
GHANA
MDG ACCELERATION FRAMEWORK
AND COUNTRY ACTION PLAN
MATERNAL HEALTH
July 2011
18605 Ghana omslag.indd 1 25/05/11 00.30
MDG ACCELERATION FRAMEWORK
AND COUNTRY ACTION PLA
MATERNAL HEALTH
July 2011
Copyright © Ministry of Health (MoH), Government of Ghana and United Nations
Country Team in the Republic of Ghana
All rights reserved.
Acknowledgements:
The Ministry of Health, Ghana Health Service and the UNDP wishes to express
its appreciation to the task team and all who in diverse ways worked tirelessly to
develop the MDG Acceleration Framework Country Action Plan. Members of the
task team involved in the preparation of the action plan include:
George K. Amofah, Deputy Director General, Ghana Health Service; Patrick Kuma-
Aboagye, Deputy Director, RCH, Ghana Health Service; Kyei-Faried, Deputy Director,
DCD, Ghana Health Service; Pa Lamin Beyai, Economic Advisor, UNDP; Akua Dua-
Agyeman, MDG Support Advisor, UNDP; Siaka Coulibaly, MDG Advisor, RSC UNDP,
Dakar; Daniela Gregr, Policy Specialist, UNDP; Ayodele Odusola, MDG Advisor,
UNDP; Shantanu Mukherjee, Policy Advisor, UNDP; Robert Mensah, NPO-RH, UNFPA;
Rhoda Manu, PMTCT-MH Specialist, UNICEF; Charles Fleischer-Djoleto, NPO-FHP,
WHO; Joseph Adomako, DDHS-Amansie West District, Ghana Health Service. We
are grateful to the consultants Alhaj Mohammed Bin Ibrahim and Moses Aikins for
their hard work in guiding the development of this document.
Design:
Phoenix Design Aid A
a carbon neutral company.
Cover photo credits:
UNDP Kayla Keenan
18605 Ghana omslag.indd 2 25/05/11 00.30

JULY 2011
GHANA
MDG ACCELERATION FRAMEWORK
A
ND
C
O
UNTRY ACTION PLAN
MATERNAL HEALTH

ACKNOWLEDGEMENTS .......................................................... 2
ABBREVIATIONS ................................................................ 8
FOREWORD ..................................................................... 10
CHAPTER 1 INTRODUCTION.................................................... 12
CHAPTER 2 PROGRESS AND CHALLENGES IN ACHIEVING MDG 5................. 22
GHAPTER 3 STRATEGIC INTERVENTIONS ………………………………………....... 40
CHAPTER 4 BOTTLENECK ANALYSIS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
CHAPTER 5 ACCELERATING MDG PROGRESS: IDENTIFYING SOLUTIONS.......... 52
CHAPTER 6 MDG ACCELERATION PLAN: BUILDING A COMPACT.................. 62
6.1 COUNTRY ACTION PLAN ............................................... 63
6.2 IMPLEMENTATION AND MONITORING PLAN............................ 72
ANNEXES ....................................................................... 80
ANNEX 1 POLICY DOCUMENTS AND REPORTS....................................... 81
ANNEX 2 QUESTIONNAIRE ADMINISTERED TO DDHS GROUP ........................ 82
ANNEX 3 MDG 5 DOCUMENTS, RECOMMENDATIONS AND LEVEL OF
IMPLEMENTATION.......................................................... 84
ANNEX 4 REFERENCES ............................................................... 87
CONTENTS
5

6
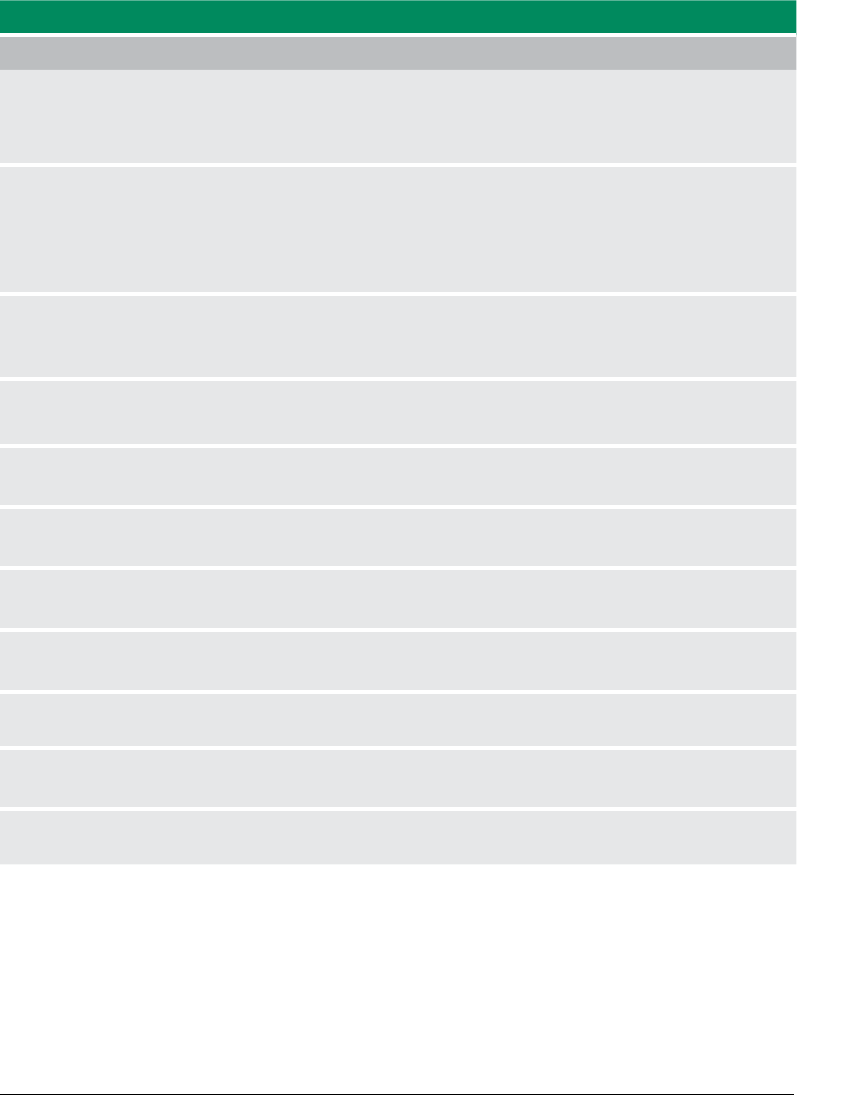
TABLE 1. HEALTH BUDGET 20062009.....................................................26
TABLE 2. TOTAL CONTRACEPTIVES FUNDING REQUIREMENTS BY PROGRAM, 20102012..30
TABLE 3. STATUS OF MDGS AND TRENDS TOWARDS ACHIEVING THEM ...................32
TABLE 4. HUMAN RESOURCE REQUIREMENTS 2010 AND STATUS AS OF 2007, GHANA ..43
TABLE 5. SUMMARY MATRIX OF KEY PRIORITY INTERVENTIONS AND INDICATIVE
INTERVENTIONS, GHANA ........................................................45
TABLE 6. SUMMARY TABLE OF BOTTLENECKS TO KEY PRIORITY INTERVENTIONS TO
ACHIEVE MDG 5 TARGETS, GHANA ...............................................49
TABLE 7. PRIORITIZED SOLUTIONS FOR ACCELERATING PROGRESS TOWARDS
MDG 5, GHANA ..................................................................56
TABLE 8. GHANA MDG 5 ACCELERATION ACTION PLAN ...................................64
TABLE 9. GHANA MDG 5 IMPLEMENTATION AND MONITORING PLAN.....................72
TABLES

7
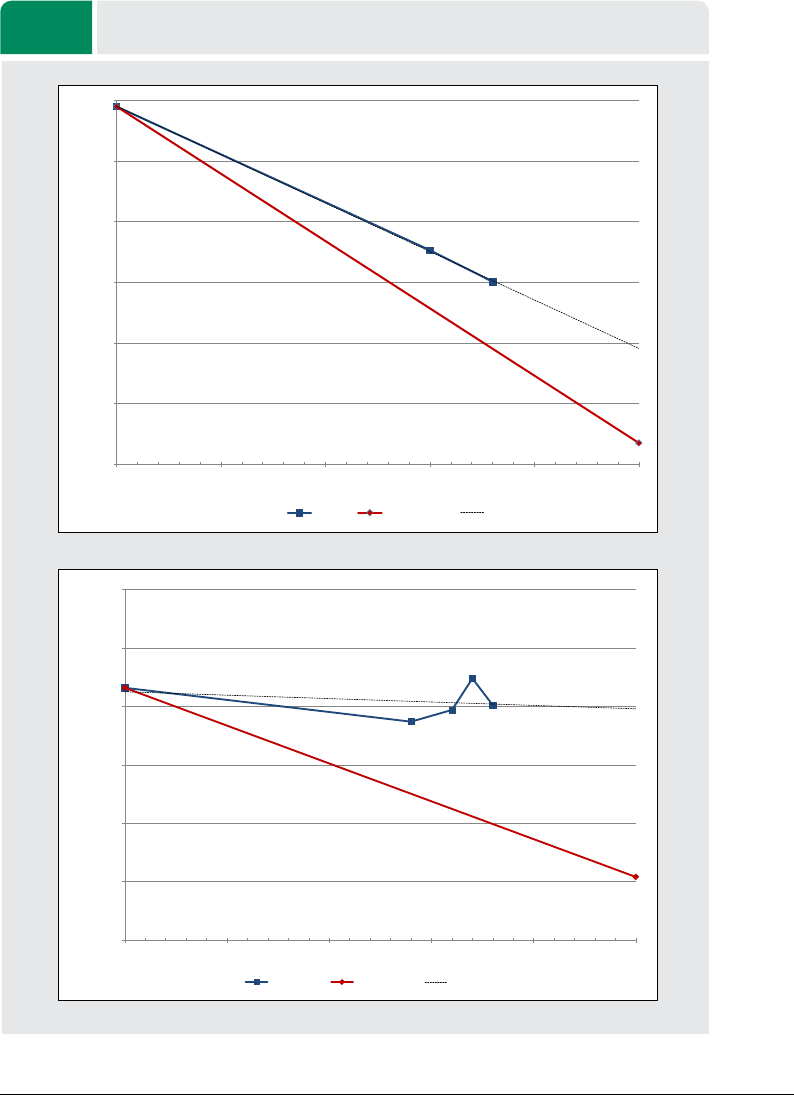
FIGURE 1. TRENDS IN MATERNAL MORTALITY .............................................24
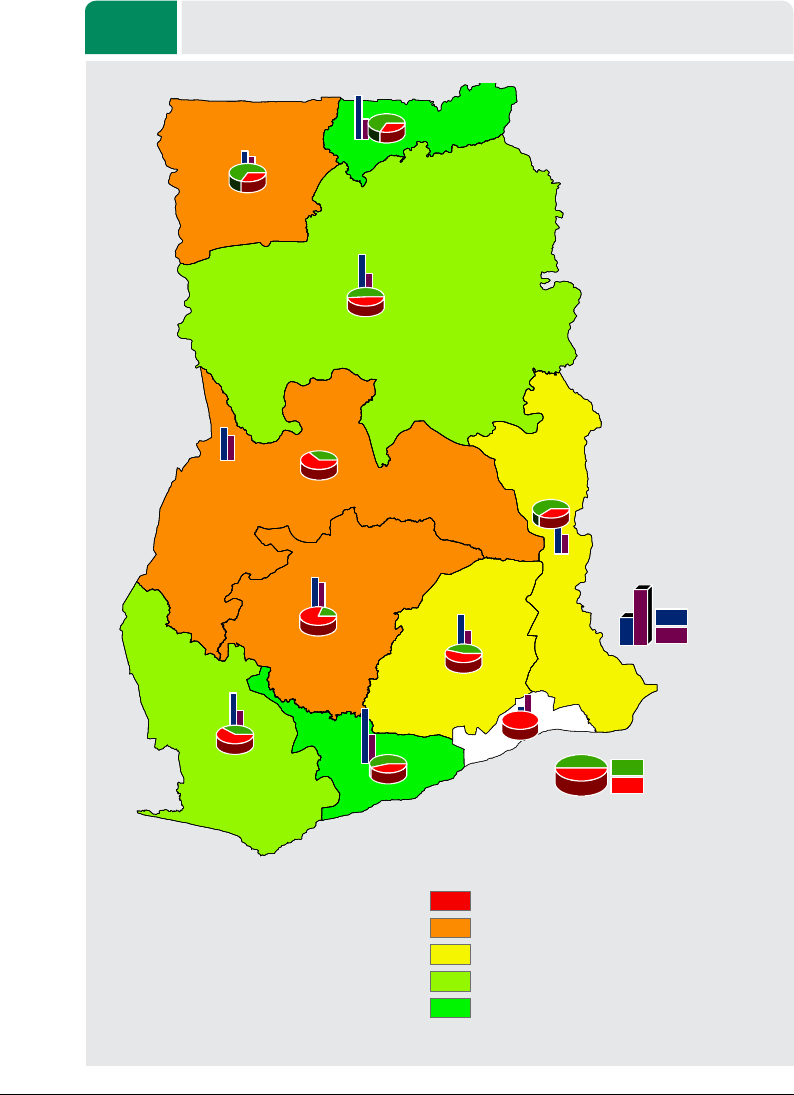
FIGURE 2. MAP OF INSTITUTIONAL MATERNAL MORTALITY RATIO IN GHANA BY REGION . 25
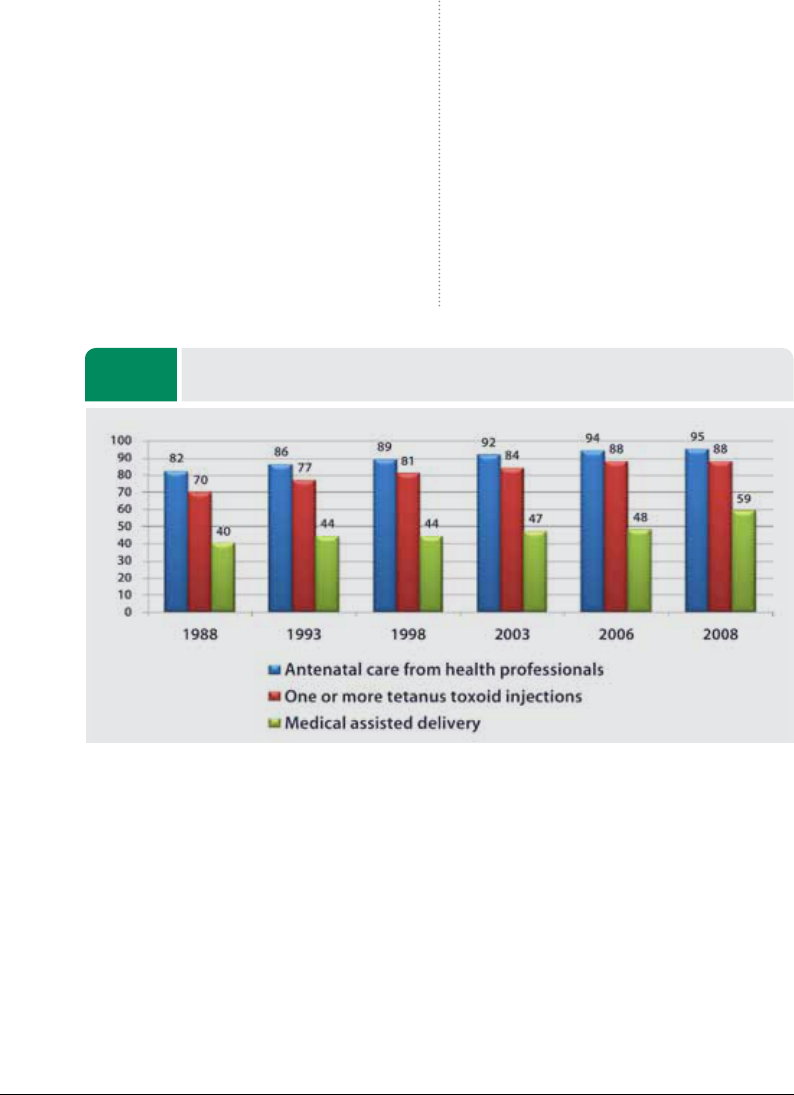
FIGURE 3. SELECTED INDICATORS OF REPRODUCTIVE HEALTH CARE, 19882008 .........27
FIGURE 4. POSTNATAL CARE COVERAGE...................................................28
FIGURE 5. FAMILY PLANNING ACCEPTOR RATE BY REGION, 20072009 ....................29
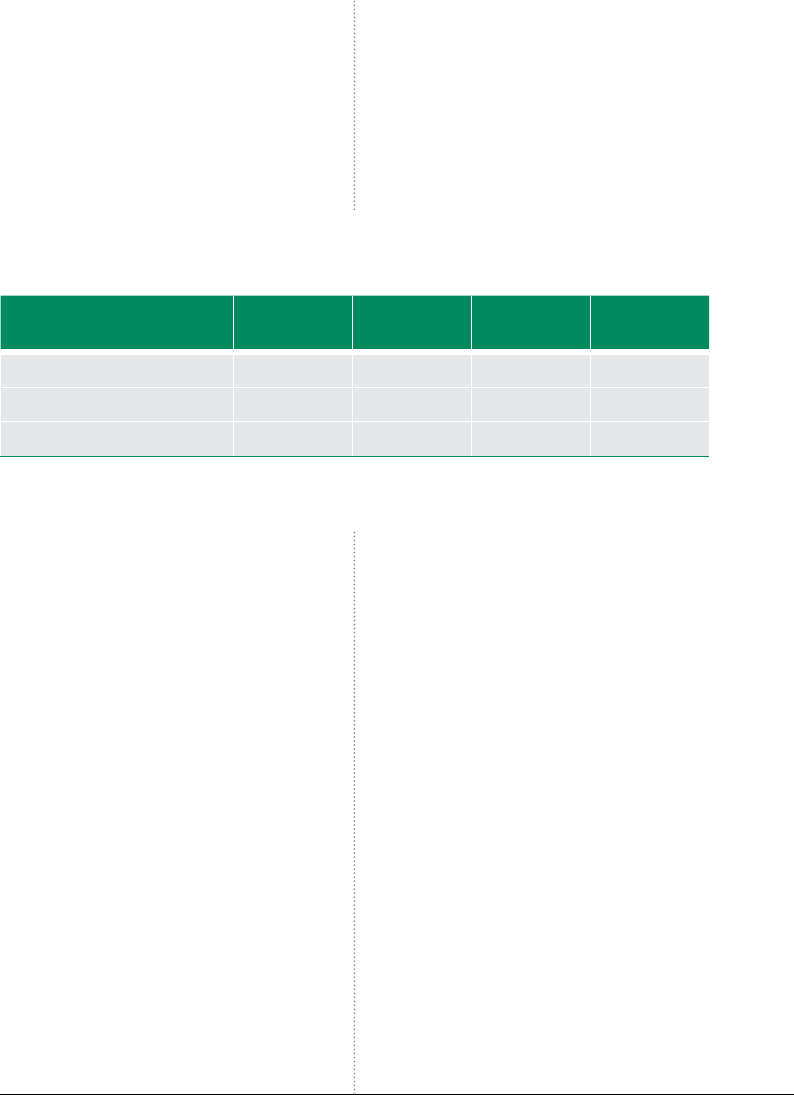
FIGURE 6. DEMAND FOR FAMILY PLANNING AMONG CURRENTLY MARRIED WOMEN .....29
FIGURE 7. VARIATIONS IN CHPS DEPLOYMENT TARGETING ................................31
FIGURES

8
ABBREVIATIONS
ANC Antenatal Care
BCC Behavioural Change Communication
BEOC Basic Emergency Obstetric Care
BTS Blood Transfusion Service
CENC Comprehensive Essential Neonatal Care
CEOC Comprehensive emergency obstetric care
CHPS Community Health Planning and Service
CSO Civil Society Organization
DAs District Assemblies
DHIMS District Health Information Management System
DHMT District Health Management Team
ENC Essential Neonatal Care
EmONC Emergency Obstetric and Neonatal Care
FP Family Planning
GAVI Global Alliance for Vaccines and Immunizations
GDP Gross Domestic Product
GHS Ghana Health Service
GNP Gross National Product
GPRS I Ghana Poverty Reduction Strategy I
GPRS II Growth and Poverty Reduction Strategy II
GNP Gross National Product
HIRD High Impact Rapid Delivery
HIV/AIDS Human Immunodeficiency Virus/ Acquired Immune Deficiency Syndrome
ICC Inter-Agency Coordinating Committee
IEC Information, Education and Communication
IUD Intrauterine Device

9
LSS Life Saving Skills
MAF MDG Accelerated Framework
MDG Millennium Development Goals
MDRI Multilateral Debt Relief Initiative
MMDAs Metropolitan, Municipal and District Assemblies
MoFEP Ministry of Finance and Economic Planning
MoH Ministry of Health
MoWH Ministry of Works and Housing
MNH Maternal and Neonatal Health
MMR Maternal Mortality Rate
NDPC National Development Planning Commission
NGO Non-Governmental Organization
NHIS National Health Insurance Scheme
PDA Personal Data Assistant
PMTCT/CT Prevention of Mother to Child Transmission/Counselling and Testing
PNC Postnatal Care
SD Skilled Delivery
STI Sexually Transmitted Infection
TOR Terms of Reference
UNAIDS Joint United Nations Programme on HIV/AIDS
UNCT United Nations Country Team
UNFPA United Nations Population Fund
UNICEF United Nations Children’s Fund
USAID United States Agency for International Development
WHO World Health Organization
WB World Bank

“The Millennium Development Goals (MDGs) are
achievable by 2015, if supported by the right set of
policies, targeted technical assistance, institutional
capacity, adequate funding and strong political
commitment. The Government of Ghana, in
collaboration with its development partners, is fully
committed to achieving the MDGs by 2015.
Recent experiences in Ghana demonstrate that
success is possible and that evidence-based effective
interventions can be identified for realizing the
MDGs. Nevertheless, although progress has been
satisfactory in MDGs 1, 2, 3, 6 and 8, it has been
less in other areas, MDGs 4, 5 and parts of 7. At the
current pace of progress, Ghana may not meet the
MDG target by 2015 with business as usual. The
present MDG Acceleration Compact capitalizes
on the existing commitment and captures the
evidence available to put forward concrete and
realistic proposals to scale up the achievement of
the MDGs in the next five years…”
This MDG Acceleration Framework (MAF) – Ghana
Action Plan was developed by the Ministry of
Health and Ghana Health Service in collaboration
with development partners particularly the United
Nations Country Team and other stakeholders in
Ghana. The focus of the Action Plan is on MDG
5 because the progress in reducing the maternal
mortality ratio by three quarters by 2015 is off
track. The 2010 MDG Report showed the maternal
mortality rate to be at 451 per 100,000 live births. The
slow progress has been of great concern to policy
decision makers to the extent that Maternal Mortality
was declared a national emergency in July 2008.
Therefore, the main reason for this MAF is to redouble
efforts to overcome bottlenecks in implementing
interventions that have proven to have worked in
reducing the maternal mortality ratio in Ghana. The
MAF focuses on improving maternal health at the
level of both community and health care facilities
through the use of evidence-based, feasible and
cost-effective interventions in order to achieve
accelerated reduction in maternal and newborn
deaths. The three key priority interventions areas
identified are improving family planning, skilled
delivery and emergency obstetric and newborn care.
At the health facility level, emphasis is placed
on the creation of an enabling environment,
including equipment and supplies, for well-trained
professionals to attend to pregnancy, childbirth
and the newborn. The community level focuses on
FOREWORD
10
11
equipping communities with knowledge and skills
to enable them to adopt good health practices and
better health-seeking behaviour and to recognize
danger signs related to pregnancy and childbirth
as well as with the newborn. This document takes
cognizance of the inseparable dyad of the mother
and the newborn as well as the interrelationships
among all the eight MDGs.
The MAF is not aimed at replacing existing
interventions. Rather, it is meant to complement
them with specific focused interventions for the
achievement of MDG 5 by 2015. To achieve that,
the Ghana MAF cannot be the business of the
government alone, but requires the support of UN
agencies, other development partners and CSOs to
better understand the deep-rooted causes militating
against positive outcomes in maternal health care
and collectively work towards overcoming them.
Once the CAP is implemented with the support of all
stakeholders, Ghana will reduce the risks of maternal
deaths and once again be on track to achieving
MDG 5 by 2015.
The declaration of His Excellency Professor John
Evans Atta Mills, President of the Republic of Ghana at
the recent African Union Heads of State Conference
in Kampala, Uganda, that “no woman should die
while giving life” is a vision that the implementation
of this Action Plan seeks people to support it
through resource mobilization, implementation
and Monitoring and Evaluation.
Minister of Health, Ghana
Hon. Dr. Benjamin Kunbuor
UN Resident Coordinator
Ruby Sandhu-Rojon

1212
Making initial plans
and establishing baselines
STAGE 1:
INTRODUCTION
Photo: Kayla Keenan
CHAPTER 1:

13
1.1: BACKGROUND
Ghana, a tropical country on the west coast of Africa,
is divided into 10 administrative regions and 170
decentralized districts. The country has an estimated
population of about 23.4 million (GSS, 2009) with a
population density varying from 897 per km
2
in the
Greater Accra Region to 31 per km
2
in the Northern
Region. Life expectancy is estimated at 56 years for
men and 57 years for women, while the adult lit-
eracy rate (age 15 and above) stands at 65 percent.
The government is a presidential democracy with
an elected parliament and independent judiciary.
The principal religions are Christianity, Islam and
Traditional African. Ghana’s economy has a domi-
nant agricultural sector (small-scale peasant farm-
ing) absorbing 55.8 percent (GLSS 5) of the adult
labour force, a small capital intensive mining sector
and a growing informal sector (small traders and
artisans, technicians and businessmen). Since in-
dependence, Ghana has made major progress in
economic growth. However, a number of questions
arise as to how to accelerate equitable growth and
sustainable human development towards attaining
middle-income country status by 2015.

14
At the turn of the century, in September 2000, Ghana,
along with 189 UN member countries adopted the
Millennium Declaration that laid out the vision for a
world of common values and renewed determination
to achieve peace and decent standards of living for
every man, woman and child. The eight Millennium
Development Goals (MDGs) derived from the Millen-
nium Declaration set time-bound and quantifiable
indicators and targets aimed at halving the proportion
of people living below the poverty line, improving ac-
cess to primary education, promoting gender equality,
reducing child mortality, improving maternal health,
combating and reversing the trends of HIV/AIDS,
malaria and other diseases, ensuring environmental
sustainability, and promoting global partnership for
development between developed and developing
countries by 2015. This set of eight clear, measurable
and time bound development goals were expected
to generate unprecedented, coordinated action, not
only within the United Nations system, including the
Bretton Woods institutions, but also within the wider
donor community and, most importantly, within de-
veloping countries themselves.
Ghana has since mainstreamed the MDGs into the
country’s successive medium-term national develop-
ment policy framework, the Ghana Poverty Reduc-
tion Strategy (GPRS I), 2003 – 2005, and the Growth
and Poverty Reduction Strategy (GPRS II), 2006–2009.
The GPRS I focuses on macroeconomic stability, pro-
duction and gainful employment, human resource
development and the provision of basic services to
the vulnerable and excluded, and good governance;
GPRS II emphasizes continued macroeconomic sta-
bility, human resource development, private sector
competitiveness, and good governance and civic
responsibility. Within the same period of the two
development policy frameworks, Ghana benefited
from the Highly Indebted Poor Country (HIPC) initia-
tive and other international development assistance
support programmes including the Multilateral Debt
Relief Initiative (MDRI), Multi-Donor Budget Support
(MDBS) and the United States-funded Millennium
Challenge Account programme, among others.
In addition to direct poverty reduction expenditures,
government expenditure outlays were also directed
at policies and programmes to stimulate growth,
which have high potential to support wealth crea-
tion and sustainable poverty reduction.
Total poverty reduction expenditure as a percentage
of total government spending declined from 34.56
percent in 2006 to 22.82 percent in 2007 and further
down to 22.3 percent in 2008 (2008 APR). In terms
of sector shares, the largest share of total poverty
spending went to basic education, which accounted
for 41.42 percent in 2007 and 47.24 percent in 2008.
This was followed by health sector spending at 19.5
percent in 2007 and 18.05 percent in 2008. Expendi-
ture on rural electrification, water supply and feeder
roads ranged from 1.57 percent to 7.23 percent in
2007 and 1.36 percent to 5.04 percent in 2008. Such
declines in poverty spending have implications for
the achievement of the MDGs despite the country
being on track to achieve poverty and related targets
which form the focus of subsequent discussions.
1.2 OVERALL PROGRESS IN
ACHIEVING THE MDGS IN GHANA
According to the 2010 MDG Report, Ghana’s progress
in achieving the MDGs is mixed. The country is
largely on track to achieve the MDG 1 target of
reducing by half the proportion of the popula-
tion living in extreme poverty. The overall poverty
rate has declined substantially over the past two
decades from 51.7 percent in 1991–1992 to 28.5
percent in 2005–2006 while the proportion of the
population living below the extreme poverty line
also declined from 36.5 percent to 18.2 percent over
the same period against the 2015 national target of
26 percent and 19 percent respectively. Although
current data on poverty is not available, trends
in economic growth suggest a further decline in
poverty between 2006 and 2008. However, de-
spite the significant decline in poverty at the national
15
level, regional, occupational and gender disparities
exist. Some regions did not record improvements
in poverty, particularly the three Northern regions
where high levels of poverty persist. Over 70 percent
of people whose incomes are below the poverty line
live in the Savannah areas. The 2009 Human Develop-
ment Report (HDR) shows Ghana’s Human Develop-
ment Index (HDI) rank had declined and inequality
remained high. Thus the high growth rate has not
necessarily been consistent with improved human
development indicators as the country continues to
face challenges in health and other social services.
With regard to MDG 1 Target 1C, halving the propor-
tion of people who suffer from hunger, Ghana is on
course to achieving the child malnutrition indicators
ahead of 2015. The prevalence of children suffer-
ing from wasting and stunting that characterized
the late nineties continued to be reversed in 2008.
The incidence of wasting has declined from a peak
level of 14 percent in 1993 to 5.3 percent in 2008,
while the occurrence of underweight children has
declined from about 23 percent in 1988 to 13.9 per-
cent in 2008. In terms of districts facing chronic food
production deficits, the trend has seen continuous
reduction from 22 in 2005 to 15 in 2006, and further
down to 12 in 2008. These achievements were made
possible as a result of numerous programmes and
interventions implemented by government, includ-
ing fertilizer subsidies and the expanded maize and
rice programmes which supported farmers with
agricultural inputs (fertilizers, improved seeds), and
subsidies to meet ploughing and labour costs.
Available data and trend analyses of MDG 2 —
achieving universal primary education — show
that Ghana is on track to achieving both the
gross and net enrolment targets by 2015. The
number of schools and enrolment rates have in-
creased tremendously over the years due to various
reforms and new policy measures instituted by the
government. The number of kindergarten schools
has increased from 14,246 in 2006–2007 to 15,449
in 2007–2008 following the government’s policy of
mandating each primary school to have a kindergar-
ten attached to it. The Gross Enrolment Ratio (GER)
for kindergarten has subsequently increased from 89
percent in 2006–2007 to 89.9 percent in 2007–2008.
The number of primary schools rose from 16,903 in
2006–2007 to 17,315 in 2007–2008, while the GER
increased from 93.7 percent to 95.2 percent over the
same period. The area where challenges exist is the
survival rate which has stagnated at 88 percent in
2007–2008 from 85.4 percent in 2006–2007.
With regard to the MDG 3 target of ensuring gen-
der parity especially at the primary and junior
high school levels, trends show that Ghana is on
track to achieving both targets, although prima-
ry level parity has stagnated at 0.96 since 2006-
–2007, while the parity at the junior high school
level increased slightly from 0.91 in 2006—2007
to 0.92 in 2007–2008. On the other hand, the parity
at the kindergarten level has declined slightly from
0.99 in 2006–2007 to 0.98 in 2007–2008. Progress to-
wards increasing the number of women in public life
suffered a setback with the reduction of the number
of women elected into parliament during the 2008
elections declining from 25 to 20. This had reduced
the proportion to below 10 percent, and puts Ghana
under the international average of 13 percent.
Although evidence shows that there has been
signicant reduction in both infant and under-
ve mortality rates in Ghana, it is unlikely that
the 2015 target of reducing the child mortality
rates will be easily met. The Ghana Demographic
and Health Survey (GDHS) 2008 showed a 30 per-
cent reduction in the under-five mortality rate, as
it declined from 111 per 1,000 live births in 2003
to 80 per 1,000 live births in 2008, while the infant
mortality rate in 2008 stood at 50 per 1,000 live births
compared to 64 per 1,000 live births in 2003. The
neonatal mortality rate also saw a decrease from
43 per 1,000 live births in 2003 to 30 per 1,000 live
births in 2008. The proportion of children aged 12
to 23 months who received the measles vaccine
increased from 83 percent in 2003 to 90 percent in

16
2008, showing an improvement in coverage in one
of the key child survival interventions (MoH, 2008;
GHS, 2003).
The key child health interventions are antenatal care
(ANC), delivery care, postnatal care, immunization,
nutrition, management of childhood illnesses and
malaria prevention. In the last decade some progress
has been made to improve child survival. Household
ownership of insecticide-treated nets has improved
to 61.6 percent (urban) and 66 percent (rural) areas,
immunization coverage is high (Penta3 87 percent,
see GHS 2008
1
), National Health Insurance Scheme
(NHIS) coverage is high, antimalaria combination
therapy is universally available and infant and child
mortality have declined (see GSS 2008
2
; MICS
3
).
Maternal health care has improved over the past
20 years albeit at a slow pace. Between 1990 and
2005, maternal mortality ratio reduced from 740
per 100,000 live births to 503 per 100,000 live
births, and then to 451 per 100,000 live births
in 2008. If the current trends continue, maternal
mortality will be reduced to only 340 per 100,000 by
2015, instead of the MDG target of 185 per 100,000
by 2015. The improvement, however, is not the same
for all regions. There are disparities in the institutional
maternal mortality rate (MMR) across the 10 regions
in Ghana from 1992 to 2008 in the Northern and
Western Regions; 120.1 per 100,000 in Volta and the
Eastern Regions; and 59.7 per 100,000 in the Upper
West, Brong Ahafo and Ashanti regions. The only
region where the ratio has worsened is in Greater
Accra (by 87.6 per 100,000). Maternal death was
declared notifiable within seven days in Ghana in
January 2006 and the notification rate in 2007 was
71.8 percent. A quarter (75.4 percent) of 751 maternal
deaths in Ghana (2007) were audited.
After a decline from a high of 3.2 percent in 2006
to a low of 2.2 percent in 2008, evidence from
the 2009 Sentinel surveillance report suggests
an increase in the HIV/AIDS prevalence rate in
Ghana to 2.9 percent in 2009. According to the
Ghana AIDS Commission, the current up-and-
down movement in the prevalence rate between
2003 and 2008 signals a leveling eect or stabi-
lization of the epidemic.
On MDG 7 – ensuring environmental sustainabil-
ity – Ghana is on track to achieve the target of
halving the proportion of people without access
to safe water. Critical challenges exist in achieving
the targets for reversing the loss of environmental
resources, reducing the proportion of people with-
out access to improved sanitation, and achieving
significant improvement in the lives of people living
in slum areas. Although up-to-date data on the rate
of forest depletion is unavailable, evidence suggests
that the country is depleting its forest cover at an
alarming rate. Between 1990 and 2005, the forest
cover declined from 32.7 percent to 24.2 percent.
While access to safe water services in rural areas
has improved considerably, there has been slow
progress on access to safe water within urban areas.
Even though Ghana has made progress in reducing
the proportion of the population without access to
improved sanitation, the target may not be achieved
by 2015 if the current trends continue. If the current
trend is maintained, the proportion of the population
with access to improved sanitation will reach 21.2
percent by 2015 instead of 52 percent. The propor-
tion of the urban population with access to improved
sanitation will be 23.4 percent instead of 55 percent
by 2015, while in the rural areas, it would be only
20.6 percent instead of 50.5 percent. Also, though
the proportion of urban population living in slums
shows a decline, if the current pattern continues, a
significant proportion (about 14 percent) will still be
living in slum areas by 2020.
In terms of global partnerships for development,
many developed countries have not met the 0.7
percent GNP target for aid. However, aid inflows to
Ghana appear to have increased in nominal terms
from $578.96 million in 2001 to $1,433.23 million
in 2008. The current concern, however, is the level
1) GHS, Disease Control and Prevention Department 2008 Annual report.
2) GSS, Demographic and Health Survey 2008.
3) MoH, Multiple Indicator Cluster Survey (MICS) 2006.
17
of increases in real terms and the quality of the aid
the country receives. In real terms, ODA inflows to
Ghana have stagnated at about 8.7 percent of GDP
between 2002 and 2008, after an initial rise from
6 percent of GDP in 1999 to 15 percent of GDP in
2001. The portfolio of aid inflows continued to be
dominated by project aid, which constitutes more
than 60 percent of ODA inflows. The global financial,
oil and food crisis appear to have impacted nega-
tively on the public debt position of Ghana, which is
gradually approaching unsustainable levels. Ghana’s
public debt as a percentage of GDP increased from
41.4 percent in 2006 to 55.2 percent in 2008.
1.3: Past and emerging
challenges and their impact on
achieving the MDGs
The global food and energy crisis, as well as the
effect of the global economic crisis and the presi-
dential and parliamentary elections between 2006
and 2008 adversely affected pro-poor expenditures.
While the debt relief fund for Highly Indebted Poor
Countries continued to fund activities in support of
both poverty reduction and growth enhancement,
the Multilateral Debt Relief Initiative(MDRI) which
came into effect in 2006 addressed the energy crisis
as well.
Prior to the onset of the financial crisis, foreign in-
flows (export earnings, investment and remittances)
were buoyant. In the beginning of 2009, however,
the country recorded a budget deficit of 14.5 percent
of GDP excluding divestiture receipts, and 11.5 per-
cent of GDP including divestiture receipts; as well as a
large current account deficit of 20.87 percent of GDP.
The country faced a high base interest rate of 27.22
percent and an average annual inflation of 18.13
percent in 2008. Average depreciation recorded was
20.6 percent and 16.1 percent against the US dol-
lar and the Euro, respectively. Ghana’s high level of
dependence on the world economy, with as much
as 30 percent of budget support from international
partners, and her strong trade links with the US and
Europe, may imply that any disturbance emanating
from the international financial system is bound to
have an effect on the domestic economy. In terms of
international trade and foreign direct investment, the
global financial crisis does not show to have created
a major setback as far as Ghana is concerned. Gold
and cocoa, Ghana’s main exports, were resilient in
the face of the crisis and as a result of investments
in the oil and gas fields, foreign direct investment
has increased. It cannot therefore be argued that
developments in international trade and FDI nega-
tively affected the achievement of any of the MDGs
in Ghana. However, the crisis brought with it negative
consequences for the financial markets. Banks have
been reluctant to provide credit to households, to
small and medium enterprises (SMEs) as well as to
big businesses, for fear of loan defaults. In addition,
discount, interest, prime and lending rates have in-
creased. As far as the stock market is concerned, the
all-share index fell drastically and trade volume has
also decreased. These developments have affected
share prices paid to clients which may have further
affected incomes of households.
The impact of climate change is now more than
ever before being felt. There is clear evidence that
the potential negative impacts of climate change
are immense, and Ghana is particularly vulnerable
due to its lack of capacity to undertake adaptive
measures to address environmental problems and
the socio-economic costs of climate change (EPA,
2000). For instance, in agricultural areas, particularly
in the central and northern regions of the country,
climate change has contributed to the deterioration
of rural livelihoods, reflected in declining incomes,
malnutrition and hunger. The flooding of coastal
areas, which are already undergoing erosion, and low
operating water levels of the only hydro-generating
dam in the country are further problems. The vul-
nerability of people to daily shocks and stresses is
intrinsically tied to the human adaptive capacity —
and strategies created — to respond to floods, high
18
temperatures, coastal erosion, rises in the sea level,
and other climate-related events. Climate change
is likely to exacerbate these shocks and stresses,
particularly among the poorest and most vulnerable
populations and, therefore, may inhibit the attain-
ment of the MDGs. The evidence of the implications
of these phenomena for the attainment of the MDGs
in Ghana may have been underreported. It is impor-
tant that this is given the needed attention since
it has the potential of not only eroding the gains
already made, but also pf frustrating efforts being
made to achieve the goals.
1.4: THE MAF, CAP AND
OBJECTIVES
Various studies have indicated that globally achiev-
ing MDG 5 is off track and is not likely to be achieved
in many countries, Ghana included, as both targets
for measuring progress appear not to have been
reached so far. A number of reviews have been made,
challenges to implementation identified and various
recommendations made. The number of policy
documents, strategic plans and review reports on
maternal health and reducing maternal mortality
is very impressive. But implementation has almost
always stalled, leading to minimal impact on the
MMR. In the opinion of one of our development
partners, “Many action plans, initiatives and working
groups exist in Ghana to tackle MDG 5. We know
the specific interventions required to achieve MDG
5 — these are well detailed in the various plans and
initiatives. Several of these initiatives have been fully
costed, so we even have a sense of the resources
required. We do not require another action plan
specifying what interventions to carry out, nor do we
need another analysis of why maternal mortality is
high in Ghana.” He goes on to indicate that “what we
need is why the specific interventions have not been
implemented”. Unfortunately, these recommenda-
tions for implementing the proposed interventions
and overcoming identified bottlenecks are scattered
in many documents, making it difficult to monitor
the progress of implementation. As we approach
the target year of 2015, all the identified bottlenecks,
recommendations and action plans scattered in the
various documents need to be brought together to
help understand why the known specific interven-
tions were not implemented.
The MAF, introduced by the UN System, falls in line
with the concerns and priorities of the Government
of Ghana. Thus the selection of Ghana along with 10
countries (four in Africa — Ghana, Tanzania, Togo and
Uganda) to develop a Country Action Plan (CAP) or
the acceleration of MDG 5, which is off track. MDG 5
is not likely to be attained by 2015 if efforts are not
redoubled. The Ghana CAP contains the elaboration
of the key prioritized interventions that are required
to achieve MDG 5, identifies the bottlenecks to the
interventions and suggests cost-effective solutions
to address the bottlenecks and accelerate progress.
The CAP includes an implementation and monitor-
ing plan for tracking progress. This is expected to
enable Ghana to address the critical constraints that
hamper the progress towards achieving MDG5 and
put maternal mortality target back on track by 2015.
1.4.1: MAF objectives
The MAF aims at supporting national governments,
UN agencies and other development partners and
civil society organizations ( CSOs) working in the
MDG areas to better understand the key causes af-
fecting positive outcomes in a particular MDG, find
key solutions and develop an action plan that can
help to reduce the risks hampering progress of that
MDG. In the case of Ghana, the MAF objectives
seek to:
• reviewexistingpoliciesandinterventionsinthe
area of MDG 5 i.e., maternal health care;
19
• identifythekeybottleneckstotheimplementa-
tion and attainment of MDG 5;
• identifygapsinexistingpoliciesandinterventions;
• developcost-eectivesolutionsthatcanacceler-
ate progress towards the attainment of MDG 5;
• designanactionplanforimplementingtheindica-
tive interventions and monitor progress.
1.4.2: Methodology used in
preparing the MAF CAP
An interactive and participatory approach was
adopted for the MAF roll-out. A National Technical
Team was established and two resource persons
were recruited to manage day-to-day activities. A
desk review of national policy documents, reports
and roadmaps was undertaken covering 30 national
reports on maternal health care delivery and 37 Na-
tional Policy Documents. To fill in the information
gaps, focus group discussions and rapid survey ques-
tionnaires to District Directors of Health Services
were also carried out. Consultative meetings of the
technical team were organized to review the initial
findings (in terms of interventions and bottlenecks)
and answer the question: Why have the specific
interventions not been implemented? The key inter-
ventions, bottlenecks and solutions were prioritized
using the method of ranking (high/medium/low)
and selection criteria (impact, sustainability, speed,
resources). Based on the findings, the technical team
worked during workshops and consultations to de-
velop the draft CAP.
1.4.3: MAF consultative process
The process of the MAF roll-out, including the prepa-
ration of the CAP, was nationally driven, interactive
and participatory, and carried out under the overall
leadership of the MoH. Ownership was further en-
hanced by engaging multiple stakeholders drawn
from key sector ministries, CSOs, the UN Country
Team (UNCT) and development partners involved
in supporting maternal health care interventions.
Stages for the MAF roll-out and preparation of the
CAP were as follows:
A UNDP-led consensus building and introduction
of the MAF with the key government sector, MoH,
which in turn led to close consultation with key UN
agencies (WHO, UNICEF, UNFPA, UNDP) to establish
an inter-agency National Technical Team. The Minis-
try of Health(MoH) and UN agencies identified the
MAF as timely and in line with their efforts to finding
a solution to the high maternal mortality in Ghana.
• AnationalproposalontheMAFroll-outwasde-
veloped and Ghana entered into a collaboration
with the global UNDP MAF team for financial,
technical and advisory support for the process.
• TheGovernmentofGhanaorganizedanincep-
tion meeting with selected partners including
the UNCT and agreed on the methodology and
identified bottlenecks for analysis, and reviewed
and adopted the action plan for MAF implementa-
tion.
• ANationalTechnicalTeamthatcomprisedthe
MoH, UNICEF, UNFPA, WHO and UNDP was es-
tablished by the MoH to support the MAF roll-
out. While the specialized UN agencies provided
technical inputs, UNDP played a coordinating role
and provided quality assurance.
• Twonationalconsultantswererecruitedtofurther
support the Technical Team and manage the day-
to-day process of the MAF roll-out.
• Initialactivitiesinvolved(i)adeskreviewofNa-
tional Policy Documents, reports and roadmaps
(30 national reports on maternal health care

20
delivery, 37 National Policy Documents). The re-
cently completed MDG Report for 2010 provided
additional data and information on the MDGs
including the impact (existing/potential) of the
global economic crises and climate change on the
attainment of the MDGs. Focused group discus-
sions and rapid survey questionnaires to District
Directors of Health Service were also conducted.
•
The National Technical Team with the consultants
and the UN inter-agency team, including a Re-
source Person from UNDP Regional Service Center,
Dakar, undertook a five-day working session in
Kumasi and reviewed the necessary interventions,
identified and prioritized bottlenecks as well as se-
quenced the solutions to remove the bottlenecks
for effective implementation to accelerate MDG 5.
• TheTechnicalTeamfurtherreconvenedinAccra
to prepare the draft CAP including the Monitoring
& Evaluation framework. At that point, additional
resource persons from UNDP Regional Bureau for
Africa (RBA) and Bureau for Development Policy
(BDP) joined the team to share global experiences
in the MAF process and provided technical inputs for
quality assurance in line with the global programme.
• TheNationalTechnicalTeambriefedUNCTaday
prior to the validation meeting to share the find-
ings, and received inputs for consideration mainly
in the areas of nutrition, gender empowerment,
girls’ education, HIV/AIDS and sexually transmitted
infections in pregnancy and childbirth.
• On12August2010,avalidationmeetingwas
organized with the wider stakeholders to discuss
and build consensus on the draft MAF CAP. The
validation provided further comments and recom-
mendations that further enhanced the quality and
ownership for the CAP. In all, 15 Agencies and 35
participants were represented.
• TheNationalTechnicalTeam,includingtheUN
Country Team, incorporated stakeholders’ com-
ments and contributions into the MAF CAP.
• Thedocumentwasdulyendorsedandnalizedas
a true reflection of Ghana’s MAF National Action
Plan for the acceleration of MDG 5 over the next
five years until the target date of 2015.
From the review of the existing policies and interven-
tions available for attaining MDG 5 in Ghana, the
team assessed the implementation status (whether
partially or not implemented) and the expected con-
tributions to the acceleration of MDG 5. It identified
and ranked the various interventions by using the
following set of criteria: impact, sustainability, speed,
coverage and available capacity for the intervention.
The three key interventions that emerged as having
great impact on maternal health were family plan-
ning (FP); skilled delivery services (SD); and emer-
gency obstetrics and neonatal care (EmONC).
Using the above three key intervention areas, the
team identified and prioritized the key bottlenecks
by answering questionnaires and ranking the bot-
tlenecks as high, medium or low/small, in the areas
of policy/planning, financing, service delivery, service
utilization and cross-cutting on the interventions.
The bottlenecks that emerged from this ranking
included accessibility, availability, coverage, knowl-
edge, acceptance, poverty, quality and intersecto-
ral coordination. Using available costing, the team
developed cost-effective solutions for the three in-
terventions to accelerate progress of MDG 5 using
‘accelerating solutions prioritization criteria’ based
on impact (magnitude, speed and sustainability)
and feasibility (governance, capacity and funding
availability).
The outputs from the overall MAF process included
(i) an analysis of the national-, regional- and
district-level constraints to implementing the
well-defined actions required to make progress on
MDG 5, with emphasis on answering the question:
21
Why have the specific interventions not been im-
plemented; (ii) a two-to-three-year business plan/
CAP outlining how all stakeholders could work to-
gether to implement the various plans and initiatives.
The CAP elaborates on key prioritized interventions
that are required to achieve MDG 5, identifies the
bottlenecks, and suggests cost-effective solutions
to address the bottlenecks and accelerate progress.
It also contains an implementation and monitoring
plan for tracking progress. All these are with a view
to addressing the critical constraints that hamper
progress towards reducing maternal mortality in
Ghana and once again put the country on track to
achieving MDG 5 by 2015.
1.4.4: September 2010 MDG
Summit
In September 2010, 10 years after the historical event
of the MDG declaration in 2000, the global leaders
involved in formulating the declaration met again to
review the progress made, and galvanized political
commitment and collective action towards the 2015
deadline. In line with the country’s own concerns and
plans, Ghana was selected by the UN system along
with 10 countries (four in Africa — Ghana, Tanzania,
Togo and Uganda) to develop a CAP for the accelera-
tion of MDG 5. The results of the pilot, which was part
of a synthesis report, was tabled at the 2010 MDG
Summit in September 2010 in New York.

PROGRESS AND CHALLENGES
IN ACHIEVING MDG 5
Photo: Kayla Keenan
CHAPTER 2:
23
2.1: OVERVIEW OF MDG REPORT
2010 ON MDG 5 MATERNAL
MORTALITY IN GHANA
Although Ghana has achieved progress in the past
10 years of MDG implementation, challenges of in-
equalities, geographical disparities and sustaining
progress still remain. With only five years remaining
to the MDG deadline, Ghana will have to accelerate
its efforts towards the achievement of all the MDGs,
especially those lagging behind such as MDG 4 (child
mortality), MDG 5 (maternal health) and part of MDG
7 (environment). The death of a mother, especially
during pregnancy, is a calamity for the family, com-
munity and society at large, something that has
been long accepted by all societies. Consequently,
it has been a concern of the international commu-
nity and various governments to initiate policies,
programmes and strategies to improve maternal
health and reduce maternal mortality and morbidity.
Unfortunately, the MMR is just too high in developing
countries, including Ghana, and the indicator is ac-
cepted as a key to assessing the level of development
of a particular country. While the MMR in developed
regions was 9 per 100,000 live births in 2008, the ratio
was 450 per 100,000 in developing regions (MDG
Report 2010). Obviously, a lot needs to be done in
developing regions to bring down the MMR if MDG
5 is to be achieved.
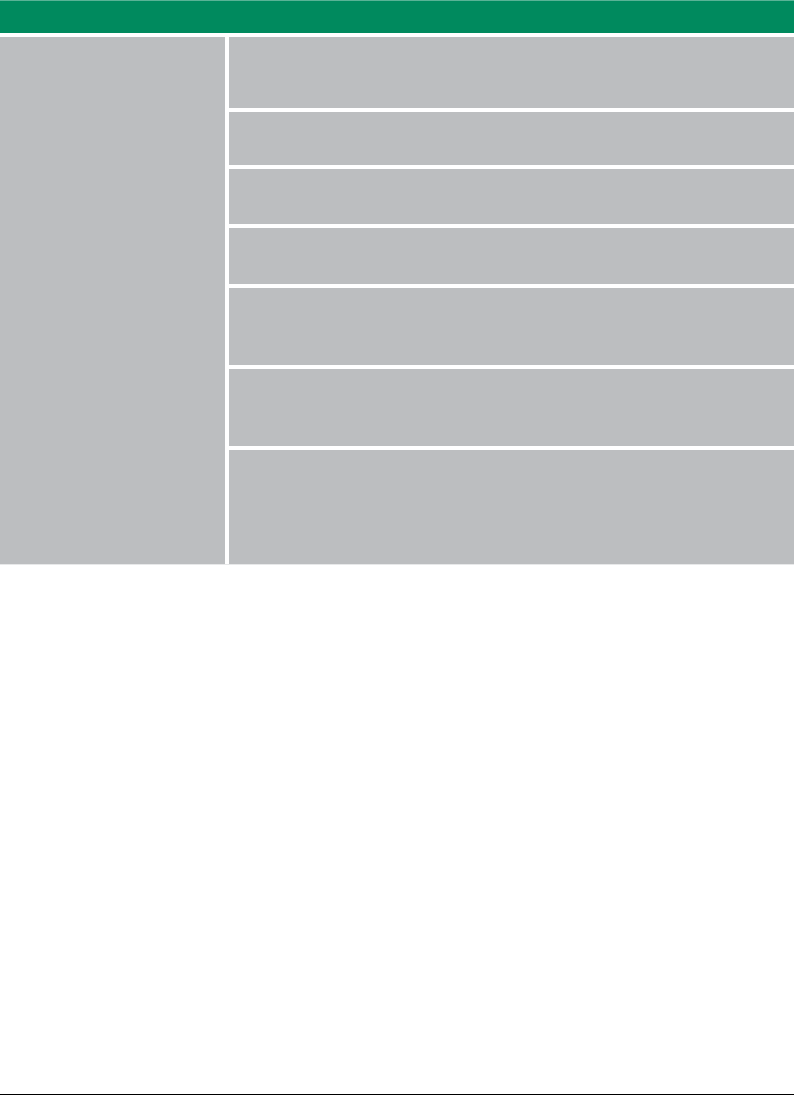
The MMR as captured by both survey and insti-
tutional data has shown an improvement over
the past 20 years. However, the pace has been
slow. Between 1990 and 2005, it reduced from
740 to 503 per 100,000 live births and then to 451
deaths per 100,000 live births in 2008. This trend
is also supported by institutional data which suggest
that maternal deaths per 100,000 live births have
declined from 224 per 100,000 in 2007 to 201 per
100,000 in 2008, after an increase from 187/100,000
in 2004 to 197 per 100,000 in 2006. If the current
trends continue, maternal mortality will be reduced
to only 340 per 100,000 by 2015 instead of the MDG
target of 185 per 100,000 by 2015. Moreover, the
improvements recorded are not evenly distributed.
There are disparities in the MMR (institutional) across
the 10 regions in Ghana from 1992 to 2008. The MMR
has decreased to 195.2 per 100,000 in the Central and
Upper East regions; 141 per 100,000 in the Northern
and Western Regions; 120.1 per 100,000 in Volta and
the Eastern Regions; and 59.7 per 100,000 in the
Upper West, Brong Ahafo and Ashanti regions. The
only region where the MMR has worsened is Greater
Accra (by 87.6 per 100,000) (fig. 2). This shows a clear
inequity in the per capita distribution of health facili-
ties and health personnel across the various regions
and districts and underscores the need to improve it.
Unless extreme efforts are made by all stakeholders,
Ghana is unlikely to meet the MDG target (fig.1). The
Ghana Maternal Health Survey 2007 found that 14
percent of deaths of women within the reproductive
age are childbirth-related and identified hemorrhage
(24 percent) as the largest single cause of maternal
deaths; abortion was the second single largest cause
of death, accounting for 15 percent. Hypertensive
disorders, sepsis, and obstructed labour were also
cited as causes of maternal death.
The MMR remains unacceptably high in Ghana in
spite of the efforts being made to reduce it. Maternal
health has remained a national priority and as such,
has become a core indicator for poverty reduction
in the Ghana Poverty Reduction Strategy (GPRS).
Additionally, improving maternal health and thereby
reducing maternal mortality is one of the priorities
of the health sector’s programme of work (POW).
24
Figure 1 TRENDS IN MATERNAL MORTALITY
Source: Ghana’s Health Sector Review Report, 2009; MOH, 2008.
740
503
451
150
250
350
450
550
650
750
1990 1995 2000 2005 2010 2015
Maternal Mortality Rate (per 100,00 live births)
Survey
Survey Path to Target Linear Trend
216
187
197
224
201
0
50
100
150
200
250
300
1990 1995 2000 2005 2010 2015
Maternal Mortality Rate (per 100,00 live births)
Instuonal
Instuonal Path to Target Linear Trend
25
Source:
Centre for Health Information Management
Ministry of Health
Northern (141.9)
Brong Ahafo (59.7)
Ashanti (42.7)
Volta (113.9)
Western (130.2)
Eastern (120.1)
Upper West (42.4)
Upper East (179.2)
Central (195.2)
Greater Accra (-87.6)
Baseline
Current Status
Portion of target met
Portion remaining
Maternal Mortality Ratio - Institutional
Change in affected population 1992 - 2008
Condition worsened by -87.6 per 100,000
Improved by up to 59.7 per 100,000
Improved by up to 120.1 per 100,000
Improved by up to 141. per 100,000
Improved by up to 195.2 per 100,000
Prepared for National Planning Commission (Ghana)
By African Centre for Statistics, UNECA
April 2010
Figure 2 MAP OF INSTITUTIONAL MATERNAL MORTALITY RATIO IN GHANA
BY REGION
26
While acknowledging the importance of focusing on
MDG 5, we also recognize that all the eight MDGs
are interrelated and mutually reinforcing. Poverty,
gender inequality, low productivity, inadequate
income opportunities, poor education, environ-
mental non-sustainability are all undermined
if health care is poor and the reverse is true in
some cases. For instance, MDGs 4, 5 and 6 are close-
ly linked. The mother is the fulcrum around which
family life revolves and her death jeopardizes the
survival of her young children. For example, the risk
of death for children under five is higher for those
whose mothers die in childbirth than those with
living mothers. Reducing death in pregnancy and
childbirth does not only improve the productivity
of women, and increase labour supply and the eco-
nomic well-being of communities, but is arguably
also a human r
ights issue. Given the numerous is-
sues that beset maternal health care leading to slow
progress in achieving MDG 5, and the inter-linkages
between improved maternal health and MDG 4, the
MAF roll-out in Ghana chose to focus on MDG 5. The
status of the MDGs in Ghana over the last 10 years
is shown in table 3.
2.2: OVERALL ASSESSMENT OF
PROGRESS TOWARDS MDG 5
Policy measures for improving health care services
in general, and maternal care in particular, are en-
shrined in the national development policy frame-
works including the GPRS I, GPRS II and the draft
Medium-Term National Development Policy Frame-
work 2010–2013 as well as specific health sector poli-
cies. Furthermore, Ghana has numerous initiatives in
place to address the issue of maternal mortality but
the results have not led to desirable improvement
in MDG 5. Particular initiatives put in place to ad-
dress the high levels of maternal deaths include the
Safe-Motherhood Initiative, Ghana Vitamin A Supple-
ment Trials (VAST) Survival Programme, Prevention
of Maternal Mortality Programme (PMMP), Making
Pregnancy Safer Initiative, Prevention and Manage-
ment of Safe Abortion Programme, Intermittent
Preventive Treatment (IPT), Maternal and Neonatal
Health Programme and the Roll Back Malaria Pro-
gramme. However, funding and other cross-cutting
constraints have hampered the full implementation
of some of the initiatives.
Resource allocation to the health sector in nominal
terms has increased over the years. However, as a
percentage of the national budget it declined from
16 percent in 2006 to about 12.76 percent in 2009.
TABLE 1 HEALTH BUDGET 20062009
Year 2006 2007 2008 2009
MoH 478,654,800 563,756,400 752,233,368 921,929,472
National budget 2,948,398,300 3,869,832,200 5,059,808,063 7,226,913,484
Total share of health in the
national budget 16.23% 14.60% 14.90% 12.76%
Source: Annual Budget Statement, MoH, Government of Ghana.
27
Apart from the general bottlenecks that affect the
entire health system of the country, there are also
specific urban and rural challenges with implica-
tions for maternal mortality. Antenatal care from
health professionals (nurses, doctors, midwives
or community health officers) increased from 82
percent in 1988 to 95 percent in 2008 (see figure
3). However, the progress is unevenly distributed.
While women in urban areas receive more antenatal
care from health professionals (98 percent) than
their rural counterparts (94 percent) the regional
figures are different: 96 percent to 98 percent of
women across all the regions received antenatal
care from health professionals. The exception is
women in Volta and the Central regions whose
antenatal care access rate is estimated at 91 percent
and 92 percent respectively. However, the lack of
information available to women about signs of
complications in pregnancy, and access to basic
laboratory services, particularly in the Northern and
Upper West regions, affect the quality of antenatal
care. In the Northern and Upper West regions, only
six in 10 pregnant women, and two in three have
access to urine testing and blood testing respec-
tively. These are against the national average of 90
percent access to these services.
Figure 3 SELECTED INDICATORS OF REPRODUCTIVE HEALTH CARE,
19882008
Source: Ghana Statistical Service (2005, 2008), Ministry of Health (2006).
28
Deliveries that were assisted by a health profes-
sional recorded slow progress, increasing from
40 percent in 1988 to 59 percent in 2008. In the
Northern region, one in four compared to four in
five children in the Greater Accra region are likely
to be delivered in a health facility. Professional
assistance at birth for women in urban areas was
found to be twice as likely to occur as in rural
areas (MOH, 2008a). The available data show that
over 40 percent of women did not deliver in a
health facility because some of them thought
it was unnecessary to do so, while others cited
lack of money, accessibility problems like distance
to a health facility, transportation problems, not
knowing where to go, and the unavailability of
someone to accompany them to the facility. The
Reproductive and Child Health Policy recom-
mends a minimum of four visits per client and a
haemoglobin check at registration and at term.
The four-plus visit coverage has stayed below
60 percent against the target of 80 percent and
the proportion of women whose haemoglobin is
checked at term remains below 10 percent.
While puerperal sepsis is a significant cause of
maternal deaths, postnatal care coverage has per-
sistently remained low and stagnated between 53
percent and 56 percent from 2001 to 2007 (fig. 4).
Figure 4 POSTNATAL CARE COVERAGE
FP prevents unwanted pregnancy and reduces the
risk of maternal deaths from pregnancy-related com-
plications and unsafe abortions. But the FP acceptor
rate has seen only a marginal rise from 21.2 to 25.4
percent of women in their reproductive age between
2007 and 2009. Greater Accra and the Western and
Ashanti regions have particularly low acceptor rates.
The Upper West and Brong Ahafo regions record
the highest FP acceptor rates (fig. 5). The preferred
methods are Depo (44.3 percent), male condom
(27.7 percent), combined pills (15.9 percent) and
injectable Norigynon.
54.2
53.4
55.7
53.3
55
53.7
56.7
50
52
54
56
58
2001 2002 2003 2004 2005 2006 2007
Postnatal Care Coverage(%)
29
Figure 5 FAMILY PLANNING ACCEPTOR RATE BY REGION, 20072009
0
10
20
30
40
50
60
70
80
90
AS BA CR ER GAR NR UE UW VR WR NAT
2007
2008
2009
Figure 6 DEMAND FOR FAMILY PLANNING AMONG CURRENTLY MARRIED
WOMEN
30
Ghana has a National Contraceptive Security (CS)
Strategic plan, supported by a Financial Sustain-
ability Plan (FSP). In 2007, however, there was a “near
crisis” in the supply of male condoms as the country
almost ran out of stock of Neo Sampoon spermicide,
which is the most preferred type. The demand for
FP among currently married women is 59 percent,
out of which only 24 percent have their demand
satisfied and 35 percent have an unmet need (fig.
6). The main challenges in FP include contraceptive
security issues (funding gap in procurement, and in
information, education and communication) and
method-specific issues (low patronage of contracep-
tive devices such as intrauterine devices (IUDs) and
female condoms due to low male involvement and
fear of side effects). The current funding requirement
(2010–2012) prior to the MAF process is estimated
at $41.2 million as shown in table 2.
TABLE 2 TOTAL CONTRACEPTIVE FUNDING REQUIREMENTS BY PROGRAMME, 20102012
IN MILLIONS USD
Product 2010 2011 2012 Total
MoH (PPAG/MBI) 11.6 8.4 13.5 33.5
EXP SM 2.9 2.4 2.4 7.7
TOTAL 14.5 10.8 10 41.2
The Community Health Planning and Service (CHPS)
was initiated in Ghana in 2000 to bridge the equity
gap in health services by partnering health pro-
vider and community efforts, to bring health services
closer to the doorstep of households. It involves
subdividing sub-districts (15,000–30,000 population)
into zones with a population of 2,000 to 5,000, as-
signing trained health workers, providing them with
logistics and with support from community health
volunteers, delivering preventive and curative care
and in some cases midwife services. Currently, it is
estimated that 2,200 CHPS zones are functional in
Ghana (fig. 7). While the concept is good, it is chal-
lenged by inconsistent targeting (both in numbers
and in relation to the Ghana poverty map), lack of
human resources and very often a different interpre-
tation of what constitutes a functional CHPS zone.

31
Behavioural change communication (BCC) is another
key initiative to create awareness about pregnancy
risk factors and danger signs, and increase demand
and utilization of antenatal services, SD services,
EmONC and postnatal care. The programme uses
the media to inform, educate and communicate
messages to promote the adoption of desired be-
haviours; prints posters, leaflets and fliers; engages in
advocacy; involves traditional leaders and religious
leaders and groups, and so on. Recently, with support
from UNICEF, the Health Promotion Department of
the Ghana Health Service (GHS) developed a com-
mon framework for behavioural change termed
‘Communication for Development’ (C4D).
The high maternal mortality in the country was de-
clared a national emergency in 2008 and therefore
emphasized the need to assign a higher priority to
reproductive health services. Unfortunately, resource
allocation was not aligned to match this good pol-
icy declaration. Furthermore, there is no systematic
tracking of set targets such as focused antenatal
care coverage, the percentage of facilities offering
basic emergency obstetric care (BEOC), the percent-
age of districts offering comprehensive emergency
obstetric care (CEOC), and the percentage of districts
with transfusion service. Issues of accessibility often
emerge as a bottleneck for pregnant women, par-
ticularly in rural areas. Sometimes, pregnant women
are not able to afford transport or do not know where
to access maternal health services.
Figure 7 VARIATIONS IN CHPS DEPLOYMENT TARGETING
0 0 0 0
73
-58
-38
-62
-22
-56
-16
-19
-14
5
0
10
20
30
40
50
60
70
80
2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 )2015
CHPS Deployment Differences in Target
Yearly difference
32
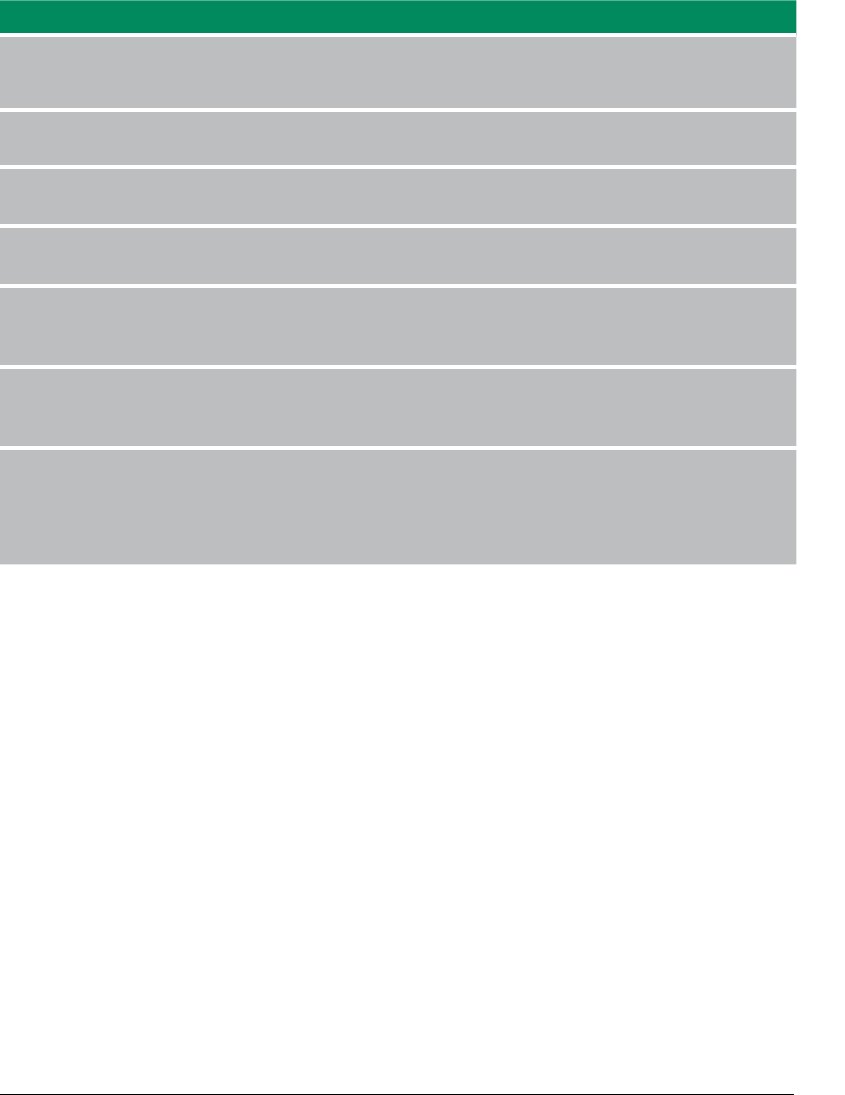
TABLE 3 STATUS OF MDGS AND TRENDS TOWARDS ACHIEVING THEM
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 1. Eradicate Extreme
Poverty and Hunger
a. Halve the proportion of
people below the extreme
poverty line by 2015
b. Halve the proportion of
people who suer from hunger
Proportion below
extreme poverty
(national basic needs) line (%)
Proportion below
upper poverty line (%)
Proportion of children
malnourished (%)
-Underweight
- Stunting
- Wasting
26.8
39.5
23 (1988)
34
(1988)
9
(1988)
-
-
23
33
(1993)
14
(1993)
-
-
20 (1998)
31
(1998)
10.0
(1998)
-
-
18
35
8
-
-
-
-
-
-
-
-
-
-
18.0
28.5
-
-
-
-
-
-
-
-
-
-
13.9
28
9
18.5
25.8
15.5
15
3.8
Goal 2: Achieve Universal
Primary Education
Achieve universal access to
primary education by 2015
- Gross enrolment ratio (%)
- Net primary
enrolment ratio (%)
- Primary completion/
survival rate (%)
72.7 (1990)
54 (1990)
63 (1990)
79.5 (2000)
61 (2000)
63 (2000)
-
-
-
-
-
-
-
-
83.2
85.7
59.1
82.6
92.1
69.2
75.6
93.7
81.1
85.4
95.2
83.7
88.0
100
100
100
Goal 3: Promote Gender
Equality and Empower Women
a. Eliminate gender disparity in
primary and junior secondary
education by 2009
b. Achieve equal access
for boys and girls to senior
secondary by 2009
Ratio of females to males in
primary schools (%)
Ratio of females to males in
junior secondary schools (%)
Ratio of females to males in
senior secondary schools (%)
Percentage of female
enrolment in senior secondary
schools (%)
-
-
-
-
-
-
-
-
0.92
0.88
-
-
0.77
0.88
-
-
0.93
0.88
-
-
0.95
0.88
-
43.5
0.95
0.88
-
49.5
0.96
0.91
-
-
0.96
0.92
-
-
1.0
1.0
-
-
33
TABLE 3 STATUS OF MDGS AND TRENDS TOWARDS ACHIEVING THEM
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 1. Eradicate Extreme
Poverty and Hunger
a. Halve the proportion of
people below the extreme
poverty line by 2015
b. Halve the proportion of
people who suer from hunger
Proportion below
extreme poverty
(national basic needs) line (%)
Proportion below
upper poverty line (%)
Proportion of children
malnourished (%)
-Underweight
- Stunting
- Wasting
26.8
39.5
23 (1988)
34
(1988)
9
(1988)
-
-
23
33
(1993)
14
(1993)
-
-
20 (1998)
31
(1998)
10.0
(1998)
-
-
18
35
8
-
-
-
-
-
-
-
-
-
-
18.0
28.5
-
-
-
-
-
-
-
-
-
-
13.9
28
9
18.5
25.8
15.5
15
3.8
Goal 2: Achieve Universal
Primary Education
Achieve universal access to
primary education by 2015
- Gross enrolment ratio (%)
- Net primary
enrolment ratio (%)
- Primary completion/
survival rate (%)
72.7 (1990)
54 (1990)
63 (1990)
79.5 (2000)
61 (2000)
63 (2000)
-
-
-
-
-
-
-
-
83.2
85.7
59.1
82.6
92.1
69.2
75.6
93.7
81.1
85.4
95.2
83.7
88.0
100
100
100
Goal 3: Promote Gender
Equality and Empower Women
a. Eliminate gender disparity in
primary and junior secondary
education by 2009
b. Achieve equal access
for boys and girls to senior
secondary by 2009
Ratio of females to males in
primary schools (%)
Ratio of females to males in
junior secondary schools (%)
Ratio of females to males in
senior secondary schools (%)
Percentage of female
enrolment in senior secondary
schools (%)
-
-
-
-
-
-
-
-
0.92
0.88
-
-
0.77
0.88
-
-
0.93
0.88
-
-
0.95
0.88
-
43.5
0.95
0.88
-
49.5
0.96
0.91
-
-
0.96
0.92
-
-
1.0
1.0
-
-
34
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 4: Reduce Child Mortality
Reduce under-ve mortality by
two-thirds by 2015
- Under-ve mortality rate
(per 1,000 live births)
- Immunization coverage (%)
122
(1990)
61
(1990)
110
(1995)
70
(2000)
109
(2000)
-
111
83
-
-
-
84
111
85
-
89
80
90
39.88
100
Goal 5. Improve Maternal
Health
Reduce maternal mortality
ratio by three quarters by 2015
- Maternal mortality per
100, 000 live births (survey)
- Maternal mortality
per 100, 000 live births in
health facilities (institutional)
- Births attended by skilled
health personnel (%)
740
(1990)
216
(1990)
40
(1988)
-
260
44
(1993)
-
204
44
(1998)
-
205
47
-
187
-
503
205
-
-
197
48
-
224
-
451
201
59
185
54
100
Goal 6. Combat HIV/AIDS &
Malaria, and Other Diseases
a. Halt and reverse the spread
of HIV/AIDS by 2015
b. Halt and reverse the
incidence of malaria
National HIV prevalence
Rate (%)
Under-ve malaria case
fatality (Institutional) (%)
1.5
-
2.9
-
3.4
2.9
3.6
2.8
3.1
2.7
2.7
2.4
3.2
2.1
2.6
-
2.2
-
≤1,5
-
35
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 4: Reduce Child Mortality
Reduce under-ve mortality by
two-thirds by 2015
- Under-ve mortality rate
(per 1,000 live births)
- Immunization coverage (%)
122
(1990)
61
(1990)
110
(1995)
70
(2000)
109
(2000)
-
111
83
-
-
-
84
111
85
-
89
80
90
39.88
100
Goal 5. Improve Maternal
Health
Reduce maternal mortality
ratio by three quarters by 2015
- Maternal mortality per
100, 000 live births (survey)
- Maternal mortality
per 100, 000 live births in
health facilities (institutional)
- Births attended by skilled
health personnel (%)
740
(1990)
216
(1990)
40
(1988)
-
260
44
(1993)
-
204
44
(1998)
-
205
47
-
187
-
503
205
-
-
197
48
-
224
-
451
201
59
185
54
100
Goal 6. Combat HIV/AIDS &
Malaria, and Other Diseases
a. Halt and reverse the spread
of HIV/AIDS by 2015
b. Halt and reverse the
incidence of malaria
National HIV prevalence
Rate (%)
Under-ve malaria case
fatality (Institutional) (%)
1.5
-
2.9
-
3.4
2.9
3.6
2.8
3.1
2.7
2.7
2.4
3.2
2.1
2.6
-
2.2
-
≤1,5
-
36
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 7:
Ensure Environmental
Sustainability
a. Integrate the principles
of sustainable development
into country policies and
programmes and reverse the
loss of environmental resources
b. Halve the proportion of
people without access to safe
drinking water
by 2015
a. Proportion of
land area covered by
forest (ha/annum)
b. Annual rate of
deforestation (%)
Proportion of population with
access to safe drinking water (%)
-Urban
-Rural
Proportion of population with
access to improved sanitation (%)
-Urban
-Rural
Population with access to
secure housing (%)
Population living in slums (%)
6,229,400
(27.4 % of
total land
area)
1.82
(135,400 ha)
56
(1990)
86
(1990)
39
(1990)
-
-
-
-
27.2 (1990)
-
1.89
(115,400 ha)
67
(1993)
90
(1993)
54
(1993)
4
(1993)
10
(1993)
1
(1993)
-
25.5
-
-
70
(1998)
94
(1998)
63
(1998)
5
(1998)
11
(1998)
1
(1998)
-
-
-
-
69
83
55
8
15
2
-
-
-
-
-
-
-
-
-
-
-
-
5,517,000
(24.3% of
land area)
1.7
(93,789 ha)
-
-
-
-
-
-
11
21
-
-
-
-
-
-
-
-
11.4
20.7
-
-
-
-
-
-
-
-
12
20
-
-
83.8
93
76.6
12.4
17.8
8.2
12.5
19.6
≥7,448,000 ha
≤1.82%
78
93
69.5
52
55
50.5
18.5 (2020)
<13
37
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 7:
Ensure Environmental
Sustainability
a. Integrate the principles
of sustainable development
into country policies and
programmes and reverse the
loss of environmental resources
b. Halve the proportion of
people without access to safe
drinking water
by 2015
a. Proportion of
land area covered by
forest (ha/annum)
b. Annual rate of
deforestation (%)
Proportion of population with
access to safe drinking water (%)
-Urban
-Rural
Proportion of population with
access to improved sanitation (%)
-Urban
-Rural
Population with access to
secure housing (%)
Population living in slums (%)
6,229,400
(27.4 % of
total land
area)
1.82
(135,400 ha)
56
(1990)
86
(1990)
39
(1990)
-
-
-
-
27.2 (1990)
-
1.89
(115,400 ha)
67
(1993)
90
(1993)
54
(1993)
4
(1993)
10
(1993)
1
(1993)
-
25.5
-
-
70
(1998)
94
(1998)
63
(1998)
5
(1998)
11
(1998)
1
(1998)
-
-
-
-
69
83
55
8
15
2
-
-
-
-
-
-
-
-
-
-
-
-
5,517,000
(24.3% of
land area)
1.7
(93,789 ha)
-
-
-
-
-
-
11
21
-
-
-
-
-
-
-
-
11.4
20.7
-
-
-
-
-
-
-
-
12
20
-
-
83.8
93
76.6
12.4
17.8
8.2
12.5
19.6
≥7,448,000 ha
≤1.82%
78
93
69.5
52
55
50.5
18.5 (2020)
<13
38
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 8: Develop a Global
Partnership for Development
Deal comprehensively
with debt and make debt
sustainable in the long term
Public debt ratio (% of GDP)
External
Domestic
Total
External debt service as a
percentage of exports of
goods & services
ODA Inows (% of GDP)
Total
Programme Aid
152.8
(2000)
28.9
(2000)
181.65
(2000)
7.8
(1990)
6
30
114.8
26.8
141.61
10.1
15
39
105.4
28.5
133.85
10.2
8
58
100.7
20.5
121.26
5.2
9
49
73
21.2
94.18
5.6
10
40
59.6
18.8
78.35
5.8
9
35
17
24.4
41.42
3.2
8.1
37.6
24.6
26.2
50.87
-
8.1
31
27.7
27.5
55.2
4.3
8.6
37
-
-
-
-
-
-
Source: Ghana MDG Report 2010.
* As reported in MoH-MNCH Strategy (2009–2015).
** MoH has changed the target from 80 percent to 55 percent in the MNCH Strategy (2009-2015).
***Ministry of Agriculture and Forestry, Forestry Sector Strategy.
39
Goals/Targets Indicator Indicator Status MDG Target
1999 2001 2002 2003 2004 2005 2006 2007 2008 2015
Goal 8: Develop a Global
Partnership for Development
Deal comprehensively
with debt and make debt
sustainable in the long term
Public debt ratio (% of GDP)
External
Domestic
Total
External debt service as a
percentage of exports of
goods & services
ODA Inows (% of GDP)
Total
Programme Aid
152.8
(2000)
28.9
(2000)
181.65
(2000)
7.8
(1990)
6
30
114.8
26.8
141.61
10.1
15
39
105.4
28.5
133.85
10.2
8
58
100.7
20.5
121.26
5.2
9
49
73
21.2
94.18
5.6
10
40
59.6
18.8
78.35
5.8
9
35
17
24.4
41.42
3.2
8.1
37.6
24.6
26.2
50.87
-
8.1
31
27.7
27.5
55.2
4.3
8.6
37
-
-
-
-
-
-

STRATEGIC
INTERVENTIONS
Photo: Kayla Keenan
CHAPTER 3:

41
3.1: STRATEGIC INTERVENTIONS
OF HIGH IMPACT FOR THE
ACHIEVEMENT OF MDGS
Most of the interventions that have been pursued
to curb the high incidence of maternal mortality
over the years are similar to those for under-five
mortality. They include:
(i) establishment of at least one fully operational and
furnished hospital in every district to deal with
complications from maternal health delivery;
(ii) result-oriented strategies for under-five children,
maternal health care and malnutrition;
(iii) increased access to health services under the
NHIS;
(iv) high vaccination coverage, increased use of
insecticide-treated nets;
(v) continuous advocacy to district assemblies (DAs)
and DHMTs to devote more resources to mater-
nal and child health;
(vi) expansion of community-based health service
delivery.
Additional policies, strategies and interventions
being pursued over the years to address the MMR
include the following:
• reproductivehealthstrategy;
• RoadMapforAcceleratingtheAttainmentofthe
MDGs related to Maternal and Newborn Health
in Ghana;
• StandardsandProtocolsforPreventionandMan-
agement of Unsafe Abortion: Comprehensive
Abortion Care Services;
• WheelforImprovingAccesstoQualityCareinFP:
Medical Eligibility Criteria (MEC) for Contraceptive
Use;
• RoadMapforRepositioningFP;
• declaringmaternalmortalityanationalemer-
gency in 2008 and a programme of free health
care for pregnant women including deliveries
through the NHIS;
• strengtheningofCommunityHealthPlanning
Services (CHPS) to facilitate the provision of mater-
nal health services; and expansion of community-
based health service delivery;
• toincreasesuperviseddeliveryatthedistrictlevel,
targeting of pregnant women for NHIS registration,
raising community awareness through CHPS zones,
Community Health Officers outreach education and
mobilization of community leaders, etc.;
• continuouseducationtotraditionalmaternal
health service providers to ensure preventable
maternal deaths;
• ongoingprocesstomakematernaldeathanoti-
able event backed by legislation;
• reductionofguineawormcases,andimprove-
ment of tuberculosis treatment;
• introductionofstepstoreviseguidelinesforthe
conduct of maternal death audits and to establish a
system of confidential enquiry into maternal deaths.
Analyses of these policy and strategic documents
and consultations with health managers have shown
the multi-dimensional initiatives adopted by Ghana
to address issues of maternal health. Further initia-
tives in addition to the ones above include free Am-
bulance Services for Obstetric Emergency, Focus ANC

42
and Supervised Delivery, Prevention of Mother to
Child Transmission/Counselling and Testing PMTCT/
CT for all pregnant women, free maternal care/deliv-
ery, comprehensive abortion care, adolescent health
programmes, providing communications, logistics
and equipment for referral systems, and supervision
and monitoring of maternal services. Additional ini-
tiatives include the use of insecticide-treated nets,
High Impact Rapid Delivery (HIRD) interventions,
CHPS, expansion of blood transfusion services and
promotion of good nutrition. In spite of these efforts
maternal deaths still remain high at 503 per 100,000
live births in 2005 and 451 per 100,000 live births in
2007. If nothing is done to accelerate progress and
the current trends continue, maternal mortality will
be reduced to only 340 per 100,000 instead of the
MDG target of 185 per 100,000 by 2015.
Under a Ministerial Task Team/Technical Team, the
Government of Ghana has identified three key priority
interventions, among several ongoing ones, with the
objective of achieving maximum benefit and ensuring
better coordinated effort and impact (table 5). These are:
1. Family planning
2. Emergency obstetric and neonatal care
3. Skilled attendant at delivery
3.1.1: Family planning
Effective FP is one of the high-impact interven-
tions that reduce the risk of maternal deaths from
pregnancy-related complications and unsafe abor-
tions. But as indicated in the earlier chapter, the FP
acceptor rate remained low, at 21.2 to 25.4 percent of
women in their reproductive age, between 2001 and
2007. There are major regional variations in coverage.
The interventions are intended to reposition FP to
improve awareness methods especially at a time
when Ghana has already revised its Contraceptives
Procurement Tables and introduced an MEC wheel
to improve procurement and quality, respectively.
The intervention will seek to improve FP coverage
with specific focus on:
• improvingsupplyanddistributionofFPcom-
modities;
• improvingcapacityinprovisionofFPservices;
• improvingpublicawarenessandunderstandingof
maternal health in different areas including FP, SD,
EmONC, nutrition, sexually transmitted infections
(STI), HIV/AIDS, gender issues, etc.
3.1.2: Skilled delivery coverage
The analysis also showed that SD is key to good ma-
ternal health care. Labour and delivery is the shortest
and most critical period–childbirth continuum. Most
maternal deaths occur from complications during
delivery. Even with the best possible antenatal care,
any delivery can become complicated. Therefore,
skilled assistance is required for a safe delivery.
There have been several attempts to widen coverage
of SD services and improve service utilization. These
include posting announcements of the introduc-
tion of free delivery, NHIS, community education
to improve demand, appointment of midwives to
health centres and CHPS compounds, and offering
training in life-saving skills. A mix of strategies exists
to improve the quality of SD care, including monitor-
ing the use of partographs, audits of maternal deaths
and maternal death notification.
However, the SD rate has remained low, at 59 percent
(GDHS 2008) annually, compared to the antenatal
registrant rate of above 90 percent. The challenges
explaining the low rate of SD, among others, are the
provider’s attitude, sociocultural challenges and in-
adequate number of midwives. Table 4 below shows
the various categories and number of health staff in
2007 and the number required in 2010.
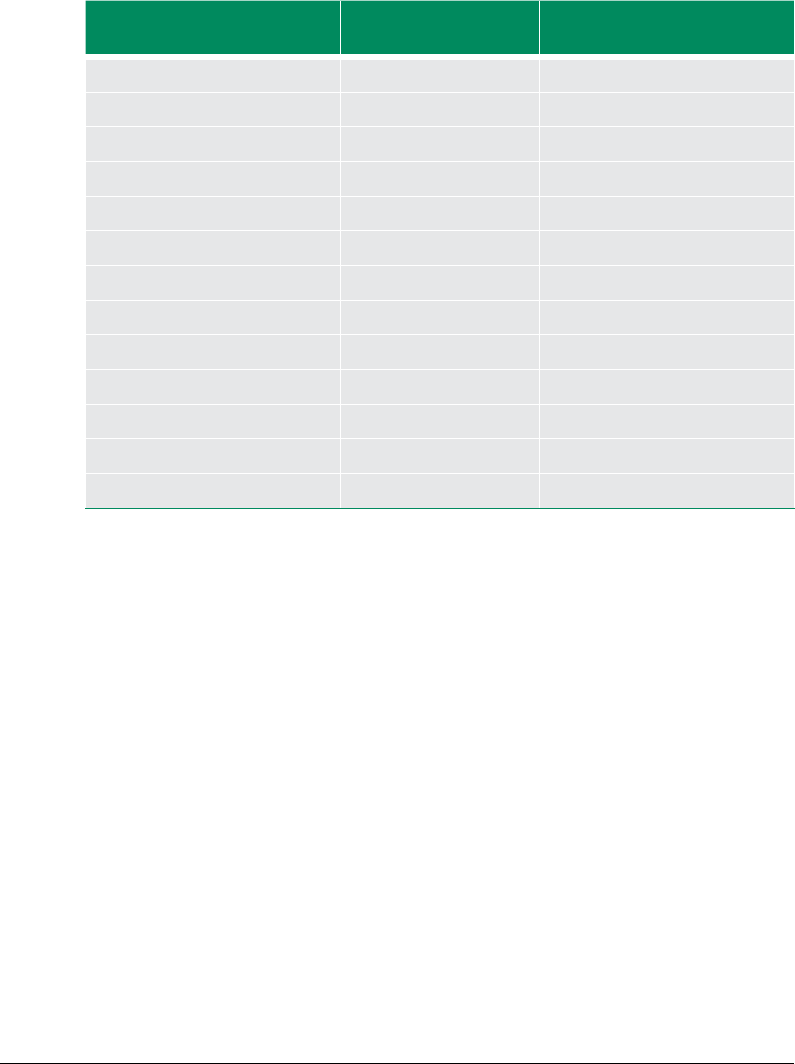
43
SD is central to achieving the MDG 5 target of a
reduction in maternal mortality by three quarters.
The interventions will seek to improve SD coverage,
and the prioritized actions will involve:
• improvingmonitoringofallstagesoflabour(e.g.,
use of partographs) and the care of the newborn
in the postnatal period;
• maintainingtheimplementationoftheFreeMa-
ternal Delivery policy in line with the NHIS;
• rollingoutCHPS,andstrengtheningreferraland
community support systems to address obstetric
emergencies;
• Extendingthereachofanintegratedpackageof
services through the HIRD approach.
3.1.3: Emergency Obstetric and
Neonatal Care
Pregnant women die from obstetric complications
that most times are not predictable. Improving ac-
cess to basic and comprehensive essential obstetric
care provides women with such complications the
care they need to survive. The Ghana government
through the MoH provides equipment, logistics and
medicines for Comprehensive Emergency Obstetric
Care (CEOC)and Comprehensive Essential Newborn
Care (CENC), monitors availability of BEOC and Es-
sential Neonatal Care (ENC) and expanded blood
transfusion services to meet maternal health needs.
For a facility to provide SD and provide essential care,
there is need for a midwife and/or a doctor with the
requisite training and orientation. In the last few
years, Ghana has established more midwifery schools
TABLE 4 HUMAN RESOURCE REQUIREMENTS 2010 AND STATUS AS OF 2007, GHANA
Category of sta
Total number
2007
Number required
by 2010
Medical ocers 2,026 3,732
Dental surgeons 31 50
Pharmacists 1,550 2,726
Expatriate doctors 200 -
Professional nurses 7,304 19,000
Enrolled nurses 2,956 -
Community health nurses 3,246 12,934
Registered midwives 2,810 8,205
Medical assistants 430 1,242
Allied health professionals 588 2,500
Traditional birth attendants 367 -
Non clinical & clinical support sta 27,918 31,100
Health assistants (clinical) - 7,176

44
(Direct Midwifery Diploma programme 2003) and
increased intake into existing schools. Despite this,
the country continues to have inequities in access
to health services resulting in large disparities in
reproductive and maternal health indicators. The
Ashanti region is the largest contributor to maternal
deaths. Yet, the region disproportionately continued
to receive financial support compared to inflows to
each of the other four ‘deprived’ regions.
Ghana also experiences gaps in monitoring and
tracking of EmONC, as well as gaps in selected es-
sential outputs and outcomes as a percentage of
facilities offering BEOC, the percentage of districts
offering CEOC and the percentage of districts with-
out transfusion services. As in the case of SD care,
the availability of human resources and adequate
distribution also remain a challenge. In 2007, Ghana
prepared a road map for accelerating the attainment
of MDG 5-related maternal and neonatal health in
Ghana. It focused on HIRD as a framework to use
evidence-based feasible and cost-effective inter-
ventions in resource-poor settings to achieve an
accelerated reduction in maternal and newborn
deaths, through increased ANC and PNC coverage,
more SD, better access to CEOC, and the promotion
of sound individual, family and community practices.
The three key areas prioritized for improving BEOC
and neonatal care includes:
• scalinguptheprocurementandimprovingdis-
tribution of BEmONC and CEmONC equipment
to health centres and hospitals, respectively;
• improvingreferralandstrengthenBloodTransfu-
sion Services (BTS) in line with the National Blood
Transfusion Policy;
• scalingupLifeSavingSkills(LSS)trainingand
building Regional Resource Teams.
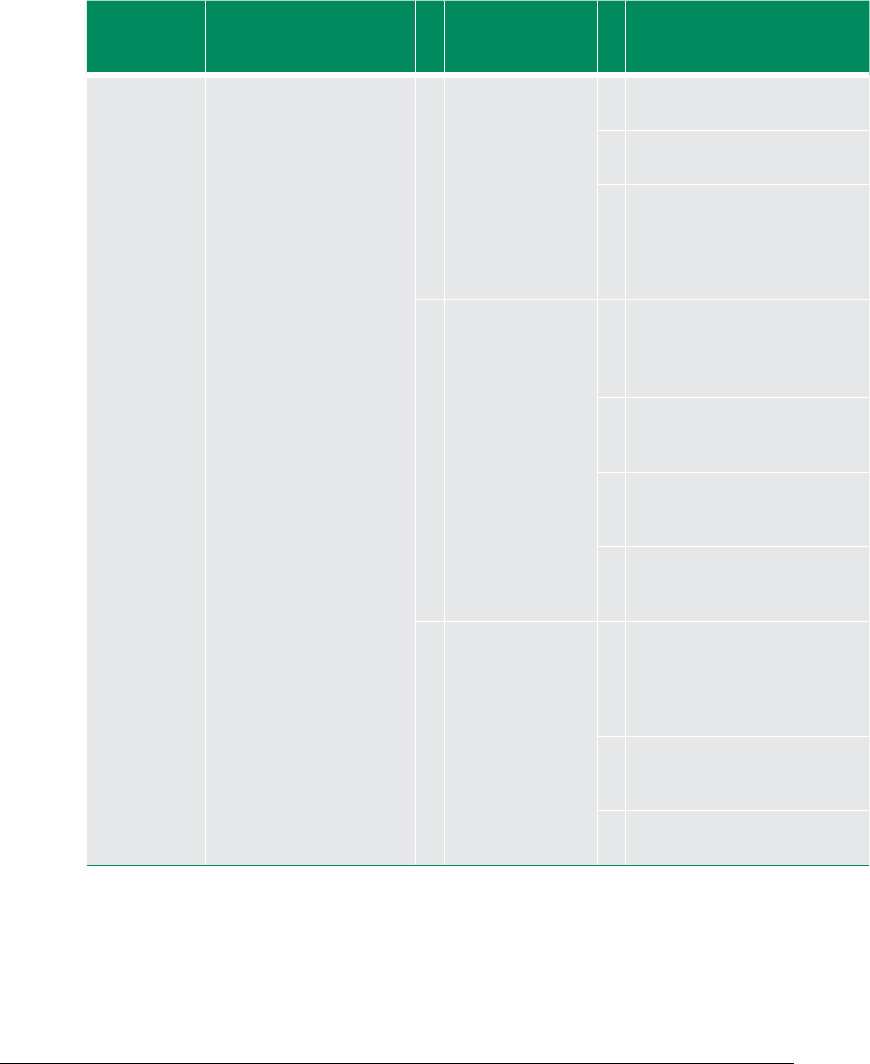
45
Figure 8.2
TABLE 5 SUMMARY MATRIX OF KEY PRIORITY INTERVENTIONS AND INDICATIVE INTERVENTIONS, GHANA
MDG MDG indicator # Key interventions # Prioritized interventions
(adapted to the country context)
2011–2015
Goal 5:
Improve
Maternal
Health
Target 5a:
Reduce
MMR by
three fourths
between 1990
and 2015
to 185 per
100,000 live
births
5.1 MMR
5.2 Proportion of births
attended by skilled health
personnel (SD rate)
1 Improving FP
coverage
1 Improving FP commodities supply
and distribution
2 Improving capacity in FP service
provision
3 Improving public awareness
and understanding of maternal
health including FP, SD, EmONC,
Nutrition, STI, HIV/AIDS, gender
issues, etc.
2 Improving SD
coverage
1 Improve monitoring of all stages
of labour (e.g., use of partograph),
of the care of the newborn and
the postnatal period
2 Maintain the implementation of
the Free Maternal Delivery policy
in line with the NHIS
3 Roll out CHPS, strengthen referral
and community support systems
to address obstetric emergencies
4 Extend the reach of integrated
package of service provision
through HIRD approach
4
3 Improving access to
EmONC
1 Scale up the procurement and
improve distribution of BEmONC
and CEmONC equipment to
health centres and hospitals
respectively
2 Improve referral and strengthen
BTS in line with the National
Blood Transfusion Policy
3 Scale up LSS training and build
Regional Resource Teams
4) The integrated package of services through HIRD includes some of elements of FP, SD and EmONC.

BOTTLENECK
ANALYSIS
Photo: Kayla Keenan
CHAPTER 4:
47
4.1: BOTTLENECKS
In the execution of interventions to reduce maternal
mortality, Ghana is challenged with many bottle-
necks related to FP, SD and BEOC that have been
identified during the implementation of initiatives
and strategies or in their documentation that was
shared among implementers and mangers. These
bottlenecks relate to access, utilization, quality, com-
modity provision, governance, funding and part-
nership. These have been analysed to ensure that
solutions match priority bottlenecks to maximize
impact. Evidence shows that if these bottlenecks
are removed, it can significantly improve maternal
health.
The prioritization of bottlenecks was based on poli-
cy/planning, budget and financing, service delivery,
service utilization and cross-cutting initiatives, as
well as the time taken for the solution to address
the bottleneck (table 6). The bottlenecks in the three
priority areas are discussed below.
4.1.1: Family planning
Since the implementation of the ‘repositioning of
FP’ to improve comprehensive FP coverage, the fol-
lowing bottlenecks, among many others, that slow
down the achievement of set targets still persist:
• stockutilizationandinventorymanagementis-
sues (including incomplete data, late reporting
and the irregular physical count of commodities);
• poorcounselling(forexample,onhowtouse
the MEC wheel) and low provider capacity for
long-term contraception methods (IUDs, implant
insertions);
• inadequatesupervisionandmonitoringofservice
delivery;
• weakownershipofandsupportformaternal
health interventions by DAs;
• culturalissues(lowmaleinvolvementincluding
lack of male service points, perception of the up-
take of FP, and non-receptive maternity units/FP
clinics);
• fearofsideeectsamongwomen(irregularmen-
struation, amenorrhea, etc.).
4.1.2: Skilled delivery
The reach of SD has consistently remained below 60
percent in Ghana. It has been a major cause of worry
to the sector and many strategies are being adopted
to address the situation. Important measures put in
place include expansion of midwifery school intake,
the redistribution of midwives, LSS training, CHPS
and free childbirth delivery. The major bottlenecks
that remain include:
• improperapplicationofaninstitutionalgrading
system and lack of customized staffing ;
• weaksupervision,monitoringandlackofasystem
to measure staff performance;
• inadequatenumberofmidwives,doctors,obstetri-
cians, and health tutors production;
• pooraccesstohealthfacilities,--geographically,
financially, and culturally (e. g., CHPS, poor refer-
ral health system, i.e. (penetration and coverage
of the National Ambulance service), community
systems);
• inadequatefundingforlogisticsandinfrastructure;
• Pooralignmentofdonorsupporttogovernment
programmes.
48
4.1.3: Emergency Obstetric and
Neonatal Care
Universal access to BEOC and neonatal care guar-
antees the best chances of survival of women who
develop obstetric complications. Ongoing inter-
ventions towards this include providing theatres
and equipping health institutions, improving refer-
ral through expansion of the National Ambulance
Service, ensuring availability of doctors or obstetri-
cians, providing safe BTS and improving customer
care. Despite these, access to BEmONC and CEmONC
is poor. The main bottlenecks underlining the poor
access to EmONC are:
• inadequatefundingforcapital-intensiveinvest-
ments in infrastructure and equipment (e.g., CHPS
compounds, EmONC equipment);
• inadequateaccessibilitytocareservicesasaresult
of inadequate transport, poor road networks, weak
referral systems;
• inadequate production and procurement of
skilled health workers (midwives, doctors, obste-
tricians, gynaecologists, tutors);
• non-implementationofrecommendationsfrom
previous EmONC assessments;
• lackofapolicyframework;
• inadequatehumanresourcescapacityandequip-
ment to expand coverage of LSS and ENC services.
Some bottlenecks are cross-cutting across the three
priority interventions, and therefore, their removal
has overarching impact on maternal health in the
country. These are the following:
• Funding: The enormity of the challenges faced
seems to be bigger than what the available re-
sources can accomplish. Thus, the inadequate
mobilization of resources to address maternal
health interventions is a major stumbling block.
• Capacity: This covers both individual and insti-
tutional capacities. There is a dearth of qualified
health professionals and related workers to deliver
an effective maternal health system care in the
country. For instance, the population per mid-
wife ranges between 5,357 (Upper West Region)
and 14,646 (Northern Region), while women of
reproductive age per midwife ranges between
920 (Volta) and 2161 (Ashanti). Incidentally, as
in 2007, the Ashanti region remained the largest
contributor (accounting for 20 percent of maternal
deaths in Ghana). Institutional capacity is also an
important issue in Ghana in terms of processes,
practices and institutional coordination, often
translating into weak absorptive capacity.
• Partnership coordination: There has been lim-
ited involvement of DAs, CSOs and non-govern-
mental organizations (NGOs) as well as the private
sector in the implementation of maternal health
in the country. Although the programme of de-
velopment partners in the health sector is aligned
with national health priorities, the challenge is
limited alignment in terms of sequencing, scope,
and pooling of resources together to achieve a
common target.
• Governance: A number of governance issues ex-
ist, relating to limited responsiveness to emerging
issues, weak transparency and accountability, lack
of effective leadership, and decentralization. Most
maternal health activities are implemented at the
district and subdistrict levels, and usually there is
a significant mismatch between the work to be
done and the resources allocated.
• Data generation and management: Effective
monitoring of progress on maternal health re-
quires substantial data. However, data generation
and management constitute a major challenge to
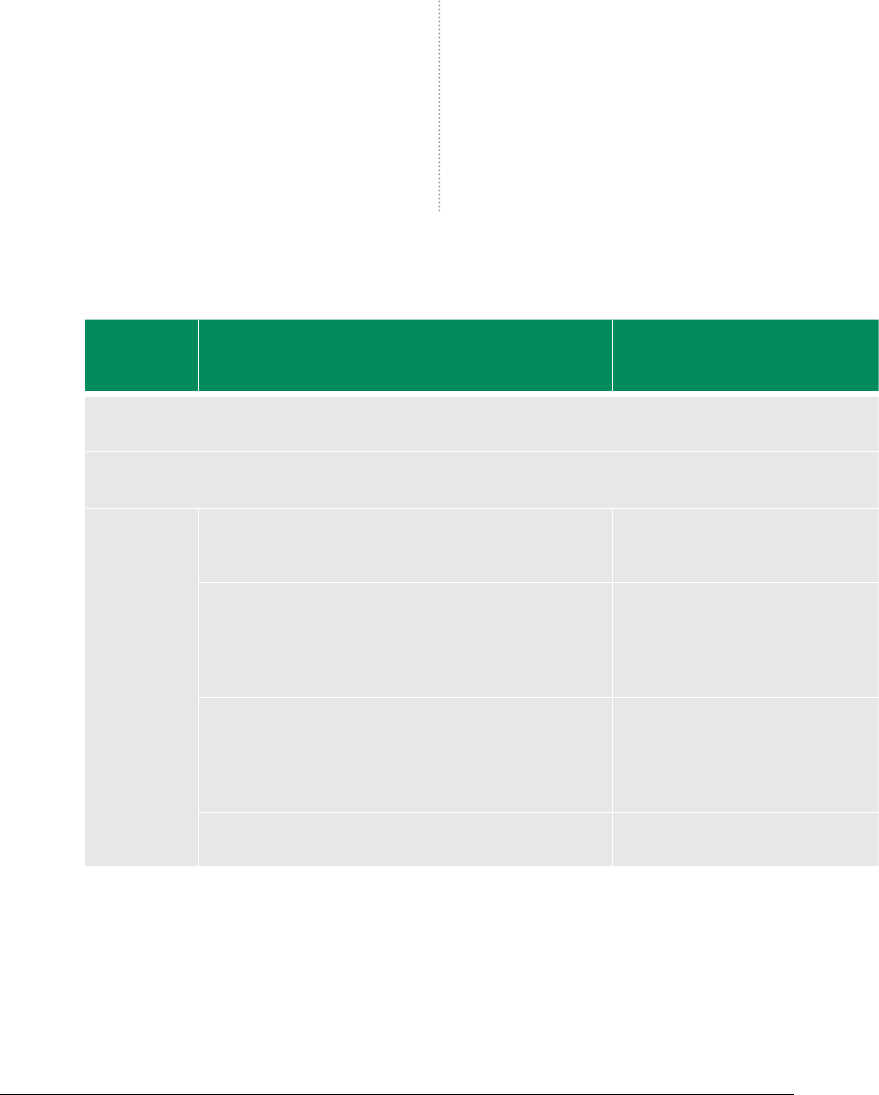
49
progress monitoring in the country. Information
on monitoring and evaluation is equally limited.
• Cultural values: Cultural factors are frequently
mentioned in most national documents includ-
ing the Roadmap for Accelerating the Attainment
of the MDGs Related to Maternal and Newborn
Health in Ghana 2007 and Ghana Democratic and
Health Survey 2008. Sociocultural factors cause
women not to use some health care services,
especially when they are related to sexual and
reproductive issues.
If women’s lives can be saved, and maternal mortal-
ity reduced, every effort should be made to address
these bottlenecks by applying the accelerating solu-
tions proposed in Chapter V and the commitment of
the Government of Ghana must be absolute.
TABLE 6: SUMMARY TABLE OF BOTTLENECKS TO KEY PRIORITY INTERVENTIONS TO ACHIEVE MDG 5
TARGETS, GHANA
Priority
interventions
Area(s)
Prioritized bottlenecks Bottleneck
category
Goal 5: Improve Maternal Health
Target 5a: Reduce the MMR by three quarters between 1990 and 2015
5.1 MMR
5.2 Proportion of births attended by skilled health personnel
(1) Improve
FP coverage
Stock utilization and inventory management issues
(including issues relating to incomplete data, late reporting,
irregular physical count of commodities, etc.)
Service delivery and cross-cutting
issue across priority interventions
Low capacity of providers of long-term methods (IUD,
Implant insertions) and poor counselling (e.g., use of MEC
wheel)
Inadequate supervision and monitoring
Service delivery/management
capacity
Weak DA ownership and support for maternal health
interventions
Sociocultural barriers (low male involvement including
inadequate male service points, perception of uptake of FP,
and non-receptive maternity units/FP clinics)
Service utilization and cross-cutting
Fear of side eects (irregular menstruation, amenorrhea,
etc.)
Service utilization
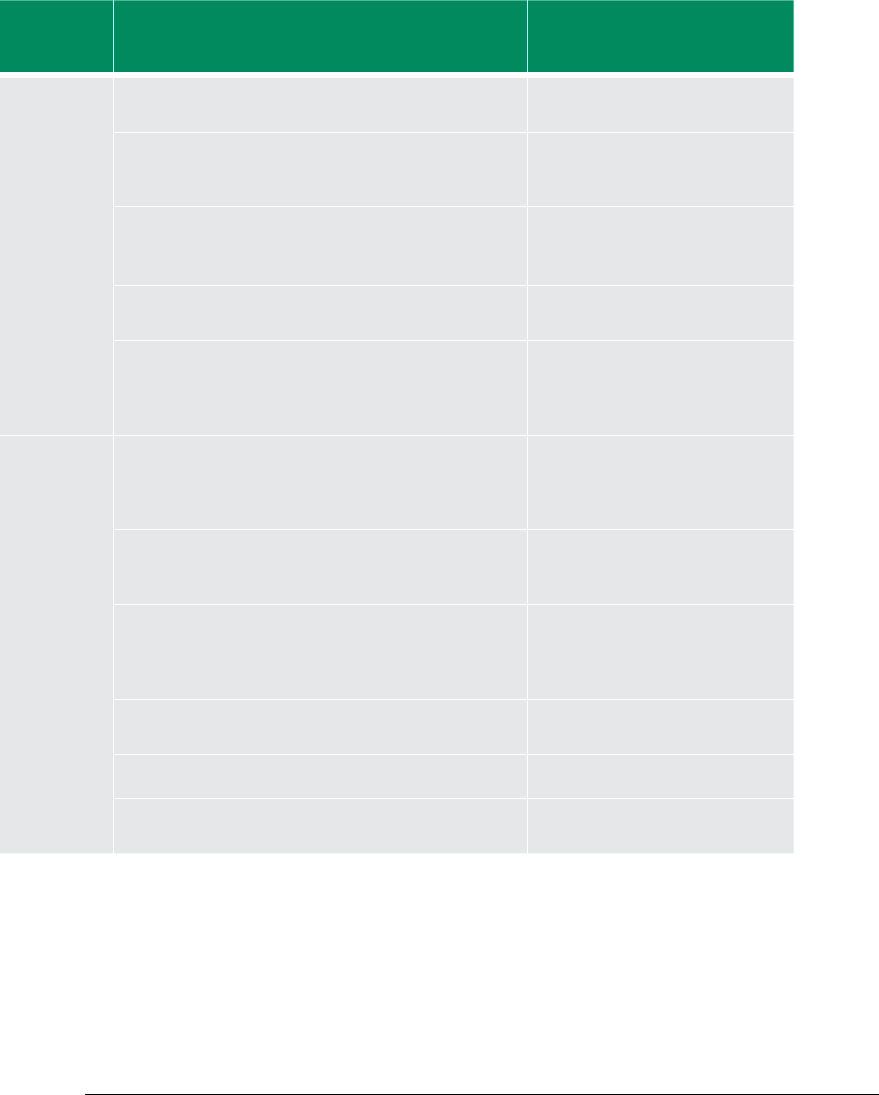
50
Priority
interventions
Area(s)
Prioritized bottlenecks Bottleneck
category
(2) Improve
SD coverage
Improper application of institutional grading system and
lack of customized stang norm
Policy/planning and service delivery
Poor leadership and management practices, weak
supervision, monitoring and weak performance
measurement system s
Service delivery/cross-cutting across
priority interventions
Inadequate number of midwives, doctors, OBG specialists,
anaesthetists and midwifery tutors
Service delivery/ cross-cutting across
priority interventions
(Inadequate funding for operations, logistics and
infrastructure (Inadequate, late release, etc)
Financing/budget
Poor alignment of donor support with government
programmes, MoH policies and agencies, and resource
allocation
Policy-planning/ nancing-budget
Cross cutting
(3) Improve
access to
emergency
obstetric and
neonatal care
Inadequate funding for capital-intensive investments in
infrastructure and equipment (e.g., CHPS compounds,
EmONC equipment, PPM) and operational funds for service
delivery
Financing/budget
Inadequate accessibility as a result of inadequate transport,
poor road networks, weak referral system (i.e., penetration
and coverage of national ambulance service)
Service utilization
Inadequate production and procurement of skilled
health workers (midwives and doctors, obstetricians
and gynaecologists, and tutors (including for SD, IST,
anaesthesia etc.)
Service delivery
Non-implementation of recommendations of previous
EmONC assessment
Policy/planning
Lack of legal framework for BTS Policy/planning
Inadequate human resource capacity and equipment to
expand coverage of LSS and ENC services
Service delivery/ cross-cutting

51

ACCELERATING MDG
PROGRESS: IDENTIFYING
SOLUTIONS
Photo: Kayla Keenan
CHAPTER 5:
53
GHANA ACTION PLAN
To address the prioritized bottlenecks identified in
Chapter IV, cost-effective solutions in the three priority
areas were proposed, based on impact (magnitude,
speed and sustainability) and feasibility (governance,
capacity and funding availability) to accelerate pro-
gress on MDG 5 (table 7). These are defined below.
5.1 IMPROVING FP COVERAGE
Key prioritized solutions
proposed:
• Procurepersonaldataassistants(PDAs)forFPdata
capture at service delivery points, stock utilization
and inventory management at all points of the sup-
ply chain and for routine and periodic monitoring.
• AddressDistrictHealthInformationManagement
System (DHIMS) bottlenecks in DHIMS-2 and roll
out training on PDAs and DHIMS at all levels of
the service delivery chain.
• Developproposalandmobilizetheinternational
community for funding.
• ImprovefundingbyadvocatingforDAstofund
maternal health interventions through the District
Development Fund.
• AdvocateforfreeFPServicesanditsinclusioninto
the NHIS package.
• ImprovecapacityofcomprehensiveFPservices
through training in comprehensive FP, including
counselling.
• IntensifypubliceducationandBCCeortsforinte-
grated maternal and child health services, through
measures such as targeting males to meet unmet
needs for FP, and education on obstetric and neo-
natal danger signs, adolescent sexual and repro-
ductive health, nutrition, gender, HIV/AIDS/STI,
etc. Target in-school and out-of-school children
and link these efforts to the communication for
development framework.
• Strengthenadvocacyonculturalfactorsaecting
maternal health (specifically in the areas of FP, SD
and EmONC).
• Improveperformancemanagementsystemsor
independent review by, for instance, NGOs.
5.2 SKILLED DELIVERY
Key prioritized acceleration
solutions:
• Developgradingsystemandupgradehealthin-
stitutions accordingly (using EmONC assessment
results).
• Categorize andproviderealisticstangnorm
(based on work load analysis to provide BEmONC
at health centres and CEmONC at district hospitals).
• Sustainthenewmidwiferyschoolsandexpansion
of midwives pre-service intake and OBG field sites.
• Sustainthecontractrecruitmentofretiredmid-
wives and medical doctors.
• Strengthenleadershipcapacityofstaatalllev-
els.
• UseEmONCassessmenttoestablishtheextentof
access and referral gaps and make recommenda-
tions to address them.

54
• Strengthenadvocacyonculturalfactorsaecting
maternal health.
• Establishandstrengthenanationalmultisector
Inter-Agency Coordinating Committee (ICC) on
Maternal and Newborn Health (with TOR to in-
clude ensuring implementation of recommenda-
tions from EmONC assessments).
• AdvocateforanOceoftheFirstLady/Gentleman
to champion maternal health and identify and
appoint maternal health and newborn champi-
ons including traditional leaders (chiefs, Queen
Mothers).
• StrengthentheNationalSecretariatoftheFHDto
support implementation of maternal and child
health interventions.
5.3 IMPROVING ACCESS TO
EMONC
Key prioritized solutions to
improve access to EmONC:
• Strengthencountrycoordinationofdonorsup-
port in line with National Aid Policy.
• AdvocatefortheNationalDevelopmentPlanning
Commission and the Ministry of Local Govern-
ment and Decentralization (MoLGD) to adopt ma-
ternal health indicators as part of DA performance
monitoring.
• Developproposalsandmobilizetheinternational
community for funding.
• Strengthenintersectoralcollaborationfordelivery
of maternal health services.
• Ensureimplementationofrecommendationsof
ongoing EmONC assessments.
• PeriodicandroutineassessmentofEmONCand
other essential maternal and health services (us-
ing appropriate tools, e.g., Systematic Coverage
Evaluation, National Development Planning Com-
mission monitoring framework).
• Strengthenauditsofmaternaldeathsandinsti-
tutionalize community audit of maternal deaths,
linking it with the community-based surveillance
system (which includes maintaining a records
system, holding review meetings, and decision
making to improve maternal health).
• Increaseproductionofmidwivesandtutors,and
target and train midwives and doctors to provide
maternal and newborn care services.
• Strengthenthereferralsystemtomakeitmore
responsive:
o Develop memorandum of understanding
(MOU) with transport unions to improve trans-
portation of pregnant women with complica-
tions.
o Develop MOU with communication agencies
to strengthen and roll out mobile-phone-based
emergency response linked with the maternal
health policy.
o Expand the National Ambulance Service includ-
ing DA ambulance support.
o Properly design the anaesthesia system.
• LobbyforthepassageoftheHealthBillincluding
BTS.
• StrengthenLSStrainingandbuildRegionalRe-
source Teams.
• ImproveaccesstoENBCatalllevels(includes
neonatal resuscitation, kangaroo mother care,
rooming-in).

55
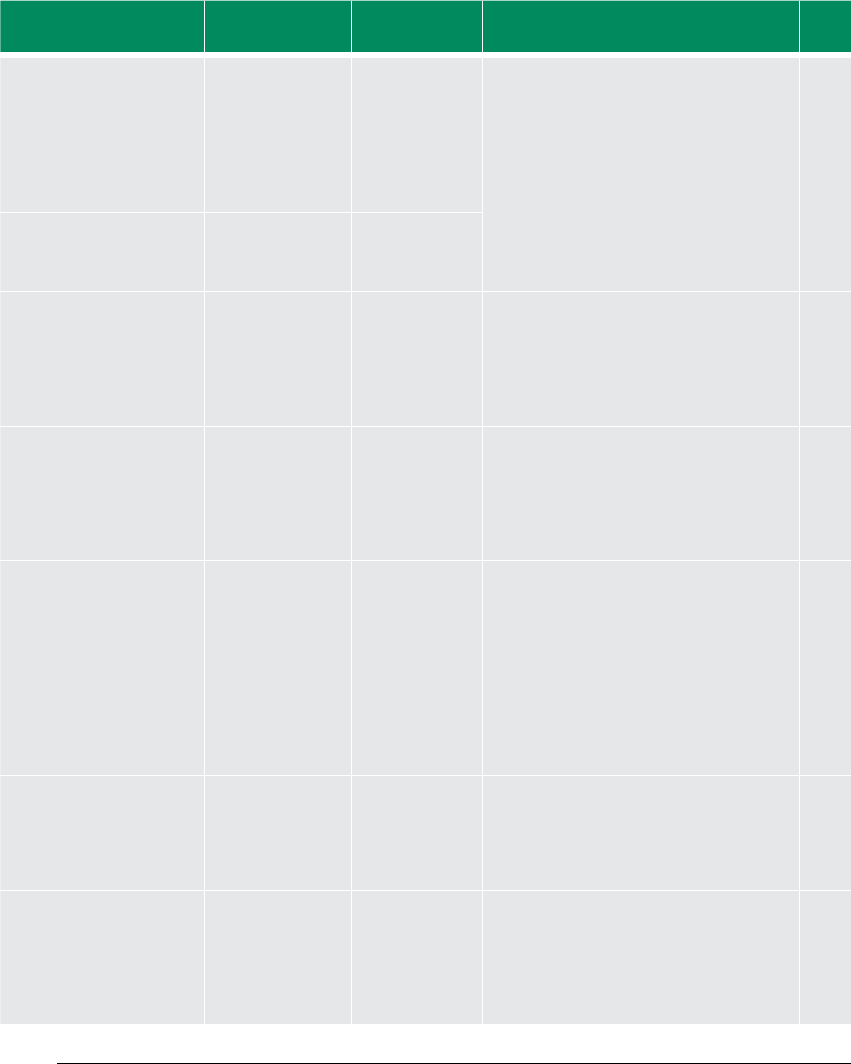
56
TABLE 7 PRIORITIZED SOLUTIONS FOR ACCELERATING PROGRESS TOWARDS MDG 5 IN GHANA
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Goal 5: Improve Maternal
Health
Target 5a: Reduce MMR by
three quarters between
1990 and 2015
5.1 MMR
5.2 Proportion of
births attended
by skilled health
personnel
(1) Improve FP
coverage
Stock utilization and inventory management
issues (including issues relating to
incomplete data, late reporting irregular
physical count of commodities, etc.)
Procure and use PDAs for FP data capture at service delivery points and at all points
of supply chain and for routine and periodic monitoring of stock utilization and
inventory management
MoH, GHS, WHO, UNFPA,
UNICEF, USAID, DFID, GAVI
Address DHIMS bottlenecks in DHIMS-2 and roll out training on PDAs and DHIMS at all
levels of the service delivery chain
MoH, GHS, DANIDA, GF, GAVI
Inadequate funding to procure commodities
and build capacity for maternal health
1. Develop a proposal and mobilize the international community for funding
2. Advocate for DAs to fund maternal health interventions through District
Development Fund
3. Advocate for free FP services and its inclusion into the NHIS package
MoF, MOH, GHS, WHO,
UNICEF, UNFPA, UNDP,
UNAIDS
Low provider capacity in the provision of
long-term methods (IUD, implant insertions)
and poor counselling (e.g., in the use of MEC
wheel)
Inadequate supervision and monitoring
Improve capacity in comprehensive FP service provision
Training in comprehensive FP including counselling
Improved performance management systems or independent review (e.g., by NGOs)
MoH/GHS, UNFPA, PPAG,
WHO
NGO partners
Weak DA ownership and support for
maternal health interventions
Sociocultural barriers (low male involvement
including inadequate male service points,
perception of uptake of FP, and non-
receptive maternity units/FP clinics)
Fear of side eects (irregular menstruation,
amenorrhea, etc.)
Improve public awareness and understanding on FP
Intensify public education and BCC for integrated maternal and child health services
(targeting males to meet unmet needs for FP, obstetric/neonatal danger signs,
adolescent sexual and reproductive health, nutrition, gender, HIV/AIDS/STI etc.)
including targeting in-school and out-of-school children and linking these eorts with
framework
Strengthen advocacy on cultural factors aecting maternal health ( FP, SD and
EmONC)
UNFPA, PPAG, WHO, MoH/
GHS
MoH, MoWCA, GHS, UNFPA,
UNICEF, WHO, NGO partners
FBOs, CSOs
(2) Improve SD
coverage
Improper application of institutional grading
system and lack of customized stang norm
Develop grading system and upgrade health institutions accordingly (using EmONC
assessment results).
Categorize and provide realistic stang norm based on work load analysis to serve
BEmONC (health centres) and CEmONC (district hospitals)
MoH, GHS, MoFEP, MoWH,
WHO, UNFPA, WB, EU, OPEC,
bilateral donors (Japan)
Inadequate number of midwives, doctors/
OBG specialists and tutors
Sustain the new midwifery schools and expansion of midwives pre-service intake and
OBG eld sites
Sustain the contract recruitment of retired midwives and medical doctors
Strengthen leadership capacity of sta at all levels
MOH, GHS, MoFEP, MoWH,
MoE, MoESW, WHO, UNFPA,
WB, EU, OPEC, bilateral
donors
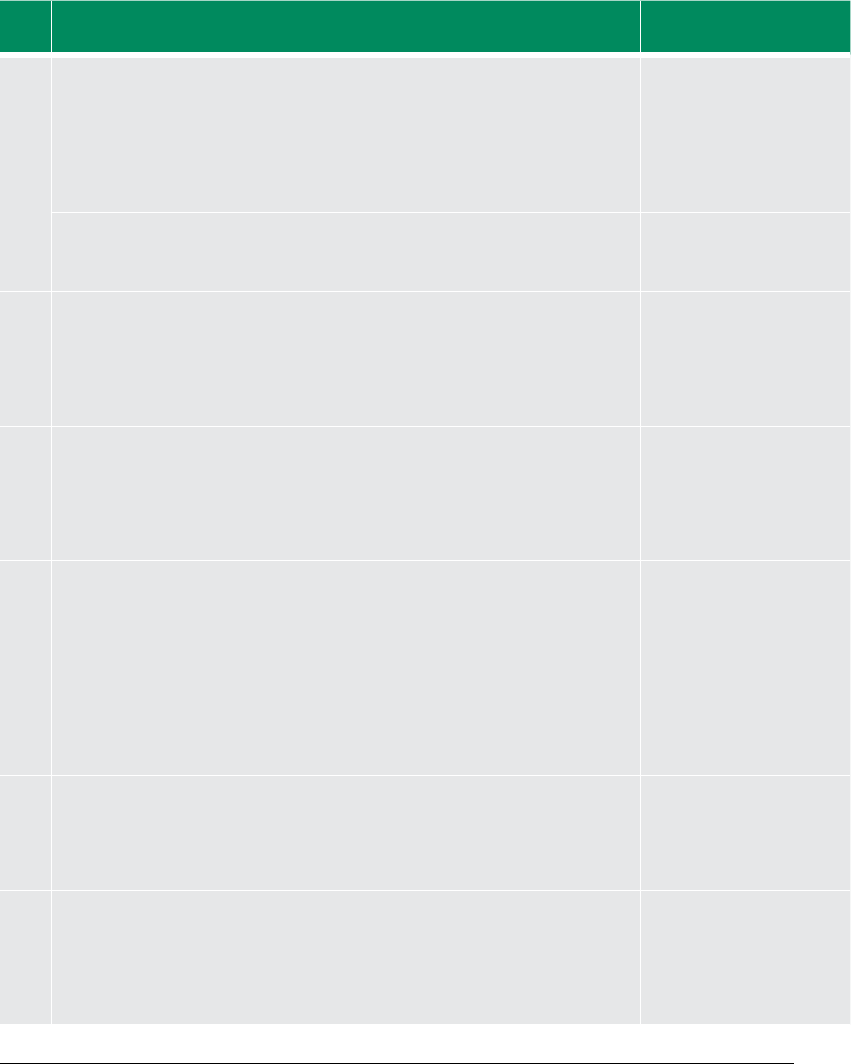
57
TABLE 7 PRIORITIZED SOLUTIONS FOR ACCELERATING PROGRESS TOWARDS MDG 5 IN GHANA
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Goal 5: Improve Maternal
Health
Target 5a: Reduce MMR by
three quarters between
1990 and 2015
5.1 MMR
5.2 Proportion of
births attended
by skilled health
personnel
(1) Improve FP
coverage
Stock utilization and inventory management
issues (including issues relating to
incomplete data, late reporting irregular
physical count of commodities, etc.)
Procure and use PDAs for FP data capture at service delivery points and at all points
of supply chain and for routine and periodic monitoring of stock utilization and
inventory management
MoH, GHS, WHO, UNFPA,
UNICEF, USAID, DFID, GAVI
Address DHIMS bottlenecks in DHIMS-2 and roll out training on PDAs and DHIMS at all
levels of the service delivery chain
MoH, GHS, DANIDA, GF, GAVI
Inadequate funding to procure commodities
and build capacity for maternal health
1. Develop a proposal and mobilize the international community for funding
2. Advocate for DAs to fund maternal health interventions through District
Development Fund
3. Advocate for free FP services and its inclusion into the NHIS package
MoF, MOH, GHS, WHO,
UNICEF, UNFPA, UNDP,
UNAIDS
Low provider capacity in the provision of
long-term methods (IUD, implant insertions)
and poor counselling (e.g., in the use of MEC
wheel)
Inadequate supervision and monitoring
Improve capacity in comprehensive FP service provision
Training in comprehensive FP including counselling
Improved performance management systems or independent review (e.g., by NGOs)
MoH/GHS, UNFPA, PPAG,
WHO
NGO partners
Weak DA ownership and support for
maternal health interventions
Sociocultural barriers (low male involvement
including inadequate male service points,
perception of uptake of FP, and non-
receptive maternity units/FP clinics)
Fear of side eects (irregular menstruation,
amenorrhea, etc.)
Improve public awareness and understanding on FP
Intensify public education and BCC for integrated maternal and child health services
(targeting males to meet unmet needs for FP, obstetric/neonatal danger signs,
adolescent sexual and reproductive health, nutrition, gender, HIV/AIDS/STI etc.)
including targeting in-school and out-of-school children and linking these eorts with
framework
Strengthen advocacy on cultural factors aecting maternal health ( FP, SD and
EmONC)
UNFPA, PPAG, WHO, MoH/
GHS
MoH, MoWCA, GHS, UNFPA,
UNICEF, WHO, NGO partners
FBOs, CSOs
(2) Improve SD
coverage
Improper application of institutional grading
system and lack of customized stang norm
Develop grading system and upgrade health institutions accordingly (using EmONC
assessment results).
Categorize and provide realistic stang norm based on work load analysis to serve
BEmONC (health centres) and CEmONC (district hospitals)
MoH, GHS, MoFEP, MoWH,
WHO, UNFPA, WB, EU, OPEC,
bilateral donors (Japan)
Inadequate number of midwives, doctors/
OBG specialists and tutors
Sustain the new midwifery schools and expansion of midwives pre-service intake and
OBG eld sites
Sustain the contract recruitment of retired midwives and medical doctors
Strengthen leadership capacity of sta at all levels
MOH, GHS, MoFEP, MoWH,
MoE, MoESW, WHO, UNFPA,
WB, EU, OPEC, bilateral
donors
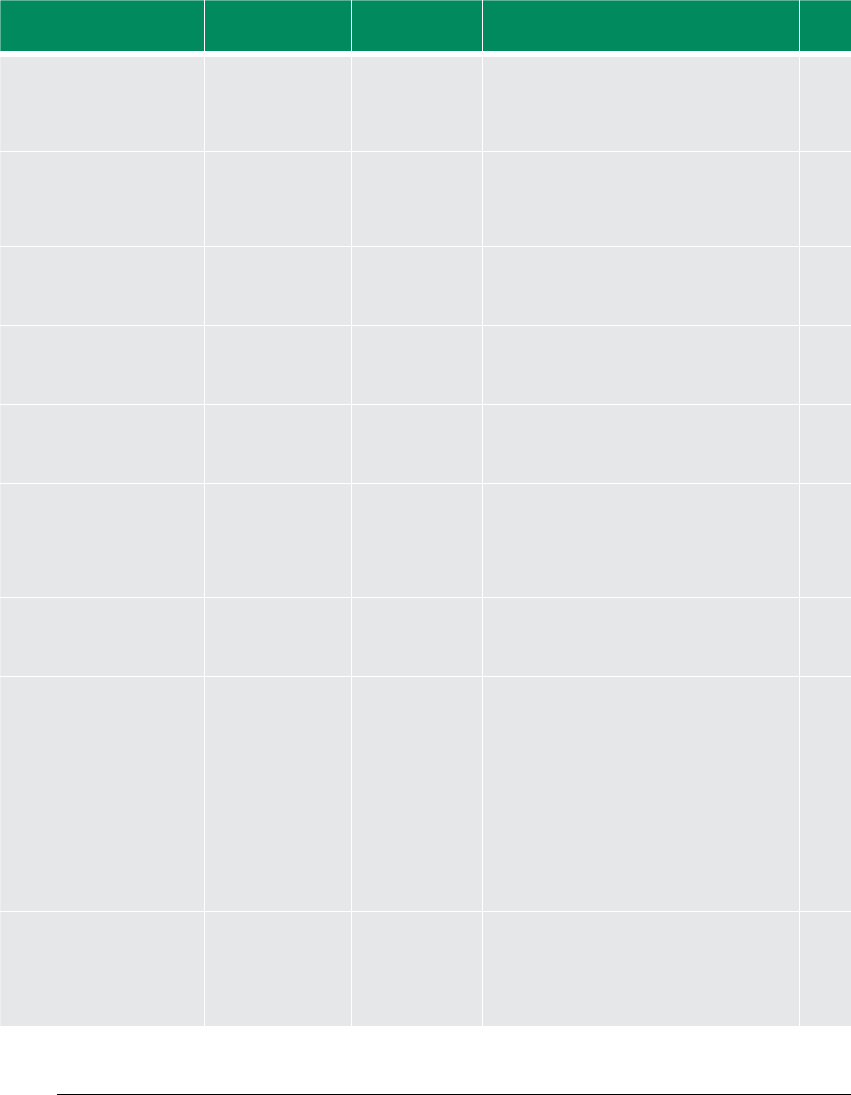
58
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Poor access to health facilities in geographic,
nancial and cultural terms (e. g., CHPS,
referral systems, community systems)
Use EmONC assessment to establish the extent of access and referral gaps and make
recommendations to address them
Strengthen advocacy on cultural factors aecting maternal health
MoH, GHS, GMA, NMWC,
GMDC
Weak overall intersectoral coordination
for maternal health and risk of non-
implementation of EmONC assessment
recommendations
Establish and strengthen (ICC) on Maternal and Newborn Health (with TOR to include
ensuring implementation of recommendations from EmONC assessment)
MoH, GHS, WHO, UNFPA,
UNICEF, USAID, DFID, WB,
EU, AfDB
Advocate for Oce of the First Lady/Gentleman to champion maternal health and
identify and appoint maternal health and newborn champions including traditional
leaders (chiefs, Queen Mothers)
MoH/GHS, UNFPA, UNDP,
WHO
(3) Improve
access to
EmONC
Strengthen the National Secretariat of the FHD to support implementation of
maternal and child health interventions
GHS
Poor alignment of donor support with
government programmes, etc.)
Strengthen country coordination of donor support in line with National Aid Policy MoFEP, MOH, GHS, UN,
MDBS, core group members
Inadequate funding for capital-intensive
investments in infrastructure and equipment
(e.g., CHPS compounds, EmONC equipment)
Advocate for DAs to fund maternal health interventions through District Development
Fund
Advocate NDPC and MoLGRD to adopt maternal health indicators as part of DA
performance monitoring
MoH, NDPC, MoLGRD,
MMDA
Develop proposal and mobilize the international community for funding MoFEP, MoH, GHS, WHO,
UNICEF, UNFPA, UNDP,
UNAIDS, MMDAs
Inadequate accessibility as a result of
inadequate transportation, weak referral
system (i.e. penetration and coverage of
National Ambulance Service) and poverty
Non-implementation of recommendations of
previous EmONC assessment
Strengthen intersectoral collaboration for delivery of maternal health services
Ensure implementation of recommendations of EmONC assessments
Periodic and routine assessment of EmONC and other essential maternal and health
services (using appropriate tools, e.g., Systematic Coverage Evaluation, NDPC
monitoring framework)
Strengthen maternal deaths audit and institutionalize community maternal deaths
audit linking it with the CBS system (records system, review meetings, decision
making to improve maternal health)
MoE, transport unions,
MoLGRD, MoFEP, MMDA,
MoRH, NGOs/CSOs, ICC for
Maternal Health
Inadequate production and procurement of
skilled health workers such as midwives and
doctors, obstetricians and gynaecologists,
specialist and tutors (including for SD, IST,
anaesthesia etc.)
Increase production of midwives, tutors, and target and train midwives and doctors to
provide maternal and newborn care services
MoE, GHS, MoH, UNFPA,
USAID, MDBS group
members

59
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Poor access to health facilities in geographic,
nancial and cultural terms (e. g., CHPS,
referral systems, community systems)
Use EmONC assessment to establish the extent of access and referral gaps and make
recommendations to address them
Strengthen advocacy on cultural factors aecting maternal health
MoH, GHS, GMA, NMWC,
GMDC
Weak overall intersectoral coordination
for maternal health and risk of non-
implementation of EmONC assessment
recommendations
Establish and strengthen (ICC) on Maternal and Newborn Health (with TOR to include
ensuring implementation of recommendations from EmONC assessment)
MoH, GHS, WHO, UNFPA,
UNICEF, USAID, DFID, WB,
EU, AfDB
Advocate for Oce of the First Lady/Gentleman to champion maternal health and
identify and appoint maternal health and newborn champions including traditional
leaders (chiefs, Queen Mothers)
MoH/GHS, UNFPA, UNDP,
WHO
(3) Improve
access to
EmONC
Strengthen the National Secretariat of the FHD to support implementation of
maternal and child health interventions
GHS
Poor alignment of donor support with
government programmes, etc.)
Strengthen country coordination of donor support in line with National Aid Policy MoFEP, MOH, GHS, UN,
MDBS, core group members
Inadequate funding for capital-intensive
investments in infrastructure and equipment
(e.g., CHPS compounds, EmONC equipment)
Advocate for DAs to fund maternal health interventions through District Development
Fund
Advocate NDPC and MoLGRD to adopt maternal health indicators as part of DA
performance monitoring
MoH, NDPC, MoLGRD,
MMDA
Develop proposal and mobilize the international community for funding MoFEP, MoH, GHS, WHO,
UNICEF, UNFPA, UNDP,
UNAIDS, MMDAs
Inadequate accessibility as a result of
inadequate transportation, weak referral
system (i.e. penetration and coverage of
National Ambulance Service) and poverty
Non-implementation of recommendations of
previous EmONC assessment
Strengthen intersectoral collaboration for delivery of maternal health services
Ensure implementation of recommendations of EmONC assessments
Periodic and routine assessment of EmONC and other essential maternal and health
services (using appropriate tools, e.g., Systematic Coverage Evaluation, NDPC
monitoring framework)
Strengthen maternal deaths audit and institutionalize community maternal deaths
audit linking it with the CBS system (records system, review meetings, decision
making to improve maternal health)
MoE, transport unions,
MoLGRD, MoFEP, MMDA,
MoRH, NGOs/CSOs, ICC for
Maternal Health
Inadequate production and procurement of
skilled health workers such as midwives and
doctors, obstetricians and gynaecologists,
specialist and tutors (including for SD, IST,
anaesthesia etc.)
Increase production of midwives, tutors, and target and train midwives and doctors to
provide maternal and newborn care services
MoE, GHS, MoH, UNFPA,
USAID, MDBS group
members
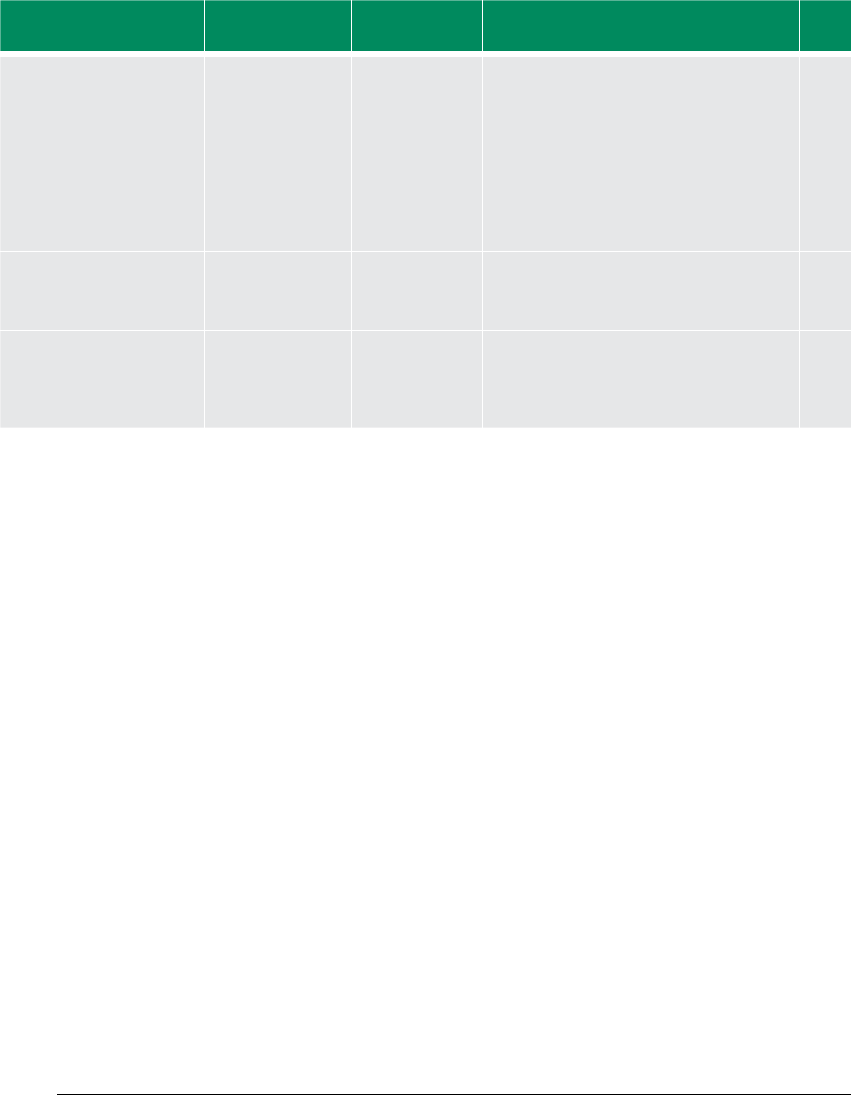
60
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Inadequate accessibility as a result of
inadequate transport, poor road networks,
weak referral systems (i.e. penetration and
coverage of National Ambulance Service)
Strengthen the referral system to make it more responsive
- Develop MOU with transport unions to improve transportation of pregnant women
with complications
- Develop MOU with communication agencies to strengthen and roll out mobile-
phone-based emergency response linked with the mobile health policy
Expand the National Ambulance Service including DA ambulance support
Design proper anaethesia system
MoH/GHS, transport unions,
MoC
Lack of legal framework for BTS
Lobby for the passage of the Health Bill including BTS ICC for maternal health,
development partners
Inadequate human resource capacity and
equipment to expand coverage of LSS and
ENC services
Strengthen LSS training and build Regional Resource Teams
Improve access to ENBC at all levels(neonatal resuscitation, kangaroo mother care,
rooming-in)
MoH/GHS, development part-
ners
6160
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Inadequate accessibility as a result of
inadequate transport, poor road networks,
weak referral systems (i.e. penetration and
coverage of National Ambulance Service)
Strengthen the referral system to make it more responsive
- Develop MOU with transport unions to improve transportation of pregnant women
with complications
- Develop MOU with communication agencies to strengthen and roll out mobile-
phone-based emergency response linked with the mobile health policy
Expand the National Ambulance Service including DA ambulance support
Design proper anaethesia system
MoH/GHS, transport unions,
MoC
Lack of legal framework for BTS
Lobby for the passage of the Health Bill including BTS ICC for maternal health,
development partners
Inadequate human resource capacity and
equipment to expand coverage of LSS and
ENC services
Strengthen LSS training and build Regional Resource Teams
Improve access to ENBC at all levels(neonatal resuscitation, kangaroo mother care,
rooming-in)
MoH/GHS, development part-
ners

61
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks Prioritized acceleration solution Potential partners
Inadequate accessibility as a result of
inadequate transport, poor road networks,
weak referral systems (i.e. penetration and
coverage of National Ambulance Service)
Strengthen the referral system to make it more responsive
- Develop MOU with transport unions to improve transportation of pregnant women
with complications
- Develop MOU with communication agencies to strengthen and roll out mobile-
phone-based emergency response linked with the mobile health policy
Expand the National Ambulance Service including DA ambulance support
Design proper anaethesia system
MoH/GHS, transport unions,
MoC
Lack of legal framework for BTS
Lobby for the passage of the Health Bill including BTS ICC for maternal health,
development partners
Inadequate human resource capacity and
equipment to expand coverage of LSS and
ENC services
Strengthen LSS training and build Regional Resource Teams
Improve access to ENBC at all levels(neonatal resuscitation, kangaroo mother care,
rooming-in)
MoH/GHS, development part-
ners
6160
Priority MDG MDG indicators Priority inter-
ventions area(s)
Prioritized bottlenecks
Prioritized acceleration solution Potential partners
Inadequate accessibility as a result of
inadequate transport, poor road networks,
weak referral systems (i.e. penetration and
coverage of National Ambulance Service)
Strengthen the referral system to make it more responsive
- Develop MOU with transport unions to improve transportation of pregnant women
with complications
- Develop MOU with communication agencies to strengthen and roll out mobile-
phone-based emergency response linked with the mobile health policy
Expand the National Ambulance Service including DA ambulance support
Design proper anaethesia system
MoH/GHS, transport unions,
MoC
Lack of legal framework for BTS
Lobby for the passage of the Health Bill including BTS ICC for maternal health,
development partners
Inadequate human resource capacity and
equipment to expand coverage of LSS and
ENC services
Strengthen LSS training and build Regional Resource Teams
Improve access to ENBC at all levels(neonatal resuscitation, kangaroo mother care,
rooming-in)
MoH/GHS, development part-
ners

MDG ACCELERATION PLAN:
BUILDING A COMPACT
Photo: Kayla Keenan
CHAPTER 6:
63
Maternal mortality has increased in Ghana, making
the objective to reduce maternal mortality unlikely
to be fulfilled if current trends continue. However,
progress in some regions of the country, such as
the Northern, Western and Central regions, where
maternal mortality improved to 195.2 per 100,000
(MDG Report 2010), clearly demonstrates that Ghana
has the potential to accelerate progress on this MDG.
The Government has already accomplished major
efforts in this direction by implementing two gen-
erations of the GPRS and the draft Medium-Term
National Development Policy Framework 2010–2013
as well as specific health sector policies. Particular in-
terventions put in place to address the high levels of
maternal deaths have been indicated in the previous
sections (Chapter 2, Section 2.2). However, as indica-
tors show, many obstacles to policies, financing and
service delivery are yet to be removed.
To accelerate progress on MDG 5, the three areas
which have been chosen as particularly catalytic are:
1. Emergency obstetric and neonatal care
2. Skilled delivery coverage
3. Family planning
6.1 COUNTRY ACTION PLAN
The present MAF analysis has uncovered the most
crippling bottlenecks as well as the most effective
solutions to address them in the near term to ef-
fectively and quickly scale-up the coverage of these
major interventions. However, the Government of
Ghana will not be able to implement these solutions
on its own. If these major bottlenecks to maternal
health are to be effectively removed within the next
five years, the Government of Ghana will need the
support of all stakeholders who can have an impact
on maternal health — not just the MoH and the GHS,
but also other ministries and government agencies,
bilateral and multilateral donors, UN funds and agen-
cies, civil society and the private sector.
Therefore, this MAF constitutes the basis of a CAP
which intends to bring together all the partners
to be able to favourably impact upon the effective
implementation and the scaling up of the three
prioritized interventions. The Government of Ghana
will be looking towards the UNCT, especially the H4,
for technical support for the formulation and imple-
mentation modalities of the solutions identified.
Additional resources will be needed, especially for
emergency obstetric care, which may be met with
the help of bilateral and multilateral donors. NGOs
and CSOs will be able to support the implementa-
tion of solutions, especially — even if not limited
to — those focusing on sensitization and advocacy
for behaviour change as well as the monitoring of
service delivery. The private sector will also be called
upon to complement the public sector service de-
livery where additional unmet needs exist. It is only
through this renewed and enhanced partnership
with clearly attributed roles and responsibilities, but-
tressed by a robust accountability framework, and
‘business as unusual’ will high maternal deaths be
reduced for the ultimate achievement of MDG 5.
This MDG 5 Action Plan does not replace existing
nationally owned planning processes and frame-
works. These will continue to be implemented to
ensure continuity, complementarity and sustain-
ability. It, rather, constitutes a subset of prioritized
actions which need to be urgently undertaken to
accelerate progress. However, to avoid duplication,
it may be useful to constitute a starting point for the
formulation of Ghana’s submission to the Secretary
General’s Initiative on Maternal and Child Health as
well as a key input into the new UNDAF (2010–2013),
currently under formulation.
Table 8 presents an overview of the CAP including
specific activities under each solution, expected part-
nerships for each, as well as the financing envelope
necessary. The table includes current commitments
(expectations based on previous commitments,
government revenue forecasts, etc.) as well as the
financing gap to be mobilized.
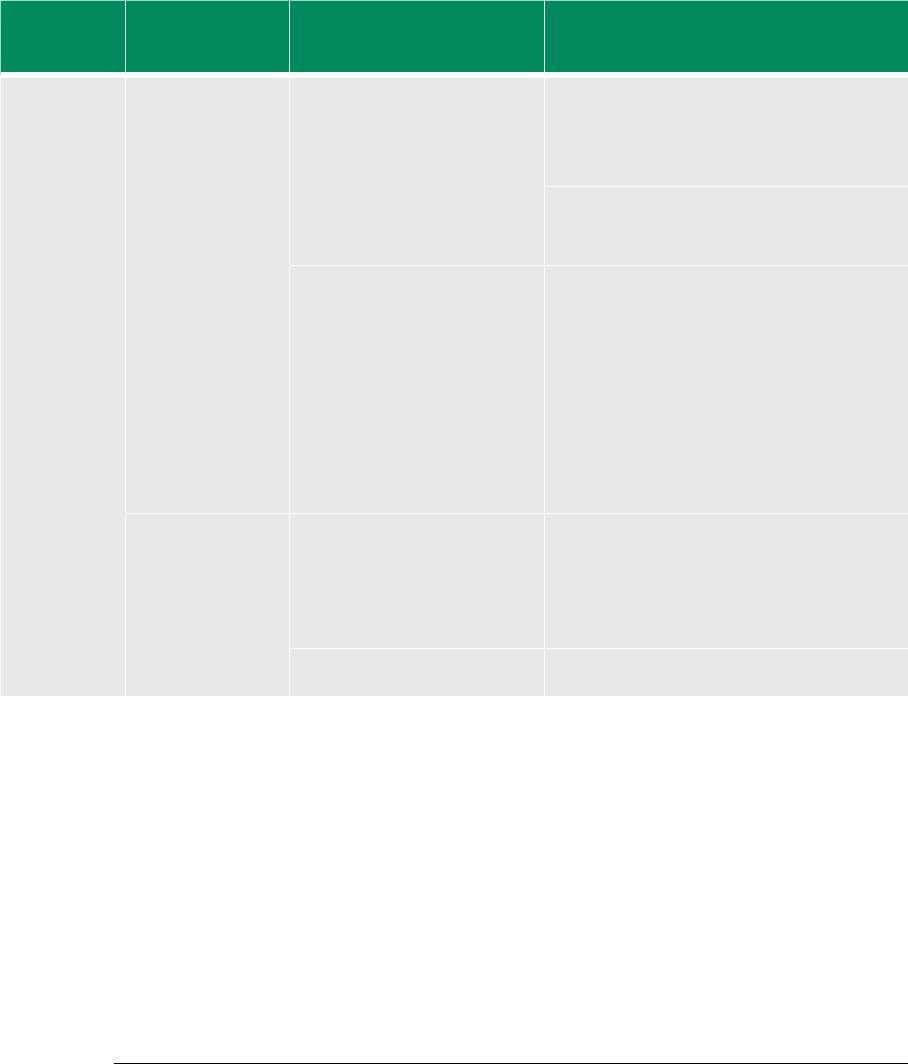
64
TABLE 8 GHANA ACTION PLAN
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
(1) Improve FP
coverage
(a) Improving FP
commodities supply
and distribution
Stock utilization and inventory
management issues (including
issues relating to incomplete data,
late reporting irregular physical
count of commodities, etc.)
Procure and use PDAs for FP data capture at
service delivery points and at all points of
supply chain and for routine and periodic
monitoring of stock utilization and inventory
management
MoH, GHS, WHO, UNFPA, UNICEF,
USAID, DFID, GAVI
3,812,500 280,000 GAVI 3,532,500
Address DHIMS bottlenecks in DHIMS-2 and
roll out training on PDAs and DHIMS at all
levels of the service delivery chain
MoH, GHS, DANIDA, GF, GAVI 560,000 70,000
5,000
PROMPT
FOCUS
485,000
Inadequate funding to procure
commodities
1.Develop proposal and mobilize the
international community for funding
2a. Advocate for DAs to fund maternal health
interventions through District Development
Fund
2b. Advocate for free FP services and its
inclusion into the NHIS package
2c. Ensure FP commodity security (procure
contraceptives)
MoFEP, MoH, GHS, WHO, UNICEF,
UNFPA, UNDP, UNAIDS
28,000
66,660,000
5,000
29,225,000
Government of
Ghana
23,000
37,441,000
(b) Improve quality
of comprehensive FP
services
Low provider capacity for long-term
methods (IUD, implant insertions)
and poor counselling (e.g. use of
Medical Eligibility Criteria (MEC)
wheel)
Training in comprehensive FP including
counselling
MoH/GHS, UNFPA, Planned
Parenthood Association Ghana
(PPAG), WHO,
Non-govt. partners
889,600 400,000
50,000
UNFPA
Government of
Ghana
439,600
Inadequate supervision and
monitoring
Improved performance management systems
or independent review (e.g. NGOs)
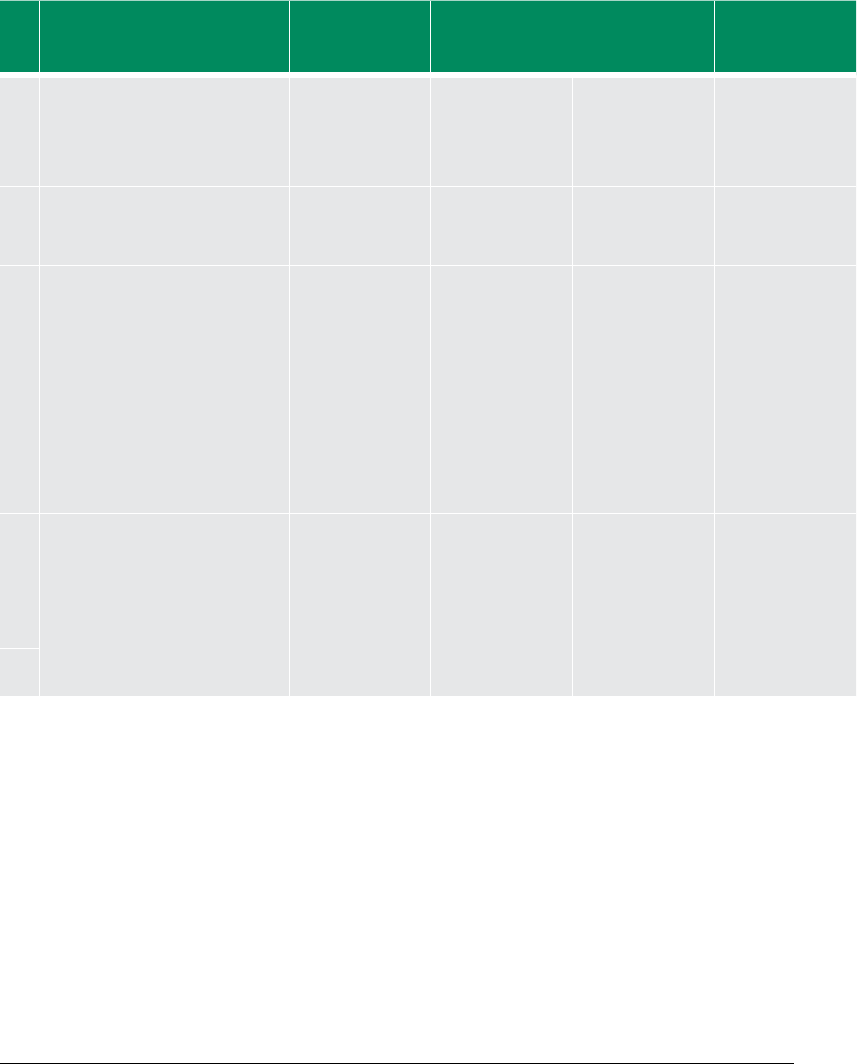
65
TABLE 8 GHANA ACTION PLAN
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
(1) Improve FP
coverage
(a) Improving FP
commodities supply
and distribution
Stock utilization and inventory
management issues (including
issues relating to incomplete data,
late reporting irregular physical
count of commodities, etc.)
Procure and use PDAs for FP data capture at
service delivery points and at all points of
supply chain and for routine and periodic
monitoring of stock utilization and inventory
management
MoH, GHS, WHO, UNFPA, UNICEF,
USAID, DFID, GAVI
3,812,500 280,000 GAVI 3,532,500
Address DHIMS bottlenecks in DHIMS-2 and
roll out training on PDAs and DHIMS at all
levels of the service delivery chain
MoH, GHS, DANIDA, GF, GAVI 560,000 70,000
5,000
PROMPT
FOCUS
485,000
Inadequate funding to procure
commodities
1.Develop proposal and mobilize the
international community for funding
2a. Advocate for DAs to fund maternal health
interventions through District Development
Fund
2b. Advocate for free FP services and its
inclusion into the NHIS package
2c. Ensure FP commodity security (procure
contraceptives)
MoFEP, MoH, GHS, WHO, UNICEF,
UNFPA, UNDP, UNAIDS
28,000
66,660,000
5,000
29,225,000
Government of
Ghana
23,000
37,441,000
(b) Improve quality
of comprehensive FP
services
Low provider capacity for long-term
methods (IUD, implant insertions)
and poor counselling (e.g. use of
Medical Eligibility Criteria (MEC)
wheel)
Training in comprehensive FP including
counselling
MoH/GHS, UNFPA, Planned
Parenthood Association Ghana
(PPAG), WHO,
Non-govt. partners
889,600 400,000
50,000
UNFPA
Government of
Ghana
439,600
Inadequate supervision and
monitoring
Improved performance management systems
or independent review (e.g. NGOs)
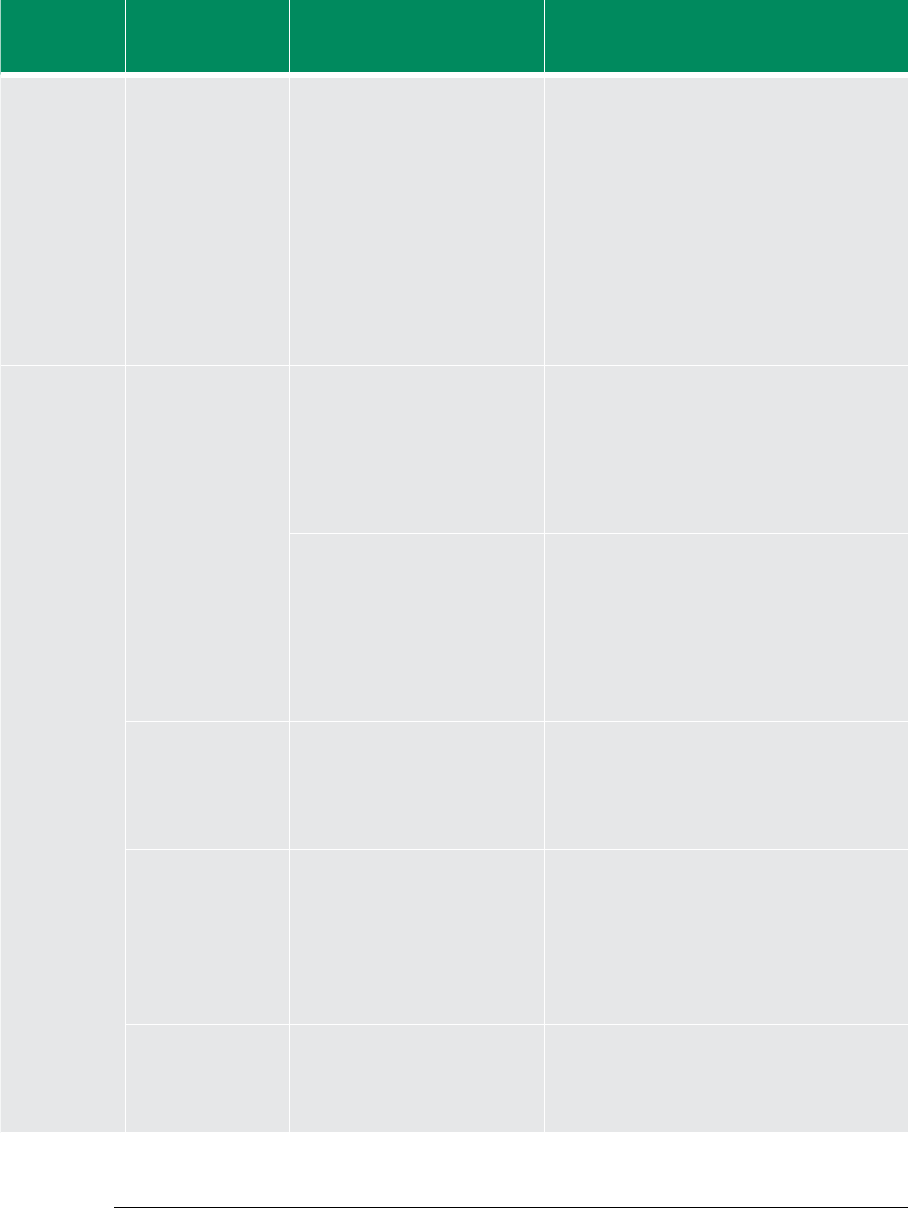
66
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
(c) Increase demand
for FP services
Weak DA ownership and support
for maternal health interventions
Sociocultural barriers (low male
involvement including inadequate
male service points, perception of
uptake of FP, and non-receptive
maternity units/FP clinics)
Fear of side eects (irregular
menstruation, amenorrhea, etc.)
1. Intensify public education and BCC for
integrated maternal and child health services
(targeting males to meet unmet needs for FP,
obstetric/neonatal danger signs, adolescent
sexual and reproductive health, nutrition,
gender, HIV/AIDS/STI, etc.) including targeting
in-school and out-of-school children and link
with C4D framework
2. Strengthen advocacy on cultural factors
aecting maternal health (FP, SD and EmONC)
3. Advocate for free FP Sservices and its
inclusion into the NHIS package
UNFPA, PPAG, WHO, MoH/GHS,
Ministry of Women and Children’s
Aairs (MoWCA), GHS, UNFPA,
UNICEF, WHO, NGO partners
Faith-based organizations, CSOs
242,500
1,541,000
120,000
975,000
UNICEF, John
Hopkins University
(JHU)
ORIO, Government
of Ghana
566,000
(2) Improve SD
coverage
(a) Improve
monitoring of all
stages of labour
and the care of the
newborn and the
postnatal period
Improper application of
institutional grading system and
lack of customized stang norm
Develop grading system and upgrade health
institutions accordingly (using EmONC
assessment results).
Categorize and provide realistic stang
norm, based on work load analysis to provide
BEmONC (health centres) and CEmONC
(district hospitals)
MoH, GHS, MoFEP, MoWHW, WHO,
UNFPA, WB, EU, OPEC, bilateral
donors (Japan)
26,094,000
28,000
17,204,000
28,000
Government of
Ghana, Health
Fund
Government of
Ghana
8,890,000
0
Inadequate midwives, doctors,
obstetricians, gynaecologists,
specialists and tutors
Sustain new midwifery schools and expansion
of midwives pre-service intake and OBG eld
sites
Sustain the contract recruitment of retired
midwives and medical doctors
Strengthen leadership capacity of sta at all
levels
MoH, GHS, MoFEP, MoWHW, MoE,
MoESW, WHO, UNFPA, WB, EU,
OPEC, bilateral donors
14,000,000
2,080,000
7,500,000
200,000
Government of
Ghana, Health
Fund
GAVI
6,500,000
1,880,000
(b) Maintain the
implementation of
the Free Maternal
Delivery policy in line
with the NHIS
Lack of funding Develop proposal and mobilize the
international community for funding
Advocate for DAs to fund maternal health
interventions through District Development
Fund
(c) Roll out CHPS,
strengthen referral
and community
support systems to
address obstetric
emergencies
Poor targeting of CHPS
Inadequate funding for capital-
intensive investments in
infrastructure and equipment
Use EmONC assessment to establish the
extent of access and referral gaps and make
recommendations to address them
MoH, GHS, Ghana Medical
Association (GMA), Nurses and
Midwives Council (MMC), Ghana
Medical and Dental Council
(GMDC)
20,000 20,000 Government of
Ghana
0
(d) Extend the
reach of integrated
package of service
provision through
HIRD approach
5
Weak overall inter-sectoral
coordination for maternal health
and Risk of non-implementation
of EmONC assessment
recommendation
Establish and strengthen ICC on Maternal and
Newborn Health (with TOR to include ensuring
implementation of recommendations from
EmONC Assessment)
MoH, GHS, WHO, UNFPA, UNICEF,
USAID, DFID, WB, EU, AfDB
40,000 20,000 UNFPA,
Government of
Ghana
20,000
5) Integrated package of services through HIRD includes some of elements of FP, SD and EmONC.
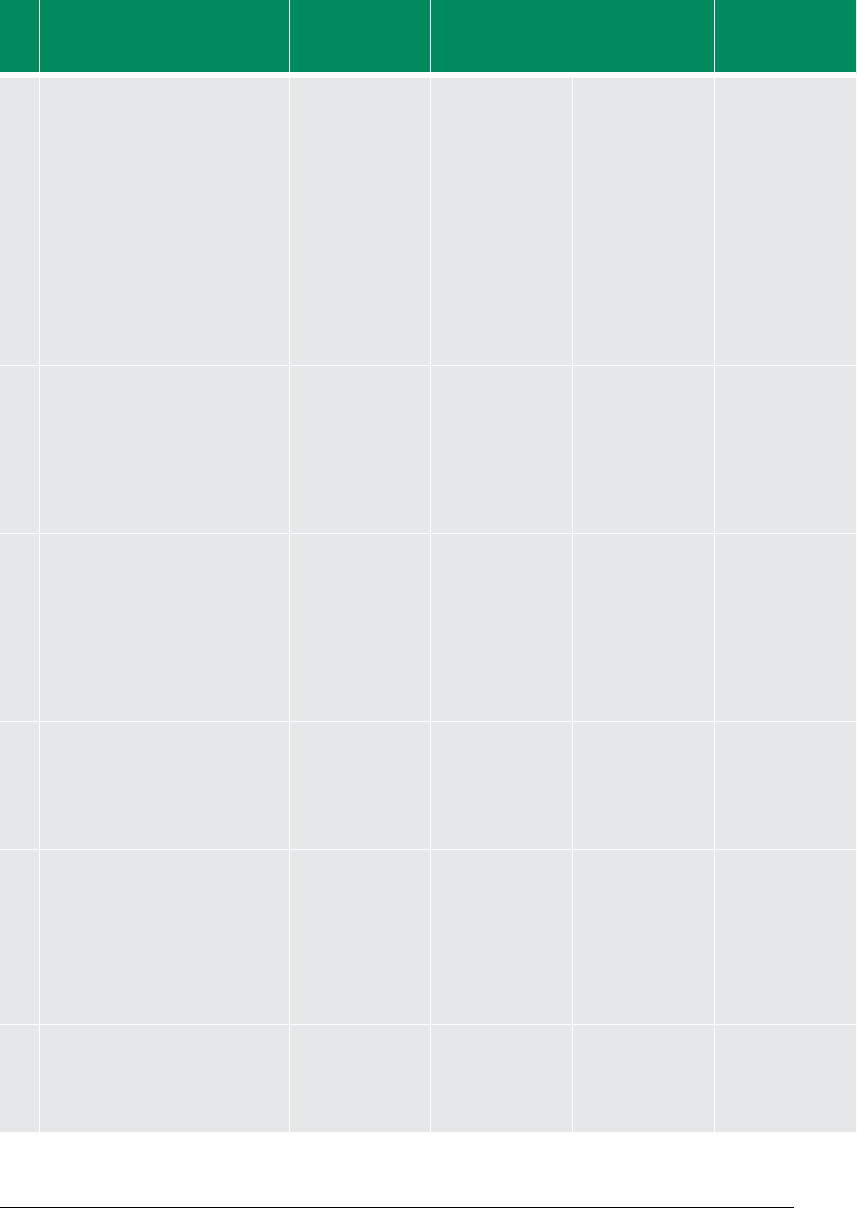
67
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
(c) Increase demand
for FP services
Weak DA ownership and support
for maternal health interventions
Sociocultural barriers (low male
involvement including inadequate
male service points, perception of
uptake of FP, and non-receptive
maternity units/FP clinics)
Fear of side eects (irregular
menstruation, amenorrhea, etc.)
1. Intensify public education and BCC for
integrated maternal and child health services
(targeting males to meet unmet needs for FP,
obstetric/neonatal danger signs, adolescent
sexual and reproductive health, nutrition,
gender, HIV/AIDS/STI, etc.) including targeting
in-school and out-of-school children and link
with C4D framework
2. Strengthen advocacy on cultural factors
aecting maternal health (FP, SD and EmONC)
3. Advocate for free FP Sservices and its
inclusion into the NHIS package
UNFPA, PPAG, WHO, MoH/GHS,
Ministry of Women and Children’s
Aairs (MoWCA), GHS, UNFPA,
UNICEF, WHO, NGO partners
Faith-based organizations, CSOs
242,500
1,541,000
120,000
975,000
UNICEF, John
Hopkins University
(JHU)
ORIO, Government
of Ghana
566,000
(2) Improve SD
coverage
(a) Improve
monitoring of all
stages of labour
and the care of the
newborn and the
postnatal period
Improper application of
institutional grading system and
lack of customized stang norm
Develop grading system and upgrade health
institutions accordingly (using EmONC
assessment results).
Categorize and provide realistic stang
norm, based on work load analysis to provide
BEmONC (health centres) and CEmONC
(district hospitals)
MoH, GHS, MoFEP, MoWHW, WHO,
UNFPA, WB, EU, OPEC, bilateral
donors (Japan)
26,094,000
28,000
17,204,000
28,000
Government of
Ghana, Health
Fund
Government of
Ghana
8,890,000
0
Inadequate midwives, doctors,
obstetricians, gynaecologists,
specialists and tutors
Sustain new midwifery schools and expansion
of midwives pre-service intake and OBG eld
sites
Sustain the contract recruitment of retired
midwives and medical doctors
Strengthen leadership capacity of sta at all
levels
MoH, GHS, MoFEP, MoWHW, MoE,
MoESW, WHO, UNFPA, WB, EU,
OPEC, bilateral donors
14,000,000
2,080,000
7,500,000
200,000
Government of
Ghana, Health
Fund
GAVI
6,500,000
1,880,000
(b) Maintain the
implementation of
the Free Maternal
Delivery policy in line
with the NHIS
Lack of funding Develop proposal and mobilize the
international community for funding
Advocate for DAs to fund maternal health
interventions through District Development
Fund
(c) Roll out CHPS,
strengthen referral
and community
support systems to
address obstetric
emergencies
Poor targeting of CHPS
Inadequate funding for capital-
intensive investments in
infrastructure and equipment
Use EmONC assessment to establish the
extent of access and referral gaps and make
recommendations to address them
MoH, GHS, Ghana Medical
Association (GMA), Nurses and
Midwives Council (MMC), Ghana
Medical and Dental Council
(GMDC)
20,000 20,000 Government of
Ghana
0
(d) Extend the
reach of integrated
package of service
provision through
HIRD approach
5
Weak overall inter-sectoral
coordination for maternal health
and Risk of non-implementation
of EmONC assessment
recommendation
Establish and strengthen ICC on Maternal and
Newborn Health (with TOR to include ensuring
implementation of recommendations from
EmONC Assessment)
MoH, GHS, WHO, UNFPA, UNICEF,
USAID, DFID, WB, EU, AfDB
40,000 20,000 UNFPA,
Government of
Ghana
20,000
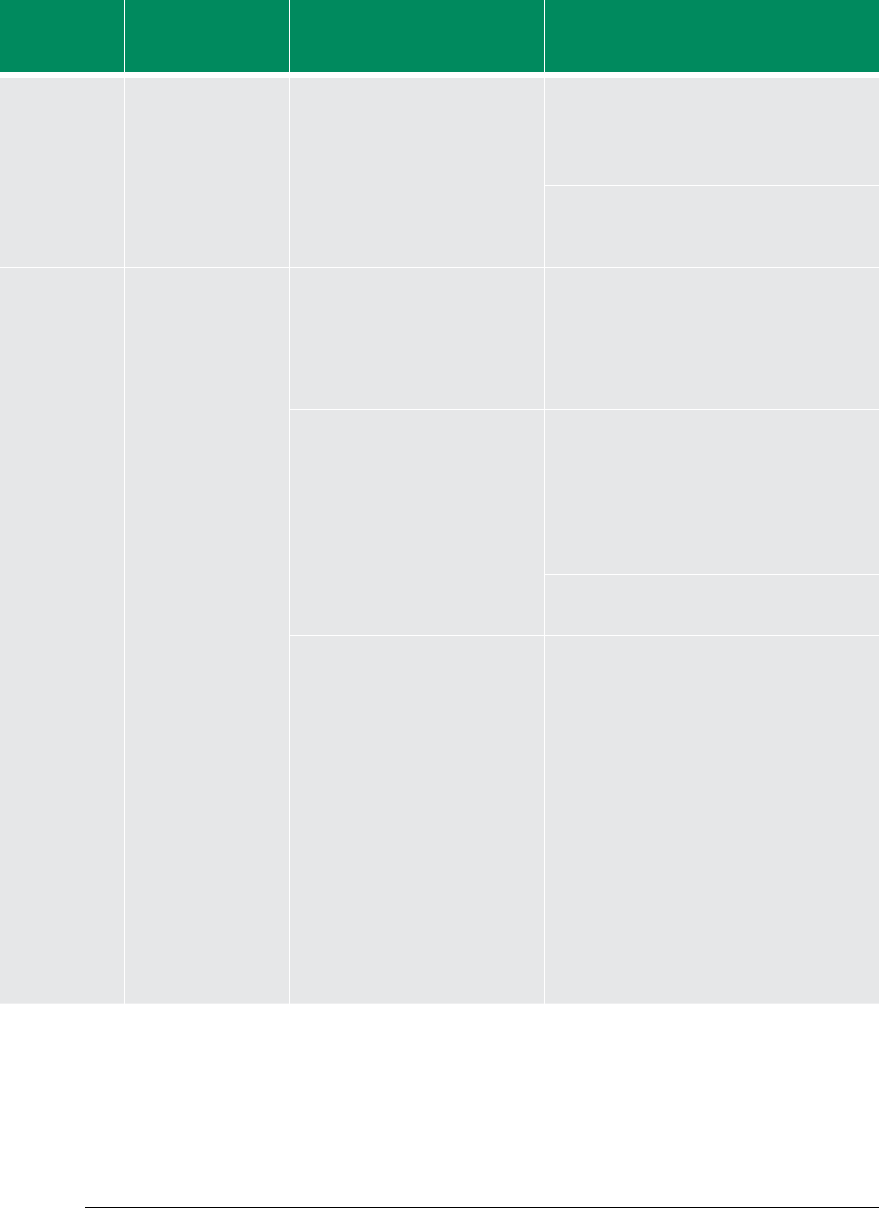
68
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
Advocate for Oce of the First Lady/
Gentleman to Champion maternal health and
identify and appoint maternal health and
newborn champions including traditional
leaders (chiefs, Queen Mothers)
MoH/GHS, UNFPA, UNDP, WHO 100,000 30,000 Government of
Ghana
70,000
Strengthen the National Secretariat of the
FHD to support implementation of maternal
and child health interventions
GHS 100,000 40,000 WHO, UNICEF,
Government of
Ghana
60,000
(3) Improve
access to
EmONC
(a) Scale up
procurement and
improve distribution
of BEmONC and
CEmONC equipment
to health centres and
hospitals respectively
Poor alignment of donor support
with government programmes
Strengthen country coordination of donor
support in line with National Aid Policy
MoFEP, MoH, GHS, UN, core
members of MDBS Group
- - -
Inadequate funding for capital-
intensive investments in
infrastructure and equipment
(e.g., CHPS compounds, EmONC
equipment)
Advocate for DAs to fund maternal health
interventions through District Development
Fund
Advocate NDPC and MoLGRD to adopt
maternal health indicators as part of DA
performance monitoring
MoH, NDPC, MoLGRD, MMDA 50,000
100,000
10,000
20,000
Government of
Ghana
Government of
Ghana
40,000
80,000
Develop proposal and mobilize the
international community for funding
MoFEP, MoH, GHS, WHO, UNICEF,
UNFPA, UNDP, UNAIDS, MMDA
- - -
Inadequate accessibility as a result
of inadequate transportation, weak
referral systems(i.e. penetration and
coverage of National Ambulance
Service) and poverty
Non-implementation of
recommendations of previous
EmONC assessment
Strengthen intersectoral collaboration for
delivery of maternal health services
Ensure implementation of recommendations
of EmONC assessments
Periodic and routine assessment of EmONC
and other essential maternal and health
services (using appropriate tools, e.g.,
Systematic Coverage Evaluation, NDPC
monitoring framework)
Strengthen maternal deaths audit and
institutionalize community maternal deaths
auditing, linking it with the CBS systems
(records system, review meetings, decision
making to improve maternal health)
MoE, transport unions, MoLGRD,
MoFEP, MMDA, MoRHW, NGOs,
CSOs, ICC for Maternal Health
9,240,000 4,620,000 Government of
Ghana, Health
Fund
4,620,000
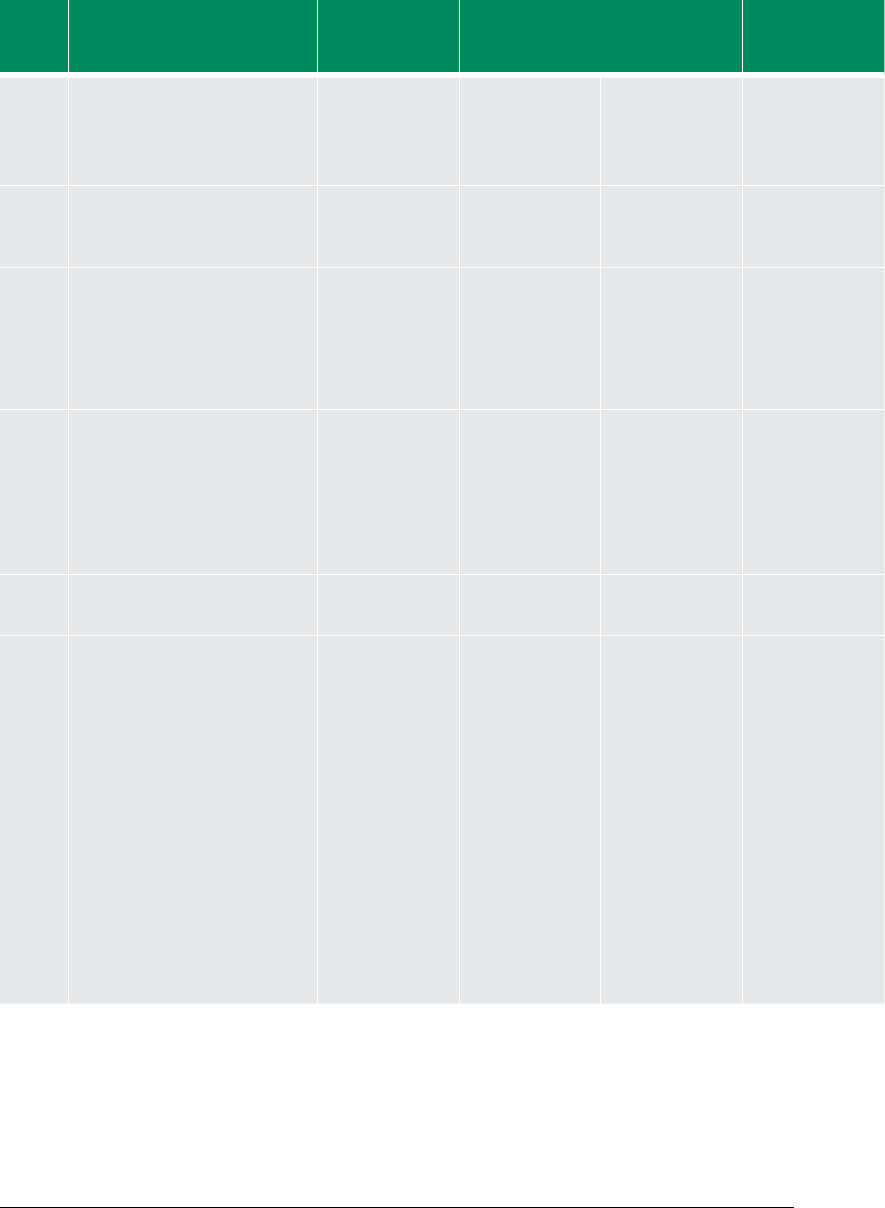
69
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
Advocate for Oce of the First Lady/
Gentleman to Champion maternal health and
identify and appoint maternal health and
newborn champions including traditional
leaders (chiefs, Queen Mothers)
MoH/GHS, UNFPA, UNDP, WHO 100,000 30,000 Government of
Ghana
70,000
Strengthen the National Secretariat of the
FHD to support implementation of maternal
and child health interventions
GHS 100,000 40,000 WHO, UNICEF,
Government of
Ghana
60,000
(3) Improve
access to
EmONC
(a) Scale up
procurement and
improve distribution
of BEmONC and
CEmONC equipment
to health centres and
hospitals respectively
Poor alignment of donor support
with government programmes
Strengthen country coordination of donor
support in line with National Aid Policy
MoFEP, MoH, GHS, UN, core
members of MDBS Group
- - -
Inadequate funding for capital-
intensive investments in
infrastructure and equipment
(e.g., CHPS compounds, EmONC
equipment)
Advocate for DAs to fund maternal health
interventions through District Development
Fund
Advocate NDPC and MoLGRD to adopt
maternal health indicators as part of DA
performance monitoring
MoH, NDPC, MoLGRD, MMDA 50,000
100,000
10,000
20,000
Government of
Ghana
Government of
Ghana
40,000
80,000
Develop proposal and mobilize the
international community for funding
MoFEP, MoH, GHS, WHO, UNICEF,
UNFPA, UNDP, UNAIDS, MMDA
- - -
Inadequate accessibility as a result
of inadequate transportation, weak
referral systems(i.e. penetration and
coverage of National Ambulance
Service) and poverty
Non-implementation of
recommendations of previous
EmONC assessment
Strengthen intersectoral collaboration for
delivery of maternal health services
Ensure implementation of recommendations
of EmONC assessments
Periodic and routine assessment of EmONC
and other essential maternal and health
services (using appropriate tools, e.g.,
Systematic Coverage Evaluation, NDPC
monitoring framework)
Strengthen maternal deaths audit and
institutionalize community maternal deaths
auditing, linking it with the CBS systems
(records system, review meetings, decision
making to improve maternal health)
MoE, transport unions, MoLGRD,
MoFEP, MMDA, MoRHW, NGOs,
CSOs, ICC for Maternal Health
9,240,000 4,620,000 Government of
Ghana, Health
Fund
4,620,000
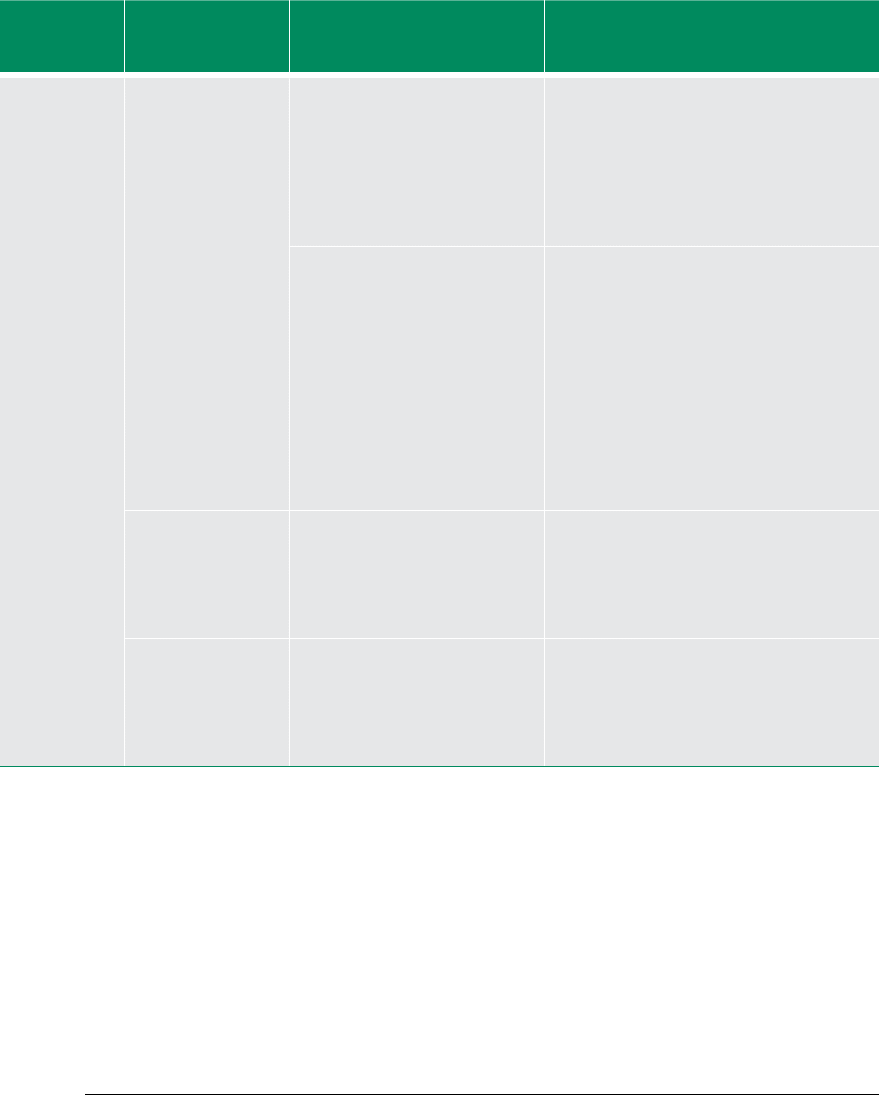
70
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
Inadequate production and
procurement of skilled health
workers including midwives,
doctors, obstetricians,
gynaecologists specialist and tutors
(covers also SD IST, Anaesthesia,
etc.)
Increase production of midwives and tutors,
and target and train midwives and doctors to
provide maternal and newborn care services
MoE, GHS, MoH, UNFPA, USAID,
MDBS group members
350,000 200,000 Government of
Ghana
150,000
Inadequate accessibility as a result
of inadequate transport, poor road
networks, weak referral systems
(i.e. penetration and coverage of
National Ambulance Service)
Strengthen the referral system to make it
more responsive
• Develop MOU with transport unions to
improve transportation of pregnant women
with complication
• Develop MOU with communication agencies
to strengthen and roll out of mobile-phone-
based emergency response linked with the
mobilehealth policy
• Expand the National Ambulance Service
including DA ambulance support
• Design proper anaesthesia system
MoH/GHS, transport unions, MoC
500,000
100,000
30,000,000
125,000
0
25,000,000
DAs
Government of
Ghana
375,000
100,000
5,000,000
(b) Improve referral
and strengthen BTS in
line with the National
Blood Transfusion
Policy
Lack of legal framework for (BTS) Lobby for the passage of the Health Bill
including BTS
ICC for Maternal Health,
development partners
(c) Scale up LSS
training and build
Regional Resource
Teams
Inadequate human resource
capacity and equipment to expand
coverage of LSS and ENC services
Strengthen LSS training and build Regional
Resource Teams
Improve access to ENBC services at all levels
(neonatal resuscitation, kangaroo mother
care, rooming-in)
MoH/GHS, development partners 768,000 300,000 Health partners,
Government of
Ghana
468,000
153,491,100 86,447,000 70,740,100
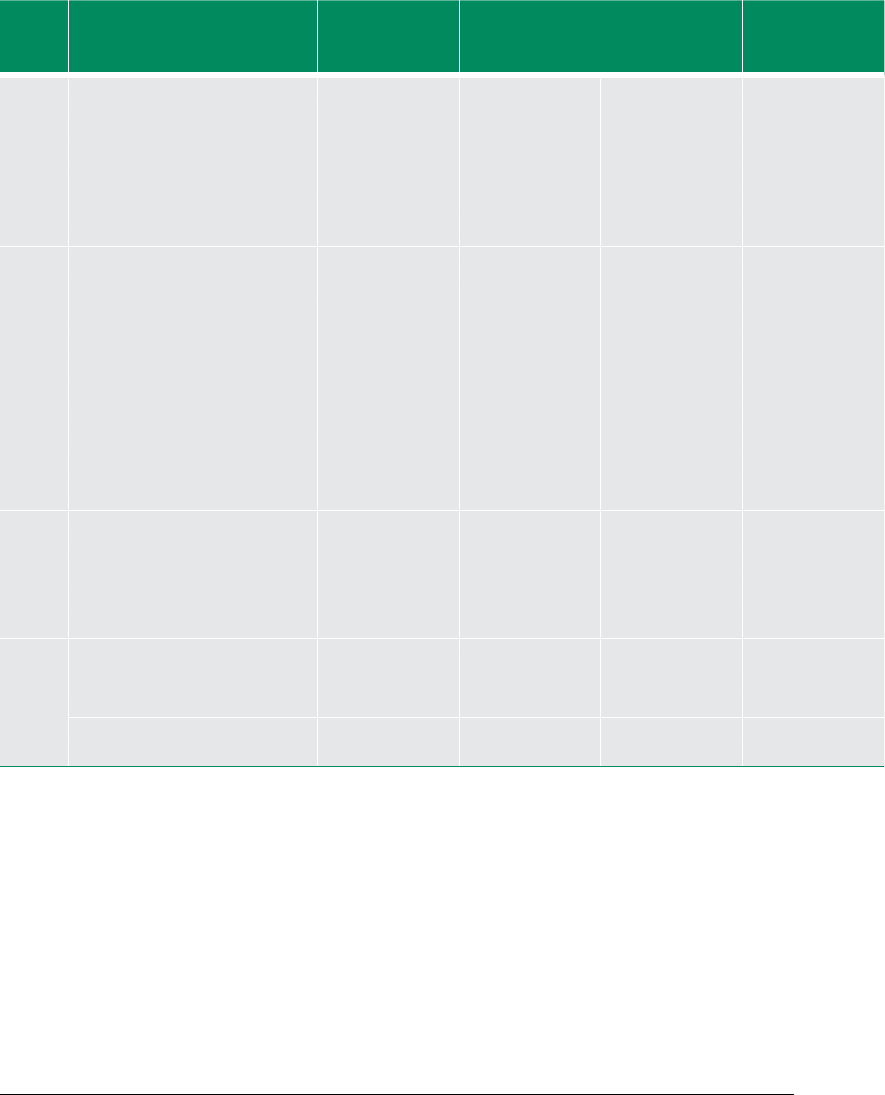
71
Priority
intervention
area(s)
Prioritized
interventions
Prioritized bottlenecks Prioritized acceleration solution Potential partners Total cost (USD) Available resources/
partners
Resource gap
Inadequate production and
procurement of skilled health
workers including midwives,
doctors, obstetricians,
gynaecologists specialist and tutors
(covers also SD IST, Anaesthesia,
etc.)
Increase production of midwives and tutors,
and target and train midwives and doctors to
provide maternal and newborn care services
MoE, GHS, MoH, UNFPA, USAID,
MDBS group members
350,000 200,000 Government of
Ghana
150,000
Inadequate accessibility as a result
of inadequate transport, poor road
networks, weak referral systems
(i.e. penetration and coverage of
National Ambulance Service)
Strengthen the referral system to make it
more responsive
• Develop MOU with transport unions to
improve transportation of pregnant women
with complication
• Develop MOU with communication agencies
to strengthen and roll out of mobile-phone-
based emergency response linked with the
mobilehealth policy
• Expand the National Ambulance Service
including DA ambulance support
• Design proper anaesthesia system
MoH/GHS, transport unions, MoC
500,000
100,000
30,000,000
125,000
0
25,000,000
DAs
Government of
Ghana
375,000
100,000
5,000,000
(b) Improve referral
and strengthen BTS in
line with the National
Blood Transfusion
Policy
Lack of legal framework for (BTS) Lobby for the passage of the Health Bill
including BTS
ICC for Maternal Health,
development partners
(c) Scale up LSS
training and build
Regional Resource
Teams
Inadequate human resource
capacity and equipment to expand
coverage of LSS and ENC services
Strengthen LSS training and build Regional
Resource Teams
Improve access to ENBC services at all levels
(neonatal resuscitation, kangaroo mother
care, rooming-in)
MoH/GHS, development partners 768,000 300,000 Health partners,
Government of
Ghana
468,000
153,491,100 86,447,000 70,740,100
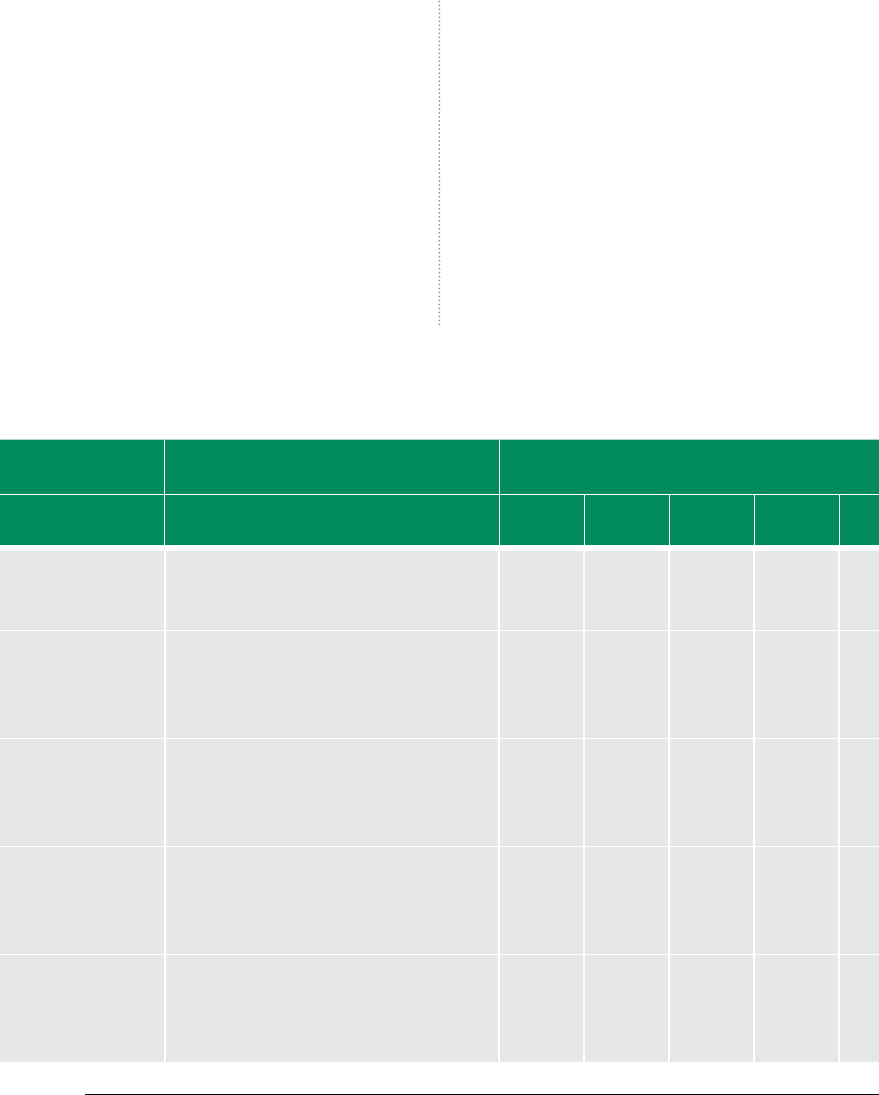
72
6.2 IMPLEMENTATION AND
MONITORING PLAN
The MDGs remain achievable by 2015 if backed by
the right policies, implementation strategies and
actions, coupled with strong political commitment,
and adequate funding and institutional capacities.
Central to the success of this Action Plan will be
the coordinated approach of implementation that
targets effective service delivery for the provision of
EmONC, SD and FP.
Usually, such an effort is hampered by a weak moni-
toring system, particularly in assessing the effec-
tiveness of services in terms of their coverage or
outcomes at all levels. By using the appropriate tools,
for example the Systematic Coverage Evaluation tool
and the NDPC monitoring framework , it is possible
for service providers and health managers to stay
on track and remain accountable.
The collaborative and inclusive process through
which this MAF and CAP have been written are ini-
tial good steps in the right direction. The objective
of the implementation and monitoring plan — as
an integral part of the Country Action Plan — is to
follow up on commitments made and, above all,
track progress over time.
TABLE 9 GHANA MDG 5 IMPLEMENTATION AND MONITORING PLAN
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Procure and use PDAs
for FP data capture at
service delivery point
Number of subdistricts/districts using PDAs for
data capture.
Number of PDAs procured.
X X See above table
8 for responsible
partners
Address DHIMS
bottlenecks in
DHIMS-2 and roll out
training on PDAs and
DHIMS
DHIMS-2 completed.
Number of districts using DHIMS-2 for data
reporting
X X
Advocate for DAs to
fund maternal health
interventions through
District Development
Fund
Percentage of districts supporting maternal
health through DDF
X X
Develop proposal
and mobilize
the international
community for
funding
Number of successful proposals for maternal
health
X X X X X X
Periodic and routine
assessment of EmONC
and other essential
maternal health
services
Number of routine assessments done,
% HFs providing ANC/PNC
% ANC clients with 4+ visits. % ITN use; %HIV
tested; % IPT2
X X X X
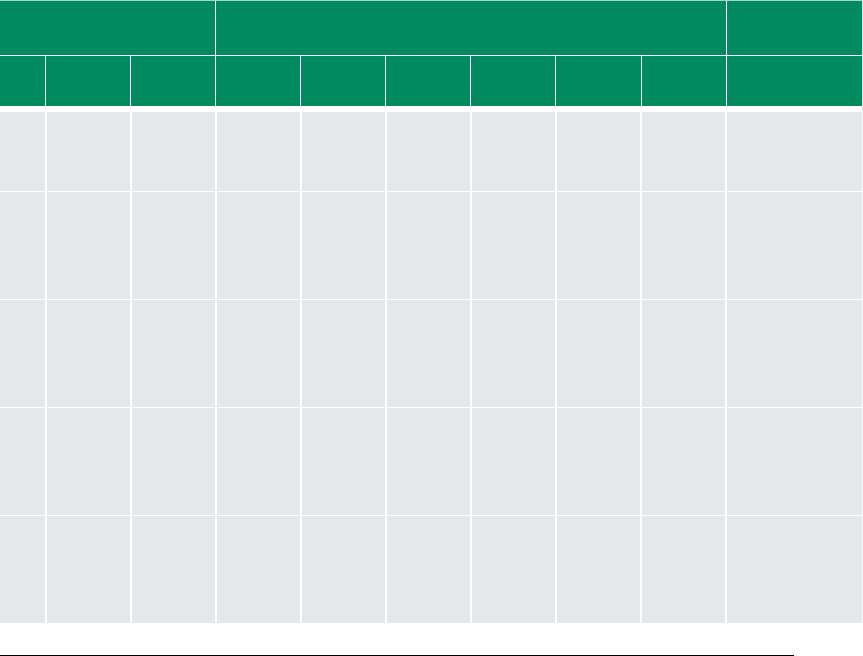
73
TABLE 9 GHANA MDG 5 IMPLEMENTATION AND MONITORING PLAN
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Procure and use PDAs
for FP data capture at
service delivery point
Number of subdistricts/districts using PDAs for
data capture.
Number of PDAs procured.
X X See above table
8 for responsible
partners
Address DHIMS
bottlenecks in
DHIMS-2 and roll out
training on PDAs and
DHIMS
DHIMS-2 completed.
Number of districts using DHIMS-2 for data
reporting
X X
Advocate for DAs to
fund maternal health
interventions through
District Development
Fund
Percentage of districts supporting maternal
health through DDF
X X
Develop proposal
and mobilize
the international
community for
funding
Number of successful proposals for maternal
health
X X X X X X
Periodic and routine
assessment of EmONC
and other essential
maternal health
services
Number of routine assessments done,
% HFs providing ANC/PNC
% ANC clients with 4+ visits. % ITN use; %HIV
tested; % IPT2
X X X X
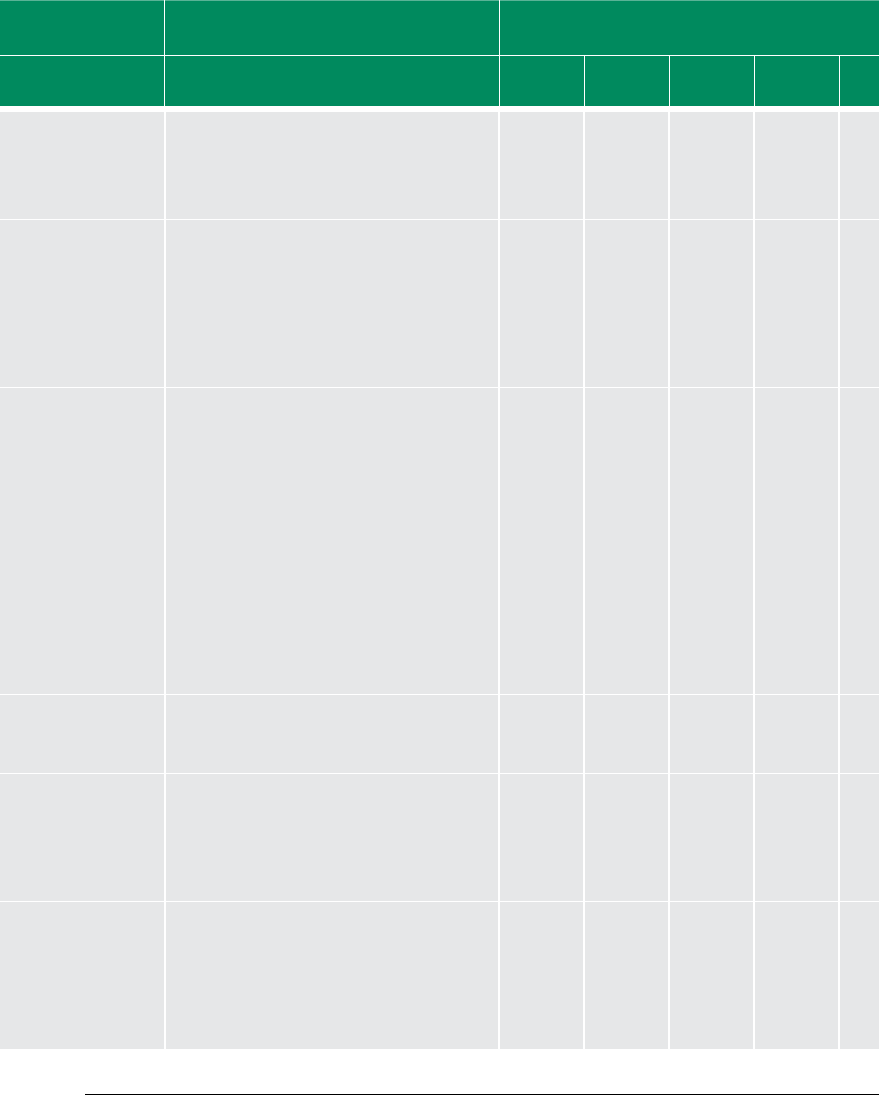
74
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Training in and
ensure the conduct
of comprehensive
FP services including
counselling
Number of sta trained X X
Intensify public
education and BCC
for integrated MCH
Services (Targeting
males to meet unmet
needs for FP, and
Obstetric/Neonatal
Danger Signs)
Contraceptive acceptor rate, % private sector
FP commodities supplumented, ratio of donor
to GOG funds for contraceptives, % of CHWs
and CHOs trained in HBLSS, number of BCC/IEC
materials,
X X X
X X
Upgrade health
institutions (using
EmONC assessment
results), categorize
and provide realistic
stang norm (based
on work load analysis
to provide BEmONC
(health centres) and
CEmONC (district
hospitals)
Number of health facilities upgraded
% facilities oering BEOC
% districts oering CEOC
% districts with transfusion service
X
Improve supervision
and monitoring
(horizontal etc.)
Improved quality of care according to national
standards
X X X
Sustain new
midwifery schools
and expansion of
midwives pre-service
intake and OBG eld
sites
New midwifery schools established.
Number of enrolled midwives in training
institutions
X X X
Use EmONC
assessment to
establish the extent
of access and
referral gaps, make
recommendations
and address them
Access gaps established X
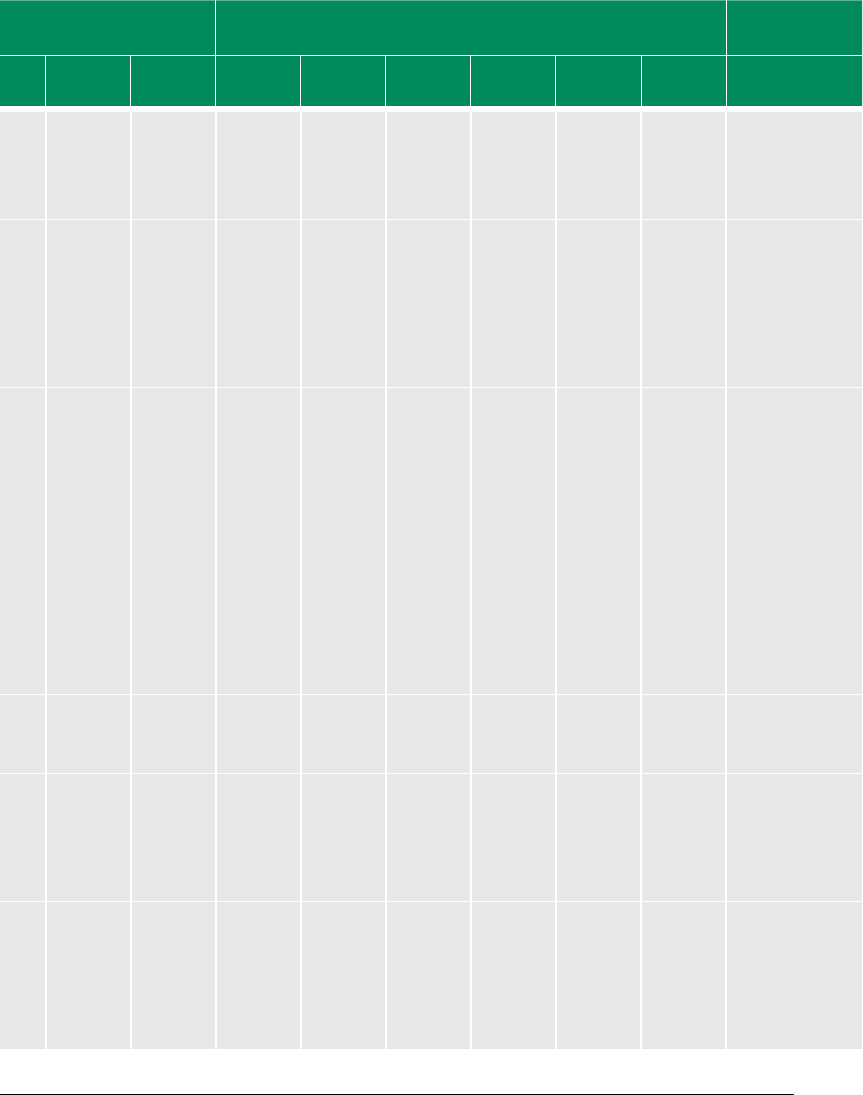
75
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Training in and
ensure the conduct
of comprehensive
FP services including
counselling
Number of sta trained X X
Intensify public
education and BCC
for integrated MCH
Services (Targeting
males to meet unmet
needs for FP, and
Obstetric/Neonatal
Danger Signs)
Contraceptive acceptor rate, % private sector
FP commodities supplumented, ratio of donor
to GOG funds for contraceptives, % of CHWs
and CHOs trained in HBLSS, number of BCC/IEC
materials,
X X X
X X
Upgrade health
institutions (using
EmONC assessment
results), categorize
and provide realistic
stang norm (based
on work load analysis
to provide BEmONC
(health centres) and
CEmONC (district
hospitals)
Number of health facilities upgraded
% facilities oering BEOC
% districts oering CEOC
% districts with transfusion service
X
Improve supervision
and monitoring
(horizontal etc.)
Improved quality of care according to national
standards
X X X
Sustain new
midwifery schools
and expansion of
midwives pre-service
intake and OBG eld
sites
New midwifery schools established.
Number of enrolled midwives in training
institutions
X X X
Use EmONC
assessment to
establish the extent
of access and
referral gaps, make
recommendations
and address them
Access gaps established X
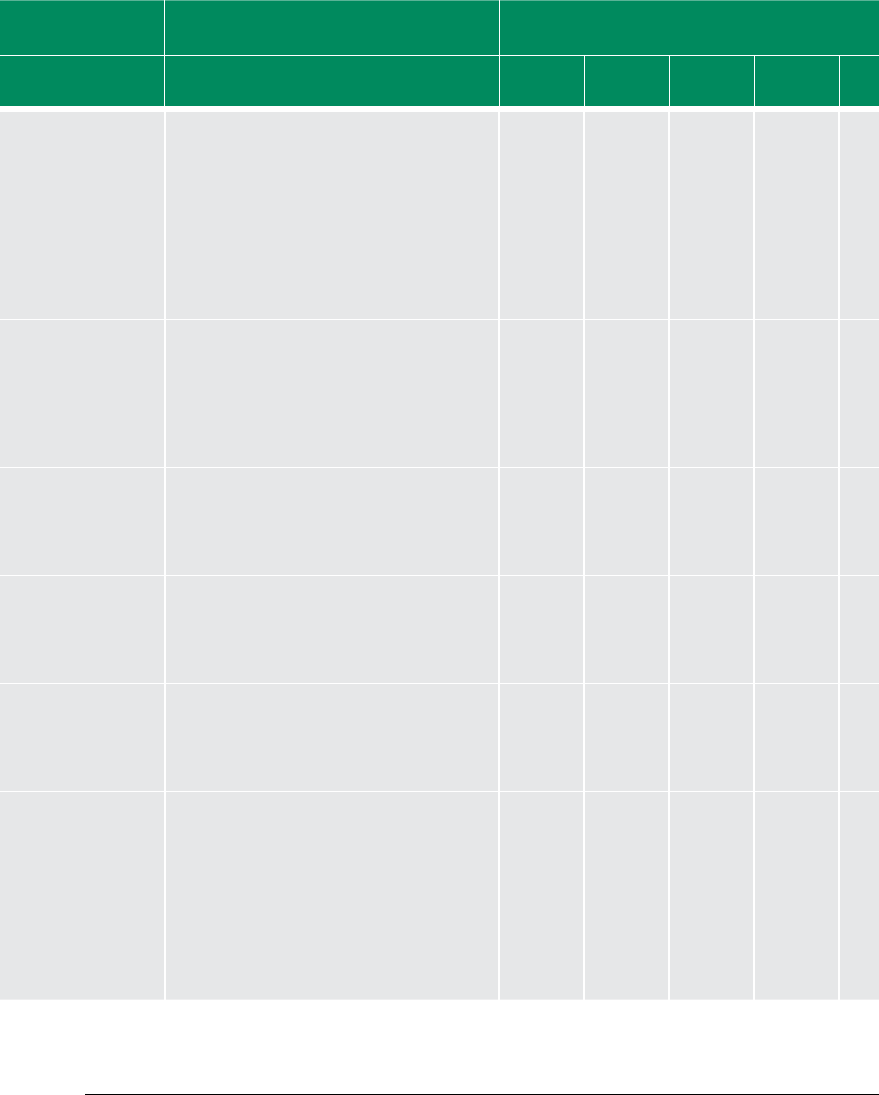
76
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Establish and
strengthen ICC
on Maternal and
Newborn Health
with TOR to
include ensuring
implementation of
recommendations
from EmONC
assessment
ICC established.
Quarterly meetings held
X X X X
Advocate for Oce
of the First Lady/
Gentleman to
champion maternal
health and identify
and appoint maternal
health champions
Oce of First Lady/Gentleman appoints
champion for maternal health
X
Strengthen country
coordination of donor
support in line with
National Aid Policy
Proper coordination of donor support as per
National Aid Policy
X X X X X
Advocate for DAs to
fund maternal health
interventions through
District Development
Fund
**Repeated above X X
Develop proposal
and mobilize
the international
community for
funding
**Repeated above X X X X X
Strengthen
intersectoral
collaboration
for delivery of
maternal health
services (Ministries,
departments,
agencies, partners,
Trade Union
Congress)
Number of intersectoral meetings held on
maternal health
X X X X X
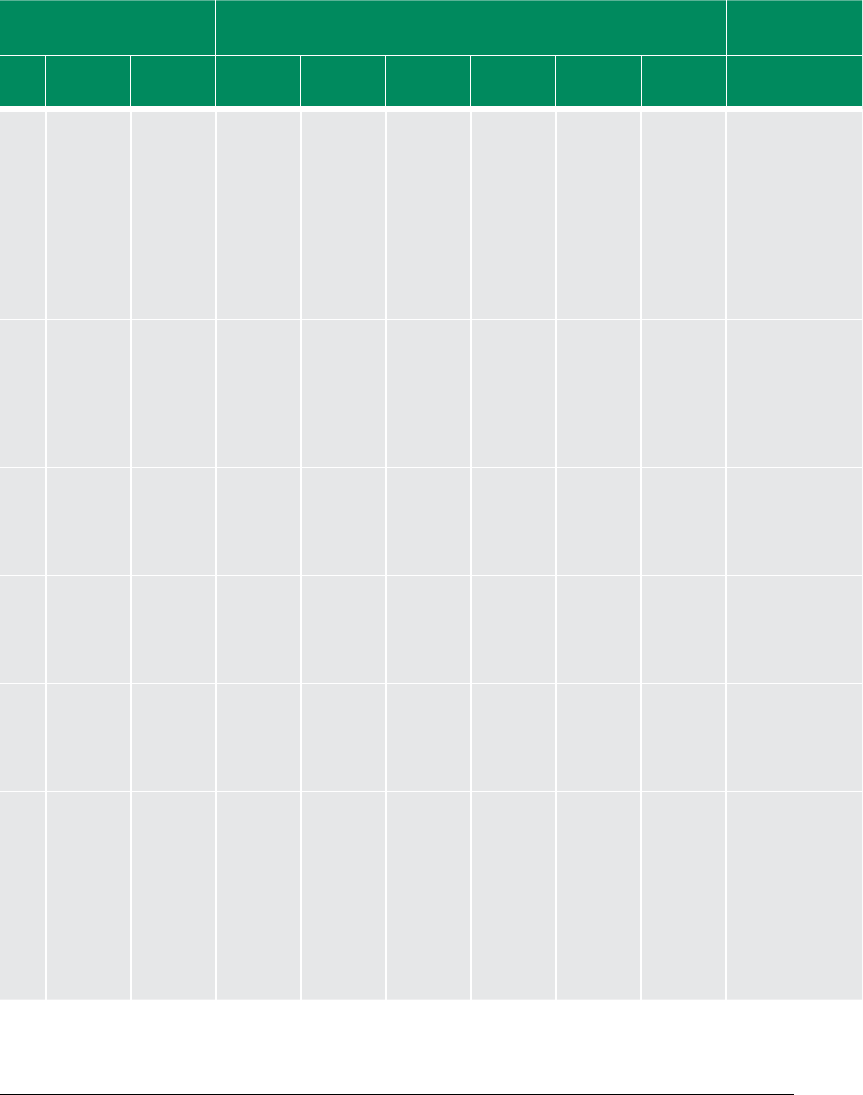
77
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Establish and
strengthen ICC
on Maternal and
Newborn Health
with TOR to
include ensuring
implementation of
recommendations
from EmONC
assessment
ICC established.
Quarterly meetings held
X X X X
Advocate for Oce
of the First Lady/
Gentleman to
champion maternal
health and identify
and appoint maternal
health champions
Oce of First Lady/Gentleman appoints
champion for maternal health
X
Strengthen country
coordination of donor
support in line with
National Aid Policy
Proper coordination of donor support as per
National Aid Policy
X X X X X
Advocate for DAs to
fund maternal health
interventions through
District Development
Fund
**Repeated above X X
Develop proposal
and mobilize
the international
community for
funding
**Repeated above X X X X X
Strengthen
intersectoral
collaboration
for delivery of
maternal health
services (Ministries,
departments,
agencies, partners,
Trade Union
Congress)
Number of intersectoral meetings held on
maternal health
X X X X X
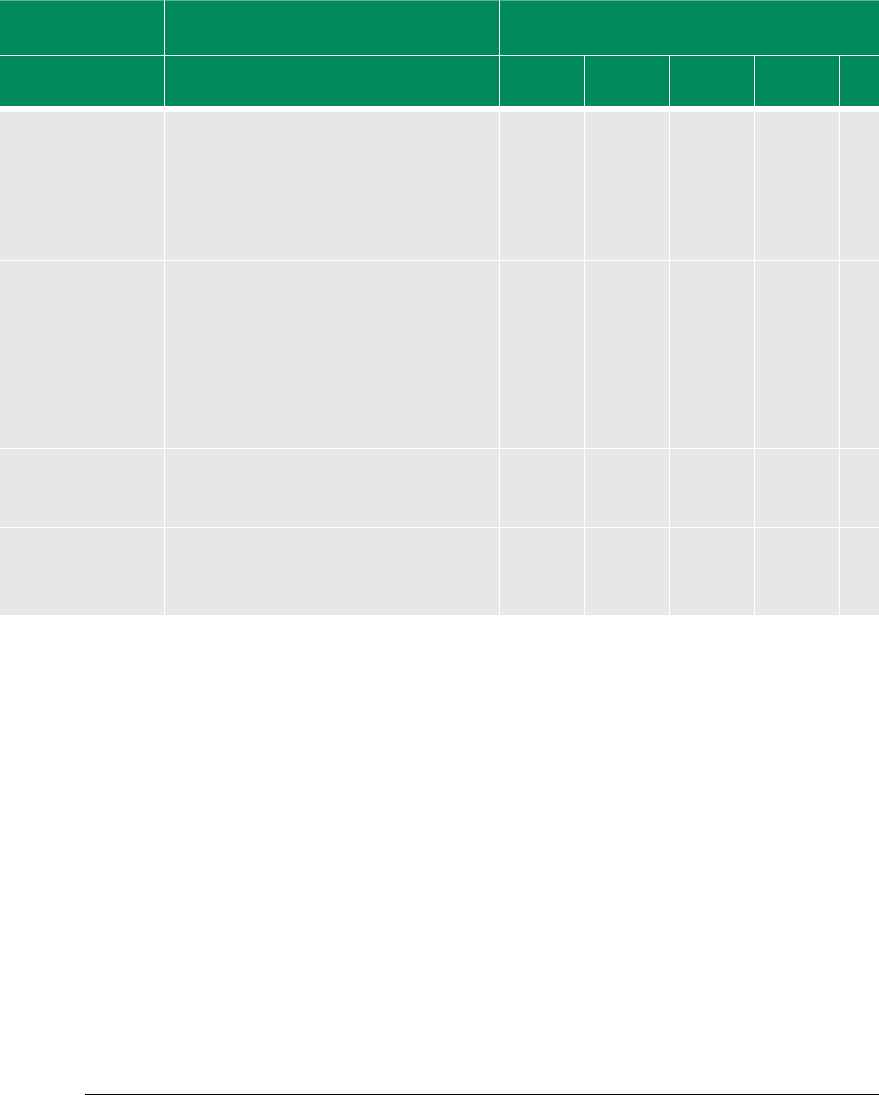
78
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Increase production
of midwives/tutors,
and target and
train midwives, and
doctors to provide
maternal and
newborn care services
Number of sta produced X X X X X
Strengthen the
referral system
to make it more
responsive
- MOU with transport
unions
-Expansion of
National Ambulance
Service
Improved referral system as per national
guidelines.
Number of districts with MOU with transport
unions
X X X X X
Lobby for the passage
of the Health Bill
including BTS
Passage of health bills X
Strengthen LSS
training and build
Regional Resource
Teams
Number of key sta trained in LSS.
Number of skilled attendants
X X
NB: Use sector-wide indicators.
7978
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Increase production
of midwives/tutors,
and target and
train midwives, and
doctors to provide
maternal and
newborn care services
Number of sta produced X X X X X
Strengthen the
referral system
to make it more
responsive
- MOU with transport
unions
-Expansion of
National Ambulance
Service
Improved referral system as per national
guidelines.
Number of districts with MOU with transport
unions
X X X X X
Lobby for the passage
of the Health Bill
including BTS
Passage of health bills X
Strengthen LSS
training and build
Regional Resource
Teams
Number of key sta trained in LSS.
Number of skilled attendants
X X
NB: Use sector-wide indicators.
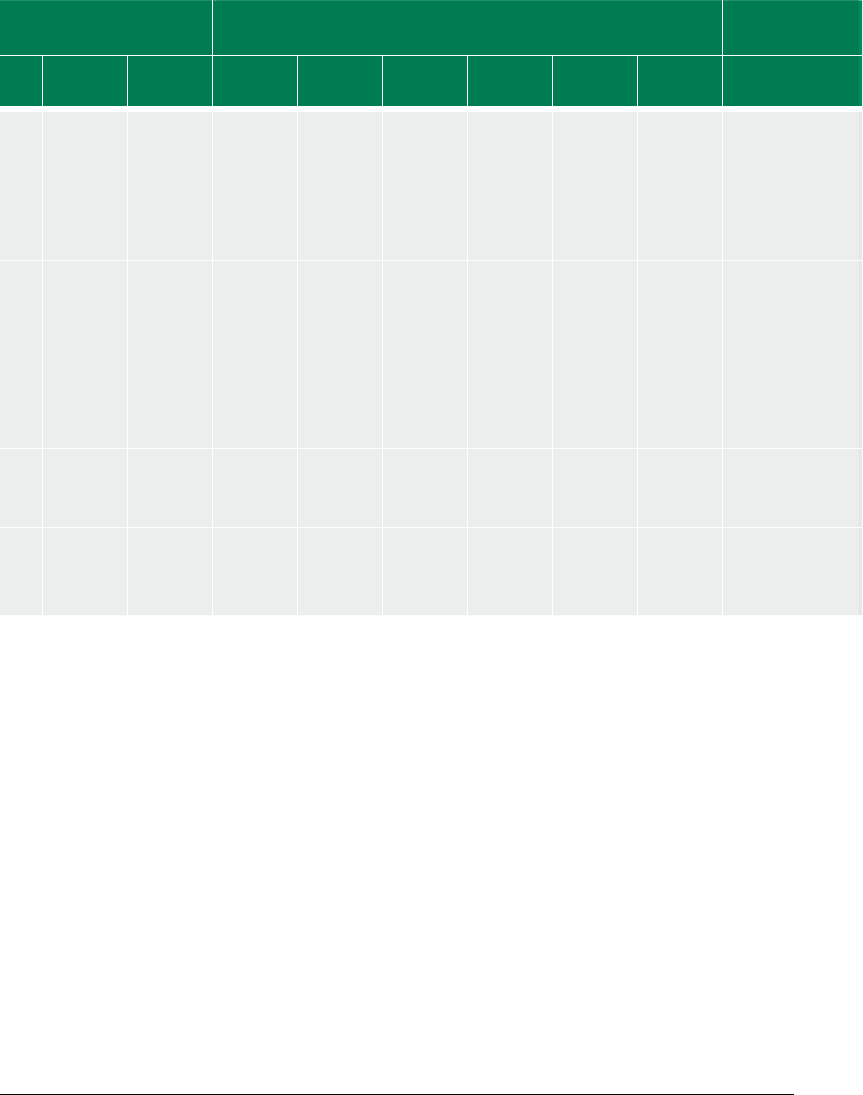
79
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013 2014 2015 2010 2011 2012 2013 2014 2015
Increase production
of midwives/tutors,
and target and
train midwives, and
doctors to provide
maternal and
newborn care services
Number of sta produced X X X X X
Strengthen the
referral system
to make it more
responsive
- MOU with transport
unions
-Expansion of
National Ambulance
Service
Improved referral system as per national
guidelines.
Number of districts with MOU with transport
unions
X X X X X
Lobby for the passage
of the Health Bill
including BTS
Passage of health bills X
Strengthen LSS
training and build
Regional Resource
Teams
Number of key sta trained in LSS.
Number of skilled attendants
X X
NB: Use sector-wide indicators.
7978
Acceleration
solution/activities
Indicator IMPLEMENTATION TIME LINE
(2011–2015
Indicator for monitoring
(yearly)
Responsible MDA
(structure)
2010 2011 2012 2013
2014 2015 2010 2011 2012 2013 2014 2015
Increase production
of midwives/tutors,
and target and
train midwives, and
doctors to provide
maternal and
newborn care services
Number of sta produced X X X
X X
Strengthen the
referral system
to make it more
responsive
- MOU with transport
unions
-Expansion of
National Ambulance
Service
Improved referral system as per national
guidelines.
Number of districts with MOU with transport
unions
X X X
X X
Lobby for the passage
of the Health Bill
including BTS
Passage of health bills X
Strengthen LSS
training and build
Regional Resource
Teams
Number of key sta trained in LSS.
Number of skilled attendants
X X
NB: Use sector-wide indicators.

80
ANNEXES
Photo: Kayla Keenan
81
ANNEX 1: POLICY DOCUMENTS
AND REPORTS
1.
Road map for accelerating the attainment of
the MDGs related to maternal and newborn
health in Ghana
2.
Road map for repositioning FP in Ghana
2006–2010
3.
Prevention and management of unsafe
abortion: comprehensive abortion services,
standards and protocol
4. National reproductive health service, policy
and standards
5. MoH 2010 POW
6.
Improving access to quality care in FP, medi-
cal eligibility criteria for contraceptive use
(MEC Wheel)
7.
Revised child health policy 2007–2015, Dr.
Aboagye/UNICEF
8.
Reproductive health strategic plan 2007–
2011
9. Safe motherhood protocol
10. FP protocol
11.
Ghana Reproductive Health Strategic Plan
(2006–2010)
12.
Creation of Inter-Ministerial Task Force for
Maternal Mortality Reduction (2008)
13.
Creation of Making Pregnancy Safer Task
Force
14.
‘REDUCE’ Model for improving maternal and
newborn survival in Ghana
15.
Proposal by UNICEF, UNFPA and WHO on
achieving the health MDGs in Ghana (2009,
enclosed)
16.
CARMMA (AU Campaign on Accelerated Re-
duction of Maternal Mortality, 2009)
17. Development of Emergency Obstetric and
Newborn Care (EmONC) Needs Assessment
(2010)
18.
Minister of Health declaring maternal mortal-
ity a national emergency (2008)
19. Report on the National Consultative Meet-
ing on the Reduction of Maternal Mortality
in Ghana (2008)
20.
Launch of the Commission of Women’s
Health in the African Region (2010)
NATIONAL (GOVERNMENT) POLICY
DOCUMENTS
21.
Ghana Poverty Reduction Strategy 2003–
2005
22.
Growth and Poverty Reduction Strategy
(GPRS II) (2006–2008)
23.
The millennium villages project Bonsaaso
Ghana cluster
24.
Draft Medium-Term National Develop-
ment Policy Framework 2010–2013
GENERAL HEALTH POLICY DOCUMENTS
25. National health policy
26. MoH gender policy
27. Adolescent reproductive health policy
28. National e-health strategy
29.
Ghana health sector five-year programme of
work 2002–2006, an in-depth review of the
health sector response to maternal mortality
in Ghana by 2003
30.
Third health sector five-year plan 2007-2011
31.
GHS five-year strategic framework for service
delivery 2007–2011
32.
Health sector medium-term development
plan 2010–2013
33. Health Sector Policy and Annual Workplans
34. Guidelines on Nutrition
35. PMTC plus guidelines
36. Early Infant diagnosis (EID) 2009
37.
Policies on orphans and vulnerable children
(OVCs)

82
REPORTS
38.
A paper on safe motherhood programme in
Ghana, prepared for Africa population com-
mission: West African regional conference
6–9 November 2006
39.
Health sector in Ghana: Facts and figures,
2009
40. Annual Report RCH 2007
41.
Annual Report FHD 2008, 2009
42.
Monitoring visit report for 2008 HIRD imple-
mentation in all regions
43.
Institutional analysis of safe motherhood
policy-making in Ghana
44.
Selected practices recommendation for con-
traceptive use 2008 update
45.
MEC wheel evaluation report WHO, Dr
Charles Fleisher
46. Strategic assessment of abortion care serv-
ices in Ghana
47. Readiness for abortion care services
48.
Time to take charge — advocacy tool for
resource mobilization
49. EmONC baseline report, 2005
50.
Annual Progress Reports of the GPRS I & II
(2005, 2006, 2007, 2008, 2009)
51. Demographic Health Survey (2003, 2008)
52.
Ghana Living Standards Survey (1999, 2006)
53. Ghana Maternal Health Survey (2007)
54.
Evaluation reports with reference to maternal
health care delivery
55. MDG Reports (2002, 2004, 2006, draft 2010
editions)
56.
Millennium Villages Project (MVP) Assess-
ment
57. Millennium Villages Project (MVP) reports
58.
WHO Access meeting/Midwifery training
and Pre-service curriculum reviews
59. MEC 2008 Update (ppt)
60.
Ghana maternal health survey 2007 dissemi-
nation (ppt)
61. Maternal mortality in Ghana (ppt)
62.
Reproductive health and maternal mortality
in Ghana (ppt)
63. Contraceptive security issues at facilities re-
view
64. HIRD progress report
65. Microeconomics in health
66. Health Sector Annual reports
67.
Citizen Assessment Report of the
NHIS
68.
Senior officers of MOH/GHS at various levels
of health care system
ANNEX 2: QUESTIONNAIRE
ADMINISTERED TO DDHS GROUP
Dear DDHS
The high maternal mortality rate in Ghana has been
of great concern to decision makers resulting in ma-
ternal being declared emergency in July, 2008. The
MAF is aimed at supporting national government
and her partners to better understand the deep-
rooted causes militating against positive outcomes
in maternal health care.
In this regard, your experience and expertise is be-
ing solicited.
In your opinion
1) What are some of the key existing policies on
Maternal Health in Ghana?
2) What are some of the key existing interventions
on Maternal Health in Ghana?
3) What are the gaps in the existing policies and
interventions on Maternal Health Care in Ghana?
4) What are the major bottlenecks (challenges)
to the effective implementation of the key in-
terventions for accelerating progress on MDG5
in Ghana?
5) What are the key cost effective solutions that
can accelerate progress of Maternal Health Care
in Ghana?

83
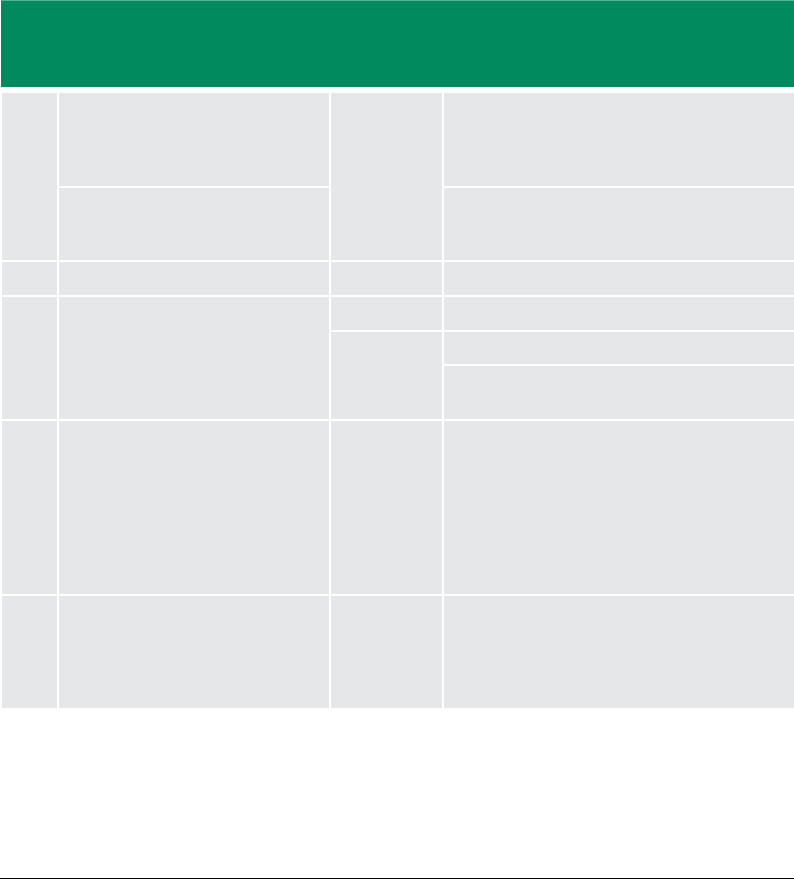
84
ANNEX 3: MDG 5 DOCUMENTS,
RECOMMENDATIONS AND
LEVEL OF IMPLEMENTATION
MAF TECHNICAL TEAM WORKING SESSION, 913 AUGUST 2010 AT GHS, ACCRA
No Document Year Recommendations Level of implementation Possible negative eect on MDG5
attainment
Comment
Partially Fully Unclear/nil Minimal Moderate High
1 Improving access to quality care
in FP: medical eligibility criteria for
contraceptive use (MEC Wheel)
3
To be used by all FP service points X X Not generally
available
GHS/Partners “revised Contraceptives
Procurement Tables (CPTs)” in March 2006
X X Level of
availability and
use not certain
2 2010 MOH Programme of Work 2010
3 A road map for repositioning FP in
Ghana, 2006–2010
4
2006 X
Expand service delivery sites X X
Expand resource mobilization and
contraceptive commodities
X X
4 Road Map for Accelerating the
attainment of the MDGs Related
Maternal and Neonatal Health In
Ghana 2007-2011
5
Track the following indicators:
-minimum of four visits per ANC client
- % facilities oering BEOC
- % districts oering CEOC
- % districts with BTS
- of HFs oering CAC
- % of facilities with good referral system for
maternal and neonatal health
X
X
X
X
X
X
5 Accelerating improvements in
maternal and newborn health in
northern Ghana, needs assessment
report, Oct 2005, UNICEF, UNFPA,
KNUST, GHS-RCH
Develop system to provide and track IST in
LSS for midwives to provide BEmOC?
X
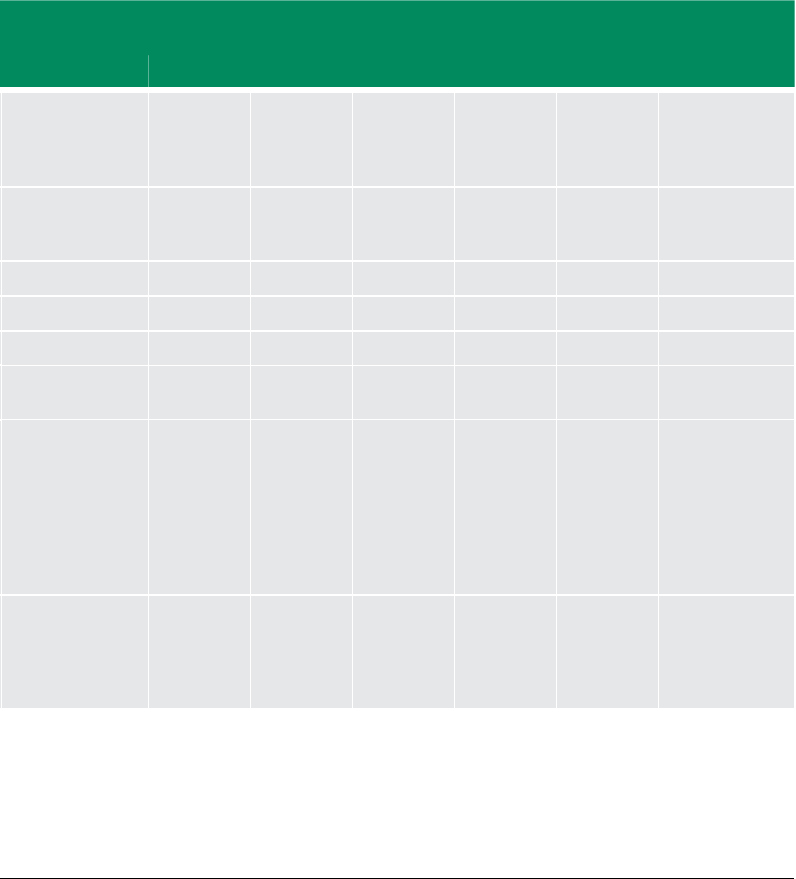
85
MAF TECHNICAL TEAM WORKING SESSION, 913 AUGUST 2010 AT GHS, ACCRA
No Document Year Recommendations Level of implementation Possible negative eect on MDG5
attainment
Comment
Partially Fully Unclear/nil Minimal Moderate High
1 Improving access to quality care
in FP: medical eligibility criteria for
contraceptive use (MEC Wheel)
3
To be used by all FP service points X X Not generally
available
GHS/Partners “revised Contraceptives
Procurement Tables (CPTs)” in March 2006
X X Level of
availability and
use not certain
2 2010 MOH Programme of Work 2010
3 A road map for repositioning FP in
Ghana, 2006–2010
4
2006 X
Expand service delivery sites X X
Expand resource mobilization and
contraceptive commodities
X X
4 Road Map for Accelerating the
attainment of the MDGs Related
Maternal and Neonatal Health In
Ghana 2007-2011
5
Track the following indicators:
-minimum of four visits per ANC client
- % facilities oering BEOC
- % districts oering CEOC
- % districts with BTS
- of HFs oering CAC
- % of facilities with good referral system for
maternal and neonatal health
X
X
X
X
X
X
5 Accelerating improvements in
maternal and newborn health in
northern Ghana, needs assessment
report, Oct 2005, UNICEF, UNFPA,
KNUST, GHS-RCH
Develop system to provide and track IST in
LSS for midwives to provide BEmOC?
X
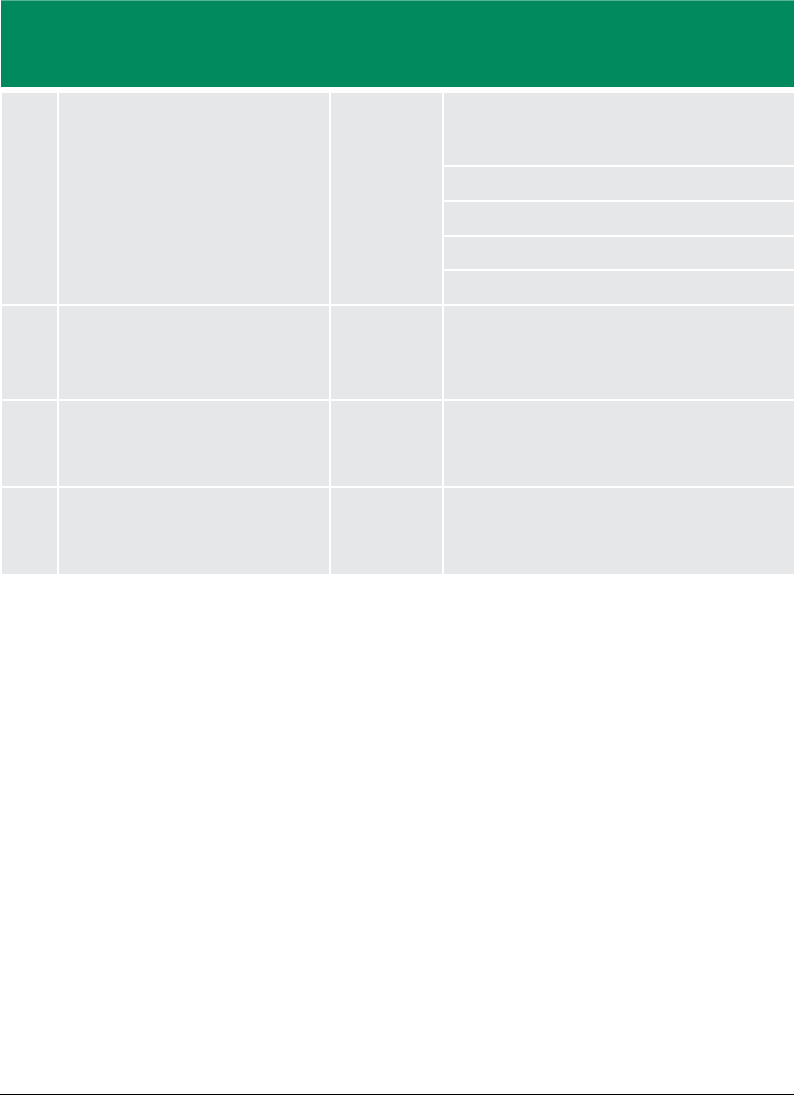
86
No Document Year Recommendations Level of implementation Possible negative eect on MDG5
attainment
Comment
Partially Fully Unclear/nil Minimal Moderate High
6 National reproductive health service
policy and standards,
6
2003, GHS
Decentralize greater proportion of funds for
reproductive health shall be decentralized to
the district level
X X
Clinical skills training, X X
Equipment supply X X
Build partnerships X X
Integrate X X
7 A paper on safe motherhood
programme in Ghana, Nov 2006, Odoi
Agyarko et al.
2006
8 Title: Ministry of Health (2009), Health
Sector Gender Policy, April 2009
Address gender inequalities in health service
delivery to ensures integration of gender
issues in service provision
9 Title: Gender Issues Paper (Second
Draft). Ministry of Health, Agyare-
Kwabi
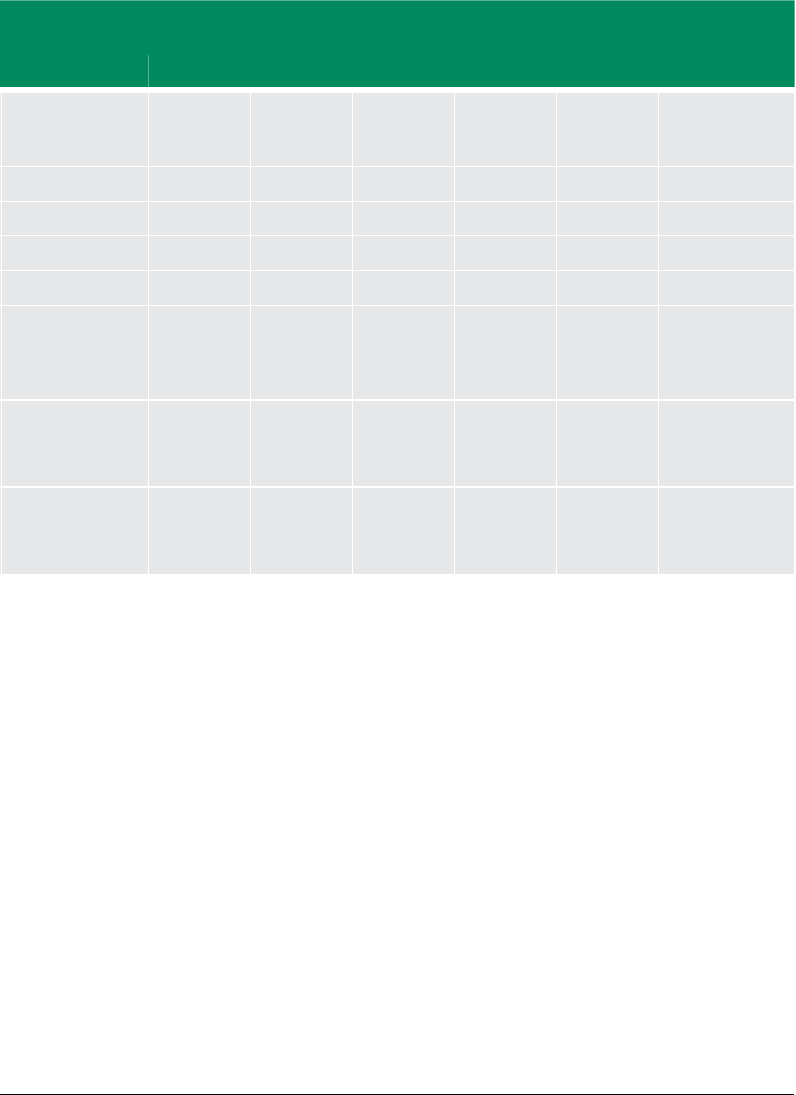
87
No Document Year Recommendations Level of implementation Possible negative eect on MDG5
attainment
Comment
Partially Fully Unclear/nil Minimal Moderate High
6 National reproductive health service
policy and standards,
6
2003, GHS
Decentralize greater proportion of funds for
reproductive health shall be decentralized to
the district level
X X
Clinical skills training, X X
Equipment supply X X
Build partnerships X X
Integrate X X
7 A paper on safe motherhood
programme in Ghana, Nov 2006, Odoi
Agyarko et al.
2006
8 Title: Ministry of Health (2009), Health
Sector Gender Policy, April 2009
Address gender inequalities in health service
delivery to ensures integration of gender
issues in service provision
9 Title: Gender Issues Paper (Second
Draft). Ministry of Health, Agyare-
Kwabi
88
ANNEX 4: REFERENCES
Ghana Poverty Reduction Strategy 2003–
2005: An Agenda for Growth and Prosper-
ity. Volume 1, Analysis and Policy Statement.
National Development Planning Commission,
February 2003
This is a comprehensive national development pol-
icy framework in support of poverty reduction and
growth. The document links HIV/AIDS strongly with
poverty and defines interventions to prevent new
infections of HIV, promote safer sex, prevent Mother
to Child Transmission, ensure safe blood and blood
products and improve STI management (target:
base year 2000 to 24 percent by 2005). It also aims
at providing a continuum of care or people living
with HIV/AIDS (PLWHA) and their families, continu-
ous supportive counseling and palliative care in the
household and community and the management
of opportunistic infections target: base year 2000
of 5.8 percent to 15 percent by 2005 for women
and 2000 of 15.4 percent to 25 percent by 2005 for
men ). Other interventions laid out include effective
institutional foundation (target: base year 2000 to 24
percent, 2005), joint interventions on health care and
safe water and environmental sanitation, access to
quality health and nutrition services, susstainable
financing arrangements that protect the poor, and
efficiency in service delivery with the following tar-
gets: IMR 57/1,000lbs (2000) to 50/1000 (2005); MMR
200/100,000lbs (2000) and 160/100,000lbs (2005)
and SD 49 percent (2000) to 55 percent (2005).
Growth and Poverty Reduction Strategy (GRSP
II) (2006–2009), Volume 1, Policy Framework,
November 2005, National Development Plan-
ning Commission
Policy issues: The policy goal was to attain middle-
income status (with a per capita income of at least
$1,000) by the year 2015 within a decentralized and
democratic environment. The main issues include a
broad national development framework, health care,
safe water and environmental sanitation, access to
quality health and nutrition services, sustainable
financing arrangements that protect the poor, and
efficiency in service delivery. The intervention and
targets were the MDGs 4 and 5 and the development
and implementation of high-impact yielding strate-
gies for U5M, maternal mortality, malnutrition and
redistribution of health workers in favour of deprived
areas and improvement of CHPS.
Monitoring Visit Report for 2008 HIRD imple-
mentation in all regions. (2008) GHS
The aim of this assessment was to look at HIRD im-
plementation at regional, district and subdistrict
levels. The assessment found that all regions had
trained staff in LSS, usage of partographs and neo-
natal resuscitation. The main challenges were: (a)
unavailability of necessary logistics; (b) insufficient
health staff (quantity and quality); (c) insufficient
funds; (d) lack of transportation; and (e) frequent
breakdown of motorbikes and high maintenance
costs (i.e., Jialing motorbikes).
Institutional Analysis of Safe Motherhood Policy-
Making in Ghana, IMMPACT, NMIMR, 2005
The main aim of the safe motherhood policy is to
reduce maternal mortality. It identifies the following
areas to be tackled to achieve the policy objective:
(a) low health education; (b) poor monitoring; (c)
sustainability of free delivery; (d) sociocultural beliefs
and practices (leading to a delay in seeking care); (e)
institutional arrangement (dilemma of clinical care
and public health); (f ) insufficient health staff; and
(g) cost of services (including transportation).
89
Under-ve Child Health Strategy: 2007–2015.
MOH, Ghana.
This strategic document focuses on achieving MDG
4 (reduction of child mortality from 111/1000 in 2006
to 10/1000 in 2015). The key interventions identified
were antenatal care, delivery care, postnatal care,
immunizations, nutrition, treatment of child illness
and prevention of malaria.
Targets are set for focused antenatal care (FANC) and
SD: proportion of deliveries undertaken by skilled
birth attendants; 50 percent (2006) to 65 percent,
neonatal interventions and children between the
ages of 1 and 59 months.
Among the targets are increasing the following rates:
exclusive breast feeding for six months, from 54 per-
cent (2006) to 75 percent (2015); the proportion of
children aged six to 59 months who have received
a dose of vitamin A in the previous six months, from
60 percent (2006) to 90 percent (2011); the propor-
tion of children aged 12 to 23 months who are fully
vaccinated, from 64 percent (2006) to 70 percent
(2011); the proportion of children sleeping under
insecticide-treated nets the previous night from 22
percent (2006) to 55 percent (2011); the proportion
of children with fever receiving an appropriate anti-
malarial within 24 hrs, from 61 percent (2006) to 70
percent (2011); the proportion of children with wa-
tery diarrhoea receiving ORT, from 37 percent (2006)
to 60 percent (2011); the proportion of children with
watery diarrhoea receiving ORT and an appropriate
course of zinc, from 25 percent (2011); and the pro-
portion of children with suspected pneumonia who
received appropriate antibiotics, from 33 percent
(2006) to 50 percent (2011).
National e-Health Strategy, MoH
The e-Health strategy, “the combined use of electron-
ic information and communication technology in
the health sector” (WHO definition) aims to improve
access to information in support of safe, efficient
and effective health care delivery in a timely manner
and at the point of need. It guides the deployment
of information and communication technology at
all levels of the health system, to enable the com-
munication and exchange of information among
multi-disciplinary health teams to provide better
coordinated and seamless health care, improve the
quality and efficiency of decision-making to clinical
practice through better access to health informa-
tion, clinical evidence and clinical decision support
tools, and provides access to appropriately packaged
information to enable individuals to make informed
health choices to manage, control and improve per-
sonal health outcomes in all parts of the country.
For the health care provider, it is to improve their sys-
tems for patient record keeping, web-based disease
surveillance, electronic prescriptions, referral man-
agement, patient appointments and e-consultation
and remote service. It aims to benefit health care
managers by improving financial, performance, hu-
man resource and logistics management systems.
Consumers are to benefit by enhanced notifica-
tion systems, scheduled appointment programmes,
packaged public health messages and a health in-
formation resource network.
MoH 2010 Programme of Work, THE GHANA
HEALTH SECTOR (Going Beyond Strategy to Ac-
tion)
The goal of the health sector in the medium term
(2010–2013) is to ensure a healthy and productive
population that continues to reproduce safely.
The key issue is ensuring improved maternal and
child care. It highlights five main priorities with re-
gard to decreasing maternal and child mortality
through improved FP, SD, access to blood services,
comprehensive abortion care, neonatal care and
malnutrition. There are also strategic budgetary al-

90
locations for infrastructure and equipment related
to MDG 5.
Improving access to quality care in family plan-
ning: Medical eligibility criteria for contraceptive
use (MEC Wheel)
The wheel contains medical eligibility criteria and
tells providers if a woman presented with a known
medical or physical condition is able to use various
contraceptive methods safely and effectively and
has recommendations for combined pills, combined
injectable contraceptive, progesterone-only pills,
implants and copper-bearing IUD. This wheel, if used
appropriately by providers, will protect women who
want to use contraceptives from infections, and pos-
sible death from cardiovascular diseases, diabetes,
cancers, hypertension and postpartum-related
health issues.
A road map for repositioning family planning in
Ghana, 2006–2010
6
This document aims to ensure that FP becomes
the fulcrum for strengthening and advancing re-
productive health and rights and reposition FP as
a national priority.
(It has eight elements, namely policy, advocacy, BCC,
institutional coordination and collaboration, human
resource development and capacity-building, ex-
panding access to FP services, strengthening re-
source mobilization and research, and monitoring
and evaluation.)
The rationale is to achieve a stabilized total fertility
rate, by addressing the rapidly growing population,
the persistent gaps between FP knowledge and
use, and high unmet need for FP 34 percent, 22
percent for spacing and 12 percent for limiting- DHS
2003. The document recognizes the role of FP in the
achievement of MDG 5 and states in the introduc-
tion: “There is growing concern among population
and health experts in Ghana that under the existing
scenario, the goals of the Ghana Poverty Reduction
Strategy, key elements of the Millennium Develop-
ment Goals (MDGs)… are unlikely to be achieved”.
Firm targets are to be set for CPR, TFR, MMR and IMR
as stated in page 37. A comprehensive plan is to be
prepared by the National Population Council with
MoH/GHS and NDPC, with key stakeholder respon-
sibilities defined. A well coordinated and integrated
advocacy plan was developed and is expected to
be implemented. Service delivery sites, resource
mobilization and contraceptive commodities are
to be expanded and standardized formats for data
collection and analysis prepared. A comprehensive
training programme was also prepared but lack of
funding has limited its implementation.
Road map for accelerating the attainment of the
MDGs related to maternal and neonatal health
in Ghana 2007–2011
7
The road map provides a framework for the imple-
mentation of HIRD which uses evidence-based, feasi-
ble and cost-effective interventions in resource-poor
settings to achieve accelerated reduction in maternal
and newborn deaths. The health care facility level
interventions are skilled attendance, equipment and
supplies and EmONC. The community interventions
are IEC to improve good health practices and health-
seeking behaviour and to recognize danger signs.
The objectives are to increase ANC and PNC cover-
age; increase the proportion of skilled deliveries, im-
prove access to comprehensive and basic essential
obstetric care; increase the capacity of providers to
implement appropriate ENC; expand FP providers
and services; promote individual, family and com-
munity practices to improve maternal and neonatal
health; strengthen systems and mobilize resources
for maternal and neonatal health, and referral and
HMIS systems; strengthen supervision and monitor-
ing systems; and develop and implement a research
agenda. The document outlines all strategies and
6) GHS, A road map for repositioning Family Planning in Ghana, 2006-2010.
7) GHS, Road Map for Accelerating the Attainment of the MDGs Related to Maternal and Neonatal Health In Ghana 2007-2011
91
interventions and identifies implementing partners,
progress indicators and a budget.
National Reproductive health service policy and
standards
,8
2003, GHS
Issues: Sets out nine priority reproductive health ar-
eas and a child-centred continuum of care approach
for integrated service delivery. These areas are:
1. Safe motherhood;
2. FP;
3.
Prevention and management of unsafe abor-
tions and PAC;
4. Prevention and management of RTIs (STIs/
HIV/AIDS);
5. Prevention and management of infertility;
6. Prevention and management of cancer, in-
cluding breast cancer;
7.
Response to menopausal and andropause
concerns;
8.
Discouragement of harmful traditional prac-
tices;
9. Information and counselling.
The defined interventions are ANC, labour and
delivery care, PNC, PMTCT of HIV, IEC, affordable
commodities, infertility management and dual pro-
tection. Others include prevention of unwanted
pregnancies (abortion care services, management
of abortion-related complications).
Other interventions include the prevention and con-
trol of RTI (STI, HIV/AIDS), management and support
(PLWHA), prevention of infertility, treatment of infer-
tility, social support for infertile couples, prevention
of cancer (early detection and treatment, manag-
ing the terminally ill), awareness and management
(awareness of dangers, management and rehabilita-
tion of victims) and advocacy, community mobiliza-
tion, outreach programmes and database training.
Paper on the safe motherhood programme in
Ghana, November 2006, Odoi Agyarko et al.
This paper reviews the safe motherhood programme
as it started in 1987 in Ghana, outlines its objective
and interventions, looks at progress made and chal-
lenges (funding gaps, inadequate empowerment,
weak integration) and makes recommendations
(improved maternal care services, BCEC/CEmOC,
FP, AdH, AdV etc.) for the way forward. The paper,
however, does not get to the bottom of why the
safe motherhood interventions (HE, ANC, delivery
care, PNC, FP, the prevention and management of
unsafe abortions) are not giving the required results.
Accelerating improvements in maternal and
newborn health in northern Ghana, needs as-
sessment report, October 2005, UNICEF, UNFPA,
KNUST, GHS-RCH
This needs assessment report is set against a target
of at least one comprehensive and four basic EmOC
and ENC facilities per 200,000 people (or per health
district). Most of the health facilities surveyed have
the capacity to provide EmOC and ENC services on
a 24-hour basis, but only a few actually provided
such services.
The report found that while the target was met for
EmONC, the proportion of expected complications
actually managed was low (0.6 percent). The CS rate
was low. Among the challenges listed were lack of
theatres, the absence of EMoC/ENC in most health
centres, weak referral systems, inadequate midwives
and limited training in LSS and SMI.
1.
It was not possible to obtain information
on the following critical questions related
to EmONC and CHPS.
2.
What proportion of district hospitals have
theatres/doctors for CEmONC?
3. What proportion of HC/SDs have midwives
and can provide BEmONC?
8) GHS, National Reproductive health service policy and standards.
92
4.
What is new in the referral system in Ghana?
5. How many CHPS compounds does Ghana
have and what proportion of them have
midwives?
6.
What is the system to provide and track IST in
LSS for midwives and how do we know what
percentage trained in the last five years?
MoH (2009). Health Sector Gender Policy. April
2009
This policy objective focuses on gender barriers in
access to health care, promotion of professional
ethics and human rights, improvement of quality of
care, gender inequalities in health service delivery,
HIV/AIDS, gender-based violence, health financing
and governance.
Gender Issues Paper (Second Draft). MoH. Ag-
yare-Kwabi
This paper focuses on addressing gender inequal-
ity in health policies and looks at the usual health
services areas such as access, communicable and
non-communicable diseases, reproductive health,
HIV/AIDS, gender-based violence, mental health,
and traditional and cultural gender issues.
The Children’s Act, 1998. Act 560. Gazette noti-
cation 5 February 1999
This act focuses on the rights of the child and paren-
tal duties of care and protection, quasi-judicial and
judicial child adjudication (child panels and family tri-
bunals), parenting, custody, access and maintenance,
foster care and adoption, employment of children,
institutionalized care and miscellaneous matters.

GHANA
MDG ACCELERATION FRAMEWORK
AND COUNTRY ACTION PLAN
MATERNAL HEALTH
July 2011
18605 Ghana omslag.indd 1 25/05/11 00.30
