TYPE Original Research
PUBLISHED 07 December 2023
DOI 10.3389/fmed.2023.1088672
OPEN ACCESS
EDITED BY
Eun-Jeong Lee,
Illinois Institute of Technology, United States
REVIEWED BY
Mansoor Malik,
The Johns Hopkins Hospital, United States
Giulia Brisighelli,
University of the Witwatersrand, South Africa
*CORRESPONDENCE
Hong Zhen-Xu
†
These authors have contributed equally to this
work and share first authorship
RECEIVED 16 November 2022
ACCEPTED 23 October 2023
PUBLISHED 07 December 2023
CITATION
Lv M, Fang YF, Wang Y and Xu HZ (2023) Factors
contributing to emotional distress when caring
for children with imperforate anus: a multisite
cross-sectional study in China.
Front. Med. 10:1088672.
doi: 10.3389/fmed.2023.1088672
COPYRIGHT
© 2023 Lv, Fang, Wang and Xu. This is an
open-access article distributed under the terms
of the
Creative Commons Attribution License
(CC BY )
. The use, distribution or reproduction
in other forums is permitted, provided the
original author(s) and the copyright owner(s)
are credited and that the original publication in
this journal is cited, in accordance with
accepted academic practice. No use,
distribution or reproduction is permitted which
does not comply with these terms.
Factors contributing to emotional
distress when caring for children
with imperforate anus: a multisite
cross-sectional study in China
Meng Lv
†
, Ya Feng-Fang
†
, Yi Wang and Hong Zhen-Xu
*
Children’s Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang, China
Background: Imperforate anus (IA) has a life-long impact on patients and their
families. The caregivers of children with IA (CoCIA) might experience distress,
which could be detrimental to them physically and mentally. However, there are
limitations in the related studies. This study aimed to investigate the prevalence of
IA an d the associated factors contributing to the distress experienced by CoCIA.
Methods: A cross-sectional study was conducted in three tertiary children’s
hospitals from November 2018 to February 2019. Distress was assessed using
the Chinese version of the Kessler Psychological Distress Scale, and possible
determinants were assessed by the Caregiver Reaction Assessment, the Parent
Stigma Scale, the Parent Perception of Uncertainty Scale, and the Social
Support Scale. Demographic and clinical information was also collected. Multiple
regression analysis was performed to explore the association between variables.
Results: Out of 229 CoCIA, 52.9% reported experiencing a high level of distress
or above. The data analysis revealed that health problems associated with
caregiving, stigma, uncertainty, social support, and children who underwent
anal reconstruction surgery 1 year before or earlier could significantly predicate
caregivers’ distress, and these factors could explain 50.1% of the variance.
Conclusions: The majority of the caregivers of children with IA experience high
levels of distress, particularly when their children undergo an al reconstruction
surgery 1 year before or earlier. Additionally, health problems related to caregiving,
stigma, uncertainty, and low social support could significantly predicate caregivers’
distress. It is important for clinical sta to be aware of the prevalent situation
of caregivers’ distress and to make targeted interventions focused on addressing
modifiable factors that should be carried out in family-based care.
KEYWORDS
anus, imperforate, caregiver, distress, cross-sectional studies
Background
Imperforate anus (IA) is one of the most common types of anore ctal malformation (1),
with an incidence ranging from 1/2,000 to1/5,000 (
2), and its prevalence appears higher in
Eastern countries, possibly due to variations in ethnic and medical settings (
3). IA is generally
categorized into three types: low, intermediate, and high, according to the Wingspread
classification (
4). Anorectal reconstruction is necessary for all affected children, following
which anal dilations are performed until the desired size for their age is achieved (
5).
Additionally, intermediate- and high-type IA patients require a temporary colostomy and
Frontiers in Medicine 01 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
typically undergo surgeries in three stages (6, 7). It is essential
for children with IA and their families to have frequent follow-up
sessions (
8).
Caregivers, who are mostly family members, often experience
significant physical, financial, and psychological pressure while
providing care (
9). Additionally, caregiving is a time-consuming
task that may disrupt the daily schedule of caregivers (
10). Thus,
the abovementioned factors may promote a certain le vel of negative
feelings, such as distress, in caregivers of children with IA (CoCIA)
(
11), and the presence of negative emotions can have a detrimental
effect on the quality of care provided. Therefore, it is import ant
to identify the factors associated with distress to help them
more effectively.
It is common to observe stigma in children who are affected
(
12). However, the family members, especially those responsible for
caregiving, may experience stigma due to their close relationship
with the patients (
13, 14). Stigma usually triggers feelings of shame
about their situation, leading to the social isolation of caregivers
(
15). Furthermore, it adversely affects their mental health, thereby
increasing their distress levels (
16).
Despite the advancements in surgical procedures over the past
several decades, postoperative constipation and fecal and urinary
incontinence are highly prevalent among affected individuals (
17),
and it was reported that CoCIA often feel inadequately informed
about the children’s prognosis and how to properly manage their
bowel functions (
1). The aforementioned factors could significantly
increase caregivers’ perception of uncertainty surrounding the
disease (
18), thus contributing to higher levels of distress of
caregivers (
19).
However, studies show that social support is an important
protective factor of an individual’s psychological health and may
have the potential to alleviate caregivers’ distress (
20). Support
from friends, family, or social organizations could alleviate
negative emotional reactions experienced by caregivers during IA
caregiving (
21). Such support might also reduce caregivers’ distress.
Nevertheless, certain studies have shown that caregivers of children
with congenital diseases often lack adequate support (
22), implying
that CoCIA may also potentially experience lower social support
than average.
To date, numerous studies have explored the mental health
of children with IA, but there is limited research on the mental
wellbeing of families caring for children with IA, which include
CoCIA (
10). A previous study indicated that approximately 50%
of CoCIA reported disruptions in their social lives and family
function (
1). However, studies related to caregivers’ psychological
health and its associated factors are currently limited. Therefore,
in this study, we aimed to explore the caregivers’ distress level
and its contributing factors to provide evidence to improve f amily-
based care.
Methods
Study design, setting, and sample
This study utilized a cross-sectional design. Sequential
participant recruitment was conducted, enrolling care givers of
children receiving treatment for IA based on their arrival
order at the hospital between November 2018 and February
2019.
The sample size was calculated using PASS 13.0 software
(NCSS, Kaysville, USA). Considering the number of variables and
pre-test analysis, the effect size was estimated to be moderate at
0.20, according to the result of the pilot study, and a sample size
of 197 caregivers was estimated to achieve the power of 0.8 when
α was set as 0.05. Considering a dropout rate of approximately
20% according to our experience, a minimum sample size of 246
caregivers was required for this study.
Participants
Children who were enrolled in the study were selected if
they met the following inclusion criteria: (1) congenital absence
of anus or congenital anal fistula, (2) a history of surgical
treatment, and (3) those whose guardians had agreed to provide
their children’s data. Children excluded from the study were as
follows:(1) those diagnosed with other life-threatening diseases or
severe comorbidity, such as congenital c ardiac malformation, and
(2) those whose guardians had refused treatment. To participate in
this study, caregivers needed to be (1) aged ≥ 18 years (2) have
cared for the children for at least 4 weeks, and (3) the primary
caregivers, who spent the longest time in caregiving, without any
remuneration. The exclusion criteria included candidates (1) who
underwent severe life events such as cancer in the past 3 months (a
short questionnaire was used for screening) and (2) who refused to
take part in this study.
Measures
Sample characteristics
This study examined the characteristics of both caregivers
and children. The characteristics of caregivers included their
age, gender, marriage, education, work status, income, place of
residence, religion, household structure, and relationship with the
affected children. On the other hand, the characteristics of children
included their age, gender, birth order, the period following anal
reconstruction surgery, IA type, and medical insurance. Some
general questions were also asked: do you deliberately conceal the
children’s disease in your social life (yes/no)?; Are you afraid to give
birth to another child because the current one was born with an IA
(yes/no)?; How frequently do you communicate with medical staff
(never/seldom/general/often/always)?; What is the degree of your
understanding of the disease (not all/little/some/a lot/very well)?
Dependent variable
In our study, distress levels were assessed using the Chinese
version of the Kessler Psychological Distress Scale (K10) (
23). The
K10 is a screening scale with 10 questions that were constructed
based on t he item response theory models. It was originally
designed for use in the annual US National Health Interview
Survey (NHIS) to measure non-specific psychological distress
experienced by individuals with different mental disorders. The
Frontiers in Medicine 02 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
K10 has demonstrated excellent precision within its intended scale
distribution range and consistent levels of severity across various
sociodemographic subgroups (
24). It can be easily administered
by participants themselves or through an interviewer, taking only
approximately 3 min to complete, and is available for free on a
website (
www.crufad.org) (25). The K10 is a validated and effective
measure of nonspecific psychological distress and is widely utilized
in international epidemiological trend surveys (
26, 27). Within the
K10, respondents were asked to indicate the frequency at which
they had experienced mental health-related conditions such as
psychological anxiety and stress over the past 30 days. Each item
was rated on a scale of 1 to 5, with higher scores indicating greater
severity. The total scores ranged from 10 to 50, with higher scores
indicating higher levels of distress (
28). According to the Victorian
Population Health Survey, a score of 10–15 represented a low level
of distress while a score of 16–21 indicated a moderate level of
distress. A score of 22–29 represented a high level of distress, and
a score of 30–50 indicated a very high level of distress (
29). We
adopted this classification in our study, and the total score of K10
was used for the analysis. The Cronbach’s alpha value of K10 was
0.93 in this study.
Independent variable
The burden of caregivers was assessed using the Chinese
version of the Caregiver Reaction Assessment (CRA) (
30).
The 24 items on the questionnaire were divided into five
dimensions, including impact on health, financial situation,
a lack of family support, disrupted daily schedule, and
caregivers’ esteem. Each dimension was analyzed as a separate
factor. The former four dimensions reflected the caregivers’
burden, while the last one assessed the positive reaction of
caregivers. In this study, the total score of each dimension
was used as independent variables (
31), and the Cronbach’s
alpha values were 0.651, 0.802, 0.710, 0.753, and 0.694 for
each dimension.
Stigma was measured using the Chinese version of the
Parent Stigma S cale (
32), which consisted of five items. A 5-
point Likert scale was used to assess each item ranging from
strongly disagree (1) to strongly agree (5) (
33). The total score
was used for analysis. In this study, the Cronbach’s alpha value
was 0.883.
The perception of uncertainty was assessed using
the revised Chinese version of the Parent Perception of
Uncertainty in Illness Scale (PPUS) (
34). The 29 items were
ranked from 1 (strongly disagree) to 5 (strongly agree)
(
34). The total score was calculated as an independent
variable. The Cronbach’s alpha value was 0.914 in
this study.
The Social Support Scale developed by Xiao (
35) was used in
this study. There were 10 items in total, and higher scores indicated
greater level of social support. This classic scale was developed in
the Chinese context and is widely used in Chinese studies (
36). In
this study, Cronbach’s alpha value was 0.819, and the total score was
summed as an independent factor.
Data analysis
For qualitative data, the frequency and percentage were
used to represent the results. For quantitative data, normally
distributed data were described using the mean plus or minus
the standard deviation, while non-normally distributed data were
described using the median and quartiles. A univariate analysis was
conducted with K10 serving as the dependent variable and sample
characteristics as the independent variable. If the independent
variable satisfies the assumption of normality and homogeneity of
variance, the Student’s t-test was used to compare the two groups,
while ANOVA was used to compare the means among multiple
groups. However, if the data deviate from a normal distribution or
display heteroscedasticity, non-parametric tests such as the Mann-
Whitney U-test were employed. In the case of non-parametric
comparisons involving multiple groups, the Kruskal-Wallis test was
utilized. The Spearman’s correlation coefficients were calculated
to assess the potential correlations between distress and variables
such as CRA, stigma, PPUS, and social support. Multiple linear
regression was performed to analyze the associated factors of
caregivers’ distress. Statistical significance was assessed at the 5%
level (p < 0.05).
Procedure
Ethical approval was obtained for this study (2018-IRB-081).
A pilot test of 30 primary caregivers was conducted to ensure
that the questionnaire contents could be properly understood. In
our formal study, we utilized an online survey to collect data.
Specifically, the principal investigator set up three separate WeChat
groups, one for each center involved in our multi-center study. In
each group, a pediatric surgeon and a wound ostomy continence
nurse were invited to act as consultants. To ensure maximum
participation, we first added each caregiver participant on WeChat.
If they expressed a willingness to complete the survey, the principal
investigator would contact them online and provide them with
the link to the online survey. This link was composed of two
parts: an electronic consent form and a set of questionnaires.
Caregivers could only proceed to the questionnaires after clicking
on “I have read all the content and agree to participate in the study”.
Participants were able to complete the survey eit her in a separate
room at the clinic of pediatric surgery or in the comfort of their
own homes, depending on their preference and convenience. For
illiterate candidates, researchers read and explained every item to
ensure inclusivity. All caregivers were informed about the WeChat
groups and given a brief introduction to the study. They were also
offered the option to join the groups, regardless of whether t hey
would like to participate in the survey. These groups provided a
forum for patients and caregivers to connect with others who had
comparable experiences. They were able to discuss any questions
that came up while filling out the questionnaires and receive
additional information and support. It is also noteworthy that
these WeChat groups continued to operate after the project had
concluded, providing ongoing medical advice and social support
to caregivers.
Frontiers in Medicine 03 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
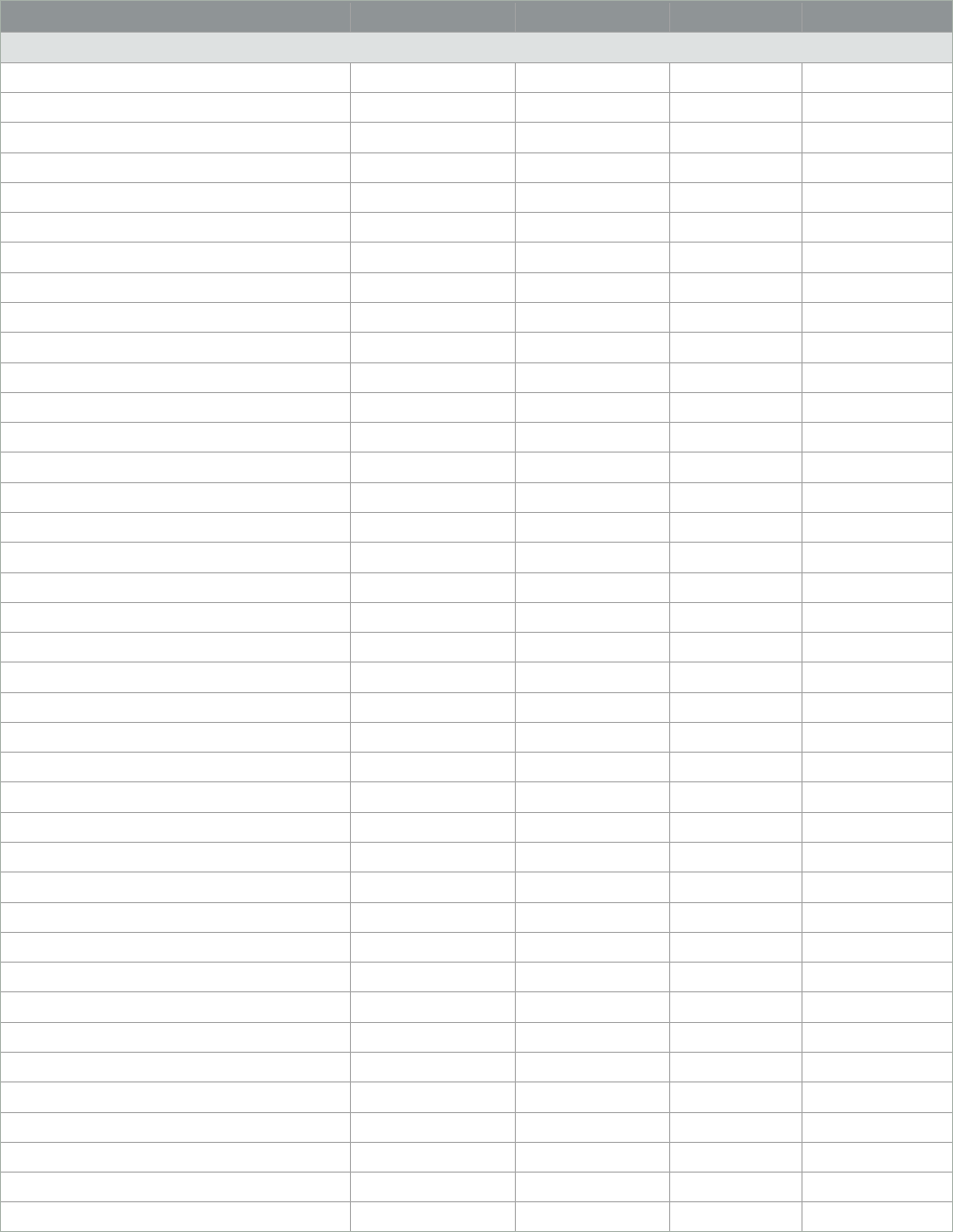
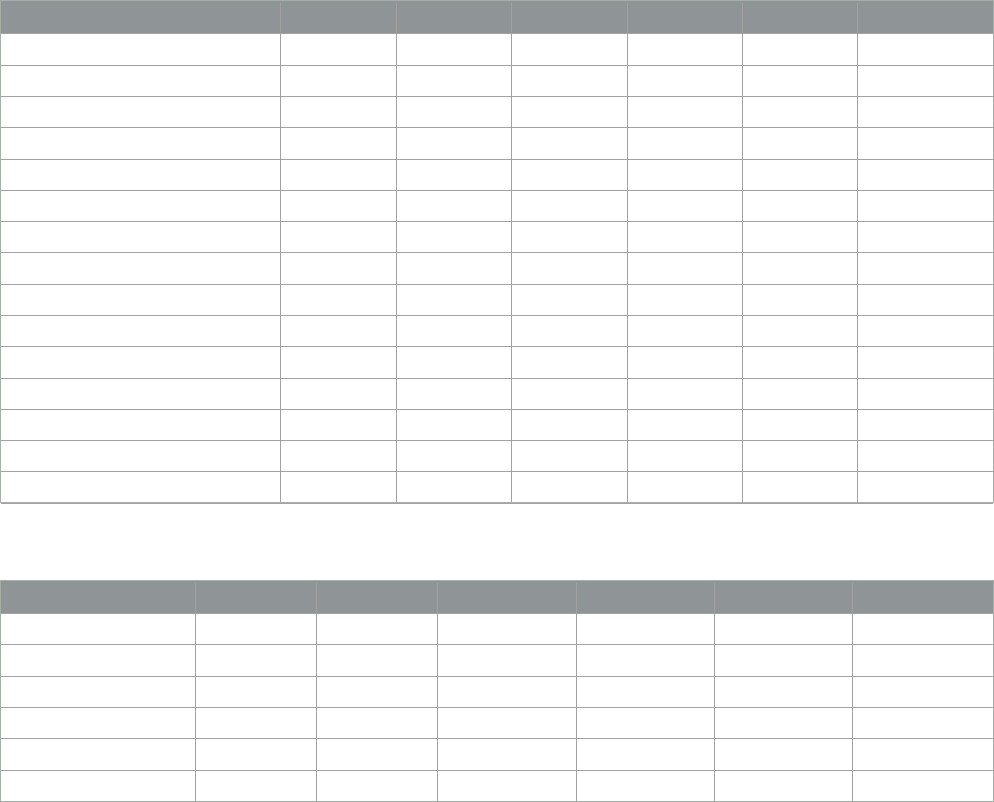
TABLE 1 Descriptive statistics and univariate analysis (N = 229).
Item N (%) K10 χ
2
/t/z P
Caregiver
Age 0.402 0.670
<30 100 (43.7) 22.80 ± 7.33
30–40 106 (46.3) 23.47 ± 7.30
>40 23 (10.0) 22.13 ± 8.56
Gender 0.677 0.499
Men 41 (17.9) 23.76 ± 6.70
Women 188 (82.1) 22.89 ± 7.58
Marriage −0.087 0.930
Married 222 (96.9) 23.04 ± 7.49
Other 7 (3.1) 23.29 ± 5.44
Education 0.543 0.653
Primary school or below 17 (7.4) 24.06 ± 6.83
Junior high school 68 (29.7) 23.77 ± 6.81
High school 45 (19.7) 22.91 ± 6.81
University/college or above 99 (43.2) 23.04 ± 7.42
Occupation 1.725 0.181
Part-time job 32 (14.0) 25.22 ± 6.50
Full-time job 84 (36.7) 22.39 ± 7.72
Unemployed 113 (49.3) 22.91 ± 7.40
Relationship wit h children 1.636 0.197
Mother 178 (77.7) 22.76 ± 7.44
Father 44 (19.2) 24.64 ± 7.00
Others 7 (3.1) 20.29 ± 8.90
Income (RMB)
<8,000 111 (48.5) 24.56 ± 6.75 −3.465 0.001
≥8,000 118 (51.5) 20 (16, 25)
Inhabitant 1.692 0.187
City 61 (26.6) 21.72 ± 7.61
Suburban 76 (33.2) 22.99 ± 7.16
Countryside 92 (40.2) 23.97 ± 7.46
Household structure −1.097 0.274
Extended family 150 (65.5) 22.65 ± 6.72
Nuclear family 79 (34.5) 23.79 ± 8.60
Religion 1.250 0.212
Yes 71 (31.0) 23.96 ± 8.62
No 158 (69.0) 22.63 ± 6.81
Medical insurance −1.633 0.104
Yes 173 (75.5) 22.59 ± 7.29
No 56 (24.5) 24.45 ± 7.71
(Continued)
Frontiers in Medicine 04 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
TABLE 1 (Continued)
Item N (%) K10 χ
2
/t/z P
Concealment behavior 2.522 0.012
Yes 161 (70.3) 23.84 ± 7.49
No 68 (29.7) 21.16 ± 6.96
Afraid to have another child 3.273 0.001
Yes 139 (60.7) 24.31 ± 7.59
No 90 (39.3) 21.09 ± 6.75
Communication frequency with medical staff 1.569 0.118
General or below 138 (60.3) 23.67 ± 7.24
Often or above 91 (39.7) 22.10 ± 7.64
Understanding of IA 0.154 0.878
Some or below 176 (76.9) 23.09±7.40
A lot or above 53 (23.1) 22.91 ± 7.57
Children
Age (y) −0.849 0.397
<2 189 (82.5) 22.85 ± 7.39
≥2 40 (17.5) 23.95 ± 7.62
Gender 0.062 0.951
Men 154 (67.2) 23.07 ± 7.18
Women 75 (32.8) 23.00 ± 7.96
Birth order −0.849 0.397
1 102 (44.5) 22.58 ± 7.22
≥2 127 (55.5) 23.42 ± 7. 60
Time since anal reconstruction surgery (y) −1.995 0.047
<1 128 (55.9) 22.18 ± 7.37
≥1 101 (44.1) 24.14 ± 7. 39
IA type 5.136 0.007
Low 124 (54.1) 21.64 ± 6.63
Intermediate 41 (17.9) 24.29 ± 9.60
High 64 (27.9) 24.97 ± 6.82
Combined with other abnormalities 1.687 0.093
Yes 94 (41.0) 24.03 ± 7.79
No 135 (59.0) 22.36 ± 7.11
Results
Sample characteristics
The data analysis was conducted using 229 completed
questionnaires from primary caregivers (response rate = 90.16%).
Out of the initial pool of 254 participants who were eligible for
this study, 18 individuals declined to participate citing the reason
as the lack of interest or unwillingness to discuss their child’s
disease. Additionally, seven participants were excluded from the
study due to incomplete questionnaires. Based on the sample
size of 229, an effective size of 0.20, and an α-value set at 0.05,
the actual statistical power of this study was calculated to be
0.857. The characteristics of both the caregivers and children are
presented in
Table 1. The age of the caregivers who participated
in the study ranged from 18 to 67 years, with a median age
of 30 (interquartile range: 28–36). The age of children who
participated in the study ranged from 0.08 to 6.37 years old,
with a median age of 0.87 years (interquartile range: 0.37–
1.78).
Frontiers in Medicine 05 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
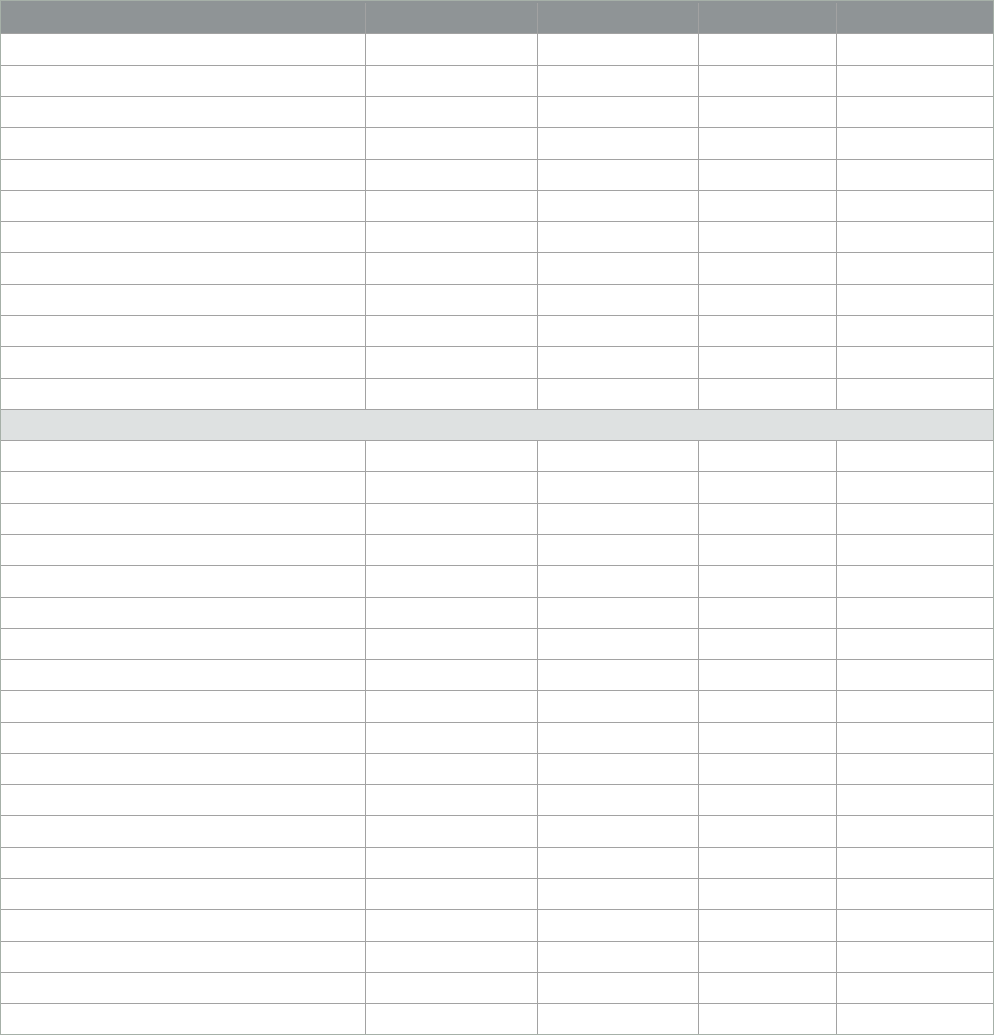
TABLE 2 Category of K10 score (N = 229).
Degree of distress N (%)
Low 34 (14.8)
Moderate 74 (32.3)
High 75 (32.8)
Very high 46 (20.1)
TABLE 3 Descriptive statistics for measurement scales (N = 229).
Item Total score (range) Item average
(range)
K10 23.04 ± 7.42 (10.00–50.00) 2.30 ± 0.74 (1.00–5.00)
CRA
Health problem 10.74 ± 2.63 (4.00–18.00) 2.69 ± 0.66 (1.00–4.50)
Financial problem 8.77 ± 2.77 (3.00–15.00) 2.92 ± 0.92 (1.00–5.00)
Lack of family support 11.22 ± 3.19 (5.00–22.00) 2.24 ± 0.64 (1.00–4.40)
Disrupted schedule 18.00 ± 3.60 (5.00–25.00) 3.60 ± 0.71 (1.00–5.00)
Self-esteem 29.01 ± 3.20 (20.00–35.00) 4.14 ± 0.46 (2.86–5.00)
Stigma 14.98 ± 4.81(5.00–25. 00) 3.00 ± 0.96 (1.00–5.00)
PPUS 72.58 ± 14.06 (29.00–102.00) 2.59 ± 0.50 (1.04–3.64)
Social support 40.33 ± 8.36 (16.00–62.00) 2.88 ± 0.60 (1.14–4.43)
K10, Kessler Psychological Distress Scale; CRA, Caregiver Reaction Assessment; PPUS, Parent
Perception of Uncertainty Scale.
Measurement results
The mean distress score of caregivers was 23.04.
Table 2
presented the distribution of distress levels, which were as follows:
low-−34 (14.8%), moderate−74 (32.3%), high−75 (32.8%), and
very high−46 (20.1%). The total score and average score of the
items for the measurement scales, including K10, CRA, PPUS,
social support, and stigma, were shown in Table 3.
Univariate analysis
The univariate analysis identified the significant differences in
income, the period following anal reconstruction surgery, IA type,
concealment behavior, and fear of having another child (
Table 1).
The relationships between CRA, stigma, PPUS, social support, and
distress are shown in
Table 4. The correlation analysis showed
that there were statistically significant correlations between CRA,
stigma, PPUS, and social support with K10.
Multiple regression analysis
The associated factors of caregivers’ distress were explored
using the multiple regression analysis.
Table 5 displays the results
of the multiple regression analysis of significant univariable factors.
Table 6 reveals that independent factors contributing to the distress
of IA care givers included health problems pertaining to caregiving
TABLE 4 Correlations (r) between CRA, stigma, PPUS, social support, and K10.
K10 CRA health
problem
CRA
financial problem
CRA lack of
family
support
CRA
disrupted schedule
CRA self-
esteem
PPUS Social
support
Stigma
K10 1.00 0.623
∗∗
0.435
∗∗
0.285
∗∗
0.322
∗∗
−0.250
∗∗
0.529
∗∗
−0.424
∗∗
0.397
∗∗
CRA
Health problem 0.623
∗∗
1.00 0.506
∗∗
0.277
∗∗
0.424
∗∗
−0.270
∗∗
0.407
∗∗
−0.343
∗∗
0.314
∗∗
Financial problem 0.435
∗∗
0.506
∗∗
1.00 0.330
∗∗
0.443
∗∗
−0.217
∗∗
0.489
∗∗
−0.378
∗∗
0.233
∗∗
Lack of family support 0.285
∗∗
0.277
∗∗
0.330
∗∗
1.00 0.263
∗∗
−0.251
∗∗
0.358
∗∗
−0.438
∗∗
0.163
∗
Disrupted schedule 0.322
∗∗
0.424
∗∗
0.443
∗∗
0.263
∗∗
1.00 00.099 0.201
∗∗
−0.275
∗∗
0.283
∗∗
Self-esteem -0.250
∗∗
−0.270
∗∗
−0.217
∗∗
−0.251
∗∗
00.099 1.00 −0.332
∗∗
0.305
∗∗
−0.185
∗∗
PPUS 0.529
∗∗
0.407
∗∗
0.489
∗∗
0.358
∗∗
0.201
∗∗
−0.332
∗∗
1.00 −0.364
∗∗
0.283
∗∗
Social support -0.424
∗∗
−0.343
∗∗
−0.378
∗∗
−0.438
∗∗
−0.275
∗∗
0.305
∗∗
−0.364
∗∗
1.00 −0.293
∗∗
Stigma 0.397
∗∗
0.314
∗∗
0.233
∗∗
0.163
∗
0.283
∗∗
−0.185
∗∗
0.283
∗∗
−0.293
∗∗
1.00
CRA, Careg iver Reaction Assessment; PPUS, Parent Perception of Uncertainty Scale.
∗∗
Correlation is significant at the 0.01 level (2-tailed).
∗
Correlation is significant at the 0.05 level (2-tailed).
Frontiers in Medicine 06 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
TABLE 5 Multiple regression analysis of significant univariable factors (N = 229).
Item B SE SB t P VIF
Constant −0.553 6.204 −0.089 0.929
Stigma 0.228 0.083 0.148 2.745 0.007 1.311
CRA
Health problem 1.333 0.183 0.472 7.278 <0.001 1.898
Finance problem −0.125 0.175 −0.047 −0.716 0.475 1.912
Lack of family support −0.011 0.134 −0.005 −0.082 0.935 1.501
Disrupted schedule −0.047 0.131 −0.022 −0.356 0.722 1.761
Self-esteem 0.119 0.127 0.051 0.934 0.351 1.354
Social support −0.104 0.053 −0.117 −1.966 0.051 1.598
PPUS 0.128 0.032 0.242 3.978 <0.001 1.675
Time since anal reconstruction surgery 1.385 0.724 0.093 1.914 0.057 1.062
Income −1.249 0.804 −0.084 −1.553 0.122 1.327
Concealment behavior −0.944 0.832 −0.058 −1.135 0.258 1.188
Afraid to have another child 0.167 0.776 0.011 0.216 0.829 1.18
IA type 0.15 0.436 0.018 0.344 0.731 1.178
R
2
= 0.524, R
2
ad
= 0.495, F = 18.178, P < 0.01. Durbin-Watson = 2.020.
TABLE 6 Multiple regression analysis of independent influencing factors (N = 229).
Item B SE SB t P VIF
Constant −0.809 3.711 – −0.218 0.828 –
CRA Health problem 1.186 0.153 0.420 7.747 <0.01 1.341
PPUS 0.132 0.028 0.251 4.652 <0.01 1.327
Stigma 0.243 0.078 0.157 3.105 0.002 1.171
Social support −0.104 0.047 −0.118 −2.212 0.028 1.289
Time since surgery 1.445 0.704 0.097 2.051 0.041 1.017
R
2
= 0.512, R
2
ad
= 0.501, F = 46.714, P <0.01. Durbin-Watson = 2.011.
(B = 1.186), PPUS (B = 0.132), stigma (B = 0.243), social support
(B = −0.104), and children who underwent anal reconstruction
surgery ≥1 year (B = 1.445). These factors accounted for a variance
of 50.1% of c are givers’ distress.
Discussion
This study investigated the extent of distress experienced
by CoCIA and identified its contributing factors. On average,
the caregivers obtained a K10 score of 23.04, which indicates
a high level of distress. This score was much higher than both
the average population score (15.42) (
37) and the score for
patients with chronic illness (20.25) (
38). According to a study,
the K10′s cutoff point was found to be 16, which falls under
the moderate classification category. The study also found that,
when higher scores were observed on the scale, the level of
psychological distress reported was proportionally higher as well
(
39). In this study, it was found that approximately 85.15% of
the caregivers scored at least 16 points, which suggested that
professional psychological consultation should be recommended
for this population. Caregivers play a crucial role in establishing
a connection between the affected children and medical staff;
however, if they experience psychological distress, the quality of
care given to IA children may be compromised due to ineffective
cooperation with the medical staff (
14). Therefore, clinical medical
staff should pay more attention to the caregivers’ mental health,
screen out the high-risk population with effective tools, such as
K10, and cooperate with professional psychiatrists.
Different stages of IA diagnosis have an effect on caregivers’
psychological state (
10). According to our study, children who
underwent surgery for IA for 1 year before or earlier were found to
be significantly associated with higher levels of caregivers’ distress,
highlighting their role as a significant predictor, that is, the longer
the caregiving duration, t he greater the possibility of burnout (
40).
One possible explanation might be that caregiving for a short
period can be manageable, but over a long period of time, it can
have a detrimental effect on the psychological health of caregivers
and ultimately result in burnout. Therefore, clinical nurses and
surgeons should pay particular attention to CoCIA with a history
Frontiers in Medicine 07 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
of anal reconstruction surgery 1 year before or earlier. While
caregiving tasks eventually reduce at the end of surgical therapy,
distress levels may, on the other hand, increase due to the long
duration of caregiving.
Health problems can play a significant role in causing distress
for IA caregivers. Caring for a child with chronic illness can be a
challenging task that imposes a considerable amount of stress on
the caregivers and can have a negative effect on the physical health
of caregivers (
41). In a previous study, it was found that caregivers
of children with chronic illness experience more healt h problems
compared to caregivers of healthy children, and this can be solely
attributed to the challenges of caregiving (
42). Moreover, the health
problems could also negatively influence caregivers’ mental health
and increase their distress level, which is harmful to both the
caregivers and their children (
43). Thus, medical staff could provide
caregivers with more he alth-keeping knowledge while treating the
affected children and encourage caregivers to ask for medical help
if necessary. Additionally, it is important to teach nursing skills
such as ostomy-c are experience and dietary recommendations
to enhance caregivers’ illness management abilities, which may
potentially alleviate caregiving burden and reduce the caregivers’
health problems (
44).
Perceiving uncertainty of the children’s illness improvement is
an important determinant of IA caregivers’ distress. The persistent
uncertainty could lead to higher levels of anxiety and distress
among caregivers, thus negatively affecting their overall wellbeing
(
19, 45). However, some studies indicated that caregivers might also
benefit from embracing uncertainty, as acknowledging it opens up
the possibility for positive prognoses in the affected children, which
could also be viewed as an opportunity for a favorable outcome
(
46). However, the impact of uncertainty on caregivers’ distress
usually depends on their individual perspectives and personal
viewpoints. On the one hand, as a member of medical staff,
we could provide additional information to support caregivers
to mitigate their unnecessary anxiety about their children and
reduce the negative effect of uncert ainty (
45). On the other hand,
encouraging caregivers to focus on the benefits that can come from
uncertainty could help promote optimism and a more positive
outlook on the prognosis. Stigma is also a determinant of caregivers’
distress. Since the children are usually unaware of their situation,
particularly when they are young, the caregivers may experience
higher perceived stigma and social discrimination since the burden
falls solely on caregivers (
16). The stigma causes them to experience
more distress because of their personal disapproval and self-
depreciation as well as poses a barrier for the c are givers to seek
help from medical services, which might result in undermining the
quality of the care given (
47). Thus, interventions focused on stigma
should be implemented. Studies have shown that providing detailed
explanations about the disease, sharing testimonies of individuals
living with the stigma, and incorporating active-learning exercises
contribute to mitigating stigmatization, thus reducing c are givers’
distress (
47).
According to the results of this study, it was found that
social support is a determinant of distress among IA caregivers.
Social support plays a significant protective role in individual
psychological health, potentially reducing caregivers’ distress (
20).
Medical staff should motivate caregivers to seek additional social
support, such as encouraging them to seek help from their family
members, and ensuring they have increased access to contact
medical staff for further inquiries. Peer support can be harnessed
through initiatives such as establishing IA-related communication
groups to provide assistance (
48).
Conclusions
CoCIA experience a high level of distress, especially when their
children undergo anal reconstruction surgery 1 year before or
earlier. This heightened distress is linked to health problems arising
from caregiving, increased perception of stigma and uncertainty,
and a lower level of social support. Therefore, it is crucial for
medical staff to pay attention to t he continuing needs of these
caregivers during follow-up appointments, e ven after the patients
have completed their surgical therapy. Additionally, some measures
aiming to improve the caregivers’ health condition and reduce
their stigma should be implemented. We should also provide
more medical information to alleviate caregivers’ anxiety caused by
uncertainty, encourage them to be optimistic, and help them find
greater social support to promote their psychological health.
Limitations
This study, as any other study, has its limitations. First, we used
an outdated classification system. During the data collection period,
the Wingspread classification was still being used as the standard in
the Chinese medical system. Unfortunately, due to restricted access
to patient data, we were unable to obtain detailed descriptions of the
disease to accurately reclassify our patients according to updated
systems such as the Krickenbeck classification. Second, due to the
correlational nature of the evidence, we could not ascertain the
direction of some associations. For example, distress resulting from
prolonged caregiving might, in turn, negatively affect the health of
caregivers. Therefore, prospective studies are required to identify
the dire ction of associations. Finally, we may have overlooked some
important factors that could potentially contribute to caregivers’
distress, such as family function, which is regarded as a crucial
factor in personal psychological health.
Data availability statement
The raw data supporting the conclusions of this article will be
made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Zhejiang
University School of Medicine, China. The studies were conducted
in accordance with the local legislation and institutional
requirements. Written informed consent for participation in
this study was provided by the participants’ le gal guardians/next
of kin.
Frontiers in Medicine 08 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
Author contributions
YF-F conceived and supervised the study and extracted data.
ML extracted data, performed data analysis, and developed the
manuscript. YW performed data analysis and provided input on
manuscript development. HZ-X helped write the manuscript and
provided critical input on its revisions. All authors contributed to
the article and approved the submitted version.
Acknowledgments
The authors thank all the participants who took part in the
survey. We also want to extend our gratitude to Dr. Shoujiang
Huang and Dr. Qi Qin for their assistance in informing the
caregivers about this study, as well as Nurse Fang Li, who patiently
answered the caregivers’ questions.
Conflict of interest
The authors declare that t he research was conducted
in the absence of any commercial or financial relationships
that could be construed as a potential conflict
of interest.
Publisher’s note
All claims expressed in this article are solely those
of the aut hors and do not necessarily represent those of
their affiliated organizations, or those of the publisher,
the editors and the reviewers. Any product that may be
evaluated in this article, or claim that may be made by
its manufacturer, is not guaranteed or endorsed by the
publisher.
References
1. Cai ro S, Gasior A, Rollins M, Rothstein D. Challenges in transition
of care for patients with anorectal malformations: a systematic review and
recommendations for comprehensive care. Dis Colon Rectum. (2018) 61:390–
9. doi: 10.1097/DCR.0000000000001033
2. Steeg Hvd, Botden S, Sloots C, Steeg Avd, Broens P, Heurn Lv, Travassos D,
Rooij Iv, Blaauw Id: Outcome in anorect al malformation type rectovesical fistula:
a nationwide cohort study in The Netherlands. J Pediat Surg. (2016) 51:1229–
33. doi: 10.1016/j.jpedsurg.2016.02.002
3. Gangopadhyay AN, Pandey V . Controversy of single versus staged
management of anorectal malformations. Indian J Pediatr. (2017)
84:636–42. doi: 10.1007/s12098-017-2373 -6
4. Steeg Hvd, Schmiedeke E, Bagolan P, Broens P, Demirogullari B, Garcia-Vazquez
A, et al. European consensus meeting of ARM-Net members concerning diagnosis and
early management of newborns with anorec tal malformations. Techniq Coloproctol.
(2015) 19:181–5. doi: 10.1007/s10151-015-1267-8
5. Jenetzky E, vanRooij IALM, Aminoff D, Schwarzer N, Reutter H, Schmiedeke E,
et al. The challenges of the European anorectal malformations-net registry. Eur J Pediat
Surg. (2015) 25:481–7. doi: 10.1055/s-0035-1569149
6. Baayen C, Feuillet F, Clermidi P, Crétolle C, Sarnacki S, Podevin G, et al. Validation
of the French versions of the Hirschsprung’s disease and Anore c tal malformations
Quality of Li fe (HAQL) questionnaires for adolescents and adults. Health Qual Life
Outc. (2017) 15:24. doi: 10.1186/s12955-017-0599-7
7. Nam SH, Kim DY, Kim SC. Can we expect a favorable outcome after
surgical treatment for an anorectal malformation? J Pediatr Surg. (2016) 51:421–
4. doi: 10.1016/j.jpedsurg.2015.08.048
8. Goudarzi Z, Askari M, Seyed-Fatemi N, Asgari P, Mehran A. The effect
of educational program on stress, anxiety and depression of the mothers of
neonates having colostomy. J Matern Fetal Neonatal Med. (2016) 29:3902–
5. doi: 10.3109/14767058.2016. 1152242
9. Al-Gamal E, Long T, Shehadeh J. Health satisfaction and family impact of parents
of children with cancer: a descriptive cross-sectional study. Scand J Caring Sci. (2019)
33:815–23. doi: 10.1111/scs.12677
10. Witvliet MJ, Bakx R, Zwaveling S. Dijk THv, Steeg AFWvd: Quality of
life and anxiety in parents of children with an anorectal malformation or
Hirschsprung disease: the first year after diagnosis. Eur J Pediat Surg. (2016) 26:002–
6. doi: 10.1055/s-0035-1559885
11. Majestic C, Eddington KM. The impact of goal adjustment and caregiver burden
on psychological distress among caregivers of cancer patients. Psychooncology. (2019)
28:1293–300. doi: 10.1002/pon.5081
12. Ojmyr-Joelsson M, Nisell M, Frenckner B, Rydelius P-A, Christensson K. A
gender perspective on the extent to which mothers and fathers each take responsibility
for care of a child with high and intermediate imperforate anus. J Pediatr Nurs. (2009)
24:207–15. doi: 10.1016/j.pedn.2007.0 9.004
13. Hamlington B. E.lvey L, Brenna E, Biesecher LG, B.Biesecker B,
Sapp J. Characterization of courtesy stigm a perceived by parents of
overweight children with bardet-biedl syndrome. PLoS ONE. (2015)
10:e0140705. doi: 10.1371/journal.pone.0140705
14. Chang C, Su JA, Tsai CS, Yen C, Liu JH, Lin CY. R asch analysis suggested three
unidimensional domains for Affiliate Stigma Scale: additional psychometric evaluation.
J Clin Epidemiol. (2015) 68:674–83. doi: 10.1016/j.jclinepi.2015.01.018
15. Li J, Mo P, Wu A, Lau J. Roles of self-stigma, social support, and
positive and negative affects as determinants of depressive symptoms among HIV
infected men who have sex with men in China. AIDS Behav. (2017) 21:261–
73. doi: 10.1007/s10461-016-1321-1
16. Zhou T, Wang Y, Yi C. Affiliate stigma and depression in caregivers of children
with Autism Spectrum Disorders in China: Effects of self-esteem, shame and family
functioning. Psychiatry Res. (2018) 264:260–5. doi: 10.1016/j.psychres.2018.03.071
17. Lane VA, Nacion KM, Cooper JN, Levitt MA, Deans KJ, Minneci P.
Determinants of quality of life in children with colorectal diseases. J Pediatr Surg. (2016)
51:1843–50. doi: 10.1016/j.jpedsurg.2016.08.004
18. Giuliani S, Decker E, Leva E, Riccipetitoni G, Bagolan P. Long term follow-up
and transition of care in anorectal malformations: an international survey. J Pediatr
Surg. (2016) 51:1450–7. doi: 10.1016/j.jpedsurg.2016.03.011
19. Aldaz BE, Hegarty RSM, Conner TS, Perez D, Treharne GJ. Is avoidance of illness
uncertainty associated with distress during oncology treatment? A daily diary study.
Psychol Health. (2019) 34:422–37. doi: 10.1080/08870446.2018.1532511
20. Choi E, Yoon S, Kim J, Park H, Kim J, Yu E. Depression and distress in
caregivers of children with brain tumors undergoing treatment: psychosocial factors
as m oderators. Psychooncology. (2016) 25:544–50. doi: 10.1002/pon.3962
21. Okuyama J, Funakoshi S, Amae S, Kamiyama T, Ueno T, Hayashi Y. Coping
patterns in a mother of a child with multiple congenital anomalies: a case study. J Intens
Criti Care. (2017) 3:1–6. doi: 10.21767/2471-8505.100075
22. Jacobs R, Boyd L, Brennan K, Sinha CK, Giuliani S. The importance
of social media for patients and families affected by congenital anomalies: a
Facebook cross-sectional analysis and user survey. J Pediatr Surg. (2016) 51:1766–
71. doi: 10.1016/j.jpedsurg.2016.07.008
23. Zhou C, Chu J, Wang T, Peng Q, He J, Zheng W, et al. Reliability and validity
of 10-item Kessler Scale (K10) Chinese version in evaluation of mental health status of
Chinese population. Chin J Clin Psychol. (2008) 16:627–9.
24. Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand
SL, et al. Short screening scales to monitor population prevalences
and trends in non-specific psychological distress. Psychol Med. (2002)
32:959–76. doi: 10.1017/S003329170200607 4
25. Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening
for serious mental illness i n the general population. Arch Gen Psychiatry. (2003)
60:184–9. doi: 10.1001/archpsyc.60.2.184
26. Sunderland M, Slade T, Stewart G, Andrews G. Estimating the prevalence
of DSM-IV mental illness in the Australian general population using the
Kessler Psychological Distress Scale. Aust N Z J Psychiatry. (2011) 45:880–
9. doi: 10.3109/00048674.2011. 606785
27. Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, et al. The
performance of the Japanese version of the K6 and K10 in the World Mental Health
Survey Japan. Int J Methods Psychiatr Res. (2008) 17:152–8. doi: 10.1002/mpr.257
Frontiers in Medicine 09 frontiersin.org
Lv et al. 10.3389/fmed.2023.1088672
28. Chan SM, Fung TCT. Reliability and validity of K10 and K6 in screening
depressive symptoms in Hong Kong adolescents. Vulnerable Child Youth Stud. (2014)
9:75–85. doi: 10.1080/17450128. 2013.86 1620
29. Victorian Population Health Survey. Victorian Population Health Survey 2008
vol. 26. Melbourne, Victoria: Department of Health. (2008).
30. Yaping Z, Yan L, Huiqin W. Validity and reliability research of Chinese
edition of caregiver reaction assessment. Chin J Nurs. (2008) 43:856–9.
doi: 10.3761/j.issn.0254-1769.2008.09.042
31. Petrinec A, Burant C, Douglas S. Caregiver reaction assessment: psychometric
properties in caregivers of advanced cancer patients. Psychooncology. (2016) 26:1–
3. doi: 10.1002/pon.4159
32. Wang D, Jia Y, Gao W, Chen S, Li M, Hu Y, et al. Relationships
between stigma, social support, and distress in caregivers of Chinese children with
imperforate anus: a multicenter cross-sectional study. J Pediat Nus. (2019) 49:e15–
e20. doi: 10.1016/j.pedn.2019.0 7.008
33. Austin J, MacLeod J, Dunn D, Shen J, Perkins S. Measuring stigma in children
with epilepsy and their parents: instrument development and testing. Epilep Behav.
(2004) 5:472–82. doi: 10.1016/j.yebeh.2004.04.008
34. Jiaxuan M, Wanhua X, Chunhua M, Yeqing D, Lili D. Initial revision of Chinese
version of parents’ perception of uncertainty scale. Chin J Pract Nurs. (2013) 29:46–50.
doi: 10.3760/cma.j.issn.1672-7088.2013.28.023
35. Xiao S. The theoretical basis and research application of Social Support Scale. J
Clini Psychol Med. (1994) 1994:98–100.
36. Yang Y, Zhang B, Meng H, Liu D, Sun M. Mediating effect of social support
on the associations between health literacy, productive aging, and self-rated health
among elderly Chinese adults in a newly urbanized community. Medicine. (2019)
98:1–8. doi: 10.1097/MD.0000000 000015162
37. Chen J. Some people may need it, but not me, not now: seeking professional
help for mental health problems in Urban China. Transcult Psychiat. (2018) 55:754–
74. doi: 10.1177/1363461518792741
38. Xu M, Markström U, Lyu J, Xu L. Survey on tuberculosis patients in rural areas
in China: tracing the role of stigma in psychological distress. Int J Environ Res Public
Health. (2017) 14:1–9. doi: 10.17504/protocols.io.i2fcgbn
39. Peltzer K, Naidoo P, Matseke G, Louw J, McHunu G, Tutshana B.
Prevalence of psychological distress and associated factors in tuberculosis patients
in public primary care clinic s in South Africa. BMC Psychiatry. (2012) 12:1–
9. doi: 10.1186/1471-244X-12-89
40. Nguyen JT, Roberts C, Thorpe CT, Thorpe JM, Hogan SL, McGregor J, et al.
Economic and objective burden of caregiving on informal careg ivers of patients
with systemic vasculitis. Musculoskeletal Care. (2019) 17:282–7. doi: 10.1002/msc.
1394
41. Riffin C, Ness PHV. L.Wolff J, Fried T. Multifactorial examination of caregiver
burden in a national sample of family and unpaid caregivers. J Am Geriatr Soc. (2019)
67:277–83. doi: 10.1111/jgs.15664
42. Brehaut JC, Guèvremont A, Arim RG, Garner RE, Miller AR, McGrail KM,
et al. Changes in caregiver health in the years surrounding the birth of a child
with health problems: administrative d ata from B ritish Columbia. Med Care. (2019)
57:369–76. doi: 10.1097/MLR.0000000000001 098
43. Venkataramani M, Cheng TL, Solomon BS, Pollack CE. Caregi ver health
promotion in pediatric primary care settings: results of a national survey. J Pediatr.
(2017) 181:1–7.e2. doi: 10.1016/j.jpeds.2016.10.054
44. Jingting W, Nengliang Y, Yuanyuan W, Fen Z, Yany an L, Zhaohui G, et al.
Developing “Care Assistant”: A smartphone application to support caregivers of
children with acute lymphoblastic leukaemia. J Telemed Telecare. (2016) 22:163–
71. doi: 10.1177/1357633X15594753
45. Szulczewski L, Mullins LL, Bidw ell SL, Eddington AR, Pai ALH. Meta-analysis:
caregiver and youth uncertainty in pediatric chronic illness. J Pediatr Psychol. (2017)
42:395–421. doi: 10.1093/jpepsy/jsw097
46. Bell M, Biesecker BB, Bodurtha J, Peay HL. Uncertainty, hope, and coping
efficacy among mothers of children with Duchenne/Becker muscular dystrophy. Clini
Genet. (2019) 95:677–83. doi: 10.1111/cge.13528
47. Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al.
Stigma in health facilities: why it matters and how we can change it. BMC Med. (2019)
17:1–15. doi: 10.1186/s12916-019-1256- 2
48. Sari BA, Demirogullari B, Ozen O, iseri E, Kale N, Basaklar C. Quality of life
and anxiety in Turkish patients with anorectal malformation. J Paediatr Child Health.
(2014) 50:107–11. doi: 10.1111/jpc.12406
Frontiers in Medicine 10 frontiersin.org
