
HANDBOOK
OCTOBER 2021
TRICARE offers comprehensive,
affordable health care, dental,
and pharmacy coverage to meet
your changing needs.
Your TRICARE Options by Sponsor Status 4
Health Care Options 6
TRICARE Pharmacy Program 13
Dental and Vision Options 14
TRICARE
®
Choices
in the United States
Welcome to
TRICARE
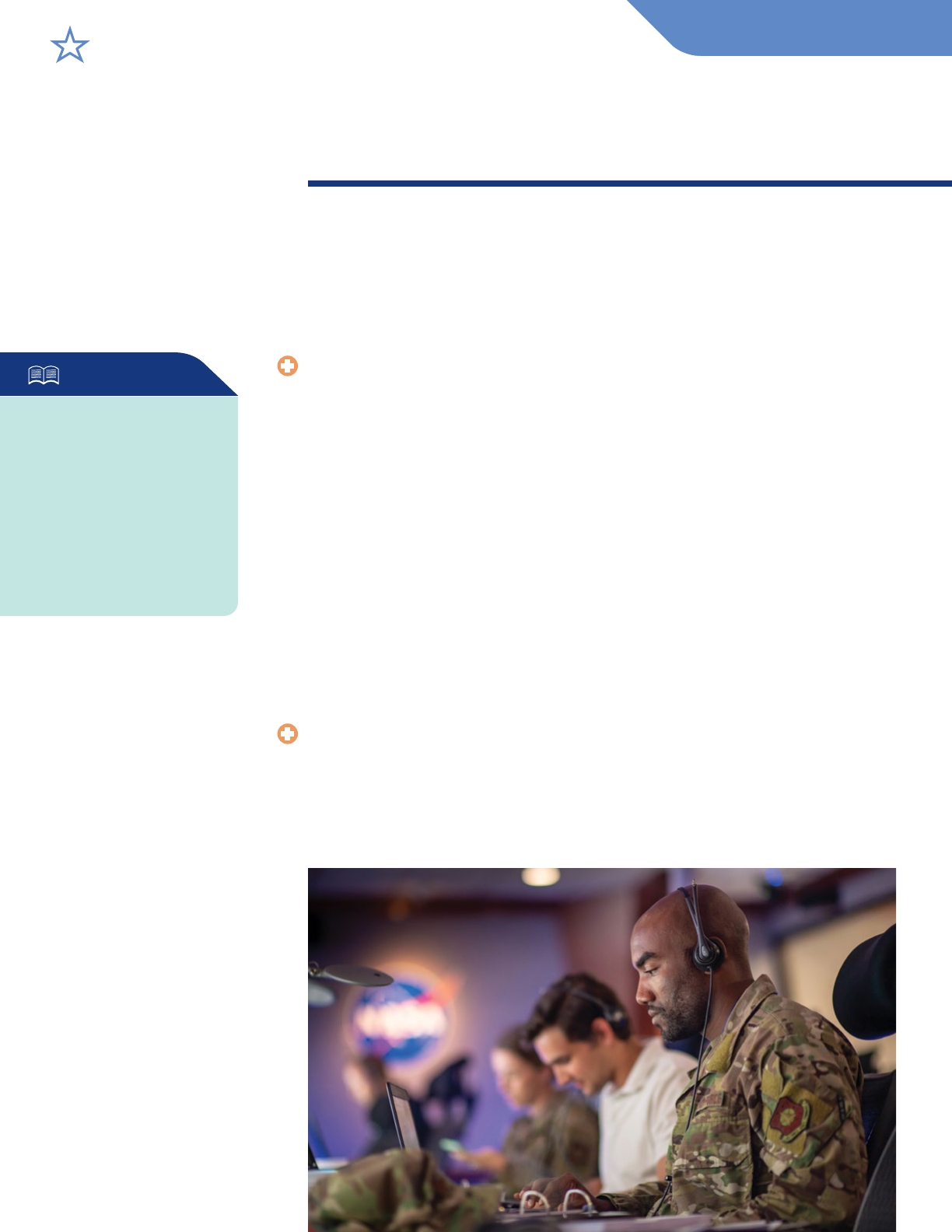
TRICARE is the Department of Defense’s premier health care program
serving 9.6 million active duty service members, retired service members,
National Guard and Reserve members, family members, and survivors
worldwide. As a TRICARE beneficiary, you have access to the health care
you need wherever you are.
TRICARE brings together military hospitals and clinics with a network of
civilian providers to offer you medical, pharmacy, and dental options that
meet your changing needs.
TRICARE partners with civilian regional contractors to administer your
TRICARE benefit in two U.S. regions (East and West) and one overseas
region. Your regional contractor is your go-to resource for information and
assistance.
This handbook outlines the TRICARE program options that may be available to
you based on who you are, your location, and your entitlement to Medicare.
We stand ready to deliver quality health
care to those who protect our country
every day—our nation’s nest. We are
proud to serve you.
Take the Publications Survey
Take the brief publications survey by using the QR code to the
left or by clicking on “Publications Satisfaction Survey” at
www.tricare.mil/publications.
2

TRICARE Meets
the Minimum
Essential Coverage
Requirement under the
Affordable Care Act
Most TRICARE plans meet the
Affordable Care Act requirement
for minimum essential coverage.
You can find other health
care coverage options at
www.healthcare.gov.
KEEP YOUR DEERS INFORMATION UP TO DATE
Eligibility for TRICARE is determined by the services and shown in the
Defense Enrollment Eligibility Reporting System (DEERS). DEERS is
a database of service members and dependents worldwide who are
eligible for military benefits.
To use TRICARE, first make sure your DEERS record is up to date
at https://milconnect.dmdc.osd.mil.
TRICARE COVERED SERVICES
This handbook describes the health care, dental, and pharmacy
options TRICARE offers. These options differ in terms of the
providers you see, how you get care, costs, and whether you file
claims. Generally, you have the same covered services, including
preventive, mental health, maternity, and pharmacy services, with
any TRICARE program option. Copayments or cost-shares may apply
for certain covered services depending on your program option and
beneficiary status. For a full list of covered services,
go to www.tricare.mil/coveredservices. For costs, go to
www.tricare.mil/costs.
3
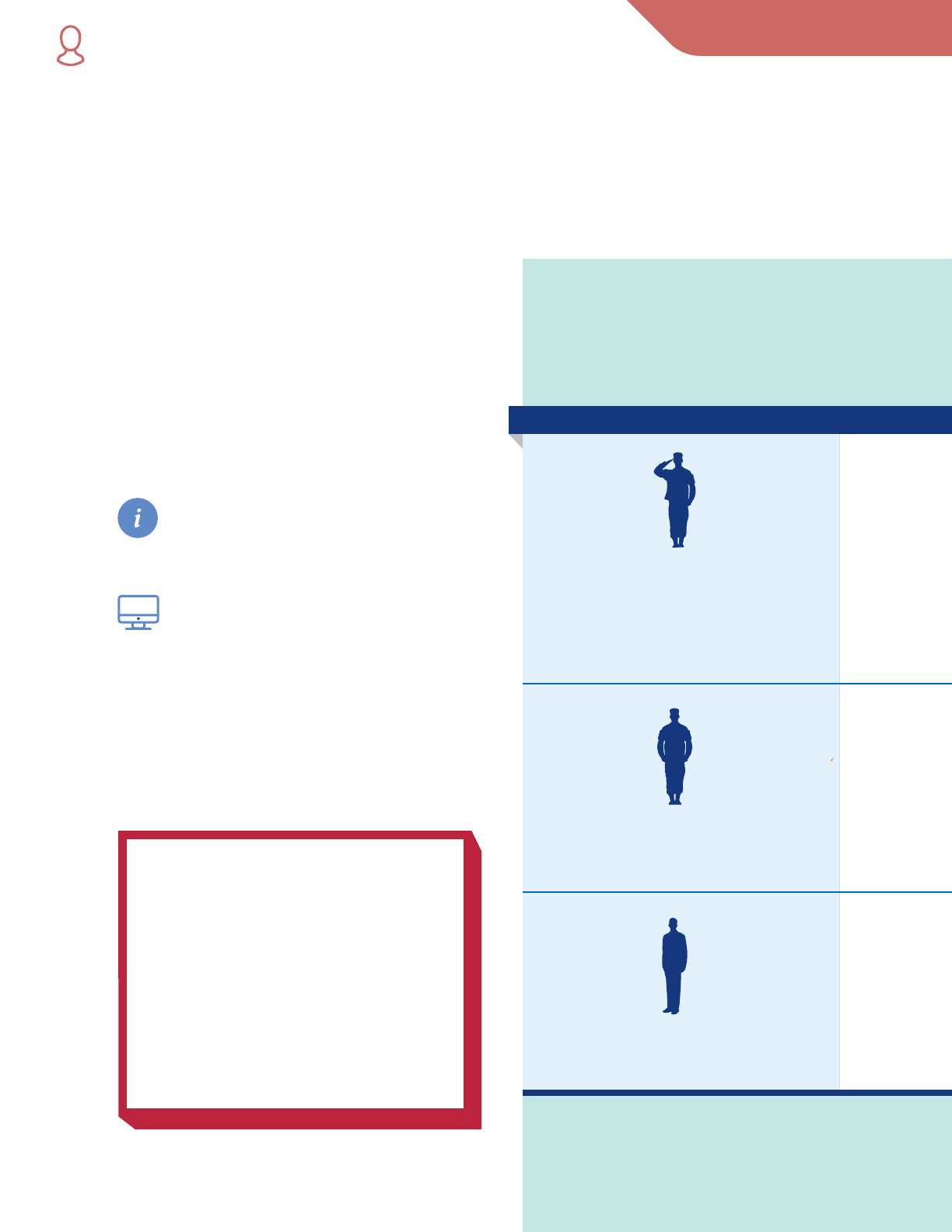
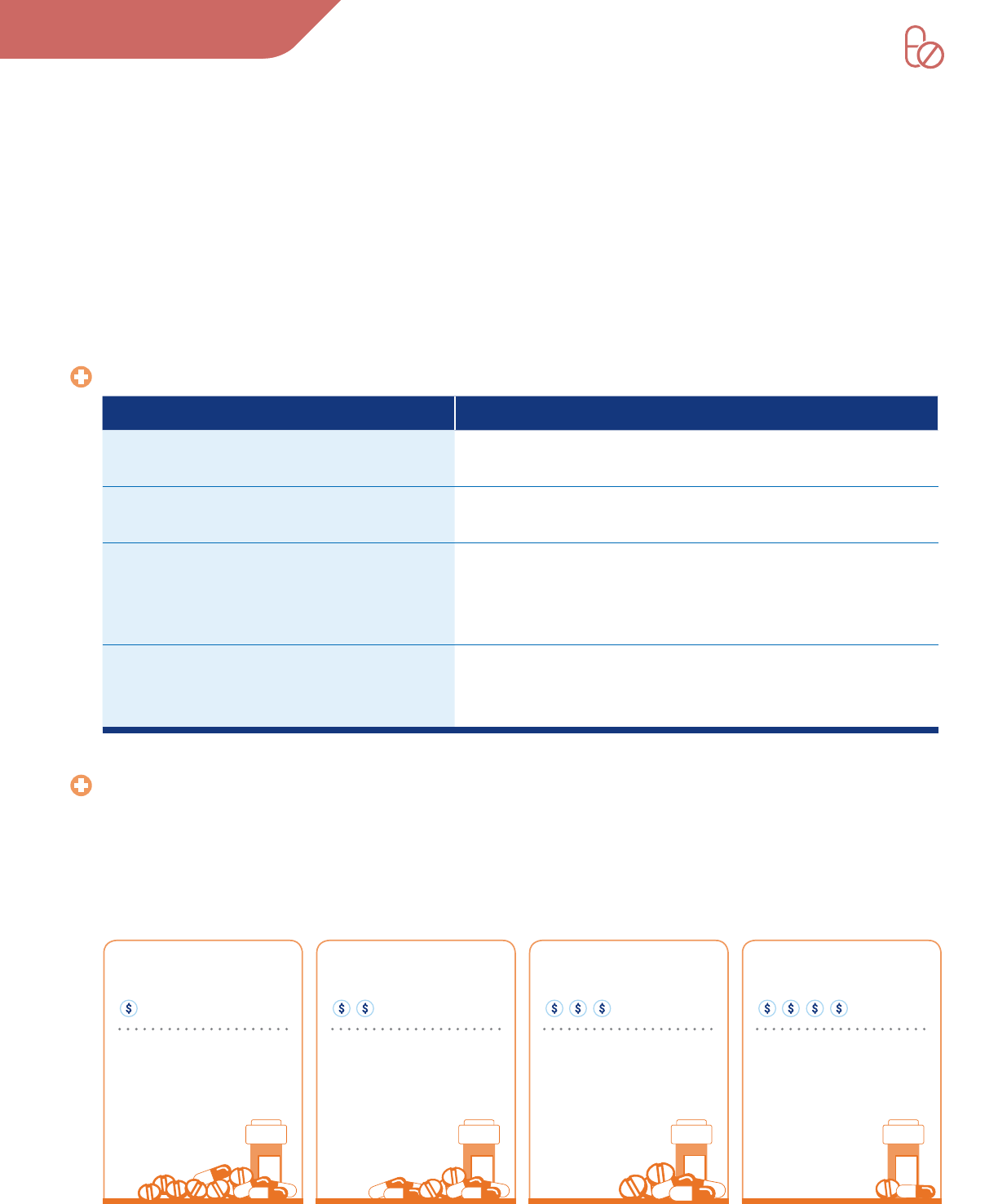
Your TRICARE health care options can
change if you move, have a life event like
getting married, or have a status change
like a sponsor retiring from service. Use
the following graphic to determine your
options based on sponsor status.
FIND MORE INFORMATION
You can get more information
about your TRICARE benefit at
www.tricare.mil/publications or
by calling your regional contractor.
Manage your TRICARE benefit
through the TRICARE website at
www.tricare.mil, where you can get to
secure services, see what’s covered,
find a provider, and much more.
We encourage you to use these resources to
take full advantage of the TRICARE programs
available to you.
Retired
Separated from Service
(non-retirement)
Active Duty
Includes National Guard
and Reserve members called or ordered
to active duty for more than 30 days for
a preplanned mission or in support of a
contingency operation
SPONSOR STATUS HEALTH CARE OPTIONS
NATIONAL GUARD AND RESERVE
Qualied non-active duty members of the Selected
Reserve and Retired Reserve
Sponsor and family member options:
• TRICARE Reserve Select
• TRICARE Retired Reserve
• TRICARE Young Adult
See the TRICARE Choices for National Guard
and Reserve Handbook for more information
at www.tricare.mil/publications.
YOUR TRICARE OPTIONS BY SPONSOR STATUS
4
Sponsor options:
• TRICARE Prime*
• TRICARE Prime Remote (TPR)
Sponsor options:
• TRICARE Prime*
• USFHP (depending on location and age)
• TRICARE Select
• TFL (if entitled to Medicare Part A and
have Medicare Part B)
Sponsor and family member options:
After separating from service (non-retirement), the sponsor and family members lose
TRICARE eligibility. However, you may qualify for a period of continued coverage under the:
• Transitional Assistance Management Program (TAMP)
• Continued Health Care Benet Program (CHCBP)
Family member options:
• TRICARE Prime*
• TPR
• US Family Health Plan (USFHP) (depending on location)
• TRICARE Select
• TRICARE Young Adult (TYA)
• TRICARE For Life (TFL) (if entitled to Medicare Part A and have
Medicare Part B)
Family member options:
• TRICARE Prime*
• USFHP (depending on location and age)
• TRICARE Select
• TYA
• TFL (if entitled to Medicare Part A and have
Medicare Part B)
HEALTH CARE OPTIONS
For up-to-date cost information for all TRICARE program options,
go to www.tricare.mil/costs or see the Costs and Fees sheet at
www.tricare.mil/publications.
Active Duty Separated from Service Retired
* TRICARE Prime is only available in Prime Service Areas (PSAs).
5
TRICARE Prime is a health care option for active duty service members (ADSMs),
retirees, family members, and certain others. It’s similar to a managed care or health
maintenance organization option, which means your access to specialty care is managed
by your primary care manager (PCM).
Other TRICARE Prime options include:
• TPR, a TRICARE Prime option for ADSMs living and working in remote locations
(outside of a PSA) and their family members.
• USFHP, a TRICARE Prime option where care is provided through networks of community-
based, not-for-profit health care systems in six areas of the United States. For more
information, go to www.tricare.mil/usfhp.
QUALIFYING FOR A TRICARE PRIME OPTION
To get TRICARE Prime, you must live in a PSA. You may also get TRICARE Prime
if you live within 100 miles of an available PCM and waive your drive-time access
standards. To find out if you live in an area where you can get TRICARE Prime, go to
www.tricare.mil/planfinder. For more information about drive-time access standards, go to
www.tricare.mil/primeaccess.
TPR is an option for ADSMs and active duty family members (ADFMs) living and working
in remote areas.
ENROLLING IN A TRICARE PRIME OPTION
You must take action to enroll in a TRICARE Prime option:
• ADSMs must use TRICARE Prime or TPR.
• ADFMs can choose to enroll in TRICARE Prime, TPR, USFHP, or TRICARE Select.
• Retirees and retiree family members may enroll in TRICARE Prime or USFHP. If neither
is available, you can enroll in TRICARE Select.
You can only enroll in or change enrollment to TRICARE Prime (if you live in a PSA)
following a Qualifying Life Event (QLE) or during the annual fall TRICARE Open Season.
You have three options to enroll in a TRICARE Prime program:
• Log in to milConnect at https://milconnect.dmdc.osd.mil and click on the “Manage
health benefits” button.
• Call your regional contractor.
• Submit a TRICARE Prime Enrollment, Disenrollment, and Primary Care Manager (PCM)
Change Form (DD Form 2876) to your regional contractor. You can find this form
at www.tricare.mil/forms.
For more information on enrollment, visit www.tricare.mil/enroll.
TRICARE Prime® Options
HELPFUL TERMS
Qualifying Life Event
A certain change in your life,
such as marriage, birth of a
child, or retirement from
active duty, which may mean
different TRICARE options
are available to you. A QLE
opens a 90-day period for
you to make eligible
enrollment changes. A QLE
for one family member
means all family members
may make enrollment
changes. To learn more, visit
www.tricare.mil/lifeevents.
TRICARE Open Season
The annual period when you
can enroll in or change your
health care coverage plan for
the following year. To learn
more, visit www.tricare.mil/
openseason.
AUTOMATIC
ENROLLMENT
If you’re an ADSM, a family
member of a new ADSM,
a new family member of
a current ADSM, or your
military sponsor has been
called to active duty, you’ll
be automatically enrolled
in TRICARE Prime if you
live in a PSA. Otherwise,
ADFMs will be automatically
enrolled in TRICARE Select.
ADSMs must remain
enrolled in TRICARE Prime.
All others automatically
enrolled have up to 90 days
to change enrollment if
eligible for other TRICARE
plans. You may also be
eligible to enroll in the
USFHP if you live in an area
where the plan is offered.
HEALTH CARE OPTIONS
6
GETTING CARE WITH A TRICARE PRIME OPTION
When you enroll in a TRICARE Prime option, you’ll get most of your routine
care from an assigned or selected PCM. Your PCM may be:
• At a military hospital or clinic
• A civilian TRICARE network provider
• A primary care provider under USFHP
Referrals and pre-authorizations may be required for certain services. For
specific information, visit www.tricare.mil/appointments.
ENROLLMENT COSTS
ADSMs, ADFMs, and transitional survivors (surviving spouses during
the first three years and surviving dependent children) pay no enrollment
fees. Retirees, their families, and others pay yearly enrollment fees. For cost
details, go to www.tricare.mil/costs.
COSTS FOR COVERED CARE
ADSMs have no out-of-pocket costs for covered health care services from a PCM,
or with the appropriate referral and pre-authorization. ADFMs have no out-of-
pocket costs for covered health care services from a network provider in their
enrolled TRICARE region, or with the appropriate referral and pre-authorization.
Retirees pay copayments or cost-shares for covered health care services from
network providers in their enrolled TRICARE region. When following the
rules of the TRICARE Prime program option, out-of-pocket costs are limited
to the catastrophic cap amount for that calendar year (Jan. 1–Dec. 31). For
more information, see www.tricare.mil/costs.
SEEING A PROVIDER WITHOUT A REFERRAL:
THE POINT-OF-SERVICE OPTION
The point-of-service (POS) option allows non-ADSMs to see any TRICARE-
authorized provider without a referral. This means you pay more money
up front to get nonemergency health care from any TRICARE-authorized
provider without a referral. Costs you pay under the POS option don’t count
toward your yearly catastrophic cap. For more information,
go to www.tricare.mil/pointofservice.
HELPFUL TERMS
Referral
When your primary care
manager (PCM) sends
you to another provider
for care. If you have
TRICARE Prime and see
a provider other than your
PCM for nonemergency
care without a referral,
you will pay more. Certain
benets, such as the
Comprehensive Autism
Care Demonstration,
require a referral and
continued authorizations.
Pre-authorization
A review of a requested
health care service done by
your regional contractor to
see if the care will be
covered by TRICARE. Check
for services that need
pre-authorization by going to
www.tricare.mil or your
regional contractor’s website.
Catastrophic Cap
The most you or your
family will pay for covered
health care services each
calendar year.
Enrollment Fee
The yearly fee that retirees,
their families, and certain
others pay when enrolled
in TRICARE Prime or
TRICARE Select.
Calendar Year
A calendar year is Jan. 1–
Dec. 31.
77

TRICARE Select® Options
TRICARE Select is for TRICARE-eligible beneficiaries who aren’t able to, or choose not to,
enroll in a TRICARE Prime option and who aren’t entitled to Medicare (with the exception
of ADFMs). This program lets you manage your own health care and get care from any
TRICARE-authorized provider without a referral.
Like TRICARE Prime options, enrollment is required. ADSMs may not use TRICARE Select.
ENROLLING IN A TRICARE SELECT OPTION
You must take action to enroll in a TRICARE Select option:
• ADFMs, retirees, and retiree family members can choose to enroll in TRICARE Select.
You can only enroll in or change enrollment to TRICARE Select following a QLE or
during the annual fall TRICARE Open Season.
You have three options to enroll in TRICARE Select:
• Log in to milConnect at https://milconnect.dmdc.osd.mil and click on the “Manage
health benefits” button.
• Call your regional contractor.
• Submit a TRICARE Select Enrollment, Disenrollment and Change Form (DD Form 3043)
to your regional contractor. You can find this form at www.tricare.mil/forms.
For more information on enrollment, visit www.tricare.mil/enroll.
GETTING CARE WITH TRICARE SELECT
With TRICARE Select, you can get care from any TRICARE-authorized network provider
without a referral or pre-authorization, in most situations. You’ll have lower out-of-pocket
costs if you use a TRICARE-authorized network provider versus a TRICARE-authorized
non-network provider. If you choose a non-authorized non-network provider, you won’t be
reimbursed by TRICARE.
To find a TRICARE network provider, go to www.tricare.mil/findaprovider or call your
regional contractor.
HELPFUL TERMS
TRICARE-Authorized
Provider
A provider approved by
TRICARE to give health care
services to beneciaries.
A provider must be
TRICARE-authorized for
TRICARE to pay any part
of your claim.
Network Provider
A provider that has agreed
to accept the contracted
rate as payment in full for
covered health care
services and les claims
for you.
Non-Network Provider
A provider that doesn’t
have an agreement with
TRICARE and may not le
claims for you. There are
two types of non-network
providers: participating
and nonparticipating.
Cost-Share
A percentage of the total
cost of a covered health
care service that you pay.
Copayment
The xed amount those
with TRICARE Prime (who
aren’t ADSMs and ADFMs)
or TRICARE Select pay for a
covered health care service
or drug.
HEALTH CARE OPTIONS
8
ENROLLMENT COSTS
There is no yearly enrollment fee for ADFMs. Retirees, their families, and
others pay enrollment fees. For cost details, go to www.tricare.mil/costs.
COSTS FOR COVERED CARE
With TRICARE Select, you pay a yearly deductible and per-visit copayments
or cost-shares. You’ll fall into one of two groups based on when you or your
sponsor entered the uniformed services. This group will determine your
costs. When following the rules of your program option, your out-of-pocket
expenses will be limited to your catastrophic cap. Nonparticipating non-
network providers may charge up to 15% above the TRICARE-allowable
amount, which won’t apply to your catastrophic cap. You’re responsible for
this amount, plus your deductible and copayments or cost-shares. For costs,
go to www.tricare.mil/costs.
FILING CLAIMS
Submit claims to the regional contractor for the area where you live. In the U.S.
and U.S. territories (American Samoa, Guam, the Northern Mariana Islands,
Puerto Rico, and the U.S. Virgin Islands), claims must be filed within one
year of the date of service or date of inpatient discharge. You’re responsible
for confirming your claims are received. For assistance, call your regional
contractor.
INVITE YOUR PROVIDER TO BECOME TRICARE-
AUTHORIZED
If your provider isn’t TRICARE-authorized, but wants to see TRICARE
patients, tell your provider he or she can do so without signing a contract
with your regional contractor. Most providers with a valid professional
license (issued by a state or a qualified accreditation organization) can
become TRICARE-authorized and then TRICARE will pay them for covered
services. Go to www.tricare.mil/findaprovider and click “Learn more.”
HELPFUL TERMS
Yearly Deductible
A xed amount you pay for
covered services each
calendar year before TRICARE
pays anything. You may have
a deductible if you have
TRICARE Select or if you have
TRICARE Prime and see a
provider without a referral.
Claim
A request for payment from
TRICARE that goes to your
regional contractor after you
get a covered health care
service.
9
TRICARE Select Options (continued)
HELPFUL TERMS
Premium
The amount you pay for a
health care plan you purchased.
Premiums apply to those using
TRICARE Reserve Select,
TRICARE Retired Reserve,
TRICARE Young Adult, and the
Continued Health Care
Benet Program.
Premium-based health care plans that work like TRICARE Select with the same copayments
or cost-shares and a choice of providers can be purchased by those who qualify. These plans
include TRICARE Reserve Select (TRS), TRICARE Retired Reserve (TRR), and the Continued
Health Care Benefit Program (CHCBP). For more on CHCBP, see “Transitional Coverage
Options” in the Other TRICARE Program Options section.
TRICARE RESERVE SELECT® AND TRICARE RETIRED RESERVE®
TRS and TRR are premium-based, worldwide health care plans for certain qualified Selected
Reserve or Retired Reserve members, their family members, and survivors. TRS and TRR
offer comprehensive health care coverage similar to TRICARE Select.
• Enrollment is required.
• TRICARE Open Season doesn’t apply to TRS and TRR. These plans offer continuous
open enrollment throughout the year.
• An initial two-month premium payment is due when you enroll.
• Monthly premiums, a yearly deductible, and copayments or cost-shares apply.
• Get care from any TRICARE-authorized provider without a referral.
• Certain services require pre-authorization.
Note: When your National Guard or Reserve sponsor is activated for more than 30 days for
a preplanned mission or in support of a contingency operation, this coverage stops while you
get active duty benefits.
PURCHASE TRICARE RESERVE SELECT OR
TRICARE RETIRED RESERVE
For more information, including how to purchase TRS or TRR coverage, go to
www.tricare.mil/trs or www.tricare.mil/trr.
HEALTH CARE OPTIONS
10
If you’re entitled to Medicare Part A, you generally must have Medicare Part B to keep TRICARE, regardless of
your age or where you live. This is a requirement based on federal law with an exception for ADSMs and ADFMs.
If you’re eligible for TRICARE and have Medicare Part A and Part B, you’re automatically covered by TFL. See
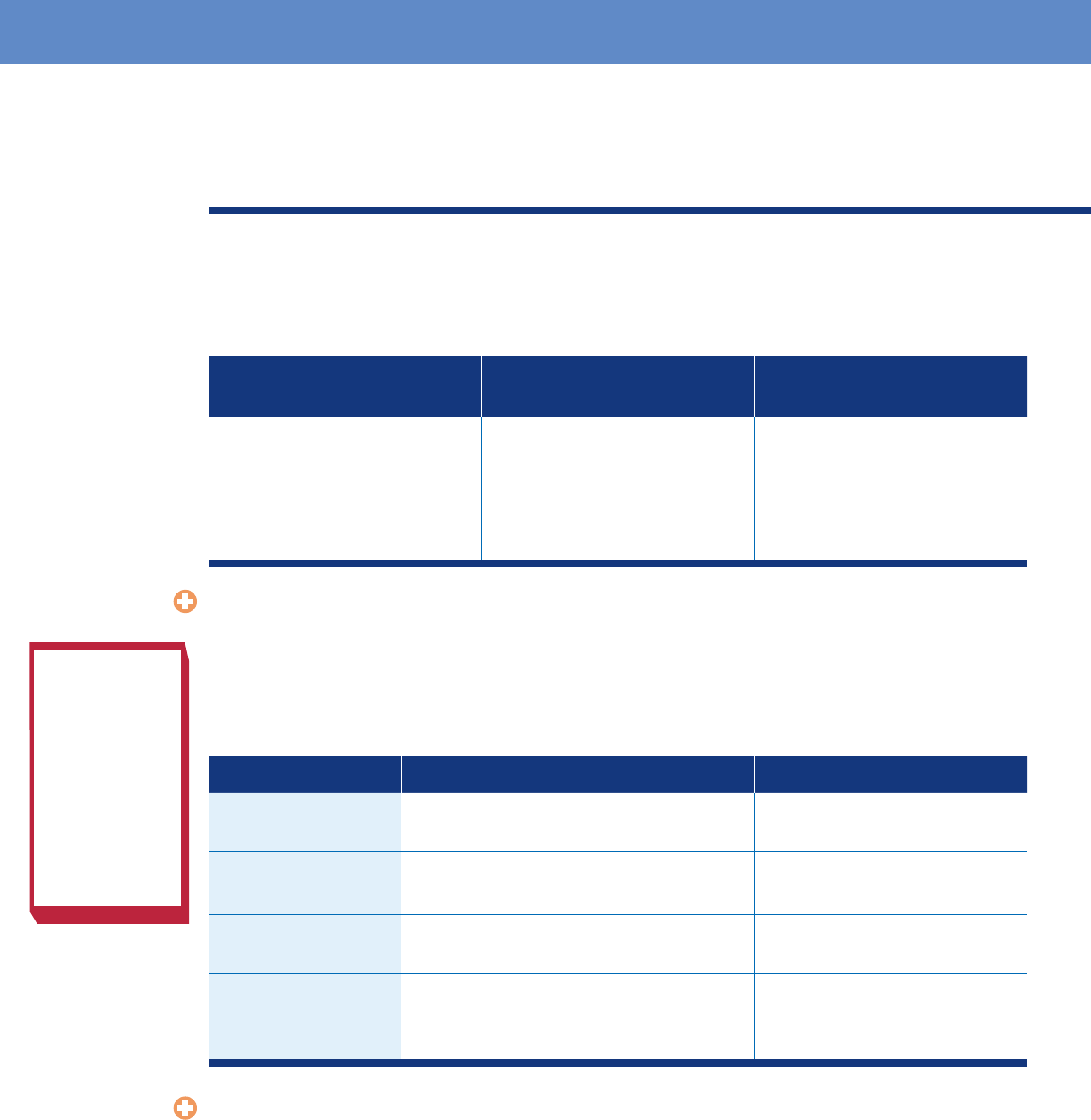
the following table for more information on what Medicare Part A, Part B, and TFL cover.
MEDICARE PART A
(Hospital Insurance)
MEDICARE PART B
(Medical Insurance)
TRICARE FOR LIFE
• Inpatient hospital care
• Hospice care
• Inpatient skilled nursing
facility care
• Some home health care
• Provider services
• Outpatient care
• Home health care
• Durable medical equipment
• Some preventive services
• Inpatient and outpatient
wraparound coverage
• Coverage for overseas care
TRICARE FOR LIFE COSTS
There are no enrollment fees or forms for TFL, but you must have Medicare Part A and Part B. Medicare Part
B has a monthly premium. Go to www.medicare.gov for the current Part B premium amounts, which vary by
income level. For more information about TFL, go to www.tricare.mil/tfl. You may also call Wisconsin Physicians
Service (WPS)—Military and Veterans Health, the contractor that administers the TFL benefit. The following
table highlights your TFL out-of-pocket costs. For detailed cost information, go to www.tricare.mil/tflcosts.
TYPE OF CARE MEDICARE PAYS TRICARE PAYS YOU PAY
Covered by TRICARE
and Medicare
Medicare-allowed
amount
Remaining amount Nothing
Covered by
Medicare only
Medicare-allowed
amount
Nothing Medicare deductible and cost-share
Covered by
TRICARE only
Nothing TRICARE-allowable
amount
TRICARE deductible and cost-share
Not covered by
TRICARE or Medicare
Nothing Nothing Billed charges (which may be more
than the Medicare- or TRICARE-
allowable amount)
TRICARE FOR LIFE AND U.S. DEPARTMENT OF VETERANS AFFAIRS BENEFITS
If you’re eligible for both TFL and U.S. Department of Veterans Affairs (VA) benefits and choose to use your TFL
benefit for health care not related to a service-connected injury or illness, you’ll pay more to see a VA provider than
you would pay to see a civilian Medicare provider. TRICARE will only pay up to 20% of the TRICARE-allowable
amount for care you get at a VA facility and you may be responsible for the remaining amount.
With TFL, your least expensive option is to see a Medicare participating or Medicare non-participating provider.
Medicare participating providers agree to accept the Medicare-allowed amount as payment in full. Medicare
non-participating providers don’t accept the Medicare-allowed amount as payment in full and may charge up to
15% above the Medicare-allowed amount. This additional cost may be covered by TFL. If you get care from a VA
provider, check with WPS to confirm coverage details.
TRICARE For Life
WISCONSIN
PHYSICIANS
SERVICE
(WPS)—
MILITARY AND
VETERANS
HEALTH
1-866-773-0404
1-866-773-0405
(TDD/TTY)
11

DRAFT DRAFT
TRICARE offers other coverage options for those who have eligibility changes, such as children
aging out of regular TRICARE coverage or sponsors separating from service. If you’ve lost all
TRICARE eligibility, you may qualify to buy coverage under CHCBP, discussed below.
TRICARE YOUNG ADULT
TYA is a premium-based health care plan for qualified adult children who have aged out
of TRICARE. TYA Prime and TYA Select are offered worldwide. Your location and sponsor’s
status determine whether you qualify for TYA Prime and/or TYA Select.
TYA includes medical and pharmacy benefits, but not dental or vision coverage. Coverage,
provider choice, and costs for TYA are the same as for TRICARE Prime and TRICARE Select.
You may generally purchase TYA coverage if you’re an adult child of a TRICARE-
eligible sponsor; unmarried; at least age 21, but not yet age 26; and not otherwise eligible for
TRICARE or employer-based coverage. TRICARE Open Season doesn’t apply to TYA. TYA
Prime and TYA Select offer continuous open enrollment throughout the year.
For more information, go to www.tricare.mil/tya.
TRANSITIONAL COVERAGE OPTIONS
TRICARE offers benefits to help certain service members and their families transition to
civilian life.
Transitional Assistance Management Program
TAMP offers 180 days of premium-free health care after your sponsor separates from the
military. If you’re eligible, TAMP starts the day after the sponsor separates from service.
For more information, go to www.tricare.mil/tamp.
Continued Health Care Benefit Program
CHCBP is a premium-based health care program managed by Humana Military. CHCBP
offers continued health coverage (18–36 months) after TRICARE coverage ends. Certain
former spouses who haven’t remarried before age 55 may qualify for an unlimited duration
of coverage. If you qualify, you can purchase CHCBP coverage within 60 days of loss of
TRICARE or TAMP coverage, whichever is later. TRICARE Open Season doesn’t apply
to CHCBP. CHCBP offers continuous open enrollment throughout the year. For more
information, go to www.tricare.mil/chcbp.
Note: While in CHCBP, you aren’t eligible to receive care at a military hospital or clinic,
except in a medical emergency.
Other TRICARE Program Options
HEALTH CARE OPTIONS
12
DRAFT DRAFT
The TRICARE Pharmacy Program provides prescription drugs through military pharmacies, TRICARE Pharmacy Home
Delivery, TRICARE retail network pharmacies, and non-network pharmacies. Your options for filling your prescription
depend on the type of drug your provider prescribes. Express Scripts, Inc. manages the TRICARE pharmacy benefit for all
TRICARE-eligible beneficiaries. If you’re in USFHP, you have different pharmacy coverage.
For more information about the TRICARE pharmacy benefit, see the TRICARE Pharmacy Program Handbook at
www.tricare.mil/publications or go to www.tricare.mil/pharmacy.
PHARMACY OPTIONS
OPTIONS FOR FILLING PRESCRIPTIONS DESCRIPTION OF OPTIONS
Military pharmacies • No cost for up to a 90-day supply of most covered drugs
• Usually don’t carry non-formulary drugs
TRICARE Pharmacy Home Delivery • No cost for ADSMs. For all other beneciaries, copayments apply
• Drugs are mailed to you with free standard shipping
TRICARE retail network pharmacies • Pay one copayment for each 30-day supply of covered drugs
• No need to le a claim
• Located in the U.S. and the U.S. territories of Guam, the Northern
Mariana Islands, Puerto Rico, and the U.S. Virgin Islands
Non-network pharmacies • Pay full price and le a claim to get money back on covered drugs
• The amount of money you get back depends on deductibles,
out-of-network cost-shares, and copayments
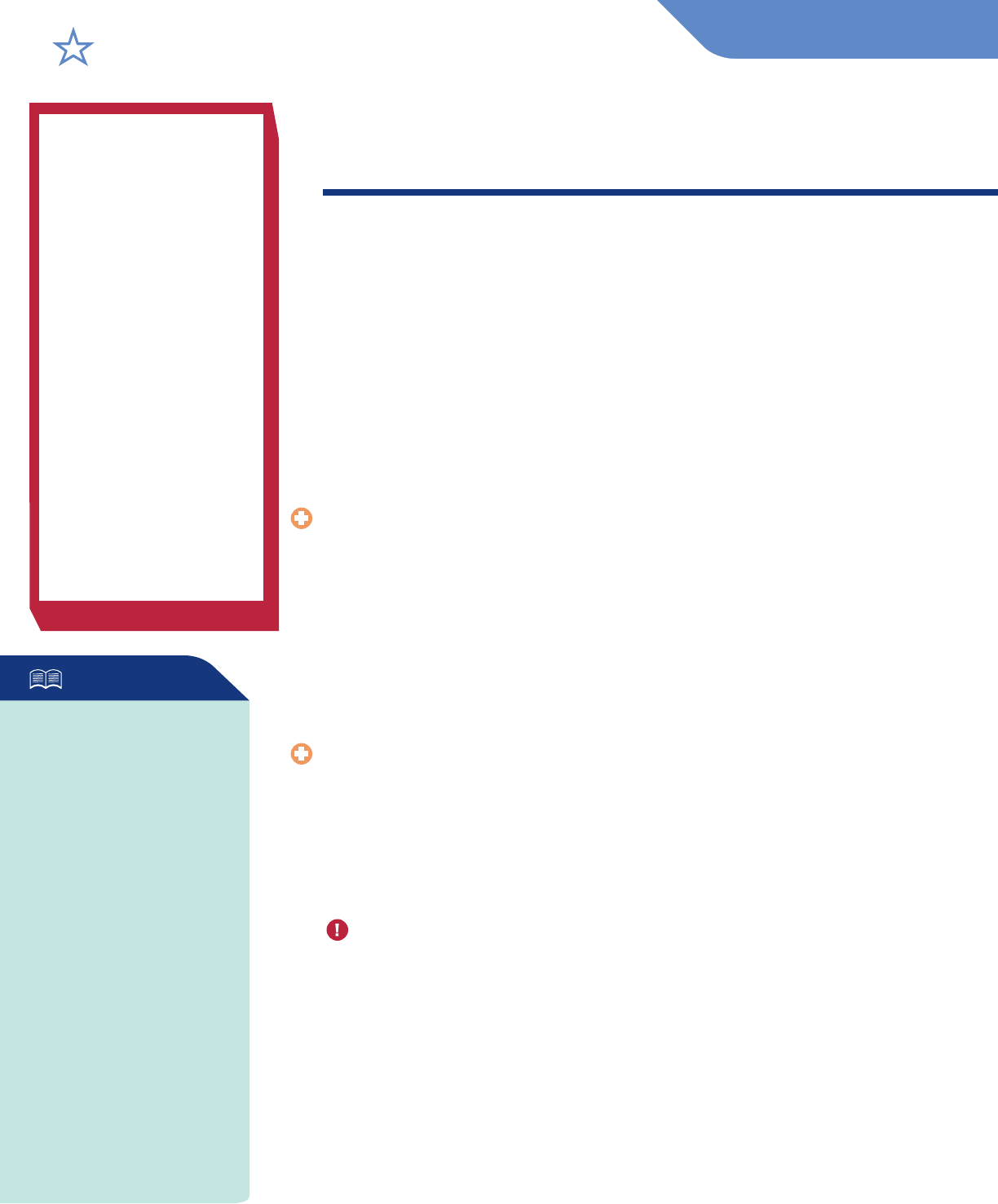
FOUR CATEGORIES OF DRUGS
TRICARE groups prescription drugs into four categories. This grouping is based on medical effectiveness and cost of a drug
compared to other drugs of the same type. The following graphic shows how drugs in different categories may cost more and be
harder to get.
Non-covered drugs
• Not covered by TRICARE
• Highest out-of-pocket
costs (You pay 100% of
the drug’s cost)
Non-formulary drugs
• May have limited
availability
• Higher out-of-pocket
costs
Brand-name
formulary drugs
• Generally available
• Moderate out-of-
pocket costs
Generic formulary
drugs
• Widely available
• Lowest out-of-pocket
costs
TRICARE PHARMACY PROGRAM
13

DRAFT DRAFT
There are three dental options that are separate
from TRICARE health care options:
• TRICARE Active Duty Dental Program (ADDP)
• TRICARE Dental Program (TDP)
• Federal Employees Dental and Vision Insurance Program (FEDVIP)
ADSMs generally get care at military dental clinics, but may
sometimes use the ADDP. For more information and for
dental costs, go to www.tricare.mil/dental.
• ADFMs
• National Guard and Reserve members and
their family members
• Individual Ready Reserve members and
their family members
• Survivors
• Retired service members and their eligible
family members
• Retired National Guard and Reserve members
and their eligible family members
• Certain survivors
• Medal of Honor recipients and their immediate
family members and survivors
TRICARE Active Duty
Dental Program
(Managed by United Concordia
Companies, Inc.)
www.addp-ucci.com
TRICARE Dental Program
(Managed by United Concordia
Companies, Inc.)
www.uccitdp.com
Federal Employees
Dental and Vision
Insurance Program
(Offered by the U.S. Ofce of
Personnel Management)
www.benefeds.com
• ADSMs
• National Guard and Reserve members called
or ordered to active duty for more than 30 days
for a preplanned mission or a contingency
operation
DENTAL AND VISION OPTIONS
VISION COVERAGE
Retirees, their
eligible family
members, and
active duty family members
enrolled in a TRICARE health
plan may qualify to purchase
vision coverage through the
Federal Employees Dental
and Vision Insurance
Program (FEDVIP), offered by
the U.S. Ofce of Personnel
Management. When eligible,
you can enroll during the fall
Federal Benets Open
Season or following a
FEDVIP QLE.
For information about
TRICARE and FEDVIP, visit
www.tricare.mil/vision.
14

DRAFT DRAFT
Single and family plans Monthly premiums Voluntary
enrollment
For ADSMs who are either referred for care by a military dental
clinic to a civilian dentist or have a duty location and live more
than 50 miles from a military dental clinic.
Coverage for most preventive
and diagnostic services
FEDVIPADDP TDP
FEDVIP is a voluntary dental program that offers eligible TRICARE
participants a choice among a number of dental carriers, with some
plans offering both high and standard options.
TRICARE Offers
Dental Coverage Options
with Worldwide,
Portable Coverage
15

For Information and Assistance
www.tricare.mil
You can sign up to get TRICARE news and publications by email at www.tricare.mil/subscriptions. For TRICARE fact sheets, brochures,
and other benet resources, go to www.tricare.mil/publications.
TRICARE Stateside Regions
TRICARE is available worldwide and managed
regionally. There are two TRICARE regions in
the U.S.: TRICARE East and TRICARE West.
Your TRICARE benefit is the same regardless
of where you are, but there are different
customer service contacts for each region.
TRICARE East Region
Humana Military
1-800-444-5445
HumanaMilitary.com
www.tricare-east.com
TRICARE West Region
Health Net Federal Services, LLC
1-844-866-WEST (1-844-866-9378)
www.tricare-west.com
TRICARE For Life
www.tricare.mil/tfl
Wisconsin Physicians Service—
Military and Veterans Health
1-866-773-0404
1-866-773-0405 (TDD/TTY)
www.TRICARE4u.com
TRICARE Young Adult
www.tricare.mil/tya
US Family Health Plan
1-800-74-USFHP (1-800-748-7347)
www.tricare.mil/usfhp
TRICARE Reserve Select
www.tricare.mil/trs
TRICARE Retired Reserve
www.tricare.mil/trr
Reserve Affairs
www.people.mil
Defense Enrollment Eligibility Reporting
System (DEERS)
1-800-538-9552
www.tricare.mil/deers
milConnect (Enroll, update DEERS,
or get eCorrespondence)
https://milconnect.dmdc.osd.mil
TRICARE Pharmacy Program
www.tricare.mil/pharmacy
Express Scripts, Inc.
1-877-363-1303
https://militaryrx.express-scripts.com
TRICARE Active Duty Dental Program
www.tricare.mil/addp www.tricare.mil/tdp
Insurance Program
www.benefeds.com
United Concordia Companies, Inc. United Concordia Companies, Inc.
(U.S. and U.S. territories) 1-844-653-4061 (CONUS)
1-866-984-ADDP (1-866-984-2337) 1-844-653-4060 (OCONUS)
www.addp-ucci.com 711 (TDD/TYY)
www.uccitdp.com
Transitional Assistance Continued Health Care Benet Program Military Health System Website
Management Program
Humana Military
www.health.mil
www.tricare.mil/tamp
1-800-444-5445
www.tricare.mil/chcbp
An Important Note About TRICARE Program Information
At the time of publication, this information is current. It is important to remember that TRICARE policies and benets are governed by public law and federal
regulations. Changes to TRICARE programs are continually made as public law and/or federal regulations are amended. Military hospital and clinic guidelines
and policies may be dierent than those outlined in this publication. For the most recent information, contact your TRICARE regional contractor or local military
hospital or clinic.
TRICARE is a registered trademark of the Department of Defense, Defense Health Agency. All rights reserved.
HA421G030921WP
TRICARE Dental Program Federal Employees Dental and Vision
STATESIDE
