Medicare & Mental Health Coverage
Page 1 of 43 MLN1986542 January 2024
CPT codes, descriptions, and other data only are copyright 2023 American Medical Association. All Rights Reserved.
Applicable FARS/HHSARS apply. Fee schedules, relative value units, conversion factors and/or related components are
not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly
or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not
contained herein.
MLN BookletMedicare & Mental Health Coverage
Page 2 of 43 MLN1986542 January 2024
Table of Contents
What’s Changed? ................................................................................................................................ 4
Medicare-Covered Services................................................................................................................ 5
Non-Covered Services
........................................................................................................................ 9
Prescription Drug Coverage ............................................................................................................... 9
Medicare Advantage Organizations ................................................................................................... 9
Eligible Professionals ....................................................................................................................... 10
Provider Information ..........................................................................................................................11
Physician ......................................................................................................................................... 11
Clinical Psychologist (CP) .............................................................................................................. 12
Clinical Social Worker (CSW) ........................................................................................................ 13
Clinical Nurse Specialist (CNS)...................................................................................................... 15
Nurse Practitioner (NP)
.................................................................................................................. 16
Physician Assistant (PA) ................................................................................................................ 17
Certied Nurse-Midwife (CNM) ...................................................................................................... 19
Independently Practicing Psychologist (IPP) ................................................................................. 20
Certied Registered Nurse Anesthetist (CRNA)............................................................................. 21
Marriage & Family Therapist (MFT)
............................................................................................... 22
Mental Health Counselor (MHC) .................................................................................................... 22
Incident to Provision ......................................................................................................................... 23
Commonly Used CPT Codes ............................................................................................................ 24
Commonly Used Mental Health-Related CPT Codes .................................................................... 24
National Correct Coding Initiative .................................................................................................... 28

MLN BookletMedicare & Mental Health Coverage
Page 3 of 43 MLN1986542 January 2024
Outpatient Psychiatric Hospital Services ....................................................................................... 28
Telehealth ....................................................................................................................................... 29
Telehealth HCPCS Codes .............................................................................................................. 30
Partial Hospitalization Program ...................................................................................................... 31
Intensive Outpatient Program ........................................................................................................ 32
Community Mental Health Centers ................................................................................................ 33
Behavioral Health Integration Services .......................................................................................... 33
Medical Records Checklist: Outpatient Psychiatric Services ....................................................... 34
Acute Care Hospital .......................................................................................................................... 37
Inpatient Psychiatric Facility Services ............................................................................................ 37
Medical Records Requirements ..................................................................................................... 37
Medical Records Checklist: Inpatient Psychiatric Services .......................................................... 38
Coverage Period ............................................................................................................................ 42
Same Day Billing Guidelines ............................................................................................................ 42
Resources .......................................................................................................................................... 43
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 4 of 43
What’s Changed?
●
Added a social determinants of health risk assessment as an optional annual wellness visit
element (page 5)
●
Added information about an annual wellness visit being a community health integration
initiating visit (page 5)
●
Added information about caregiver training services (page 6)
●
Added community health integration when covered as mental health services (page 6)
●
Added information on intensive outpatient program services (pages 7, 32)
●
Added telehealth non-facility payment rate through 2024 (page 7)
●
Added marriage and family therapists as eligible practitioners (pages 7, 22)
●
Added mental health counselors as eligible practitioners (pages 8, 22)
●
Added principal illness navigation when covered as mental health services (page 8)
●
Updated payment rate for clinical social workers (page 14)
●
Added information about an exception to the direct supervision requirement for “incident to”
services and supplies (page 23)
●
Added 2 new HCPCS codes for psychotherapy for crisis services (page 27)
●
Added information about HCPCS code G0136 (pages 28, 30)
●
Added 2025 in-person visit requirements for mental health services provided by telehealth
(page 29)
●
Added information about marriage and family therapists and mental health counselors
providing telehealth services (page 29)
●
Added frequency information for partial hospitalization program plan of care certication (page 31)
Substantive content changes are in dark red.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 5 of 43
Medicare-covered behavioral health services, typically known as mental health and substance use
services, can aect a patient’s overall well-being. It’s important to understand Medicare’s covered
services and who can provide them.
Anyone experiencing a mental health crisis, including substance use crisis or thoughts of suicide,
can get condential support 24/7 by calling 988 or visiting 988lifeline.org. Visit the Substance
Abuse and Mental Health Administration 988 Partner Toolkit for information and resources.
Medicare-Covered Services
We may cover these behavioral health and wellness services:
●
Alcohol misuse screening and counseling for adults who use alcohol but aren’t dependent; if you
detect misuse, we cover up to 4 brief, face-to-face counseling sessions per year if the patient is
competent and alert during counseling
●
Alcohol treatment, detoxication, outpatient hospital treatment, and rehabilitative services,
including inpatient hospital stays
●
Annual wellness visit (AWV) to develop or update a personalized prevention plan, including health
risk assessment and depression screening
●
If you detect cognitive impairment at an AWV or other routine visit, you may perform a more
detailed cognitive assessment and develop a care plan during a separate visit
● Starting in 2024, we’ll cover a Social Determinants of Health (SDOH) Risk Assessment at no
cost to the patient when it’s provided as an optional AWV element (as part of the same visit
with the same date of service as the AWV)
● The AWV can be a community health integration (CHI) or principal illness navigation (PIN)
initiating visit when the practitioner identies an unmet SDOH need that prevents the patient
from carrying out the recommended personalized prevention plan
●
Advance care planning (ACP) to discuss a patient’s health care wishes if they can’t make
decisions about their care, as part of the AWV or a separate Part B service, including an
advance directive
●
Behavioral health integration (BHI) by clinical sta to assess, monitor, and plan care
●
Biofeedback therapy, where patients learn non-drug treatments to control bodily responses, like
heart rate and muscle tension
MLN BookletMedicare & Mental Health Coverage
Page 6 of 43 MLN1986542 January 2024
●
Bundled substance use disorder (SUD) payments (see HCPCS G2086, G2087, and G2088 billing
codes) for:
●
SUD management and counseling
●
SUD services provided in an oce setting, including:
▪
Overall management
▪
Care coordination
▪
Individual and group psychotherapy
▪
Substance use counseling
Opioid Treatment Programs
We now pay certied Opioid Treatment Programs (OTPs) through bundled opioid use disorder
(OUD) Medicare Part B treatment services payments. Covered services include FDA-approved
opioid agonist and antagonist medication (including methadone, buprenorphine, and naltrexone)
and their administration (if applicable), substance use counseling, individual and group therapy,
toxicology testing, intake activities, periodic assessments, take-home supplies of naloxone, and
intensive outpatient program services.
Opioid Treatment Program Directory and OTPs Billing & Payment have more information.
●
Caregiver-focused behavioral health risk assessment of their own behavior and health risks, which
benets the patient
●
We’ll pay for caregiver training services when a physician, non-physician practitioner (NPP), or
therapist provides them as part of the patient’s individualized treatment plan or therapy plan of care
●
Chemical and electrical aversion therapy to condition a person to avoid undesirable behavior by
pairing the behavior with unwanted stimuli
●
Community health integration (CHI) services help patients who have unmet social needs that
aect the diagnosis and treatment of their medical problems identify and connect with appropriate
clinical and social support resources
●
Practitioners may provide CHI services monthly, as medically necessary, following an initiating
Evaluation and Management (E/M) visit (CHI initiating visit) where the practitioner identies
the presence of SDOH needs that signicantly limit their ability to diagnose or treat the patient
problems addressed in the visit
●
Community health workers, care navigators, peer support specialists, and other auxiliary
personnel may be employed by community-based organizations (CBOs) if the billing practitioner
provides the required supervision for these services, similar to other care management services
●
Cognitive assessment and care planning, a comprehensive evaluation of a new or existing
patient who exhibits cognitive impairment signs and symptoms, required to establish or conrm a
diagnosis, etiology, and condition severity
MLN BookletMedicare & Mental Health Coverage
Page 7 of 43 MLN1986542 January 2024
●
Chronic care management (CCM) and complex CCM for patients with multiple chronic conditions
placing them at high risk
●
Chronic pain management (CPM) for patients with chronic pain
●
Depression screening, up to 15 minutes annually, when sta-assisted depression care supports
can assure accurate diagnosis, eective treatment, and follow-up; screening by clinical sta in a
primary care setting who can advise the physician of results and coordinate treatment referrals
●
Diagnostic psychological and neuropsychological tests
●
Drug therapy or pharmacological management using medications to treat a disease
●
Drug withdrawal treatment to monitor signs and symptoms after changes in regular drug dose
●
Electroconvulsive therapy (ECT) treating depression and other mental illness that involves passing
small electric currents through the brain, intentionally triggering a seizure
●
Family psychotherapy with or without the patient present, as medically reasonable and necessary,
with patient treatment as the primary purpose
●
Health and behavioral assessment and intervention that identies or treats psychological, behavioral,
emotional, cognitive, and social factors important to prevent, treat, or manage physical health issues
●
Hypnotherapy
●
Individual and group psychotherapy; individual therapy with 1 or more therapists or more than 1
person in a therapy session with 1 or more therapists
●
Individual activity therapy that’s part of a partial hospitalization program (PHP), which may be
cognitive, physical, social, and spiritual but not recreational or diversionary
●
PHP, a structured, intensive, outpatient psychiatric services program, is an alternative to
inpatient psychiatric care provided during the day (doesn’t require an overnight stay) through a
hospital outpatient department or community mental health center (CMHC)
●
Initial preventive physical exam (IPPE) to review medical and social health history and provide
preventive services education, counseling, and referral, as appropriate
●
Intensive outpatient program (IOP) services
●
Interactive psychotherapy
●
Interactive telecommunications, including 2-way, interactive audio-only technology to diagnose,
evaluate, or treat certain mental health or SUDs using telehealth services if the patient is in their home
●
Hospital clinical sta must have the capability to provide 2-way, interactive, audio-video
technology services but may use audio-only technology given an individual patient’s
technological limitations, abilities, or preferences
●
You can provide telehealth using 2-way, interactive, audio-only technology through
December 31, 2024
●
Telehealth services provided to people in their homes will be paid at the non-facility PFS rate
through December 31, 2024
●
Marriage and family therapist (MFT) services (also available through telehealth)
MLN BookletMedicare & Mental Health Coverage
Page 8 of 43 MLN1986542 January 2024
●
Medication for Opioid Use Disorder (MOUD) management when a patient agrees to a medication
trial period treatment option and its eectiveness is monitored
●
Medication-Assisted Treatment (MAT) uses medications with counseling and behavioral therapy
to treat SUDs, including OUDs; when a certied opioid treatment program (OTP) provider treats
OUDs, we pay for certain medications and services
● Mental health counselor (MHC) services (also available through an acceptable telehealth mental
health disorder service site)
● Addiction counselors or alcohol and drug counselors who meet the applicable MHC
requirements can enroll in Medicare as MHCs
●
Narcosynthesis, a form of narcoanalysis when a patient recalls repressed memories under hypnosis
● PIN services help patients who are diagnosed with high-risk conditions (for example, mental
health conditions, substance use disorder, and cancer) identify and connect with appropriate
clinical and social support resources
● PIN services can be performed after a psychiatric evaluation, which can serve as the initiating visit
● Principal illness navigation-peer support (PIN-PS) services are similar to PIN services except they
have more focus on services performed by peer support specialists under general supervision
●
Psychiatric collaborative care services using BHI to enhance primary care services and include a
psychiatric consultant
●
Psychoanalysis that treats mental disorders by investigating the interaction of conscious and
unconscious elements
●
Psychiatric evaluation that systematically evaluates a psychiatric disorder’s causes, symptoms,
course, and consequences
●
Screening, brief intervention, and referral to treatment (SBIRT) services that are early
interventions for people with non-dependent substance use to help them prevent more extensive
or specialized treatment
●
SUD treatment in a patient’s home (an acceptable telehealth substance use treatment or a
co-occurring mental health disorder service site)
●
Tobacco use cessation counseling
●
Therapeutic activities that can improve the patient’s condition, like occupational therapy,
recreational therapy, and milieu therapies
●
Transitional care management, within 30 days of an inpatient hospital setting discharge,
interactive contact, certain non-face-to-face services, and face-to-face visits
●
Urgent care to treat sudden illness or injury that doesn’t need emergency medical attention to
prevent disability or death
Your patients can nd more information in the Roadmap to Behavioral Health guide to
understand how to use their health coverage to improve their mental and physical health.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 9 of 43
Non-Covered Services
We don’t cover these mental health services:
●
Environmental intervention or modications
●
Adult day health programs, like structured therapeutic health services and supervised activities
●
Biofeedback training (any modality)
●
Pastoral counseling
●
Report preparation
●
Results or data interpretation or explanation
●
Hemodialysis specically for treating schizophrenia (experimental)
●
Transportation or outpatient meals
●
Phone apps
Prescription Drug Coverage
Medicare Part A and Part B generally don’t cover drugs, but Part B covers some medications patients can’t
self-administer. For other prescription coverage, patients must enroll in a separate Medicare drug plan.
Drug plans cover certain protected mental health treatment drug classes, including antipsychotics,
antidepressants, and anticonvulsants. Drug plans must cover most medications in these drug classes,
with some exceptions.
Medicare Advantage Organizations
Medicare Advantage (MA) enrollees can get Part A, Part B, and Part D benets under a single
plan. MA Plans provide Part B-covered mental health services and may oer certain (for example,
telehealth) benets beyond what Part B pays. They may also provide supplemental benets Parts
A or B don’t cover. For example, supplemental mental health benets may address coping with life
changes, conict resolution, or grief counseling, all oered as individual or group sessions.

MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 10 of 43
Eligible Professionals
The tables below list the coverage requirements for behavioral health services and the Medicare
Physician Fee Schedule (PFS) payment amount that physicians and these practitioners are eligible
to bill and be paid under the Medicare Part B Program:
●
Physicians (Medical Doctors (MDs) and Doctors of Osteopathy (DOs)), particularly Psychiatrists
●
Clinical Psychologists (CPs)
●
Clinical Social Workers (CSWs)
●
Clinical Nurse Specialists (CNSs)
●
Nurse Practitioners (NPs)
●
Physician Assistants (PAs)
●
Certied Nurse-Midwives (CNMs)
●
Independently Practicing Psychologists (IPPs)
●
Certied Registered Nurse Anesthetists (CRNAs) (supervision of diagnostic psychological and
neuropsychological tests)
● Marriage and Family Therapists (MFTs)
● Mental Health Counselors (MHCs)
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 11 of 43
Provider Information
These tables list individual provider-type required qualications, coverage, and payment criteria. Each
provider type must meet all qualications and coverage requirements. See the Commonly Used CPT Codes
section for specic billing codes.
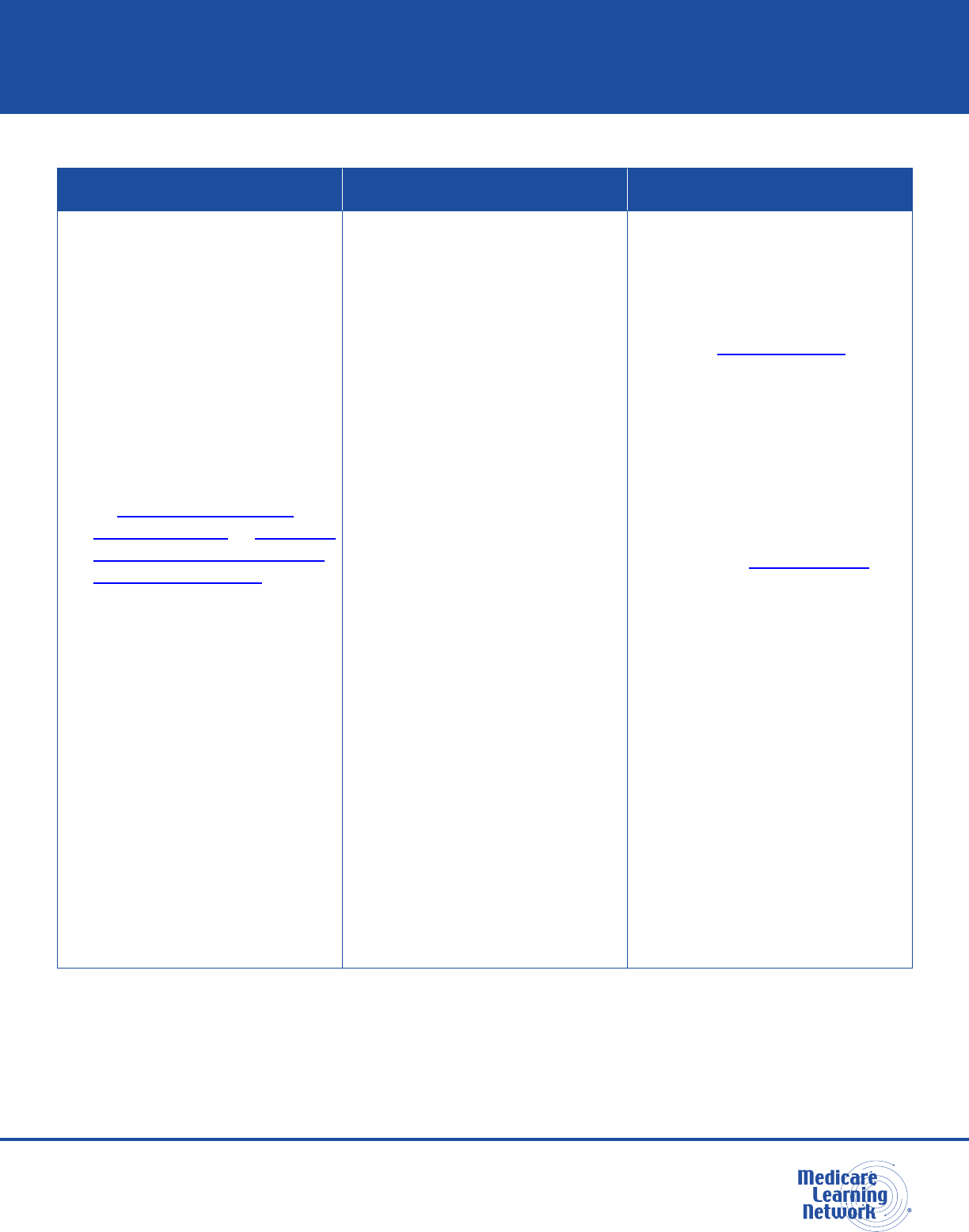
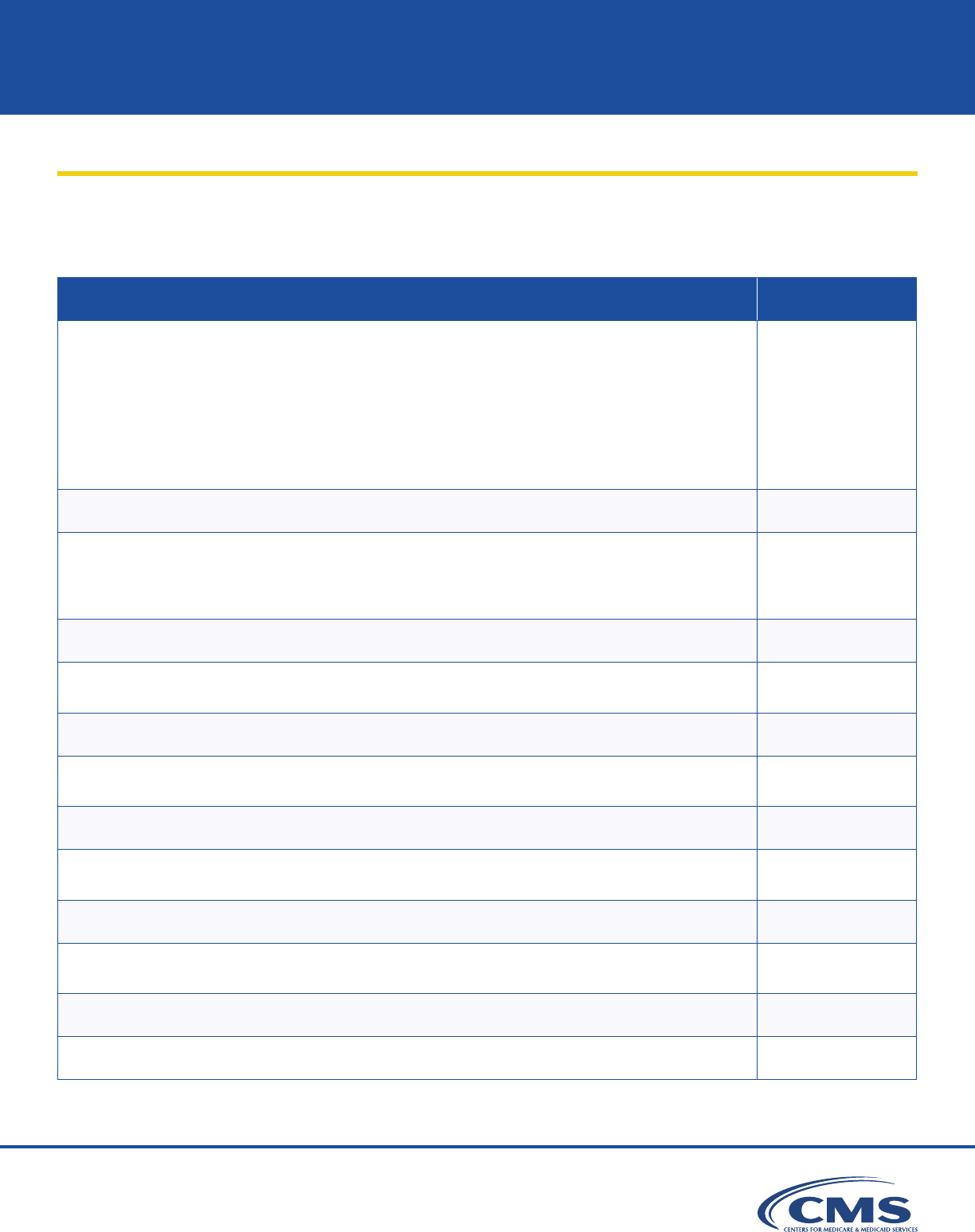
Table 1. Physician
Required Qualications Coverage Requirements Payment
●
MD or DO
●
Act within the scope of
your license
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
Generally, in addition to
performing tests, you
may also supervise the
performance of diagnostic
psychological and
neuropsychological tests
●
You may have services
and supplies provided
incident to your personal
professional services
●
Paid at 100% under the
Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 12 of 43
Table 2. Clinical Psychologist (CP)
Required Qualications Coverage Requirements Payment
●
Psychology doctoral degree
●
Licensed or certied in the
state where you practice at
the independent level and
directly provide diagnostic,
assessment, preventive, and
therapeutic patient services
●
Legally authorized to practice
psychology in the state
where you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
If the patient consents, you
must attempt to consult their
attending or primary care
physician about provided
services and either:
●
Document the date the
patient consented or
declined consultation
and the consultation
dates in the patient’s
medical record
●
If consultations are
unsuccessful, document
that in the patient’s
medical record with the
date and the physician
notication method
(doesn’t apply if the
physician referred the
patient to a CP)
●
Generally, in addition to
personally performing
diagnostic psychological
and neuropsychological
tests, you may supervise
the performance of
diagnostic psychological and
neuropsychological tests
●
You may have services
and supplies provided
incident to your personal
professional services
●
We pay only on assignment
●
Paid at 100% of assigned
services under the
Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 13 of 43
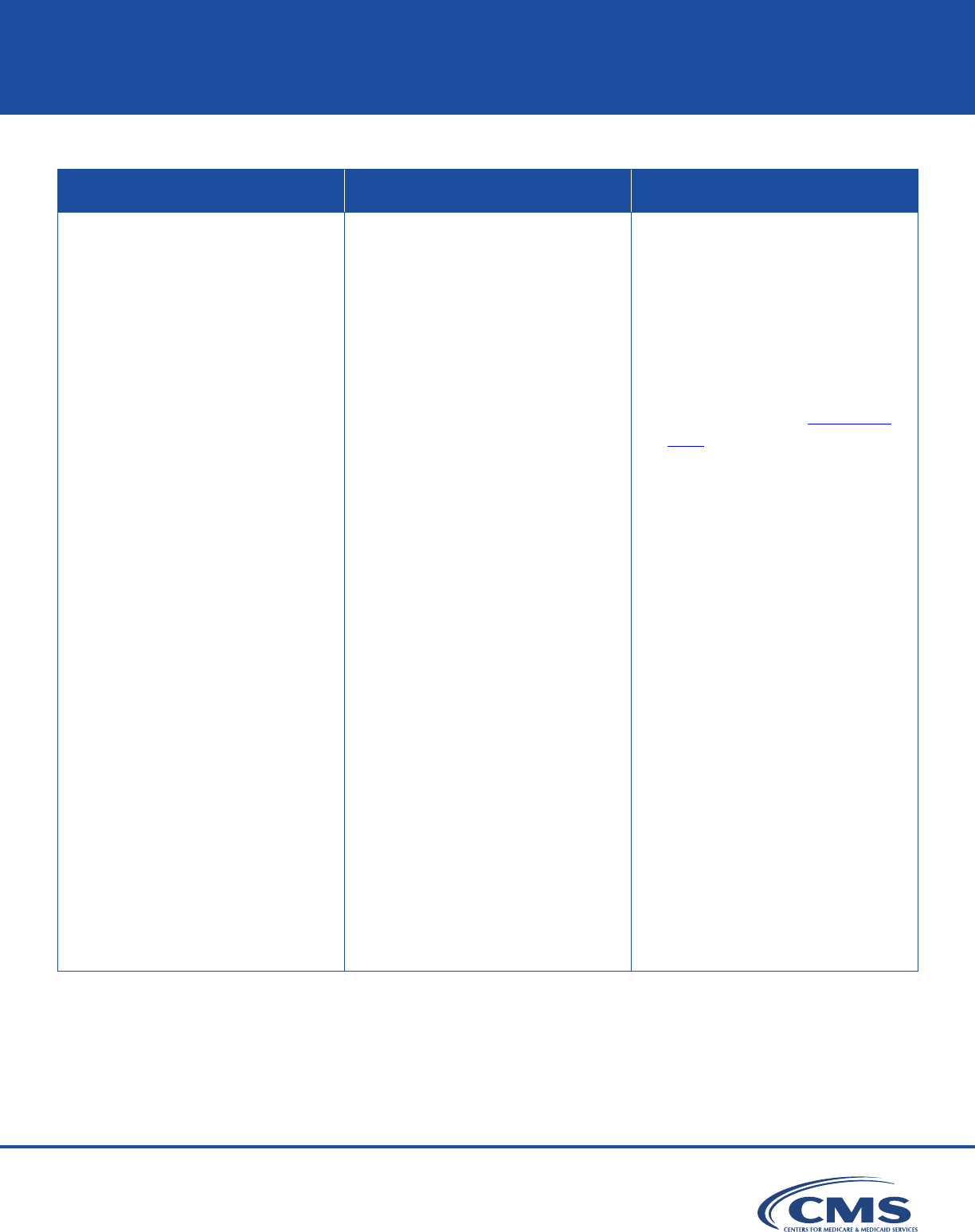
Table 3. Clinical Social Worker (CSW)
Required Qualications Coverage Requirements Payment
●
Social work master’s or
doctoral degree
●
At least 2 years of supervised
clinical social work
●
Licensed or certied CSW
by the state where you
provide services
●
Legally authorized to
practice clinical social work
in the state where you
provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
You provide mental health
services for diagnosing and
treating a mental illness and
you’re legally authorized to
perform them under state law
●
We don’t pay CSWs
under the CSW benet
category for their hospital
inpatient services
●
We cover CSW hospital
outpatient services and pay
for CSW services under
the CSW benet category
when hospitals bill under the
CSW’s NPI
●
We don’t pay under the
CSW benet category for
CSW services to patients
under a PHP or an IOP
by a hospital outpatient
department or CMHC
●
We don’t pay under the
CSW benet category
for CSW services to SNF
inpatients and patients
in Medicare-participating
ESRD facilities if the
services are under the
respective provider’s
participation requirements
●
We pay only on assignment
MLN Booklet
MLN1986542 January 2024
Medicare & Mental Health Coverage
Page 14 of 43
Table 3. Clinical Social Worker (CSW) (cont.)
Required Qualications Coverage Requirements Payment
●
If you practice in a state
that doesn’t have licensure
or certication and you
completed at least 2 years or
3,000 hours of post-master’s
degree clinical supervised
experience in social work
practice in an appropriate
setting (for example, a
hospital, SNF, or clinic)
●
We may cover ancillary CSW
services when provided as
auxiliary personnel incident
to the personal professional
services of a physician, a
CP, a CNS, an NP, a PA, or
a CNM
●
We don’t cover services
provided incident to your
personal professional services
● Paid at 80% of the lesser
of the actual charge for the
service or 75% of the CP’s
Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 15 of 43
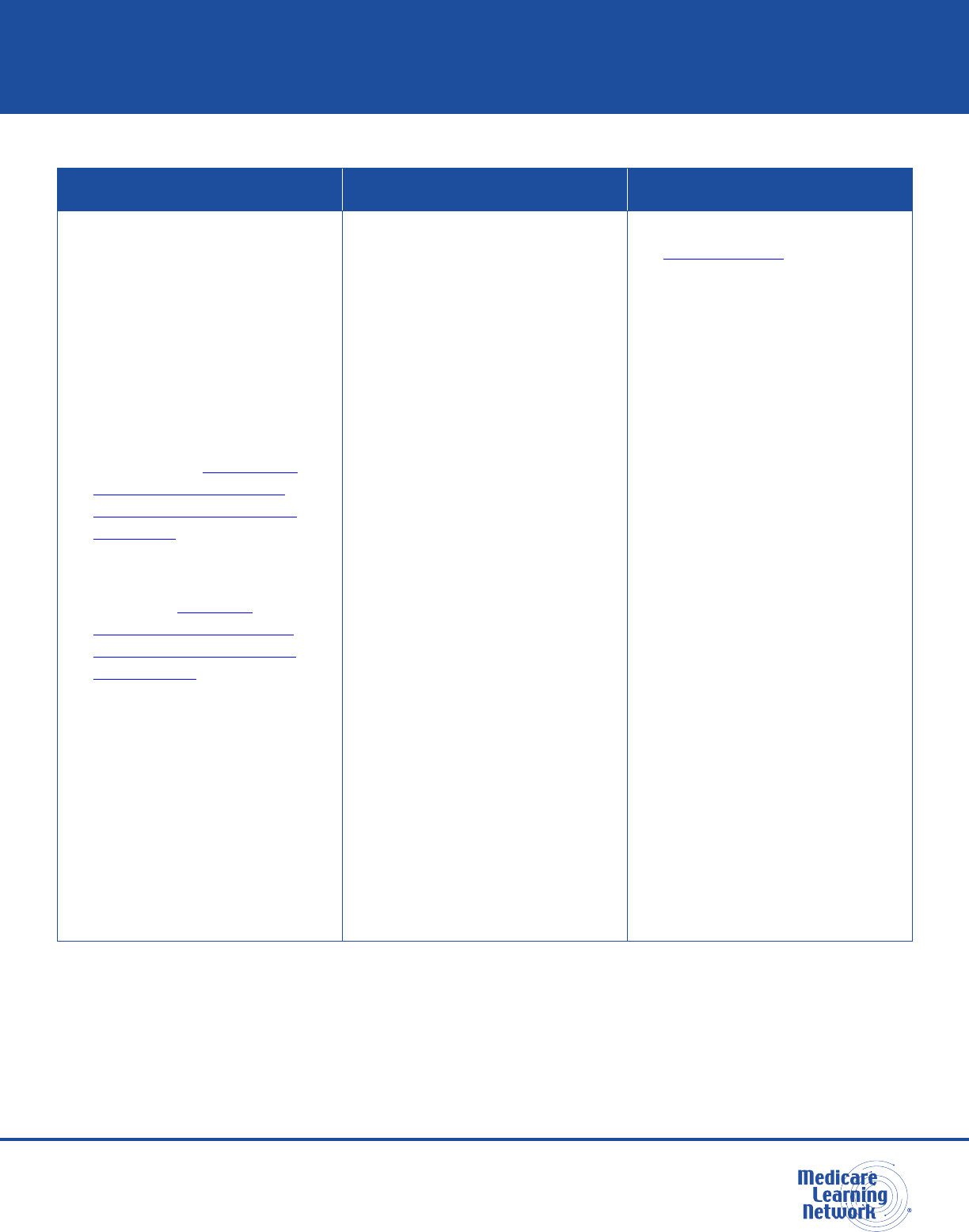
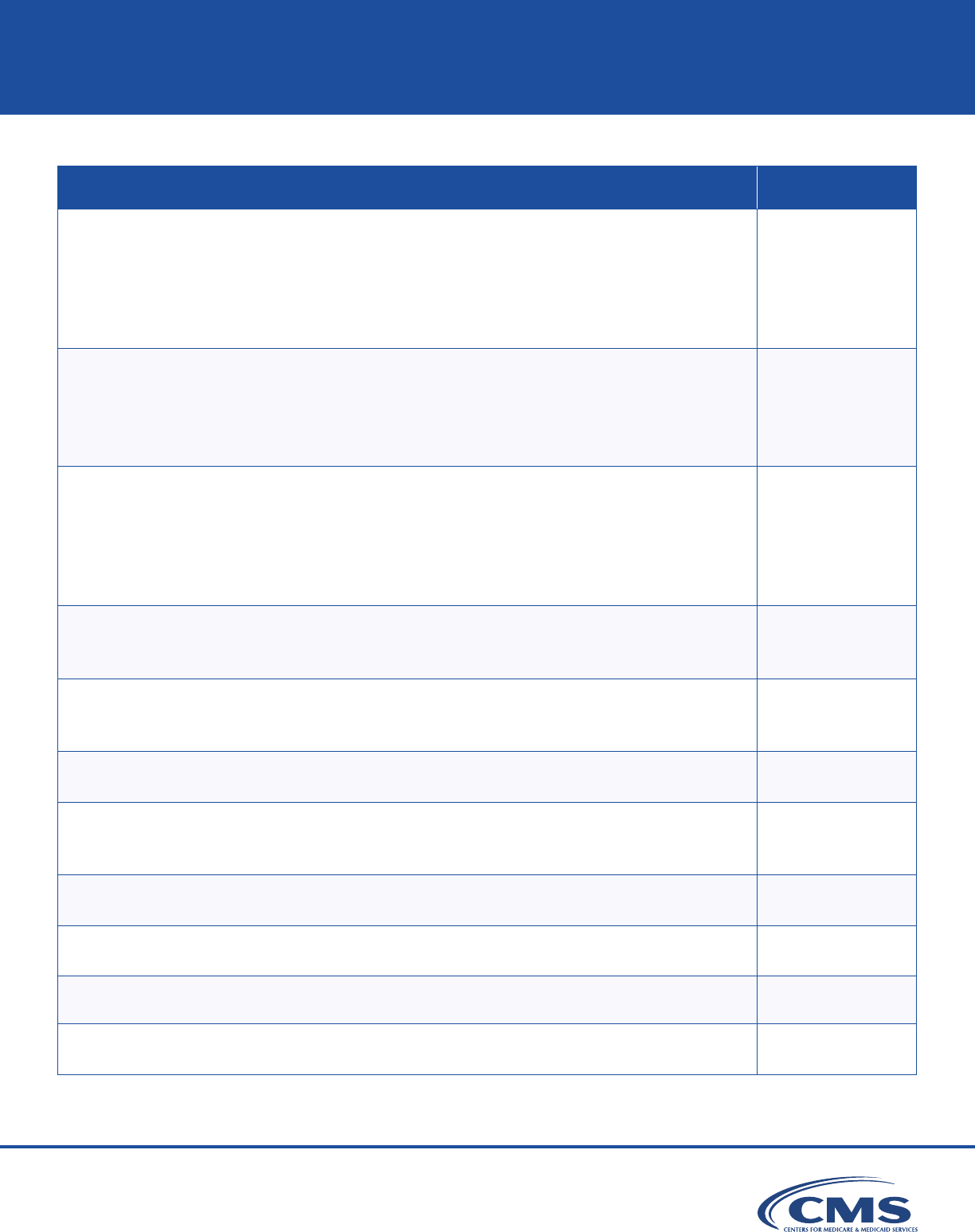
Table 4. Clinical Nurse Specialist (CNS)
Required Qualications Coverage Requirements Payment
●
Registered nurse (RN)
currently licensed in the
state where you practice
and authorized to provide
CNS services according to
state law
●
Doctor of Nursing Practice
or master’s degree in a
dened clinical nursing
area from an accredited
educational institution
●
Certied as a CNS by
a recognized national
certifying body with
established CNS standards
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
We consider the services
physicians’ services if
they’re provided by an MD
or a DO
●
You provide the services
while working in collaboration
with a physician
●
We may cover assistant-at-
surgery services you provide
●
You may personally perform
diagnostic psychological
and neuropsychological tests
to the extent authorized by
state law to perform tests in
collaboration with a physician
as required under the
CNS benet; we authorize
CNSs to supervise the
performance of diagnostic
tests according to state law
and scope of practice
●
You may have services
and supplies provided
incident to your personal
professional services
●
We pay only on assignment
●
If you provide services
on assignment, you can’t
charge a patient more than
the amounts permitted
under 42 CFR 424.55
●
If a patient paid for a
service over these
limits, you must refund
their payment
●
We pay for services at
80% of the lesser of the
actual charge or 85% of the
amount a physician gets
under the Medicare PFS
●
We pay for assistant-at-
surgery services directly at
85% of 16% of the amount
a physician gets under the
Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 16 of 43
Table 5. Nurse Practitioner (NP)
Required Qualications Coverage Requirements Payment
●
RN licensed and authorized
by the state where you
provide NP services
according to state law
●
Be a registered professional
nurse who’s authorized by
the state where they provide
services to practice as an
NP by December 31, 2000
●
Got Medicare NP billing
privileges for the rst time
since January 1, 2003, and:
●
NP certied by a
recognized national
certifying body with
established NP standards
●
Master’s degree in
nursing or a Doctor
of Nursing Practice
Doctoral degree
●
Got Medicare NP billing
privileges for the rst time
before January 1, 2003,
and meets certication
requirements
●
Got Medicare NP billing
privileges for the rst time
before January 1, 2001
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
We consider the services
physicians’ services if they’re
provided by an MD or a DO
●
You provide the services
while working in collaboration
with a physician
●
We may cover assistant-at-
surgery services you provide
●
You may personally perform
diagnostic psychological and
neuropsychological tests
to the extent authorized
by state law to perform
tests in collaboration with a
physician as required under
the NP benet; we authorize
NPs to supervise the
performance of diagnostic
tests according to state law
and scope of practice
●
You may have services
and supplies provided
incident to your personal
professional services
●
We pay only on assignment
●
If you provide services
on assignment, you can’t
charge a patient more than
the amounts permitted
under 42 CFR 424.55
●
If a patient paid for a
service over these
limits, you must refund
their payment
●
We pay for services at
80% of the lesser of the
actual charge or 85% of the
amount a physician gets
under the Medicare PFS
●
We pay for assistant-at-
surgery services directly at
85% of 16% of the amount
a physician gets under the
Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 17 of 43
Table 6. Physician Assistant (PA)
Required Qualications Coverage Requirements Payment
●
Licensed by the state where
you practice and 1 of these
criteria apply:
●
Graduated from
a PA educational
program accredited
by the Accreditation
Review Commission
on Education for the
Physician Assistant
(or its predecessor
agencies, Commission
on Accreditation of
Allied Health Education
Programs and
Committee on Allied
Health Education and
Accreditation)
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
We consider the services
physicians’ services if
provided by an MD or a DO
●
Someone who meets all PA
qualications provides
the services
●
You provide services under
an MD or a DO’s supervision
●
We may cover assistant-at-
surgery services you provide
●
We pay only on assignment
●
If you provide services
on assignment, you can’t
charge a patient more than
the amounts permitted
under 42 CFR 424.55
●
If a patient paid for a
service over these
limits, you must refund
their payment
●
We pay for your professional
services, including services
and supplies provided
incident to your services
●
We pay for your professional
services provided in all rural
and non-rural settings
and areas
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 18 of 43
Table 6. Physician Assistant (PA) (cont.)
Required Qualications Coverage Requirements Payment
●
Passed a national
certication exam
administered by
National Commission
on Certication of
Physician Assistants
●
You may personally perform
diagnostic psychological and
neuropsychological tests
under physician supervision
as required under the
PA benet category and
as authorized by state
law; we authorize PAs to
supervise the performance
of diagnostic tests according
to state law and scope
of practice
●
You may have services
and supplies provided
incident to your personal
professional services
●
We pay only if no facility or
other provider charges or we
didn’t pay any other service
amount they provided
●
We pay for services at 80%
of the lesser of the actual
charge or at 85% of the
amount a physician gets
under the Medicare PFS
●
We pay for your assistant-
at-surgery services directly
at 85% of 16% of the
amount a physician gets
under the Medicare PFS
●
We pay for services
provided incident to a PA
outside a hospital at 85% of
the amount a physician gets
under the Medicare PFS
●
When you bill a hospital
inpatient and outpatient
service directly, we unbundle
the payment and pay
you directly
●
You can bill Medicare and
we pay for your services
directly like we do NPs
and CNSs
●
You may reassign your
service payment rights and
incorporate as a group of
practitioners only in your
specialty and bill Medicare
like NPs and CNSs do
●
You must bill under your NPI
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 19 of 43
Table 7. Certied Nurse-Midwife (CNM)
Required Qualications Coverage Requirements Payment
●
RN legally authorized to
practice as a nurse-midwife
in the state where you
provide services
●
Successfully completed a
nurse-midwives program
of study and got clinical
experience accredited by
an accrediting body the
U.S. Department of
Education approves
●
Certied as a Nurse-Midwife
by American College of
Nurse-Midwives or American
College of Nurse-Midwives
Certication Council
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
We consider the services
physicians’ services if they’re
provided by an MD or a DO
●
You provide the services
without physician
supervision and without
association with a physician
or other health care provider,
unless otherwise required
under state law
●
You may personally perform
diagnostic psychological
and neuropsychological
tests without physician
supervision or oversight as
required under the CNM
benet category and as
authorized under state
law; we authorize CNMs to
supervise diagnostic tests
performed according to state
law and scope of practice
●
You may have services
and supplies provided
incident to your personal
professional services
●
We pay only on assignment
●
If you provide services
on assignment, you can’t
charge a patient more than
the amounts permitted
under 42 CFR 424.55
●
If a patient paid for a
service over these
limits, you must refund
their payment
●
We pay for services at 80%
of the lesser of the actual
charge, or 100% of the
amount a physician gets
under the Medicare PFS
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 20 of 43
Table 8. Independently Practicing Psychologist (IPP)
Required Qualications Coverage Requirements Payment
●
Psychologist who isn’t a CP
●
Meets 1 of these criteria:
●
Practices independent
of an institution, agency,
or physician’s oce and
is licensed or certied to
practice psychology in
the state or jurisdiction
where you provide
the services
●
Practicing psychologist
who provides services in
a jurisdiction that doesn’t
issue licenses
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
Provide services on your
own responsibility, free
of administrative and
professional control of an
employer (for example,
physician, institution,
or agency)
●
You treat your own patients
●
When you practice in an
oce in an institution:
●
The oce is conned to
a separately identied
part of the facility used
solely as an oce
and not confused as
extending throughout the
entire institution
●
You operate a private
practice (patients outside
an institution and
non-institutional patients)
●
You may perform diagnostic
psychological and
neuropsychological tests
when a physician or certain
NPPs order them
●
You can bill directly and
collect and retain service fees
●
We don’t subject diagnostic
psychological and
neuropsychological tests to
assignment; however, on
the claim, you must include
the name and address of
the physician or NPP who
orders the tests
●
Paid at 100% of Medicare
PFS for diagnostic tests
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 21 of 43
Table 9. Certied Registered Nurse Anesthetist (CRNA)
Required Qualications Coverage Requirements Payment
●
Licensed as a registered
professional nurse by the
state where you practice
●
Meet any licensure
requirements the state
imposes on non-physician
anesthetists
●
Graduated from a nurse
anesthesia educational
program that meets
standards of Council on
Accreditation of Nurse
Anesthesia Educational
Programs (COA) or other
accreditation organization the
HHS Secretary designates
●
Passed a National
Board of Certication &
Recertication of Nurse
Anesthetists (NBCRNA)
certication exam
●
Graduated from a nurse
anesthesia educational
program that meets the
COA Educational Program’s
standards and, within 24
months of graduation,
passed a certication exam
from NBCRNA or another
certication organization the
HHS Secretary designates
●
Legally authorized to practice
medicine in the state where
you provide services
●
We don’t statutorily preclude
the services, and they’re
reasonable and necessary
●
You may personally perform
diagnostic psychological and
neuropsychological tests
under physician supervision
as required under the CRNA
benet category and as
authorized by state law;
we authorize CRNAs to
supervise the performance
of diagnostic tests
according to state law
and scope of practice
●
You can bill directly and
collect and retain
service fees
●
Paid at 100% under the
Medicare PFS
●
You may bill your services
directly to Medicare, get paid
directly, or have payment
made to any person or
entity (for example, hospital,
critical access hospital,
physician, group practice, or
ambulatory surgical center)
if you have an employment
or contractor relationship
that’s paying you or them
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 22 of 43
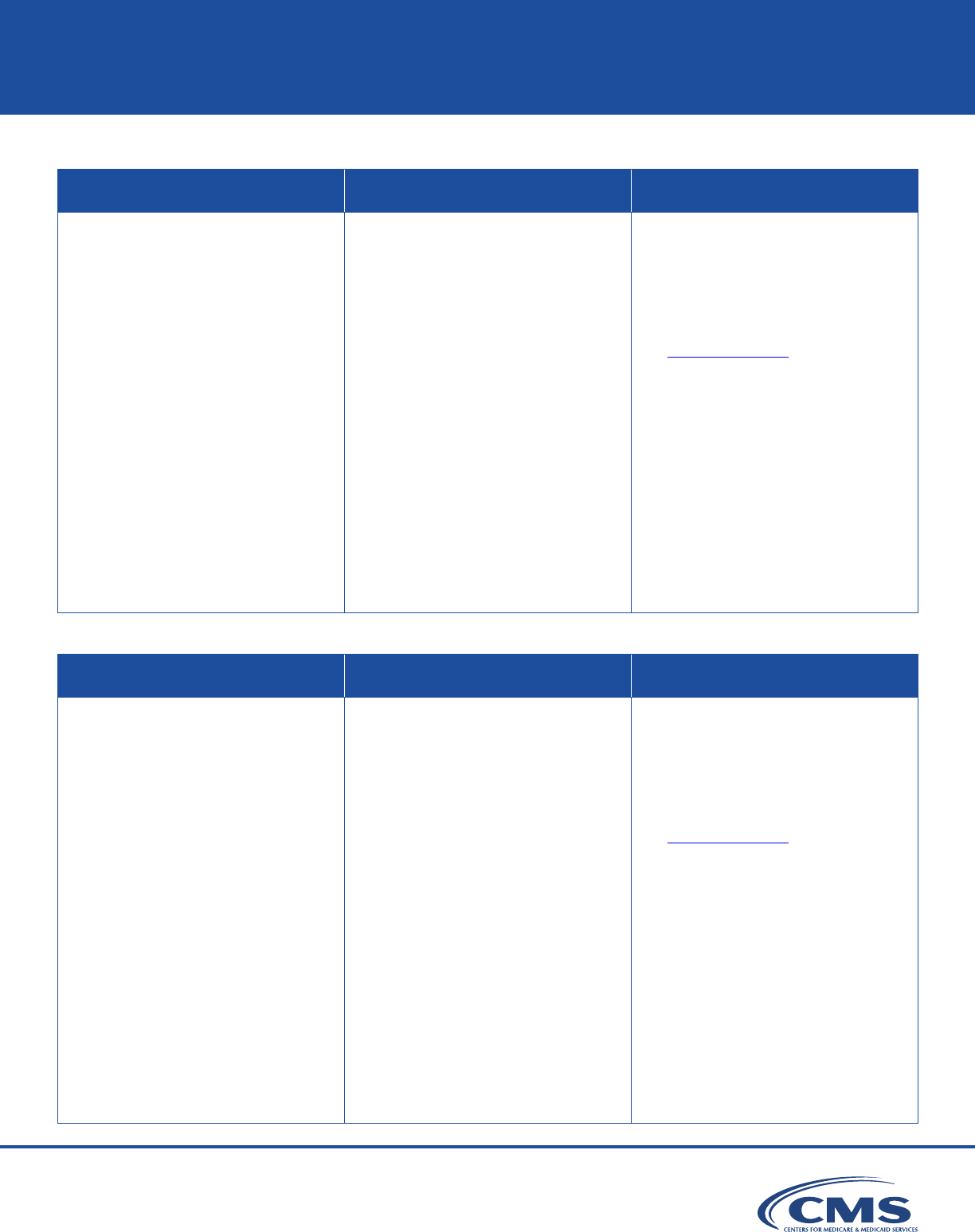
Table 10. Marriage & Family Therapist (MFT)
Required Qualications Coverage Requirements Payment
● Master’s or doctor’s degree
that qualies for licensure
or certication as an MFT
according to the state law
where you provide services
● Licensed or certied as an
MFT in the state where you
provide services
● After getting your degree,
you complete at least 2
years or 3,000 hours of
post-master’s degree clinical
supervised experience in
marriage and family therapy
in an appropriate setting (for
example, a hospital, SNF,
or clinic)
● Legally authorized to
practice as an MFT in
the state where you
provide services
● You may enroll in
Medicare and bill Medicare
independently beginning
January 1, 2024
● You may also still provide
services and supplies as
auxiliary personnel
incident to a physician’s
or certain NPP’s personal
professional service
● We pay only on assignment
● We pay for services at
80% of the lesser of the
actual charge or 75% of the
amount a CP gets under the
Medicare PFS
● We don’t pay under the MFT
benet category for MFT
services to patients under
a PHP or an IOP by
a hospital outpatient
department or CMHC
Table 11. Mental Health Counselor (MHC)
Required Qualications Coverage Requirements Payment
● Master’s or doctor’s degree
that qualies for licensure
or certication as an MHC
according to the state law
where you provide
MHC services
● Licensed or certied as an
MCH; a clinical professional
counselor; an addiction,
alcohol, or drug counselor;
or a professional counselor
in the state where you
provide services
● After getting your degree and
you complete at least 2 years
or 3,000 hours of clinical
supervised experience in
mental health counseling
● Legally authorized to practice
as an MHC in the state
where you provide services
● You may enroll in
Medicare and bill Medicare
independently beginning
January 1, 2024
● You may also still provide
services and supplies
as auxiliary personnel
incident to a physician’s
or certain NPP’s personal
professional service
● We pay only on assignment
● We pay for services at
80% of the lesser of the
actual charge or 75% of the
amount a CP gets under the
Medicare PFS
● We don’t pay under the
MHC benet category for
MHC services to patients
under a PHP or an IOP
by a hospital outpatient
department or CMHC
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 23 of 43
Incident to Provision
Physicians and certain NPPs have a provision under their benet category that authorizes them to
have ancillary services and supplies provided by auxiliary personnel “incident to” their own personal
professional services.
Physicians and specically CPs, NPs, CNSs, CNMs, and PAs can bill for these integral, although
incidental, services and supplies provided by auxiliary personnel as if they furnished the services
themselves and, are paid for these services as if they furnished them personally, if all the incident to
requirements are met. However, there’s no payment under the Medicare PFS to physicians or NPPs
for incident to services in an institutional setting (hospital or SNF).
●
Services and supplies are integral to the patient’s normal treatment course and the physician or
other listed NPP personally furnished an initial service to which the auxiliary personnel’s services
are incidental. The physician or NPP must remain actively involved in treating the patient.
●
The auxiliary personnel provide services and supplies without charge (included in the physician’s
or other listed NPP’s bill).
●
Services and supplies are an expense to the physician or other listed NPP.
●
Services and supplies are commonly oered in the physician’s or other listed NPP’s oce or clinic.
●
Typically, the incident to regulations require the physician or other listed NPP to furnish direct
supervision; they’re present in the oce suite and immediately available if needed.
We oer an exception to the direct supervision requirement for incident to behavioral health services
provided by auxiliary personnel. That is, incident to behavioral health services can be provided
under the general supervision of a physician or an NPP, instead of direct supervision. Under general
supervision, the physician or NPP may be contacted by phone if necessary, as the physician’s or
NPP’s presence isn’t required during a procedure.
We don’t dene behavioral health services by HCPCS codes; however, we generally understand
a behavioral health service to be any service a provider furnishes for the diagnosis, evaluation, or
treatment of a mental health disorder, including an SUD.
Physicians, NPPs, and practitioners can also serve as auxiliary personnel and provide services and
supplies incident to the personal professional services of another physician or NPP. Appropriate
payment can be made to the other supervising physician or NPP in this case if you meet all the
incident to requirements.
42 CFR 410.26 and 42 CFR 410.27 have more information.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 24 of 43
Commonly Used CPT Codes
With thousands of CPT codes, using the correct CPT code to show the mental health services you
provide to patients is essential for billing correctly.
Table 12. Commonly Used Mental Health-Related CPT Codes
Description CPT Code
Interactive complexity (List separately in addition to the code for primary procedure)
(Use 90785 in conjunction with codes for diagnostic psychiatric evaluation
[90791, 90792], psychotherapy [90832, 90833, 90834, 90836, 90837, 90838),
and group psychotherapy [90853])
(Use 90785 in conjunction with 90853 for the specied patient when group
psychotherapy includes interactive complexity)
90785
Psychiatric diagnostic evaluation 90791
Psychiatric diagnostic evaluation with medical services
(Use 90785 in conjunction with 90791, 90792 when the diagnostic evaluation
includes interactive complexity services)
90792
Psychotherapy, 30 minutes with patient 90832
Psychotherapy, 30 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90833
Psychotherapy, 45 minutes with patient 90834
Psychotherapy, 45 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90836
Psychotherapy, 60 minutes with patient 90837
Psychotherapy, 60 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90838
Psychotherapy for crisis; rst 60 minutes 90839*
Psychotherapy for crisis; each additional 30 minutes (List separately in addition
to code for primary service)
90840
Psychoanalysis 90845
Family psychotherapy (without the patient present), 50 minutes 90846
CPT only copyright 2023 American Medical Association. All rights reserved.
*Mental health code not approved for partial hospitalization program.

MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 25 of 43
Table 12. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Family psychotherapy (conjoint psychotherapy) (with patient present), 50 minutes 90847
Multiple-family group psychotherapy 90849*
Group psychotherapy (other than of a multiple-family group) 90853*
Electroconvulsive therapy (includes necessary monitoring) 90870
Assessment of aphasia (includes assessment of expressive and receptive
speech and language function, language comprehension, speech production
ability, reading, spelling, writing, eg, by Boston Diagnostic Aphasia Examination)
with interpretation and report, per hour
96105
Developmental test administration (including assessment of ne and/or gross
motor, language, cognitive level, social, memory and/or executive functions by
standardized developmental instruments when performed), by physician or other
qualied health care professional, with interpretation and report; rst hour
96112
Developmental test administration (including assessment of ne and/or gross
motor, language, cognitive level, social, memory and/or executive functions by
standardized developmental instruments when performed), by physician or other
qualied health care professional, with interpretation and report; each additional
30 minutes (List separately in addition to code for primary procedure)
96113
Neurobehavioral status exam (clinical assessment of thinking, reasoning and
judgment, [eg, acquired knowledge, attention, language, memory, planning and
problem solving, and visual spatial abilities]), by physician or other qualied
health care professional, both face-to-face time with the patient and time
interpreting test results and preparing the report; rst hour
96116
Neurobehavioral status exam (clinical assessment of thinking, reasoning and
judgment, [eg, acquired knowledge, attention, language, memory, planning and
problem solving, and visual spatial abilities]), by physician or other qualied
health care professional, both face-to-face time with the patient and time
interpreting test results and preparing the report; each additional hour (List
separately in addition to code for primary procedure)
96121
Psychological testing evaluation services by physician or other qualied
health care professional, including integration of patient data, interpretation of
standardized test results and clinical data, clinical decision making, treatment
planning and report, and interactive feedback to the patient, family member(s) or
caregiver(s), when performed; rst hour
96130
*Mental health code not approved for partial hospitalization program.
CPT only copyright 2023 American Medical Association. All rights reserved.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 26 of 43
Table 12. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Psychological testing evaluation services by physician or other qualied
health care professional, including integration of patient data, interpretation of
standardized test results and clinical data, clinical decision making, treatment
planning and report, and interactive feedback to the patient, family member(s) or
caregiver(s), when performed; each additional hour (List separately in addition to
code for primary procedure)
96131
Neuropsychological testing evaluation services by physician or other qualied
health care professional, including integration of patient data, interpretation of
standardized test results and clinical data, clinical decision making, treatment
planning and report, and interactive feedback to the patient, family member(s) or
caregiver(s), when performed; rst hour
96132
Neuropsychological testing evaluation services by physician or other qualied
health care professional, including integration of patient data, interpretation of
standardized test results and clinical data, clinical decision making, treatment
planning and report, and interactive feedback to the patient, family member(s) or
caregiver(s), when performed; each additional hour (List separately in addition to
code for primary procedure)
96133
Psychological or neuropsychological test administration and scoring by physician
or other qualied health care professional, two or more tests, any method; rst
30 minutes
96136
Psychological or neuropsychological test administration and scoring by physician
or other qualied health care professional, two or more tests, any method; each
additional 30 minutes (List separately in addition to code for primary procedure)
96137
Psychological or neuropsychological test administration and scoring by
technician, two or more tests, any method; rst 30 minutes
96138
Psychological or neuropsychological test administration and scoring by
technician, two or more tests, any method; each additional 30 minutes (List
separately in addition to code for primary procedure)
96139
Psychological or neuropsychological test administration, with single automated,
standardized instrument via electronic platform, with automated result only
96146
Health behavior assessment, or re-assessment (ie, health-focused clinical
interview, behavioral observations, clinical decision making)
96156**
Health behavior intervention, individual, face-to-face; initial 30 minutes 96158**
Health behavior intervention, individual, face-to-face; each additional 15 minutes
(List separately in addition to code for primary service)
96159**
**CPs, CSWs, MFTs, and MHCs can bill these codes.
CPT only copyright 2023 American Medical Association. All rights reserved.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 27 of 43
Table 12. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Health behavior intervention, group (2 or more patients), face-to-face; initial 30 minutes 96164**
Health behavior intervention, group (2 or more patients), face-to-face; each
additional 15 minutes (List separately in addition to code for primary service)
96165**
Health behavior intervention, family (with the patient present), face-to-face; initial
30 minutes
96167**
Health behavior intervention, family (with the patient present), face-to-face; each
additional 15 minutes (List separately in addition to code for primary service)
96168**
Health behavior intervention, family (without the patient present), face-to-face;
initial 30 minutes
96170**
Health behavior intervention, family (without the patient present), face-to-face;
each additional 15 minutes (List separately in addition to code for primary service)
96171**
Psychotherapy for crisis furnished in an applicable site of service (any place of
service at which the non-facility rate for psychotherapy for crisis services applies,
other than the oce setting); rst 60 minutes
G0017
Psychotherapy for crisis furnished in an applicable site of service (any place of
service at which the non-facility rate for psychotherapy for crisis services applies,
other than the oce setting); each additional 30 minutes (List separately in
addition to code for primary service)
G0018
**CPs, CSWs, MFTs, and MHCs can bill these codes.
CPT only copyright 2023 American Medical Association. All rights reserved.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 28 of 43
HCPCS code G0136 (Administration of a standardized, evidence-based social determinants of
health risk assessment tool, 5-15 minutes), not provided more often than every 6 months, can
also be provided with CPT code 90791 (Psychiatric diagnostic evaluation) and the health behavior
assessment and intervention (HBAI) services, described by CPT codes 96156, 96158, 96159, 96164,
96165, 96167, and 96168. We allow the HBAI services described by the above CPT codes, and any
successor codes, to be billed by CPs, CSWs, MFTs, and MHCs.
National Correct Coding Initiative
The National Correct Coding Initiative (NCCI) promotes national correct coding methods and oers
national guidance on code pair edits preventing billing certain services on the same day.
Outpatient Psychiatric Hospital Services
Outpatient psychiatric hospital services and supplies are:
●
Medically necessary for diagnostic study or if the patient’s condition is reasonably expected to
improve (see the Same Day Billing Guidelines section for more information)
●
Provided under an individualized, written plan of care (POC) that states the:
●
Type, amount, frequency, and services duration
●
Diagnosis
●
Expected goals (except when you only provide a few brief services)
●
Supervised and periodically evaluated by a physician who:
●
Prescribes the services
●
Determines the extent the patient reached treatment goals and if the POC should change
●
Provides supervision and direction to therapists treating the patient
●
Documents their involvement in the patient’s medical record
●
For diagnostic study or, at a minimum, designed to reduce or control a patient’s psychiatric
symptoms to prevent a relapse or hospitalization and improve or maintain their level of functioning
Generally, we cover these outpatient hospital psychiatric treatment services:
●
Medically necessary diagnostic services for patients when extended or direct observation is
necessary to determine functioning and interactions, identify problem areas, and prepare a POC
●
Individual and group psychotherapy with physicians, CPs, CSWs, or other eligible providers
authorized or licensed by the state where they provide services
●
Social workers, psychiatric nurses, and other sta trained to work with psychiatric patients
CPT only copyright 2023 American Medical Association. All rights reserved.

MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 29 of 43
●
Occupational therapy services, when part of a PHP or an IOP, that:
●
Require qualied occupational therapist skills
●
Are provided by, or under supervision of, a qualied occupational therapist
●
Are included in a patient’s POC
●
Activity therapies, when part of a PHP or an IOP, that:
●
Are individualized and essential for treating a patient’s diagnosed condition and progressing
toward treatment goals
●
Have a POC that clearly supports and shows each therapy’s need (not primarily recreational
or diversionary)
●
Family counseling services while treating a person’s condition
●
Patient training and education when they’re closely and clearly related to care and treating an
individual’s diagnosed psychiatric condition
●
Therapeutic drugs and biologicals a patient can’t self-administer
●
CCM to patients with multiple chronic conditions (for example, patients with dementia typically have
multiple chronic conditions that could involve physical and behavioral health issues, like depression)
Telehealth
Beginning in 2025, in-person visit requirements will apply for mental health services provided by telehealth.
This includes a required in-person visit within the 6 months before the initial telehealth treatment as
well as the required subsequent in-person visits at least every 12 months.
We’ll continue to dene direct supervision to permit the immediate availability of the supervising practitioner
through real-time audio and visual interactive telecommunications through December 31, 2024.
The regulations at 42 CFR 410.78(b)(3)(xiv) describe 2 exceptions to the in-person requirements that
take eect on January 1, 2025:
1. Patients who already get telehealth behavioral health services and have circumstances where
in-person care may not be appropriate
2. Groups with limited availability for in-person behavioral health visits have the exibility to arrange for
practitioners to provide in-person and telehealth visits with dierent practitioners, based on availability
The telehealth policies described above also apply to Rural Health Clinics (RHCs) and Federally
Qualied Health Centers (FQHCs).
Beginning January 1, 2024, MHCs and MFTs can provide and bill Medicare telehealth services.
Exceptions to the in-person visit requirement require a clear justication documented in the patient’s
medical record. Hospitals must also document that patients have a regular source of general medical
care and can get any needed point-of-care testing, including vital sign monitoring and lab studies.

MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 30 of 43
We created 3 Outpatient Prospective Payment System (OPPS)-specic HCPCS codes to describe
that the patient must be in their home and that no associated professional service is billed under the
PFS. Hospital sta must be licensed to provide these services consistent with all applicable state
scope of practice laws. We exempt these services from having sta physically located in the hospital
or outpatient department when providing services remotely using communication technology.
Table 13. Telehealth HCPCS Codes
Description HCPCS Code
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, initial 15-29 minutes, provided remotely by hospital sta who are
licensed to provide mental health services under applicable state law(s), when
the patient is in their home, and there is no associated professional service
C7900
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, initial 30-60 minutes, provided remotely by hospital sta who are
licensed to provide mental health services under applicable state law(s), when
the patient is in their home, and there is no associated professional service
C7901
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, each additional 15 minutes, provided remotely by hospital
sta who are licensed to provide mental health services under applicable
state law(s), when the patient is in their home, and there is no associated
professional service (list separately in addition to code for primary service)
C7902
Administration of a standardized, evidence based social determinants of health
risk assessment tool, 5-15 minutes
G0136
We assigned HCPCS codes C7900 and C7901 to ambulatory payment classications (APCs) based
on the PFS facility payment rates for CPT codes 96158 and 96159. C7902 is an add-on code;
payment is packaged, and the code isn’t assigned to an APC.
Generally, we don’t cover these outpatient hospital services:
●
Meals and transportation
●
Activity therapies, group activities, or other primarily recreational or diversionary services and programs
●
Outpatient psychosocial programs (we cover outpatient psychosocial components not primarily for
social or recreational purposes)
●
Vocational training related only to specic employment opportunities
CPT only copyright 2023 American Medical Association. All rights reserved.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 31 of 43
Partial Hospitalization Program
Partial hospitalization programs (PHPs) are distinct and structured programs that provide intensive
outpatient psychiatric care through active treatment by combining clinically recognized items and
services. We cover PHP in hospital outpatient departments and CMHCs.
Patients may pay a percentage of each doctor’s or other qualied mental health professional’s
approved service amount if they accept assignment. Patients may also pay each day’s PHP
services
coinsurance in a hospital outpatient setting or CMHC.
PHPs oer psychiatric treatment less than 24 hours a day to patients:
●
Discharged from an inpatient hospital treatment and a PHP replaces continued inpatient treatment
●
At reasonable inpatient hospitalization risk without partial hospitalization
PHPs must meet these program and patient criteria:
●
Active treatment includes an individual POC with coordinated services designed for the patient’s needs
●
The POC treatment includes a physician-directed multi-disciplinary team care approach certifying
the patient’s need for partial hospitalization therapeutic services a minimum of 20 hours per week,
and this determination must occur no less frequently than monthly
●
Treatment goals should be:
●
Measurable
●
Functional
●
Time framed
●
Medically necessary
●
Directly related to admission reason
●
The patient requires a comprehensive, highly structured, scheduled, multi-modal individualized
POC requiring medical supervision and coordination because their mental disorder severely
interferes with multiple areas of daily life (social, vocational, activities of daily living (ADLs) or
instrumental ADLs, and educational functioning)
●
The patient can cognitively and emotionally participate in the active treatment process and tolerate
its intensity
Partial hospitalization services don’t include:
●
Hospital inpatient services
●
Meals, self-administered medications, transportation
●
Support groups where people talk and socialize (dierent than group psychotherapy, which we cover)
●
Job skills training or testing skills not part of mental health treatment

MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 32 of 43
Intensive Outpatient Program
Intensive outpatient services are provided under an IOP.
Outpatients may get IOP services from their hospital, or through a CMHC, an FQHC, or an RHC, as a
distinct and organized intensive ambulatory treatment service, oering less than 24-hour daily care, in
a location other than an individual’s home or inpatient or residential setting.
IOP services may also be provided in OTPs for treating an OUD.
Physicians prescribe IOP for an individual determined (not less frequently than once every other
month) to need these services for a minimum of 9 hours per week. They’re provided under the
physician’s supervision pursuant to an individualized, written treatment plan established and
periodically reviewed by the physician (in consultation with appropriate sta participating in such
program). This determines the physician’s diagnosis, the type, amount, frequency, and duration of
the items and services provided under the plan and the treatment goals.
Intensive outpatient services include:
● Individual and group therapy with physicians or psychologists (or other mental health professionals
to the extent authorized under state law)
●
Occupational therapy requiring the skills of a qualied occupational therapist
●
Services of social workers, trained psychiatric nurses, and other sta trained to work with
psychiatric patients
● Drugs and biologicals provided for therapeutic purposes (which can’t be self-administered)
● Individualized activity therapies that aren’t primarily recreational or diversionary
● Family counseling (the primary purpose of which is treatment of the individual’s condition)
● Patient training and education (to the extent that training and educational activities are closely and
clearly related to individual’s care and treatment)
● Diagnostic services
● Other items and services (excluding meals and transportation) that are reasonable and necessary for
the diagnosis or active treatment of the individual’s condition, can be reasonably expected to improve
or maintain the individual’s condition and functional level, and to prevent relapse or hospitalization
Intensive outpatient services must include a physician certication and POC. However, although PHP
requires the physician to certify that the services are instead of inpatient hospitalization, IOP services
aren’t intended for those who otherwise need an inpatient level of care.
In addition to physicians, the following NPPs may perform the required certication and POC
requirements for IOP services furnished in the OTP setting: NPs, PAs, CPs, CSWs, MHCs, MFTs, and
any other NPPs dened in Section 1842(b)(18)(C) of the Social Security Act, as permitted by state
law and consistent with scope of practice requirements.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 33 of 43
Community Mental Health Centers
We cover Part B partial hospitalization services that community mental health centers (CMHCs) provide,
subject to the OPPS. Medicare-authorized CMHCs must meet these program and patient criteria:
●
Have appropriate state and local CMHC licensing or certication
●
Provide:
●
Outpatient services, including specialized services for children, older adults, chronically
mentally ill patients, and residents of its service area discharged from an inpatient mental
health treatment facility
●
24-hour emergency care services with clinician access and appropriate disposition with
follow-up documentation of the emergency in the patient’s CMHC medical record
●
Day treatment, partial hospitalization services, or psychosocial rehabilitation services with
structured daily treatment plans varying in intensity, frequency, and duration based on the
patient’s needs
●
At least 40% of its services is to patients who are ineligible for Social Security Act, Title XVIII benets
●
Clinically evaluated state mental health facility candidate admissions by clinical personnel and
authorized under state law, except those provided by a 24-hour facility; a CMHC operating in
a state that, by law, prevents it from providing these services may contract with an entity the
HHS Secretary approves
A CMHC is an originating telehealth services site.
Behavioral Health Integration Services
Integrating behavioral health and primary care helps improve patient mental and behavioral health
condition outcomes. We separately pay physicians and NPPs providing behavioral health integration
(BHI) services over a calendar month.
CPs, CSWs, MFTs, and MHCs can bill the general BHI code HCPCS G0323 when they’re personally
performing services to account for monthly care integration, and those services are the focal point of
care integration. We allow general supervision for G0323.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 34 of 43
Medical Records Checklist: Outpatient Psychiatric Services
This outpatient psychiatric medical records services checklist reminds clinicians and sta of
required documentation.
Community Mental Health Center & Partial Hospitalization Program
Medical Record Content
□
Patient identication data
□
Diagnosis, including intercurrent disease diagnosis and psychiatric diagnosis
□
Indicate signicant illnesses and medical conditions on a problem list
□
Prominently note medication allergies and adverse reactions in the record; note in the record
if the patient has no known allergies or adverse history of reactions
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 35 of 43
Standard Initial Evaluation
□
Complete within 24 hours of patient admission
□
Include admitting diagnosis and other diagnoses
□
Referral source
□
Admission reason as stated by the patient or other person signicantly involved
□
Identify the patient’s immediate clinical care needs for their psychiatric diagnosis
□
Current patient prescriptions list, including over-the-counter medications and other substances
they take
□
For PHPs only, an explanation of the patient’s hospitalization risk if a PHP isn’t provided
□
Identify the patient’s appropriate interdisciplinary team members
Standard Comprehensive Assessment
□
Interdisciplinary treatment team completed a timely assessment consistent with the patient’s
needs, but no later than 4 working days after the patient’s admission
□
Identies the patient’s psychiatric illness and ensures the physical, psychological, psychosocial,
emotional, and therapeutic active treatment plan needs are consistent with your ndings
□
Includes the patient’s:
□
Admission reason
□
Psychiatric evaluation containing medical history and symptoms severity
□
Previous and current mental health status information
□
Onset of illness symptoms and admission circumstances
□
Description of attitudes and behaviors aecting their treatment plan
□
Intellectual, memory functioning, and orientation assessment
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 36 of 43
Standard Comprehensive Assessment (cont.)
□
Care planning risk factor complications
□
Functional status, including whether they can participate in their own care and their
strengths and goals
□
Factors aecting their or others’ safety, including suicide risk factors
□
Prescription drug prole, including over-the-counter medications
□
Referral needs and further health care professional evaluation
□
Considered discharge planning factors
□
Current social and health care support systems
□
For pediatric clients, assess social service needs and make needed referrals
□
Make interdisciplinary team updates when the patient’s status or treatment response changes
occur or when they meet goals
□
Upon patient discharge or transfer to another entity, within 2 working days the CMHC must
forward the patient’s:
□
Discharge summary
□
Clinic record, if requested
□
If the patient refuses CMHC services or is non-compliant with the treatment plan, the CMHC
must forward to their primary health care provider:
□
CMHC discharge summary copy
□
Client record, if requested
□
Discharge summary includes the patient’s:
□
Current active treatment plan
□
Most recent physician orders
□
Documentation to help in post-discharge continuity of care
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 37 of 43
Acute Care Hospital
When a physician admits a patient to the hospital for inpatient psychiatric facility services, we
cover the services only if the patient needs intensive, appropriate, and active treatment in this type
of setting. The psychiatric facility must be a general hospital with a distinct psychiatric unit or a
psychiatric hospital that cares only for people with mental health conditions.
We certify inpatient psychiatric facilities (IPFs) and distinct psychiatric units in acute care hospitals
and critical access hospitals (CAHs).
We cover:
●
Semi-private rooms
●
Meals
●
General nursing
●
Drugs (including methadone to treat OUD)
●
Other inpatient hospital treatment services and supplies
Deductible and coinsurance apply. See the Coverage Period section for more information.
If appropriate, physicians can admit patients to a general acute care hospital that doesn’t have a
distinct psychiatric unit to get mental health and SUD services. These inpatient services are covered
like other inpatient services in a general acute care hospital.
Inpatient Psychiatric Facility Services
IPFs include freestanding, certied psychiatric hospitals, and psychiatric units in acute care hospitals or
CAHs, providing routine hospital and psychiatric services to diagnose and treat patients’ mental disorders.
We pay for inpatient psychiatric services under the Inpatient Psychiatric Facility Prospective Payment
System (IPF PPS) when the facility is certied and meets inpatient psychiatric hospital services regulations.
We require updated hospital inpatient rights and discharge planning conditions of participation for
short-term acute-care, rehabilitation, psychiatric, children’s, cancer, and CAHs.
42 CFR 482.43 outlines current discharge planning conditions of participation requirements.
Medical Records Requirements
IPF medical records must show the physician or NPP treatment level and intensity for each patient
they admit to the hospital, among other requirements detailed at 42 CFR 482.61.
Patients must be able to access their medical records when requested verbally or in writing, and the
hospital must quickly meet the patient’s request, detailed at 42 CFR 482.13.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 38 of 43
Medical Records Checklist: Inpatient Psychiatric Services
This inpatient psychiatric services medical records checklist reminds clinicians and sta of
required documentation.
Medical Record Content
□
Patient identication data, including inpatient legal status
□
Incoming patient history ndings and treatment plan
□
Patient provisional or admitting diagnosis, including intercurrent disease diagnosis and
psychiatric diagnosis
□
Sta or others signicantly involved clearly document inpatient admission reasons
□
Social service records must include:
□
Inpatient, family members, and others’ interviews
□
Home plans assessment
□
Family attitudes
□
Community resources
□
Contacts
□
Social history
□
If indicated, a completed and recorded neurological exam during the admission physical
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 39 of 43
Psychiatric Evaluation
□
Completed within 60 hours of patient admission
□
Medical history
□
Mental status record
□
Admission illness onset and circumstances noted
□
Attitudes and behavior described
□
Estimated intellectual and memory functioning and orientation
□
Inpatient assets inventory, descriptive and not interpretive
Comprehensive Written Treatment Plan
□
Individual plan based on inpatient strengths and disabilities
□
Substantiated diagnosis
□
Short- and long-term goals
□
Specic treatment modalities used
□
Each treatment team member’s responsibilities
□
Adequate documentation justifying diagnosis, treatment, and completed rehabilitation activities
□
All active therapeutic inpatient treatment eorts documented
Recorded Progress
□
All physicians, psychologists, or other licensed independent practitioners record
patient progress
□
Others signicantly involved in active treatment modalities, when appropriate
□
Determine the patient’s progress note frequency by condition; less than weekly during the rst
2 months and at least once per month thereafter
□
Progress notes must include treatment plan revision recommendations, when necessary
□
Progress notes must include a precise patient treatment plan progress assessment
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 40 of 43
Discharge Plan
□
Discharge summary
□
Patient’s hospital stay recap
□
Recommended patient follow-up and aftercare
□
Patient discharge condition summary
*Discharge Planning Evaluation, Plan, and Summary
□
Does the hospital have a discharge planning process that applies to all hospital patients?
□
Early in the patient’s hospitalization, did you identify if they’re likely to suer adverse health
consequences if discharged without adequate discharge planning?
□
If yes, did you complete a discharge planning evaluation or was it requested by the
patient, their representative, or the physician?
□
Did an RN, a social worker, or another appropriately qualied sta member develop or
supervise the plan?
□
Did the evaluation include the patient’s post-hospital services need and their self-care capacity
or the possibility of returning to their pre-hospital environment?
□
Was the planning evaluation timely to allow appropriate post-hospital arrangements?
□
Does the patient’s medical record document the interaction of relaying discharge planning
evaluation results to them or their representative?
*Identies the newest discharge planning conditions of participation.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 41 of 43
*Standard Discharge Plan
□
Did an RN, a social worker, or another appropriately qualied sta member develop or
supervise discharge plan development if indicated in the evaluation?
□
If the evaluation showed no discharge plan nding, did the patient’s physician request it?
□
Did the hospital re-assess the patient’s discharge plan if factors aecting the patient’s
continuing care needs develop?
□
Did the hospital arrange to implement the patient’s discharge plan?
□
Did the patient, family, and interested persons get counseling to prepare them for
post-hospital care?
□
Did the hospital include a Medicare home health agencies (HHAs) discharge plan list (HHAs
must request that hospital list when available) and skilled nursing facilities (SNFs) serving
that geographic area where the patient lives or, in the SNF’s case, in the requested
geographic area?
□
Did you present that list to the patient only if they needed home health or post-hospital
extended care services indicated in the discharge planning evaluation?
□
If the patient was enrolled in a managed care organization, did the hospital indicate those
contracted managed care organization services?
□
Did you document in the medical record that you presented the HHA list to the patient?
□
Did the hospital inform the patient and family of their freedom to choose among participating
providers’ post-hospital care services and respect the patient’s and family’s preference (the
hospital must not specify or limit available, qualied providers)?
□
Did the hospital disclose any HHA or SNF nancial interest it may have with them?
*Transfer or Referral
□
If you transferred or referred a patient, did you provide follow-up or ancillary care medical
information to appropriate facilities, agencies, or outpatient services?
*Identies the newest discharge planning conditions of participation.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 42 of 43
Coverage Period
We cover IPF patient services in specialty facilities for 90 days per illness with a 60-day lifetime
reserve and 190 days of care in freestanding psychiatric hospitals (this 190-day limit doesn’t apply
to certied psychiatric units). The patient gets no further benets after using 190 days of psychiatric
hospital care.
Under the IPF PPS, federal per diem rates include inpatient operating and capital-related costs
(including routine and ancillary services). We determine them by:
●
Geographic factors
●
Patient characteristics
●
Facility characteristics
IPFs get additional payments for:
●
Patients treated in IPFs with a qualifying emergency department
●
The number of ECT treatments provided
●
Outlier cases (cases with extraordinarily high costs)
The Medicare Benet Policy Manual, Chapter 2 has more information on how Medicare covers IPFs.
Same Day Billing Guidelines
Integrating mental health and SUD services addresses all patients’ needs whether they get care in a
traditional primary care setting or a specialty mental or SUD health care setting. Services include:
●
Mental health care services (we include substance use treatment)
●
Alcohol and substance use (other than tobacco) structured assessment and intervention services
(SBIRT services) billed under HCPCS codes:
●
G2011: Alcohol and/or substance (other than tobacco)
misuse structured assessment (e.g., audit, dast), and
brief intervention, 5-14 minutes
●
G0396: Alcohol and/or substance (other than tobacco)
misuse structured assessment (e.g., audit, dast), and
brief intervention 15 to 30 minutes
●
G0397: Alcohol and/or substance (other than tobacco) misuse structured assessment (e.g.,
audit, dast), and intervention, greater than 30 minutes
AUDIT: Alcohol Use Disorders
Identication Test
DAST: Drug Abuse Screen Test
●
Primary health care services
Part B pays for reasonable and necessary integrated health care services provided on the same day,
to the same patient, by the same or dierent professionals in the same or dierent locations.
MLN BookletMedicare & Mental Health Coverage
MLN1986542 January 2024Page 43 of 43
The Eligible Professionals section lists eligible Part B providers that may provide diagnostic and
therapeutic mental, psychoneurotic, personality disorder, and SBIRT treatment services allowed
under state law.
We cover medically reasonable and necessary services or supplies to treat the patient’s overall
diagnosis and condition or improve a malformed body part. Services must meet standards of good
medical diagnosis, direct care, and patient medical treatment condition practice, and must not be
mainly for patient, provider, or supplier convenience.
Services must also meet specic National Coverage Determination (NCD) and Local Coverage
Determination (LCD) medical necessity criteria.
Every service billed must indicate the specic sign, symptom, or patient complaint requiring the
service. Although a provider may consider a service or test good medical practice, we don’t pay for
services without patient symptoms, complaints, or specic documentation.
We also pay for multiple mental health services for the same patient on the same day. However, we
don’t pay for inappropriate or duplicate services on the same day. If you have questions about local or
national policies that may prevent you from billing certain services, nd your MAC’s website.
Resources
●
CMS Behavioral Health Strategy
●
CMS Blog: Important New Changes to Improve Access to Behavioral Health in Medicare
●
CMS Opioid Treatment Programs
●
Marriage and Family Therapist & Mental Health Counselors
●
Medicare Benet Policy Manual, Chapters 2, 6, and 15
●
Medicare Claims Processing Manual, Chapters 3 and 4
●
MLN Matters®: Provider Enrollment Changes to the Medicare Program Integrity Manual
(MM13331)
●
Notices and Forms
●
Quality Improvement Organizations
●
SAMHSA: What is Mental Health?
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure.
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department
of Health & Human Services (HHS).
