Renee Campion
Commissioner
Daniel Pollak
First Deputy Commissioner
General Counsel
Office of Labor Relations
E
MPLOYEE
B
ENEFITS
P
ROGRAM
22 Cortlandt Street, 12th Floor, New York, NY 10007
nyc.gov/olr
Georgette Gestely
Director, Employee Benefits Program
Beth Kushner
Deputy Director, Administration
Sang Hong
Deputy Director, Operations
Michael Babette
Director, Financial Management Unit
Important Information Concerning Coverage Under COBRA in the State of New York
The attached information concerns coverage that may be available to you through the Federal
Consolidated Omnibus Reconciliation Act (“COBRA”) which provides access to continuing
health coverage for a period of 18 months to 36 months depending on the reason for COBRA
eligibility.
The State of New York enacted legislation intended to provide continued access to group
health insurance for all persons eligible for COBRA or state continuation (“mini-COBRA”)
coverage up to a total of 36 months of coverage. For more information concerning how this
may impact your coverage under COBRA please use the following link:
http://www.dfs.ny.gov/consumer/cobra_ext_36.htm
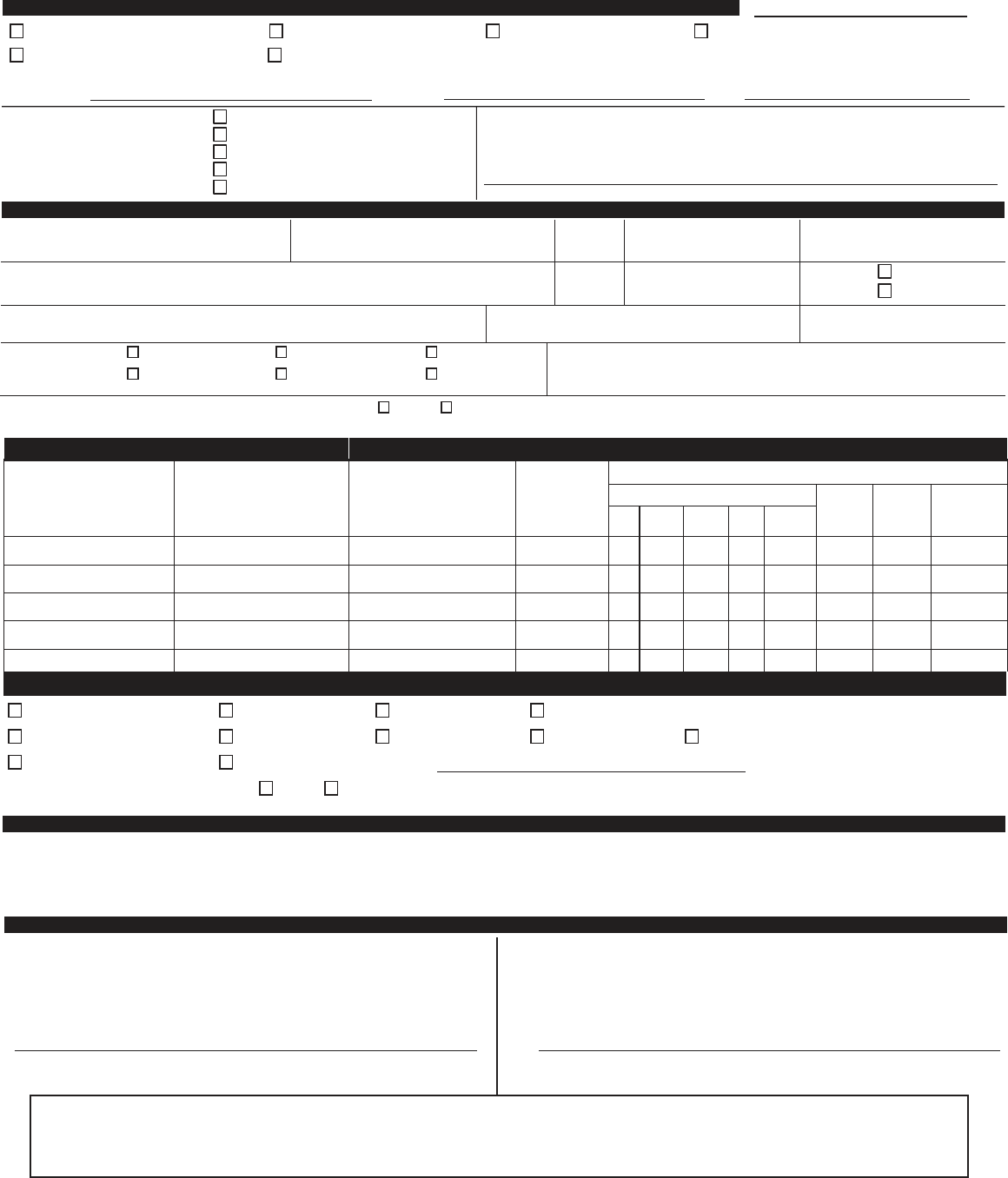
CITY OF NEW YORK EMPLOYEE BENEFITS PROGRAM
CONTINUATION OF COVERAGE APPLICATION
REASON
FOR
SUBMISSION
(PLEASE
PRINT
CLEARLY)
(CHECK ONE)
Date of Qualifying Event
/ /
Termination of Employment/Member Reduction of Work Schedule Divorce or Legal Separation Termination of Domestic Partnership
Death of Employee/Retiree
Present
or
former
Contract
Loss of Eligibility as a Dependent Child
Present
or
Former
Social
Secruity
Number:
Holder’s
Name:
Health
Plan:
Relationship to
Present or
Former Contract
Holder
Self
Spouse (former or current)
Domestic Partner
Son
Daughter
Present or Former City
Employee’s Welfare Fund:
APPLICANT
INFORMATION
(PLEASE
PRINT)
Last Name:
First Name:
M.I.:
Social Security Number:
Home Telephone #:
( )
Mailing Address:
Apt.:
Date of Birth:
Sex: Male
Female
City:
State:
Zip Code:
Marital Status: Married Single Widowed
Domestic Partner Legally Separated Divorced
Date of Marital Status Event:
/ /
Is
Applicant
or
Any
Dependent
Covered by
Medicare?
Yes
No
If
Yes, a
COPY
of
the
Medicare
Card
MUST
be attached.
FAMILY
INFORMATION
(PLEAS
E
LIST
ALL
PERSONS
TO
BE
CO
VERED,
INCLUDING
EMPLOYE
E
IF
APPLICABLE
(PLEASE
PRINT)
First Name
Last Name
Social Security
Number
Date of
Birth
Check if Applicable
Relationship
Full
Time
Student
Perm-
anently
Disabled
Covered by
Other Group
Insurance
Self
Spouse
Dom.
Partner
Son
Daughter
Aetna
EPO
Cigna
Health
DC
37
Med-Team
Empire
EPO
-
Nationwide
Empire
HMO
-
New
York
GHI-
CBP/EBCBS
GHI
HMO
HIP Prime
HMO
HIP
Prime
POS
MetroPlus
Vytra
Health
Plan
OTHER
Optional
Benefits
(Please
check
one):
Yes
No
WELFARE
FUND
- COBRA
Contact your your union or welfare fund directly for the necessary forms, available options and costs. You will pay
the union welfare fund directly for the
cost of these benefits.
AUTHORIZATION
I certify
that the above information is correct.
I fully
understand that I am responsible
for the full cost of my continuance of coverage and will be subject to the terms and
condictions of the group contract.
/ /
Applicant’s Signature Date
I choose to waive my rights to extend my current health coverage under COBRA.
I wish to convert to a direct payment policy.
Please send me a conversion contract.
/ /
Applicant’s Signature Date
ebpcobraform06302017.indd
THIS
NOTICE
MUST
BE
MAILED
DIRECTLY
TO
YOUR
HEALTH
PLAN
FOR
COBRA
CONTINUATION
COVERAGE
OR
FOR
DIRECT
PAYMENT
CONVERSION
(See
Plan
Description
for
address)
HEALTH PLAN REQUESTED (check the box before the plan you want and you must check “yes or no” for the optional rider benefits).
}

City of New York
Office of Labor Relations
Health Benefits Program
COBRA Premiums
Under the Federal Consolidated Omnibus Budget Reconciliation Act (COBRA), you have the opportunity to continue
health benefits coverage through the City of New York group.
You are responsible for paying the full premium for your plan and coverage. The premium levels indicated on the back of
this page reflect 102% of the current rate (because these rates are subject to change, you should check with the plan to
determine the premium at the time of your COBRA enrollment). Payments may be made monthly on the first of the
month. There is usually a 30 day grace period. The City will not "carve out" benefits provided through your Welfare Fund
that are similar to those available in your plan's Optional Rider. If you decide to purchase the Optional Rider, you must
pay for the entire Optional Rider offered by your chosen plan. If you decide to purchase any of your Welfare Fund
benefits, you should contact the Welfare Fund to determine what benefits are available, and the associated cost.
Health Plan Addresses
Payment should be mailed directly to the plan chosen for COBRA continuation coverage. The plan addresses are:
Aetna HealthCare
151 Farmington Ave.
Hartford, CT 06156
Attn: Michele Wrenn
CIGNA Healthcare
140 East 45th Street, 9th Fl
New York, NY 10017
Attn: Erika Larson
Engagement Consultant
DC 37 Med-Team
55 Water Street, 23
rd
Fl.
New York, NY 10041
Attn: Magaly Mendez-Bravo
Accounting Department
Empire BlueCross BlueShield
3 Huntington Quadrangle, 3 Fl.
Melville, NY 11747
Attn: Lashern Pendergast
GHI CBP\EBCBS*
GHI HMO
EmblemHealth
55 Water Street
New York, NY 10041
Attn: Membership Department
HIP HMO
HIP POS
EmblemHealth
55 Water Street
New York, New York 10041
Attn: Membership Department
MetroPlus Health Plan
50 Water Street, 7
th
Fl.
New York, NY 10004
Attn: COBRA/Finance Dept.
Vytra
EmblemHealth
55 Water Street
New York, NY 10041
Attn: Membership Department
*The GHI CBP/EBCBS is offered as package under COBRA. The premium should be sent to the EmblemHealth
address indicated above.
CONVERSION CONTRACTS - City Health Plan Benefits
If you do not wish to continue coverage under COBRA you may use the same application to request direct payment
conversion contracts from all plans. Conversion contract payments will be due quarterly. Upon receipt of an application
for conversion, the health plan will send you a direct payment contract and a bill. Generally, conversion contracts will be
more expensive than COBRA for the same benefits or will offer benefits less comprehensive than COBRA, with the
exception of certain Medicare supplemental contracts. Optional benefits are not available under conversion. You may
purchase either Group Health Inc. or Empire BlueCross BlueShield direct payment plan separately. Decide whether direct
payment conversion or COBRA continuation coverage is best to meet your needs. If you decide to continue coverage
under COBRA, you will again be eligible to obtain direct payment contracts when COBRA terminates. Contact the health
plan for more information concerning direct payment contracts.
Welfare Fund Benefits
Contact your welfare fund directly for COBRA rates. If you do not wish to continue coverage of benefits provided by your
welfare fund under COBRA, conversion to private coverage may be available for medical and life insurance benefits within
45 days of termination of coverage. If you intend to obtain welfare fund benefits under COBRA, please so indicate on the
COBRA Continuation of Coverage application.
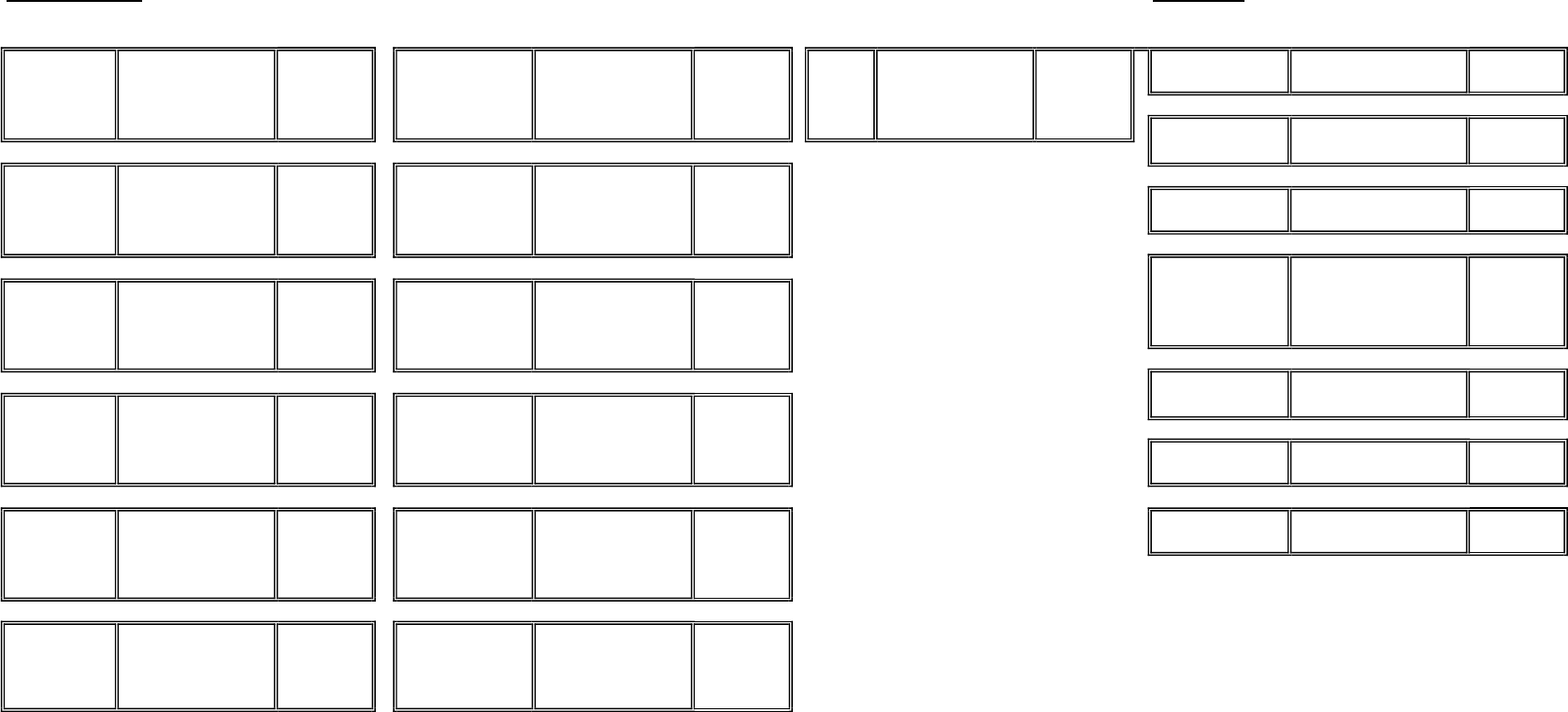
NON-MEDICARE
Monthly COBRA Rates for Effective October 2022
MEDICARE
Plans Monthly COBRA Rates for Effective January 2023
PLAN Coverage COBRA RATE PLAN Coverage COBRA RATE PLAN Coverage COBRA RATE PLAN Coverage COBRA RATE
INDIVIDUAL BASIC $1,395.85 INDIVIDUAL BASIC $937.68 INDIVIDUAL BASIC $1,147.38 PER PERSON BASIC $208.18
FAMILY BASIC $4,179.98 FAMILY BASIC $2,299.85 FAMILY BASIC $3,014.03 PER PERSON with RIDER $339.00
INDIVIDUAL with RIDER
$3,563.69
INDIVIDUAL with RIDER
$1,289.49
INDIVIDUAL with RIDER
$1,550.56
FAMILY with RIDER $10,311.34 FAMILY with RIDER $3,161.83 FAMILY with RIDER $4,062.95 PER PERSON BASIC $874.53
PER PERSON with RIDER $961.23
INDIVIDUAL BASIC $2,015.00 INDIVIDUAL BASIC $937.68
FAMILY BASIC $5,207.31 FAMILY BASIC $2,299.85 PER PERSON BASIC $220.72
INDIVIDUAL with RIDER
$2,351.49
INDIVIDUAL with RIDER
$1,047.87 RIDER NOT AVAILABLE
FAMILY with RIDER $6,225.70 FAMILY with RIDER $2,501.86
ONE PERSON BASIC $353.34
INDIVIDUAL BASIC $1,929.33 INDIVIDUAL BASIC $2,082.33 TWO PERSONS BASIC $498.49
FAMILY BASIC $4,824.32 FAMILY BASIC $5,104.24 ONE PERSON with RIDER $558.31
INDIVIDUAL with RIDER
$2,333.34
INDIVIDUAL with RIDER
$2,461.94 TWO PERSONS w/RIDER $908.43
FAMILY with RIDER $5,814.77 FAMILY with RIDER $6,034.30
PER PERSON BASIC $7.65
INDIVIDUAL BASIC $1,342.28 INDIVIDUAL BASIC $966.84 PER PERSON with RIDER $117.81
FAMILY BASIC $3,485.53 FAMILY BASIC $2,371.29
INDIVIDUAL with RIDER
$1,746.29 PER PERSON BASIC $28.05
FAMILY with RIDER $4,475.98 PER PERSON with RIDER $108.63
INDIVIDUAL BASIC $1,202.15 INDIVIDUAL BASIC $937.68 PER PERSON BASIC $7.65
FAMILY BASIC $3,062.14 FAMILY BASIC $2,299.85 PER PERSON with RIDER $188.79
INDIVIDUAL with RIDER
$1,674.99
INDIVIDUAL with RIDER
$1,222.23
FAMILY with RIDER $4,268.01 FAMILY with RIDER $3,011.22
Rates are Subject to Change
INDIVIDUAL BASIC $957.86 INDIVIDUAL BASIC $937.68
FAMILY BASIC $2,514.09 FAMILY BASIC $2,299.85
INDIVIDUAL with RIDER
$1,067.83
INDIVIDUAL with RIDER
$1,079.38
FAMILY with RIDER $2,715.68 FAMILY with RIDER $2,558.73
NOTE: If you were enrolled in a Medicare HMO you MUST
contact your health plan DIRECTLY for benefit and cost
information regarding continuation of coverage.
Return the completed COBRA form to your chosen plan. Addresses are listed on the front of this pamphlet. Wait for notification from the plan before
mailing in your first payment. Checks and/or money orders must be made payable to the health plan and mailed DIRECTLY to the plan. Enrollees of all
plans not listed must contact the plan DIRECTLY for enrollment options.
Aetna PPO/ESA
(NY/NJ/PA)
Aetna PPO/ESA
(All other areas)
GHI-CBP/BCBS
METROPLUS
(Grandfathered)
HIP VIP
METROPLUS
(Standard)
AETNA EPO
CIGNA
EMPIRE EPO
EMPIRE Blue
Access Gated
EPO
GHI HMO
GHI SENIOR CARE
GHI HMO Medicare
Senior Supplement
HIP HMO Gold
Preferred Plan
(Grandfathered)
HIP PRIME POS
DC 37 MED TEAM
(no rider available)
DC37 MED TEAM
EMPIRE
MEDICARE
RELATED
HIP HMO Gold
Preferred Plan
(Standard)
VYTRA

City of New York
Office of Labor Relations
Health Benefits Program
Notice of Rights
WHEN YOUR HEALTH BENEFITS TERMINATE
The Consolidated Omnibus Budget Reconciliation Act (Public Law 99-2721, Title X), also known as
COBRA, was enacted April 7, 1986. This law requires that, effective July 1, 1987, in addition to offering
normal conversion opportunities, the City and the union welfare funds must offer employees and their
families the opportunity for a temporary extension of group health and welfare fund coverage (called
“continuation of coverage”) at 102% of the group rates, in certain situations in which benefits under either
City basic or the applicable welfare fund would be reduced or terminated. This notice is intended to inform
you of your rights and obligations under the continuation coverage provisions of this law as well as your
normal conversion option.
As a result of collective bargaining agreements, Medicare-eligible enrollees and/or their Medicare-
eligible dependents will be offered continuation benefits similar to COBRA if a COBRA event should occur.
(See Medicare-Eligible Section.)
Employees
All City group health benefits including the optional benefits riders are available under COBRA
continuation coverage. Welfare fund benefits eligible for continuation under COBRA are dental, vision,
prescription drugs and other related medical benefits. Welfare funds offer core benefits (prescription drugs
and major medical plans) and non-core benefits (dental and vision) which may be purchased separately or
combined with City core benefits.
If you are a non-Medicare-eligible employee covered by the City program, you have the right, in
certain situations, to continue benefits if you lose your coverage because of a reduction in your hours of
employment; or upon the termination of your employment (for reasons other than gross misconduct on your
part); or if you take an unpaid leave of absence. If you are Medicare-eligible, you may be entitled to
continuation of coverage as is described in the Medicare-eligible section below.
Retirees
You and your dependents are eligible to receive City-paid health care coverage if you have, at the
time of retirement:
a.
Ten (10) years of credited service as a member of a retirement or pension system maintained by
the City (if you were an employee of the City on or before December 27, 2001, then at the time of your
retirement you must have at least five (5) years of credited service as a member of a retirement or pension
system maintained by the City). This requirement does not apply if you retire because of accidental disability;
and
b.
You have been employed by the City immediately prior to retirement as a member of such
system, and have worked regularly for at least 20 hours per week; and
c.
You receive a pension check from a retirement system maintained by the City.
If you do not meet these eligibility requirements, you and your dependents (if not Medicare-eligible)
may continue under COBRA the benefits you received as an active employee, for a period of 18 months at
102% of the City’s cost. If your welfare fund benefits are reduced at retirement, you are eligible to continue
those benefits that were reduced under the welfare fund as a COBRA enrollee for a period of 18 months at
102% of the cost to the union welfare fund. You should contact your union welfare fund for the premium
amounts and benefits available.
Spouse/Domestic Partners and Dependents
If you are the non-Medicare-eligible spouse/domestic partner of an eligible employee or a retiree,
you have the right to continue coverage under any of the available NYC health benefits plans and the
applicable welfare funds if your health insurance or welfare fund benefits are reduced or terminated for any
of the following reasons:
1)
The death of your spouse/domestic partner;
2
2)
The termination of your spouse/domestic partner's employment (for reasons other than gross
misconduct) or reduction in your spouse/domestic partner's hours of employment;
3)
Divorce or legal separation from your spouse.
In the case of an eligible dependent child of an employee or retiree (including a newborn child who
was born to the covered beneficiary or an adopted child who is placed for adoption with the covered
beneficiary during a period of COBRA continuation coverage) he or she has the right to continue coverage
under any of the available NYC health benefits plans and the applicable welfare fund if coverage is reduced
or terminated for any of the following reasons:
1)
The death of the covered parent;
2)
The termination of the covered parent’s employment (for reasons other than gross
misconduct) or reduction in the parent’s hours of employment;
3)
The dependent ceases to be a “dependent child” under the terms of the Employee
Benefits Program;
4)
Retirement of the covered parent (see “Retiree” above).
If you are a Medicare-eligible spouse/domestic partner or dependent, see section on Medicare-eligible's.
Disabled Persons
If a disability has led to Medicare eligibility, see section on Medicare-eligibles below.
Covered persons who are disabled, under the definition established by the Social Security law, up to
60 days after the COBRA qualifying event of termination of employment or reduction of hours, are entitled to
continue coverage for up to a total of twenty-nine (29) months from the date of the initial qualifying event.
The cost of coverage during the last eleven (11) months of this extended period is one hundred and fifty
percent (150%) of the City cost for the benefit. Persons so disabled must inform the health plan within sixty
(60) days of the disability determination and within thirty (30) days of disability ceasing.
Medicare-
Eligibles
Employees, retirees, spouses/domestic partners and dependents who are eligible for Medicare may
be eligible to receive continued coverage, similar to COBRA, under the City’s Medicare-Supplemental plans.
Periods of eligibility shall date from the original qualifying event up to eighteen (18) months in the case of
loss of coverage because of termination of employment or reduction in hours, or up to thirty-six (36) months
in the case of loss of coverage for all other reasons.
If a COBRA qualifying event occurs and you lose coverage, but you and/or your dependents are
Medicare-eligible, you may continue coverage by using the COBRA Continuation of Coverage application
form. You should indicate your Medicare claim number and effective dates where indicated on the form for
Medicare-eligible family members. If you and/or your dependents are about to become eligible for
Medicare, and are already continuing coverage under COBRA, inform the carrier of Medicare eligibility for
you and/or your dependents, at least thirty (30) days prior to date of Medicare eligibility. COBRA-
enrolled dependents of the person who becomes Medicare eligible will be able to continue their COBRA
coverage, whether or not the Medicare-eligible person enrolls in the Medicare-Supplemental coverage. The
COBRA continuation period for dependents will be unaffected by the decision of the Medicare-eligible
employee or retiree.
NOTE: You should contact your carrier for information about other Medicare-Supplemental plans which are
offered; some other plans may be better suited to your needs and/or less costly than the plan which is
provided under the City’s contract.
3
Notice
Under the law you have sixty (60) days from the date you receive this notice to elect continuation
coverage for your City basic and/or optional benefits. Contact your welfare fund administrator for further
instructions on how to continue your welfare fund benefits. Payments of the initial monthly premium may
accompany the enclosed Continuation of Coverage Application opting for continuation. However, under the
law you have a grace period of 45 days from the date you applied for COBRA coverage to pay the premium.
You will receive a partial bill for any remaining portion of the following calendar month to bring your billing
date to the first of the month. All subsequent bills will be charged from the first day of the month during your
COBRA continuation period. Payment shall be on a monthly basis. There is a 30-day grace period for
subsequent late payments.
If you choose COBRA continuation coverage, and you are not Medicare-eligible, the City is required to
offer you the same coverage which is provided to similarly situated employees, retirees or family members.
The law requires that you be afforded the opportunity to maintain continuation coverage for a maximum of
thirty-six (36) months unless you lost coverage because of a termination of employment or reduction in
hours. In the latter case, the required continuation coverage period is a maximum of 18 months. The
maximum period of continuation begins on the first day of the month following the month in which the initial
qualifying event occurred, regardless of when any additional events may take place. However, the law also
provides that your continuation of coverage may be cut short for any of the following reasons:
1)
The premium for continuation coverage is not paid in a timely fashion;
2)
The continuation enrollee becomes covered as an employee or dependent under another
group health or welfare plan (under this occurrence the spouse and dependents may
continue their COBRA coverage for the remaining months of eligibility).
NOTE: If the new plan contains any exclusion or limitation for a pre-existing condition of the continuation
enrollee, then coverage may not be terminated.
You do not have to show that you are insurable to choose continuation coverage. However, under
the law, you have to pay 102% of the cost of benefits for the continuation coverage. Also, at the end of the
continuation period you are allowed to convert to a self-paid direct payment policy.
Conversion Options
If you do not choose continuation, your City group coverage will end. You will still be offered the
opportunity to convert your City health insurance benefits to a non-City direct payment health insurance
policy and, where applicable, convert certain welfare fund benefits. Benefits offered under the non-City group
direct payment health insurance policy are offered on a quarterly basis for an indefinite period of time,
provided premiums are paid on time. These benefits may vary from the City's "basic" health benefits package
in terms of scope of benefits and cost. Benefits available from welfare funds that may be converted to direct
payment are insured medical/ surgical/ hospital and life insurance coverage. Such benefits may be
converted within 45 days of termination of coverage.
In order to receive continuation coverage for welfare fund benefits or to convert to direct payment,
you must contact your welfare fund directly.
For further information about this law, employees should contact their agency benefits representative
and retirees should e-mail the Health Benefits Program at healthbenefits@olr.nyc.gov
4
