
2019-2020
ACADEMIC
YEAR
HR Policies
and Procedures
Kaiser Foundation Hospitals
Residency & Fellowship Training Programs
Issued by the Institutional Graduate Medical Education Office
Physician Education and Development
1800 Harrison Street, 21
st
Floor
Oakland, CA 94612
Contact: Michele.R.Ben[email protected]
- ii -
TABLE OF CONTENTS
MISSION STATEMENT ........................................................................................................................ 1
RESIDENT ELIGIBILITY AND SELECTION ......................................................................................... 1
A. Appointment ................................................................................................................................. 1
B. Conditions of Reappointment ...................................................................................................... 1
C. Notice ............................................................................................................................................ 1
D. Salary Schedule and Job Codes .................................................................................................. 2
E. Resignation .................................................................................................................................. 2
HUMAN RESOURCES POLICIES........................................................................................................ 2
A. Scheduling and Duty Hours ......................................................................................................... 2
B. Supplemental Employment (Moonlighting) ................................................................................. 2
C. Holidays ........................................................................................................................................ 2
D. Vacation ........................................................................................................................................ 3
E. Educational Leave ........................................................................................................................ 3
F. Sick Leave .................................................................................................................................... 3
1. Occupational Injuries and Illness .......................................................................................... 3
2. Needlestick or Bodily Fluid Exposure ................................................................................... 3
G. Long Term Disability (LTD) Insurance......................................................................................... 4
H. Other Time Off .............................................................................................................................. 5
1. Family and Medical Leave ...................................................................................................... 5
2. Pregnancy Disability Leave ................................................................................................... 5
3. Leave under California Family Rights Act (CFRA) ............................................................... 6
4. Military Leave ......................................................................................................................... 6
5. Bereavement ......................................................................................................................... 6
6. Personal Leave....................................................................................................................... 6
7. Reinstatement and Consequences of Leave ........................................................................ 7
I. Freedom from Harassment Policy ............................................................................................... 7
J. Equal Employment Opportunity (EEO) Policy ............................................................................ 7
K. Accommodation for Disabilities……………………………………………………… ......................... 7
APPOINTMENT OF THE TEACHING STAFF ...................................................................................... 7
PROFESSIONAL DEVELOPMENT ...................................................................................................... 7
SUPERVISION OF RESIDENTS .......................................................................................................... 8
PERSONNEL RECORDS ..................................................................................................................... 8
A. Evaluations ................................................................................................................................... 8
1. Evaluation of Residents ......................................................................................................... 8
2. Evaluation of Program ........................................................................................................... 9
B. Corrective Action ......................................................................................................................... 9
C. Requirements ............................................................................................................................... 9
1. Licensure ................................................................................................................................ 9
2. Health Screenings .................................................................................................................. 9
3. Universal Precautions.......................................................................................................... 10
4. Cardio-Pulmonary Resuscitation (CPR) Certificate ............................................................ 10
BENEFITS AND SERVICES .............................................................................................................. 10
A. Health Insurance ........................................................................................................................ 10
B. Preferred Provider Option (PPO) Plan ....................................................................................... 10
- iii -
C. Dental Plan ................................................................................................................................. 10
D. Life Insurance, Accidental Death & Dismemberment, Survivor Assistance ............................ 10
E. Professional Liability Insurance ................................................................................................ 11
F. Retirement Programs ................................................................................................................. 11
G. Tax Sheltered Annuity Plan ....................................................................................................... 11
H. Unemployment Insurance .......................................................................................................... 11
I. Physician Assistance Program.................................................................................................. 12
J. Parent Medical Coverage ........................................................................................................... 12
K. License Fees............................................................................................................................... 12
L. Other Benefits ............................................................................................................................ 12
1. Meals .................................................................................................................................... 12
2. Sleep Rooms ........................................................................................................................ 12
3. Support Services.................................................................................................................. 12
4. Lab Coats and Scrubs ......................................................................................................... 12
5. Identification Badge ............................................................................................................. 13
6. Health Sciences Library ....................................................................................................... 13
7. Parking ................................................................................................................................. 13
8. Child and Elder Care Referral .............................................................................................. 13
9. Commuter Choice Program ................................................................................................. 13
10. Dependent Care Plan ........................................................................................................... 13
11. Alliant Credit Union .............................................................................................................. 13
12. Kaiser Permanente Activity Program .................................................................................. 13
13. Educational Stipend.………………………………………………………………. ....................... 13
14. Fitness Membership…………………………………………………………………………………..13
15. Housing Allowance……………………………………………………………………………………13
PROFESSIONAL CONCERNS: MEDICAL/LEGAL SERVICES ........................................................ 14
A. Witnessing Legal Documents .................................................................................................... 14
B. Medical Treatment and Authorization and Patient Consents ................................................... 14
C. Responding to Legal Documents .............................................................................................. 14
D. Contact with Attorneys/Other Individuals ................................................................................. 14
E. Patient Rights and Responsibilities .......................................................................................... 15
F. No Code Status .......................................................................................................................... 15
G. Durable Power of Attorney for Health Care ............................................................................... 15
H. Unusual Incident or Occurrence Reports.................................................................................. 15
MEDICAL RECORDS ........................................................................................................................ 15
A. Admission History and Physical Examination .......................................................................... 16
B. Progress Notes ........................................................................................................................... 16
C. Operation Report ........................................................................................................................ 16
D. Discharge Summary ................................................................................................................... 16
E. Death Summary .......................................................................................................................... 17
F. Completion of Medical Records ................................................................................................ 17
ENVIRONMENTAL, HEALTH, AND SAFETY POLICIES ................................................................... 17
A. Smoking Policy .......................................................................................................................... 17
B. Electrical Safety ......................................................................................................................... 17
C. Fire and Disaster Drills .............................................................................................................. 18
D. Blood-borne and Air-borne Pathogens ..................................................................................... 18
E. Physician Impairment ................................................................................................................ 18
F. Security....................................................................................................................................... 18
G. Violence in the Workplace ......................................................................................................... 18
RESIDENT REPRESENTATION ON MEDICAL CENTER COMMITTEES .......................................... 19
PHARMACEUTICAL COMPANIES AND REPRESENTATIVES......................................................... 19
FINAL CLEARANCE.......................................................................................................................... 19
RESIDENCY CLOSURE OR REDUCTION IN SIZE ........................................................................... 19
- iv -
APPENDICES
APPENDIX A: Resident Academic and Professional Appeal Processes
APPENDIX B: Current Monthly Salary Schedule and Job Codes
APPENDIX C: Resident Conflict of Interest Policy
APPENDIX D: Disaster Response Policy
APPENDIX E: Pre-Employment Drug Testing Policy
APPENDIX F: Resident Council
APPENDIX G: RAS Policy for Residents
APPENDIX H: Resident Transfer Policy
APPENDIX I: United States Medical Licensing Exam (USMLE) Step 3
APPENDIX J: ACGME Duty Hour Requirements
APPENDIX K: Supervision of Residents
APPENDIX L: Funding for Board Preparation Courses
- 1 -
Kaiser Permanente
Northern California Region Residency Training Programs
RESIDENT POLICY AND PROCEDURE MANUAL
MISSION
Kaiser Permanente (KP), a leader in the delivery of quality medical care, has been committed to graduate
medical education (GME) for over 60 years. Our goal is to provide organized educational programs in a
scholarly and supportive integrated managed care environment, facilitating the ethical, professional and
personal development of the resident while ensuring safe and appropriate care for patients.
RESIDENT ELIGIBILITY AND SELECTION
Applicants must fulfill either the Accreditation Council for Graduate Medical Education (ACGME)
qualifications for appointment to ACGME-accredited programs or the Council for Podiatric Medical
Education (CPME) qualifications for appointment to CPME-accredited programs. All our ACGME-
approved residency programs participate in the National Residency Matching Program (NRMP).
Selection to residency is on the basis of preparedness, ability, aptitude, academic credentials,
communication skills, and personal qualities such as motivation and integrity. Selection practices are not
unlawfully influenced or affected by a person's race, religion, color, national origin, ancestry, physical or
mental disability, veteran's status, medical condition, marital status, age, sex, sexual orientation or gender
identity. Additionally, Kaiser Permanente provides a work environment free of harassment and will not
tolerate any kind of illegal harassment, including sexual harassment, of employees or applicants. This
policy governs all employment, including hiring, compensation and benefits, assignment, promotion,
discharge, and all other terms and conditions of employment.
A. Appointment
Appointment to resident positions is initiated by the Program Director and, following final approval by the
Director of Graduate Medical Education, a formal contract is offered. The term of the contract is one year,
unless terminated earlier in accord with the Hospital's established policies, as described herein.
B. Conditions for Reappointment
Reappointment to any subsequent year is subject to annual review and is based on satisfactory
performance, including demonstrated ability to perform at the expected level in the subsequent year. As
circumstances reasonably allow, in the case of non-renewal of appointment or non-promotion, every effort
will be made to give four months written notice.
C. Notice
Written notice of appointment/reappointment shall be provided to each resident and shall include the
terms and conditions of appointment, salary, level of appointment, and applicable requirements, such as
licensure.
Notification of non-renewal of contract shall be made in writing, promptly after the decision has been
made, and no later than four months prior to the end of the contract. However, if the primary reason for
non-renewal occurs less than four months before expiration of the contract, notice shall be given as soon
as circumstances will reasonably allow. Notification will also include the resident's right to implement the
academic and professional appeals process.
Each resident is entitled to the benefits of the academic and professional appeals process upon receipt of
notice that his or her participation in a training program is to be terminated, suspended or significantly
reduced in scope of professional activity. (Please refer to Resident Academic and Professional Appeal
Processes, Appendix A. This is also available in the GME office.)
- 2 -
D. Salary Schedule and Job Codes
See Appendix B for the current salary schedule and job codes. This is also available in the GME office.
Payroll checks are issued every other Friday. Arrangements may be made for direct deposit to a checking
or savings account.
E. Resignation
Residents who voluntarily separate from the residency program are considered to have resigned. A
resident must give written notice to the Program Director at least 30 calendar days prior to resignation.
Notice to the Program Director is also required at least three months before the end of the training year, if
the resident has been offered reappointment but does not intend to accept the reappointment. Please
also review Resident Transfer Policy, Appendix H.
HUMAN RESOURCES POLICIES
A. Scheduling and Work Hours
Work hours are defined as all clinical and academic activities related to the residency program, i.e.,
patient care (both inpatient and outpatient), administrative duties related to patient care, the provision for
transfer of patient care, time spent in-house during call activities and scheduled academic activities such
as conferences. Work hours do not include reading and preparation time. Resident work schedules are
organized so as to promote an educational environment and facilitate safe patient care while supporting
the physical and emotional well being of the resident. Residents must complete their full assigned shift
and may not leave early, unless it is excused by their supervisor or to abide by the ACGME work hour
requirements. In-house call and rotations will be equitably distributed among residents.
Each program shall schedule work time and provide adequate off work hours. These schedules will be
posted. The schedule must be in compliance with the ACGME Common Program Requirements for all
Core and Subspecialty Programs and with specialty specific Residency Review Committee (RRC)
requirements, as appropriate. No exceptions to these rules are allowed. See Appendix J.
B. Supplemental Employment (Moonlighting)
Supplemental employment outside the residency (moonlighting) may be undertaken only by residents
who hold a Postgraduate Training License (PTL). The holder of a PTL may engage in the practice of
medicine only in connection with his or her duties as an intern or resident in an ACGME accredited
postgraduate training program in California, with written authorization from the program director of his or
her program. The approval must be in writing and maintained in the trainee’s file.
The hours involved should not be so excessive as to interfere with the educational purpose of the
residency program and must be in compliance with the Work Hour Rules (noted above) and the residency
program schedule requirements. The resident's performance will be monitored by the Program Director,
and permission to moonlight may be withdrawn if it adversely affects performance. Residents, however,
are not required to engage in "moonlighting" as a part of their residency program.
All residents engaged in moonlighting must be licensed for unsupervised medical practice in the state
involved and must comply with the appropriate credentialing and liability coverage requirements of the
institution involved. Information regarding credentialing requirements at Kaiser Permanente may be
obtained from the Director of Graduate Medical Education or the Medical Staff office at each facility.
C. Holidays
Holidays that are observed are: New Year's Day, President's Day, Memorial Day, Independence Day,
Labor Day, Thanksgiving, and Christmas Day. Holiday call will be equitably distributed by the Program
Director.
D. Vacation

- 3 -
Vacation is earned each month. A request for time off must be submitted in advance of the scheduling of
any vacation and must be approved by the Program Director. Medical records must be completed before
the resident begins vacation.
Your vacation is time you may use for vacation, leisure or personal reasons. Vacation details by specialty
may be found at residency-ncal.kp.org
.
E. Educational Leave
Educational Leave is provided to assist you in the maintenance of your professional license(s) and/or to
upgrade and maintain professional skills. Educational leave may be granted by the Program Director at
the rate of five workdays per year. Unused days may not carry over from one academic year to the next.
F. Sick Leave
Sick Leave is time you may use when you are ill or injured. Residents are allowed 13 days of sick leave
each anniversary year. Sick leave hours do not accumulate from year to year; instead a resident begins
each anniversary year with a new block of sick leave. Sick leave balances are not paid off when a
resident completes training as a resident.
Residents may use sick leave only if they are unable to work or absent for diagnosis or treatment due to
an illness, injury or medical condition. Residents may also use available sick leave to attend to an ill
child, parent or spouse/domestic partner and the domestic partner’s child(ren), as defined by California
law (AB 109). The total amount of sick leave available to a resident in any calendar year to care for an ill
child, parent or spouse/domestic partner and the domestic partner’s child(ren) shall not exceed one-half
of the block of sick leave provided to the resident at the beginning of the anniversary year in which the
illness begins (6.5 days).
A resident should immediately notify the Program Director, Chief Resident, and Graduate Medical
Education office of illness requiring sick leave. Medical certification is required to support a request for
leave because of a serious health condition or for an illness lasting for three or more days. In the event of
excessive sick leave usage, the Program Director may inform the resident in writing that medical
documentation is required for all sick leave.
In the case of extended illness or injury, residents may qualify for State Disability benefits or Workers'
Compensation benefits.
1. Occupational Injuries and Illness
In order to receive Workers’ Compensation benefits, it is necessary that job-related
injuries/illnesses sustained by the resident be examined and treated by the attending
physician at the Employee Health Center or by another physician. The "Doctor's First
Report" must be completed so that the visit may be identified as a reported work-related
injury. Following treatment, an "Employee's Report of Industrial Injury" must be submitted by
the resident to the Graduate Medical Education office within 24 hours. These forms may be
obtained on any nursing unit or in the Emergency Department. Before the resident returns to
duty, he/she must notify both the Program Director and the Graduate Medical Education
Director that he/she is prepared to return to duty and has complied with the fitness-for-duty
medical certification requirements, as necessary.
2. Needlestick or Bodily Fluid Exposure
Needlestick information is available 24 hours per day. The internal telephone extension
varies by facility.
a. Resident should seek medical care as soon as possible after the exposure. From
Monday to Friday, 8:00 am - 5:00 pm, the resident should seek care at the Employee
Health Center (EHC). If the EHC is not open, he/she may be seen in the General
Medical Clinic or, if necessary, in the Emergency Department. If known, the name and
medical record number of the source patient must be reported.
- 4 -
b. Resident should report the incident to the Graduate Medical Education office as soon as
possible, and complete an "Employee Injury Report."
c. Follow-up in the EHC will be necessary in almost every case for completion of Hepatitis B
and HIV protocols.
G. Long Term Disability (LTD) Insurance
A resident must be employed in a regular status to be eligible for Long Term Disability (LTD) coverage.
His/her LTD coverage becomes effective upon date of hire as a resident. The resident will not become
insured unless on the day he/she would otherwise become insured, he/she is actively employed in a
regular status and is physically able to perform all the regular duties of employment. This LTD benefit is
offered through the Metropolitan Life Insurance Company (ML). At the present time, the resident’s
employer pays the entire cost of LTD coverage.
A resident must complete a qualifying period of six months of total disability before he/she is entitled to
LTD benefit payments. During this qualifying period, the resident may use any unused sick leave days to
which he/she is entitled, but once these days are exhausted, he/she will be changed to an unpaid leave
status. In addition, the resident’s LTD claim must be received within 12 months of the date of disability.
Benefits continue until the resident recovers from the disability, or if earlier, to the end of the month
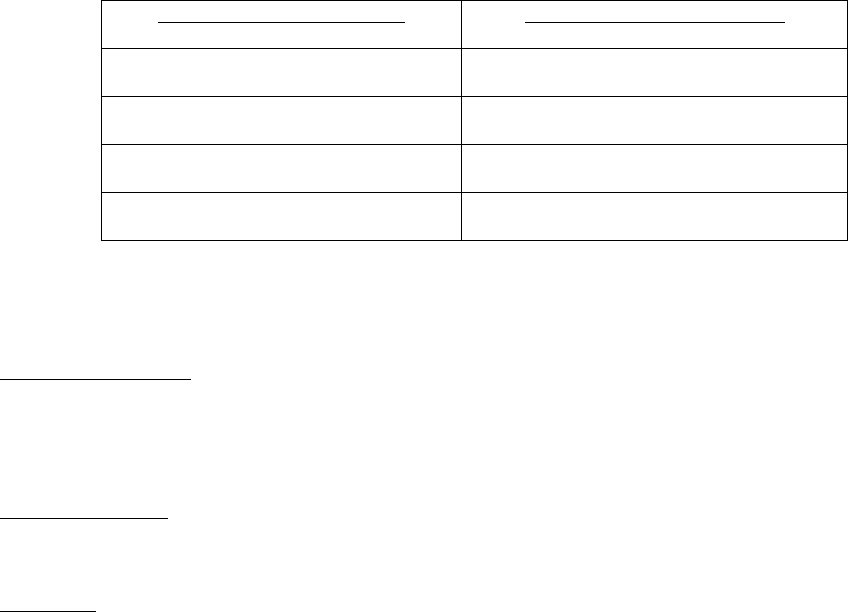
specified under the following limits:
Age When Disability Occurs
Duration of Benefit Payments
Under 61
To age 65
61 through 65
3.5 years
66 through 68
1.5 years
69 and over
0.5 years
ML has the right to require a physical examination as often as deemed necessary while the resident
claims LTD benefits under this policy.
Definition of Disability – A resident is considered totally disabled if, during the first 24 months of his/her
disability, he/she is continuously unable to perform any and every duty pertaining to his/her occupation.
After the resident’s disability continues for 24 months, he/she is considered totally disabled if he/she is
continuously unable to engage in any and every occupation for compensation or profit for which he/she is
reasonably qualified by education, training or experience.
Pre-existing Illness - There is a pre-existing clause under LTD that excludes disability coverage during the
first 12 months of coverage for a disability resulting from a condition that is treated within three months
prior to coverage becoming effective.
Exclusions - Benefits are not payable for disability caused by intentionally self-inflicted injuries,
participation in or as a result of having participated in the commission of a felony, war or any act of war,
declared or not.
This coverage provides the resident with a monthly benefit which is determined according to his/her
monthly base salary in effect at the end of the six-month qualifying period and the amount of any disability
income received from other sources, as follows:
• If the LTD benefit is the resident’s only source of disability income, he/she will receive 50% of
his/her monthly salary.
• If the resident is eligible for disability benefits from other sources (such as State Disability, Social
Security Disability Award, individual or family, or Workers' Compensation), his/her LTD benefit will

- 5 -
equal 60% of his/her monthly salary minus the amount of other disability income. (It is assumed
that disabled residents will continue to receive Social Security benefits indefinitely unless they
return to work.) Any benefits a resident receives from private, individual policies will not reduce
this amount.
• If a resident returns to work under a rehabilitation program, his/her LTD benefit will equal 70% of
his/her monthly salary minus the amount of wages received and any other disability income.
In no circumstances will ML pay more than 50% of the resident’s monthly salary.
Medical and dental care benefits continue for a period equal to half his/her length of service up to a
maximum of five years. If a resident’s death occurs or he/she becomes ineligible for LTD benefits before
the end of the continuation period outlined above, benefits will cease.
A resident may apply to have his/her life insurance premiums waived while on LTD. If approved, his/her
basic life insurance (gift or contributory) will remain in effect for the duration of the resident’s LTD eligibility
period.
Long Term Disability coverage ends on the date a resident’s employment ends or he/she reclassifies to
an ineligible status. The resident cannot convert this coverage.
If there are additional questions regarding LTD, the facility’s Graduate Medical Education Department
may be contacted.
H. Other Time Off
1. Family and Medical Leave
Residents who meet the eligibility requirements of having completed one year of service and
worked at least 1250 hours during the immediately preceding 12-month period, may be entitled to
up to 12 weeks of leave within a 12-month period for the birth or adoption of a child, the
placement of a foster child, the care of a sick family member, or the resident's own serious health
condition; and to restoration of his or her former position or an equivalent one, in accord with the
federal Family and Medical Leave Act (FMLA) of 1993. (See Fact Sheet No. 028 on the
Department of Labor Web site: dol.gov/whd/fmla
.)
The resident must provide the Program Director at least 30 days' advance notice when leave is
foreseeable, and must provide notice within a reasonable time when the request for leave is not
foreseeable.
Medical certification is required when leave is requested to care for a family member with a
serious health condition or one’s own serious health condition. The resident’s medical and dental
coverage will continue during this 12-week period regardless of whether he/she is in a paid or
unpaid status.
At any time the resident is on leave for a reason other than his/her own illness or disability, it is
mandatory that any vacation time available be used except to the extent the resident is entitled to
use sick leave to attend to an ill child, parent or spouse/domestic partner as set forth above.
Questions regarding FMLA entitlement should be directed to the Graduate Medical Education
office.
2. Pregnancy Disability Leave
Under California Pregnancy Disability Leave Regulations (PDL), a resident may take up to four
months leave for a disability due to pregnancy and related medical conditions. The first 12 weeks
of disability are concurrently covered by FMLA. Any available sick leave will be paid during this
leave period and will automatically be integrated with State Disability Insurance (SDI). Accrued
vacation time may also be used. All paid time taken by the resident because of a pregnancy
- 6 -
related disability will be counted against the four-month California Pregnancy Disability Leave
(PDL) as well as the 12-week entitlement under FMLA.
If the leave is due to pregnancy, it is the responsibility of the resident to notify the Program
Director and Chief Resident as early as possible in her pregnancy so that, if necessary,
schedules can be rearranged to lessen the impact on the training program and to ensure that the
educational training of the resident can continue in an orderly fashion.
A written statement regarding the arrangements made must be placed in the resident’s file in the
Graduate Medical Education office. The National HR Policy on Family and Medical Leave can be
found on the MyHR website: epf.kp.org/wps/portal/hr or the National KP Policy Library website:
http://kpnational.policytech.com.
3. Leave under California Family Rights Act (CFRA)
An eligible resident is also entitled to up to 12 additional weeks leave to bond with her newborn
under the California Family Rights Act (CFRA). This leave may not be taken concurrently with
PDL or FMLA for pregnancy disability and begins at the point the resident is released to return to
work by her physician (i.e., SDI benefits cease). At the point the resident begins CFRA leave to
bond with the newborn, any remaining FMLA will now run concurrently with CFRA. For example,
a resident goes out on maternity leave two weeks prior to her due date. FMLA and PDL begin
immediately, even if the resident remains in a paid status due to sick leave and vacation pay.
Generally, SDI allows a woman a six-week period of recuperation after the birth of the child for a
vaginal delivery. In this example, FMLA and PDL would be in effect for eight weeks. At this
point, FMLA and CFRA run concurrently for the remaining four weeks of FMLA. However, the
reason for the leave has changed from the resident’s disability to time to bond with the newborn.
PDL is no longer valid as the disability period has ended. The resident is entitled to an additional
eight weeks of CFRA to continue bonding with the child. Once the reason for the leave is to bond
with the newborn, accrued vacation time must be taken concurrently with FMLA and CFRA.
Questions regarding pregnancy disability and entitlement to family leave should be directed to the
Graduate Medical Education office.
4. Military Leave
Military leaves of absence are granted to eligible employees who are absent from employment in
order to perform duty on either a voluntary or involuntary basis in the United States’ Uniformed
Services. For more information, read the Military Leave Policy on the MyHR website:
epf.kp.org/wps/portal/hr or the National KP Policy Library: http://kpnational.policytech.com
5. Bereavement Leave
A resident may be eligible for up to three days of paid bereavement leave (or five days if it
involves over 300 miles of travel one way) in the event of the death of an immediate family
member. "Immediate family" is defined as the resident's spouse or domestic partner, children,
legal wards, and children of the employee's spouse or domestic partner, parents, step-parents,
legal guardians, and parents and step-parents of resident's spouse or domestic partner,
grandparents, brothers and sisters, grandchildren and grandchildren of resident's spouse or
domestic partner.
6. Personal Leave
Leaves of absence without pay for personal reasons may be granted at the discretion of the
Program Director.
7. Reinstatement and Consequences of Leave
Any resident who has been on a leave of absence for more than four weeks must obtain a
fitness-for-duty certification from a physician in the Employee Health Center or from another staff
physician before he/she can return to duty.
- 7 -
A resident may be required to make up time missed in order to meet the educational
objectives and certification requirements of the department or the specialty. This should be
discussed with the Chief Resident or Program Director, who must approve all proposals to make
up time. Funding for make-up time, particularly time extending beyond the period of appointment,
cannot be guaranteed.
I. Freedom from Harassment Policy
Kaiser Permanente is committed to maintaining a work environment free of discrimination. In keeping
with this commitment, Kaiser Permanente strongly disapproves, and will not tolerate, any kind of
harassment of employees, applicants for employment, or independent contractors by anyone, including
any manager, supervisor, physician, co-worker or non-employee.
Please read the Commitment to a Harassment-Free Workplace Policy for procedures addressing
sexual harassment complaints and issues. This policy is available on the MyHR website:
epf.kp.org/wps/portal/hr or the National KP Policy Library: http://kpnational.policytech.com
J. Equal Employment Opportunity (EEO) Policy
Employment by Kaiser Permanente is based on merit, qualifications, and competence. Employees and
applicants will not be discriminated against on the basis of race, religion, color, national origin, ancestry,
physical or mental disability, veteran status, medical condition, marital status, age, sex, sexual
orientation, or gender identify. The Equal Employment Opportunity Policy is available on the MyHR
website: epf.kp.org/wps/portal/hr or the National KP Policy Library: http://kpnational.policytech.com
. The
EEO Internal Complaint Procedure and Internal EEO Complaint Form for addressing EEO complaints and
issues are also accessible on the
MyHR website.
K. Accommodation for Disabilities
Kaiser Permanente provides job accommodations that are both reasonable and necessary to meet the
known functional limitations of employees with disabilities.
APPOINTMENT OF THE TEACHING FACULTY
Generally, teaching faculty are members of the professional staff of Kaiser Foundation Hospitals.
Teaching faculty may also be members of affiliated residency programs or other institutions. Teaching
faculty members are always licensed independent practitioners and supervise residents in the field in
which they hold clinical privileges.
Faculty members for residency programs are selected by the Program Director on the basis of clinical and
teaching skills, and an interest in teaching. Peers and residents evaluate faculty members.
All faculty members are reviewed annually by the Program Director and Department Chief for continued
participation in the teaching and supervision of residents.
PROFESSIONAL DEVELOPMENT
The resident is expected to develop a personal program of learning and professional growth with
guidance from the faculty. The resident will be given graded responsibility and will be evaluated on a
continuous basis by the faculty and at formal semi-annual or quarterly evaluations by the Program
Director. Each program, in accordance with its ACGME Residency Review Committee (RRC) or Council
for Podiatric Medical Education (CPME) Program Requirements, will define the specific knowledge, skills
and attitudes to be attained by residents at each PGY level. Evaluations will address the six ACGME
core competencies of patient care, medical knowledge, practice-based learning, interpersonal and
communication skills, professionalism, and systems-based practice.
The resident shall participate fully in programs and activities of the training institution. The resident shall
also adhere to established practices, procedures and policies of the institution.
- 8 -
SUPERVISION OF RESIDENTS
Residency training is based on graduated responsibility that culminates in a high level of individual
accountability achieved by graduation. Throughout training, residents become more competent to make
judgments of increasing complexity and perform procedures of increasing difficulty.
A supervisory relationship exists between residents and faculty, such that the beginning resident has
limited independence and progresses to assume ultimate responsibility for patient care. Each training
program must have a program specific policy addressing supervision that is consistent with ACGME or
CPME to ensure that the appropriate level of supervision is in place for all residents.
See APPENDIX K for additional policies on Supervision of Residents
PERSONNEL RECORDS
The Office of Graduate Medical Education shall establish and maintain personnel records pertaining to
residents. These files are secure and confidential. Records are stored after the resident leaves the
program.
The records include documentation of appointment, performance evaluations, corrective actions, and
correspondence pertaining to that resident. These letters and documents are reviewed by the Director of
Graduate Medical Education prior to filing.
The residents may inspect their personnel files in the presence of the Director of Graduate Medical
Education or a designated representative. However, records, such as letters of reference, may be
withheld if protected by legal privilege. The resident may request a correction or deletion of a record by
submitting a request to the Program Director who will notify the resident whether his/her request has been
granted or denied. If dissatisfied with the decision, the resident may submit a written appeal of the
Program Director's decision to the Director of Graduate Medical Education specifying the grounds for the
appeal and facts and evidence in support thereof. Following a review, the Director of Graduate Medical
Education will notify the resident of his/her decision. The resident may submit a written statement of
his/her disagreement for inclusion in the personnel file.
Personnel records and information therein shall be released upon the written authorization of the resident,
or as authorized or permitted by law. A Program Director may provide an oral evaluation of a resident to
a prospective employer based on personal knowledge.
A. Evaluations
1. Evaluation of Residents
The Program Director or his/her designee shall provide each resident with a formal written
evaluation at least twice a year. Evaluations will assess competency in the following areas: (1)
patient care; (2) medical knowledge; (3) practice-based learning; (4) interpersonal and
communication skills; (5) professionalism; and (6) systems-based practice. The evaluations will
be based on observations of some or all of the following: physicians supervising the resident,
peers, ancillary personnel, Health Plan members, and review of medical records and
procedure/surgery logs. Deficiencies will be described in detail and a course of remediation, if
appropriate, will be outlined in writing.
Each evaluation should be reviewed with the resident. The resident should sign the evaluation to
acknowledge its receipt. The resident may submit a written response or statement for attachment
to the evaluation.
The written evaluations become part of the resident's permanent record and are an important
basis for reappointment, certification and future reference letters.

- 9 -
2. Evaluation of Program
During some academic years, the Institutional GME office sends a confidential survey evaluating
the quality of residency training and compliance with Resident Duty Hours rules to all residents in
Kaiser Permanente-sponsored programs in Northern California. This is conducted to help our
residency programs offer the best education and learning climate possible. The Institutional Office
provides each facility Director of Graduate Medical Education a summary of the results and
comments.
B. Corrective Action
A resident is either in good standing, in remediation, suspended, or dismissed. Corrective action may be
necessary to address performance deficits, misconduct or failure to meet professional standards by a
resident. Corrective action is normally progressive. However, certain clear and serious actions of
misconduct, e.g., abandonment of patients, gross negligence in the performance of duties, willful
destruction, damage, or theft of the property of another, and other actions of a similar nature do not need
to be disciplined progressively and may be grounds for immediate dismissal.
Each resident is entitled to the benefits of the academic and professional appeals process upon receipt of
notice that his/her participation in a training program is to be terminated, suspended, or significantly
reduced in scope of professional activity.
Please see Appendix A for a detailed description of the academic and professional appeals process.
C. Requirements
1. Licensure
Effective January 1, 2020, SB 798 will change the current minimum requirements of postgraduate
training for U.S./Canadian graduates requiring twelve (12) months and international medical
school graduates requiring twenty-four (24) months to thirty-six months (36) of a Board-approved
program
A trainee must obtain a PTL within 180 days after enrollment in a Board-approved postgraduate
program and would be valid until 90 days after the trainee has completed the required thirty-six
(36) months of training.
A Postgraduate Training Authorization Letter (PTAL) will no longer be required for international
medical graduates.
Minimum requirements for postgraduate training in California will require successful completion of
thirty-six (36) months of a Board-approved program for all applicants, regardless of whether the
medical school attended was domestic or international.
After successful completion of thirty-six (36) months of training, the trainee will apply for a
Physician’s and Surgeon’s Certificate with the Board within 90 days to continue practicing
medicine in California.
2. Health Screenings
All residents are required to have the physical and mental ability to perform the essential duties of
the residency training program and meet hospital standards for immunity to rubella, mumps and
varicella zoster. Residents must also be screened for Hepatitis B status. Hepatitis B vaccine is
offered and residents with non-immune status are strongly advised to receive the vaccine series.
In addition, all residents are required annually to provide evidence of freedom from infection with
tuberculosis. (See Health Screenings Policy available on the MyHR website:
epf.kp.org/wps/portal/hr
.)
- 10 -
3. Universal Precautions
All residents are required to meet and practice hospital standards for universal precautions and
air and blood-borne pathogens.
4. Cardio-Pulmonary Resuscitation (CPR) Certification
Each training program, in accordance with the RRC and medical staff requirements, determines
the regulations for CPR certification.
BENEFITS AND SERVICES (Group Benefits are subject to change. Notification of change will be
provided in advance.)
A. Health Insurance
Health Insurance is provided to a resident, resident’s spouse/domestic partner, and unmarried dependent
children under 26 years of age. The resident may choose Kaiser Foundation Health Plan (KFHP) or
Preferred Provider Option (PPO) Plan administered by Harrington Benefit Services, Inc. (HBSI).
Effective April 1, 2018, if elected, Kaiser Foundation Health Plan (KFHP) coverage becomes effective the
first of the month following the date of hire. If the hire date is the first of the month, coverage becomes
effective that day. The plan covers the resident, spouse or domestic partner, and unmarried dependent
children under 26 years of age. KFHP is a comprehensive medical plan that provides covered services
directly at Kaiser Permanente medical facilities. Coverage includes basic and major medical care such as
hospitalization, surgery, maternity care, x-ray and laboratory expenses, durable medical equipment, as
well as emergency care. This plan also provides vision care, which includes eye examinations, frames, or
one pair of contact lenses, not to exceed a pre-determined amount, every 24 months. The Plan covers
prescriptions by a physician of The Permanente Medical Group (TPMG), mental health provider, or a
dentist. There is a pre-determined co-payment for each prescription filled at a Kaiser Permanente
pharmacy. Prescriptions filled at non-Kaiser Permanente pharmacies are not covered. In addition, over-
the-counter drugs may be purchased at a discount from any Kaiser Permanente pharmacy. The Plan
also provides mental health coverage at Kaiser Permanente facilities. Coverage for outpatient care
includes unlimited visits at no charge. Also, there is no charge for inpatient care for up to a pre-
determined number of days.
Health insurance coverage ends on the last day of the month in which your employment with Kaiser
Permanente ends.
B. Dental Plan
Effective April 1, 2018, Delta Dental Plan coverage becomes effective the first day of the month following
three months of continuous employment. The plan covers a resident, spouse or domestic partner, and
unmarried dependent children under 26 years of age. The Delta Dental Plan covers 90% of the
reasonable and customary charges for diagnostic and preventive services such as X-rays and
semiannual cleanings, 90% for basic services such as fillings, 90% of services such as crowns, and 50%
of services such as prosthodontics. Orthodontics is limited to dependent children under age 19 and is
covered at 50%, with a lifetime maximum benefit of $1,000. The Delta Dental Plan allows a resident to
select any dentist. However, to receive full benefits, it is necessary to visit a participating Delta dentist.
The majority of California dentists participate in the Delta Dental Plan. The maximum dental benefit is
$1,000 per person each calendar year. Dental insurance coverage ends on the last day of the month in
which your employment with Kaiser Permanente ends.
D. Life Insurance, Accidental Death and Dismemberment, and Survivor Assistance
A resident is eligible for $5,000 company-paid group term life insurance effective the first day of the
month after date of hire. A resident has an option to purchase Optional Life Insurance in the amount of
$14,000. If this option is waived when first eligible and a resident wishes to purchase it at a later time,
Evidence of Insurability (EOI) may be required.

- 11 -
The company-paid life insurance also provides Accidental Death and Dismemberment (AD&D) coverage
in the amount of $5,000. If Optional Life Insurance is purchased, it also will include AD&D coverage in the
amount of $6,500.
A resident is automatically enrolled in the Survivor Assistance Benefit. Survivor Assistance provides
financial assistance to a beneficiary in the event of the resident's death. This benefit is equal to one
month of base wage.
E. Professional Liability Insurance
Kaiser Foundation Health Plan, Inc. (KFHP) provides professional liability protection for its employees
and residents and the employees of the following organizations: Kaiser Foundation Hospitals, Kaiser
Foundation Health Plan, Inc. and The Permanente Medical Group, Inc. if any such employee is named as
a defendant in a law suit alleging negligence arising from work performed on behalf of these
organizations. It is, therefore, unnecessary for a resident to carry professional liability insurance.
KFHP will provide a defense for each employee and will pay, when appropriate or legally obligated, all
sums which may be required in judgment or settlement of damages or injuries sustained by an injured
third party, provided the employee was acting in good faith and within the course and scope of his/her job
responsibilities when the negligent act is alleged to have taken place. KFHP is not obligated to provide a
defense for or indemnify the employee if he/she is deemed to have acted wrongfully outside the scope of
his or her employment, for example, in committing a crime or deliberate act which is intended to harm
another person or damage property.
KFHP's protection of the above mentioned employees is financially secured through a combination of self
insurance reserves which are actuarially determined and recorded as liabilities on KFHP's balance sheet,
and excess professional liability insurance policies which are underwritten by credit worthy commercial
insurers and reinsurers. Professional Liability Insurance covers residents while they are on residency
duties in Kaiser Foundation Hospitals or a designated training site. This coverage does not include
professional work outside of the residency program or volunteer activities without prior written approval of
the Director of Graduate Medical Education. Any employee is free to obtain professional liability
insurance if desired, but the cost of such independently purchased must be borne by the employee.
F. Retirement Programs
Retirement benefits at Kaiser Foundation Hospitals and The Permanente Medical Group, Inc. are
designed to provide financial security in retirement. A resident does not accrue a pension benefit during
his/her time in the Residency Program. However, if hired as a Permanente physician following
completion of the Residency Program, training at the PG-2 level and beyond will count toward pension
service in the Retirement Plan for Physicians.
G. Tax Sheltered Annuity Plan
A resident may elect to participate in the Tax Sheltered Annuity (TSA) Plan on date of hire or anytime
thereafter regardless of employment status or work schedule. The TSA Plan is designed to save money
for retirement with pre-tax income. Pre-tax contributions may be made by deferring a percentage of
wages into the plan. Contributions may be invested in a broad range of investment funds.
H. Unemployment Insurance
Employees of Kaiser Permanente are covered by the State Unemployment Compensation Disability
Benefit Program. These benefits are designed to partially replace loss of wages when absent from work
due to a non-work related accident or sickness. A brochure on the State plan may be obtained from the
Human Resource Service Center. A State Disability claim form must be filled out immediately upon being
hospitalized or within the first week of illness if disabled at home. Benefits become payable on the first
day of hospital confinement or on the eighth day of disability at home for those who are eligible.
I. Physician Assistance Program
Physician Assistance Program is available for confidential, cost-free counseling services. It is available to
residents by self-referral or by referral from another source, e.g., Program Director. Services include

- 12 -
counseling and referrals to professional resources for problems with alcohol, drugs, marital difficulties,
family crises, financial or legal problems, and emotional or other concerns. The program is confidential;
however, in certain situations, e.g., substance abuse, the Program Director will require a statement
verifying that the resident is receiving ongoing therapy and is fit to practice in a clinical situation. For
more information, visit the MyHR website: epf.kp.org/wps/portal/hr
.
J. Parent Medical Coverage
Kaiser Permanente offers a group Health Plan coverage for eligible parents, step-parents, parents-in-law
and parents' domestic partners. In order for a resident's parents to qualify, the resident must be an active
employee and eligible for Health Plan coverage. Also, the resident and the eligible parents must reside in
the same Kaiser Permanente region. Premiums are based on age, sex, Medicare eligibility and the
region in which the resident and his/her parents reside. The eligible parent(s) will be responsible for the
entire amount of the monthly premium as well as any applicable co-payments.
K. License Fees
Physician residents continuing in Kaiser Permanente-sponsored programs beyond the PG-1 year will be
reimbursed one time for the USMLE Step 3 or COMLEX Level 3 fee upon successfully passing the
examination provided that the exam is taken by end of the 15
th
month of training. Residents who take the
exam after the end of the 15
th
month of training forfeit their right to reimbursement.
Residents will be reimbursed for licenses and renewals required during residency training including
California Medical license, Drug Enforcement Administrative (DEA) license, and Fluoroscopy license.
Podiatric Surgery residents will be reimbursed for their resident license and renewals from the California
Board of Podiatric Medicine which is the only required license during residency training.
L. Other Benefits
1. Meals
Food services are available 24 hours a day in the cafeteria or vending machines.
Meals will be provided to residents "on call" in-hospital.
2. Sleep Rooms
On-call sleep rooms are provided for in-hospital call duties. A resident lounge may also be
provided.
3. Support Services
Patient support services, such as intravenous services, phlebotomy services, and laboratory
services, as well as messenger and transportation services, are provided.
Laboratory/Pathology/Radiology Services are provided on a 24-hour basis, including access to
reports by computer information systems.
Access to medical records is available 24 hours per day.
4. Lab Coats and Scrubs
White coats and surgical scrubs are provided for residents. Personal laundry service is not
provided. Clothing should be neat, clean, and professional in alignment with the medical facility's
dress policy.
5. Identification Badge
A photo ID badge is provided to each resident. This must be worn at all times.

- 13 -
6. Health Science Library
Health Science Library and services are provided. Access to the health science library is
available 24 hours per day. Computers are available in the library for resident use, and the
Librarian can provide instruction in their use.
7. Parking
Parking facilities are available for residents. Night escort service to the parking area is available
through the Security Department.
8. Child and Elder Care Referral
A resident is eligible on date of hire for Child and Elder Care Referral. This program offers help in
locating and selecting child and elder care by providing information on the resources available
locally. Consultation is available through the Employee Assistance Program.
9. Commuter Choice Program
A resident is eligible to participate in the Commuter Choice Program. This Program allows
residents to set aside tax-free dollars to pay for qualified public transportation, vanpooling and
parking expenses to and from work.
10. Dependent Care Plan
A resident is eligible to participate in the Dependent Care Plan. The Dependent Care Plan allows
contributions of up to $5,000 pre-tax on an annual basis to pay for eligible dependent care
expenses. Examples of such expenses include care at a licensed daycare center or practical
nursing care for an adult.
11. Alliant Federal Credit Union
A resident is eligible to join a full service credit union which offers savings accounts, checking
accounts, loans, home mortgages and other financial services.
12. Kaiser Permanente Activity Program
A resident may take advantage of Kaiser Permanente’s Activity Program that offers discounted
rates as well as customized packages and other specials on a variety of entertainment venues
and events, travel, gifts, products, and services.
13. Educational Stipend
Residents are eligible for an Educational Stipend to attend a conference or for the purchase of
books, CDs or other educational materials subject to the approval of the Program Director.
Educational Stipend details by program specialty may be found at residency-ncal.kp.org
.
14. Fitness Membership
Your health and wellness are important to Kaiser Permanente. You may be reimbursed up to $60
per month for a qualified Fitness Club membership. Please contact your program’s GME
Coordinator to learn details about membership reimbursement.
15. Housing Allowance
A (taxable) housing allowance will be provided to residents in the 2019-2020 academic year to
offset the cost of living in Northern California.
- 14 -
PROFESSIONAL CONCERNS: MEDICAL/LEGAL SERVICES
A. Witnessing Legal Documents
Residents should not sign wills, power of attorney forms or other legal documents as witnesses.
Frequently, proceedings to establish the validity of a will involve witnesses in lengthy court proceedings.
A request to act as witness to a document should be courteously, but firmly, refused.
B. Medical Treatment and Authorization and Patient Consents
Upon admission to the hospital, a patient signs a general treatment authorization form. Subsequently, it
may be necessary that specific treatment or operative consents be obtained in compliance with hospital
policy and legal requirements. No specific treatment, procedures, or examinations may be carried out
unless an appropriate informed consent has been obtained from the patient or guardian or legal
representative. It is essential that the patient gives informed consent that he/she fully understands the
planned procedure, its potential benefits and risks and possible resulting problems. Any unauthorized
procedure, treatment, or examination may be legally construed as an assault and battery. Please note
"appropriate" means informed consent on the part of the patient, which includes discussion and
documentation in the medical record of alternative forms of therapy.
Residents are required to become familiar with the sections relating to permits, consents, and releases in
the Nursing Policy and Procedure Manual located in each nursing unit. These outline the procedures to
be followed in securing the appropriate authorization, permits and consents. In addition, there is a
Consent Manual and a Consent Forms Manual located in the hospital Nursing Supervisor's office and in
Health Information Management (Medical Records) which provide additional legal information.
Special care must be exercised in cases involving minors under age 18, unconscious or confused
patients, operative procedures involving reproductive organs or therapeutic abortions and suspected child
abuse. In such cases, the attending physician or the administrator's office should be contacted for
guidance.
In the case of a medical emergency where treatment is required immediately, treatment may be given
without the patient's express consent if the patient or legal representative is unable to consent. Consent
to treatment is implied in an emergency when the patient or his/her legal representative is unable or
unavailable to give consent. The details of the emergency must be documented, and two licensed
physicians must sign the document.
Patients may refuse treatment. Physicians shall then document that treatment was explained and the
consequences of refusal discussed with the patient.
Securing the patient's informed consent and authorization for treatment is the primary responsibility of the
attending physician. The resident will carry out any instructions indicated by the attending physician in
this regard and will make sure that all appropriate consents have been obtained prior to any treatment or
procedure requiring same.
C. Responding to Legal Documents
Receipt of a subpoena, summons to a court, request to examine a patient's medical record or otherwise
obtain information from it, or a letter from a lawyer concerning patient or hospital matters should be
reported immediately to the Medical-Legal Chief and to the Program Director.
D. Contact with Attorneys/Other individuals
Patient information is confidential and protected by law. Patient or chart information cannot be released
to anyone without the consent of the patient or as authorized by law. The Health Information
Management Department (Medical Records) handles release of medical records. Generally, residents
should not discuss patient care matters with persons who are not part of the patient's health care team,
including investigators or attorneys, without notice to and in the presence of attorneys representing Kaiser

- 15 -
Foundation Hospitals and/or The Permanente Medical Group, Inc. The Medical-Legal Department is
available for further information.
E. Patient Rights and Responsibilities
Patient rights and responsibilities, as outlined in the Kaiser Foundation Hospitals Local Policies and
Procedures Manual, shall be observed at all times.
F. No Code Status
Residents are encouraged to become familiar and comfortable with discussing advanced directives with
patients and their families and with the attending staff.
"No Code" orders are written, when appropriate, in accord with the Hospital's Rules and Regulations and
policies and procedures. A progress note documenting the decision and any discussion with the patient,
family members, and the patient's legal representative must be placed in the patient chart.
G. Durable Power of Attorney for Health Care
Patients admitted to the hospital will be asked by the Admissions Department whether they have
executed a Durable Power of Attorney for Health Care (DPAHC), advance directives, living wills, or other
related documents. Documentation of the discussion and any such available document are included in
the chart.
H. Unusual Incident or Occurrence Reports
An Unusual incident or occurrence in which patients, visitors, or other persons are involved must be
immediately reported in writing by any employee, including residents, witnessing the incident. The
resident physician will complete a "Report of Unusual Incident or Occurrence" which should be forwarded
immediately to the responsible administrator. In urgent cases, the report should be made by telephone.
The resident should also notify the attending physician of unusual occurrences affecting his/her patients.
The report is not part of the medical record, although relevant patient-specific information should be
included in the medical record, as required and appropriate.
Examples of unusual occurrences include, but are not limited to, the following: patient falling out of bed,
incorrect administration or dosage of the medication, patient, visitor or employee injury in the hospital,
major complaints made by patient or visitor, etc.
MEDICAL RECORDS
Medical records are compiled for use in the care and treatment of the patient. It is a documentary of the
course of the illness and treatment. Only approved abbreviations and symbols may be used. Medical
student entries must be co-signed by a resident or attending staff. Residents' history and physical
examinations, operative reports, consultations, and discharge summaries must be reviewed, corrected as
required, and countersigned by the attending physician. Dictation to the medical records is done only by
residents or attending staff.
Kaiser Permanente maintains compliance with requirements to protect the confidentiality and security of
patient information under applicable state and federal law or regulations (e.g., the Health Insurance
Portability and Accountability Act, the California Confidentiality of Medical Information Act, and Title 22 of
the California Code of Regulations), the standards of health care accreditation bodies such as the Joint
Commission, the National Committee for Quality Assurance (NCQA) and internal policies, including the
KP Principles of Responsibility.
To protect each patient’s confidentiality, only those persons responsible for a patient’s care should use
the paper or computer records. The identity of each user of the computer record can be provided to the
patient or their physician upon request. (See Obligations Regarding Confidentiality Policy available on
the MyHR website: epf.kp.org/wps/portal/hr
or the National KP Policy Library:
http://kpnational.policytech.com.
- 16 -
A. Admission History and Physical Examination
The admission history and physical examination requires the physician to clearly document the reason(s)
why the patient needs admission to the hospital. A complete examination must be recorded on all
patients within 24 hours of admission (including pelvic, rectal when appropriate). In the case of patients
admitted for surgery, the history and physical examination must be recorded before surgery.
B. Progress Notes
The patient's progress is to be documented at least daily. All notes should be dated, timed and signed.
In general, elements of the progress notes include:
1. Diagnosis
2. Plan for treatment
3. Need for continued stay at the acute (hospital) level of care
4. Need for diagnostic or therapeutic services
5. Procedures performed
6. Indicators for discharge
The record should be sufficiently detailed and organized so that the responsible physicians can provide
effective, continuing care to the patient and can, if necessary, at a later date, determine what the patient's
condition was at a specific time and can review the diagnostic and therapeutic intervention. Changes in
condition of the patient and results of treatment need to be documented. The record should also enable
another physician to assume care of the patient at any time.
C. Operation Report
An operation report must be dictated immediately after surgery. Resident dictations must be
countersigned by the attending staff physician. In addition to the dictated report, a brief handwritten note
should be placed in the chart. The operation report includes:
1. Preoperative diagnosis
2. Postoperative diagnosis
3. Operation performed
4. Surgeons
5. Findings
6. Procedure in detail
D. Discharge Summary
A discharge summary should be dictated before the patient leaves the hospital. The discharge summary
must be reviewed and signed by the dictating resident.
The discharge summary includes:
1. Identification of MD dictating, patient medical record number, dates of admission and discharge

- 17 -
2. Attending staff MD and consultant services and MDs where appropriate
3. History of present illness/chief complaint in brief summary
4. Pertinent past history, social history, family history, and review of systems
5. Pertinent physical examination on admission
6. Pertinent laboratory and radiographic examinations
7. Course in hospital
8. Operations
9. Procedures
10. Final diagnosis in the same order as on the face sheet. (Note: Abbreviations are not allowed on the
face sheet.)
11. Patient condition upon discharge
12. Discharge medications with dose(s) and frequency
13. Dietary instructions
14. Activities
15. Follow-up appointments
E. Death Summary
A death note and summary must be completed on all patients who expire in the hospital. The chart note
should be written by the physician pronouncing the death and should contain the time and presumed
cause of death. The dictation should follow the discharge summary format with additional information to
include cause of death and autopsy information.
Residents are encouraged to request permission for an autopsy (including limited autopsy). Residents
should also attend the autopsy or review the gross findings with the pathologist.
F. Completion of Medical Records
The law requires that medical records be completed within 14 days of a patient's discharge. A delinquent
record is one that is incomplete more than 14 days after the date of discharge. Physicians with
delinquent records will be notified and may face disciplinary action including suspension if records are not
complete within seven days of notification.
Medical charts cannot be removed from patient care units or from the Health Information Management
Department (Medical Records), except for patient care.
ENVIRONMENTAL HEALTH AND SAFETY POLICIES
Kaiser Permanente ensures safe and healthful working conditions in accordance with all federal, state
and local regulations. (See Environmental Health and Safety Policy available on the MyHR website:
epf.kp.org/wps/portal/hr or the National KP Policy Library: http://kpnational.policytech.com
.
A. Smoking Policy
Smoking is not permitted anywhere inside or outside buildings on the Medical Center Campus.
- 18 -
B. Electrical Safety
All electrical equipment must have proper shielding, power requirements and wiring to be compatible with
the medical center's electrical system. Any personally-owned electrical devices must have appropriate
clearance.
C. Fire and Disaster Drills
As part of the ongoing disaster awareness program, fire drills are conducted once each shift, each
quarter, and disaster drills are conducted at least twice yearly. All members of the professional staff,
resident staff, and support services are expected to be familiar with fire and disaster procedures and to
participate, as required, when they are conducted. In addition to increasing awareness, the drills meet
the requirements of various regulatory agencies governing the licensure of the hospital. (For details, see
the Fire and Disaster Procedures available in the Graduate Medical Education office and discuss
questions with any of the nursing supervisors.) Also, see the Appendix D: Disaster Response Policy.
D. Blood-borne and Air-borne Pathogens
All body fluids and specimens are regarded as potentially infectious. Universal precautions are practiced
in all areas of the medical center. Each resident is required to attend a seminar or review a video
outlining these practices at the commencement of his/her residency.
Syringes and needles and all sharp objects are to be disposed of in the "sharps" disposal boxes. Needles
should not be recapped nor should any sharp objects be left unattended.
All physicians are advised to receive the Hepatitis B vaccine, if indicated.
E. Physician Impairment
Since patient health and safety are the paramount concerns of the institution, no physician shall provide
patient care while impaired by drugs or alcohol. This rule also prohibits the use of alcohol or drugs while
on "beeper call" from home.
A resident suspected or found to have a substance abuse problem will be referred to the Physician Well-
being Committee or to the Chemical Dependency Recovery Program for professional evaluation and
assistance. This service is also available to any resident by self-referral. A resident concerned about the
health and competence of a colleague or about a potential threat to patient care is strongly advised to
report this to his/her Program Director or to the Director of Graduate Medical Education. Confidentiality is
guaranteed for both the person reporting the possibility of substance abuse and for the person suspected
of the abuse.
After treatment and rehabilitation and demonstrated evidence of an ongoing successful recovery
program, the resident may be allowed to rejoin the residency program with appropriate monitoring and
other terms and conditions.
Reporting to legal authorities will be limited to the extent required by law. Circumstances which will result
in reporting to regulatory agencies include resident refusal of treatment or non-compliance with the
treatment plan, unsatisfactory progress towards recovery, risk to the safety of patients, or criminal
activities such as stealing or selling illicit drugs.
F. Security
The hospital has instituted policies and procedures and other measures in an effort to enhance the
security of staff, patients and visitors throughout hospital facilities and grounds, including parking facilities.
Security measures are reviewed on a regular basis. Residents are required to comply with program and
hospital policies, procedures and practices regarding staff and patient security including, but not limited
to, wearing photograph identification badges while on duty, participating in security measures training,
and using hospital facilities for their designated purposes only.

- 19 -
G. Violence in the Workplace
Acts and/or threats of violence by employees or physicians on Kaiser Foundation Hospital premises,
including carrying weapons in other than an official capacity, will not be tolerated and will be grounds for
appropriate remedial action. Similarly, acts and/or threats of violence by patients or visitors against
employees or physicians will not be tolerated and will be grounds for appropriate remedial action. The
Violence in the Workplace policy is available on the MyHR website: epf.kp.org/wps/portal/hr
or the
National KP Policy Library: http://kpnational.policytech.com.
RESIDENT REPRESENTATION ON MEDICAL CENTER COMMITTEES
Resident representation is strongly encouraged on medical center committees. Details may be obtained
in the Graduate Medical Education office.
The institutional and facility Graduate Medical Education Committees must include peer-selected resident
representation. Each facility has a protocol for the annual selection of the resident representatives.
Resident matters and concerns may be brought to the committees through the resident members.
However, any resident may directly contact the Director of Graduate Medical Education or any member of
the Graduate Medical Education Committee.
PHARMACEUTICAL COMPANIES AND REPRESENTATIVES
Resident interaction with pharmaceutical companies and their representatives shall be conducted in strict
compliance with The Permanente Medical Group (TPMG) Conflict of Interest Policy (Exhibit C). Any
questions regarding the interpretation of the TPMG Conflict of Interest Policy should be discussed with
the Program Director.
FINAL CLEARANCE
A check out form must be completed by the resident and submitted to the Graduate Medical Education
office to receive his/her final pay check. The following items are required:
1. Forwarding address and phone number or email address
2. Signature of Health Management Information (Inpatient Medical Records) or Program Director
documenting that all incomplete and delinquent medical records have been dictated and signed
3. Signature of Program Director or GME coordinator
4. Clearance from the Graduate Medical Education Office
5. Return of parking card, meal card, ID badge, keys, lab coats, scrubs, pager, phone, laptop, XyLoc
proximity badge and RAS (Remote Access) token
6. Clearance from the Health Science Library for return of books.
RESIDENCY CLOSURE OR REDUCTION IN SIZE
In the event that a residency program is reduced in size or closed, Kaiser Permanente will inform the
Institutional Graduate Medical Education Committee, Designated Institutional Official and residents
involved as soon as possible. Kaiser Permanente will also, if necessary, assist residents in securing a
position in another ACGME-accredited program or otherwise allow the affected residents to complete
their education.
APPENDICES
APPENDIX A
Medical Care Program
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME G7.5
TITLE
:
RESIDENT ACADEMIC AND PROFESSIONAL
APPEAL PROCESSES
EFFECTIVE DATE:
June 27, 2000
REVISION DATE:
June 21, 2010
CONTACT PERSON: Institutional Director of Medical Education
PAGE 1 of 6 .
I. POLICY
The purpose of this policy is to facilitate the fair and timely resolution of issues concerning a Resident’s academic or
professional performance. This policy, as of its effective date, and thereafter as from time to time amended, sets out
the exclusive internal administrative procedures by which a Resident may obtain review of a decision which directly
concerns his or her academic or professional performance. This policy shall supersede any prior policies, bylaws, rules
or regulations addressing Residents’ academic and professional appeals processes, including the Professional Staff
Bylaws.
II. DEFINITIONS: Capitalized terms are defined in Exhibit A, or in the text of this policy.
III. SCOPE OF POLICY AND PROCEDURE
A. Informal Review (Section IV) is the process available to a Resident to appeal all Decisions that do not fall under
the definition of an Adverse Decision.
B. A Resident subject to an Adverse Decision has a right to request a hearing under the Formal Appeal and Hearing
Procedure (Section V below).
C. Residents do not have a right to the Informal Review or the Formal Appeal and Hearing Procedure for actions
taken against Residents acting in any other capacity, e.g. in his/her capacity as a “moonlighter.”
IV. INFORMAL REVIEW
A. Scope:
Informal Review is the process available to the Resident to appeal Decisions other than Adverse Decisions.
Decisions subject to Informal Review include, for example, routine assessments of the Resident’s performance or
progress, letters of warning, letters of remediation, suspensions for medical record delinquencies pending
completion of the records where the period(s) of suspension total less than thirty (30) calendar days in a twelve
(12) month period, and Administrative Suspensions or Dismissals, e.g., for failure to obtain a California
physician’s license in the requisite time period, or restrictions imposed on a California physician’s license.
B. Process:
1. When the Resident disagrees with a Decision, the Resident has the right and the responsibility to address the
disputed matter with his/her Program Director within 30 calendar days of the Decision. The Program
Director shall meet with the Resident to discuss his or her concerns, and provide the Resident with a written
response within ten (10) business days of the meeting. All written documentation about the disputed matter
shall be made part of the Resident’s Residency Program file (“File”). If the Resident fails to discuss a
Decision with his/her Program Director within thirty (30) calendar days, he/she waives any right to Informal
Review of the Decision.
2. If the Resident is dissatisfied with the outcome of the Program Director’s review of the matter, the Resident
may submit a written statement to the facility Director of Graduate Medical Education (“DGME”), or the
Regional DGME, if the DGME is the Resident’s Program Director. The written statement must describe the
Resident’s concern(s), the reasons why the Resident believes the matter remains unresolved, and the
resolution the Resident is seeking. The DGME shall meet with the Resident to discuss his or her concerns,
and provide a written response within ten (10) business days of the meeting. All written documentation shall
be made part of the Resident’s File. The Resident has no further right to review of the matter.
V. FORMAL APPEAL AND HEARING PROCEDURE
A. Scope:
This Formal Appeal and Hearing Procedure is the process available to a Resident to appeal an Adverse Decision.
B. Procedure:
1. Notice of Adverse Decision and Right to Request Hearing: A Resident who is subject to an Adverse
Decision shall be notified in writing mailed or delivered within ten (10) business days of the Adverse
Decision. The written notice shall advise the Resident of his/her right to request a hearing before an Ad Hoc
Review Panel and the time limit for requesting the hearing. The written notice shall be hand-delivered to the
affected Resident or sent by certified or registered mail, return receipt requested to the Resident’s last known
address on file in the Office of Graduate Medical Education. It is the Resident’s responsibility to keep the
Office informed of his/her current mailing address. Failure to do so may be deemed a waiver of the
Resident’s right to a hearing and acceptance of the Adverse Decision. The written notice shall be deemed
received the sooner of the documented date of actual delivery to the Resident or three (3) calendar days after
the date it is mailed.
2. Time to Request Hearing/Notice of Attorney Representation: To obtain a hearing, the Resident must
submit a written request to the Regional Director of Graduate Medical Education (DGME) within thirty (30)
calendar days of receipt of the written notice to the Resident of the Adverse Decision. If the Resident
intends to be represented by an attorney in the hearing (as further described at Section VB4), his/her request
for a hearing must so state and must provide the name and address of the attorney.
3. Parties: The parties to the hearing shall be the Resident, and the Program Director (or his/her designee)
acting on behalf of the Residency Program.
4. Representation: The Resident shall be entitled to be represented by an attorney or an advisor, at his/her
expense. In addition to notifying of intent to be represented by an attorney when submitting his/her request
for a hearing, the Resident must promptly notify the DGME, the Hearing Officer, and the Program Director
in writing, and in any case no later than fifteen (15) calendar days before the date set for commencement of
the hearing, of any change in representation or any decision to proceed without representation. If the
Resident timely notifies the DGME, Hearing Officer, and Program Director of his/her decision not to be
represented by an attorney, an attorney shall not represent the Residency Program at the hearing. If the
Resident fails to timely notify of a decision not to be represented by an attorney, the Residency Program may
proceed with attorney representation in the hearing, even if the Resident is not represented by an attorney in
the hearing, which shall be decided by the DGME. Whether or not either party is represented by an attorney
during the hearing, each party shall be entitled to receive assistance of an attorney (including
communications between the attorneys and the Hearing Officer) with respect to pre-hearing matters,
preparation for the hearing, and preparation of any written statements.
5. Failure to Timely Request a Hearing—Effect: The Resident’s failure to submit a timely written request for
the hearing shall constitute waiver of his/her right to a hearing and acceptance by the Resident of the
Adverse Decision.
6. Hearing Arrangements; Appointment of Ad Hoc Review Committee and Hearing Officer; Role and
Authority of Hearing Officer:
a) Within ten (10) business days of receipt of the Resident’s written request for a hearing, the DGME
shall arrange for the hearing. This responsibility includes such matters as scheduling a hearing date,
appointing the Ad Hoc Review Panel, appointing a Hearing Officer, and notifying the parties of the
names of the Ad Hoc Review Panel members and the Hearing Officer and the date, time, and place of
the hearing. The hearing shall be scheduled to begin within no less than thirty (30) and no more than
sixty (60) calendar days of receipt of the Resident’s request.
b) The Ad Hoc Review Panel membership shall consist of:
i) Two faculty members, one of whom shall act as Chairperson (“Chair”);
ii) One resident.
The Ad Hoc Review Panel members must not have acted as accusers, fact finders, or initial decision-
makers in, or previously taken an active part in, the matter contested. One Panel member must be in
the same specialty as the affected Resident. Where feasible, the other members shall be from a
different department than the Resident requesting the hearing. The Resident shall be afforded a
reasonable opportunity to question the Ad Hoc Review Panel members, and to challenge the
impartiality of any member, as further described at Section VB7a below.
c) A Hearing Officer shall be appointed to preside at the hearing.
i) The Hearing Officer may participate in the deliberations and act as a legal advisor to the Ad Hoc
Review Panel, but he or she shall not be entitled to vote. He or she shall act to assure that all
participants in the hearing have a reasonable opportunity to be heard and to present all relevant
oral and documentary evidence, and that proper decorum is maintained. He or she shall be entitled
to determine the order of or procedure for presenting evidence and argument during the hearing,
and to set reasonable schedules for timing and/or completion of all matters related to the hearing.
ii) He or she shall have the authority and discretion, in accordance with this Policy, to grant
continuances, to rule on disputed discovery requests, to decide when evidence may or may not be
introduced, to rule on witness issues, including disputes regarding expert witnesses, to rule on
challenges to Ad Hoc Review Panel members, to rule on challenges to himself or herself serving
as a Hearing Officer, and to rule on questions which are raised prior to or during the hearing
pertaining to matters of law, procedure, or the admissibility of evidence.
iii) If the Hearing Officer determines that either side in a hearing is not proceeding in an efficient and
expeditious manner, the Hearing Officer may take such discretionary action as seems warranted by
the circumstances, including, but not limited to, limiting the scope of examination and cross-
examination and setting fair and reasonable time limits on either side’s presentation of the case.
Under extraordinary circumstances, the Hearing Officer’s discretionary action includes, to the
extent permitted by law and subject to concurrence of the Ad Hoc Review Panel, termination of
the hearing. If the termination order is against the AD Hoc Review Panel, the charges against the
resident will be deemed to have been dropped. If, instead, the order is against the resident, the
resident will be deemed to have waived his/her right to a hearing. The party against whom
termination sanctions have been ordered may appeal the matter to the DGME.
iv) In all matters, the Hearing Officer shall act reasonably under the circumstances and in compliance
with applicable legal principles and this Policy. In making rulings, the Hearing Officer shall
endeavor to promote a less formal, rather than more formal, hearing process and also to promote
the swiftest possible resolution of the matter, consistent with the standards of fairness set forth in
this Policy. When no attorney is accompanying any party to the proceedings, the Hearing Officer
shall have authority to interpose any objections and to initiate rulings necessary to ensure a fair
and efficient process.
7. Pre-Hearing Procedures
a) As soon as possible after appointment of the Hearing Officer and the members of the Ad Hoc Review
Panel, the Hearing Officer shall arrange a reasonable process to enable the Resident to pose reasonable
and relevant questions and receive answers from the Hearing Officer and each of the Ad Hoc Review
Panel members as to possible bias. This may, in the discretion of the Hearing Officer, be conducted in
writing, by telephonic meeting, or in person. All challenges must be raised prior to the start of the
hearing, unless the challenging party did not know, and could not have known with reasonable
diligence, the information upon which the challenge is based prior to the start of the hearing. All
challenges shall be ruled upon by the Hearing Officer.
b) Within ten (l0) business days after receipt of the Resident’s written request for a hearing, the Program
Director shall prepare a brief written statement setting forth the Adverse Decision and the reasons for
the Adverse Decision, including the acts or omissions with which the Resident is charged. A copy of
the statement shall be hand-delivered or sent to the Resident by certified or registered mail, return
receipt requested, at his or her last known address on file in the Office of Graduate Medical Education,
with a copy to the DGME.
c) As soon as reasonably practicable after receipt of the request for a hearing, each party shall have the
right to inspect and copy, at the requesting party’s expense, relevant documents of the other party,
subject to applicable privileges. The right of inspection and copying does not extend to confidential
information referring solely to individually identifiable practitioners other than the affected Resident.
The Hearing Officer shall consider and rule on any request for access to information and may impose
any safeguards that the protection of the hearing process, patient confidentiality, and justice require.
d) Upon request, either party may request, and within ten (10) business days of such request, the other
party shall provide a list of witnesses (including name, title, and address) expected to testify on behalf
of that party at the hearing.

e) Additionally, whether or not previously requested, at least ten (10) business days before the scheduled
hearing date, each party shall distribute the following items to the other party and to the Hearing
Officer:
i) A list and copies of the documents which the party intends to introduce;
ii) A list of the party’s witnesses with a summary of the subject matter about which each witness will
be testifying and the relevance of that witness’ testimony to the matters at issue in the hearing.
Failure, without good cause, to provide copies of documents and/or information about intended
witnesses and testimony shall be grounds for the Hearing Officer to exclude the proffered documents
and/or testimony. The Hearing Officer may provide for prior distribution of documents to the Ad Hoc
Review Panel once each party has had a reasonable opportunity to review and pose any objections to
the proffered evidence.
f) The Hearing Officer shall address any other pre-hearing procedural disputes. Objections to any pre-
hearing decision or ruling should be posed to the Hearing Officer and ruled upon as promptly as
possible prior to the hearing, and may be succinctly reasserted at the hearing.
8. Rights of the Parties at the Hearing: During the hearing, both parties shall have the following rights:
a) To be provided with all information made available to the Ad Hoc Review Panel;
b) To call, examine, and cross-examine witnesses;
c) To present and rebut evidence determined to be relevant by the Hearing Officer;
d) To submit a written statement at the close of the hearing;
e) To be accompanied at the hearing by an advisor and/or an attorney, as further described at Section
VB4.
9. Resident’s Failure to Personally Appear and Proceed—Effect: The Resident’s failure to personally appear
and proceed at the hearing without good cause shall constitute a waiver of the right to a hearing and
acceptance by the Resident of the Adverse Decision.
10. Presence of Ad Hoc Review Panel: All members of the Ad Hoc Review Panel are expected to be present
throughout the hearing. However, if an Ad Hoc Review Panel is unavoidably absent from any part of the
proceedings, the absent Panel member may review the recording or transcript of the missed hearing (or
portion thereof), and thereafter may participate in deliberations and the final decision.
11. Procedure at the Hearing
a) The Hearing Officer shall preside at the hearing and assure that all parties are heard and given an
adequate opportunity to present relevant evidence and arguments.
b) Order of presentation:
i) Each party may make an opening statement.
ii) After each party has made or waived its opening statement, the Program Director shall present,
including any witness(es) he or she intends to call.
iii) The Resident shall present second, including any witness(es) the Resident intends to call.
iv) The Resident may be called as a witness and is expected to testify in response to questions posed
by the Program Director.
v) The Ad Hoc Review Panel or Hearing Officer may pose questions to any witness, including the
Resident.
c) Continuances may be granted by the Hearing Officer upon timely request and a showing of good
cause. The Hearing Officer should consider the schedules and availability of the Ad Hoc Review
Panel members in ruling on any requested continuances, and shall afford priority to expeditious
completion of the hearing.
d) The hearing shall be closed and informal. Rules of evidence or judicial procedure need not be
followed. Testimony, however, shall be under oath.
e) On conclusion of the presentation of evidence and arguments, the Hearing Officer shall declare the
hearing closed.
f) Thereafter, the Ad Hoc Review Panel shall deliberate privately and reach a decision based on the
evidence presented at the hearing, including oral testimony, written statements, and other documents,
including medical record information, introduced at the hearing. The Chair shall preside over the
deliberations, with the assistance of the Hearing Officer who shall be present at and may participate in
these deliberations for the purpose of assuring that all relevant issues are addressed, and that
appropriate legal standards and procedural rights are observed, but shall not vote. The Hearing Officer
shall also be responsible to prepare the written report of the Ad Hoc Review Panel’s decision.
g) Within thirty (30) calendar days of the close of the hearing, the Ad Hoc Review Panel shall issue its
report and decision in writing to the Hospital Administrator and the DGME. The report shall include
findings of fact and a conclusion stating the connection between the evidence produced at the hearing
and the decision reached. The report, which shall constitute the final decision of the Ad Hoc Review
Panel, shall make findings as to whether the Adverse Decision was or was not reasonable and
warranted; but the Ad Hoc Review Panel shall not have authority to modify or impose an alternative
Adverse Decision.. The Hearing Officer shall have a copy of the report sent to the Resident by
personal delivery or registered or certified mail, with a copy to the Program Director.
h) The decision of the Ad Hoc Review Panel is final, and neither party has any further right to review of
the matter.
i) The report and decision of the Ad Hoc Review Panel shall be made part of the Resident’s File.
C. Other Hearing Issues:
1. 1. Burden of Going Forward and Burden of Persuasion: The Program Director or other decision making
body which made the Adverse Decision shall initially come forward with evidence in support of the
decision concerning the Resident. Thereafter the burden will shift to the Resident to come forward with
evidence to establish the decision was improper. The Ad Hoc Review Panel will evaluate the evidence
presented. The decision of the Program Director or other decision making body will be upheld unless the
Ad Hoc Review Panel finds upon review of the evidence presented that by clear and convincing proof the
disputed action was arbitrary or capricious.
2. Fees and Costs: Each party shall bear its own legal fees and other costs.
3. Recording the Proceeding: The Hearing Officer shall arrange to have the hearing recorded by a court
reporter, at the expense of the Residency Program. A party shall not be permitted to independently audio
or videotape, or otherwise record the proceedings. The Hearing Officer shall provide a copy of the
transcript to a requesting party upon payment of the cost therefore, as follows: The cost of a transcription
of the matters reported by the court reporter shall be borne by the party requesting the transcription. A
party requesting a copy of a transcription shall pay the cost of the copy. The Office of Graduate Medical
Education shall retain the original transcripts.
GLOSSARY
Adverse Decision means an action or proposed action which directly concerns the Resident’s academic or
professional performance and involves the Resident’s proposed dismissal or dismissal (other than
Administrative Dismissals) from the Residency Program, or otherwise threatens a Resident’s intended career
development. An Adverse Decision includes, but is not limited to:
• Notice of intent to suspend or suspension (except Administrative Suspensions or suspensions which total
no more than thirty (30) calendar days in any twelve month period, e.g., for medical records delinquency
pending completion of the records);
• notice of intent to dismiss or dismissal (except Administrative Dismissal);
• requiring the resident to repeat a residency training year
• nonrenewal of the Resident’s contract;
• any action for which a report is required to a government agency, e.g., a report to the Medical Board of
California for a medical disciplinary cause or reason under California Business and Professions Code
section 805.
Administrative Suspension or Dismissal means an automatic suspension or dismissal, such as a dismissal for
failure to obtain a California physician’s license in the requisite time period.
Decision means an action or proposed action which directly concerns the Resident’s academic and professional
performance.
Resident means a post-graduate medical or podiatric trainee, including a training fellow, who is enrolled in an
approved medical or podiatric residency program sponsored by a Kaiser Foundation Hospital.
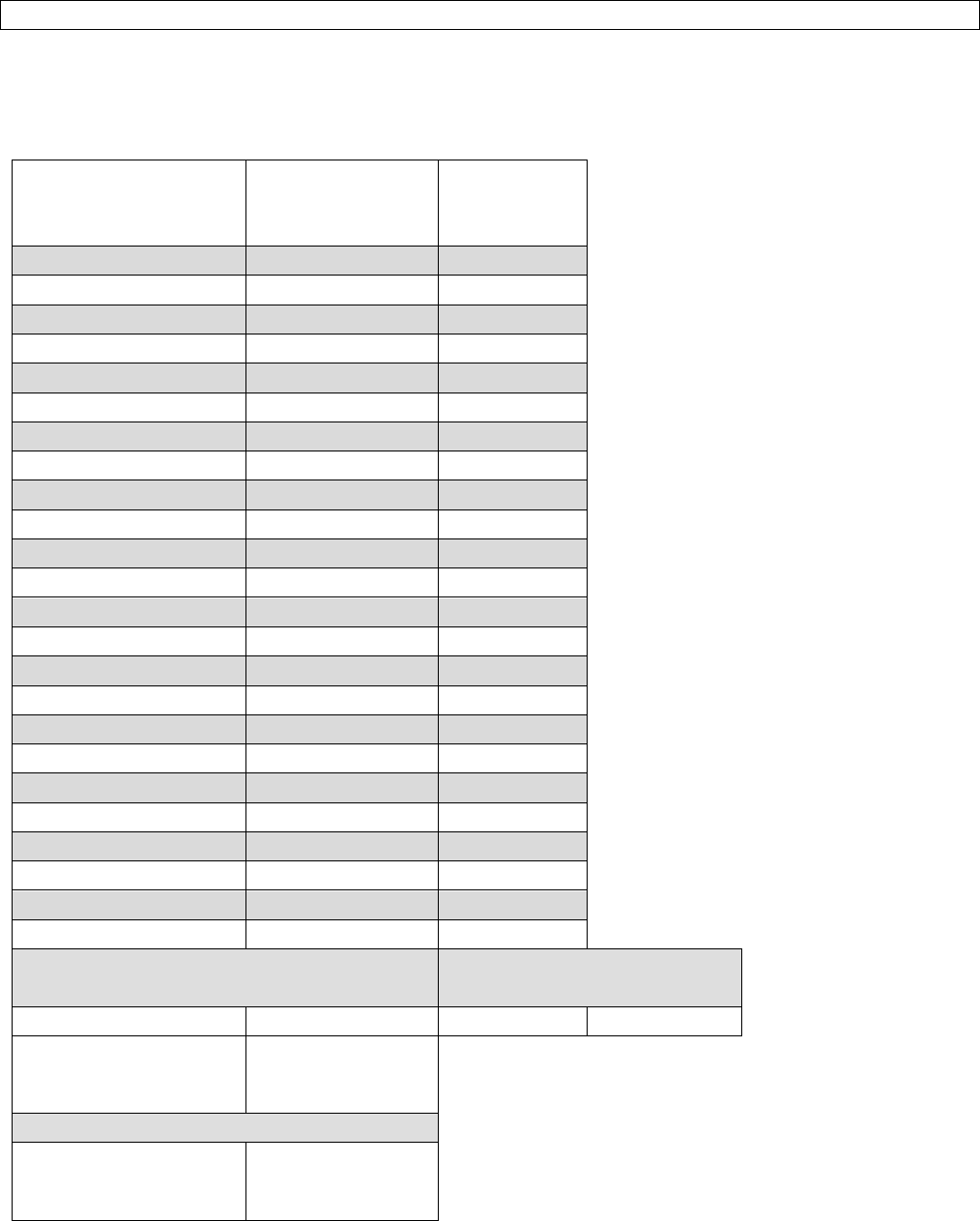
APPENDIX B
2019-2020 Annual Resident Salary Schedule and Job Codes
Effective July 1, 2019
Job Title/Job Code
2019-2020
Annual Rate
2019-2020
Annual
Hourly Rate
Resident I
$67,036.03
$32.2289
22400
Resident II
$70,628.65
$33.9561
22411
Resident III
$75,119.18
$36.1150
22412
Resident IV
$79,510.28
$38.2261
22413
Resident V
$83,415.53
$40.1036
22440
Chief Resident III
$77,726.78
$37.3686
22417
Chief Resident IV
$82,117.88
$39.4797
22416
Chief Resident V
$86,023.13
$41.3573
22415
Resident Faculty
$125,150.45
$60.1685
22419
Fellow I
$88,630.73
$42.6109
22437
Fellow II
$91,238.33
$43.8646
22438
Fellow III
$93,845.93
$45.1182
22441
Annual Housing Allowance (2019-2020)
Gym Membership (2019-
2020)
$3,500.00
SFO, SRO
$60/m
All sites
$2,000.00
SCL, OAK, VAL, SAC,
SNL, SJO, SSAC
Relocation Stipend (2019-2020)
$1,000.00
All new KP residents
and fellows
APPENDIX C
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME G6.5
TITLE:
CONFLICT OF INTEREST POLICY
EFFECTIVE DATE:
July 1, 2007
CONTACT PERSON: Institutional Director of Graduate Medical Education
I. PURPOSE
Kaiser Permanente Residents shall not engage in any activities which create, or appear to create, a conflict of
interest, and which could
1. Adversely impact the independence and objectivity of their judgment in carrying out their responsibilities
as a trainee, or
2. Conflict with the interests of Kaiser Permanente members and patients, or
3. Create the appearance of impropriety from an ethical, legal or compliance perspective.
II. SCOPE
This policy applies to all KFH sponsored resident physicians. Conflict of Interest means any personal
relationships or interests, including financial interests, which interfere or have the potential to interfere with
professional roles, responsibilities or judgments of residents, and which place the interests of trainees ahead of
the interests of Kaiser Permanente.
III. POLICIES
Competitor, Vendor and Supplier Relationships
To protect the interests of Kaiser Permanente (KP) members and patients, The Permanente Medical Group
(TPMG), and the Kaiser Permanente Medical Care Program, the selection of drugs, devices, supplies,
equipment and services for purchase, or inclusion in a formulary or Clinical Practice Guideline, must be based
on sound clinical (quality, safety and effectiveness) and business (dependability, value, service, price) criteria.
Relationships between KP residents and Vendors, (including suppliers and commercial entities doing business
with or seeking to do business with Kaiser Permanente) must be free of conflict of interest, or the appearance of
conflict of interest.
Physicians, trainees, and others with the ability to direct or influence the selection, purchase or utilization of
goods or services by Kaiser Permanente must have a current, signed Conflict of Interest disclosure attesting
that they or an immediate family member,
1. Have not received direct or indirect remuneration from a Vendor.
2. Have no financial interest in the Vendor or a competitor of the Vendor.
3. Vendor, in this section, refers to a Vendor whose products or services will be, or could be, considered
for selection, purchase or utilization by a group on which the resident serves.
Should a conflict develop, physicians and trainees serving in these capacities shall disclose the conflicts, and
recuse themself from participating in purchasing decisions or deliberations related to the selection, purchase or
utilization of the products or services of the Vendor, or a competitor of the Vendor.
“Financial interest” means ownership interest in stocks, bonds, privately held companies, debt obligations,
options, rights to buy or sell stock, shares in profits, investments, or other proprietary interests. “Financial
interest” does not include ownership of mutual fund shares or stock holdings in a publicly traded company,
provided the shares in the publicly traded company total 1% or less of the company’s ownership and are not a
controlling interest in the company.
For purposes of this policy, “immediate family member” means a current or former spouse or domestic partner;
an adopted or biological child or stepchild; the spouse or domestic partner of an adopted child, biological child
or stepchild, whether or not they reside in the trainee’s household; or anyone residing in the trainee’s
household.
“Family member” includes parents, grandchildren, siblings, aunts, uncles, cousins, in-laws, spouse or domestic
partner’s immediate family and other close relatives.
Gifts
Residents may not accept products or services from Vendors, Consultants or organizations doing business or
seeking to do business with Kaiser Permanente, which are free, or at reduced or discounted prices, and which
are for the benefit of the physicians or their family members.
Residents may not accept Vendor funding for items of value, including but not limited to equipment, supplies,
salaries, for the Residency Program, Department, or the Medical Center other than as stipulated in an approved
research arrangement, negotiated as part of a purchasing agreement, or arranged through a contract with
Kaiser Permanente for evaluation of a new technology.
Commercial Support for Education
TPMG Physician Education and Development (PED) shall maintain fiscal oversight and fiscal control of any
commercial funds used to support CME and GME programs in Northern California. Unrestricted educational
grants from Vendors will be accepted through written contract with PED. The Director of Continuing Medical
Education/and or Director of Graduate Medical Education will work with internal program planners to ensure
compliance with CME and/or GME policies and facilitate disbursement of funds.
Commercial entities providing unrestricted grants for CME and/or GME may not disperse separate from the
contract, and residents may not accept directly from the commercial entity, honoraria, faculty expenses, travel
reimbursement, gifts, gratuities or other compensation.
Drug, device, equipment and biotech companies (Vendors) and other commercial entities may not provide
funding for meals, snacks, gifts or other forms of compensation for departmental meetings, CME and/or GME
meetings on-site in Kaiser Permanente facilities, or off-site at meetings directed specifically to KP physicians
and trainees, employees, or allied health professionals.
Vendor support for meals provided to all participants as part of a CME and/or GME meeting or professional
society meeting which is open to all physicians is considered to be a legitimate part of attendance at the
meeting and is allowed.
Residents who serve as faculty at CME and/or GME or other educational programs must sign a “Disclosure of
Conflict of Interest” form, even if no conflict exists.
Involvement with Organizations Outside Kaiser Permanente
Participation in professional societies and medical societies is encouraged. Residents may serve as Officers
and Directors of these associations.
Residents may not serve as Officers, Partners, Directors or consultants to an organization or entity which
competes with Kaiser Permanente.
Residents may not serve as Officers, Partners, Directors or consultants to an organization which does business
with, or which may seek or plan to do business with, KP without prior approval of the Program Director and
Designated Institutional Official (DIO), who will evaluate the request based on the potential for conflict of interest
or adverse impact on Kaiser Permanente. This includes drug, biotech, device and equipment suppliers among
others.
For the purpose of this policy, proprietary information is information in which Kaiser Permanente has an
ownership interest, potential ownership interest, or other legal right (e.g. license or Copyright), or the disclosure
of which could adversely impact the organization.
Speakers’ Bureaus
Residents may not receive remuneration, gifts, gratuities, travel expenses or honoraria from Vendors for
participation in a Vendor’s Speakers’ Bureau. Residents must receive prior approval from the Program Director
to participate, and approval will be granted only in those circumstances in which participation is deemed to be in
the interest of Kaiser Permanente.
Honoraria and Presentations
Residents may not accept and retain honoraria from a Vendor for teaching or giving presentations, including
payment for time, travel expenses, meals, entertainment, recreational or social activities.
Honoraria from educational institutions, training programs, professional associations, non-profit organizations,
or government agencies may be accepted and retained, with prior approval from the Program Director and DIO.
Inclusion of confidential or proprietary Kaiser Permanente data or information in outside teaching or lecture
materials is prohibited.
Vendor-Sponsored Product Demonstrations, Non-CME Educational Programs and Conferences
Residents may not accept reimbursement from Vendors for the cost of travel and/or attendance at product
demonstrations, conferences, or non-CME educational programs. KP may choose to sponsor/support a
resident’s attendance at such a meeting if it is deemed to be in the interest of KP.
Residents may, on their own time and at their own expense, attend such meetings as long as:
1. Nothing of substantial value is received by the resident.
2. The meeting is available to all residents within and outside KP.
Representing Kaiser Permanente
A resident, in his/her professional capacity should not represent himself/herself as a representative of TPMG or
Kaiser Permanente in any manner outside the scope of his/her job responsibilities and duties, without prior
approval of the Program Director.
Employment of Family Members or Other Relatives
Residents should not hire, manage or supervise family members. Family members who are employed
by KP should be reasonably separated from each other with respect to the scope of supervision and
influence in job assignments, appraisals, promotions, compensation and other employment-related
matters.

Medicare and Medicaid Referrals
Residents may not offer, pay, solicit or receive anything of value for the referral of any Medicare patient
if Medicare is reasonably expected to pay for any part of the service or supply that is provided as part
of the referral.
Residents may not refer any Medicare or Medicaid beneficiary for health services (including supplies
and prescription drugs) to any entity in which the physician or a family member has an ownership
interest or a compensation arrangement.
APPENDIX D
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME G11.1
TITLE:
DISASTER POLICY
EFFECTIVE DATE:
July 1, 2007
CONTACT PERSON: Institutional Director of Graduate Medical Education
I. PURPOSE
In the event of a disaster impacting the graduate medical education programs sponsored by Kaiser Permanente
(KP), the Institutional Graduate Medical Education Committee (IGMEC) establishes this policy to protect the
well being, safety and educational experience of residents enrolled in our training programs.
II. SCOPE
This policy applies to all KFH sponsored resident physicians.
III. POLICIES
For the purposes of this policy, the definition of a disaster is the prolonged interruption of patient care services
or as defined by the ACGME in their policies or procedures published at a later date. Following a disaster, the
IGMEC working with the Designated Institutional Official (DIO) and other sponsoring institution leadership will
strive to restructure or reconstitute the educational experience as quickly as possible following the disaster. In
order to maximize the likelihood that residents will be able to complete program requirements within the
standard time required for certification in that specialty, the DIO and IGMEC will make the determination that
transfer to another KP medical center is necessary.
Once the DIO and IGMEC determine that the current program site can no longer provide an adequate
educational experience for its residents, the sponsoring institution will to the best of its ability arrange for the
temporary transfer of the residents to other existing KP programs at other facilities until such time as the
current program site is able to resume providing the educational experience. Residents who transfer to other
programs as a result of a disaster will be provided by their Program Directors with an estimated time that
relocation to another program or facility will be necessary. Should that initial time estimate need to be extended,
the resident will be notified by their Program Directors using written or electronic means identifying the
estimated time of the extension. If the disaster prevents the current program site from
re-establishing an adequate educational experience within a reasonable amount of time following the disaster,
then permanent transfers will be arranged.
The DIO will be the primary institutional contact with the ACGME and the Institutional Review Committee
regarding disaster plan implementation and needs within the sponsoring institution.
In the event of a disaster affecting other sponsoring institutions of graduate medical education programs, the
program leadership at KP will work collaboratively with the KP DIO who will coordinate on behalf of KP the
ability to accept transfer residents from other institutions. This will include the process to request complement
increases with the ACGME that may be required to accept additional residents for training.
Programs will be responsible for establishing procedures to protect the academic and personnel files of all
residents from loss or destruction by disaster. This should include at least a plan for storage of backup
computerized data in a separate geographic location away from the program site.
APPENDIX E
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME 14.0
TITLE:
Pre-Employment Drug Testing
EFFECTIVE DATE:
July 1, 2008
CONTACT PERSON: Institutional Director of Graduate Medical Education
1.0 Policy Statement
The Kaiser Permanente Northern California Region (KP) is committed to providing comprehensive employment
screening of all applicants upon a conditional offer of employment. In addition, KP requires that all individuals
external to KP who have been offered employment complete pre-employment drug testing demonstrating the
absence of illegal drugs or inappropriate use of legal drugs.
2.0 Purpose
The purpose of this policy is to take appropriate action designed to ensure a safe environment for employees,
members, patients and the community, and to protect the financial resources and assets of KP.
3.0 Scope/Coverage
This policy applies to all individuals external to KP who received a conditional offer for employment in the
Northern California Region in full-time, part-time, temporary or on-call/per diem positions, any paid student or
intern, and Home Health/Hospice volunteers with any of the following entities (collectively referred to as “Kaiser
Permanente”):
3.1 Kaiser Foundation Health Plan, Inc. and Kaiser Foundation Hospitals (together, KFHP/H);
3.2 KFHP/H’s subsidiaries; and
3.3 The Permanente Medical Group (TPMG) [NOTE: This policy is not applicable to individuals applying for
positions as physicians, podiatrists or Vice Presidents of TPMG, which are covered by separate TPMG
policies.]
4.0 Definitions
n/a
5.0 Provisions
5.1 Pre-employment drug testing is a condition of employment with KP. It is standard, mandatory, and
applies to all external new hire individuals (“applicants”) listed in the Scope/Coverage section of this
policy.
5.2 All positive test results will require rescission of the conditional offer of employment.
5.3 Applicants who fail or refuse the pre-employment drug screening will not be hired. Applicants must sign
the consent form and comply with all other aspects of the drug screening process.
5.4 Pre-employment drug testing and results are to be completed prior to the first day of work.
5.5 KP utilizes an external laboratory to conduct the drug testing.
5.6 All information received by KP as part of the pre-employment drug testing program including the drug
test results is confidential. Unless authorized by state or federal laws, rules or regulations or required by
a court order, KP will not release this information without a written consent signed by the applicant who
was screened.
6.0 Procedure
6.1 Recruitment notifies the candidate the job offer is contingent on:
6.1.1 completion of the pre-employment drug testing; and
6.1.2 satisfactory drug test results.
6.2 KP will enlist the services of an outside laboratory certified by the U.S. Department of Health and
Human Services (DHHS certified) to conduct all pre-employment drug testing.
6.3 Following a conditional offer of employment, Human Resources-Recruitment will provide applicants with
a consent form and other documents relating to the drug screening. Within 48 hours (Monday-Friday) of
receiving the consent form, the candidate must present him/herself to a DHHS certified laboratory
authorized by KP, to provide a urine specimen for drug testing. NOTE: If notified on a Friday, the
candidate will be required to complete the drug test no later than 5:00 PM the following Tuesday.
6.4 Independent medical review of all positive results is conducted by a trained medical review officer
(MRO) who is not employed by KP. KP’s authorized laboratory will provide all positive test results to the
MRO. The MRO will notify the applicant of positive test results and obtain the applicant’s explanation.
The MRO will interpret each positive test result and will provide verified drug tests as negative or
positive to Human Resources-Recruitment.
6.5 Human Resources-Recruitment will rescind the conditional offer of employment upon receipt of positive
test results.
6.6 Applicants with positive test results may reapply after 12 months.
APPENDIX F
Kaiser Permanente Resident Council Mission
Established June, 2008
The Regional Resident Council is comprised of resident representatives to the Institutional Graduate
Medical Education Committee (IGMEC). It was created to evaluate local, regional, and systemic issues
affecting residents in Kaiser Permanente Northern California-based residency programs. Our goal is to
continually look for areas of improvement to enrich the graduate medical education at Kaiser Permanente while
ensuring program compliance with ACGME requirements.
The council will also serve as an anonymous forum where residents may present concerns without fear
of retribution regarding their local program if their concerns cannot be resolved at the program level, or if
regional changes to the Kaiser Graduate Medical Education system are required. This allows residents to have
a means of reaching IGMEC and the Designated Institutional Official (DIO) through a direct channel, while
retaining personal anonymity.
We also hope to serve as a forum for “best practices”, where residents can share program successes
and areas that work well to be integrated into other programs for improvement in our graduate medical
educational quality throughout the region.
APPENDIX G
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME G8.0
TITLE:
REMOTE ACCESS TOKENS FOR RESIDENTS
EFFECTIVE DATE:
July 1, 2008
CONTACT PERSON: Institutional Director of Graduate Medical Education
I. POLICY STATEMENT
Resident physicians while training at Kaiser Foundation Hospitals (KFH) may receive remote access tokens
upon approval by their KP (Kaiser Permanente) Program Director or Site Director.
II. PURPOSE
The purpose of this policy is to provide a mechanism and procedure for the disbursement and collection of
remote access token provided to resident physicians.
III. SCOPE
This policy applies to all KFH sponsored resident physicians. This policy also applies to affiliate resident
physicians that rotate to KFH. Affiliate residents must have additional approval by the facility Director of
Graduate Medical Education.
IV. POLICIES
Resident physicians are provided remote access token through their assigned or local Kaiser Permanente
Graduate Medical Education office. The resident physician is required to sign an affidavit confirming receipt of
the remote access token and acknowledging the token will be returned upon completion of their residency
training at KFH. The local Graduate Medical Education office will terminate the use of the remote access token
and/or reset it for another user.
V. RESPONSIBILITIES
a) Resident physicians are responsible for the safety and security of the remote access token at all
times.
b) The facility GME office is responsible for disbursement and collection of remote access tokens,
including returning the tokens or resetting the tokens for future use by new resident physicians.
APPENDIX H
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME IGME G13.0
TITLE:
Resident Transfers
EFFECTIVE DATE:
April 3, 2009
CONTACT PERSON: Institutional Director of Graduate Medical Education
I. PURPOSE
Residents may transfer into or out of Kaiser Permanente Northern California (KPNC) Residency Programs to
complete their training. The purpose of this policy is to outline the requirements for such transferred residents
II. SCOPE
This policy applies to all ACGME sponsored programs.
III. POLICIES
In the event that a resident transfers from another residency program into a KPNC sponsored residency
program, the Accreditation Council of Graduate Medical Education (ACGME) requirements must be met. The
total number of a program’s ACGME approved positions, may not exceed the capacity established, without
approved from the Designated Institutional Official and ACGME.
To determine the appropriate level of education for residents who are transferring from another residency
program, the program director must receive written verification of previous educational experiences and a
statement, in accordance with the ACGME, regarding the performance evaluation of the transferring resident
prior to their acceptance into the KPNC program. The written verification will become part of the resident’s
personnel file.
If a KPNC sponsored resident leaves the program prior to completion of their education, the program director is
responsible for notifying ACGME and compliance with the ACGME Institutional, Common and Program Specific
requirements governing such program transfers.
In the event a resident leaves the KPNC program prior to completion of their education, the program director is
required to provide verification of residency education and final evaluation. As defined by ACGME, to the new
program that the resident intends to transfer.
APPENDIX I
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGME IGME G16.1
TITLE
: United States Medical Licensing Exam (USMLE)
Step III Requirement
EFFECTIVE DATE:
July 1, 2010
CONTACT PERSON: Institutional Director of Graduate Medical Education
II. PURPOSE
Residents are required to take and pass the United States Medical Licensing Exam (USMLE) Step 1 and 2
before applying for the Postgraduate Training License (PTL). The purpose of this policy is to outline the time
requirements for Kaiser Permanente sponsored residents to take the USMLE Step 3.
II. SCOPE
This policy applies to all Kaiser Permanente sponsored residents.
IV. POLICIES
Kaiser Permanente sponsored residents must take the USMLE Step 3 by the end of their 15
th
month of
residency training. Time spent in residency training includes previous time spent at other residency programs.
If residents fail the USMLE Step 3, they must inform their Program Director immediately and schedule to retake
the exam. If the resident does not pass the exam before the date that the California Medical Board requires
them to, the resident could risk being placed on unpaid administrative leave and/or not receiving a resident
appointment agreement for the subsequent academic year.
Appendix J
ACGME The Learning and Working Environment – Effective July 1, 2017
Residency education must occur in the context of a learning and working environment
that emphasizes the following principles:
• Excellence in the safety and quality of care rendered to patients by residents today
• Excellence in the safety and quality of care rendered to patients by today’s residents
in their future practice
• Excellence in professionalism through faculty modeling of:
o the effacement of self-interest in a humanistic environment that supports the
professional development of physicians
o the joy of curiosity, problem-solving, intellectual rigor, and discovery
• Commitment to the well-being of the students, residents, faculty members, and all
members of the health care team
Maximum Hours
of Clinical and
Educational Work
per Week
Clinical and educational work hours must be limited to no more than 80
hours per week, averaged over a four-week period, inclusive of all in
house clinical and educational activities, clinical work done from home,
and all moonlighting.
(Core)
Moonlighting
• Moonlighting must not interfere with the ability of the resident to
achieve the goals and objectives of the educational program,
and must not interfere with the resident’s fitness for work nor
compromise patient safety.
(Core)
• Time spent by residents in internal and external moonlighting
(as defined in the ACGME Glossary of Terms) must be counted
toward the 80-hour maximum weekly limit.
(Core)
• PGY-1 residents are not permitted to moonlight.
(Core)
Mandatory Time
Free of Duty
The program must design an effective program structure that is
configured to provide residents with educational opportunities, as well
as reasonable opportunities for rest and personal well-being.
(Core)
• Residents should have eight hours off between scheduled
clinical work and education periods.
(Detail)
o There may be circumstances when residents choose to
stay to care for their patients or return to the hospital with
fewer than eight hours free of clinical experience and
education. This must occur within the context of the 80-
hour and the one-day-off-in-seven requirements.
(Detail)
• Residents must have at least 14 hours free of clinical work and
education after 24 hours of in-house call.
(Core)
• Residents must be scheduled for a minimum of one day in
seven free of clinical work and required education (when
averaged over four weeks). At-home call cannot be assigned on
these free days.
(Core)
Maximum Clinical
Work and
Education Period
Length
• Clinical and educational work periods for residents must not
exceed 24 hours of continuous scheduled clinical assignments.
(Core)
o Up to four hours of additional time may be used for
activities related to patient safety, such as providing
effective transitions of care, and/or resident education.
(Core)
Additional patient care responsibilities must not be
assigned to a resident during this time.
(Core)
PGY-1 – 16 hour maximum
PGY-2 and above –
• 24 hour maximum (24+4) Additional 4 hours if needed to ensure
appropriate, effective, safe transition of care after 24 hours.
• No new patients, procedures, or clinics after 24 hrs of
continuous in-house duty.
• Residents, at their discretion, may attend educational
conferences.
• Strategic napping strongly suggested after 16 hours of
continuous duty and between the hours of 10pm-8am.
In-House Night
Float
Night float must occur within the context of the 80-hour and one-day-
off-in-seven requirements. (Core)
[The maximum number of consecutive weeks of night float, and
maximum number of months of night float per year may be further
specified by the Review Committee.]
Maximum In-
House Call
Frequency
Residents must be scheduled for in-house call no more frequently than every
third night (when averaged over a four-week period). (Core)
At-Home Call
• Time spent on patient care activities by residents on at-home
call must count toward the 80-hour maximum weekly limit. The
frequency of at-home call is not subject to the every-third-night
limitation, but must satisfy the requirement for one day in seven
free of clinical work and education, when averaged over four
weeks.
(Core)
o At-home call must not be so frequent or taxing as to
preclude rest or reasonable personal time for each
resident.
(Core)
• Residents are permitted to return to the hospital while on at-
home call to provide direct care for new or established patients.
These hours of inpatient patient care must be included in the
80-hour maximum weekly limit.
(Detail)
Clinical and
Educational Work
Hour Exceptions
In rare circumstances, after handing off all other responsibilities, a
resident, on their own initiative, may elect to remain or return to the
clinical site in the following circumstances:
• to continue to provide care to a single severely ill or unstable
patient;
(Detail)
• humanistic attention to the needs of a patient or family; or,
(Detail)
• to attend unique educational events.
(Detail)
These additional hours of care or education will be counted toward the
80-hour weekly limit. (
(Detail)
A Review Committee may grant rotation-specific exceptions for up to
10 percent or a maximum of 88 clinical and educational work hours to
individual programs based on a sound educational rationale.
• In preparing a request for an exception, the program director
must follow the clinical and educational work hour exception
policy from the ACGME Manual of Policies and Procedures.
(Core)
• Prior to submitting the request to the Review Committee, the
program director must obtain approval from the Sponsoring
Institution’s GMEC and DIO. (Core)
Important Notes:
Programs must have a duty hour monitoring procedure which details
how violations are addressed, resolved, and prevented from occurring
in the future
Averaging must occur by rotation – 4 week period, 1 month period, or
the period of a rotation if less than 4 weeks.
Vacation and leave must be excluded when calculating duty hours, call
frequency, or days off.
APPENDIX K
Supervision of Residents
Each patient must have an identifiable, appropriately-credentialed and privileged attending
physician who is ultimately responsible for that patient’s care. This information should be
available to residents, faculty, and patients. Residents and faculty should inform patients of
their respective roles in each patient’s care.
Each training program must demonstrate that the appropriate level of supervision is in place
for all residents who care for patients. Supervision may be exercised through a variety of
methods. Some activities require the physical presence of the supervising faculty member.
For many aspects of patient care, the supervising physician may be more advanced
residents. Other portions of care provided by the resident can be adequately supervised by
immediate availability of the supervising faculty member or resident physician, either in the
institution, or by means of telephonic and/or electronic modalities. In some circumstances,
supervision may include post-hoc review of resident-delivered care with feedback as to the
appropriateness of that care.
Levels of Supervision
To ensure oversight of resident supervision and graded authority and responsibility, each
program must use the following classification of supervision:
Direct Supervision:
• The supervising physician is physically present with the resident and patient.
Indirect Supervision:
• With direct supervision immediately available – the supervising physician is physically
within the hospital or other site of patient care, and is immediately available to provide
direct supervision.
• With direct supervision available – the supervising physician is not physically present
within the hospital or other site of patient care, but is immediately available by means
of telephonic and/or electronic modalities, and is available to provide direct
supervision.
Oversight:
• The supervising physician is available to provide review of procedures/encounters with
feedback provided after care is delivered.
The privilege of progressive authority and responsibility, conditional independence, and a
supervisory role in patient care delegated to each resident must be assigned by the program
director and faculty members.
The program director must evaluate each resident’s abilities based on specific criteria and
when available, evaluation should be guided by specific national standards-based criteria.
Faculty members functioning as supervising physicians should delegate portions of care to
residents based on the needs of the patient and the skills of the residents.
Senior residents should serve in a supervisory role of junior residents in recognition of their
progress toward independence, based on needs of each patient and the skills of the
individual resident.
Programs must set guidelines for circumstances and events in which residents much
communicate with appropriate supervising faculty members, such as the transfer of a patient
to an intensive care unit, or end-of-life decisions.
Each resident must know the limits of his/her scope of authority and the circumstances under
which he/she is permitted to act with conditional independence.
In particular, PGY1 residents should be supervised either directly or indirectly with direct
supervision immediately available.
Faculty supervision assignments should be of sufficient duration to assess the knowledge
and skills of each resident and delegate to him/her the appropriate level of patient care
authority and responsibility.
APPENDIX L
NORTHERN CALIFORNIA
POLICY AND PROCEDURE
POLICY
SECTION: GME INSTITUTIONAL ADMINISTRATION
NUMBER:
IGMEC
TITLE
:
FUNDING AND SUPPORT FOR BOARD PREPARATION
COURSES
EFFECTIVE DATE:
February 10, 2016
CONTACT PERSON: Institutional Director of Graduate Medical Education
Approved By: IGMEC (2.10.16)
I. PURPOSE
To aide in the successful preparation and completion of the residents’ specialty specific board exam
the Institution may provide support and funding for an extra-mural board preparation course.
II. SCOPE
This policy applies to all Kaiser Permanente sponsored residents at the PGY2 Level and above.
III. POLICY
Kaiser Permanente sponsored residents will have the opportunity to take an extra-mural board
preparation course one time during their residency at the PGY2 Level or above. The Institution will
fund the cost of the course, expenses for travel and accommodations up to $1,500. Residents may
use their educational stipend towards the board preparation expense as well.
IV. PROCEDURE
In order for the course to be covered, residents are required to register and submit requests for
course payment and related expenses no later than May 1 of the PG year that the expenses were
incurred.
