
CLINICAL ROTATIONS MANUAL
2021-2022
TABLE OF CONTENTS
KYCOM CORE ROTATION SITES. .
....................................................................................................................................
CLASS OF 2023 CLINICAL ROTATION
PROGRAM. .......................................................................................................
KYCOM ABSOLUTES. ..
..................................................................................................................................................... ..
INTRODUCTION ..
................................................................................................................................................................
ELECTIVE TIME. ..............................................................................................................................................................
COMLEX BOARD REVIEW GUIDELINES. ..................................................................................................................
INDEPENDENT STUDY – OST 799 AND OST 899. ......................................................................................................
SELECTIVE ROTATIONS. ..
........................................................................................................................................ ...
COMLEX-USA POLICY .............................................................................................................................................. ....
OBJECTIVES ................................................................................................................................................................ ....
STUDENT ELIGIBILITY FOR CLINICAL ROTATIONS. .................................................................................................
DRUG SCREEN POLICY. ......................................................................................................................................
CRIMINAL BACKGROUND CHECK POLICY. .............................................................................................. ...
IMMUNIZATIONS. ........................................................................................................................................... .....
ACADEMICS ..................................................................................................................................................... .....
ATTESTATION FORM. .................................................................................................................................... .....
STUDENT RESPONSIBILITIES ...................................................................................................................................... ....
REPORT FOR ROTATION ............................................................................................................................... ....
ATTENDANCE. ................................................................................................................................................. .....
SUBMISSION OF STUDENT CASE LOGS AND ROTATION EVALUATION .......................................... ....
MEDICAL INSURANCE. ........................................................................................................................................
HOUSING. ...............................................................................................................................................................
PROFESSIONALISM ........................................................................................................................................ .....
APPROVED ABSENCE AND LEAVE POLICIES. ......................................................................................................... ....
PERSONAL ILLNESS. ...................................................................................................................................... .....
TEMPORARY ABSENCE. ............................................................................................................................... .....
ATTENDANCE AT PROFESSIONAL CONFERENCES. ....................................................................................
INTERVIEW POLICY. ............................................................................................................................................
VACATIONS AND HOLIDAYS ...........................................................................................................................
EXTENDED LEAVE ....................................................................................................................................... ........
GENERAL ROTATIONS INFORMATION ..........................................................................................................................
STUDENT LIABILITY INSURANCE. ............................................................................................................ ......
STUDENT EVALUATION (GRADE). ............................................................................................................ .......
GRADE APPEALS. ..................................................................................................................................................
REMEDIATION POLICY ......................................................................................................................................
BLOOD BORNE PATHOGEN EXPOSURE AND POST-EXPOSURE PROPHYLAXIS ...................................
PREPARATION FOR RESIDENCY. .....................................................................................................................
SCHEDULING OF CORE CLINICAL ROTATIONS. ...........................................................................................
SCHEDULING OF ELECTIVE CLINICAL ROTATIONS. ........................................................................... .......
SCHEDULING OF SELECTIVE CLINICAL ROTATIONS ................................................................................
VISITNG STUDENT APPLICATION SYSTEM (VSAS) . ....................................................................................
CHANGES IN CORE CLINICAL ROTATIONS. ..................................................................................................
CHANGES IN ELECTIVE CLINICAL ROTATIONS ................................................................................... .......
THE CLINICAL COMPETENCY PROGRAM .....................................................................................................................
INTRODUCTION ..
.................................................................................................................................................
CLINICAL JOURNAL CLUB .................................................................................................................................
END OF SERVICE EXAMINATION MODULES COMAT ................................................................................
OPC V AND OPC VI ..............................................................................................................................................
EDUCATIONAL VIDEOS AND PROGRAMS. ............................................................................................. .......
CLINICAL CAPSTONE COURSE. ................................................................................................................. .......
AWARD OF HONORS. ................................................................................................................................... ........
GUIDELINES FOR PRECEPTORS ................................................................................................................................ .......
PRECEPTOR EDUCATIONAL RESPONSIBILITIES .................................................................................. .......
INSTRUCTIONAL OBJECTIVES FOR PRECEPTORS ............................................................................... ......
ATTENDING PHYSICIAN RESPONSIBILITIES ......................................................................................... ........
STUDENT RECORD KEEPING ..................................................................................................................................... .......
LOGS ................................................................................................................................................................ .......
GRADUATION REQUIREMENTS ................................................................................................................ ........
2
4
6
6
8
9
9
10
10
11
13
14
14
14
15
16
16
16
16
16
17
17
17
17
22
23
23
23
23
24
24
24
25
25
25
26
26
28
29
29
29
30
30
30
30
30
31
32
33
34
34
36
37
37
37
37
38
38
39
COURSE SYLLABI. .
........................................................................................................................................................... 40
CORE ROTATION CURRICULUM. .................................................................................................................................. 49
SELECTIVE ROTATION CURRICULUM .
...................................................................................................................... 69
ELECTIVE ROTATION CURRICULUM ........................................................................................................................ 80
REQUEST FOR
MS AND EVALUATION FORMS. ........................................................................................................ 110
3
ONLINE/VIRTUAL ROTATION CURRICULUM .......................................................................................................... 80

KYCOM CORE ROTATIONS SITES
Kentucky Core Sites
Pikeville Core Site
Pikeville Medical Center, Pikeville, Kentucky
Highlands ARH, Prestonsburg, Kentucky
ARH Our Lady of the Way, Martin, Kentucky
Paul B. Hall Medical Center, Paintsville, Kentucky
McDowell ARH Hospital, McDowell, Kentucky
Tug Valley ARH Hospital, South Williamson, Kentucky
Hazard Core Site
Hazard ARH Regional Medical Center, Hazard, Kentucky
Kentucky River Medical Center, Jackson, Kentucky
Henderson Core Site
Deaconess Henderson Hospital, Henderson, Kentucky
Lexington Core Site
Saint Joseph Health, Lexington, Kentucky
Baptist Health Hospital, Lexington, Kentucky
Lincoln Trail Core Site
Owensboro Health Twin Lakes Medical Center, Leitchfield, Kentucky
Louisville Core Site
Norton Healthcare, Louisville, Kentucky
Northeast Kentucky Area Health Education Center Core Site
Clark Regional Medical Center, Winchester, Kentucky
King’s Daughters Medical Center, Ashland, Kentucky
Meadowview Regional Medical Center, Maysville, Kentucky
St. Claire Regional Medical Center, Morehead, Kentucky
Saint Joseph Mount Sterling, Mount Sterling, Kentucky
Three Rivers Medical Center, Louisa, Kentucky
Northern Kentucky Core Site
Saint Elizabeth Healthcare, Covington, Ft. Thomas, Florence, and Edgewood, Kentucky
Owensboro Kentucky Core Site
Owensboro Medical Health System, Owensboro, Kentucky
Prestonsburg Kentucky Core Site
Highlands ARH Regional Medical Center, Prestonsburg, Kentucky
4

Somerset Core Site
Lake Cumberland Regional Hospital, Somerset, Kentucky
South Central Kentucky Area Health Educations Center Core Site
Graves Gilbert Clinic, Bowling Green, Kentucky
TriStar Greenview Regional Hospital, Bowling Green, Kentucky
Southern Kentucky Area Health Education Center Core Site
Russell County Hospital, Russell Springs, Kentucky
Baptist Health, Corbin, Kentucky
Baptist Health, Richmond, Kentucky
Whitesburg Core Site
Harlan ARH, Harlan, Kentucky
Whitesburg ARH, Whitesburg, Kentucky
Other Regional Core Sites
Indiana Core Site
King’s Daughters Health, Madison, Indiana
Reid Health, Richmond, Indiana
Michigan Core Site
McLaren Bay Region Medical Center, Bay City Michigan
McLaren Oakland Hospital, Pontiac, Michigan
Mississippi Core Site
Rush Foundation Hospital, Meridian, Mississippi
Regency Hospital Company, Meridian, Mississippi
Ohio Core Sites
Adena Medical Center, Chillicothe, Ohio
Mercy Health – St. Rita’s Medical Center, Lima, Ohio
Virginia Core Sites
Norton Community Hospital, Norton, Virginia
Lonesome Pine Hospital, Big Stone Gap, Virginia
Purchase Area Health Education Center Core Site
Crittenden Health Systems, Marion, Kentucky
Jackson Purchase Medical Center, Mayfield, Kentucky
Livingston Hospital and Healthcare Services, Salem, Kentucky
Lourdes Hospital, Paducah, Kentucky
Marshall County Hospital, Benton, Kentucky
Murray-Calloway County Hospital, Murray, Kentucky
Baptist Health, Paducah, Kentucky
5

CLASS OF 2023 CLINICAL ROTATION PROGRAM
KYCOM ABSOLUTES
This manual is required reading for all third and fourth-year students. Submittal of the
attestation form, located in the Request Forms, Case Logs and Evaluation Forms
section of this manual, is required before entry to clinical rotations. All items under
Student Eligibility for Clinical Rotations must be completed before entry to clinical
rotations.
KYCOM requires all students to use and check the UPIKE email DAILY for
communication with the school and to maintain the UPIKE inbox at a level whereas it can
accept correspondence.
All students are expected, unless excused by their attending physician, to attend
morning reports, M&M rounds, and all site scheduled didactics and workshops. These
didactic programs are part of your rotation and do not meet your requirement for
Clinical Competency #4. Attendance at Educational Programs.
The Comprehensive Osteopathic Medical Self-Assessment Examination (COMSAE)
must be taken, and approval received, before any student may sit for either Level 1 or
Level 2 CE of the Comprehensive Osteopathic Medical Licensing Examination
(COMLEX-USA). See COMLEX-USA Policy.
The COMLEX-USA Level 2 PE may not be taken before completion of the clinical
capstone course. See The Clinical Competency Program.
The COMLEX-USA Level 2 CE may not be taken before successful completion of all
third-year core rotations. See The Clinical Competency Program.
All log items must be completed and submitted electronically within nine (9) calendar days
from the last day of the rotation, or will be incomplete. If the completed logs are received
after nine, but within fourteen (14) days, the grade may be raised to a maximum of 70%
at the discretion of the Associate Dean for Clinical Affairs. After fourteen (14) days, if
the completed logs have not been received, a grade of 69% will be entered on the
transcript, resulting in a failing grade for this rotation. The last date that activity is
logged into E*Value will be considered the last date of the rotation and late logs will
be calculated using that date, regardless of any “scheduled date’ listed on VSLO
or the Rotation Request Form.
Viewing of two educational videos per core rotation block is required, even when off
rotation for board study. (OPC V and OPV VI courses for third year students) These are
pass/fail courses during the Fall and Spring semesters of third year. A minimum
of 70% must be obtained on the total quizzes for each semester in order to pass the
course. If a failure is received for the Fall semester, the course will be remediated
during Winter Break. If a failure is received for the Spring semester, the course will
be remediated during the Capstone Course and you will be referred to the Promotion and
Matriculation Committee.
6
Viewing of two educational videos, is required per fourth year selective clinical
rotation a maximum of two video receipts will be accepted (for credit) per rotation
month, and submitted as part of rotation log items. (See THE CLINICAL
COMPETENCY PROGRAM for further explanation.) During your third year, you are
required to participate in one Aquifer and/or iHuman case each block. Attendance at
one Journal Club meeting is required during your fourth year. Journal Club dates are
assigned. Substitution of assigned dates is the responsibility of the student. Changes
to the schedule must be reported to the Associate Dean for Clinical Affairs at least 24
hours before the Journal Club meeting. See Clinical Journal Club.
KYCOM maintains a “No Tolerance Policy” for violations of the dress code. See,
Student Responsibilities - Dress.
Denial for Conference and Rotation requests will be issued for submittals beyond the
required timeline. See, Attendance at Professional Conferences and, Scheduling of
Elective/Selective Clinical Rotations.
Students on rotation during the “Make-up” block in April of 4
th
year will not receive
a diploma at the graduation ceremony. The diploma will be awarded to the student
once all rotation log documents are submitted and reviewed and all graduation
requirements listed, in Graduation Requirements, have been satisfied.
All times indicated are Eastern Time.
7
Patient Care (Amended 10/8/2021)
University of Pikeville, Kentucky College of Osteopathic Medicine (KYCOM) students may only
be involved in patient care activities as part of an approved activity and under the supervision of an
assigned clinical faculty member/preceptor. KYCOM students are not legally or ethically
permitted to practice medicine or assume responsibility for patients. The student’s assigned
clinical site will determine the degree of student involvement in patient care activities and the
supervising clinical faculty/preceptor is ultimately responsible for the patient care. Students are
required to comply with all general and specific rules and medical ethics established by the clinical
rotation site at which they are placed.
Students are not permitted to provide any type of medical procedures, without the direct
supervision of an assigned clinical faculty member/preceptor. If a student receives approval, they
may take histories, perform physical examinations, and enter findings into the patient’s chart.
Students may not perform any medical treatment, procedures, or invasive examinations without
appropriate supervision of the faculty member/preceptor. Students are not permitted to write or
enter patient care orders independently and/or issue prescriptions, any such orders/prescriptions
must be reviewed and approved by the clinical faculty member/preceptor.
KYCOM students should accurately represent themselves as an “osteopathic medical student” or
“student doctor.” If any entries are made into patient medical records, student signatures should be
followed by “OMS-III” or “OMS-IV” written legibly or entered electronically. Students are not
permitted to introduce themselves as “Doctor” at any time, regardless of any previous degrees they
may hold. Students should never provide care beyond what is appropriate for their level of
training, even under supervision.
INTRODUCTION
The mission of University of Pikeville Kentucky College of Osteopathic Medicine (KYCOM)
includes preparation of our graduates for competency in the world of primary care medicine. A
successful KYCOM graduate will, after completion of the program, demonstrate sufficient
knowledge, skill sets, experience, values, and behaviors that meet established professional
standards, supported by the best available medical evidence, that are in the best interest of the well-
being and health of the patient. The maturation process from clinical years three to four, and
ultimately successful graduation is the shared responsibility of the individual student, KYCOM
and the host hospitals and physicians that provide the clinical experiences.
All hospital sites are required to maintain affiliation agreements with KYCOM, are credentialed
by the Joint Commission (JCAHO) or the Healthcare Facilities Accreditation Program (HFAP),
and are duly licensed within their jurisdiction. All adjunct clinical faculty are required to re-
credential with KYCOM every three years, are actively licensed in their respective jurisdictions,
maintain specialty board certification, and carry regionally acceptable malpractice insurance. All
clinical education sites:
1. Provide and maintain an environment conducive to the education and training of
osteopathic medical students.
2. Assist the osteopathic medical students in obtaining experience in patient care by
allowing students to share responsibility for patient care with qualified staff physicians.
3. Provide and maintain an environment which encourages critical dialogue between the
medical staff physicians and students through clinical rotations, rounds and conferences.
Professional Student Behavior as defined by KYCOM includes:
1. Performance of medically ethical behavior, i.e. all actions are in the best interest of
patients.
2. Cognizance of the concept of social accountability to preceptor, host site and/or peers.
3. Cognizance of the concept of professional duty to supervising faculty and their patients.
During the 3
rd
and 4
th
years, a total of nineteen four-week rotation blocks have been provided to
complete 76 weeks of clinical requirements, which include:
1. 36 weeks of required Core rotations (9 blocks)
2. 16 weeks of required Selective rotations (4 blocks)
3. 24 weeks of Elective rotations (6 blocks)
4. Up to 8 weeks for COMLEX preparation (2 blocks) if needed.
Completing additional rotations, either for credit or not for credit, will not be approved and
could result in disciplinary action.
The schedule includes two weeks in the 3
rd
year devoted to clinical skills evaluation and a
mandatory class meeting, and four weeks of winter holiday breaks (2 weeks per year, per KYCOM
calendar).
The Promotion and Matriculation Committee regularly reviews the academic progress of
students. Upon completion of each course, students receive notification of their grades and grade
reports are reviewed by the P & M Committee.
8
Core Rotation Requirements
Commission on Osteopathic College Accreditation (COCA), requires that students, during third
year, must have one in-patient rotation, one out-patient rotation, and one rotation having
interaction with residents. KYCOM will work with every student to make sure they satisfy these
requirements.
ELECTIVE TIME
Elective rotations are intended to fulfill the interests of the osteopathic medical student and
provide residency audition opportunities. Approval from the Associate Dean for Clinical
Affairs is required; however, both the location and the preceptor are chosen by the student.
Twenty-four (24) weeks of elective time are required during the clinical years. Elective time
must be utilized and logs must be submitted for audition/elective rotations.
Elective time may be utilized as follows:
1. Can be in an in-patient or out-patient setting, and chosen from any medical or surgical
subspecialty; however, must be served for a minimum of two weeks. See Course
Descriptions in Selective/Elective section of manual for suggested endeavors.
2. Clinical Research – maximum of eight (8) weeks – See OST 897 – Clinical Research
3. Electives may be completed in two-week or four-week blocks. (No more than two, four-
week time periods can be divided into four, two-week rotations per year.)
COMLEX BOARD REVIEW GUIDELINES
Description
The third-year osteopathic medical student may elect to utilize up to eight weeks to prepare for
COMLEX. The student is expected to perform independently and adhere to established study
protocols, and subject content. An approved form of the COMSAE is part of the study plan, and
is taken at the determined point within the scheduled study program and results submitted for
KYCOM review, BEFORE COMLEX IS TAKEN.
Location
The study program may be offered commercially, or completed privately within a private
residence, a library or within a study carrel. The program site may be remote from KYCOM or
on campus.
Length of rotation
two 4-week blocks
two 4-week blocks
one 4-week block
one 4-week block
one 4-week block
one 4-week block
Rotation
Family Medicine (Required and assigned)
General Internal Medicine (Required and assigned) General
Surgery (Required and assigned)
Osteopathic Principles and Practice (Required and assigned)
Pediatrics - Neonate (Required and assigned)
Psychiatry (Required and assigned)
Women’s Health (Required and assigned)
one 4-week block
9

INDEPENDENT STUDY – OST 799 AND OST 899
Course Description: This is an independent study course in which students will be provided a
detailed individualized study plan to prepare them for their COMLEX-USA Level 1, Level 2 CE
or Level 2 PE examination. The study plan will include required assessments to provide
benchmarks for preparedness, as well as usage of specified question banks and study resources.
This course will be four weeks in duration, but can be continued in four week increments as
approved by the course director as long as the student is preparing for their COMLEX-USA retake
examination. In addition, if the student’s board examination retake is not passed, this course may
be repeated if approved by the course director and the Promotions and Matriculation Committee
Course Goal: The primary goal of this course is to provide the student additional time and
structure to prepare for the COMLEX-USA examination.
Course Format: Students will have an individual study plan to follow with built-in assessments
and question bank goals to serve as benchmarks for preparedness to retake their COMLEX-USA
board examination.
Grades: Grades will be reported as Pass or Fail. Students following the assigned study plan and
taking the COMLEX-USA examination on their assigned date will Pass. Students who do not
follow the assigned study plan or who do not take their COMLEX on the assigned date will fail
this course. Failure of this course can be grounds for dismissal from KYCOM.
SELECTIVE ROTATIONS
Pre-Requisite Courses: General Internal Medicine I, Family Medicine I, General Surgery I and
Pediatrics are recommended for completion prior to the selective rotation experience. See
individual “OST” course descriptions for specific pre-requisite requirements.
Selective rotations are intended to transition the osteopathic medical student from active learner
to active medical decision maker and care planner. Four (4) selectives are required for a total of
sixteen (16) weeks within the two-year clinical schedule. Approval from the Associate Dean for
Clinical Affairs is required, however; both the location and the preceptor are chosen by the
student. See course descriptions for selectives in Medicine, Surgery, Rural Health and
Emergency Medicine for specific course details.
The rotation can be arranged as one four-week block or two, two-week blocks. A total of four
weeks must be devoted to each of the SELECTIVE categories, i.e. Medicine, Surgery, Rural
Health, and Emergency Medicine.
No more than two, four-week time periods (selective or elective) can be divided into four
two-week rotations per year.
Selective Rotation Requirements
Length of rotation
one 4-week block
one 4-week block
one 4-week block
Rotation
Emergency Medicine
Medicine subspecialty
Rural Medicine
Surgical subspecialty
one 4-week block
10
COMLEX-USA Policy
Graduation requirements from KYCOM include successful completion of COMLEX-USA Level
1, Level 2 CE, and Level 2 PE. KYCOM requires Level 1 to be taken upon successful
completion of years one and two of osteopathic medical education. KYCOM requires Level 2
CE to be taken after successful completion of Level 1 and years one, two, and three of
osteopathic medical education, which includes successful completion of all core rotations. The
Capstone course must be completed before taking COMLEX Level 2 PE.
KYCOM will use student performance on their third year Comprehensive Osteopathic Medical
Achievement Tests (COMATs), performance on the COMSAE Phase 2, and performance on
KYCOM-purchased question banks and assessment tests, as indicators of readiness to pass the
COMLEX Level 2 CE exam. Students may be advised to take additional COMSAEs or practice
exams.
KYCOM will use student performance in their clinical Capstone course as an indicator of
readiness for the COMLEX Level 2 PE. Students will be required to remediate their Capstone
course if their performance is unsatisfactory.
All students are limited to a maximum of four attempts to pass each required COMLEX-USA
examination in order to meet graduation requirements. Failure of four attempts on any
COMLEX-USA examination will result in dismissal from KYCOM.
Level 1. Before entry into the third year of osteopathic medical education, all students must sit
for COMLEX-USA Level 1 on a date agreed upon by the Associate Dean for Academic
Affairs. Delays from this schedule will prevent the start of the third year of study and require
pre-approval from the P and M Committee. When the Level 1 exam is taken, the student will be
permitted to enter third year clinical rotations at the beginning of the next scheduled rotation
period.
Failure of the Level 1 examination will result in removal from third year clinical rotations at the
end of the current rotation. A plan of study will be developed by the student and approved by the
P and M Committee to assist students to prepare for a retake of the examination.
The student will be enrolled in course 799 and remain off rotations until the Level 1 examination
has been retaken. Failure to retake this examination in the period of time allotted by the P and M
Committee will result in a meeting with this Committee to determine disciplinary
consequences. Following the initial retake of the examination, the student will be permitted to
return to clinical rotations while awaiting results. However, after two or more failures, the
student will be removed from rotations until a passing score is received and a return to rotations
is approved by the P and M Committee.
The P and M Committee will determine the appropriate length of time to be devoted to studying
for a retake of the examination. Under no circumstances will a period of time greater than one
semester be granted to study for a retake of the examination. Failure to follow the study plan or
take the examination in the period of time allotted by the P and M Committee will result in a
disciplinary hearing.
11
Failure to achieve a passing score by December 31st of the third year will result in removal from
clinical rotations and review by the P and M Committee. The student will be allowed to return to
clinical rotations only after a passing score has been received by KYCOM. The Associate Dean
for Clinical Affairs will determine student placement in accordance with scheduling and
curricular requirements.
Level 2 CE and Level 2 PE.
KYCOM requires the Level 2 CE examinations be taken after
successful completion of Level 1 and years one, two, and three of osteopathic medical education,
which includes successful completion of all core rotations. COMLEX Level 2 PE may be taken
any time after successful completion of the Clinical Capstone Course. Upon successful
completion of COMLEX-USA Level 1, NBOME will notify students of their eligibility to
schedule their COMLEX-USA Level 2 examinations. All students are required to take both the
Level 2 CE and Level 2 PE examinations between the start of the fourth year and December 1st
of the fourth year of study. The student has the option to take Level 2 CE or Level 2 PE in any
order. Failure to take the exams prior to December 1st of the fourth year will result in a referral
to the KYCOM Promotion and Matriculation Committee for consideration of disciplinary
action.
Failure of the Level 2 CE examination will result in the removal of the student from clinical
rotations and being enrolled in course 899. A plan of study will be developed by the student and
approved by the P and M Committee to assist students to prepare for a retake of this
examination. Following the first retake of this examination, the student will be permitted to
return to clinical rotations while awaiting results. However, after two or more failures, the
student will be removed from rotations until a passing score is received and a return to rotations
is approved by the P and M Committee.
The P and M Committee will determine the appropriate length of time to be devoted to studying
for a retake of the examination. Under no circumstances will a period of time greater than one
semester be granted to study for a retake of the examination. Failure to take the examination in
the period of time allotted by the P and M Committee will result in a disciplinary hearing.
Failure of the Level 2 PE will require a mandatory remediation course be completed prior to a
retake of the examination. If a student fails the exam two or more times, this may result in the
removal of the student from clinical rotations pending review by the Associate Dean for Clinical
Affairs and a study plan to be developed by the P and M Committee. This plan may include (a)
the student being counseled on how to prepare for the examination or (b) being removed from
clinical rotations, and (c) matriculation into a review course at student expense.
Failure to successfully complete the COMLEX-USA graduation requirements within two years
from the start of the student’s fourth year of study will result in dismissal from KYCOM.
12
SAMPLE CALENDAR
Start Date End Date Third Year Start Date End Date Fourth Year
7/26/21 8/20/21
Core #1
6/27/22 7/22/22
Board Study,
Selective or Elective
8/23/21 9/17/21 Core #2 7/25/22 8/19/22 Selective or Elective
9/20/21 10/15/21 Core #3 8/22/22 9/16/22 Selective or Elective
10/18/21 11/12/21 Core #4 9/19/22 10/14/22 Selective or Elective
11/15/21 12/10/21 Core #5 10/17/22 11/11/22 Selective or Elective
12/13/21 12/24/21
Winter Break
11/14/22
12/9/22
Selective or Elective
12/27/21 1/22/22 Core #6 12/12/22 12/23/22
Winter Break
1/24/22 2/18/22 Core #7 12/26/22 1/20/23 Selective or Elective
2/21/22 3/18/22 Core #8 1/23/23 2/17/23 Selective or Elective
3/21/22 4/15/22 Core #9 2/20/23 3/17/23 Selective or Elective
4/18/22 5/13/22
Board Study,
Selective or Elective
3/20/23 4/14/23 Selective or Elective
5/16/22 5/27/22
Tentative Clinical Capstone Course
5/6/23 Graduation
5/30/22 6/24/22 Board Study
OBJECTIVES
The clinical years at KYCOM are a transition from the pre-clinical experience to the world of
integrative, experience based medicine. In twenty-one months, KYCOM aims to see the student
successfully achieve comprehension and skills, at the supervised level, of the “Seven Core
Competencies” as outlined by the National Board of Osteopathic Medical Examiners, and
evaluated by both KYCOMs internal evaluative tools and the successful completion of COMLEX
Level 2-CE and 2-PE before graduation.
Educational and Performance Goals include:
1. Comprehension of the osteopathic philosophy, recognition of the need for its application,
and demonstration of clinical OMT skills.
2. Comprehension of the applicability of biomedical, clinical, epidemiologic,
biomechanical, and the social/behavioral sciences to clinical situations, and
demonstration of application to patient-centered care.
3. Demonstration of patient-centered care. To include:
a. Effective data gathering
b. Development of effective physician-patient relationships
c. Recognition of age-related preventive health issues
d. Sensitivity to cultural influences
e. Development of treatment plans that are both evidence based and patient specific.
f. Development of treatment plans with both scientific basis and integration with
osteopathic philosophy.
4. Demonstration of good communication and interpersonal skills that facilitate quality
physician-patient, physician-family and physician-health professional relationships.
5. Demonstration of professional behavior. To include:
13
a. Performance of medically ethical behavior
b. Cognizance of the concept of social accountability
c. Cognizance of the concept of professional duty.
6. Ability to develop treatment plans that demonstrate the interpretation of epidemiologic
information, and its applicability to patient-specific issues.
7. Comprehension of the concepts of Systems-Based Practices (Can effectively identify and
integrate health care resources to provide complete patient centered care.)
Required Encounters:
Over the course of the third and fourth year clinical experience at KYCOM, all osteopathic
medical students must encounter and assess the following clinical conditions:
1. Ischemic heart disease/coronary artery disease
2. Cerebrovascular accident
3. Liver disease
4. Renal disease
5. Substance abuse
6. Mental health disorders such as anxiety/depression
7. Neuromuscular trauma
8. Hypertension
9. Diabetes Mellitus
10. Pregnancy
11. Otitis Media
12. Hypercholesterolemia
13. Abdominal pain
14. Asthma
15. Chronic Obstructive Pulmonary Disorder (COPD)
16. Well-child care
STUDENT ELIGIBILITY FOR CLINICAL ROTATIONS
1. DRUG SCREEN POLICY
KYCOM requires a urine screen for drugs immediately after matriculation with KYCOM, prior
to the beginning of third and fourth year clinical clerkships. Students are responsible for the
expense involved with this evaluation. Positive findings will be reviewed by the Assistant Dean
of Student Affairs for Graduate and Health Professions and/or the Associate Dean for Clinical
Affairs and be referred to the P&M Committee. Further evaluation by external professional
consultants may be required. A positive test result may become grounds for dismissal.
Drug Testing on Demand –
Any student may be required to submit to drug and/or alcohol
testing at any time based on reasonable suspicion.
2. CRIMINAL BACKGROUND CHECK
KYCOM requires criminal background checks for all students prior to matriculating to KYCOM
and prior to the beginning of third year clinical rotations. Students will be responsible for the
14

expenses involved with this evaluation. The mechanism for evaluation will be determined by the
Assistant Dean of Student Affairs for Graduate and Health Professions and/or the Associate
Dean for Clinical Affairs. Infractions may be referred to the Promotion and Matriculation
Committee.
Mandatory Self-Reporting for Criminal Behavior
All accepted and currently enrolled medical students are required to promptly (within 10
calendar days) report any criminal charges filed against them to the Assistant Dean for
Professional Student Affairs. Criminal behavior includes any felony and misdemeanor
violations of the law, but excludes minor traffic violations, such as parking tickets. Any
charges that were previously disclosed on the AACOMAS application need not be reported
again. Student violations of the law will be reviewed by the Assistant Dean for Professional
Student Affairs in the context of future implications for licensure, threat to patient safety, and
the ability to be an appropriate member of the osteopathic medical profession. Depending on
the nature and severity of the criminal offense, student suspension or dismissal is possible.
3. IMMUNIZATIONS
KYCOM, in conjunction with requirements of all hospitals accredited by the Joint Commission
on Accreditation of Healthcare (JCAHO) and/or Healthcare Facilities Accreditation Program
(HFAP), have required the following immunizations:
a. TB testing yearly
i. Chest radiography, every three years, if TB test is considered positive
ii. If previously received the BCG vaccination, the Interferon Gold or T-Spot blood
test is required
b. Tdap immunization once during adulthood, followed by the Tetanus toxoid
immunization, every ten years
c. Measles, Mumps, Rubella, and Varicella immunity, established by documented
immunizations
d. Hepatitis B immunity, established by documented immunizations and antibody titer
e. Influenza immunization yearly
f. COVID-19 immunizations may be required by individual facilities/sites.
15
UPIKE/KYCOM does not currently require the COVID-19 vaccination; however, many of
KYCOM’s clinical partners do require proof of immunization to train at their facility. Students are
guests in these clinical facilities/sites and KYCOM has no control over the policies they set in
place. A clinical partner may provide a pathway to request a reasonable accommodation based on a
medical necessity or a sincerely held religious belief.
ALL TB tests must be current by June 1 of each year of clinical rotations. A current, updated
documentation of TB evaluation must be uploaded into E*Value prior to that date. Failure to
provide a current TB evaluation will prevent the student from participating in any clinical
activities for the following year, which will result in delay and/or failure to achieve graduation.
ALL Influenza vaccinations must be current by October 1 of each year of clinical rotations. A
current, updated documentation of Influenza vaccine must be uploaded into E*Value prior to that
date. Failure to provide proof of current vaccine will prevent the student from participating in any
clinical activities, which will result in delay and/or failure to achieve graduation.

It is policy that all Measles, Mumps, Rubella, Varicella and Hepatitis B immunity
documentation will be completed on June 1 of the first year of school. This documentation
must be uploaded into E*Value. Failure to provide a completed documentation will prevent
the student from participating in any clinical activites, which will result in delay and/or failure
to achieve graduation.
Immunizations must be administered within the CDC recommended time frame, or you could
be required to repeat the series.
Documentation of an updated tetanus vaccination is required prior to matriculation to KYCOM.
This must be on file in E*Value.
4. ACADEMICS
a. All pre-clinical courses will have been completed before entry into the 3
rd
clinical year
rotation schedule.
b. COMLEX Level 1 must be taken before entry into the 3
rd
clinical year rotation schedule.
5. ATTESTATION FORM
Submittal of the signed and dated form which attests that the clinical rotations manual has both
been completely read and understood is a mandatory requirement before entry into the third year
of osteopathic medical study. This must be uploaded to eValue prior to starting clinical activities.
STUDENT RESPONSIBILITIES
KYCOM maintains a “NO TOLERANCE” policy for diversions from the mandatory guidelines
below:
1. REPORT FOR ROTATION
Each rotation begins on the first Monday of each block and ends on the last Friday of the block.
It is the student’s responsibility to contact the clinical preceptor one week before the
commencement of the rotation to determine a “first day meeting place and time.” Failure to contact
the preceptor and/or failure to find the preceptor can lead to failure of the rotation. It is the
responsibility of each student to be present on the commencement of each rotation. One week
prior to the start date of each rotation, it is the responsibility of the student to send contact
information to the Director of Clinical Rotations for scheduling in E*Value and to ensure that a
COMAT exam is scheduled.
In the event of an unavoidable tardiness to the rotation, it is the responsibility of the student to
notify the Supervising Physician and the Office of the Associate Dean for Clinical Affairs at
KYCOM. If an orientation is required at a clinical rotation site, it is imperative that the student
participate in that orientation and follow the protocols established by that rotation.
2. ATTENDANCE
Prompt student attendance is expected for a minimum of 20 days each four-week rotation period
and 10 days each two-week rotation period. The expectation is that students work Monday through
Friday with weekends off. However, the work day will vary by rotation. If the preceptor works
weekends, the student is expected to work weekends also. Attendance is mandatory for all clinical
rotations. On occasion, a student may need to miss days from a clinical rotation. A maximum of
three (3) days for excused absence is permitted, only if prior approval is given by the KYCOM
Clinical Affairs Department, and must be recorded on student logs for the rotation. Absence in
excess of the 3-day standard will result in an “incomplete” for the rotation, until such time that the
16

activity requirement is satisfied. If a pattern of missing three days for each rotation is noted
by KYCOM staff, it will be referred to the Promotions and Matriculation Committee.
Unexcused absence constitutes referral to the Promotions and Matriculation Committee, and may
result in failure of the clinical rotation. An example of an unexcused absence includes, but is
not limited to, taking a study day for the COMAT exam.
3. SUBMISSION OF STUDENT CASE LOGS AND ROTATION EVALUATION
All students are required to submit a complete electronic case log for each clinical rotation within
nine (9) calendar days of the last day of the rotation. The Case Log consists of the student’s daily
activities. e.g. all patient contact, all procedures performed, all readings (assigned and unassigned),
conferences attended, etc. and is submitted within nine (9) calendar days of the last rotation day.
Logs not submitted within nine (9) calendar days are considered late and an incomplete grade will
be entered for this rotation and may result in a referral to the Promotions & Matriculation
Committee. If the completed logs are received after nine (9) but within fourteen (14) days, the
incomplete grade may be raised to a maximum of 70% at the discretion of the Associate Dean
for Clinical Affairs. After fourteen (14) days, if the completed logs have not been received, a
grade of 69% will be entered on the transcript for this rotation.
a. All students are required to include their level of participation in each activity. Level of
participation – (1) Observed, (2) Assisted, (3) Managed Under Supervision.
b. The student is required to evaluate each rotation electronically. This evaluation will
reflect the student’s attitude and observations regarding the quality of training received on
each rotation.
c. In the event of late submittal of log materials (within fourteen (14) days), if acceptable to
the Associate Dean for Clinical Affairs, the rotation grade will be converted from an
incomplete to an absolute maximum score of 70%. If the late log materials are not
received within fourteen (14) days, students will receive a 69% (Failure) for the rotation.
d. Clinical rotation failures are reviewed by the P and M Committee. Failure of more than
two clinical rotations is grounds for dismissal.
4. MEDICAL INSURANCE
Students must maintain personal health insurance throughout their enrollment and present
documentation of health insurance coverage as instructed by the KYCOM Office of
Professional Affairs prior to the start of each academic year. KYCOM students are responsible
for the costs of their health insurance.
5. HOUSING
All housing needs while the students have relocated to the individual rotation sites are at the
student’s expense. Neither KYCOM nor the individual rotation site is responsible for student
housing.
6. PROFESSIONALISM
As a representative of both KYCOM and the osteopathic profession, it is the student’s
responsibility to maintain professional deportment at all times.
17
a. DRESS
KYCOM students are expected to dress professionally at all times and to be attentive to
personal hygiene and cleanliness. It is the right of patients, peers and healthcare staff to
expect a safe, non-offensive, non-infective, and non-allergenic environment. Personal
appearance and hygiene reflect concern and respect for both staff and patient safety. It
contributes to the delivery of quality health care, and sends a message to the public that
the healthcare facility maintains a positive, respectful and safe environment. Unclean
and unkempt individuals provoke discomfort, and create a barrier to healthcare access.
KYCOM maintains a “NO TOLERANCE” policy for diversions from the mandatory
guidelines below:
1. At all times a student must be clearly identified as a KYCOM student.
2. Short white lab coats with KYCOM identification are expected to be worn unless
specifically instructed otherwise by the healthcare facility or preceptor physician.
3. Scrub suits are to be worn in the operating room, procedure rooms, during call
hours, and at the discretion of individual preceptor physician and/or healthcare
facility.
4. Clothing, at all times, must be neat, clean and free from offensive odors. Clothing
must be professional, consistent with the standards for a professional
environment, and not attract undue attention or serve as a distraction to others.
Clothing that contains unprofessional or offensive writing or caricatures may not
be worn. Students should dress in a non-provocative manner that demonstrates
respect for patients, fellow students, and staff. It must also be appropriate to the
type of work being performed and take into account the potential expectations of
patients, staff or fellow students.
5. Open-toed and casual shoes, such as sandals and flip-flops are not considered
professional attire.
6. Jewelry, neckwear, scarves and accessories can be worn; however, must be
removed if either preceptor or healthcare facility consider them to interfere with
duty, or a potential for infection and possible harm to patients, staff or self exists.
7. Tattoos and body art can often be perceived as affronts or threats to religion and
family. Tattoos and body art should be covered to prevent potential for offensive
reactions from patients, peers or staff.
8. KYCOM students must be physically clean, well groomed, and take steps to
prevent and/or address problems of offensive body odor.
a. Avoid excessive use of fragrances – scented chemicals pose a threat for
allergic and/or adverse reactions by patients, peers and healthcare staff.
b. Hairstyle and length (including mustaches and beards) must be clean, neat
and controlled. Hair should not interfere with duties or pose a threat to
infection for patient, peer or healthcare staff.
b. SEXUAL HARASSMENT
Any incident of suspected sexual harassment must be reported immediately to the
Supervising Physician, Associate Dean for Clinical Affairs and the Assistant Dean of
18
Student Affairs for Graduate and Health Professions. Any student involved in sexual
harassment will be referred to the Assistant Dean of Student Affairs for Graduate
and Health Professions and the University Title IX Coordinator for further action.
c. STUDENT/PATIENT/PHYSICIAN RELATIONSHIPS
The relationship between an osteopathic medical student and a patient must always be kept
on a professional basis. A student shall not date or become intimately involved with a
patient due to the ethical and legal considerations. Conduct in such an unprofessional
manner shall be considered improper behavior and will be grounds for disciplinary action,
including dismissal from KYCOM. KYCOM directs that no member of its faculty
establish or maintain a therapeutic relationship with any KYCOM student. A therapeutic
relationship exists when a physician/patient relationship is established between a
KYCOM employee and a KYCOM student. In the event a therapeutic relationship is
established or in any way is maintained by and between a KYCOM employee and a
KYCOM student, the employee must identify and recuse themselves from any academic
assessment or promotion of the student with whom the employee has the therapeutic
relationship. KYCOM also requires that all clinical preceptors complete an attestation
that they do not maintain a physician/patient relationship with the student being evaluated.
d. KYCOM PHARMACEUTICAL AND INDUSTRY REPRESENTATIVE POLICY
Introduction
Kentucky College of Osteopathic Medicine (KYCOM) operates as a not-for-profit
osteopathic medical educational institution engaged in educating osteopathic medical
students and advancing osteopathic medical education. KYCOM has been granted
accreditation by the American Osteopathic Association’s Commission on Osteopathic
College Accreditation. Our mission includes preparation of our graduates for competency
in the world of primary care medicine. A successful KYCOM graduate will, after
completion of the educational program, demonstrate sufficient knowledge, skill sets,
experience, values, and behaviors that meet established professional standards, supported
by the best available medical evidence, that are in the best interest of the well-being and
health of the patient.
Code of Ethics
KYCOM is guided by Section 17 of the American Osteopathic Association Code of
Ethics
1
which specifically relates to the interaction of physicians with pharmaceutical
companies, and is clarified as follows:
1. The physicians’ responsibility is to provide appropriate care to patients. This
includes determining the best pharmaceuticals to treat their condition. This
requires that physicians educate themselves as to the available alternatives and
their appropriateness so they can determine the most appropriate treatment for an
individual patient. Appropriate sources of information may include journal
articles, continuing medical education programs, and interactions with
pharmaceutical representatives.
2. It is ethical for osteopathic physicians to meet with pharmaceutical companies and
their representatives for the purpose of product education, such as, side effects,
clinical effectiveness and ongoing pharmaceutical research.
1
American Osteopathic Association Code of Ethics adopted July 2003, updated July 2016.
19
3. Pharmaceutical companies may offer gifts to physicians from time to
time. These gifts should be appropriate to patient care or the practice
of medicine. Gifts unrelated to patient care are generally inappropriate.
The use of a product or service based solely on the receipt of a gift
shall be deemed unethical.
4.
When a physician provides services to a pharmaceutical company, it is
appropriate to receive compensation. However, it is important that compensation
be in proportion to the services rendered. Compensation should not have the
substance or appearance of a relationship to the physician’s use of the employer’s
products in patient care.
Pharmaceutical Research and Manufacturers of America (PhRMA)
2
Guidelines from the PhRMA code, developed voluntarily by the pharmaceutical industry,
and adhered to by KYCOM include:
1. A conference or meeting is any activity, held at an appropriate location, where (a)
the gathering is primarily dedicated, in both time and effort, to promoting
objective scientific and educational activities and discourse, and (b) the main
incentive for bringing attendees together is to further their knowledge on the
topic(s) being presented.
2. Financial assistance for scholarships or other educational funds to permit medical
students, residents, fellows, and other healthcare professionals in training to
attend carefully selected educational conferences may be offered so long as the
selection of individuals who will receive the funds is made by the academic or
training institution. “Carefully selected educational conferences” are generally
defined as the major educational, scientific, or policy-making meetings of
national, regional, or specialty medical associations.
3. Any financial support provided by PhRMA certified companies, should be given
to the educational activity (CME) provider with the intent to reduce the overall
CME registration fee for all participants.
4. No grants, scholarships, subsidies, support, consulting contracts, or educational or
practice related items should be provided or offered to a healthcare professional in
exchange for prescribing products or for a commitment to continue prescribing
products. Nothing should be offered or provided in a manner or on conditions that
would interfere with the independence of a healthcare professional’s prescribing
practices.
5. It is appropriate for companies, where permitted by law, to offer items designed
primarily for the education of patients or healthcare professionals if the items are
not of substantial value ($100.00 or less) and do not have value to healthcare
professionals outside of his or her professional responsibilities.
6. Any healthcare professional that serves as either part of a program planning
committee or as a program speaker, and who also serves as a company speaker
and/or consultant, is required to disclose the relationship to all.
Adjunct Clinical Faculty and Clinical Rotation Sites
Pharmaceutical and industry representatives (PI reps) are not received on the KYCOM
campus, and maintain no direct exposure to the osteopathic medical students educated
there. PI rep exposure to students, is limited to “off-campus” health care facilities which
2
Code on Pharmaceutical Company Interactions with Healthcare Professionals, originally adopted in July 2002, and
amended in January 2009.
20

include physicians’ offices, hospital clinics and hospitals, and “pre-approved” attendance
at graduate medical education programs. KYCOM students are professionally bound by
the applicable sections of the AOA Code of Ethics.
Summary
The pharmaceutical and pharmaceutical research industry is a recognized member of the
healthcare team that is voluntarily bound by a set of guidelines. KYCOM supports the
guidelines, and will follow them within the definitions of the school’s mission, and those
professional duties as outlined within publications of the American Osteopathic
Association and all published school catalogues and/or manuals.
e. ISSUES DEEMED REPORTABLE
1. It is the student’s responsibility to notify the preceptor and/or supervisory house
staff of any critical issue(s) that affect the student doctor and/or his/her patient(s)
during the rotation.
2. If necessary, it is the student’s responsibility to notify the regional coordinator
and/or KYCOM of any critical issue(s) that affect him/her during the rotation.
f. FINANCIAL COMPENSATION
A KYCOM osteopathic medical student engaged in a clinical rotation within the hospital,
office or any patient care setting is there as both an observer and registered student. A
student is neither an employee or entitled to any financial compensation or means of
compensatory reward. Any student that enters a financial and/or compensatory relationship
within the rotation site has violated the professional agreements between KYCOM and the
core site.
g. MOBILE TELEPHONES AND HANDHELD DEVICES
KYCOM students are welcomed guests at clinical rotation sites. They are given the
courtesy to participate as a member of the staff; however, as guests, should be mindful
that mechanical sounds, attention to electronic messages and use of keyboards within the
confines of examination rooms, operating rooms, procedure rooms and at bedside can
both be perceived (by patients and staff) as a lack of interest, and potentially distract
preceptor physicians and healthcare staff from the delivery of safe healthcare. The
following guidelines for the use of mobile devices are mandated by KYCOM:
1. Handheld devices are not to be used to take photographs of patients, patient’s
records, or to store patient’s confidential information.
2. No handheld device is to be carried into operating or procedure rooms.
3. Upon entry into a hospital or outpatient facility, all ringers are to be set for
“QUIET” or “VIBRATE”, and alarms disabled.
4. Ringers and alarms for handheld devices must be disabled or set to “QUIET” or
“VIBRATE” at all conferences.
5. Handheld devices may be used on patient rounds, and within patient rooms ONLY
if permission is obtained from the preceptor physician and the patient.
6. Handheld devices may be used at nurses’ stations, the intensive care unit(s), and
within the emergency department, with preceptor physician and nursing approval
ONLY.
21
7. Handheld devices may be used within the confines of on-call rooms and hospital
cafeterias.
h. SOCIAL MEDIA EXPECTATIONS
KYCOM students are expected to adhere to standards of professionalism and abide by
applicable laws, policies, and rules that govern privacy and the dissemination of protected
information (e.g.,HIPAA). When using social media and other internet sites that involve
postings, comments, and images, students are expected to refrain from posting protected
information, disparaging others, or otherwise conducting themselves in a way that could
reasonable be perceived as unethical or unprofessional. Care should be taken when
expressing opinions. When expressing opinions, particularly opinions about medical or
health care issues, students should clearly state that their viewpoints are their own and do
not necessarily represent the views of KYCOM or others. Further, cyber stalking and
similarly inappropriate online activity can be viewed as forms of harassment. KYCOM
students should be mindful of the fact that social media and other internet sites are never
completely secure; what is posted can be seen by many, including prospective residency
programs and future employers.
Social media conduct that is contrary to this policy may result in disciplinary action (up to
and including dismissal from KYCOM and in some instances, legal action, if postings
violate applicable laws).
i. STUDENT IN “GOOD STANDING” DESIGNATION
KYCOM defines a student in “Good Standing” as an individual who has conformed to
established policy guidelines, passed, or is in the process of passing, all required
milestone examinations to date, satisfied all course requirements to date, and has
maintained all records and supporting documents, including immunizations as required
by the student handbook.
APPROVED ABSENCE AND LEAVE POLICIES
Absence of the attending physician or the student, from rotation for a period greater than one
day, requires the student to notify the office for Clinical Affairs, of the interruption of activity.
Only the Supervising Physician and the Associate Dean for Clinical Affairs may grant time off
during a prescribed clinical rotation. At the discretion of the Associate Dean for Clinical Affairs
either a reading assignment or alternate duty assignment will be made.
Reasons for approved absence may include illness, pre-approved conference attendance or
extended leave.
Any unexcused absence will be referred to the Promotions and Matriculation Committee with a
recommendation of failure for the clinical rotation.
The student is not permitted to leave the designated clinical rotation prior to the scheduled
departure date without prior approval of both the Associate Dean for Clinical Affairs and the
attending physician. Departures prior to the scheduled departure date without prior consent will
be considered an unauthorized absence and is subject to referral to the Promotions and
Matriculation Committee and potential failure of that clinical rotation.
22
a. PERSONAL ILLNESS
It is paramount that the well-being of the student is considered in any illness. If a student
is absent for more than one day during a rotation, the Office of the Associate Dean for
Clinical Affairs of KYCOM must be notified and the student must be seen by a physician
for documentation and for the well-being of the student. The student should not hesitate
whatsoever to report an illness as the welfare of the student and his/her patient contacts is
of prime importance.
b. TEMPORARY ABSENCE
A “short period of time” is defined as less than one day and may be requested to attend to
personal business (e.g. banking, child care, etc.). Permission of the supervising physician
and/or office of clinical rotations is required. No duration or frequency restrictions are
defined; however, it is intended that the student provide clear reason for the temporary
absence.
c. ATTENDANCE AT PROFESSIONAL CONFERENCES
Kentucky College of Osteopathic Medicine is committed to providing quality medical
education for our students. This experience includes excellence in academic and clinical
medicine, research and community service. In order to maximize this process, it is felt
that participation in professional meetings can greatly enhance a student’s professional
and personal growth. Attendance of AOA-sponsored national meetings, osteopathic
divisional society meetings and AOA/osteopathic specialty meetings will be provisionally
approved. All other meetings must have an individual request and be approved by the
Associate Dean for Clinical Affairs.
1. Students on clinical rotations wishing to attend a provisionally approved
professional meeting will submit a student travel request to the Associate Dean for
Clinical Affairs at least 30 days prior to the meeting indicating the name and
location of the professional meeting, sponsoring agency, and dates of prospective
absence.
2. Only one professional conference will be allowed per student per year of clinical
rotations. Any deviation from this policy must be approved by the Associate
Dean for Clinical Affairs on an individual basis.
3. Students must obtain permission from both the Associate Dean for Clinical
Affairs and the supervising preceptor and be in good standing, see Student
Responsibilities section of this manual.
4. A student travel request will be denied if the student is not in good standing or at
the discretion of the Associate Dean for Clinical Affairs.
5. Each student will be required to submit a one-page report on the meeting, and the
value added to the student’s education, in E*Value. Participation of professional
meetings outside of normal KYCOM curriculum is considered a privilege and
honor. Students must document meeting attendance in their eValue daily logs.
d. INTERVIEW POLICY
The following policy has been adopted regarding residency/internship interviews:
1. Students will be required to submit an Interview Request Form, signed by the
preceptor.
23
2. A maximum of three (3) days for absence is permitted, if approved by the Associate
Dean for Clinical Affairs, and must be recorded on student logs for the rotation.
Absence in excess of the 3-day standard will result in an “Incomplete” for this
rotation, until such time that the activity requirement is satisfied. Students that require
time away from the rotation, that would jeopardize the attendance policy, may request
for individual consideration from the Associate Dean for Clinical Affairs.
e. VACATIONS AND HOLIDAYS
Two winter breaks and the clinical capstone course are the only pre-approved leaves from
clinical rotations. Clinical service attendance during religious or national holidays is at
the discretion of the Supervising Physician, hospital or clinic facility. There are no
designated religious and/or national holidays approved by KYCOM during the
clinical rotations. Additional vacation time beyond what has already been described, can
be requested and scheduled during the clinical rotation period, and requires a submitted
request, sixty (60) days in advance of the event.
f. EXTENDED LEAVE
Direct written requests for extended leave to the Assistant Dean for Professional Student
Affairs. The Associate Dean for Clinical Affairs should be copied on all correspondence.
A leave of absence may be granted for one of the following reasons:
1. Health
2. Personal / Family
3. Financial Hardship
4. Pursuit of a graduate degree at this or another college or university
Extended leave of absence, for a maximum period of one year, may be granted by the
KYCOM Dean. Following an extended leave of absence, a student must submit a written
request to return to KYCOM to the KYCOM Dean.
Students that require time away from rotations, that would jeopardize the attendance
requirement, may request individual consideration from the Associate Dean for Clinical
Affairs.
GENERAL ROTATIONS INFORMATION
Student responsibilities listed below are expected of all KYCOM students, and subject to
individual hospital policies:
1. Students will write daily notes on all patients during rounds.
2. Student will be prepared to present their patients on rounds.
3. Students will have all patient charts on rounds and have prepared a maintained up to date
flow chart, with labs, medications, and other pertinent data.
4. Students will gather medical histories and conduct physical and osteopathic structural
examinations on all assigned patients.
5. Students will write discharge notes which include physical exam, diagnosis, medications
list, and follow-up appointments.
24

6. Students will keep a log in E*Value on all patients seen.
STUDENT LIABILITY INSURANCE
KYCOM students are covered with liability insurance and are covered only if the student is
participating in an officially approved rotation. This applies to core rotations as well as approved
elective and selective sites. If a student is aware of a potential legal liability situation, the Associate
Dean for Clinical Affairs must be notified immediately. Progression of any legal liability action
is to be detailed in writing by the student and regularly sent to the Office of the Associate Dean
for Clinical Affairs.
STUDENT EVALUATION (GRADE)
1. The student will be evaluated for each clinical rotation.
2. Only one grade will be applied per clinical rotation. The Associate Dean for Clinical
Affairs is responsible for the verification of all clinical rotation grades.
3. The evaluation is intended to measure the student in comparison to others at the same
level of education.
4. The “KYCOM Student Assessment Form” for in-person clinical rotations measures:
a. Mastery of Osteopathic Philosophy and Application of Manipulative Medicine
b. Medical Knowledge
c. Patient Care
d. Interpersonal and Communication Skills
e. Professionalism
f. Application of Practice Based Learning Skills
g. Application of Systems Approach to Medicine
5. The “KYCOM Student Assessment Form” for non in-person clinical experiences
measures;
a. Completion of all assigned readings
b. Completion of all quizzes
c. Completion of all assigned iHuman cases
d. Completion of all assigned Aquifer cases
e. Completion of at least 3 unique/original board type questions for each assigned
reading, with documentation
f. Any acts of plagiarism
g. Any acts of unprofessional behavior
6. Specific documentation of a failing grade should accompany the evaluation.
7. At the midpoint of the clinical rotation, a student-preceptor conference should take place
to indicate the level of student performance. A discussion as to the areas of strength and
weakness should be discussed at that time.
8. The Associate Dean for Clinical Affairs will refer a failing grade to the Promotions and
Matriculation Committee for further action or remediation.
9. Clinical grades may be reported as numeric scores or Pass/Fail as outlined in the course
syllabus.
GRADE APPEALS
A student who seeks to appeal a particular rotation grade must file a written request with
supporting documents for grade review within one month of the rotation grade being recorded.
25
The Associate Dean for Clinical Affairs will inform the student in writing of their decision to
either uphold or change the rotation grade. If the Associate Dean for Clinical Affairs denies the
grade appeal, the student may appeal to the P&M Committee for a final appeal of the grade.
The recommendation of the Committee will be forwarded to the Dean for a final decision on the
student’s grade. The decision of the Dean will be sent in writing to the student, P&M
Committee, Associate Dean for Clinical Affairs, and the Office of Academic Affairs.
REMEDIATION POLICY
All clinical rotations must be successfully completed with a passing grade prior to graduation.
Failure of any required or elective clinical rotation will be referred to the Promotions and
Matriculation Committee for consideration. Appeal of any rotation failure will follow the same
guidelines of any failure as stated in the Student Handbook. In cases where a passing grade is not
achieved, if deemed appropriate by the Promotions & Matriculation Committee, the student will
be given the opportunity to repeat the rotation. Upon successful completion of the repeated
rotation, a maximum grade of 70% will be recorded on the student transcript.
EMERGENCY PREPAREDNESS PLAN:
The University of Pikeville, which includes KYCOM, has undertaken an extensive risk analysis
and has approved protocols for a variety of potential disasters and emergencies. However,
because every emergency and/or disaster, whether natural or manmade, is unique and one or
even several plans cannot cover all scenarios; KYCOM students, faculty and staff are instructed
to follow these directions.
1. Any disaster or emergency announcement/instructions involving the University of
Pikeville or Pikeville community will be transmitted to all UPIKE individuals, including
KYCOM students, through the Alertus emergency notification system and via UPIKE
email. Responses to on campus emergencies come from the University President or his/
her designee.
2. In the event of an emergency or disaster at any KYCOM affiliated clinical site, the
student should refer to and follow the local emergency preparedness disaster plan and
instructions for that healthcare facility or site.
BLOOD BORNE PATHOGEN EXPOSURE AND POST-EXPOSURE PROPHYLAXIS
1. GENERAL: The goals of this policy are to insure the immediate cleansing of the
exposure site, reporting of the incident and, when indicated, immediate appropriate post-
exposure prophylactic treatment be started using CDC&P guidelines within two hours of
the exposure or less, and that appropriate laboratory work-up, counseling and follow-up
be provided. All costs above what is paid by the student's health insurance are borne by
KYCOM. The Blood Borne Pathogen (BBP) policy includes three (3) components;
a. Education.
b. Immediate post-mishap evaluation of exposure risk, as outlined by current Center
for Disease Control and Prevention (CDC&P) guidance and recommendations.
c. Appropriate follow-up.
2. EDUCATION: All KYCOM 2nd year students will attend a 2-hour block of instruction
on HIV and a 1-hour block on Universal Precautions annually which will address
26
CDC&P current relevant universal exposure precautions, the post-exposure reporting
process, prophylactic treatment of BBP and other transmitted disease as indicated.
3. BBP/HIV EXPOSURE
All students with medical education related BBP/HIV exposure through another person’s
blood or body fluids – by sharps injury or exposure to mucous membranes/skin – will
take the following steps immediately.
a. PERFORM BASIC FIRST AID: IMMEDIATELY clean the wound and skin with
soap and running water. Flush any mucous membranes or eyes with copious
amounts of water or normal saline for several minutes. Blood should be allowed to
flow freely from the wound. Blood should not be squeezed or “milked” from the
wound.
b. IMMEDIATELY NOTIFY your Preceptor or Attending physician. Any KYCOM
students with medical education related BBP/HIV exposure will be immediately
released from his/her preceptorship/rotation and go to the nearest affiliated
hospital Emergency Room (ER). If no affiliated hospital is in the area, go to the
nearest hospital with an ER.
c. NOTIFY the Office of Clinical Affairs of the incident.
d. The goals of the student reporting to the ER for BBP/HIV exposure are:
i. To help the student assess whether the exposure is low or high risk using
the most current CDC&P guidelines.
ii. Starting post-exposure prophylactic medication within two hours, if the
incident is a high risk. High-risk exposure is typically defined as
significant blood or bodily fluid exposure, of a source person with any of
the following: known HIV and/or symptoms of AIDS, multiple blood
transfusions 1978-1985, IV drug user, multiple sexual partners,
homosexual activity.
iii. Counseling the student on medication side effects and clarifying the
benefit/risk ratio of their use.
iv. Check baseline labs: HIV antibody testing, complete blood count, renal
and hepatic chemistry profile, and hepatitis evaluation.
e. The Associate Dean for Clinical Affairs shall be a point of contact for any
problem that may arise.
f. The student shall report for follow-up to the previously identified physician who is
the designated site clinical contact for BBP/HIV exposure. This individual will be
designated by the Chief of Staff or Director of Medical Education at each of the
core areas and be identified to the student prior to starting
preceptorship/rotation. This physician shall, at a minimum, be responsible for:
i. Insuring HIV antibody testing is done at 12 weeks and 6 months and
results checked.
ii. Writing prescriptions for the four-week drug regimen if needed.
iii. Repeating complete blood count and renal and hepatic chemistry profiles
at the discretion of treating physician.
27
1. Three (3) bullet points of your most noteworthy accomplishments. Each bullet should be
no longer than 2 sentences long and can be in any of the following areas:
a) Academic Achievements
b) Community Service
c) Research/Scholarly Activity
d) Leadership Activities
e) Awards, and/or Fellowships
Bullets are to be written in the third person (i.e. he, she, NOT I ) in a Word Document
naming it “your last name, first initial” (i.e. Doe, J.doc) and send it to Cathy Derry at
[email protected] before June 30th.
2. You will be sent a survey via email to complete and return via email. The survey will be
used to determine your recommendation. Recommendations are based on:
a) Academic Performance
b) Leadership Activities
c) Extracurricular Activities
Upon completion of the survey, save it as a Word document, naming it “your last name,
first initial survey” (i.e., Doe, J Survey.doc), and send it to Cathy Derry at
[email protected] before June 30th.
3. Your Core Rotation Grades and Comments. Please check your grades via Webadvisor
on a monthly basis to ensure your preceptors are submitting your grades in a timely
basis. You will also want to encourage your preceptors to provide comments on your
performance via E*Value. Your core rotations grades will be presented in graphs
comparing your performance to the class average and accompanied by the coordinating
comments from your preceptors.
If time allows, you will be provided an unsigned copy of your letter to review for
accuracy. You will have 3 business days to submit any corrections that are needed
before the letter is signed and finalized.
All letters will be uploaded prior to the deadline for Medical Student Performance
Evaluations.
PREPARATION FOR RESIDENCY
The Graduate Medical Education Application Process - The Associate Dean for Academic
Affairs authors the MSPE (Medical Student Performance Evaluation). This document is a peer
group evaluation which details the student in comparison to the entire class. In order to assist in
the preparation of the letter, the Office of Academic Affairs will need the following before June
30th of the third year of study:
28

SCHEDULING OF CORE CLINICAL ROTATIONS
The core site clinical rotations schedule will be established through the Office of Clinical Affairs
and Core Site Coordinators or Area Health Education Centers (AHEC), where available.
SCHEDULING OF ELECTIVE CLINICAL ROTATIONS
1. Twenty-four weeks of elective rotations are at the discretion of the individual student with
the approval of the Associate Dean for Clinical Affairs. Good Standing, as defined in
Student Responsibilities section of this manual, is required to apply.
2. All elective rotations are in four week blocks, and will begin on the first Monday of the first
week and end on the last Friday of the fourth week with no less than five (5) days per each
full week. Two elective rotation blocks may be divided into two, two-week blocks with
approval from the Associate Dean for Clinical Affairs.
3. Elective Clinical Rotation Forms are available from the Director of Clinical Rotations.
Elective Request forms must be completed and submitted to the Director of Clinical
Rotations at least 60 days prior to the anticipated start date of the rotation. Elective rotation
requests may be denied if paperwork completion requirements are not met. Twenty weeks of
elective rotations must be completed to meet graduation requirements.
4. Failure to submit an elective rotation request in the allotted time and to obtain elective
rotation approval, will jeopardize the elective, and may disrupt and/or lengthen a student’s
academic schedule.
5. Some sites require payment for completed elective rotations, which will be paid by the
student. Check with site coordinator before scheduling.
SCHEDULING OF SELECTIVE CLINICAL ROTATIONS
Selective rotations must include Emergency Medicine, Rural Medicine, Surgical Subspecialty
and Medicine Subspecialty. See the course descriptions
of these rotations for more detailed
information.
The objective of selective clinical rotations is to provide a framework for the evaluation and
management of the patient with acute and chronic pathophysiology that requires the consultation
of the specialty physician. The osteopathic medical student is given the opportunity to observe and
participate in the management of medical cases in the hospital environment, and experience the
intricacies of necessary diagnostic and therapeutic planned procedures. It is suggested that
se
lective rotations are served in the core site, to facilitate recognition of the role played by the
medical specialist in the care of hospitalized patients. Students must follow the following
procedure:
1. Submit a Selective Request Form to the Director of Clinical Rotations.
2. All requests must be submitted to the Director of Clinical Rotations at least 60 days
prior to
the anticipated start date of the rotation, and approved by the Associate Dean for
29

Clinical Affairs. Students must be in Good Standing, as defined in Student
Responsibilities section of this manual in order to apply. Selective rotation requests may
be denied if requests are submitted without sufficient time to process them.
VISITING STUDENT LEARNING OPPORTUNITIES (VSLO)
VSLO® is an electronic application service designed to streamline the application process for
senior selective/elective rotations at U.S. hospitals and medical centers that are members of the
Council of Teaching Hospitals and Health Systems (COTH). The service requires only one
application for all participating institutions, effectively
reducing paperwork, miscommunication,
and time.
KYCOM is a member of the Visiting Student Learning Opportunities (VSLO). KYCOM
students may apply for multiple rotations using the VSLO website. During February of the third
year of study, you will receive instructions on how to gain access to the VSLO website, via
UPIKE e-mail. Most programs begin accepting applications by May 1
st
of the third year of
study. When given access, you will need to complete your profile information and upload a
photograph. Students can upload all information, EXCEPT the transcript. The transcript will be
uploaded into your file by the UPIKE registrar’s office once your application has been
submitted. Credentialing documents, e.g. immunization records, letter of good standing or
criminal background check can be uploaded by the Clinical Affairs Office. However, KYCOM
cannot upload any document until the application is submitted by the student. Due to the
ongoing COVID-19 pandemic, all students should be aware that VSLO applications and
procedures may be modified throughout the year.
CHANGES IN CORE CLINICAL ROTATION
Changes in core clinical rotations are only permitted for compelling reasons. Written
documentation as to the reasons for a change should be directed to the Associate Dean for
Clinical Affairs. The decision as to the ability to change schedules will be at the discretion of the
Associate Dean for Clinical Affairs.
CHANGES IN ELECTIVE CLINICAL ROTATIONS
Changes in unconfirmed elective clinical rotations may be allowed only once per clinical rotation
after the schedule has been established. Rotations may not be changed less than sixty (60) days
prior to the start date. All changes are submitted in writing to the Associate Dean for Clinical
Affairs as to the changes and the reasons for the change. Changes in confirmed electives will
not be allowed without approval of the Associate Dean for Clinical Affairs. Any deviation from
this policy will result in a referral to the Promotions and Matriculation Committee for
further consideration.
THE CLINICAL COMPETENCY PROGRAM
Introduction
Competency in the world of evidence based medicine requires solid clinical skills, the ability to
work with other healthcare professionals, broad medical knowledge and familiarity with the
information highway. The clinical competency program is an adjunct to the clinical rotations
requirement and is designed to meet the following objectives:
30
Development of good communication and interpersonal skills
Demonstrate ability to identify and integrate health care resources
Effectively gather and present data
Expand basic medical knowledge
There are five programs that constitute The Clinical Competency Program. They are:
1. The iHuman and/or Aquifer Supplemental Cases, 3
rd
year and Clinical Journal Club, 4
th
year
2. The “End of Service” (COMAT) Exam Modules and COMSAE Exam
3. OPC V and OPC VI
4. Viewing of Educational Videos – During 4
th
year unless approved otherwise.
5. The Clinical Capstone Course
All components of the Clinical Competency Program are graded as “Pass/Fail”. However, they
are based on numerically graded formats as described below. “Fail” is defined as any numerical
score < 70 points.
1A. iHUMAN / AQUIFER SUPPLEMENTAL CASES - 3rd Year
iHuman and/or Aquifer Cases are assigned to the 3
rd
year osteopathic medical student
each block by the Clinical Affairs Department as an additional educational tool.
Objectives
a. To broaden medical knowledge
b. To allow osteopathic medical students to obtain a step by step approach on
how to perform a history and physical examination on a simulated patient.
c. To allow the osteopathic medical student to practice valuable skills such as
formulating a differential diagnosis, assessment, and plan for each patient.
d. To provide the osteopathic medical student with valuable feedback regarding
their performance on their simulated case experiences.
Format
All 3
rd
year students are required to complete all assigned cases each block.
iHuman and/or Aquifer assignments will be sent to the website by the Department
of Clinical Affairs and students will have access to them on the first day of each
clinical rotation.
Student Responsibilities
Complete the case each block, as assigned.
Grading
The grade will be based on adequate time spent on and the completion of the
assigned cases. Participation is Pass/Fail.
1B. CLINICAL JOURNAL CLUB - 4th Year
Articles will be chosen by KYCOM faculty. The 4th year osteopathic medical student
is partnered with peers and 4th year colleagues to review current topics in the medical
literature.
31
Objectives
a. To promote professional reading habits.
b. To encourage critical evaluation of published medical information.
c. To broaden medical knowledge.
d. To support collegiality among professionals
Format
All 4
th
year students are required to attend one journal club. Students will connect
to the program from their personal computers. Meeting assignments will be
issued by the Associate Dean for Clinical Affairs as follows:
a. Journal Club date assignments will be sent by University of Pikeville
(UPIKE) e-mail to all class members no later than the first day of rotations.
Substitution of assigned dates is the responsibility of the student. Changes to
the schedule must be reported to the Associate Dean for Clinical Affairs at
least 24 hours before the planned Journal Club meeting.
b. Notification of assigned journal articles will be released via Upike e-mail no
later than one week before the assigned date.
At the conclusion of each journal club session, the facilitator will assign five
questions to be answered via e-mail by noon eastern the following day.
c. Failure to pass or complete questions by noon eastern the following day will
restult in the failure of Journal Club and student must repeat.
Student Responsibilities
a. Read and outline the assigned journal article in advance of the meeting.
b. Be prepared to be called upon during the online meeting to discuss the article
content, related theory/clinical practice or study question material.
c. Submission of completed facilitator questions before 12:00 Noon ET on the
day following the meeting.
Attendance
a. Students are expected to attend the journal club meeting on the date assigned.
All attendance is verified by Go To Webinar.
b. If absences are reported to the Associate Dean for Clinical Affairs, prior to
airtime, a make-up date or alternate assignment will be given.
c. Failure to notify the Associate Dean for Clinical Affairs about unavoidable
absence from journal club requires a written explanation. Remediation will
be at the discretion of the Associate Dean for Clinical Affairs.
Grading
The grade will be based on successful completion of the five quiz questions, and
verified attendance. Study questions submitted by absentees or submitted
beyond the deadline will not be accepted. The question responses will be due
the morning after the session, and should be e-mailed to the program facilitator.
2. END OF SERVICE EXAMINATION MODULES - COMAT
a. Completion of on-line examination modules in the areas of Family Medicine,
Emergency Medicine, Internal Medicine, Surgery, Pediatrics, Women’s
Health, Osteopathic Principles & Practices, and Psychiatry is a mandatory
32

requirement to receive full credit for each of the above rotation disciplines.
The modules are prepared by the National Board of Osteopathic Medical
Examiners and entitled “Comprehensive Osteopathic Medical Achievement
Test” (COMAT). Each module is designed to assess medical knowledge in
the core subject area. The modules also serve to prepare the osteopathic
medical student for the COMLEX Level 2CE examination, taken by
KYCOM students after completion of the third year of study.
b. Exams will be completed during the fourth week of the rotation.
c. For two rotation disciplines, e.g. family medicine exams will be completed
during the fourth week of both rotations (Rotation grades for each discipline
will be considered an “incomplete” until the exam result is received by the
Associate Dean for Clinical Affairs.
d. The exam will account for 50% of the rotation grade.
Class of 2023 COMAT Grading Chart
0
55
60
65
70
75
80
85
90
95
100
<74
75-79
80-81
82-84
85-87
88-92
93-97
98-102
103-106
107-109
≥110
3. OPC V AND OPC VI
OST 703 AND OST 704 Course Description:
OPC V and VI are designated for (1) one
credit hour each. These third-year courses are a continuation of the OPC I-IV course(s)
and will serve to further expand and develop the world of osteopathic patient care
through a multifaceted approach. These
courses will be a standard didactic program for
third year students. Students will be required to complete 2 video modules per 4-week
block. These must be completed during each block, even if the student is off
rotation for board study. All modules will be presented on the Panopto Video Center.
Sessions will work in conjunction with the scheduled third year rotations.
Grading Policy: Students must complete a post-exam. Each post-exam will be
worth 5 points. There will be 5 post-exam questions per module.
OPC V Post-Exam (5 points) 50 Points
Total Possible Points for the Course:
50 Points
Course Passage = 70% or 35 of the total points available
OPC VI Post-Exam (5 points)
50 Points
Total Possible Points for the Course:
50 Points
Course Passage = 70% or 35 of the total points available
Remediation Policy: Students who do not achieve 70% or better in the course have
failed the OPC course. According to the KYCOM Student Handbook, all failures
are reviewed by the Promotion & Matriculation Committee and a decision is made
whether or not a student is allowed to remediate failed courses. If the Promotion &
Matriculation Committee decides a student is allowed remediate OPC, the student
33

will revisit and pass the modules failed. Remediation will be required during winter
break for OPC V and during the clinical capstone course for OPC VI.
4. EDUCATIONAL VIDEOS AND PROGRAMS
Each student is required to view or attend a minimum of ten (10) clinical programs (your
choice) during fourth year. The program(s), viewed and/or attended, must have the
capacity to issue a certificate of successful completion. A limit of two completed program
certificates must be earned per clinical rotation period, and submitted via e-mail to your
clinical clerkship coordinator. No more than two (2) clinical programs can be viewed on
the same day, and no more than two (2) certificates can be submitted at the same time to
receive credit.
Grading is “Pass/Fail” and remediation is at the discretion of the Associate Dean
for Clinical Affairs. Logs are considered INCOMPLETE without submittal of the
two (2) required certificates.
KYCOM allows the student to opt to attend AOA/AMA credentialed Continuing
Medical Education Programs (CMEs) held at the student’s host hospital or
medical center, on campus in Pikeville, on-line with UPIKE or at another COCA
accredited osteopathic medical school, or on-line or in-person at one of the two
other Kentucky medical schools. These do not include scheduled didactic
education meetings such as Morning Report, Tumor Board, rotation assignments,
UpToDate, or Clinical Key, etc. Alternative educational resources include:
• Annual KYCOM Pediatrics Symposium attendance – Equivalent to two (2)
certificates
• Annual KYCOM Alumni CME attendance – Equivalent to two (2)
certificates
• On-line viewing of A-OPTIC monthly Grand Rounds – Equivalent to one
(1) certificate. (www.A-OPTIC.org)
• On-line viewing of University of Kentucky CE CENTRAL video series –
Equivalent to one (1) certificate, regardless of the credit hours received per
certificate. (www.CECENTRAL.com)
5. THE CLINICAL CAPSTONE COURSE - TENTATIVE SCHEDULE
Introduction
A two-week period is provided on KYCOM campus to prepare the osteopathic medical
student for the challenges of both the 4
th
year of study and COMLEX Level 2
Performance Evaluation. Housing is provided. The student is responsible for their own
bedding, towels, toiletry items and meals. Program segments include:
a. WELCOME
i. Update contact information
ii. Complete order forms for graduation regalia
iii. Update financial aid information
iv. Introduction to the Clinical Skills Testing Performance Evaluation
b. PREPARATION FOR RESIDENCY - An on-line recorded program will be
available for off-campus viewing, for each of the following topics.
a) Electronic Residency Application Service (ERAS)
34

b) Medical Student Performance Evaluation – refer to General Rotations
Information: “Preparation for Residency” for submittal information
deadlines and content.
c. CLINICAL SKILLS TESTING PERFORMANCE EVALUATION
d. DRUG SCREEN
e. PROFESSIONALISM
f. MENTAL HEALTH
g. TITLE IX
Objectives
a. To strengthen the level of competency in clinical skills possessed by the
osteopathic medical student-in-training.
b. To determine necessary areas of concentration to achieve successful
professional competency.
c. To evaluate the osteopathic medical student’s readiness toward professional
competency.
d. To evaluate the osteopathic medical student’s readiness for graduation from
medical school.
e. To aim for success in the COMLEX Level 2 Performance Evaluation
Description
Modules have been developed to portray clinical encounters commonly seen by the
osteopathic physician in either the outpatient, primary care or emergency department
settings. Standardized patients have been trained to portray clinical scenarios in a
standardized fashion, appropriate to the clinical setting, and should be interviewed,
examined and treated as you would care for a “real patient”.
Format
The class will randomly be divided into groups, and scheduled to sequentially rotate
through simulated patient encounters. The student will review the chart information,
conduct a patient interview, perform a physical examination, perform any treatment
maneuvers, give (age/gender/race) appropriate health promotion information, review
findings with the patient, and answer any patient questions or concerns. At the end of
each encounter, the student will leave the room, and report to the “SOAP Note
Writing Station”. All SOAP notes (for proper credit) must be generated and stored on
the assigned computer. The student will document information gathered during the
patient history and physical examination, develop a “most to least likely” differential
diagnosis (at least three is recommended) and propose a treatment plan.
35

Evaluation
The student’s clinical performance will be graded by KYCOM clinicians in the
departments of Family Medicine, Osteopathic Principles and Practice and Bio
Medical Sciences. The standardized patients have been trained to provide an
evaluation of the student’s humanistic qualities (communication and listening skills,
patient respect, etc.).
Remediation
Students who are unsuccessful during the capstone course must attend a remediation
session on campus at KYCOM prior to taking the COMLEX Level 2 PE. The date of
the remediation will be determined by the Associate Dean for Clinical Affairs.
Suggested References
Le, Tao, First Aid for the USMLE Step 2 CS, latest edition
Savarese, Robert G., OMT Review, latest edition
Nelson, Kenneth E., Somatic Dysfunction in Osteopathic Family Medicine, latest
edition
Porter, Robert, The Merck Manual, 20th Ed., 2011.
Seidel’s Guide to Physical Examination, 9
th
Ed.
Gomella and Haist, Clinician’s Pocket Reference, 11
th
Ed., McGraw-Hill Co., latest
edition
Award of Honors
For the KYCOM Class of 2015 and subsequent KYCOM classes, class ranks are no longer
reported on student transcripts. Beginning with the 2021-2022 academic year, KYCOM will
recognize superior student achievement with the designation of Honors for any course or
clinical rotation in which the students achieves a 90% or greater final grade on core rotations.
The award of Honors recognizes superior student achievement and will be reported on the
student transcript. In order to be eligible for Honors, students must be in good academic
standing with no course or COMLEX board exam failures earned during the term or year under
consideration.
Further, students cannot be on a partial or decelerated schedule or repeating a course previously
taken to be considered for Honors designation.
36
GUIDELINES FOR PRECEPTORS
PRECEPTOR EDUCATIONAL RESPONSIBILITIES
Preceptors will provide instruction, supervision, and evaluation of the performance of students. If
for any reason the preceptor decides a student’s performance is unsatisfactory, he/she should
contact the rotations office before the rotation’s completion. If a problem arises with a student’s
performance, the KYCOM Associate Dean for Clinical Affairs will decide on the appropriate
action to be taken. The preceptor is encouraged to conduct a mid-rotation meeting with the student
to provide specific feedback on the student’s performance. This is especially important if the
student is not meeting expectations. The preceptor will evaluate the performance of the students
in writing immediately following completion of the rotation. Preceptors are encouraged to discuss
the evaluation with the student before returning it to KYCOM. The student will evaluate his/her
own performance, the educational services, and faculty participation at the rotation site. This
evaluation will also be submitted to the rotations office during the week following rotation. Copies
of KYCOM evaluation instruments are included at the end of this manual.
INSTRUCTIONAL OBJECTIVES FOR PRECEPTORS
The following guidelines are provided to aid supervising physicians and staff in meeting the
objectives of the curriculum for the students. The preceptor will:
1. Provide direction and guidance to enable the student to master the objectives listed in the
curriculum for the rotation.
2. Demonstrate availability for support, directional guidance and consultations with the
students.
3. Demonstrate a wide variety of knowledge necessary for the instruction of the student.
4. Effectively encourage questions and stimulate problem solving.
5. Admit freely a lack of knowledge when he or she encounters a situation that is not a
familiar medical problem.
6. Display the following personal traits:
a. attentive to the needs of the students
b. a calm and relaxed manner
c. enthusiasm about the practice of medicine
d. interest in presenting information to students
7. Effectively define and illustrate clinical signs and symptoms.
8. Help the students in developing skills in clinical problem solving.
9. Display a manner which exemplifies those characteristics that promote effective
physician/patient communication.
10. Display the appropriate psychosocial interactions that promote effective physician/patient
communication.
11. Provide the students with educational programs that will increase their knowledge.
ATTENDING PHYSICIAN RESPONSIBILITIES
The preceptor/attending physician possesses the experience and training to:
1. Review and co-sign all written materials
a. Progress Notes
b. History and Physical Exams
c. Admit Notes and Discharge Summaries
37

d. Treatment Orders
2. Review Student Performance
a. Conduct a mid-rotation evaluation session to discuss the student’s progress
b. Completion and Submittal of the “KYCOM Student Assessment Form” at the
completion of the rotation.
3. Attend Patient Rounds
a. Answer case specific questions
b. Emphasize important “learning” points
c. Direct the student’s case management activities
4. Serve as a Mentor
5. Suggest Reading
STUDENT RECORD KEEPING
LOGS
All students are required to maintain an accurate electronic log of every patient seen each day
during ambulatory and hospital care. All attending physicians are entitled to review this log at
any time, and encouraged to review them at the end of the rotation. Logs and evaluations are to
be completed within fourteen (14) calendar days from the last day of the rotation. After 14
days, if logs are not completed, the maximum rotation score will be 70% and the student will
be referred to the P&M Committee for further action.
The following Case Log components are mandatory:
1. Student Assessment Form
2. Rotation Evaluation Form –
utilized for student evaluation of the clinical experience.
This evaluation will be accumulated and reviewed for credentialing and curricular
purposes and must accompany all Case Logs.
The following entries are suggested for each of the following log areas:
1. Student Log – Ambulatory Clinic Rotation – utilized on all ambulatory clinical rotations,
including but not limited to rotations such as Family Medicine, General Internal
Medicine, and Pediatrics. This would be an outpatient log and would not include
hospitalized patients.
2. Student Log – Hospital Case Participation – noting the following:
a. Patient identification number or initials only. It is a HIPAA violation to identify
patients by name.
b. Admission date
c. Diagnosis –
Provisional or Final
d. Level of Participation
e. H&P Performed
f. Attending Physician
g. OMT
38
4. Student Log – Surgery – utilized during the surgical core and elective rotations noting the
surgical procedures, level of participation, final diagnosis, and whether the procedure was
performed on an inpatient or outpatient basis.
5. Student Log – Obstetrics – utilized on all obstetrical cases.
6. Student Log – Special Procedures – examples such as laceration repair, Pap smear,
Electrocardiography, Surgical biopsy, Cardiac stress test, etc.
7. Student Log – Educational Programs – listing of all clinical didactic lecture activities
including Journal Club, Morbidity & Mortality Review, Tumor Board, Videoconferences,
County Medical Society, etc.
8. Student Log – Reading Program – noting the breadth and depth of the student’s
professional reading experience during the clinical rotation. This would also include any
references for research performed at the request of the preceptor. The log would list the
names of books, journals, or other educational material completed during the log period.
No Case Logs will be considered complete without the appropriate completed component parts.
For purposes of credentialing, gaining future practice privileges or certification, students should
permanently keep signed copies of their logs. This can be done by exporting the log documents
from E*Value to Microsoft Excel. KYCOM will not keep file copies of such documents for more
than one year, and it is the student’s responsibility to be able to produce original documentation
of his/her training.
GRADUATION REQUIREMENTS
1. Successful Completion of COMLEX level 1, Level 2-CE, and Level 2-PE
2. Completion of Educational Programs
3. Completion of Capstone Course
4. Completion of Clinical Journal Club and iHuman and/or Aquifer modules
5. Successful completion of end-of-service examination modules in Internal Medicine,
Family Medicine, Pediatrics, General Surgery, Women’s Health, Osteopathic
Manipulative Medicine, Psychiatry and Emergency Medicine.
6. Successful completion of OPC V and OPC VI.
7. Successful Completion of all clinical rotations and submittal of all documentation
a. Submittals of all clinical rotation logs
b. Student Assessment Forms
c. Documentation of required encounters
8. Attendance at all class meetings
a. Class meeting at conclusion of the 3
rd
year of study
b. Exit class meeting at conclusion of 4
th
year of study
c. Attendance at graduation exercises
39
COURSE SYLLABI
40
OST 799 INDEPENDENT STUDY I
Faculty: Dr. Joshua Crum (Course Director)
Office: Coal Building 611
Hours: By appointment
E-mail: [email protected]
Texts: N/A
Supplemental Texts: N/A
Hours: 4.0 credit hours
Every four-credit course as outlined in this policy, and the appropriate grade will be part of the
student’s permanent KYCOM transcript. However, credits earned in this course will NOT take
the place of any clinical rotation requirements as outlined in the Student Handbook and Clinical
Rotations Manual. The credit hours earned in this course will not be calculated into the student’s
grade point average.
Course Description: This is an independent study course in which students will be provided a
detailed individualized study plan to prepare them for their COMLEX-USA Level 1 examination.
The study plan will include required assessments to provide benchmarks for preparedness, as well
as usage of specified question banks and study resources.
This course will be four weeks in duration, but can be continued in four week increments as
approved by the course director as long as the student is preparing for their COMLEX-USA retake
examination. In addition, if necessary, this course may be repeated approved by the course director
and the Promotions and Matriculation Committee if the student’s board examination retake is not
passed.
Course Goal: The primary goal of this course is to provide the student additional time and
structure to prepare for the COMLEX-USA Level 1 examination.
Course Attendance: N/A.
Course Format: Students will have an individual study plan to follow with built-in assessments
and question bank goals to serve as benchmarks for preparedness to retake their COMLEX-USA
board examination.
Grades: Grades will be reported as Pass or Fail. Students following the assigned study plan and
taking the COMLEX-USA Level 1 examination on their assigned date will Pass. Students who
do not follow the assigned study plan or who do not take their COMLEX Level 1 on the assigned
date will fail this course. Failure of this course can be grounds for dismissal from KYCOM.
Examination Policy: There are no examinations in this course other than the assigned assessment
tests.
41
Challenge of Examination Questions: N/A
Remediation Policy: According to the KYCOM Student Handbook, all failures are reviewed by
the Promotion & Matriculation Committee and a decision is made whether or not a student is
allowed to remediate failed courses. The Promotion & Matriculation Committee could
recommend dismissal or decide a student may remediate Independent Study 1. Should remediation
be recommended the student will meet with Dr. Crum to develop a new study plan and set new
dates for assessments and the COMLEX-USA Level 1 examination. The format for remediation
will be at the discretion of Dr. Crum but may require the student to purchase/attend a third-party
preparatory course.
42
OST 899 INDEPENDENT STUDY II
Faculty: Dr. Joshua Crum (Course Director)
Office: Coal Building 611
Hours: Anytime or by appointment
E-mail: [email protected]
Texts: N/A
Supplemental Texts: N/A
Hours: 4.0 credit hour
Every four-credit course as outlined in this policy, and the appropriate grade will be part of the
student’s permanent KYCOM transcript. However, credits earned in this course will NOT take
the place of any clinical rotation requirements as outlined in the Student Handbook and Clinical
Rotations Manual. The credit hours earned in this course will not be calculated into the student’s
grade point average.
Course Description: This is an independent study course in which students will be provided a
detailed individualized study plan to follow to prepare them for their COMLEX-USA Level 2CE
or Level 2 PE examination. The study plan will include required assessments to provide
benchmarks for preparedness, as well as usage of specified question banks and study resources.
Course Goal: The primary goal of this course is to provide the student additional time and
structure to prepare for the COMLEX-USA Level 2CE or Level 2PE examination.
Course Attendance: N/A.
Course Format: Students will have an individual study plan to follow with built-in assessments
and question bank goals to serve as benchmarks for preparedness to retake their COMLEX-USA
board examination.
Grades: Grades will be reported as Pass or Fail. Students following the assigned study plan and
taking the COMLEX-USA Level 2CE or Level 2 PE examination on their assigned date will Pass.
Students who do not follow the assigned study plan or who do not take their COMLEX Level 2CE
or Level 2 PE on the assigned date will fail this course. Failure of this course can be grounds for
dismissal from KYCOM.
Examination Policy: There are no examinations in this course other than the assigned assessment
tests.
Challenge of Examination Questions: N/A
43
Remediation Policy: According to the KYCOM Student Handbook, all failures are reviewed by
the Promotion & Matriculation Committee and a decision is made whether or not a student is
allowed to remediate failed courses. The Promotion & Matriculation Committee could
recommend dismissal or decide a student may remediate Independent Study Level II. Should
remediation be recommended the student will meet with Dr. Crum to develop a new study plan
and set new dates for assessments and the COMLEX-USA Level 2CE or Level 2 PE examination.
The format for remediation will be at the discretion of Dr. Crum but may require the student to
purchase/attend a third-party preparatory course.
44
OSTEOPATHIC PATIENT CARE (OPC) V
Faculty: Joshua Crum, D.O., Course Director
Laura Griffin, D.O., et al.
Course Hours: OPC V is designated for (1) one credit hour. Training modules are scheduled to be
recorded and made available via Panopto Video System and/or the AOPTIC website. Please
refer to the lecture schedule on CANVAS for instructions on how to access videos and the days
and times as to when these training modules will be made available. The course extends from the
first day of clinical rotation, 3
rd
year, until the last day of the fifth clinical rotation, 3
rd
year.
Course Description: This third-year course is a continuation of the OPC I-IV course(s) and will
serve to further expand and develop the world of osteopathic patient care through a multifaceted
approach. The course will be a standard didactic program for third year students. This course
will consist of recorded modules and online exercises (via Panopto Video Center and/or the
AOPTIC website in addition to pre-video and post-video exams on CANVAS). Essential
components of the course will include reinforcement of principles of medical issues incurred
after graduation including but not limited to, osteopathic manipulative treatment, physicians’
relationship with patients and social dilemmas in medicine, pain management, physician
payment systems, substance abuse, landmark trials and Good Samaritan laws.
Course Goals:
1. To integrate Osteopathic Principles and Practices throughout the third year clinical clerkship
experience.
2. To standardize the clinical curriculum and to further develop an appreciation of the:
a. Ethical issues relevant to practicing medicine.
b. Patient’s role in his/her healthcare.
c. The key issues in relationships between physicians and patients.
d. Professionalism needed in healthcare profession
e. The potential impact of working with patients and others with different moral,
cultural, and religious views etc.
f. Domestic violence and Abuse, Substance abuse and Disorders, Right to Die, Pain
management, Global issues in Medicine, billing systems and laws affecting the
healthcare profession.
3. To further develop medical decision making skills.
4. To hone diagnostic and treatment/management skills.
5. To hone effective physician-patient communication skills.
6. To further develop and maintain a good physician and patient relationship and continue to
master the art of osteopathic manipulative treatment.
Course Format:
Students will be required to complete 2 video modules per rotation. This course will consist of 5
rotations (August -December) and 10 modules. All modules will be presented on the Panopto
45

Video Center and/or AOPTIC websites. After viewing each module, students will take a post-
exam on CANVAS. Sessions will work in conjunction with the scheduled third year rotations, and
designed to meet the course objectives noted above. These videos must be completed during
each block, even if you are off rotations for board study.
Grading Policy: Students will complete a post-exam worth 5 points (5 questions).
10 Post-Exams (5 points each) 50 Points
Total Possible Points for the Course: 50 Points
Course Passage = 70% or 35 of the total points available
Examination Policy: The examination policy for UP-KYCOM will be followed for all block
exams (if applicable).
Remediation Policy: Students who do not achieve 70% or (35) cumulative points or better in
the course have failed the OPC V course. According to the KYCOM Student Handbook, all
failures are reviewed by the Promotion & Matriculation Committee and a decision is made
whether or not a student is allowed to remediate failed courses. If the Promotion &
Matriculation Committee decides a student is allowed remediate OPC V, the student will revisit
and pass the modules failed. Remediation will be required during Winter Break of third year.
46
OSTEOPATHIC PATIENT CARE (OPC) VI
Faculty: Joshua Crum, D.O., Course Director
(606) 218-5428
Laura Griffin, D.O., et al.
Course Hours: OPC VI is designated for (1) one credit hour(s). Training modules are scheduled to
be recorded and made available via Panopto Video System and/or the AOPTIC website. Please
refer to the lecture schedule on CANVAS for instructions on how to access videos and the days
and times as to when these training modules will be made available. The course extends from the
first day of the sixth clinical rotation, 3
rd
year, through the last day of the eleventh clinical rotation,
3
rd
year.
Course Description: This third-year course is a continuation of the OPC I-V course(s) and will
serve to further expand and develop the world of osteopathic patient care through a multifaceted
approach. The course will be a standard didactic program for third year students. This course
will consist of recorded modules and online exercises (via Panopto Video Center and/or the
AOPTIC website with post-video exams on CANVAS). Essential components of the course will
include reinforcement of principles of medical issues incurred after graduation including but not
limited to, osteopathic manipulative treatment, physicians’ relationship with patients and social
dilemmas in medicine, pain management, physician payment systems, substance abuse,
landmark trials and Good Samaritan laws.
Course Goals:
1. To integrate Osteopathic Principles and Practices throughout the third-year clinical clerkship
experience.
2. To standardize the clinical curriculum and to further develop an appreciation of the:
a. Ethical issues relevant to practicing medicine.
b. Patient’s role in his/her healthcare.
c. The key issues in relationships between physicians and patients.
d. Professionalism needed in healthcare profession
e. The potential impact of working with patients and others with different moral,
cultural, and religious views etc.
f. Domestic violence and Abuse, Substance abuse and Disorders, Right to Die, Pain
management, Global issues in Medicine, billing systems and laws affecting the
healthcare profession.
3. To further develop medical decision-making skills.
4. To hone diagnostic and treatment/management skills.
5. To hone effective physician-patient communication skills.
6. To further develop and maintain a good physician and patient relationship and continue to
master the art of osteopathic manipulative treatment.
47

Students will be required to complete 2 videos per 4-week block. All modules will be presented
on the Panopto Video Center and/or AOPTIC websites. Sessions will work in conjunction with the
scheduled third year rotations, and designed to meet the course objectives noted above. All students
must complete the sessions even if rotations are suspended for board study due to a board failure.
Grading Policy: Each post-exam will be worth 5 points. There will be 5 post-exam questions
per module.
Post-Exam (5 points) 50 Points
Total Possible Points for the Course: 50 Points
Course Passage = 70% or 35 of the total points available
Examination Policy: The examination policy for UP-KYCOM will be followed for all block
exams (if applicable).
Remediation Policy: Students who do not achieve 70% or (35) cumulative points or better in
the course have failed the OPC VI course. According to the KYCOM Student Handbook, all
failures are reviewed by the Promotion & Matriculation Committee and a decision is made
whether or not a student is allowed to remediate failed courses. If the Promotion &
Matriculation Committee decides a student is allowed remediate OPC VI, the student will revisit
and pass the modules failed. Remediation will be required in May, prior to the beginning of
fourth year.
Course Format:
48

CORE ROTATION CURRICULUM
The following applies to all core rotations:
Student Hours
Daily hours are to parallel the hours of the attending physician, however, the following
guidelines are suggested:
1. A work day may be considered 12 hours in duration.
2. A work week may be considered typically 72 hours, however, should not exceed 80 hours
in duration.
3. Maximum continuous duty should not exceed 24 hours and should be followed by a
minimum of 12 hours off duty.
4. Two days out of every 14 days should be provided as a weekend break.
5. Students are required to work a minimum of 40 hours per week.
Location
The physician’s office, outpatient clinic, and/or participating hospital(s) within the core site.
Dress
At all times, KYCOM students will act as a representative of the school, and be attentive to
personal hygiene, cleanliness and personal demeanor. Short white lab coats with KYCOM
identification are expected to be worn unless specifically instructed by the hospital or preceptor.
Scrub suits are to be worn in the operating room, procedure rooms, during call hours and at the
discretion of individual physicians and/or institution/facility. At all times, however, the student
must be clearly identified as a KYCOM student. See Student Responsibilities section of this
manual for clarification.
Attendance
Prompt student attendance is expected for a minimum of 20 days each four-week rotation period
and 10 days for each two-week rotation period. The expectation is that students work Monday
through Friday with weekends off. However, the work day will vary by rotation. If the preceptor
works weekends, the student is expected to work weekends also. The activities of each day must
be recorded on student logs for the rotation. A maximum of three (3) days for absence is
permitted, with prior approval by the associate dean for Clinical Affairs, and must be recorded
on student logs for the rotation. Absence in excess of the 3-day standard will result in an
“incomplete” for this rotation, until such time that the activity requirement is satisfied.
Absence of the attending physician or the student, from the practice for a period greater than one
day, requires the student to notify the office for Clinical Affairs, of the interruption of activity.
At the discretion of the associate dean for Clinical Affairs either a reading assignment or
alternate duty assignment will be made.
Lectures and Meetings
It is the responsibility of the student to be familiar with the hospital’s didactic lecture schedule,
and to document attendance within the student log. Didactic programs include but are not limited
to: Morning Report, Journal Club, Morbidity/Mortality Conference, Grand Rounds, and Noon
Conference. Absence from any of these events requires the signature of the preceptor, and should
49

be sent with the student log reports to KYCOM. It is expected that the student will attend a
minimum of 70% of each kind of event.
Grading
The KYCOM Student Assessment Form for CORE (and EM) rotations, which is completed by
the attending physician, comprises 50% of the rotation grade. The COMAT examination score
comprises the balance of the grade. Upon receipt and review of all information, the associate
dean for Clinical Affairs evaluates the material, and assigns a numerical grade, as per the
Clinical Rotations Manual, Student Evaluation (Grade). The evaluation is intended to measure
the student in comparison to others at the same level of education.
The KYCOM Student Assessment Form measures:
1. Mastery of Osteopathic Philosophy and Application of Manipulative Medicine
2. Medical Knowledge
3. Patient Care
4. Interpersonal and Communication Skills
5. Professionalism
6. Application of Practice Based Learning Skills
7. Application of Systems Approach to Medicine
Challenge of Grades
Any challenges or questions are to be directed to the Associate Dean for Clinical Affairs. The
student has the right for review of the challenge by the Promotions and Matriculation
Committee, if the associate dean’s response requires further clarification.
Remediation
In cases where a passing grade is not achieved, if deemed appropriate by the Promotions &
Matriculation Committee, the student will be given the opportunity to repeat the rotation. Upon
successful completion of the repeated rotation, a maximum grade of 70% will be recorded on
the student transcript.
50
OST 700: Clinical Osteopathic Medicine
Course Description
Clinical Osteopathic Medicine is a mandatory CORE rotation. The program attempts to answer
the questions of “WHEN”, “WHY”, “HOW”, “WHERE”, and “IF” to utilize osteopathic
manipulative techniques as part of the treatment plan for the medical/surgical patient. The
appreciation of the intercommunication of the body systems, and the interpretation of T A R T
findings is incorporated into the diagnosis and treatment of neural, muscular, joint, and visceral
dysfunction. The osteopathic medical student is introduced to the evaluation and management of
medical/surgical patients in both the out-patient and in-hospital setting.
Course Objectives
1. To master examination skills of both the axial and appendicular skeleton for disorders,
and/or somatic dysfunction.
a. Displays knowledge of neurologic and muscular diagnostic tools.
b. Displays knowledge of the osteopathic structural examination.
2. To recognize physical changes of soft tissue structures for somato-somatic, somato-
visceral, viscero-visceral and viscero-somatic reflex dysfunction.
3. To display clinical competency in the use of direct treatment approaches:
a. High Velocity, Low Amplitude treatment of articular somatic dysfunction.
b. Application of Muscle Energy to treatment of articular somatic dysfunction.
c. Application of myofascial release to restricted soft tissue structures.
4. To display clinical competency in the use of indirect treatment approaches:
a. Application of Counterstrain to restricted soft tissue structures.
b. Application of Myofascial Release to restricted soft tissue structures.
c. Application of “Balance and Hold” techniques to treatment of articular and fascial
somatic dysfunction.
d. Application of “Osteopathic Cranial Manipulative Medicine” to treatment of cranial
and sacral somatic dysfunction.
e. Application of “Progressive Inhibition of Neuromusculoskeletal Structures” to
restricted soft tissue structures.
5. To display clinical competency with the “decision making” process for proper
utilization/application of osteopathic manipulative procedures to clinical problems.
a. Osteopathic approaches as diagnostic tools.
b. Osteopathic techniques as primary and/or secondary treatment tools.
c. Osteopathic approaches as palliative tools.
Student Duties
1. The student participates in the out-patient setting. Responsibilities include:
a. Performance of physical examinations to include performance of Osteopathic
Structural Examination.
b. Performance of Osteopathic Manipulative Treatment under supervision.
c. Production of progress, SOAP notes on each assigned patient.
d. Participation in “after-hours” call rotation.
51

e. Attendance at hospital conferences.
2. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
See CANVAS on the University of Pikeville website.
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-principles/
See also the CORE ROTATION CURRICULUM cover page in this manual.
52
OST 708: Family Medicine I
Course Description
Family Medicine I is a mandatory, four-week, third-year core rotation that may be served in
either the in-patient or out-patient setting. The third-year osteopathic medical student is
progressed from the clinical courses introduced during the two pre-clinical years to their
application in patient care. A hospital setting is preferable, however, course objectives can be
achieved in an office setting. Preventive care, family planning, end of life care, acute and chronic
care applied across all age groups, coordination of medical services and the operation of a
professional practice are among the many experiences gained over the four weeks.
Course Objectives
1. To provide a framework for care of the general medical patient.
a. To develop and apply interviewing skills to the patient encounter, as a means to both
solidify physician-patient relationships and produce preliminary differential
diagnosis.
b. To utilize physical examination skills to progress from preliminary differential
diagnosis to a probable differential diagnosis and the development of a diagnostic and
treatment plan.
c. To experience the evolution of a diagnostic plan, and the establishment of a working
diagnosis and its associated treatment plan.
d. To identify and apply core osteopathic principles and practices to the care of the
general medical patient
e. To identify available social and medical resources and the family physician’s role in
their coordination to patient care, i.e. referral decision-making.
f. To view the role of experience based medicine to medical decision-making.
2. To provide a framework for preventive medical care to all age groups.
3. To expose students to the operation of a professional office:
a. The roles of staff and physician(s) in the delivery of healthcare.
b. The influences of third party insurance and medical decision-making.
c. Care and recording of medical records.
d. The roles of the “International Classification of Diseases” and “Current Procedural
Terminology” and their impact on physician reimbursement.
e. The role of the telephone, and other electronic communication tools in the delivery of
healthcare.
f. Awareness of physician responsibilities under HIPAA and OSHA regulations.
4. To provide knowledge of office procedures, their associated equipment, and laboratory
submittal requirements.
a. Phlebotomy
b. Wound repair and suture removal
c. Electrocardiography
d. Spirometry
e. Audiometry
f. Screening examinations of the male and female breast
g. The anal, rectal and prostate examination
h. The female internal examination
53

5. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
c. Telephone and in-person communication with other medical and health professionals
involved in common, with the care of the general medical patient.
Student Duties
The student participates as both a member of the hospital house staff and office staff.
Responsibilities include:
1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients including:
a. Production of a progress SOAP note in each assigned patient chart.
b. Investigation of all diagnostic studies ordered for the patient.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
3. Assist and/or perform office procedures under supervision.
4. Office set-up and performance of procedures:
a. Osteopathic Manipulative Treatment
b. Preventive health screens
c. Minor surgery
d. Preparation of laboratory specimens
e. Draping and gowning
5. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-family-medicine/
See also the CORE ROTATION CURRICULUM cover page in this manual.
54
OST 709: Family Medicine II
Course Description
Family Medicine II is a mandatory, third year, upper level, four-week core rotation, that may be
served in either the in-patient or out-patient setting. The osteopathic medical student is, under
preceptor supervision, actively engaged in both the care and the medical decision-making for
both the in-patient and out-patient population. During the four weeks, the osteopathic medical
student will evaluate patients, develop comprehensive care plans and experience the
responsibilities associated with physician actions.
Prerequisite: Family Medicine I
Course Objectives
1. To develop efficient and complete evaluative and management skills for the care of the
general medical patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination, while including preventive medical care for all age groups.
b. To formulate and test preliminary differential diagnosis during the physical
examination.
c. To develop a diagnostic and treatment plan.
d. To establish a working diagnosis and the challenges associated with the
implementation of the treatment plan.
e. To apply core osteopathic principles and practices to the care of the general medical
patient.
f. To coordinate available social and medical resources as part of the comprehensive
treatment plan.
g. To, under preceptor supervision, take the family physician’s role in referral decision-
making.
i. To view the role of experience based medicine to medical decision-making.
ii. To view the availability of services and its impact on patient care.
iii. To view the effect of outside influences, e.g. third party insurance, on medical
decision-making.
2. To develop a model for the operation of a professional office:
a. Examine the roles of staff and physician(s) in the delivery of healthcare. This may
include, with the consent of the preceptor, attendance at office staff meetings.
b. Develop an understanding of the influences that third party insurances have on
medical decision-making.
c. Understand the laws that govern the care and recording of medical records.
d. Gain a working knowledge of the “International Classification of Diseases” and
“Current Procedural Terminology” and their impact on physician reimbursement.
e. Examine the telephone system, and other electronic communication tools in relation
to the delivery of healthcare.
f. Know the HIPAA and OSHA regulations in regard to the operation of a professional
medical practice.
i. Confidentiality
ii. Hazardous waste removal
55

iii. Emergency procedures
g. To develop an inventory of necessary property and supplies for the daily operation of
a general medical practice.
3. To continue development of written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
Telephone and in-person communication with other medical and health professionals involved in
common, with the care of the general medical patient.
Student Duties
The student participates as both a member of the hospital house staff and office staff.
Responsibilities include:
1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients including:
a. Production of a “problem-based” progress SOAP note in each assigned patient chart.
b. Maintain “out of chart” treatment plans on each assigned patient for purposes of
bedside discussion and comprehensive care planning.
c. Investigation and interpretation of all diagnostic studies ordered for the patient, and
be prepared to discuss findings for purposes of comprehensive care planning.
d. Follow-up with all consultants on assigned patients, and be prepared to discuss
findings for purposes of comprehensive care planning.
e. Production of any case summaries and/or discharge summaries for the admitted
patient.
f. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
g. Assist and/or perform office procedures under supervision.
h. Office set-up and performance of procedures:
i. Osteopathic Manipulative Treatment
ii. Preventive health screens
iii. Minor surgery
iv. Preparation of laboratory specimens
v. Draping and gowning
i. Attend and observe, with preceptor permission, family meetings.
3. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-family-medicine/
See also the CORE ROTATION CURRICULUM cover page in this manual.
56
OST 720: General Internal Medicine I
Course Description
General Internal Medicine I is a mandatory, four-week third year core rotation that may be
served in either the in-patient or out-patient setting. The third year osteopathic medical student is
progressed from Course No. 607, second year Introductory Internal Medicine, and Course No.
604, Clinical Applications of Osteopathic Medicine, to practical application in the hospital
setting. The pathophysiology of cardiovascular, cerebrovascular, pulmonary, renal,
gastrointestinal and endocrine disorders are among the patient population seen. As a member of a
multi-disciplinary internal medicine “teaching” service, under the supervision of hospitalists,
general internists, and medicine subspecialists, the osteopathic medical student participates in the
admission, in-hospital care and discharge of the patients served.
Course Objectives
1. To develop age and gender specific, problem oriented history and physical examination
skills.
2. To learn effective communication skills.
a. The focused patient interview
b. Peer case presentation techniques
c. Production of coherent admission, progress, and discharge notes
3. To correlate information gained from the patient’s chief complaint, medical, surgical,
social, and familial histories with the signs and symptoms seen on examination to
develop differential diagnoses in order of likelihood.
4. To appreciate the role that experience based medicine plays in the management of the
medical patient.
5. To appreciate the need for preventive medical care as part of the total treatment regimen
for the medical patient.
6. To learn the principles of the production and implementation of a total treatment plan.
7. To expose students to the operation of a hospital.
a. The hospital laboratory
b. The radiology department
c. The nursing staff and patient care management.
d. The physical, occupational, speech, and respiratory therapy teams.
e. The social services department
f. The strict observance of HIPAA and OSHA regulations.
g. The coordination of patient care.
8. To provide practical procedural knowledge:
a. Phlebotomy and arterial blood gases
b. Insertion of nasogastric tubes
c. Insertion of urinary catheters
d. Insertion of central vascular catheters
e. Electrocardiography
f. The rectal examination
g. Cardiovascular resuscitation
h. Lumbar spinal puncture
i. Culture of blood, body fluid and soft tissues
57

Student Duties
The student participates as a member of the hospital house staff.
1. Performance of admission histories and physicals for the patients of “teaching” attending
physicians
2. Completion of rounds on all in-patients of “teaching” attending physicians.
3. Performance of afterhours call.
4. Attendance at hospital conferences.
5. Performance, under supervision, of minor bedside procedures.
6. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
Gomella, Leonard and Steven Haist, Clinicians Pocket Reference, Latest Edition
o Ch. 2: Chartwork
o Ch. 15: Imaging Studies
o Ch. 19: Basic ECG Reading
Thaler, Malcolm, The Only EKG Book You’ll Ever Need, 9th ed.
o Ch. 8: Putting It All Together – 11Step Method for EKG Reading
Simon, Roger P., Greenberg, David A., and Michael Aminoff, Lange Clinical Neurology,
Latest Edition
o Ch. 1 Ch. 1 Neurologic History & Examination or Appendix: Clinical
Examination of Common Isolated Peripheral Nerve Disorders
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-internal-
medicine/
See also the CORE ROTATION CURRICULUM cover page in this manual.
58
OST 721: General Internal Medicine II
Course Description
General Internal Medicine II is a mandatory, four-week core rotation that may be served in either
the in-patient or out-patient setting. The osteopathic medical student, under the supervision of
either a general internist, or medical subspecialist and house staff, is encouraged to incorporate
evaluative skills, and evidence based medical information, to develop a comprehensive treatment
regimen based on logical medical decision-making.
Pre-requisite: General Internal Medicine I
Course Objectives
1. To experience the responsibilities of an intern or resident.
2. To experience case management and the coordination of systems based medical care.
a. The use of subspecialists and other medical/surgical disciplines.
b. The use of social services and outpatient programs
c. The use of physical therapy
d. The use of in-house care services.
3. To produce and implement a total treatment plan.
4. To experience prioritization skills.
5. To develop a problem oriented approach to patient care.
6. To develop a sense of cost-effective medical care.
Student Duties
1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients.
3. Performance of after-hours call.
4. Attendance at hospital conferences.
5. Performance of bedside procedures.
a. Placement of catheters
b. Central and peripheral line placement
c. Electrocardiography
d. Spirometry
e. Sepsis work-up and procedures
6. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Readings
Longo, Fauci, Kasper, Hauser, Jameson & Loscalzo, Harrison’s Manual of Medicine,
McGraw Hill, Latest Edition
o Ch. 5: Principles of Critical Care Medicine
o Ch. 7: Assessment of Nutritional Status
o Ch. 14: Sepsis and Septic Shock
o Ch. 16: Acute Respiratory Distress Syndrome
o Ch. 19: Stroke
59

o Ch. 121: ST-Segment Elevation Myocardial Infarction (STEMI)
o Ch. 122: Unstable Angina and Non-ST-Elevation Myocardial Infarction
o Ch. 140: Chronic Obstructive Pulmonary Disease
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-internal-
medicine/
See also the CORE ROTATION CURRICULUM cover page in this manual.
60
OST 740: General Surgery
Course Description
General Surgery I is a mandatory third year core rotation. The third year osteopathic medical
student is introduced to the department of surgery within the hospital. Assignments are inter-
disciplinary, and subject to the operative schedule. The osteopathic medical student is given the
opportunity to explore the evaluation and management of the surgical patient, pre-operatively,
intra-operatively and during the post-operative period.
Course Objectives
1. To provide a framework for care of the surgical patient.
2. To provide a review of:
a. Asceptic technique
b. Gowning and gloving
c. Methods for entry/departure from the surgical theatre
3. To identify and apply core osteopathic concepts to the care of the surgical patient.
4. To experience the pathophysiology relevant to affected organ systems, and the efficacy of
surgical care.
5. To expose students to an evaluative approach to diagnosis and management of the surgical
patient by use of:
a. Physical examination
b. Laboratory and Diagnostic Testing
c. Evidence based medicine
6. To provide knowledge of common operative procedures, and equipment.
Student Duties
The student participates as a member of the house staff, and responsibilities include:
1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients (may include):
a. Production of a progress SOAP note in each assigned patient chart.
b. Investigation of all diagnostic studies ordered for the patient.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of pre and post-operative Osteopathic Manipulative Treatment at the
discretion of the attending surgeon.
3. Assistant within the operating room suite – aimed to:
a. Gain Surgical knot tying experience
b. Gain wound closure experience
c. Properly identify anatomic structures and provide surgical retraction for the attending
surgeon.
d. Experience methods for circulation of Surgical Tools
4. Perform essential study and preparation for each planned procedure on the attending
surgeon’s surgical schedule.
5. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
61

Related Reading
Lawrence, Peter F., Essentials of General Surgery and Surgical Specialties, 6th ed.
Ch. 1: Perioperative Evaluation and Management of Surgical Patients
Ch. 2: Fluids, Electrolytes and Acid Base Balance
Ch. 3: Surgical Nutrition
Ch. 7: Wounds and Wound Healing
Ch. 8: Surgical Infections
Gomella, Leonard G., and Steven A. Haist, Clinician’s Pocket Reference, Latest Edition
Ch. 2: Chartwork
Ch. 16: Introduction to the Operating Room
Ch. 17: Suturing Techniques and Wound Care https://www.nbome.org/exams-
assessments/comat/clinical-subjects/comat-surgery/
See also the CORE ROTATION CURRICULUM cover page in this manual.
62
OST 706: Pediatrics
Course Description
Pediatrics is a mandatory, four-week, third year core rotation. The third year osteopathic medical
student is progressed from the second year introductory pediatrics course, to experience the care
of infants, children and adolescents in the out-patient population. Common childhood diseases,
genetic and developmental disorders, preventive health care, physical examination skills, and
diagnosis and management strategies are among the rotation’s experiences.
Course Objectives
1. To provide a framework for care of the general pediatric patient.
a. The patient (parent) interview.
b. The physical examination
c. The utilization of laboratory and Diagnostic Testing
d. The utilization of evidence based medicine for diagnosis and treatment
e. The utilization of available social and medical resources for pediatric patient care, i.e.
referral decision-making.
2. To identify and apply core osteopathic principles and practices to the care of the pediatric
patient.
3. To provide a framework for preventive medical care to the pediatric population.
4. To expose students to the influences of third party insurance on medical decision-making.
5. To expose students to the influences of HIPAA and OSHA regulations on the operation
of a professional pediatric practice.
6. To gain knowledge of office procedures, their associated equipment, and laboratory
submittal requirements.
a. Phlebotomy
b. Wound repair and suture removal
c. Spirometry
d. Audiometry
e. Cerumen removal
f. Culture collection
7. To recognize developmental milestones in the pediatric population.
8. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
c. Telephone and in-person communication with other medical and health professionals
involved in common, with the care of the general pediatric patient.
63

Student Duties
1. Performance of admission histories and physicals on in-patients.
2. Completion of rounds on all in-patients including:
a. Daily examination and evaluation of clinical status
b. Production of a progress SOAP note in each assigned patient chart.
c. Investigation of all diagnostic studies ordered for the patient.
d. Production of any case summaries and/or discharge summaries for the admitted
patient.
e. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
3. Completion of “after hours” on-call duty per preceptor or hospital assignment.
4. Assist and/or perform office procedures under supervision.
5. Office set-up and performance of procedures:
a. Osteopathic Manipulative Treatment
b. Preventive health screens
c. Minor surgery
d. Preparation of laboratory specimens
6. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
Behrman, Kleigman and Jenson, Nelson Textbook of Pediatrics, Latest Edition
o Chapters 68-71: Fluid and Electrolyte Disorders
o Chapters 166-177: Allergic Disorders
o Chapters 195-330: Infectious Diseases
o Chapters 400-446: The Respiratory System
o Chapters 654-662: The Ear
Marcdante, K and R. Kliegman, H. Jenson & R. Behrman, Nelson Essentials of
Pediatrics, Latest Edition
1. Ch. 67: Overview and Assessment of Adolescents
2. Ch. 68: Well-Adolescent Care
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-pediatrics/
See also the CORE ROTATION CURRICULUM cover page in this manual.
64

OST 718: Psychiatry
Course Description
Psychiatry is a mandatory, third year, four-week core rotation, that may be served in either the
in-patient or out-patient setting. The osteopathic medical student is, under preceptor supervision,
actively engaged in the evaluation and care for the psychiatric patient. During the four weeks, the
osteopathic medical student will interview and evaluate patients, perform an admission history
and physical on all admitted patients, and develop multi-axial assessments on all patients seen.
Course Objectives
1. To develop evaluative and management skills for the care of the psychiatric patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination.
b. To perform a mental status examination
c. To become acquainted with a psychiatric diagnostic and treatment plan.
Includes understanding of the DSM Multi-Axial Classification System
d. To establish a working diagnosis with reference to The Diagnostic and Statistical
Manual IV.
Includes the medical work-up for the psychiatric patient
e. To apply core osteopathic principles and practices to the care of the psychiatric
patient.
f. To participate with available social and medical resources as part of the
comprehensive treatment plan.
g. To view the role of evidence based medicine to treatment decision-making.
h. To view the availability of services and its impact on patient care.
i. To view the effect of outside influences, e.g. third party insurance, on medical
decision-making.
j. To view the efficacy of psychotherapeutic treatment modalities, which include:
i. The mechanism of action for psychotherapeutic agents.
ii. The role of psychopharmacology, and side-effect profiles
iii. The treatment of Axis III comorbid states
iv. Awareness of procedural alternatives to chemical therapies, e.g. cognitive
treatment.
2. To gain an understanding for the operation of an in-patient psychiatric unit.
a. Examine the roles of staff and physician(s) in the delivery of healthcare. This includes
with the consent of the preceptor, attendance at group and individual treatment
sessions.
b. Know the HIPAA and OSHA regulations in regard to the operation of a psychiatric
unit.
i. Confidentiality
ii. Emergency procedures
c. The need for security measures required for the safe operation of a psychiatry
unit.
3. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
65

Student Duties
The student participates as a member of the unit staff. Responsibilities include:
1. Performance of admission histories and physicals. To include:
a. A complete mental status examination
b. A global assessment of functioning
2. Completion of rounds on all in-patients including:
a. Production of a “problem-based” progress SOAP note in each assigned patient chart.
b. Investigation and interpretation of all diagnostic studies ordered for the patient, and
be prepared to discuss findings for purposes of comprehensive care planning.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
3. Attendance at all psychiatric unit treatment sessions for assigned patients.
4. Attend and observe, with preceptor permission, family care plan meetings.
5. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
Black, Donald and Andreasen, Nancy: Introductory Textbook of Psychiatry, Latest
Edition
o Ch. 1 – Diagnosis and Classification
o Ch. 2 – Interviewing and Assessment
o Ch. 4 – Neurodevelopmental (Child) Disorders
o Ch. 6 – Mood Disorders
o Ch. 7 – Anxiety Disorders
o Ch. 15 – Substance-Related and Addictive Disorders.
o Ch. 16 – Child Psychiatry.
o Ch. 21 – Psychopharmacology and Electroconvulsive Therapy
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-psychiatry/
See also the CORE ROTATION CURRICULUM cover page in this manual.
66
OST 705: Women’s Health
Course Description
Women’s Health is a mandatory third year core rotation. The third year osteopathic medical
student is introduced to the evaluation and management of the pregnant patient, preventive care
regimens, family planning, malignancy, diagnosis and treatment of infectious diseases, urinary,
ovarian and uterine disorders, and endocrine disorders. The experience serves primarily the in-
patient woman at her time of confinement, however, may include out-patient gynecologic care
The experience may be served within a multi-practitioner service, or on the service of one
obstetrician/gynecologist.
Course Objectives
1. To provide a framework for care of the obstetrical patient.
2. To provide a framework for preventive medical care of the gynecologic patient.
3. To identify and apply core osteopathic concepts to the care of the female patient.
4. To experience the pathophysiology relevant to diseases of the breast, ovaries, urinary
bladder, and uterus, and their medical/surgical management.
5. To expose students to an evaluative approach to diagnosis and management of the adult
female patient by use of:
a. Physical examination
b. The gynecologic and medical/surgical history
c. Laboratory and Diagnostic Testing
d. Experience based medicine
6. To provide knowledge of gynecologic and obstetrical office and operative procedures,
and their associated equipment.
Student Duties
The student participates as both a member of the. host hospital’s women’s health department
service. Responsibilities include:
1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients (To include):
a. Production of a progress SOAP note in each assigned patient chart.
b. Investigation of all diagnostic studies ordered for the patient.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of Osteopathic Manipulative Treatment at the discretion of the attending
physician.
3. Assistant within the office, operating room suite and labor & delivery, and may include
some office duty.
a. Office procedures may include: Pelvic Examination
i. Breast Examination
ii. Biopsy
iii. Preparation of pathologic specimens
iv. Draping and gowning
b. Assist with the management of the Obstetrical patient during labor and delivery
c. Assist with deliveries (vaginal and C-section), as appropriate.
67

d. Assist with all gynecologic surgical procedures.
4. Essential study and preparation for each planned procedure on the attending physician’s
schedule.
5. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
Beckmann, Charles et al, Obstetrics and Gynecology, Latest Edition
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-obgyn/
See also the CORE ROTATION CURRICULUM cover page in this manual.
68

SELECTIVE ROTATION CURRICULUM
The following applies to all selective rotations:
Student Hours
Daily hours are to parallel the hours of the attending physician, however, the following
guidelines are suggested:
1. A work day may be considered 12 hours in duration.
2. A work week may be considered typically 72 hours, however, should not exceed 80 hours
in duration.
3. Maximum continuous duty should not exceed 24 hours and should be followed by a
minimum of 12 hours off duty.
4. Two days out of every 14 days should be provided as a weekend break.
Location
The physician’s office, outpatient clinic, approved hospital or medical center. See “Requisites”
specific to the Rural Medicine Selective.
Dress
At all times, KYCOM students will act as a representative of the school, and be attentive to
personal hygiene, cleanliness and personal demeanor. Short white lab coats with KYCOM
identification are expected to be worn unless specifically instructed by the hospital or preceptor.
Scrub suits are to be worn in the operating room, procedure rooms, during call hours and at the
discretion of individual physicians and/or institution/facility. At all times, however, the student
must be clearly identified as a KYCOM student. See Student Responsibilities section of this
manual for clarification.
Attendance
Prompt student attendance is expected for a minimum of 20 days for each four-week rotation
period and 10 days for each two-week rotation period. The expectation is that students work
Monday through Friday with weekends off. However, the work day will vary by rotation. If the
preceptor works weekends, the student is expected to work weekends also. The activities of each
day must be recorded on student logs for the rotation. A maximum of three (3) days for absence
is permitted, with prior approval by the associate dean for Clinical Affairs, and must be recorded
on student logs for the rotation. Absence in excess of the 3-day standard will result in an
“incomplete” for this rotation, until such time that the activity requirement is satisfied.
Absence of the attending physician or the student, from the practice for a period greater than one
day, requires the student to notify the office for Clinical Affairs, of the interruption of activity.
At the discretion of the associate dean for Clinical Affairs either a reading assignment or
alternate duty assignment will be made.
Lectures and Meetings
It is the responsibility of the student to be familiar with the hospital’s didactic lecture schedule,
and to document attendance within the student log. Didactic programs include but are not limited
to: Morning Report, Journal Club, Morbidity/Mortality Conference, Grand Rounds, and Noon
69

Conference. Absence from any of these events requires the signature of the preceptor, and should
be sent with the student log reports to KYCOM. It is expected that the student will attend a
minimum of 70% of each kind of event.
Grading
The KYCOM Student Assessment Form for CORE rotations, which is completed by the
attending physician, comprises 50% of the rotation grade. The COMAT examination score
comprises the balance of the grade. Upon receipt and review of all information, the associate
dean for Clinical Affairs evaluates the material, and assigns a numerical grade, as per the
Clinical Rotations Manual, Student Evaluation (Grade). The evaluation is intended to measure
the student in comparison to others at the same level of education.
The KYCOM Student Assessment Form measures:
1. Mastery of Osteopathic Philosophy and Application of Manipulative Medicine
2. Medical Knowledge
3. Patient Care
4. Interpersonal and Communication Skills
5. Professionalism
6. Application of Practice Based Learning Skills
7. Application of Systems Approach to Medicine
Challenge of Grades
Any challenges or questions are to be directed to the associate dean for Clinical Affairs. The
student has the right for review of the challenge by the Promotions and Matriculation
Committee, if the associate dean’s response requires further clarification.
Remediation
In cases where a passing grade is not achieved, if deemed appropriate by the Promotions &
Matriculation Committee, the student will be given the opportunity to repeat the rotation. Upon
successful completion of the repeated rotation, a maximum grade of 70% will be recorded on
the student transcript.
70
OST 804 Emergency Medicine Selective
Course Description
Emergency Medicine is a mandatory, four-week, hospital based, third or fourth year selective
rotation that affords the medical student the opportunity to learn in an Emergency Medicine
setting. The osteopathic medical student, under the supervision of an emergency medicine
specialist, sees the essentials of Emergency Medicine through observation and performance of
clinical procedures, hands on clinical experiences and direct interaction with faculty, individual
patients, and families. Integration of clinical skills and evidence-based medicine is achieved
with emphasis on didactic discussions, and development of clinical skills.
Pre-requisites: General Internal Medicine I, General Internal Medicine II, Family
Medicine I, General Surgery, Pediatrics, and Woman’s Health
Course Objectives
1. To integrate osteopathic principles and practice concepts into the conventional care of
emergency patients
2. To experience case management and the coordination of systems based medical care.
a. The use of subspecialists and other medical/surgical disciplines.
b. The use of social services and outpatient programs
c. The use of in-house care services.
d. To recognize the social and economic factors that affect patient care.
3. To employ the knowledge, attitudes, and skills necessary to provide preventive, episodic,
or continuing care to individual patients in an emergency medicine setting
4. To experience prioritization skills.
5. To learn assessment skills for classification of the type, level and urgency of care needed
for the particular patient encounter.
6. To integrate the utilization of appropriate health maintenance screening protocols into
emergency medicine care.
7. To demonstrate the ability to assess a patient and differentiate the need for urgent versus
non-urgent care.
8. For students to experience the practice of evidence-based medicine.
a. To assess, apply, and assimilate investigative knowledge to improve patient care.
b. To realize the Emergency Medicine physician’s role in the community and Society.
c. To cite and communicate information in an organized and succinct manner
9. For students to respect and be sensitive to the individuality, values, goals, concerns, and
rights of all with whom they interact in the healthcare setting.
10. Demonstrate understanding of ethical principles of autonomy, beneficence, informed
consent, and confidentiality.
11. To accomplish the use of effective written, and verbal language skills.
Student Duties
1. Performance of bedside assessment and physical examination
a. Production of a problems based progress note.
b. Be prepared to suggest a diagnostic and treatment plan with a differential diagnosis
basis.
71

2. Performance of bedside procedures.
a. Placement of catheters
b. Electrocardiography
c. Suturing and simple wound care
d. Assist with cardiopulmonary resuscitation under supervision.
e. Phlebotomy
f. Performance of OMT as deemed appropriate by supervising physician
g. Casting of simple fractures under supervision.
3. Performance of after-hours call.
4. Attendance at hospital conferences.
5. Completion of an “End of Service” examination (COMAT) administered by the National
Board of Osteopathic Medical Examiners, during the fourth week of the rotation.
Related Reading
Case Files Emergency Medicine, Lange case files
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-emergency-
medicine/
Suggested Topics to Review
Chest Pain - UA, NSTEMI, STEMI, Thoracic Aortic Aneurysm, Pulmonary Embolism, Acute
Exacerbation Of COPD, Asthma, CHF, AFIB, HTN Urgency And Emergency, Pneumonia -
HCAP, CAP, Stroke, Dizziness, Bell’s Palsy, Headache, Seizure, Musculoskeletal Pain - Neck
Pain, Back Pain, Acute Injuries Like Ankle/Knee Sprain, Shoulder Pain, Fracture Evaluation
And Management, Hip Fracture, Abdominal Pain - Appendicitis, Cholecystitis, Pancreatitis,
Diverticulitis, Pyelonephritis, Gastroenteritis, UTI, Kidney Stone, Gastric/Duodenal Ulcers,
Small Bowel Obstruction, Ileus, Mesenteric Ischemia, GI Bleed, AAA, OB/Gyn - Vaginal
Bleeding, Vaginal Discharge, Miscarriage, Pregnancy Management, Ovarian Cyst/Torsion
Prostatitis, Orchitis, Testicular Torsion, Epididymitis, ACLS, ATLS - Trauma Evaluation -
Primary Survey and Secondary Survey, Burns, DKA, Laceration Care, SIRS/Sepsis, Meningitis,
Alcohol and Other Drug Intoxication/Withdrawal/Overdose
See also the SELECTIVE ROTATION CURRICULUM cover page in this manual.
72
Medicine Selective Guidelines
Course Description
The medical selective is a four-week clinical rotation that may be served with subspecialists from
the general fields of family medicine, internal medicine, or pediatrics. The osteopathic medical
student is given the opportunity to observe and participate in the management and care of
patients referred for specialty consultation. The experience can serve either the in-patient or out-
patient population. Suggested areas of study may include:
Cardiology
Dermatology
Endocrinology
Gastroenterology
Hematology/Oncology
Infectious Diseases
Nephrology
Pulmonary Medicine
Radiology
Prerequisites: Completion of Internal Medicine I, Family Medicine I and Pediatrics
Course Objectives
1. To recognize the role of the medical specialist in the general management of the adult or
pediatric patient.
2. To provide a framework for the:
a. Criteria to be considered/information needed, when specialty consultation is
contemplated.
b. Evaluation and management of adult or pediatric medical disorders.
c. Communication process between the primary care physician and the specialty
physician.
3. To experience atypical pathophysiologies and their diagnostic work-up
4. To utilize evidence based medicine
Student Duties
The student participates as both a member of the hospital house staff and office staff.
Responsibilities include:
1. Performance of histories and physicals
2. Completion of rounds on all in-patients (To include):
a. Production of a progress SOAP note in each assigned patient chart.
b. Investigation of all diagnostic studies ordered for the patient.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of Osteopathic Manipulative Treatment at the discretion of the attending
physician.
3. Assistant within the office and/or procedure room suite
4. Essential study and preparation for each planned procedure on the attending physician’s
schedule.
See also the SELECTIVE ROTATION CURRICULUM cover page in this manual.
73

OST 865: Radiology
Course Description
Radiology may be a two or four-week clinical rotation. The Radiology rotation can fulfill the
medical selective requirement or can serve as elective time. It can be served with a radiologist
within the following areas: general diagnostic radiology, pediatric radiology, vascular and
interventional radiology, nuclear radiology, or neurological radiology. The osteopathic medical
student is given the opportunity to observe and perhaps participate in the interpretation,
performance and care of patients referred for imaging, and/or consultation. The experience can
serve either the in-patient or out-patient population. Suggested areas of study may include:
Computed Tomography of the Head, Neck, Abdomen & Axial Skeleton
Magnetic Resonance Imaging of Neural and Vascular Structures
Diagnostic Ultrasound of vascular structures, abdomen and pelvis
Screening or Diagnostic Mammography
Nuclear Radiology for Endocrine, Vascular and Skeletal Diagnosis
Prerequisites: General Internal Medicine I or Family Medicine I, Women’s Health,
Pediatrics & General Surgery.
Course Objectives
1. To recognize the role of the radiologist in the general management of the adult or
pediatric medical/surgical patient.
2. To develop an understanding of the influences that third party insurances have on
medical/surgical decision-making, and the choice and/or necessity for medical/surgical
imaging.
3. To experience the criteria to be considered, when radiology consultation is contemplated.
4. To experience the information needed from the ordering physician for the optimal
interpretation of diagnostic studies ordered for medical/surgical patients.
5. To experience the role of the radiologist in the Evaluation and Management of adult or
pediatric medical/surgical disorders.
6. To experience atypical pathophysiologies and their diagnostic work-up
7. To expand personal interpretation skills.
8. To see how outcomes evidence serves as the basis for consultant recommendations.
Student Duties
The student participates as both an observer and an assistant within the Radiology Suite.
Responsibilities may include:
1. Performance of patient histories
2. Review of outcomes on preceptor selected in-patients. This may include:
a. Investigation of all diagnostic studies ordered for the patient.
b. Participation in case reviews, e.g. Morbidity & Mortality Conference
3. Assist within the procedure room suite
4. Essential study and preparation for each planned radiologic procedure on preceptor’s
schedule.
5. Preparation for daily and/or weekly recitation, which may include, self-interpretation of
studies under preceptor supervision, review of recent cases or discussion of preceptor
reading assignments.
74
Suggested Reading
• Holmes, Erskine, J.; Forrest-Hay, Anna C.; Misra, Rakesh R.: Interpretation of
Emergency Head CT: A Practical Handbook, Cambridge University Press, Latest
Edition.
• Mirvis, Stuart E; Shanmuganathan, K.; Miller, Lisa A.; Sliker, C.W.: Emergency
Radiology: Case Review Series, Mosby, Latest Edition.
• Novelline, Robert A.: Squire’s Fundamentals of Radiology, Harvard University Press,
Latest Edition.
See also the SELECTIVE ROTATION CURRICULUM cover page in this manual.
75

OST 809: Rural Medicine
Course Description
Rural Medicine is a mandatory primary care selective rotation, and is four weeks in duration. It is
an upper level third or fourth year course that may be served preferably in an office based
setting, however, can be accomplished in a hospital out-patient clinic. The osteopathic medical
student is, under preceptor supervision, actively engaged in both the care and the medical
decision-making for the delivery of the healthcare needs to the out-patient population. During the
four weeks, the osteopathic medical student will evaluate patients, develop comprehensive care
plans and experience the responsibilities and challenges associated with physician care in a
medically underserved area. For more information visit this website:
https://data.hrsa.gov/tools/shortage-area/by-address
Requisites: Community Population < 5000 people, Nearest Full Service Hospital > 50 miles,
Local Hospital Bed Capacity < 100 beds, and Preceptor Specialty may include Family Medicine,
Internal Medicine, Pediatrics, or Women’s Health.
Prerequisites: Family Medicine I, Family Medicine II, General Internal Medicine I, Pediatrics,
General Surgery I, and Women’s Health
Course Objectives
1. To experience the unique challenges of medical practice in a medically underserved area.
2. To apply the knowledge, skill sets, experience, values, and behaviors seen previously in
more structured settings, to meet the needs of the region served.
3. To utilize practice skills, supported by the best available medical evidence, that serve the
best interest, well-being and health of the patient.
4. To demonstrate competency in primary care medicine.
5. To develop efficient and complete evaluative and management skills for the care of the
general medical or surgical patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination and to include preventive medical care for all age groups
b. To establish a working diagnosis and see the challenges associated with the
implementation of the treatment plan.
c. To apply core osteopathic principles and practices to the care of the general medical
or surgical patient.
d. To coordinate available social and medical resources as part of the comprehensive
treatment plan.
6. To develop an understanding of the operation of a rural health facility.
a. Examine the roles of staff and physician(s) in the delivery of healthcare.
b. Develop an understanding of the influences that third party insurances have on
medical decision-making.
c. Develop an inventory of necessary property and supplies for the daily operation of a
rural medical practice.
7. To continue development of written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
76
c. The production of electronic medical records, where appropriate.
d. Telephone and in-person communication with other medical and health professionals
involved in common, with the care of the general medical patient.
Student Duties
Student responsibilities include:
1. Performance of histories and physicals
2. Develop treatment plans on each assigned patient for purposes of comprehensive care
planning.
3. Perform proposed care plans, and develop self-evaluative tools to assess efficacy of
regimen.
a. Interpretation of all diagnostic studies ordered for treated patients.
b. Follow-up with all consultants on assigned patients.
c. Production of any case summaries and/or discharge summaries for assigned patients.
d. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
4. Assist and/or perform duties and procedures under supervision.
a. Office set-up and performance of procedures:
i. Osteopathic Manipulative Treatment
ii. Preventive health screens
iii. Minor surgery
b. Attend and observe family meetings when appropriate
c. Evaluate patients in the emergency department
i. Write admit orders
ii. Develop a care plan
iii. Request consultation(s)
d. Assistance or Performance of Procedures within local hospital procedure room.
i. Surgery
ii. Wound Repair
iii. Line insertion/Removal
See also the SELECTIVE ROTATION CURRICULUM cover page in this manual.
77
Surgery Selective Guidelines
Course Description
The surgery selective is a hospital based, four-week clinical rotation that may be served with the
subspecialists from the surgery field. The fourth year osteopathic medical student is engaged to
exercise diagnostic skills to evaluate the surgical patient, hone surgical skills as an assistant in
the operating room suite, and develop an appreciation for evidence based surgical care criteria.
Assignments are inter-disciplinary, and subject to the operative schedule. Suggested surgical
departments may include:
Colorectal
Urologic
Head & neck
Cardiovascular
Peripheral-vascular
Thoracic
Neurosurgery
Prerequisite: General Surgery
Course Objectives
1. To provide a framework for care of the surgical patient, which include:
a. Principles of Nutrition
b. Use of Osteopathic Manipulative Treatment
c. Principles of hydration
d. Infectious disease considerations
e. Thrombosis prevention
f. Airway management
g. Physical activity guidelines
h. Applications of evidence based surgical care criteria
i. Utilization of diagnostic imaging and the laboratory
2. To experience the pathophysiology relevant to affected organ systems, and the efficacy of
surgical care.
3. To provide knowledge and experience with the performance of bedside procedures, which
may include:
a. Placement of central venous catheters
b. Placement of gastrointestinal catheters
c. Placement of Urinary catheters
d. Removal of sutures and catheters
e. Wound care
f. Ostomy care
4. To provide knowledge and experience as an operative assistant with operative procedures, and
their associated equipment.
Student Duties
The student participates as a member of the house staff, and responsibilities include:
78

1. Performance of admission histories and physicals
2. Completion of rounds on all in-patients (may include):
a. Production of a SOAP note in each assigned patient chart.
b. Investigation of all diagnostic studies ordered for the patient.
c. Production of any case summaries and/or discharge summaries for the admitted patient.
d. Performance of pre and post-operative Osteopathic Manipulative Treatment at the
discretion of the attending surgeon.
e. Performance of bedside procedures as outlined above.
3. Assistant within the operating room suite
a. The student must be gowned, gloved and positioned at bedside, within the sterile field for
all surgical procedures.
b. The student must have reviewed the surgical procedure a priori, and be prepared to
outline the operative goals, and anatomical landmarks.
c. The student should be prepared to close surgical wounds with use of accepted knot tying
techniques.
4. Conduct essential study and preparation for each planned procedure on the attending surgeon’s
surgical schedule.
Related Reading
https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-surgery/
See also the SELECTIVE ROTATION CURRICULUM cover page in this manual.
79
ELECTIVE ROTATION CURRICULUM
The following applies to all elective rotations:
Student Hours
Daily hours are to parallel the hours of the attending physician, however, the following
guidelines are suggested:
1. A work day may be considered 12 hours in duration.
2. A work week may be considered typically 72 hours, however, should not exceed
80 hours in duration.
3. Maximum continuous duty should not exceed 24 hours and should be followed
by a minimum of 12 hours off duty.
4. Two days out of every 14 days should be provided as a weekend break.
Location
The physician’s office and the participating locations where the preceptor provides care.
Dress
At all times, KYCOM students will act as a representative of the school, and be
attentive to personal hygiene, cleanliness and personal demeanor. Short white lab
coats with KYCOM identification are expected to be worn unless specifically
instructed by the hospital or preceptor. Scrub suits are to be worn in the operating
room, procedure rooms, during call hours and at the discretion of individual
physicians and/or institution/facility. At all times, however, the student must be
clearly identified as a KYCOM student. See Student Responsibilities section 8.a. of
this manual for clarification.
Attendance
1. Prompt student attendance is expected for the a minimum of 20 days each four-week
rotation period and 10 days each two-week rotation period. The expectation is that
students work Monday through Friday with weekends off. However, the work day will
vary by rotation. If the preceptor works weekends, the student is expected to work
weekends also. The activities of each day must be recorded on student logs for the
rotation. A maximum of three (3) days for absence is permitted, with prior approval by
the associate dean for Clinical Affairs, and must be recorded on student logs for the
rotation. Absence in excess of the 3-day standard will result in an “incomplete” for this
rotation, until such time that the activity requirement is satisfied.
2. Absence of the attending physician, or the student, from the practice for a period greater
than one day, requires the student to notify the office for Clinical Affairs, of the
interruption of activity. At the discretion of the associate dean for Clinical Affairs either a
reading assignment or alternate duty assignment will be made.
3. Lectures and Meetings
Grading
The basis for the rotation grade is the KYCOM Student Assessment Form for Selective/Elective
Rotations, which is completed by the attending physician. Upon receipt and review of all
80
information, the associate dean for clinical affairs evaluates the material, and assigns a numerical
grade. A grade of 70% is considered passing, as per the Clinical Rotations Manual. The
evaluation is intended to measure the student in comparison to others at the same level of
education.
The KYCOM Student Assessment Form measures:
1. Mastery of Osteopathic Philosophy and Application of Manipulative Medicine
2. Medical Knowledge
3. Patient Care
4. Interpersonal and Communication Skills
5. Professionalism
6. Application of Practice Based Learning Skills
7. Application of Systems Approach to Medicine
Challenge of Grades
Any challenges or questions are to be directed to the associate dean for Clinical Affairs. The
student has the right for review of the challenge by the Promotions and Matriculation
Committee, if the associate dean’s response requires further clarification.
Remediation
In cases where a passing grade is not achieved, if deemed appropriate by the Promotions &
Matriculation Committee, the student will be given the opportunity to repeat the rotation. Upon
successful completion of the repeated rotation, a maximum grade of 70% will be recorded on
the student transcript.
81
OST 808: Addiction Medicine
Course Description
Addiction Medicine is an elective, third or fourth year medical student, four-week rotation,
served primarily in an in-patient setting. The elective is intended for the osteopathic medical
student to experience the reality of the physician-patient relationship through an active and
observational clinical experience. The osteopathic medical student is, under preceptor
supervision, and actively engaged in the evaluation and care for both the hospitalized and
ambulatory patient. During the four weeks, the osteopathic medical student will interview and
evaluate patients, perform an admission history and physical on all admitted patients, and
develop assessments and care plans on all patients seen.
Course Objectives
1. To develop evaluative and management skills for the care of the patient with addiction,
through observation and interaction with physicians in a real world environment.
a. To conduct an age, gender and problem associated patient interview and physical
examination.
b. To perform a mental status examination
c. To demonstrate effective communication and interaction with patients and families
with a broad range of demographic, socioeconomic, ethnic, cultural, and religious
backgrounds and to develop effective skills in interviewing and data-gathering, and
demonstrate empathic attunement and boundary establishment. To allow the student
to experience the development of those important communication skills while
interacting with physicians, support staff, and patients.
d. To conduct a comprehensive diagnostic assessment and treatment formulation, and
view the role of evidence based medicine to treatment decision-making.
e. To apply core osteopathic principles and practices to the care of the patient with
addiction.
f. To participate with available social and medical resources as part of the
comprehensive treatment plan.
g. To view the availability of support services and its impact on patient care.
h. To view the effect of outside influences, e.g. third party insurance, on medical
decision-making.
i. To view routine detoxification protocols, both inpatient and outpatient, and smoking
cessation approaches.
j. To demonstrate knowledge about the variety of psychopharmacological,
psychotherapeutic, group, religious, and residential treatments.
k. To view the efficacy of psychotherapeutic treatment modalities, which include:
The mechanism of action for psychotherapeutic agents.
The role of psychopharmacology, and side-effect profiles.
Maintenance drug therapies, which include naltrexone, buprenorphine,
methadone, disulfiram, acamprosate, and nicotine replacements.
l. To allow students to understand the construction of treatment plans.
2. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
82
Related Reading
Black, Donald and Andreasen, Nancy: Introductory Textbook of Psychiatry, Latest Edition
Ch. 2 – Interviewing and Assessment
Ch. 15 – Substance-Releated and Addictive Disorders
Ch. 21 – Psychopharmacology and Electroconvulsive Therapy
Principles of Addiction Medicine: The Essentials, https://go.openathens.net/redirector/upike.edu?
url=https%3A%2F%2Fclerkship.lwwhealthlibrary.com%2Fbook.aspx%3Fbookid%3D1276
Student Duties
The student participates as a member of the unit staff. Responsibilities include:
1. Performance of admission histories and physicals. To include:
a. A complete mental status examination
b. A global assessment of functioning
2. Completion of rounds on all in-patients including:
a. Production of a “problem-based” progress SOAP note in each assigned patient chart.
b. Investigation and interpretation of all diagnostic studies ordered for the patient, and
be prepared to discuss findings for purposes of comprehensive care planning.
c. Production of any case summaries and/or discharge summaries for the admitted
patient.
d. Performance of Osteopathic Manipulative Treatment under the direction of the
attending physician.
3. Attendance at all treatment sessions for assigned patients.
4. Attend and observe, with preceptor permission, family care plan meetings.
See also the ELECTIVE ROTATION CURRICULUM cover page in this manual.
83
OST 897: Research
Course Description
Prerequisites: All Core Rotations
Complete the Research Elective Form found in the back of your manual.
Attach a brief description of the project, detailing your study and what you wish to
accomplish. This should include an overview of the hypothesis, the methods that will be
employed, and the expected outcomes and analytic methods that will be used. Specific details
of the student role in the proposed project should be outlined. The osteopathic medical
student must present the goals, objectives and expectations of the rotation to the Associate
Dean of Clinical Affairs to obtain approval before the rotation will begin. The student must
present the research request form and outline for the project at least 30 days prior to the start
of the rotation.
Attach a statement asserting that the amount of time spent in the lab/etc. on your research
project will be greater than and or equal to 40 hours per week.
The research rotation length must be a minimum of 2 weeks but no more than 4 weeks. The
purpose of the research rotation is to allow the student an opportunity to engage in clinical or
bench research, to learn the principles of research, study, design and data analysis.
The principal teaching method of the research rotation will be participation in a structured
research activity with supervision and assistance provided by an experienced, approved
faculty or preceptor.
At the conclusion of the rotation a brief narrative of the research activities and outcome
results must be submitted to the Associate Dean of Clinical Affairs. Upon receipt, review,
and evaluation of all material and information, a Pass/Fail grade shall be assigned by the
Associate Dean of Clinical Affairs.
84
OST 896: International Rotation
Course Description
This international rotation is a four-week fourth year rotation that is completed in an outpatient
or inpatient setting. The osteopathic medical student is, under preceptor supervision, actively
engaged in both the care and the medical decision-making for the delivery of the healthcare
needs to the out-patient population. During the four weeks, the osteopathic medical student will
evaluate patients, develop comprehensive care plans and experience the responsibilities and
challenges associated with physician care in a medically underserved area. A maximum of eight
weeks may be completed on an international rotation. See the U.S. Department of State website
for travel advisory levels. Only Level 1 or Level 2 travel advisory areas will be approved.
Prerequisites: Family Medicine I, Family Medicine II, General Internal Medicine I,
General Surgery I, Pediatrics, and Women’s Health
Course Objectives
1. To experience the unique challenges of medical practice in a medically
underserved international area.
2. To apply the knowledge, skill sets, experience, values, and behaviors seen
previously in a more structured settings, to meet the needs of the region served.
3. Recognize cultural and regional influences that affect access to, implementation,
and effectiveness of medical care.
4. To utilize practice skills, supported by the best available medical evidence, that
serve the best interest, well-being and health of the patient.
5. To demonstrate competency in primary care medicine.
6. To develop efficient and complete evaluative and management skills for the care
of the general medical patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination and to include preventive medical care for all age groups
b. To establish a working diagnosis and see the challenges associated with the
implementation of the treatment plan.
c. To apply core osteopathic principles and practices to the care of the general
medical patient.
d. To coordinate available social and medical resources as part of the comprehensive
treatment plan.
7. To develop an understanding of the operation of an international health facility.
a. Examine the roles of staff and physician(s) in the delivery of healthcare.
b. Develop an understanding of the influences that national health insurances and
mission organizations have on medical decision-making.
c. Develop an inventory of necessary property and supplies for the daily operation of
an international medical clinic.
8. To continue development of written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
c. The production of electronic medical records, where appropriate.
85
d. Telephone and in-person communication with other medical and health
professionals involved in common, with the care of the general medical patient.
e. Recognize unique challenges to care when providing care in a non-native
language, using interpreters, and utilizing non-medical providers in medical
situations.
Student Hours
About 25% of rotation time (at discretion and approval by Associate Dean for
Clinical Affairs and clinical preceptor) may be spent in preparation for in country
experience including language familiarity, review of country/region specific medical
problems, review of public health policies for the country/region, and preparation of
a research project related to this international rotation.
Student Duties
Student responsibilities include:
1. Performance of histories and physicals
2. Develop treatment plans on each assigned patient for purposes of comprehensive
care planning.
3. Perform proposed care plans, and develop self-evaluative tools to assess efficacy
of regimen.
a. Interpretation of all diagnostic studies ordered for treated patients.
b. Follow-up with all consultants on assigned patients.
c. Production of any case summaries and/or discharge summaries for assigned
patients.
d. Performance of Osteopathic Manipulative Treatment under the direction of
the attending physician.
4. Assist and/or perform duties and procedures under supervision.
a. Office set-up and performance of procedures:
b. Osteopathic Manipulative Treatment
c. Preventive health screens
d. Minor surgery
e. Attend and observe family meetings when appropriate.
5. Complete a case presentation in written form
6. The presentation will be delivered in a professional manner, in the following order:
a. Patient Identifier (__ is a __ y.o. “race,” “gender”)
b. Subjective patient presentation (Paint The Scene)
c. History of chief complaint
d. PMH/PSH
e. Social and Family History
f. Obstetrical and Gynecologic history if applicable
g. Medication List (include dosage and regimen)
h. Allergies (include reaction)
i. Physical Exam (Description of Major Related Findings)
j. Labs and Imaging
k. Differential Diagnosis
l. Patient Outcome
86
m. Case Discussion – include unique aspects of the case relevant to presentation in
this international context.
See also the ELECTIVE ROTATION CURRICULUM cover page in this manual.
87
ONLINE/VIRTUAL ROTATION CURRICULUM
88
ONLINE/VIRTUAL ROTATION CURRICULUM
The following applies to all online/virtual rotations:
Student Hours
The student will be expected to devote at least 40 hours per week for online rotations.
Attendance
Prompt student attendance is expected for the a minimum of 20 days each four-week rotation
period and 10 days each two-week rotation period. The expectation is that students work
Monday through Friday with weekends off. The activities of each day must be recorded on
student logs for the rotation. A maximum of three (3) days for absence is permitted, with
prior approval by the Associate Dean for Clinical Affairs, and must be recorded on student
logs for the rotation. Absence in excess of the 3-day standard will result in an “incomplete”
for this rotation, until such time that the activity requirement is satisfied.
Grading
The basis for the rotation grade is reported as Pass/Fail.
Challenge of Grades
Any challenges or questions are to be directed to the Associate Dean for Clinical Affairs. The
student has the right for review of the challenge by the Promotions and Matriculation
Committee, if the Associate Dean’s response requires further clarification.
Remediation
In cases where a passing grade is not achieved, if deemed appropriate by the Promotions &
Matriculation Committee, the student will be given the opportunity to repeat the rotation. Upon
successful completion of the repeated rotation, a maximum grade of 70% will be recorded on
the student transcript.
89
OST 708: Family Medicine I Online
Course Description
Family Medicine I is a four-week, third-year core clinical experience. The third-year osteopathic
medical student is progressed from the clinical courses introduced during the two pre-clinical
years to their application in patient care. Preventive care, family planning, end of life care, acute
and chronic care, applied across all age groups, are among the many experiences gained over the
four weeks.
Course Objectives
1. To provide a framework for care of the general medical patient.
a. To develop and apply interviewing skills to the patient encounter, as a means to both
solidify physician-patient relationships and produce preliminary differential
diagnosis.
b. To utilize physical examination skills to progress from preliminary differential
diagnosis to a probable differential diagnosis and the development of a diagnostic and
treatment plan.
c. To experience the evolution of a diagnostic plan, and the establishment of a working
diagnosis and its associated treatment plan.
d. To identify and apply core osteopathic principles and practices to the care of the
general medical patient
e. To identify available social and medical resources and the family physician’s role in
their coordination to patient care, i.e. referral decision-making.
f. To view the role of experience based medicine to medical decision-making.
2. To provide a framework for preventive medical care to all age groups.
3. To expose students to the operation of a professional office:
a. The roles of staff and physician(s) in the delivery of healthcare.
b. The influences of third party insurance and medical decision-making.
c. Care and recording of medical records.
d. The roles of the “International Classification of Diseases” and “Current Procedural
Terminology” and their impact on physician reimbursement.
e. The role of the telephone, and other electronic communication tools in the delivery of
healthcare.
f. Awareness of physician responsibilities under HIPAA and OSHA regulations.
4. To provide knowledge of office procedures, their associated equipment, and laboratory
submittal requirements.
a. Phlebotomy
b. Wound repair and suture removal
c. Electrocardiography
d. Spirometry
e. Audiometry
f. Screening examinations of the male and female breast
g. The anal, rectal and prostate examination
h. The female internal examination
5. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
90

b. The production of a written and/or dictated encounter progress note.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
family-medicine/
E*Value Summaries
COMAT Exam
Related Reading
THE WASHINGTON MANUAL® OF MEDICAL THERAPEUTICS, 36th Edition
https://bookshelf.vitalsource.com/#/books/9781496361363/cfi/6/2[;vnd.vst.idref=Bhat_Cover.xh
tml]!
See also
the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
91
OST 709: Family Medicine II Online
Course Description
Family Medicine II is a third year four-week core clinical experience During the four weeks, the
osteopathic medical student will evaluate patients, develop comprehensive care plans and
experience the responsibilities associated with physician actions.
Prerequisite: Family Medicine I
Course Objectives
1. To develop efficient and complete evaluative and management skills for the care of the
general medical patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination, while including preventive medical care for all age groups.
b. To formulate and test preliminary differential diagnosis during the physical
examination.
c. To develop a diagnostic and treatment plan.
d. To establish a working diagnosis and the challenges associated with the
implementation of the treatment plan.
e. To apply core osteopathic principles and practices to the care of the general medical
patient.
f. To coordinate available social and medical resources as part of the comprehensive
treatment plan.
g. To, under preceptor supervision, take the family physician’s role in referral decision-
making.
iv. To view the role of experience based medicine to medical decision-making.
v. To view the availability of services and its impact on patient care.
vi. To view the effect of outside influences, e.g. third party insurance, on medical
decision-making.
2. To develop a model for the operation of a professional office:
a. Examine the roles of staff and physician(s) in the delivery of healthcare. This may
include, with the consent of the preceptor, attendance at office staff meetings.
b. Develop an understanding of the influences that third party insurances have on
medical decision-making.
c. Understand the laws that govern the care and recording of medical records.
d. Gain a working knowledge of the “International Classification of Diseases” and
“Current Procedural Terminology” and their impact on physician reimbursement.
e. Examine the telephone system, and other electronic communication tools in relation
to the delivery of healthcare.
f. Know the HIPAA and OSHA regulations in regard to the operation of a professional
medical practice.
iv. Confidentiality
v. Hazardous waste removal
vi. Emergency procedures
g. To develop an inventory of necessary property and supplies for the daily operation of
a general medical practice.
92
3. To continue development of written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-family-
medicine/
E*Value Summaries
COMAT Exam
Related Reading
Seidel’s Guide to Physical Examination, 9
th
Edition
https://bookshelf.vitalsource.com/#/books/9780323112406/cfi/6/2!/4/2@0:0
Textbook of Family Medicine, 9
th
Edition
https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20130000850
Clinician's Pocket Reference, 11
th
Edition
htt
ps:/
/l
ibg
uides.li
bra
r
y
.upike.edu/c.php?g=970657&p=7014938
See also
the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
93
OST 720: General Internal Medicine I Online
Course Description
General Internal Medicine I is four-week third year core clinical experience. The
pathophysiology of cardiovascular, cerebrovascular, pulmonary, renal, gastrointestinal and
endocrine disorders are among the patient population seen.
Course Objectives
1. To develop age and gender specific, problem oriented history and physical examination
skills.
2. To learn effective communication skills.
a. The focused patient interview
b. Peer case presentation techniques
c. Production of coherent admission, progress, and discharge notes
3. To correlate information gained from the patient’s chief complaint, medical, surgical,
social, and familial histories with the signs and symptoms seen on examination to
develop differential diagnoses in order of likelihood.
4. To appreciate the role that experience based medicine plays in the management of the
medical patient.
5. To appreciate the need for preventive medical care as part of the total treatment regimen
for the medical patient.
6. To learn the principles of the production and implementation of a total treatment plan.
7. To expose students to the operation of a hospital.
a. The hospital laboratory
b. The radiology department
c. The nursing staff and patient care management.
d. The physical, occupational, speech, and respiratory therapy teams.
e. The social services department
f. The strict observance of HIPAA and OSHA regulations.
g. The coordination of patient care.
8. To provide practical procedural knowledge:
a. Phlebotomy and arterial blood gases
b. Insertion of nasogastric tubes
c. Insertion of urinary catheters
d. Insertion of central vascular catheters
e. Electrocardiography
f. The rectal examination
g. Cardiovascular resuscitation
h. Lumbar spinal puncture
i. Culture of blood, body fluid and soft tissues
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
94

o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
internal-medicine/
E*Value Summaries
COMAT Exam
Related Reading
Harrison's Principles of Internal Medicine, 20
th
Edition
https://bookshelf.vitalsource.com/#/books/9780071802161/cfi/6/2!/4/2@0:0
See also the CORE ROTATION CURRICULUM cover page in this manual.
95

OST 721: General Internal Medicine II Online
Course Description
General Internal Medicine II is a four-week core clinical experience. The osteopathic medical
student is encouraged to incorporate evaluative skills, and evidence based medical information,
to develop a comprehensive treatment regimen based on logical medical decision-making.
Pre-requisite: General Internal Medicine I
Course Objectives
1. To experience the responsibilities of an intern or resident.
2. To experience case management and the coordination of systems based medical care.
a. The use of subspecialists and other medical/surgical disciplines.
b. The use of social services and outpatient programs
c. The use of physical therapy
d. The use of in-house care services.
3. To produce and implement a total treatment plan.
4. To experience prioritization skills.
5. To develop a problem oriented approach to patient care.
6. To develop a sense of cost-effective medical care.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
internal-medicine/
E*Value Summaries
COMAT Exam
Related Readings
Harrison's Principles of Internal Medicine, 20
th
Edition
https://bookshelf.vitalsource.com/#/books/9780071802161/cfi/6/2!/4/2@0:0
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
96
OST 740: General Surgery Online
Course Description
General Surgery Online is a third year clinical experience designed to introduce the student to
the department of surgery.
Course Objectives
1. To provide a framework for care of the surgical patient.
2. To provide a review of:
a. Asceptic technique
b. Gowning and gloving
c. Methods for entry/departure from the surgical theatre
3. To identify and apply core osteopathic concepts to the care of the surgical patient.
4. To experience the pathophysiology relevant to affected organ systems, and the efficacy of
surgical care.
5. To expose students to an evaluative approach to diagnosis and management of the surgical
patient by use of:
a. Physical examination
b. Laboratory and Diagnostic Testing
c. Evidence based medicine
6. To provide knowledge of common operative procedures, and equipment.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
surgery/
E*Value Summaries
COMAT Exam
Related Reading
Essentials of General Surgery & Surgical Specialties, 6
th
Edition
https://bookshelf.vitalsource.com/#/books/9781975107123/cfi/6/2!/4/[email protected]:0.00
Essentials of General Surgery, 5
th
Edition
https://bookshelf.vitalsource.com/#/books/9781469819181/cfi/6/2!/4/2@0:0
Clinician's Pocket Reference, 11
th
Edition
https://libguides.libra
ry.upike.edu/c.php?g=970657&p=7014938
See also
the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
97

OST 706: Pediatrics Online
Course Description
Pediatrics is a four-week, third year core clinical experience. The third year osteopathic medical
student is progressed from the second year introductory pediatrics course, to experience the care
of infants, children and adolescents. Common childhood diseases, genetic and developmental
disorders, preventive health care, and diagnosis and management strategies are among the
rotation’s experiences.
Course Objectives
1. To provide a framework for care of the general pediatric patient.
a. The patient (parent) interview.
b. The physical examination
c. The utilization of laboratory and Diagnostic Testing
d. The utilization of evidence based medicine for diagnosis and treatment
e. The utilization of available social and medical resources for pediatric patient care, i.e.
referral decision-making.
2. To identify and apply core osteopathic principles and practices to the care of the pediatric
patient.
3. To provide a framework for preventive medical care to the pediatric population.
4. To expose students to the influences of third party insurance on medical decision-making.
5. To expose students to the influences of HIPAA and OSHA regulations on the operation
of a professional pediatric practice.
6. To gain knowledge of laboratory submittal requirements.
a. Phlebotomy
b. Wound repair and suture removal
c. Spirometry
d. Audiometry
e. Cerumen removal
f. Culture collection
7. To recognize developmental milestones in the pediatric population.
8. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
pediatrics/
E*Value Summaries
98

OST 718: Psychiatry Online
Course Description
Psychiatry is a mandatory, third year, four-week core clinical experience. During the four weeks,
the osteopathic medical student will learn to interview and evaluate patients, perform an
admission history and physical on all admitted patients, and develop multi-axial assessments.
Course Objectives
1. To develop evaluative and management skills for the care of the psychiatric patient.
a. To conduct an age, gender and problem associated patient interview and physical
examination.
b. To perform a mental status examination
c. To become acquainted with a psychiatric diagnostic and treatment plan.
Includes understanding of the DSM Multi-Axial Classification System
d. To establish a working diagnosis with reference to The Diagnostic and Statistical
Manual V.
Includes the medical work-up for the psychiatric patient
e. To apply core osteopathic principles and practices to the care of the psychiatric
patient.
f. To participate with available social and medical resources as part of the
comprehensive treatment plan.
g. To view the role of evidence based medicine to treatment decision-making.
h. To view the availability of services and its impact on patient care.
i. To view the effect of outside influences, e.g. third party insurance, on medical
decision-making.
j. To view the efficacy of psychotherapeutic treatment modalities, which include:
i. The mechanism of action for psychotherapeutic agents.
ii. The role of psychopharmacology, and side-effect profiles
iii. The treatment of Axis III comorbid states
iv. Awareness of procedural alternatives to chemical therapies, e.g. cognitive
treatment.
2. To gain an understanding for the operation of an in-patient psychiatric unit.
a. Examine the roles of staff and physician(s) in the delivery of healthcare. This includes
with the consent of the preceptor, attendance at group and individual treatment
sessions.
b. Know the HIPAA and OSHA regulations in regard to the operation of a psychiatric
unit.
i. Confidentiality
ii. Emergency procedures
c. The need for security measures required for the safe operation of a psychiatry unit.
3. To develop written and oral communication skills.
a. The production of a written and/or dictated history and physical.
b. The production of a written and/or dictated encounter progress note.
Student Duties
2 Aquifer and/or iHuman cases per day, if available on the website;
estimated to take 4 hours
100
o Assigned by the website. Choose 38 cases from those provided.
Assigned videos from Symptom Media
o https://symptommedia.com
Username: UPikeCOM
Password: UPikeCOM415
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-
psychiatry/
E*Value Summaries
COMAT Exam
Related Reading
KAPLAN & SADOCK’S Concise Textbook of Clinical Psychiatry, 4th ed. https://
go.openathens.net/redirector/upike.edu?url=https%3A%2F%2Fclerkship.lwwhealthlibrary.com
%2Fbook.aspx%3Fbookid%3D2067
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
101

OST 705: Women’s Health Online
Course Description
Women’s Health is a mandatory third year core clinical experience. The third year osteopathic
medical student is introduced to the evaluation and management of the pregnant patient,
preventive care regimens, family planning, malignancy, diagnosis and treatment of infectious
diseases, urinary, ovarian and uterine disorders, and endocrine disorders.
Course Objectives
1. To provide a framework for care of the obstetrical patient.
2. To provide a framework for preventive medical care of the gynecologic patient.
3. To identify and apply core osteopathic concepts to the care of the female patient.
4. To experience the pathophysiology relevant to diseases of the breast, ovaries, urinary
bladder, and uterus, and their medical/surgical management.
5. To expose students to an evaluative approach to diagnosis and management of the adult
female patient by use of:
a. Physical examination
b. The gynecologic and medical/surgical history
c. Laboratory and Diagnostic Testing
d. Experience based medicine
6. To provide knowledge of gynecologic and obstetrical office and operative procedures,
and their associated equipment.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-obgyn/
E*Value Summaries
COMAT Exam
Related Reading
Obstetrics and Gynecology, 7th Edition
https://bookshelf.vitalsource.com/#/books/978-1-4698-3679-9/cfi/6/2!/4/2@0:0
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
102

Surgery Selective Online Guidelines
Course Description
The surgery selective is a four-week clinical experience designed to aid the fourth year
osteopathic medical student in exercising diagnostic skills to evaluate the surgical patient and
develop an appreciation for evidence based surgical care criteria.
Course Objectives
1. To provide a framework for care of the surgical patient, which include:
a. Principles of Nutrition
b. Use of Osteopathic Manipulative Treatment
c. Principles of hydration
d. Infectious disease considerations
e. Thrombosis prevention
f. Airway management
g. Physical activity guidelines
h. Applications of evidence based surgical care criteria
i. Utilization of diagnostic imaging and the laboratory
2. To experience the pathophysiology relevant to affected organ systems, and the efficacy of
surgical care.
3. To provide knowledge and experience with the performance of bedside procedures, which
may include:
a. Placement of central venous catheters
b. Placement of gastrointestinal catheters
c. Placement of Urinary catheters
d. Removal of sutures and catheters
e. Wound care
f. Ostomy care
4. To provide knowledge and experience as an operative assistant with operative procedures, and
their associated equipment.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
Assigned reading; 3 cases / 3 hours per day
o Each reading assignment (case) requires 3 questions, with answers, be submitted.
Questions are to be unique/original board type questions with documentation as to
why your chosen answer is correct.
COMLEX Study; 1 hour per day
E*Value Summaries
Related Reading
CASE FILES SURGERY, 5th Edition, ISBN 9781259585227
https://casefiles.mhmedical.com/CaseTOC.aspx?gbosContainerID=92&categoryID=40971
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
103
Women’s Health Selective Online
Course Description
Women’s Health is a mandatory third year core clinical experience. The third year osteopathic
medical student is introduced to the evaluation and management of the pregnant patient,
preventive care regimens, family planning, malignancy, diagnosis and treatment of infectious
diseases, urinary, ovarian and uterine disorders, and endocrine disorders.
Course Objectives
1. To provide a framework for care of the obstetrical patient.
2. To provide a framework for preventive medical care of the gynecologic patient.
3. To identify and apply core osteopathic concepts to the care of the female patient.
4. To experience the pathophysiology relevant to diseases of the breast, ovaries, urinary
bladder, and uterus, and their medical/surgical management.
5. To expose students to an evaluative approach to diagnosis and management of the adult
female patient by use of:
e. Physical examination
f. The gynecologic and medical/surgical history
g. Laboratory and Diagnostic Testing
h. Experience based medicine
6. To provide knowledge of gynecologic and obstetrical office and operative procedures,
and their associated equipment.
Student Duties
2 Aquifer and/or iHuman cases per day; estimated to take 4 hours
o Assigned by the website. Choose 38 cases from those provided.
Assigned reading; 3 chapters / 3 hours per day
o Each reading assignment (chapter) requires 3 questions, with answers, be
submitted. Questions are to be unique/original board type questions with
documentation as to why your chosen answer is correct.
COMAT / COMLEX Study; 1 hour per day
o https://www.nbome.org/exams-assessments/comat/clinical-subjects/comat-obgyn/
E*Value Summaries
COMAT Exam
Related Reading
Obstetrics and Gynecology, 7th Edition
https://bookshelf.vitalsource.com/#/books/978-1-4698-3679-9/cfi/6/2!/4/2@0:0
HARRISON'S™ PRINCIPLES OF INTERNAL MEDICINE, 20th Edition
https://bookshelf.vitalsource.com/#/books/9780071748902/cfi/6/2!/4/2@0:0.125
See also
the ONLINE/VIRTUAL
ROTATION CURRICULUM cover
page in this manual.
104

OST 865: Radiology Online
Course Description
Diagnostic Radiology is a four-week course to be completed online through Canvas. The
Radiology course can fulfill the medical selective requirement or can serve as elective time. This
online course will cover: general diagnostic radiology, pediatric radiology, vascular and
interventional radiology, nuclear radiology, neurological radiology, and breast imaging. This
course will serve to further expand and develop the world of radiology to the osteopathic medical
student. Suggested areas of study may include:
Computed Tomography of the Head, Neck, Abdomen & Axial Skeleton
Magnetic Resonance Imaging of Neural and Vascular Structures
Diagnostic Ultrasound of vascular structures, abdomen and pelvis
Screening or Diagnostic Mammography
Nuclear Radiology for Endocrine, Vascular and Skeletal Diagnosis
Course Objectives
1.
To recognize the role of the radiologist in the general management of the adult
or pediatric patient.
2.
To develop an understanding of the influences that third party insurances have on
decision-making, and the choice and/or necessity for medical/surgical imaging.
3.
To experience the criteria to be considered, when radiology consultation is
contemplated.
4.
To experience the information needed from the ordering physician for the
optimal interpretation of diagnostic studies ordered for medical/surgical
patients.
Student Duties
The student will be required to complete 1 video lecture from Dr. Joshua Crum and 1 quiz per
week with a summary to be completed at the end of the 4-week cycle. A total of 4 video lectures,
4 quizzes and 1 summary question must be successfully completed and passed in order to receive
full (4-hour) credit for course.
Grading Policy
Students must complete viewing the required lectures and 1 quiz per week. A written summary
will need to be completed at the end of the 4-week rotation cycle to summarize outcome results
of the course contents. The written summary should be submitted directly to Dr. Joshua Crum
via email. The summary should include but not limited to how this course was beneficial to each
student and how this course will help the student as they progress in their medical education.
Each (4) quiz will contain 5 questions each with (1) written summary question to be graded on a
case by case basis. These will be worth 20 points each.
105

Quizzes = 80%
Course Written Summary = 20%
Course Passage = 70%
Responsibilities may include:
1.
Viewing Dr. Joshua Crum’s lecture modules (4 per month)
2.
View lectures as assigned on www.learningradiology.com
3.
Successfully complete 1 quiz per lecture (4 per month)
4.
Complete essay to summarize course contents
5.
Reading suggested material
Suggested Reading
•
www.learningradiology.com
•
www.radiology.com
•
https://libguides.library.upike.edu/radiology
•
Canvas: Radiology #865 Lecture and quizzes (4)
Remediation Policy: Students who do not achieve 70% or bette
r in the course fail this course.
According to the KYCOM Student Handbook, all failures are reviewed by the Promotion &
Matriculation Committee and a decision is made whether or not a student is allowed to remediate
failed courses. If the Promotion & Matriculation Committee decides a student is allowed
remediate, the student will revisit and pass the modules failed.
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
106
OST 804 Emergency Medicine Selective Online
Course Description
Emergency Medicine is a mandatory, four-week, third or fourth year selective clinical
experience. Integration of clinical skills and evidence-based medicine is achieved with emphasis
on didactic discussions, and development of clinical skills.
Pre-requisites: General Internal Medicine I, General Internal Medicine II, Family
Medicine I, General Surgery, Pediatrics, and Woman’s Health
Course Objectives
1. To integrate osteopathic principles and practice concepts into the conventional care of
emergency patients
2. To experience case management and the coordination of systems based medical care.
a. The use of subspecialists and other medical/surgical disciplines.
b. The use of social services and outpatient programs
c. The use of in-house care services.
d. To recognize the social and economic factors that affect patient care.
3. To employ the knowledge, attitudes, and skills necessary to provide preventive, episodic,
or continuing care to individual patients in an emergency medicine setting
4. To experience prioritization skills.
5. To learn assessment skills for classification of the type, level and urgency of care needed
for the particular patient encounter.
6. To integrate the utilization of appropriate health maintenance screening protocols into
emergency medicine care.
7. To demonstrate the ability to assess a patient and differentiate the need for urgent versus
non-urgent care.
8. For students to experience the practice of evidence-based medicine.
a. To assess, apply, and assimilate investigative knowledge to improve patient care.
b. To realize the Emergency Medicine physician’s role in the community and Society.
c. To cite and communicate information in an organized and succinct manner
9. For students to respect and be sensitive to the individuality, values, goals, concerns, and
rights of all with whom they interact in the healthcare setting.
10. Demonstrate understanding of ethical principles of autonomy, beneficence, informed
consent, and confidentiality.
11. To accomplish the use of effective written, and verbal language skills.
107

Related Reading
Rosen's Emergency Medicine: Concepts and Clinical Practice, 9
th
Edition
https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20141019850
Suggested Topics to Review
Chest Pain - UA, NSTEMI, STEMI, Thoracic Aortic Aneurysm, Pulmonary Embolism, Acute
Exacerbation Of COPD, Asthma, CHF, AFIB, HTN Urgency And Emergency, Pneumonia -
HCAP, CAP, Stroke, Dizziness, Bell’s Palsy, Headache, Seizure, Musculoskeletal Pain - Neck
Pain, Back Pain, Acute Injuries Like Ankle/Knee Sprain, Shoulder Pain, Fracture Evaluation
And Management, Hip Fracture, Abdominal Pain - Appendicitis, Cholecystitis, Pancreatitis,
Diverticulitis, Pyelonephritis, Gastroenteritis, UTI, Kidney Stone, Gastric/Duodenal Ulcers,
Small Bowel Obstruction, Ileus, Mesenteric Ischemia, GI Bleed, AAA, OB/Gyn - Vaginal
Bleeding, Vaginal Discharge, Miscarriage, Pregnancy Management, Ovarian Cyst/Torsion
Prostatitis, Orchitis, Testicular Torsion, Epididymitis, ACLS, ATLS - Trauma Evaluation -
Primary Survey and Secondary Survey, Burns, DKA, Laceration Care, SIRS/Sepsis, Meningitis,
Alcohol and Other Drug Intoxication/Withdrawal/Overdose
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this
manual.
108

OST 805 Emergency Medicine Elective Online
Course Description
Emergency Medicine is a four-week fourth year elective clinical experience. Integration of
clinical skills and evidence-based medicine is achieved with emphasis on didactic discussions,
and development of clinical skills.
Pre-requisites: General Internal Medicine I, General Internal Medicine II, Family
Medicine I, General Surgery, Pediatrics, Woman’s Health and Emergency Medicine
Selective
Course Objectives
1. To integrate osteopathic principles and practice concepts into the conventional care of
emergency patients
2. To experience case management and the coordination of systems based medical care.
a. The use of subspecialists and other medical/surgical disciplines.
b. The use of social services and outpatient programs
c. The use of in-house care services.
d. To recognize the social and economic factors that affect patient care.
3. To employ the knowledge, attitudes, and skills necessary to provide preventive, episodic,
or continuing care to individual patients in an emergency medicine setting
4. To experience prioritization skills.
5. To learn assessment skills for classification of the type, level and urgency of care needed
for the particular patient encounter.
6. To integrate the utilization of appropriate health maintenance screening protocols into
emergency medicine care.
7. To demonstrate the ability to assess a patient and differentiate the need for urgent versus
non-urgent care.
8. For students to experience the practice of evidence-based medicine.
a. To assess, apply, and assimilate investigative knowledge to improve patient care.
b. To realize the Emergency Medicine physician’s role in the community and Society.
c. To cite and communicate information in an organized and succinct manner
9. For students to respect and be sensitive to the individuality, values, goals, concerns, and
rights of all with whom they interact in the healthcare setting.
10. Demonstrate understanding of ethical principles of autonomy, beneficence, informed
consent, and confidentiality.
11. To accomplish the use of effective written, and verbal language skills.
Related Reading
Rosen's Emergency Medicine: Concepts and Clinical Practice, 9
th
Edition
https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20141019850
See also the ONLINE/VIRTUAL ROTATION CURRICULUM cover page in this manual.
109
REQUEST FORMS AND EVALUATION FORMS
110
University of Pikeville
Kentucky College of Osteopathic Medicine
Conference Attendance Request
Student’s Name _________________________________ Class of 2023
Current Rotation ____________________________________________________
Preceptor’s Name ___________________________________________________
Rotation Begin Date ___________________ End Date ______________________
Conference _________________________________________________________
Location ___________________________________________________________
Departure Date _____________________ Return Date _____________________
(First date absent from rotation) (First date back to rotation)
Student’s Signature_________________________________________________
Preceptor’s Signature _______________________________________________
Preceptor at time of absence
KYCOM Approval _________________________________________________
Associate Dean for Clinical Affairs
Date:__________________________
111
UNIVERSITY OF PIKEVILLE
KENTUCKY COLLEGE OF OSTEOPATHIC MEDICINE
SELECTIVE REQUEST FORM
Student Name_______________________________________________________Class of 2022
EMail Address ____________________________________Phone # _____________________
Rotation Begin Date: _________________________ End Date: _________________________
Did your Core Site Coordinator arrange this rotation? □ Yes □ No
Preceptor: ____________________________________________________________________
Address: _____________________________________________________________________
Street City State Zip
Phone #: _____________________________ Fax #: _________________________________
Email address: ________________________________________________________________
Hospital preceptor affiliated with: _________________________________________________
Hospital Address: _______________________________________________________________
Street City State Zip
Phone #: ________________________________ Fax #: _______________________________
Office use only:
Date Received _____________________ Mailed _______________________________
Faxed ___________________________ E-mailed _____________________________
Selective Rotation:
Preceptor’s Specialty / Board Certification:
□ Emergency Medicine
□ Medicine Subspecialty
□ Surgical Subspecialty
□ Rural Medicine
___________________________________
___________________________________
___________________________________
___________________________________
112
UNIVERSITY
OF PIKEVILLE
KENTUCKY COLLEGE OF OSTEOPATHIC MEDICINE
ELECTIVE REQUEST FORM
Student Name: _______________________________________________ Class of 2023
EMail Address: _______________________________ Phone # ___________________
Rotation Type: __________________________________________________________
Rotation Begin Date: _______________________ End Date: ________________________
Preceptor (If known): _____________________________________________________
Address: _______________________________________________________________
________________________________________________________________
Phone number: ______________________ Fax number: ________________________
Preceptor Email Address: __________________________________________________
Hospital preceptor affiliated with: __________________________________________________
Address: _______________________________________________________________
__________________________________________________________________________
Contact / Coordinator Email address:
_________________________________________ Contact phone number:
_____________________ Fax number: ____________________
Below for KYCOM Office Use Only
_____ Approved _____ Not Approved
____ Medicine ____ Surgery
Office use only:
Received _____________________________
Mailed ______________________________
Faxed _______________________________
E-mailed _____________________________
113
University of Pikeville
Kentucky College of Osteopathic Medicine
Interview Request Form
Name _______________________________________________________ Class of 2023
Rotation______________________ Preceptor’s Name____________________________
First Interview
Residency Program ________________________________________________________
Departure Date ________________________ Return Date ________________________
(First date absent from rotation) (First date back to rotation)
Student’s Signature___________________________________ Date ________________
Preceptor’s Signature _________________________________ Date ________________
KYCOM Approval ____________________________________ Date________________
Associate Dean for Clinical Affairs
Second Interview
Residency Program ________________________________________________________
Departure Date ________________________ Return Date ________________________
(First date absent from rotation) (First date back to rotation)
Student’s Signature___________________________________ Date ________________
Preceptor’s Signature _________________________________ Date ________________
KYCOM Approval ___________________________________ Date________________
Associate Dean for Clinical Affairs
Third Interview
Residency Program ________________________________________________________
Departure Date ________________________ Return Date ________________________
(First date absent from rotation) (First date back to rotation)
Student’s Signature___________________________________ Date ________________
Preceptor’s Signature _________________________________ Date ________________
KYCOM Approval ___________________________________ Date________________
Associate Dean for Clinical Affairs
114

KYCOM Class of 2023
Student Assessment Form
Core Rotations & Emergency Medicine
(To be completed by PRECEPTOR)
Student ____________________________________________ Rotation Dates: _____________________
Preceptor: _________________________________ Primary Hospital: ____________________________
Instructions to preceptors: Clinical rotation grades are based 50% on this form, as completed by you, and 50% their score on
the COMAT exam. Each of 9 rotation objectives is scaled from a least desirable (50) to a most desirable (100). Students should
be evaluated in comparison to other students seen at similar levels of medical education. Please fax this completed form to
(606) 218-5168 within 7 days after the completion of the rotation.
PRECEPTOR: Please complete the following or attach your business card.
Print Name
Street Address
Business, City/State/Zip
Business Telephone
Business Fax
At the time of this rotation, did you have a physician-patient relationship with this student. □ Yes □ No
_______________________________________________ □ D.O. □ M.D. __________________
Preceptor’s Signature Check One Date
Evaluation continues on next page.
Please Check Appropriate Discipline
□ OST 740 General Surgery
□ OST 700 OP&P
□ OST 706 Pediatrics
□ OST 718 Psychiatry
□ OST 708 Family Medicine I
□ OST 709 Family Medicine II
□ OST 705 Women’s Health
□ OST 720 General Internal Medicine I
□ OST 721 General Internal Medicine II
□ OST 804 Emergency Med Selective
D.O.s – Please complete the following for CME Credit.
AOA Number
M.D.s –For accreditation purposes, enter the number of Contact Hours for possible CME Credit.
Please utilize this space for any comments, descriptions or supporting statements. All information is held
confidential for internal purposes only.
List any comments you wish to include in the student’s MSPE/Dean’s Letter
Email Address
115

Student _______________________________________ KYCOM ID_________________________
Nine (9) rated spheres are listed below. Each can earn up to 100 points.
1.
Professionalism (Demeanor, Appearance, Reliability)
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Major Concerns.
◄
Appropriate.
Above average.
Exemplary.
2.
Interpersonal Relationships - Health Care Team/Patients
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Distant, strained,
dysfunctional
cool or awkward.
F
Forms constructive
relationships.
Constructive & professional.
High quality, accepted as team
member.
3.
Performance of History & Physical Examinations
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Often misses major,
important findings & relevant
data.
A
Usually elicits most relevant
data & identifies findings
accurately.
Almost always elicits all
relevant data & identifies
findings accurately.
Elicits data efficiently & in great
depth; often discovers subtle
physical findings.
4.
Diagnostic Test Selection & Interpretation
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Frequently suggests or
interprets diagnostic tests
inappropriately.
I
Usually suggests & interprets
diagnostic tests appropriately.
Almost always suggests &
interprets diagnostic tests
appropriately.
Always reveals exceptional
insights.
5.
Treatment
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Demonstrates major
misunderstandings about
treatment plans.
L
Usually suggests appropriate
treatment plans.
Almost always suggests
appropriate treatment plans.
Exhibits exceptional insights in
treatment plans.
6.
Charting
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Notes are often formatted
improperly, illegible,
inaccurate, or lists are not
updated.
I
Notes are usually formatted
properly, legible & accurate,
lists are updated.
Notes are almost always well
organized, concise &
demonstrate good synthesis.
Notes are always well organized,
concise, and demonstrate excellent
synthesis.
7.
Clinical Reasoning
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Frequently illogical or
impractical.
N
Usually practical & logical.
Almost always
practical & logical.
Frequent astute insights.
8.
Progression Through Rotation
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Minimal or inconsistent effort
or gain.
G
Showed good, consistent effort
or gain.
Showed strong effort or gain.
Made extraordinary effort or gain.
9.
Osteopathic Manipulative Medicine Skills
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Fails to perform structural
exam. Unsatisfactory OMT
skills.
◄
Occasionally performs structural
exam. Acceptable OMT skills.
Routinely performs structural
exam. Above average OMT
skills.
Always performs structural exam.
Excellent OMT skills.
__________________________________________________________________ __________________________
Student’s Signature Date
Total __________ Grade_________ ____________________________________ ________________
Signature, Associate Dean for Clinical Affairs Date
Revised 5/2020
116

KYCOM Class of 2023
Student Assessment Form – Selective/Elective
(To be completed by PRECEPTOR)
Student ____________________________________________ Rotation Dates: _____________________
Preceptor: __________________________________ Primary Hospital: ___________________________
Instructions to preceptors: Clinical rotation grades are based on this Student Assessment Form as completed by you. Each of 10
rotation objectives is scaled from a least desirable (50) to a most desirable (100). Students should be evaluated in comparison to
other students seen at similar levels of medical education. Please fax this completed form to (606) 218-5168 within7 days after the
completion of the rotation.
PRECEPTOR: Please complete the following or attach your business card.
Print Name
Street Address
Business City/State/Zip
Business Telephone
Business Fax
At the time of this rotation, did you have a physician-patient relationship with this student. □ Yes □ No
_______________________________________________ □ D.O. □ M.D. ______________________
Preceptor’s Signature Check One Date
Student ________________________________________________KYCOM ID ____________________
Evaluation continues on next page.
D.O.s – Please complete the following for CME Credit.
AOA Number
M.D.s –For accreditation purposes, enter the number of Contact Hours for possible CME Credit.
Please utilize this space for any comments, descriptions or supporting statements. All information is held
strictly confidential for internal purposes only.
Please Check Appropriate Discipline:
□ OST 809 Rural Health Selective
□ OST ______ Elective #1_____________ □ OST ______ Elective #2___________ □ OST ______ Elective #3_________
□ OST ______ Elective #4__________ □ OST ______ Elective #5___________ □ OST _____ Elective #6 __________
□ OST ______ Surgical Selective □ OST ______ Medicine Selective
List any comments you wish to include in the student’s MSPE / Dean’s Letter.
Email Address
117
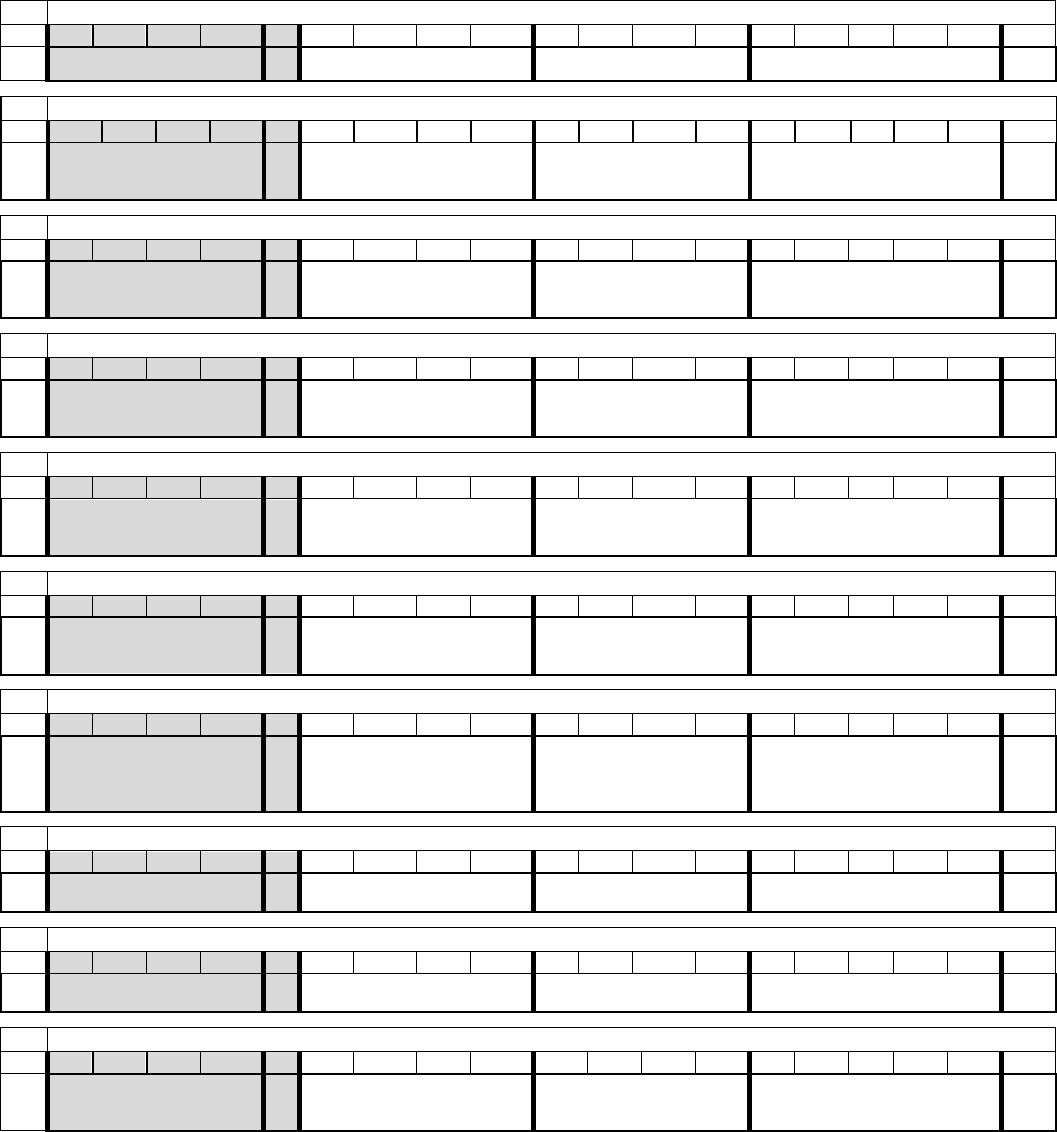
Student _______________________________________ KYCOM ID_________________________
Ten (10) rated spheres are listed below. Each can earn up to 100 points.
1.
Professionalism (Demeanor, Appearance, Reliability)
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Major Concerns.
◄
Appropriate.
Above average.
Exemplary.
2.
Interpersonal Relationships - Health Care Team/Patients
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Distant, strained,
dysfunctional
cool or awkward.
F
Forms constructive
relationships.
Constructive & professional.
High quality, accepted as team
member.
3.
Basic Medical Knowledge
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Generally fair or good. Major
deficiencies in important
areas.
A
Generally good for student level.
Excellent depth in important
areas.
Outstanding.
4.
Performance of History & Physical Examinations
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Often misses major,
important findings & relevant
data.
I
Usually elicits most relevant
data & identifies findings
accurately.
Almost always elicits all
relevant data & identifies
findings accurately.
Elicits data efficiently & in great
depth; often discovers subtle
physical findings.
5.
Diagnostic Test Selection & Interpretation
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Frequently suggests or
interprets diagnostic tests
inappropriately.
L
Usually suggests & interprets
diagnostic tests appropriately.
Almost always suggests &
interprets diagnostic tests
appropriately.
Always reveals exceptional
insights.
6.
Treatment
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Demonstrates major
misunderstandings about
treatment plans.
I
Usually suggests appropriate
treatment plans.
Almost always suggests
appropriate treatment plans.
Exhibits exceptional insights in
treatment plans.
7.
Charting
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Notes are often formatted
improperly, illegible,
inaccurate, or lists are not
updated.
N
Notes are usually formatted
properly, legible & accurate,
lists are updated.
Notes are almost always well
organized, concise &
demonstrate good synthesis.
Notes are always well organized,
concise, and demonstrate excellent
synthesis.
8.
Clinical Reasoning
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Frequently illogical or
impractical.
G
Usually practical & logical.
Almost always
practical & logical.
Frequent astute insights.
9.
Progression Through Rotation
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Minimal or inconsistent effort
or gain.
◄
Showed good, consistent effort
or gain.
Showed strong effort or gain.
Made extraordinary effort or gain.
10.
Osteopathic Manipulative Medicine Skills
50
60
65
68
70
73
75
78
80
83
85
88
90
93
95
98
100
NA
Fails to perform structural
exam. Unsatisfactory OMT
skills.
◄
Occasionally performs structural
exam. Acceptable OMT skills.
Routinely performs structural
exam. Above average OMT
skills.
Always performs structural exam.
Excellent OMT skills.
_______________________________________________________________ ____________________________
Student’s Signature Date
Total __________ Grade_________ ____________________________________ __________________
Signature, Associate Dean for Clinical Affairs Date
Revised 5/2020
118
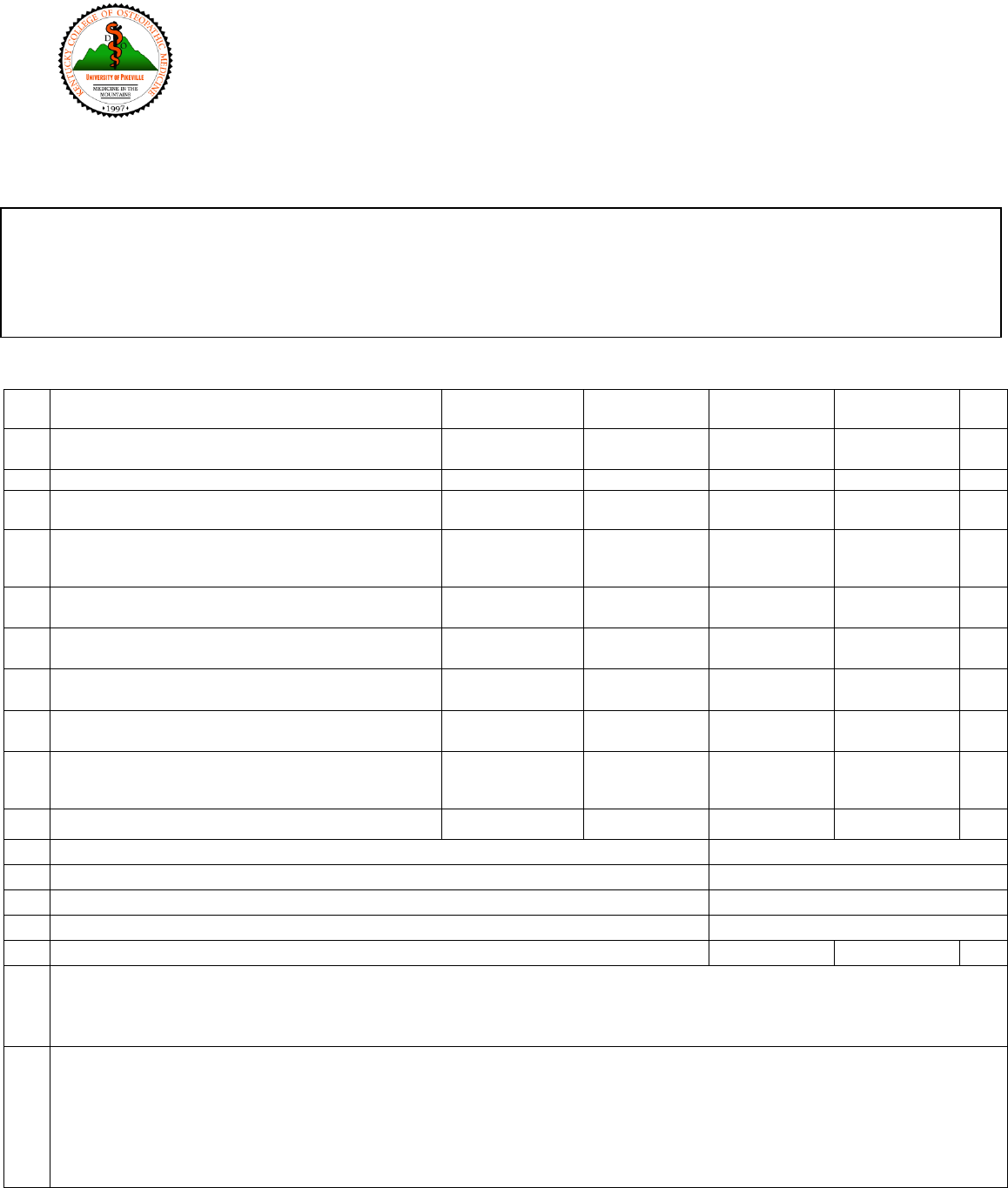
KYCOM Rotation Assessment Form – Class of 2023
(To be completed by STUDENT)
Check Year: □ OMS III □ OMS IV Rotation Dates: _____________________
Preceptor: ________________________________________________ Core Site: __________________________
Please Circle Your Response:
1
Describe how well this rotation prepared you for the
rotation subject.
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
2
Describe how receptive the attending physician(s) were
to student questions.
Very
Receptive (1)
Somewhat
Receptive (2)
Somewhat
Unreceptive (3)
Not
Receptive (4)
NA
3
Rate the quality of the didactic training.
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
4
Describe the extent to which you were allowed to
participate in and/or perform medical procedures.
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
5
Describe the variety of patients and problems
(pathology, scope and volume) you observed during
this rotation.
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
6
Was osteopathic theory discussed on rounds and during
presentations?
Daily
(1)
Very Frequently
(2)
Frequently
(3)
Infrequently
(4)
NA
7
Were osteopathic techniques utilized on both office and
hospital patients?
Daily
(1)
Very Frequently
(2)
Frequently
(3)
Infrequently
(4)
NA
8
Describe the extent to which you had the opportunity to
work with patients on a one-to-one basis.
Daily
(1)
Very Frequently
(2)
Frequently
(3)
Infrequently
(4)
NA
9
Describe the extent which the attending
physician(s)/preceptor(s) verbally quizzed you.
Excellent
(1)
Good
(2)
Fair
(3)
Poor
(4)
NA
10
Describe the networking opportunities provided during
the rotation. (e.g. introduction for future employment
opportunities)
Excellent
(1)
Good
(2)
Fair
(3)
Poor
(4)
NA
11
Describe how well you were received by office staff.
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
12
How many times per day were rounds conducted? (Please enter a number.)
times per day
13
How long did it take you to drive from your core site to this rotation?
____________hrs. ____________mins.
14
How many weekends did you work during this rotation?
________________________weekends
15
What were the daily hours for this rotation?
to
16
Were you provided meals on this rotation?
Yes (1)
No (2)
NA
17
What reading/reference materials do you recommend that might benefit a student about to begin this rotation?
18
Please discuss any preparations or advance arrangements, if any, not covered by the AHEC or the Dept. of Family Medicine that must
be made prior to requesting/beginning this rotation?
Please Check Appropriate Discipline:
□ Family Medicine □ General Internal Medicine □ Pediatrics
□ General Surgery □ Women’s Health □ Psychiatry
□ OP&P □ Selective _________________ □ Elective _________________
119

19
Please list the strengths of this rotation.
20
Please list the weaknesses of this rotation.
21
Additional Comments:
22
Was an instructional resource center (IRC) available for your use?
Yes (1)
No (2)
Rate the following:
IRC Staff
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Computers
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Printers
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Scanners
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Hours of Operation
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Inter-Library Access
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Instructional Software
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Simulation Equipment
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Accessibility
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Periodical Library
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Reference Library
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Internet Subscriptions
Excellent (1)
Good (2)
Fair (3)
Poor (4)
NA
Core Site Facilities Survey
Number of Students During the Rotation
WiFi Access
Yes (1)
No (2)
Call Room
Yes (1)
No (2)
Shower
Yes (1)
No (2)
Secured Storage Area
Yes (1)
No (2)
Student Study Space
Yes (1)
No (2)
Dining Room
Yes (1)
No (2)
Classroom with Video Conference Capability
Yes (1)
No (2)
Revised 5/2020
120
University of Pikeville
Kentucky College of Osteopathic Medicine
OST 897: Research Request Form
Student name ___________________________________________ Class of 2023
Student email ______________________________________________________
Research title _______________________________________________________
Preceptor name _____________________________________________________
Preceptor email _____________________________________________________
Research Begin Date ___________________ End Date ______________________
Location ___________________________________________________________
Student’s Signature_________________________________________________
Preceptor’s Signature _______________________________________________
KYCOM Approval _________________________________________________
Associate Dean for Clinical Affairs
Date:__________________________
121
122

READ RECEIPT
I attest that I have read the KYCOM Clinical Rotations Manual released for use by the
Class of 2023. I further acknowledge that I accept all of the rules and regulations within the
text, and am bound to follow them as written. I understand that submittal of this attestation
form is a requisite to begin the clinical rotation experience.
Date
Printed Name
Signature
123
124

