Strategic Review of
Maternal Level of Care
Designations
As Required by
Senate Bill 749, 86th
Legislature, Regular Session,
2019
February 2022
Table of Contents
Executive Summary ............................................................................... 1
1. Introduction ...................................................................................... 3
2. Background ....................................................................................... 4
Creation of Neonatal and Maternal Levels of Care ..................................... 4
3. Designation Implementation Evaluation ............................................ 7
Initial Designations ............................................................................. 7
Appeals Process .................................................................................. 8
Evaluation ....................................................................................... 10
Barriers to Requested Level of Designation............................................ 11
Geographic Considerations for Designation ............................................ 13
Impact of COVID-19 .......................................................................... 13
Improvement in Maternal Care ............................................................ 14
DSHS Actions and Next Steps ............................................................. 15
4. Conclusion ....................................................................................... 16
List of Acronyms .................................................................................. 17
Appendix A. Literature Review Sources............................................... A-1
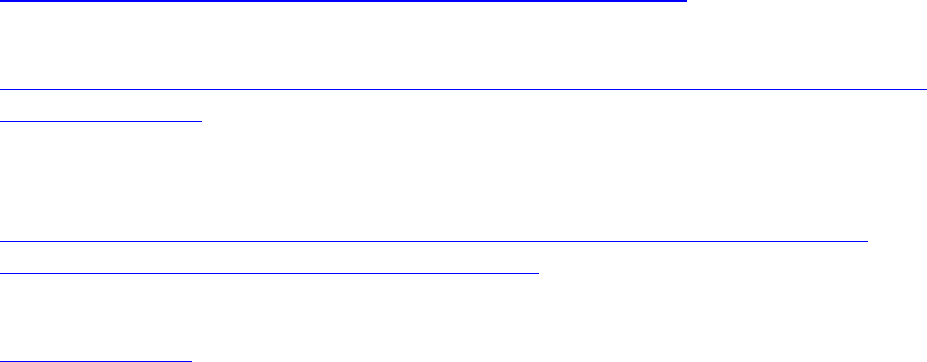
Appendix B. Designation Process Summary ........................................ B-1
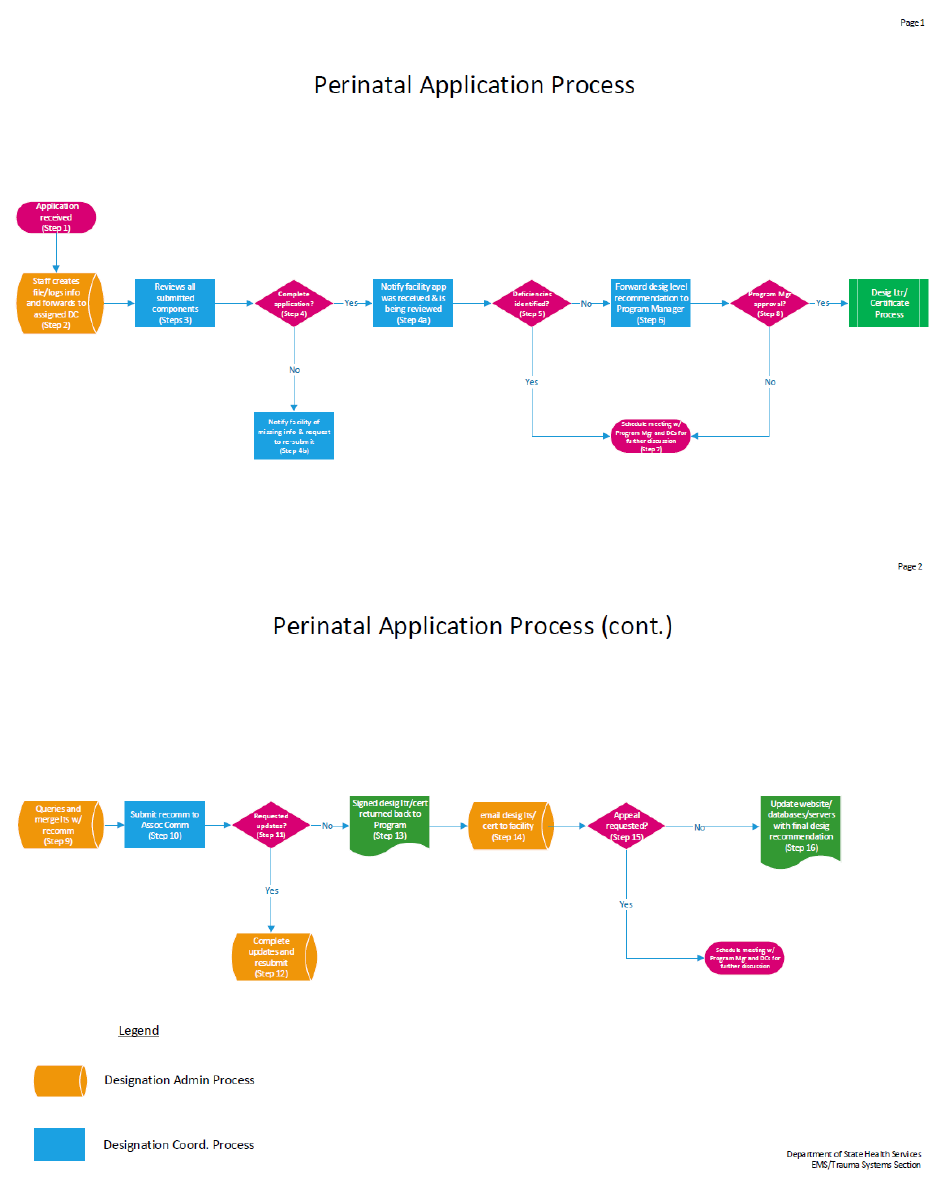
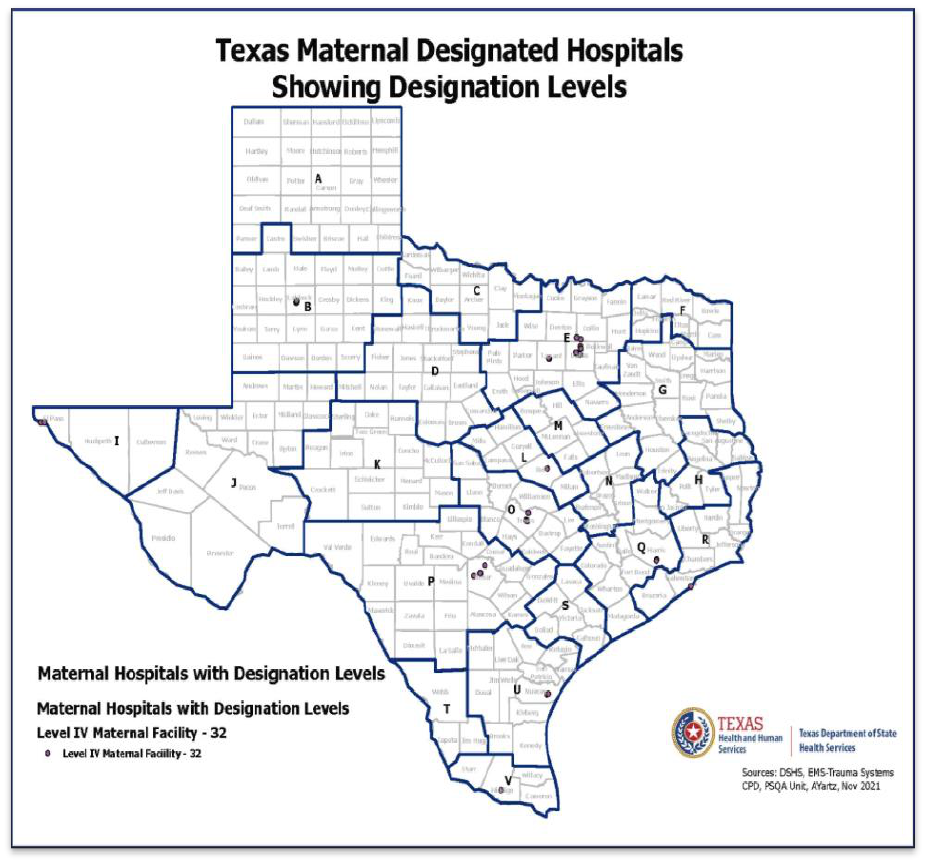
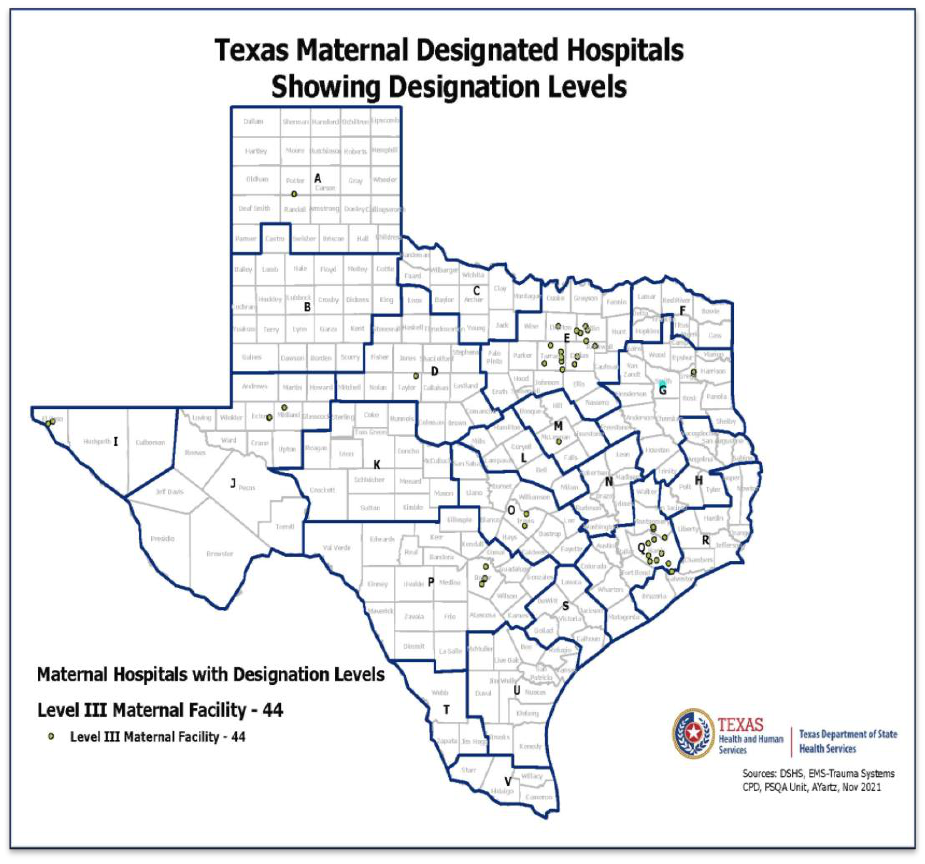
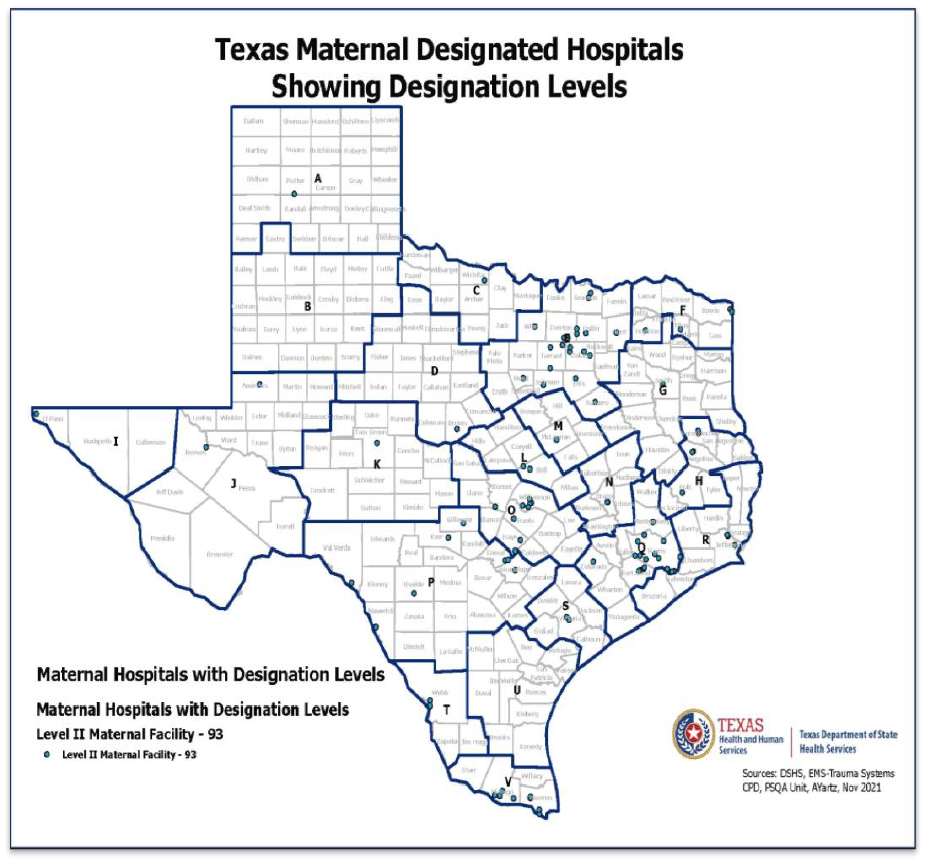
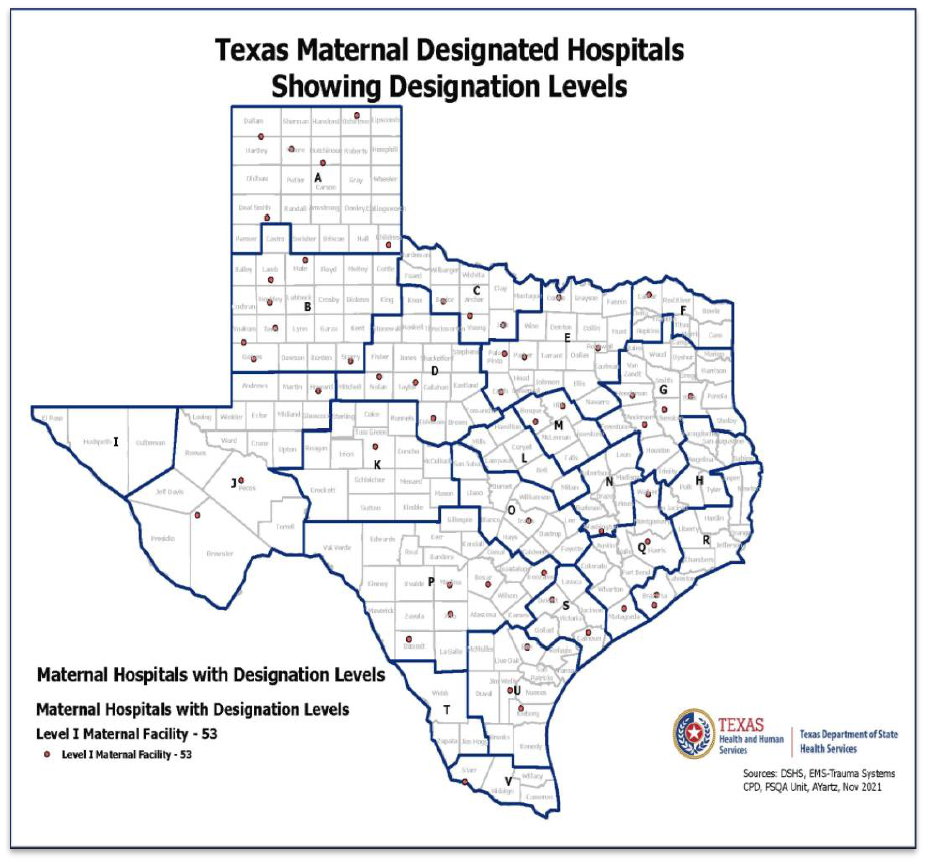
Appendix C. Texas Maps of Maternal Designated Facilities .................. C-1
Appendix D. Texas Maternal Level of Care Designation Requirements
defined as barriers to achieving the hospital’s desired designation level
compared to the other state designation requirements. ................. D-1
Appendix E. Geographic Considerations and Mileage .......................... E-1

1
Executive Summary
The Department of State Health Services (DSHS), in consultation with the Perinatal
Advisory Council (PAC), completed a strategic review of the practical
implementation of Hospital Level of Care Designations for Maternal and Neonatal
Care pursuant to Senate Bill 749 (S.B. 749), 86
th
Legislature, Regular Session,
2019. The legislation requires that the strategic review should, at a minimum,
identify:
● Barriers to a hospital obtaining its requested level of care designation
● Whether the barriers are appropriate to ensure and improve neonatal and
maternal care
● Requirements for a level of care designation that relate to gestational age
and
● Whether, in making a level of care designation for a hospital, the department
or PAC should consider:
Geographic area in which the hospital is located, and
Regardless of the number of patients of a particular gestational age
treated by the hospital, the hospital’s capabilities in providing care to
patients of a particular gestational age as determined by the hospital.
The Texas maternal level of care designation requirements are consistent with the
nationally recognized and accepted American College of Obstetricians and
Gynecologists and Society for Maternal-Fetal Medicine guidelines and are
comparable to nine other states with perinatal systems.
There are currently 222 designated maternal facilities in Texas. From 2019-2021,
206 facilities received their requested level of designation. 14 facilities either
appealed or utilized a new survey to establish compliance with the requirements for
their requested level of designation. In total, 99 percent of facilities ultimately
received their requested level of designation.
DSHS analyzed numerous materials related to the designation process, including
222 surveys or self-assessments, 3,126 patient record reviews, pertinent sections
of the Texas Administrative Code, geographical considerations, and level of care
requirements in other states. Based on this review, DSHS identified the following

2
barriers that potentially impacted hospitals from receiving their initial requested
level of designation:
● Level IV - not providing comprehensive care for pregnant and postpartum
patients with low-risk conditions to the most complex medical, surgical, or
obstetrical conditions and their fetuses, that present a high risk of maternal
morbidity or mortality.
● Level III - not ensuring access to consultation to a full range of medical and
maternal subspecialists, surgical specialists, and behavioral health
specialists.
● Level II – not having in place effective Quality Assessment Performance
Improvement (QAPI) processes, medical staff team-based education and
training, and evidence of collaboration between the maternal medical director
and the maternal program manager.
● Level I – not creating or implementing written policies and procedures
specific to the maternal program.
To further improve the maternal level of care designation process, DSHS
coordinates regular calls with the maternal facilities to provide technical assistance,
share best-practices, and provide education customized to these facilities’ needs.
DSHS continues to focus on improving maternal care across Texas through the
designation process, system development, and collaborative efforts with
stakeholders and the PAC.
DSHS reviewed recommendations provided by the PAC specific to rule clarification
and suggestions. The PAC provided recommendations for integrating S.B. 749
language into the rules, with two recent subcommittees focusing on specific rule
language, one of which focuses on House Bill 1164, 87th Legislature, Regular
Session, 2021, which requires specific requirements related to placenta accreta
spectrum disorder be added to the maternal levels of care rules. The maternal rules
incorporating recommendations from the PAC are in the formal Health and Human
Services (HHS) rulemaking process. The proposed rules will be considered by the
HHS Executive Council prior to appearing in the Texas Register as proposed rules
for formal comment.

3
1. Introduction
Senate Bill 749 (S.B. 749), 86
th
Legislature, Regular Session 2019, directs the
Department of State Health Services (DSHS), in consultation with the Perinatal
Advisory Council (PAC), to conduct a strategic review of the practical
implementation of the adopted Hospital Maternal Levels of Care Designations rules.
This review includes information on the maternal designation process and current
appeal process. The review explores the development and creation of the maternal
designation process and how DSHS worked with the PAC to develop the current
rules. The outcome of the initial maternal designation reviews and the identified
barriers to successful designation are highlighted.
This report includes a comparison with the three states with specific and similar
maternal designation requirements (Georgia, Indiana, and Louisiana). The primary
barriers identified in the Texas maternal designation process were compared to
these three states’ designation requirements.
Geographic alignment and consideration of the levels of maternal designation are
included in this review. This information includes the counties without a maternal
designated facility and those counties that have only a designated Level I maternal
facility.
Finally, the report also highlights improvements in maternal care and next steps by
the PAC and DSHS.
4
2. Background
The Maternal Levels of Care Designation process was first required by House Bill 15,
83
rd
Legislature, Regular Session, 2013 and House Bill 3433, 84
th
Legislature,
Regular Session, 2015. Designation for a maternal level of care has been an
eligibility requirement for hospitals for Medicaid reimbursement since September 1,
2021. While designation itself is voluntary, non-designated maternal hospitals that
submit maternal-related billing to Medicaid will have their billing denied.
Hospital designations are a formal recognition process that categorizes hospital
capabilities, capacity, and resources to provide specific types of care. The levels of
care are defined by established requirements. The designation status allows the
public, patients, and their families to have confidence in the hospital’s services. The
designation also communicates to Emergency Medical Services (EMS) providers and
other health care workers the types of care capabilities the facility can provide to
patients.
Hospital designations can establish systems of care that, over time, improve health
outcomes for patients. Designation recognizes the highest functional level of
maternal care provided by a hospital inclusive of all lower-level care provided.
Hospitals choose the specific type and level of designations they seek based on
their capabilities. Designation does not dictate who a hospital can care for, what
services a hospital can provide, and does not mandate patient transfers or limit a
doctor’s decision about patient care.
Designated facilities of the same level and type have requirements for standard
procedures, processes, and evidence-based care practices. In Texas, hospitals can
receive designations for the following care categories: Trauma, Stroke, Neonatal,
and Maternal. (Note: The term hospital refers to an entity seeking or applying for a
level of designation. Once the hospital achieves designation, it is referred to as a
designated facility.)
Creation of Neonatal and Maternal Levels of Care
The 83
rd
and 84
th
Legislatures directed the formation and functions of the Perinatal
Advisory Council (PAC) to establish maternal and neonatal levels of care.
5
The PAC, per statute, is composed of pertinent specialists and subspecialists
involved in the care of pregnant patients and newborns, and representatives from
hospital administration. The PAC served as the primary source of health care
expertise and stakeholder comments for DSHS’ development of the formal
administrative rules that define the maternal levels of care designation
requirements. The Legislature tasked the PAC with:
● Developing and recommending criteria for designating neonatal and maternal
levels of care.
● Developing and recommending a process for assigning levels of care to a
hospital.
● Recommending state perinatal care regions.
● Reviewing and examining neonatal and maternal outcomes.
DSHS reviewed maternal levels of care requirements and rules established in
Illinois, Indiana, Louisiana, Maryland, Massachusetts, Missouri, New York, Ohio, and
South Carolina. Only Georgia, Indiana, and Louisiana have clear and separate levels
of care for the maternal and neonatal populations. Other states combine their
maternal and neonatal levels of care. See Appendix A for a list of literature review
and resources utilized for this review.
The PAC researched and received extensive stakeholder feedback to frame the
maternal levels of care rules. In alignment with PAC recommendations, Texas
adopted rules consistent with the Guidelines for Perinatal Care, Seventh Edition
(American Academy of Pediatrics [AAP] and the American College of Obstetricians
and Gynecologists [ACOG], 2012), which serves as a national resource on perinatal
care. Like other states, the rules also align with the Obstetric Care Consensus:
Levels of Maternal Care (American College of Obstetricians and Gynecologists and
Society for Maternal-Fetal Medicine, 2015), an additional national resource on
maternal levels of care. More information on the process, stakeholder feedback,
and PAC composition can be found in the September 2016 Perinatal Advisory
Council Report on Determinations and Recommendations.
Title 25, Chapter 133, Texas Administrative Code, Sections 133.206 – 133.209
establishes the following maternal levels of care with corresponding designation
requirements:
● Level IV, Comprehensive Care. The hospital provides comprehensive care
for pregnant and postpartum patients with low-risk conditions to the most
6
complex medical, surgical, or obstetrical conditions and their fetuses, that
present a high risk of maternal morbidity or mortality.
● Level III, Subspecialty Care. The hospital provides care for pregnant and
postpartum patients with low-risk conditions to significant complex medical,
surgical, or obstetrical conditions that present a high risk of maternal
morbidity or mortality.
● Level II, Specialty Care. The hospital generally provides care for pregnant
and postpartum patients with medical, surgical, or obstetrical conditions that
present a low to moderate risk of maternal morbidity or mortality.
● Level I, Basic Care. The hospital generally provides care for pregnant and
postpartum patients who are generally healthy, and have medical, surgical,
or obstetrical conditions that present a significant risk of maternal morbidity
or mortality.
Facilities with lower levels of designation can, according to the hospital’s discretion
and medical decision-making, retain care of a pregnant or postpartum patient with
any medical problem. DSHS does not regulate the practice of medicine.
7
3. Designation Implementation Evaluation
Initial Designations
DSHS awards maternal level of care designations based on compliance with the
designation requirements defined in the Title 25, Chapter 133, Texas Administrative
Code (TAC), Sections 133.203 – 133.209. Designations are intended to recognize
the functional level of care demonstrated and maintained by an individual hospital.
Hospital compliance with the designation requirements is determined through a
survey process for Level II, III, and IV maternal facilities. Hospitals seeking Level I
maternal level of care designation complete a self-assessment and an attestation of
compliance to the designation requirements. A survey is not completed for the
Level I facilities. The surveys for Level II, III, and IV facilities are completed by a
department-approved survey organization. The survey process is designed to
function as a peer-to-peer process. The survey reviewers must have experience in
maternal care and meet specific requirements for surveyor credentialing. The
surveyors review the hospital’s compliance with each of the defined designation
requirements and complete patient care reviews.
The review validates that the facility provides maternal standards of care and
follows established maternal guidelines. The surveyor evaluates that the facility has
established Quality Assessment Performance Improvement (QAPI) processes to
assess situations in which variances from the standard of care occur. The surveyor
reviews many forms of documentation, including the QAPI process and committee
minutes, outreach activities, multidisciplinary team education, and documented
evidence of the maternal program’s participation in their Perinatal Care Region.
The designation survey summary report includes the patient-care-record review
summaries, which are then submitted to the facility within 30 days of the survey
date. This report is submitted by the hospital to the department with a designation
application and a plan of correction for any deficiencies identified by the survey
organization. See Appendix B: Designation Process Summary for additional
information related to the designation process.
The hospital’s designation application is reviewed to verify documented evidence of
compliance with the designation requirements. The department provides
recommendations for designation to the DSHS commissioner. The commissioner or

8
designee makes designation decisions. Further details regarding the review
processes for the designation summary report are in Appendix B, Survey Process
Summary.
The DSHS commissioner awarded maternal level of care designations to 222
facilities by September 1, 2021. Every facility that met the requirements for a
maternal level of care designation received a designation award letter. For hospitals
that did not receive their desired designation level, DSHS provided a written
summary and outlined processes to meet compliance. These facilities were awarded
designation at the level where they demonstrated compliance with the designation
requirements.
Below is a breakdown of the 222 hospitals by the maternal level of care designation
awarded. A map detailing the geographic location of the Texas maternal designated
facilities by level is available in Appendix C, Texas Maps of Maternal Designated
Facilities.
● Level IV, Comprehensive Care – 32
● Level III, Subspecialty Care – 44
● Level II, Specialty Care – 93
● Level I, Basic Care – 53
Of the 222 designated hospitals, 16 hospitals (approximately 7 percent) were
initially designated at a lower level than requested by the hospital. This cohort was
seeking Level III or Level IV designation. These 16 hospitals were designated at the
highest demonstrated level of care for which minimum requirements were met.
● Designated as a Level II with a Level III application – 11 hospitals
● Designated as a Level III with a Level IV application – 5 hospitals
Appeals Process
As defined in the rule (TAC Section 133.204(e)), if a hospital disagrees with the
designation level awarded, the facility can request an appeal. The appeal process
includes two levels of appeal and the opportunity to dispute the findings of the
original survey. The current appeals process requires the facility to submit a written
appeal within 60 days of receiving the department’s formal designation award. This
appeal is to the DSHS EMS/Trauma Systems director. If the first level of appeal
review upholds the original determination, the designation level remains
unchanged. The facility will receive a written summary of the appeal and appeal
9
decisions. If the hospital disagrees with this decision, the hospital can request in
writing a second level appeal with the DSHS Consumer Protection Division’s
associate commissioner.
Thirteen of the 16 hospitals that were designated at a level lower than their
application submitted an appeal. Through the appeals process, these hospitals
submitted additional evidence of their care, capabilities, and documented evidence
of compliance to specific designation requirements. Twelve hospitals obtained their
requested designation through the appeals process. One hospital chose to complete
a full maternal survey two years later. At that time, the facility demonstrated
program improvements and compliance with all designation requirements and was
designated at the level originally requested. Therefore, the final determinations
resulted in approximately 99 percent of the total number of hospitals (222)
receiving designation at their requested level.
The department is currently updating the appeals process and has drafted
guidelines to implement the appeal panel defined in S.B. 749. The appeal panel
guidelines were reviewed and approved during the February 7, 2022 meeting of the
Perinatal Advisory Council (PAC). The revised appeal process establishes a seven-
member panel, with expertise in maternal care. One of the seven panel members
will participate in a designation appeal along with a member from the department
and a representative from the Health and Human Services Commission.

10
Evaluation
DSHS analyzed maternal designation applications to ascertain the evidence of
services available, care provided, and patient disposition to determine a hospital’s
compliance with the TAC Section 133.205. In addition, DSHS performed an in-depth
retrospective analysis of patient record reviews submitted with a Level II, III, or IV
application to evaluate the documented abilities of hospitals for each level of
designation.
The overall results of this review reflect that hospitals throughout the state provide
comparable services at each designation level. Examples of comparable hospital
services by designation level include:
● Level IV Maternal Facilities:
97 percent have skilled personnel with documented training,
competencies, and annual continuing education, specific for the
population served.
97 percent have a board-certified obstetrics and gynecology physician
with maternal privileges on-site and available for urgent situations at all
times.
94 percent ensure the capability to perform major surgery on-site.
91 percent have a Maternal-Fetal-Medicine Critical Care Team.
84 percent provide comprehensive care for the most complex medical,
surgical, or obstetrical conditions.
● Level III Maternal Facilities:
100 percent ensure the capability to perform major surgery on-site.
98 percent have an obstetrics and gynecology physician with maternal
privileges on-site and available for urgent situations at all times.
89 percent have skilled personnel with documented training,
competencies, and annual continuing education, specific for the
population served.
86 percent demonstrated care to patients with complex medical, surgical,
or obstetrical conditions.
● Level II Maternal Facilities:
100 percent demonstrated care to pregnant and postpartum patients with
medical, surgical, or obstetrical conditions presenting a low to moderate
risk of maternal morbidity or mortality.
11
91 percent have skilled personnel with documented training,
competencies, and annual continuing education, specific for the
population served.
91 percent have a board-certified, Maternal-Fetal-Medicine physician
available at all times for consultation.
● Level I maternal facilities completed a self-assessment to meet the
designation requirements and are not included in this comparison review.
Barriers to Requested Level of Designation
DSHS reviewed maternal designation survey reports and patient record reviews
from 169 facilities to identify barriers to designation. These records reflect 93
survey reports from Level II facilities with 1,538 patient care records. DSHS
reviewed 44 survey reports from Level III facilities with 764 patient care records,
and 32 survey reports from Level IV facilities with 824 patient care records.
Level IV Barriers
Five hospitals seeking Level IV designation did not initially meet the standards
outlined in rule. The primary reason a hospital did not achieve Level IV designation
was its inability to demonstrate it provided the full spectrum of care for pregnant
and postpartum patients, from low-risk conditions to the most complex medical,
surgical, or obstetrical conditions that present a high risk of morbidity or mortality.
The Level IV maternal facilities are designed to care for the most critical and
complex patients with all necessary resources at immediate availability. This level
of care includes specialists, subspecialists, and well-trained hospital personnel. In
some cases, the most critical patients were transferred to the hospital’s main
campus for intensive care. These main campus hospitals were not designated as
maternal facilities. In addition, these situations required the patient to be
transferred in an ambulance. In other situations, the lack of documentation from
the specialist led to the non-compliance of this specific requirement.
In further consultation with these facilities, DSHS identified the improvements
needed to demonstrate evidence of compliance. All five facilities were able to
present documentation during their appeal which resulted in them receiving their
requested Level IV designation.
12
Level III Barriers
Eleven hospitals seeking Level III designation did not initially meet the standards
outlined in rule. The primary reason hospitals did not achieve Level III designation
was an inability to demonstrate that they provide access to consultation to a full
range of medical and maternal subspecialists, surgical specialists, and behavioral
health specialists. Upon further review with these hospital administrators, medical
directors, and program managers, DSHS provided guidance of what is needed to
demonstrate evidence of compliance for this designation requirement.
Eight of the facilities appealed and provided documentation to meet the
requirement and obtained designation as a Level III maternal facility. Three
hospitals continued to improve their program and chose not to request an appeal.
One hospital completed a full re-survey for designation two years later and was
then designated as a maternal Level III facility. Two additional hospitals continue to
improve their programs and have surveys scheduled for later this year.
Level II Barriers
The most common designation barriers experienced by the Level II maternal
hospitals were related to an ineffective QAPI program, lack of team-based maternal
medical staff education and training, and lack of evidence of collaboration between
the maternal medical director and the maternal program manager. A few Level II
hospitals received deficiencies because they did not provide evidence to
demonstrate compliance with maternal management guidelines. These hospitals
completed a plan of correction and improved their processes to remove the
contingencies and achieve full designation.
Level I Barriers
All facilities requesting Level I status received the requested level of designation.
The most common potential designation barriers experienced by Level I maternal
hospitals were related to the lack of written policies and procedures specific to the
maternal program. Each hospital completed a plan of correction that allowed them
to achieve full designation. DSHS continues to provide guidance for these hospitals.
Comparison with Other States
DSHS compared the identified barriers to the three other states with established
maternal level of care designation requirements: Georgia, Indiana, and Louisiana.
The Texas maternal designation requirements identified as barriers were

13
comparable to these three states’ similar requirements. See AppendixD for the
specific comparison.
Geographic Considerations for Designation
Texas maternal level of care rules include consideration of a hospital’s location.
However, the geographic location alone does not define the designation decision.
Instead, every hospital with a maternal designation is required to participate in a
perinatal care region (PCR). A PCR aligns with the established boundaries of the
state’s trauma regional advisory councils. Designated maternal hospitals are
required to develop collaborative relationships and participate in a PCR’s
performance improvement initiative. The goal is to keep maternal patients and their
infants as close as possible to their support systems and provide safe, equitable,
timely, efficient, quality care for their unique situations. This creates a hub and
spoke model, where the higher designated hospitals (hubs) can provide outreach to
the lower-level designated hospitals (spokes) for implementing best practices,
education and collaboratives designed to improve the regional perinatal care.
There are 151 out of 254 Texas counties without a maternal designated hospital
(59.4 percent). However, most Texas counties that have a hospital have a maternal
designated facility (151 of 183). Specifically, 47 (18.5 percent) counties have a
designated Level I maternal hospital. Also, 55 percent of the Level I maternal
hospitals are farther than 50 miles from a Level III or Level IV maternal hospital. Of
the 94 Level II maternal facilities, 33 percent are farther than 50 miles from a Level
III or Level IV maternal hospital. The geographical distances between designated
hospitals underscore the need for the collaboration facilitated by perinatal care
regions.
The PCRs focus on maternal transport needs, education, and collaborative practice
to facilitate the movement or transfer of a maternal patient who requires a higher
level of care. Appendix C has the current maternal designation maps to reflect the
location of the maternal facilities. In addition, Appendix E contains geographic
considerations and reflect mileage considerations when transferring a patient.
Impact of COVID-19
The COVID-19 pandemic created challenges and barriers in 2020 and 2021.
Hospitals and survey organizations could not complete fully in-person surveys
required for Level II-IV designations. To address this, DSHS developed guidelines
to facilitate virtual survey options. Forty-two hospitals conducted virtual surveys. In
14
some situations, one reviewer was on-site, and the other surveyor participated
virtually. The department-approved survey organization collaborated with DSHS
and the hospitals to streamline functions and evaluate agendas to establish optimal
virtual survey guidelines.
The pandemic and staffing challenges continue to impact the designated maternal
hospitals. Some hospitals have responded to the challenges in varying ways,
including entering into diversion status for maternal care, leading to patients in
labor to be transferred to other hospitals, discontinuation of perinatal services, and
consolidation of maternal care with other facilities within a hospital system.
Improvement in Maternal Care
The maternal level of care rules were adopted in March 2018 with 222 hospitals
completing the designation process by September 2021. Comprehensive metrics of
improvements in maternal outcomes cannot be determined at this time. However,
DSHS has identified many small advances in processes and care through hospital
designation applications, documented plans of correction, site visits, and
discussions with hospital program staff.
DSHS has identified improvements in facility QAPI programs and systems of
maternal care coordination and collaboration, not only in the designated facilities
but also in the PCRs. The QAPI program evaluates the provision of maternal care
and emphasizes a multidisciplinary approach to continuous improvement for the
system, patient management and outcomes. The QAPI program is the core and
strength of any designation program. Implementation of a robust maternal
systemwide QAPI process is an area of opportunity throughout the state. This
requires established data elements, monitoring systems, and processes to compare
benchmarking and risk-adjusted outcomes.
An identified system strength is the Perinatal Care Regions (PCRs). PCRs are
geographically aligned with and are supported by the RAC. The PCRs have
established perinatal committees. Maternal designated facilities collaborate in these
regional committees to discuss issues that affect the system delivery of care and to
share best practices in this regional forum. The PCR committee chairs meet every
quarter to identify quality improvement initiatives that can be implemented in all 22
PCRs. Many PCR chairs attend the Perinatal Advisory Council meetings in
conjunction with the PCR meetings and may provide feedback on their quality
improvement initiatives at the PAC meeting. This strengthens the collaboration
between the PAC, PCR, hospitals, and the regional systems of care.

15
DSHS Actions and Next Steps
Draft guidelines for the perinatal appeal panel and the designation waiver guidelines
will be discussed at future PAC meetings.
DSHS initiated conference call meetings with stakeholders across the state to
provide an open forum to discuss issues that impact the maternal and neonatal
levels of designation and to share facility best practices. A major focus in 2021 was
stakeholder calls to prepare facilities for completing the designation application,
preparing for surveys, and building an effective QAPI plan. The chair and vice-chair
of the PAC are included in these stakeholder calls. In addition, DSHS met with
individual hospitals to answer questions and assist them in meeting designation
requirements. DSHS provided explanations and examples of ways to document
compliance.
DSHS reviewed and revised internal and external maternal-related designation
documents to incorporate feedback and opportunities improve designation review
workflows. For example, DSHS is revising the survey guidelines to integrate the
opportunities identified in the survey reviews. These survey guidelines outline the
expectations for the DSHS-approved survey organizations and define the surveyor
credentialing and performance expectations. The survey guidelines will be reviewed
internally and shared with the PAC. These guidelines integrate the processes for the
virtual surveys.
DSHS collaborated with two PAC subcommittees focused on implementing House
Bill 1164 (H.B. 1164), 87th Legislature, Regular Session, 2021 and reviewing
telehealth/telemedicine requirements. DSHS integrated the PAC’s rule
recommendations for managing placenta accreta spectrum disorder and
telehealth/telemedicine into the current maternal rules.
The maternal rules incorporating previous recommendations from the PAC, placenta
accreta spectrum disorder requirements, and telehealth/telemedicine rule
recommendations are in the formal Health and Human Services (HHS) rulemaking
process. These proposed rules were open for informal comment from January 31
through February 14, 2022. The proposed rules will be considered by the HHS
Executive Council prior to appearing in the Texas Register as proposed rules for
formal comment.

16
4. Conclusion
The Texas maternal level of care designation requirements are consistent with the
nationally recognized and accepted American College of Obstetricians and
Gynecologists and Society for Maternal-Fetal Medicine guidelines and are
comparable to nine other states with similar programs.
DSHS performed a strategic review encompassing analysis of hospital survey
reports, patient record reviews, relevant to current designation rules, geographical
considerations, and level of care designation requirements in other states. DSHS
identified the following barriers that impacted hospitals from potentially receiving
their initial requested level of designation:
● Level IV - not providing comprehensive care for pregnant and postpartum
patients with low-risk conditions to the most complex medical, surgical, or
obstetrical conditions and their fetuses, that present a high risk of maternal
morbidity or mortality.
● Level III - not ensuring access to consultation to a full range of medical and
maternal subspecialists, surgical specialists, and behavioral health
specialists.
● Level II – effective QAPI processes, medical staff team-based education and
training, and evidence of collaboration between the maternal medical director
and the maternal program manager.
● Level I – written policies and procedures specific to the maternal program.
There are currently 222 designated maternal facilities in Texas. Following the initial
designation to meet the September 2021 deadline for Medicaid reimbursement, 206
facilities received their requested level of designation. 14 facilities either appealed
or utilized a new survey to establish compliance with the requirements for their
requested level of designation. In total, 99 percent of facilities ultimately received
their requested level of designation.
The maternal rules incorporating recommendations from the PAC are in the formal
Health and Human Services (HHS) rulemaking process. The proposed rules will be
considered by the HHS Executive Council prior to appearing in the Texas Register
as proposed rules for formal comment.
17
List of Acronyms
Acronym
Full Name
AAP
American Academy of Pediatrics
ACOG
American College of Obstetricians and Gynecologists
DSHS
Department of State Health Services
EMS
Emergency Medical Services
MMD
Maternal Medical Director
MPM
Maternal Program Manager
PAC
Perinatal Advisory Committee
PCR
Perinatal Care Region
QAPI
Quality Assessment and Performance Improvement
RAC
Regional Advisory Council
TAC
Texas Administrative Code
TSA
Trauma Service Area
A-1
Appendix A. Literature Review Sources
“CDC Levels of Care Assessment Tool (CDC Locate).” Centers for Disease Control
and Prevention, Centers for Disease Control and Prevention, 16 June 2021,
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/cdc-
locate/index.html.
Code of Massachusetts, CMR 130.000: Hospital Licensure, Reg. Title 105 547-
604.30, 17 July 2017. https://www.mass.gov/regulations/105-CMR-13000-
hospital-licensure
Part 640 Regionalized Perinatal Health Care Code: General Assembly Illinois
Administrative Code, Illinois Admin. Code, title 77, ch. I, sub-ch. 1, §640
Regionalizes Perinatal Health Care Code, Vol 35 Ill. Reg. 2583, 31 January
2011.https://www.ilga.gov/commission/jcar/admincode/077/07700640sections.ht
ml
Illinois Department of Public Health. Report for the Illinois Perinatal Advisory
Committee. Maternal and Neonatal Levels of Care in Illinois, 2016.
https://dph.illinois.gov/content/dam/soi/en/web/idph/files/publications/data-
report-illinois-levels-care.pdf
“Indiana Perinatal Levels of Care Program.” Indiana Department of Health, 2021,
https://www.in.gov/health/mch/indiana-perinatal-levels-of-care-program/indiana-
perinatal-levels-of-care-program/
“Level of Care - Arkansas Department of Health.” Health Arkansas,
https://www.healthy.arkansas.gov/images/uploads/LevelofCare.pdf
“Maryland Perinatal System Standards 2013-Final 11.4.” Healthy Maryland,
https://health.maryland.gov/phpa/mch/Documents/Maryland_Perinatal_System_St
andards_2013.pdf
Maternal & Child Health Section, Office of Family and Community Health. Core
Requirements and Recommended Guidelines for Designated Regional Perinatal
Centers, May 2017,
https://dph.georgia.gov/sites/dph.georgia.gov/files/related_files/document/Core%2
0Requirements%20and%20Guidelines%20%206.14.17.pdf
“Maternal and Neonatal Center Designation Program.” Georgia Department of Public
Health, https://dph.georgia.gov/maternal-and-neonatal-center
A-2
“Maternity and Newborn Facilities.” Ohio Department of Health.
https://odh.ohio.gov/wps/portal/gov/odh/know-our-programs/maternity-and-
newborn-facilities/maternityadnnewbornfacilities
NY Codes, Rules, and Regulations. Title 10, Ch. V, sub-ch. C, Part 721.3: Perinatal
Designation of Hospitals. 2019.
NY Codes, Rules, and Regulations. Title 10, Ch. V, sub-ch. A, Part 405.21: Perinatal
Services. 2019.
Practice, AAP Committee on Fetus and Newborn, and ACOG Committee on
Obstetric. “Guidelines for Perinatal Care.” Guidelines for Perinatal Care, AAP Books,
American Academy of Pediatrics, 17 Sept. 2017,
https://publications.aap.org/aapbooks/book/522/Guidelines-for-Perinatal-
Care?autologincheck=redirected
Missouri Code of State Regulations - “Rules of Department of Health and Senior
Services - Missouri.” sos.mo.gov,
https://www.sos.mo.gov/CMSImages/AdRules/csr/current/19csr/19c20-60.pdf
South Carolina Code of Regulations – Designation of Inpatient Perinatal Care
Services - “S.C. Code Regs. § 61-16.1306.” Casetext, 24 Sept. 2021,
https://casetext.com/regulation/south-carolina-code-of-regulations/chapter-61-
department-of-health-and-environmental-control/subchapter-61-16-minimum-
standards-for-licensing-hospitals-and-institutional-general-infirmaries/section-61-
161300-perinatal-services/section-61-161306-designation-of-inpatient-perinatal-
care-services
American College of Obstetricians and Gynecologists Levels of Maternal Care -
“State Implementation.” ACOG, 2021, https://www.acog.org/programs/lomc/state-
implementation
Tennessee Department of Health Division of Family Health and Wellness. Guidelines
for Regionalization, Hospital Care Levels, Staffing and Facilities, Seventh Edition.
Tennessee Perinatal Care System. 2021,
https://www.tn.gov/content/dam/tn/health/documents/Regionalization_Guidelines_
Approved_2014.pdf Accessed Oct. 17, 2019.
“Title: Section 721.6 - Qualification and Responsibilities of Physicians and Other
Licensed Obstetrical Practitioners at Each Designated Level of Care.” New York
Codes, Rules and Regulations, 14 Sept. 2005,
A-3
https://regs.health.ny.gov/content/section-7216-qualification-and-responsibilities-
physicians-and-other-licensed-obstetrical
“Title 44 - Health CHAPTER 89 Birthing Center Licensure Act.” South Carolina
Legislature, https://www.scstatehouse.gov/code/t44c089.php#44-89-300
Washington State Department of Health. Washington State: Perinatal and Neonatal
Level of Care (LOC) 2018 Guidelines. 2018 Barfield, MD, MPH, CAPT Wanda Denise
& Papile, MD, FAAP, Lu-Ann.
American Academy of Pediatrics, American College of Obstetricians and
Gynecologists. Guidelines for Perinatal Care. 8th Ed. USA: American Academy of
Pediatrics; 2017.
VOLUME E (Title 10) SubChapter –C - State Hospital Code Article –3 - Hospital
Operation Part 72–1 - Perinatal Regionalization Section 721–6 - Qualification and
Responsibilities of Physicians and Other Licensed Obstetrical Practitioners At Each
Designated Level of Care | New York Codes, Rules and Regulations (ny.gov).
https://regs.health.ny.gov/content/section-7216-qualification-and-responsibilities-
physicians-and-other-licensed-obstetrical
Arkansas Department of Health. Arkansas Neonatal and Maternal Levels of Care
Regulations for Levels 1, 2, 3A, 3B, and 4. Arkansas Perinatal Level of Care
Regulations. 2014.
Georgia Department of Public Health. Core Requirements and Recommended
Guidelines for Designated Regional Perinatal Centers. Maternal & Child Health
Section, Office of Family and Community Health Perinatal Health Unit. 2013.
https://dph.georgia.gov/maternal-and-neonatal-center 3/19/2020
Illinois Admin. Code, title 77, ch. I, sub-ch. 1, §640 Regionalizes Perinatal Health
Care Code, Vol 35 Ill. Reg. 2583, 31 January 2011.
Illinois Department of Public Health. Report for the Illinois Perinatal Advisory
Committee. Maternal and Neonatal Levels of Care in Illinois, 2016.
Indiana Department of Health - Indiana Perinatal Levels of Care Program.
https://www.in.gov/health/mch/indiana-perinatal-levels-of-care-program/indiana-
perinatal-levels-of-care-program/
A-4
Title 410 Indiana State Department of Health, Article 39. Perinatal Hospital
Services. https://www.in.gov/health/mch/files/18-416-Final-Rule.pdf
Tennessee Department of Health Division of Family Health and Wellness. Guidelines
for Regionalization, Hospital Care Levels, Staffing and Facilities, Seventh Edition.
Tennessee Perinatal Care System. 2014.
Washington State Department of Health. Washington State: Perinatal and Neonatal
Level of Care (LOC) 2018 Guidelines. 2018 Barfield, MD, MPH, CAPT Wanda Denise
& Papile, MD, FAAP, Lu-Ann.
Arkansas Department of Health – Arkansas Neonatal and Maternal Levels of Care
Regulations for Levels 1, 2, 3A, 3B and 4.
https://www.healthy.arkansas.gov/images/uploads/LevelofCare.pdf
Mary M, DAS P, Creanga AA. Perinatal telemedicine at lower-level birthing hospitals
in Maryland. Lessons learned from a landscape analysis. Minerva Obstet Gynecol.
2021 Sep 9. https://pubmed.ncbi.nlm.nih.gov/34498838/ DOI: 10.23736/S2724-
606X.21.04933-2
American College of Obstetricians and Gynecologists - Programs, Levels of Maternal
Care, State Implementation.
https://www.acog.org/programs/lomc/state-implementation
Centers for Disease Control and Prevention – CDC Levels of Care Assessment Tool.
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/cdc-
locate/index.html
Missouri Secretary of State: Code of State Regulations – Rules of Department of
Health and Senior Services, Division 20 – Division of Community and Public Health,
Chapter 60 – Maternal and Neonatal Care.
https://www.sos.mo.gov/CMSImages/AdRules/csr/current/19csr/19c20-60.pdf
Wisconsin Association for Perinatal Care – position statements.
https://perinatalweb.org/page/positionstatements
South Carolina Code of Regulations – Chapter 61 Department of Health and
Environmental Control, Designation of Inpatient Perinatal Care Services – S.C. Code
Regs §61-16.1306
https://www.scstatehouse.gov/coderegs/Chapter%2061-1%20through%2061-
17.pdf
A-5
South Carolina Code of Laws - Title 44 - Chapter 89 - Birthing Center Licensure Act.
https://www.scstatehouse.gov/code/t44c089.php#44-89-300
Maryland Perinatal System Standards 2013-Revised Nov. 4, 2013
https://health.maryland.gov/phpa/mch/Documents/Maryland_Perinatal_System_St
andards_2013.pdf
Ohio Department of Health’s Bureau of Regulatory Operations – Maternity and
Newborn Facilities.
https://odh.ohio.gov/wps/portal/gov/odh/know-our-programs/maternity-and-
newborn-facilities/maternityadnnewbornfacilities
Association of State and Territorial Health Officials.
https://astho.org
B-1
Appendix B. Designation Process Summary
Hospital compliance with the Texas Administrative Code (TAC) Section 133.205 is
determined through evidence of Perinatal Care Region participation, survey
findings, and patient record reviews. The designation application includes the
survey report with the patient record reviews that detail the hospital’s compliance
with the defined designation rules.
● Level I hospital applications require submission of a self-survey report with
an administrative attestation to confirm compliance with the rules.
● Level II, III and IV hospitals require submission of a survey report with the
patient record reviews documenting requirement compliance from
department-approved survey organizations before application. The hospital
chooses one of the department-approved survey organizations to perform its
survey and contracts for services with that organization.
For maternal levels of care, the American College of Obstetricians and
Gynecologists (ACOG) and the Texas EMS Trauma and Acute Care Foundation
(TETAF) are DSHS-approved survey organizations. They complete the designation
surveys to verify compliance with the maternal level of designation requirements.
The level of designation a hospital requests defines the survey team and processes.
The pandemic response created the need for virtual surveys. DSHS implemented
virtual survey guidelines to continue the maternal designation reviews to meet the
August 31, 2021, deadline.
The individual survey organizations select surveyor candidates to participate in a
maternal surveyor course to gain essential knowledge and skills before a survey is
conducted. The survey organizations are responsible for the credentialing of each of
the selected surveyor applicants as identified in the rules, 25 Tex. TAC §133.190
(2019) (DSHS, Survey Team). Every surveyor must be a practicing professional
with relevant experience and knowledge of maternal care. The surveyors must also
meet the geographical distance restrictions defined in the rules and must have no
conflicts of interest with the hospital they survey.
Survey organizations must define their survey process and methodology, as well as
their tools, to ensure compliance and/or noncompliance with designation
requirements. These processes must align with the DSHS survey guidelines. Survey
teams consist of multidisciplinary professionals. Team size and composition are
based on the requested level of designation. As an example, if a hospital is applying
B-2
for Level IV designation, it must be surveyed by a registered nurse and an
obstetrician as well as a maternal-fetal medicine specialist.
Once the survey is completed, the survey organization must provide its summary
reports to the hospital no later than 30 days after the date of the survey. The
hospital then completes a plan of correction for any identified potential deficiencies,
completes its application packet, and submits an application packet to DSHS within
120 days of the survey date.
Once DSHS receives an application from a hospital, a DSHS perinatal designation
coordinator, who is a registered nurse with perinatal experience, performs a desk
review that includes an in-depth analysis of the survey report findings and patient
record reviews submitted by the hospital. The purpose of this review is to verify
documented evidence of compliance with the requirements. The quality of the
survey report and completeness of the report is determined. The designation is
then recommended to the DSHS commissioner or designee based on compliance
with the requirements.
The individual surveyor summaries and patient care records are reviewed and
tracked for compliance with the current survey guidelines to share with the
appropriate approved survey organization.
B-3

B-4
Perinatal Designation Application Review Process
1. The designation administrative assistant or other designation staff receive
perinatal designation application packets by physical mail or electronically
in the DSHS.EM[email protected]as.gov inbox.
2. The designation staff member will review the designation application packet
for required documents. All physical application packets will be scanned to
an electronic file. The designation application packet requires the following:
a. a complete designation application form for the appropriate level of
designation;
b. the designation fee;
c. a designation survey report, including case reviews or a completed
attestation and self-survey report;
d. evidence of participation in the application RAC/PCR;
e. a plan of correction if needed; and
f. any subsequent documents requested by the department.
Application information data received are entered into the database and the
perinatal log for review. The application packet is then electronically sent to
the Perinatal Designation Coordinators and filed in the facility folder.
3. The Designation Coordinator will review the designation application form to
ensure it is complete for the appropriate level of designation including:
a. Ensure all requested information is provided
i. Hospital Demographic information
ii. Hospital information (TSA, TPI, License# and Beds)
iii. Fee amount
iv. Level requested
v. Designation type
vi. Program Manager, Medical Director and Chief Executive Officer
information.
vii. Chief Executive Officer or designee signature with date.
viii. Statistical information
ix. Program Manager and Medical Director signatures with dates.
b. Verify the designation application fee has been received and deposited
by Cash Receipts Branch Office.
B-5
i. Check the corresponding database to verify if the payment has
been processed.
ii. The remit information is located in the Payment Coupon screen
of each database.
iii. Verify that the correct fee amount and current date is
documented in the Payment Coupon fields. Completed
information indicates the fee has been received and the
application review may proceed.
iv. If the information is not current or blank, contact a designation
staff member with Cash Branch access to verify the fee online.
Once the fee has been verified online, the application review
may proceed.
v. If the fee is not verified in the database or online, mark the fee
as pending.
vi. The application is incomplete and cannot be recommended until
the fee is received.
c. Verify that all pages of the designation survey report, and all medical
record reviews are present if applicable.
d. Verify the RAC/PCR letter of participation is present and reflects the
facility meets the participation requirements. A facility that does not
meet the RAC/PCR requirements is considered non-compliant until the
participation letter is submitted. A plan of correction to achieve
compliance may be considered.
e. If designation requirements are not met and identified potential
deficiencies are defined, a correction action plan must be included in
the application packet and reviewed.
f. The plan of correction with supporting documentation is reviewed to
identify if the facility is making progress in meeting the designation
requirements.
i. Ensure all potential deficiencies are listed and addressed in the
plan of correction (POC).
ii. Ensure all elements of the plan of correction are included and
appropriate:
1. any deficiencies cited in the survey report;
2. the corrective action;
3. the title of the person responsible for ensuring the
correction(s) is implemented.
iii. How the corrective action will be monitored; and
iv. The date by which the POC will be completed.
g. Verify any subsequent documents requested by the department are
attached. Subsequent documents may be a Board Resolution, Medical
B-6
Staff Resolution, or any other documentation requested by the
department.
4. The Designation Coordinator determines if the application packet is
complete.
a. If all documents are provided, the Designation Coordinator will notify
the facility that the application packet is complete and in the review
process.
b. If documents are missing, the Designation Coordinator will contact the
facility designation program manager and notify the facility of the
missing documents and that the application review process will be on
hold, waiting on receipt of the required documents.
5. The designation application packet review will continue if all documents are
complete and present with the exception of the fee. The Designation
Coordinator will:
a. Review the survey report for surveyor identified compliance,
noncompliance, or weakness with requirements.
b. Verify if the surveyor documented evidence to support the identified
findings.
c. Review the medical record review documentation to identify evidence
supporting facility compliance, noncompliance, or weakness with the
rule requirements for the requested level of care.
d. Verify the medical record review documented evidence supports the
findings documented in the survey report.
e. Review the plan of correction and supporting documentation to verify
all potential criteria deficiencies identified by the surveyors are
addressed appropriately.
i. The corrective action must include a detailed plan to achieve
compliance.
ii. The position responsible for implementing the corrective action
must be appropriate and the action within their responsibilities.
Example – The Program Manager cannot be responsible for
physician interventions, physician recruitment or other
corrective actions outside of their responsibilities.
iii. The corrective action monitoring includes a detailed plan and
specified time frame.
iv. The date the POC is completed must be acceptable for the
specific deficiency to meet compliance as quickly as possible.
f. Verify the plan of correction is complete, acceptable, and addresses
the potential deficiencies cited in the survey report or for RAC
participation.
B-7
g. If supporting documentation is submitted with evidence of compliance
for the potential criteria deficiency or RAC participation, the
Designation Coordinator will determine the deficiency is met.
h. If the POC and/or supporting documentation are approved and
implemented, the Designation Coordinator may determine the
potential criteria deficiency as met.
i. If the POC is incomplete or not acceptable, the potential criteria
deficiency may remain as “not met.”
j. If the Designation Coordinator has questions regarding the
documentation in the survey report or medical record reviews
requiring clarification or explanation, the survey organization will be
contacted for additional information. The Designation Coordinator and
Designation Program Manager will meet with the survey organization
representatives.
k. If the Designation Coordinator has questions regarding application
documents or the plan of correction, the facility program manager will
be contacted for additional information. If the CEO, CNO or Medical
Director are needed, the Designation Coordinator and Designation
Program Manager will meet with the facility representatives.
l. If the Designation Coordinator has questions regarding the RAC/PCR
participation letter, the RAC will be contacted for additional
information. The Designation Coordinator and Designation Program
Manager will meet with the RAC/PCR representative.
m. Additional information received from the survey organization, facility
or RAC/PCR will be included in the summary as appropriate and
considered to determine if the facility meets the minimum
requirements for the level of care requested.
n. The Designation Coordinator will complete a summary of the findings
from the designation application packet review.
o. The Designation Coordinator will determine if the facility meets the
minimum requirements for designation at the level of care requested.
6. If the Designation Coordinator determines the facility successfully meets the
minimum requirements for designation at the level of care requested, a
recommendation for designation at the level requested will be initiated.
7. If the Designation Coordinator determines the facility does not meet the
minimum criteria, the Designation Program Manager will be notified of the
findings. The Designation Coordinators and Designation Program Manager
will meet to review the designation application packet and summary of
findings.
B-8
a. If determined that the facility meets the minimum requirements for
designation at the level of care requested, a recommendation for
designation at the level requested will be initiated and approved.
b. If determined that the facility does not meet the minimum
requirements for designation at the level of care requested, the
EMS/Trauma Systems Director will be notified.
i. The Designation Program Manager will provide the facility
application documents, review summary and proposed
designation determination to the Director for review and
consideration.
ii. The Director will review the documents and make a final
designation determination.
iii. The Director will notify the Designation Program Manager of the
designation determination, recommendations, or a corrective
action plan.
iv. The Designation Program Manager will provide the final
determination and approval to the appropriate Designation
Coordinator to initiate the recommendation and develop a
corrective action plan if required.
c. The Designation Coordinator or Designation Program Manager will
notify the facility when the application review is complete. The
Designation Coordinator will document the date of the application
review completion.
d. If a facility is recommended for a Contingent Designation, the
Designation Staff will schedule a conference call/virtual meeting with
the facility.
8. The Designation Coordinator will send a designation recommendation to the
Designation Program Manager and Designation Program Specialist. The
Program Manager will review the recommendation for the correct program,
level, and new expiration date. The Designation Program Manager will
approve the recommendation and send it to the Designation Program
Specialist for processing.
9. The Designation Program Specialist will develop the Action Memo,
designation letter, certificate and spreadsheet as required with the correct
facility information to submit to the Associate Commissioner for approval.
Designation documents for approval may be compiled by program and levels
for approval.
10.The designation recommendation approval packets are reviewed by the
Designation Program Manager and sent to the EMS/Trauma Systems
Director for review and approval. The EMS/Trauma Systems Director will
B-9
sign facility certificates and send approved recommendations to the
Associate Commissioner for review and approval.
11.The Associate Commissioner will contact the EMS/Trauma Systems Director
for any questions or clarifications on recommendations.
12.The designation staff will update any documents as required and resubmit
them to the Associate Commissioner for approval.
13.The Associate Commissioner will sign the facility designation letters and
certificates for approved recommendations.
14.The signed letters and certificates will be returned to the Designation
Program to be issued to the facilities. Electronic copies of the signed letters
and certificates will be issued to the facility CEO, Medical Director and
Program Manager as available.
15.An appeal may be submitted by a facility that did not receive the
designation requested. If an appeal is submitted, the EMS/Trauma Systems
Director, Designation Program Manager and Designation Coordinators will
meet to review the appeal and original designation determination. The
EMS/Trauma Systems Director will make the designation determination for
all appeals.
16.Designations approved or awarded by the Associate Commissioner will be
added or updated on the DSHS Designation webpages and in the database.
C-1
Appendix C. Texas Maps of Maternal Designated
Facilities
C-2
C-3
C-4
C-5
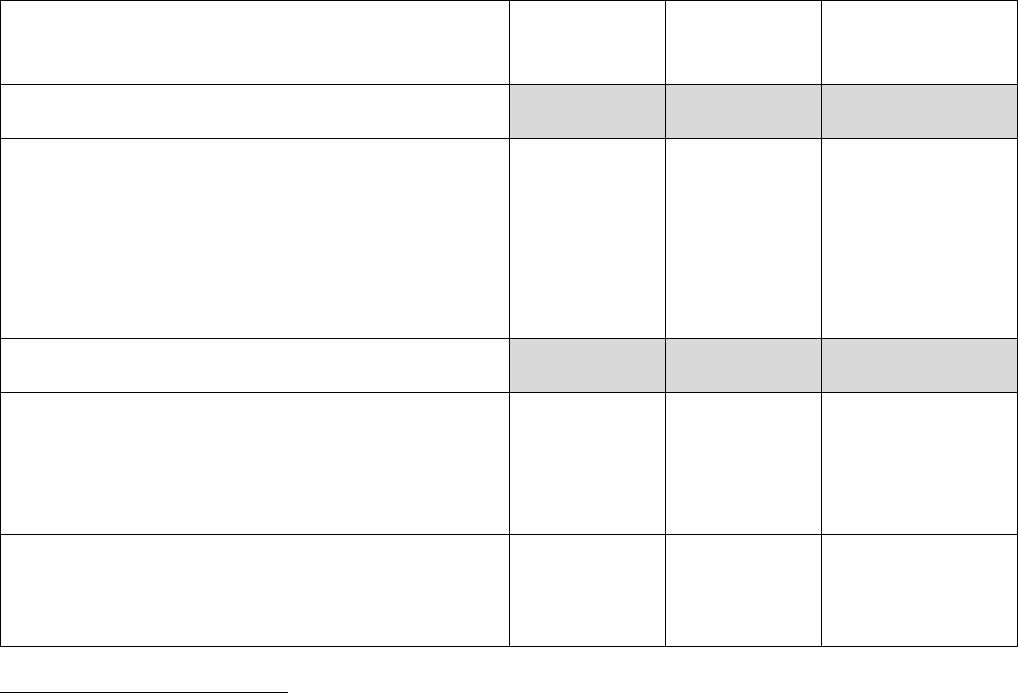
D-1
Appendix D. Texas Maternal Level of Care
Designation Requirements defined as barriers to
achieving the hospital’s desired designation level
compared to the other state designation requirements.
Identified Texas Designation Requirement
Barriers
Georgia
i
Indiana
ii
Louisiana
iii
Level IV Barrier
133.209(a)(1) Providing comprehensive care
for pregnant and postpartum with low-risk
conditions to the most complex medical,
surgical, and/or obstetrical conditions and their
fetuses, that present a high risk of morbidity or
mortality.
UK
√
√
Level III Barriers
133.208(a)(2) Ensuring access for consultation
from a full range of medical and maternal
subspecialists, surgical specialists, and
behavioral specialists,
√
√
√
133.208(d)(5) Maternal-Fetal Medicine
physician with the availability to arrive at the
Required to
be readily
available at
Required to
be readily
available at
Required to be
readily available
at all times
i
Georgia Department of Public Health notes that their requirements and guidelines reflect
current edition of the Guidelines for Perinatal Care, AAP and ACOG.
ii
Indiana State Department of Health (ISDH) states that they developed their standards
“based on the requirements of the American College of Obstetrics and Gynecology (ACOG),
the American Academy of Pediatrics (AAP), the Association of Women’s Health and Obstetric
Nurses (AWOHN) and other medical professional organizations.”
iii
Louisiana Administrative Code states that, “Obstetrical services shall be provided in
accordance with acceptable standards of practice as delineated in the 2014 AAP/ACOG
Guidelines for Perinatal Care.” LAC 48:I.Chapter 93 §9507.C
D-2
patient bedside within 30 minutes of urgent
request
all times
onsite, by
telephone or
telemedicine.
Must be
physically
present to
provide
direct care
within 24
hours.
all times
onsite, by
telephone or
telemedicine.
Must be
physically
present to
provide
direct care
within 24
hours.
onsite, by
telephone or
telemedicine and
in person onsite
as needed by the
facility.
Level II Barriers
133.205(b)(2)(F) Documented QAPI Program
Requires
participation
in a perinatal
quality
collaborative
but not
specific to
on-site QAPI
√
√
133.207(c)(12)(A) Anesthesia personnel with
training and expertise in obstetrical anesthesia
Board
certified in
anesthesia
but does not
address
training and
expertise.
Board
certified in
anesthesia
but does not
address
training and
expertise.
√
133.205(d)(6) & 133.205(e)(4) Maternal
Medical Director and Maternal Program Manager
collaboration
UK
UK
UK
133.207(c)(3), 133.207(c)(5),
133.207(c)(8)(A), 133.207(c)(11),
133.207(c)(12)(A) Physician response to urgent
request
Required to
be readily
available at
all times but
does not
address 30-
minute
UK
Required to be
readily available
at all times but
does not address
30-minute
response time or
urgent request
D-3
response
time or
urgent
request
response.
response.
Requires 20-
minute response
time for
anesthesia.
133.207(c)(19) Social Services availability
√
UK
UK
133.205(b)(2)(A)(ii) Lack of dissemination of
policies and procedures and documentation to
reflect compliance.
UK
UK
UK
Level I Barriers
133.205(b)(2)(F) Documented QAPI Program
Requires
participation
in a perinatal
quality
collaborative
but not
specific to
on-site QAPI
√
√
133.206(c)(13) Written policies and procedures
specific to the maternal program
√
√
UK
State has the same or similar requirement = Check Mark (√).
State does not have the same or similar requirement = X
Unable to determine = UK
E-1
Appendix E. Geographic Considerations and
Mileage
Women living in rural areas may have the greatest distances to travel for accessing
higher-level neonatal care. Women travel longer distances to a higher level of care
maternal hospitals as evidenced in the tables below. This distance may prevent
them from delivering in the most appropriate maternal facility.
Maternal designations are determined by verifying evidence of compliance with the
requirements in the rule. This standard consistency in the care provided through
the designation process assures consumers that maternal services do not differ
much from one geographical area to another. Designation informs patients, their
families, health care providers, and emergency medical services organizations,
about the hospital’s maternal level of care provided.
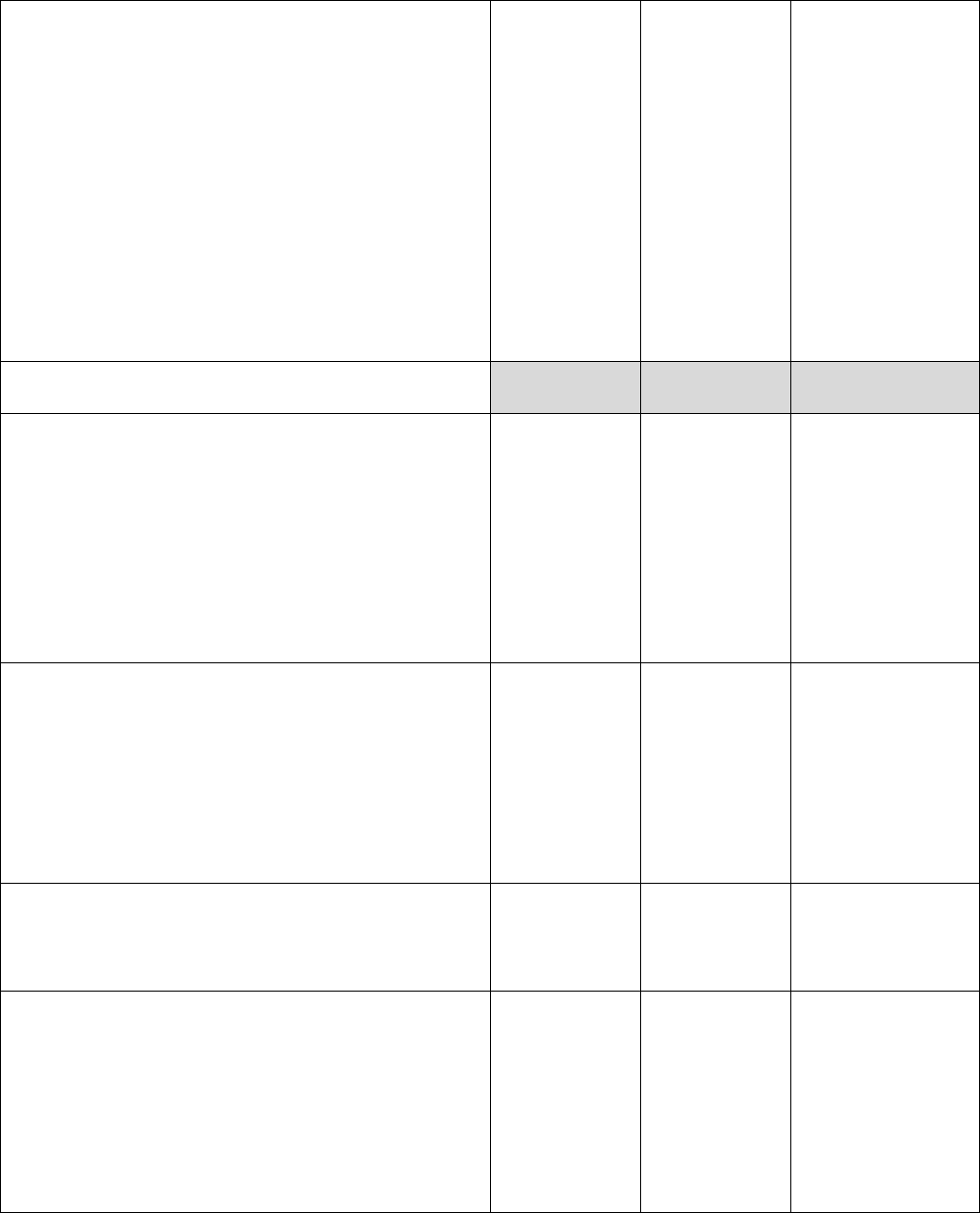
Table 1. Distance of Level I Maternal Facility from Level III or IV
Maternal Designated Facility
Twenty-nine (55 percent) of the 53 Level I maternal hospitals are located farther
than 50 miles from a Level III or IV maternal hospital.
Nearest Level III or IV
Level I (53)
More than 150 miles
0
100 – 149 miles
4
75-99 miles
10
50-74 miles
15
25-49 miles
19
Less than 25 miles
5
E-2
Table 2. Distance of Level II Facilities from Level III or Level IV
Maternal Designated Facility
Thirty-one (33 percent) of the 94 Level II hospitals are farther than 50 miles from a
Level III or IV maternal hospital. Fifty-one percent of Level II hospitals are less
than 25 miles from Level III or Level IV maternal hospitals.
Nearest Level III or IV
Level II (94)
More than 150 miles
0
100 – 149 miles
8
75-99 miles
12
50-74 miles
11
25-49 miles
15
Less than 25 miles
48
E-3
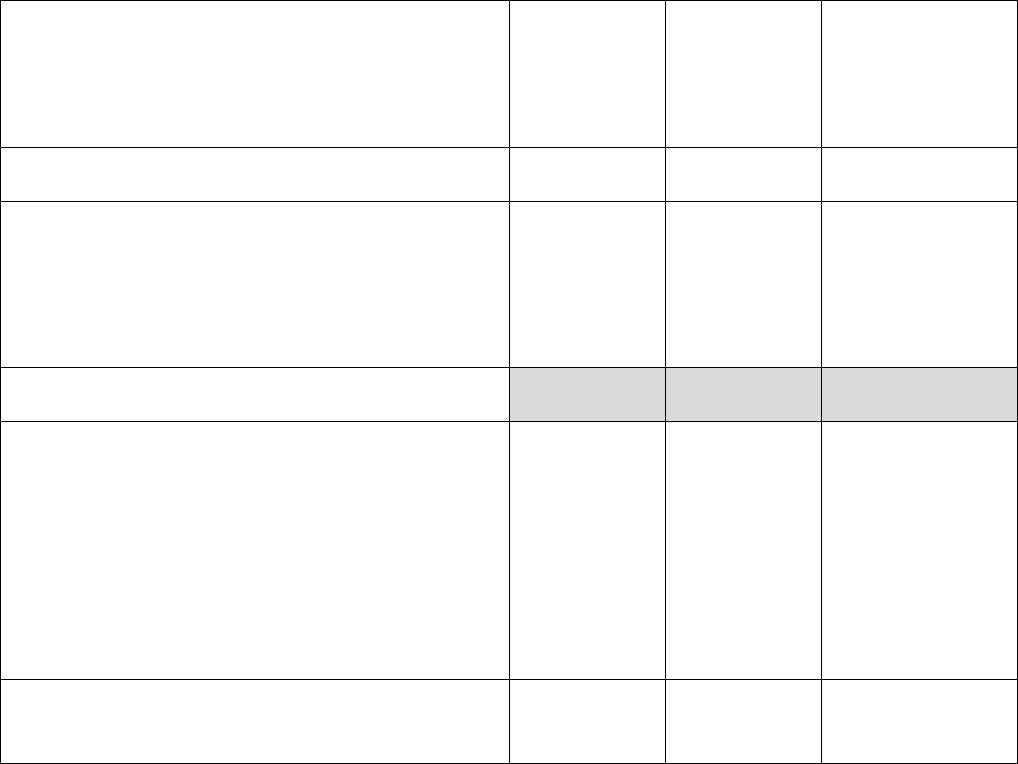
Table 3. Number of Counties Per Regional Advisory Council Without a
Maternal Designated Facility (151/254 or 59%)
TSA
Counties per
TSA
Counties Without a
Designated Facility
No Designated
Facility (%)
A
25
18
72%
B
22
14
64%
C
10
6
60%
D
16
12
75%
E
19
3
16%
F
8
4
50%
G
19
13
68%
H
7
4
57%
I
3
2
67%
J
17
10
59%
K
14
13
93%
L
6
5
83%
M
5
2
40%
N
7
5
71%
O
11
7
64%
P
22
10
45%
Q
9
3
33%
R
9
6
67%
S
6
3
50%
T
3
2
67%
U
12
8
67%
V
4
1
25%
Total
254
151
59%
E-4
Table 4. Counties with Maternal Level I Designated Facility
Forty-seven (18.5%) counties have only Level I Maternal Designated hospitals. Of
those, 38 are rural and nine are urban counties.
TSA
County
Facility
Designation
Level
Class
A
Childress
Childress Regional Medical Center
I
Rural
A
Deaf Smith
Hereford Regional Medical Center
I
Rural
A
Hartley
Coon Memorial Hospital and Home
I
Rural
A
Hutchinson
Golden Plains Community Hospital
I
Rural
A
Moore
Memorial Hospital***Dumas
I
Rural
A
Ochiltree
Ochiltree General Hospital
I
Rural
B
Gaines
Memorial Hospital***Seminole
I
Rural
B
Hale
Covenant Hospital Plainview
I
Rural
B
Hockley
Covenant Hospital Levelland
I
Rural
B
Lamb
Lamb Healthcare Center
I
Rural
B
Scurry
Cogdell Memorial Hospital
I
Rural
B
Terry
Brownfield Regional Medical Center
I
Rural
B
Yoakum
Yoakum County Hospital
I
Rural
C
Baylor
Seymour Hospital
I
Rural
C
Jack
Faith Community Hospital
I
Rural
C
Young
Hamilton Hospital
I
Rural
D
Coleman
Coleman County Medical Center
Company
I
Rural
D
Nolan
Rolling Plains Memorial Hospital
I
Rural
E
Cooke
North Texas Medical Center
I
Rural
E
Erath
Texas Health Harris Methodist
Hospital Stephenville
I
Rural
E
Palo Pinto
Palo Pinto General Hospital
I
Rural
E
Parker
Medical City Weatherford
I
Urban
F
Lamar
Paris Regional Medical Center North
Campus
I
Rural
G
Anderson
Palestine Regional Medical Center
I
Urban
E-5
TSA
County
Facility
Designation
Level
Class
G
Cherokee
UT Health East Texas Jacksonville
Hospital
I
Urban
G
Henderson
UT Health East Texas Athens
Hospital
I
Urban
G
Rusk
UT Health East Texas Henderson
Hospital
I
Urban
J
Brewster
Big Bend Regional Medical Center
I
Rural
J
Howard
Scenic Mountain Medical Center, a
Steward Family Hospital
I
Rural
J
Pecos
Pecos County Memorial Hospital
I
Rural
M
Bosque
Goodall - Witcher Hospital
I
Rural
M
Hill
Hill Regional Hospital
I
Rural
N
Washington
Baylor Scott & White Medical Center
- Brenham
I
Rural
P
Dimmit
Dimmit Regional Hospital
I
Rural
P
Frio
Frio Regional Hospital
I
Rural
P
Gonzales
Memorial Hospital***Gonzales
I
Rural
P
Medina
Medina Regional Hospital
I
Rural
Q
Matagorda
Matagorda Regional Medical Center
I
Rural
Q
Walker
Huntsville Memorial Hospital
I
Urban
R
Brazoria
CHI St. Luke’s Health - Brazosport
I
Urban
R
Brazoria
UTMB Health Angleton Danbury
Campus
I
Urban
S
Calhoun
Memorial Medical Center
I
Rural
S
DeWitt
Cuero Regional Hospital
I
Rural
U
Bee
CHRISTUS Spohn Hospital Beeville
I
Rural
U
Jim Wells
CHRISTUS Spohn Hospital Alice
I
Rural
U
Kleberg
CHRISTUS Spohn Hospital Kleberg
I
Rural
E-6
Table 5. Level of Maternal Designated Facilities Per Regional
Advisory Council or Trauma Service Area (TSA)
TSA
Facility Name
Designation
Level
County
A
Childress Regional Medical Center
I
Childress
A
Coon Memorial Hospital and Home
I
Hartley
A
Golden Plains Community Hospital
I
Hutchinson
A
Hereford Regional Medical Center
I
Deaf Smith
A
Memorial Hospital***Dumas
I
Moore
A
Ochiltree General Hospital
I
Ochiltree
A
Baptist St. Anthony’s Hospital
II
Potter
A
Northwest Texas Hospital
III
Potter
B
Brownfield Regional Medical Center
I
Terry
B
Cogdell Memorial Hospital
I
Scurry
B
Covenant Hospital Levelland
I
Hockley
B
Covenant Hospital Plainview
I
Hale
B
Lamb Healthcare Center
I
Lamb
B
Memorial Hospital***Seminole
I
Gaines
B
Yoakum County Hospital
I
Yoakum
B
Covenant Children’s Hospital
IV
Lubbock
B
University Medical Center
IV
Lubbock
C
Faith Community Hospital
I
Jack
C
Hamilton Hospital
I
Young
C
Seymour Hospital
I
Baylor
C
United Regional Healthcare System
II
Wichita
D
Coleman County Medical Center Company
I
Coleman
D
Hendrick Medical Center South
I
Taylor
D
Rolling Plains Memorial Hospital
I
Nolan
D
Hendrick Medical Center Brownwood
II
Brown
E-7
TSA
Facility Name
Designation
Level
County
D
Hendrick Medical Center
III
Taylor
E
Medical City Weatherford
I
Parker
E
North Texas Medical Center
I
Cooke
E
Palo Pinto General Hospital
I
Palo Pinto
E
Texas Health Harris Methodist Hospital
Stephenville
I
Erath
E
Texas Health Hospital Rockwall
I
Rockwall
E
Baylor Scott & White Medical Center -
Frisco
II
Collin
E
Baylor Scott & White Medical Center -
Grapevine
II
Tarrant
E
Baylor Scott & White Medical Center -
Irving
II
Dallas
E
Baylor Scott & White Medical Center -
Waxahachie
II
Ellis
E
City Hospital at White Rock
II
Dallas
E
Dallas Regional Medical Center
II
Dallas
E
Hunt Regional Medical Center Greenville
II
Hunt
E
Lake Granbury Medical Center
II
Hood
E
Medical City Alliance
II
Tarrant
E
Medical City Las Colinas
II
Dallas
E
Medical City Lewisville
II
Denton
E
Navarro Regional Hospital
II
Navarro
E
Texas Health Harris Methodist Hospital
Cleburne
II
Johnson
E
Texas Health Hospital Frisco
II
Collin
E
Texas Health Huguley Hospital
II
Tarrant
E
Texas Health Presbyterian Hospital Allen
II
Collin
E
Texas Health Presbyterian Hospital Flower
Mound
II
Denton
E
Texoma Medical Center
II
Grayson
E
Wilson N. Jones Regional Medical Center
II
Grayson
E
Wise Health System
II
Wise
E-8
TSA
Facility Name
Designation
Level
County
E
Baylor Scott & White Medical Center -
Centennial
III
Collin
E
Baylor Scott & White Medical Center - Lake
Pointe
III
Rockwall
E
Baylor Scott & White Medical Center -
McKinney
III
Collin
E
Medical City Arlington
III
Tarrant
E
Medical City Frisco, a Medical Center of
Plano Facility
III
Collin
E
Medical City McKinney
III
Collin
E
Methodist Charlton Medical Center
III
Dallas
E
Methodist Dallas Medical Center
III
Dallas
E
Methodist Mansfield Medical Center
III
Tarrant
E
Methodist Richardson Medical Center
III
Collin
E
Texas Health Arlington Memorial Hospital
III
Tarrant
E
Texas Health Harris Methodist Hospital
Alliance
III
Tarrant
E
Texas Health Harris Methodist Hospital
Hurst-Euless-Bedford
III
Tarrant
E
Texas Health Harris Methodist Hospital
Southwest Fort Worth
III
Tarrant
E
Texas Health Presbyterian Hospital Denton
III
Denton
E
Baylor Scott & White All Saints Medical
Center - Fort Worth
IV
Tarrant
E
Baylor University Medical Center
IV
Dallas
E
John Peter Smith Hospital
IV
Tarrant
E
Medical City Dallas Hospital
IV
Dallas
E
Medical City Plano
IV
Collin
E
Parkland Memorial Hospital
IV
Dallas
E
Texas Health Harris Methodist Hospital Fort
Worth
IV
Tarrant
E
Texas Health Presbyterian Hospital Dallas
IV
Dallas
E
Texas Health Presbyterian Hospital Plano
IV
Collin
E
William P. Clements University Hospital
IV
Dallas
E-9
TSA
Facility Name
Designation
Level
County
F
Paris Regional Medical Center North
Campus
I
Lamar
F
CHRISTUS Mother Frances Hospital -
Sulphur Springs
II
Hopkins
F
CHRISTUS St. Michael Health System
II
Bowie
F
Titus Regional Medical Center
II
Titus
F
Wadley Regional Medical Center
II
Bowie
G
Palestine Regional Medical Center
I
Anderson
G
UT Health East Texas Athens Hospital
I
Henderson
G
UT Health East Texas Henderson Hospital
I
Rusk
G
UT Health East Texas Jacksonville Hospital
I
Cherokee
G
UT Health East Texas Tyler Regional
Hospital
II
Smith
G
CHRISTUS Good Shepherd Medical Center -
Longview
III
Gregg
G
CHRISTUS Mother Frances Hospital - Tyler
III
Smith
G
Longview Regional Medical Center
III
Gregg
H
CHI St. Luke’s Health - Memorial Livingston
II
Polk
H
CHI St. Luke’s Health Memorial Lufkin
II
Angelina
H
Nacogdoches Medical Center
II
Nacogdoches
H
Nacogdoches Memorial Hospital
II
Nacogdoches
H
Woodland Heights Medical Center
II
Angelina
I
The Hospitals of Providence Transmountain
Campus
II
El Paso
I
Del Sol Medical Center, a Campus of LPDS
Healthcare
III
El Paso
I
The Hospitals of Providence East Campus
III
El Paso
I
Las Palmas Medical Center A Campus of
LPDS Healthcare
IV
El Paso
I
The Hospitals of Providence Memorial
Campus
IV
El Paso
I
University Medical Center of El Paso
IV
El Paso
J
Big Bend Regional Medical Center
I
Brewster
J
Pecos County Memorial Hospital
I
Pecos
E-10
TSA
Facility Name
Designation
Level
County
J
Scenic Mountain Medical Center, a Steward
Family Hospital
I
Howard
J
Permian Regional Medical Center
II
Andrews
J
Reeves County Hospital
II
Reeves
J
Medical Center Hospital***Ector
III
Ector
J
Midland Memorial Hospital
III
Midland
J
Odessa Regional Medical Center
III
Ector
K
Shannon Medical Center South
I
Tom Green
K
Shannon Medical Center
II
Tom Green
L
AdventHealth Central Texas
II
Bell
L
Seton Medical Center Harker Heights
II
Bell
L
Baylor Scott & White Medical Center -
Temple
IV
Bell
M
Goodall - Witcher Hospital
I
Bosque
M
Hill Regional Hospital
I
Hill
M
Ascension Providence
II
McLennan
M
Baylor Scott & White Medical Center -
Hillcrest
III
McLennan
N
Baylor Scott & White Medical Center -
Brenham
I
Washington
N
Baylor Scott & White Medical Center -
College Station
II
Brazos
N
CHI St. Joseph Health College Station
Hospital
II
Brazos
O
Dell Children’s Medical Center
I
Travis
O
Ascension Seton Hays
II
Hays
O
Ascension Seton Williamson
II
Williamson
O
Baylor Scott & White Medical Center -
Lakeway
II
Travis
O
Baylor Scott & White Medical Center -
Marble Falls
II
Burnet
O
Baylor Scott & White Medical Center -
Round Rock
II
Williamson
O
Cedar Park Regional Medical Center
II
Williamson
E-11
TSA
Facility Name
Designation
Level
County
O
CHRISTUS Santa Rosa Hospital - San
Marcos
II
Hays
O
Round Rock Medical Center
II
Williamson
O
St. David’s Georgetown Hospital - A St.
David’s Medical Center Facility
II
Williamson
O
Ascension Seton Northwest
III
Travis
O
St. David’s South Austin Medical Center
III
Travis
O
Ascension Seton Medical Center Austin
IV
Travis
O
North Austin Medical Center
IV
Travis
O
St. David’s Medical Center
IV
Travis
P
Dimmit Regional Hospital
I
Dimmit
P
Frio Regional Hospital
I
Frio
P
Medina Regional Hospital
I
Medina
P
Memorial Hospital***Gonzales
I
Gonzales
P
Mission Trail Baptist Hospital
I
Bexar
P
CHRISTUS Santa Rosa Hospital - New
Braunfels
II
Comal
P
Fort Duncan Regional Medical Center
II
Maverick
P
Guadalupe Regional Medical Center
II
Guadalupe
P
Hill Country Memorial Hospital
II
Gillespie
P
P
Peterson Regional Medical Center
II
Kerr
P
Resolute Health
II
Comal
P
Uvalde Memorial Hospital
II
Uvalde
P
Val Verde Regional Medical Center
II
Val Verde
P
Children’s Hospital of San Antonio
III
Bexar
P
Methodist Stone Oak Hospital
III
Bexar
P
Metropolitan Methodist Hospital
III
Bexar
P
Texas Vista Medical Center
III
Bexar
E-12
TSA
Facility Name
Designation
Level
County
P
CHRISTUS Santa Rosa Hospital - Westover
Hills
IV
Bexar
P
Methodist Hospital
IV
Bexar
P
North Central Baptist Hospital
IV
Bexar
P
St. Luke’s Baptist Hospital
IV
Bexar
P
University Hospital
IV
Bexar
Q
Huntsville Memorial Hospital
I
Walker
Q
Matagorda Regional Medical Center
I
Matagorda
Q
St. Luke’s Hospital at The Vintage
I
Harris
Q
Columbus Community Hospital
II
Colorado
Q
HCA Houston Healthcare Conroe
II
Montgomery
Q
HCA Houston Healthcare Tomball
II
Harris
Q
HCA Houston Healthcare West
II
Harris
Q
Houston Methodist Baytown Hospital
II
Harris
Q
Houston Methodist Clear Lake Hospital
II
Harris
Q
Houston Methodist Sugar Land Hospital
II
Fort Bend
Q
Houston Methodist West Hospital
II
Harris
Q
Memorial Hermann Cypress Hospital
II
Harris
Q
Memorial Hermann Greater Heights
Hospital
II
Harris
Q
Memorial Hermann Katy Hospital
II
Harris
Q
Memorial Hermann Northeast Hospital
II
Harris
Q
Memorial Hermann Southeast Hospital
II
Harris
Q
Memorial Hermann Sugar Land Hospital
II
Fort Bend
Q
OakBend Medical Center***Williams Way
Campus
II
Fort Bend
Q
St. Joseph Medical Center
II
Harris
Q
St. Luke’s Sugar Land Hospital
II
Fort Bend
Q
UTMB Health Clear Lake Campus
II
Harris
E-13
TSA
Facility Name
Designation
Level
County
Q
Harris Health System Lyndon B. Johnson
Hospital
III
Harris
Q
HCA Houston Healthcare Clear Lake
III
Harris
Q
HCA Houston Healthcare Kingwood
III
Montgomery
Q
HCA Houston Healthcare Northwest
III
Harris
Q
HCA Houston Healthcare Southeast
III
Harris
Q
Houston Methodist Hospital
III
Harris
Q
Houston Methodist The Woodlands Hospital
III
Montgomery
Q
Houston Methodist Willowbrook Hospital
III
Harris
Q
Memorial Hermann Memorial City Medical
Center
III
Harris
Q
Memorial Hermann Southwest Hospital
III
Harris
Q
Memorial Hermann The Woodlands Medical
Center
III
Montgomery
Q
St. Luke’s The Woodlands Hospital
III
Harris
Q
Harris Health System Ben Taub Hospital
IV
Harris
Q
Memorial Hermann - Texas Medical Center
IV
Harris
Q
Texas Children’s Hospital
IV
Harris
Q
The Woman’s Hospital of Texas
IV
Harris
R
CHI St. Luke’s Health - Brazosport
I
Brazoria
R
UTMB Health Angleton Danbury Campus
I
Brazoria
R
Baptist Hospitals of Southeast Texas
II
Jefferson
R
CHRISTUS Southeast Texas - St. Elizabeth
& St. Mary
II
Jefferson
R
The Medical Center of Southeast Texas
II
Jefferson
R
University of Texas Medical Branch
IV
Galveston
S
Cuero Regional Hospital
I
DeWitt
S
Memorial Medical Center
I
Calhoun
S
Citizens Medical Center
II
Victoria
S
DeTar Healthcare System
II
Victoria
E-14
TSA
Facility Name
Designation
Level
County
T
Doctors Hospital of Laredo
II
Webb
T
Laredo Medical Center
II
Webb
U
CHRISTUS Spohn Hospital Alice
I
Jim Wells
U
CHRISTUS Spohn Hospital Beeville
I
Bee
U
CHRISTUS Spohn Hospital Kleberg
I
Kleberg
U
CHRISTUS Spohn Hospital Corpus Christi
South
IV
Nueces
U
The Corpus Christi Medical Center - Bay
Area
IV
Nueces
V
Starr County Memorial Hospital
I
Starr
V
Harlingen Medical Center
II
Cameron
V
Knapp Medical Center
II
Hidalgo
V
Mission Regional Medical Center
II
Hidalgo
V
Rio Grande Regional Hospital
II
Hidalgo
V
South Texas Health System Edinburg
II
Hidalgo
V
South Texas Health System McAllen
II
Hidalgo
V
Valley Baptist Medical Center
II
Cameron
V
Valley Baptist Medical Center - Brownsville
II
Cameron
V
Valley Regional Medical Center
II
Cameron
V
Women’s Hospital at Renaissance
IV
Hidalgo
