ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 1 of 16
Completion Instructions Date: 2022Feb11
Introduction
The ADA’s Council on Dental Benefit Programs has responsibility for electronic and paper dental claim
content and completion instructions. Staff from the Center for Dental Benefits, Coding and Quality
within the ADA’s Practice Institute maintain the paper ADA Dental Claim Form and its completion
instructions. According to ADA policy the paper form’s data content must be in harmony with the
HIPAA standard electronic dental claim transaction.
The ADA Dental Claim Form was last structurally revised in 2012 to incorporate key data content
changes that enables diagnosis code reporting that was also incorporated into the now current version
of the HIPAA standard (837D v5010) electronic dental claim. This version of the ADA form incorporates
editorial changes to further its consistency with the 837D.
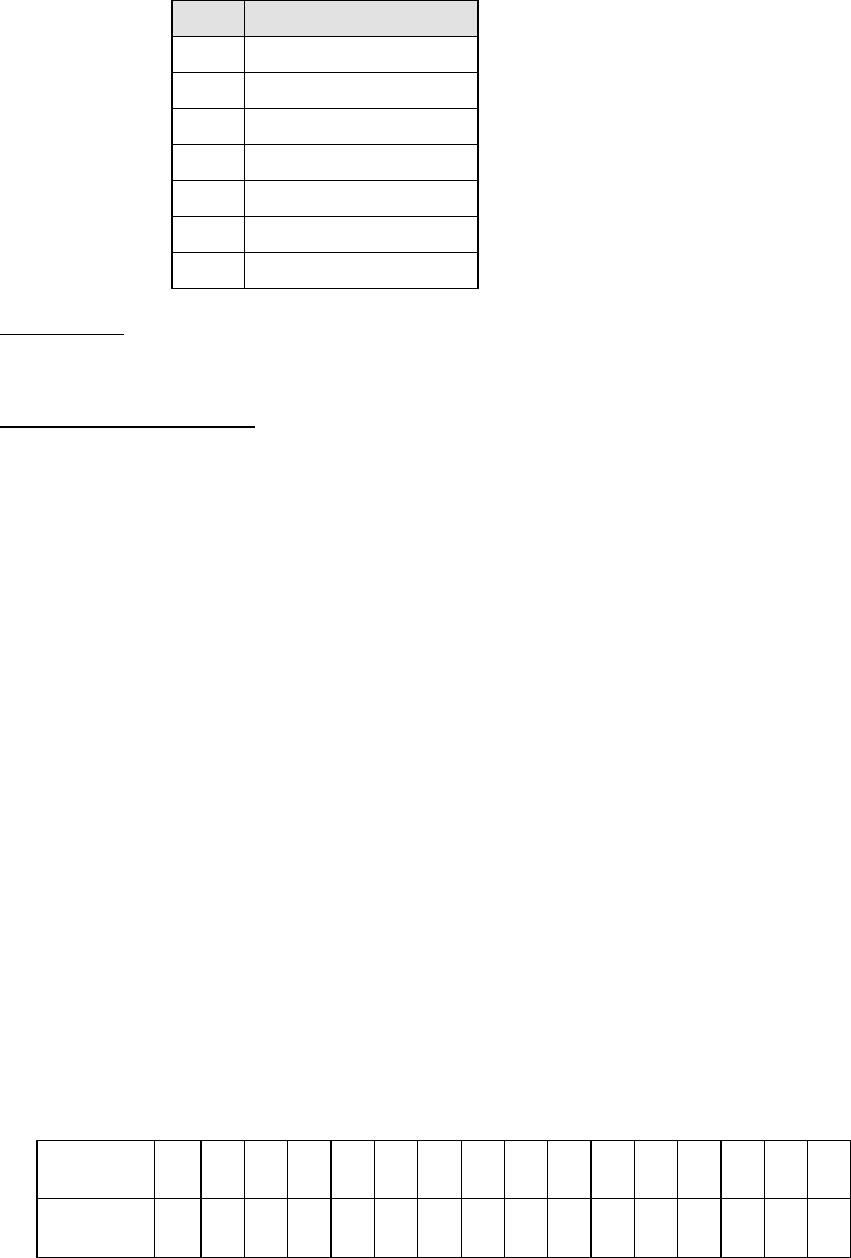
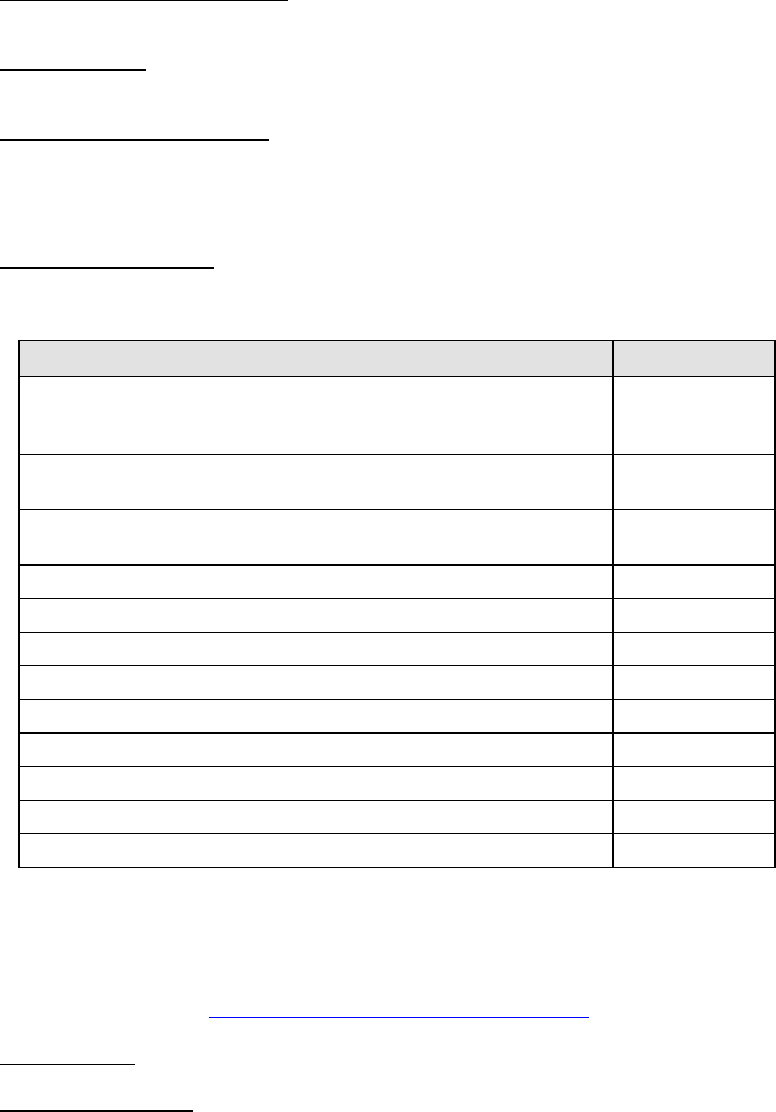
Summary of Form Version 2019 Editorial and Completion Instruction Changes
Change Description
Affected Form
# Field Name
Consistent completion instruction captions for these fields.
8
15
Policyholder/Subscriber
Identifier
Changed from two check boxes, one for Male (M) and another for
Female (F), to three with the third being a box for Unknown (U).
7
14
22
Gender
Addition of NOTE that points to other online guidance on when
this information is reported.
25 Area of Oral Cavity
Consistent instructions for reporting procedures involving multiple
teeth
27 Tooth Numbers or Letters
Addition of NOTE to clarify that tooth numbers are based on
morphology, not anatomic location.
27
33
35
Tooth Numbers or Letters
Missing Teeth
Remarks
Removal of coding option “B” as it applies to an ICD-10-CM
version that is no longer valid for use.
34 Diagnosis Code List Qualifier
Addition of clarifying NOTE that: a) addresses when this
information would be reported; and b) refers to other online
guidance for completion when this information is reported.
34
34a
Diagnosis Code List Qualifier
Diagnosis Code(s)
Additional information concerning completion when teledentistry
procedure code is reported.
38
56
Place of Service Code
Treatment Location Address
The current version of the paper form (2019 © American Dental Association), front and reverse sides, is
illustrated on the
next two pages. The illustrations are then followed by comprehensive form completion
instructions.

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 2 of 16
Completion Instructions Date: 2022Feb11

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 3 of 16
Completion Instructions Date: 2022Feb11

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 4 of 16
Completion Instructions Date: 2022Feb11
DATA ELEMENT SPECIFIC INSTRUCTIONS
Form completion instructions are provided for each data item, which is indicated by a number. Please
note that data items are in groups of related information. These instructions explain the reasons for
such groupings, and the relationships (if any) between groups.
Header Information
The ‘header’ provides information about the type of submission being made. This information applies
to the entire transaction.
1.
Type of Transaction: There are three boxes that may apply to this submission. If services have
been performed, mark the “Statement of Actual Services” box. If there are no dates of service,
mark the box marked “Request for Predetermination / Preauthorization”. If the claim is through
the Early and Periodic Screening, Diagnosis and Treatment Program, mark the box marked
‘EPSDT/Title XIX’.
2.
Predetermination/Preauthorization Number: If you are submitting a claim for a procedure that has
been pre-authorized by a third party payer, enter the preauthorization or predetermination number
provided by the insurance company.
Insurance Company/Dental Benefit Plan Information
3.
Company/Plan Name, Address, City, State, Zip Code: This Item is always completed. Enter the
information for the insurance company or dental benefit plan that is the third party payer receiving
the claim.
•
If the patient is covered by more than one plan, enter the primary insurance company
information here for the initial claim submission.
•
When submitting a separate claim to the secondary carrier, place the secondary carrier’s
company/plan name and address information here.
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 5 of 16
Completion Instructions Date: 2022Feb11
Other Coverage
This area of the claim form provides information on the existence of additional dental or medical
insurance policies. This is necessary to determine if multiple coverages are in effect, and the possibility of
coordination of benefits.
•
When the claim form is being prepared for submission to the primary carrier the information in
“Other Coverage” applies to the secondary carrier.
•
When the claim form is being prepared for submission to the secondary carrier the information in
“Other Coverage” applies to the primary carrier.
4.
Other Dental or Medical Coverage?: Mark the box after “Dental?” or “Medical?” whenever a
patient has coverage under any other dental or medical plan, without regard to whether the
dentist or the patient will be submitting a claim to collect benefits under the other coverage.
• Leave blank when the dentist is not aware of any other coverage(s).
• When either box is marked, complete Items 5 through 11 in the “Other Coverage” section
for the applicable benefit plan.
• If both Dental and Medical are marked, enter information about the dental benefit plan in
Items 5 through 11.
5.
Name of Policyholder/Subscriber with Other Coverage Indicated in #4 (Last, First, Middle Initial,
Suffix): If the patient has other coverage through a spouse, domestic partner or, if a child, through
both parents, the name of the person who has the other coverage is reported here.
6.
Date of Birth (MM/DD/CCYY): Enter the date of birth of the person listed in Item #5. The date
must be entered with two digits each for the month and day, and four digits for the year of birth.
7.
Gender: Mark the gender of the person who is listed in Item #5. Mark “M” for Male, “F” for
Female, or “U” for Unknown as applicable.
8.
Policyholder/Subscriber Identifier (Assigned by Plan): Enter the unique identifying number
assigned by the third-party payer (e.g., insurance company) to the person named in Item #5,
which is on their identification card.
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 6 of 16
Completion Instructions Date: 2022Feb11
9.
Plan/Group Number: Enter the group plan or policy number of the person identified in Item #5.
10.
Patient’s Relationship to Person Named in Item #5: Mark the patient’s relationship to the other
insured named in Item #5.
11.
Other Insurance Company/Dental Benefit Plan Name, Address, City, State, Zip Code: Enter the
complete information of the additional payer, benefit plan or entity for the insured named in Item
#5.
Policyholder/Subscriber Information (For Insurance Company Named in Item #3)
This section documents information about the insured person who may or may not be the patient.
•
When the claim form is being prepared for submission to the primary carrier the information
supplied applies to the person insured by the primary carrier.
•
When the claim form is being prepared for submission to the secondary carrier the information
entered applies to the person insured by secondary carrier.
12.
Policyholder/Subscriber Name (Last, First, Middle Initial, Suffix), Address, City, State, Zip Code:
Enter the complete name, address and zip code of the policyholder/subscriber with coverage
from the company/plan named in #3.
13.
Date of Birth (MM/DD/CCYY): A total of eight digits are required in this field; two for the month,
two for the day of the month, and four for the year.
14.
Gender: This applies to the primary insured, who may or may not be the patient. Mark “M” for
Male, “F” for Female, or “U” for Unknown as applicable.
15.
Policyholder/Subscriber Identifier (Assigned by Plan): Enter the unique identifying number
assigned by the third-party payer (e.g., insurance company) to the person named in Item #12,
which is on their identification card.
16.
Plan/Group Number: Enter the policyholder/subscriber’s group plan/policy number.
17.
Employer Name: If applicable, enter the name of the policyholder/subscriber’s employer.

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 7 of 16
Completion Instructions Date: 2022Feb11
Patient Information
The information in this section of the claim form pertains to the patient.
18.
Relationship to Policyholder/Subscriber in #12 Above: Mark the relationship of the patient to the
person identified in Item #12 who has the primary insurance coverage. The relationship between
the insured and the patient may affect the patient’s eligibility or benefits available. If the patient
is also the primary insured, mark the box titled ‘Self’ and skip to item #23.
19.
Reserved For Future Use: Leave blank and skip to Item #20. (#19 was previously used to report
“Student Status.”)
20.
Name (Last, First, Middle Initial, Suffix), Address, City, State, Zip Code: Enter the complete name,
address and zip code of the patient.
21.
Date of Birth (MM/DD/CCYY): A total of eight digits are required in this field; two for the month,
two for the day of the month, and four for the year of birth of the patient.
22.
Gender: This applies to the patient. Mark “M” for Male, “F” for Female, or “U” for Unknown as
applicable.
23.
Patient ID/Account # (Assigned by Dentist): Enter if the dentist’s office has assigned a number to
identify the patient. This is not required to process claim.
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 8 of 16
Completion Instructions Date: 2022Feb11
Record Of Services Provided
This section contains information regarding the proposed treatment (predetermination/preauthorization),
or treatment performed (actual services).
NOTE: Items 24 through 31, following, apply to each of the 10 available lines on the claim form for
reporting dental procedures provided to the patient. The remaining Items in this section of the form
(33-35) do not repeat.
24.
Procedure Date (MM/DD/CCYY): Enter procedure date for actual services performed or leave
blank if the claim is for preauthorization/predetermination. The date, if included, must have two
digits for the month, two for the day, and four for the year.
The presence or absence of a Procedure Date should be consistent with the type of
transaction(s) marked in Item #1 (e.g., actual services; predetermination / preauthorization).
25.
Area of Oral Cavity: Use of this field is conditional. Always report the area of the oral cavity
when the procedure reported in Item #29 (Procedure Code) refers to a quadrant or arch and the
area of the oral cavity is not uniquely defined by the procedure’s nomenclature. For example:
a.
Report the applicable area of the oral cavity when the procedure code nomenclature includes
a general reference to an arch or quadrant, such as D4263 bone replacement graft – first
site in quadrant
b.
Do not report the applicable area of the oral cavity when the procedure either: 1) incorporates
a specific area of the oral cavity in its nomenclature, such as D5110 complete denture –
maxillary; or 2) does not relate to any portion of the oral cavity, such as D9222 deep
sedation/general anesthesia – first 15 minutes.
NOTE: Detailed guidance on reporting Area of the Oral Cavity, Tooth Numbers and
Tooth Surfaces by CDT code is posted on the ADA Dental Claim Form web
page –
ADA Dental Claim Form
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 9 of 16
Completion Instructions Date: 2022Feb11
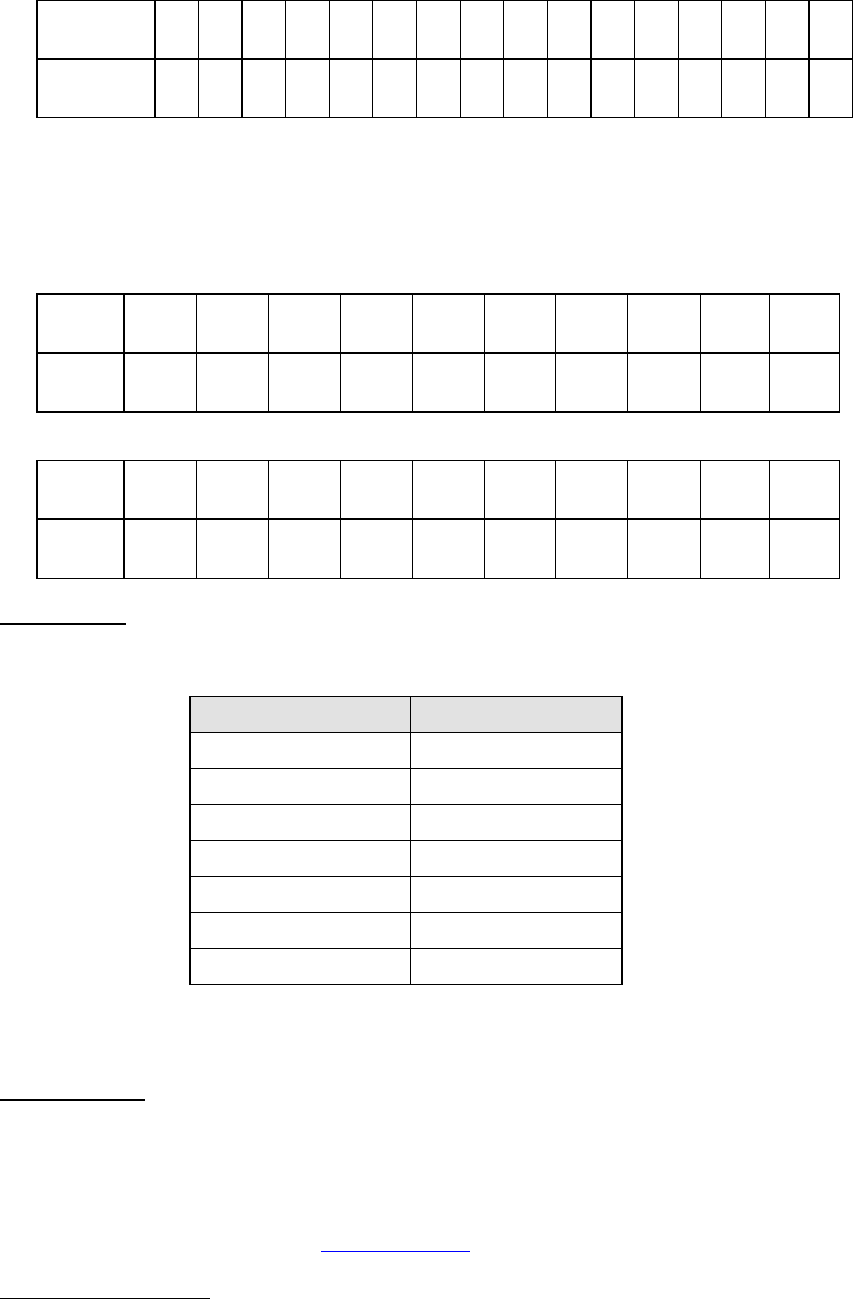
Area of the oral cavity is designated by a two-digit code, selected from the following code list:
Code Area
00 entire oral cavity
01 maxillary arch
02 mandibular arch
10 upper right quadrant
20 upper left quadrant
30 lower left quadrant
40 lower right quadrant
26.
Tooth System: Enter “JP” to indicate that teeth are being designated using the ADA’s
Universal/National Tooth Designation System (1-32 for permanent dentition and A-T for primary
dentition).
27.
Tooth Number(s) or Letter(s): Enter the appropriate tooth number or letter when the
procedure directly involves a tooth or range of teeth. Otherwise, leave blank.
NOTE: Numbers or letters reported are based on tooth morphology, not anatomic
position. This is the traditional and important concept to understand for
accurate documentation and reporting. For instance, a tooth may migrate
into an edentulous space, but that movement does not change its
morphology. Similarly, placement of an implant body need not be in an
anatomic tooth position, but the prosthesis placed is the morphological
equivalent of a missing tooth or range of teeth.
If the same procedure is performed on more than a single tooth on the same date of service there
are two options for reporting –
• Report each procedure, the tooth involved, and the fee on separate service lines
• Report the procedure on a single service line with the teeth involved in #27, the number
of times the procedure was delivered in the #29b (Quantity), and the total fee for all in
#31 (Fee)
When a procedure involves a range of teeth, the range is reported in this field. This is done either
with a hyphen “-” to separate the first and last tooth in the range (e.g., 1-4; 7-10; 22-27), or by the
use of commas to separate individual tooth numbers or ranges (e.g., 1, 2, 4, 7-10; 3-5, 22-27).
Supernumerary teeth in the permanent dentition are identified in the ADA’s Universal/National
Tooth Designation System (“JP”) by the numbers 51 through 82, beginning with the area of the
upper right third molar, following around the upper arch and continuing on the lower arch to the
area of the lower right third molar (for example, supernumerary number 51 is adjacent to the
upper right molar number 1; supernumerary number 82 is adjacent to the lower right third molar
number 32). This enumeration is illustrated in the following chart:
Upper Arch (commencing in the upper right quadrant and rotating counterclockwise)
Tooth # 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16
‘Super’ # 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 10 of 16
Completion Instructions Date: 2022Feb11
Lower Arch
Tooth # 32 31 30 29 28 27 26 25 24 23 22 21 20 19 18 17
‘Super’ # 82 81 80 79 78 77 76 75 74 73 72 71 70 69 68 67
Supernumerary teeth in the primary dentition are identified by the placement of the letter "S"
following the letter identifying the adjacent primary tooth (for example, supernumerary "AS" is
adjacent to "A"; supernumerary "TS" is adjacent to "T"). This enumeration is illustrated in the
following chart:
Upper Arch (commencing in the upper right quadrant and rotating counterclockwise)
Tooth # A B C D E F G H I J
‘Super’#
AS BS CS DS ES FS GS HS IS JS
Lower Arch
Tooth “#”
T S R Q P O N M L K
Super “#”
TS SS RS QS PS OS NS MS LS KS
28.
Tooth Surface: This Item is necessary when the procedure performed by tooth involves one or
more tooth surfaces. Otherwise leave blank. The following single letter codes are used to identify
surfaces:
Surface Code
Buccal B
Distal D
Facial (or labial) F
Incisal I
Lingual L
Mesial M
Occlusal O
Do not leave any spaces between surface designations in multiple surface restorations (e.g.,
MOD).
29.
Procedure Code: Enter the appropriate procedure code found in the version of the Code
on Dental Procedures and Nomenclature in effect on the “Procedure Date” (Item #24).
NOTE: Additional guidance concerning reporting select CDT codes (e.g.,
Teledentistry; Sales Tax) are in Coding Education and the ADA Claim Form
content linked to the CDT Code Portal web page –
www.ada.org/cdt
29a Diagnosis Code Pointer: Enter the letter(s) from Item 34 that identify the diagnosis code(s)
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 11 of 16
Completion Instructions Date: 2022Feb11
applicable to the dental procedure. List the primary diagnosis pointer first.
29b Quantity: Enter the number of times (01-99) the procedure identified in Item 29 is delivered to the
patient on the date of service shown in Item 24. The default value is “01.”
30.
Description: Provide a brief description of the service provided (e.g., abbreviation of the
procedure code’s nomenclature).
31.
Fee: Report the dentist’s full fee for the procedure. Resolution 44-2009 Statement on Reporting
Fees on Dental Claims adopted by the ADA House of Delegates, as follows, provides guidance
on the appropriate entry for this item.
Statement on Reporting Fees on Dental Claims
1)
A full fee is the fee for a service that is set by the dentist, which reflects the costs of
providing the procedure and the value of the dentist’s professional judgment.
2)
A contractual relationship does not change the dentist’s full fee.
3)
It is always appropriate to report the full fee for each service reported to a third-party
payer.
(Note: Item 31 above is the last of the repeating ‘service line’ items.)
31a Other Fee(s): When other charges applicable to dental services provided must be reported, enter
the amount here. Charges may include state tax and other charges imposed by regulatory
bodies.
32.
Total Fee: The sum of all fees from lines in Item #31, plus any fee(s) entered in Item #31a
33.
Missing Teeth Information: Mark an “X” on the number of the missing tooth – for identifying
missing permanent dentition only. Report missing teeth when pertinent to Periodontal,
Prosthodontic (fixed and removable), or Implant Services procedures on a particular claim
NOTE: Numbers marked are based on tooth morphology, not anatomic position.
34.
Diagnosis Code List Qualifier: Enter the appropriate code to identify the diagnosis code source:
AB = ICD-10-CM
34a Diagnosis Code(s): Enter up to four applicable diagnosis codes after each letter (A. – D.). The
primary diagnosis code is entered adjacent to the letter “A.”
NOTE: #34 and #34a are required when a) the diagnosis may have an impact on the
adjudication of the claim in cases where specific dental procedures may
minimize the risks associated with the connection between the patient’s oral
and systemic health conditions; or b) when required by state regulation (e.g.,
Medicaid) or third-party payer contract provisions.
Detailed guidance on reporting ICD-10-CM diagnosis codes is posted on the
ADA Dental Claim Form web page –
ICD Reporting on ADA Dental Claim Form
35.
Remarks: This space may be used to convey additional information for a procedure code that
requires a report, or for multiple supernumerary teeth. It can also be used to convey additional
information you believe is necessary for the payer to process the claim (e.g., for a secondary
claim, the amount the primary carrier paid).
Remarks should be concise and pertinent to the claim submission. Claimants should note that an
entry in “Remarks” may prompt review by a person as part of claim adjudication, which may affect
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 12 of 16
Completion Instructions Date: 2022Feb11
overall time required to process the claim.
NOTE: When the claim is for a multi-unit implant supported prosthesis the supporting
implant body locations may not correlate to the anatomic location of a natural
tooth. An appropriate notation in “Remarks” may avoid a misunderstanding
when the claim is submitted to a third-party payer.
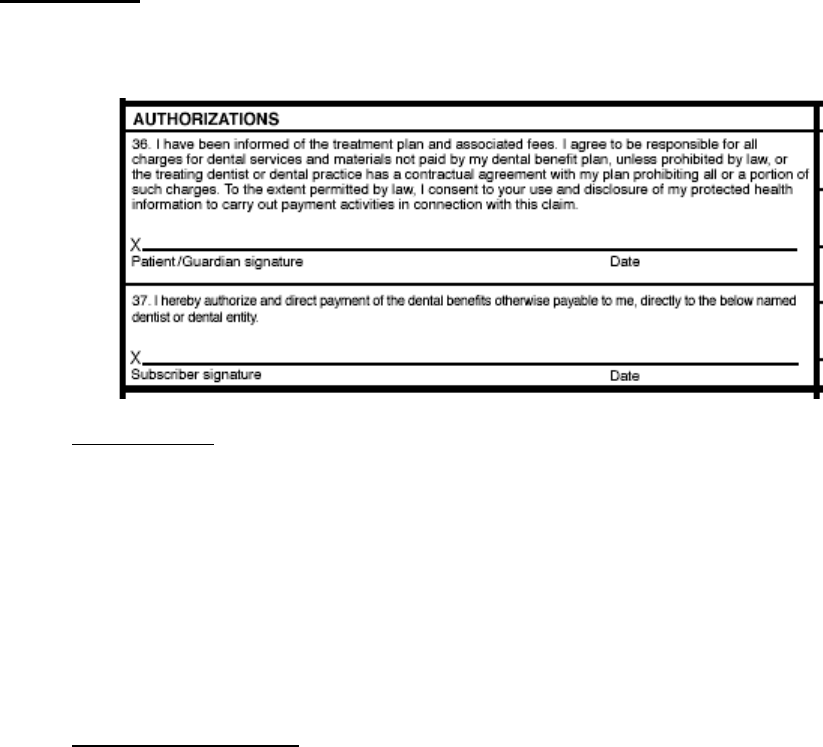
Authorizations
This section provides consent for treatment as well as permission for the payer to send any patient
benefit available for procedures performed directly to the dentist or the dental business entity.
36.
Patient Consent: The patient is defined as an individual who has established a professional
relationship with the dentist for the delivery of dental health care. For matters relating to
communication of information and consent, the term includes the patient’s parent, caretaker,
guardian, or other individual as appropriate under state law and the circumstances of the case.
By signing (or “Signature on File” notice) in this location of the claim form, the patient or patient’s
representative has agreed that he/she has been informed of the treatment plan, the costs of
treatment and the release of any information necessary to carry out payment activities related to
the claim.
Claim forms prepared by the dentist’s practice management software may insert “Signature on
File” when applicable in this Item.
37.
Authorize Direct Payment: The signature and date (or “Signature on File” notice) are required
when the Policyholder/Subscriber named in Item #12 wishes to have benefits paid directly to the
dentist/provider. This is an authorization of payment. It does not create a contractual relationship
between the dentist or dental entity and the insurance company.
Claim forms prepared by the dentist’s practice management software may insert “Signature on
File” when applicable in this Item.

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 13 of 16
Completion Instructions Date: 2022Feb11
Ancillary Claim/Treatment Information
This section of the claim form provides additional information to the third party payer regarding the claim.
38. Place of Treatment: Enter the 2-digit Place of Service Code for Professional Claims, a
HIPAA standard. Frequently used codes are:
11 = Office; 12 = Home; 21 = Inpatient Hospital; 22 = Outpatient Hospital; 31 =
Skilled Nursing Facility; 32 = Nursing Facility; 02 = Telehealth (aka Teledentistry)
All current codes are available online from the Centers for Medicare and Medicaid Services in
PDF format for download –
CMS Place of Service Code Set
39. Number of Enclosures (00 to 99): Enter a “Y” or “N” to indicate whether or not there are
enclosures of any type included with the claim submission (e.g., radiographs, oral
images, models)
.
40.
Is Treatment for Orthodontics?: If no, skip to Item #43. If yes, answer Items 41 & 42.
41.
Date Appliance Placed (MM/DD/CCYY): Indicate the date an orthodontic appliance was placed.
This information should also be reported in this section for subsequent orthodontic visits.
42.
Months of Treatment: Enter the total number of months required to complete the orthodontic
treatment, from the beginning to the end of the treatment plan.
43.
Replacement of Prosthesis?: This Item applies to Crowns and all Fixed or Removable Prostheses
(e.g., bridges and dentures).
Please review the following three situations in order to determine how to complete this Item.
a)
If the claim does not involve a prosthetic restoration mark “NO” and proceed to Item
45.
b)
If the claim is for the initial placement of a crown, or a fixed or removable prosthesis,
mark “NO” and proceed to Item 45.
c)
If the patient has previously had these teeth replaced by a crown, or a fixed or
removable prosthesis, or the claim is to replace an existing crown, mark the “YES”
field and complete section 44.
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 14 of 16
Completion Instructions Date: 2022Feb11
44.
Date of Prior Placement (MM/DD/CCYY): Complete if the answer to Item #43 was “YES.”
45.
Treatment Resulting From: If the dental treatment listed on the claim was provided as a result of
an accident or injury, mark the appropriate box in this item, and proceed to Items #46 and #47. If
the services you are providing are not the result of an accident, this Item does not apply;
skip to Item #48.
46.
Date of Accident (MM/DD/CCYY): Enter the date on which the accident noted in Item #45
occurred. Otherwise, leave blank.
47.
Auto Accident State: Enter the state in which the auto accident noted in Item #45 occurred.
Otherwise, leave blank.
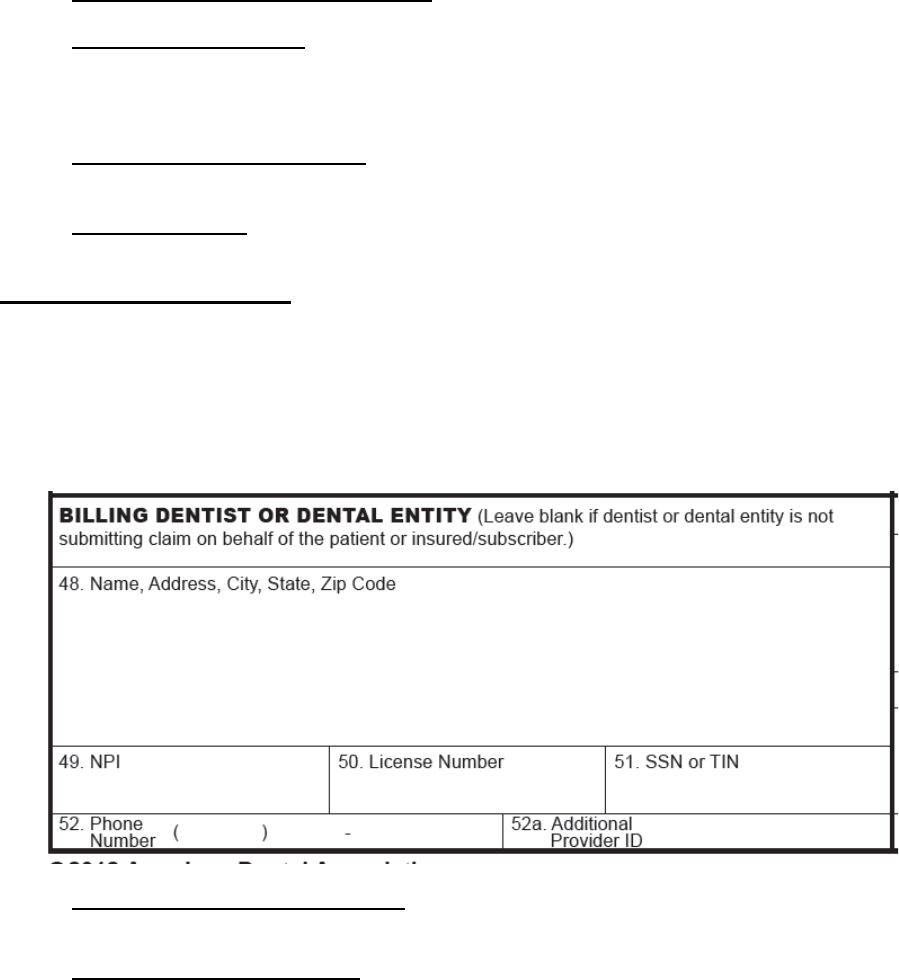
Billing Dentist Or Dental Entity
The ‘Billing Dentist’ or ‘Dental Entity’ section provides information on the individual dentist’s name, the
name of the practitioner providing care within the scope of their state licensure, or the name of the group
practice/corporation that is responsible for billing and other pertinent information. Depending on the
business relationship of the practice and the treating dentist, the information provided in this section may
not be the treating dentist. If the patient is submitting the claim directly, do not complete Items 48-
52a.
48.
Name, Address, City, State, Zip Code: Enter the name and complete address of a dentist or the
dental entity (corporation, group, etc.).
49.
NPI (National Provider Identifier): Enter the appropriate NPI type for the billing entity. A Type 2
NPI is entered when the claim is being submitted by an incorporated individual, group practice or
similar legally recognized entity. Unincorporated practices may enter the individual practitioners
Type 1 NPI.
NOTE: The NPI is an identifier assigned by the Federal government to all providers
considered to be HIPAA covered entities. Dentists who are not covered entities may
elect to obtain an NPI at their discretion, or may be enumerated if required by a
participating provider agreement with a third-party payer, or applicable state
law/regulation.
An NPI is unique to an individual dentist or dental entity, and has no intrinsic meaning.
There
are two types of NPI available to dentists and dental practices:
• Type 1 Individual Provider - All individual dentists are eligible to apply for Type 1

ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 15 of 16
Completion Instructions Date: 2022Feb11
NPIs, regardless of whether they are covered by HIPAA.
• Type 2 Organization Provider - A health care provider that is an organization, such
as
a group practice or corporation. Individual dentists who are incorporated may
enumerate as Type 2 providers, in addition to being enumerated as a Type 1. All
incorporated dental practices and group practices are eligible for enumeration as
Type 2 providers.
On paper, there is no way to distinguish a type 1 from a type 2 in the absence of any
associated data; they are identical in format. Additional information on NPI and
enumeration
can be obtained from the ADA’s Internet Web Site –
National Provider Identifier
50.
License Number: If the billing dentist is an individual, enter the dentist’s license number. If a
billing entity (e.g., corporation) is submitting the claim, leave blank.
51.
SSN or TIN: Report the: 1) SSN or TIN if the billing dentist is unincorporated; 2) corporation TIN of
the billing dentist or dental entity if the practice is incorporated; or 3) entity TIN when the billing
entity is a group practice or clinic.
52.
Phone Number: Enter the business phone number of the billing dentist or dental entity.
52a. Additional Provider ID: This is an identifier assigned to the billing dentist or dental entity other
than a Social Security Number (SSN) or Tax Identification Number (TIN). It is not the provider’s
NPI.
The additional identifier is sometimes referred to as a Legacy Identifier (LID). LIDs may not be
unique as they are assigned by different entities (e.g., third-party payer; federal government).
Some Legacy IDs have an intrinsic meaning.
Treating Dentist And Treatment Location Information
This section must be completed for all claims. Information that is specific to the dentist or practitioner
acting within the scope of their state licensure who has provided treatment is entered in this section.
53.
Certification: Signature of the treating or rendering dentist and the date the form is signed. This is
the dentist who performed, or is in the process of performing, procedures, indicated by date, for
the patient. If the claim form is being used to obtain a pre-estimate or pre-authorization, it is not
necessary for the dentist to sign the form.
ADA Dental Claim Form Completion Instructions
Version 2019 © American Dental Association
Page 16 of 16
Completion Instructions Date: 2022Feb11
Claim forms prepared by the dentist’s practice management software may insert the treating
dentist’s printed name in this Item.
54.
NPI (National Provider Identifier): Enter the treating dentist’s Type 1 – Individual Provider NPI in
Item # 54. (See Item #49 for more NPI information.)
55.
License Number: Enter the license number of the treating dentist. This may vary from the billing
dentist.
56.
Address, City, State, Zip Code: Enter the physical location where the treatment was rendered.
Must be a street address, not a Post Office Box.
NOTE: For teledentistry encounters the treatment location is the dentist’s practice location,
not the patient’s location.
56a. Provider Specialty Code: Enter the code that indicates the type of dental professional who
delivered the treatment. Available codes describing treating dentists follow. The general code
listed as “Dentist” may be used instead of any other dental practitioner codes.
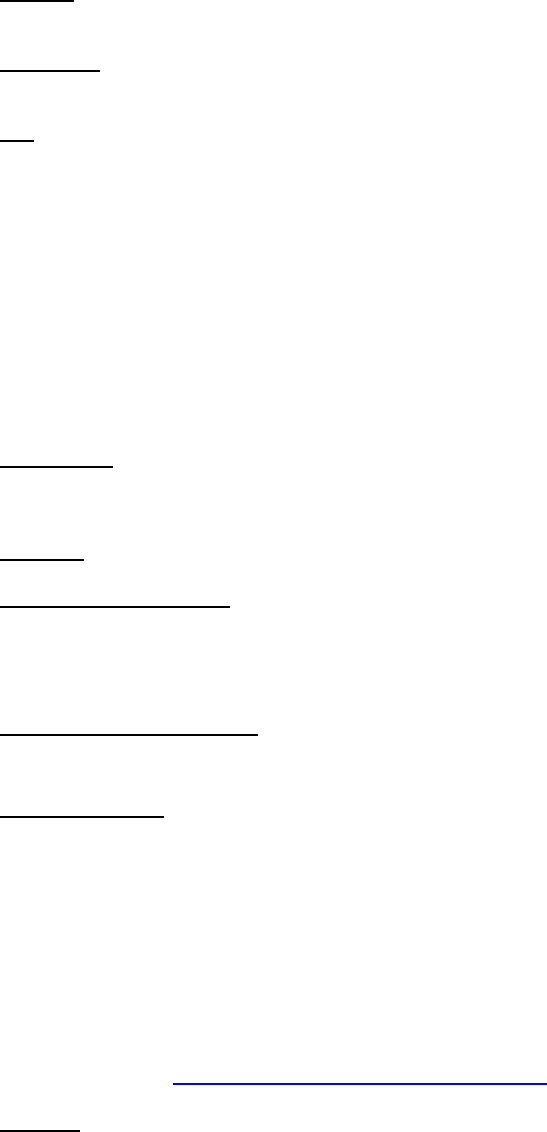
Category / Description Code
Dentist / a person qualified by a doctorate in dental surgery
(D.D.S) or dental medicine (D.M.D.) licensed by the state to
practice dentistry, and practicing within the scope of that license.
122300000X
General Practice / a dentist who provides a variety of dental
services to address patient needs.
1223G0001X
Dental Specialty
/ a practitioner in one of the nine specialty areas
recognized by the ADA.
See following list
Dental Public Health 1223D0001X
Endodontics 1223E0200X
Orthodontics 1223X0400X
Pediatric Dentistry 1223P0221X
Periodontics 1223P0300X
Prosthodontics 1223P0700X
Oral & Maxillofacial Pathology 1223P0106X
Oral & Maxillofacial Radiology 1223D0008X
Oral & Maxillofacial Surgery 1223S0112X
These codes are from the “Dental Service Providers” section of the Healthcare Providers
Taxonomy code list, a HIPAA standard, and are a subset of the full list that includes codes for
other types of practitioners including dental assistants, dental hygienists, denturists, and dental
lab technicians. The current full list is posted online –
Health Care Provider Taxonomy Code Set
57.
Phone Number: Enter the business telephone number of the treating dentist.
58.
Additional Provider ID: This is an identifier assigned to the treating dentist other than a Social
Security Number (SSN) or Tax Identification Number (TIN). It is not the provider’s NPI.
The additional identifier is sometimes referred to as a Legacy Identifier (LID). LIDs may not be
unique as they are assigned by different entities (e.g., third-party payer; Federal government).
Some Legacy IDs have an intrinsic meaning.
