• Only contracted with COEs when a specific highly-specialized method of care was not available in-network;
established single case referrals with COEs for specific procedures
• Stringent selection criteria for choosing COEs; only included in provider directory if contracted for long-term
versus one-time arrangements
• Used COEs for transplants approved by the Department of Health Care Services (DHCS)
• No formal COEs, but network included specific hospitals for tertiary and transplant cases
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
35
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.
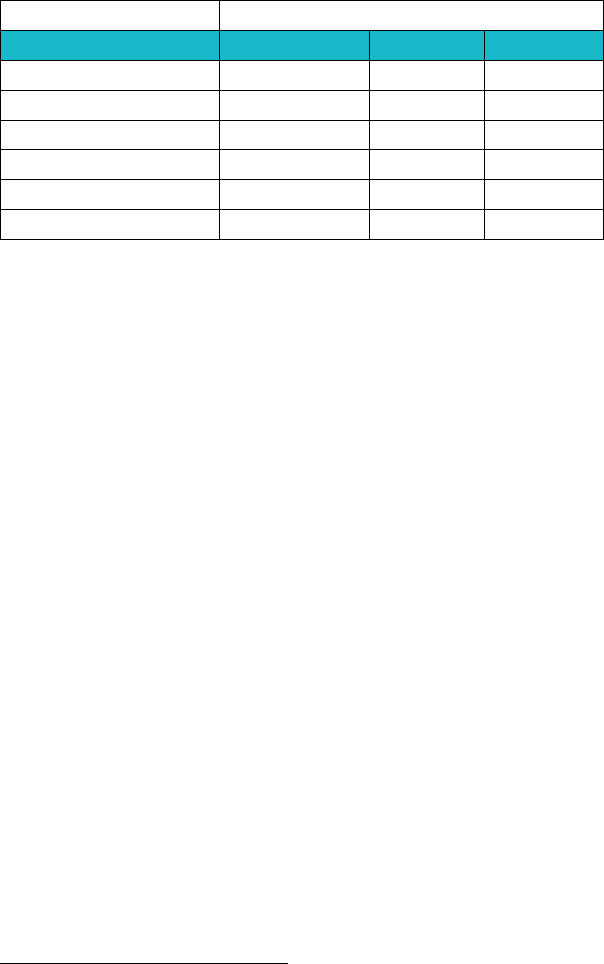
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 54
All 11 health insurance companies provided enrollees’ access to at least two types of Centers of
Excellence in 2018. Nine insurers provided access to at least one type of COE specializing in
transplants, eight health plans offered a COE for cancer care, seven health plans offered a COE for
bariatric surgery, and six plans offered a COE for burn care (see Table 25. Covered California
Enrollees’ Access to Centers of Excellence for Specialized Conditions, 2015, 2017 and 2018). A lower
number of health plans offered COEs for cardiac care and orthopedics (such as hip and knee surgery).
Table 25. Covered California Enrollees’ Access to Centers of Excellence for Specialized Conditions, 2015,
2017 and 2018
36
Number of Health Plans
2015
2017
2018
Cancer
9
9
8
Transplants
11
11
9
Cardiac Care
3
3
4
Bariatric Surgery
3
3
7
Orthopedics
2
2
5
Burn Care
7
7
6
Note: Covered California did not specifically ask if health plans contract with COEs for cardiac care or orthopedics. Additional health plans
may contract with COEs for these conditions.
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Collecting Information to Monitor Enrollee Health Status
Health insurance companies are required to describe how they collect and report, at both the individual
and aggregate levels, changes in enrollee health status. For example, reporting by insurers may
include a comparative analysis of health status improvements across geographic regions and
demographic groups. Health insurance companies are required to describe their process to monitor and
track health status, which may include identifying individuals who show a decline in health status, and
referral of such enrollees to care management programs.
In 2018, eight insurers described a system for collecting data on enrollee health status (either a clinical
system for determining health status or the use of a survey). All insurers leveraged medical and
pharmacy claims as well as demographic information to identify high-cost or high-risk patients for
various care and case management support. Integrated delivery systems, such as Kaiser Permanente
and Sharp Health Plan, leveraged access to more clinical data, such as lab results.
Health risk assessments (HRAs) can be used in concert with clinical data for predictive modeling for
early intervention. HRAs are an important tool that can accurately stratify individuals with the highest
risk because they capture both physical and behavioral health needs as well as social needs.
36
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.
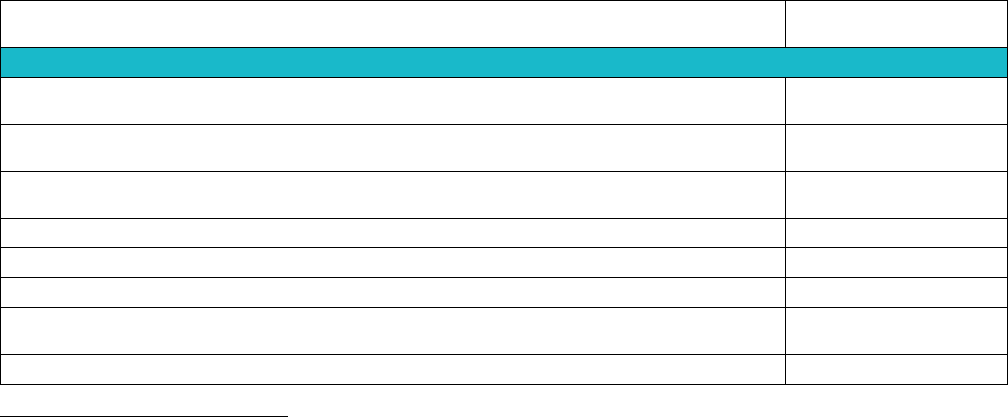
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 55
Determining Enrollee Health Status and Use of Health Risk Assessments
Health insurance companies are required to describe their capabilities in collecting information about
enrollees’ health status and behaviors for health promotion and improved care management. If the
insurer used health risk assessments to determine health status, the following requirements apply:
1. The assessment must be offered in all threshold languages to enrollees over the age of 18,
including those that have previously completed such an assessment;
2. The assessment tool must adequately evaluate an enrollee’s current health status and provide a
mechanism to conduct ongoing monitoring for future intervention(s); and
3. Enrollees should be made aware at the beginning of the assessment about how information
collected may be used, that they may opt in to receive information from the insurer, and that
participation in the assessment is optional.
Most insurers offered HRAs on a voluntary basis, but completion rates reported by insurers for 2018
were very low. HRA completion rates ranged from 0 to 38 percent with 8 of the 11 insurers reporting
under 6 percent completion.
While HRA completion rates were low for the overall population, insurers had several activities and
capabilities that supported HRAs and best evidence supports targeted HRA collection for at-risk
individuals (see Table 26. Covered California Insurer Activities and Capabilities Supporting Health Risk
Assessments, 2018).
37
Most health insurance companies took multiple steps to address at-risk
behaviors reported in an HRA. Eleven insurers generated a personalized report after completion which
provided members specific actions they can take to lower their risk and directed them to a targeted
intervention module. Three insurers auto-enrolled members into a disease management program and
two allowed members the option to send assessment results to their physician. Given the lack of data,
health insurance companies reported limited ability to proactively link enrollees with smoking cessation
or weight management programs that they all offer.
Table 26. Covered California Insurer Activities and Capabilities Supporting Health Risk Assessments,
2018
Number of
Health Plans
Addressing At-Risk Behaviors
Personalized HRA report is generated after HRA completion that provides member-
specific risk modification actions based on responses
11
Members are directed to targeted interactive intervention module for behavior change
upon HRA completion
10
At point of HRA response, risk-factor education is provided to member based on
member-specific risk
6
Case manager or health coach outreach call triggered via HRA results
8
Member can update responses and track against previous responses
7
Ongoing push messaging for self-care based on member's HRA results
6
Member is automatically enrolled into a disease management or at-risk program
based on responses
3
Member can elect to have HRA results sent electronically to physician
2
37
The capabilities reported by health insurance companies only apply to the small number of enrollees they reported as successfully
completing the Health Risk Assessment.
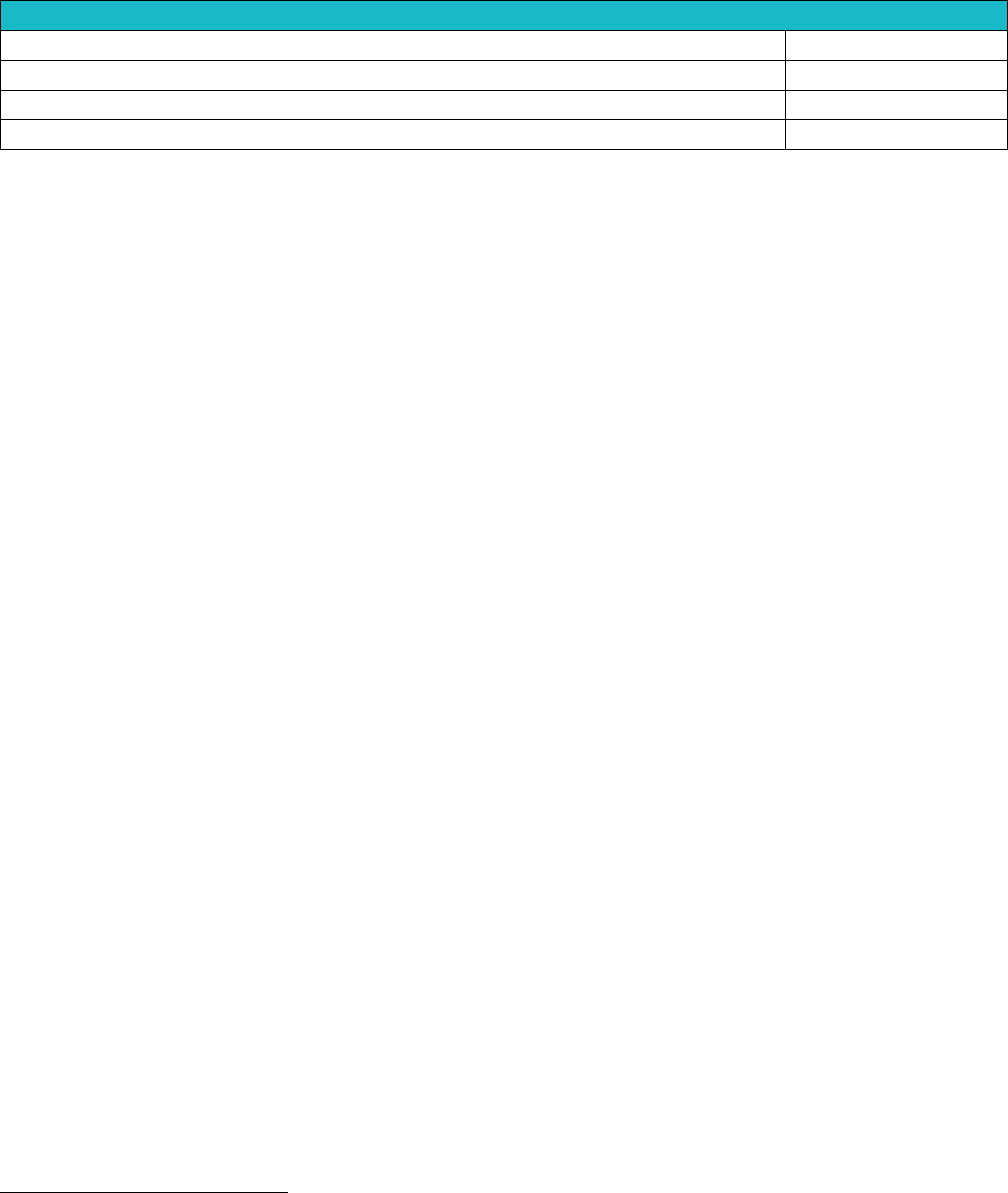
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 56
Tracking Health Status
HRA responses tracked over time to observe changes in health status
8
HRA responses incorporated into member health record
5
HRA responses used for analysis of health status across demographics
5
HRA responses used for analysis of health status across regions
2
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Supporting At-Risk Enrollees Requiring Transition
Health insurance companies must demonstrate that they are able to facilitate transitions of care with
minimal disruption for enrollees that (1) switched from one insurer into another or (2) into or out of
coverage through Covered California. This requirement for supporting at-risk enrollees is broader than
the continuity of care requirements in state law. Covered California’s contracts with the majority of
health insurance companies in California which places it in the unique position to better facilitate
transitions of care for this population that will result in enrollees receiving the right care at the right time.
Covered California is particularly concerned about transitions for the following “at-risk” enrollees:
1. Individuals in the middle of acute treatment, third trimester pregnancy, or those who would
otherwise qualify for continuity of care under California law;
2. Individuals in case management programs;
3. Individuals in disease management programs; and
4. Individuals on maintenance prescription drugs for a chronic condition.
If enrollees experience a service area disruption, Covered California may automatically transition the
enrollee into a different health insurance company to avoid gaps in coverage and facilitate care
transitions. If this occurs, the insurer terminating the enrollee has several requirements, including
conducting outreach to the affected enrollee, obtaining authorization to send personal health
information to the receiving health insurance company, and collaborating with impacted providers.
Identification and Services for At-Risk Enrollees
Health insurance companies are required to identify and proactively manage enrollees with existing and
newly diagnosed chronic conditions, including “at-risk enrollees” with diabetes, asthma, heart disease,
or hypertension, who are most likely to benefit from well-coordinated care. Insurers must agree to
support disease management activities at the insurer or provider level that meet standards of
accrediting programs such as NCQA. Health insurance companies provide Covered California with a
documented process, care management plan and strategy for targeting and managing at-risk enrollees.
Such documentation may include (but is not limited to) methods to identify and target at-risk enrollees,
description of predictive analytic capabilities, member communication plans, care and network
strategies, and data on the number of enrollees identified as well as the types of services provided.
Most health insurance companies reported identifying at-risk enrollees with algorithms and other
proprietary technology based on claims and utilization data.
38
Some insurers described using
demographic data, HRA data, hospital discharge data, clinical data, and nurse advice line and provider
referral data.
38
No data was summarized in a table for 2018 due to specific proprietary technologies mentioned and because four out of 11 insurers
explained what data they collected but did not explain how they analyzed the data for at-risk enrollee identification.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 57
The type of services offered to at-risk enrollees varies substantially across insurers (see Table 27.
Types of Interventions for Covered California At-Risk Enrollees Eligible for Case Management, 2018).
All health insurance companies offered some level of live outbound telephonic coaching to members.
Most offered member-specific reminders for health maintenance services (10 of 11) or face-to-face
visits (six of 11). Online interactive self-management support was less common, with four of 11 plans
offering it to high-risk or all enrollees.
Supporting At-Risk Enrollees Transitioning between Covered California Insurers:
Experience Assuring Care Transitions for over 135,000 Californians in 2018
In much of the nation, there has been substantial instability in insurers serving different states’
individual market. One of the risks of insurers exiting markets is the potential for disruption of care
for those with complex health care needs. California has been marked by stability among its
insurers. The only significant disruption from an insurer changing its service areas occurred when
Anthem exited multiple rating regions in 2018, affecting nearly 137,000 consumers — about 10
percent of Covered California enrollees — while remaining in large portions of the state. Covered
California worked closely with Anthem and all other health insurers receiving transitioning enrollees
to assure effective transitions. Carrying out an effective transition of Anthem enrollees required
partnership and collaboration among Covered California staff, the health insurance companies
receiving transitioning enrollees, and Anthem. Covered California and receiving insurers began
working with Anthem staff months before the transitions in coverage to ensure appropriate and
seamless continuity and transitions of care to protect the most vulnerable populations. The goal was
to identify enrollees with specific care needs and to transfer information about enrollee’s care needs
to the receiving insurer.
This collaboration required Anthem and receiving insurers to agree to identifying an appropriate
level of data required for transitioning enrollees, parameters on data sharing and use and processes
to receive and act upon consumer information. At-risk enrollees included those undergoing case or
disease management services as well as those with pregnancy/maternity and specialty medication
needs. The data sharing resulted in receiving insurers having sufficient information to do timely
consumer outreach. This outreach was of utmost benefit to consumers who would have otherwise
navigated the health care system alone.
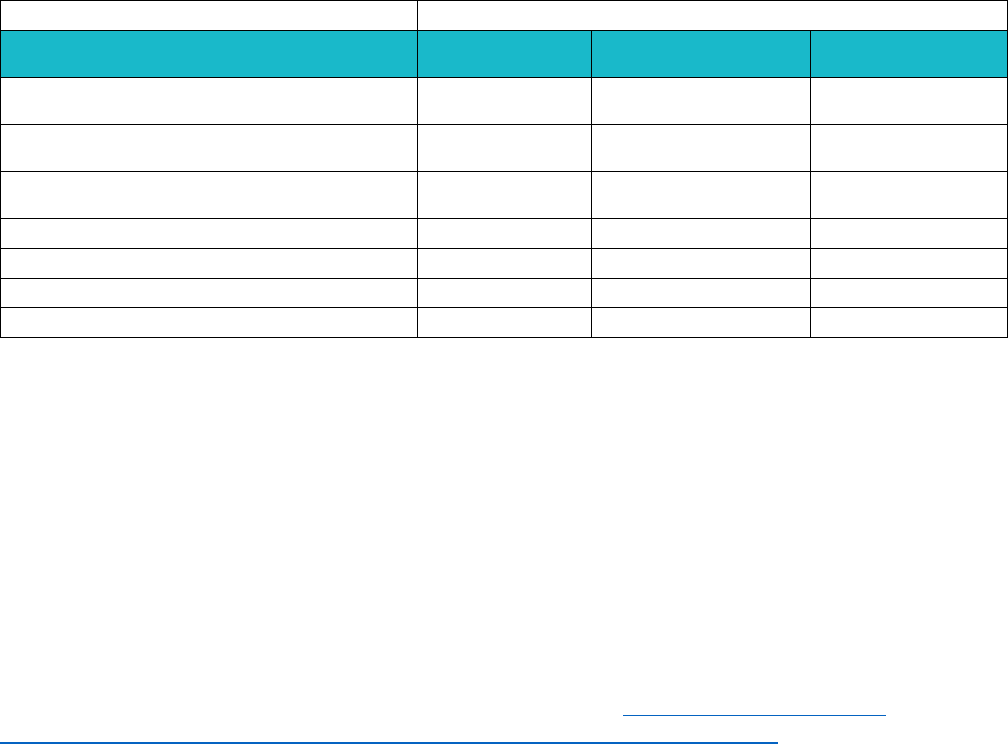
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
ASSURING QUALITY CARE • CHAPTER 6
COVERED CALIFORNIA 58
Table 27. Types of Interventions for Covered California At-Risk Enrollees Eligible for Case Management,
2018
Number of Health Plans
Type of Intervention
Not Offered
Offered in High-Risk
Program
Available for All
Enrollees
Member specific reminders for health
maintenance services
1
7*
3
Member specific reminders for medication
events
5**
5
1
Interactive voice response with outbound
messaging only
7
2*
2
Live outbound telephonic coaching program
0
7
4
Self-initiated text/email messaging
9
1
1
Online interactive self-management support
7
1
3
Face-to-face visits
5
5
1
*Includes contradictory responses from one health plan.
**Includes contradictory responses from two health plans.
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Section 2: Implications for the Future
Measurement of performance in caring for enrollees requiring complex care requires further
development. Covered California found no standard quality measures for Complex Care to include in
this chapter. The current Marketplace Quality Rating System measure set has one measure for
behavioral health subpopulations, Follow Up After Hospitalization for Mental Illness (FUH) (HEDIS),
which is presented in Chapter 4. The Plan All-Cause Readmissions measure, which is presented in
Chapter 5, may include complex care patients but does not specifically measure care management
processes or outcomes.
In a Covered California sponsored report released in July 2019, Current Best Evidence and
Performance Measures for Improving Quality Care and Delivery System Reform, Health Management
Associates (HMA) recommended a hybrid method of population stratification starting with automated
data to identify high cost enrollees combined with survey data such as HRAs, behavioral health
screening, screening for social needs or measuring patient activation to determine enrollees who are
likely to continue to be high-risk and high-cost. In the same report, PricewaterhouseCoopers (PwC)
recommended that Covered California use its claims data warehouse to track rates of inpatient and
Emergency Department use and Emergency Department follow-up among complex care patients. PwC
also recommended that Covered California consider the Transition of Care HEDIS measure which
would require collection of discharge information that includes test results.
Covered California is working with health insurance companies and other stakeholders to establish best
practices for population identification and management including a standardized approach to defining
and measuring performance of Centers of Excellence.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 59
EFFECTIVE CARE DELIVERY
Chapter 7: Promotion of Effective
Primary Care
Effective Primary Care that is accessible, well-
integrated, coordinated, continuous, team-based,
and data driven is a core foundation of providing
appropriate and equitable care. While many
consumers benefit from an ongoing continuous
relationship with a single physician, others may be
able to receive effective primary care through
sites of care or delivery systems that are well-
integrated.
This chapter on Promotion of Effective Primary
Care presents performance data for current
contract requirements reported by health
insurance companies for the 2015-18 plan years
and includes assessments and observations by
Covered California. This chapter is organized as
follows:
Section 1. Qualified Health Plan Experience
Section 2: Health Plan Measures Reported to the
Marketplace Quality Rating System
Section 3. Implications for the Future
Section 1: Qualified Health Plan
Experience
Covered California believes promoting the Triple
Aim and promoting health equity requires a
foundation of effectively delivered primary care,
which the Institute of Medicine defines as follows:
“the provision of integrated, accessible health
care services by clinicians who are accountable
for addressing a large majority of personal health
needs, developing a sustained partnership with
patients, and practicing in the context of family
and community.”
39
To this end, Covered California
promotes effective primary care with the following
requirements:
39
Institute of Medicine. 1994. Defining Primary Care: An Interim Report. Washington, DC: The National Academies Press.
https://doi.org/10.17226/9153.
• Starting in 2017, virtually all Covered
California’s enrollees either selected or
were matched with a primary care
provider — including all enrollees in PPO
model plans. Covered California is
assessing the impact of this novel effort.
• While virtually all primary care provided in
Kaiser Permanente is delivered by
patient-centered medical home-
recognized practices, outside of this
system, enrollment served by PCMHs
increased from 3 percent to 11 percent
between 2016 and 2018.
• Several insurers are supporting primary
care providers in clinical transformation to
advanced primary care, though not
meeting PCMH standards. Measurement
of primary care performance will likely
need to go beyond PCMH recognition
process measures to include outcomes.
• Based on the Health Care Payment
Learning and Action Network Alternative
Payment Model Framework, 10 insurers
now have Positive Incentives or Strong
Incentives for transitioning from volume-
based to value-based primary care
payment.
• Significant increases were observed for
shared savings and capitation-based
payments between 2015-18. However,
further assessment is needed to
determine the extent to which capitation to
medical groups or physician organizations
cascades to individual providers.
• For insurers to continue to adopt value-
based primary care payment or to
increase investment, measurement of
primary care performance will likely need
to include outcomes.
Highlights

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 60
1. Ensure that all enrollees either select or be matched with a primary care physician (PCP) within 60
days of enrollment;
2. Insurers are required to have an increasing percentage of their enrollees cared for in patient-
centered medical home models and annually report the number and percent of enrollees who
obtain their care in a patient-centered medical home (PCMH); and
3. Describe how the insurer’s payment strategy supports primary care physicians in adopting
accessible, data-driven, team-based care with accountability for meeting the Triple Aim goals of
enhanced quality, improved outcomes and lower costs.
Primary Care Physician Matching
In January 2017, Covered California required that all enrollees in preferred provider organizations
(PPO), health maintenance organizations (HMO), and exclusive provider organizations (EPO), be
matched to a primary care physician (PCP) or other primary care clinician, such as a nurse practitioner,
upon enrollment. The purpose of the requirement was to bring the PCP match concept to the PPO and
EPO environment and give enrollees a single point of contact who can help them navigate the health
care system. A primary care physician can provide continuity and
address most health care needs, helps consumers select the proper
specialist, coordinates their care with other providers and ensures
they understand their treatment options. While having a PCP can
help select and coordinate care across specialty providers, enrollees
in PPO and EPO plans can still choose to navigate the health care
system on their own without permission from their PCP to seek
treatment or a referral to see a specialist.
Since 2017, virtually all Covered California’s enrollees, over 99
percent, either selected or were matched with a PCP upon enrollment
which was nearly a 30-percentage point increase from the 2016
baseline rate of 70 percent.
Covered California believes this PCP match will ultimately help people get better access to care in a
timelier manner. However, many enrollees may need more explanation of why working with their PCP
is beneficial. Covered California is currently working with its plans to examine the data to understand
the patient experience and clinical and financial effects of this program. Covered California will look to
examine outcomes of clinical measures that may improve with a strong foundation in primary care.
Promoting Enrollment in Patient-Centered Medical Homes
A growing body of evidence shows that advanced models of primary care, which include patient-
centered medical homes (PCMHs), greatly improve the care delivered to patients and support Triple
Aim goals. Advanced primary care models utilize a patient-centered, accessible, team-based approach
to care delivery, enrollee engagement and data-driven improvement, as well as integration of care
management, behavioral health and community resources for patients with complex conditions. Under
the existing contract requirement, insurers are required to have an increasing portion of enrollees who
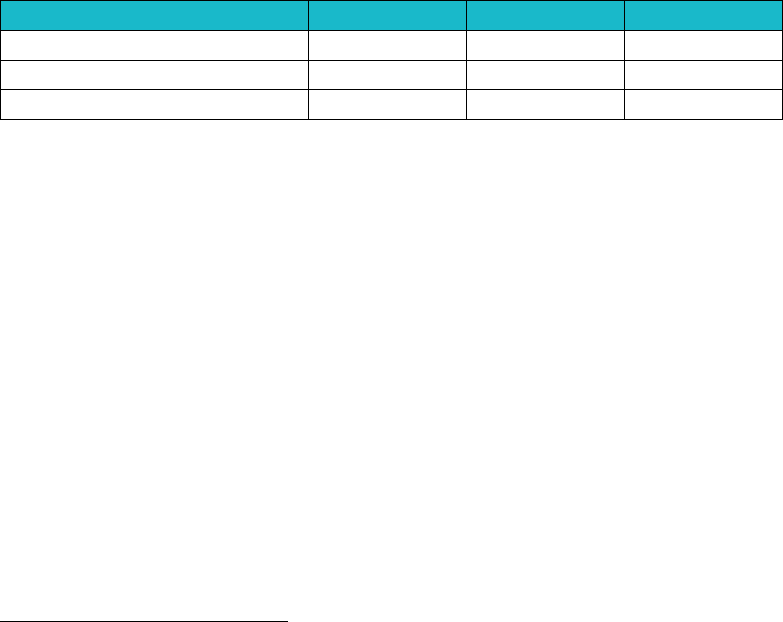
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 61
obtain their care in a PCMH model and plans must use formal recognition programs to assess which
providers are PCMHs.
40
While there have been significant increases in the percentage of enrollees seen in PCMH settings,
health insurance companies report that many in their primary care networks believe the current
requirement tied to PCMH recognition is too limited and burdensome. As of 2018, about 40 percent of
Covered California enrollees received primary care through providers that met PCMH standards. The
great majority of that enrollment, however, was through Kaiser Permanente, which represented 82
percent of total PCMH enrollment in 2018. The percentage of enrollees cared for by PCMH-recognized
practices, outside of the Kaiser Permanente system, increased threefold from 3 percent to 11 percent
between 2016 and 2018, an 8-point increase (see Table 28. Percentage of Covered California
Enrollees Cared for in Patient Centered Medical Homes, 2016-18). When looking at all insurers during
the three years, the percent of Covered California enrollees who were cared for in PCMHs increased
from 25 percent in 2015 to 40 percent in 2018. One of Sharp Health Plan’s integrated medical groups
achieved PCMH recognition in 2018 to comply with the Covered California requirement and this change
accounts for most of the overall increase outside Kaiser Permanente. The percent of Sharp Health Plan
enrollees cared for in a PCMH increased from 15 percent in 2017 to 66 percent in 2018.
Table 28. Percentage of Covered California Enrollees Cared for in
Patient-Centered Medical Homes, 2016-18
2016
2017
2018
All Enrollment
25%
32%
40%
Kaiser Permanente
100%
100%
100%
Non-Kaiser Permanente
3%
6%
11%
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Covered California has found that formal PCMH recognition programs have limitations and have been
challenged as other measures of advanced primary care have evolved. The formal PCMH recognition
programs largely document process improvement without measuring outcomes. Many advanced
primary care practices have not sought formal recognition and many that have been recognized have
implemented process improvements, but these may not have led to improvement in clinical quality or
reduced cost. Additionally, several health insurance companies are focusing on primary care practice
transformation programs that include practice coaching to support primary care providers in improving
quality and efficiency rather than requiring or promoting PCMH recognition. Based on this feedback
from health insurance companies and providers, Covered California is examining alternative
approaches to promote improvements in primary care and assuring more enrollees benefit from these
programs.
Payment Strategies that Promote Effective Primary Care
The Affordable Care Act included several demonstration projects and grants to test payment reforms
that would shift volume-driven Fee-for-Service (FFS) payments to methods that link provider payment
40
The current contract requirements list the following recognition programs: a) National Committee for Quality Assurance PCMH recognition;
b) The Joint Commission Primary Care Medical Home certification; c) Accreditation Association for Ambulatory Health Care, Inc. Medical
Home accreditation; and d) URAC PCMH Certification.
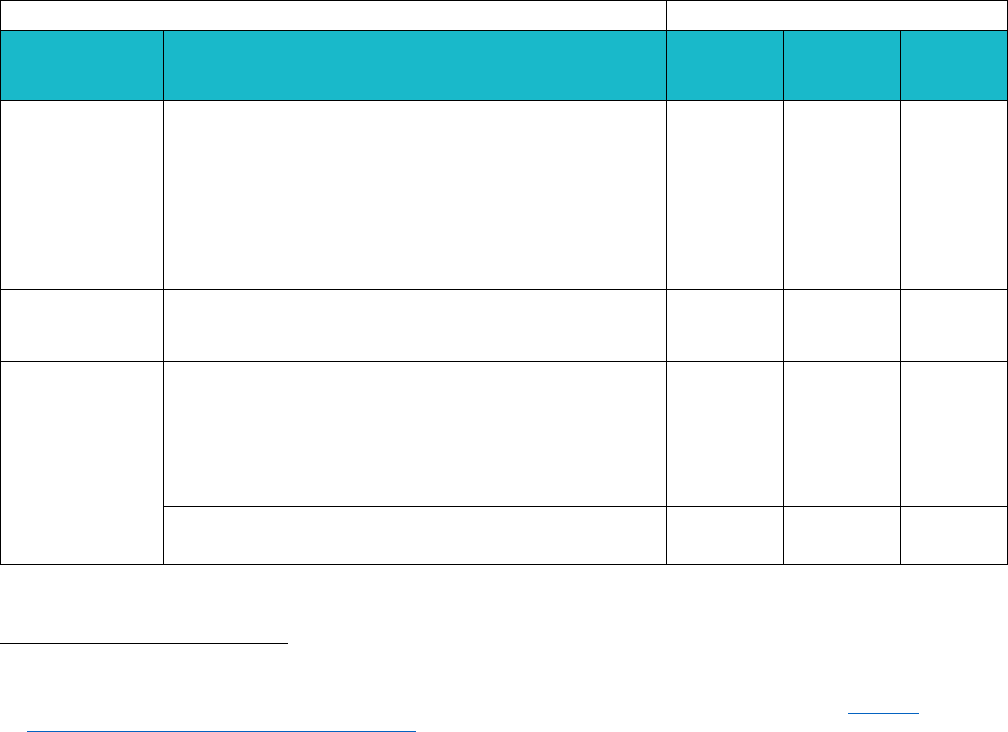
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 62
with performance on cost and quality. To measure health insurance company progress in payment
strategies that promote accountability for Triple Aim goals, Covered California leveraged the four
categories in the Health Care Payment Learning and Action Network (HCP LAN) Alternative Payment
Model (APM) Framework
41
(see Table 29. Covered California Assessment of Primary Care Payment
Strategies Based on the HCP LAN Alternative Payment Model Framework, 2015, 2017 and 2018).
While PCMHs are delivery models, not payment models, the Alternative Payment Model Framework
notes that PCMHs and advanced primary care need the support of value-based payment models.
Shifting payments from FFS to payments that increasingly hold primary care providers financially at-risk
for high-quality care creates incentives for managing cost and quality. In assessing payment strategies,
Covered California requires its contracted health plans to pay increasingly based on “Category 3:
Shared Savings” and “Category 4: Population-based Payment,” which Covered California reports below
as having Positive Incentives and Strong Incentives, respectively.
As of 2018, Covered California assessment found that 10 health insurance companies were paying
providers with either Positive Incentives or Strong Incentives for value – an increase of two insurers
from 2015. More insurers are now assessed to have Positive Incentives or Strong Incentives.
Table 29. Covered California Assessment of Primary Care Payment Strategies
Based on the HCP LAN Alternative Payment Model Framework, 2015, 2017 and 2018
42
Number of Health Plans
Covered
California
Assessment
APM Framework
2015
2017
2018
Strong
Incentives
Category 4 – Population-based Payment
• Condition-specific population-based payment
including per member per month payments
• Comprehensive population-based payment such
as global budgets or percent of premium
payments
• Integrated finance and delivery system such as
global budgets in integrated systems
2
2
2
Positive
Incentives
Category 3 – APMs built on an FFS architecture:
• APMs with shared savings (upside risk only)
• APMs with share savings and downside risk
6
7
8
Weak
Incentives
Category 2 – FFS– Link to quality and value
• Foundational payments for infrastructure and
operations
• Pay for reporting
• Pay for performance
• Rewards and penalties for performance
3
2
1
Category 1 – Fee-for-Service (FFS)– No link to
quality and value
1
1
1
41
Health Care Payment Learning and Action Network. (2017). Alternative Model Payment Framework. Retrieved from http://hcp-
lan.org/workproducts/apm-refresh-whitepaper-final.pdf.
42
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.
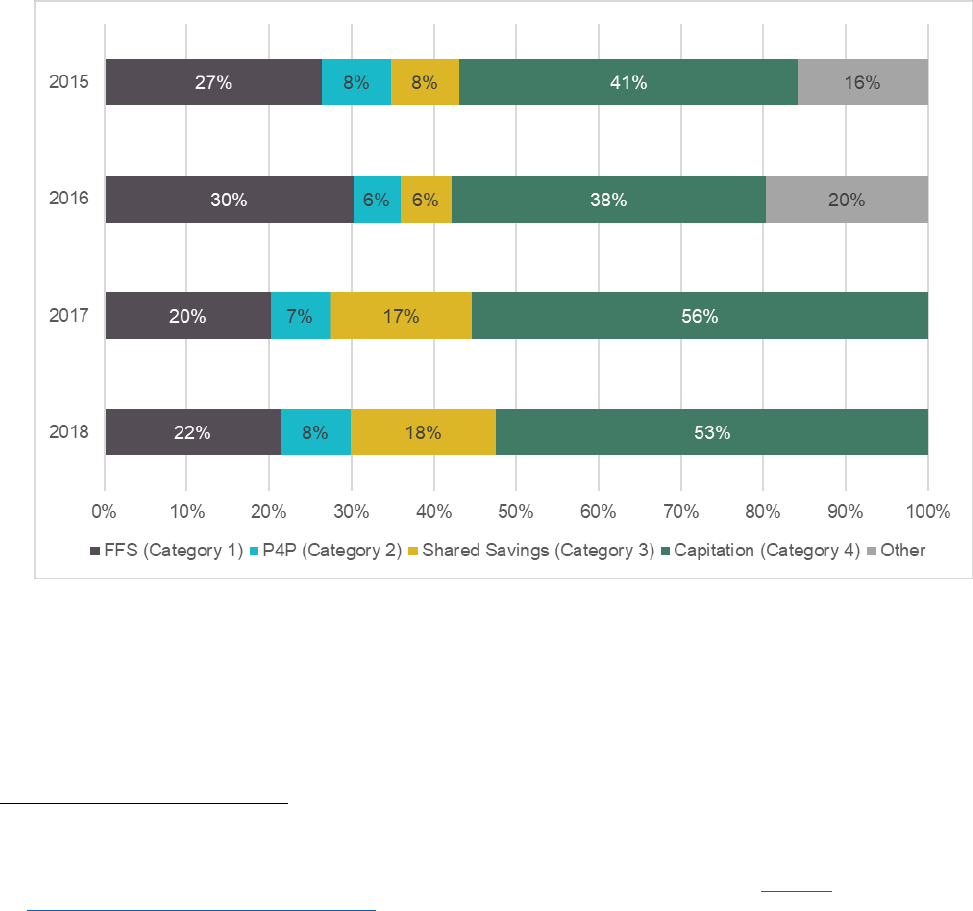
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 63
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
As expected, payment strategies to PCPs vary widely (see Figure 4. Covered California Insurer
Payment Strategies for Primary Care Providers, 2015 – 2018), but from 2015 to 2018 there has been a
significant increase in payment to providers being based on capitation (increasing from 41 percent to 53
percent) and shared savings (increasing from 8 percent to 18 percent). The decline in payments to
primary care providers based on fee-for-service and the fact that Covered California plans now pay 71
percent of primary care providers using capitation or shared savings is important progress. At the same
time, based on discussions with insurers and provider groups, there is reason to be concerned that
capitation payments made to medical groups or physician organizations may not cascade to individual
providers, many of whom continue to be largely paid on a fee-for-service basis.
Figure 4. Covered California Insurer Payment Strategies for Primary Care Providers, 2015 – 2018
Note: “Other” refers to payments types that insurers could not breakdown into the four HCP LAN categories. These percentages are
enrollment weighted and may not equal 100 due to rounding.
Source: California Staff Analysis of Qualified Health Plan Submitted Data
According to the HCP LAN, in calendar year 2018, about 56 percent of national commercial market
total health care payments were FFS (Category 1), 14 percent of payments were FFS with a link to
quality (Category 2), 28 percent of payments were shared savings (Category 3) and only 2 percent of
payments were population-based payments or capitation.
43
This data is collected through surveys of
43
Health Care Payment Learning and Action Network. Measuring Progress: Adoption of Alternative Payment Models in Commercial,
Medicaid, Medicare Advantage, and Traditional Medicare Programs. October 24, 2019. Retrieved from: http://hcp-
lan.org/workproducts/apm-methodology-2019.pdf.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 64
health insurance companies and represents about 133.5 million covered lives which is 61 percent of the
national commercial market. Although this data represents all commercial health care payments, it
suggests that Covered California insurers have made significant progress in moving towards capitation
or population-based payment and away from FFS payments for primary care providers compared to the
rest of the nation. In 2018, only 22 percent of Covered California insurer’s primary care payments were
FFS compared to the national rate of 56 percent FFS for all health care payments for the commercial
market.
Interaction of Payment Strategies, Patient-Centered Medical Homes, and Promotion of
Advanced Primary Care
At this time, there is not enough information to establish a link between payment strategies and the
percent of members cared for in a PCMH. There appears to be a clearer relationship between
increased enrollment in a PCMH model and whether the plan is part of an integrated delivery system.
Some health insurance companies assessed by Covered California to have Strong Incentives for their
payment strategies also had a higher percent of enrollees cared for in PCMHs (e.g., Kaiser
Permanente pays 100 percent of its primary care physicians a population-based payment, which is
considered a Category 4 APM, and 100 percent of its providers are PCMH recognized). Kaiser
Permanente and Sharp Health Plan, both fully integrated delivery systems, are high outliers for
enrollment in a PCMH model. However, the other nine health insurance companies of which some are
considered to have Weak Incentives because they paid their providers FFS, had similar percentages of
enrollees cared for in a PCMH as those with Strong Incentives or Positive Incentives. In some
instances, it was also difficult to attribute a relationship between specific payment strategies and
enrollees cared for in a PCMH because some providers simultaneously received enhanced
reimbursements for PCMH recognition from other payers, such as Medi-Cal.
Strategies to Enroll or Attribute Enrollees to Patient-Centered Medical Homes
Although not definitive, there may be a relationship between promoting PCMH-recognized providers to
enrollees and the percent of enrollees cared for in a PCMH. Between 2015 and 2018, most health
insurance companies did not actively promote PCMH providers to enrollees or actively assign or match
enrollees to PMCHs. The few insurers that listed PCMH recognition in provider directories were
observed to have higher rates of enrollees cared for in a PCMH.
Section 2: Health Plan Measures Reported to the Marketplace Quality
Rating System
Health Plan Measures Reported to the Marketplace Quality Rating System details health plan
performance on Healthcare Effectiveness Data Information Set (HEDIS) and Consumer Assessment of
Healthcare Providers and Systems (CAHPS) measures reported to the Centers for Medicaid and
Medicare Services’ Quality Rating System (QRS). These standard performance measures are a key
mechanism used by Covered California for health plan oversight and accountability.
See Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System, for Quality
Rating System measures that pertain to Promotion of Effective Primary Care:
1. Rating of Personal Doctor (CAHPS) (Table A21)
2. Rating of Specialist (CAHPS) (Table A22)
The patient experience reporting of enrollees Rating of Personal Doctor showed wide variation but was
marked by the fact that 9 of 11 health plans — representing 89 percent of enrollees — had ratings
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 7
COVERED CALIFORNIA 65
below the 25
th
percentile nationally. However, the range of scores is exceedingly narrow; for Rating of
Personal Doctor, a raw score below 86 is below the 25
th
percentile, while a raw score of 90 is the 90
th
percentile.
Section 3: Implications for the Future
Ensuring all enrollees have a PCP, regardless of their health plan product, provides a single point of
contact to help them navigate the health care system. Covered California is evaluating the impact of
PCP matching in EPO and PPO plans based on outcomes including utilization, continuity of care, cost
and quality that may improve with a strong foundation in primary care. Covered California continues to
work with insurers to help all enrollees understand the value of primary care.
Further assessment is needed to determine the extent to which capitation to medical groups or
physician organizations cascades to individual providers. Covered California will continue to require
health insurance companies to increasingly implement value-based payments for primary care
providers like shared savings and population-based payment or capitation. One of the biggest barriers
to full adoption of advanced primary care, despite the changes to payment structure described above,
appears to be inadequate revenue or resources to support well-rounded care teams, underscoring the
importance of continued efforts at primary care payment reform.
For health insurance companies to make these investments, measurement of performance will likely
need to go beyond the PCMH recognition process measures to include outcome measures that reflect
the impact advanced primary care can have improving quality, enhancing the patient experience, and
reducing total cost of care and documenting a return on investment for insurers that increase primary
care payment such that it accounts for a larger share of the overall health care budget.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 66
Chapter 8: Promotion of Integrated
Delivery Systems and Accountable
Care Organizations
Promotion of integrated delivery systems and
accountable care organizations is premised on
the increasing evidence that effectively caring for
and managing a person’s health requires an
integrated care system that can coordinate
across providers, sites and times for a variety of
conditions while delivering good outcomes and
quality at an affordable cost.
44
,
45
This chapter on Promotion of Integrated Delivery
Systems and Accountable Care Organizations
presents performance data reported by health
insurance companies for contract requirements
and includes assessments and observations by
Covered California. This chapter is organized as
follows:
Section 1. Qualified Health Plan Experience
Section 2. Implications for the Future
Section 1: Qualified Health Plan
Experience
Covered California has the following
requirements for integrated delivery systems
(IDSs) or accountable care organizations (ACOs):
1. Increase enrollment over time and report
the number and percent of enrollees who
are managed under an IDS or ACO as
well as provide comparison reporting for
other lines of business;
44
Covered California’s recently completed evidence review affirmed the value and positive impact on quality and cost of effective care
integration and some models of Accountable Care Organization (see Current Best Evidence and Performance Measures for Improving
Quality Care and Delivery System Reform). In addition, recent data from the Integrated Health Care Association (IHA) Cost and Quality
Atlas, shows clinical quality was higher for ACO and HMO members compared to PPO members for commercial plans (see
https://atlas.iha.org/story/aco).
45
An integrated delivery system (IDS) is a network of physicians and healthcare facilities that provide a continuum of healthcare services
managed under one organization or one parent company. Accountable care organizations (ACOs) are groups of physicians and
healthcare facilities that share financial and medical responsibility for providing coordinated care, with financial incentives to provide high-
quality care and to limit avoidable, unnecessary spending.
• In 2018, 60 percent of Covered California
enrollees were cared for in an Integrated
Delivery System (IDS) or an Accountable
Care Organization (ACO), which
represents a 12-point increase from 2015.
After excluding the fully-integrated delivery
systems, Kaiser Permanente and Sharp
Health Plan, 25 percent of Covered
California enrollees were cared for in an
ACO, which represents a 4-point increase
from 2015 and far exceeds state and
national benchmarks.
• Nine insurers reported offering technical
support, data sharing support, or
promoting participation in health
information exchanges for providers in
2018, an increase from four insurers in
2015. Covered California has also seen a
steady increase in the number of insurers
using other common components of
integrated coordinated care such as
population health management support
and holding providers accountable using
standard quality measure sets.
• Insurers are required to report 2018
performance based on the IHA
Commercial ACO measures by year-end
2019, which will allow better
understanding of performance variation of
different ACO models and inform future
contract requirements.
Highlights
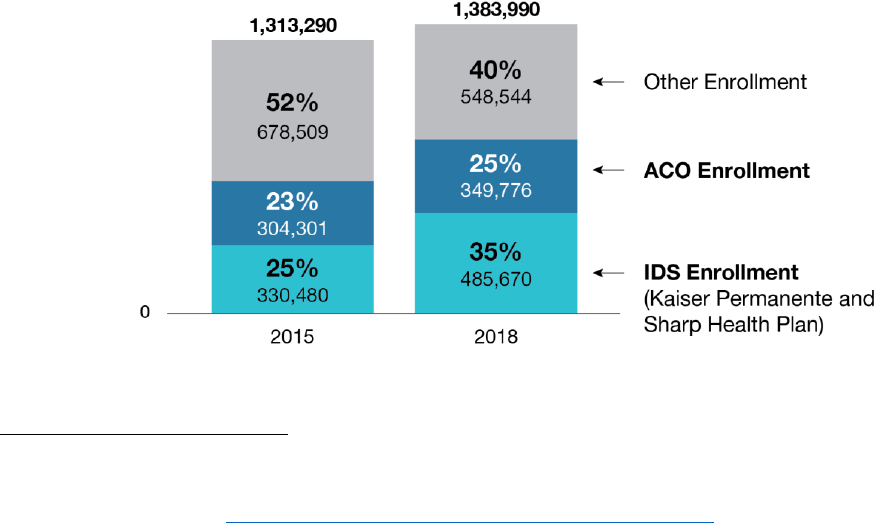
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 67
2. Provide details on the key design characteristics of existing or planned integrated systems of
care and how these systems of care compare to the definition in the Covered California
contract; and
3. Report performance of different ACO models for all lines of business using the IHA Commercial
ACO Measure Set once data becomes available for plan year 2018.
Percent of Enrollees in an Integrated Delivery System or Accountable Care Organization
Covered California requires health insurance companies to report the number and percent of enrollees
who are managed under an IDS or ACO as well as provide comparison reporting for their other lines of
business. Insurers are also are required to demonstrate an increase in the percent of enrollees who
obtain their care in an IDS or ACO model between 2017 and 2019.
Nationally, the Centers for Medicare and Medicaid Services (CMS) is leading a drive to implement
value-based payment models including integrated and coordinated delivery models such as ACOs.
Leavitt Partners tracks the growth and spread of ACOs including the new models supported by CMS
and their commercial and Medicaid analogs.
46
As of 2018, 10 percent of the U.S. population or 32.7
million Americans were cared for in ACOs in the commercial, Medicaid and Medicare markets. This
includes every state, with penetration ranging from 2 percent to over 20 percent. Leavitt Partners
reports that between 10 to 15 percent of Californians are cared for in such models.
In 2018, 60 percent of Covered California enrollees were cared for in an IDS or ACO, which represents
a 12-point increase from 2015 (see Figure 5. Covered California Enrollment in Integrated Delivery
Systems or Accountable Care Organizations, 2015 and 2018).
47
Figure 5. Covered California Enrollment in Integrated Delivery Systems or Accountable Care
Organizations, 2015 and 2018
46
Muhlestein et al. (2018). Recent Progress in The Value Journey: Growth of ACOs and Value-Based Payment Models in 2018. Health
Affairs blog. Retrieved from https://www.healthaffairs.org/do/10.1377/hblog20180810.481968/full/
47
Data only available for plan year 2015 and plan year 2017-18. Covered California did not ask this question in the Certification Application
for plan year 2016.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 68
Source: Covered California Staff Analysis of Qualified Health Plan Data Submitted for 2015 and 2018
Note: Enrollment figures reflect only on-Exchange enrollment.
Two insurers, Kaiser Permanente and Sharp Health Plan, are fully integrated delivery systems and
account for about 60 percent of the overall number.
48
As of 2018, after excluding enrollment in Kaiser
Permanente and Sharp Health Plan, 25 percent of Covered California enrollees among the other
insurers were cared for in an ACO, which represents a 2-percentage point increase from 2015. It is this
latter statistic that is most comparable to the national data from Leavitt Partners; based on this report,
California has greater penetration of these new models than the U.S. and Covered California
penetration exceeds the rest of California even excluding those enrolled with Kaiser Permanente or
Sharp Health Plan.
Health Plan Components of Integrated Delivery Systems or Accountable Care
Organizations
Covered California places great importance on the adoption and expansion of integrated, coordinated
and accountable systems of care. As such, health insurance companies are required to provide details
on existing or planned integrated systems of care and how these systems of care compare to the
following definition:
1. A system of population-based care coordinated across the continuum including multi-discipline
physician practices, hospitals and ancillary providers; and
2. Having combined risk sharing arrangements and incentives between the health insurance
company and providers, and among providers across specialties and institutional boundaries,
holding the ACO accountable for nationally recognized evidence-based clinical, financial, and
operational performance, as well as incentives for improvements in population outcomes.
Based on the descriptions of their IDS or ACO models provided by insurers, Covered California has
identified several components many insurers are using in their respective models. In 2018, most
insurers (nine out of 12) reported offering technical support, data sharing support, or promoting
participation in health information exchanges for providers, an increase from four insurers in 2015 (see
Table 30. Components of Covered California Insurer’s Support for Integrated Delivery Systems or
Accountable Care Organizations, 2015, 2017 and 2018). Covered California has also seen a steady
increase in the number of health insurance companies using other common components like population
health management support and holding providers accountable using standard quality measure sets.
48
In Covered California, Kaiser Permanente and Sharp Health are fully integrated delivery systems while other health plans base their ACO
model on existing provider organizations, such as integrated medical group and hospitals.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 69
Table 30. Components of Covered California Insurer’s Support for Integrated Delivery Systems or
Accountable Care Organizations, 2015, 2017 and 2018
49
,
50
Component
Number of Health Plans
2015
2017
2018
Data Sharing, Data Exchange and Health Information
Technology
Offers providers technical support, data sharing support, or
promotes participation in health information exchanges
4
6
9
Provider Support and Feedback
Offers providers opportunities to share best practices,
participate in learning collaboratives, or offers practice coaching
5
5
6
Quality Measurement and Improvement
Providers are held accountable for improvement using a
standardized measure set
4
5
6
Population Health and Case Management
Supports providers in case management or population health
management such as providing registries or care gap reports
4
5
6
Financial Incentives
Uses population-based capitation, shared savings or shared
risk, may also use incentives for quality
5
5
6
Note: Not all insurers are listed for each component. Some insurers may only be using one of these components, while others are using
several.
Source: Covered California Staff Analysis of Qualified Health Plan Data Submitted for 2015 and 2017-18.
Comparing Performance of Different ACO Models using the Integrated Healthcare
Association Commercial ACO Measure Set
The Integrated Healthcare Association (IHA) has developed a Commercial ACO Measure Set
51
derived
from their long-standing physician organization performance measures which has been widely adopted
in California. While it is early to assess ACO performance in California as there is enormous variation in
the structure of ACO contracts and many have only a few years of performance, IHA has begun to
report on results from using the Commercial ACO Measure Set for 85 ACO contracts in California
based on 2017 performance.
In the charts below, IHA reports performance for three mutually exclusive groups: members cared for
by ACOs representing a mix of models built on both HMO and PPO platforms, members cared for by
provider organizations under capitated, delegated HMO contracts (excluding Kaiser Permanente
medical groups), and members cared for by physicians under PPO contracts aggregated across the 19
Covered California pricing regions (see Figure 6. California Commercial ACO Performance Compared
to HMOs and PPOs, 2017). Based on IHA analysis, ACOs provide care that is the same quality at a
somewhat lower cost than either HMOs or PPOs.
49
Data only available for plan year 2015 and plan years 2017-18. Covered California waived data collection for plan year 2016.
50
The 11 health insurance companies in Covered California are: Anthem Blue Cross, Blue Shield of California, Chinese Community Health
Plan, Health Net, Kaiser Permanente, L.A. Care, Molina Healthcare, Oscar Health, Sharp Health Plan, Valley Health Plan, and Western
Health Advantage. In the tables below, Health Net is counted twice because its reports data separately for Health Net Life (PPO/EPO
products) and Health Net of California (HMO/HSP products).
51
See more: https://www.iha.org/our-work/accountability/commercial-aco.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 70
Figure 6: California Commercial ACO Performance Compared to HMOs and PPOs, 2017
Source: Integrated Healthcare Association, 2019
The aggregate ACO performance is encouraging but represents an average with wide variation among
the ACOs measured (see Figure 7. Variation in Quality and Cost in California Commercial ACO
Performance, 2017).
Figure 7: Variation in Quality and Cost in California Commercial ACO Performance, 2017
Source: Integrated Healthcare Association, 2019
The 14 “high value” ACOs in the upper right-hand quadrant — representing both lower cost and better
quality — rival and sometimes exceed the performance of the best medical groups contracting with
insurance companies within HMO models and one third of these high value ACOs are operating under
PPO contracts (see Figure 8: Characteristics of 14 “High Value” ACOs in California, 2017).

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 71
Figure 8: Characteristics of 14 “High Value” ACO in California, 2017
Source: Integrated Healthcare Association, 2019
This first report from IHA comparing ACOs to other models demonstrates the potential value of
integration and coordination through ACOs and that they can be implemented through all health plan
products including PPOs.
The IHA Commercial ACO Measure Set reports for performance based on 2018 were recently released
and health insurance companies are required to report these results to Covered California. The
variation in performance among ACO contracts will be examined in cooperation with IHA, insurance
companies and provider organizations and compared to the design elements MedPAC and others
52
have cited as predictors of success including two-sided risk, physician leadership (as compared to
hospital leadership) and greater emphasis on advanced primary care.
53
Section 2: Implications for the Future
Outside of the integrated delivery systems, Covered California’s contracted health insurance
companies that share overlapping networks are implementing a variety of ACO models or components
of ACO models within their networks. Covered California enrollment in ACOs, excluding integrated
delivery systems, exceeds comparisons in California and the nation. Performance variation among
ACO models may be attributed to design elements such as the structure of financial incentives
including downside risk, the role of physicians in sponsorship and leadership structure, the percent of
budget spent in primary care and the sophistication of population health and case management
52
The most current best evidence is documented in Chapter 8, Promotion of Integrated Delivery Systems and Accountable Care
Organizations, of a companion Covered California report, Current Best Evidence and Performance Measures for Improving Quality of Care
and Delivery System Reform.
53
Primary Care Collaborative. (August 2018). Advanced Primary Care: A Key Contributor to Successful ACOs. Retrieved from:
https://www.pcpcc.org/sites/default/files/resources/PCPCC%202018%20Evidence%20Report.pdf.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 8
COVERED CALIFORNIA 72
strategies. IHA is building a registry based on such elements for all ACOs they measure. As discussed
above, Covered California is working with insurers to use the performance data from the IHA
Commercial ACO measure set to establish correlations with the design elements in the registry of ACO
characteristics to determine best practices and inform future contract requirements. This report cites
several ways in which integrated delivery systems are outperforming network model health plans. The
success of ACOs in replicating the performance of integrated delivery systems may depend on
alignment in adopting common best practice design elements.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 73
Chapter 9: Networks Based on Value
As a major strategy for effective care delivery,
Covered California requires health insurance
companies to select and regularly assess all
clinicians, providers, hospitals and sites of care to
ensure that care is safe, timely, effective, efficient,
equitable, and patient-centered. Ideally, every
network is designed to integrate and coordinate care,
provides effective primary care and maximizes its
value to enrollees.
For many consumers, whether the provider they
want to see is in their network or not is the first sign
of value. Assuring consumers have access to the full
range of providers and treatments and that networks
are composed of a range of quality providers is a
central part of Covered California’s review and
selection process of its contracted insurers (see
“Covered California Network Composition Review”).
Covered California works to ensure health plan
networks are designed and maintained with a
deliberate strategy to promote better quality, lower
cost, improved health and health equity.
This chapter on Networks Based on Value presents
performance data and processes reported by health
plans for contract requirements and includes
assessments and observations by Covered
California. This chapter is organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Implications for the Future
Section 1: Qualified Health Plan
Experience
Covered California’s requirements for “Networks
Based on Value” include multiple elements related to
ensuring that network design and selection of
providers considers quality and patient experience in
addition to cost and efficiency.
Under current contract requirements, insurers report
progress to Covered California for the following:
1. The factors used to select providers and hospitals in the health plan network, including cost,
clinical quality, patient reported experience, or other factors.
• Between 2015 and 2018, more health
insurance companies were assessed
as having Considered Comprehensive
Factors (cost, quality, and patient
experience) or Considered Cost Only
as criteria for selecting or contracting
with providers and hospitals.
• For selecting providers, most insurers
noted using provider credentialing,
member satisfaction results,
grievances and appeals information,
and quality based on HEDIS
measures. Fewer insurers reported
using referral patterns to hospitals,
value or cost reduction, or IHA Align
Measure Perform (AMP) program
results for selecting providers.
• All insurers indicated that a hospital’s
designation as a Center of Excellence
was a selection factor and most
reviewed and tracked publicly reported
quality data from the Leapfrog Group,
CMS Hospital Compare, and other
quality-based organizations to
determine whether to contract with a
hospital. Fewer insurers reported
evaluations of cost or participation in
quality collaboratives as a factor in
hospital selection.
• Hospital acquired infection rates are
now reviewed routinely by health plans
with their contracted hospitals. Cal
Hospital Compare has provided health
plans four partially overlapping lists of
hospitals with consistently low
performance. Covered California is
tracking and learning how insurers use
these lists to determine next steps.
Highlights
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 74
2. Adopt policies and procedures to only contract with providers and hospitals that demonstrate
quality and promote safety at a reasonable price. Based on a definition provided by Covered
California, develop plans to exclude “outlier poor performers” on either cost or quality or
document the rationale for continued contracting with poor performers, including any
improvement efforts the provider or hospital has undertaken by year-end 2020.
3. Demonstrate action on high cost providers
54
by annually reporting the following:
a. The factors a health plan considers in assessing the relative unit prices and total costs of
care;
b. The extent to which the reasons for cost factors are adjusted or analyzed by elements
such as area of service, population served, market dominance, services provided by the
facility (e.g., trauma or tertiary), or other factors;
c. How such factors are used in the selection of providers and hospitals; and
d. Identification of specific hospitals and their distribution by cost deciles or other ways
providers and hospitals are grouped by costs, e.g., as a percentage of Medicare costs.
There are few best practices broadly adopted for managing networks based on value. Integrated
delivery systems such as Kaiser Permanente and Sharp Health Plan have largely exclusive networks of
hospitals and medical groups. This chapter includes an assessment of these integrated delivery
systems but largely focuses on the various strategies adopted by health insurance companies that do
not have fully integrated delivery systems and often have overlapping hospital and provider networks.
Covered California adopted a common strategy in assessing hospital quality based on publicly reported
data described in the “Sites and Expanded Approaches to Care Delivery” chapter. The hospital quality
and safety requirements serve as a foundation on which insurers can build networks based on value.
In addition to requiring insurers to design their networks based on value, Covered California conducts
annual reviews of each health plan’s network (see Covered California Network Composition Review).
54
Covered California also requires health plans to report on the use of cost transparency tools as one of the strategies to ensure providers
are not charging unduly high prices. See Chapter 10, Appropriate Interventions for health plan reporting on this topic.
Covered California Network Composition Review
As part of its annual contracting cycles, Covered California assesses network composition including
the number and types of physicians, medical groups and hospitals that are unique to particular health
plans or available through multiple plans. Covered California also assesses the geographical
distribution of health plan networks through drive times to hospitals and other indicators of how a
health plan’s distribution of providers assures consumers have timely access to care. Covered
California coordinates with the California Department of Managed Health Care and the California
Department of Insurance to ensure each health plan’s network meets network adequacy standards
and time and distance standards.
Covered California also requires its contracted insurers to include Essential Community Providers
(ECPs) who serve low-income and medically underserved communities in their provider networks.
Covered California provides insurers a list of ECPs each year that includes federally designated 340B
providers, California disproportionate share hospitals, federally qualified health centers and Indian
health and Tribal health organizations, among others. Each year, Covered California assesses the
degree to which health plans have included a variety of ECPs in their networks.
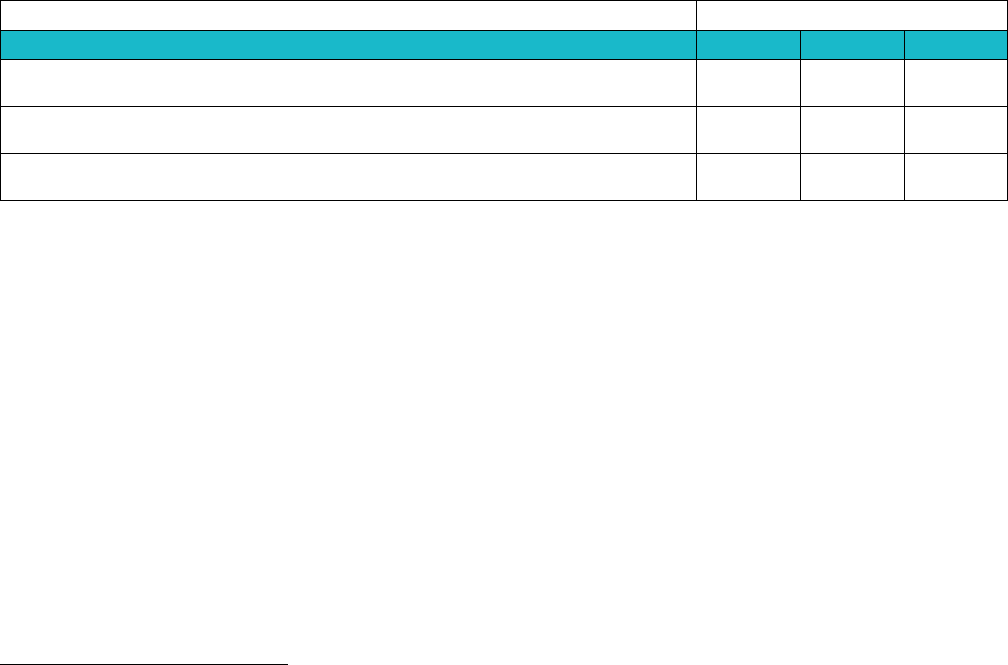
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 75
Factors Used by Insurers to Select Medical Groups and Individual Providers
As described below (Table 31. Assessment of Factors Used by Covered California Insurers to Select
Physician Organizations and Individual Providers, 2015, 2017 and 2018), Covered California assessed
the number of health insurance companies using cost, quality and patient experience as criteria for
selecting or contracting with a provider.
55
Between 2015 and 2018, Covered California assessment of
provider selection factors found that the number of insurers that Considered Comprehensive Factors or
Considered Cost Only increased from seven to 10.
Table 31. Assessment of Factors Used by Covered California Insurers to Select Physician Organizations
and Individual Providers, 2015, 2017 and 2018
56
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
For plan years 2017 and 2018, health insurance companies were asked generally about factors used to
select providers.
57
For both years, most insurers reported using provider credentialing, member
satisfaction results and grievances and appeals information, and quality or HEDIS measures for
selecting providers. While six Covered California insurers formally participate in IHA’s Align Measure
Perform (AMP) program, few insurers described using AMP program results for selecting providers
during 2017-18.
58
Three insurers reported reviewing referral patterns of providers or provider groups to
determine whether they refer to in-network hospitals or have established referral patterns to in-network
hospitals. Only two insurers cited cost savings or cost reduction as a factor for selecting providers.
Factors Used by Insurers to Select Hospitals
Covered California assessed and categorized the number of health insurance companies using cost,
quality and patient experience as criteria for selecting or contracting with hospitals (see Table 32.
Assessment of Factors Used by Covered California Insurers to Select Hospitals, 2015, 2017 and
55
The 11 health insurance companies in Covered California are: Anthem Blue Cross, Blue Shield of California, Chinese Community Health
Plan, Health Net, Kaiser Permanente, L.A. Care, Molina Healthcare, Oscar Health, Sharp Health Plan, Valley Health Plan, and Western
Health Advantage. In the tables below, Health Net is counted twice because its reports data separately for Health Net Life (PPO/EPO
products) and Health Net of California (HMO/HSP products).
56
Data only available for plan year 2015 and plan year 2017-18. Covered California did not ask this question in the Certification Application
for plan year 2016.
57
Information described here is based on insurers’ narrative responses to questions in the Certification Application. Covered California asked
generally about factors considered and did not specifically prompt insurers about each of them. As such, insurers could be using a factor
to select providers but may not have described it.
58
For the IHA AMP program, one insurer does not formally participate but reviews the program results as a provider selection factor and
another insurer is planning to participate but does not formally participate currently.
Number of Health Plans
Assessment
2015
2017
2018
Considered Comprehensive Factors
Includes cost, quality, and patient experience in selecting providers
5
7
6
Considered Cost
Includes cost in provider selection
2
1
4
Considered Minimal Factors
Does not include cost, quality, or patient experience in selecting providers
5
4
2
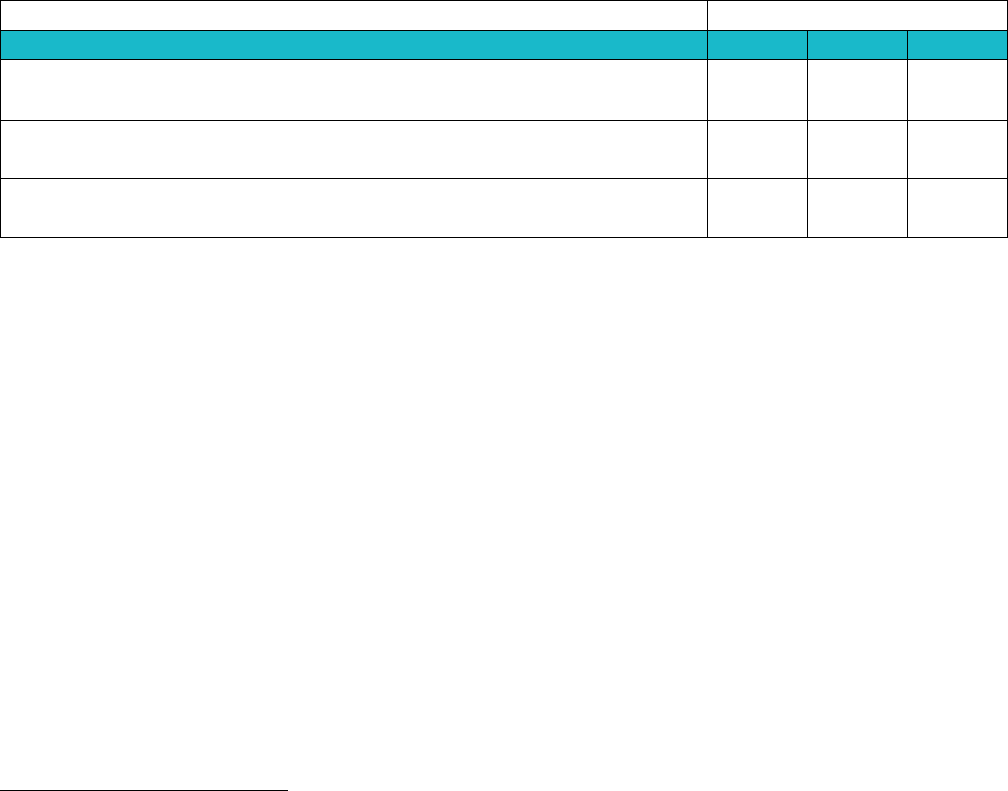
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 76
2018).
59
Covered California’s assessment of hospital selection factors found that as of 2018 four
insurers Considered Comprehensive Factors, while others considered cost. While many insurers do not
currently use comprehensive factors in hospital selection, most insurers have been actively engaged in
work to promote improvement in hospital quality performance as described in Chapter 11: Sites and
Expanded Approaches to Care.
Table 32. Assessment of Factors Used by Covered California Insurers to Select Hospitals,
2015, 2017 and 2018
60
Number of Health Plans
Assessment
2015
2017
2018
Considered Comprehensive Factors
Include cost, quality, and patient experience in selecting hospitals
3
4
4
Considered Cost
Includes cost in hospital selection
4
5
7
Considered Minimal Factors
Does not include cost, quality, or patient experience in selecting hospitals
5
3
1
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
For 2017 and 2018, health insurance companies were asked generally about factors used to select
hospitals.
61
For both years, all Covered California insurers indicated that they had processes to
designate a hospital as a Center of Excellence which was a factor for determining inclusion of a
hospital in-network. Several health plans also reviewed and tracked publicly reported quality data from
the Leapfrog Group, CMS Hospital Compare, and other quality-based organizations to determine
whether to contract with a hospital.
Health insurance companies considered the cost or prices charged by a hospital when determining
whether to contract with them. For example, some insurers evaluated costs as a percentage of
Medicare rates and used Diagnosis-Related Group (DRG) case-mix adjusted cost per discharge to
identify and group hospitals by cost deciles. Similarly, other insurers developed cost indices for
hospitals and used a combination of cost and quality measures to determine whether to remove the
hospital from their network.
One insurer reported hospital participation in collaboratives, such as the California Maternal Quality
Care Collaborative, as a factor for contracting with hospitals during 2017-18.
59
The 11 health insurance companies in Covered California are: Anthem Blue Cross, Blue Shield of California, Chinese Community Health
Plan, Health Net, Kaiser Permanente, L.A. Care, Molina Healthcare, Oscar Health, Sharp Health Plan, Valley Health Plan, and Western
Health Advantage. In the tables below, Health Net is counted twice because its reports data separately for Health Net Life (PPO/EPO
products) and Health Net of California (HMO/HSP products).
60
Data only available for plan year 2015 and plan year 2017-18. Covered California did not ask this question in the Certification Application
for plan year 2016.
61
Information described here is based on insurers’ narrative responses to questions in the Certification Application. Covered California asked
generally about factors considered and did not specifically prompt insurer about each of them. As such, insurer could be using a factor to
select hospitals but may not have described it.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 77
Covered California Targeting Outlier Poor Performance for Potential Exclusion from
Networks
Covered California requires health insurance companies to exclude a hospital from their network if the
hospital is an outlier poor performer and not working to improve safety and maternity care. To support
insurers in meeting the requirement to exclude hospital outlier poor performers, Covered California has
worked with Cal Hospital Compare to determine if there is a valid way to define outlier poor
performance for hospitals in a way that can be implemented consistently across all insurers. This
definition is based on specific measures of cost and quality, national benchmarks, analysis of variation
in California performance, best evidence for quality improvement, and effective stakeholder
engagement. Based on their review, Cal Hospital Compare found no single composite measure
meeting these criteria was available so they provided insurers with four distinct lists of hospitals with
consistently low performance based on:
1. The Hospital Acquired Condition Reduction Program (HACRP) through CMS that uses six
publicly available measures in to publicly report and financially penalize hospitals that perform in
the bottom 25 percent of all hospitals nationally;
2. An honor roll of top hospital performers developed by Cal Hospital Compare using the CMS
HACRP metrics;
3. The Leapfrog Group’s Hospital Safety Score; and
4. A report from the California Department of Public Health focused only on Hospital Associated
Infections.
These tools do not meet the requirement for a single composite system, and none include key safety
concerns where there is no standard publicly reported measure, like Adverse Drug Events. However,
these four lists provide “signals of concern” and the measures on these lists include the five Hospital
Associated Infections (HAIs) that Covered California has focused on. The greater the number of “low
performance” lists a hospital appears on, the greater the concern. These lists are not yet publicly
reported but have been provided to insurers for use in hospital negotiations. Insurers are responsible to
notify Covered California which if any of these hospitals will be excluded from their networks or reasons
for continued inclusion by year-end 2020.
Covered California’s requirements for hospital quality and safety serve as a foundation for which health
insurance companies can build networks based on value. As such, the requirement for excluding
“outlier poor performers” and describing the factors they use to select hospitals is related to the
requirement for insurers to work with hospitals to improve quality and safety, described in Chapter 11:
Sites and Expanded Approaches to Care.
Assessing Relative Unit Prices and Total Costs of Care
Covered California supports strategies that promote a competitive market with restraint on prices and
provides access to high quality care. Health insurance companies consider a range of processes and
factors when assessing the relative unit prices and total costs of care at the hospital, medical group, or
provider level. Insurer reported data shows that most insurers compared the cost of providers and
hospitals to other similar providers in the market or region when assessing the costs of providers (see
Table 33. Covered California Insurer’s Process and Factors for Assessing Costs of Providers and
Hospitals, 2015, 2017 and 2018). Most insurers also used specific fee schedules or fee schedules
based on a percent of Medicare reimbursement in their contracts with providers. Three health
insurance companies annually adjusted capitation payments to providers and hospitals or paid as a
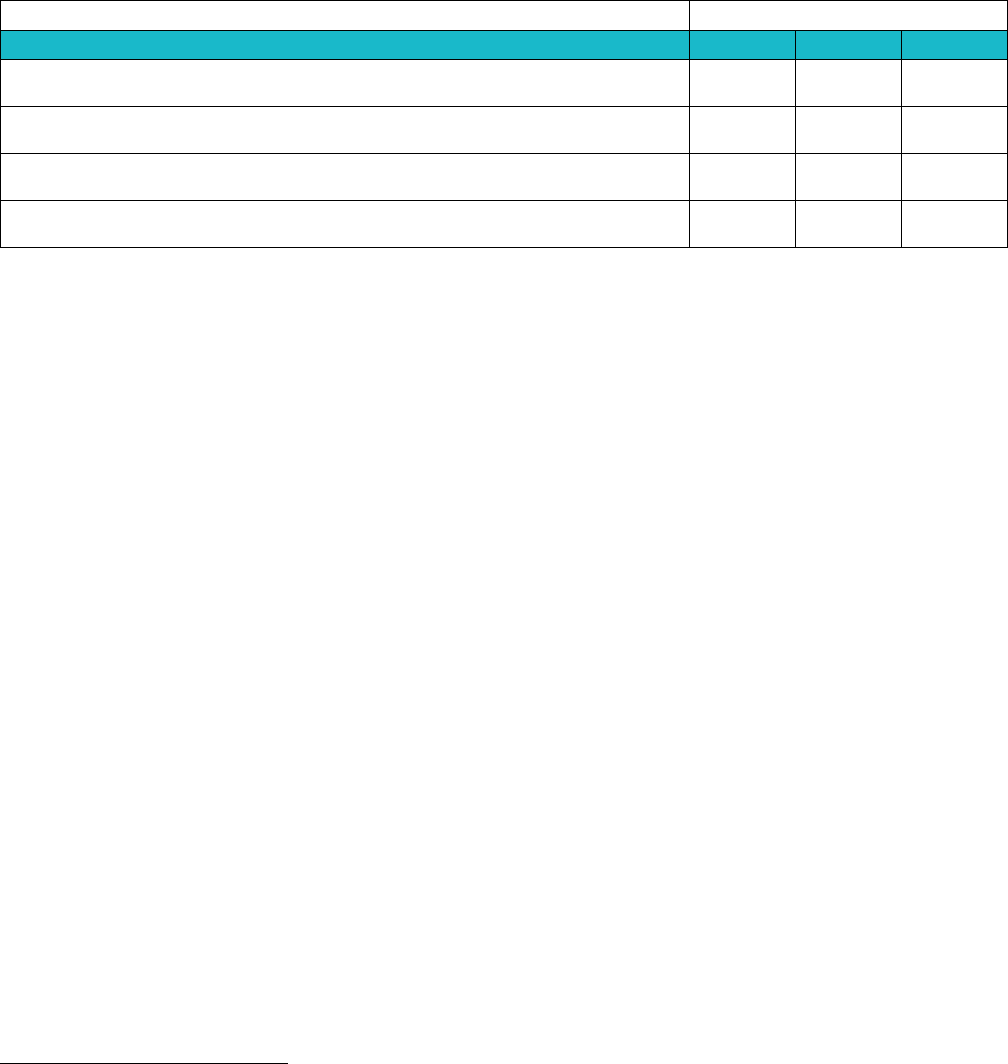
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 9
COVERED CALIFORNIA 78
percent of premium. One insurer used Office of Statewide Health Planning and Development (OSHPD)
data to understand the cost-to-charge ratios of specific hospitals.
Table 33. Covered California Insurer’s Process and Factors for Assessing Costs of Providers and
Hospitals, 2015, 2017 and 2018
62
Number of Health Plans
Process and Factors Used
2015
2017
2018
Compare the cost of providers and hospitals to other similar providers in
the market or region
9
9
9
Use specific case rates, fee schedules or fee schedules based on a
percent of Medicare reimbursement when contracting with providers
7
8
8
Annually adjust payments to providers and hospitals or pay as a percent of
premium
3
3
3
Use Office of Statewide Health Planning and Development data to
understand the cost-to-charge ratios of specific hospitals
1
1
1
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Section 2: Implications for the Future
Covered California holds health insurance companies accountable to manage variation across their
networks in addition to reporting overall quality measures which reflect averages. In managing
variation, enrollees should be assured that any provider they go to for care will meet high standards for
quality and cost management. Variation in hospital performance was a first target since performance is
publicly reported for several key safety measures. Insurers joined Covered California in focusing on a
common set of measures in hospital performance evaluation and contracting. As reported in Chapter
11, this effort has led to improvements in hospital quality and safety. Covered California plans to
continue to work with insurers, other purchasers, hospitals and other stakeholders to assess what can
be done to establish common summary quality and cost hospital performance indicators that would
appropriately be used for purposes of either targeting hospitals for improvement or exclusion from
Covered California networks.
Covered California is also partnering with the Integrated Healthcare Association’s (IHA) California
Regional Health Care Cost and Quality Atlas to profile insurer’s physicians and physician organization
networks based on the wide variation in clinical quality, satisfaction, and total cost of care across the 19
Covered California regions by insurance type. Covered California encourages insurers to use the IHA
Atlas data to profile their networks by displaying the cost and quality of physician organizations and
physicians that serve HMO, EPO and PPO enrollees. Covered California is working with other
purchasers, insurers, physician organizations and other stakeholders to define or create a standard for
low-quality and high-cost physician organizations that could be the basis for targeted improvement or
removing such physician organizations from their networks. As with variation in hospital networks, the
first priority will be to seek ways to align efforts to improve care.
62
Data only available for plan year 2015 and plan year 2017-18. Covered California did not ask this question in the Certification Application
for plan year 2016.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 79
Chapter 10: Appropriate
Interventions
Appropriate Interventions include examining
clinical interventions, such as prescription and
nonprescription pharmaceutical treatments,
procedures (like surgery), diagnostic tests (lab
tests, X-rays, MRIs, etc.) and devices (like
implants and pacemakers), to ensure they are
rooted in the Institute of Medicine’s six aims for
ensuring every individual’s care is safe, timely,
effective, efficient, equitable, and patient-
centered.
63
Equally important is effective
consumer and patient engagement that (1)
supports consumers in making decisions about
health care services, treatments, and providers
that are consistent with their values and
preferences and (2) fosters access to care.
Appropriate Interventions is an expansive topic,
but this chapter, focuses on the following: (1)
pharmacy utilization management; (2) consumer
and patient engagement, which includes the use
of cost transparency tools and shared decision-
making; (3) addressing overuse of care through
Smart Care California; and (4) appropriate use of
services, as measured through standard
measures in the Marketplace Quality Rating
System.
This chapter on Appropriate Interventions is
organized as follows:
Section 1. Qualified Health Plan Experience
Section 2. Health Plan Measures Reported to
the Marketplace Quality Rating System
Section 3. Implications for the Future
Section 1. Qualified Health Plan Experience
Qualified Health Plan Experience presents performance data reported by health insurance companies
for contract requirements and includes assessments and observations by Covered California.
63
Committee on Quality Health Care in America, Institute of Medicine. (2001). Crossing the quality chasm: a new health system for the 21st
century. Washington, D.C.: National Academy Press.
• In 2018, ten insurers considered value in
pharmacy formulary management and ten
insurers used at least one third-party value
assessment methodology (e.g. ICER Value
Assessment Framework).
• All health insurance companies use a
systematic, evidence-based process for
monitoring off-label use of
pharmaceuticals.
• Virtually all of Covered California enrollees
have access to cost transparency tools to
assist consumer decision making about
treatments or procedures (ten of 11
insurers covering 99 percent of enrollees).
• Insurers are approaching completion of
implementation of many of the
recommended Smart Care California
improvements to reduce opioid overuse
including limiting the quantity of tablets in
first prescriptions, removing barriers to
medication-assisted treatment and drugs
used to reverse overdoses. This
collaborative work with other California
state purchasers has contributed to
reduced opioid prescribing and increased
prescribing for buprenorphine, the leading
medication to treat opioid disorders.
• Covered California is continuing to expand
the scope and nature of its efforts to reduce
waste and assure patients are only getting
medically necessary care.
Highlights
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 80
Pharmacy Utilization Management
One component of appropriate interventions is the appropriate use of prescriptions and how health
insurance companies consider cost and quality in determining their drug lists or formularies. Drug costs
continue to increase at a higher rate than other health care costs for generics, name brands and
specialty drugs across all insurance markets. Health insurance companies can put downward pressure
on drug spending through a variety of mechanisms. Covered California requires insurers to describe
ways they are working to achieve value in drug spending, ranging from formulary decision making to
decision support tools. Covered California collects information on health insurance company activities
to inform its analysis of the relative efficacy of different strategies. As part of contract requirements on
achieving value in prescription drug spend, insurers annually report the following:
1. How they currently consider value in formulary selection;
2. If independent value assessment methodologies are used, which ones are used;
3. If and how construction of formularies is based on total cost of care;
4. If and how off-label use is monitored; and
5. The extent of decision support provided to prescribers and members.
Because insurers reported information in a narrative format, further data would be needed to assess
the effectiveness and impact of their activities, which may be facilitated by the addition of cost data to
the information currently submitted by insurers to Covered California.
Ten of 11 health insurance companies considered value in pharmacy formulary management in 2018
(see Table 34. Covered California Insurer’s Consideration of Value in Formulary and Value Assessment
Methods, 2017 and 2018). Nine insurers described the use of a value assessment methodology as part
of their Pharmacy and Therapeutics (PandT) Committee, which all insurers are required to use.
Health insurance companies also report on the use of the following third-party value assessment
methodologies:
• Drug Effectiveness Review Project (DERP)
• NCCN Resource Stratification Framework (NCCN‐RF)
• NCCN Evidence Blocks (NCCN‐EB)
• ASCO Value of Cancer Treatment Options (ASCO‐ VF)
• ACC/AHA Cost/Value Methodology in Clinical Practice Guidelines
• Oregon State Health Evidence Review Commission Prioritization Methodology
• Premera Value‐Based Drug Formulary (Premera VBF)
• DrugAbacus (MSKCC) (DAbacus)
• The Institute for Clinical and Economic Review (ICER) Value Assessment Framework (ICER‐
VF)
• Real Endpoints
• Blue Cross/Blue Shield Technology Evaluation Center
• International Assessment Processes (e.g., United Kingdom’s National Institute for Health and
Care Excellence (NICE))
Eight of 11 insurers used at least one third-party value assessment methodology as part of its PandT
Committee process in 2018. Seven insurers consider value assessment in formulary tier placement.
Health insurance companies use one of several different independent value assessment methodologies
listed, but the Institute for Clinical and Economic Review (ICER) assessment is the most commonly
used. ICER is considered to have a strong methodology compared to others and emphasizes
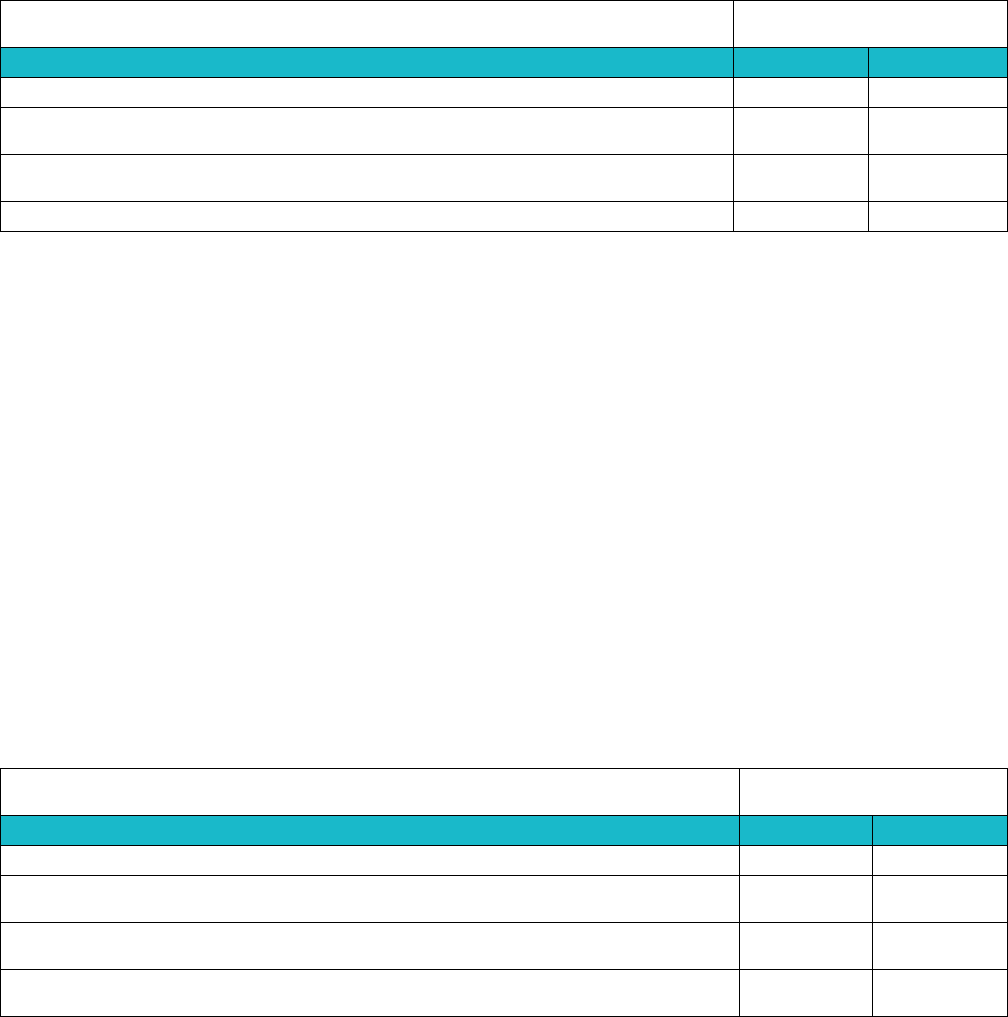
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 81
transparency, conflict-free funding, and actionable activities for plans that consider the total cost of
care. ICER also includes a framework for evaluating short and long-term budget impacts, and includes
a “value-based price benchmark,” reflecting how each drug should be priced to appropriately reflect
long-term improved patient outcomes.
Table 34. Covered California Insurer’s Consideration of Value in Formulary and Value Assessment
Methods, 2017 and 2018
Number of
Health Plans
Consideration of Value
2017
2018
Consider value in pharmacy management
9
10
Use value assessment methodology as part of Pharmacy and Therapeutics
(PandT) process
6
9
Use at least one third-party value assessment methodology
(e.g. ICER Value Assessment Framework)
10
8
Consider value assessment in formulary tier placement
7
7
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
For constructing formularies based on the total cost of care, seven of 11 insurers used a process for
analyzing drug efficacy in context of total cost of care and outcomes (see Table 35. Covered California
Insurer’s Consideration of Total Cost of Care in Formulary, Off-Label Use Monitoring and Decision
Support for Providers and Consumers, 2017 and 2018).
All 11 health insurance companies engaged in systematic, evidence-based process for monitoring off-
label use of pharmaceuticals, which reflects state law requirements for using nationally recognized
sources for evidence-based off label monitoring.
In 2018, nine of 11 insurers provided member-specific decision support for both prescribers and
consumers, of which seven provided this support at the point-of-care. Several new software products
have recently become available and are now being used by Covered California’s insurers to allow
physicians to see pricing information on drugs they are prescribing and the availability of cheaper,
equally effective alternatives. Examples of these software tools include Gemini Health’s Drug-Cost
Transparency Service, Sure Scripts Real-Time Prescription Benefit, and OptumRx’s PreCheck
MyScript.
Table 35. Covered California Insurer’s Consideration of Total Cost of Care in Formulary, Off-Label Use
Monitoring and Decision Support for Providers and Consumers, 2017 and 2018
Number of
Health Plans
Consideration of Total Cost of Care
2017
2018
Analyze drug efficacy in context of total cost of care and outcomes
7
7
Use a systematic, evidence-based process for monitoring off-label use of
pharmaceuticals
11
11
Offer member-specific decision support initiatives for both the prescriber and
consumer, including point-of-care support software
5
7
Offer member-specific decision support initiatives for both prescriber and
consumer, but not at the point of care
1
2
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
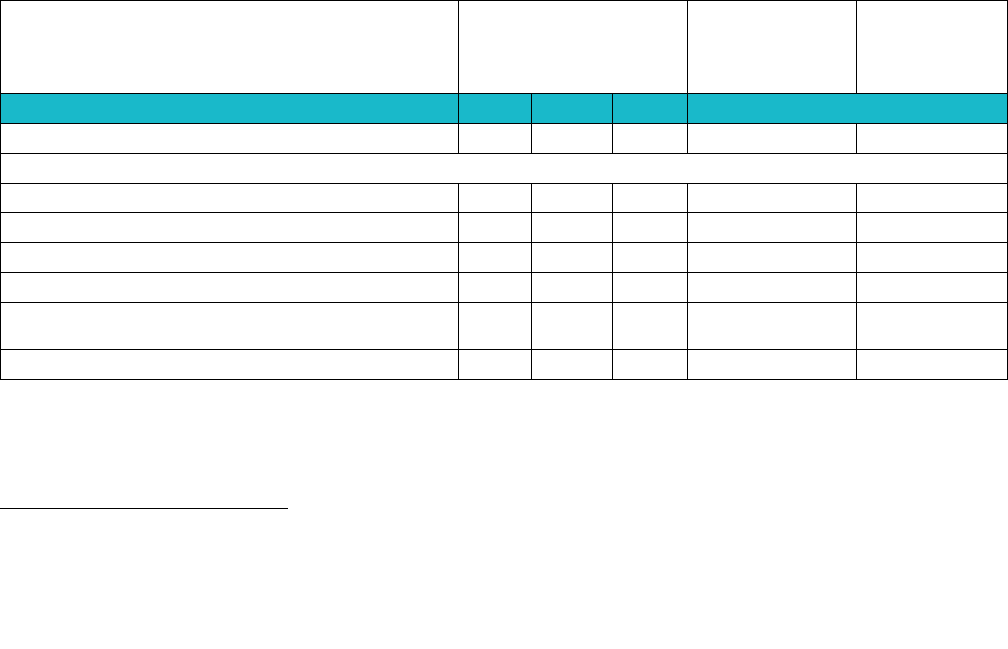
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 82
Consumer and Patient Engagement
Cost Transparency Tools
Covered California supports strategies that promote a competitive market with restraint on prices and
provide access to high quality care. As part of its requirements for demonstrating action on high cost
providers, Covered California required insurers to report on their efforts to make variation in provider or
hospital cost transparent to consumers and the use of cost transparency tools by consumers.
64
Cost
transparency tools have the potential to reduce costs by enabling patients to switch to lower priced
providers and publicly acknowledging high-priced providers which could lead to these providers
reducing their prices.
65
Covered California required health insurance companies with more than 100,000 enrollees to deploy
online tools and 10 of the 11 insurers now do so, representing 99 percent of Covered California
enrollees. Table 36. Covered California Insurer’s Use of Cost Transparency Tools, 2015, 2017 and
2018 describes the number of insurers that use cost transparency tools, what services are provided,
and the percentage of enrollees with access to each type of tool.
As of 2018, the tools offered to the
most enrollees were Online Procedure and Treatment Cost Estimators, which were available through
three different health plans to about 70 percent of enrollees. Other tools include Provider-Specific Cost
Information which three health plans provide to about 21 percent of enrollees.
Table 36. Covered California Insurer’s Use of Cost Transparency Tools, 2015, 2017 and 2018
66
Number of Insurers
Number of
Enrollees with
Access to Tool
Percent of
Total
Enrollment
(1,384,030)
2015
2017
2018
2018
Insurers Offering Cost Transparency Tools
6
9
10
1,371,720
99%
Services Offered
Online Cost and Quality Tool
1
1
1
67,070
5%
Provider-Specific Cost Information
2
2
3
289,460
21%
Online Procedure and Treatment Cost Estimator
3
3
3
974,780
70%
Online Drug Cost Lookup Tool
1
5
5
706,140
51%
Online Real-time Tracking of Out-of-Pocket
Costs
3
6
7
1,218,270
88%
Planning to add Cost Information Online
3
2
0
N/A
N/A
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
The consumer utilization of available tools varied widely among Covered California’s contracted health
insurance companies. The tools available to the largest number of enrollees were used by 3 percent to
64
Network design and reference pricing are also strategies in this requirement. Network design is discussed in Chapter 9: Networks Based
on Value in the sections on provider and facility selection criteria. No insurers reported using reference pricing, which would require
Covered California making changes to its standard benefit design.
65
Mehrotra, Ateev. "Defining the Goals of Health Care Price Transparency: Not Just Shopping Around." NEJM Catalyst, June 26 (2018).
66
Data only available for plan year 2015 and plan year 2017-18. Covered California did not ask this question in the Certification Application
for plan year 2016.
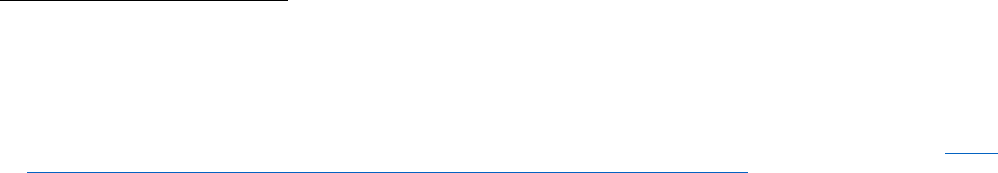
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 83
7.5 percent of consumers. There are not standard national benchmarks to assess the volume and type
of consumer utilization of cost transparency tools, so Covered California is in the process of
determining how best to assess what volume and type of utilization best meets consumers’ needs.
While there is growing research on how best to effectively engage consumers in their care, discussions
about value should both educate consumers and help them work with their providers to make better
choices to align their preferences and likely outcomes.
67
However, there are currently no standard
benchmarks related to use of consumers tools and definitions of the types of users. Similarly, there are
multiple definitions for consumer engagement, with all assuming that consumers have the knowledge
and skills to understand and participate in the engagement process.
68
Covered California is reviewing
these issues and the available evidence to inform future contract expectations.
Shared Decision-Making
There is clear evidence that for many “preference-sensitive” conditions, clinicians do not regularly elicit
patients’ preferences or provide information to support informed patient decision-making. Too often
variation in care tracks with provider preferences rather than those of patients. Shared decision-making
engages patients in bringing their values and preferences to bear often with the help of decision aids
that present the basic science of the condition being treated, the various options for treatment and the
tradeoffs such as quality or length of life. Shared decision-making is designed for preference-sensitive
conditions, such as breast cancer, prostate cancer, and knee and hip replacements where more than
one evidence-based treatment is available or where the evidence is incomplete or uncertain. Variation
in treatment of these conditions based on patient preferences is important and the Covered California
contract requirements included reporting how insurers support shared decision-making including the
proportion of patients with preference sensitive conditions who have used a decision aid.
The requirement for health insurance companies to report on shared decision-making was put on hold
to enable health insurance companies to focus on cost and quality tools and implement the Smart Care
initiatives described below. Based on Covered California’s ongoing discussions with insurers, several
have contracts with vendors that publish decision aids and are using them in case management.
Evidence documents that when patients use decision aids to support shared decision-making with their
clinician at the time and place decisions are made, their knowledge of their options improves, and they
feel better about what matters to them.
69
There are a variety of vendors for decision aids which vary in
quality and evidence supporting their effectiveness. Each insurance company and many medical
groups have made their own vendor selections and therefore offer different tools. None has achieved
implementation at scale and it’s unlikely they will with this diversity. Covered California has an
opportunity over the next several years to work with stakeholders across the delivery system to
consider selecting a single vendor and to support broad adoption of shared decision-making at the
point of care.
67
S, Delbanco, T. Delbanco, Technology and Transparency: Empowering Patients and Clinicians to Improve Health Care Value, Ann Intern
Med. 2018;168(8):585-586.
68
Hibbard JH. (September 2017). Refining Consumer Engagement Definitions and Strategies. Journal of Ambulatory Care Management.
69
The most current best evidence is documented in Chapter 9: Appropriate Interventions of a companion Covered California report, Current
Best Evidence and Performance Measures for Improving Quality of Care and Delivery System Reform.
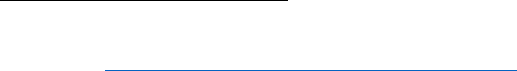
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 84
Addressing Overuse of Care through Smart Care California
In 2015, Covered California joined the other state purchasers, the Department of Health Care Services
(DHCS) and the California Public Employees’ Retirement System (CalPERS), to form a multi-
stakeholder workgroup called Smart Care California to address overuse of services that result when
evidence-based practices are not being followed. This multi-stakeholder work group is facilitated by the
Integrated Healthcare Association (IHA), with funding and thought leadership from the California Health
Care Foundation (CHCF). Smart Care California selected three areas of focus from the list of Choosing
Wisely guidelines published by the American Board of Internal Medicine Foundation in cooperation with
other specialty societies: (1) low-risk (nulliparous term, singleton, vertex (NTSV)) deliveries performed
without medical indication; (2) opioid overuse and misuse; and (3) imaging for low back pain.
70
Health insurance companies are invited to participate in the development of improvement strategies
and are required to adopt the guidelines developed by Smart Care California. All insurers are
participating either as regular attendees or by implementing guidelines published by Smart Care
California. Work is underway for adopting best practices for payment for maternity services as well as
for combatting the opioid crisis. At this time, Smart Care has focused on these two areas, while overuse
of imaging for low back pain, which would entail a large-scale effort to change the care patterns of
thousands of physicians across California, has been on hold while resource and other implementation
challenges are considered. The measure for imaging for low back pain will still be collected in
Marketplace QRS and other quality measurement programs.
Health insurance companies’ efforts to reduce low-risk C-section deliveries are impacting the entire
maternity population served at each plan’s network hospitals, not just Covered California’s enrolled
population. In addition, Covered California, DHCS, and CalPERS are collaboratively engaged in efforts
to reduce low-risk C-sections, so the same initiatives are positively impacting their hospitals and care
regardless of the source of the consumer’s coverage. Further discussion of efforts to reduce low-risk C-
sections is included in Chapter 11: Sites and Expanded Approaches to Care Delivery.
Smart Care California Efforts to Reduce Opioid Overuse
The Smart Care California work group has surveyed health insurance companies on their efforts to
reduce opioid overuse in four categories: (1) preventing new starts; (2) managing pain safely; (3)
treating addiction; and (4) stopping death. Comparison of performance in these areas are based on
aggregated survey data from Covered California, CalPERS and DHCS is provided in Figure 9. Smart
Care California Purchaser Level Performance on Opioid Overuse Reduction, 2018. Covered California
insurers are approaching completion of implementation for many of the recommended improvements
including limiting the quantity of tablets in first prescriptions, removing barriers to medication-assisted
treatment and for drugs used to reverse overdoses. The table below reflects remarkable improvement
as none of these recommendations were practices before Smart Care California published their
guidelines. This survey will continue to be conducted annually.
According to the Smart Care survey, all 11 Covered California insurers now implement quantity limits
for new starts of opioids and nine Covered California insurers have removed prior authorization for
physical therapy for back pain, improving timely patient access to care and preventing new starts of
opioid medications. The survey also indicates that more than half of insurers have increased access to
70
See more: https://www.iha.org/our-work/insights/smart-care-california.
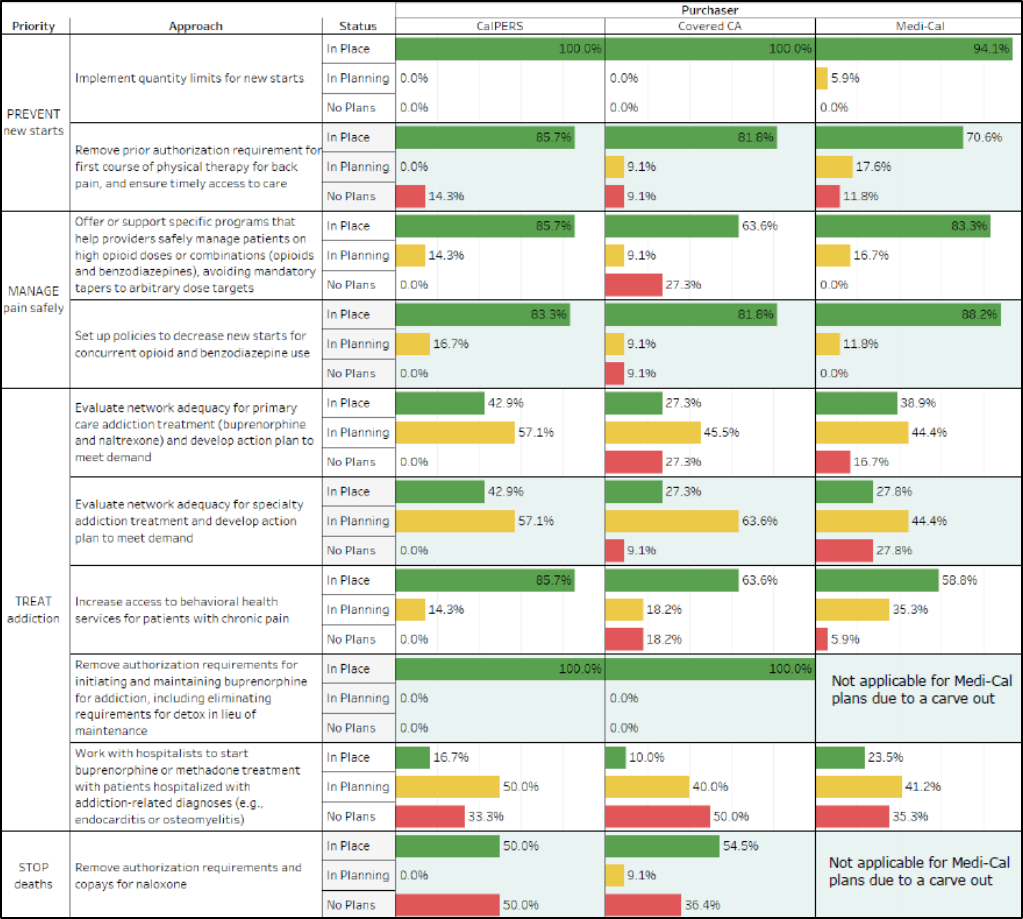
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 85
behavioral health services for patients with chronic pain, while two insurers are in the planning stages
to increase access. These improvements have the potential to greatly aide in curbing the opioid
epidemic in the state.
Figure 9. Smart Care California Purchaser Level Performance on Opioid Overuse Reduction, 2018
Source: Smart Care California, 2019
As seen below in Figure 10. California 2010-2018 Progress on Opioid Overuse Reduction, prescribing
for opioids is falling and prescribing for buprenorphine, the leading medication to treat opioid disorders,
is rising. But overdose deaths remain high. The reason overdoses are still such a threat appears to be
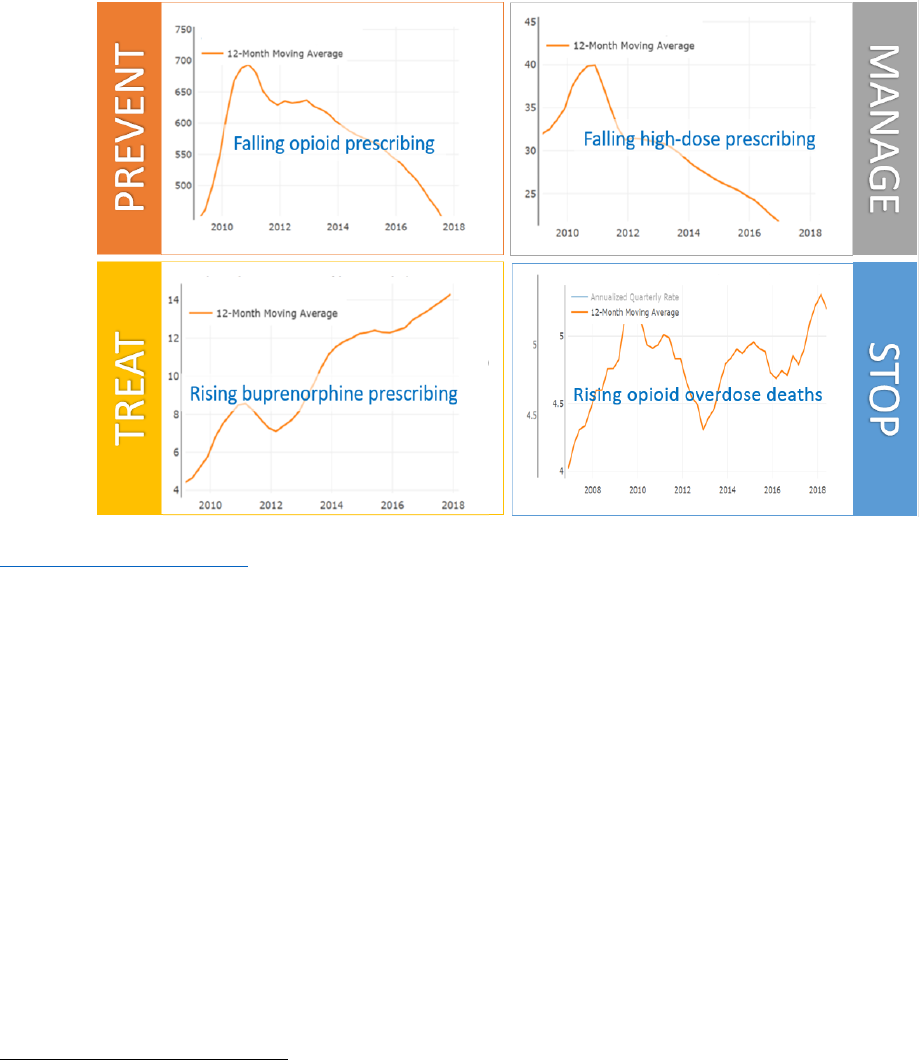
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 86
that street drugs are replacing prescription drugs as the cause of death.
71
This data implies that neither
California or the nation has found the right balance for treating opioid addiction. Opioid prescriptions
appear to have fallen faster than capacity for treatment has expanded.
Figure 10: California 2010-2018 Progress on Opioid Overuse Reduction
Source: California Health Care Foundation analysis of data from the California Department of Public Health
www.cdph.ca.gov/opioiddashboard
Much more needs to be done to support providers in reducing opioid prescriptions safely including
expanding access to medication assisted treatment. While efforts to address the opioid epidemic have
benefited from many sectors focusing needed attention on this problem, Covered California believes
the Smart Care initiative is an example of how improvement can be encouraged when major
purchasers — in this case Medi-Cal, CalPERS and Covered California — align to work with insurers
and providers to meet a common clinical need. Additionally, Covered California is more closely tracking
opioid use and medication assisted treatment use through its Healthcare Evidence Initiative database.
Section 2: Health Plan Measures Reported to the Marketplace Quality
Rating System
Health Plan Measures Reported to the Marketplace Quality Rating System details health plan
performance on Healthcare Effectiveness Data Information Set (HEDIS) and Consumer Assessment of
Healthcare Providers and Systems (CAHPS) measures reported to the Centers for Medicaid and
Medicare Services’ Quality Rating System (QRS). These standard performance measures are a key
mechanism used by Covered California for health plan oversight and accountability.
71
The New York Times, “Short Answers to Hard Questions About the Opioid Crisis”, Josh Katz, August 10, 2017
https://www.nytimes.com/interactive/2017/08/03/upshot/opioid-drug-overdose-epidemic.html.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 87
See Appendix 2: Additional Health Plan Measures Reported to the Quality Rating System, for six
Quality Rating System measures that pertain to Appropriate Interventions:
1. Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis (Table A23)
2. Appropriate Testing for Children with Pharyngitis (Table A24)
3. Appropriate Treatment for Children with Upper Respiratory Infection (Table A25)
4. Use of Imaging Studies for Low Back Pain (Table A26)
5. Annual Monitoring for Patients on Persistent Medications (Table A27)
6. Access to Information (Table A28)
These measures address the both the overuse of low value services and the appropriate use of
services. The first three measures above reflect efforts to reduce overuse of antibiotics which is
resulting in wide spread resistance to potentially lifesaving treatment.
Imaging for low back pain, especially CT and MRI scans, should only be used when considering
surgery for intractable pain or neurologic complications related to low back pain.
Many patients with conditions like rheumatoid arthritis are on complex medications with potential side-
effects. Standard routine monitoring, as measured by Annual Monitoring for Patients on Persistent
Medications, may be overlooked if not tracked and implemented systematically.
As detailed under the section on shared decision-making, supporting patients with the right information
to partner with their providers to decide on appropriate interventions for their care is critical not only for
preference sensitive care but to increase adherence to evidence-based care.
Section 3: Implications for the Future
There is good evidence that a very high proportion of care delivered is unwarranted or delivered poorly;
some diagnostic tests are overused, and there is limited information available to assess relative efficacy
and value of many drugs, devices and even some surgical interventions. Genetic testing is starting to
show value in guiding clinical decisions and “personalized” approaches to cancer care are being
developed and tested. All these innovations come with extraordinary costs and only preliminary
understanding of which patients will benefit the most.
Shared decision making requires that there is active and transparent information sharing between
consumers and their providers. Cost and quality tools provide consumers with the knowledge to better
engage with their own health decision making, but even among the tools that are available today there
is little success engaging patients or providers in their adoption. Future improvements in technology
and data sharing will lead to better consumer engagement. Covered California is continuing to monitor
insurers to ensure that consumers are being provided the most reliable tools and information so that
they can receive the best care at the right time. Covered California has an opportunity over the next
several years to work with stakeholders across the delivery system to consider selecting a single
vendor and to support broad adoption of shared decision-making at the point of care.
Over the next few years, a wide range of innovations in care delivery will have dramatic impacts on how
care is provided, and the quality and cost of that care. Covered California has shown how purchasers,
payers and providers can work together in adopting best practices to reduce variation in hospital
performance and address overuse of opioids. Decision support to providers and patients at the point of
care is particularly promising, whether through consumer cost tools integrated with the medical record,
shared decision-making decision aids or point of care software integrated with electronic health record
order entry to support adherence to formularies, bringing this information to where decisions are made
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 10
COVERED CALIFORNIA 88
appears to be critical to successful adoption. Covered California is assessing the extent to which its
contractual requirements can assist in prioritizing and standardizing implementation of best practices to
benefit all Californians.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 89
Chapter 11: Sites and Expanded
Approaches to Care Delivery
Covered California is better understanding and
promoting evidence-based health interventions and
treatments beyond the traditional physician office
and hospital-based care, whether on an inpatient or
outpatient basis: urgent care facility, retail facilities
such as drop-in clinics, at home, or through a variety
of emerging telehealth strategies. Expanded
approaches to care delivery also includes who
provides care in addition to physicians including
clinically appropriate providers such as registered
nurses, pharmacists, midwives, nurse practitioners,
physician assistants or non-licensed providers like
community health workers.
This chapter on Sites and Expanded Approaches to
Care Delivery has a different organization. “Sites”
refer to the traditional medical care settings of
hospitals and physician offices. Care in physician
offices is covered in Chapter 7: Promotion of
Effective Primary Care, while Chapter 10:
Appropriate Interventions, examines various clinical
interventions largely delivered in or ordered by
physician offices, to ensure they are rooted in the
Institute of Medicine’s six aims for safe, timely,
effective, efficient, equitable and patient-centered
care.
72
Hospital care is a broad topic and can include a
range of system level reforms. This chapter focuses
on publicly reported performance data that health
insurance companies are using to establish contract
requirements for hospital quality and safety, which
are (1) within an insurer’s oversight authority; (2)
help foster alignment across contracted insurers and
their contracted hospitals; and (3) benefit from the
availability of publicly reported hospital performance
data reflecting the experience of the hospital’s entire
patient population. Covered California has worked
with hospitals and the California Hospital Association
to select measures for which coaching programs,
72
Committee on Quality Health Care in America, Institute of Medicine. (2001). Crossing the quality chasm: a new health system for the 21st
century. Washington, D.C.: National Academy Press.
• The California Department of Public
Health reports that as of 2018 there
has been a statistically significant
reduction in major types of hospital
associated infection rates in California
hospitals (CLABSI, SSI, MRSA, and C.
difficile bacterial). Covered California’s
contract requirements — aligned with
those of CMS and other purchasers —
insurer engagement, and work with
improvement collaboratives have
contributed to 3,392 infections avoided,
251 lives saved and over $62M in one-
year cost savings.
• Covered California’s support for
appropriate C-Sections helped 56% of
California hospitals achieve the
national goal of NTSV C-section rates
of 23.9% or lower in 2018,
representing a 12-point improvement
from 2015, avoiding 7,200 C-sections
over 3 years.
• The number of insurers that
participated in the Smart Care
California collaborative, increased from
six to all 11 by 2017 with full
participation continuing since then.
Similarly, the number of insurers that
participated in Partnership for Patients
collaborative increased from two to ten
insurers between 2016 and 2018.
• For insurer engagement of network
hospitals, 10 insurers were assessed
as having Full Engagement or
Engaged for hospital safety in 2018.
For maternity care, all 11 insurers were
assessed as Full Engagement or
Engaged for maternity care in 2018.
Highlights
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 90
quality collaboratives and change packages are available and aligned with priorities established by
national consensus including CMS and Healthy People 2020.
For expanded approaches to care delivery, current requirements pertaining to (1) telehealth and (2)
Centers of Excellence are discussed, while Covered California has not developed reporting or contract
requirements related to many of the existing and evolving sites of care or approaches.
Qualified Health Plan Experience
For hospital quality and safety, Covered California has the following requirements of contracted
health plans:
73
1. Encouraging hospital participation in quality improvement collaboratives and coaching programs
2. Reducing the avoidable hospital associated infections (HAIs) starting with the metrics included
in the CMS Hospital Acquired Condition Reduction Program (HACRP)
a. Catheter associated urinary tract infection (CAUTI)
b. Central line associated blood stream infections (CLABSI)
c. Methicillin-resistant Staphylococcus aureus (MRSA)
d. Clostridioides difficile (formerly Clostridium difficile bacterial infection) (CDI)
e. Surgical site infection of the colon (SSI Colon)
3. Reducing low-risk, nulliparous term singleton vertex (NTSV) C-section rates to 23.9 percent or
lower (a national Healthy People 2020 goal);
74
4. Expanding value-based payments for hospital quality and maternity care including:
a. Tying two percent of hospital payments to value by the end of 2019
b. Eliminating financial incentives for hospitals or physicians to perform C-Sections; and
5. Excluding a hospital from their network initially by year-end 2020 if the hospital is an outlier poor
performer and not working to improve safety and maternity care.
For expanded approaches to care delivery, Covered California requires health plans to use
technology, including telehealth and remote home monitoring,
75
to assist in higher quality, accessible,
patient-centered care.
Hospital Quality and Safety
Encouraging Hospital Participation in Coaching Programs and Collaboratives
Health insurance companies are required to encourage hospitals to participate in the Partnership for
Patients coaching program, which is funded by the federal Department of Health and Human Services
(HHS) to support designated Hospital Improvement Innovation Networks (HIINs).
76
In California, there
are 5 HIINs which engage individual hospitals and systems to participate in trainings to reduce hospital
associated infections, adverse drug events, falls, pressure ulcers, and other negative health events that
occur in hospital settings.
77
This encouragement can be accomplished through hospital administrator
73
Currently, hospital quality and safety performance are tracked at general acute care (GAC) hospitals, because specialized hospitals (such
as long-term care) have different performance benchmarks and variables to consider.
74
First pregnancy (nulliparous), full term, no twins or beyond (singleton), and head down (vertex) or NTSV pregnancies are generally thought
of as low risk. See more: https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health
75
Telehealth services can include remote monitoring when used for disease management in between visits.
76
See more: https://partnershipforpatients.cms.gov/about-the-partnership/aboutthepartnershipforpatients.html.
77
In California, the five HIINs are: (1) Health Services Advisory Group, which is managed by the Hospital Quality Institute, (2) Dignity, (3)
Vizient (created by the VHA/UHC merger), (4) Children’s Hospitals’ Solutions for Patient Safety, and (5) Premiere Inc.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 91
engagement, letter campaigns to providers, contracting discussions, and other creative means that
communicate the importance and urgency of reducing the incidence of avoidable negative health
events in hospitals.
Covered California also requires insurers to engage with their network hospitals to promote awareness
of (1) NTSV C-section rates, (2) availability of provider and consumer education, and (3) promote
participation in data sharing and coaching offered by the California Maternal Quality Care Collaborative
(CMQCC), with the goal of reducing NTSV C-sections to the national Healthy People 2020 target of
23.9 percent of deliveries or lower. The CMQCC is a multi-stakeholder organization that provides real
time data sharing, quality improvement toolkits, and coaching collaboratives to improve maternal and
neonatal health in several measure areas, including NTSV C-sections. Additionally, Smart Care
California built consensus around a menu of payment structures to promote the goal of ending financial
incentives for providing NTSV C-Sections: (1) blended case rates; (2) low risk C-section reduction as a
metric for payment incentive programs; or (3) population-based payment models.
78
As shown in Table 37. Covered California Insurer Participation in Improvement Collaboratives, the
number of insurers that participated in Smart Care California increased from six to 11 between 2016
and 2017 and this trend of full participation continued through 2018. Similarly, the number of insurers
that participated in Partnership for Patients increased from two to ten health plans between 2016 and
2018.
Table 37. Covered California Insurer Participation in Improvement Collaboratives
79
Collaborative
2016
2017
2018
Smart Care California
Focuses on outreach to reduce NTSV C-Sections through
collaboration with California Maternal Quality Care Collaborative
6
11
11
Partnership for Patients
U.S. Department of Health and Human Services program that
focuses on reducing infections in hospitals
2
10
10
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Health insurance companies have engaged network hospitals on the importance of reducing hospital
associated infections and NTSV C-sections and are spreading awareness of ways that performance
can be improved, such as coaching programs through Partnership for Patients funded HIINs and
CMQCC. Insurer activities range from sending tailored mail to hospitals, physicians and administrative
staff, tracking measures and discussing performance in regular hospital quality meetings or contract
renewal meetings, including participation in coaching programs as a metric in hospital incentive
programs, hosting webinars, adjusting website content for members and providers, and visiting
hospitals to distribute materials.
As summarized below (Table 38. Covered California Insurer Engagement with Network Hospitals),
Covered California assessment of insurer engagement activities with hospitals on improving quality
78
Smart Care California. October 2017. Aligning Birth Payment to Reduce Unnecessary C-Section.
http://www.iha.org/sites/default/files/files/page/c-section_menu_of_payment_and_contracting_options.pdf
79
Covered California did not ask the specific collaborative participation question in 2019 QHP Certification Application (reported in 2018).
The year in these tables refers to the year the information was submitted by the insurer to Covered California, so it may refer to activities in
the previous year or in the first quarter of that year. For example, a summary for 2017 likely includes activities from 2016 and the first
quarter of 2017.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 92
found the number of insurers with Full Engagement for hospital safety tripled from three to nine
between 2016 and 2017. As of 2018, 10 insurers had Full Engagement or were Engaged for Hospital
Safety. For maternity care, most insurers have consistently had Full Engagement from 2016 to 2018,
with all plans having Full Engagement or Engaged as of 2018.
Table 38. Covered California Insurer Engagement with Network Hospitals
Hospital Safety
Maternity Care
Assessment
2016
2017
2018
2016
2017
2018
Full Engagement
Active engagement with hospitals in quality
improvement includes best practices to be potentially
shared among health plans.
3
9
8
9
9
8
Engaged
Has initiated engagement with hospitals either through
internal planning or external action.
5
1
2
1
1
3
Minimal Engagement
Has not acted either internally or externally to engage
with hospitals.
3
1
1
1
1
-
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Partly as a result of insurers’ encouragement and other factors, including growing hospital awareness
of Covered California’s focus on outlier poor performance, there is now nearly universal participation in
improvement collaboratives among California’s hospitals. Publicly reported data on hospital
participation in quality improvement programs shows a positive trend over the past four years, with 148
hospitals participating in 2014 to 251 hospitals in 2018 (see Figure A2. California Hospitals Involved in
Hospital Quality Institute Hospital Improvement Innovation Networks, 2014-18 in Appendix 4: Additional
Publicly Reported Hospital Quality and Safety Data). Participation in the five HIIN improvement
programs is near universal, with fewer than ten acute care hospitals in California not participating,
according to the Hospital Quality Institute.
Collectively Reducing Avoidable Hospital Associated Infections
Covered California has focused on aligned and collaborative efforts to promote hospital safety based
on the recognition that improving hospital performance in this area requires a comprehensive and
cross-payer approach.
Every day, about one in 25 hospital patients nationally contracts at least one hospital associated
infection (HAI).
80
These infections can significantly delay recovery, increase the expense of a hospital
stay, and even result in death. Of the approximately two million American patients who acquire a HAI
annually, an estimated 90,000 will die.
81
Before implementation of the Partnership for Patients program,
80
Centers for Disease Control and Prevention. Healthcare-associated Infections. Retrieved from: https://www.cdc.gov/hai/index.html.
81
Stone, P. W. (2009). Economic burden of healthcare-associated infections: an American perspective. Expert review of
pharmacoeconomics and outcomes research, 9(5), 417-422.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 93
it was estimated that HAIs and other avoidable hospital complications were associated with more than
400,000 deaths per year.
82
,
83
Not only are HAIs harmful, they are also a burden on the healthcare system. The cost of a single case
can range from just under $1,000 to nearly $50,000, with costs borne by insurers, employers, and
patients through out-of-pocket expenses.
84
Depending upon the type of infection, the direct cost of HAIs
to hospitals ranges from $28 billion to $45 billion.
85
Measures to track HAIs are readily available through CMS Hospital Compare, California Department of
Public Health (CDPH), and Cal Hospital Compare. Covered California determined the five HAIs to focus
on through consultation with stakeholders and subject matter experts including CDPH, Cal Hospital
Compare, Hospital Quality Institute (a quality improvement center within the California Hospital
Association), Centers for Medicare and Medicaid Services (CMS), insurers, and consumer advocates.
The criteria for selecting these measures were:
• Clinical importance;
• Robust, publicly available performance data;
• Alignment with other purchasers including CMS;
• Wide variation in performance among California hospitals; and
• Availability of coaching collaboratives with change packages to support improvement for free or
minimal cost to hospitals.
Understanding Hospital Performance Variation to Target Quality Improvement Efforts
Covered California assists insurers in understanding hospital performance variation to enable better
targeting of hospitals for engagement and quality improvement. Covered California displays hospital
performance through graphic distributions where every California hospital’s measure score is
represented by a dot, and dots are color coded to denote in- or out-of-network status. The goal of these
graphs is to bring attention to the variation in hospital performance on each HAI and to help insurers
know which hospitals to focus on in their engagement and quality improvement efforts. For example,
below Figure 11. Sample of One Covered California Insurer’s Hospital Associated Infection Incidence
for Catheter-associated Urinary Tract Infection (CAUTI) — In-Network and Out-of-Network Hospitals,
2018 shows the performance of an insurer’s 2018 network for CAUTI standardized infection ratios. The
hospitals identified by blue dots on the right-hand side of the chart represent in-network hospitals for
this insurer that have infection rates above the risk adjusted expected rate. Covered California’s
identification and display of hospital infection rates provides additional information for insurers to use in
their design of networks and in their engagement with hospitals to encourage participation in quality
improvement initiatives.
82
James, J. T. (2013). A new, evidence-based estimate of patient harms associated with hospital care. Journal of patient safety, 9(3), 122-
128.
83
Potentially avoidable errors were grouped into the following categories: 1) errors of commission; 2) errors of omission; 3) errors of
communication; 4) errors of context; and 5) diagnostic errors.
84
Castlight and The Leapfrog Group. (2018). Healthcare-Associated Infections. Retrieved from: https://www.leapfroggroup.org.
85
Ibid.
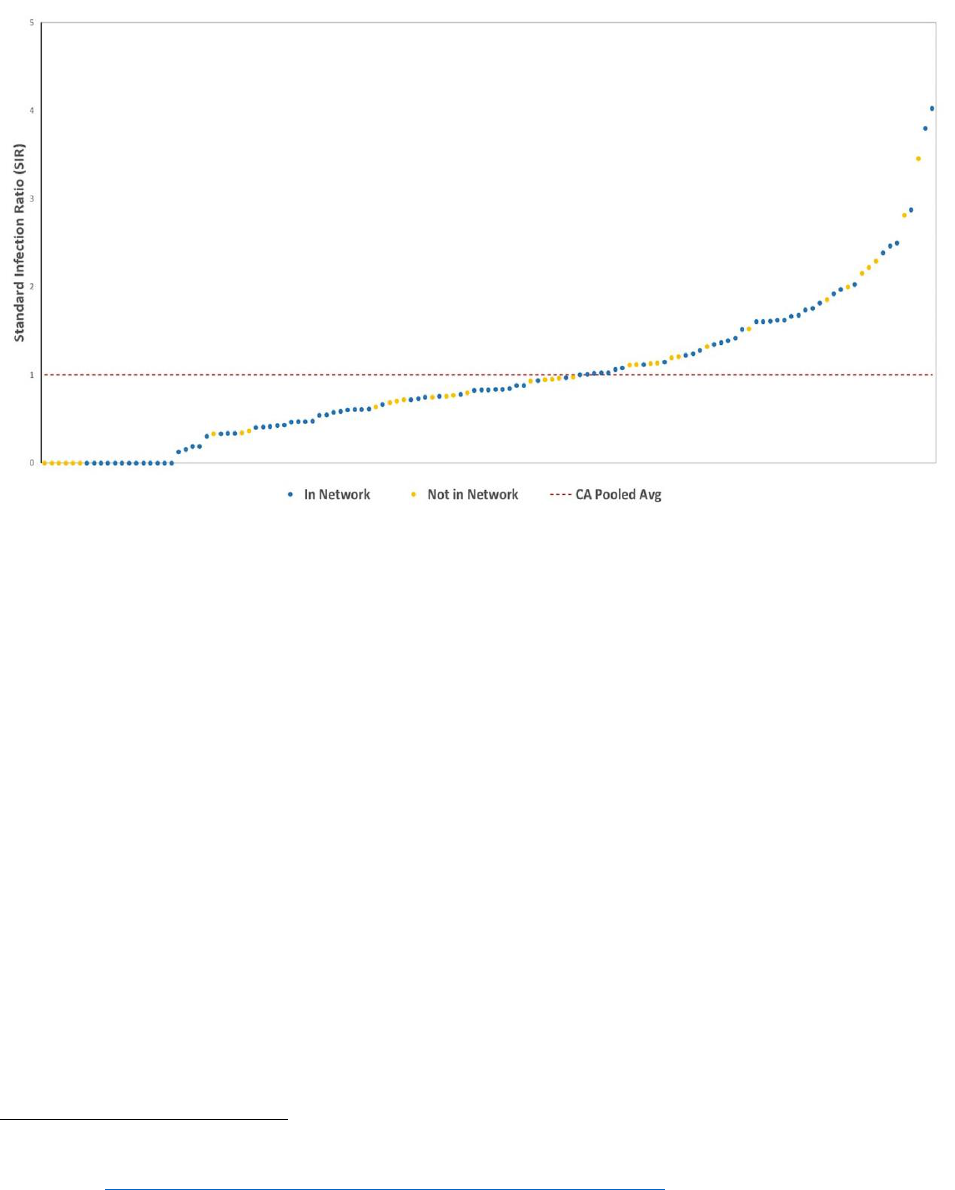
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 94
Figure 11. Sample of One Covered California Insurer’s Hospital Associated Infection Incidence for
Catheter-associated Urinary Tract Infection (CAUTI) — In-Network and Out-of-Network Hospitals, 2018
Source: 2018 Data from Cal Hospital Compare and California Department of Public Health (CDPH).
To develop tailored approaches for targeting network hospitals for improvement, insurers can also
leverage the 2018 HAI reports from CDPH,
86
which list hospitals with better or worse HAI incidence
than the national baseline by county (see Appendix 4: Additional Publicly Reported Hospital Quality and
Safety Data).
Publicly reported data on HAIs are reported at the hospital level, not the insurer level, through CDPH
data on infection rate trends. According to the CDPH, there has been a statistically significant reduction
in CLABSI, SSI, MRSA, and C. difficile bacterial infection rates between 2015 and 2018 (see Figure 12.
Hospital Associated Infection Incidence in California Hospitals, 2015-18).
87
For these four HAI measures, the above chart shows a steady drop over three years, of which C.
Difficile infections were the last to show progress, but as of 2018 has dropped 41 percent since 2015.
The rates are expressed as a ratio of observed over a risk adjusted expected rate based on national
standards. For all infection rates to be falling and for all rates to be below the national expected ratio of
1.0 reflects concerted effort among many stakeholders in California and represents remarkable
progress. CDPH does not include hospital CAUTI information in its analysis.
86
See more: https://www.cdph.ca.gov/Programs/CHCQ/HAI/Pages/AnnualHAIReports.aspx.
87
For additional data, see C. Diff Incidence Rates in California Counties in Appendix 4.
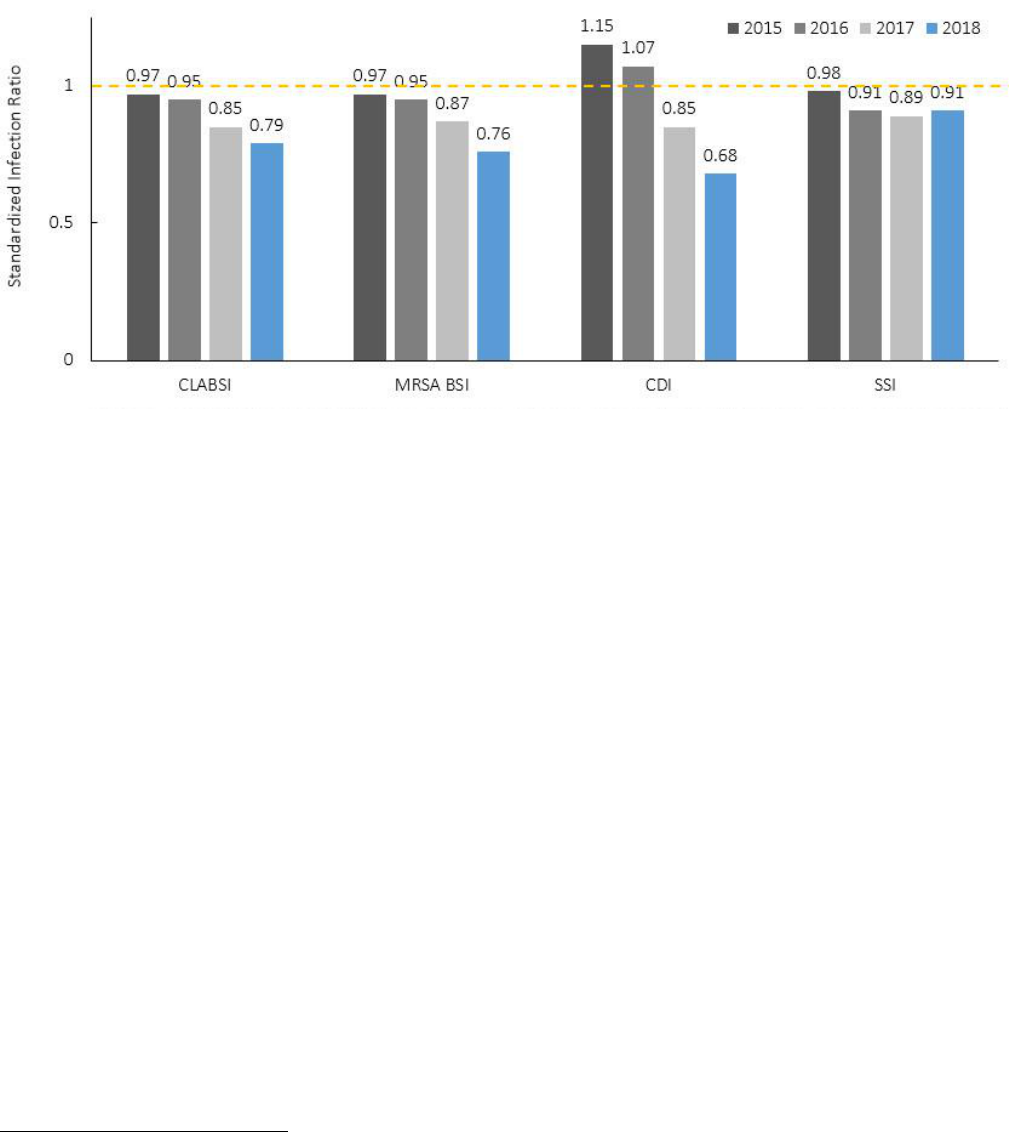
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 95
Figure 12. Hospital Acquired Infection Incidence in California Hospitals, 2015-18
Note: Hospital associated infections are reported as a standardized infection ratio (SIR), a risk-adjusted measure managed nationally that
compares observed versus expected number of complications per year. The dashed line represents an SIR of 1.0. A score of 1.0 means a
hospital has an expected rate while below 1.0 is better and above is worse.
Source: California Department of Public Health. November 2019.
It is challenging to calculate the impact of hospital infections that have been prevented. However, Cal
Hospital Compare, with support from IBM Watson, calculated the mortality rates of hospital associated
infections and the usual costs of caring for those infections based on evidence from the literature. They
have evidence to support this calculation for four of the targeted infections: CLABSI, CAUTI, SSI Colon,
and C. Diff. The result, for the twelve months between October 1, 2017 and September 30, 2018,
compared to April 1, 2016 to March 31, 2017, shows that 3,392 infections were avoided resulting in 251
Californian lives saved and $62 million dollars saved.
It is important to note that Covered California insurer engagement and payment strategy efforts did not
create this improvement alone, but the contract requirements were likely helpful contributors to the
success.
88
Covered California has partnered with existing stakeholder groups and organizations, to
implement hospital quality and safety requirements that include a standard set of metrics and several
common approaches to quality improvement with aligned expectations across 11 health insurance
companies. Prior to 2016, health insurance companies did not find most hospitals receptive to
discussion of quality performance in contract discussions and insurer medical management and
network management teams were traditionally siloed internally. Importantly, under the leadership of the
Hospital Quality Institute, the California Hospital Association has taken a lead in increasing the focus on
quality. Health insurance companies also reported that the alignment of 11 insurers with consistent
message of insurer accountability for variation and a prioritized set of measures has changed the
environment and supported measurable improvement.
88
Of note, these requirements became effective in 2017 but stakeholder discussions on the importance of quality improvement began in
summer of 2015. Some plans began engaging hospitals earlier than 2017 and some as early as summer 2015.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 96
Collectively Reducing Unnecessary C-Sections: Reduce Low-Risk NTSV C-Section
Rates to 23.9 Percent or Lower
C-sections can be life-saving, but significant numbers of healthy first-time mothers are undergoing this
major surgery when it is not medically necessary. Unnecessary C-sections are dangerous for the
mother and baby, increasing the risk of complications such as hemorrhage, infection, transfusions,
blood clots, respiratory complications, and neonatal intensive care unit (NICU) admission.
89
Roughly 90
percent of women with a prior C-Section currently deliver by C-section for future births, leading to
higher risks of additional complications, including placenta previa or accreta and uterine rupture (which
can cause hemorrhage, hysterectomy, or death).
90
Compared to vaginal delivery, babies born by repeat
C-section have higher rates of respiratory morbidity and NICU admission rates resulting in longer
hospital stays and higher medical costs.
91
Covered California holds health insurance companies responsible to manage variation in provider
performance across their contracted networks rather than manage to average performance. To that
end, insurers are required to engage with their network hospitals to promote awareness of (1) low risk
C-section rates, (2) availability of provider and consumer education, and (3) promote participation in
data sharing and coaching offered by the California Maternal Quality Care Collaborative (CMQCC), with
the goal of reducing NTSV C-sections to 23.9 percent of deliveries or lower (as set in the national
Healthy People 2020 goals).
CMQCC gained national attention for contributing to California’s decreasing maternal mortality rates
and now works to reduce NTSV C-sections. Hospital participation in the CMQCC data collection and
improvement collaborative is now nearly universal partly due to insurer encouragement and inclusion in
contracting discussions with hospitals. As of July 2018, nearly 95 percent of California hospital births
occur at hospitals participating in data reporting or collaboratives managed by the Maternal Data Center
(MDC) within the CMQCC (see Figure A3: Percentage of California Hospital Births at CMQCC
Participating Hospitals in Appendix 4: Additional Publicly Reported Hospital Quality and Safety Data).
92
Progress to reduce NTSV C-sections has been substantial between 2015 and 2018. In 2015, the
variation in C-section rates for NTSV deliveries among maternity hospitals in California was enormous,
ranging from 10 to 75.8 percent. Figure 13. Distribution of NTSV C-section Rates for Hospitals that
Reported to the California Maternal Quality Care Collaborative, 2018 shows the range of NTSV C-
section rates for hospitals reporting to CMQCC in 2018. The range was 6.2 to 41.1 percent with an
aggregated rate of 23.3 percent and a median of 23.2 percent, which are both below the Healthy
People 2020 target of 23.9 percent. The absence of the highest outliers signifies substantial change in
maternity practice in the state of California.
89
J. P. Souza et al., “Caesarean Section Without Medical Indications Is Associated with an Increased Risk of Adverse Short-Term Maternal
Outcomes: The 2004-2008 WHO Global Survey on Maternal and Perinatal Health,” BMC Medicine 8 (November 10, 2010): 71,
doi:10.1186/1741-7015-8-71.
90
Smart Care California. (2017). Aligning Birth Payment to Reduce Unnecessary C-Section: A Menu of Options. Retrieved from
http://www.iha.org/sites/default/files/files/page/c-section_menu_of_payment_and_contracting_options.pdf
91
Kamath, B. et al. “Neonatal Outcomes After Elective Cesarean Delivery”. Obstetrics and Gynecology. 113(6):1231-1238, JUN 2009.
92
As of July 2018, 221 of 240 maternity hospitals representing nearly 95 percent of California hospital births occur at hospitals participating
in data reporting or collaboratives managed by the Maternal Data Center (MDC) within the CMQCC.
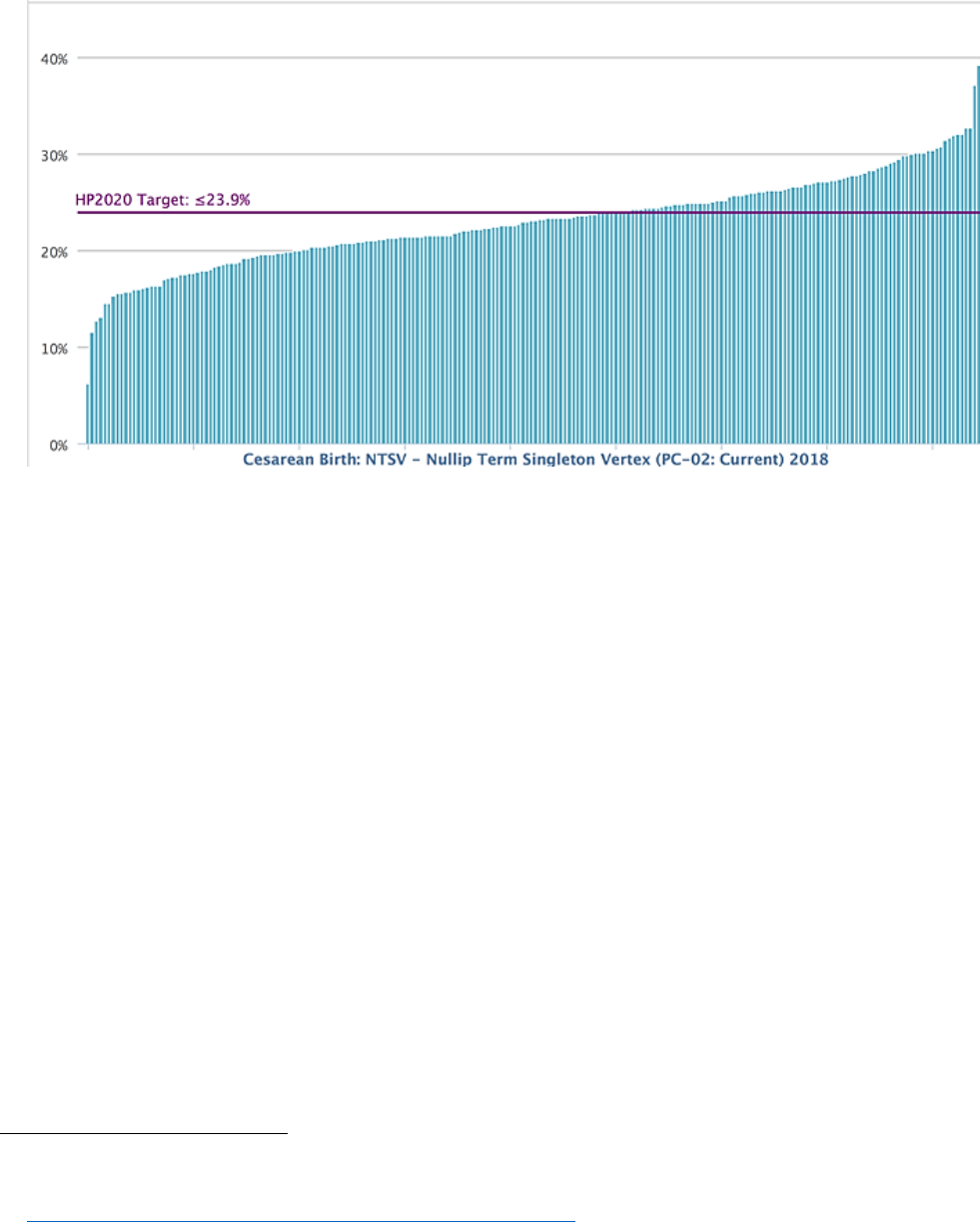
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 97
Figure 13. Distribution of NTSV C-section Rates for Hospitals that Reported to the
California Maternal Quality Care Collaborative, 2018
Note: Each of the blue bars represents each of the hospitals for which there is data available. HP 2020 refers to the Healthy People 2020
target of reducing NTSV C-Sections to 23.9 percent or less of deliveries.
Source: CMQCC Maternal Data Center
After concerted effort by almost every maternity hospital in the state with contractual and other support
from the three large state purchasers — Medi-Cal, CalPERS and Covered California — and the Pacific
Business Group on Health, representing both public and private purchasers, 56 percent of California
maternity hospitals that report to CMQCC (122 of 221) have achieved the national goal of NTSV C-
section rates of 23.9 percent or lower.
93
On an aggregate level, CMQCC reported that 7,200 C-sections
were avoided statewide from 2015 to 2018.
As of the first half of 2019, the number hospitals that participate in CMQCC and meet the NTSV C-
section target was 63 percent (compared to 44 percent in 2015) and there has been a 22 percent
decrease in the percent of hospitals with a rate above 26 percent (42 percent in 2015) (see Figure 14.
Hospitals with C-Sections Rates Below 23.9 Percent or Above 26 Percent Reported to the California
Maternal Quality Care Collaborative, 2018).
93
Smart Care California. (2018). 2018 Hospital C-Section Honor Roll. Retrieved from
https://www.iha.org/sites/default/files/2018_hospital_award_winners_final.pdf.
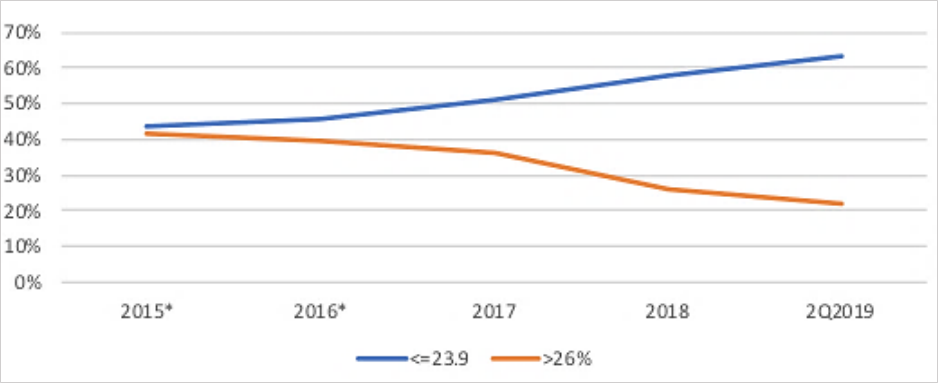
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 98
Figure 14. Hospitals with C-Sections Rates Below 23.9 Percent or Above 26 Percent
Reported to the California Maternal Quality Care Collaborative, 2018
Source: CMQCC Maternal Data Center, 2019
Expand Value-based Payments for Hospitals and Maternity Care
Just as Covered California promotes changes in how physicians are paid to foster payments that
encourage coordination and advanced primary care (see Chapter 7: Promotion of Effective Primary
Care), it requires insurers to change payments to improve hospital quality and maternity care. Health
plans are required to adopt payment methods that (1) tie at least two percent of hospital payments to
value, and (2) eliminate financial incentives for hospital facilities or physicians to perform C-Sections.
Hospital Payments: Health insurance companies are required to adjust payments to hospitals so that
at least two percent of overall hospital payments are tied to value for each product by the end of 2019
and increasing over the following years to at least 6 percent by year-end 2023. This can be
accomplished by either withholding payment pending documentation of quality performance, bonuses,
or a combination of both depending on the circumstances at each hospital. Health insurance
companies are required to include the five specific HAI measures and the NTSV C-section measure,
but insurers are given flexibility to include appropriate additional metrics based on their judgment and
priorities such as patient satisfaction, additional clinical quality measures, safety, or readmissions.
However, the entire two percent cannot be attributed to readmissions due to concern that hospitals
serving a disproportionate share of disadvantaged populations may be inadvertently harmed.
Maternity Care Payments: Health insurance companies are encouraged to adjust labor and delivery
payments to physicians and hospitals so that by year-end 2019 payment does not incentivize
performing C-sections. To provide guidance to hospitals and insurers, Smart Care California, a public-
private multi-stakeholder workgroup led by California state purchasers, built consensus around the
following payment structures: (1) blended case rates; (2) low risk C-section reduction as a metric for

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 99
payment incentive programs; or (3) population-based payment models.
94
While Smart Care California
emphasizes blended case rates, any of the payment structures would fulfill the requirement for payment
to not incentivize performing C-sections.
As described in Table 40. Covered California Insurer Engagement in Changing Payments to Hospitals,
2016-18, most insurers have been Re-contracting with value-based payments for hospitals. As of 2018,
10 insurers were Actively Re-contracting or Re-contracting. The percent of network hospitals with
value-based payments from the insurer is an indicator for the extent to which the insurer is scaling the
program. Data reported for 2018 indicates wide variation in the extent to which an insurer’s network
hospitals have value-based payments, after excluding insurers with integrated delivery systems (Kaiser
Permanente and Sharp Health Plan). Four insurers reported between 20 to 100 percent of hospitals
have value-based payment contracts, two insurers reported less than 10 percent of hospitals have
value-based payment contracts, and four insurers reported that 0 percent of network hospitals have
value-based payment contracts.
For value-based payments for NTSV C-Sections, health plans made significant progress, from six
health plans assessed as Actively Re-contracting or Re-contracting in 2016 to 10 health plans in 2018.
Table 40. Covered California Insurer Engagement in Changing Payments to Hospitals, 2016-18
Hospital Payments
NTSV
C-Sections
Assessment
2016
2017
2018
2016
2017
2018
Actively Re-contracting
Active re-contracting of network to adjust payment.
2
3
4
4
6
7
Re-contracting
Describes efforts to start re-contracting payments (e.g.
internal planning) and has initiated the process.
7
7
6
2
3
3
Minimal Re-contracting
Has not yet started re-contracting toward value-based
payment to hospitals.
2
1
1
5
2
1
Source: Covered California Staff Analysis of Qualified Health Plan Data Submitted for 2016-2018.
Covered California has worked with some insurers to amend their contract on this requirement, either
because they function as a capitated integrated delivery system that has a payment structure aligned
with quality performance or their population is too small to be the basis for leverage in contract
negotiations to change the business model. The common elements in amendments involve continuing
to track measures, engaging hospitals to improve and continually making efforts to change payment if
not already aligned.
In summary, Covered California has worked with the California Hospital Association, Cal Hospital
Compare, CMQCC and Smart Care California, all multi-stakeholder forums that include insurers, to
adopt a focused list of maternity and safety metrics for hospitals. By working together and aligning 11
insurers on a common set of metrics and payment structure, quality performance is now part of hospital
contract discussions in ways it was not in prior years. The state is seeing reductions in NTSV C-
sections and avoidable hospital associated infections.
94
Smart Care California. October 2017. Aligning Birth Payment to Reduce Unnecessary C-Section. Retrieved from:
http://www.iha.org/sites/default/files/files/page/c-section_menu_of_payment_and_contracting_options.pdf.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 100
Covered California’s requirements link hospital payment reform with hospital improvement efforts.
Hospital performance is improving faster than implementation of hospital payment reforms. Sustaining
these improvements in hospital quality and safety will be reinforced as payment is gradually more
aligned with quality and safety goals.
Expanded Approaches to Care Delivery
Telehealth
Health insurance companies are required to report the extent to which they support and use technology
to assist in higher quality, accessible, patient-centered care and the utilization for enrollees on the
number of unique patients and number of separate services provided for telehealth. Health insurance
companies must describe whether these models are implemented in association with patient-centered
medical homes, integrated delivery systems or accountable care organization models of care or are
independently implemented.
All Covered California insurers offered a telehealth or web-based service in 2018, but they vary in their
capabilities. Most insurers that offered a telehealth service in 2018 used a vendor with two insurers
offering telehealth visits only through contracted medical groups and not as a free-standing program
(see Table 41. Covered California Insurer Telehealth Capabilities, 2015, 2017 and 2018).
The percent of enrollees with a telehealth visit for Covered California insurers ranged from 0 percent to
59 percent in 2018. The high outlier, Kaiser Permanente, an integrated delivery system that uses
telehealth as part of their model, reported that 59 percent of enrollees used telehealth or had a web visit
in 2018. Oscar Health Plan reported that 17 percent of enrollees used telehealth or a web visit in 2018.
Oscar Health Plan consistently and actively promotes the use of telehealth to its enrollees. Most other
insurers reported that fewer than 10 percent of enrollees had engaged with care through telehealth.
Table 41. Covered California Insurer Telehealth Capabilities, 2015, 2017 and 2018
Number of Health Plans
2015
2017
2018
Telehealth
Telehealth with video through vendor
2
6
5
Telehealth through medical groups only
1
1
2
Telehealth with phone
2
2
4
Telehealth for mental health visits only
1
0
0
Web Visit using instant messaging
1
2
1
Note: 10 health plans offered a telehealth service in 2017 while all 11 health plans offered a telehealth service in 2018.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 101
Table 42. Covered California Insurer Telehealth Cost Shares and Promotion to Enrollees, 2017-18
Number of Health Plans
2017
2018
Cost-Share
No cost-share*
4
4
Same cost as primary care or specialist visit
5
6
A $5 copay with vendor, but other services are the same an in-person visit
1
1
Promotion to Enrollees
Promoted via email, print, online resources
5
5
Added telehealth visit cost-share next to ED cost-share on member ID card
1
1
Used as Follow up to Lab Visits
0
1
Promoted through Open Enrollment marketing
1
1
Promote on website, member portal, or mobile app
3
3
Promotes through medical groups
2
2
Did not promote telehealth services
3
1
*Note Bronze High Deductible enrollees or those with a Health Savings Account are subject to the deductible.
Source: Covered California Staff Analysis of Qualified Health Plan Submitted Data
Implications for the Future
Improving hospital quality and safety through reducing HAIs and NTSV C-section rates will continue to
be areas of focus for Covered California. Additional measures will be incorporated as they are publicly
reported. As acute care appropriately moves from the hospital to hospital outpatient centers and to
ambulatory surgery centers, Covered California will support efforts to obtain and publicly report on the
quality of care delivered in these sites. Covered California is exploring opportunities to measure
volume, both in the number of patients served and the number of services delivered, as a proxy for
safety at all sites of care. In addition, Covered California recognizes the need to look at additional
measures or indications of health care quality or safety, including what other measures or indicators of
appropriate care should be used.
The adoption of telehealth services, retail or convenience clinics and Centers of Excellence are
examples of using alternative sites of care or expanded approaches to care delivery beyond the
traditional hospital and physician office. Others include care at home and expanded use of technology
such as eConsult and Project ECHO to facilitate integration and coordination across specialties and
adoption of team-based care. Covered California is working with insurers to ensure telehealth or other
technology programs are offered in the languages spoken by their enrollees and further promote the
availability of translation services. Covered California is assessing how best to evaluate the extent to
which these programs foster care that improves quality and patient experience while lowering costs.
Although this report heavily focuses on the hospital and physician office experience, Covered California
recognizes that health care is being delivered to consumers outside of these traditional venues. Moving
forward, Covered California will be evaluating quality outcomes from sites such as outpatient surgery
centers, birthing centers, retail clinics and home care services. More and more consumers are turning
to these non-traditional care sites and Covered California has an obligation to ensure that these sites
meet its high-quality standards while keeping health care costs affordable.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
EFFECTIVE CARE DELIVERY • CHAPTER 11
COVERED CALIFORNIA 102
Chapter 12: Summary and Implications for the Future
This report presents the initial findings of insurer progress towards meeting Covered California’s
contractual requirements to assure quality care and promote delivery system reform.
The most consistent finding across all domains was the remarkable variation in performance with the
consistent high performance for Kaiser Permanente and Sharp Health Plan. This was true not only for
measures included in the Quality Rating System, but also for disadvantaged populations when profiled
for disparities. Hospitals in these integrated systems show much less variation in safety scores and
both insurers have adopted best practices in primary care. Their focus on integrated, coordinated care
likely explains their performance and reinforces Covered California’s intent to promote ACOs to better
organize care in the delivery systems of other insurers. While the integrated plans excelled, it was
reassuring that, with few exceptions, most performance was between the 25
th
and 90
th
percentile
nationwide for other plans across a wide range of measures. There are some measures, especially for
behavioral health and preventive care, where several plans perform below the 25
th
percentile. However,
Covered California has no outlier poor performing health plans.
Covered California worked with insurers to collect baseline data on race and ethnicity for all enrollees
under 65 across all lines of business. Despite significant challenges with data quality, each insurer is
moving ahead to address health disparities based on actionable differences found across a wide variety
of population characteristics. This program is a priority to enhance and expand.
All Covered California enrollees now have a primary care physician and a growing number are cared
for within Integrated Delivery Systems or ACOs. Significant work remains to support the implementation
of advanced primary care models and to establish best practices for ACOs as they attempt to replicate
the success of integrated systems.
Covered California holds health insurance companies accountable to manage variation in performance
in addition to reporting overall average measurement through the Quality Rating System. Hospital
performance was an initial focus using publicly reported data and supported by collaborative programs
improving safety and maternity care. There has been important progress made demonstrating the value
of alignment across multiple purchasers and payers as well as significant leadership from providers.
Hospital care in California is safer as a result.
Covered California has established a framework and approach to systematic improvement that has
started to show important results: slower cost growth, modest improvement in quality measures,
adoption of more effective primary care models, progress toward implementation of integrated delivery
systems and ACOs and, through collaboration with others, substantial gains in patient safety.
Moreover, by requiring all insurers to stratify performance measures by race and ethnicity, Covered
California has set the stage for achieving progress in reducing disparities.
Much remains to be done, especially in the arena of consistent and effective measurement that
supports quality improvement strategies for better health outcomes. Covered California acknowledges
that efforts to meet the long-term goals of consistent measurement would potentially increase
administrative burden initially for providers and hospitals but if done effectively and carefully, would
establish consistent data measurement across insurers and purchasers that targets improvement
opportunities for the delivery system in quality, cost, effectiveness and equity. In the end, this would be
expected to reduce administrative burden and complexity. Covered California is committed to working
collaboratively and transparently to ensure that we contribute to a state where “Health Care for All”
means that all Californians receive the best possible care.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 103
APPENDICES
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 104
Appendix 1: Limitations and Major Caveats about Health Disparities Data
The data collected for the health disparities measures described in Chapter 2 is unique because it
includes data for enrollees under age 65 across all lines of business for 11 insurers. Covered California
cautions that it has several limitations and major caveats:
• These are baseline results not reported for accountability: Insurers have been required to
collect ethnic and racial identity by law in California since 2003. The results were used only to
determine which language translation services were needed. This is the first time ethnic and
racial identity information has been used to stratify clinical outcomes data for the purpose of
defining and addressing disparities. It has taken three years to establish a baseline for which
strategies are being developed to reduce disparities.
• Varying populations by insurer: Health insurance companies collected data for their entire
populations under 65 regardless of line of business. Because each insurer has different
proportions of commercial and Medi-Cal populations, the results cannot be compared between
insurers.
• No formal audit process: While insurers were encouraged to follow the measures
specifications for HEDIS and PQI, the data reported by insurers has not been verified through a
third-party audit as it would be for reporting to the National Committee for Quality Assurance’s
Quality Compass. Third-party auditors examine information practices and control procedure,
sampling methods and procedures, data integrity, compliance with HEDIS specifications,
analytic file production, and reporting and documentation.
• Variation in data quality and collection: Data quality varies by insurer, with some missing key
data elements such as identification of certain groups (e.g., Native Hawaiian) and ability to
identify claims using the measure specifications for admissions. Most insurers aggregated their
400-person HEDIS samples across all lines of business and a few had access to robust clinical
data from electronic health records. HEDIS samples are drawn to represent the entire
population but may not represent the ethnic and racial diversity of the plan’s population.
• Small denominators: Because the health disparities measures are based on a subset of
individuals with a diagnosed chronic condition and reported by six race/ethnicity categories, this
results in small denominators among some groups for certain measures and make it difficult to
identify actual differences in care and outcomes. Some admissions measures and American
Indian/Alaskan Native populations are especially impacted by small denominators. As a result,
no insurer proposed an admission measure as a focus of disparity reduction efforts. However,
admissions are important enough that further work is needed to determine if interventions might
be appropriate despite the small numbers.
• Interpretation of data and identifying health Care disparities: Health insurance companies
report the numerators, denominators, and rates by race/ethnicity for each measure, and early
discussions between Covered California and insurers have centered on observed rate
differences in admissions, disease control, and medication management between race/ethnicity
groups. An observed rate difference may require further analysis to consider confounding
factors and statistical significance.

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 105
Appendix 2: Additional Health Plan Measures Reported to Quality Rating
System
The following tables display the Covered California weighted average, highest and lowest performing
plans, plan-specific performance, as well as national percentiles for all Marketplace plans for the
remaining measures in the Marketplace Quality Rating System (QRS) measure set. A priority set of 13
measures were presented in the subject chapters of this report.
How to Interpret Quality Performance Data
Within the QRS measure set, HEDIS measures rely on claims or encounter data while CAHPS
measures are collected as part of the Qualified Health Plan Enrollee Survey. Since insurers can offer
multiple products that vary by network type (HMO, PPO, or EPO), the data below shows 16 total plans.
The data is listed by year the health plans reported the QRS measure set data such that the 2019
reporting year data represents health plan performance during the 2018 calendar year or measurement
year and so on.
Only data for products meeting CMS participation criteria for QRS score eligibility are displayed in the
tables. Blank cells indicate the following: (1) CMS participation criteria were not met for scoring
because the health plan did not offer a product for two consecutive years through Covered California;
(2) CMS participation criteria were met but denominator size for a given measure was below the
minimum threshold for scoring; or (3) the health plan chose not to report the measure (Not
Reported/NR).
The percentile values provide benchmark information for measure rates, allowing a health plan to
compare its results to all other health plans and products nationally. CMS reports benchmark values
that include the standardized 25
th
, 50
th
, 75
th
, and 90
th
percentile values for the numerical rates across all
health plans and products. To create these benchmark values, CMS uses only measure rates that have
met the minimum denominator size criteria for scoring.
95
95
Centers for Medicaid and Medicare Services. (2018). Quality Rating System and Qualified Health Plan Enrollee Experience Survey:
Technical Guidance for 2019. Retrieved from https://www.cms.gov.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 106
Additional Measures Related to Health Promotion and Prevention
In Chapter 3: Health Promotion and Prevention, three QRS measures are presented as potential
“Priority Measures.” These measures and the eight additional QRS measures pertaining to Health
Promotion and Prevention are:
Potential Priority Measures
1. Breast Cancer Screening (Table 13)
2. Cervical Cancer Screening (Table 14)
3. Colorectal Cancer Screening (Table 15)
Additional Measures
4. Chlamydia Screening in Women (Table A1)
5. Adult BMI Assessment (Table A2)
6. Childhood Immunizations (Combination 3) (Table A3)
7. Immunizations for Adolescents (Combination 2) (Table A4)
8. Flu Vaccinations for Adults (Table A5)
9. Medical Assistance with Smoking and Tobacco Use Cessation (Table A6)
10. Weight Assessment and Counseling for Nutrition and Physical Activity for Children and
Adolescents (Table A7)
11. Annual Dental Visit (Table A8)

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 107
Chlamydia Screening in Women
The Chlamydia Screening measure is the percentage of women 16–24 years of age who were
identified as sexually active and who had at least one test for chlamydia during the measurement year.
Table A1. Chlamydia Screening in Women for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
61 +
64 +
65 +
67 +
36%
477,683
1
Plans at 50th to 90th
Percentile
44 to 61
45 to 64
48 to 65
47 to 67
46%
622,371
8
Plans at 25th to 50th
Percentile
37 to 44
38 to 45
39 to 48
40 to 47
18%
245,176
3
Plans Below 25th Percentile
Below 37
Below 38
Below 39
Below 40
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest
Performer
69
73
75
73
Covered CA Weighted
Average
52
59
60
58
Covered CA Lowest
Performer
45
44
46
44
Covered California Plan-Specific Performance
Anthem HMO
52
52
Anthem PPO
45
47
Anthem EPO
48
44
5%
64,031
Blue Shield HMO
53
51
49
7%
93,322
Blue Shield PPO
45
48
50
49
25%
335,176
CCHP HMO
55
55
58
59
1%
10,013
Health Net HMO
47
50
51
47
11%
145,183
Health Net EPO
44
58
Health Net PPO
Kaiser Permanente HMO
69
73
75
73
36%
477,683
LA Care HMO
47
57
59
59
6%
84,750
Molina Healthcare HMO
55
64
59
52
4%
56,023
Oscar Health Plan EPO
55
46
3%
35,962
Sharp Health Plan HMO
58
62
58
60
1%
17,335
Valley Health Plan HMO
65
55
1%
16,366
Western Health Advantage
HMO
57
54
46
56
1%
9,386
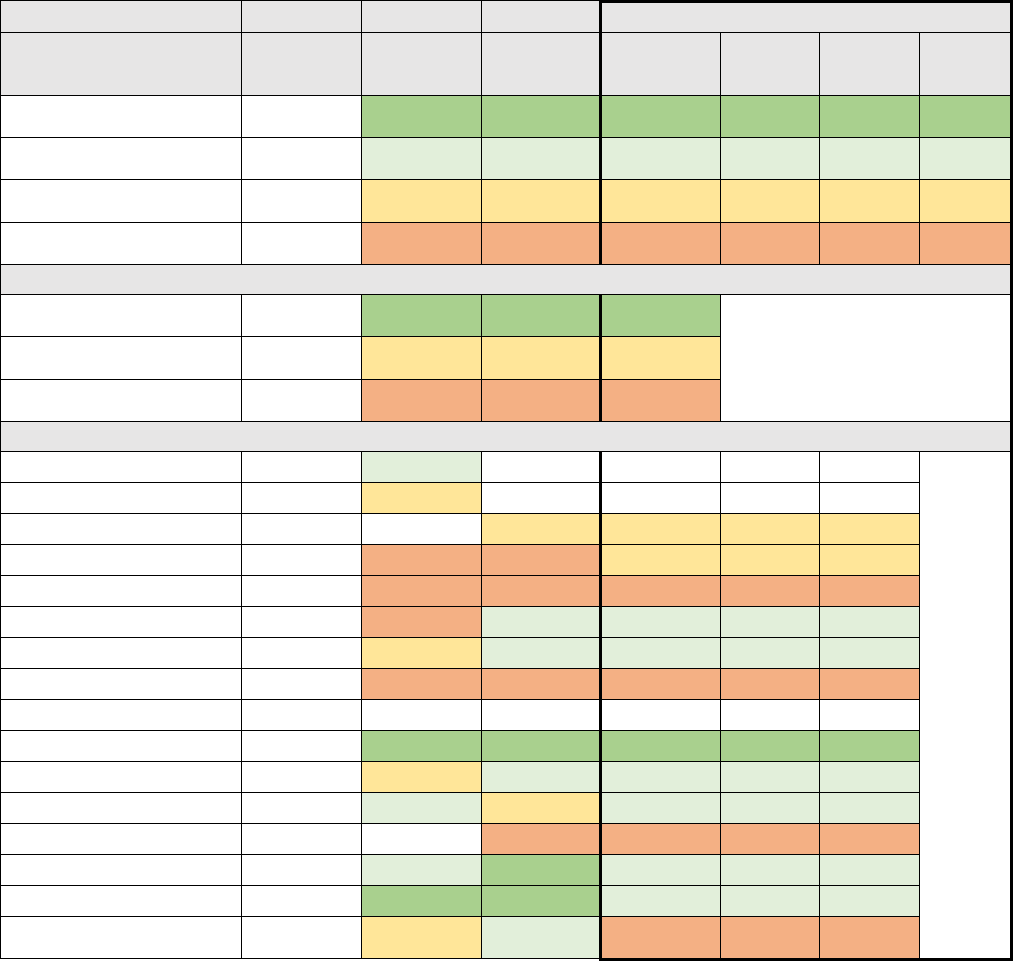
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 108
Adult Body Mass Index Assessment
The Adult BMI measure is the percentage of members 18–74 years of age who had an outpatient visit
and whose body mass index (BMI) was documented during the measurement year or the year prior to
the measurement year.
Table A2. Adult Body Mass Index Assessment for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile
and Above
MN-S
95 +
94 +
96 +
35%
477,683
1
Plans at 50th to 90th
Percentile
MN-S
84 to 95
85 to 94
86 to 96
24%
329,670
6
Plans at 25th to 50th
Percentile
MN-S
73 to 84
75 to 85
79 to 86
12%
157,353
2
Plans Below 25th
Percentile
MN-S
Below 73
Below 75
Below 79
28%
381,920
4
Covered California High/Average/Low Performers
Covered CA Highest
Performer
97
96
97
97
Covered CA Weighted
Average
79
83
82
85
Covered CA Lowest
Performer
37
37
35
67
Covered California Plan-Specific Performance
Anthem HMO
82
86
Anthem PPO
76
81
Anthem EPO
81
83
5%
64,031
Blue Shield HMO
37
37
35
79
7%
93,322
Blue Shield PPO
67
71
68
67
25%
335,176
CCHP HMO
92
71
88
94
1%
10,013
Health Net HMO
75
80
85
89
11%
145,183
Health Net EPO
71
71
75
0%
1,396
Health Net PPO
Kaiser Permanente HMO
97
96
97
97
35%
477,683
LA Care HMO
79
82
93
95
6%
84,750
Molina Healthcare HMO
77
84
81
86
4%
56,023
Oscar Health Plan EPO
70
70
3%
35,962
Sharp Health Plan HMO
92
94
96
95
1%
17,335
Valley Health Plan HMO
90
95
95
91
1%
16,366
Western Health Advantage
HMO
81
83
88
74
1%
9,386
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
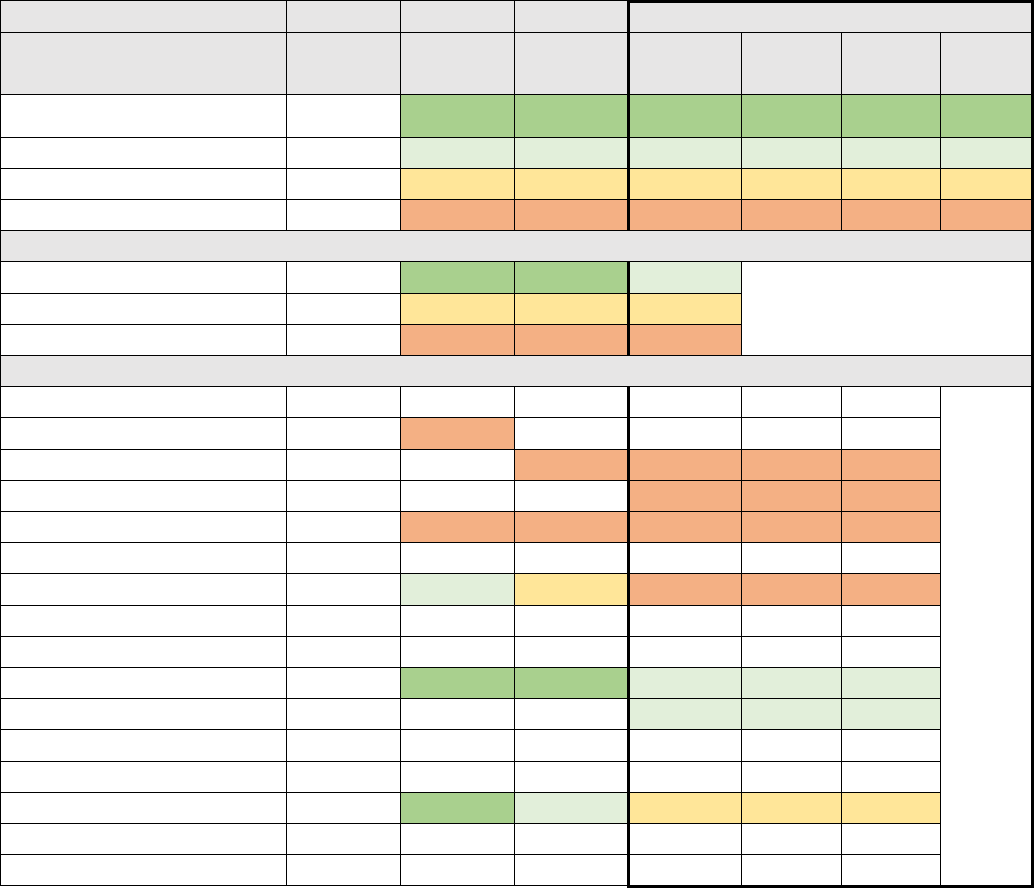
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 109
Childhood Immunizations Status (Combination 3)
The Childhood Immunization Status measure is the percentage of children 2 years of age who had four
diphtheria, tetanus and acellular pertussis (DTaP); three polio (IPV); one measles, mumps and rubella
(MMR); three haemophilus influenza type B (HiB); three hepatitis B (HepB), one chicken pox (VZV);
and four pneumococcal conjugate (PCV) vaccines by their second birthday. The measure calculates a
rate for each vaccine and one combination rate.
Table A3. Childhood Immunization Status (Combination 3) for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
85 +
86 +
86 +
0%
-
0
Plans at 50th to 90th Percentile
MN-S
76 to 85
75 to 86
77 to 86
46%
562,433
2
Plans at 25th to 50th Percentile
MN-S
69 to 76
65 to 75
65 to 77
1%
17,335
1
Plans Below 25th Percentile
MN-S
Below 69
Below 65
Below 65
52%
637,712
4
Covered California High/Average/Low Performers
Covered CA Highest Performer
83
90
87
84
Covered CA Weighted Average
70
74
73
72
Covered CA Lowest Performer
62
60
56
50
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
62
66
Anthem EPO
64
50
5%
64,031
Blue Shield HMO
64
8%
93,322
Blue Shield PPO
63
60
56
63
28%
335,176
CCHP HMO
Health Net HMO
78
80
73
58
12%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
83
85
87
84
39%
477,683
LA Care HMO
82
7%
84,750
Molina Healthcare HMO
Oscar Health Plan EPO
Sharp Health Plan HMO
67
90
80
69
1%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
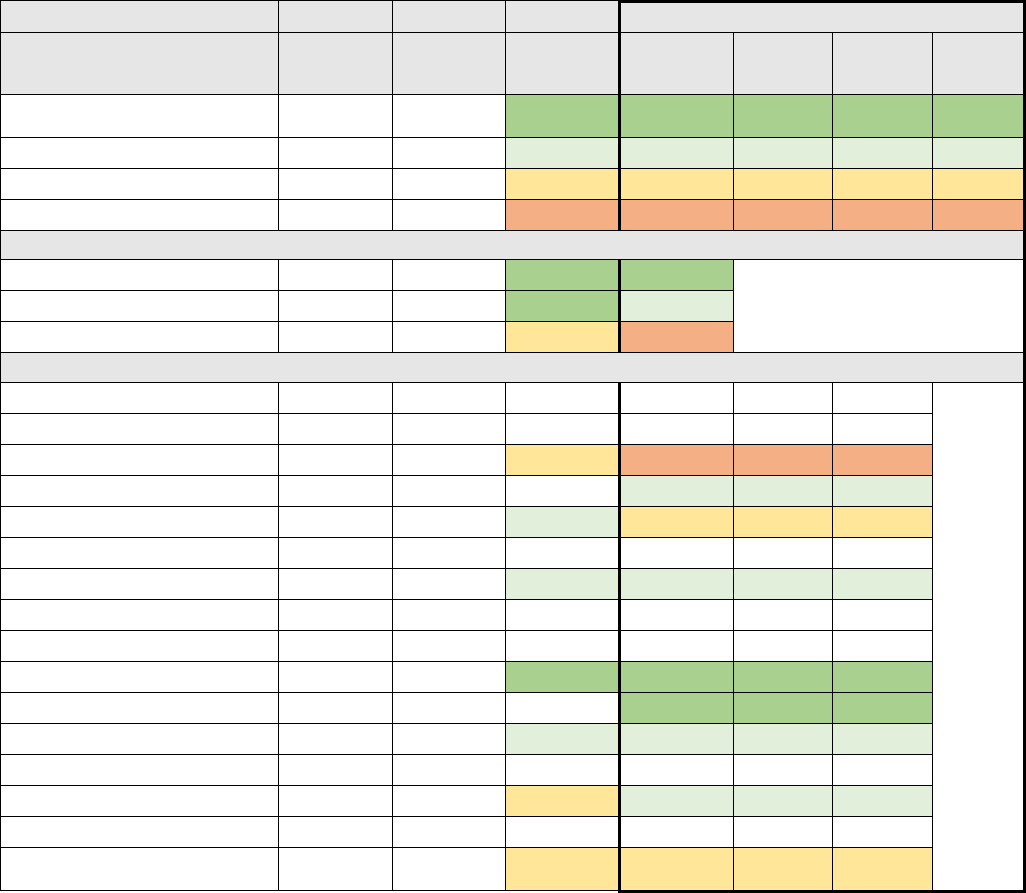
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 110
Immunizations for Adolescents (Combination 2)
The Immunizations for Adolescents (Combination 2) measure is the percentage of adolescents 13
years old who had one dose of meningococcal vaccine, one tetanus, diphtheria toxoids and acellular
pertussis (Tdap) vaccine, and have completed the human papillomavirus (HPV) vaccine series by their
13
th
birthday. The measure calculates a rate for each vaccine and two combination rates.
Table A4. Immunizations for Adolescents (Combination 2) for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
MN-S
31 +
36 +
44%
562,433
2
Plans at 50th to 90th Percentile
MN-S
MN-S
19 to 31
23 to 36
24%
311,863
4
Plans at 25th to 50th Percentile
MN-S
MN-S
15 to 19
17 to 23
27%
344,562
2
Plans Below 25th Percentile
MN-S
MN-S
Below 15
Below 17
5%
64,031
1
Covered California High/Average/Low Performers
Covered CA Highest Performer
83
33
51
54
Covered CA Weighted Average
63
22
34
35
Covered CA Lowest Performer
54
11
16
16
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
54
11
Anthem EPO
16
16
5%
64,031
Blue Shield HMO
24
7%
93,322
Blue Shield PPO
57
14
22
23
26%
335,176
CCHP HMO
Health Net HMO
58
20
24
24
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
83
33
51
54
37%
477,683
LA Care HMO
39
7%
84,750
Molina Healthcare HMO
29
26
4%
56,023
Oscar Health Plan EPO
Sharp Health Plan HMO
23
19
23
1%
17,335
Valley Health Plan HMO
Western Health Advantage
HMO
18
22
1%
9,386
Note: National percentiles not scored for Reporting Years 2016 and 2017. Between Reporting Years 2016 and 2019, this measure was
renamed to “Immunizations for Adolescents (Combination 2)” and expanded to include the HPV vaccine alongside the Tdap and
meningococcal vaccines.
*M-NS: This measure was not used in determining the overall QRS rating in 2016 or 2017.
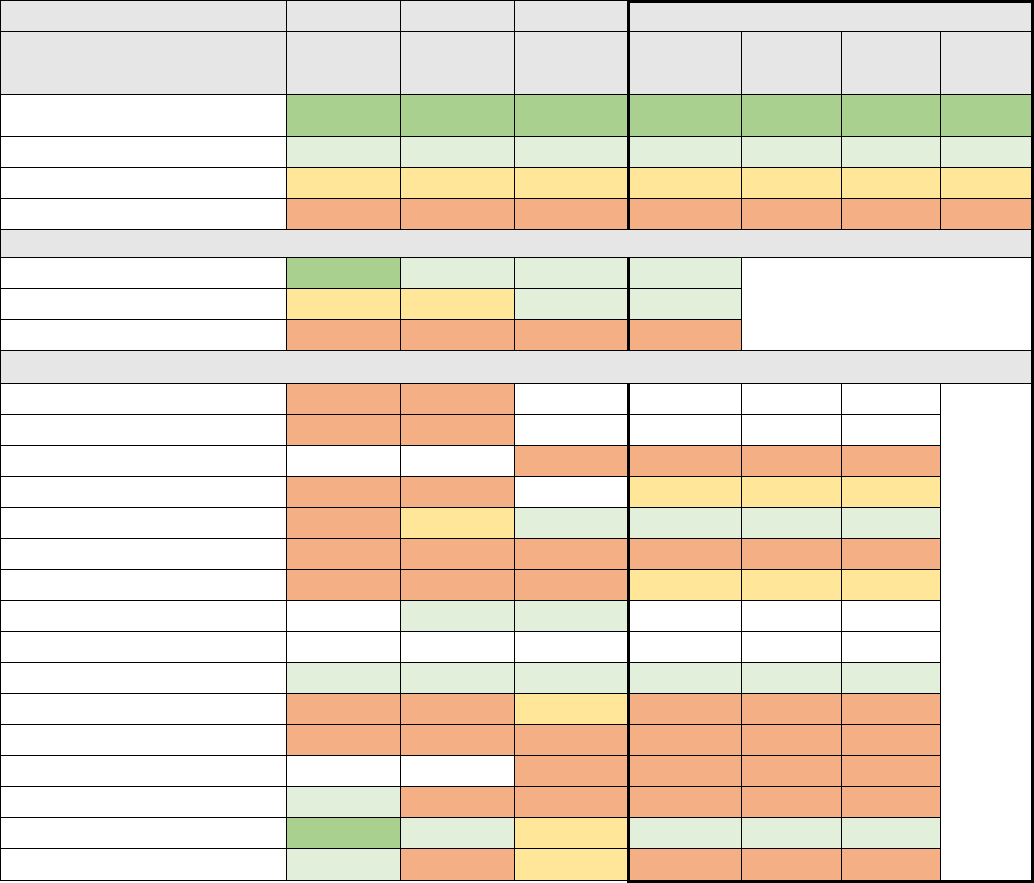
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 111
Flu Vaccinations for Adults
The Flu Vaccination for Adults measure is the percentage of members 18-64 years of age who received
a flu vaccination between July 1 of the measurement year and the date when the QHP Enrollee Survey
was completed. This is the only immunization measure that includes adults, who make up the majority
of Covered California plan enrollment.
Table A5. Flu Vaccinations for Covered California Enrollees Ages 18-64 (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
50 +
50 +
54 +
58 +
0%
-
0
Plans at 50th to 90th Percentile
40 to 50
40 to 50
43 to 54
47 to 58
62%
829,225
3
Plans at 25th to 50th Percentile
35 to 40
37 to 40
38 to 43
43 to 47
18%
238,505
2
Plans Below 25th Percentile
Below 35
Below 37
Below 38
Below 43
21%
277,500
7
Covered California High/Average/Low Performers
Covered CA Highest Performer
57
48
51
56
Covered CA Weighted Average
36
40
45
48
Covered CA Lowest Performer
25
30
30
29
Covered California Plan-Specific Performance
Anthem HMO
25
36
Anthem PPO
32
30
Anthem EPO
30
41
5%
64,031
Blue Shield HMO
27
32
45
7%
93,322
Blue Shield PPO
34
39
48
47
25%
335,176
CCHP HMO
32
34
37
39
1%
10,013
Health Net HMO
31
36
36
46
11%
145,183
Health Net EPO
44
44
Health Net PPO
Kaiser Permanente HMO
48
47
51
56
36%
477,683
LA Care HMO
30
33
38
40
6%
84,750
Molina Healthcare HMO
29
35
30
29
4%
56,023
Oscar Health Plan EPO
35
32
3%
35,962
Sharp Health Plan HMO
45
36
35
42
1%
17,335
Valley Health Plan HMO
57
48
42
47
1%
16,366
Western Health Advantage HMO
41
31
42
41
1%
9,386
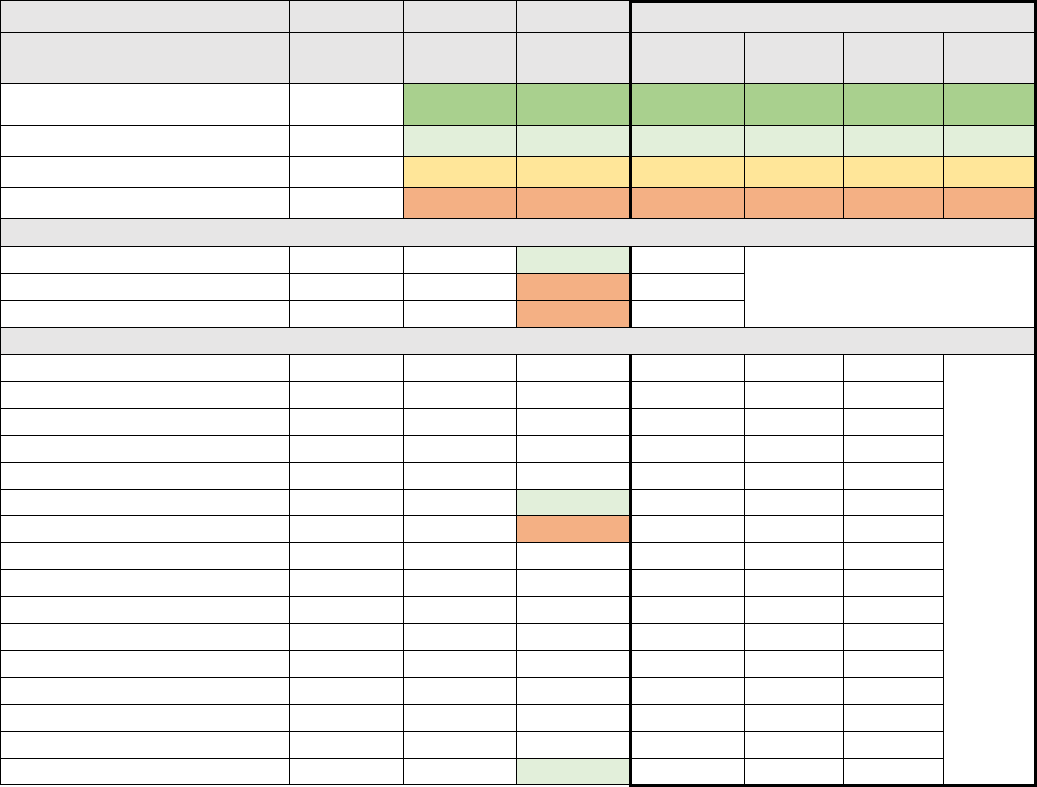
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 112
Medical Assistance with Smoking and Tobacco Use Cessation
The Medical Assistance with Smoking and Tobacco Use Cessation measure is comprised of the
following components:
1. Advising Smokers and Tobacco Users to Quit: A rolling average represents the percentage of
members 18 years of age and older who were current smokers or tobacco users and who
received advice to quit during the measurement year.
2. Discussing Cessation Medications: A rolling average represents the percentage of members 18
years of age and older who were current smokers or tobacco users and who discussed or were
recommended cessation medications during the measurement year.
3. Discussing Cessation Strategies: A rolling average represents the percentage of members 18
years of age and older who were current smokers or tobacco users and who discussed or were
provided cessation methods or strategies during the measurement year.
Table A6. Medical Assistance with Smoking and Tobacco Use Cessation for Covered California Enrollees
(CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
59 +
60 +
63 +
-
0
Plans at 50th to 90th Percentile
MN-S
50 to 59
50 to 60
54 to 63
-
0
Plans at 25th to 50th Percentile
MN-S
45 to 50
45 to 50
48 to 54
-
0
Plans Below 25th Percentile
MN-S
Below 45
Below 45
Below 48
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
55
Covered CA Weighted Average
39
Covered CA Lowest Performer
37
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
Anthem EPO
Blue Shield HMO
Blue Shield PPO
CCHP HMO
51
Health Net HMO
37
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
LA Care HMO
Molina Healthcare HMO
Oscar Health Plan EPO
Sharp Health Plan HMO
Valley Health Plan HMO
Western Health Advantage HMO
55
*QRS did not collect this measure in 2016.
**M-NS: This measure was not used in determining the overall QRS rating in 2016.
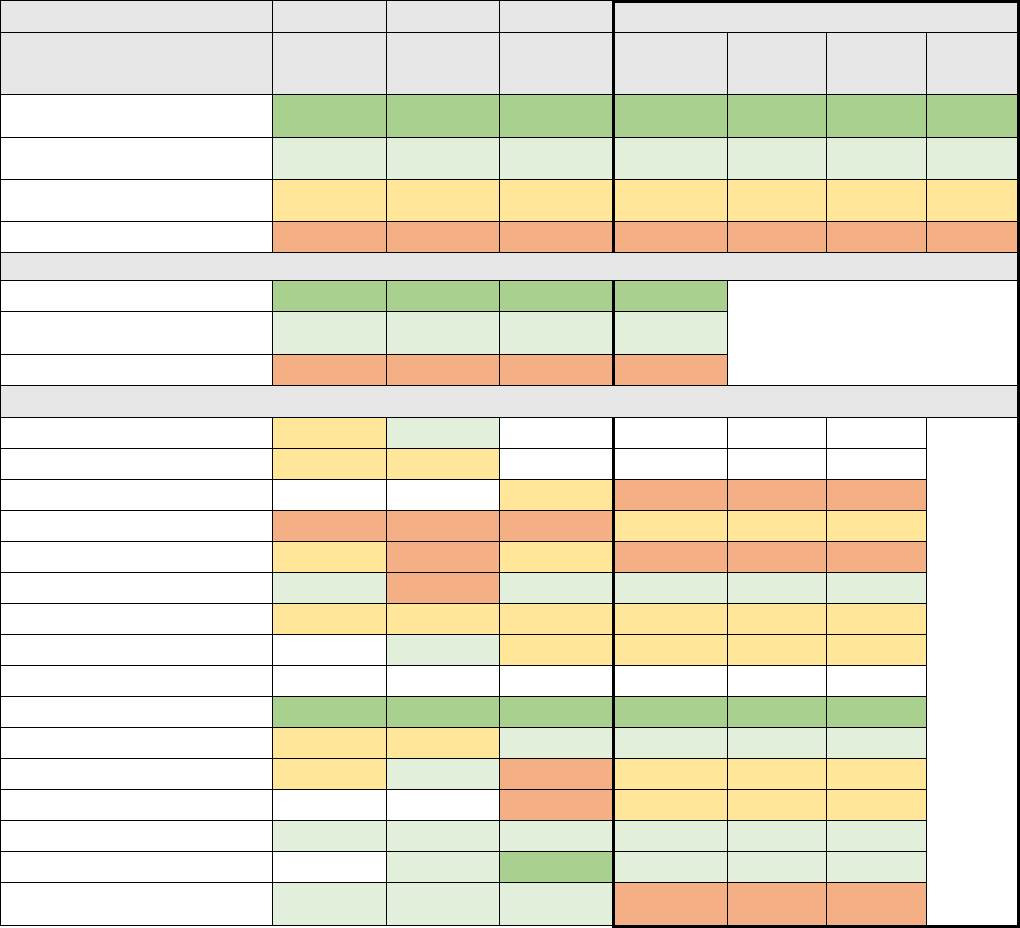
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 113
Weight Assessment and Counseling for Nutrition and Physical Activity for Children and
Adolescents
The Weight Assessment and Counseling for Nutrition and Physical Activity for Children and
Adolescents measure is the percentage of members 3-17 years of age who had an outpatient visit with
a PCP or OB/GYN and who had evidence of the following during the measurement year:
• BMI percentile documentation. Because BMI norms for youth vary with age and gender, this
measure evaluates whether BMI percentile is assessed rather than an absolute BMI value;
• Counseling for nutrition; and
• Counseling for physical activity.
Table A7. Weight Assessment and Counseling for Nutrition and
Physical Activity for Covered California Children and Adolescents Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
82 +
83 +
84 +
87 +
35%
477,683
1
Plans at 50th to 90th
Percentile
56 to 82
63 to 83
66 to 84
69 to 87
10%
128,464
4
Plans at 25th to 50th
Percentile
46 to 56
51 to 63
53 to 66
59 to 69
25%
331,886
5
Plans Below 25th Percentile
Below 46
Below 51
Below 53
Below 59
30%
408,593
3
Covered California High/Average/Low Performers
Covered CA Highest Performer
95
94
95
94
Covered CA Weighted
Average
61
68
68
73
Covered CA Lowest Performer
4
4
7
33
Covered California Plan-Specific Performance
Anthem HMO
52
68
Anthem PPO
52
56
Anthem EPO
64
56
5%
64,031
Blue Shield HMO
4
4
7
60
7%
93,322
Blue Shield PPO
48
50
53
58
25%
335,176
CCHP HMO
68
21
81
71
1%
10,013
Health Net HMO
54
58
62
61
11%
145,183
Health Net EPO
65
66
63
0%
1,396
Health Net PPO
Kaiser Permanente HMO
95
94
95
94
35%
477,683
LA Care HMO
48
54
74
80
6%
84,750
Molina Healthcare HMO
52
68
52
69
4%
56,023
Oscar Health Plan EPO
10
60
3%
35,962
Sharp Health Plan HMO
65
74
77
80
1%
17,335
Valley Health Plan HMO
77
84
78
1%
16,366
Western Health Advantage
HMO
73
67
74
33
1%
9,386
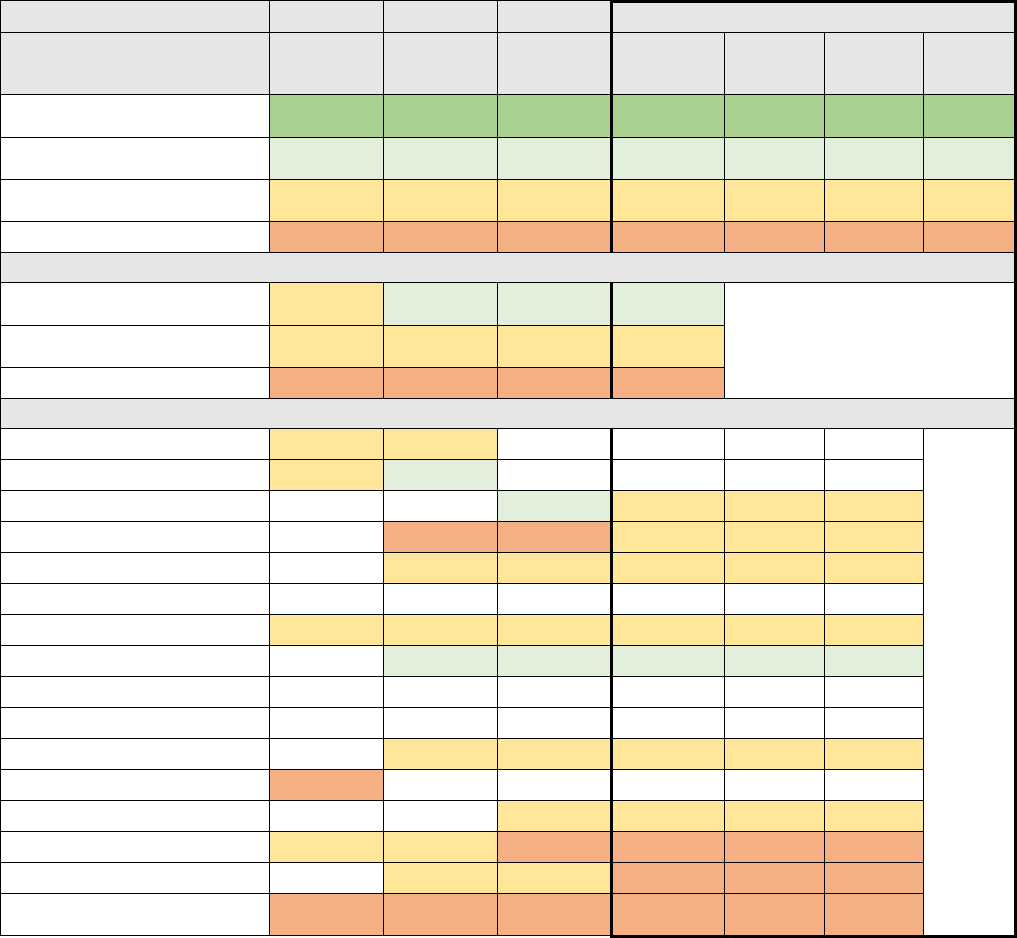
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 114
Annual Dental Visit
The Annual Dental Visit measure is the percentage of members 2–20 years of age who had at least
one dental visit during the measurement year.
Table A8. Annual Dental Visit for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
55 +
57 +
55 +
55 +
0%
-
0
Plans at 50th to 90th
Percentile
27 to 55
27 to 57
32 to 55
31 to 55
0%
1,396
1
Plans at 25th to 50th
Percentile
9 to 27
8 to 27
13 to 32
16 to 31
94%
758,424
6
Plans Below 25th Percentile
Below 9
Below 8
Below 13
Below 16
5%
43,087
3
Covered California High/Average/Low Performers
Covered CA Highest
Performer
24
38
41
43
Covered CA Weighted
Average
17
14
20
22
Covered CA Lowest Performer
2
7
2
3
Covered California Plan-Specific Performance
Anthem HMO
13
18
Anthem PPO
24
32
Anthem EPO
35
28
8%
64,031
Blue Shield HMO
7
13
18
12%
93,322
Blue Shield PPO
12
21
25
42%
335,176
CCHP HMO
Health Net HMO
10
12
17
20
18%
145,183
Health Net EPO
38
41
43
0%
1,396
Health Net PPO
Kaiser Permanente HMO
LA Care HMO
13
18
18
11%
84,750
Molina Healthcare HMO
2
Oscar Health Plan EPO
28
21
4%
35,962
Sharp Health Plan HMO
9
11
9
12
2%
17,335
Valley Health Plan HMO
22
20
9
2%
16,366
Western Health Advantage
HMO
3
7
2
3
1%
9,386
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 115
Additional Measures Related to Mental Health and Substance Use Disorder
Treatment
In Chapter 4: Mental Health and Substance Use Disorder, three QRS measures are presented as
potential “Priority Measures.” These measures and one additional QRS measure pertaining to Mental
Health and Substance Use Disorder are:
Potential Priority Measures
1. Antidepressant Medication Management (Table 16)
2. Follow Up After Hospitalization for Mental Illness (Table 17)
3. Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (Table
18)
Additional Measures
4. Follow Up Care for Children Prescribed ADHD Medication (ADD) measure (Table A9)
Covered California is evaluating available behavioral health measures for children as part of its work in
finding the right measures for subpopulations.
Follow Up Care for Children Prescribed ADHD Medication (HEDIS)
The Follow Up Care for Children Prescribed ADHD Medication (ADD) measure is the percentage of
children newly prescribed attention-deficit/hyperactivity disorder (ADHD) medication who had at least
three follow-up care visits within a 10-month period, one of which was within 30 days of when the first
ADHD medication was dispensed. Two rates are reported:
1. Initiation Phase: The percentage of members 6–12 years of age as of the Index Prescription
Start Data (IPSD) with an ambulatory prescription dispensed for ADHD medication, who had
one follow-up visit with practitioner with prescribing authority during the 30-day Initiation Phase.
2. Continuation and Maintenance (CandM) Phase: The percentage of members 6–12 years of
age as of the IPSD with an ambulatory prescription dispensed for ADHD medication, who
remained on the medication for at least 210 days and who, in addition to the visit in the Initiation
Phase, had at least two follow-up visits with a practitioner within 270 days (9 months) after the
Initiation Phase ended.
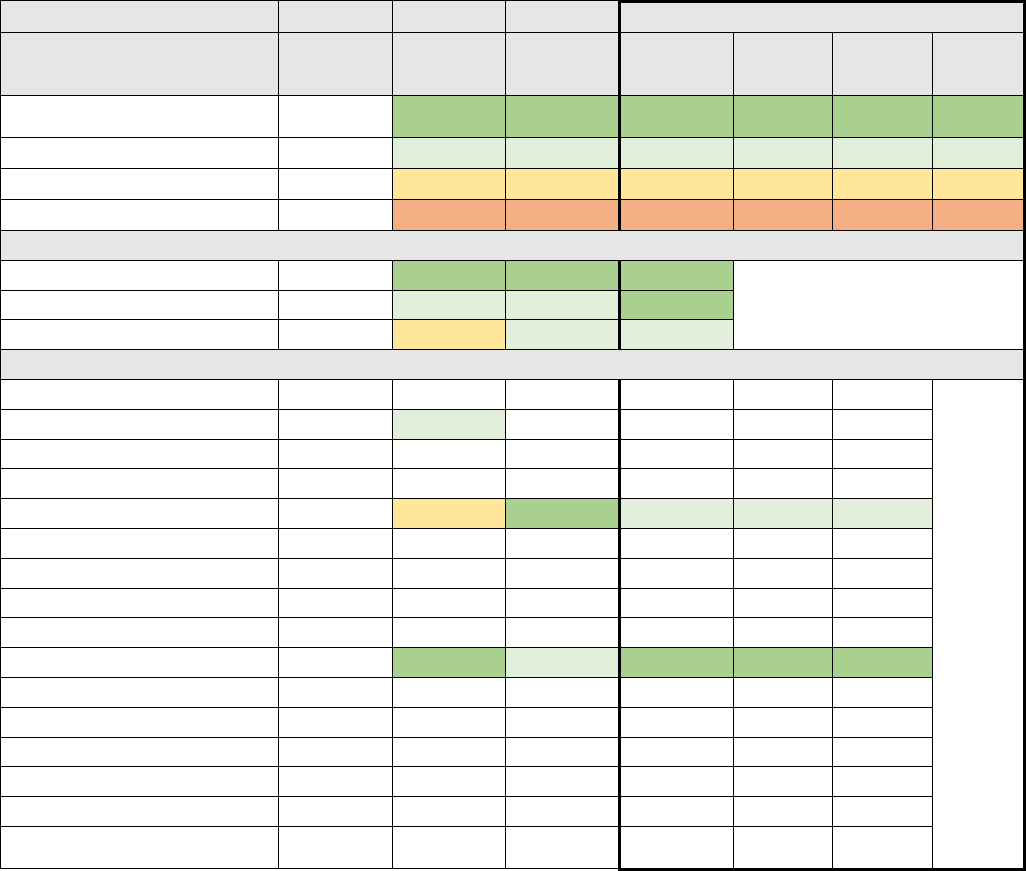
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 116
Table A9. Follow Up Care for Covered California Children Enrollees Prescribed ADHD Medication (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
53 +
63 +
51 +
59%
477,683
1
Plans at 50th to 90th Percentile
MN-S
36 to 53
41 to 63
45 to 51
41%
335,176
1
Plans at 25th to 50th Percentile
MN-S
29 to 36
35 to 41
39 to 45
0%
-
0
Plans Below 25th Percentile
MN-S
Below 29
Below 35
Below 39
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
60
63
57
Covered CA Weighted Average
47
60
53
Covered CA Lowest Performer
32
58
46
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
51
Anthem EPO
Blue Shield HMO
Blue Shield PPO
32
63
46
41%
335,176
CCHP HMO
Health Net HMO
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
60
58
57
59%
477,683
LA Care HMO
Molina Healthcare HMO
Oscar Health Plan EPO
Sharp Health Plan HMO
Valley Health Plan HMO
Western Health Advantage
HMO
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 117
Additional Measures Related to Acute, Chronic and Other Conditions
In Chapter 5: Acute, Chronic and Other Conditions, five QRS measures are presented as potential
“Priority Measures.” These measures and the 11 additional QRS measures pertaining to Acute, Chronic
and Other Conditions are:
Potential Priority Measures
1. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%) (Table 19)
2. Controlling High Blood Pressure (Table 20)
3. Plan All-Cause Readmissions (Table 21)
4. Access to Care (Table 22)
5. Care Coordination (Table 23)
Additional Measures
6. Proportion of Days Covered (RAS Antagonists) (Table A10)
7. Proportion of Days Covered (Statins) (Table A11)
8. Proportion of Day Covered (Diabetes All Class) (Table A12)
9. Comprehensive Diabetes Care: Eye Exam (Retinal) Performed (Table A13)
10. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Testing (Table A14)
11. Comprehensive Diabetes Care: Medical Attention for Nephropathy (Table A15)
12. Medication Management for People with Asthma (75% of Treatment Period) (Table A16)
13. Prenatal and Postpartum Care (Postpartum Care) (Table A17)
14. Prenatal and Postpartum Care (Timeliness of Prenatal Care) (Table A18)
15. Well-Child Visits in the First 15 Months of Life (6 or More Visits) (Table A19)
16. Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life (Table A20)
The following proportion of days covered measures track the percentage of patients adhering to their
medications for their condition. Once started, adherence to medications long term is important for
chronic disease management and to prevent complications. Ideally, adherence or percent of days
covered should approach 100 percent, but the measure is met if it was above the 80 percent threshold.
Barriers to adherence to medications may include limited knowledge or awareness of long-term
treatment goals, adverse side effects, financial barriers, or forgetfulness.
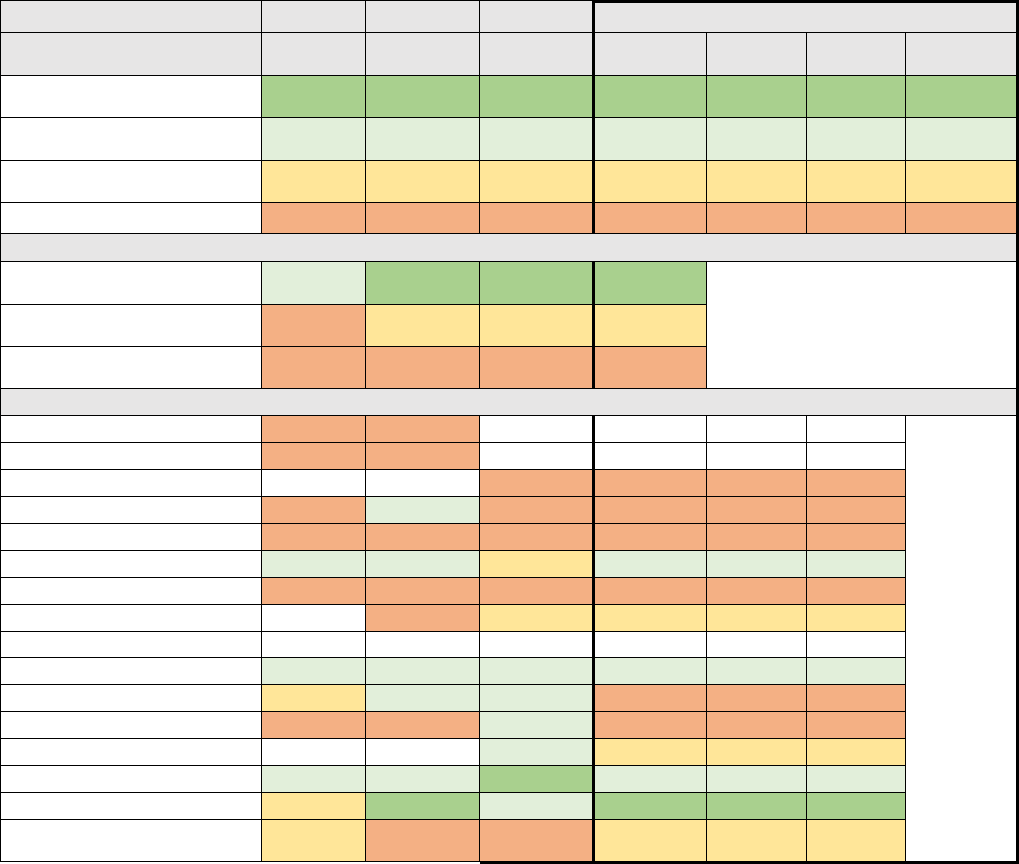
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 118
Proportion of Days Covered (RAS Antagonists) (Pharmacy Quality Alliance)
Diabetes is the most common cause of renal failure. Renin Angiotensin System (RAS) Antagonists
protect patients against diabetic kidney disease. This drug also treats high blood pressure which is a
common co-morbidity for diabetic patients. Patients typically receive a screening test to determine
whether or not they need to be prescribed these medications if not already using them for hypertension.
The Pharmacy Quality Alliance (PQA) Proportion of Days Covered RAS Antagonists measure is the
percentage of patients 18 years and older who met the proportion of days covered threshold of 80
percent for RAS Antagonists during the measurement period. A higher rate indicates better
performance.
Table A10. Proportion of Days Covered (RAS Antagonists) for Covered California Enrollees (PQA)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number of
Plans
Plans at 90th Percentile and
Above
82 +
83 +
83 +
85 +
1%
16,366
1
Plans at 50th to 90th
Percentile
73 to 82
75 to 83
76 to 83
78 to 85
38%
505,031
3
Plans at 25th to 50th
Percentile
67 to 73
70 to 75
72 to 76
73 to 78
3%
46,744
3
Plans Below 25th Percentile
Below 67
Below 70
Below 72
Below 73
58%
778,485
6
Covered California High/Average/Low Performers
Covered CA Highest
Performer
81
84
88
87
Covered CA Weighted
Average
67
71
75
74
Covered CA Lowest
Performer
59
59
66
63
Covered California Plan-Specific Performance
Anthem HMO
59
62
Anthem PPO
59
61
Anthem EPO
67
63
5%
64,031
Blue Shield HMO
66
76
71
68
7%
93,322
Blue Shield PPO
65
66
70
70
25%
335,176
CCHP HMO
79
75
72
79
1%
10,013
Health Net HMO
59
69
66
72
11%
145,183
Health Net EPO
65
72
75
0%
1,396
Health Net PPO
Kaiser Permanente HMO
81
82
81
81
35%
477,683
LA Care HMO
68
79
76
73
6%
84,750
Molina Healthcare HMO
62
59
82
65
4%
56,023
Oscar Health Plan EPO
79
76
3%
35,962
Sharp Health Plan HMO
78
79
88
82
1%
17,335
Valley Health Plan HMO
72
84
79
87
1%
16,366
Western Health Advantage
HMO
68
68
66
74
1%
9,386
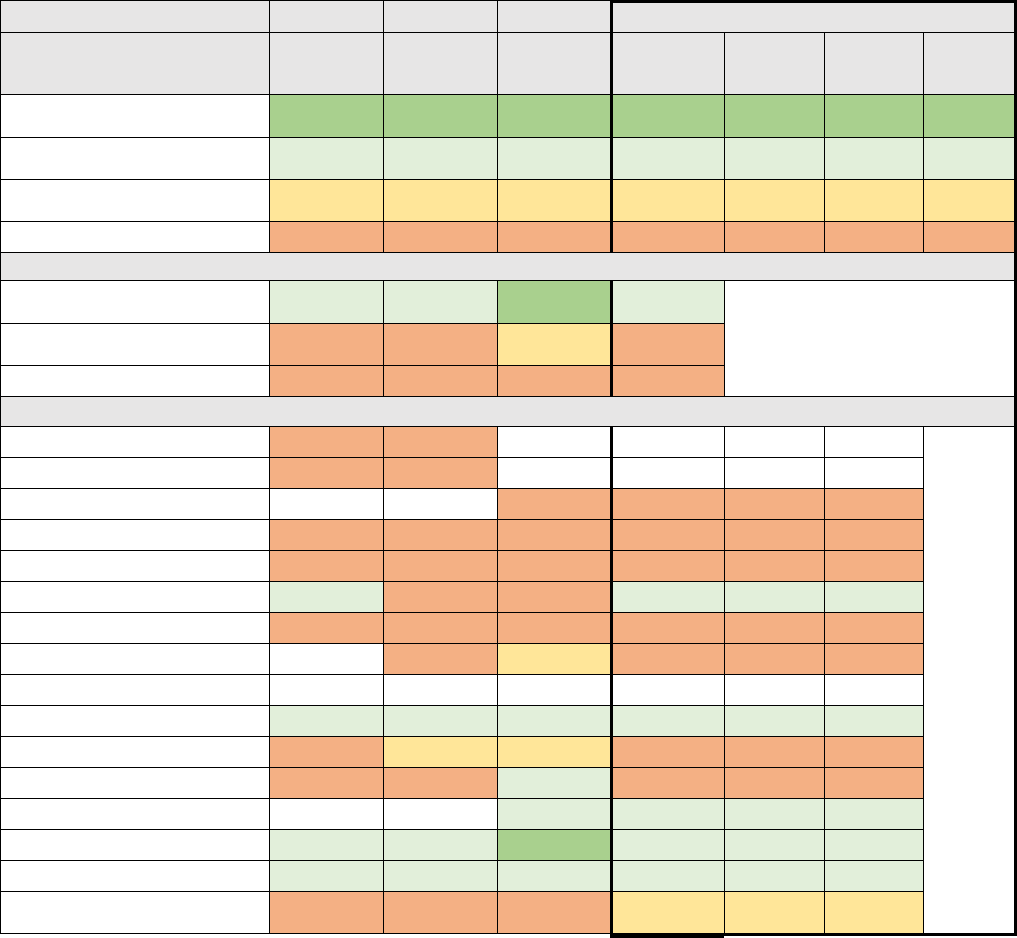
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 119
Proportion of Days Covered (Statins)
The PQA Proportion of Days Covered Statins (PDC-STA) measure is the percentage of patients 18
years and older who met the proportion of days covered threshold of 80 percent for statins during the
measurement period. Statins are a class of drugs that lower blood cholesterol to prevent cardiovascular
disease in patients with diabetes. Almost every diabetic can be on a statin. A higher rate indicates
better performance.
Table A11. Proportion of Days Covered (Statins) for Covered California Enrollees (PQA)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
77 +
78 +
80 +
82 +
0%
-
0
Plans at 50th to 90th
Percentile
67 to 77
69 to 78
71 to 80
72 to 82
41%
557,359
5
Plans at 25th to 50th
Percentile
63 to 67
64 to 69
66 to 71
68 to 72
1%
9,386
1
Plans Below 25th Percentile
Below 63
Below 64
Below 66
Below 68
58%
779,881
7
Covered California High/Average/Low Performers
Covered CA Highest
Performer
76
75
85
81
Covered CA Weighted
Average
59
63
68
68
Covered CA Lowest Performer
48
47
57
51
Covered California Plan-Specific Performance
Anthem HMO
49
52
Anthem PPO
53
55
Anthem EPO
64
57
5%
64,031
Blue Shield HMO
48
62
62
60
7%
93,322
Blue Shield PPO
57
58
63
64
25%
335,176
CCHP HMO
69
63
61
74
1%
10,013
Health Net HMO
52
60
57
63
11%
145,183
Health Net EPO
63
66
66
0%
1,396
Health Net PPO
Kaiser Permanente HMO
73
75
75
76
35%
477,683
LA Care HMO
60
68
67
63
6%
84,750
Molina Healthcare HMO
52
47
74
51
4%
56,023
Oscar Health Plan EPO
72
73
3%
35,962
Sharp Health Plan HMO
76
75
85
79
1%
17,335
Valley Health Plan HMO
70
75
71
81
1%
16,366
Western Health Advantage
HMO
60
62
61
69
1%
9,386
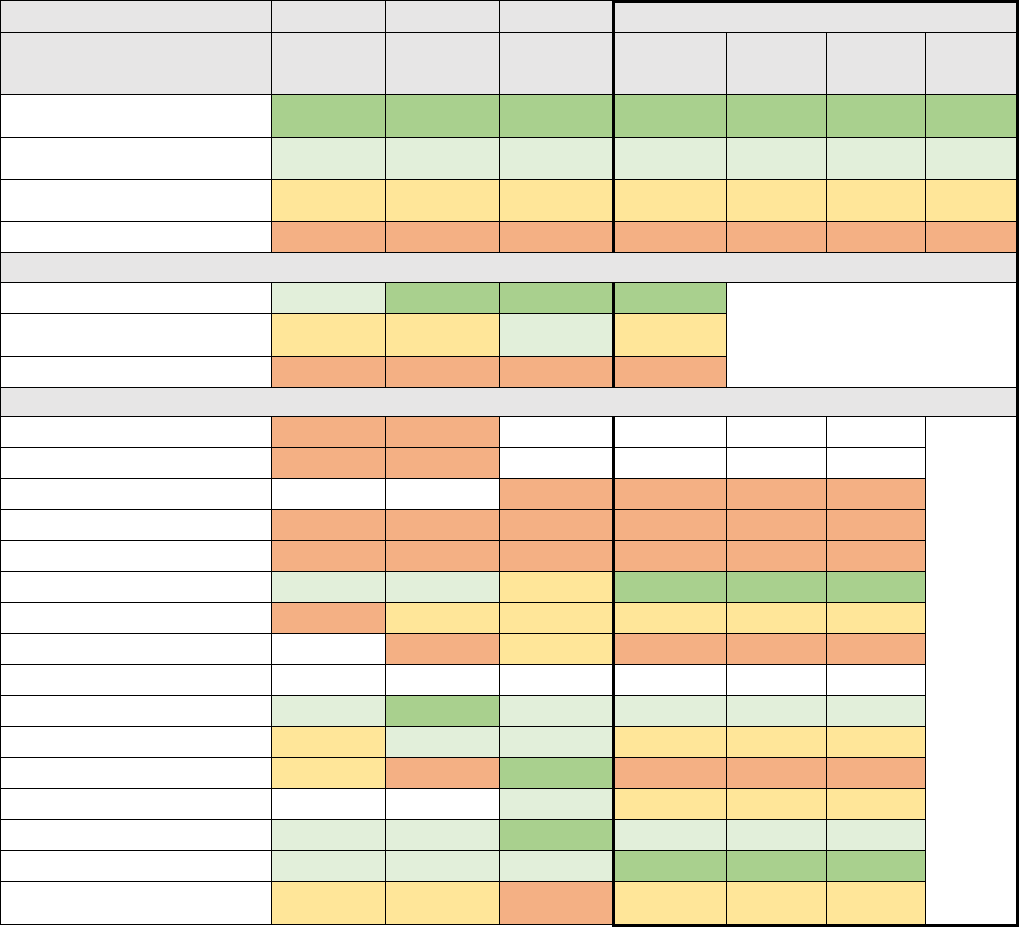
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 120
Proportion of Days Covered (Diabetes All Class)
The PQA Proportion of Days Covered Diabetes All Class (PDC-DR) measure is the percentage of
patients 18 years and older who met the proportion of days covered threshold of 80 percent for
diabetes medications during the measurement period. These medications control blood sugar. Nearly
every diabetic patient will be prescribed a medication in this group. A higher rate indicates better
performance.
Table A12. Proportion of Days Covered (Diabetes All Class) for Covered California Enrollees (PQA)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
79 +
79 +
80 +
82 +
2%
26,379
2
Plans at 50th to 90th
Percentile
68 to 79
69 to 79
71 to 80
72 to 82
37%
495,018
2
Plans at 25th to 50th
Percentile
61 to 68
64 to 69
66 to 71
68 to 72
20%
275,281
4
Plans Below 25th Percentile
Below 61
Below 64
Below 66
Below 68
41%
549,948
5
Covered California High/Average/Low Performers
Covered CA Highest Performer
77
80
87
86
Covered CA Weighted
Average
63
68
72
71
Covered CA Lowest Performer
55
50
61
57
Covered California Plan-Specific Performance
Anthem HMO
55
60
Anthem PPO
56
57
Anthem EPO
63
58
5%
64,031
Blue Shield HMO
60
59
65
65
7%
93,322
Blue Shield PPO
60
61
66
66
25%
335,176
CCHP HMO
77
77
69
86
1%
10,013
Health Net HMO
57
66
67
71
11%
145,183
Health Net EPO
50
67
66
0%
1,396
Health Net PPO
Kaiser Permanente HMO
77
80
79
78
35%
477,683
LA Care HMO
66
78
75
71
6%
84,750
Molina Healthcare HMO
64
56
81
57
4%
56,023
Oscar Health Plan EPO
76
70
3%
35,962
Sharp Health Plan HMO
73
74
87
80
1%
17,335
Valley Health Plan HMO
75
76
76
85
1%
16,366
Western Health Advantage
HMO
64
64
61
71
1%
9,386
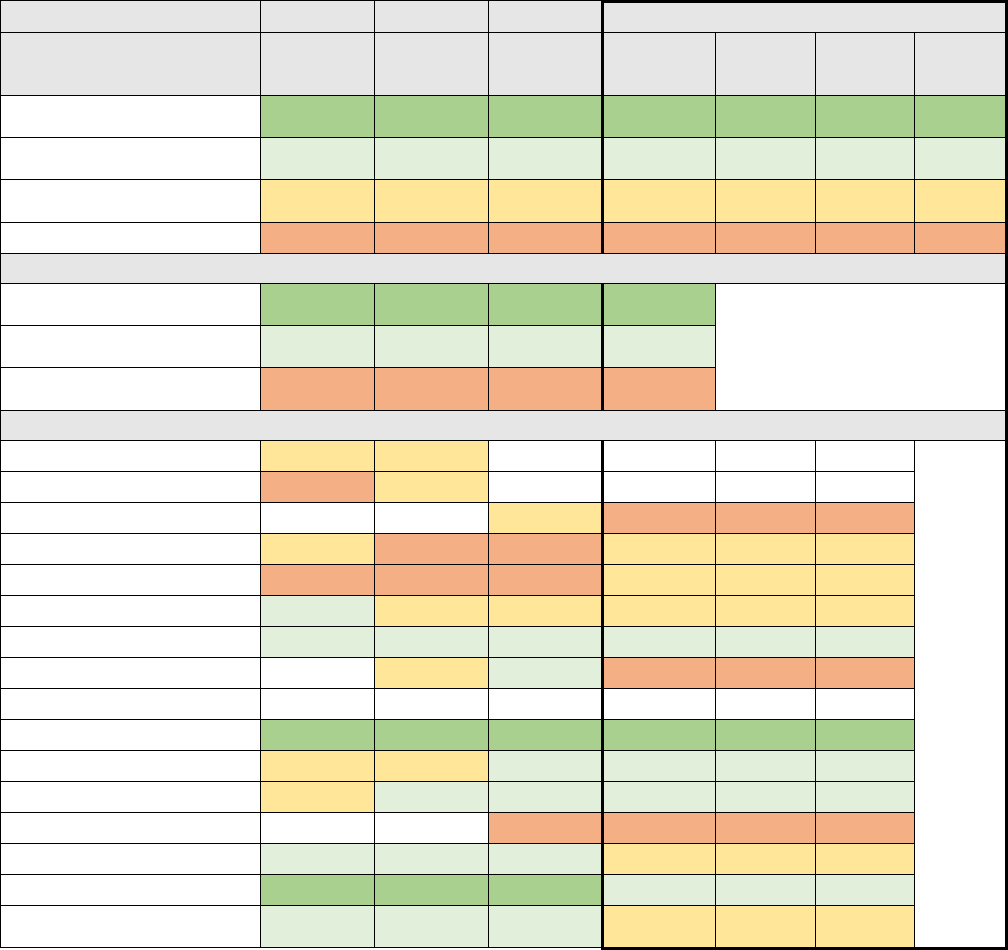
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 121
Comprehensive Diabetes Care: Eye Exam (Retinal) Performed
The Comprehensive Diabetes Care: Eye Exam (Retinal) Performed measure is the percentage of
members 18-75 years of age with diabetes (type 1 and type 2) who had an eye exam (retinal)
performed that screened or monitored for diabetic retinal disease.
Table A13. Comprehensive Diabetes Care: Eye Exam (Retinal) Performed for Covered California Enrollees
(HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
64 +
65 +
65 +
66 +
35%
477,683
1
Plans at 50th to 90th
Percentile
43 to 64
45 to 65
48 to 65
49 to 66
22%
302,322
4
Plans at 25th to 50th
Percentile
35 to 43
37 to 45
38 to 48
41 to 49
35%
465,232
5
Plans Below 25th Percentile
Below 35
Below 37
Below 38
Below 41
8%
101,389
3
Covered California High/Average/Low Performers
Covered CA Highest
Performer
74
74
74
77
Covered CA Weighted
Average
47
50
53
57
Covered CA Lowest
Performer
34
28
33
29
Covered California Plan-Specific Performance
Anthem HMO
38
43
Anthem PPO
34
37
Anthem EPO
38
36
5%
64,031
Blue Shield HMO
37
33
33
46
7%
93,322
Blue Shield PPO
35
28
37
41
25%
335,176
CCHP HMO
46
38
44
46
1%
10,013
Health Net HMO
51
51
52
49
11%
145,183
Health Net EPO
39
52
29
0%
1,396
Health Net PPO
Kaiser Permanente HMO
74
74
74
77
35%
477,683
LA Care HMO
39
43
48
60
6%
84,750
Molina Healthcare HMO
41
46
50
51
4%
56,023
Oscar Health Plan EPO
33
30
3%
35,962
Sharp Health Plan HMO
51
48
50
48
1%
17,335
Valley Health Plan HMO
71
67
67
60
1%
16,366
Western Health Advantage
HMO
54
47
52
48
1%
9,386
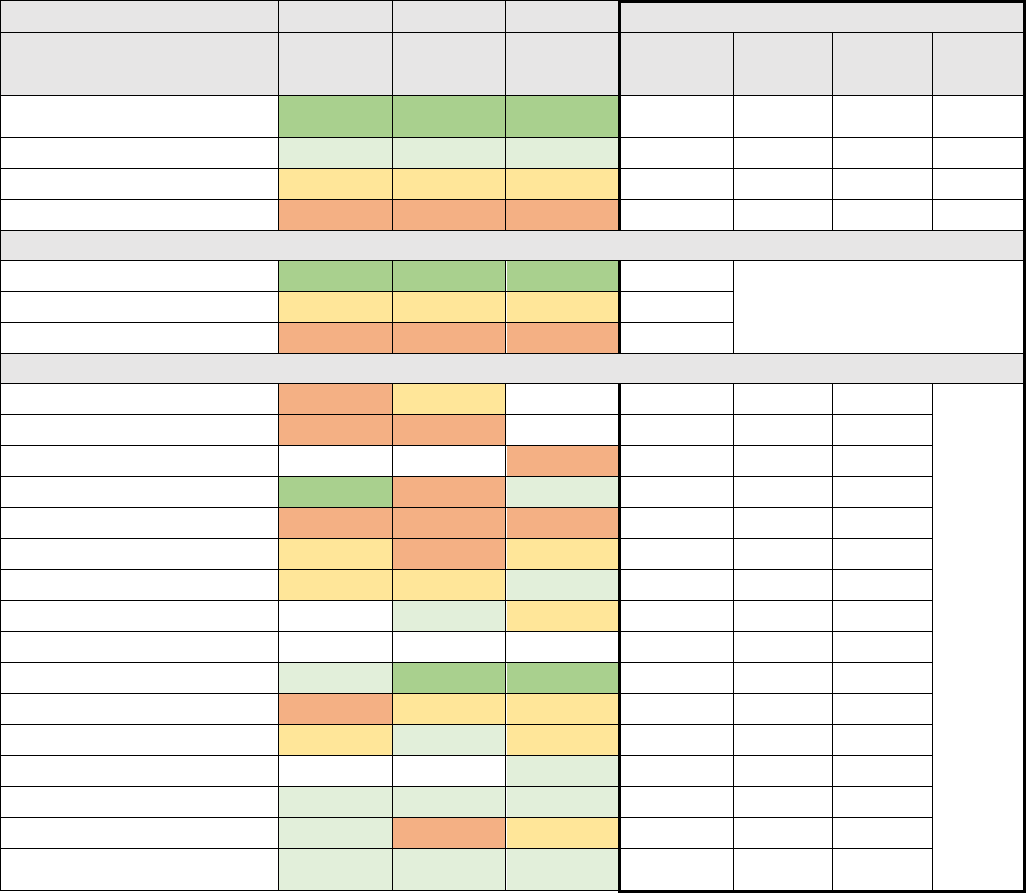
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 122
Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Testing
The Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Testing measure is the percentage of
members 18-75 years of age with diabetes (type 1 and type 2) who had a hemoglobin A1c (HbA1c)
test.
Table A14. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Testing for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
96 +
95 +
95 +
-
0
Plans at 50th to 90th Percentile
92 to 96
92 to 95
92 to 95
-
0
Plans at 25th to 50th Percentile
89 to 92
90 to 92
91 to 92
-
0
Plans Below 25th Percentile
Below 89
Below 90
Below 91
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
96
96
96
Covered CA Weighted Average
90
91
91
Covered CA Lowest Performer
87
83
85
Covered California Plan-Specific Performance
Anthem HMO
88
91
Anthem PPO
87
86
Anthem EPO
86
64,031
Blue Shield HMO
96
83
92
93,322
Blue Shield PPO
87
87
85
335,176
CCHP HMO
89
87
91
10,013
Health Net HMO
91
90
92
145,183
Health Net EPO
94
91
1,396
Health Net PPO
Kaiser Permanente HMO
96
96
96
477,683
LA Care HMO
87
91
91
84,750
Molina Healthcare HMO
90
93
91
56,023
Oscar Health Plan EPO
93
35,962
Sharp Health Plan HMO
93
94
95
17,335
Valley Health Plan HMO
93
88
91
16,366
Western Health Advantage
HMO
96
92
93
9,386
*This measure was not used in determining the overall QRS rating in 2019.
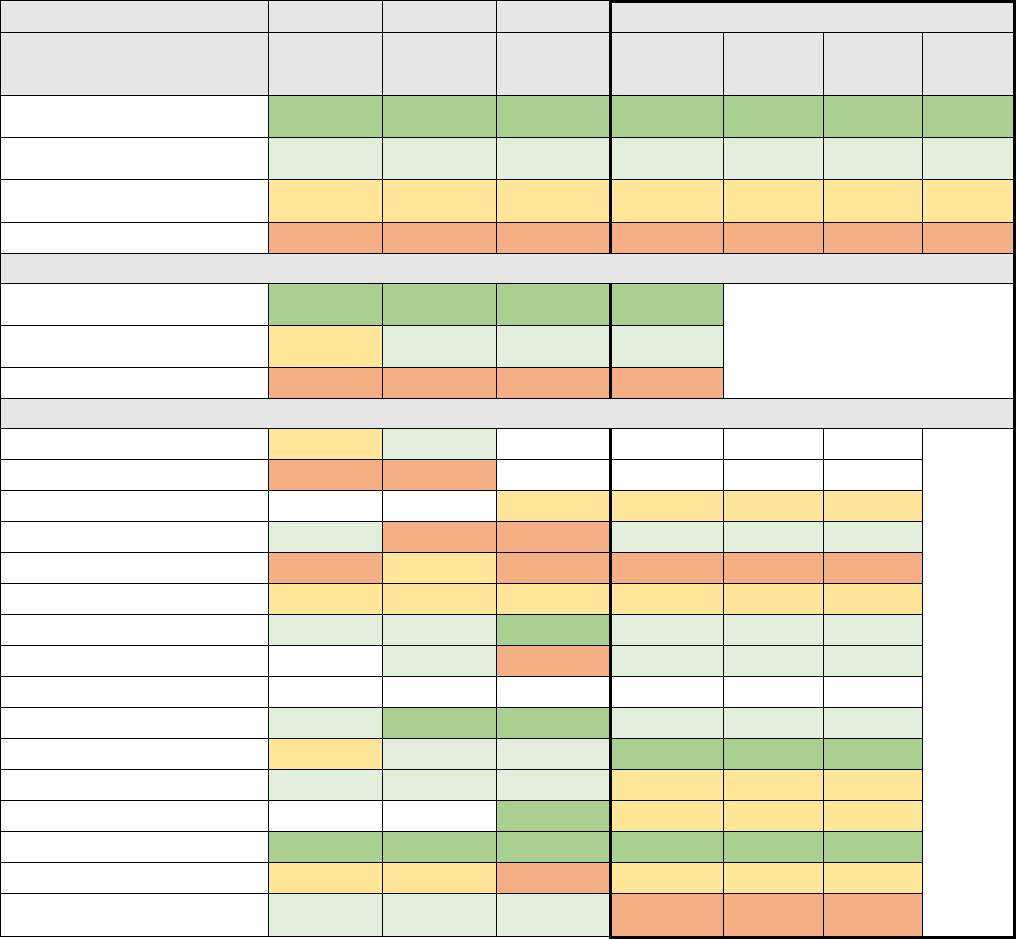
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 123
Comprehensive Diabetes Care: Medical Attention for Nephropathy
The Comprehensive Diabetes Care: Medical Attention for Nephropathy measure is the percentage of
members 18-75 years of age with diabetes (type 1 and type 2) who had medical attention for
nephropathy through a screening or monitoring test or treatment for nephropathy.
Table A15. Comprehensive Diabetes Care: Medical Attention for Nephropathy for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
94 +
94 +
94 +
95 +
8%
102,085
2
Plans at 50th to 90th
Percentile
91 to 94
91 to 94
91 to 94
91 to 95
53%
717,584
4
Plans at 25th to 50th
Percentile
89 to 91
88 to 91
89 to 91
89 to 91
14%
182,395
5
Plans Below 25th Percentile
Below 89
Below 88
Below 89
Below 89
26%
344,562
2
Covered California High/Average/Low Performers
Covered CA Highest
Performer
96
95
96
95
Covered CA Weighted
Average
90
92
92
91
Covered CA Lowest Performer
86
83
86
88
Covered California Plan-Specific Performance
Anthem HMO
90
92
Anthem PPO
87
88
Anthem EPO
89
89
5%
64,031
Blue Shield HMO
92
83
89
94
7%
93,322
Blue Shield PPO
86
89
87
88
25%
335,176
CCHP HMO
90
90
91
89
1%
10,013
Health Net HMO
92
93
95
94
11%
145,183
Health Net EPO
92
86
91
0%
1,396
Health Net PPO
Kaiser Permanente HMO
94
94
94
93
35%
477,683
LA Care HMO
90
94
94
95
6%
84,750
Molina Healthcare HMO
93
93
93
90
4%
56,023
Oscar Health Plan EPO
94
90
3%
35,962
Sharp Health Plan HMO
96
95
96
95
1%
17,335
Valley Health Plan HMO
89
89
89
90
1%
16,366
Western Health Advantage
HMO
92
92
91
88
1%
9,386
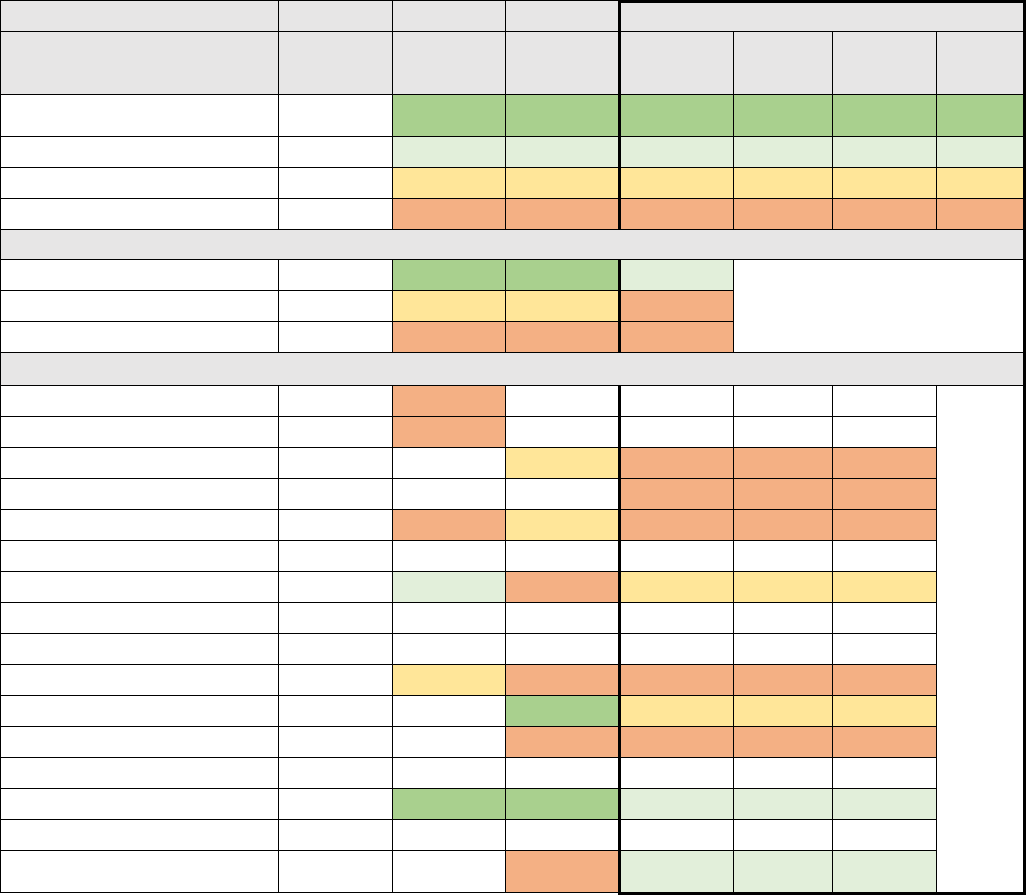
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 124
Medication Management for People with Asthma (75% of Treatment Period)
The Medication Management for People with Asthma (75% of Treatment Period) measure is
percentage of members 5–64 years of age during the measurement year who were identified as having
persistent asthma and who remained on an asthma controller medication for at least 75% of their
treatment period.
Table A16. Medication Management for Covered California Enrollees with Asthma (75% of Treatment
Period) (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
63 +
67 +
68 +
0%
-
0
Plans at 50th to 90th Percentile
MN-S
53 to 63
56 to 67
57 to 68
2%
26,721
2
Plans at 25th to 50th Percentile
MN-S
48 to 53
49 to 56
51 to 57
18%
229,933
2
Plans Below 25th Percentile
MN-S
Below 48
Below 49
Below 51
80%
1,026,235
5
Covered California High/Average/Low Performers
Covered CA Highest Performer
65
64
78
62
Covered CA Weighted Average
49
49
51
50
Covered CA Lowest Performer
44
44
47
38
Covered California Plan-Specific Performance
Anthem HMO
44
44
Anthem PPO
51
44
Anthem EPO
50
45
5%
64,031
Blue Shield HMO
49
7%
93,322
Blue Shield PPO
45
46
50
50
26%
335,176
CCHP HMO
Health Net HMO
65
57
47
52
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
46
48
49
50
37%
477,683
LA Care HMO
78
53
7%
84,750
Molina Healthcare HMO
49
38
4%
56,023
Oscar Health Plan EPO
Sharp Health Plan HMO
54
64
68
62
1%
17,335
Valley Health Plan HMO
Western Health Advantage
HMO
49
58
1%
9,386
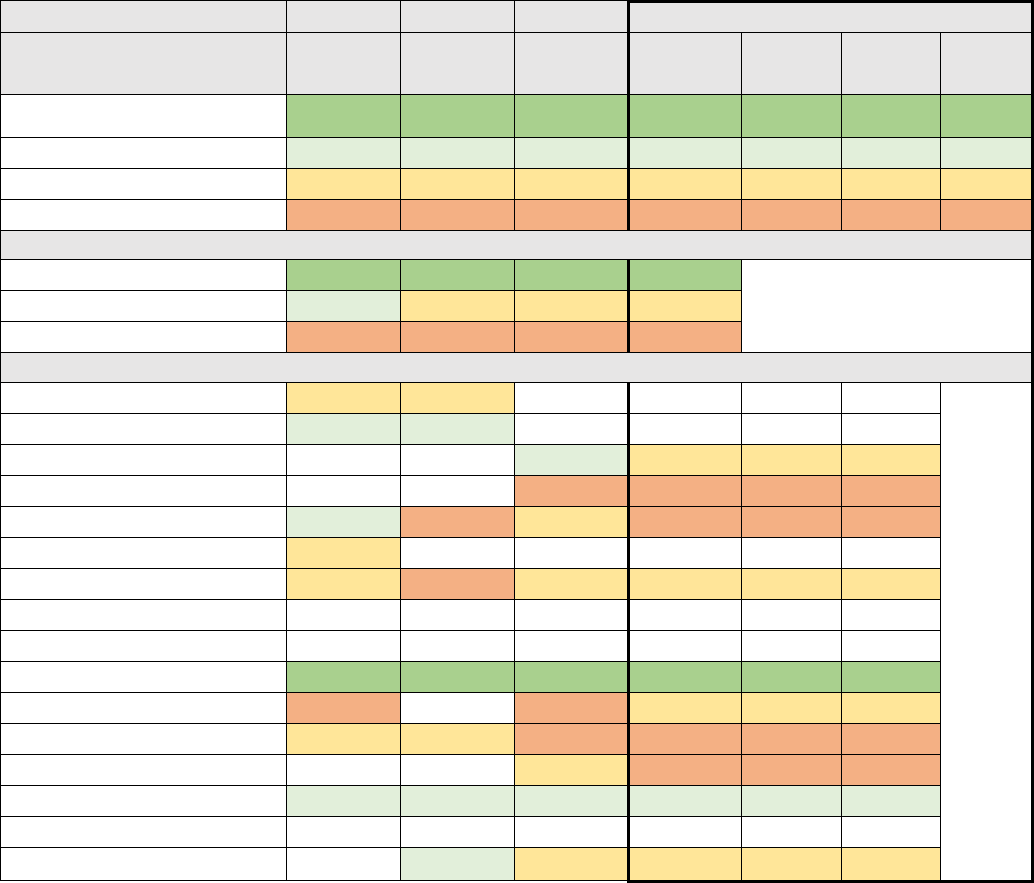
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 125
Prenatal and Postpartum Care: Postpartum Care
The Prenatal and Postpartum Care: Postpartum Care measure is the percentage of deliveries that had
a postpartum visit on or between 21 and 56 days after delivery.
Table A17. Prenatal and Postpartum Care: Postpartum Care for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
86 +
87 +
87 +
88 +
36%
477,683
1
Plans at 50th to 90th Percentile
70 to 86
74 to 87
75 to 87
74 to 88
1%
17,335
1
Plans at 25th to 50th Percentile
60 to 70
65 to 74
65 to 75
66 to 74
23%
303,350
4
Plans Below 25th Percentile
Below 60
Below 65
Below 65
Below 66
39%
520,483
4
Covered California High/Average/Low Performers
Covered CA Highest Performer
88
87
87
88
Covered CA Weighted Average
73
72
73
73
Covered CA Lowest Performer
38
59
43
59
Covered California Plan-Specific Performance
Anthem HMO
61
66
Anthem PPO
71
75
Anthem EPO
76
70
5%
64,031
Blue Shield HMO
43
62
7%
93,322
Blue Shield PPO
71
63
68
63
25%
335,176
CCHP HMO
65
Health Net HMO
64
59
70
66
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
88
87
87
88
36%
477,683
LA Care HMO
38
63
69
6%
84,750
Molina Healthcare HMO
60
67
61
59
4%
56,023
Oscar Health Plan EPO
71
65
3%
35,962
Sharp Health Plan HMO
78
80
78
83
1%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
79
72
67
1%
9,386
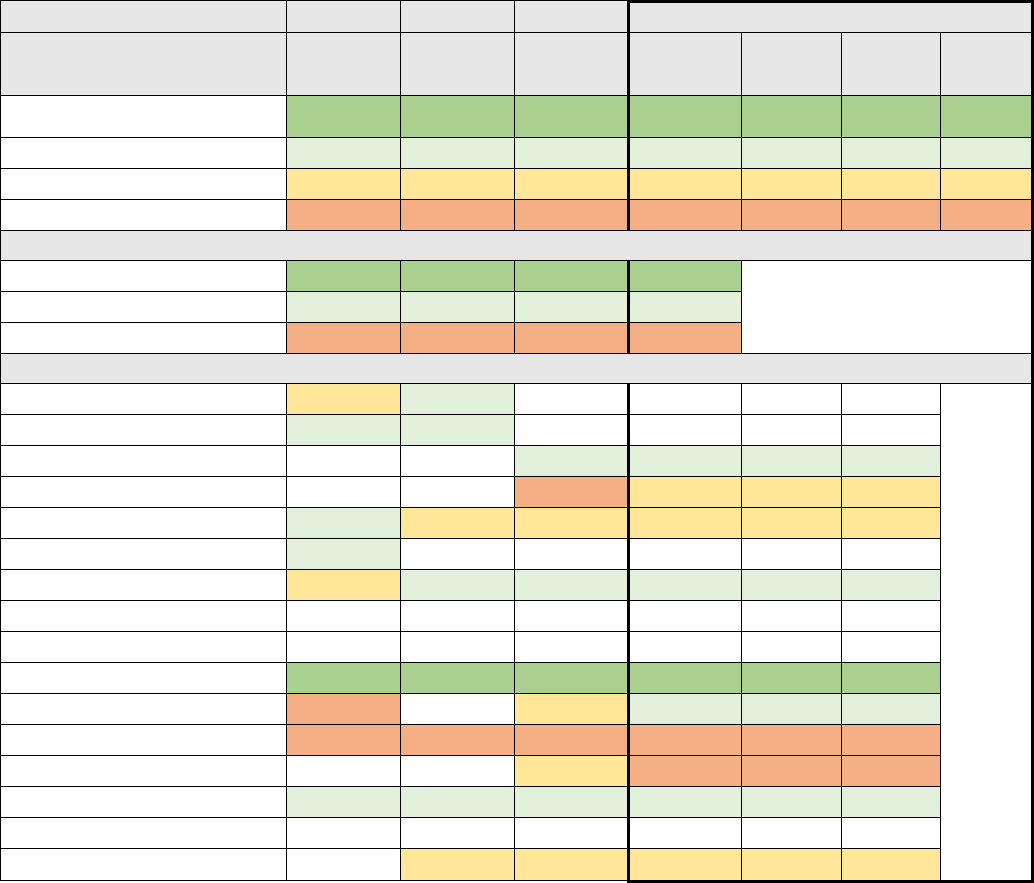
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 126
Prenatal and Postpartum Care: Timeliness of Prenatal Care
The Prenatal and Postpartum Care: Timeliness of Prenatal Care measure is the percentage of
deliveries that received a prenatal care visit as a member of the organization in the first trimester, on
the enrollment start date or within 42 days of enrollment in the organization.
Table A18. Prenatal and Postpartum Care: Timeliness of Prenatal Care for Covered California Enrollees
(HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
93 +
96 +
95 +
95 +
36%
477,683
1
Plans at 50th to 90th Percentile
81 to 93
85 to 96
84 to 95
85 to 95
24%
311,299
4
Plans at 25th to 50th Percentile
71 to 81
76 to 85
76 to 84
77 to 85
33%
437,884
3
Plans Below 25th Percentile
Below 71
Below 76
Below 76
Below 77
7%
91,985
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
96
96
96
96
Covered CA Weighted Average
85
85
86
88
Covered CA Lowest Performer
47
74
52
73
Covered California Plan-Specific Performance
Anthem HMO
77
87
Anthem PPO
85
90
Anthem EPO
88
86
5%
64,031
Blue Shield HMO
52
78
7%
93,322
Blue Shield PPO
83
76
83
84
25%
335,176
CCHP HMO
87
Health Net HMO
79
87
85
88
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
96
96
96
96
36%
477,683
LA Care HMO
47
80
88
6%
84,750
Molina Healthcare HMO
60
74
71
73
4%
56,023
Oscar Health Plan EPO
84
74
3%
35,962
Sharp Health Plan HMO
93
92
94
92
1%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
81
83
78
1%
9,386
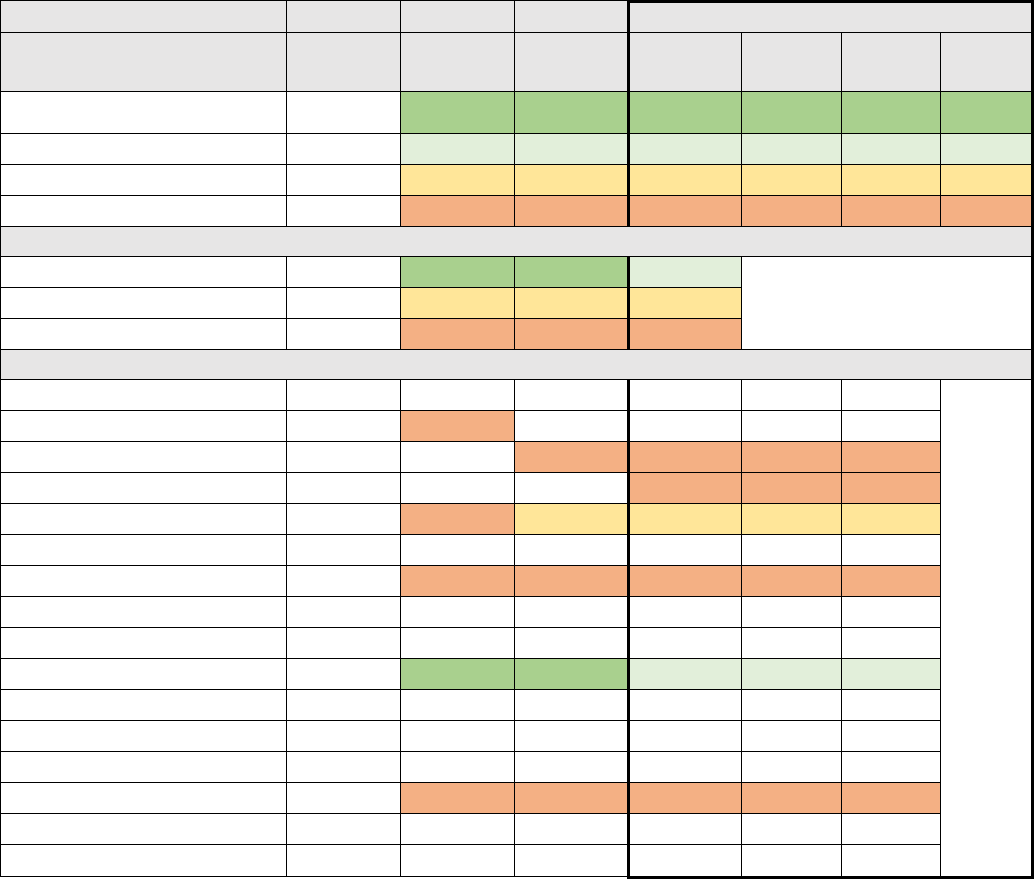
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 127
Well-Child Visits in the First 15 Months of Life (6 or More Visits)
The Well-Child Visits in the First 15 Months of Life (6 or More Visits) measure is the percentage of
members who turned 15 months old during the measurement year and who had six or more well-child
visits with a PCP during their first 15 months of life.
Table A19. Well-Child Visits in the First 15 Months of Life (6 or More Visits) for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
88 +
87 +
89 +
0%
-
0
Plans at 50th to 90th Percentile
MN-S
78 to 88
77 to 87
75 to 89
42%
477,683
1
Plans at 25th to 50th Percentile
MN-S
68 to 78
67 to 77
66 to 75
30%
335,176
1
Plans Below 25th Percentile
MN-S
Below 68
Below 67
Below 66
28%
319,871
4
Covered California High/Average/Low Performers
Covered CA Highest Performer
92
89
87
87
Covered CA Weighted Average
57
69
70
72
Covered CA Lowest Performer
20
33
28
36
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
51
67
Anthem EPO
65
62
6%
64,031
Blue Shield HMO
64
8%
93,322
Blue Shield PPO
50
64
68
72
30%
335,176
CCHP HMO
Health Net HMO
20
33
28
36
13%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
92
89
87
87
42%
477,683
LA Care HMO
Molina Healthcare HMO
Oscar Health Plan EPO
Sharp Health Plan HMO
33
59
53
66
2%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
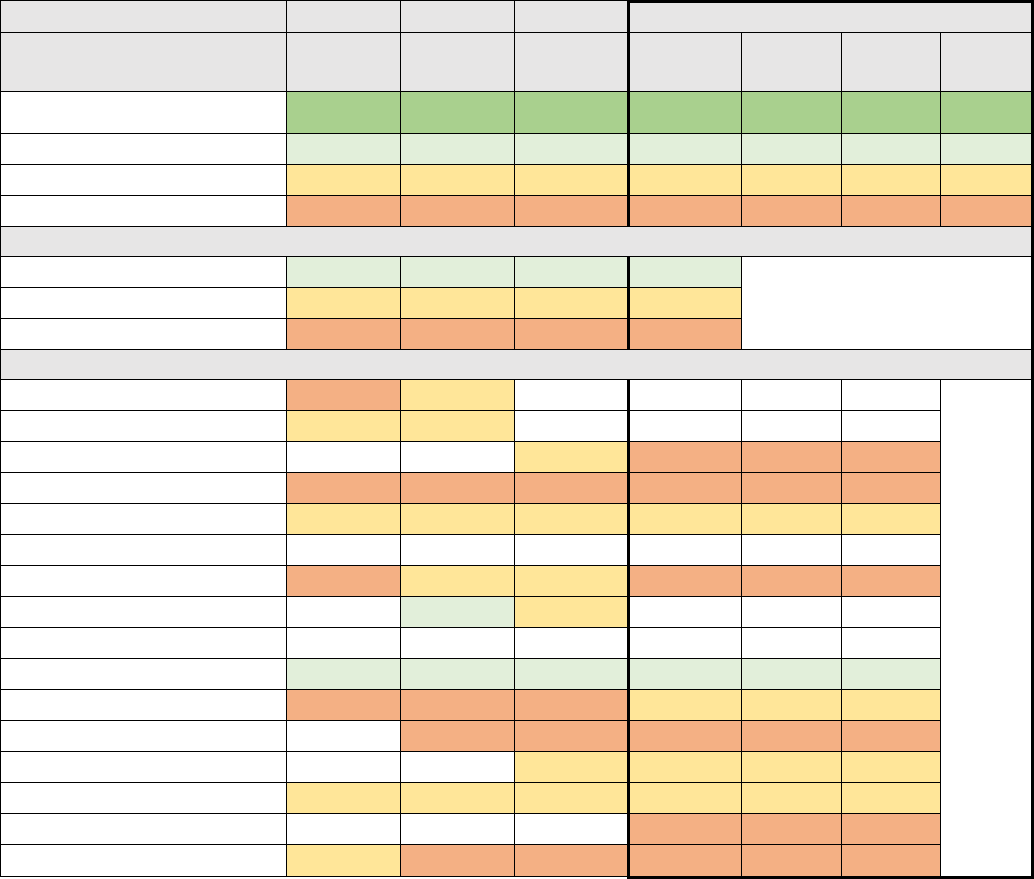
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 128
Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life
The Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life measure is the percentage of
members 3–6 years of age who had one or more well-child visits with a PCP during the measurement
year.
Table A20. Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
86 +
88 +
89 +
88 +
0%
-
0
Plans at 50th to 90th Percentile
75 to 86
76 to 88
75 to 89
76 to 88
36%
477,683
1
Plans at 25th to 50th Percentile
65 to 75
66 to 76
68 to 75
68 to 76
35%
473,223
4
Plans Below 25th Percentile
Below 65
Below 66
Below 68
Below 68
29%
384,311
6
Covered California High/Average/Low Performers
Covered CA Highest Performer
79
85
81
79
Covered CA Weighted Average
69
71
74
73
Covered CA Lowest Performer
46
57
61
50
Covered California Plan-Specific Performance
Anthem HMO
64
66
Anthem PPO
68
68
Anthem EPO
69
63
5%
64,031
Blue Shield HMO
59
64
61
65
7%
93,322
Blue Shield PPO
68
70
73
74
25%
335,176
CCHP HMO
Health Net HMO
59
67
72
66
11%
145,183
Health Net EPO
85
74
Health Net PPO
Kaiser Permanente HMO
79
79
81
79
36%
477,683
LA Care HMO
46
57
66
75
6%
84,750
Molina Healthcare HMO
66
66
58
4%
56,023
Oscar Health Plan EPO
69
74
3%
35,962
Sharp Health Plan HMO
71
68
69
75
1%
17,335
Valley Health Plan HMO
50
1%
16,366
Western Health Advantage HMO
72
57
65
66
1%
9,386
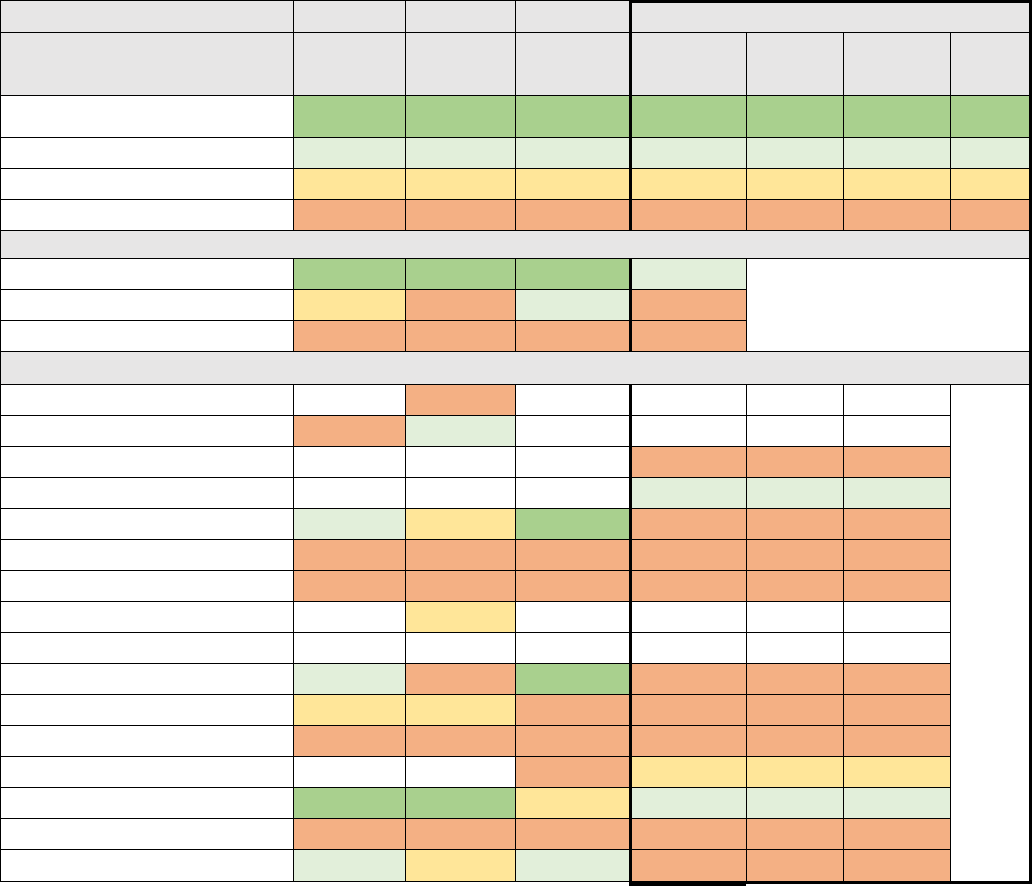
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 129
Additional Measures Related to Promotion of Effective Primary Care
In Chapter 7: Promotion of Effective Primary Care, Covered California does not indicate any potential
“Priority Measures.” The two additional QRS measures pertaining to the Promotion of Effective Primary
Care are:
Additional Measures
1. Rating of Personal Doctor (Table A21)
2. Rating of Specialist (Table A22)
Rating of Personal Doctor
The Rating of Person Doctor measure indicates enrollee experience related to the rating of personal
doctor QHP Enrollee Survey question.
Table A21: Covered California Enrollees Rating of Personal Doctor (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
91 +
92 +
91 +
90 +
0%
-
0
Plans at 50th to 90th Percentile
89 to 91
89 to 92
89 to 91
87 to 90
8%
110,657
2
Plans at 25th to 50th Percentile
88 to 89
88 to 89
88 to 89
86 to 87
3%
35,962
1
Plans Below 25th Percentile
Below 88
Below 88
Below 88
Below 86
89%
1,198,611
9
Covered California High/Average/Low Performers
Covered CA Highest Performer
91
93
92
88
Covered CA Weighted Average
88
87
90
85
Covered CA Lowest Performer
79
85
81
83
Covered California Plan-Specific Performance
Anthem HMO
85
Anthem PPO
87
90
Anthem EPO
84
5%
64,031
Blue Shield HMO
88
7%
93,322
Blue Shield PPO
90
89
92
85
25%
335,176
CCHP HMO
82
85
87
84
1%
10,013
Health Net HMO
81
85
85
83
11%
145,183
Health Net EPO
89
Health Net PPO
Kaiser Permanente HMO
91
87
92
86
36%
477,683
LA Care HMO
88
89
87
83
6%
84,750
Molina Healthcare HMO
79
85
81
83
4%
56,023
Oscar Health Plan EPO
87
87
3%
35,962
Sharp Health Plan HMO
91
93
88
87
1%
17,335
Valley Health Plan HMO
84
87
85
84
1%
16,366
Western Health Advantage HMO
90
89
89
85
1%
9,386
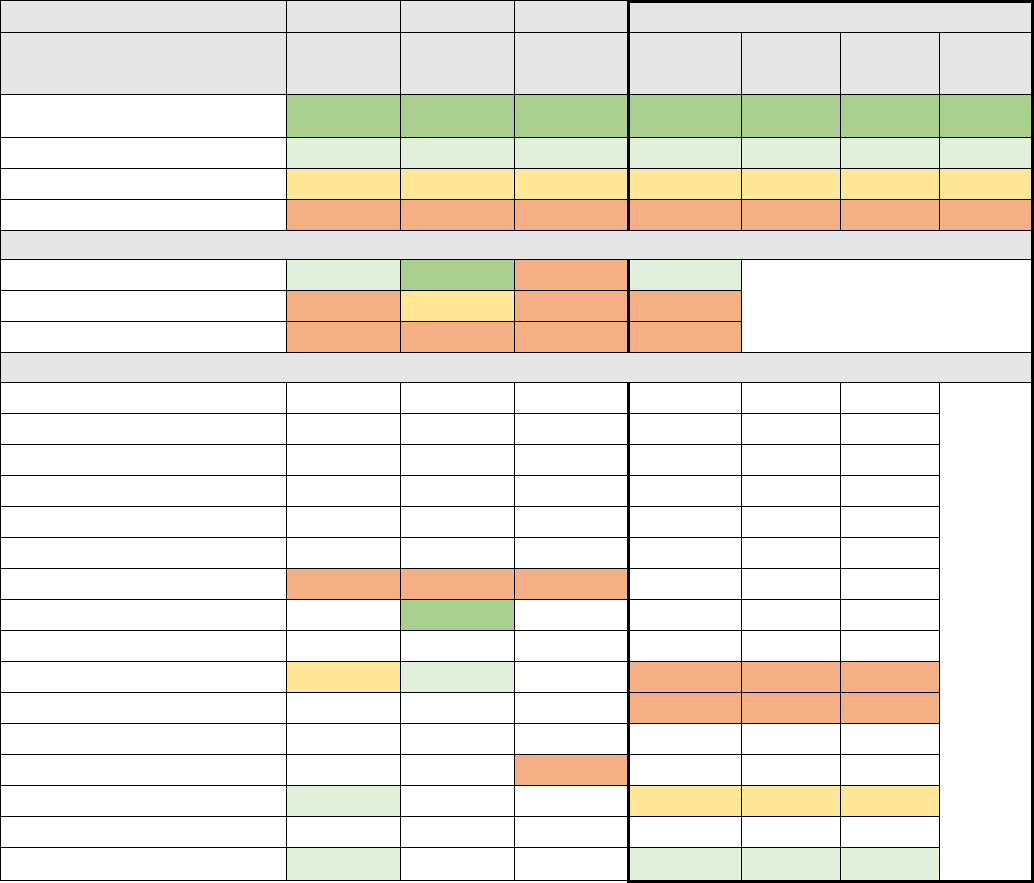
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 130
The Rating of Specialist measure indicates enrollee experience related to the rating of specialist seen
most often QHP Enrollee Survey question.
Table A22: Covered California Enrollees Rating of Specialist (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
89 +
90 +
90 +
87 +
0%
-
0
Plans at 50th to 90th Percentile
87 to 89
88 to 90
87 to 90
85 to 87
2%
9,386
1
Plans at 25th to 50th Percentile
86 to 87
87 to 88
85 to 87
84 to 85
3%
17,335
1
Plans Below 25th Percentile
Below 86
Below 87
Below 85
Below 84
95%
562,433
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
88
90
83
86
Covered CA Weighted Average
85
87
82
81
Covered CA Lowest Performer
82
81
82
81
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
Anthem EPO
Blue Shield HMO
Blue Shield PPO
CCHP
Health Net HMO
82
81
82
Health Net EPO
90
Health Net PPO
Kaiser
86
90
81
81%
477,683
LA Care
83
14%
84,750
Molina
Oscar
83
Sharp
88
85
3%
17,335
Valley
Western Health Advantage
87
86
2%
9,386
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 131
Additional Measures Related to Appropriate Interventions
In Chapter 10: Appropriate Interventions, Covered California does not indicate any potential “Priority
Measures.” The six additional QRS measures pertaining to Appropriate Interventions are:
Additional Measures
1. Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis (Table A23)
2. Appropriate Testing for Children with Pharyngitis (CWP) (Table A24)
3. Appropriate Treatment for Children with Upper Respiratory Infection (URI) (Table A25)
4. Use of Imaging Studies for Low Back Pain (Table A26)
5. Annual Monitoring for Patients on Persistent Medications (Table A270
6. Access to Information (A28)
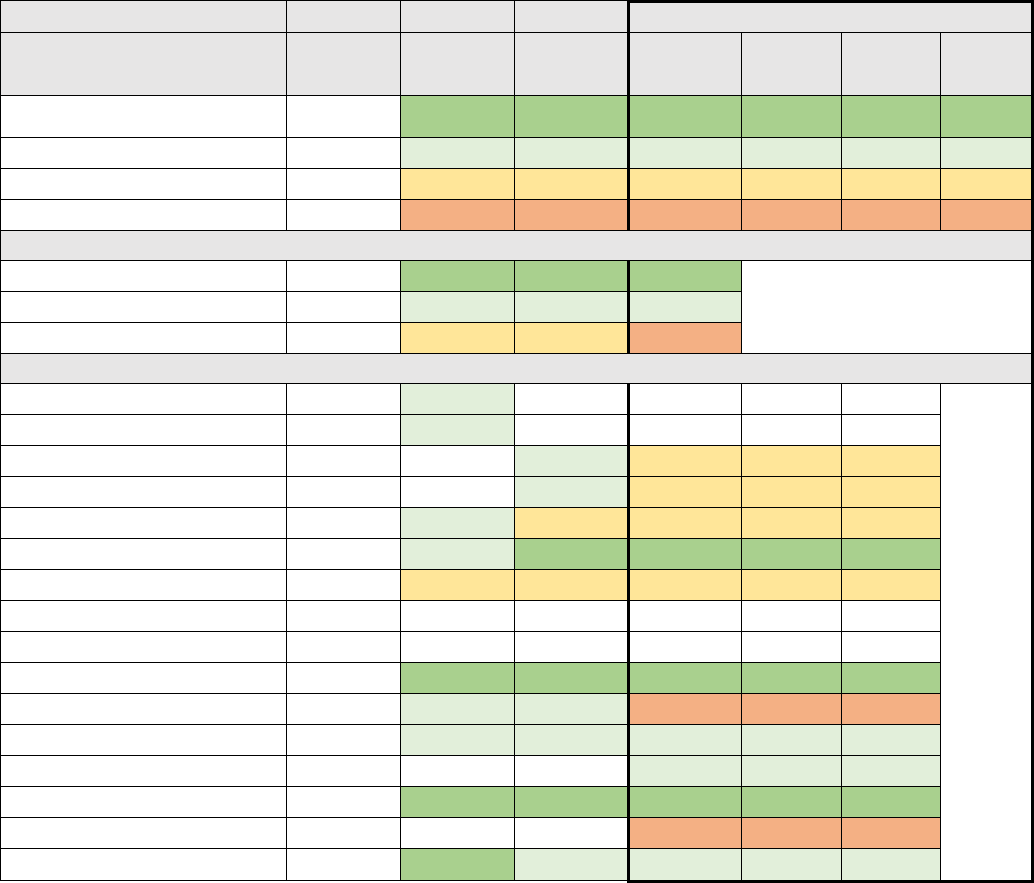
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 132
Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis
The HEDIS Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis measure assesses adults
18–64 years of age with a diagnosis of acute bronchitis who were not dispensed an antibiotic
prescription. A higher rate represents better performance.
Table A23. Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
MN-S
44 +
47 +
48 +
38%
505,031
3
Plans at 50th to 90th Percentile
MN-S
26 to 44
28 to 47
30 to 48
8%
101,371
3
Plans at 25th to 50th Percentile
MN-S
21 to 26
24 to 28
24 to 30
47%
637,712
4
Plans Below 25th Percentile
MN-S
Below 21
Below 24
Below 24
8%
101,116
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
49
52
59
59
Covered CA Weighted Average
31
35
37
38
Covered CA Lowest Performer
23
24
25
21
Covered California Plan-Specific Performance
Anthem HMO
29
26
Anthem PPO
23
28
Anthem EPO
32
27
5%
64,031
Blue Shield HMO
35
29
7%
93,322
Blue Shield PPO
27
27
28
29
25%
335,176
CCHP HMO
36
39
52
59
1%
10,013
Health Net HMO
28
24
25
29
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
47
44
49
53
36%
477,683
LA Care HMO
33
27
35
24
6%
84,750
Molina Healthcare HMO
42
31
34
4%
56,023
Oscar Health Plan EPO
31
3%
35,962
Sharp Health Plan HMO
49
52
59
53
1%
17,335
Valley Health Plan HMO
21
1%
16,366
Western Health Advantage HMO
44
43
40
1%
9,386
*M-NS: This measure was not used in determining the overall QRS rating in 2016.
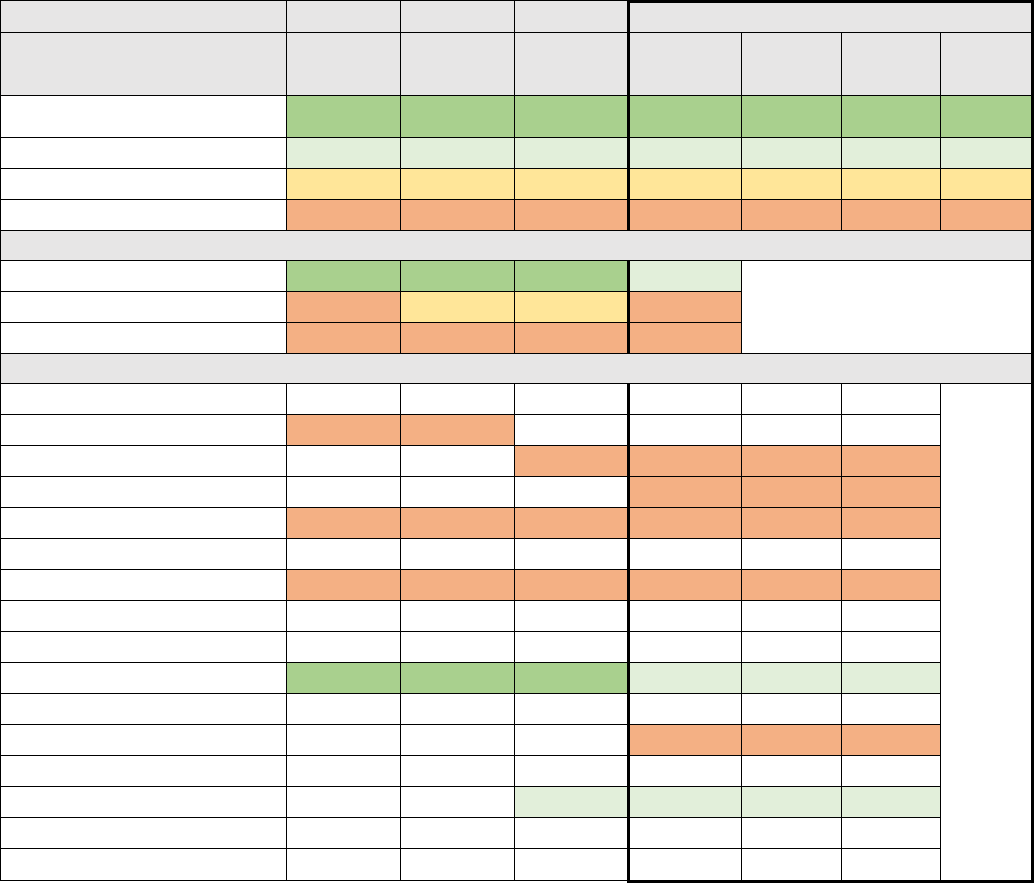
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 133
Appropriate Testing for Children with Pharyngitis
The HEDIS Appropriate Testing for Children with Pharyngitis measure assesses children 2–18 years of
age who were diagnosed with pharyngitis, dispensed an antibiotic and received a group A
streptococcus test for the episode. A higher rate represents better performance.
Table A24. Appropriate Testing for Children with Pharyngitis for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
93 +
94 +
94 +
95 +
0%
-
0
Plans at 50th to 90th Percentile
81 to 93
84 to 94
88 to 94
87 to 95
42%
495,018
2
Plans at 25th to 50th Percentile
72 to 81
76 to 84
79 to 88
80 to 87
0%
-
0
Plans Below 25th Percentile
Below 72
Below 76
Below 79
Below 80
58%
693,735
5
Covered California High/Average/Low Performers
Covered CA Highest Performer
95
94
94
93
Covered CA Weighted Average
71
79
83
79
Covered CA Lowest Performer
37
55
69
42
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
65
72
Anthem EPO
71
70
5%
64,031
Blue Shield HMO
70
8%
93,322
Blue Shield PPO
72
73
78
78
28%
335,176
CCHP HMO
Health Net HMO
37
55
69
55
12%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
95
94
94
93
40%
477,683
LA Care HMO
Molina Healthcare HMO
42
5%
56,023
Oscar Health Plan EPO
Sharp Health Plan HMO
92
92
1%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
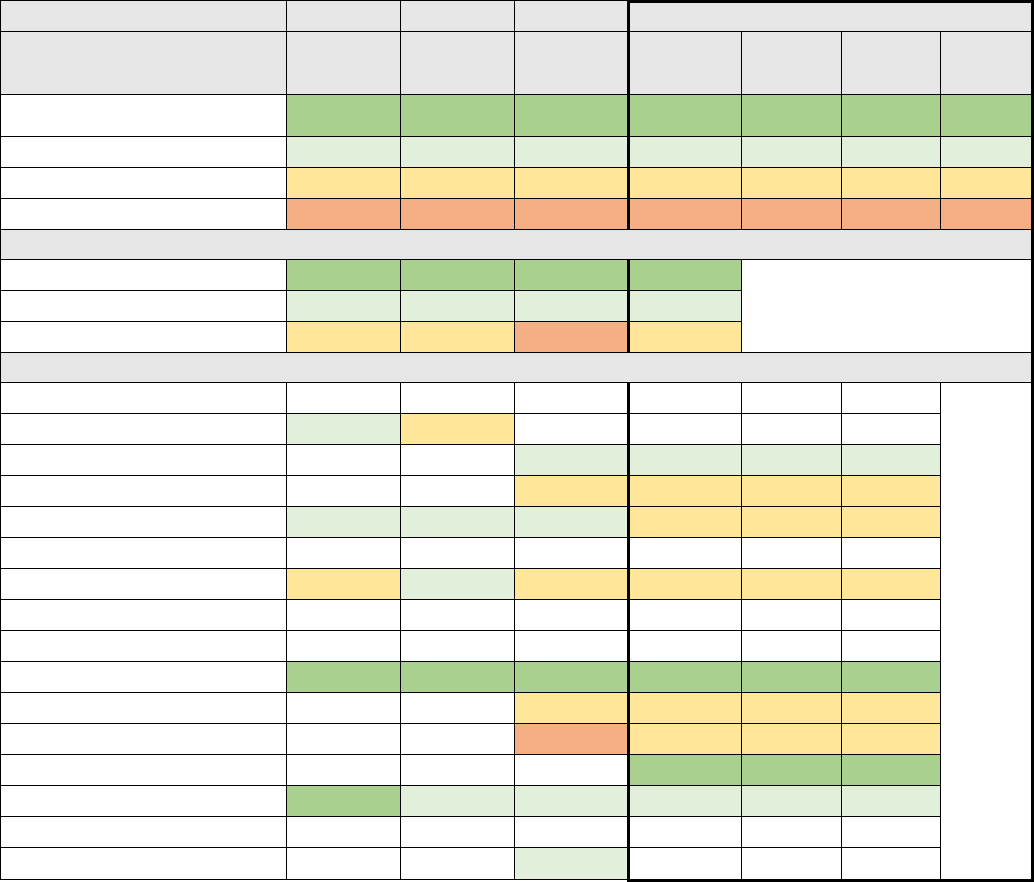
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 134
Appropriate Treatment for Children with Upper Respiratory Infection
The HEDIS Appropriate Treatment for Children with Upper Respiratory Infection measure assesses
children 3 months–18 years of age who were given a diagnosis of upper respiratory infection (URI) and
were not dispensed an antibiotic prescription. A higher rate indicates appropriate treatment of children
with URI.
Table A25. Appropriate Treatment for Children with Upper Respiratory Infection for Covered California
Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
96 +
96 +
97 +
97 +
39%
513,645
2
Plans at 50th to 90th Percentile
89 to 96
89 to 96
90 to 97
92 to 97
6%
81,366
2
Plans at 25th to 50th Percentile
82 to 89
84 to 89
84 to 90
86 to 92
55%
714,454
5
Plans Below 25th Percentile
Below 82
Below 84
Below 84
Below 86
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
98
99
98
100
Covered CA Weighted Average
92
93
93
94
Covered CA Lowest Performer
88
89
83
87
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
89
89
Anthem EPO
93
94
5%
64,031
Blue Shield HMO
86
91
7%
93,322
Blue Shield PPO
91
90
91
91
26%
335,176
CCHP HMO
Health Net HMO
88
89
88
87
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
98
99
98
99
36%
477,683
LA Care HMO
87
90
6%
84,750
Molina Healthcare HMO
83
88
4%
56,023
Oscar Health Plan EPO
100
3%
35,962
Sharp Health Plan HMO
98
92
97
96
1%
17,335
Valley Health Plan HMO
Western Health Advantage HMO
94
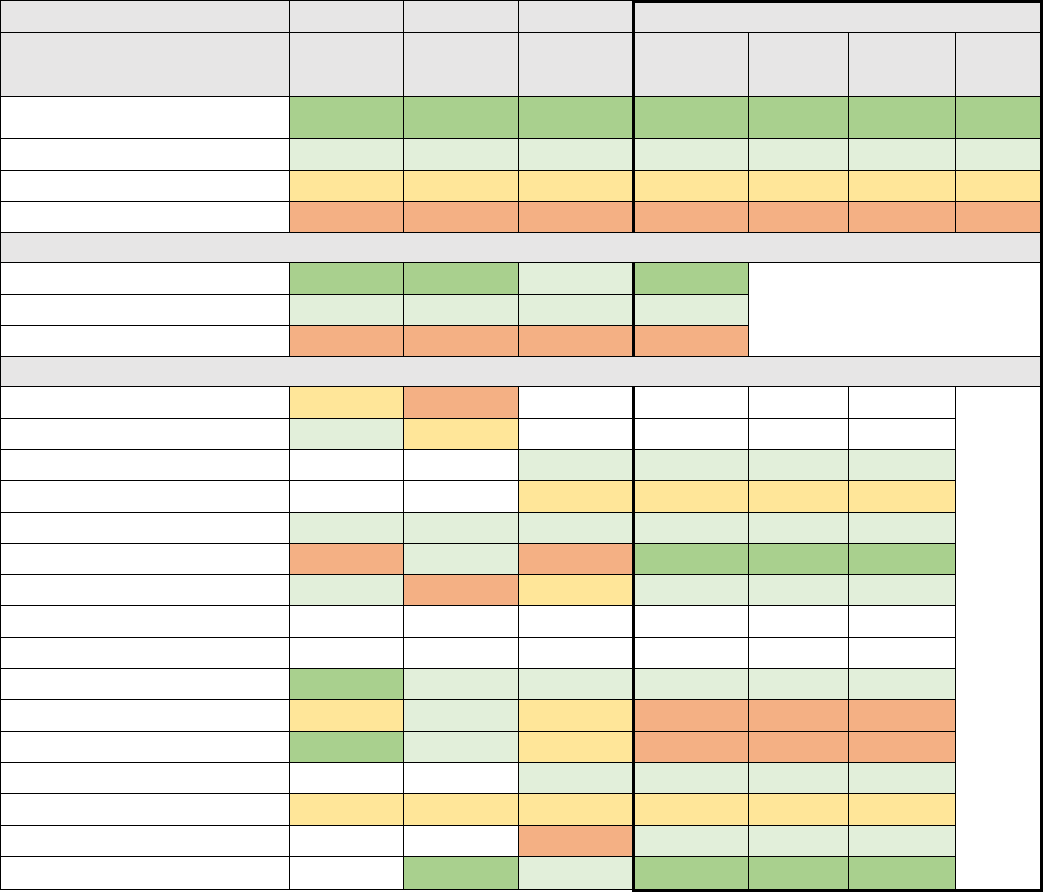
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 135
Use of Imaging Studies for Low Back Pain
The HEDIS Use of Imaging Studies for Low Back Pain measure assesses adults 18–50 years of age
with a primary diagnosis of low back pain who did not have an imaging study (plain X-ray, MRI or CT
scan) within 28 days of the diagnosis. A higher rate represents better performance.
Table A26: Use of Imaging Studies for Low Back Pain for Covered California Enrollees (HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
84 +
84 +
86 +
86 +
1%
19,399
2
Plans at 50th to 90th Percentile
75 to 84
74 to 84
76 to 86
77 to 86
80%
1,074,401
6
Plans at 25th to 50th Percentile
70 to 75
69 to 74
72 to 76
72 to 77
8%
110,657
2
Plans Below 25th Percentile
Below 70
Below 69
Below 72
Below 72
10%
140,773
2
Covered California High/Average/Low Performers
Covered CA Highest Performer
88
88
84
91
Covered CA Weighted Average
80
79
79
80
Covered CA Lowest Performer
69
69
67
71
Covered California Plan-Specific Performance
Anthem HMO
74
69
Anthem PPO
76
73
Anthem EPO
77
78
5%
64,031
Blue Shield HMO
76
77
7%
93,322
Blue Shield PPO
78
83
82
81
25%
335,176
CCHP HMO
69
82
67
91
1%
10,013
Health Net HMO
78
69
73
77
11%
145,183
Health Net EPO
Health Net PPO
Kaiser Permanente HMO
88
83
82
85
36%
477,683
LA Care HMO
73
74
76
71
6%
84,750
Molina Healthcare HMO
86
76
74
72
4%
56,023
Oscar Health Plan EPO
84
80
3%
35,962
Sharp Health Plan HMO
74
72
72
73
1%
17,335
Valley Health Plan HMO
72
78
1%
16,366
Western Health Advantage HMO
88
77
87
1%
9,386
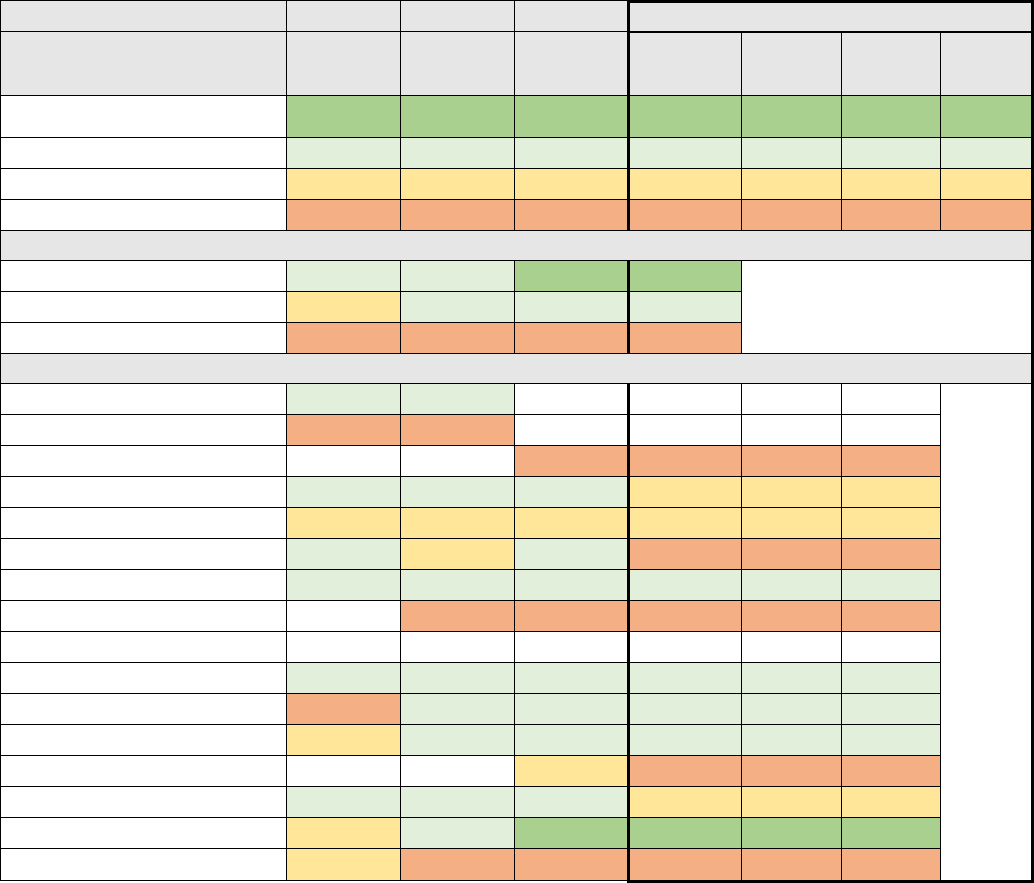
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 136
Annual Monitoring for Patients on Persistent Medications
The Annual Monitoring for Patients on Persistent Medications measure is the percentage of members
18 years of age and older who received at least 180 treatment days of ambulatory medication therapy
for a select therapeutic agent during the measurement year and at least one therapeutic monitoring
event for the therapeutic agent in the measurement year.
Table A27. Annual Monitoring for Patients on Persistent Medications for Covered California Enrollees
(HEDIS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
89 +
89 +
89 +
89 +
1%
16,366
1
Plans at 50th to 90th Percentile
84 to 89
84 to 89
84 to 89
84 to 89
57%
763,639
4
Plans at 25th to 50th Percentile
81 to 84
81 to 84
81 to 84
82 to 84
33%
445,833
3
Plans Below 25th Percentile
Below 81
Below 81
Below 81
Below 82
9%
120,788
5
Covered California High/Average/Low Performers
Covered CA Highest Performer
88
89
90
89
Covered CA Weighted Average
84
85
85
85
Covered CA Lowest Performer
77
75
77
76
Covered California Plan-Specific Performance
Anthem HMO
84
85
Anthem PPO
80
80
Anthem EPO
80
81
5%
64,031
Blue Shield HMO
84
89
85
83
7%
93,322
Blue Shield PPO
82
82
82
83
25%
335,176
CCHP HMO
86
84
85
82
1%
10,013
Health Net HMO
87
86
87
87
11%
145,183
Health Net EPO
77
77
76
0%
1,396
Health Net PPO
Kaiser Permanente HMO
88
87
88
88
35%
477,683
LA Care HMO
77
86
86
89
6%
84,750
Molina Healthcare HMO
83
89
86
84
4%
56,023
Oscar Health Plan EPO
83
77
3%
35,962
Sharp Health Plan HMO
88
89
88
82
1%
17,335
Valley Health Plan HMO
82
85
90
89
1%
16,366
Western Health Advantage HMO
83
75
80
79
1%
9,386
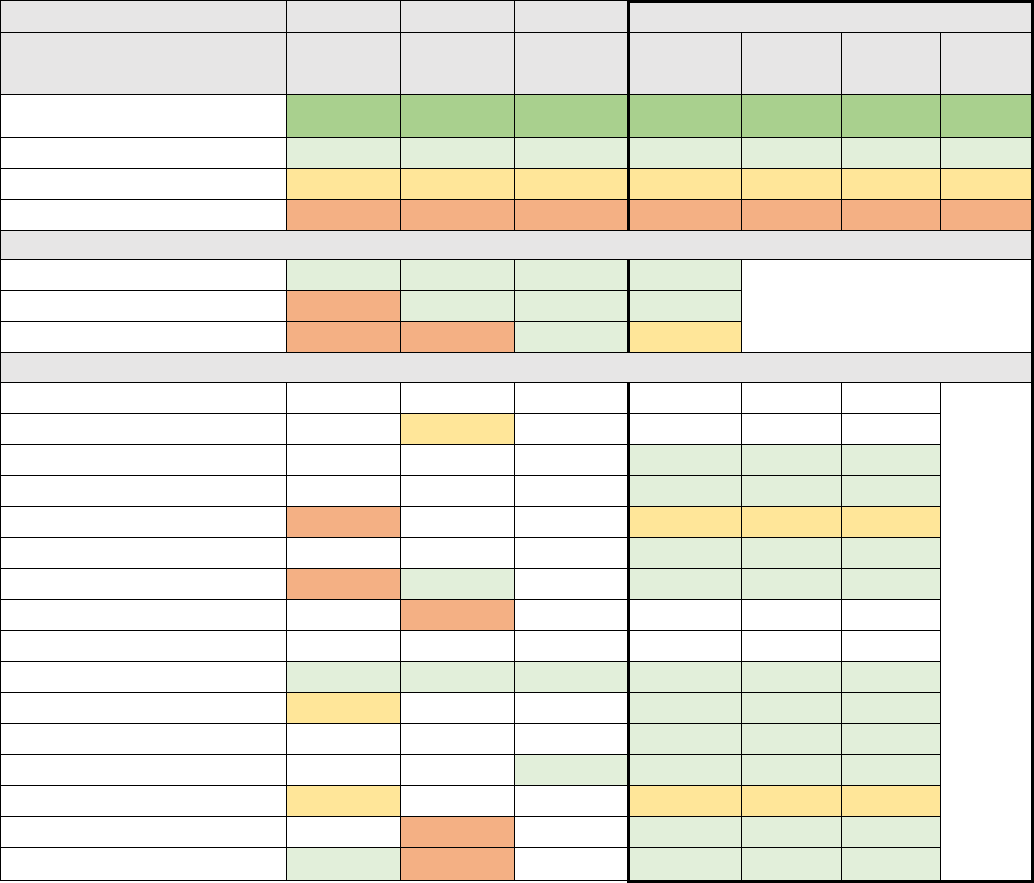
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 137
Access to Information
The Access to Information measure describes enrollee experience related to the following:
• Written materials or Internet provided information needed about how plan works;
• Found out from health plan about cost for health care service or equipment; and
• Found out from health plan about cost for specific prescriptions.
Table A28: for Covered California Enrollees’ Access to Information (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
62 +
64 +
63 +
54 +
0%
-
0
Plans at 50th to 90th Percentile
55 to 62
57 to 64
58 to 63
48 to 54
74%
992,719
10
Plans at 25th to 50th Percentile
52 to 55
54 to 57
54 to 58
44 to 48
26%
352,511
2
Plans Below 25th Percentile
Below 52
Below 54
Below 54
Below 44
0%
-
0
Covered California High/Average/Low Performers
Covered CA Highest Performer
59
61
61
53
Covered CA Weighted Average
51
59
60
50
Covered CA Lowest Performer
46
46
60
46
Covered California Plan-Specific Performance
Anthem HMO
Anthem PPO
55
Anthem EPO
50
5%
64,031
Blue Shield HMO
50
7%
93,322
Blue Shield PPO
46
46
25%
335,176
CCHP HMO
50
1%
10,013
Health Net HMO
52
61
51
11%
145,183
Health Net EPO
51
Health Net PPO
Kaiser Permanente HMO
56
59
60
53
36%
477,683
LA Care HMO
54
50
6%
84,750
Molina Healthcare HMO
49
4%
56,023
Oscar Health Plan EPO
61
53
3%
35,962
Sharp Health Plan HMO
55
46
1%
17,335
Valley Health Plan HMO
46
51
1%
16,366
Western Health Advantage HMO
59
52
48
1%
9,386
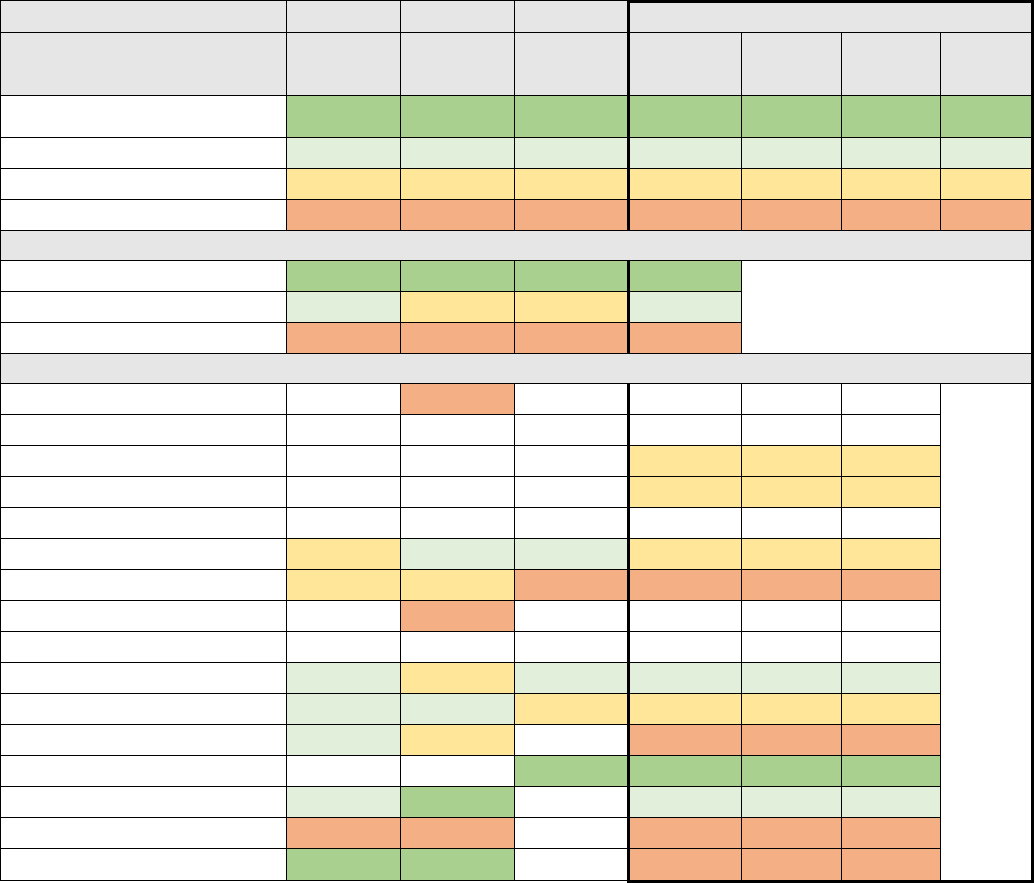
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 138
Additional Measures
Plan Administration
The Plan Administration measure (Table A 29) describes enrollee experience related to the following:
• Customer service gave necessary information/help;
• Customer service staff courteous and respectful;
• Wait-time to talk to customer service took longer than expected;
• Forms were easy to fill out; and
• Health plan explained purpose of forms.
Table A29: Plan Administration for Covered California Enrollees (CAHPS)
2016
2017
2018
2019
US
Benchmark
US
Benchmark
US
Benchmark
US
Benchmark
Percent of
Enrollees
Number of
Enrollees
Number
of Plans
Plans at 90th Percentile and
Above
77 +
79 +
79 +
76 +
4%
35,962
1
Plans at 50th to 90th Percentile
70 to 77
73 to 79
74 to 79
70 to 76
49%
495,018
2
Plans at 25th to 50th Percentile
66 to 70
68 to 73
71 to 74
67 to 70
25%
252,116
4
Plans Below 25th Percentile
Below 66
Below 68
Below 71
Below 67
22%
226,958
4
Covered California High/Average/Low Performers
Covered CA Highest Performer
79
81
80
78
Covered CA Weighted Average
74
71
74
70
Covered CA Lowest Performer
65
67
65
64
Covered California Plan-Specific Performance
Anthem HMO
68
Anthem PPO
Anthem EPO
69
6%
64,031
Blue Shield HMO
69
9%
93,322
Blue Shield PPO
CCHP HMO
68
76
75
69
1%
10,013
Health Net HMO
69
72
65
64
14%
145,183
Health Net EPO
67
Health Net PPO
Kaiser Permanente HMO
76
70
77
73
47%
477,683
LA Care HMO
70
75
73
70
8%
84,750
Molina Healthcare HMO
75
71
66
6%
56,023
Oscar Health Plan EPO
80
78
4%
35,962
Sharp Health Plan HMO
77
81
71
2%
17,335
Valley Health Plan HMO
65
67
67
2%
16,366
Western Health Advantage HMO
79
79
67
1%
9,386

Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 139
Appendix 3: 2019 Marketplace Quality Rating System Measure Set
2019 Quality Rating System Measure Set
The global quality rating is a roll-up of three summary components per the following weighting:
Summary Components
Weights
Getting Right Care (HEDIS)
66%
Members’ Care Experience (CAHPS)
17%
Plan Services (HEDIS and CAHPS)
17%
The QRS measure set is listed below indicating which measures are included in the three summary
components, the measure type and the measure source.
QRS Summary
Component
Measure Title
QRS
Measure
Type
Measurement
Source
Getting the
Right Care
Adult BMI Assessment
Clinical
HEDIS
Annual Dental Visit
Clinical
HEDIS
Annual Monitoring for Patients on Persistent
Medications
Clinical
HEDIS
Antidepressant Medication Management
Clinical
HEDIS
Breast Cancer Screening
Clinical
HEDIS
Cervical Cancer Screening
Clinical
HEDIS
Childhood Immunization Status (Combination 3)
Clinical
HEDIS
Chlamydia Screening in Women
Clinical
HEDIS
Colorectal Cancer Screening
Clinical
HEDIS
Comprehensive Diabetes Care: Eye Exam (Retinal)
Performed
Clinical
HEDIS
Comprehensive Diabetes Care: Hemoglobin A1c
(HbA1c) Control (<8.0%)
Clinical
HEDIS
Comprehensive Diabetes Care: Hemoglobin A1c
(HbA1c) Testing
Clinical
HEDIS
Comprehensive Diabetes Care: Medical Attention for
Nephropathy
Clinical
HEDIS
Controlling High Blood Pressure
Clinical
HEDIS
Flu Vaccinations for Adults Ages 18-64
Survey
QHP Enrollee
Survey
96
Follow-Up After Hospitalization for Mental Illness (7-
Day Follow-Up)
Clinical
HEDIS
Follow-Up Care for Children Prescribed ADHD
Medication
Clinical
HEDIS
Immunizations for Adolescents (Combination 2)
Clinical
HEDIS
Initiation and Engagement of Alcohol and Other Drug
Dependence Treatment
Clinical
HEDIS
Medication Management for People with Asthma
(75% of Treatment Period)
Clinical
HEDIS
96
The QHP Enrollee Survey draws heavily from the CAHPS® Health Plan Surveys, which are used widely to assess Medicare,
Medicaid, and other commercial health plan performance.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform
APPENDICIES
COVERED CALIFORNIA 140
QRS Summary
Component
Measure Title
QRS
Measure
Type
Measurement
Source
Medical Assistance with Smoking and Tobacco Use
Cessation
Survey
QHP Enrollee
Survey
Plan All-Cause Readmissions
Clinical
HEDIS
Prenatal and Postpartum Care (Postpartum Care)
Clinical
HEDIS
Prenatal and Postpartum Care (Timeliness of
Prenatal Care)
Clinical
HEDIS
Proportion of Days Covered (RAS Antagonists)
Clinical
Pharmacy Quality
Alliance (PQA)
Proportion of Days Covered (Statins)
Clinical
PQA
Proportion of Days Covered (Diabetes All Class)
Clinical
PQA
Weight Assessment and Counseling for Nutrition and
Physical Activity for Children and Adolescents
Clinical
HEDIS
Well-Child Visits in the First 15 Months of Life (6 or
More Visits)
Clinical
HEDIS
Well-Child Visits in the Third, Fourth, Fifth, and Sixth
Years of Life
Clinical
HEDIS
Member
Experience with
Their Doctors
and Care
Access to Care
Survey
QHP Enrollee
Survey
Care Coordination
Survey
QHP Enrollee
Survey
Rating of All Health Care
Survey
QHP Enrollee
Survey
Rating of Personal Doctor
Survey
QHP Enrollee
Survey
Rating of Specialist
Survey
QHP Enrollee
Survey
Plan
management of
care and
customer
service
Appropriate Testing for Children with Pharyngitis
Clinical
HEDIS
Appropriate Treatment for Children with Upper
Respiratory Infection
Clinical
HEDIS
Avoidance of Antibiotic Treatment in Adults with
Acute Bronchitis
Clinical
HEDIS
Use of Imaging Studies for Low Back Pain
Clinical
HEDIS
Access to Information
Survey
QHP Enrollee
Survey
Plan Administration
Survey
QHP Enrollee
Survey
Rating of Health Plan
Survey
QHP Enrollee
Survey
Source: Quality Rating System and Qualified Health Plan Enrollee Experience Survey: Technical Guidance for 2019
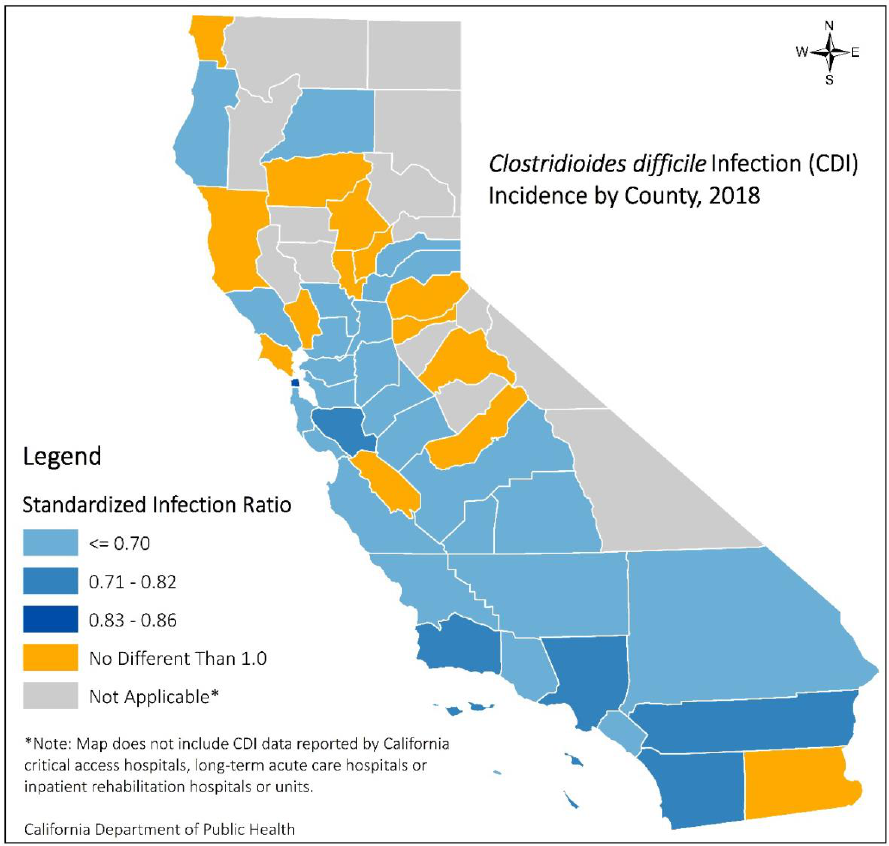
COVERED CALIFORNIA 141
Appendix 4: Additional Publicly Reported Hospital Quality and Safety Data
CDI Incidence Rates in California Counties
Clostridioides difficile (CDI) is a bacterium that causes diarrhea and inflammation of the colon. It can be
spread by healthcare workers and patients when they come in contact with contaminated surfaces.
Because CDI can spread quickly among hospitals, clinics and nursing facilities, it is important to
understand the infection rates by counties to inform prevention efforts.
The graphic below shows California counties’ CDI incidence rates for 2018 presented as significantly
lower, higher, or no different compared with the national baseline standardized infection ratio of 1.0.
Figure A1: CDI Incidence Rates in California, 2018
Source: California Department of Public Health (CDPH), November 2019
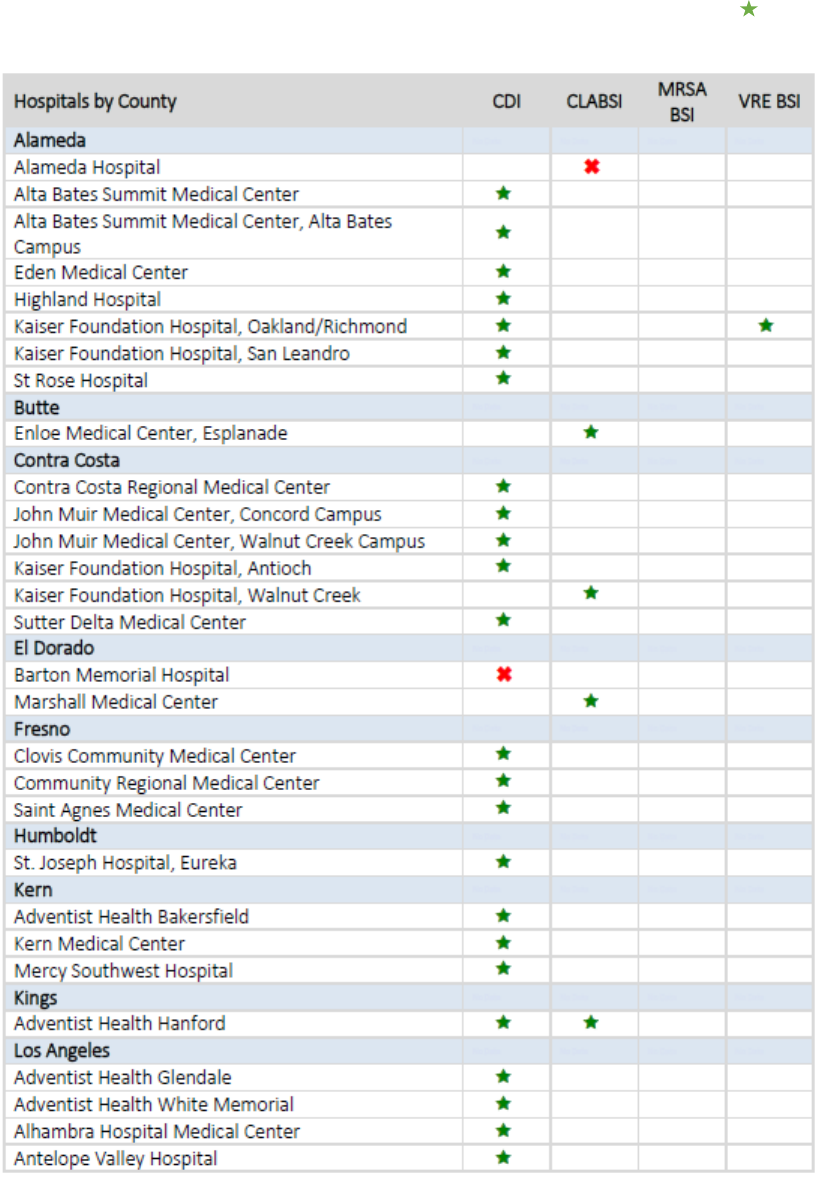
COVERED CALIFORNIA 142
California Hospitals with Hospital Associated Infection Incidence Better ( ) or Worse (x)
than National Baseline, 2018
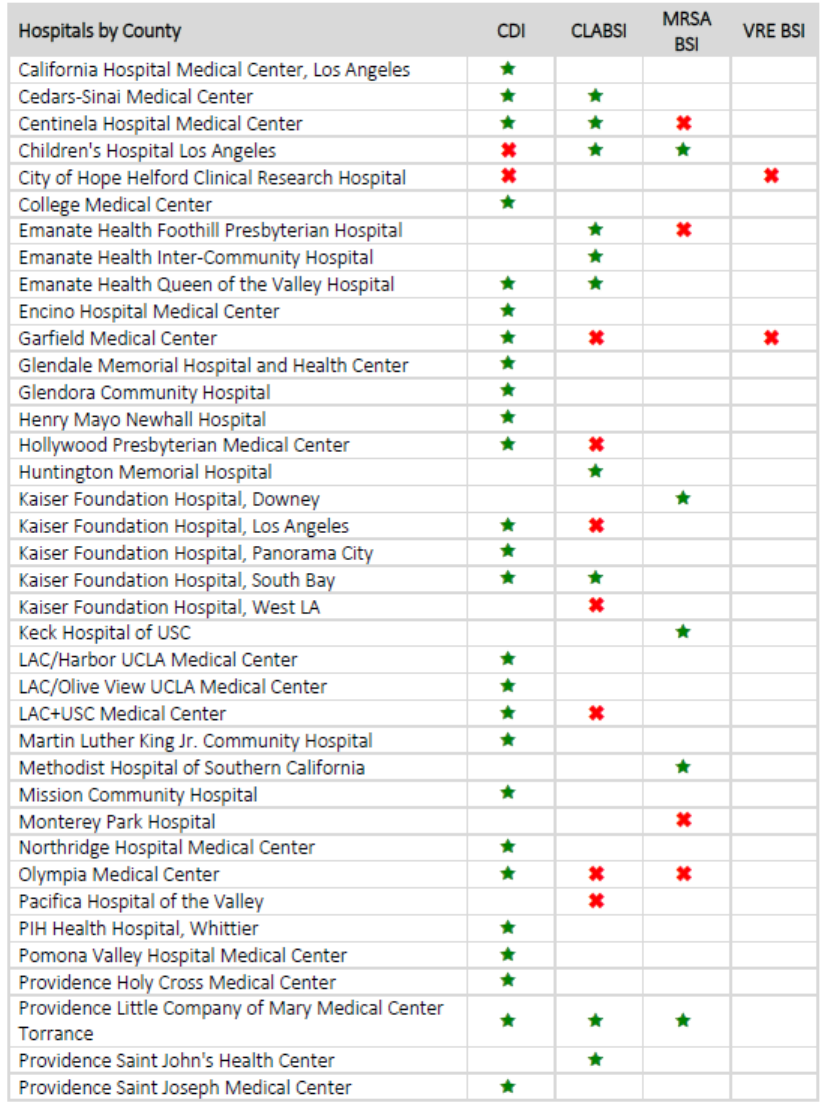
COVERED CALIFORNIA 143
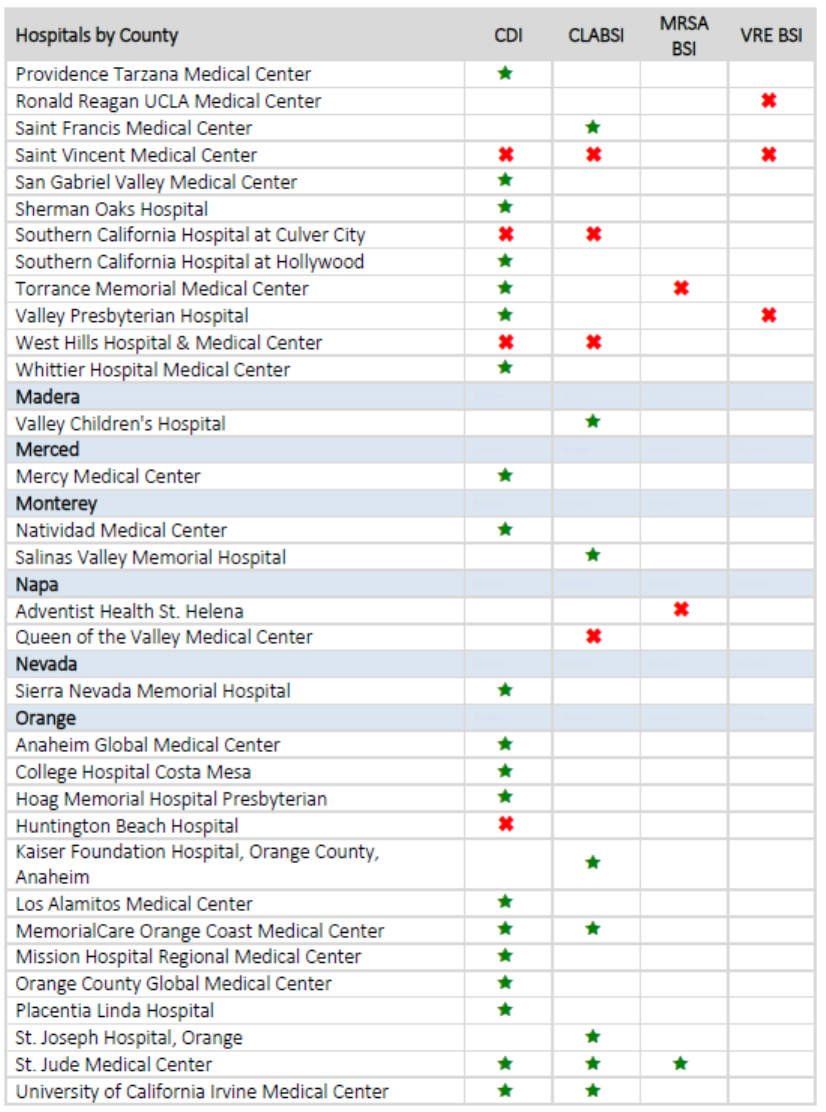
COVERED CALIFORNIA 144
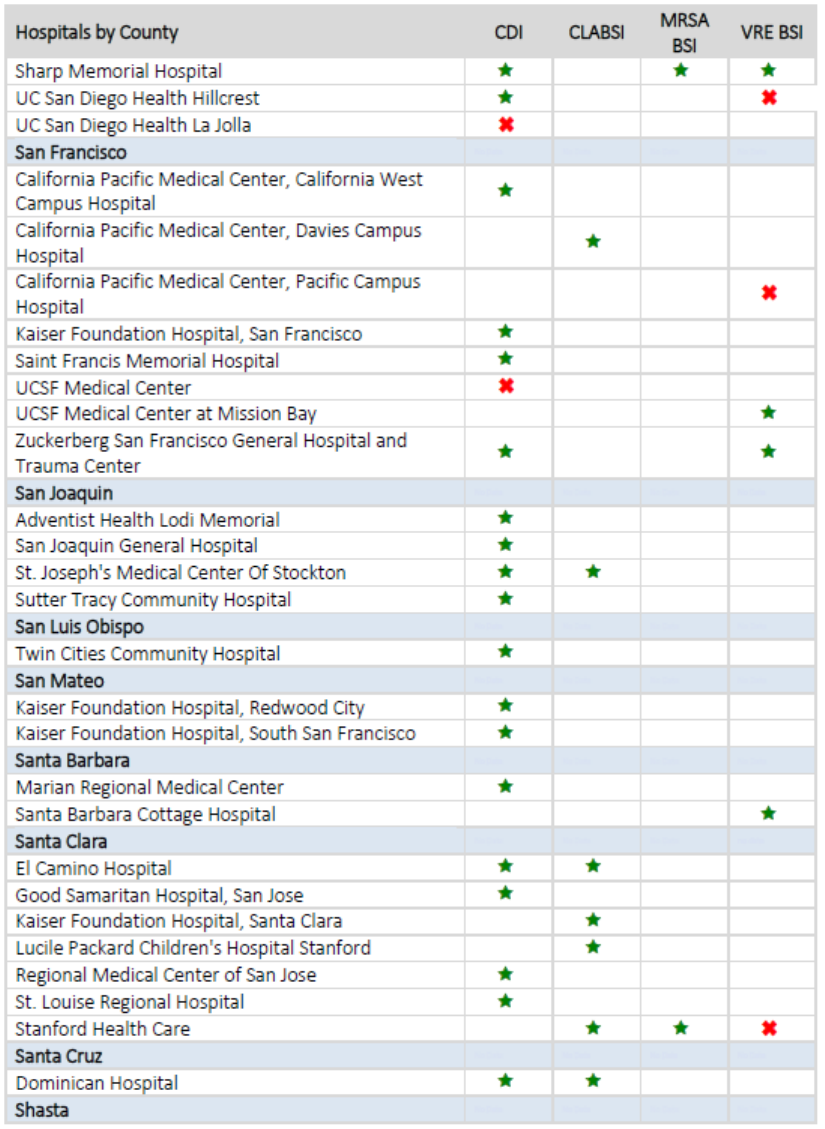
COVERED CALIFORNIA 145
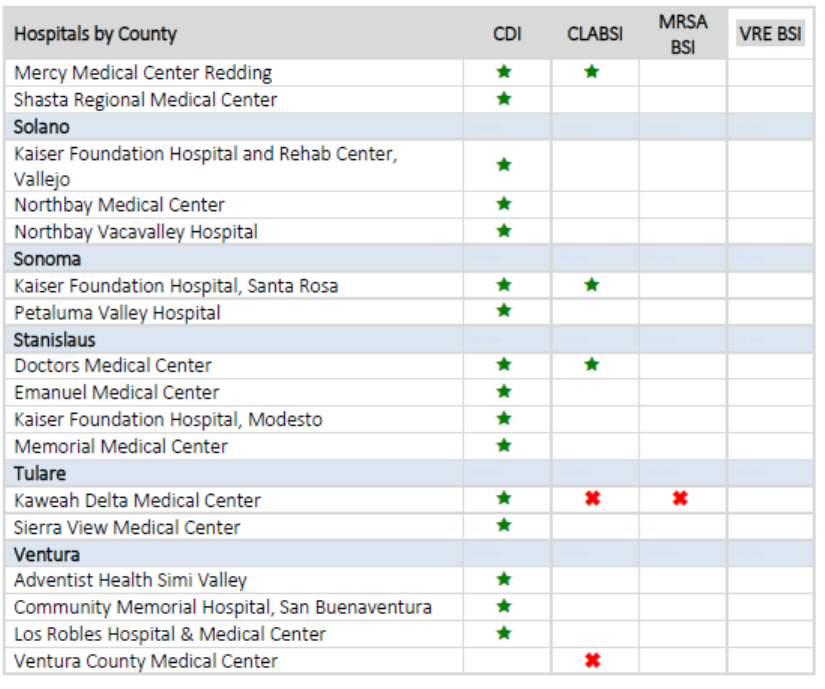
COVERED CALIFORNIA 146
Source: California Department of Public Health (CDPH) 2018 HAI Annual Report.
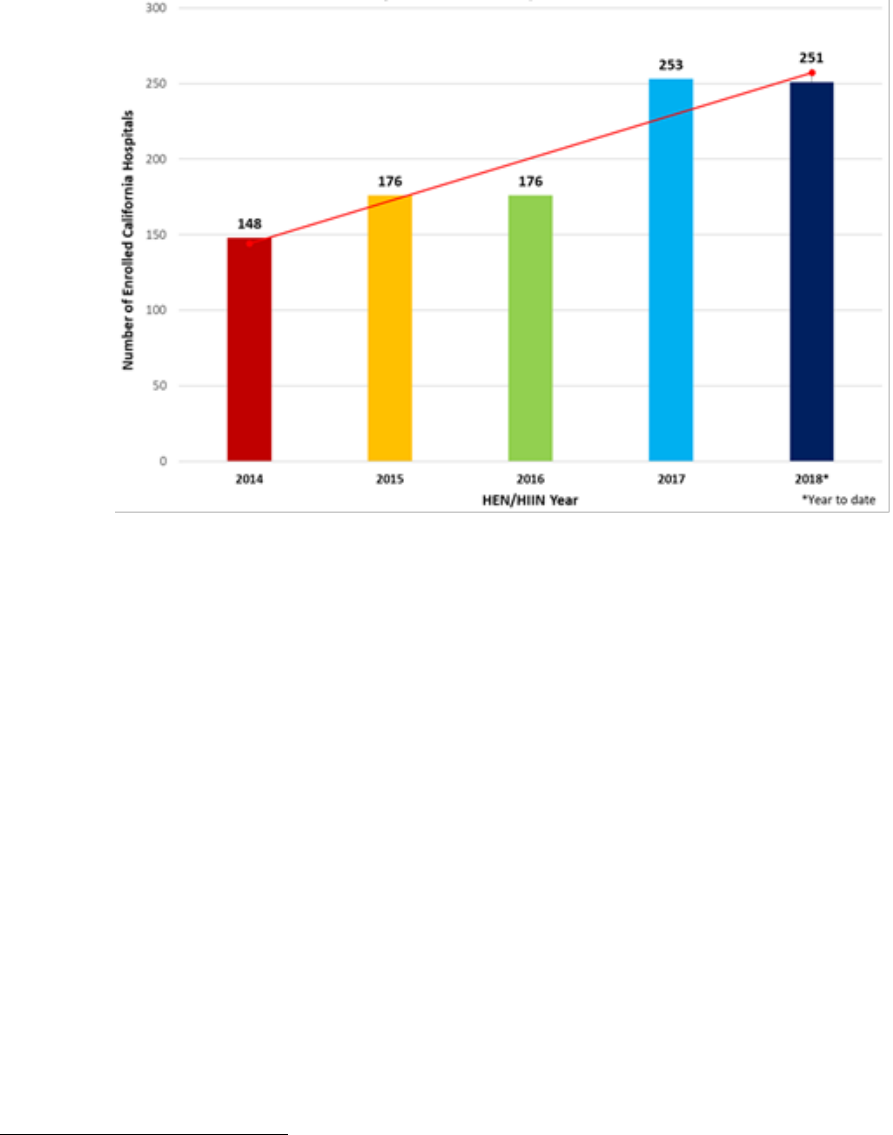
COVERED CALIFORNIA 147
Figure A2. California Hospitals Involved in Hospital Quality Institute Hospital Improvement Innovation
Networks, 2014-18
97
Source: Hospital Quality Institute, 2018
97
Note: The two fewer hospitals participating in the HIIN in 2018 compared to 2017 represent hospital closures. The acronym changed in
2016 from Hospital Engagement Networks (HEN) to Hospital Improvement Innovation Networks (HIINs).
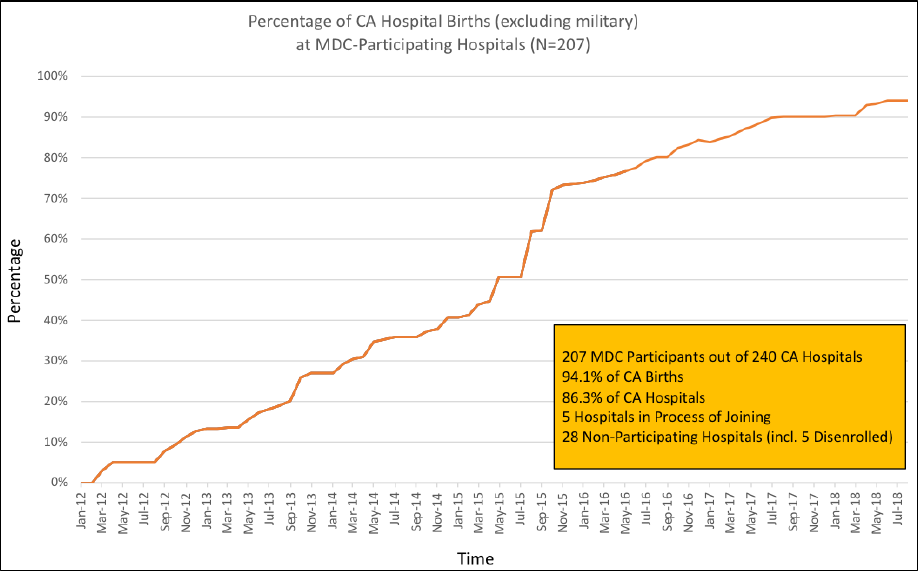
COVERED CALIFORNIA 148
Figure A3: Percentage of California Hospital Births at California Maternal Quality Care Collaborative
Participating Hospitals
Source: California Maternal Quality Care Collaborative, 2018
Acknowledgements
This report describes the results of efforts that continue to evolve and began before the first individual
enrolled in a health plan through Covered California in 2013. Covered California wants to acknowledge
the leadership of its Board of Directors that directed it to take an active role in creating a marketplace
that put consumers at the center and holds health insurance companies accountable. From the outset,
Covered California was given the twin mission of expanding coverage as well as assuring and
improving the delivery of high-quality, equitable and cost-efficient care.
The work represented in this report has been guided by Covered California’s Plan Management
Advisory Committee, composed of representatives of consumer advocates, clinicians, health insurance
companies and subject-matter experts. The health insurance companies Covered California contracts
with have been constructive and engaged and have welcomed having a high bar of accountability
reflected in the contractual expectations. At Covered California, many have contributed to shaping the
work behind this report: the leadership and staff of the Plan Management division, including James
DeBenedetti, Jan Falzarano, John Bertko, Lance Lang and his predecessor as medical director, Jeff
Rideout. For the research, analysis and writing of this report, thanks go to Taylor Priestley, Margareta
Brandt, Vishaal Pegany, Whitney Li, Thai Lee, Allie Mangiaracino, Lindsay Petersen, and two
consulting advisors, Ted von Glahn and Elliott Fisher. Thanks also go to Kelly Green, Sarah Vu,
LaToya Holmes-Green, Kristen Downer, Thomas LeBlanc, Isaac Menashe and Robert Seastrom,
whose assistance made the publication of this report possible.

CoveredCA.com
