
COMMUNITY-BASED
PARTICIPATORY
RESEARCH
FOR HEALTH

COMMUNITY-BASED
PARTICIPATORY
RESEARCH
FOR HEALTH
Advancing Social and
Health Equity
third edition
NINA WALLERSTEIN
BONNIE DURAN
JOHN G. OETZEL
MEREDITH MINKLER
Editors
Copyright © 2018 by John Wiley & Sons, Inc. All rights reserved.
Published by Jossey-Bass
A Wiley Brand
One Montgomery Street, Suite 1000, San Francisco, CA 94104-4594—www.josseybass.com
Edition History
John Wiley and Sons, Inc. (2e, 2008; 1e, 2003)
The right of Nina Wallerstein, Bonnie Duran, John Oetzel, and Meredith Minkler to be identied as the authors of the editorial
material in this work has been asserted in accordance with law.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic,
mechanical, photocopying, recording, scanning, or otherwise, except as permitted under Section107 or 108 of the 1976 United
States Copyright Act, without either the prior written permission of the publisher, or authorization through payment of the
appropriate per-copy fee to the Copyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923, 978-750-8400,
fax 978-646-8600, or on the Web at www.copyright.com. Requests to the publisher for permission should be addressed to the
Permissions Department, John Wiley & Sons, Inc., 111 River Street, Hoboken, NJ 07030, 201-748-6011, fax 201-748-6008, or
online at www.wiley.com/go/permissions.
Limit of Liability/Disclaimer of Warranty: While the publisher and author have used their best efforts in preparing this book,
they make no representations or warranties with respect to the accuracy or completeness of the contents of this book and
specically disclaim any implied warranties of merchantability or tness for a particular purpose. No warranty may be created
or extended by sales representatives or written sales materials. The advice and strategies contained herein may not be suitable
for your situation. You should consult with a professional where appropriate. Neither the publisher nor author shall be liable
for any loss of prot or any other commercial damages, including but not limited to special, incidental, consequential, or other
damages. Readers should be aware that Internet Web sites offered as citations and/or sources for further information may have
changed or disappeared between the time this was written and when it is read.
Jossey-Bass books and products are available through most bookstores. To contact Jossey-Bass directly call our Customer Care
Department within the U.S. at 800-956-7739, outside the U.S. at 317-572-3986, or fax 317-572-4002.
Wiley publishes in a variety of print and electronic formats and by print-on-demand. Some material included with standard print
versions of this book may not be included in e-books or in print-on-demand. If this book refers to media such as a CD or DVD
that is not included in the version you purchased, you may download this material at http://booksupport.wiley.com. For more
information about Wiley products, visit www.wiley.com.
Library of Congress Cataloging-in-Publication Data
Names: Wallerstein, Nina, 1953- editor.
Title: Community-based participatory research for health: advancing social
and health equity / edited by Nina Wallerstein, Dr.P.H, Professor of
Public Health, College of Population Health Director, Center for
Participatory Research, University of New Mexico (UNM), Bonnie Duran,
Dr.P.H., Associate Professor, University of Washington School of Social Work,
Director of the Center for Indigenous Health Research, Indigenous Wellness
Research Institute, John G. Oetzel, Professor, Waikato Management School,
University of Waikato, Meredith Minkler, Dr.P.H., MPH, Professor, Graduate
School, Community Health Sciences, University of California, Berkeley,
Professor Emerita, School of Public Health.
Description: Third edition. | Hoboken, NJ : Jossey-Bass & Pfeiffer Imprints,
Wiley, [2017] | Includes bibliographical references. |
Identiers: LCCN 2017018499 (print) | LCCN 2017021064 (ebook) | ISBN
9781119258865 (epdf) | ISBN 9781119258872 (epub) | ISBN 9781119258858
(paperback)
Subjects: LCSH: Public health—Research—Citizen participation. | Public
health—Research—Methodology. | Community health services. | BISAC:
MEDICAL / Public Health.
Classication: LCC RA440.85 (ebook) | LCC RA440.85 .C65 2017 (print) | DDC
362.1072—dc23
LC record available at https://lccn.loc.gov/2017018499
Cover design: Wiley
Cover image: © MAGNIFIER/Shutterstock
Printed in the United States of America
PB Printing 10 9 8 7 6 5 4 3 2 1
From Nina: To my late parents, Robert and Judith Wallerstein,
who modeled for me values of justice and compassion.
From Bonnie: Gratitude to my parents, siblings, and community
members for sharing their values, wisdom, and patience.
From John: To my children, Spencer and Ethan, who inspire me
to make a positive contribution in the community.
From Meredith: To Roy and Fran Minkler, who as parents and
human beings taught by example the power of deep concern
with fairness, caring, keeping a sense of humor,
and never giving up.
CONTENTS
The Editors xiii
The Contributors xv
Preface xxxiii
Camara Phyllis Jones
Acknowledgments xxxvii
PART ONE: INTRODUCTION: HISTORY AND PRINCIPLES
ONE: ON COMMUNITY-BASED PARTICIPATORY RESEARCH 3
Nina Wallerstein, Bonnie Duran, John G. Oetzel, and Meredith Minkler
TWO: THEORETICAL, HISTORICAL, AND PRACTICE ROOTS OF CBPR 17
Nina Wallerstein and Bonnie Duran
THREE: CRITICAL ISSUES IN DEVELOPING AND FOLLOWING
CBPR PRINCIPLES 31
Barbara A. Israel, Amy J. Schulz, Edith A. Parker, Adam B. Becker,
Alex J. Allen, III, J. Ricardo Guzman, and Richard Lichtenstein
PART TWO: POWER, TRUST, AND DIALOGUE:
WORKING WITH DIVERSE COMMUNITIES
FOUR: UNDERSTANDING CONTEMPORARY RACISM, POWER,
AND PRIVILEGE AND THEIR IMPACTS ON CBPR 47
Michael Muhammad, Catalina Garzón, Angela Reyes, and
The West Oakland Environmental Indicators Project
FIVE: TRUST DEVELOPMENT IN CBPR PARTNERSHIPS 61
Julie E. Lucero, Kathrine E. Wright, and Abigail Reese
viii Contents
PART THREE: CBPR CONCEPTUAL MODEL: CONTEXT
AND PROMISING RELATIONSHIP PRACTICES
SIX: SOCIO-ECOLOGIC FRAMEWORK FOR CBPR:
DEVELOPMENT AND TESTING OF A MODEL 77
Sarah L. Kastelic, Nina Wallerstein, Bonnie Duran, and John G. Oetzel
SEVEN: YOUTH-LED PARTICIPATORY ACTION RESEARCH (YPAR):
PRINCIPLES APPLIED TO THE US AND DIVERSE GLOBAL SETTINGS 95
Emily J. Ozer and Amber Akemi Piatt
EIGHT: PARTNERSHIP, TRANSPARENCY, AND ACCOUNTABILITY:
CHANGING SYSTEMS TO ENHANCE RACIAL EQUITY IN CANCER
CARE AND OUTCOMES 107
Eugenia Eng, Jennifer Schaal, Stephanie Baker, Kristin Black,
Samuel Cykert, Nora Jones, Alexandra Lightfoot, Linda Robertson,
Cleo Samuel, Beth Smith, and Kari Thatcher
NINE: SOUTH VALLEY PARTNERS FOR ENVIRONMENTAL JUSTICE:
A STORY OF ALIGNMENT AND MISALIGNMENT 123
Magdalena Avila, Shannon Sanchez-Youngman, Michael Muhammad,
Lauro Silva, and Paula Domingo de Garcia
PART FOUR: PROMISING PRACTICES: INTERVENTION
DEVELOPMENT AND RESEARCH DESIGN
TEN: CBPR IN HEALTH CARE SETTINGS 141
Margarita Alegría, Chau Trinh-Shevrin, Bowen Chung, Andrea Ault,
Alisa Lincoln, and Kenneth B. Wells
ELEVEN: NATIONAL CENTER FOR DEAF HEALTH RESEARCH:
CBPR WITH DEAF COMMUNITIES 157
Steven Barnett, Jessica Cuculick, Lori Dewindt, Kelly Matthews, and Erika Sutter
TWELVE: CBPR IN ASIAN AMERICAN COMMUNITIES 175
Nadia Islam, Charlotte Yu-Ting Chang, Pam Tau Lee, and Chau Trinh-Shevrin
Contents ix
THIRTEEN: ENGAGED FOR CHANGE: AN INNOVATIVE CBPR
STRATEGY TO INTERVENTION DEVELOPMENT 189
Scott D. Rhodes, Lilli Mann, Florence M. Simán, Jorge Alonzo,
Aaron T. Vissman, Jennifer Nall, and Amanda E. Tanner
PART FIVE: PROMISING PRACTICES: ETHICAL ISSUES
FOURTEEN: CBPR PRINCIPLES AND RESEARCH ETHICS
IN INDIAN COUNTRY 207
Myra Parker
FIFTEEN: DEMOCRATIZING ETHICAL OVERSIGHT
OF RESEARCH THROUGH CBPR 215
Rachel Morello-Frosch, Phil Brown, and Julia Green Brody
SIXTEEN: EVERYDAY CHALLENGES IN THE LIFE CYCLE OF CBPR:
BROADENING OUR BANDWIDTH ON ETHICS 227
Sarah Flicker, Adrian Guta, and Robb Travers
PART SIX: PROMISING PRACTICES
TO OUTCOMES: CBPR CAPACITY AND HEALTH
SEVENTEEN: EVALUATION OF CBPR PARTNERSHIPS AND OUTCOMES:
LESSONS AND TOOLS FROM THE RESEARCH FOR IMPROVED
HEALTH STUDY 237
John G. Oetzel, Bonnie Duran, Andrew Sussman, Cynthia Pearson,
Maya Magarati, Dmitry Khodyakov, and Nina Wallerstein
EIGHTEEN: PARTICIPATORY EVALUATION AS A PROCESS
OF EMPOWERMENT: EXPERIENCES WITH COMMUNITY
HEALTH WORKERS IN THE UNITED STATES AND LATIN AMERICA 251
Noelle Wiggins, Laura Chanchien Parajón, Chris M. Coombe,
Aileen Alfonso Duldulao, Leticia Rodriguez Garcia, and Pei-Ru Wang
NINETEEN: ACADEMIC POSITIONS FOR FACULTY OF COLOR:
COMBINING LIFE CALLING, COMMUNITY SERVICE, AND RESEARCH 265
Lorenda Belone, Derek M. Grifth, and Barbara Baquero
x Contents
PART SEVEN: PROMISING PRACTICES TO OUTCOMES:
HEALTHY PUBLIC POLICY
TWENTY: COMMUNITY-BASED PARTICIPATORY RESEARCH
FOR HEALTH EQUITY POLICY MAKING 277
Lisa Cacari-Stone, Meredith Minkler, Nicholas Freudenberg,
and Makani N. Themba
TWENTY ONE: IMPROVING FOOD SECURITY AND TOBACCO
CONTROL THROUGH POLICY-FOCUSED CBPR: A CASE STUDY OF
HEALTHY RETAIL IN SAN FRANCISCO 293
Meredith Minkler, Jennifer Falbe, Susana Hennessey Lavery,
Jessica Estrada, and Ryan Thayer
TWENTY TWO: CRIMINAL JUSTICE REFORM THROUGH
PARTICIPATORY ACTION RESEARCH 305
Saneta deVuono-Powell, Meredith Minkler, Evan Bissell, Tamisha Walker,
LaVern Vaughn, Eli Moore, and The Morris Justice Project
TWENTY THREE: GLOBAL HEALTH POLICY: SLUM SETTLEMENT
MAPPING IN NAIROBI AND RIO DE JANEIRO 321
Jason Corburn, Ives Rocha, Alexei Dunaway, and Jack Makau
APPENDIX 1: CHALLENGING OURSELVES: CRITICAL
SELF-REFLECTION ON POWER AND PRIVILEGE 337
Cheryl Hyde
APPENDIX 2: GUIDING CBPR PRINCIPLES: FOSTERING
EQUITABLE HEALTH CARE FOR LGBTQ+ PEOPLE 345
Miria Kano, Kelley P. Sawyer, and Cathleen E. Willging
APPENDIX 3: QUALITY CRITERIA OF THE INTERNATIONAL
COLLABORATION FOR PARTICIPATORY HEALTH RESEARCH (ICPHR) 351
Michael T. Wright
Contents xi
APPENDIX 4: CULTURAL HUMILITY: REFLECTIONS
AND RELEVANCE FOR CBPR 357
Vivian Chávez
APPENDIX 5: FUNDING IN CBPR IN US GOVERNMENT
AND PHILANTHROPY 363
Laura C. Leviton and Lawrence W. Green
APPENDIX 6: REALIST EVALUATION AND REVIEW FOR
COMMUNITY-BASED PARTICIPATORY RESEARCH: WHAT WORKS,
FOR WHOM, UNDER WHAT CIRCUMSTANCES, AND HOW? 369
Justin Jagosh
APPENDIX 7: PARTNERSHIP RIVER OF LIFE: CREATING
A HISTORICAL TIME LINE 375
Shannon Sanchez-Youngman and Nina Wallerstein
APPENDIX 8: PURPOSING A COMMUNITY-GROUNDED RESEARCH
ETHICS TRAINING INITIATIVE 379
Cynthia Pearson and Victoria Sánchez
APPENDIX 9: PARTNERSHIP AGREEMENTS: A PRACTICAL
GUIDE TO DEVELOPING DATA SHARING, OWNERSHIP,
AND PUBLISHING AGREEMENTS 385
Patricia Rodríguez Espinosa and Al Richmond
APPENDIX 10: INSTRUMENTS AND MEASURES
FOR EVALUATING COMMUNITY ENGAGEMENT
AND PARTNERSHIPS 393
Nina Wallerstein
APPENDIX 11: PARTICIPATORY MONITORING AND EVALUATION
OF COMMUNITY HEALTH INITIATIVES USING
THE COMMUNITY CHECK BOX EVALUATION SYSTEM 399
Stephen Fawcett, Jerry Schultz, Vicki Collie-Akers, Christina Holt,
Jomella Watson-Thompson, and Vincent Francisco
xii Contents
APPENDIX 12: POWER MAPPING: A USEFUL TOOL FOR
UNDERSTANDING THE POLICY ENVIRONMENT AND ITS
APPLICATION TO A LOCAL SODA TAX INITIATIVE 405
Jennifer Falbe, Meredith Minkler, Robin Dean, and Jana Cordeiero
APPENDIX 13: CBPR INTERACTIVE ROLE-PLAYS: THREE SCENARIOS 411
Michele Polacsek and Gail Dana-Sacco
AFTERWORD 417
Budd Hall and Rajesh Tandon
INDEX 419
NINA WALLERSTEIN, DrPH, professor of public health, College of Population Health, and
director, Center for Participatory Research (cpr.unm.edu), University of New Mexico (UNM),
has been developing CBPR and empowerment, Paulo Freire–based interventions for more
thanthirty years. She has written over 150 articles and chapters and seven books, including the
Freirean Problem-Posing at Work: A Popular Educator’s Guide. In 2016, she received the inau-
gural Community Engaged Research Lecture award from UNM. She’s had a long-term CBPR
research relationship with several New Mexican tribes to support intergenerational culture-
centered family prevention programming with children, parents, and elders; and she has worked
with the Healthy Native Community Partnership for more than ten years. Since 2006, she has
worked to strengthen the science of CBPR and community-engaged research. She is currently
principal investigator (PI) of Engage for Equity, an NINR-funded RO1 to assess promising
partnering practices associated with outcomes and to develop partnership evaluation and reec-
tion tools and resources. She has collaboratively produced with Latin American colleagues an
empowerment, participatory research, and health promotion curriculum available in Spanish,
Portuguese, and English (http://cpr.unm.edu/curricula-classes/empowerment-curriculum.html)
and cosponsors an annual summer institute in CBPR for health at the University of New Mexico.
BONNIE DURAN, DrPH (mixed-race Opelousas and Coushatta) is professor in the department
of health services, University of Washington School of Public Health and is also Director of the
Center for Indigenous Health Research at the Indigenous Wellness Research Institute (www.
iwri.org). Using Indigenous theories to guide her work, Bonnie’s research includes intervention
and prevalence studies of substance abuse and other mental disorders, violence, and treatment
seeking in Native communities. Her overall aims are to work with communities to design inter-
ventions and descriptive studies that are empowering, culture-centered, sustainable, and that
have maximum public health impact.
JOHN G. OETZEL is a professor in the Waikato Management School at the University of
Waikato. He uses CBPR to collaboratively work with communities to address various health
issues to improve health equity. His current work includes the collaborative development of
interventions with two Māori health organizations in New Zealand related to pre-diabetes and
positive aging. He is also a member of the Engage for Equity research team investigating prom-
ising practices for CBPR in the United States. He contributes expertise in research design and
evaluation and believes in the importance of collaborative design to ensure that the research
evaluation ts the context and needs of communities as well as to ensure interventions are
culturally centered. He is author or coauthor of three books: Managing Intercultural Commu-
nication Effectively (with Stella Ting-Toomey, 2001, Sage); Intercultural Communication: A
Layered Approach (2009, Pearson); and Theories of Human Communication, 11th ed. (with Ste-
phen Littlejohn and Karen Foss, 2017, Waveland). He is coeditor of two other books: The Sage
THE EDITORS
xiv The Editors
Handbook of Conict Communication (with Stella Ting-Toomey, 2006, Sage, and 2ndedition in
2013). In addition, he is also author of more than ninety articles and book chapters.
MEREDITH MINKLER, DrPH, MPH, is professor in the Graduate School, Community
Health Sciences, University of California, Berkeley, and professor emerita in the School of
Public Health. Founding director of the UC Berkeley Center on Aging, Minkler continues to
work with community and other partners to help develop the evidence base for implementing
healthy public policy in areas including healthy retail in low-income neighborhoods, environ-
mental exposures, immigrant worker health and safety, criminal justice reform, and HIV/AIDS.
A recent Fulbright specialist in South Africa in CBPR, she has offered trainings on community-
engaged research in Hong Kong, Singapore, Australia, the United Kingdom, and in numerous
states and provinces in the United States and Canada. Minkler has coauthored close to two
hundred articles and coauthored or edited nine books, including Community Organizing and
Community Building for Health and Welfare (Rutgers, 2012).
THE CONTRIBUTORS
MARGARITA ALEGRÍA, PhD, is the chief of the Disparities Research Unit at Massachusetts
General Hospital and professor in the Departments of Medicine and Psychiatry at Harvard
Medical School. Alegría has served as PI on more than fteen federally funded research
grants and has published more than two hundred professional publications on topics such as
the improvement of health care services delivery for diverse racial and ethnic populations,
conceptual and methodological issues with multicultural populations, and ways to bring the
community’s perspective into the design and implementation of health services.
ALEX J. ALLEN, III, MSA, is the president and CEO of the Chandler Park Conservancy. He
collaborates with residents, stakeholders, local institutions, business, government, and the phil-
anthropic community to transform Chandler Park into a campus with exceptional educational,
recreational, and conservation opportunities for youth and families on Detroit’s eastside and
the region. He has effectively led organizations, collaborative initiatives, and has improved the
quality of life for people who live, work, play, and visit communities in the United States. His
experience includes managing grants for compliance and budget integrity, convening stake-
holders for planning and project implementation, supervising and monitoring youth programs,
fund-raising, reporting and evaluation, and CBPR.
JORGE ALONZO, JD, is a research associate at Wake Forest School of Medicine and is part
of a team that specializes in HIV-prevention research using CBPR with immigrant Latinos.
He has been involved in the design, implementation, and evaluation of HIV-prevention inter-
ventions for Latino gay and bisexual men and men who have sex with men (MSM) and Latina
transgender women. He has also been involved in projects exploring the impact of immigration
enforcement on access to and use of public health services among Latinos.
ANDREA AULT, PhD, MPA, is the senior director of the Mental Health Innovation Lab in
the New York City Department of Health and Mental Hygiene. She was previously the
associate director of the Health Equity Lab at Cambridge Health Alliance, where her research
focused on racial-ethnic disparities in mental health care, dissemination and implementation
research, and CBPR.
MAGDALENA AVILA, DrPH, MPH, MSW, is associate professor, community health educa-
tion, Department of Health, Exercise and Sports Science, College of Education, University of
New Mexico. She self-identies as an activist scholar in community health and CBPR, in her
partnering with Latino and other Indigenous communities of color, and in her use of a social
justice framework. Her areas of research are environmental health, environmental racism, and
community health impact assessments in working with rural and urban communities, and she
has expanded her research capacity by incorporating digital story making into her CBPR work
with Latino communities.
xvi The Contributors
STEPHANIE BAKER, PhD, MS, PT, is assistant professor of public health at Elon Univer-
sity and a member of the Greensboro Health Disparities Collaborative. Her work is focused
on social determinants of racial inequities in health, community organizing as a tool for public
health change, antiracism pedagogy, and CBPR.
BARBARA BAQUERO, PhD, MPH, is assistant professor of community and behavioral
health at the University of Iowa, College of Public Health. She is a founding member of the
Healthy Equity Advancement Lab (HEAL), an academic-community research lab dedicated to
advancing health equity through research and training. She serves as PI and deputy director of
the University of Iowa, Prevention Research Center, funded by the CDC.
STEVEN BARNETT, MD, is associate professor of family medicine and public health sci-
ences at the University of Rochester and director of the Rochester Prevention Research Center:
National Center for Deaf Health Research. He is a sign language–skilled family physician
researcher with a career focus on health care and collaborative health research with deaf sign
language users and people with hearing loss, their families, and communities.
ADAM B. BECKER, PhD, MPH, is associate professor of pediatrics and preventive med-
icine in the Feinberg School of Medicine at Northwestern University. He is also execu-
tive director of the Consortium to Lower Obesity in Chicago Children (CLOCC) at Ann
and Robert H. Lurie Children’s Hospital of Chicago. He has used CBPR to examine and
address the impact of stressful community conditions on the health of women raising chil-
dren, youth violence prevention, and the impact of the social and physical environment on
physical activity.
LORENDA BELONE, PhD, MPH, (Diné/Navajo) is assistant professor at the University of New
Mexico (UNM) College of Education. She is a senior fellow with the Center for Participatory
Research, a center that supports networks of research with community partners in New Mexico
addressing health inequities, and a senior fellow with the UNM Center for Health Policy. Since
2000, she has been actively engaged in CBPR research that has involved southwest Native
American communities. She currently is co-PI on a NIDA-funded RIO multi-tribal implemen-
tation and evaluation study (1R01DA037174-03).
EVAN BISSELL, MPH, MCP, is an artist based in the Bay Area. He teaches art and social
change at UC Berkeley and is involved in participatory research and art projects in multiple set-
tings across the country that support equitable systems and liberatory processes. His work has
been exhibited in institutions and galleries across the country. He is the creator of knottedline
.com and freedoms-ring.org.
KRISTIN BLACK, PhD, MPH, is a postdoctoral fellow in the Cancer Health Disparities
Training Program in the Department of Health Behavior at the University of North Carolina at
Chapel Hill. Her PhD is in maternal and child health, and her career commitment is to use CBPR
approaches to understand and address race-specic inequities in cancer survivorship and repro-
ductive health.
The Contributors xvii
JULIA GREEN BRODY, PhD, is executive director and senior scientist at Silent Spring
Institute, an independent research group founded in 1994 by breast cancer activists to create a
“lab of their own” focused on environmental factors and prevention. Her research, supported by
the National Institutes of Health, investigates everyday exposures to carcinogens and endocrine-
disrupting chemicals from consumer products, workplaces, and pollution.
PHIL BROWN, PhD, is University Distinguished Professor of Sociology and Health Sciences
at Northeastern, where he directs the Social Science Environmental Health Research Institute.
His books include No Safe Place: Toxic Waste, Leukemia, and Community Action; Toxic Expo-
sures: Contested Illnesses and the Environmental Health Movement; and Contested Illnesses:
Citizens, Science, and Health Social Movements. He directs an NIEHS training program “Trans-
disciplinary Training at the Intersection of Environmental Health and Social Science.”
LISA CACARI-STONE, PhD, MA, MS, is associate professor in the College of Population Health
and assistant director with the RWJF Center for Health Policy at the University of New Mexico.
Her scholarly interests focus on upstream determinants of health, including societal and political
structures and relationships that differentially affect population health and policy interventions
that inuence health equity. Her community-engaged research with Latino and US-Mexico border
communities encompass macro-level determinants (e.g., immigration policy, health reform); the
community level (e.g., impact of neighborhood context and migration on substance use); and the
interpersonal level (e.g., the role of promotores de salud in chronic disease management among
Latinos). Cacari Stone is widely trusted for her work in translating and disseminating data for
policy making with governments, community-based organizations, coalitions, and foundations.
CHARLOTTE YU-TING CHANG, DrPH, MPH, is coordinator of research to practice and
evaluation and associate project scientist at the Labor Occupational Health Program, School
of Public Health, University of California, Berkeley. Her work has focused on advancing the
movement of research into practice in worker health and safety, with a particular interest in the
role and processes of research partnerships with workers and community members. She has
worked and written on a range of projects involving immigrant worker populations and commu-
nities as well as on research to practice lessons learned in construction health and safety.
VIVIAN CHÁVEZ, DrPH, is associate professor of health education at San Francisco State
University. A storyteller by nature, she has collaborated with community-based organiza-
tions to disseminate their work. She coedited Prevention Is Primary: Strategies in Community
Well-Being, coauthored Drop That Knowledge: Youth Radio Stories, translated Media Advocacy
into Spanish, and made a lm about cultural humility that is widely accessible. Her work inte-
grates the language of the arts, culture, and the body for health and social change.
BOWEN CHUNG, MD, MSHS, is associate professor–in-residence of psychiatry at the UCLA
David Geffen School of Medicine, an adjunct scientist at the RAND Corporation, and an
attending physician at Harbor-UCLA Medical Center. He has been a PI and co-PI on ten feder-
ally funded research grants and is the author of more than thirty scientic publications. He has
been working with the same community partners for nearly fteen years.
xviii The Contributors
VICKI COLLIE-AKERS, PhD, MPH, is associate director of health promotion research at the
KU Center for Community Health and Development. She serves as an investigator on several
projects promoting health equity and reduction in health disparities in the Kansas City met-
ropolitan area. Additionally, she directs several evaluation projects that support partners who
are working to promote health through their comprehensive initiatives. Her research pri-
marily focuses on applying a CBPR orientation to understand how collaborative partnerships
and coalitions can improve social determinants of health and equity and reduce disparities in
health outcomes.
CHRIS M. COOMBE, PhD, MPH, is assistant research scientist in the Department of Health
Behavior/Health Education at the University of Michigan School of Public Health and is afl-
iated with the Detroit Community-Academic Urban Research Center. She has extensive expe-
rience designing, implementing, and evaluating collaborative research and interventions using
CBPR. Coombe’s work focuses on understanding how urban social and physical environments
contribute to racial and socioeconomic inequities and translating that knowledge into policy
interventions to promote health and equity.
JASON CORBURN, PhD, MCP, is professor in the Department of City and Regional Planning
and the School of Public Health, University of California, Berkeley. He directs the Institute of
Urban and Regional Development and the Center for Global Healthy Cities. He is the author
of a number of award-winning books on community-based action research for health equity,
including Street Science (MIT Press, 2005), Toward the Healthy City (MIT Press, 2009), and
Slum Health (University of California Press, 2016).
JANA CORDEIERO, MPH, is an independent public health and nonprot consultant, strate-
gist, and researcher with more than twenty-ve years of experience working with universities,
foundations, community-based organizations, and health departments to develop and evaluate
effective public health policies and programs. She worked with other advocates in the Bay Area
to successfully pass public health policies to prevent chronic diseases fueled by sugary drinks,
including warning label legislation, sugary drink taxes on distributors, and resisting pouring
rights contracts at universities.
JESSICA CUCULICK, PhD, is associate professor, Department of Liberal Studies, at the
National Technical Institute for the Deaf, Rochester Institute of Technology. Cuculick coor-
dinates the applied liberal arts associate degree program and is the professional development
director for the Rochester bridges to the doctorate program (www.deafscientists.com). She is
codirector for the Deaf Health Lab and the PI for the deaf health literacy research project. Cucu-
lick has been involved with CBPR with the National Center for Deaf Health Research (NCDHR)
at the University of Rochester, such as breastfeeding and cardiovascular health perspectives in
the Deaf community.
SAMUEL CYKERT, MD, is a professor of medicine at UNC-CH in the Division of General
Internal Medicine and Clinical Epidemiology. He also serves as the director of the UNC School
of Medicine program on health and clinical informatics. Combining his research training and
The Contributors xix
interest in health policy, he currently serves as a PI on multiple projects that address health
disparities in cancer treatment and chronic care management.
GAIL DANA-SACCO, PhD, MPH, is on the faculty of the Center for American Indian Health
at the Johns Hopkins University, where she works with tribal communities to research vio-
lence and injury and to develop and implement structural and behavioral strategies to improve
health outcomes.
ROBIN DEAN, MPH, MA, is a public health consultant offering health advocacy and qualitative
research services to clients working to create healthy, connected communities in which
everyone has a voice. In 2014, she advocated through coordinating writers’ media submissions
for soda tax campaigns in San Francisco and Berkeley, and in 2016 she secured endorsements
for Oakland’s and San Francisco’s winning soda tax measures. Robin has produced case studies
and evaluations, including a Berkeley Media Studies Group issue brief on an Oregon affordable
housing coalition’s media advocacy effort and a case study of girls’ education in Mali.
SANETA DEVUONO-POWELL, JD, MCP, is a city planner and attorney who works on
community health. She is currently senior planner at Changelab Solutions and has written
on incarceration and its impacts on families as well as on community-based participatory
action research. Her current work is focused on racial disparities in health and the links
between health disparities and housing.
LORI DEWINDT, MA, is health project coordinator, Rochester Prevention Research Center:
National Center for Deaf Health Research (RPRC/NCDHR), University of Rochester Med-
ical Center. DeWindt has worked in the eld of Deaf community health as a RPRC/NCDHR
research coordinator and as a psychotherapist at the Deaf Wellness Center at the University of
Rochester.
PAULA DOMINGO DE GARCIA is a resident of the South Valley and one of the main pro-
motoras of the S.V.P.E.J. research team. She is an immigrant from the Indigenous community
Nahua de Cuentepec in Temixco, Mexico. Before coming to New Mexico, she worked with the
Independent Commission of Human Rights of Morelos to save her native language, Nahuatl,
and with the National Council to Promote Education in the rural community of Tlatepetl, Tepoz-
tlan. She currently works as a teaching assistant at Dolores Gonzales Elementary School and as
a federal court interpreter translating from Nahuatl to Spanish. She is currently studying for her
AA in Early Childhood Multicultural Education.
AILEEN ALFONSO DULDULAO, PhD, MSW, is the maternal, child, and family health epi-
demiologist for the Multnomah County Health Department in Portland, Oregon. She has held
research fellowships from the National Institute of Mental Health, the National Institute of
Minority Health and Health Disparities, and the University of Washington Institute for Trans-
lational Health Sciences. Her social work background includes extensive experience in direct
social service provision with immigrant and refugee communities experiencing domestic vio-
lence, sexual assault, mental illness, poverty, and employment discrimination.
xx The Contributors
ALEXEI DUNAWAY is the executive director of Ongoza, an accelerator for youth-led social
businesses in Nairobi, Kenya. Previously he contributed to several human rights trials in Spain,
the United States, and El Salvador; conducted research for Human Rights Watch and the Council
on Foreign Relations; and helped coordinate the world pilot of a youth-led community mapping
initiative at the Centro de Promoção da Saúde (CEDAPS) in Rio de Janeiro, Brazil. He also
served as a Fulbright research scholar in Mozambique.
EUGENIA ENG, MPH, DrPH, is professor of health behavior at the Gillings School of Global
Public Health, University of North Carolina at Chapel Hill. She has more than thirty years of
CBPR experience, including eld studies conducted with rural communities of the US South,
Sub-Saharan Africa, and Southeast Asia to address socially stigmatizing health problems such
as pesticide poisoning, cancer, and STI-HIV. Her CBPR projects include the NCI-funded
Accountability for Cancer Care through Undoing Racism and Equity, the CDC-funded Men
As Navigators for Health, the NCI-funded Cancer Care and Racial Equity Study, the NHLBI-
funded CVD Black Church: Are We Our Brother’s Keeper? In addition to her coedited book,
Methods for Community-Based Participatory Research for Health, she has more than 115 pub-
lications on the lay health advisor intervention model, the concepts of community competence
and natural helping, and community assessment procedures.
JESSICA ESTRADA is a health program coordinator at the San Francisco Department of
Public Health Community Health Equity & Promotion Branch, and formerly co-coordinator
of the Tenderloin Healthy Corner Store Coalition. She received her bachelor of science from
the University of California, Davis, and has worked in public health, youth development, and
community organizing, with a passion for health equity, since 2006.
JENNIFER FALBE, ScD, MPH, is an assistant professor of nutrition and human development
at the University of California, Davis. Her research focuses on evaluating policies and programs
to reduce health disparities and improve diet quality, such as soda taxes, healthy retail pro-
grams, and primary care and community interventions.
STEPHEN FAWCETT, PhD, is senior advisor in KU Center for Community Health and
Development, and codirector of the World Health Organization Collaborating Centre for
Community Health and Development at the University of Kansas. Author of nearly two hundred
publications and cofounder of the Community Tool Box, his research examines how collabora-
tive action affects improvements in population health and equity.
SARAH FLICKER, PhD, is associate professor in the Faculty of Environmental Studies at
York University in Toronto, Canada. Her program of research focuses on youth environmental,
sexual, and reproductive justice issues. Her research has informed policy at the municipal, pro-
vincial, and federal levels. Flicker and her teams have won a number of prestigious awards for
youth engagement in health research.
VINCENT FRANCISCO, PhD, is Kansas Health Foundation Professor of Community Leader-
ship and senior scientist with the Schiefelbusch Institute for Life Span Studies. He is codirector
The Contributors xxi
of the KU Center for Community Health and Development, a World Health Organization
Collaborating Centre at the University of Kansas.
NICHOLAS FREUDENBERG, DrPH, is Distinguished Professor of Public Health at the City
University of New York Graduate School of Public Health and Health Policy, where he also
directs the CUNY Urban Food Policy Institute. For the past thirty years, he has developed,
implemented, and evaluated community health policies and programs designed to improve the
health and reduce health inequalities facing vulnerable urban populations.
CATALINA GARZÓN, PhD, has coordinated CBPR, leadership development, action planning,
and curriculum development partnerships with environmental and social justice organizations
and coalitions for more than twenty years. Her recent collaborations include a photo-novella
on alternatives to the criminalization of youth with Communities United for Restorative Youth
Justice and a Health Impact Assessment of freight transport planning with the Ditching Dirty
Diesel Collaborative. Garzón is a recipient of the Thomas I. Yamashita Prize honoring out-
standing social change activists who serve as a bridge between academia and the community.
LAWRENCE W. GREEN, DrPH ScD (Hon), emeritus professor of epidemiology and biosta-
tistics at the University of California at San Francisco, served as director of the US Ofce of
Health Information and Health Promotion under the Carter Administration and director of the
Ofce of Science and Extramural Research at CDC. He has been on the full-time faculties of
UC Berkeley, Johns Hopkins University, Harvard, the University of Texas, and the University
of British Columbia. He headed a Canadian team in producing the rst study of participatory
research in health promotion for the Royal Society of Canada.
DEREK M. GRIFFITH, PhD, is associate professor of medicine, health, and society and
founder and director of the Center for Research on Men’s Health at Vanderbilt University. In
November 2013, Grifth was presented with the Tom Bruce Award by the Community-Based
Public Health Caucus of the American Public Health Association in recognition of his leader-
ship in community-based public health and for his research on “eliminating health disparities
that vary by race, ethnicity, and gender.”
ADRIAN GUTA, MSW, PhD, is assistant professor at the School of Social Work, University
of Windsor, Canada. His research examines the social, cultural, and ethical dimensions of HIV
prevention, treatment, and care; related clinical and social service programing; and public health
interventions through a combination of critical theoretical work and applied CBPR.
J. RICARDO GUZMAN, MSW, MPH, served as CEO for the Community Health and Social
Services Center (CHASS), a federally qualied health center, in Detroit from 1982 through
2016. During his tenure, he increased funding for the uninsured and underinsured residents
of Detroit, focusing on African American and Latino communities, and broadened services to
include domestic violence and sexual assault programs and CBPR efforts to address underlying
causes of health disparities in minority populations. He has received national and local awards
for his role in expanding access to culturally and linguistically appropriate health services.
xxii The Contributors
Guzman currently serves as chairperson of the board of directors for the National Association of
Community Health Centers in Washington, DC.
BUDD HALL, PhD, is professor of community development at the University of Victoria and
UNESCO co-chair in community- based research and social responsibility in higher education.
He has been working within a participatory research framework since 1973.
SUSANA HENNESSEY LAVERY, MPH, is health educator with the San Francisco Department
of Public Health, Community Health Equity and Promotion Branch (1992 to present). She
codesigns and implements the CAM (community action model) for policy development with
San Francisco’s diverse communities. She played a lead role in development of healthy retail
efforts, is the SFDPH staff member for the HealthyRetailSF program, and sits on the steering
committee of the Tenderloin Healthy Corner Store Coalition. For more than a decade, she has
participated on the Bay Area committee of Vision y Compromiso, a statewide community health
worker network. She is coauthor of numerous professional publications.
CHRISTINA HOLT serves as the associate director for Community Tool Box services at the KU
Center for Health Promotion and Community Development, where she directs the Community
Tool Box, a free global resource that offers seven thousand pages of practical guidance for cre-
ating change and improvement. She has served as a speaker and technical consultant for groups
including the World Health Organization, World Bank, United Nations, Peace Corps, and Insti-
tute of Medicine.
CHERYL HYDE, MSW, PhD, is associate professor at Temple University, School of Social
Work. Her primary areas of scholarship and teaching are organizational and community capacity
building, multicultural education, feminist praxis, social movements and collective action, and
socioeconomic class issues. She is a past president of the Association for Community Organi-
zation and Social Administration, former editor of the Journal of Progressive Human Services,
and a member of several social science and social work editorial boards and has practice expe-
rience in feminist, labor, and anti-oppression movements.
NADIA ISLAM, PhD, is an assistant professor in the Department of Population Health at
NYU School of Medicine. She is deputy director of the NYU Center for the Study of Asian
American Health and the research director for the NYU-CUNY Prevention Research Center.
She serves as PI on numerous federally funded initiatives evaluating the impact of culturally
adapted community- clinical linkages strategies on improving health outcomes in racial and
ethnic minority communities. Islam’s work has been featured in Diabetes Care, the American
Journal of Public Health, and other peer-reviewed journals.
BARBARA A. ISRAEL, DrPH, MPH, is professor of health behavior and health education,
School of Public Health, University of Michigan. She has published widely and is actively
involved in a number of CBPR partnerships examining and addressing, for example, the social
and physical environmental determinants of health inequities in cardiovascular disease and
childhood asthma and capacity building for and translating research ndings into policy change.
The Contributors xxiii
JUSTIN JAGOSH, PhD, is honorary research associate, Institute for Psychology, Health and
Society, University of Liverpool, and director for the Centre for Advancement in Realist Eval-
uation and Synthesis (www.liv.ac.uk/cares). He was coinvestigator on a comprehensive realist
review and evaluation of the CBPR. He runs regular training workshops in realist methodology,
including an annual summer school and a biennial international realist methodology conference.
See his website at www.realistmethodology-cares.org.
CAMARA PHYLLIS JONES, MD, MPH, PhD, a family physician and social epidemiolo-
gist, focuses on naming, measuring, and addressing the impacts of racism on the health and
well-being of the nation. Her allegories on race and racism illuminate topics that are otherwise
difcult for many Americans to understand or discuss. She is past president of the American
Public Health Association and a senior fellow at the Satcher Health Leadership Institute and
Cardiovascular Research Institute at the Morehouse School of Medicine. She was previously an
assistant professor, Harvard School of Public Health (1994 to 2000), and a medical ofcer at the
Centers for Disease Control and Prevention (2000 to 2014).
NORA JONES, MS, is executive director of the Partnership Project and the founding president
of Sisters Network Greensboro, a national breast cancer survivorship organization for African
American women. Currently, she is the lead community coinvestigator for the ACCURE
(Accountability for Cancer Care Through Undoing Racism and Equity) Research Study.
MIRIA KANO, PhD, research investigator, Department of Family and Community Medi-
cine, University of New Mexico, is the director of regional coordination for the geographic
management of cancer health disparities program region 3. She served as PI on the Patient-
Centered Outcomes Research Institute Pipeline to Proposal Award (highlighted in Appendix 2).
Kano has been a coinvestigator and research team member on four federally funded research
grants, as well as senior program manager for the New Mexico Center for the Advancement
of Research, Engagement and Science on Health Disparities, a P-20 center funded through the
National Institute for Minority Health and Health Disparities.
SARAH L. KASTELIC, PhD, MSW, is executive director of the National Indian Child Wel-
fare Association, where she serves as PI on several federally funded projects addressing the
well-being of American Indian and Alaska Native children. She is a citizen of the Native village
of Ouzinkie near Kodiak, Alaska, and the founding director of the Policy Research Center at the
National Congress of American Indians.
DMITRY KHODYAKOV, PhD, is senior behavioral-social scientist at RAND and core fac-
ulty member at Pardee RAND Graduate School. He specializes in methods of stakeholder and
patient engagement, expert elicitation, and intervention evaluation. Khodyakov is the author of
more than forty-ve peer-reviewed publications and has served as PI or co-PI on research pro-
jects funded by PCORI, NIEHS, and CMS, among others.
LAURA C. LEVITON, PhD, is senior advisor for evaluation at the Robert Wood Johnson
Foundation in Princeton, New Jersey, having overseen more than 120 national, state, and local
xxiv The Contributors
evaluations and a wide variety of other social research related to health. Leviton has coauthored
three books: Foundations of Program Evaluation (Sage, 1991), Confronting Public Health
Risks (Sage, 1997), and Managing Applied Social Research (Wiley, 2017).
RICHARD LICHTENSTEIN, PhD, recently retired as S. J. Axelrod Collegiate Professor of
Health Management and Policy at the University of Michigan School of Public Health, where
he taught for more than forty years. His research interests include CBPR, racial and ethnic dis-
parities in health, barriers to health insurance coverage for low-income children, and efforts to
increase diversity in the health workforce.
ALEXANDRA LIGHTFOOT, EdD, is research assistant professor in the Department of Health
Behavior in the Gillings School of Global Public Health at the University of North Carolina
at Chapel Hill. She also directs the Community Engagement, Partnerships and Technical
Assistance Core at the Center for Health Promotion and Disease Prevention, a CDC-sponsored
prevention research center. She conducts research using the CBPR approach in collaboration
with communities across North Carolina and provides training and technical assistance to build
and strengthen community-academic research partnerships.
ALISA LINCOLN, MPH, PhD, is interdisciplinary professor of Sociology and Health Sciences
and the director of the Institute on Urban Health Research and Practice at Northeastern Univer-
sity. Lincoln’s research examines the way that social exclusion and marginalization contribute
to and are a consequence of poor mental health. She has led the way in developing innovative
models by which we can increase the involvement of stakeholders and mental health service
users in the process of research through her NIMH-funded CBPR projects.
JULIE E. LUCERO, MPH, PhD, is assistant professor in the School of Community Health Sci-
ences at the University of Nevada, Reno. She is a mixed-methods researcher who uses CBPR to
promote social justice and health equity. She researches trust in community-academic partner-
ships, social determinants, diversity and inclusion, and research ethics.
MAYA MAGARATI, PhD, is a sociologist at the Indigenous Wellness Research Institute (IWRI)
in the University of Washington’s School of Social Work, where she serves as the associate
director of the Community Engagement and Outreach Core. She has served as a coinvestigator
in multiple federally funded participatory research studies to cocreate knowledge with Indige-
nous communities focused on culture-centered behavioral health protective factors.
JACK MAKAU is executive director of Shack/Slum Dwellers International–Kenya (SDI-
Kenya). He has almost twenty years of experience with mapping and surveying informal set-
tlements. He has worked in cities across Africa and advised the UN-Habitat, World Bank, and
numerous organizations on participatory slum upgrading.
LILLI MANN, MPH, is research associate in the Department of Social Sciences and Health
Policy at Wake Forest School of Medicine. She is involved in the development, implementation,
and evaluation of CBPR studies, focusing on interventions promoting health services access,
The Contributors xxv
sexual and reproductive health, HIV prevention, HIV care linkage, and retention among racial
and ethnic minority and sexual and gender-identity minority communities.
KELLY MATTHEWS, BSW, is outreach coordinator for the Rochester Prevention Research
Center: National Center for Deaf Health Research. Matthews has worked in the Deaf community
in the elds of HIV/AIDS, mental health, supported employment, obesity, and multiple public
health initiatives.
ELI MOORE, MA, was cofounder of the Safe Return Project and has facilitated CBPR processes
with environmental justice communities, farm workers, youth, and others over the last fteen
years. Eli is currently a program manager at the Haas Institute for a Fair and Inclusive Society
at UC Berkeley.
RACHEL MORELLO-FROSCH, PhD, is an environmental health scientist and professor in the
School of Public Health and the Department of Environmental Science, Policy and Management
at the University of California, Berkeley. Her research examines social determinants of environ-
mental health disparities among diverse communities in the United States with a focus on envi-
ronmental chemicals, air pollution, and climate change.
THE MORRIS JUSTICE PROJECT (MJP) is a collaborative research team of neighborhood
residents in the south Bronx and members of the Public Science Project, the CUNY Graduate
Center, John Jay College, and Pace University Law Center. The project was founded in 2011
after a group of local mothers, whose sons had been harassed by police as a result of a stop-
and-frisk policy disproportionately affecting African Americans and Latinos, decided to take
action. MJP’s research includes large community surveys and “sidewalk science,” for example,
temporary art installations in public spaces to gather and share data on residents’ concerns. The
collective has shared its research in numerous venues including the 2015 Citizen Science Forum
at the White House.
MICHAEL MUHAMMAD, PhD, is the current Paul B. Cornely Postdoctoral Fellow in the
University of Michigan’s School of Public Health Center for Research on Ethnicity, Culture,
and Health (CRECH). His work focuses on contemporary racism, eugenic ideology, struc-
tural inequality, and the evaluation of CBPR partnerships including the Detroit Community-
Academic Urban Research Center University of Michigan.
JENNIFER NALL, MPH, is health-promotion disease-prevention director at the Forsyth County
Health Department in Winston-Salem, North Carolina. She has worked in the eld of HIV/STIs
for more than fteen years and has experience with HIV counseling and testing, community-
based interventions, and program evaluation.
EMILY J. OZER, PhD, is clinical-community psychologist, professor of community health
sciences at the UC Berkeley School of Public Health, and cofounder of the Innovations for
Youth (I4Y) Center. She has authored more than sixty articles in participatory research, trauma
and resilience, and school-based interventions (funded by NIDA, NICHD, William T. Grant
xxvi The Contributors
Foundation, and CDC). Learning experiences with participatory research in India and Latin
America inspired her dual foci on youth-led participatory research and psychological resil-
iency in the face of stress and trauma. Ozer seeks equitable and sustained collaborations to
challenge rigid notions of evidence and to highlight insider expertise in changing the conditions
for positive development of marginalized adolescents and their communities.
LAURA CHANCHIEN PARAJÓN, MD, MPH, is the medical director and cofounder of the
nonprot organization AMOS Health and Hope. Based in Nicaragua, AMOS is dedicated to
using community-based and empowering approaches to reduce health disparities in Nicaragua.
She is passionate about applying CBPR frameworks in global health as well as training health
professionals and community health workers in CBPR principles and practice.
EDITH A. PARKER, DrPH, MPH, is professor and chair of the Department of Community
and Behavioral Health, University of Iowa College of Public Health, and was previously
associate professor at University of Michigan School of Public Health. Her research focuses on
community- engaged health promotion interventions. She has served as the PI or Co-PI on more
than twenty federally funded grants.
MYRA PARKER, JD, PhD, is an enrolled member of the Mandan and Hidatsa tribes and serves
as an assistant professor in the Center for the Study of Health and Risk Behavior in the University
of Washington School of Medicine’s Department of Psychiatry. Her research experience as a
coinvestigator on public health research with American Indian and Alaska Native communities
involves CBPR and disparities research funded through NIMHD, NIAAA, NIDA, and NIDDK.
CYNTHIA PEARSON, PhD, is the director of the research at the Indigenous Wellness Research
Institute. She is the author of more than sixty scientic publications and has served as a principal
and coinvestigator on more than thirty-two federally funded grants using an CBPR approach in
developing ethical research training curriculum, conducting studies on epidemiology of HIV
prevention and co-occurring mental and drug use disorders, and developing trauma-informed
HIV-prevention interventions among American Indian and Alaska Natives.
AMBER AKEMI PIATT, MPH, works at PolicyLink with the Convergence Partnership, advising
funders on strategies to advance health and equity through policy and practice changes. She
also serves on the Innovations for Youth (I4Y) community advisory board, Alameda County
Human Relations Commission, and the Sea Change Program’s advisory board. She has worked
on CBPR and YPAR projects since 2010 and sees participatory research as a critical way to
democratize knowledge and build community power.
MICHELE POLACSEK, PhD, MHS, is associate professor of public health at the University
of New England and recently served as PI on three grants examining school food and bev-
erage marketing environments, including digital marketing. She also recently served as lead
investigator on two studies evaluating innovative approaches to promote nutrition among low-
income populations in a supermarket setting. Michele has taught CBPR online and worked to
develop innovative teaching tools for this setting.
The Contributors xxvii
ABIGAIL REESE, CNM, MSN, is a doctoral candidate in health policy at the UNM College
of Nursing, and a Robert Wood Johnson Foundation Nursing and Health Policy Collabora-
tive Fellow. She is a certied nurse-midwife with extensive clinical and teaching experience in
diverse practice settings. She currently serves as the program director for the New Mexico Peri-
natal Collaborative. Her research focuses on access to care for underserved women.
ANGELA REYES, MPH, is the founder and executive director of Detroit Hispanic Development
Corporation, a nonprot community-based organization that works to create individual-level
change with youth and families and community systems–level change. She is also a founding
board member of the Detroit Community-Academic Urban Research Center, established in
1995, which involves multiple funded collaborative research and intervention projects aimed at
increasing knowledge and addressing factors associated with health disparities of residents in
Detroit, Michigan.
SCOTT D. RHODES, PhD, MPH, FAAHB, is professor and chair of the Department of
Social Science and Health Policy, Wake Forest School of Medicine in Winston-Salem, North
Carolina. He is director of the Program in Community Engagement within the Wake Forest
Clinical and Translational Science Institute. Rhodes currently has published more than 150
articles and thirty book chapters. His community-engaged and CBPR has been funded by the
National Institutes of Health, the Centers for Disease Control and Prevention (CDC), Health
Resources & Services Administration (HRSA), Robert Wood Johnson Foundation, amfAR:
The American Foundation for AIDS Research, the Cone Health Foundation, and the Kate B.
Reynolds Foundation.
AL RICHMOND, MSW, executive director of Community Campus Partnerships for Health
(CCPH), has a career that has uniquely blended social work and public health to address racial
and ethnic health disparities. As an international community health leader, Richmond advocates
for transformative partnerships to address the most critical issues facing our society. He is ada-
mant that “no meaningful and impactful change in our society is possible without partnerships.
Partnerships are not an option, but an imperative.”
LINDA ROBERTSON DrPH, RN, MSN, is associate director, health equity, education
and advocacy at the University of Pittsburgh Cancer Institute (UPCI) and assistant pro-
fessor of medicine at the University of Pittsburgh. She focuses her efforts and research on
building community partnerships and addressing health equity issues along the cancer care
continuum.
IVES ROCHA is a psychologist from Federal University of Rio de Janeiro and has worked
with public health, health promotion, and grassroots development since 2007. He is program
technical advisor of CEDAPS—The Centre for Health Promotion—and coordinator of youth-
led digital mapping in Brazil, a global initiative of UNICEF. He develops and monitors par-
ticipatory methodologies, especially with adolescents and young people. Ives is procient in
Construção Compartilhada de Soluções Locais social technology, consisting of participatory and
local-based diagnostic, plans of action, monitoring, and evaluation of grassroots experiences.
xxviii The Contributors
PATRICIA RODRÍGUEZ ESPINOSA, MS, MPH, is a doctoral candidate in clinical
psychology, University of New Mexico; a Robert Wood Johnson fellow, UNM Center
for Health Policy; and a psychology intern with VA Palo Alto Health Care System, afl-
iated with Stanford. Her research centers on the health of Latino and other minorities in
the U.S. with special attention to the role of cultural and social determinants of health in the
development of health disparities. She is interested in the application of CBPR in multicul-
tural psychology.
LETICIA RODRIGUEZ GARCIA, MPH, Community Health Worker (CHW) is a graduate
research assistant at Portland State University. She has more than fteen years of experience as
a CHW. Her research interests include CBPR, the roles of CHWs, and health disparities among
immigrant communities. She has presented at various local and national conferences on CHW
research–related efforts.
CLEO SAMUEL, PhD, is assistant professor of health policy and management at the University
of North Carolina at Chapel Hill. She is a health services researcher with expertise in cancer
care disparities and health informatics.
VICTORIA SÁNCHEZ, DrPH, associate professor in the College of Population Health at
the University of New Mexico, focuses her research on how people come together and build
capacity to enhance health equity and community well-being.
SHANNON SANCHEZ-YOUNGMAN, PhD, is a research assistant professor and political
scientist at the University of New Mexico. Her research focuses on the development and impact
of health and social policy on women of color and children in the United States.
KELLEY P. SAWYER is a PhD candidate in anthropology at the University of New Mexico.
JENNIFER SCHAAL, MD, retired ob-gyn, is a founding member of the Greensboro Health
Disparities Collaborative (GHDC) and an active antiracist organizer. She was a clinical
investigator for hormone replacement research while in practice and has participated actively
in the CBPR work of the GHDC. She has served on community research advisory boards for
local and national research grants; has copresented multiple CBPR workshops, keynotes, and
research presentations; and has coauthored peer-reviewed publications and book chapters.
JERRY SCHULTZ, PhD, is co-director of the KU Center for Community Health and
Development at the University of Kansas. His work is focused on building the capacity of
communities to solve local problems, understanding community and systems change, eval-
uating community health and development initiatives, and developing methodologies for
community improvement. He has coauthored numerous articles on evaluation, empowerment,
and community development. He has been a consultant to foundations, community coalitions,
and state agencies. Schultz was given the Society for Community Research and Action Award
for Distinguished Contribution to the Practice of Community Psychology in 2007 and is a fel-
low of the Society for Applied Anthropology.
The Contributors xxix
AMY J. SCHULZ, PhD, MPH, is professor of health behavior and health education at the
University of Michigan School of Public Health. She has served as PI for the Healthy
Environments Partnership since 2000 and multi-PI for community action to promote healthy
environments since 2014, both CBPR partnerships focused on environmental justice and health
equity in Detroit. She has authored more than 130 professional publications and has served as
PI on eleven federally funded research grants.
LAURO SILVA is a native-born New Mexican from the Capitan Mountains. As a grassroots
organizer and legal professional, Lauro has worked for social justice for ve decades with rural
and urban communities in public policy, community organizing, and law, especially for poor
Chicanos/as, Mexican immigrants, and Native Americans. He has worked with New Mexico’s
asylum refugees from Honduras, Guatemala, and El Salvador; with the Migrant Farmworker
Councils and Clinics; and with the environmental civil rights health movement. Among
many positions, he has been president of the Mountain View Neighborhood Association and
community PI of the South Valley Partners for Environmental Justice in Albuquerque.
FLORENCE M. SIMÁN, MPH, is the director of health programs at El Pueblo, an organiza-
tion based in Raleigh, North Carolina, whose mission is for Latinxs to achieve positive social
change. Florence is a founding board member of El Pueblo. She has worked on several pho-
tovoice projects, some led by UNC students, and is passionate about using photos as a tool to
encourage dialogue and to advocate for social justice.
BETH SMITH, RN, NE-BC, MSN, is the professional services practice manager at the
Cone Health Cancer Center. She has served as the oncology navigator for the ACCURE
Research Study.
ANDREW SUSSMAN, PhD, MCRP, is assistant professor in the Department of Family and
Community Medicine at the University of New Mexico. He is the director of RIOS Net, a
practice-based research network and has conducted research on a variety of primary care health
disparities topics among medically underserved populations in New Mexico.
ERIKA SUTTER, MPH, is deputy director of the Rochester Prevention Research Center: National
Center for Deaf Health Research at the University of Rochester Medical Center. She has worked
with RPRC/NCDHR since 2004 and is skilled in American Sign Language (ASL). Her research
experience includes the design, implementation, and dissemination of research studies and
community- based initiatives in the areas of Deaf health, health disparities, community health and
CBPR, adolescent health and mental health, adolescent access to care, and youth development.
RAJESH TANDON, PhD, is internationally acclaimed in participatory research, and founder and
director of the Society for Participatory Research in Asia (PRIA), providing support to grassroots
initiatives in South Asia. He has championed capacity building of the marginalized through their
knowledge and empowerment and has authored more than one hundred articles, a dozen books,
and training manuals on democratic governance, civic engagement, participatory research, and
people-centered development. For his work on gender, he received the Government of India’s
xxx The Contributors
Social Justice award, 2007; is the rst Indian inducted into the International Adult and Continuing
Education Hall of Fame, 2011; and was appointed UNESCO co-chair on Community-Based
Research and Social Responsibility in Higher Education (2012–2016 and 2016–2020).
AMANDA E. TANNER, PhD, MPH, is associate professor in the Department of Public Health
Education at the University of North Carolina Greensboro. Her research focuses on sexual and
reproductive health with specic areas of expertise including HIV and sexually transmitted
disease prevention, HIV care, intervention science, and microbicide and contraceptive access
and acceptability. She has served as PI or coinvestigator on multiple federally funded research
grants and has more than fty peer-reviewed publications.
PAM TAU LEE, BA, is a retired instructor at City College of San Francisco and a former
project director at the Labor Occupational Health Center, School of Public Health, University of
California, Berkeley. She also was a founding member of the Chinese Progressive Association,
San Francisco, and the Asian Pacic Environmental Network. A long-time activist and practi-
tioner of popular education, community organizing, and CBPR, she has made major contribu-
tions to improving the working conditions of immigrants and women.
KARI THATCHER, MPH, is the prevention specialist at the North Carolina Coalition Against
Domestic Violence and began serving as cochair of the Greensboro Health Disparities Collab-
orative in January 2017. She takes a network-oriented approach to community and institutional
organizing, driven by a belief in the importance of leadership and capacity building at the neigh-
borhood level. She also works independently, training and consulting with organizations and
communities working for racial equity.
RYAN THAYER, MA, is a community organizer and co-coordinator of the Tenderloin Healthy
Corner Store Coalition. As a sixth-generation San Franciscan, he holds a BA in urban studies and
planning from San Francisco State University and an MA in urban affairs from the University of
San Francisco. Since 2010, Thayer has cultivated community leadership to participate in a food
system that promotes equity and justice.
MAKANI N. THEMBA is chief strategist at Higher Ground Change Strategies based in Detroit,
Michigan. A social justice innovator and pioneer in the eld of change communications and
narrative strategy, she has spent more than twenty years supporting organizations, coalitions,
and philanthropic institutions in developing high-impact change initiatives. Higher Ground
Change Strategies is her newest project, which she describes as “a place where change makers
can get the support they need to take their work to the next level.” Higher Ground helps partners
integrate authentic engagement, systems analysis, and change communications and more for
powerful, vision-based change.
ROBB TRAVERS, PhD, is associate professor and chair, Department of Health Sciences,
Wilfrid Laurier University, Waterloo, Ontario. He is director of the Equity, Sexual Health and
HIV Research Group at Laurier’s Centre for Community Research, Learning and Action. His
CBPR focuses on social exclusion and its impact on the health of gender and sexual minorities.
The Contributors xxxi
CHAU TRINH-SHEVRIN, DrPH, is associate professor of population health and medicine at
the NYU School of Medicine and directs the Department of Population Health’s Section for
Health. Trinh-Shevrin is PI and founding director of the NIH NIMHD Center of Excellence, the
Center for the Study of Asian American Health, and co-PI of a CDC-sponsored NYU-CUNY
Prevention Research Center. She has more than ninety peer-review scientic and professional
publications.
LAVERN VAUGHN is case manager for Catholic Charities of San Francisco and a founding
member of The Safe Return Project in Richmond, California. The Safe Return Project is a
participatory action research process involving formerly incarcerated residents in conducting
research, engaging community members, and developing policy proposals to reduce recidivism
and improve community health and safety. During her years with Safe Return, Vaughn and
seven other Safe Return leaders conducted an extensive survey of recently released residents,
interviewed more than six hundred community members, and researched and developed pol-
icies that have been adopted at the city, county, and state level. Vaughn is a lifelong Richmond
resident, mother, grandmother, and passionate advocate for justice and her community.
AARON T. VISSMAN, PhD, MPH, is associate director of the Center for Health and Human
Services Research at Talbert House in Cincinnati, Ohio. He has published mixed-methods
research investigating correlates of antiretroviral adherence and the effectiveness of multilevel
HIV/AIDS prevention interventions. He received the Ruth L. Kirschstein National Research
Service Award (2013–2015). Ongoing studies investigate multilevel correlates of naloxone dis-
tribution and the effectiveness of opioid overdose and HCV prevention interventions.
TAMISHA WALKER is founder and executive director of Safe Return Project. Walker has
been a Richmond-based community organizer and known advocate on issues related to mass
incarceration and racial disparity in the criminal justice system since her release from incar-
ceration in 2009. Tamisha shares a powerful personal story about the journey to healing and
successful reentry. She has six years of community-organizing experience in a city affected
by trauma and economic inequality, including her own personal experience with trauma and
poverty growing up in Richmond, California. Her educational experience includes professional
training in research and advocacy for the formerly incarcerated and their families, violence-
prevention strategies, and conict mediation to reduce urban gun violence.
PEI-RU WANG, PhD, is senior research and evaluation analyst at the Multnomah County
Health Department Community Capacitation Center in Oregon. She leads a number of eval-
uation projects on community health worker and community leadership programs. She is also
a seasonal facilitator and trainer using popular education, inspired by Paulo Freire. She has
years of experience working in a nonprot organization supporting CHWs in the Asian Pacic
Islander, African, and Slavic communities.
JOMELLA WATSON-THOMPSON, PhD, is associate professor of applied behavioral sci-
ence and associate director for the KU Center for Community Health and Development at the
University of Kansas. She leads participatory research and evaluation efforts in the areas of
xxxii The Contributors
adolescent substance abuse prevention, community and youth violence prevention, and positive
youth development.
KENNETH B. WELLS, MD, MPH, is afliated adjunct staff at RAND and David Weil
Endowed Professor of Psychiatry and Biobehavioral Sciences at UCLA David Geffen School of
Medicine and of Health Policy and Management at UCLA Fielding School of Public Health. He
is director of the Semel Institute Center for Health Services and Society and codirector of the
California Behavioral Health Center of Excellence and Robert Wood Johnson Clinical Scholars
Program at UCLA. His research focuses on improving mental health outcomes, particularly
depression, through a community-partnered, participatory research approach.
WEST OAKLAND ENVIRONMENTAL INDICATORS PROJECT (WOEIP) is a nonprot
dedicated to working with neighborhood organizations, physicians, researchers, and public
ofcials to ensure West Oakland residents have a clean environment, safe neighborhoods, and
access to economic opportunity. It is codirected by Brian Beveridge, and Margaret Gordon, who
has received multiple city, county, and Bay Area honors for her environmental justice work.
NOELLE WIGGINS, EdD, MSPH, is director of Capacity Building and Collaboration, Whole
Person Care Program, LA County Dept. of Health Services. Previously, director at Multnomah
County Community Capacitation Center Portland, Oregon, she has more than thirty years training
and supervising community health workers (CHWs). Publications and presentation topics include
CHWs, popular education, participatory research and evaluation, and empowerment theory and
measurement.
CATHLEEN E. WILLGING, PhD, is center director and senior research scientist at Behavioral
Health Research of the Southwest, Pacic Institute for Research and Evaluation. As a medical
anthropologist, her research focuses on public mental health and substance use services in the
United States, health care reform, implementation science, and the advancement of culturally
and contextually relevant programs to support populations affected by health and health care
disparities.
KATHRINE E. WRIGHT, MPH, is a public health doctoral student at the University of Nevada,
Reno, specializing in social and behavioral health. She received her master of public health
degree at Michigan State University, where she specialized in public health nutrition. Her
research interests include using CBPR to address the causes and impacts of food insecurity and
hunger to promote health equity in marginalized populations.
MICHAEL T. WRIGHT, LICSW, MS, has been involved in community-based health initiatives
since 1984 in the United States and Germany, having served as a psychotherapist, program man-
ager, clinical supervisor, researcher, and consultant. Wright was formerly the director of inter-
national relations at the Deutsche AIDS-Hilfe, the national German AIDS organization. He is
currently professor for research methods, Catholic University of Applied Sciences, Berlin, and
heads the central ofce of the International Collaboration for Participatory Health Research. He
is coordinator of PartKommPlus, a national research consortium in Germany applying partici-
patory health research to examine integrated municipal strategies for health promotion.
Health equity is assurance of the conditions for optimal health for all people.
Achieving health equity requires valuing all individuals and populations
equally, recognizing and rectifying historical injustices, and providing resources
according to need. Health disparities will be eliminated when health equity
is achieved.
Camara Phyllis Jones
This third edition of Community-Based Participatory Research for Health: Advancing Social
and Health Equity shows the long-standing importance of doing research and interventions
with communities rather than to communities or only in communities. Community- originated
research questions, borne from lived experience, guide the work. Community-designed program
evaluations, whose results will provide important bases for action, are prioritized. Academics,
or other professionally trained research partners, collaborate on research in service of the
community rather than pursuing questions that only scratch the tickle of their own intellectual
curiosity.
In this book, community-based participatory research (CBPR) practitioners share their
experiences, models, tools, and lessons learned about the enriching work of academically
trained researchers and community members who join together in partnership. They partner to
identify and answer urgent scientic questions. They partner to design, conduct, and evaluate
relevant interventions. They partner to acknowledge and address the impacts of systems and
structures on human health, pushing beyond our society’s dominant and narrow focus on the
individual. They partner not only to acknowledge the importance of context on health but also to
intervene on those contexts. And they partner to address the systems of structured inequity that
determine the range of contexts in our society and the differential distribution of populations
into those contexts.
CBPR is the research operationalization of health equity. Operationalizing health equity
involves answering three questions: What is health equity? How do we get there? And how is
health equity related to health disparities (Jones,2014)?
1. What is health equity? Health equity is assurance of the conditions for optimal health for
all people. Assurance is a process, not an outcome, and assurance of the conditions for optimal
health requires making sustained, long-term investments in communities. It requires going
beyond a narrow focus on individual genes and individual behaviors to address the contexts of
people’s lives, the social determinants of health (including poverty and adverse neighborhood
conditions). As an important theoretical and well-illustrated addition to this third edition, CBPR
acknowledges the importance of context and sees context as a major and legitimate focus for
intervention.
PREFACE
xxxiv Preface
But assurance of the conditions for optimal health for all people also requires intervention
on the social determinants of equity (including racism and other systems of structured inequity).
These social determinants are the systems of power that determine the range of contexts in a
given place and time, as well as who lives in which context. Their mechanisms are embodied in
our structures, policies, practices, norms, and values, which, in turn, are the elements of decision
making. Structures are the who, what, when, and where of decision making, including who is
at the table and who is not and what is on the agenda and what is not. As illustrated particularly
in the nal section of this book, policies are the written how of decision making. Practices and
norms are the unwritten how of decision making, and values are the why. By connecting the
power bases of academia, community, progressive policy makers, and other key stakeholders,
CBPR enables a more concerted effort to shape structures, change policies, reveal practices,
inuence norms, and challenge those values that are antithetical to health and social equity.
2. How do we get there? Achieving health equity requires (a) valuing all individuals and
populations equally, (b) recognizing and rectifying historical injustices, and (c) providing
resources according to need. Academically trained CBPR researchers value community mem-
bers by honoring all they bring to the work. This means honoring, rst, their lived experience as
the basis for identifying important research questions and their expertise in creating solutions
as the basis for promising interventions. But it also means honoring their wisdom by bringing
unrepresented voices to research and policy decision-making tables, their time through equi-
table resource sharing, their talent through investment and training, and their treasure in people
and organizations. Community members involved in CBPR value academics and other outside
research partners by honoring their expertise in rening research questions and evaluation strat-
egies and honoring their good will, a necessary element for an authentic, empowering, and
sustained partnership.
Recognizing and rectifying historical injustices requires researching the history of each
“problem” to be solved in order to gain insights into effective solutions. As theorized and illus-
trated throughout this book, the context of CBPR acknowledges the possibility of previous
academic research efforts in communities that were not predicated on equal partnership, were
not sustained over time, did not invest in community knowledge or resources, or did not return
ndings and other resources for reection and action to the community.
Providing resources according to need requires agreement on metrics of need, followed
by a fearlessness in making sustained unequal investments that are based on need. Within the
context of CBPR, it is reected in the investment of research expertise, money, and infrastruc-
ture in those communities with the highest burdens, not in communities of convenience. And it
respects community prioritization of need in terms of problem identication.
3. How is health equity related to health disparities? Health disparities will be eliminated
when health equity is achieved. Health disparities are differences in outcomes, whereas health
equity is all about opportunity structures and societal valuation. To operationalize this notion,
researchers and non-researchers alike need to invest in opportunities, measure impacts on oppor-
tunities, and patiently await outcomes in a generation. We should make long-term investments in
communities and develop deep intergenerational partnerships. This includes research funding for
CBPR, which continues to go disproportionately to academic and other non-community partners.
CBPR moves the research enterprise from indulging the intellectual curiosity of aca-
demics in the ivory tower to unearthing and addressing questions of high relevance to partner
Preface xxxv
communities. It can bridge resources between those who currently have the power to decide, the
power to act, and the control of resources with those whose lives are currently undervalued and
whose opportunities are currently constrained.
Health equity, the assurance of the conditions for optimal health for all people, is an active
process requiring all hands on deck. CBPR offers one potent mechanism for engaging in the
work of achieving health equity. Indeed, the very act of partnership between academically
trained researchers and community members can be a revolutionary rst step. Whether you
are currently positioned in academia, a health or social services department, a city or regional
planning ofce, or in a community, open these pages and learn from the history of others to
become inspired and better equipped for your part in this journey.
REFERENCE
Jones, C. P. (2014). Systems of power, axes of inequity: Parallels, intersections, braiding the strands, Medical Care, 52,
S71–S75.
C P J, MD, MPH, PhD
August 2017
The burgeoning growth across the world of community-based participatory research (CBPR),
community-engaged research, action research, and other participatory approaches to health,
education, and social justice has made this book a challenge and a gift to produce almost a
decade after the second edition. We owe many thanks to the countless academic, practitioner,
and community colleagues who have built on the legacy of participatory pioneers and global
histories of struggle to re-form and re-create research as a place for knowledge democracy and
social and health equity. We have learned so much from others’ narratives, personal stories, and
the many theoretical frameworks, scientic and cultural analyses, ethical dilemmas faced in
practice, and other insights, which have enriched this book, and us, immeasurably. Although too
numerous to mention by name, their contributions are cited throughout the book, and they are
deserving of special recognition.
Many people in specic helped us to make this book a reality, and we are grateful to the
many coauthors whose hard work and belief in the power and potential of CBPR are reected in
the following pages. Each of them writes with commitment and passion, whether as a community
partner, practitioner, clinician, or academic for whom conducting participatory action-oriented
research with, rather than on or in, communities is a continuing goal.
Each of us also is supported and inspired by our colleagues, students, and community
partners working with the University of New Mexico, University of Washington, University
of Waikato, New Zealand, and the University of California, Berkeley. We owe thanks to the
W.K. Kellogg Foundation, the California Endowment, the Robert Wood Johnson Foundation
(RWJF), PolicyLink, the Community-Campus Partnerships for Health, and the Community-
Based Public Health Caucus of the American Public Health Association for their trail-blazing
support and inspiration in CBPR on so many levels. We thank especially community members
who have been our teachers, as well as our families and friends, because this book, similar to the
rst two editions, is in part due to their collective wisdom and support.
From Nina: great appreciation goes rst to my colleagues as editors and authors on this
book, who together have made this an almost completely new work. I am thrilled to see the
strength of effort throughout the country and globally that these chapters represent. For me
personally, I owe a great deal of thanks to the tribal research partners I have had the honor of
working with, including education and health professionals, elders, youth, and others from the
Pueblo of Jemez, the Ramah Band of Navajo, the Mescalero Apache Tribe, the Navajo Nation,
and from the Healthy Native Community Partnership. I continue to appreciate colleagues and
friends from public and community health throughout New Mexico, who have maintained a
commitment to social justice these many years.
In a wider network, I have deep gratitude to partners in the Engage for Equity and Research
for Improved Health studies, members of the national CBPR Think Tank, and to my participatory
health research colleagues around the world, especially from Latin America, Brazil and Nicara-
gua, who keep opening my eyes to Freirean empowerment as a path to equity. I wouldn’t be able
to do this work without the co-learning community connected to UNM’s College of Population
Health and Center for Participatory Research: students, faculty, staff, doctoral RWJF and UNM
ACKNOWLEDGMENTS
xxxviii Acknowledgments
Health Policy fellows, as well as other community-engaged committed scholars across the UNM
campus. Special thanks also to colleagues from San Francisco State University’s Department of
Health Education. My friends and family, siblings, parents, and especially now the younger gen-
eration of nieces and nephews have been deep sources of inspiration. Finally, I couldn’t do this
work without the love from my lifelong partner, David Dunaway, and our son, Alexei, whom I
now have the pleasure of seeing create his own equity-based work.
From Bonnie: a deep bow of gratitude to Meredith Minkler for my doctorate—I wouldn’t have
it without her faith in me and encouragement; to Nina for her brilliant, kind, and stern mentorship
and partnership over many years; and to John for applying his remarkable skills and values in our
work together. I’d like to thank all the tribal communities who have taught me the fundamental
meaning of participatory research, self-determination, and decolonization and who have gener-
ously shared Indigenous epistemologies and healing modalities. A special thanks to the Tribal
College and university presidents and community, including AIHEC, the Navajo, and Lummi
Nation IRBs, for their truth-telling, insistence on tribal benet, and use of Indigenous theories of
etiology and change. Deep gratitude bows to my Buddhist teachers and colleagues at the Insight
Meditation Society and Spirit Rock Meditation Center for the wisdom, compassion, and refuge.
And special thanks and love to Stan Kondo for his warmth, patience, support, and partnership.
From John: I want to thank Nina and Meredith for including me as a coeditor of this edition
and to Nina and Bonnie for being long-time collaborators. I look forward to our continued
work together. I also want to thank my community and academic partners on the He Pikinga
Waiora and Kaumātua Mana Motuhake projects for their inspiration, passion, collaboration,
and inclusiveness (Tihei Mauri Ora!). It is such a pleasure to work with you. Further, I want to
thank a few people whom I collaborate with outside of work. To my mates at the Raglan Vol-
unteer Fire Brigade (EAD), thanks for being great teachers and practitioners of collaboration
and helping me do something positive for the community. And last and most important, to my
family, Spencer, Ethan, and Keri: I appreciate your love and support always.
From Meredith: my sincere thanks to friends and coeditors Bonnie Duran, John Oetzel,
and our visionary lead, Nina Wallerstein, who remains a dear friend and role model and one
who never lets overcommitment keep her (or me) from taking on exciting, new collaborative
efforts, such as this book. My deepest gratitude goes as well to my community teachers and
partners, including the Tenderloin Healthy Corner Store Coalition, the Chinese Progressive
Association, the Richmond (California) Safe Return Project, and the California Senior Leaders
Alliance. I also remain indebted from afar to the men and women of Concerned Citizens of
Tillery, North Carolina, their visionary leaders Gary Grant and Naeema Muhammad, and their
lead academic research partner, the late Steve Wing, who together exemplied a standard of
CBPR and community organizing to which I can only aspire.
Among my family and friends, my late father was my inspiration, guide, and shining light,
even in his last days, and the greatest teacher I have ever known. My late mother showed in her
long struggle with Alzheimer’s the same gifts of love, concern for others, and optimism that
characterized the whole of her life. My siblings Donna, Jay, Chris, and Joan are each among my
closest friends and a source of pride in the separate paths they have taken and the values they
share. I am grateful, as well, to extended family members Betsy Minkler, Rose Marie Springer,
Joyce Lashof, and to dear friends whose deep caring and support make my own work possible.
My husband, Jerry Peters, and our sons, Jason Peters and Marquis Parks, have been the source
of much love, pride, support, and humor, and I owe them my deepest gratitude.
COMMUNITY-BASED
PARTICIPATORY
RESEARCH
FOR HEALTH

PART
1
INTRODUCTION:
HISTORY AND
PRINCIPLES

1
CHAPTER
COMMUNITY-BASED PARTICIPATORY RESEARCH (CBPR) has established itself as a
valued research approach for its contributions to increasing health equity through an orientation
that is community-based, and often community-directed, rather than merely community placed.
Increasing demand by communities, tribal nations, governmental and philanthropic funders,
and committed academics have altered much of the landscape of research and its production
of knowledge by integrating community leaders and members as key partners throughout a
community-engaged research process. The W.K. Kellogg Foundation’s Community Health
Scholars Program (2001) dened community-based participatory research in the health eld
as “a collaborative approach to research that equitably involves all partners in the research pro-
cess and recognizes the unique strengths that each brings. CBPR begins with a research topic
of importance to the community with the aim of combining knowledge and action for social
change to improve community health and eliminate health disparities” (p. 2).
Reecting the growing application of CBPR principles and strategies in community
development, program design and implementation, and evaluation, we propose a broader de-
nition that still incorporates the use of research and data. “CBPR embraces collaborative efforts
among community, academic, and other stakeholders who gather and use research and data to
build on the strengths and priorities of the community for multilevel strategies to improve health
and social equity.”
Together with many related action, participatory, and community-engaged research tradi-
tions, CBPR turns upside down the more traditional applied research paradigm, in which the
ON COMMUNITY-BASED
PARTICIPATORY RESEARCH
NINA WALLERSTEIN, BONNIE DURAN, JOHN G. OETZEL,
AND MEREDITH MINKLER
4 Community-Based Participatory Research for Health
outside researcher largely has determined the questions asked, the research tools employed, the
interventions developed, and the kinds of outcomes documented and valued (Gaventa & Corn-
wall,2015). In their new edited book, Budd Hall and Rajesh Tandon, two of the early founders of
global participatory research, reiterate the call for knowledge democracy to reclaim the “exper-
tise residing in the world of practice, beyond academia” (Hall, Tandon, &Tremblay,2015, p. 26).
Although often and erroneously referred to as research methods, CBPR and other collabora-
tive approaches are not methods at all but an orientation or a fundamentally different approach
to research. As Cornwall and Jewkes (1995) classically pointed out, what is distinctive about
this approach “is not the methods but the methodological contexts of their application; the atti-
tudes of researchers, which in turn determine how, by and for whom research is conceptualized
and conducted,” and “the corresponding location of power at every stage of the research pro-
cess” [italics added, p. 1667].
Central to CBPR and related approaches is a commitment to consciously change the power
relationship between researcher and researched, seeking to eradicate the distinction between
who does the studying and who gets studied (or decides what gets studied). CBPR, as an
overall approach, has been used with every kind of research method (Israel, Eng, Schulz, &
Parker,2013): from qualitative focus groups or ethnographic inquiry, to neighborhood mapping
or use of geographical information systems, to epidemiology, and to survey methods. What
matters is “the experience and partnership of those we are normally content simply to mea-
sure” (Schwab & Syme,1997, p. 2050) and the creation of a “mutually reinforcing partnership”
(Cargo & Mercer,2008, p. 327).
NEW AND CONTINUING CHALLENGES AND OPPORTUNITIES
In the decade since the publication of the second edition of this book (Minkler & Waller-
stein,2008), CBPR has grown as a eld in its effectiveness in creating culture-centered research
(Dutta, Anaele, & Jones,2013), improving external validity and attention to implementation
contexts (Yano et al.,2012), honoring practice-based and community evidence (Green,2006),
strengthening reexive practice (Muhammad et al.,2015), and solidifying connections to com-
munities of color and other marginalized communities to challenge health inequities (Waller-
stein & Duran,2010). However, CBPR faces continuing and new challenges.
Key among these is the stark contextual realities within which we work. Health and social
inequities continue to rise to untenable levels, across the United States and globally (Bor, Cohen,
Galea,2017; Marmot & Bell,2012). Within the United States, structural racism within institutions,
such as the criminal justice system, and conscious and unconscious bias still pervade our national
consciousness and contribute to the suffering of real people and communities. As this book goes
to press, a new and troubling political context in the United States, with grave threats to vulnerable
groups, including to undocumented immigrants, the devaluation of science and inquiry, and the
threatened withdrawal of federal funding in a wide range of areas, portend real threats to CBPR
partnerships and health and social equity. These conditions affect all of us and our capacities to rec-
ognize and redress power and privilege differences across academia and communities and agencies.
The research institution is not immune from this context, with historical and current abuse
or misuse all too often having fostered mistrust of research within communities who have
faced “helicopter” or “drive-by” research when data is solicited, taken, and not returned to the
On Community-Based Participatory Research 5
community. “Evidence-based” approaches, those that have received sufcient funding to be
systematically evaluated and published in the academic literature, still dominate the accept-
able choices for research interventions and privilege internal validity over external validity, or
relevance of ndings to “real-world” contexts. Such approaches are sometimes unacceptable
or non-translatable to other diverse communities. Further, the “evidence-based” approaches
that “count” in traditional academic and other research settings often ignore, discount, or erase
the “community evidence” and local knowledge necessary to create culturally effective and
sustainable interventions. Growing calls for translational research, whose ndings can more
quickly and effectively be incorporated into practice, programs, and policies, have been critical
in beginning to redress such imbalances (Cytron et al.,2014). Yet often, translation is thought
to be unidirectional, that is, a one-way or top-down approach to move research results from the
academy to the community, rather than as bidirectional, mutual-learning processes.
Despite these challenges, there has been increased visibility of and support for CBPR and
community-engaged research (CEnR) in multiple sectors. The Centers for Disease Control and
Prevention (CDC) launched its Prevention Research Centers in 1986 with community partic-
ipation a central part of their mission. The rst of the National Institutes of Health (NIH) to
fund CBPR was the National Institute of Environmental Health Science (NIEHS), supporting
environmental justice research in 1995. NIEHS was followed by multiple other institutes, most
notably the National Institute of Minority Health and Health Disparities and the Native American
Research Centers for Health, a partnership between the Indian Health Service and NIH.
Since the mid-2000s, there has been additional growth in federal and foundation funding
opportunities for CBPR (see Appendix 5). These have included community engagement com-
ponents within Clinical Translational Science Awards (CTSAs); the Patient Centered Outcomes
Research Institute (PCORI), inviting patient, family, and patient advocate engagement; NIH
transdisciplinary team science centers that include community partner involvement; as well as
leading foundations sponsorship of CBPR training programs (see Chapter19 and Appendix 5).
Support has become evident through new federal publications, with a recent Institute of
Medicine (IOM) call to educate health professionals about social determinants through forming
community partnerships for transformational learning (IOM,2016). This builds on an Ofce of
Behavioral and Social Science Research (OBSSR) report, calling for working with communities
to understand the complexities of culture (Kagawa-Singer, Dressler, George, & Elwood,2015)
and a previous IOM call for leveraging community involvement and culture for improved health
interventions (IOM,2012). In 2015, the North American Primary Care Group updated their
1988 policy on responsible participatory research in primary care settings and called for even
greater patient and community involvement in research (Allen et al.,2017).
CBPR and CEnR publications have grown across multiple health, clinical, education, and
social science disciplines, with top-ranked academic journals offering special issues on CEnR,
CBPR, and Action Research in addition to multiple new books (Abma et al.,2018, Blumenthal,
DiClemente, Braithwaite, & Smith,2013; Bradbury,2015; Hacker,2013; Hall et al.,2015; Israel
et al.,2013; Rowell, Bruce, Shosh, & Riel,2017; Stringer,2014; Wright & Kongats,2018).
Finally, many new resources, training programs, and guides are proliferating, and can often be
found through the Community Campus Partnerships for Health and CES4 Health websites, as
well as on individual program sites (see, for example, Parry, Salsberg, & Macaulay,2017; see
Appendix 10 for resources specically on measures of engagement).
6 Community-Based Participatory Research for Health
Although these increased opportunities, especially in the acceptance of CEnR and CBPR,
have been welcome, they also have brought new challenges. The rst of these is denitional,
with the question of whether we have fallen into the trap of believing that any community
engagement is a good thing (Draper, Hewitt, & Rifkin,2010). Trickett (2011) has raised con-
cerns about utilitarian usage of CBPR by researchers, for example, seeking engagement to facil-
itate recruitment of minorities into “our” research trials, versus a broader worldview that seeks
a range of community capacity, health, and social justice outcomes.
A second challenge is the need for more rigorous and mixed-method evaluation of whether
and how participatory practices contribute to outcomes, with a complementary inquiry to iden-
tify metrics or measures to assess engagement practices and outcomes. A plethora of reviews
within the last several years have begun to identify multilevel health outcomes from CBPR and
related research, with several analyzing the ingredients of participatory practices that make a
difference (Drahota et al.,2016; O’Mara-Eaves et al.,2015; Rifkin,2014; Salimi et al.,2012).
Although many of us are part of this effort to identify emerging “best” or promising prac-
tices, the most important questions may be (1) under what conditions and contexts do partner-
ships choose which practices are “best” or promising in their experience; and (2) how will our
chosen practices affect research designs and interventions to produce our desired (and also pos-
sibly unintended) outcomes within communities and the academy, including, most importantly,
improvement of health equity?
Further, some still question the scientic rigor of the eld, for example, regarding the
challenge of how to maintain community decision-making after starting a randomized con-
trol trial protocol (Buchanan, Miller, & Wallerstein, 2007; Coghlan, 2004; Northridge
et al., 2000; Salimi et al., 2012). Greater interest in complexity science, adaptive designs,
and social network analyses, however, have enabled a broader discussion of methodologies
for evaluating community participation and interventions (Franco et al., 2015; Hawe,2015;
Trickett et al., 2011) and for incorporating strategies that promote a broader bandwidth of
validity ( Bradbury,2015). Decolonizing research methodologies (Denzin, Lincoln, & Tuhiwai
Smith,2008; Tuhiwai Smith,2012) have called for Indigenous and community knowledge and
use of mixed methodologies for ascertaining partnership effectiveness to reach broad goals of
knowledge democracy and justice.
AGENDA FOR THE NEW EDITION
With this backdrop of challenges and opportunities, this is an almost completely new edition
of Community-Based Participatory Research for Health, offering a twofold agenda. First, we
wish to celebrate the recognition of CBPR and CEnR as solid, community-driven, and shared
leadership enterprises and their importance for making inroads toward health equity. Second,
we wish to tackle head on the challenges frequently encountered in this work through inter-
weaving theory, methods, and case studies with thoughtful exploration of core issues of trust,
racism, cultural humility, power and privilege, self-reective practice, and ethics, with emphasis
on practices that contribute to outcomes.
We invite you, as students, academics, and community practitioners in elds such as public
health, social welfare, nursing, medicine, communication, community and regional planning,
public policy, education, social sciences, and other elds, to enter these explorations with us
On Community-Based Participatory Research 7
and become more inspired by and procient in applying CBPR approaches in your own work.
The new edition has been reframed to follow the CBPR conceptual model rst presented in the
second edition (Wallerstein et al.,2008). Use of this revised model (see Chapter6) enables us
to more deeply present cases that address the contextual settings for research, the partnership
relationships and practices, the ethics and choice of research and evaluation methods, and a
commitment to individual and community health, equity, and social justice outcomes. All of
our case studies are new, many of which tackle core issues of our time, such as institutional
racism and its contributions to inequities and suffering. We look to CBPR as one strategy for
promoting healing within communities and for advocating for desperately needed policy and
societal change.
In this chapter, we now situate CBPR principles within a brief history of other traditions
and provide an overview of current reviews of CBPR and community engagement effectiveness.
We end the chapter with an outline of the book and a hope that the conceptual frameworks, case
studies, and practical tools presented through the chapters and appendices are useful as you
reect on and strengthen your own partnering practices.
CORE PRINCIPLES OF CBPR WITHIN A CONTINUUM
OF COMMUNITY ENGAGEMENT
Over the last several decades, the term community-based participatory research has moved sol-
idly into US and global health discourse and practice. Numerous variations of the term exist,
however; key among them are action research (widely used in the education eld and within the
United Kingdom, Australia, and New Zealand); collaborative action research (used in Austra-
lia); community-based research (term in Canada); participatory action research and participatory
research (widely used in Latin America, the Global South, and for youth); collaborative inquiry;
reexive practice, feminist participatory research; community-partnered participatory research;
tribal participatory research; street and citizen science; and participatory health research, the
term of the International Collaboration for Participatory Health Research (see Appendix 3).
These terms have largely come from two historical traditions: the Northern, more pragmatic
tradition (with social psychologist Kurt Lewin originally proposing action research in the 1940s
as a cycle of fact-nding, action, and reection) and the Southern emancipatory tradition (with
the terms participatory research and participatory action research emerging from the roots
of Brazilian educator Paulo Freire’s (1970,1973) popular education and the liberatory move-
ments in the 1970s in Asia, Africa, and Latin America). (See Chapter2 for discussion of these
traditions.)
Adherents to these different terms continue to engage in lively debate over which one
best captures the principles and ideological commitments espoused. We argue, however, that
although these different approaches often vary in goals and in change theories, they also share
a set of core principles, summarized by Israel and her colleagues (see Chapter3), who say the
following of CBPR:
■ It is participatory.
■ It is cooperative, engaging community members and researchers in a joint process in which
both contribute equally.
8 Community-Based Participatory Research for Health
■ It is a co-learning process.
■ It involves systems development and local community capacity building.
■ It is an empowering process through which participants can increase control overtheir lives.
■ It achieves a balance between research and action.
Building on the work of scholars of color, Indigenous, and feminist participatory
researchers, we add to these principles an additional one, recognizing the importance of inter-
sectional power and privilege, i.e., how race-ethnicity, racism, immigrant status, gender, sexual
orientation, social class, and culture affect the research process (Minkler, Garcia, Rubin, &
Wallerstein,2012). As discussed in Chapter4, such realities underscore the need for academics
to adopt cultural humility (see Appendix 4) and its task of lifelong learning, being open to
reecting on one’s biases and positions of power and privilege.
Indigenous researchers have added other principles grounded in tribal sovereignty, recog-
nizing the authority of tribal communities to control research processes, demand that data be
shared and returned to tribes, and approve all publications, in addition to deepening the rec-
ognition of core values of respect and relevance (Noe et al.,2006; Walters et al.,2009). Tribal
institutional review and research review boards have added the principle of returning benet
to the communities (Becenti-Pigman et al.,2008) as part of their authority (Chapter14), and
so have emerging numbers of community ethics boards and review processes (see Chap-
ters15 and16).
The growth in the use of the term community-engaged research in the 2000s was
spawned, in part, by the extensive investment in CTSA translational research infrastructures
in academic health centers. A CTSA published continuum of engagement (in English and
Spanish) ranges from community outreach at one end, through coordination and collab-
oration, to shared leadership at the other (McCloskey et al.,2011). Although recognizing
that community engagement can shift over time, the inclusion of outreach, unfortunately,
may reinforce a unidirectional, rather than bidirectional, perspective. The continuum, “on-
in-with,” from the Community Engagement Core of the University of New Mexico NM-
CARES Health Disparities Center clearly shows the difference of research that takes place
on targeted communities, versus in community settings, versus research with community
partners. It is the with perspective that reects the CBPR denition of equity and strengths
of all partners.
1
Community development advocates and public health professionals, however, have long
warned against the cooptation or manipulation of communities through language and methods
that purport to foster participation and engagement, while in fact using local communities to
the advantage of the researchers (Arnstein,1969; Cooke & Kothari,2001; Draper et al.,2010).
Although an extreme example, the four-decade-long Tuskegee study of untreated syphilis in
Black males, which continued to withhold treatment long after penicillin was available, to study
the long-term effects of the disease (Reverby,2009), provides a deeply disturbing example. As
Thomas and Quinn (2001) point out,
the study included culturally-appropriate and grassroots approaches to ensure the involvement
and continued participation of [Black physicians and prisoners]...The Public Health Service was
extremely successful in enlisting Black church leaders, elders in the community and plantation
owners to encourage participation. (p. 1499)
On Community-Based Participatory Research 9
The underlying racism inherent in this study remains an indelible reminder of the human
costs of unethical scientic research and the ways in which “community participation,” can, and
sometimes has, been used to for horric and unjust ends.
To ensure the inclusion of CBPR values and principles, in a recent review of the acceler-
ating extent of community-engaged and partnered research awards within the US Environmental
Protection Agency, Yuen, Park, Seifer, and Payne-Sturges (2015) added a “community-driven”
column to the CTSA continuum, beyond shared leadership, which mirrors the CBPR deni-
tion that research should be based on community priorities, strengths, and actions. Balazs and
Morello-Frosch (2013) have gone further in constructing an explanatory continuum that shows
the evolution from community members being research subjects to becoming research part-
ners, depending on their level of participation. Focus groups to elicit community opinions,
for example, are not in themselves CBPR. CBPR requires structures for participation such as
community advisory boards or equitable partnership teams that have decision-making authority.
As Balazs and Morello-Frosch (2013) further assert, integrating community members as full
research partners enables science to be rigorous and relevant, with greater reach, by working
deeply with communities (see Chapter15).
Ultimately, these continua remind us of the importance of reecting on our own values and
commitment to confront power dynamics within research processes to benet communities.
To live up to the espoused principles of CBPR for health—principles accenting true partner-
ships among researchers, communities, clinical providers, patients, and other stakeholders and
achieving a balance between research and action toward health equity—is the emancipatory
end of the continuum that should serve as a gold standard for CBPR practice. Particularly for
professionals in elds such as public health, social welfare, and community planning, among
others, with their roots in concerns for social justice, CBPR in this sense provides an important
goal for which to strive in our collaborative work with communities.
EFFECTIVENESS OF CBPR AND COMMUNITY-ENGAGED RESEARCH
The rst systematic review of CBPR, by the Agency of Health Care Research and Quality in
2004, spanned the years 1975–2003 and found sixty CBPR studies, with thirty identied as
interventions and thirteen with a policy focus. Few of these studies had rigorous designs and
only twelve documented outcomes (Viswanathan et al.,2004). Within Britain, corollary interest
in assessing the impact of community engagement within research and population health initia-
tives spawned multiple reports (Popay et al.,2007; Staley,2009).
Since that time, and especially since 2009, when CBPR became a medical subject head-
ing (MESH) in the Library of Medicine, there has been a signicant growth of systematic
reviews and meta-analyses that have found compelling evidence of positive impacts on health
outcomes (Anderson et al.,2015; Carter, Tregear, & Lachance,2015; Cook,2008; Cyril, Smith,
Possamai-Inesedy, & Andre,2015; de las Nueces, Hacker, DiGirolamo, & Hicks, 2012; Drahota
et al.,2016; Milton et al.,2012; O’Mara-Eves et al.,2015; Yuen et al.,2015).
In a systematic review of impacts of community engagement among disadvantaged popula-
tions, Cyril and colleagues (2015) found that 88 percent of twenty-four studies had positive out-
comes, with dened CBPR studies showing higher community involvement throughout research
processes. A meta-analysis of 131 CEnR articles, including randomized and non-randomized
10 Community-Based Participatory Research for Health
designs, found positive impacts on health behavior, health consequences, self-efcacy, and per-
ceived social support (O’Mara-Eves et al.,2015). de Las Nueces et al. (2012), in a systematic
review of CBPR clinical trials with racial-ethnic minorities, found 89 percent of their nineteen arti-
cles to have behavioral and clinical outcomes and high success in retaining minority participants.
Thompson et al. (2016) identied NIH-funded population health and disparities centers
that focused on CBPR projects to empower communities toward health equity. Salimi and col-
leagues (2012) sought to review community empowerment by assessing community partic-
ipation in all the stages of research. They found that more studies involved community members
in selecting research questions (42 percent), with only 8 percent having community mem-
bers involved in proposal writing or with nancial responsibilities. Involving community
members throughout research processes has been validated as a promising practice that is asso-
ciated with outcomes of shared power relations in research and community transformation (see
Chapters6 and17). Drahota and colleagues (2016), in their systematic review across multiple
disciplines, identied fty community-academic partnership studies, documenting 78 percent
with proximal outcomes, such as synergy or knowledge exchange, with one-third reporting
capacity and system outcomes, such as improved community care, sustainable partnerships, or
changed community context.
Some studies have sought to identify the type of participatory engagement, such as com-
munities identifying health needs and mobilizing, communities collaborating on design,
communities consulting on intervention design, and community members collaborating or
leading intervention delivery, such as using lay health workers (Brunton, O’Mara-Eves, &
Thomas,2014; O’Mara-Eves et al.,2015). Lay-delivered interventions had the largest effect
sizes in a recent Cochrane Review of collaborations, which found limited other impacts on
ethnic-racial minority health (Anderson et al.,2015).
The growing number and positive outcomes of these reviews help document the power
of CBPR and CEnR in contributing to intermediate outcomes such as community capacities
and longer-term health outcomes. Recent NIH-funded experimental trials, based in long-time
culturally-grounded CBPR partnerships, are producing more evidence of outcomes (Dickerson
et al., in press). For meta-studies, however, the Cochran criteria of comparison trials or health-
specic outcomes are too limited.
A growing literature exists, for example, in CBPR policy studies, which don’t show up in
comparison designs but that document substantial health impacts from policy changes (Minkler
et al.,2012). Because they often affect the health and social environments of large numbers of
people, such studies (see Chapters20 to23) also should be included in systemic reviews.
Increasing evidence of impacts from participatory processes document that they are highly
complex and not controllable as dened intervention impacts (Abma et al.,2017; Rifkin,2014;
South & Phillips,2014; Trickett et al.,2011). Empowerment strategies in CBPR, for example,
based on Paulo Freire’s (1970) dialogical methods, are not predictable interventions but rather
dynamic processes within dynamic contexts. Evaluation of such efforts needs to include con-
text as much as processes and outcomes. Jagosh and colleagues (2012) have found that broader
goals of joint policy advocacy and capacity-building may be equally important to perceived
partnership success, in addition to specic grant outcomes. Calls for CBPR as a liberatory social
movement further challenge us to critically analyze how we can best achieve improved health
equity for all (Devia et al., 2016; Tremblay, Martin, Macaulay, & Pluye,2017).
On Community-Based Participatory Research 11
In sum, CBPR should not be seen simply as an instrumental strategy but rather as grounded
by its commitment to community priorities and decision making. Although we are pleased by
the growing evidence of specic outcomes, we also seek broader intermediate and long-term
outcomes, such as changed power dynamics, cultural revitalization, community empowerment,
and improved health and social equity (see Chapters17 and18).
ORGANIZATION OF THIS BOOK
In this third edition, we build on our core values of health equity and social justice as we present
new diverse case studies that represent ongoing frontiers of CBPR and CEnR. With the addition of
two new editors, we have made major changes in our framing, following the domains of the CBPR
conceptual model (see Chapter6), rst introduced in the second edition. Although much cutting-
edge participatory research continues outside the United States, our purpose is to focus primarily on
CBPR in the contemporary United States, in part so that we can carefully attend to the geopolitical
and sociohistorical contexts so central to this work. However, we frequently draw on the wisdom
of leading participatory research, action research, participatory action research, and participatory
health research scholars and practitioners in the Global South from Latin America, Asia, and Africa,
and from Canada, Europe, the United Kingdom, Australia, New Zealand, and elsewhere, and we
believe that many of the skills and conceptual and ethical issues raised will have relevance beyond
the United States. (See global issues in Chapters7,18,23; Appendices 3, 6; and the Afterword.)
Part 1 begins with this chapter introducing the eld, with Chapter2 presenting its historical and
theoretical antecedents and new concepts of cognitive justice and knowledge democracy from the
Global South. Chapter3 describes and illustrates the classic, as well as evolving principles of CBPR.
In Part 2, Chapter4 examines race, racism, power and privilege; Chapter5 discusses the
dynamics of trust in partnerships.
Part 3 begins the new framing by introducing the CBPR conceptual model with its four
domains, with case studies focusing on the rst domain, “Context,” and the second domain,
“Partnering Processes.” Chapter 6 rst introduces the history and domains of the CBPR
conceptual model. Chapter7 discusses CBPR within a youth context. Chapter8 provides a
randomized control trial to transform structural racism and bias within the context of cancer
health care. Chapter9 discusses the challenges of alignment and misalignment among academic
and community partners.
Part 4 continues to the third domain of the model, “Research and Interventions,” with
case studies on how partnering processes contribute to the promising practices of culturally
and locally appropriate research design and implementation. Chapter10 explores community-
engaged methods within health care system research projects. Chapter11 speaks to the creation
of culture-centered interventions within the Deaf and hearing impaired community. Chapter12
challenges us to integrate CBPR principles into interventions with highly diverse Asian popula-
tions. Chapter13 presents a developmental process for engaging Latino communities in every
step of research design and implementation.
In Part 5, we extend our research methods into core ethical promising practices. We learn
the importance of culture and governance within tribal contexts (Chapter14) and unpack eth-
ical issues within (Chapter15) and beyond (Chapter16) institutional review boards (IRBs) and
research review boards.
12 Community-Based Participatory Research for Health
Part 6 then continues to the fourth “Outcomes” domain of the model, with Chapter17
providing evidence, from testing the CBPR model, of promising partnering practices associated
with a range of intermediate and long-term outcomes. Chapter18 showcases US and Nica-
raguan case studies of participatory evaluation outcomes with lay health advisors. Chapter19
shares personal stories and outcomes for faculty members of color who have beneted from
CBPR pipeline programs.
In Part 7, we deepen the focus on policy outcomes, with Chapter20 providing an over-
view and an adapted CBPR policy model. We incorporate powerful examples of policy envi-
ronmental changes within food security and healthy retail (Chapter21), criminal justice reform
(Chapter22), and youth mapping of their living conditions within Kenyan and Brazilian slums
(Chapter23).
We conclude with appendices designed to provide tools and applications so partnerships
can put some of the messages central to this book into practice in their own CBPR efforts.
The afterword by long-time participatory research international scholars brings us back to
knowledge democracy in the global context.
CONCLUSION
Although the United States continues to have profound health and social inequities based on
race, ethnicity, class, gender, age, ability-disability, sexual orientation, and gender identity, the
ght for equity can be won only if vulnerable and oppressed communities can be fully engaged
as partners in taking action to address the health and social problems about which they—not
“outsider experts”—know most deeply. With communities now more directly under siege, the
need for CBPR visibility and sustainability is even more pronounced.
Our primary goal in this book is to provide a highly accessible text that will stimulate prac-
titioners, students, and academics in health and related elds, as well as community partners
and researchers, as they engage—intellectually and in practice—in collaborative inquiry for
action. We hope that those with substantial experience and newcomers will nd themselves
challenged by the theory, methods, and case studies.
We end this chapter with a quote from Pia Moriarty (1993), who in her work with the
Commission on Social Justice for the San Francisco Archdiocese wrote about the visceral
nature of deep learning and its importance for us, as we seek to create equitable partnerships
and knowledge for personal and societal transformation:
Deep learning involves the whole body, blood and bone, not just the theoretical or cataloguing
of insightful facts and analyses. Deep learning moves the feet to walk in a new way, moves the
eyes to see from the new perspective won by that walking, and moves the hands to fashion the
tangible world into a new image envisioned by the new seeing. (p. 1)
QUESTIONS FOR DISCUSSION
1. Cornwall and Jewkes (1995) argue that CBPR is not a research method but an “orienta-
tion to research” that reects a different stance from traditional research. How would you
describe this alternative paradigm to a friend or colleague who’s never heard of CBPR?
On Community-Based Participatory Research 13
2. CBPR is described as a promising approach for health equity research. What CBPR char-
acteristics do you think are most important for the study of health inequities with margin-
alized communities?
3. Community engagement is described as a continuum from outreach to shared leadership and
community-driven approaches. The more emancipatory forms of CBPR are presented as a
“gold standard” for which professionals might strive. Do you agree with this? Why or why not?
NOTE
1. http://hsc.unm.edu/programs/nmcareshd/cec.shtml
REFERENCES
Abma, T., Cook, T., Ramgard, M., Kleba, E., Harris, J., & Wallerstein, N. (2017). Social impact of participatory health
research: Collaborative non-linear processes of knowledge mobilization. Journal of Action Research. www.tandfonline.
com/doi/full/10.1080/09650792.2017.1329092
Abma, T., Banks, S., Cook, T., Dias, S., Madsen, W., Springett, J., & Wright, M. (2018). Participatory research for health and
social well-being. New York: Springer Basic.
Allen, M. L., Salsberg, J., Knot, M., LeMaster, J. W., Felzien, M., Westfall, J. M., Herbert, C. P., Vickery, K., Culhane-Pera,
K. A., Ramsden, V. R., Zittleman, L., Martin, R. E., & Macaulay, A. C. (2017). Engaging with communities, engaging
with patients: Amendment to the NAPCRG 1998 policy statement on responsible research with communities. Family
Practice, 34(3), 313–321.
Anderson, L. M., Adeney, K. L., Shinn, C., Safranek, S., Buckner-Brown, J., & Krause, L. K. (2015). Community coalition-
driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database of
Systematic Reviews, 6(CD009905). doi:10.1002/14651858.CD009905.pub2
Arnstein, S. R. (1969). A ladder of citizen participation. Journal of American Instructional Planners, 35, 216–224.
Balazs, C. L., & Morello-Frosch, R. (2013). The three Rs: How community-based participatory research strengthens the rigor,
relevance, and reach of science. Environmental Justice, 6(1), 9–16.
Becenti-Pigman, B., White, K., Bowman, B., Palmenteer-Holder, N. L., & Duran, B. (2008). Research policies, processes and
protocol: The Navajo Nation Human Research Review Board. In M. Minkler & N. Wallerstein, Community-based partici-
patory research for health: Processes and outcomes (2nd ed., pp. 441–446). San Francisco, CA: Jossey-Bass.
Blumenthal, D., DiClemente, R., Braithwaite, R., & Smith, S. (2013). Community-based participatory health research:
Issues, methods and translation to practice (2nd ed.). New York: Springer.
Bradbury, H. (Ed.). (2015). The Sage handbook of action research (3rd ed.). Thousand Oaks, CA: Sage.
Bor, J., Cohen, G. H., & Galea, S. (2017). Population health in an era of rising income inequality: USA, 1980–2015, Lancet,
389(10077), 1475–1490.
Brunton, G., O’Mara-Eves, A., & Thomas, J. (2014). The “active ingredients” for successful community engagement
with disadvantaged expectant and new mothers: A qualitative comparative analysis. Journal of Advanced Nursing, 70,
2847–2860.
Buchanan, D. R., Miller, F. G., & Wallerstein, N. (2007). Ethical issues in community-based participatory research: Balancing
rigorous research with community participation in community intervention studies. Progress in Community Health Part-
nerships: Research, Education, and Action, 1, 153–160.
Cargo, M., & Mercer, S. L. (2008). The value and challenges of participatory research: Strengthening its practice. Annual
Review of Public Health, 29, 325–350.
Carter, M. W., Tregear, M. L., & Lachance, C. R. (2015). Community engagement in family planning in the U.S.: A systematic
review. American Journal of Preventive Medicine, 49(2 Suppl 1), S116.
Coghlan, D. (2004). Action research in the academy: Why and whither? Reections on the changing nature of research. Irish
Journal of Management, 25(2), 1–10.
14 Community-Based Participatory Research for Health
Cook, W. K. (2008). Integrating research and action: A systematic review of community-based participatory research to
address health disparities in environmental and occupational health in the USA. Journal of Epidemiology and Community
Health, 62(8), 668–676.
Cooke, B., & Kothari, U. (2001). Participation: The new tyranny? New York, NY: Zed Books.
Cornwall, A., & Jewkes, R. (1995). What is participatory research? Social Science & Medicine, 41, 1667–1676.
Cyril, S., Smith, B. J., Possamai-Inesedy, A., & Andre, M.N.R. (2015). Exploring the role of community engagement in
improving the health of disadvantaged populations: A systematic review. Global Health Action, 8, 1–12.
Cytron, N., Pettit, K. L., Kingsley, G. T., Erickson, D. J., & Seidman, E. S. (Eds.). (2014). What counts: Harnessing data
for America’s communities. San Francisco, CA: Federal Reserve Bank of San Francisco and Washington, DC: Urban
Institute. Retrieved from www.whatcountsforamerica.org
de las Nueces, D., Hacker, K., DiGirolamo, A., & Hicks, L. S. (2012). A systematic review of community-based participatory
research to enhance clinical trials in racial and ethnic minority groups. Health Services Research, 47, 1363–1386.
Denzin, N. K., Lincoln, Y. S., & Tuhiwai Smith, L. (2008). Handbook of critical and indigenous methodologies. Thousand
Oaks, CA: Sage.
Devia, C., Baker, E., Sanchez-Youngman, S., Barnidge, E., Golub, M., Motton, F., Muhammad, M., Ruddock, C., Vicuña, B.,
& Wallerstein, N. (2017). CBPR to advance social and racial equity: Urban and rural partnerships in Black and Latino
communities. BMC International Journal of Health Equity, 16, 17. doi:10.1186/s12939-016-0509-3
Dickerson, D. L., Baldwin, J., Belcourt, A., Belone, L., Gittelsohn, J., Kaholokula, J. K., Lowe, J., Patten, C., & Wallersteinl,
N. (in press). Encompassing cultural contexts within scientic research methodologies in the development of health
promotion interventions. Prevention Science. Special Issue: Innovations in intervention research with indigenous popula-
tions in the U.S.
Drahota, A., Meza, R., Brikho, B., Naaf, M., Estabillo, J. A., Gomez, E., Vejnoska, S., Sufek, S., Stahmer, A., & Aarons, G.
(2016). Community-academic partnerships: A systematic review of the state of the literature and recommendations for
future research. Milbank Quarterly, 94(1), 163–214.
Draper, A. K., Hewitt, G., & Rifkin, S. (2010). Chasing the dragon: Developing indicators for the assessment of community
participation in health programmes. Social Science & Medicine, 71, 1102–1109.
Dutta, M. J., Anaele, A., & Jones, C. (2013). Voices of hunger: Addressing health disparities through the culture-centered
approach. Journal of Communication, 63, 159–180.
Franco, Z. E., Ahmed, S. M., Maurana, C. A., DeFino, M. C., & Brewer, D. D. (2015). A social network analysis of 140
community-academic partnerships for health: Examining the Healthier Wisconsin Partnership Program. Clinical and
Translational Science, 8, 311–319.
Freire, P. (1970). Pedagogy of the oppressed. New York, NY: Seabury Press.
Freire, P. (1973). Education for critical consciousness. New York, NY: Seabury Press.
Gaventa, J., & Cornwall, A. (2015). Power and knowledge. In H. Bradbury (Ed.), The Sage handbook of action research: Par-
ticipative inquiry and practice. (3rd ed.). Thousand Oaks, CA: Sage.
Green, L. W. (2006). Public health asks of systems science: To advance our evidence-based practice, can you help us get more
practice-based evidence? American Journal of Public Health, 96, 406–409.
Hacker, K. (2013). Community-based participatory research. Thousand Oaks, CA: Sage.
Hall, B., Tandon, R., & Tremblay, C. (Eds.). (2015). Strengthening community-university research partnerships: Global per-
spectives. Victoria, BC, Canada: University of Victoria.
Hawe, P. (2015). Lessons from complex interventions to improve health. Annual Review of Public Health, 36, 307–323.
Institute of Medicine (IOM). (2012). An integrated framework for assessing the value of community-based prevention. Wash-
ington, DC: National Academies Press.
IOM. (2016). A framework for educating health professionals to address the social determinants of health. Washington, DC:
National Academy of Sciences.
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (Eds.). (2013). Methods in community-based participatory research for
health (2nd ed.). San Francisco, CA: Jossey-Bass.
Jagosh, J., Macaulay, A. C., Pluye, P., Salsberg, J., Bush, P. L., Henderson, J., Sirett, E., Wong, G., Cargo, M., Herbert, C. P.,
Seifer, S. D., Green, L. W., & Greenhalgh, T. (2012). Uncovering the benets of participatory research: Implications of a
realist review for health research and practice. Milbank Quarterly, 90(2), 311–346.
On Community-Based Participatory Research 15
Kagawa-Singer, M., Dressler, W. W., George, S. M., & Elwood, W. N. (2015). The cultural framework for health: An inte-
grative approach for research and program design and evaluation. Bethesda, MD: Ofce of Behavioral and Social
Sciences Research.
Lewin, K. (1946). Action research and minority problems. Journal of Social Issues, 2, 34–46.
Marmot, M., & Bell, R. (2012). Fair society, healthy lives. Public Health, 126, S4–S10.
McCloskey, D. J., et al. (2011), Principles of community engagement (2nd ed.). NIH Publication No. 11-7782, Clinical
and Translational Science Awards Community Engagement Key Function Committee Task Force on the Principles of
Community Engagement. Bethesda, MD: National Institutes of Health. Retrieved May 15, 2017, from www.atsdr.cdc.
gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf; see: https://ncats.nih.gov/ctsa/community.
Milton, B., Attree, P., French, B., Povall, S., Whitehead, M., & Popay, J. (2012). The impact of community engagement on
health and social outcomes: A systematic review. Community Development Journal, 47, 316–334.
Minkler, M., Garcia, A., Rubin, V., & Wallerstein, N. (2012). Community-based participatory research: A strategy for
building healthy communities and promoting health through policy change. Retrieved from www.policylink.org/sites/
default/files/CBPR.pdf
Minkler, M., & Wallerstein, N. (2008). Community-based participatory research for health: Processes and outcomes (2nd
ed.). San Francisco, CA: Jossey-Bass.
Moriarty, P. (1993). Deep learning for earthquake country. Future of prophetic Christianity: Essays in honor of Robert
McAfee Brown. New York, NY: Orbis Books.
Muhammad, M., Wallerstein, N., Sussman, A. L., Avila, M., Belone, L., & Duran. B. (2015). Reections on researcher iden-
tity and power: The impact of positionality on community-based participatory research (CBPR) processes and outcomes.
Critical Sociology, 41(7–8), 1045–1063.
Noe, T. D., Manson, S. M., Croy, C., McGough, H., Henderson, J. A., & Buchwald, D. S. (2006). The inuence of
community-based participatory research principles on the likelihood of participation in health research in American
Indian communities. Ethnicity & Disease, 17(1 Suppl 1), S6–S14.
Northridge, M. E., Vallone, D., Merzel, C., Greene, D., Shepherd, P., Cohall, A. T., et al. (2000). The adolescent years:
An academic-community partnership in Harlem comes of age. Journal of Public Health Management and Practice,
6(1), 53–60.
O’Mara-Eves, A., Brunton, G., Oliver, S., Kavanagh, J., Jamal, F., & Thomas, J. (2015). The effectiveness of community
engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health, 15(1), 1352.
Parry, D., Salsberg, J., & Macaulay, A. C. (2017). Guide to researcher and knowledge-user collaboration in health research.
Retrieved May 2017 from www.cihr-irsc.gc.ca/e/documents/Guide_to_Researcher_and_KU_Collaboration.pdf
Popay, J., Attree, P., Hornby, D., Milton, B., et al. (2007), Community engagement in initiatives addressing the wider social
determinants of health: A rapid review of evidence on impact, experience and process. London, UK: National Collabo-
rating Center of Community Engagement, National Institute for Health and Health Care Excellence.
Reverby, S. M. (2009). Tuskegee’s truths: Rethinking the Tuskegee syphilis study. Ann Arbor, NC: UNC Press Books.
Rifkin, S. (2014). Examining the links between community participation and health outcomes: A review of the literature.
Health Policy and Planning, 29, ii98–ii106.
Rowell, L., Bruce, C., Shosh, J., & Riel, M. (Eds.). (2017). Palgrave international handbook of action research. New York,
NY: Springer Nature.
Salimi, Y., Shahandeh, K., Malekafzali, H., Loori, N., Kheiltash, A., Jamshidi, E., Frouzan, A. S., & Majdzadeh, R. (2012).
Is community-based participatory research (CBPR) useful? A systematic review on papers in a decade. International
Journal of Preventive Medicine, 3(6), 386–393.
Schwab, M., & Syme, S. L. (1997). On paradigms, community participation, and the future of public health. American
Journal of Public Health, 87, 2049–2052.
South, J., & Phillips, G. (2014). Evaluating community engagement as part of the public health system. Journal of Epidemi-
ology and Community Health, 68, 692–696.
Staley, K. (2009). Exploring impact: Public involvement in NHS, public health and social care research. Eastleigh,
UK: INVOLVE.
Stringer, E. (2014). Action research (4th ed.). Thousand Oaks, CA: Sage.
Thomas, S. B., & Quinn, S. C. (2001). Light on the shadow of the syphilis study at Tuskegee. Health Promotion Practice,
1, 234–237.
16 Community-Based Participatory Research for Health
Thompson, B., Molina, Y., Viswanath, K., Warnecke, R., & Prelip, M. (2016). Strategies to empower communities to reduce
health disparities. Health Affairs, 35, 1424–1428.
Tremblay, M. C., Martin, D. H., Macaulay, A. C., & Pluye, P. (2017). Can we build on social movement theories to develop
and improve community-based participatory research? A framework synthesis review. American Journal of Community
Psychology. doi:10.1002/ajcp.12142
Trickett, E. J. (2011). Community-based participatory research as worldview or instrumental strategy: Is it lost in translation(al)
research? American Journal of Public Health, 101(8), 1353–1355.
Trickett, E. J., Beehler, S., Deutsch, C., Green, L. W., Hawe, P., McLeroy, K., Miller, R., Rapkin, B., Schensul, J., Schulz, A.,
& Trimble, J. (2011). Advancing the science of community-level interventions. American Journal of Public Health, 101,
1410–1419.
Tuhiwai Smith, L. (2012). Decolonizing methodologies: Research and Indigenous peoples (2nd ed.). New York, NY:
Zed Books.
Viswanathan, M., Ammerman, A., Eng, E., Gartlehner, G., Lohr, K. N., Grifth, D., et al. (2004). Community-based
participatory research: Assessing the evidence (Evidence Report/Technology Assessment No. 99; Prepared by RTI
International–University of North Carolina). Rockville, MD: Agency for Healthcare Research and Quality.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(Suppl 1), S40.
Wallerstein, N., Oetzel, J., Duran, B., Tafoya, G., Belone, L., & Rae, R. (2008). What predicts outcomes in CBPR? In M.
Minkler & N. Wallerstein (Eds.). Community-based participatory research for health: Processes and outcomes (2nd ed.,
pp. 371–392). San Francisco, CA: Jossey-Bass.
Walters, K., Stately, A., Evans-Campbell, T., Simoni, J., Duran, B., Schultz, K., Stanley, E., Charles, C., & Guerrero, D.
(2009). “Indigenist” collaborative research efforts in Native American communities. In A. R. Stiffman (Ed.), The eld
research survival guide (pp. 146–173). New York, NY: Oxford University Press.
W.K. Kellogg Foundation Community Health Scholars Program. (2001). Stories of impact [brochure]. Ann Arbor: University
of Michigan, School of Public Health, Community Health Scholars Program, National Program Ofce.
Wright, M., & Kongats, K. (Eds.). (2018). Participatory health research: International perspectives. New York: Springer.
Yano, E. M., Green, L. W., Glanz, K., Ayanian, J. Z., Mittman, B. S., Chollette, V., & Rubenstein, L. V. (2012). Implementa-
tion and spread of interventions into the multilevel context of routine practice and policy: Implications for the cancer care
continuum. Monographs: Journal of the National Cancer Institute, 2012(44), 86.
Yuen, T., Park, A. N., Seifer, S. D., & Payne-Sturges, D. (2015). A systematic review of community engagement in the
US Environmental Protection Agency’s extramural research solicitations: Implications for research funders. American
Journal of Public Health, 105(12), e44–e52.
2
CHAPTER
The next few years comprise a key moment in which social science must up its
game to address and challenge inequality, in alliance with other actors who are
already raising their voices. The time is now.
ISSC
IN THIS HISTORICAL moment, the presuppositions of the academy, research, and health and
social interventions cannot assert neutrality. Insights into the nature of science, language, and
subjectivity outlined in history and critical social theory alert us to the operation of power in
familiar discourses that have tended to disguise or neutralize it. Social and clinical research
and practice benet from this investigation, which provides an opportunity for professional,
collective, and personal reexivity on how and where research produces change. Health and
social interventions benet from agents (ourselves as researchers, practitioners, providers)
who acknowledge how we embody histories, theories, values, and political stances, which may
include documenting historical and current resistances to research. As CBPR and community-
engaged researchers and practitioners, we can also benet from the values and contributions of
THEORETICAL, HISTORICAL,
AND PRACTICE
ROOTS OF CBPR
NINA WALLERSTEIN AND BONNIE DURAN
18 Community-Based Participatory Research for Health
“knowledge systems of the South” (de Sousa Santos,2013). The challenge for us is how to use
our science to co-construct knowledge with those living with inequalities who may be best posi-
tioned to inuence change in social and health practices, policies, and politics.
The forces promoting community-academic research partnerships come from government
public policies, academic structures and incentives, and the pressures for engagement gener-
ated by civil society. Community and scientic leaders and workers and patients from many
disenfranchised groups have begun to demand that research show greater sensitivity to com-
munities’ perceptions, needs, and unique circumstances, bringing new attention to the meaning
of relationships, codes of conduct, trust, and mutually benecial partnerships (Anderson &
Olson,2013).
Health disparities research is increasingly conducted within the framework of participatory
research approaches (see Chapter1 for multiple complementary terms and approaches). These
approaches have the advantage of providing greater external validity, challenging standardized
research protocols, and promoting responsible research conduct (Wallerstein & Duran,2010).
We see more deeply how race and racism, ethnicity, socioeconomic status, nativity, gender iden-
tity, sexual orientation, ableism, and so on affect core values and communication that constitute
our research practices, even within our research partnerships (Muhammad et al.,2015), with
implications for mistrust within research and science itself (Oetzel et al.,2015).
By broadening and deepening the team of researchers to include those who are often simply
“researched,” we not only strengthen research processes but also contribute to more nuanced,
complex, and authentic research outcomes. The results are not “alternative facts” of the sort put
forward by the Trump administration in the United States. Rather, they are a deeper and richer
understanding of the topic under study, which in turn can improve the science and the transla-
tion of research ndings into actions to improve health and social equity.
The majority of participatory research approaches can be traced to one of two histor-
ical traditions that represent distinct approaches within a continuum of values. Collaborative
utilization–focused research, with practical goals of systems improvement, is sometimes called
the Northern tradition. This is juxtaposed against openly emancipatory research, challenging
the historical colonizing practices of research and political domination of knowledge by the
elites, which is often called the Southern tradition
1
(Hall, Tandon, & Tremblay,2015).
This chapter will articulate the historical roots of these two traditions and briey discuss
theories of participation, knowledge democracy, power, and contributions from feminist, post-
colonial, and post-structuralist perspectives to clarify points of convergence and difference.
Although we articulate differences, both traditions have embraced four pillars of “engaged
excellence”: delivering high-quality research, co-constructing knowledge, mobilizing impact-
oriented evidence, and building enduring partnerships (Oswald, Gaventa, & Leach,2017).
This chapter ends with practical approaches for implementing Freirean dialogical education
to address challenges in the eld. Key among these challenges are how—and how much—trans-
formative change can, in fact, occur at the local level given current complex external forces,
including growing conservative forces advocating deep cuts in federal and other government
support. Although such questions may have relevance for the Northern and Southern traditions,
their deep intersections with knowledge democracy, power sharing, and other concepts central
to the progressive Southern tradition make them particularly relevant to CBPR praxis embedded
in this worldview.
Theoretical, Historical, and Practice Roots of CBPR 19
Although the best of CBPR contains dimensions from multiple traditions, this chapter
argues that the paramount public health goal of eliminating health and social inequities demands
a research practice within the emancipatory perspective, a practice that fosters the democratic
participation of community members to transform their communities as well as for academics
to transform institutions of higher education. Any discussion of theories of research engagement
must acknowledge the systemic processes that produce widespread suffering and therefore afrm
liberation and processes of liberation (Dussel,2013). As the 2016 World Social Science Report
species, social science is under an ethical demand to respond critically to such suffering (ISSC/
IDS,2016). Inequality has become a global concern for citizens, activists, scholars, and policy
makers, because it is inexorably linked to issues of planetary survival, health, gender justice,
cultural and cognitive justice, knowledge democracy, and more. Society’s future directions have
to be based on universally accepted values of equity, justice, inclusion, peace, and sustainability.
TWO HISTORICAL TRADITIONS
As part of the genesis of the Northern collaborative utilization-focused research approach, in the
1940s German social psychologist Kurt Lewin coined the term action research (Bargal,2008).
Lewin challenged the gap between theory and practice and sought to solve practical problems
through a research cycle involving planning, action, and investigating the results of the action
(Lewin & Gold,1999). He rejected the positivist belief that researchers study an objective world
separate from the meanings understood by participants as they act in their world.
This tradition emanates most broadly from sociologist Talcott Parsons and his predecessors,
who viewed social progress as based on rational decision making, applying ever- increasing
scientic knowledge to real-world problems. With an emphasis on practitioners acting as
coequals to academically trained researchers in their inquiry process, action science researchers
have often worked in a consensus model, with institutional changes based on new knowledge
and transformational leadership that inspires a self-reective community of inquiry. In edu-
cation, for example, teachers have joined academics as co-researchers in research-practice
partnerships (Glassman, Erdem, & Bartholomew,2013; Coburn & Penuel, 2016). Humanistic
psychology strengthened cooperative inquiry within this tradition, adopting a belief in human
agency through reexive inquiry (Rowan,2006).
In the early 1970s, a second Southern tradition of participatory research was born, with
impetus from Marxist critiques of structural crises of underdevelopment, liberation theology,
and the search for new practice by adult educators and community developers among popula-
tions vulnerable to globalization. An outow of social science and education academics from
universities to work with land movements and community-based organizations created an open-
ness to knowledge from people’s experience (Fals-Borda,2006).
Exiled Brazilian philosopher Paulo Freire, whose writings were banned during Latin
American dictatorships in the 1970s, helped transform the research relationship from commu-
nities as objects of study to community members participating in the inquiry (Freire,1970,1982).
To Freire (1982), reality was not objective facts to be discovered but “includes the ways in
which the people involved with facts perceive them. . . The concrete reality is the connec-
tion between subjectivity and objectivity, never objectivity isolated from subjectivity” (p. 29).
Rather than viewing research as neutral, participatory researchers adopted commitments to
20 Community-Based Participatory Research for Health
social justice, with the ideology that people who are poor and oppressed can transform their
conditions through their own actions based on their critical consciousness (Fals-Borda & Rah-
man,1991). (See also Chapter 18 on Transformative-Participatory Evaluation.)
By mid-1970s, progressive institutions outside academia took the lead with the International
Participatory Research Network, composed of the International Council for Adult Education,
Toronto, and centers in India, Tanzania, Netherlands, and Latin America. Similar nodes have
included the Collaborative Action Research Group in Australia (Kemmis et al.,2013) and the High-
lander Research and Education Center, Tennessee, the oldest adult education and social change
center in the United States (Horton & Freire,1990). The rst international symposium on partic-
ipatory research was held in Cartagena, Colombia, in 1977; and the eighth in 1997 also in Carta-
gena, attracting two thousand delegates from sixty-one countries, based in social movements and
the popular education of Paulo Freire (Fals-Borda,2006). Forty years after the rst conference, the
Action Research Network of the Americas, formed in 2012, joined this international movement
with a third conference in Cartagena, honoring the memory of Orlando Fals-Borda.
The interests of CBPR participants from US communities of color often resonate with the
Southern approach because these participants have recognized the colonizing role of research,
education, and religion (Said,1994). With Indigenous peoples, public health and medical dis-
courses have often “deauthorized” traditional ways of knowing for the purposes of controlling
Native populations. As recently as the 1960s, top health journals were publishing “research”
and medical characterizations of Indigenous peoples as primitive, lacking hygiene, having
exotic mental disorders, or dying out (e.g., Bahl,1961).
Placing the different participatory and action research terms used by various disciplines on
a continuum between the problem-solving utilitarian approach and the emancipatory approach
is difcult because actual research practice varies by local context, history, and ideology of
stakeholders. The same term may even be used with opposite meanings. Action research (Brad-
bury,2015) and participatory action research (PAR), for example, have been used to describe the
emancipatory participatory research tradition (McTaggart, Nixon, & Kemmis,2017) and the orga-
nizational development tradition (Argyris & Schön,1996; Whyte,1991). In an exhaustive mono-
graph on the different paradigms of collaborative social inquiry, Trickett and Espino (2004) called
for greater transparency of researchers on their own assumptions, practice, and desired outcomes.
In general, however, organizational action science and related traditions grounded in the
Lewinian model are to be found at the end of the continuum focusing on pragmatic use of
knowledge, with participatory and “PAR” approaches (Fals-Borda,1998, pg.169) associated
with Southern liberatory Freirian goals generally clustered at the other end. The term CBPR
emerged from the language and history of “community-based” public health practice in the
United States with the “participatory research” values of the Southern tradition. Understanding
these issues within the core concepts of participation, knowledge democracy, power, and
Freirian praxis will enable each of us to reect on our own practice at different times along the
continuum, including how we may embody different elements from each tradition.
PARTICIPATION
Habermas (1987) observed that “in the process of enlightenment, there can only be participants”
(p. 40). If we adopt Habermas’s succinct statement for CBPR, the core questions become, What
Theoretical, Historical, and Practice Roots of CBPR 21
do we mean by participation? Who is participating, for whom are we participating, in what
spheres are we participating, to what ends are we participating, and perhaps most important of
all, who or what is limiting participation in shaping our lives? In other words, where does the
power lie (Gaventa & Cornwall,2015)?
For CBPR, in particular, we need to ask, “If all research involves participation, what makes
research participatory?” (Cornwall & Jewkes, 1995, p. 1668). Despite decades of a value-
based rhetoric of participation from the World Health Organization or development studies,
only relatively recently have researchers begun to question whether the reality of participa-
tion reects the ideal. Some have questioned the authenticity of the participatory process (Tan-
don,1988) or through NIH-funding have sought participation for a limited purpose, such as
increasing minority recruitment into research trials.
Cooke and Kothari (2001) argue that communities are often viewed naively, concealing
power relations and masking biases. They propose three tyrannies: when community member
decision making is overridden by development experts (or researchers), when group dynamics
may reinforce individuals already in power, and when research methods dictate only one level
of inquiry, that is, seeking local data rather than identifying larger social policies that constrain
local action. These issues remind us that CBPR is not “reied out there, but constructed by a
cadre...of professionals, be they academics, practitioners or policymakers, whose ability to
create this discourse is indicative of the power they possess” (Cooke & Kothari,2001, p. 15).
The most important issue for community-based participatory researchers may be the rela-
tionship between academic researchers and community members. Habermas (1987) theo-
rizes about two distinct modern worlds: the systems world of legal, economic, and political
systems and the life world of families and cultural traditions in which individuals reproduce
their identities and knowledge. As the life world has become dominated by the systems world,
people increasingly see themselves as objects—clients and consumers—rather than subjects
or democratic members of civil society. Within CBPR, outside researchers may unwittingly
become part of this dynamic. Even within CBPR goals of authentic partnership, the actual
practice between researchers and community members remains complex and involves making
power and positionality transparent (see Chapter4; Appendix 4; Muhammad et al.,2015). In a
participatory study of healthy communities in New Mexico, for example, not recognizing power
differences between communities and the evaluator inhibited equal collaboration and therefore
use of research ndings (Wallerstein,1999).
Participation or lack of participation in research has been shaped by patterns of historical
abuse, with communities increasingly demanding decision making to determine what research
is done and who will do it. If CBPR practitioners fail to recognize these histories, they might
be denied entry or have their research undermined through overt or hidden forms of resistance.
At the same time, the contribution of CBPR researchers should not be undervalued. Academics
often know of funding opportunities and have key expertise to offer about important health
issues. Negotiation, therefore, of shared guidelines or formal agreements, and paying attention
to ethical issues, which are both part of IRBs (Chapter15) and extend beyond individual harm
and benet considerations (Chapters16), can become critical for participatory partnerships. In
working with tribal sovereign nations, in particular, codes of ethics and tribal IRBs often couple
community and cultural benet with permission to conduct research (see Chapter14; Canadian
Institutes of Health Research,2007–2010).
22 Community-Based Participatory Research for Health
Who represents the community remains a key issue in participation. Although service pro-
viders are asked to serve on community advisory boards, they may or may not represent their
constituents (Jewkes & Murcott,1998). CBPR takes the view that community members them-
selves should participate in ongoing collaborative advisory and decision-making structures that
go beyond participating in focus groups or in a single step of the research process. As discussed
in Chapter 17, the community engaged for research index (CERI) documents community
involvement in all research steps, from problem identication through data analysis and dissem-
ination. Community involvement, along with other promising practices, such as sharing budgets
(or the community agency as the principal investigator with subcontracts to academics), can
facilitate greater equality in participation in the partnership (see Chapter17). As Rifkin (1996)
indicates, participation should not be seen as a magic bullet but as a complex and iterative pro-
cess, which can change, grow, or diminish, based on the unfolding of power relations and the
historical and social context of the research project.
KNOWLEDGE DEMOCRACY
The creation and the use of knowledge are inherently the motivating forces behind all research;
yet similar to participation, CBPR raises questions of by whom, about whom, and for what
purpose this knowledge is dened (Hall et al.,2013). Although positivist research paradigms
consider knowledge creation to be neutral and value-free, CBPR researchers have often drawn
from reexive and interpretative inquiry that explore the dialectic between researcher and what
is being researched (Denzin & Lincoln,2000) or from viewing knowledge as historically and
socially constructed (McTaggart et al.,2017).
CBPR critiques of positivism have been pointed, stating that traditional inquiry discounts
experiential knowledge, reinforces subjects’ passivity, and obscures other voices (Gaventa &
Cornwall,2015). Not only is positivism, “not the only method for gaining valid knowledge, but
it is a powerful ideology that thwarts the eld’s interests in alleviating suffering and promoting
social justice” (Buchanan,1998, p. 440). Indigenous researchers have posed this difference as
knowledge for the sake of knowing (i.e., for categorizing objective reality) versus knowledge
for decolonizing, healing, and mobilizing (Atalay,2012; Tuhiwai Smith,2012). Dutta (2008)
proposes a culture-centered approach (CCA) for health research, challenging ways that
dominant-culture communication (re)produces marginalization of disenfranchised populations
and promoting community agency and knowledge for transforming inequitable conditions.
CCA is increasingly being adopted within CBPR as a mechanism for knowledge democracy
(Wallerstein et al., under review).
Fundamental to knowledge democracy is understanding that knowledge within universities,
as published evidence-based science, for example, is a partial percentage of knowledge across
the globe. The earliest universities created exclusionary walls and were part of sociopolitical
processes that enabled the canonization of academic disciplines and what the Portuguese soci-
ologist Boavenura has called epistemicide, or the killing of community knowledge systems (de
Sousa Santos,2007; Hall & Tandon,2017).
Knowledge democracy practices, however, are embedded within CBPR and other partic-
ipatory research approaches. Inherent to knowledge democracy is the recognition of multiple
ways of knowing, especially from marginalized, excluded populations, of multiple expressions
Theoretical, Historical, and Practice Roots of CBPR 23
of knowing, such as narrative, songs, theater; of using knowledge as a tool for social action
and democracy; and, nally, as shared through open-access venues. Knowledge democracy
requires unpacking of universalist premises by identifying those processes of discrimination
or racism (Chapter4; Singh,2016) that have prevented people’s experiences from being seen
as valid. Most important for CBPR practitioners, it involves our own reections, as ongoing
reexive practice, about our positionalities of power, our own questions of how to best co-
construct knowledge, and our own challenges in applying research knowledge for social and
health equity.
POWER RELATIONS
Although knowledge is a major source of power and control, other structural power relations are
also central. CBPR takes place not only in the context of personal and historical relationships
among researchers, their universities, and communities but also in the broader societal context
of power relations in which the research takes place, the origins of the research, and the purpose
of the research itself. Gaventa and Cornwall (2015) identify four dimensions of power in CBPR,
analyzing how power is exercised and who is excluded. The pluralist liberal view assumes that
power is a product of an open system of equal competing agendas, with lack of participation,
possibly in expressing views within a partnership, seen as a function of choice. The second view
argues that there is a hidden face to power in which some actors and issues are kept from open
discussion through a mobilization of bias by powerful social norms or organizations. CBPR
researchers may unwittingly play into this bias in calling, for example, for evidence-based inter-
ventions (Green,2006). The third, and more insidious, dimension of power is one that excludes
grievances by preventing conicts or community ideas from even surfacing. Internalized racism
(see Chapter4), for example, may contribute to a culture of community members not feeling
their voices are as valued as when academics speak.
To Foucault (1980), these three dimensions represent repressive forms of power, exercised
through direct control, microaggressions, or indirect language that shapes people’s opportu-
nities to participate fully. Emancipatory CBPR uncovers these mechanisms of control, biases,
and internalized representations of reality as key strategies for change. Foucault articulates a
fourth perspective of power as productive. Rather than seeing repressive monolithic power, he
conceptualizes power as a web of discourses and practices found in institutions, communities,
and families. These power relationships are inherently unstable and therefore open to challenge.
To Foucault, knowledge symbolizes power. Repressive power, for example, can be used
in overly technical research language that may inhibit community response. As productive
power, however, research knowledge can enable communities to challenge existing limits and
advocate for change. As Deveaux (1999) has noted, “Where there is power, there is resis-
tance” (p. 242).
In CBPR, relationships between researchers and communities require commitment and
trust, which may ebb and ow over time depending on contexts, events, and power relations (see
Chapter5). When researchers walk into a community, they bring histories of the research insti-
tution and other researchers with them. Scott (1990) has outlined the importance of recognizing
the dynamic nature of public and hidden discourse. Public transcripts contain information in
ofcial language and are often what is brought to the table initially. Yet hidden transcripts,
24 Community-Based Participatory Research for Health
what community members fully think, may remain outside the knowledge given to the outside
research team. With trust, some hidden transcripts may become public over time. Academics,
however, may never have full access to phenomena being studied, such as spiritual ceremonies,
though openness to mutual learning and community knowledge can enrich all of our under-
standings of the world.
A key strategy for mutual learning is the practice of cultural humility (Appendix 4), in
which all partners are reexive about their positions of power, whether by race-ethnicity, edu-
cation, or community status, and are willing to negotiate these dynamics. Diane Wolf (1996)
has argued that research power can be challenged in three specic arenas: (1) the positional-
ity between researcher and researched, (2) decision making during the research, and (3) voice
and representation in writing and publishing. In Foucault’s framework, positions of power can
reverse, and initial power of researchers may give way to community knowledge and gatekeeper
functions, with new reciprocity of shared power or community-driven leadership.
In CBPR, there is never a perfect equilibrium of power. All research efforts undergo cycles
of participation and questioning by community members, bringing greater or lesser partici-
pation and ownership. This dialectic of collaboration and skepticism between academic and
community partners is probably a healthy tension for all to acknowledge and work with, even as
relationships strengthen and grow.
FEMINISM, POST-STRUCTURALISM, AND POSTCOLONIALISM
Feminist participatory researchers add critical dimensions to our understanding of the theory
and practice of CBPR. In early critiques, feminist writing challenged the exclusion of women
through the use of universal language of “the oppressed” and the lack of attention to gender dif-
ferences in data collection and analysis (Maguire,2006). Over the past fty years, feminism has
shifted from studying women as a universal construct to understanding gender culturally and
historically, with shifting and intersectional identities of class, race and ethnicity, sexual orien-
tation, and other differences (Collins,2000; Maguire,2006; Reid & Frisby,2008). Arguing for a
transnational feminist praxis of understanding one’s historical and political locations, Swarr and
Nagar (2010) propose that dialogical collaboration in knowledge production (as opposed to the
individual scholar) offers transformational opportunities to rethink and reclaim feminist issues
of voice, subalternity, and representation in scholarship and in social activism.
Post-structuralism focuses on the ways that language and narratives construct reality and
our view of social institutions, such as academia, public health, or medicine, and how these
constructions are resisted by communities. Postcolonialism takes this further by using race or
ethnicity as a primary lens through which to understand European colonization of other peoples
and lands (Said,1994). To counter the dominant portrayals of the other, CBPR research within a
postcolonial tradition seeks to honor and integrate into interventions the cultural and community
narratives of people’s lives (Duran & Duran,1995; Whitesell, Stanley & Allen, 2018).
The role of the outside researcher in this context may therefore be largely to weaken the
power of dominant culture explanations and create spaces for competing community ideas
and practices to emerge, furthering goals of knowledge democracy. African American women,
for example, in public spaces may conform to societal roles, yet in church or family contexts,
adopt more powerful roles (Collins,2000). In complex ways, they are not accepting stories of
Theoretical, Historical, and Practice Roots of CBPR 25
themselves as the other, but creating new stories based on their productive power as strong sis-
ters, mothers, or advocates.
In CBPR, feminist, post-structuralist, and postcolonialist theory share certain methods and
goals: analyzing personal lives in relation to the structures (overt and hidden) that might control
people’s lives; celebrating strengths and agency, not just victimization; working for goals of social
justice; and undermining the notion of the objectivity of science by taking into account political,
sociocultural contexts and knowledge of people living within those contexts. These literatures have
challenged the right of researchers to overstate their interpretations and thereby unintentionally
silence the community. Although data analysis is often seen as an academic exercise (with special-
ized skills needed), community participation in analytic discussions and interpretation of the data
can be one of the most important for translation of ndings into applied use (Cashman et al.,2008).
In a now-classic paper, Fine (1994) articulated three researcher stances in relation to
community: (1) ventriloquy, when researchers describe the other as objective truth, never using
the word I nor connecting themselves to their analysis; (2) voices, when researchers speak for
the other, presenting quotes without a critical analysis of context or history of people’s expe-
rience; and (3) activist feminist research, when researchers negotiate, are explicit about their
identity, and create community dialogue for a context-based interpretation of knowledge. Fine
and Sirin (2007) took this third stance further with a participatory action research project under-
taken with a Muslim American youth advisory board to investigate hyphenated identities in a
post-9-11 politically contentious and fear-generating world. They were able to explore public
and hidden discourses, focusing on the Freirian praxis of resistance from these young people
“working the hyphen” as they spoke out about their lives.
PAULO FREIRE AND PRAXIS
Brazilian educator Paulo Freire has been a major source of inspiration within the Southern
emancipatory participatory research tradition. Freire’s popular or empowerment educational
approach is one of collective dialogue to facilitate conscientização (Portuguese for critical con-
sciousness in becoming a social change agent) and praxis, or the continuous cycle of action-
reection-action to improve community conditions (1970, 1982).
To promote learners as the subjects of their own liberation, Freire proposes a listening-
dialogue-action-reection approach (Wallerstein & Auerbach,2004). The rst step is listening
to problems and themes identied by community members as shared issues providing motiva-
tion to act. The next step is creating opportunities for dialogue to generate collective analyses
of these issues within their sociocultural or political context and then identifying strategies for
collective actions. Reection, or evaluating the impact of the actions, leads back to the next
cycle of listening, further dialogue, and actions.
Much of the creativity of the Freirian approach lies in the development of codes, or trig-
gers, about the issues or themes, such as pictures, videos, role-plays—any form that helps par-
ticipants “see” their reality with new eyes and develop alternative ways of thinking and acting.
For research, these could include identifying issues through photo-documentary and photo-
voice (see Chapters13 and23), characterizing conditions through Augusto Boal’s theater of the
oppressed, creating digital stories to make research accessible for community action, and other
forms of participatory practices for transformation (Ledwith & Springett,2012).
26 Community-Based Participatory Research for Health
Freire’s writings reinforce a deep belief in humanity and people’s role in making change
and as such have critical importance to CBPR:
To be a good [participatory researcher] means above all to have faith in people; to believe in
the possibility that they can create and change things...Liberation begins to the extent that
men [and women] reect on themselves and their condition in the world—the world in which
and with which they nd themselves. To the extent that they are more conscientized, they insert
themselves as subjects into their own history. (adapted from Freire,1971, p. 61)
In a dialogue book with Ira Shor, Freire discusses the risks and fears of transformation,
which for researchers could mean letting go of control, acknowledging that resistance may be
real, “if you don’t risk, you don’t create anything. Without risking, for me, there is no possibility
to exist” (Shor & Freire,1987, p. 61). McTaggart and colleagues (2017) call for transcending
single-dimension research for a complex research practice that draws on critical theory, applied
problem-solving, and reexive-dialectical practice, all of which promote our understand-
ings of personal and collective agency under specic local and global historical conditions.
Freirian methodologies can be helpful in pointing researchers and communities to the dialogical
processes that facilitate these complex understandings and support personal transformations so
that partners, as individuals and within the partnership, can see their roles in applying research
for change.
CONCLUSION
Issues of participation, power, knowledge democracy, and praxis are not abstract phenomena
but rather authentic tensions that are enacted in academia and in community settings. If we, as
partners, are not honest and reexive about our own power bases, there is little hope that we
will be able to transform power dynamics. We need to understand how our personal biogra-
phies inform our ability to interpret the world in understanding the problems and in visioning
community strengths.
A major challenge for those of us in the CBPR eld lies in the potential limits of CBPR,
given the realities of globalization, the imposition of Western cultural and economic struc-
tures on the rest of the world, and the difculties for local communities in making meaningful
change. Scaling up has become a buzzword in world institutions seeking to bring lessons from
small communities to nation-states (Gaventa & Cornwall,2015). Can CBPR be scaled up when
so much depends on relationship building and commitment to collaborative work over time?
Can realities be transformed at the local level in order to enhance health and contribute to a
more equitable society? Although these questions are important, we must ensure that critiques
and challenges of CBPR do not play into conservative strategies that dismiss the role of com-
munities participating in change (or that, conversely, leave the work of change to local commu-
nities without adequate external or public sector support).
Ultimately, CBPR is about knowledge democracy, recognizing the interconnections bet-
ween the personal and the social, life worlds and system worlds, and the barriers and facilitators
of human actions that move toward research for social change. This can be a daunting and con-
tradictory task but one full of promise and hope as academics and communities engage together
to promote more just societies.
Theoretical, Historical, and Practice Roots of CBPR 27
QUESTIONS FOR DISCUSSION
1. What are the contributions of different participatory research traditions (for example, fem-
inist participatory research, Lewinian action research, Freire, etc.) to CBPR?
2. For self-reection, what is your particular theoretical approach to CBPR, or what are the
components from which you draw?
3. How are tensions embedded in the concepts of participation, knowledge democracy,
power, and Freirian praxis expressed in your current work? In future work you hope to do?
NOTE
1. The Global South includes Africa, Latin America, and developing Asia, including the Middle East;
countries formally referred to as third world, developing, or low resource. The Global North includes
the United States, Canada, Western Europe, and developed parts of Asia, as well as Australia and
New Zealand: highly industrialized and “democratic” countries.
REFERENCES
Anderson, K., & Olson, S. (2013). Leveraging culture to address health inequalities: Examples from Native communities;
Workshop summary. Washington, DC: Roundtable on Promotion of Health Equity and the Elimination of Health Dispar-
ities, Institute of Medicine, National Academies Press.
Argyris, C., & Schön, D. A. (1996). Organizational learning II. Reading, MA: Addison-Wesley.
Atalay, S. (2012). Community-based archeology: Research, with, by, and for Indigenous and local communities. Berkeley,
CA: UC Press.
Bahl, I. (1961). I couldn’t have gotten along without Sam. Nursing Outlook, 9(6), 352–356.
Bargal, D. (2008). Action research: A paradigm for achieving social change. Small Group Research, 39(1), 17–27.
Bradbury, H. (Ed.). (2015). The Sage handbook of action research (3rd ed.). Thousand Oaks, CA: Sage.
Buchanan, D. (1998). Beyond positivism: Humanistic perspectives on theory and research in health education. Health
Education Research, 13, 439–450.
Canadian Institutes of Health Research. (2007–2010). CIHR guidelines for health research involving aboriginal people.
Retrieved February 2017 from www.cihr-irsc.gc.ca/e/29134.html
Cashman, S., Adeky, S., Allen, A., Corburn, J., Eng, E., Israel, B., Montaño, J., Rafelito, A., Rhodes, S. D., Swanston, S., &
Wallerstein, N. (2008). The power...the promise: Working with communities to analyze and interpret data and get to
outcomes. American Journal of Public Health, 98, 1407–1418.
Coburn, C. E., & Penuel, W. R. (2016). Research–practice partnerships in education: Outcomes, dynamics, and open ques-
tions. Educational Researcher, 45(1), 48–54.
Collins, P. H. (2000). Black feminist thought: Knowledge, consciousness, and the politics of empowerment (2nd ed.). New
York, NY: Routledge.
Cooke, B., & Kothari, U. (Eds.). (2001). Participation: The new tyranny? London, UK: Zed Books.
Cornwall, A., & Jewkes, R. (1995). What is participatory research? Social Science & Medicine, 41, 1667–1676.
Denzin, N. K., & Lincoln, Y. S. (Eds.). (2000). Handbook of qualitative research (2nd ed.). Thousand Oaks, CA: Sage.
de Sousa Santos, B. (2007). Beyond abyssal thinking: From global lines to ecologies of knowledge. Eurozine, 33, 45–89.
de Sousa Santos, B. (2013). Epistemologies of the south: Justice against epistemicide. Boulder, CO: Paradigm Publishers.
Deveaux, M. (1999). Feminism and empowerment. In S. Hesse-Biber, C. Gilmartin, & R. Lydenberg (Eds.), Feminist
approaches to theory and methodology (pp. 236–256). New York, NY: Oxford University Press.
Duran, E., & Duran, B. (1995). Native American postcolonial psychology. Albany, NY: State University of New York Press.
28 Community-Based Participatory Research for Health
Dussel, E. (2013). Ethics of liberation: In the age of globalization and exclusion. Durham, NC: Duke University Press.
Dutta, M. J. (2008). Communicating health: A culture-centered approach. Malden, MA: Polity Press.
Fals-Borda, O., (1998). People’s participation: Challenges ahead. New York. Apex Press.
Fals-Borda, O. (2006). Participatory (action) research in social theory: Origins and challenges. In P. Reason & H. Bradbury
(Eds.), Handbook of action research: Participative inquiry and practice (Concise ed., pp. 27–37). Thousand Oaks, CA: Sage.
Fals-Borda, O., & Rahman, M. A. (Eds.). (1991). Action and knowledge: Breaking the monopoly with participatory action
research. New York, NY: Apex Press.
Fine, M. (1994). Working the hyphens. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research (pp. 70–82).
Thousand Oaks, CA: Sage.
Fine, M., & Sirin, S., (2007). Theorizing hyphenated selves: Researching youth development in and across contentious
political contexts. Social and Personality Psychology Compass, 1(1),16–38.
Foucault, M. (1980). Power/knowledge: Selected interviews and other writings, 1972–1977 (C. Gordon, Ed.). New York, NY:
Pantheon Books.
Freire, P. (1970). Pedagogy of the oppressed. New York, NY: Seabury Press.
Freire, P. (1971). To the coordinator of the culture circle. Convergence, 4(1), 61–62.
Freire, P. (1982). Creating alternative research methods: Learning to do it by doing it. In B. L. Hall, A. Gillette, & R. Tandon
(Eds.), Creating knowledge: A monopoly? Participatory research in development (pp. 29–37). New Delhi, India: Society
for Participatory Research in Asia.
Gaventa, J., & Cornwall, A. (2015). Power and knowledge. In H. Bradbury (Ed.), The Sage handbook of action research: Par-
ticipative inquiry and practice (3rd ed.). Thousand Oaks, CA: Sage.
Glassman, M., Erdem, G., & Bartholomew, M. (2013). Action research and its history as an adult education movement for
social change. Adult Education Quarterly, 63, 272–288.
Green, L. W. (2006). Public health asks of systems science: To advance our evidence-based practice, can you help us get more
practice-based evidence? American Journal of Public Health, 96, 406–409.
Habermas, J. (Ed.). (1987). Lifeworld and system: A critique of functionalist reason. Boston, MA: Beacon Press.
Hall, B., Tandon, R., & Tremblay, C. (2015). Strengthening community university research partnerships: Global perspectives.
Victoria, Canada: University of Victoria and PRIA.
Hall, B. L., Jackson, E. T., Tandon, R., Fontan, J., & Lall, N. (2013). Knowledge, democracy and action: Community-
university research partnerships in global perspectives. Manchester, UK: Manchester University Press.
Hall, B. L., & Tandon, R. (2017). Decolonization of knowledge, epistemicide, participatory research and higher education.
Research for All, 1(1), 6–19.
Horton, M., & Freire, P. (1990). We make the road by walking: Conversations on education and social change. Edited by
B. Bell, J. Gaventa, & J. Peters. Philadelphia, PA: Temple University Press.
ISSC/IDS. (2016). Challenging inequalities: Pathways to a just world: World Social Science Report 2016. Paris, France:
UNESCO Publishing. Retrieved February 25, 2017, from http://en.unesco.org/wssr2016
Jewkes, R., & Murcott, A. (1998). Community representatives: Representing the “community”? Social Science & Medicine,
46, 843–858.
Kemmis, S., Wilkinson, J., Edwards-Groves, C., Hardy, I., Grootenboer, P., & Bristol, L. (2013). Changing practices, chang-
ing education. London, UK: Springer.
Ledwith, M., & Springett, J. (2012). Participatory practice: Community-based action for transformative change. Bristol, UK:
Policy Press.
Lewin, K., & Gold, M. (1999). The complete social scientist: A Kurt Lewin reader. Washington, DC: American Psychological
Association.
Maguire, P. (2006). Uneven ground: Feminisms and action research. In P. Reason & H. Bradbury (Eds.), Handbook of action
research: Participative inquiry and practice (Concise ed., pp. 60–70). Thousand Oaks, CA: Sage.
McTaggart, R., Nixon, R., & Kemmis, S. (2017). Critical participatory action research. In L. Rowell, C. Bruce, J. Shosh, & M.
Riel (Eds.), Palgrave international handbook of action research (pp. 21–36). New York, NY: Springer Nature.
Muhammad, M., Wallerstein, N., Sussman, A. L., Avila, M., Belone, L., & Duran, B. (2015). Reections on researcher iden-
tity and power: The impact of positionality on community-based participatory research (CBPR) processes and outcomes.
Critical Sociology, 41, 1045–1063.
Theoretical, Historical, and Practice Roots of CBPR 29
Oetzel, J. G., Villegas, M., Zenone, H., White Hat, E. R., Wallerstein, N., & Duran, B. (2015). Enhancing stewardship of
community-engaged research through governance. American Journal Public Health, 105, 1161–1167.
Oswald, K., Gaventa, J., & Leach, M. (2017). Introduction: Interrogating engaged excellence in research. IDS Bulletin, 47(6).
Retrieved from http://bulletin.ids.ac.uk/idsbo/article/view/2827
Reid, C., & Frisby, W. (2008). Continuing the journey: Articulating dimensions of feminist participatory research. In P.
Reason & H. Bradbury (Eds.), The Sage handbook of action research: Participative inquiry and practice (2nd ed., pp.
93–105). Thousand Oaks, CA: Sage.
Rifkin, S. (1996). Paradigms lost: Toward a new understanding of community participation in health programmes. Acta
Tropica, 61, 79–92.
Rowan, J. (2006). The humanistic approach to action research. In P. Reason & H. Bradbury (Eds.), Handbook of action
research: Participative inquiry and practice (concise ed., pp. 106–116). Thousand Oaks, CA: Sage.
Said, E. (1994). Culture and imperialism. New York, NY: Vintage Books.
Scott, J. (1990). Domination and the arts of resistance: Hidden transcripts. New Haven, CT: Yale University Press.
Shor, I., & Freire, P. (1987). A pedagogy for liberation: Dialogues on transforming education. Westport, CT: Bergin & Garvey.
Singh, J. (2016). Cultivating an anti-racist position in post-race society. In People’s Knowledge Editorial Collective (Eds.),
People’s knowledge and participatory action research: Escaping the white-walled labyrinth (pp. 45–52). Warwickshire,
UK: Practical Action Publishing.
Swarr, A., & Nagar, R. (2010). Critical transnational feminist praxis. Albany, NY: State University of New York Press.
Tandon, R. (1988). Social transformation and participatory research. Convergence, 21(2), 5–18.
Trickett, E. J., & Espino, S.L.R. (2004). Collaboration and social inquiry: Multiple meanings of a construct and its role in
creating useful and valid knowledge. American Journal of Community Psychology, 34(1–2), 1–69.
Tuhiwai Smith, L. (2012). Decolonizing methodologies: Research and Indigenous peoples (2nd ed.). New York, NY:
Zed Books.
Wallerstein, N. (1999). Power between evaluator and community: Research relationships within New Mexico’s healthier
communities. Social Science & Medicine, 49, 39–53.
Wallerstein, N., & Auerbach, E. (2004). Problem-posing at work: A popular educator’s guide. Edmonton, AB, Canada:
Grassroots Press.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal Public Health, 100(Suppl 1), S40–S46.
Wallerstein, N., Oetzel, J., Duran, B., Magarati, M., Pearson, C., Belone, L., Davis, J., Dewindt, L., Lucero, J., Ruddock, C.,
Sutter, E., Villegas, M., & Dutta., M. (under review). Conceptualizing and measuring the culture-centered approach in
community based participatory research. Social Science & Medicine.
Whitesell, N., Stanley, L., Allen, J. (2018). Prevention Science. Special Issue: Innovations in intervention research with indig-
enous populations in the U.S.
Whyte, W. (Ed.). (1991). Participatory action research. Thousand Oaks, CA: Sage.
Wolf, D. (Ed.). (1996). Feminist dilemmas in eldwork. Boulder, CO: Westview Press.
3
CHAPTER
CRITICAL ISSUES IN
DEVELOPING AND
FOLLOWING CBPR PRINCIPLES
BARBARA A. ISRAEL, AMY J. SCHULZ, EDITH A. PARKER,
ADAM B. BECKER, ALEX J. ALLEN, III, J. RICARDO GUZMAN,
AND RICHARD LICHTENSTEIN
RESEARCHERS HAVE SOUGHT to address the disproportionate and growing burden of mor-
bidity and mortality in recent decades in low social and economic resource communities and
in communities of color. Yet, the history of research abuse and frequent absence of benet to
the communities most affected have understandably made community members skeptical of
research. These challenges, as well as systematic exclusion of non-researchers from inuence
over the research process, have made it important for researchers to address fundamental ques-
tions such as, What is the purpose of research? Who benets from research? How are the results
of research used? How can research contribute to reducing health inequities? And what role
does research play in community change and knowledge generation?
Community-based participatory research (CBPR), with its growing inuence in addressing
health inequities (Braun et al.,2015; Israel, Eng, Schulz, & Parker,2013b; Jones & Wells,2007;
Minkler, Garcia, Rubin, & Wallerstein,2012), has embraced the importance of these questions.
A set of CBPR principles, rst proposed in 1998 (Israel, Schulz, Parker, & Becker,1998), has
offered guidelines to encourage researchers to think about their own assumptions in conducting
research with communities and to adopt an approach toward equitable community engagement.
32 Community-Based Participatory Research for Health
Recognizing that each setting and research partnership is unique, local issues need to be consid-
ered when adhering to or adapting CBPR principles for distinct contexts. This chapter presents
principles derived from the literature and the collective experiences of the authors and then uses
case examples from the Detroit Community-Academic Urban Research Center (Detroit URC)
and its afliated partnerships
1
to illustrate them. Throughout the chapter, we emphasize the
importance of exibility, reection, and critical analysis in applying and adapting these princi-
ples in different contexts.
CBPR DEFINITION AND KEY PRINCIPLES
The following ten principles capture key elements of CBPR as currently understood; the rst
nine of which were initially identied in 1998 by Israel and colleagues.
2
They are presented
with the recognition that they will continue to evolve as further work is conducted and eval-
uated and that the extent to which any research endeavor achieves any combination of these
principles will vary depending on the context, purpose, and participants involved. Most of the
principles are located on a continuum, with the principles as described here representing an
ideal goal toward which to strive. Finally, although each is presented here as a distinct principle,
ultimately CBPR is an integration of them all.
CBPR Recognizes Community as a Unit of Identity
The concept of community as an aspect of collective and individual identity is central to CBPR.
Units of identity—for example, membership in a family, friendship network, or geographical
neighborhood—are socially constructed, created, and re-created through social interactions
(Hatch et al., 1993; Steuart, 1993). Community is characterized by identication with and
emotional connection to other members, common symbol systems, shared values and norms,
mutual (although not necessarily equal) inuence, collective interests, and joint commitment
to meeting shared needs (Israel, Checkoway, Schulz, & Zimmerman, 1994). Communities
of identity may exist within dened geographical boundaries or be made up of members of
a dispersed group with acknowledged commonalities (e.g., shared racial, ethnic, gender, or
ability-related identities). Community-based participatory approaches to research attempt to
work with existing communities of identity and to strengthen a sense of community through
collective engagement (Israel et al.,1994). Communities of identity contain many individual
and organizational resources but may also benet from skills and resources available outside
of the community.
CBPR Builds on Strengths and Resources within the Community
CBPR seeks to identify and build on strengths, resources, and relationships that exist within
communities of identity to address members’ communal health concerns (Steuart,1993). These
may include individuals’ skills and assets; networks of relationships characterized by trust,
cooperation, and mutual commitment; and mediating structures such as churches and other
organizations where members come together. CBPR explicitly recognizes and seeks to support
or expand social structures and processes that contribute to the ability of community members
to work together to improve health.
Critical Issues in Developing and Following CBPR Principles 33
CBPR Facilitates Collaborative, Equitable Partnership in All Research Phases
and Involves an Empowering and Power-Sharing Process That Attends to
Social Inequalities
In CBPR all parties participate in and share control, as desired, over all phases of the research
process, including problem denition, data collection, interpretation of results, and application
of results to address community concerns (Israel et al.,1998; Stringer,2007). CBPR partner-
ships focus on issues identied by community members (Israel, Eng, Schulz, & Parker,2013a)
and create processes that enable equitable engagement in the research. Recognizing that mar-
ginalized communities often have limited power to name or dene their own experience and
that inequalities among community members shape participation and inuence in collective
research and action, researchers involved with CBPR acknowledge inequalities between them-
selves and community participants. Attempts to address these inequalities involve explicit
attention to the knowledge and expertise of community members and an emphasis on empower-
ing processes that include sharing information, decision-making power, resources, and support
among members of the partnership (Israel et al.,1994; Jones & Wells,2007; Wallerstein,2006).
CBPR Promotes Co-learning and Capacity Building among All Partners
CBPR is a co-learning process that facilitates the reciprocal transfer of knowledge, skills, and
capacity (Corbie-Smith et al.,2015). For example, researchers can learn from community mem-
bers’ management and leadership skills and understandings about the community and broader
social context, and community members can acquire further research skills. The emphasis here
is on enhancing the capacity of all partners, improving the effectiveness of the CBPR effort, and
increasing capacity that can be applied to members’ other endeavors.
CBPR Integrates and Achieves a Balance between Research and Action
for the Mutual Benefit of All Partners
CBPR seeks to build a broad body of knowledge about health while using the knowledge gen-
erated to support community and social change efforts that address concerns of the involved
community (Corbie-Smith et al., 2015). Information is gathered to inform action, and new
understandings emerge as participants reect on actions taken. CBPR incorporates a commit-
ment to the translation and integration of research results with community change efforts for the
benet of all partners.
CBPR Emphasizes Public Health Problems of Local Relevance and Ecological
Perspectives That Attend to the Multiple Determinants of Health and Disease
CBPR addresses public health problems of concern to the community and considers the con-
cept of health from a multidimensional perspective that emphasizes physical, mental, and social
well-being. It also emphasizes an ecological model of health (Sallis & Owen,2015) that con-
siders and encompasses the individual, his or her immediate contexts (e.g., family, social net-
work), and the larger social spheres or institutions in which they are embedded. Such approaches
recognize and attend to biomedical, social, economic, cultural, and physical environmental
factors as determinants of health and disease. Given these foci, CBPR efforts strive to achieve
broadscale social changes intended to eliminate health inequities.
34 Community-Based Participatory Research for Health
CBPR Involves Systems Development through a Cyclical and Iterative Process
CBPR involves systems development, so that a system (e.g., a partnership) develops the
competencies to engage in a cyclical, iterative process that includes multiple phases. These
include partnership development and maintenance; community assessment; problem denition,
development of research methodology; data collection and analysis; interpretation of data; deter-
mination of action and policy implications; dissemination of results; action taking (as appro-
priate); and establishment of mechanisms for sustainability (Israel et al.,1994; Stringer,2007).
CBPR Disseminates Findings and Knowledge Gained to All Partners
and Involves All Partners in the Dissemination Process
CBPR disseminates ndings and knowledge gained to all partners involved, in language that
is understandable and respectful, and “where ownership of knowledge is acknowledged”
(Bishop,1994, p. 186; see also Hall, Tandon, & Tremblay,2015). The ongoing feedback of
data and use of results to inform action are integral to this approach (Baker, Mutton, Barnidge,
& Rose,2013; Schulz et al.,2011). This principle also calls for opportunities for all partners
to engage in dissemination activities, for example, as coauthors or copresenters (Parker
et al.,2013).
CBPR Requires a Long-term Process and Commitment to Sustainability
Given the negative experiences many communities have with research and the time and effort
needed to rigorously follow the principles described here, CBPR requires a long-term process and
commitment to sustainability on the part of all partners (Hatch et al.,1993; Israel et al.,2013a;
Jones & Wells,2007). To establish and maintain the trust required to conduct CBPR successfully
and to accomplish the aim of reducing health inequities, this commitment must extend beyond
a single research project or funding period and include a willingness to continue the partnership
even without funding. Although there is no set time frame for the “long term,” the emphasis is
placed on development of relationships and commitments that extend beyond any one project.
Some goals, for example, reducing environmental risks in a local community, may take decades
to realize. Although a specic partnership may at some point decide not to continue, commitment
to the relationships among partners or their organizations and to continued collaboration and
support as needed and desired are critical characteristics of CBPR.
CBPR Addresses Issues of Race, Ethnicity, Racism, and Social Class
and Embraces “Cultural Humility”
CBPR partnerships frequently involve community partners from historically marginalized
groups and “outside” researchers and other institutional partners from more privileged back-
grounds (Minkler, Garcia, et al.,2012). CBPR partners must strive to achieve what Tervalon
and Murray-Garcia (1998) refer to as “cultural humility,” recognizing that no one can fully
master another’s culture (Israel et al.,2013a; Minkler, Garcia, et al.,2012) (see Appendix 4).
Cultural humility means a commitment to self-critique and self-reection, including examining
one’s own racism and classism, addressing power imbalances, and establishing and maintain-
ing authentic partnerships. One aspect of cultural humility in the research process is an under-
standing of the ways that questions of research validity may fail to reect validity and relevance
Critical Issues in Developing and Following CBPR Principles 35
to diverse engaged communities (i.e., external validity). Thus, in addition to recognizing the
need for traditional research validity, to develop sound and useful knowledge for policy and
social change, CBPR partnerships must also encompass critical reection regarding the ways
that racism, classism, sexism, and other isms operate to delegitimize community knowledge. A
commitment to cultural humility and to addressing these power imbalances can support part-
nerships’ efforts to develop a more complete and less biased understanding of social processes,
enhancing the “rigor, relevance, and reach” of the science produced in the process (Balazs &
Morello-Frosch,2013) (See also Appendix 1).
ISSUES IN DEVELOPING AND FOLLOWING CBPR PRINCIPLES
A number of critical issues can arise that need to be addressed when adopting or adapting
guidelines such as those previously described. Several examples are discussed in the follow-
ing sections.
No One Set of CBPR Principles Is Applicable to All Partnerships
Although our partnerships strongly support and work to apply the described CBPR princi-
ples, we recommend equally strongly that this particular set of principles not be adopted as
is and imposed on other partnerships. Although some core values underlying the principles
may be applicable in most situations, not all of the principles will be applicable in all settings
and communities. Other principles, with complementary values, have been published, for
example, for tribes (LaVeaux & Christopher,2009; Walters et al.,2009); health care partner-
ships (Jones & Wells,2007); HIV/AIDS partnerships in and with marginalized communities
(Udoh et al.,2013); or they are written as ethical guidelines (also see Chapters14–16 and
Appendices 2, 3, 8, and 9). In keeping with the CBPR approach, principles must be owned
by the partners involved and therefore need to be adapted to the local context of each part-
nership. The process of jointly developing principles provides an opportunity for dialogue
and sharing of perspectives that helps build trust and establish relationships among partners
(Udoh et al.,2013). (See Appendix 2 for development of LGBTQ+ principles and referral
to Latino border principles and Appendix 3 for a set of international participatory health
research principles.)
Developing our initial set of CBPR principles took nearly two years and involved
numerous negotiations and revisions before adoption by the original partners (Schulz,
Israel, Selig, & Bayer, 1998). Several years later, when the Detroit URC partnership was
established, these principles were distributed, discussed, and adapted over a much shorter
time frame. It took the partnership longer to internalize and own the principles through expe-
riences gained over time. As particular decision points were faced, partners’ interpretations
of the meaning of some principles deepened. A set of CBPR principles therefore needs to
develop and change within the dynamics of a specic partnership, ultimately viewed as a uid
and evolving process.
Each CBPR Partnership Must Define Its “Community”
CBPR principles will vary across partnerships, in part depending on how the “community” is
dened and who represents that community. Recognizing that no single denition is applicable
36 Community-Based Participatory Research for Health
in all situations, an emerging CBPR partnership needs to discuss critical questions such as the
following:
■ Who is or represents the community?
■ Who has inuence, and how, if at all, are they involved?
■ Who decides who the community partners will be in a CBPR effort?
■ Are the community partners involved as individuals or as representatives of community-
based organizations (CBOs)?
■ If as individuals, do community members have a constituency that they represent and to
whom are they accountable?
■ If as a CBO, what is the connection or link between the CBO and the residents of the
community in which it works?
■ How do the participants involved in the partnership compare to members of the community
in terms of income, education, gender, race or ethnicity, and other identities?
■ Who has the time, resources, skills, and exibility to serve on committees, attend meetings,
or review documents as necessary?
The Detroit URC and afliated partnerships initially involved two geographically bounded
communities of identity: predominantly African American East Side Detroit and southwest
Detroit, with Detroit’s largest percentage of Latinos. During the formation phase, academic and
health department partners who established the Detroit URC invited community partners as orga-
nizational representatives from CBOs highly respected by the community (Israel et al.,2001). To
the extent possible, individuals who held or were appointed by those who held leadership posi-
tions within a CBO were selected to serve on the Detroit URC board (Israel et al.,2001).
Members of the board, even those who reside within the community, can be somewhat
different from community members at large, often in education and income. But such differ-
ences do not mean that they are not community members, and partners from academia and
health agencies need to be careful not to impose a denition of what it means to be “from the
community.” Indeed, in marginalized communities, it is often those with more formal educa-
tion and income who are best situated to participate in CBPR but at the same time having an
inside view of life in the community (Steuart, 1993). Critical reections by individuals and
the collective are central to these conversations about who represents the community and the
accountability of the partnership to the community.
All Partners Must Decide What It Means to Have a “Collaborative, Equitable
Partnership” and How to Make That Happen
Perhaps one of the most critical principles of CBPR is the emphasis on shared control in
decision making. As an ideal to strive for, this is a core value of CBPR, but how is equity and
shared inuence and control ensured? Every partnership needs to ask itself whether members
are partners or just part of the partnership—in other words, are all partners ready and able to
share power? This requires considerable time and attention to the partnership process from all
involved, which may be frustrating for some, particularly if it is perceived to draw time and
energy away from accomplishing specic objectives (Israel, Lantz, et al.,2013).
The Detroit URC has engaged in a number of strategies to dene and try to achieve a collab-
orative, equitable partnership (Israel et al.,2001). In one group exercise, each member identied
Critical Issues in Developing and Following CBPR Principles 37
the characteristics of effective groups that they had belonged to and then used them to create
operating norms for working together (e.g., mutual respect, everyone’s opinion is valued, agree to
disagree) (Israel et al.,2001). These norms were distributed at a board meeting, used as key indi-
cators in the partnership evaluation, and reviewed and revised as deemed necessary by the board.
Another procedure is the board’s use of consensus rather than majority rule in decision mak-
ing. Although substantial evidence shows that consensus results in improved decisions on com-
plex issues and enhanced commitment to the decision, it can take considerable time and may
hamper some decision making (Johnson & Johnson,2014). The Detroit URC board employs a
slight variation, referred to as the 70 percent rule, which requires that each partner be at least 70
percent in favor of a given decision. This approach has enabled board members to thoroughly
examine issues and consider multiple perspectives prior to making a decision, giving everyone
the opportunity to express opinions, inuence the decisions made, and develop support for
decisions reached without the expectation that everyone will be in complete agreement on all
decisions (Becker, Israel, & Allen,2013; Israel et al.,2001).
The Detroit URC also works toward equitable distribution of resources for involved part-
ners, including direct and indirect costs associated with grants (Lantz et al.,2001). Recent evi-
dence shows that sharing resources is associated with improved partnership outcomes (Oetzel
et al., 2015). Although core Detroit URC funding and some afliated partnership’s project
funds go primarily to the university involved, several arrangements contribute to more equi-
table distribution. These include (1) board and steering committee review of core funding and
inuence in budget-related decisions, (2) CBOs serving as duciary and lead organizations on
some grants, (3) CBOs subcontracting for specic work, and (4) CBOs always receiving modest
compensation. The distribution of resources has the potential to create conicts in a partnership
and requires ongoing consideration (Jones & Wells,2007). Not all partner organizations may
have an interest in or capability for managing large-scale projects, and this may be an area in
which to focus capacity-building efforts. In addition, other ways to distribute the benets and
rewards of participating in CBPR projects need to be explored by a partnership (for example,
attendance and presentations at professional meetings) (Brakeeld Caldwell et al.,2015).
Although, for the most part, the Detroit URC and afliated partnerships have used a highly
participatory, informal, and somewhat uid approach to achieve equity, there has also been
attention to more formal, structural approaches, such as establishing memoranda of understanding
(MOUs) and developing partnership bylaws (Oetzel et al.,2015; Yonas et al.,2013). Although
these may be helpful for partnership success, in other situations, the very formality of such struc-
tures may negatively affect trust and power sharing. Here again, partnerships should discuss and
select strategies that are most appropriate based on their history, norms, and preferences.
Although shared inuence and equity are goals of CBPR, some inequities among partners
are difcult to erase, especially when they involve race, gender, and class. Acknowledging and
discussing these inequities may reduce the impact they may have on the relationships and the
work of the partnership (Udoh et al.,2013).
Not Everyone Will Be Involved in the Same Way in All Activities
Another core value of CBPR is that all partners participate in all phases of the research process.
Here again, CBPR partnerships need to determine what that means for them, realizing that not
everyone may be involved in the same way in all activities. For example, in the East Side Village
38 Community-Based Participatory Research for Health
Health Worker Partnership and the Healthy Environments Partnership (Detroit URC–afliated
partnerships), the steering committees played major roles in developing a conceptual frame-
work, designing a survey, interpreting results, and applying them to implement intervention
strategies (Schulz et al.,2011,2015). By their own choice, the steering committees were not
involved in survey data entry or statistical analysis. Given time demands and technical aspects,
different levels of involvement may be appropriate for different partners, and partners are also
given opportunities to enhance their skills, as desired. Finally, and regardless of decisions made
about data entry and analysis, it is crucial that results be fed back to partners in ways that
are understandable and useful and that all partners engage in the interpretation process, which
might include requesting additional statistical analyses.
Establish Procedures for Dissemination
Questions related to the dissemination of ndings include the following:
■ Who will be the coauthors of publications and copresenters at professional meetings?
■ How are these decisions made?
■ What are their roles and responsibilities?
■ What happens when only one partner is invited to present or submit an article?
■ How is a balance reached between providing feedback to the community and writing
publications?
Here again, there is no one answer to these questions that will work for all partnerships.
Rather, a partnership needs to develop procedures to ensure that the dissemination principle
is followed.
The Detroit URC–afliated Community Action Against Asthma (CAAA) steering
committee established a dissemination subcommittee, made up of an equal number of uni-
versity and community partners, which met over several months to draft dissemination pro-
cedures (also see Appendix 9). These procedures, subsequently modied by the full steering
committee, spell out selection processes and roles for coauthors and copresenters (Parker
etal.,2013). Although we recommend that written dissemination procedures be established,
exibility is important in order to accommodate requests that may not t within the specied
parameters.
Recognize and Value Priorities Identified by the Community
Although CBPR emphasizes the importance of addressing social determinants of health at mul-
tiple levels of practice, researchers need to be careful not to impose that approach on the part-
nership. Understandably, community partners may initially be interested in addressing issues
that seem more amenable to change than trying to address policies associated with social deter-
minants of health. Indeed, community-organizing literature indicates that effective organizing
is built on winning tangible, small-scale changes in a relatively short period of time (Minkler &
Wallerstein,2012). As noted by Minkler, Pies, and Hyde (2012), one of the key ethical precepts
of community organizing and, we would add, of CBPR partnerships, is self-determination. A
CBPR effort may begin by addressing priority issues identied by the community, evolve over
time as partners engage in dialogue about the impact of social determinants on their priority
issues, and eventually develop strategies to affect those determinants.
Critical Issues in Developing and Following CBPR Principles 39
The East Side Village Health Worker Partnership used a stress process model as a conceptual
framework for addressing the social determinants of health on Detroit’s East Side (Parker,
Schulz, Israel, & Hollis,1998). Although the general model was included in the proposal written
by members of the researcher team, a more specic, locally dened stress process model was
developed by the steering committee (Parker et al.,1998). Based on this model and subsequent
in-depth interviews and surveys with community members, village health workers prioritized the
issues they wanted to address, such as enhancing relationships with the police, safety for children,
and fostering environments that support diabetes management and prevention. Although each of
these issues has underlying social determinants, the partnership’s initial strategies emphasized
short-term activities (Halloween parties for children or participating in a “Police Week”). These
successful events led to an increased sense of community, and through ongoing conversations,
some participants also began to engage in broader-scale policy and social changes.
Work with the Cultural Diversity of the Partners Involved
CBPR partnerships are likely to involve partners who differ in ethnicity and race, gender, social
class, sexual orientation, ability-disability, community or academic role, academic discipline,
and more. The multiple perspectives represented require development of a common language,
trust, and mutual respect; understanding of the various cultures; and recognition that different
participants may have different goals, agendas, and degrees of commitment to CBPR. Partici-
pants will also contend with conicting loyalties and multiple demands on their time and will
vary in what they can contribute to the CBPR effort. As noted, each CBPR partnership also has
to consider how structural inequities contribute to the cultural differences that exist within it.
The Community Action Against Asthma project was the rst Detroit URC–afliated project
to involve participants from East Side and southwest Detroit as well as researchers from envi-
ronmental health and behavioral sciences. Initially, some researchers who had less experience
with CBPR were perceived by community partners as being somewhat aloof and interested only
in their research ndings and not in the community members themselves. In addition, some
Latino community partners interpreted some comments from African American partners as dis-
criminatory toward Latinos. Undoing Racism training, small-group meetings, conict resolu-
tion, and other strategies may be effective means of ensuring that partner diversity is respected
and celebrated (Becker et al.,2013; Yonas et al.,2006,2013; also see Chapters4 and8).
Differences also occur across research disciplines. On several occasions, for example,
environmental and social scientists in CAAA have used the same words with different mean-
ings. The term qualitative data, for example, was used by environmental scientists to mean any
data not calibrated by a machine; thus, the results of a closed-ended survey were considered
qualitative. In the social sciences, however, qualitative data involves open-ended data collec-
tion approaches. The recognition of these language differences has contributed some humor
to our conversations but also a commitment to ongoing work to develop mutually understand-
able language.
Partnership Size Must Be Decided by and Appropriate for the Community
A frequently asked question is, What is the most appropriate or effective number of part-
ners to include in a CBPR effort? No rm answer can be found in the literature; rather, the
specic context and goals have to be considered, and the initial partners involved have to
40 Community-Based Participatory Research for Health
decide what is most appropriate in their particular situation. Our own experience suggests
that a CBPR partnership start small, beginning with partner organizations from only one or
two communities of identity. Such an approach has the advantage of building on existing
relationships and the likelihood of identifying mutually agreed-on goals. It is further sup-
ported by evidence that the most effective size for problem-solving groups is eight to twelve
individuals (Johnson & Johnson,2014). If there are preestablished, long-standing relation-
ships in the community of identity, a partnership might be effective with a somewhat larger
initial number of partners. There also may be limits to skills and resources in smaller groups,
such that a slightly larger core group (ideally not more than twelve to sixteen partner orga-
nizations) may be needed.
In our own work, we often use a Venn diagram approach to participation. At the center of
a series of overlapping circles is a core group of project partners who make up the partnership
decision-making core. Specic work groups or action teams may consist of other individuals
or organizations invited to participate as members of an outer, nonoverlapping circle, along
with members of the core group. Another approach that we use could more closely be repre-
sented using a concentric circle diagram, in which the core partners in the CBPR effort are
represented in the center circle, and other organizations are invited to participate in a more
limited way (outer circle). For example, the Detroit URC board, which is the core gover-
nance body, has established a Community-Academic Research Network involving more than
one hundred academic researchers and fty CBOs (www.detroiturc.org/expertise-programs/
community-academic-research-network.html). In general we recommend that the core group
remain fairly small, recognizing that there are multiple approaches to expanding to include
others as needed. It is helpful to develop a set of criteria for new membership and for the
existing partners to discuss and agree on the needs of the partnership and the expectations
and responsibilities of new members. Spelling out criteria more formally (see, for example,
Detroit URC criteria for membership: www.detroiturc.org/resources/urc-cbpr-tools.html) can
be useful, while retaining exibility in implementation to retain the strength of a community-
driven participatory process.
Recognize That CBPR Principles Alone Do Not Dictate Research Design
Some confusion in the eld is manifested in the suggestion that CBPR, by denition, dictates
the types of research design and methods that are appropriate. CBPR is an approach to con-
ducting research, rather than a method, and no one design or method is appropriate for all
CBPR efforts (see Chapter1). Instead, each partnership must decide what works best for its
research question and community context. In our East Side Village Health Worker Partnership,
in addition to conducting in-depth group dialogues and interviews on the stress process, we
conducted a random sample survey with community residents to assess beliefs, opinions, and
experiences more broadly (Parker et al.,1998).
In addition, although we suggest that research designs that involve the use of a control
group that receives no direct benet from the research are neither appropriate nor ethical in
the context of CBPR, there are other viable designs. For example, the Healthy Environments
Partnership implemented a lagged study design in which half of the participants in any cohort
were randomly selected to receive the intervention and the lagged “control group” waited eight
weeks before they began the intervention, a fairly standard design (Schulz et al.,2015).
Critical Issues in Developing and Following CBPR Principles 41
Continually Evaluate How Well CBPR Principles Are Followed
To develop and maintain an effective CBPR partnership and to enhance participants’ under-
standing of the factors that contribute to this effectiveness, it is necessary to conduct an ongoing
evaluation of the extent to which, and in what ways, the CBPR principles are being imple-
mented (Israel et al.,2001; Israel, Lantz, et al.,2013). Increasingly, partnerships are seeking
methods and metrics to reect on their own development and to assess their effectiveness over
time (Israel et al.,2013; Oetzel et al.,2015) (see also Appendix 10).
Since its founding, the Detroit URC has conducted evaluations to assess board mem-
bers’ perceptions and experiences of the board’s activities, processes, and progress, including
accomplishments, adherence to CBPR principles, challenges, and facilitating factors (Israel
etal.,2001; Israel, Lantz, et al.,2013). An evaluation subcommittee of the board initially guided
this assessment, which included multiple data collection methods (e.g., in-depth interviews,
closed-ended survey questionnaires). Evaluation results have been fed back and discussed at
board meetings. This process has enhanced members’ understanding of the CBPR principles
adopted and contributed to modications in board processes to more effectively follow them
(Israel et al.,2001; Israel, Lantz, et al.,2013).
CONCLUSION
Researchers, practitioners, and community members committed to addressing social and
economic inequities in health status need more equitable approaches to research that involve
action and knowledge generation benecial to, and reective of, the communities involved.
CBPR is one approach that engages diverse partners in strategies aimed at obtaining multiple
perspectives in order to address community-identied concerns. Our CBPR principles may be
used as guidelines by those interested in this approach. We reiterate that no one set of existing
principles is appropriate for all communities and all situations. Similarly, there is not just one
approach to CBPR. As partnerships consider the issues raised here, each will develop its own
approach to inquiry and change, along with principles that are appropriate for its own partners
working together in their specic context. What is crucial is the long-term commitment to
reducing fundamental inequalities that exist throughout the systems in which we live and work.
QUESTIONS FOR DISCUSSION
1. In what ways do the principles discussed in this chapter add to our understanding of
CBPR’s theoretical base? How do they reect this theory?
2. The chapter authors state that “no one set of CBPR principles is applicable to all partner-
ships.” Think of a partnership you are familiar with or that you have read about. Are there
principles you might modify to better meet the needs of this partnership? Is there a new
principle you would propose?
3. The Detroit URC made a conscious decision to include as partners community-based orga-
nizations rather than less formal, grassroots groups or individuals. What might be a benet
or downside of this approach?
42 Community-Based Participatory Research for Health
NOTES
1. The Detroit Community-Academic Urban Research Center, established in 1995, fosters and
supports the development, implementation, and evaluation of interdisciplinary, collaborative,
community-based participatory research projects that aim to eliminate health inequities in Detroit
(www.detroiturc.org). The authors thank Katie Abdou and Julia Weinert for their valuable assistance
in the preparation of this manuscript.
2. This discussion includes excerpts and revised portions from a set of CBPR principles originally
presented by Israel et al. (1998, pp. 177–180), with permission from the publisher.
REFERENCES
Baker, E. A., Mutton, F., Barnidge, E., & Rose, F. (2013). Collaborative data collection, interpretation, and action planning
in a rural African American community: Men on the move. In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.),
Methods in community-based participatory research for health (2nd ed., pp. 435–462). San Francisco, CA: Jossey-Bass.
Balazs, C. L., & Morello-Frosch, R. (2013). The three R’s: How community-based participatory research strengthens the
rigor, relevance and reach of science. Environmental Justice, 6(1). doi:10.1089/env.2012.0017
Becker, A. B., Israel, B. A., & Allen, A. (2013). Strategies and techniques for effective group process in CBPR partnerships.
In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods in community-based participatory research for health
(2nd ed., pp. 69–96). San Francisco, CA: Jossey-Bass.
Bishop, R. (1994). Initiating empowering research? New Zealand Journal of Educational Studies, 29, 175–188.
Brakeeld Caldwell, W., Reyes, A. G., Rowe, Z., Weinert, J., & Israel, B. A. (2015). Community partner perspectives on
benets, challenges, facilitating factors, and lessons learned from community-based participatory research partnerships in
Detroit. Progress in Community Health Partnerships: Research, Education, and Action, 9(2), 299–311.
Braun, K. L., Stewart, S., Baquet, C., Berry-Bobovski, L., Blumenthal, D., Brandt, H. M., et al. (2015). The National Cancer
Institute’s community networks program initiative to reduce cancer health disparities: Outcomes and lessons learned.
Progress in Community Health Partnerships (Suppl. 9), 21–32.
Corbie-Smith, G., Bryant, A. R., Walker, D. J., Blumenthal, C., Council, B., Courtney, D., & Adimora, A. (2015). Building
capacity in community-based participatory research partnerships through a focus on process and multiculturalism.
Progress in Community Health Partnerships: Research, Education, and Action, 9(2), 261–273.
Hall, B., Tandon, R., & Tremblay, C. (Eds.). (2015). Strengthening community-university research partnerships: Global per-
spectives. Victoria, BC, Canada: University of Victoria.
Hatch, J., Moss, N., Saran, A., Presley-Cantrell, L., & Mallory, C. (1993). Community research: Partnership in Black commu-
nities. American Journal of Preventive Medicine, 9(6), 27–31.
Israel, B. A., Checkoway, B., Schulz, A. J., & Zimmerman, M. A. (1994). Health education and community empowerment:
Conceptualizing and measuring perceptions of individual, organizational, and community control. Health Education
Quarterly, 21, 149–170.
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (2013a). Introduction. In B. A. Israel, E. Eng, A. J. Schulz, & E.
Parker (Eds.), Methods for community-based participatory research for health (2nd ed., pp. 3–37). San Francisco, CA:
Jossey-Bass.
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (Eds.). (2013b). Methods for community-based participatory research for
health (2nd ed.). San Francisco, CA: Jossey-Bass.
Israel, B. A., Lantz, P. M., McGranaghan, R., Guzman, J. R., Lichtenstein, R., & Rowe, Z. (2013). Documentation and evalu-
ation of community-based participatory research partnerships: The use of in-depth interviews and closed-ended question-
naires. In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods for community-based participatory research
for health (2nd ed., pp. 369–397). San Francisco, CA: Jossey-Bass.
Israel, B. A., Lichtenstein, R., Lantz, P. M., McGranaghan, R. J., Allen, A., Guzman, J. R., et al. (2001). The Detroit
Community-Academic Urban Research Center: Lessons learned in the development, implementation, and evaluation of
a community-based participatory research partnership. Journal of Public Health Management and Practice, 7(5), 1–19.
Critical Issues in Developing and Following CBPR Principles 43
Israel, B. A., Schulz, A. J., Parker, E. A., & Becker, A. B. (1998). Review of community-based research: Assessing partnership
approaches to improve public health. Annual Review of Public Health, 19, 173–202.
Johnson, D. W., & Johnson, F. P. (2014). Joining together: Group theory and group skills (11th ed.). Boston, MA:
Allyn & Bacon.
Jones, L., & Wells, K. (2007). Strategies for academic and clinician engagement in community-partnered participatory
research. Journal of the American Medical Association, 297, 407–410.
Lantz, P. M., Viruell-Fuentes, E., Israel, B. A., Softley, D., & Guzman, J. R. (2001). Can communities and academia work
together on public health research? Evaluation results from a community-based participatory research partnership in
Detroit. Journal of Urban Health, 78, 495–507.
LaVeaux, D., & Christopher, S. (2009). Contextualizing CBPR: Key principles of CBPR meet the Indigenous research con-
text. Pimatisiwin: A Journal of Aboriginal and Indigenous Community Health, 7(1), 1–25.
Minkler, M., Garcia, A. P., Rubin, V., & Wallerstein, N. (2012). Community-based participatory research: A strategy for
building health communities and promoting health through policy change. Oakland, CA: PolicyLink.
Minkler, M., Pies, C., & Hyde, C. A. (2012). Ethical issues in community organization and community participation. In M.
Minkler, Community organizing and community building for health and welfare (3rd ed., pp. 110–129). New Brunswick,
NJ: Rutgers University Press.
Minkler, M., & Wallerstein, N. (2012). Improving health through community organization and community building: Perspec-
tives from health education and social work. In M. Minkler, Community organizing and community building for health
and welfare (3rd ed., pp. 37–58). New Brunswick, NJ: Rutgers University Press.
Oetzel, J. G., Villegas, M., Zenone, H., White Hat, E., Wallerstein, N., & Duran, B. (2015). Enhancing stewardship of
community-engage research through governance. American Journal of Public Health, 105(6), 1161–1167.
Parker, E. A., Robins, T. G., Israel, B. A., Brakeeld, C. W., Edgren, K., & Wilkins, D. J. (2013). Developing and implement-
ing guidelines for dissemination: The experience of the Community Action Against Asthma Project. In B. A. Israel, E.
Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods for community-based participatory research for health (2nd ed., pp.
405–433, 639–643). San Francisco, CA: Jossey-Bass.
Parker, E. A., Schulz, A. J., Israel, B. A., & Hollis, R. (1998). Detroit’s East Side Village Health Worker Partnership:
Community-based lay health advisor intervention in an urban area. Health Education & Behavior, 25(1), 24–45.
Sallis, J. F., & Owen, N. (2015). Ecological models of health behavior. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.),
Health behavior: Theory, research and practice (5th ed., pp. 43–64). San Francisco, CA: Jossey-Bass.
Schulz, A. J., Israel, B. A., Coombe, C., Gaines, C., Reyes, A., Rowe, Z., et al. (2011). A community-based participatory
planning process and multilevel intervention design: Toward eliminating cardiovascular health inequities. Health Promo-
tion Practice, 12(6), 900–912.
Schulz, A. J., Israel, B. A., Mentz, G. B., Bernal, C., Caver, D., DeMajo, R., et al. (2015). Effectiveness of a walking group
intervention to promote physical activity and cardiovascular health in predominantly non-Hispanic Black and His-
panic urban neighborhoods: Findings from the Walk Your Heart to Health Intervention. Health Education & Behavior,
42(3), 380–392.
Schulz, A. J., Israel, B. A., Selig, S. M., & Bayer, I. S. (1998). Development and implementation of principles for community-
based research in public health. In R. H. MacNair (Ed.), Research strategies for community practice (pp. 83–110). New
York, NY: Haworth Press.
Steuart, G. W. (1993). Social and cultural perspectives: Community intervention and mental health. Health Education
Quarterly (Suppl 1), S99–S111.
Stringer, E. T. (2007). Action research (3rd ed.). Thousand Oaks, CA: Sage.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in dening phy-
sician training outcomes in multicultural education. Journal of Healthcare for the Poor and Underserved, 9(2), 117–125.
Udoh, I., Minkler, M., Dillard Smith, C., Chopel, A., Walton, S., Grijalva, C., et al. (2013). Developing and using a partner-
ship covenant to guide a study of late stage HIV diagnosis. Progress in Community Health Partnerships: Research, Edu-
cation, and Action, 7(4), 403–411.
Wallerstein, N. (2006). Evidence of effectiveness of empowerment interventions to reduce health disparities and social
exclusion. Copenhagen, DK: Health Evidence Network, Regional Ofce, World Health Organization. Retrieved from
www.euro.who.int/__data/assets/pdf_le/0010/74656/E88086.pdf
44 Community-Based Participatory Research for Health
Walters, K., Stately, A., Evans-Campbell, T., Simoni, J., Duran, B., Schultz, K., et al. (2009). “Indigenist” collaborative
research efforts in Native American communities. In A. R. Stiffman (Ed.), The eld research survival guide (pp. 146–
173). New York, NY: Oxford University Press.
Yonas, M., Aronson, R., Coad, N., Eng, E., Petteway, R., Schaal, J., & Webb, L. (2013). Infrastruture for equitable decision
making in research. In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods for community-based participa-
tory research for health (2nd ed., pp. 97–126). San Francisco, CA: Jossey-Bass.
Yonas, M. A., Jones, N., Eng, E., Vines, A. I., Aronson, R., Grifth, D. M., White, B., & DuBose, M. (2006). The art and sci-
ence of integrating undoing racism with CBPR: Challenges of pursuing NIH funding to investigate cancer care and racial
equity. Journal of Urban Health, 83(6), 1004–1012.

2
PART
POWER, TRUST, AND
DIALOGUE: WORKING
WITH DIVERSE
COMMUNITIES
Well-documented and complex health and social inequities continue to challenge all nations
across the globe and contribute to an immeasurable amount of suffering for living beings.
These inequities are associated, in part, with historic and current-day power imbalances that
often lead to loss of cultural and language identity, the discounting of traditional and place-
based knowledge systems, and the pathologizing of ways of being. CBPR or community-
engaged research (CEnR) is one response to health and social disparities among communities
46 Part 2
underserved by large national institutions such as economic systems, higher education, health
and medicine, and social services and policy.
Consequently, most if not all CBPR and CEnR takes place among groups of people with
varying types and degrees of diversity: race, cultural, language, economic, education, geo-
graphic, ability, and so on. Key elements of engagement success, therefore, are related to the
ability of mainstream research institutions and community and other partners to acquire the
skills and abilities to work across difference with trust and competence.
The two chapters in Part Two provide expert history, theory, and guidance about the need
for trust, cultural and racial competence, and skill building when working across differences for
equity. In Chapter4, Michael Muhammad and colleagues adopt a critical perspective to explain
how the intersecting dimensions of racism, power, and privilege can be reinscribed through the
white normalcy found in everyday research practices, even among groups with similar values,
ethnicities, and histories. The pernicious resistance to dismantling covert exploitive social struc-
tures (e.g., race and gender, education, economic privilege, etc.) is played out in CBPR through
language: microaggressions, invalidations, and insults that affect trust and expose conflicted
commitment, knowledge, and skills. The chapter illustrates problems and solutions through two
case studies that highlight intersecting oppressions and power structures in research: pressures
to conform to institutional research process that privileges dominant group values and commu-
nication styles and that devalue others. The chapter ends with recommendations for disrupting
business as usual and creating equity in research partnerships. (Chapter8 also provides concrete
measures to undo racism in CBPR projects.)
In Chapter 5, Julie E. Lucero and colleagues review the strengths and challenges of the
current literature and research on trust and its conceptualization and use in partnership
research. Early literature on the topic often considered trust only from the academic partners’
perspective and characterized trust as an “outcome” and dichotomous variable, present or
absent. Lucero outlines the problems with these conceptualizations and provides qualitative
and quantitative evidence from multiple partner perspectives for a multidimensional trust
typology. The comprehensive and multisector perspectives of the typology provide important
process variables for partnership to consider when assessing partnership relational dynamics
and provide guidance on the ground for working with integrity across difference. Further issues
of relationship processes are outlined in the descriptions of the CBPR model and partnership
evaluation methods in Chapters6 and 17.
4
CHAPTER
UNDERSTANDING
CONTEMPORARY RACISM,
POWER, AND PRIVILEGE AND
THEIR IMPACTS ON CBPR
MICHAEL MUHAMMAD, CATALINA GARZÓN, ANGELA REYES, AND
THE WEST OAKLAND ENVIRONMENTAL INDICATORS PROJECT
RACISM IS AN inescapable structural social determinant in the United States and globally,
with deep and broad impact on health inequities in communities of color, and therefore with
signicant implications for the practice and outcomes of CBPR partnerships. The distribution
of health inequities reects the extensive structural inequalities prevalent within society inter-
secting across racial, ethnic, gender, sexual orientation, and socioeconomic class designations.
Social attitudes and opinions also affect health for marginalized populations through knowledge
produced that further constrain their ability to access resources providing health benets.
Because of the cumulative effect of racism, which leads to widespread negative health out-
comes, this chapter focuses on the complexities of racism. Structural inequality and institutional
racism, most notably the residue of political and legal disenfranchisement and discrimination of
American Indians, Asians, Blacks, and Latinos, has contributed to signicant inequities in health
for people of color (Gee & Ford,2011; King, Smith, & Gracey,2009; Williams,2012). Cultural
beliefs about the inherent differences between racialized social groups rationalize differential
access to health-promoting resources through stereotypes, stigmatization, and implicitly held
48 Community-Based Participatory Research for Health
bias (Smedley,2012). The multiple vulnerabilities produced by racism are further complicated
through the intersection of positionality and power inequality.
This chapter adopts a critical perspective for how the intersecting dimensions of racism,
power, and privilege can be reinscribed while conducting CBPR, even when participants share
a common identity as people of color. In comprehending how whites benet from a system of
racialized oppression and privilege, CBPR practitioners will be positioned to better understand
the systemic organization of modern racism, making overt acts of prejudice and discrimination
obsolete, and understand how hegemonic reinforcement of existing racialized social relations
can be consciously or unconsciously reproduced by any person, regardless of racial or ethnic
identity. Readers also will become more familiar with the various forms that power and priv-
ilege can take in our work, within and beyond racism. Our goal is to build on these under-
standings and strengthen existing CBPR approaches for disrupting the reproduction of racial
inequality and other hierarchies of power and privilege to promote sustainable, equitable part-
nering processes within diverse academic-community partnerships.
We offer two examples of how academics and community leaders can engage in ongoing
strategies to conduct antiracist and power-equalizing interventions to deepen CBPR partner-
ships and increase the impact of research endeavors. In an environmental justice (EJ) case study
from West Oakland, California, we illustrate how an African American community leader in the
EJ movement and her academically trained research partner, a Latina who shared her deep com-
mitment to addressing environmental racism, collaborated to colead an effective CBPR effort
for action and change while also increasing honest dialogue within the partnership about power
and privilege. Second, we offer the reections of a multiracial, multicultural, interdisciplinary
team at the University of New Mexico in confronting their own opportunities and limitations
in seeking to create equitable research partnerships with communities of color who have faced
long histories of racism.
CBPR AND THE EXPLORATION OF RACISM
More than twenty-ve years of evidence demonstrate the role of CBPR in seeking to cre-
ate equitable research environments in the pursuit of shared goals of health equity and envi-
ronmental and social justice. However, far less attention has been placed on integrating the
conceptual frames developed from antiracism research as a component of participatory partner-
ing processes. This is especially important for confronting contemporary racism in the conduct
of CBPR. Here is the uncomfortable part: all “whites” derive some degree of benet (often
including economic) from racism in the United States. A major challenge, therefore, concerning
the practice of authentic CBPR is the need to train practitioners to perceive the covert mecha-
nisms by which racism is reproduced within social relations and to maintain a self-awareness
for how attention to equitable partnering processes is essential to disrupting the perpetuation of
systemic racism.
Some CBPR scholars have employed theoretical, interpretive, and conceptual frameworks
that aid researchers in clarifying how racial inequality undermines a genuine commitment to
equitable partnering practices (Chavez et al.,2008). Popular approaches for antiracism work
within CBPR coalesce around social justice, white privilege, cultural humility, and postcolonial
epistemologies (Wallerstein & Duran,2006). Jones’s (2000) insightful allegory, the gardener’s
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 49
tale, has been used to deconstruct the differences among structural, interpersonal, and inter-
nalized racism. Each of these frameworks offers unique strengths, perspectives, and analytical
techniques useful for studying the impact of racism in diverse CBPR partnerships. We add to
these paradigms three cutting-edge theoretical and analytical approaches of antiracism scholar-
ship—systemic racism, covert racism, and linguistic racial accommodation (LRA)—which are
more specically attuned to the task of clarifying the often obfuscated and subtle nature of con-
temporary racism.
UNDERSTANDING RACISM AND ANTIRACISM FRAMEWORKS
A major obstacle confronting those engaged in antiracism research, activism, and scholarship
working from diverse backgrounds and across major disciplines is the lack of consensus in
clearly dening the terms race, racist, and racism. Although social construction of identity
has gained credibility over biological classications of superior and inferior races (Smedley
& Smedley,2005), the addition of bi- and multiracial classications along with the conation
of race with ethnicity increases the potential for confusion, miscommunication, and lack of
conceptual clarity for antiracism CBPR work.
Three-Tiered Racism Framework
Jones (2000) has developed a framework for understanding racism as institutionalized, per-
sonally mediated, and internalized. Institutionalized racism manifests itself in material condi-
tions and access to power, such as differential access to quality education, gainful employment,
appropriate medical facilities, and clean environments. With regard to power, institutionalized
racism includes differential access to information, including one’s own history, resources, and
voice, and differential representation in government and the media. Personally mediated racism
refers to prejudice, discrimination, and judgments based on assumptions about others according
to their race. As Jones (2000) notes, this “is what most people think of when they hear the word
racism...It manifests as lack of respect, suspicion, devaluation, scapegoating, and dehuman-
ization” (p. 300). Internalized racism does not need an outside judge of character. It is character-
ized by people’s own belief in the negative messages they receive about their race or ethnicity.
The core of this perspective is that “an oppressive society re-creates itself in its victims’ hearts”
(Sherover-Marcuse, 1986, p. 4). Internalized oppression addresses subjectivity, questions of
power, and the part each person plays in the evolution of his or her own life story. It acknowl-
edges that oppression does not only come from an external intersection of multiple systems of
inequality; the enemy is also within.
Systemic Racism
Systemic racism adds a conceptual and interpretative scheme of structured relations with inter-
dependent features that Feagin (2006) refers to as the white racial frame. This frame comprises
a web of interrelated social practices, policies, attitudes, norms, and stereotypes that serve to
reinforce social relations perpetuating white racial dominance. This interplay of social forces
and institutional practices has created privileges and advantages for whites as a direct result
of denying the same for people of color. Racial oppression has lasted for several centuries and
has become well entrenched and pervasive across all major US institutions because of a “social
50 Community-Based Participatory Research for Health
inertia” that resists change. The white racial frame rationalizes and justies racial and socioeco-
nomic inequality according to a belief system that conveniently omits the violent oppression of
people of color, including decades of legal discrimination as fundamental tenets of white privi-
lege and status. Concurrently, a continuously shifting narrative lauding work ethic, intelligence,
and cultural superiority is socially reproduced explaining white racial dominance.
Systemic racism will remain intact until the social processes reproducing the multilevel
structures of racial hierarchy and power inequity are disrupted. What this implies is that whites
must acknowledge the unearned privileges and benets accruing from the ongoing oppression
of American Indians, Asians, Blacks, and Latinos and become actively engaged in deconstruct-
ing embedded racist beliefs, practices, and policies throughout society.
Covert Racism and Microaggression
In contemporary society, overt expressions of racial prejudice and discriminatory practices are
most often no longer publicly acceptable and, in some cases, illegal. However, resistance to dis-
mantling inegalitarian social structures and relations is often encountered indirectly. Covert rac-
ism is subtle and allows for informal mechanisms of reward, prestige, or privilege not based on
the rule of law (Coates,2011). Covert racism can be language interwoven with racially coded
meaning to induce racial animus and practices that serve to reinforce white privilege. Covert
racist practices are skillfully employed to avoid open criticism of being racially motivated or
clearly recognized as prejudice or discrimination. Covert racism is often expressed through
microlevel interactions as microaggressions, meaning “commonplace verbal or behavioral
indignities, whether intentional or unintentional, which communicate hostile, derogatory,
or negative racial slights and insults” (Sue et al.,2007, p. 278). These can be micro-insults,
expressed as unconscious remarks or actions that convey rudeness, such as a white county
planning commissioner’s openly snickering while Latino community residents offer testimony
during public hearings, or micro-invalidation, often unconscious verbal comments or actions
that exclude or negate the feelings or lived experiences of a person of color, such as holding
an important community meeting in a Latino community with a large non-English-speaking
population without Spanish language translators.
Racism is often subsumed within the dimensions of positionality and power inequity. In
community-academic CBPR partnerships, power (e.g., positionality, education, income, and
privilege) usually resides with academic researchers who are often white and live outside the
communities they partner with. “Outside” experts can be faced with the dilemma of reinterpret-
ing “insider” knowledge. The predilection to impose dominant group interpretive frames on
local knowledge through re-articulation into more technical language may result in (uninten-
tional) micro-invalidations that undermine mutual respect, co-learning, and devalues community
partner contributions.
Linguistic Racial Accommodation (LRA)
A recent LRA framework and repertoire of analytical tools was developed by Cazenave (2016)
for explicating “language-centered evenness and denial practices” that have become prevalent
in mainstream discourses on race and racism. Cazenave calls the social reproduction of systemic
racism through language, the ignorance, privilege, arrogance syndrome, a condition that occurs
when dominant group members fail to recognize the oppression of subordinated groups: “that
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 51
is the ignorance of not knowing, the privilege of not needing to know, and the arrogance of not
wanting to know” (p. 17). Benign, abstract, and inconsequential language is often elicited to
evade a serious critique of how whites continue to benet from racism. For example, the terms
disadvantaged, at risk, or marginalized are often used to describe communities of color. What
is seldom mentioned is how these communities arrived in such condition, to what extent is rac-
ism responsible, and how whites as a dominant group derive benet from impoverished and
unstable communities of color. LRA conceptualizes how asymmetric power relations captivate
the production of knowledge about racism with words and concepts that align with attitudes
and behaviors of the dominant group, leaving the structural organization of racial oppression
relatively unchallenged.
These frameworks have been introduced to aid in understanding racism as a complex
system for creating and replicating social inequality within various domains and at multiple
levels of social interaction. Racism is systemic, mediated at individual and institutional levels,
and can be openly or subtly expressed. The recognition of racism in its various forms is only
the rst step in antiracism work. The social processes and practices sustaining inequality must
be deconstructed with concise language that has the conceptual power to detect and clarify the
racist underpinnings of white normalcy in everyday practices. The objective is to develop an
awareness capable of grasping the mechanisms by which racial inequality is socially repro-
duced and disrupt the process.
BEYOND (AND WITHIN) RACISM: POWER AND PRIVILEGE IN CBPR
Similar to racism, the concepts of power and privilege are central to CBPR, particularly in fem-
inist and Indigenous participatory research (Fine,2004; Lonczak et al.,2013). In-depth work
in the eld has explored how participatory approaches challenge, reinforce, or change power
relationships between trained researchers and community groups. However, this too is com-
plicated. “Though practitioners of participatory research routinely draw on the concept that
knowledge is power, they seldom publicly share how power dynamics between researchers
and community partners have played out in particular partnerships ...” (Garzón et al.,2013,
p. 72). Discourse on power and privilege frequently is intertwined with explorations of race
and racism, and appropriately so, given the interlocking systems of oppression in which race
or ethnicity bear long and deep relationships to the power and privilege experienced. Yet power
and privilege also are played out when, for example, an African American researcher with a
PhD is heavily advantaged nancially with status and perceived authority in a CBPR project,
when compared to the lead community partner who is also an African American woman but
lives in poverty and has a high school diploma.
Further, and particularly in CBPR and related partnerships, conventional conceptualiza-
tions of power and privilege may not capture the nuances involved. Privilege, for example, is
frequently dened as “unearned access to resources” because of one’s advantaged social loca-
tion, whereas power is the ability to decide who will have access to resources as well as “the
capacity to inuence the behaviors of others or one’s self, or the course of events” (Myers &
Ogino,2016, p. 8). These terms are all examples of linguistic racial accommodation, which
don’t convey historical and structural reasons for lack of resource access or how the capacity to
inuence people and events was acquired.
52 Community-Based Participatory Research for Health
CBPR STRATEGIES TO COMBAT RACISM
CBPR partnerships should consider incorporating strategies that help clarify the multilevel
mechanisms through which racism, power, and privilege can affect partnering processes and
research outcomes. This would include the ways the partnerships themselves may inadvertently
reinscribe positions of power through racially accommodative language based on white privi-
lege within partnering processes (Yonas et al.,2006). Especially important for diverse partner-
ships is the need to create an atmosphere that fosters open communication about partners’ lived
experiences negotiating racial oppression and privilege. Periodic sessions (formal or informal)
encouraging reexivity about partners’ experience with racism may generate useful insights that
can inform research design, knowledge production, and identify areas where racism is uninten-
tionally being reproduced within the partnership (see Chapter8 on formal antiracism training).
Team reections about race and racism, however difcult, may yield a synergism contributing
knowledge and research for combatting social, racial, and health inequities.
CBPR CASE STUDIES: PRACTICAL APPLICATIONS
In this section, we use examples from two case studies that examine how racism, power, and
privilege can be reproduced unintentionally within a CBPR partnership and showcase new
theoretical conceptions of identity that should be considered within diverse partnerships and
research teams. We will draw on our conceptual and theoretical frames to provide recommen-
dations to help CBPR researchers and partnerships be aware of subtle forms of racism, power,
and privilege and how they can be addressed among partners. These case studies offer a chance
to examine more deeply the ways American Indians, Blacks, Latinos, and other people of color
may be subjected to systemic racism and marginalization through the interpersonal dynamics
of communication. What is considered acceptable ways of communication are subject to many
factors, such as type of discourse (formal-informal), positionality within the power hierarchy,
identity, and communicative context or setting (Muhammad et al.,2015). Applying a microlevel
lens examining how communication is marginalized within participatory research illustrates
how racism can be reproduced within partnerships unintentionally, including when navigating
pressures to conform to institutional research process and when reporting on scientic data,
which privileges dominant group values and communication styles.
West Oakland Environmental Indicators Project
The largely African American and Latino community of West Oakland, California, has a long
and proud history of activism, dating to its role as the birthplace of the Pullman Porters’ Union
and later of the Black Panthers Party (Rhomberg,2004). Bounded on three sides by freeways,
however, and home to the state’s second busiest port and other trucking-related industries, West
Oakland has also long suffered high rates of illnesses exacerbated by air pollution, including
asthma hospitalization rates in children seven times the state average (Pacic Institute & West
Oakland Environmental Indicators Project,2002). To address these issues, a CBPR partnership
was established in 1999 between a local environmental justice group, now known as the non-
prot West Oakland Environmental Indicators Project (WOEIP), and a local nonprot research
institute, the Pacic Institute (PI). Through its Community Strategies for Sustainability and
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 53
Justice (CSSJ) program, PI helped train residents who undertook air sampling, truck counts,
and other methods that demonstrated highly disproportionate exposures borne by its mostly
low-income African American and Latino residents. The fteen-year WOEIP-PI partnership is
best known for its use of its data collection and strong media and policy advocacy to help create
systems-level changes (e.g., a truck route ordinance). In 2016, WOEIP was involved in citywide
efforts to successfully ban the storage of coal at the Port of Oakland. But the partnership also
has engaged in deep reection and dialogue on its own processes as these relate to power and
privilege (see Garzón et al.,2013; Gonzales et al.,2011), to which we now turn.
The intersections among race, ethnicity, gender, and class were among the areas explored
by the partnership in relation to power and privilege. Within PI, a highly educated Latina who
co-led CSSJ noted that she had experienced “racialized and gendered stereotypes” causing her
to need to be “twice as good as my white male counterpart to get the same level of respect and
recognition.” She went on to note that “it throws people off when the researcher in the room is
not a white male, because the expectation is that women of color should be the recipients, and
not the providers of services” (Garzón et al.,2013, p. 74). By contrast, the white male who co-
led WOEIP noted that although he was acutely aware of the unearned power his race and gender
accorded him in other spheres (e.g., in being able to get a police response when his neighbors
of color could not), within the partnership he clearly didn’t “carry the weight” that his African
American female colead did in their community work, and he routinely deferred to her for that
reason (p. 74).
Microaggression occurred in the course of the partnership’s work. The act of translation
for community and decision-maker audiences was a common role that CSSJ and WOEIP staff
members played for each other. In community meetings, WOEIP staff members often would
elaborate on what CSSJ staff members said by using less formal and more emotive language.
By contrast, when drafting technical documents, CSSJ staff members would often wordsmith
what WOEIP staff members said to conform to a scientic writing style by editing statements
that could be interpreted as anecdotal or emotional. Although this often worked well, a CSSJ
leader noted that WOEIP staff members had sometimes “called me on being too academic,” and
WOEIP staff members also sometimes felt that their words had just been reiterated in a more
“jargony” way.
WOEIP and CSSJ partners commented on such dynamics in further reecting on their
communication styles and related power differences. A WOEIP staffer thus remarked that “the
ability to have technical skills to write...gives power to the research group” and sometimes
results in power dynamics and perceived devaluating that takes the form of unconscious micro-
insults. WOEIP staff members noted that they thus didn’t have “the ability to put things into
print, reports, or responding to email, but as a result had to deal with how [CSSJ] gets disap-
pointed on not getting deliverables in a timely manner” (Garzón et al.,2013, p. 75). Conversely,
CSSJ staff members often felt uncomfortable refraining from expressing themselves in front of
WOEIP in order to show deference to the community partner. As one staff member reected:
One thing I noticed myself doing a lot of is giving WOEIP staff space to talk. By not taking up
space I gave them space to talk, but I don’t think I was actively listening...I felt like I was
reproducing the dynamic of when residents speak to decision makers. There is no real engage-
ment there ...
54 Community-Based Participatory Research for Health
Finally, and despite deep recognition of the mutual benets of working in partnership, ten-
sions also played out concerning power dynamics and were reected in a partner’s comment
that “I had to learn the difference [among] being authentic in my testimony, telling the truth
based on my experience, and being tactful.”
Central tenets of CBPR recognize the value of local knowledge and the idea of community
as a fundamental unit of identity (see Chapter3). Does community cultural identity, knowledge,
expertise, and communication style only have value as long as it remains within the connes
of the community or bracketed with quotations as qualitative data (Reyes Cruz, 2008)? The
practice tacitly suggests that during the process of dominant group cultural translation, the
feelings, thoughts, and experiences of people of color must be expressed in a format that privi-
leges the perspective of the oppressor and not the oppressed to have scientic validity. Revising
communication styles to conform to “scientic writing” standards is a type of oppression that
imposes dominant group standards depriving the speaker of his or her cultural communica-
tion (Sue et al.,2007). The potential to reproduce systemic racism through microaggression
within this CBPR partnership was witnessed in two ways: (1) as micro-insults, when institu-
tional norms devalued the ways people of color expressed themselves about their lived experi-
ence as anecdotal or emotional communication and therefore inferior styles (Sue,2007); and
(2) as micro-invalidations, by conceptualizing language expressed by community partners as
somehow lacking scientic merit because it lacked conformity to dominant group technical
communication standards.
UNM CBPR Team Reflections
CBPR academic practitioners have recognized the potential for reproduction of gender, racial,
ethnic, and socioeconomic inequalities and power differentials within the research process and
within the production of scientic knowledge itself. Researchers also may have power and privilege
from their class, education, racial-ethnic backgrounds, or other identity positions. Both of these
positionalities (power and privilege) have the potential for reproducing systemic health inequities
and disadvantaging community partners. Reection on issues of power, identity, and positionality
has led the research team at the Center for Participatory Research at the University of New Mexico
(UNM-CPR) to examine in greater detail the need for theoretical frameworks for understanding
power and privilege and their effects on research partnering processes and outcomes (Muhammad
et al.,2015). This team has sought to better understand research positionality through examining
their ascribed and achieved identities that confer status on an individual researcher, such as race
and ethnicity or level of education attained. They have grappled with how to better share power as
a dening factor in building effective academic-community collaborations.
A panel, “Insider/Outsider: Our Ascribed and Achieved Identities as Researchers,” con-
ducted at the 2011 University of New Mexico “CBPR for Health” annual summer institute,
uncovered these issues, reecting on their own personal life experiences, motivations, and con-
nections between themselves and communities they partner with (e.g., such as the differences
for a Latina scholar working in her own community versus working in one very different in
history or origin).
From the panel, a Chicana scholar spoke about the inextricable link between her personal
and professional identities. For her, CBPR is not merely a research paradigm but “a way of life.”
She stated a researcher committed to the ideals of CBPR must be willing to undergo a process
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 55
of deconstruction. In other words, researchers must be willing to have one’s various identities
and lived experiences confronted within the context of societal power inequity as a necessary
process for building genuine CBPR teams and partnerships. A Native scholar shared this view
but from a slightly different perspective. The CBPR team approach enabled her to more seam-
lessly bridge core identity beliefs with her research. “You know I’ve always said that CBPR
allowed me to be who I am...I haven’t had to be someone else in the research process.” This
comfort resonated as a way to handle the stress often felt by researchers of color working within
dominant group institutions that perceive them as subordinated to others. Tensions may arise
when researchers feel compelled to sublimate one’s cultural identity, appearance, or style of
communicating to conform to majority group norms about knowledge construction.
The importance of CBPR research reinforcing the life experiences of scholars of color does
not necessarily extend to researchers from more outside identities. A white researcher from an
academic middle class background discussed how she never claimed similar life experiences
to the tribes she works with, though she has developed long-term relationships and friendships
with tribal partners. She is well aware that she has power and privilege not just as an academic
but also attributable to the characteristic of whiteness. “My question has always been, how can I
do participatory research with integrity and use the resources and power that I have to work with
communities in a positive way.” A Black academic researcher also saw his racial identity as a
resource to be used within the research environment. While conducting eld work in southern
rural Missouri, he talked about noticing the local cultural norm discouraged discussion of racial
inequality and used that insight to enhance data collection through private conversations. In this
community, whites often denied that racism still existed, yet Blacks acknowledged its existence
but preferred not to dwell on the past, and they were able to talk with the Black researcher
more directly about their experiences than if he had been white. The scholars of color on the
panel expressed their strong attachment for racial, ethnic, or cultural identity as protective and
a valuable research skill. One scholar concurred about the importance of having a clear under-
standing of her identity as a researcher of color, “I feel as an American Indian woman, with me
strongly attached to my identity and my community, that I am able to address some of the most
persistent health disparities among American Indian women.”
DISRUPTING THE POTENTIAL FOR REINSCRIPTION OF RACISM IN CBPR
In this chapter, racism is conceptualized as a comprehensive interaction among systemic-
institutional, interpersonal, covert, and internalized racism, often embodied in linguistic racial
accommodations. These understandings manifest themselves in multiple positions of power and
privilege that can permeate partnerships, often in unintentional ways, and affect the capacity
of the partnership to challenge external inequities. The examples presented here show how
CBPR practitioners working with communities of color can consider incorporating partnering
processes that dislodge the centrality of white privilege throughout all phases of the research.
People of color have well learned that open criticism of institutional policies and practices
as being racist can result in retaliation and the denial of benets (i.e., grants, community
investment, employment promotions).
A genuine commitment to the ideals of CBPR and social justice is essential to avoid the
co-optation of CBPR under the inuence of instrumentalist variants of participatory research
56 Community-Based Participatory Research for Health
(Trickett,2011) that exploits communities of color for funding and professional advancement
while replicating power hierarchies and white hegemony in knowledge production. Several
aspects of the research process can unintentionally (or covertly) reinscribe systemic racism at
critical junctures across the life span of the partnership and therefore need to be elevated to a
conscious antiracism reection and action (Yonas et al.,2006). For examples of deliberate work
against covert and overt systemic racism, see Chapter8 on a CBPR project within two cancer
care institutions and Chapter22 on participatory action research efforts to challenge the unjust
criminal system. (See also anti-racism training in Yonas et al., 2013.)
In conclusion, recommendations are provided on how to add antiracism enhancements to
traditional CBPR in three key research areas.
Community Capacity Building
A fundamental aim of CBPR is to enhance the skills, provide opportunities for training, and
expand the knowledge base of community and university partners and stakeholders. The
question facing the next generation of academically trained CBPR practitioners is, to what
extent are academic institutions, funding bureaucracies, academic publishers and journal edi-
tors, and academic researchers willing to participate in a social and intellectual revolution that
undermines the present system of inequality?
A popular strategy used to frame this often-difcult dialogue about racism and community
capacity relies on Cazenave’s (2016) linguistic racial accommodation. It is not uncommon for
researchers, policy experts, community partners, and activists, for example, to reject the notion
of a “decit” assessment of community resources, choosing instead to emphasize community
assets as a focal point for discussion. Although an important change of framework, this assets
approach can unfortunately fail to address the structural factors that contributed to the destabi-
lization of communities of color. This approach is tantamount to asking a person whose home
has been burglarized to focus more on what the thief left than what was stolen. Community
capacity building, especially for communities of color, is directly linked to the principle of
restorative justice. More specically, it comes with the recognition that white privilege is an
unearned benet and, therefore, creates a responsibility to act to counter historical oppression
of people of color.
Equitable Distribution of Funding
Another major challenge for participatory research is the inherent bias favoring academic and
research institutions over the control and distribution of resources. It is now a standard require-
ment for most federally funded CBPR and community-engaged research projects to have at
least one of the partners be a community-based organization. Usually, grant applications are
submitted on behalf of a CBPR partnership consisting of academic and community partners.
Although community groups or partners may be increasingly receiving budget subcontracts,
universities and research institutions as the centers for expert knowledge and as nancial
intermediaries enjoy the bulk of grant funding primarily through university indirect costs and
academic salaries. Community partners may receive nominal stipends (individually or as an
organization) as compensation for their participation. Community-based organizations who
partner with universities on CBPR projects are often located in impoverished, racially segre-
gated, environmentally hazardous, violent, and politically isolated communities of color. Why?
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 57
Because communities so affected by structural inequality and systemic racism also just happen
to contain easily identiable research populations (racial segregation) with high prevalence of
negative health outcomes that politicians, funders, universities, research institutions, and aca-
demically trained researchers are concerned about. Systemic racism and the relative obscurity
of its functioning within present funding effectively reproduces racial and ethnic inequality
through academic research and helps to keep communities of color in a state of dependency
and subordination to academic institutions. An alternative to the current research funding struc-
ture is to direct more money toward development of federally funded permanent community
research institutions and paid community research staff within existing or new community-
based organizations similar to a federally qualied health center or centers of excellence. Just as
it was shown that certain protections for human subjects was morally correct, similar arguments
and advocacy can be made against the economic injustices pertaining to current research fund-
ing practices.
Researcher Identity and Positionality
Researcher identity and positionality reect statuses (in part) derived from dominant group
social and academic institutions and may have an impact on the valuation of community
knowledge and outcomes. Under CBPR research processes, external and internalized power
dimensions are the underlying context for academic and community collaboration (Wallerstein
& Duran,2008). CBPR partnerships face additional forms of power hierarchy: that which is
most described, the relationships between academics and community partners, and that which
may exist within the academic team between the principal investigator (often still from a white
and more privileged background) and other investigators or research staff (Lingard, Schryer,
Spafford, & Campbell,2007).
Scholars of color on the research team may experience their own knowledge being mar-
ginalized in the academy, because their communities have been led to believe that their cultural
heritage and knowledge is devalued by mainstream society. Historically, they have seen their
communities as often the objects of research, with the knowledge generated appropriated to
reect the theories and requirements of the academy. At the same time, they face the contra-
diction that they are the academics, too, and question which knowledge paradigms to embrace.
One important strategy is to include academic team members whose identities (i.e., gender,
race, ethnicity, sexual orientation, and class) intersect or bridge with those of the community
partners. If there is not a cultural match of research team members with the community
population, it becomes essential to work diligently to diversify your institution’s faculty mem-
bers and students and seek a cultural broker from the community itself. Changing the face of the
academy is an important structural way to make a difference in knowledge production, because
diverse academies foster trust, effective communication, access to local knowledge, and the val-
uing of epistemological diversity.
CONCLUSION
One under-theorized outcome of CBPR is liberation from traditional forms of knowledge pro-
duction for the community and the academics involved in the work. When the ideals of CBPR
are faithfully adhered to, the community is better able to free itself from the social structural
58 Community-Based Participatory Research for Health
factors that have historically silenced its voices of concern and marginalized its aspirations
for hope (i.e., from colonization, racism, sexism, and economic exploitation). The academic
researcher may likewise nd release from personal and cultural biases that can develop through
the achieved status of rigorous academic training and through the ascribed status arising from
individual power, privilege, and prestige accruing as an academic. It is essential to acknowledge
the continued importance of cultural humility (see Appendix 4) even when there are shared
communities of identity between researchers and community partners. Level of formal educa-
tion, institutional afliation, lived experience, and roles in the partnership can also create power
differentials that need to be navigated carefully and can take on even more signicance when
other identity markers such as race and gender are shared. Deconstructing these issues from
one’s personal positionality, within the partnership and within societal structures, can be the
beginning to the long journey of the struggle for racial justice.
QUESTIONS FOR DISCUSSION
1. Describe how systemic racism is able to function with little observation in today’s society.
Can you give examples of your personal experience with incidences of covert racism, priv-
ilege, or microaggression?
2. Why is researcher identity and positionality important to consider when forming a CBPR
partnership?
3. Consider the different phases of CBPR research. In what ways can microaggression, micro-
invalidation, and micro-insult become a usual part of a community-academic partnership?
REFERENCES
Cazenave, N. A. (2016). Conceptualizing racism: Breaking the chains of racially accommodative language. Lanham, MD:
Rowman & Littleeld.
Chavez, V., Duran, B., Baker, Q., Avila, M., & Wallerstein, N. (2008). The dance of race and privilege in community-based
participatory research. In M. Minkler & N. Wallerstein, (Eds.), Community-based participatory research in health (pp.
81–97). San Francisco, CA: Jossey-Bass.
Coates, R. D. (2011). Covert racism: An introduction. In R. D. Coates (Ed.), Covert racism: Theories, institutions, and expe-
riences (Studies in Critical Social Sciences). Leiden, the Netherlands: Koninklijke Brill NV.
Feagin, J. R. (2006). Systemic racism: A theory of oppression. New York, NY: Taylor & Francis.
Fine M. (Ed.). (2004). Off white: Readings on power, privilege, and resistance. New York, NY: Routledge.
Garzón, C., Beveridge, B., Gordon, M., Martin, C., Matalon, E., & Moore, E. (2013). Power, privilege, and the process of
community-based participatory research: Critical reections on forging an empowered partnership for environmental jus-
tice in West Oakland, California. Environmental Justice, 6(2), 71–78.
Gee, G. C., & Ford, C. (2011). Structural racism and health inequities: Old issues, new directions. Du Bois Review,
8(1), 115–132.
Gonzales, P., Minkler, M., Garcia, A., Gordon, M., Garzón, C., Palaniappan, M., Prakash, S., & Beveridge, B. (2011).
Community-based participatory research and policy advocacy to reduce diesel exposure in West Oakland, California.
American Journal of Public Health, 101(Suppl 1), S166–S175.
Jones, C. P. (2000). Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health, 8,
1212–1215.
Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR 59
King, M., Smith, A., & Gracey, M. (2009). Indigenous health part 2: The underlying causes of the health gap. Lancet,
374, 76–85.
Lingard, L., Schryer, C. F., Spafford, M. M., & Campbell, S. L. (2007). Negotiating the politics of identity in an interdisci-
plinary research team. Qualitative Research, 7(4), 501–519.
Lonczak, H. S., Thomas, L. R., Donovan, D., Austin, L., Sigo, R. L., Lawrence, N., & Suquamish Tribe. (2013). Navigating
the tide together: Early collaboration between tribal and academic partners in a CBPR Study. Pimatisiwin, 11(3), 395–409
Muhammad, M., Wallerstein, N., Sussman, A. L., Avila, M., Belone, L., & Duran. B. (2015). Reections on researcher iden-
tity and power: The impact of positionality on community-based participatory research (CBPR) processes and outcomes.
Critical Sociology, 41(7–8), 1045–1063.
Myers, A., & Ogino, Y. (2016). Power, privilege, & oppression. Retrieved from www.scrippscollege.edu/xbk/wp-content/
uploads/sites/35/les/Power-Privilege-and-Oppression.pdf
Pacic Institute & West Oakland Environmental Indicators Project. (2002). Neighborhood knowledge for change: The West
Oakland environmental indicators project. Oakland, CA: Pacic Institute.
Reyes Cruz, M. (2008). What if I just cite Graciela? Working toward decolonizing knowledge through critical ethnography.
Qualitative Inquiry, 14(4), 651–658.
Rhomberg, C. (2004). No there there: Race, class, and political community in Oakland. Berkeley: University of California Press.
Sherover-Marcuse, R. (1986). Emancipation and consciousness: Dogmatic and dialectical perspectives in the early Marx.
Malden, MA: Blackwell.
Smedley, A., & Smedley, B. (2005). Race as biology is ction, racism as a social problem is real: Anthropological and histor-
ical perspectives on the social construction of race. American Psychologist, 60, 16–26.
Smedley, B. (2012). The lived experience of race and its health consequences. American Journal of Public Health, 102,
933–935. doi:10.2105/AJPH.2011.300643
Sue, D. W., Capodilupo, C. M., Torino, G. C., Bucceri, J. M., Holder, A., Nadal, K. L., & Esquilin, M. (2007). Racial microag-
gressions in everyday life: Implications for clinical practice. American Psychologist, 62(4), 271–286.
Trickett, E. J. (2011). Community-based participatory research as worldview or instrumental strategy: Is it lost in translation(al)
research? American Journal of Public Health, 101(8), 1353–1355.
Wallerstein, N. B., & Duran B. (2006). Using community-based participatory research to address health disparities. Health
Promotion Practice, 7, 312–323.
Wallerstein, N., & Duran B. (2008). The theoretical, practical, and historical roots of CBPR. In M. Minkler & N. Waller-
stein (Eds.), Community-based participatory research for health: From process to outcomes (2nd ed., pp. 25–46). San
Francisco, CA: Jossey-Bass.
Williams, D. R. (2012). Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior,
53(3), 279–295.
Yonas, M. A., Jones, N., Eng, E., Vines, A. I., Aronson, R., Grifth, D. M., White, B., & DuBose, M. (2006). The art and sci-
ence of integrating undoing racism with CBPR: Challenges of pursuing NIH funding to investigate cancer care and racial
equity. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 83(6), 1004–1012.
Yonas, M. A., Aronson, R., Coad, N., Eng, E., Petteway, R., Schaal, J., & Webb, L. (2013). Infrastructure for equitable
decision making in research. In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods for community-based
participatory research (2nd ed., pp. 97–126). San Francisco, CA: Jossey-Bass.
5
CHAPTER
TRUST IS FOUNDATIONAL to all human relationships and becomes exceedingly important in
relationships in which risk and safety are concerned. Associations developed because of health
research are one such type of relationship. Community-academic partnerships are examples of
situations in which researchers are granted a position to help in the goal of improving health, yet
they pose a real threat of opportunistic behavior. Research has often been concerning to under-
served communities because of the historical practices that contribute to risk and destabilizing
safety. These have included undermining of autonomy, coercion and power imbalances, research
without community benet, interpretation and reporting of data resulting in community stigma
or cultural misunderstanding, and general lack of reconciling community concerns (Cochran
et al.,2008; Cook & Jackson,2012). Related to risk is conict, and when trying to resolve or
lessen risk, conict can emerge because of inherent differences in perceptions, culture, goals,
and values (Cochran et al.,2008; Lucero & Wallerstein,2013; Pondy,1992). Therefore, con-
scious reconciliation of these differences has the potential to mitigate conict, decrease risk,
improve safety, and build trust.
Community-based participatory research (CBPR), a research approach that falls under the
umbrella of community-engaged research, seeks to democratize research and promote health
equity. Through the democratization process, partners can reconcile conict-causing differ-
ences and challenge the position of power, knowledge creation, and oppression within historic
research endeavors (Chavez et al.,2008; Freeman et al.,2006). Despite the promise of equity,
many underserved communities may still be wary of CBPR research because of the history of
inappropriate research and opportunistic researchers (Cochran et al.,2008). It is impossible
TRUST DEVELOPMENT IN
CBPR PARTNERSHIPS
JULIE E. LUCERO, KATHRINE E. WRIGHT, AND ABIGAIL REESE
62 Community-Based Participatory Research for Health
to ignore the importance of trust, yet the trust development process in research partnerships is
often not a conscious process and is assumed to be present or absent.
The majority of trust and CBPR literature conceptualizes trust as an outcome and acknowl-
edges that research on trust development is lacking. Although numerous CBPR scholars have dis-
cussed the importance of trust and offer anecdotal suggestions, very few systematically research
it. CBPR scholars often report the presence of trust as personal attributes of the researcher,
such as authenticity, action, listening, commitment, recognizing the expertise of community,
voicing expectations, taking a facilitator role as opposed to a director role, and getting to know
the community (Christopher, Watts, McCormick, & Young,2008; Hora, Prochaska, Bolin, &
Ory,2007; Jones et al.,2008). However, time is the variable necessary for the community to
decide whether the demonstrations of trust-building personal attributes are genuine.
CBPR and trust literature suggests that a process of trust development begins with demon-
strating trust-building behaviors and ends with sustaining trust. However, this process of trust
development lacks empirical support. Trust development in early CBPR literature was assumed
and reported from perceptions of the academic partners, an age-old criticism (Molyneux, Peshu,
& Marsh,2005). However, in recent years community voices have begun to be represented
more in efforts such as the journal Progress in Community Health Partnerships. To bridge the
gap, the CBPR literature needs to represent all partner voices.
Another limitation of trust research is that trust is often investigated and measured as a
binary variable despite the documentation of several observed trust types (Connell & Man-
nion,2006; Lucero & Wallerstein,2013). The conceptualization of trust as present or absent
limits the understanding of trust as a complex, dynamic, and multidimensional construct.
A binary conceptualization also keeps key components hidden, including individual and
systematic factors, of trust maintenance as well as trust functioning in the phases of partner-
ship and research processes. In one study of CBPR that looked across the research spectrum,
trust was identied as a critical element within all phases of research, not just in partnership
development (Belone et al.,2016). The eld will benet from the integration of trust types, a
missing component of current models.
The extant CBPR literature has yet to document the process of trust development, leaving
it under-theorized. Organizational communication and behavior literature is useful in theorizing
the components involved in trust development, because CBPR partnerships are composed of
two or more organizations working to achieve a common goal. This chapter presents a trust
typology as an alternative to binary distinctions of trust in CBPR. The typology is discussed
and qualitative and quantitative data are presented from data collected during two different but
related projects to support the existence of these types in practice. Although the focus of this
chapter is at the partnership level, the typology can also be used to inform partnerships about
the level of trust between the partnership and the community.
STUDY BACKGROUND
From 2006–2008, supplemental funding was secured from the National Center for Minority
Health and Health Disparities through the Native American Research Centers for Health mech-
anism to understand what constructs matter most to CBPR partnerships and outcomes (Waller-
stein et al.,2008). The product of the pilot grant was a CBPR conceptual model. Through a
Trust Development in CBPR Partnerships 63
literature review, web-based survey, and a series of community consultations, historical mistrust
and trust-mistrust between a community and a specic research team was highly ranked by par-
ticipants as important elements for the success of CBPR projects (Belone et al.,2016). During
the community consultations, participants stated that trust resides throughout the process of
CBPR and is not isolated from historical mistrust as a contextual factor (Belone et al.,2016).
As a result, the development of a trust typology ensued (see Lucero,2013, for more detail). In
the development of this trust development framework, the need to support the product with evi-
dence was imminent.
First, qualitative support was provided by data collected during the community consultation
focus groups that preceded the Research for Improved Health (RIH) study to illustrate the trust
types that exist in practice. A brief discussion of the community consultation process and data
generation is described here because it is not presented elsewhere in the book. The quantitative
measurement of the trust typology was done with data from the RIH study (see Chapters6
and17). Results from the RIH survey illustrate how to measure trust types.
This iteration of the typology includes six types that were validated by community experi-
ences and supported within interorganizational literature (Table5.1). It is important to under-
stand that this typology should not be interpreted as being anchored at opposite poles. The
authors do not assume that partnerships begin in trust decit. Rather, a partnership can start
and move between trust types. For each project, a required or ideal type of trust will need to be
determined by partnership members (Wicks, Berman, & Jones,1999).
TRUST TYPOLOGY: SUPPORT FOR A DEVELOPMENTAL FRAMEWORK
Several iterations of the trust typology were developed. The version presented here proved
salient as evidenced by the following section.
TABLE 5.1 Trust Typology Model with Characteristics
Trust Types Characteristics
Critical-reective trust Trust is at the place where mistakes and other issues resulting from
differences can be talked about and resolved.
Proxy trust Partners are trusted because someone who is trusted invited them.
Functional trust Partners are working together for a specic purpose and time frame,
but mistrust may still be present.
Neutral trust Partners are still getting to know each other; there is neither trust
nor mistrust.
Role-based trust Trust is based on a member’s title or role with limited or no direct
interaction.
Trust decit (suspicion) Partnership members do not trust each other.
64 Community-Based Participatory Research for Health
Community Consultation
In 2009, six focus groups were conducted with American Indian, African American, Chinese
origin, Puerto Rican, Mexican, and a few white community members to review and revise
the CBPR conceptual model (full details are found in Belone et al.,2016). The focus group
method was used to fulll two aims: (1) seek face validity of the model and (2) determine if
the model could be used for self-reection and diagnosis. Partnerships were asked to “think
about the major drivers and barriers to authentic participation in the CBPR project” and to
reect on “which issues [outlined in the model] matter the most to your partnership now?” Each
discussion ended by asking partnerships to determine what they needed to strengthen their part-
nership or provide advice on best practices. In each focus group, trust was identied as a key
issue. For this reason and with permission of the principal investigator, these focus group data
were used for secondary analysis to answer the question of which trust types exist in practice.
Secondary analysis of qualitative data is useful when investigating sensitive topics in elusive
populations (Long-Sutehall, Sque, & Addington-Hall,2010). A synthesized matrix and reports
on validated, expanded, and new constructs from six community consultations were reviewed,
analyzed, and reported next. Each type of trust is presented with exemplar quotes from the
community consultations.
Partnerships in critical reective (CR) trust are characterized as having open communica-
tion. Mistakes and other issues resulting from differences can be discussed and resolved. CR
trust is similar to Rousseau, Sitkin, Burt, and Camerer’s (1998) relational trust. Relational trust
develops over time and through repeated interactions. Repeated interactions provide evidence
of reliability and dependability of partners and give rise to positive expectations. Interdepen-
dence between partners increases over time as new opportunities and initiatives are pursued. As
one community partner stated,
If there wasn’t the kind of trust and collaboration that was there before, I think this would have
been an even more challenging process. I think because of the relationships it just helps to know
that we’re all doing our best to try and make this work part of trust is knowing that you’re
aware, that you’re mindful of other people’s capacity.
CR trust contains aspects of identication-based trust (Lewicki & Bunker, 1995) and
cognitive-based trust (McAllister, 1995). Identication-based trust requires values and goals
to be shared by partners, and cognitive-based trust is an individual’s beliefs about another per-
son’s reliability, dependability, and competence. Further, the notion of citizenship behaviors in
organizations, or going above and beyond to help team members and the team to be successful,
is central to critical reective trust. These relationships share ethical values and interpersonal
relationships. The importance of this aspect of critical reective trust was demonstrated in the
course of the community consultations:
So, you know, that’s that trust factor, and that’s also that bond, or being able to recognize that
we at some point in time might mess up in an area, you know; that we can trust each other that
you’re not saying this to hurt me but to help me grow who I am, you know, things like that.
As with any trust type, the potential for growth or deterioration exists. In CR, trust part-
nership nurturing is ongoing and small mistakes do not critically affect the partnership. In sum,
Trust Development in CBPR Partnerships 65
critical reective trust is thought to develop over time, with ongoing interactions with reliable
behavior and demonstrated care and concern for partners, community, and health issues. The
centrality of respect and safety to group dynamics was referenced repeatedly by community
partners: “our relationship, it’s created a safety net where we feel free as individuals to be able
to do the work that needs to be done in order to meet our goals. But if for some reason we mess
up, there’s a net there.”
Proxy trust occurs in partnerships when members are trusted because someone who is
trusted invited them. This is similar to giving an unfamiliar person the “benet of the doubt” for
a period of time. This can occur in a negative space as well and is called proxy mistrust. Early
knowledge about partners or knowledge about a partner’s reputation is thought to affect trust in
small group teams (McKnight, Cummings, & Chervany,1998). Knowledge about team mem-
bers can arise from prior personal experience working together or from others’ prior experience
with team members. Race, ethnicity, and cultural background of team members can inuence
proxy trust by inuencing the trust that community members have in the research team. For
example, having partners who mirror community characteristics can increase the community’s
trust in the research team.
One time when we were doing surveys in the East Side Detroit and wanted to hire some kind of
temp agency in Ann Arbor with these young students to come down to the East Side of Detroit
to knock on folks doors and do surveys. And none of the young people look like the people
on the East Side of Detroit and I was trying to explain that folks aren’t even gonna open the
door. They are going to look out the window and say, “I’m not opening the door.” So, in fact,
what they did was hire and train residents from the East Side to actually implement the surveys
which really turned out great. To add to that, it really should be a reection on...a mirror of
the community that’s involved.
Webber (2008) found prior experiences to be positively associated with early development
of trust in a team environment, but this association did not predict trust at later stages of team
functioning, suggesting that proxy or familiarity with team members offers a probationary
period that must be maintained through positive interactions and resolution of key issues. Proxy
trust also has added benets for the partnership, such as decreasing the time factor (assuming
the relationships continue to establish trust). For example:
I would certainly say that the fact that [research partner], you had this long-standing relation-
ship with an organization that you actually helped found and the fact that you previously had
worked with [research partner] and there were all these relationships between various partners
that were very strong. There was a lot of trust going and I think we saved a lot of time.
Functional trust occurs when members of a partnership are working together for a specic
function and time frame. Panteli and Sockalingam (2005) call this type co-alliance trust, which
results when organizations make equal contributions of resources, competencies, and knowledge
for specic projects and time frames. Additionally, Shapiro (1987) and Sitkin and Roth (1993)
conceptualize a type of trust based on formal legal agreements, formal rules, and memoranda
of agreement. Formal agreements can diminish mistrust by explicating roles and respon-
sibilities, expectations, and decision-making processes. Ground rules and agreements were
identied as a priority by a community partner, “When we were writing renewal, weeducated
66 Community-Based Participatory Research for Health
our brand-new community advisory committee; we went over principles of CBPR and laid a
foundation right there, and I had pushed very hard for that.”
Aspects of knowledge-based trust (KBT) (Lewicki & Bunker, 1995) also t within
functional trust. In KBT, partners possess enough knowledge to understand and predict behavior
partly because of the “t” of partners. Functional trust depends on the function of the partner-
ship. Therefore, functional trust is task and time dependent; based on equitable contributions of
resources, competencies, and knowledge; may include formal arrangements; and partners pos-
sess enough knowledge of each other to predict behavior and commitment.
Neutral trust means partners are still getting to know each other; neither trust nor mistrust
exists at this point. In this stage, individuals rely on the purpose or task of the relationship to
buttress interpersonal trust. Neutral trust resembles swift trust, a type of trust that needs to form
very quickly to make progress (Meyerson, Weick, & Kramer,1996). Swift trust is time, task,
and goal dependent and is driven more by contextual cues, such as economics, than by interper-
sonal relations. Neutral trust, similar to swift trust, is fragile because situations requiring quick
decisions about trust without the ability to weigh the risks might be more prone to conict than
relationships that grow together and develop shared goals and values along the way. The estab-
lishment of a successful partnership depends on the ability to sustain trust between partners past
the initial development of trust. One community member explained the importance of contex-
tual factors and the continual development of trust:
I think one of the things that actually [member] said at one point was the difference of working
with someone [at university] and here; that cultural factor piece was that you really need to
spend the time to get to know people before you can start doing the work, doing the tasks, and
I think that is an important contextual factor, that culture. How things operate in your experi-
ence versus someone else needs to be thought about because you might never feel the move
from point A to point B because what someone needs from their experience is to get to know
you rst, or vice versa, and I think that affects those group dynamics, and we don’t talk about
that much, but I think it’s important.
Once tasks are complete, individuals or organizations will evaluate the relationships and
determine whether they dissolve or continue their relationships based on needs of their orga-
nization or community. The following quote illustrates the decision making that community
members undertake to determine whether it makes sense to continue with a partnership:
We demand a certain level not only of respect but time and resources that sometimes people
aren’t prepared to give. You know they come in thinking well we could do this thing and you
end up putting more time into it and you nd that it’s like a job. So in some ways we demand
a lot. So that’s another aspect of partnerships is that we will tend to work towards groups or
organizations that are willing to invest the time that we’re willing to invest into a project. If we
see that a group is laissez-faire with our relationship then we’ll evaluate that partnership and
see if it’s useful to have that.
Role-based trust is based on the titles or roles of members with limited or no direct inter-
action prior to the relationship. Presumptive trust (Webb,1996), or role-based trust, suggested
that people who function in certain roles—a physician for example—are trained to have patients’
best interest in mind thereby reducing uncertainty even if other trust-building characteristics
Trust Development in CBPR Partnerships 67
are missing. Role-based trust can be quite fragile and produce failures in cooperation and
coordination because trust based on roles is short term and requires reinforcement through
meeting established expectations. One community partner lamented the lack of follow-through
from a group of researchers granted role-based trust:
Like the last group that came from the university to collect data, I was making sure they were
going to do what they said they were going to do. I invited them to sit with the community
and the community leaders, let everyone know that they were collecting data. They even came
back and spoke after collecting their data and made all these promises [they didn’t keep]; and
that was it. I think following through is very important, is very key for staying in the trust of the
community.
Because of the historical experience of research in marginalized communities, it has been
assumed that trust based on the position a person holds is equivalent to no trust during rela-
tionship development. In fact, our community consultations indicate that suspicion toward the
researchers is more likely to be present: “Often, they [researchers] just assume that we don’t
have an agenda, that we do not have the plan, that we do not lead our own lives, that we do not
have a plan for our future, and so they just push their own agenda.”
Trust decit (suspicion) means partnership members do not trust each other because of
historical relationships or conduct. It is likely that trust will not develop between partners. One
community member reected on the community’s historical mistrust with research partners:
“Someone is always testing us for something. Let’s not let the community feel like they are
just guinea pigs again and when it’s over with its smoke and mirrors again.” Deutsch (1958)
introduced suspicion as an expectation of a malevolent event; this personality trait is a result of
personal and observed experience. The trust decit type is the most sensitive to the disposition
of the actors and the trust situation. Trust disposition is based on early trust-related experiences
and eventually becomes a stable personality characteristic (Hardin,1996; Rotter,1971,1980).
The implication of suspicion as a personality trait is that individuals with a pessimistic disposi-
tion toward trust will demonstrate lower levels of trust on initial contact. The historical context
contributes to past experiences and colors trust decit. Focus group members identied the
actions of outsiders and the omission of results to the community as a reason for historical mis-
trust (Belone et al.,2016).
I believe that in the past we have seen so many other org[anizations] and different people com-
ing here to do different things, and it didn’t happen. It didn’t happen, or they would use the
information they got from this area and do whatever they were gonna do with it, and we never
got back the results from whatever they were doing. So some of it may have been mistrust...I
believe some of it, not a lot of it, but some of it may be mistrust.
That’s where I thought that the trust and the mistrust had to be addressed because a lot
of times when you walk into a community if you’re from the outside there is no openness until
they can trust you and so take the time on group dynamics and get to know people and that
equates to developing trust.
Data from the community consultation focus groups provided ample support for the six trust
types. More data was found for critical reective, proxy trust, and trust decit. Less support was

68 Community-Based Participatory Research for Health
available for functional, role-based, and neutral trust, but data still supported praxis, the interac-
tive understanding of the theory and practice of trust as a dynamic concept, that can change over
time. The next step was the quantitative measurement of the trust typology in the RIH study.
Research for Improved Health (RIH)
RIH was a mixed methods study that included a key informant and community engagement (CE)
web-based surveys (Lucero et al.,2016; see Chapters6 and17 for details). As the trust typology
provides a new view on trust, the social trust scale was used to establish construct validity. This
scale is four-item forced-choice measure designed to assess the general condence that one
has in the integrity, ability, and character of others (Figueroa, Kincaid, Rani, & Lewis,2002).
Higher scores on a ve-point Likert scale indicate higher levels of trust. The means plot in
Figure5.1 reveals higher scores for the social trust scale and corresponds with critical reective
trust. Similarly low scores on the social trust scale correspond with suspicion. This provides
some validity for the trust typology measure.
As agreement between the two scales existed, a measure was created to operationalize the
trust typology. The trust typology resulted in a three-item forced-choice measure designed to
assess the change of trust types over time. The measure asked about level of trust at the beginning
Suspicion
3.60
3.80
4.00
Mean of level of trust among team members
4.20
4.40
4.60
Functional Proxy
Current trust fewer categories
Critical Reflective
FIGURE 5.1 Means Plot of Social Trust and Trust Types
Trust Development in CBPR Partnerships 69
of the partnership, level currently, and level desired for the future, using a category scale with
responses ranging from critical reexive trust to no trust (see Table5.1). The majority of survey
participants reported critical reective trust in partnerships at the time they responded to the
RIH questionnaire. To have enough data in each cell for analysis, the types suggestive of less
trust were combined to create a four-level typology: critical reective trust (n = 296), proxy trust
(n = 56), functional trust (n = 64), and suspicion (n = 16). Conceptually this categorization makes
sense because the types of no trust, proxy mistrust, unearned trust, and neutral trust all suggest
suspicion. These results were reported elsewhere; see Lucero et al. (2016) for more information.
CONCLUSION
Investigating and measuring trust as a binary variable is a limitation of trust research, because
scholars have documented several types of observed trust (Connell & Mannion,2006; McKnight
& Chervany,2006). The conceptualization of trust as present or absent limits the understanding
of trust as a complex and multidimensional construct. This chapter presents a trust typology as
an alternative measure. As it stands, the use of the typology at the different time periods enables
partners to reect on trust over time rather than assuming it has been present or absent. In the
quantitative data, participants reported movement in trust levels over time. This reinforces the
assertion of trust being a process and not just an outcome. The typology can assist partners in
determining the different types of trust present within the partnership (e.g., community at proxy
and researchers at critical reective). It can be used as a reection tool, and can help partnership
members address divergent perspectives and attempt to resolve differences.
Although innovative, typologies are problematic in research because signicant variation
and overlap exist within each category, making it extremely difcult to use a typology as a
dependent variable. However, the typology is useful in organizing theory as part of exploratory
research. The next step in trust development theory is to develop a new measure using trust
types as latent variables. A new measure should include the totality of the trust environment
using a systems perspective. The vision for the new instrument is for partnerships to implement
it at multiple time points to determine the type they are functioning within and determine if that
is where the members want to be. If not, members need to decide what kind of trust they want
to achieve and what they need to get there. Evidence from the community consultations that led
to the development of this trust typology indicates that the goal of partners regarding trust is an
environment in which partners share similar goals, feel that safety outweighs risks, and mem-
bers are responsible for the partnership. Once the partnership achieves an appropriate level or
type of trust, energy reserved for conict mediation can be redirected into the research project
and health outcomes.
QUESTIONS FOR DISCUSSION
1. Reect on partnerships you know or have participated in. How has trust in these partner-
ships changed over time? In what ways did they trust, and where are they now?
2. If you are seeking to strengthen trust in a partnership, what strategies could you imagine
would be helpful?
70 Community-Based Participatory Research for Health
REFERENCES
Belone, L., Lucero, J. E., Duran, B., Tafoya, G., Baker, E. A., Chan, D., Chang, C., Greene-Moton, E., Kelley, M. A., &
Wallerstein, N. (2016). Community-based participatory research conceptual model: Community partner consultation and
face validity. Qualitative Health Research, 26(1), 117–135. doi:10.1177/1049732314557084
Chavez, V., Duran, B., Baker, Q. E., Avila, M. M., & Wallerstein, N. (2008). The dance of race and privilege in community-
based participatory research. In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health:
From process to outcomes (2nd ed., pp. 91–106). San Francisco, CA: Jossey-Bass.
Christopher, S., Watts, V., McCormick, A., & Young, S. (2008). Building and maintaining trust in a community-based partic-
ipatory research partnership. American Journal of Public Health, 98(8), 1398–1406.
Cochran, P.A.L., Marshall, C. A., Garcia-Downing, C., Kendall, E., Cook, D., McCubbin, L., & Gover, R.M.S. (2008). Indig-
enous ways of knowing: Implications for participatory research and community. American Journal of Public Health,
98(1), 22–27.
Connell, N. A. D., & Mannion, R. (2006). Conceptualisations of trust in the organisational literature: Some indicators from a
complementary perspective. Journal of Health Organization and Management, 20(5), 417–433.
Cook, B. D., & Jackson, T. R. (2012). Eighty years of bad blood: The evolution of human research after the Tuskegee Study.
Journal of Healthcare, Science, and Humanities, 2(2), 31–58.
Deutsch, M. (1958). Trust and suspicion. Journal of Conict Resolution, 2(4), 265–279.
Freeman, E. R., Brugge, D., Bennett-Bradley, W. M., Levy, J. I., & Carrasco, E. (2006). Challenges of conducting
community-based participatory research in Boston’s neighborhoods to reduce disparities in asthma. Journal of Urban
Health, 4(6), 1013–1021.
Figueroa, M. E., Kincaid, D. L., Rani, M., & Lewis, G. (2002). Communication for social change: An integrated model for
measuring the process and its outcomes. (The Communication for Social Change Working Paper Series, No.1). New York:
The Rockefeller Foundation.
Hardin, R. (1996). Trustworthiness. Ethics, 107(1), 26–42.
Hora, K. L., Prochaska, J. D., Bolin, J. N., & Ory, M. G. (2007). Lessons learned utilizing the CBPR model to address disease
management guidelines in rural communities. Texas Public Health Journal, 59(2), 17–21.
Jones, K. M., Gray, A. H., Paleo, J., Branden, C. J., & Lesser, J. (2008). Community and scholars unifying for recovery. Issues
in Mental Health Nursing, 29(5), 495–503.
Lewicki, R. J., & Bunker, B. B. (1995). Developing and maintaining trust in work relationships. In R. M. Kramer & T. R.
Tyler (Eds.), Trust in organizations: Frontiers of theory and research (pp. 114–139). Thousand Oaks, CA: Sage.
Long-Sutehall, T., Sque, M., & Addington-Hall, J. (2010). Secondary analysis of qualitative data: A valuable method for
exploring sensitive issues with an elusive population? Journal of Research in Nursing, 16(4), 335–344. Retrieved Febru-
ary 10, 2017, from www.wlv.ac.uk/pdf/Secondary%20analysis%20JRN3815531.pdf
Lucero, J., Wallerstein, N., Duran, B., Alegria, M., Greene-Moton, E., Israel, B., Kastelic, S., Magarati, M., Oetzel, J., Pear-
son, C., Schulz, A., Villegas, M., & White Hat, E. (2016). Development of a mixed methods investigation of process and
outcomes of community-based participatory research. Journal of Mixed Methods. doi:10.1177/1558689816633309
Lucero, J. E. (2013). Trust as an ethical construct in community-based participatory research partnerships (published doc-
toral dissertation). Albuquerque, NM: University of New Mexico.
Lucero, J. E., & Wallerstein, N. (2013). Trust in community-academic research partnerships: Increasing the consciousness
of conict and trust development. In J. Oetzel & S. Ting-Toomey (Eds.), Sage handbook of conict communication: Inte-
grating theory, research, and practice (2nd ed.). Thousand Oaks, CA: Sage.
McAllister, D. J. (1995). Affect- and cognitive-based trust as foundations for interpersonal cooperation in organizations.
Academy of Management Journal, 38(1), 24–59.
McKnight, D. H., & Chervany, N. L. (2006). Reections on an initial trust-building model. In R. Bachmann & A. Zaheer
(Eds.), Handbook of trust research (pp. 29–51). Cheltenham, UK: Edward Elgar Publishing.
McKnight, D. H., Cummings, L. L., & Chervany, N. L. (1998). Initial trust formation in new organizational relationships.
Academy of Management Review, 23(3), 473–490. doi:10.5465/AMR.1998.926622
Meyerson, D., Weick, K., & Kramer, R. M. (1996). Swift trust and temporary groups. In R. M. Kramer & T. R. Tyler (Eds.),
Trust in organizations: Frontiers of theory and research (pp. 166–195). Thousand Oaks, CA: Sage.
Trust Development in CBPR Partnerships 71
Molyneux, C., Peshu, N., & Marsh, K. (2005). Trust and informed consent: Insights from community members on the Kenyan
coast. Social Science and Medicine, 67(7), 1463–1473.
Panteli, N., & Sockalingam, S. (2005). Trust and conict within virtual interorganizational alliances: A framework for facili-
tating knowledge sharing. Decision Support Systems, 39(4), 599–617.
Pondy, L. R. (1992). Conict and negotiation in organizations: Historical and contemporary perspectives. Journal of Organi-
zational Behavior, 13(3), 257–261.
Rotter, J. B. (1971). Generalized expectancies for interpersonal trust. American Psychologist, 26(5), 443–452.
Rotter, J. B. (1980). Interpersonal trust, trustworthiness, and gullibility. American Psychologist, 35(1), 1–7.
Rousseau, D. M., Sitkin, S. B., Burt, R. S., & Camerer, C. (1998). Not so different after all. A cross discipline view of trust.
Academy of Management Review, 23(3), 393–404.
Shapiro, S. P. (1987). The social control of impersonal trust. American Journal of Sociology, 93(3), 623–658.
Sitkin, S. B., & Roth, N. L. (1993). Explaining the limited effectiveness of legalistic “remedies” for trust/distrust. Organiza-
tion Science, 4(3), 367–392.
Wallerstein, N., Oetzel, J., Duran, B., Tafoya, G., Belone, L., & Rae, R. (2008). CBPR: What predicts outcomes? In M. Min-
kler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes (2nd ed.).
San Francisco, CA: Jossey-Bass.
Webb, G. (1996). Trust and crises. In R. M. Kramer & T. R. Tyler (Eds.), Trust in organizations (pp. 288–302). Thousand
Oaks, CA: Sage.
Webber, S. S. (2008). Development of cognitive and affective trust in teams: A longitudinal study. Small Group Research,
39(6), 746–769. doi:10.1177/1046496408323569
Wicks, A. C., Berman, S. J., & Jones, T. M. (1999). The structure of optimal trust: Moral and strategic implications. Academy
of Management Review, 24(1), 99–116.

3
PART
CBPR CONCEPTUAL
MODEL: CONTEXT
AND PROMISING
RELATIONSHIP PRACTICES
One of the most studied features of CBPR is partnership processes or dynamics. Numerous studies
have examined the key elements of what makes a high-functioning partnership. The argument
(with growing evidence to this effect) is that if partnering practices are effective, then inter-
vention and research design will reflect mutual learning and partner synergy, or ability to work
together effectively. These dynamics and the research or intervention then also have a positive
impact on system, capacity, and health outcomes (see Chapters6 and17 along with Appendix 6).
74 Part 3
Partnership processes are the means of structuring the work and interacting among part-
ners and include three elements. First, individual characteristics (e.g., displaying cultural humility
and being bridges among different groups) shape the interactions. Second, structures of the
partnership include formal agreements, sharing of resources, and alignment with CBPR princi-
ples. Third, relationships, or how partners interact with one another, including features such as
participatory decision making, trust, dialogue, and influence.
However, partnership processes do not operate in a vacuum and thus CBPR models, the-
ories, and practice need to account for context. The emphasis on context is one of the hallmarks
of CBPR. Context includes local and larger politics and policy trends, socio-economic-cultural
characteristics, historical collaborations of trust-mistrust, university and community capacities
and readiness, and the importance of health issues being researched. Contextual factors pro-
vide a backdrop for influence on partnership processes, that is, on partnership structures and
members and on relationships, including how they are managed and strengthened.
The chapters in this section all consider the role of context for shaping partnership
processes and the importance of seeking equitable group dynamics practices for sustainability
of a successful partnership. In Chapter6, Sarah L. Kastelic, Nina Wallerstein, Bonnie Duran, and
John G. Oetzel introduce the history of the Research for Improved Health (RIH) study and the
development of the CBPR conceptual model that is used to organize this book. Further, this
chapter provides an overview of the RIH research design of mixed qualitative and quantitative
methods, the data collection of a multilevel survey and in-depth case studies, and integration
of quantitative and qualitative data analyses. Although the CBPR model has been further devel-
oped and refined, the authors argue that the model is a dynamic tool that should be adapted
by local partnerships and used creatively.
In Chapter7, Emily J. Ozer and Amber Akemi Piatt provide an overview of youth-led par-
ticipatory action research (YPAR), discussing key contexts for youth research processes, identi-
fying relevant curricular resources, and highlighting potential dilemmas and choice points in
engaging in YPAR. They provide illustrative examples from the United States and other country
contexts such as Guatemala, Brazil, Portugal, and Australia. The authors consider the value of
YPAR for promoting equity and positive development, particularly for the majority of young
people in the world who must negotiate racism, economic inequalities, violence, and other
threats to healthy development. YPAR engages young people’s expertise in scientific inquiry
Part 3
75
about youth development and health. Finally, they consider the challenge of “scaling” YPAR
and related participatory approaches into broader systems change efforts and initiatives, capi-
talizing on social media and web-based platforms while maintaining the integrity and spirit of
the approach.
In Chapter 8, Eugenia Eng and colleagues present a case study grounded in the history
and context of racism, particularly institutional racism. Today’s effects from institutional rac-
ism are subtle and require careful and authentic identification and recognition. This chapter
describes how the Greensboro Health Disparities Collaborative applied antiracism principles to
an NIH-funded CBPR project designed to test a system change intervention to enhance race-
specific equity in quality and completion of cancer care at two cancer centers in Greensboro,
North Carolina, and Pittsburgh, Pennsylvania. The authors present four intervention compo-
nents to address the context of transparency and accountability for racial equity, including
staff equity trainings, an analysis of patient interviews of their experiences with the power and
authority in the system, nurse navigators, and real-time physician champions. Initial findings
from integrating a CBPR approach with antiracism principles indicate benefits of this collabora-
tive approach.
In Chapter9, Magdalena Ávila, Shannon Sanchez-Youngman, Michael Muhammad, Lauro
Silva, and Paula Domingo de Garcia introduce a CBPR case on environmental justice in the South
Valley of Albuquerque, New Mexico. This chapter examines context and the promises and pit-
falls of their policy partnership through a lay health worker (promotora) intervention to address
policy targets. The South Valley Partners for Environmental Justice were able to achieve some
of their key goals over their ten-year partnership, including the training and empowering of a
cadre of community researchers. However, the case also illustrates the impacts of context and
partnering processes when there is misalignment among community members and academic
researchers. More specifically, the case reveals how conflicting ways of knowing and divergent
social justice tactics contributed tensions that eroded trust among the partners. Additional chal-
lenges included the historical context and inhospitable policy environment that further contrib-
uted to misalignment in dynamics.

6
CHAPTER
SOCIO-ECOLOGIC
FRAMEWORK FOR CBPR
DEVELOPMENT AND TESTING OF A MODEL
SARAH L. KASTELIC, NINA WALLERSTEIN, BONNIE DURAN,
AND JOHN G. OETZEL
THE SIGNIFICANCE OF stakeholder knowledge and participation in research addressing
complex health problems has grown exponentially (Barkin, Schlundt, & Smith,2013) and is
reected in multiple national NIH and CDC initiatives (Ahmed & Palermo,2010; Greenlund &
Giles,2012; Selby, Beal, & Frank,2012) in the United States. Additionally, the Patient Protec-
tion and Affordable Care Act’s focus on eliminating disparities relies on community-engaged
research (CEnR), including engagement of patient stakeholders, to align academic health cen-
ters with community priorities. Multidirectional learning is especially important for research
projects among disenfranchised and hard-to-reach populations and academic institutions with
insidious traditions of knowledge asymmetry (Michener et al.,2012). Internationally, there has
been a concurrent growing interest in public participation in government-funded health research
through engagement of service users and nonprofessionals as a strategy for democratization of
knowledge and to address health inequities. (For more historical and theoretical background on
CBPR and CEnR, see Chapter2.)
The move toward wider use of CBPR and CEnR approaches is also motivated by protests
from, and lack of research participation by, groups historically ignored or subject to unethical
and biased research questions and methods (Duran & Duran,1995; Tuhiwai Smith,1999). CBPR
78 Community-Based Participatory Research for Health
efforts with historically marginalized groups are commonly aimed at “decolonizing” essentialist
narratives (racial, cultural, gender, etc.) created by “scientic” discourse that serves, in part, as the
philosophical and moral grounds for the colonization and stratication of the global enterprise to
this day. CBPR prevents ongoing abuses by prioritizing community-dened research questions,
ensuring community-level benet, and promoting knowledge democracy that privileges well-
established community-derived theories of etiology and change (Hicks etal.,2012; Trickett,2011).
An important contribution to illustrating the legitimacy and value of CBPR was the
development of a conceptual model to serve as a guide for elucidating potential pathways of
partnering practices to outcome and capture barriers and promoters of effective CBPR partner-
ships. Model development was the starting point of a three-stage federally funded research pro-
cess to support the study of the art and science of community-academic research partnerships:
(1) creation of the model (2006–2009), (2) rst national testing of measures of the model (2009–
2013), and (3) renement of measures (including translation into Spanish) and intervention study
(2015–2020). This chapter summarizes this iterative development and expanded use of the model
in the United States and internationally. Based on the rst national testing of the model, we also
offer analyses of potential pathways of promising practices contributing to outcomes. Chapter17
provides complementary information on using the CBPR conceptual model for evaluation, on
measures and metrics to assess constructs within the model (see also Appendix 10), and on
empirical data assessing relationships among partnership practices and outcomes.
STAGE ONE: CREATING THE MODEL
In 2006, believing in CBPR as a methodology to promote community wisdom in health research,
Nina Wallerstein from the University of New Mexico Center for Participatory Research (UNM
CPR) and Bonnie Duran from the University of Washington Indigenous Wellness Research
Institute (UW IWRI) started, with pilot funding from the National Institute of Minority Health
and Health Disparities (NIMHD), to create an overarching research design to study CBPR.
Throughout this pilot and into the next stages, we convened and were guided by a “think tank”
of community and academic CBPR practitioners providing expert consultation throughout the
project. Face-to-face meetings, when possible, were supplemented by conference calls and
guidance by subcommittees.
Using multiple data collection methodologies, we rst conducted an interdisciplinary
review of academic literature, building on search terms from the rst Agency for Health Care
Research and Quality review of CBPR (Viswanathan et al.,2004) about community participa-
tion, engagement, and collaborative forms of inquiry and partnership. Literature was reviewed
from disciplines as varied as ethnic and Indigenous studies, business administration, commu-
nication, education, as well as the social sciences, law, public health, and other biomedical and
nursing sciences. Results identied evaluations primarily of CBPR principles and processes, and
coalition, organizational, and group dynamic measures. An earlier model provided important
concepts and constructs (Schulz, Israel, & Lantz,2003), but there was little research on associ-
ations of practices with outcomes (summarized in Wallerstein et al.,2008). From 2002 to 2008,
258 articles were identied in a review of the CBPR (and related) literature. Forty-six instru-
ments, including 224 individual measures of characteristics in the CBPR conceptual model,
were reviewed, and reliability and validity were assessed if possible (Sandoval et al.,2012).
Socio-Ecologic Framework for CBPR 79
The research team then conducted an Internet survey of more than one hundred CBPR projects,
collecting data about the resonance of the partnering and outcome constructs identied through
the literature review and think tank guidance. This preliminary investigation resulted in the
rst iteration of the CBPR conceptual model, which was further validated through qualitative
community consultation with six partnerships (Belone et al.,2016).
In creating the conceptual model, we wanted to explicate the specic domains, such as
contexts, partnership characteristics and processes, that contribute to research and interven-
tion designs and that ultimately inuence outcomes of CBPR. By denition and through guid-
ing principles (Israel, Eng, Schulz, & Parker,2013; Minkler & Wallerstein,2008), effective,
authentic CBPR requires local identication of health problems and builds on community con-
texts, including local strengths and resources, to participate in the project and address health
inequities. The CBPR model adopted this transformational framework to showcase how part-
nering practices could have a broad range of outcomes, from increased synergy as a short-term
output; to intermediate-level policy, system, and capacity changes; to more long-term opportu-
nities for social justice, equity, and health outcomes.
We also saw the model as embedding a theory of change from Paulo Freire’s educational
pedagogy of conscientization and praxis: an ongoing cycle of partners listening and engaging in
dialogue with each other, making decisions and choosing actions as a result of their dialogues,
reecting on those actions, and then continuing with another cycle of listening, dialogue, action,
and reection (Freire,1970,1982; Wallerstein & Auerbach,2004). Thus, the conceptual model
was created to facilitate CBPR partnerships’ ability to put their partnership in a framework that
supports ongoing collective reection and evaluation for strengthening the quality and effec-
tiveness of their partnership to reach desired outcomes.
The model was intentionally created as a dynamic tool that has changed over time as research
identies other factors that promote or inhibit effective, authentic CBPR; and understanding of
how domains and variables may interact deepens and becomes more nuanced. Even with the rst
iteration of the model, we saw the model as a framework to be adapted by partnerships in ways
that most closely reect each project’s and partnership’s goals. The intention was never to offer
the singular, authoritative view on community-academic partnership characteristics, processes,
and outcomes, that is, to become the “CBPR police,” determining who is “doing CBPR right.”
Rather, we sought to offer through literature, data from the eld, and ongoing expert consulta-
tion the best available thinking about contexts, partnering processes, interventions and research,
and outcomes. Undoubtedly the hundreds of community-academic research partnerships in the
United States (let alone throughout the world) have varying contexts, dynamics, health inter-
ventions or programs, research designs and outcomes, and priorities. In fact, the most salient
question continues to be, under what conditions or contexts are which engagement and partner-
ing practices the most effective to contribute to research and intervention design and to best
affect a wide range of research, systems, capacity, and health and equity outcomes?
What follows is a conceptual model that seeks to be of use to community-academic part-
nerships and can be adjusted or customized in ways that emphasize any partnership’s realities
and goals (see Figure 6.1). Some model adaptations are presented here as well as in Chapter17.
Through multiple iterations and applications, the model continues to grow and be rened over
time. The domains and constructs of the 2017 version of the conceptual model are described in
the next sections (http://cpr.unm.edu/research-projects/cbpr-project/cbpr-model.html).

Partnership Structures:
• Diversity: Who is involved
• Complexity
• Formal Agreements
• Control of Resources
• % Dollars to Community
• CBPR Principles
• Partnership Values
• Bridging Social Capital
• Time in Partnership
• Social -Structural: Social-Economic
Status, Place, History, Environment,
Community Safety, Institutional
Racism, Culture
• Role of Education and Research
Institutions
• Political & Policy: National / Local
Governance / Stewardship
Approvals of Research; Policy &
Funding Trends
• Health Issue: Perceived Severity
• Collaboration: Historic Trust /
Mistrust between Partners
• Capacity: Community History of
Organizing/ Academic Capacity /
Partnership Capacity
Partnership ProcessesContexts OutcomesIntervention & Research
Relationships: How we interact
• Safety / Respect / Trust
• Influence / Voice
• Flexibility
• Dialogue and Listening / Mutual
Learning
• Conflict Management
• Leadership
• Self & Collective Reflection /
Reflexivity
• Resource Management
• Participatory Decision-Making
• Task Roles Recognized
Commitment to Culture-
Centeredness
Individual Characteristics:
• Motivation to Participate
• Cultural Identities/Humility
• Personal Beliefs/Values
• Spirituality
• Reputation of P.I.
• Processes that honor community
and cultural knowledge and voice,
fit local settings, and use both
academic & community language
lead to Culture-Centered
Interventions
• Empowering Co -Learning
Processes lead to Partnership
Synergy
• Community Members Involved in
Research Activities leads to
Research/Evaluation Design that
Reflects Community Priorities
• Bidirectional Translation,
Implementation & Dissemination
Intermediate System & Capacity Outcomes
• Policy Environment: University & Community
Changes
• Sustainable Partnerships and Projects
• Empowerment Multi-Level
•
Shared Power Relations in Research /
Knowledge Democracy
• Cultural Reinforcement / Revitalization
• Growth in Individual Partner & Agency Capacities
• Research Productivity: Research Outcomes, Papers,
Grant Applications & Awards
Long-Term Outcomes: Social Justice
• Community / Social Transformation: Policies &
Conditions
• Improved Health / Health Equity
Partnership
Structures
Relationships
Individual
Characteristics
Health Care
Agency
Government
Intervention
& Research
Outcomes
Long-term
Intermediate
• Policy Environment
•
Sustained Partnership
• Empowerment
• Equal Power Relations
in Research
• Cultural Reinforcement
• Individual / Agency
Capacity
• Research Productivity
Community
CBOs
Contexts
Capacity
&
Readiness
Collaboration
Trust &
Mistrust
Political
&
Policy
Social
&
Structural
• Community
Transformation
• Social Justice
• Health / Health Equity
Health
Issue
Importance
Funders
Integrate
Community
Knowledge
Culture-
Centered
Interventions
Empowering
Processes
Partnership
Synergy
Appropriate
Research
Design
Community
Involved in
Research
Academic
Partnership Processes
Processes
Outputs
Visual from amoshealth.org 2017
FIGURE 6.1 CBPR Conceptual Model
Source: Adapted from Wallerstein et al. (2008) and Wallerstein and Duran (2010, p. S1). Visual from
amoshealth.org (2016).
Socio-Ecologic Framework for CBPR 81
The conceptual model is organized into four overarching domains: contexts, partnership
processes, intervention and research, and outcomes. Although it may initially appear complex,
the basic domains of the model are straightforward. The model hypothesizes that the context of
any given community-academic partnership grounds the partnership processes, which include
individual characteristics, relationships, and partnership structures. In turn, the context and part-
nership processes, with community involvement in all research stages, can affect and alter the
“science” or the design of the research and health interventions. The implementation of research
methods and interventions then can affect intermediate system and capacity outcomes within
communities and academia as well as long-term changes in community health conditions and
health equity.
Within each domain, several predominant constructs have been identied. The relative
importance of the constructs may vary by partnership. In the context domain, ve constructs (see
Box6.1) follow a socio-ecologic framework commonly used in public health. Social- structural
and political factors are the highest level of social determinants, followed by organizational
capacities of academic and community institutions, which are followed by interpersonal collab-
oration and levels of trust and mistrust, and perceptions of importance of health issues.
To highlight just a few factors, the perceived importance of the health issue describes the
partners’ perceived severity of the health problem(s) and, relatedly, the urgency of the health
issue(s) being addressed by the partnership. The collaboration context accounts for the historic
trust or mistrust between the partners. The capacity and readiness context addresses multiple
capacities: the community’s history of organizing or prior research experience; the academic
institution’s capacity to engage with communities; and their mutual capacity to partner.
The partnership processes domain (see Box6.2) links the individual, interpersonal, and
organization levels of the socio-ecologic framework and consists specically of individual
characteristics, structural features, and relationships among the academic, community, agency,
health systems, and community-based organizations.
Among other things, the individual characteristics account for the core values, participa-
tion motivation, cultural identities and cultural humility (see Appendix 4), and personal belief
systems and spirituality of the individuals involved in the partnership. The structural features
account for the diversity of who is participating, as organizations or individuals; complexity of
kinds of stakeholders participating; formal agreements or lack thereof; as well as team members’
Box 6.1 Contexts
■ Social-structural: social-economic status, place, history, environment, community safety,
institutional racism, culture, role of education and research institutions
■ Political policy: national, local governance, stewardship, approvals of research, policy and
funding trends
■ Health issue: perceived severity by partners
■ Collaboration: historic trust-mistrust between partners
■ Capacity: community history of organizing, academic capacity, partnership capacity
82 Community-Based Participatory Research for Health
capacity to bridge across cultures and positions of power. The relationships between stakeholders
in partnership, or how the partnership interacts, include constructs such as safety, community
voice and inuence or lack thereof, dialogue and listening, self- and collective reexivity prac-
tices, use of participatory decision making, and task roles recognized.
Box 6.2 Partnership Processes
Partnership Structures
■ Diversity: who is involved
■ Complexity
■ Formal agreements
■ Control of resources
■ Percentage of dollars to community
■ CBPR principles
■ Partnership values
■ Bridging social capital
■ Time in partnership
Individual Characteristics
■ Motivation to participate
■ Cultural identities, humility
■ Personal belief, values
■ Spirituality
■ Reputation of PI
Relationships: How We Interact
■ Safety/respect/trust
■ Community voice/inuence
■ Flexibility
■ Dialogue and listening, mutual learning
■ Conict management
■ Leadership
■ Self- and collective reection, reexivity
■ Resource management
■ Participatory decision making
■ Task roles recognized
Commitment to Culture-Centeredness
Socio-Ecologic Framework for CBPR 83
In the science or intervention and research domain, processes lead to outputs (see Box6.3).
The ability to integrate community and cultural knowledge and voice leads to a culture-centered
nature of the intervention and a t with local settings. Empowering processes lead to partner-
ship synergy. The third construct, community members involved in research activities, leads to
appropriate research design. Taken together, the processes lead to the bidirectional translation,
implementation, and dissemination of research.
In the outcomes domain (see Box6.4), partnering processes and their impact on research
and interventions may produce multilevel impacts, from system and capacity outcomes for
the community and academic partners as well as the potential for improved health and health
equity. Intermediate system and capacity outcomes may include policy environment changes,
whether the intervention is sustainable and culturally centered for broader reach, changes in
power relations and knowledge democracy, and changes in cultural reinforcement—whether
the intervention supports cultural revitalization or cultural continuity in the community. The
Box 6.3 Intervention and Research
Processes and Outputs
■ Processes that honor community and cultural knowledge and voice, t local settings, and use
academic and community language leading to culture-centered interventions
■ Empowering co-learning processes lead to partnership synergy
■ Community members involved in research activities lead to research and evaluation designs that
reect community priorities
■ Bidirectional translation, implementation, and dissemination
Box 6.4 Outcomes
Intermediate System and Capacity Outcomes
■ Policy environment changes in universities and communities
■ Sustainable partnerships and projects
■ Empowerment: multilevel
■ Shared power relations in research, knowledge democracy
■ Cultural reinforcement, revitalization
■ Growth in partner and agencies capacities
■ Research productivity: research outcomes, papers, grant applications, and awards
Long-Term Outcomes: Social Justice
■ Community/social transformation: policies, programs, conditions
■ Improved health, health equity
84 Community-Based Participatory Research for Health
long-term improved health outcomes include potentially transformed social and economic con-
ditions, reduced health disparities, and increased social justice.
The CBPR conceptual model hypothesizes multiple pathways that context affects: partner-
ship dynamics, research and intervention design, and outcomes. With feedback loops, outcomes
can circle back to affect other domains, which then inuence each other. A policy outcome, for
example, which the partnership advocated for, could open up the policy environment to more
input by the partnership, which could then bring in other stakeholders to identify additional
data for action, thus creating more community capacities to use research to effect policy and
community changes. These interactions, which may proceed partially along linear pathways,
may also therefore be thought of as dynamic complex systems of reciprocal or mutual inuence.
Once the initial model was created, we sought further community consultations, starting
in 2009, to establish community face validity and make revisions as necessary. Qualitative data
were gathered from six focus groups drawn from a purposive sample of the think tank members’
community partners. The aims of the focus groups were to gain community partner perspectives
on the conceptual model (i.e., the meanings, strengths, and weaknesses of the four domains and
various constructs) and to adapt the model based on community wisdom about the constructs
and deepen understandings about new constructs added to the model (Belone et al.,2016).
The six CBPR projects that participated in the focus group research included four geo-
graphically and ethnically diverse partnerships: two in the Midwest (one rural and one urban),
one in the West, and one in the Southwest, as well as two national CBPR nonprot organi-
zations. Findings from the community consultations included (1) the model had strong face
validity across geographically, racially, and ethnically diverse partnerships, with support for
existing constructs and suggestions for new constructs; (2) the dimensions and constructs were
useful prompts for discussion of partnership practices within specic communities; and (3) four
cross-cutting constructs were seen in all domains of the model—trust development (also see
Chapter5), capacity, mutual learning, and power dynamics. The conversations underscored the
usefulness of the conceptual model in promoting self- and collective reection and a continual
process evaluation for partnerships.
In summary, this rst-stage exploratory pilot yielded an initial model and an interdisci-
plinary literature review of measurement instruments for constructs in the model (Pearson
et al.,2011; Sandoval et al.,2012) to contribute to theory about effective, authentic CBPR. Test-
ing the model was the next step.
STAGE TWO: RESEARCH FOR IMPROVED HEALTH: TESTING
AND STRENGTHENING THE MODEL
As UNM CPR and UW IWRI came to the end of their three-year NIMHD-funded pilot, they
sought additional support and a new partner to continue the process of rening and testing
the conceptual model, all with an eye toward creating tools and information that support the
continual strengthening of CBPR science. In 2008, co-PIs Wallerstein and Duran invited the
National Congress of American Indians Policy Research Center (NCAI PRC) to join their think
tank of CBPR practitioners and to partner as a new PI on their next funding application.
A grant from the Native American Research Centers for Health (NARCH), a funding part-
nership between the Indian Health Service and the National Institutes of Health, supported the
Socio-Ecologic Framework for CBPR 85
next phase of work to test the model.
1
Wallerstein and Duran intentionally selected a junior
investigator to mentor in the PI role. NCAI PRC director Sarah (Hicks) Kastelic brought a focus
on CBPR in American Indian/Alaska Native (AI/AN) tribal communities and thereby strength-
ened the Indigenous lens of the role of governance, stewardship, and Indigenous knowledge
within the model. Founded in 2003, the NCAI PRC’s mission was to provide tribal leaders
with the best available knowledge to make strategic policy decisions in a framework of Native
wisdom that positively affects the future of Native peoples.
2
This mission positioned NCAI PRC
to credibly lead a project to engage with community-academic partnerships including commu-
nities of color and tribal communities to further test the conceptual model.
This new partnership of three organizations and their teams represented several principles of
CBPR: the coming together of different knowledge bases, recognition that each knowledge base
brought complementary strengths, the shared goals of research for the purpose of community
benet and equity, and research capacity building of a more junior investigator from the community
partner. This last principle, although not specically within the CBPR literature, has been threaded
throughout the years in this initiative, as well as in others around the country, to welcome new
scholars, students, and community partners into a community of practice and mutual learning.
For CBPR as a eld, mentorship, in particular of scholars of color, has been a common practice
with the goal of changing the face of the academy to bring in colleagues who can best serve and
understand the communities they come from (see Chapter19 for particular pipeline programs).
The NARCH V grant (2009–2013) funded a mixed-methods, cross-site research study enti-
tled “Research for Improved Health: A Study of Community-Academic Partnerships” (RIH)
to test the CBPR conceptual model and its four domains across a wide variety of federally
funded community engaged and CBPR projects. Two Internet surveys of about two hundred
partnerships and seven in-depth case studies were used to explore the following study aims:
(1) describe the variability of CBPR characteristics across dimensions in the CBPR conceptual
model to identify differences and commonalities across partnerships; (2) describe and assess the
impact of governance on CBPR processes and outcomes across AI/AN and other communities
of color; (3) examine the associations among group dynamic processes and three major CBPR
outcomes: culturally responsive and centered interventions, strengthened research infrastruc-
ture and other community capacities, and new health-enhancing policies and practices, under
varying conditions and contexts; and (4) identify promising practices, assessment tools, and
future research needs for the eld of CBPR. The intention was for NCAI, in particular, to bring
those practices and tools to tribal leaders and researchers (Hicks et al.,2012). Again, the think
tank of CBPR community and academic practitioners advised the research team in an ongoing
fashion, including quantitative and qualitative instrument development and data analysis (see
http://cpr.unm.edu/research-projects/cbpr-project/research-for-improved-health.html).
As described in signicant detail by Lucero et al. (2016) (and with some information in
Chapter17), the RIH research design integrated mixed methods at each stage of the research pro-
cess. Further, by revisiting stages to integrate new knowledge gleaned from practice, the research
team had signicant innovation in what they termed an “expanded iterative integration...grounded
in an Indigenous-transformative [emphasis added] paradigm that recognized different ways of
knowing at each stage and at critical decision points” (Lucero et al., 2016, p. 3).
The study design began with shared sample nalization and inclusion criteria for the
quantitative web-based survey and qualitative case studies. The qualitative research began rst,
86 Community-Based Participatory Research for Health
as the quantitative instruments were still being designed. The quantitative and qualitative instru-
ments drew on the literature review during the pilot. The rst case study was conducted, and
results of the analysis were integrated into the survey design; further, qualitative materials were
revised. This integration of practice, reection, and new knowledge strengthened the qualitative
materials and informed quantitative instrument development, recruitment, and instrument revi-
sion. The case studies continued on parallel track with the implementation of the web-based
survey. Quantitative and qualitative analyses were conducted, and data validation occurred.
The sampling frame was constructed using a 2009 download of all federally funded CBPR
and community-engaged research projects from the NIH RePORTER database. (For sampling
details, see Pearson et al., 2015.) Of the participating community-academic partnerships, 45
percent were funded by three federal agencies: National Institute on Minority Health and Health
Disparities (19.1 percent), National Cancer Institute (13.3 percent), and the Centers for Disease
Control (12.6 percent). The majority of participating projects were intervention research (66
percent) as opposed to descriptive research (20.7 percent) or other research, such as dissemina-
tion and implementation or policy projects (13.3 percent). Nearly 59 percent of projects were
funded by NIH R mechanisms. The average length of the project was 4.6 years. Twenty-one
percent of projects served AI/AN populations (n = 63); 23 percent served other minority popu-
lations (Hispanic/Latino [n = 24], African American [n = 20], and Asian American [n = 7]); and
55 percent served no specied population (n = 85) or multiple populations (n = 17).
With oversampling of AI/AN projects because of targeted outreach to NARCH projects,
we were able to identify specic issues related to governance differences between AI/AN proj-
ects and those of other populations. Projects serving AI/AN populations were more likely to
share resources and power, including making key decisions together; more likely to have formal
written research agreements, including publication guidelines and review, intellectual property
agreements, and data sharing and use guidelines; and, generally, less well-funded (i.e., received
less total funds than projects serving multiple race–unspecied racial groups). (For additional
ndings related to the relationship of CEnR research approval type to governance processes,
productivity, and perceived outcomes, see Oetzel et al., 2015.) There were no signicant dif-
ferences between AI/AN-serving projects and those serving multiple races or unspecied racial
groups in partners’ engagement throughout the research process. Across all projects, community
partners were engaged in an average of 6.5 research activities.
In addition to the survey, seven diverse case studies were identied from distinct regions,
subpopulations, and health and social issues (see Table6.1). The goal of the case studies was to
complement and triangulate with the survey data and to focus more specically on the mech-
anisms and pathways of how partnering practices may contribute to short-term, intermediate,
and long-term outcomes. (For case study descriptions, see Chapters9 and 11; Devia et al.
[2017]; Lucero et al. [under review]; Wallerstein et al. [under review].)
Achievement of synergy as a proximal outcome, for example, as the capacity of partners to
get the tasks of research done collaboratively, can promote a series of intermediate outcomes,
such as greater equality between academics and community members in their decision-making
and respect for each other’s knowledge and, therefore, the co-development of interventions that
would be centered within local cultural values and contexts. This cultural t would then lead
to a higher likelihood of sustainability of these interventions and increased chance of health
improvement over the long run.

Socio-Ecologic Framework for CBPR 87
With the case study and the survey data together, we conducted a mixed-method analysis of
the RIH data to examine how all domains relate to each other. This analysis involved a structural
equation model (SEM) to test the complex relationships as well integration of case study data
to add depth and better understanding of the mechanisms of change to the statistical analysis.
We could not include every variable from the original conceptual model and so focused
on specic variables within each domain. The tested model was a good t with the data and
TABLE 6.1 Projects and Health and Social Issues
Region Population Partners
Healing of the Canoe:
Substance abuse pre-
vention, youth life skills
Pacic Northwest Native youth University of Washington and
two tribes
Men on the Move:
Cardiovascular disease
prevention, men’s
employment
Boothill, Missouri African
American men
St. Louis University;
community members
Bronx HealthREACH:
Faith-based diabetes
management and
prevention, unequal
access to care
Bronx, New York African
American
and Latino
congregations
Institute for Family Health,
New York University,
churches, and community
organizations
Lay health workers
to increase colorectal
cancer screening and
nutrition education
San Francisco Residents
of Chinatown
(55–64)
University of California, San
Francisco; San Francisco State;
NICOS (Community partner),
Chinatown Health Department
Tribal Nation: Barriers to
Cancer Prevention
South Dakota Native adults Black Hills Center
for American Indian
Health and tribe
South Valley Partners for
Environmental Justice:
Policies to reduce unequal
exposure to toxins
Albuquerque,
New Mexico
Hispanic
population
University of New Mexico,
Bernalillo County, Rio
Grande Community
Development Corporation,
community partners
Assessment of health
issues for Deaf and
hearing impaired
Rochester,
New York
Deaf or
hearing impaired
Center for Deaf
Health, University of
Rochester, partners from
Deaf community
88 Community-Based Participatory Research for Health
included two context variables (partnership capacity and nal approval), with paths to the part-
nership processes domain to two larger constructs: (1) partnership structures, including, for
example, shared control over resources and percentage of resources to community, and (2)
relationships, including, for example, leadership, trust, and participatory decision making),
which led to the intervention and research domain (e.g., community involvement in research
and synergy). Although interrelated, two pathways emerged. The material structural pathway,
starting with nal approval of the project on behalf of the community by a tribal government or
health board compared to other approvals, is associated with a greater percentage of resources
to the community. The percentage of resources, along with shared control of the resources, is
associated with higher levels of community involvement in the research. The second relation-
ship pathway starts with partnership capacity shaping partnership values, which is associated
with stronger relationships and then synergy. Both of these pathways were positively associ-
ated with intermediate outcomes, and then intermediate outcomes are positively associated with
long-term outcomes of community transformation and health outcomes.
Case study examples added the time element and directionality of how pathways worked.
For example, in the San Francisco Chinatown case study on effectiveness of lay health workers,
partners included a well-esteemed community organization. By receiving a subcontract and
research training, the community organization (NICOS Chinese Health Coalition) controlled
resources to hire staff members for each research step. Interviewees discussed how their col-
laborative structures led to greater involvement of community members in the research and
collective decision making, which led to enhanced synergy, contributing to outcomes of inter-
vention effectiveness, enhanced research capacity for NICOS, and increased recognition by aca-
demics of NICOS’s goals for workforce development, a community benet far beyond specic
grant aims. Together, the qualitative data, coupled with the SEM analysis, demonstrated support
for the robustness of the CBPR model (Oetzel et al.,in press).
Through analysis of the model, we learned that effective partnering may not be a generic
“promising practice,” but dependent on holistic contextual factors (including those supported by
survey data such as partner capacity to be advocates). When viewed organically, effective part-
nerships apply symbiotic strategies in response to their environments (e.g., history or political
policy context) and their ability to transform internal group-level relationship dynamics (e.g.,
power sharing, trust, co-learning, and community voice) into greater partnership synergy
and broad capacity and system changes. Another RIH case study, Bronx Health REACH, for
example, worked with church pastors steeped in the civil rights movement as their historical
context to demand their voice be heard. The power of the community partners supported strong
equitable relationships with their academic partners, such as power sharing, which created a
formidable synergy that was able to advocate for improved food environments and school nutri-
tion policies to reduce excess rates of diabetes (Devia et al.,2017; Kaplan et al.,2009). The
qualitative data therefore recommends adoption of promising practices with consideration of
contexts and implications for actions within specic political-cultural conditions.
As RIH funding ended in 2013, the research partners shared instruments and materials
widely to openly invite stakeholders to explore and use the model.
3
One example has been
NCAI’s subsequent NARCH grant to create a dissemination and implementation tool kit for
several of the constructs, including trust and culture, and to highlight the role of governance and
sovereignty in partnership evaluation.
4
Socio-Ecologic Framework for CBPR 89
STAGE THREE: CONTINUING TO ADAPT AND EXPAND
THE MODEL: DISCOVERING NEW USES
On the heels of RIH, UNM CPR and UW IWRI sought additional partners to continue to
adapt, expand, and test the CBPR conceptual model. With support from the National Insti-
tute of Nursing Research (2015–2020), UNM CPR and UW IWRI recruited other University
of Washington colleagues, Community-Campus Partnerships for Health, the National Indian
Child Welfare Association, University of Waikato, New Zealand, and Rand Corporation to join
“Engage for Equity (E
2
),” a national study of community and academic partnerships, to con-
tinue development of measures and metrics of CBPR practices and outcomes. The specic aims
are to (1) reconvene the national think tank of academic and community CBPR experts for
their oversight and guidance; (2) rene, translate into Spanish, and test nalized metrics and
measures with up to two hundred federally funded partnerships; and (3) conduct a randomized
control trial comparing a workshop intervention that integrates partnership evaluation and
self-reection tools for forty partnerships versus access to materials and resources on the web.
The Engage for Equity team has begun to deepen our understanding of theories of change that
may matter in partnerships, such as the role of empowering processes or the role of culture-
centeredness approaches in creating successful outcomes.
It is clear that the CBPR conceptual model has strong resonance and meaning in the eld of
community-engaged research and CBPR science. The model continues to evolve as a dynamic
tool to explore, support, evaluate, and strengthen CBPR science. The research partners believe
that rather than serving as a static model of the one “true” perspective on CBPR, the model
serves a eld-building and unifying purpose. The CBPR conceptual model has been continually
promoted as a dynamic tool to be adapted by local partnerships and used creatively.
In the last ve years, the research partners have learned much about how community
and academic partnerships are organically making the model their own, adapting its content
and format in ways that support their perspectives and experiences. For example, Lisa Gibbs,
principal investigator of Teeth Tales, a CBPR study addressing children’s oral health for
Australian families in Melbourne from migrant backgrounds, adapted the conceptual model
in 2014 (see Figure 6.2). With multiple community partners, including immigrant Pakistani
and Arabic organizations, the University of Melbourne adapted the model in the nal research
stages to represent their study experience. They reected on the model dimensions, kept rele-
vant constructs, and added their own. Partners found it a useful summary exercise to identify
and assess their most important partnering practices and outcomes.
5
More recently, the Minnesota Rochester Healthy Community Partnership,
6
a ten-year
established CBPR partnership working with the Somali, Hispanic, and Cambodian commu-
nities to promote community health and well-being, approached UNM CPR about support and
tools for evaluating their partnership. (See Chapter17 for a description of how they adapted the
model, surveys, and interview instruments to evaluate their history and current partnering prac-
tices to envision future directions.)
The model has also been translated into Spanish and Portuguese.
7
A nonprot health system,
AMOS Health and Hope (Amoshealth.org), for example, has used the model to strengthen their
training of community health workers (promotores) as coresearchers of maternal and child
health inequities in remote rural underserved areas of Nicaragua. The promotores collect data

Context
• Cultural and linguistic diversity • Existing partnerships between
some organizations
• Exploratory qualitative research
• Contribution to evidence base
• Evidence about child oral health
knowledge and behaviors
• Oral health peer educators
• Community outreach oral health care
• Increased toothbrushing
• Child oral health education manual
• Clinical guidelines
• Guidelines for organizational cultural
competency (CORe)
• Increased research capacity of
community partners
• Increased cultural competence of
researchers
• Increased organizational cultural
competency
• Dissemination of findings
• Ongoing partnerships
• Development of intervention
framework
• Pilot study
• Exploratory trial
- CORe
- Screening
- Peer-led community oral health
education program
• New partnerships formed
• Organizations seeking research
partnerships
• Project budgets, staffing, and
resources shared across organizations
• Joint funding submissions
• Community health
• Priority health issue
• Oral health inequity
• Barriers to care
• Committment to CBPR*
• Funding model for dental care
Partnerships Research Outcomes
FIGURE 6.2 Teeth Tales Model
Note: CBPR = community-based participatory research.
Source: Adapted from http://mspgh.unimelb.edu.au/centres-institutes/centre-for-health-equity/research-
group/jack-brockhoff-child-health-wellbeing-program/research/physical-health-and-wellbeing/teeth-tales
Socio-Ecologic Framework for CBPR 91
on households to monitor family health and to identify community empowerment strategies,
such as women’s and youth groups, to address root causes of ill health (see Chapter18). AMOS
is also using the model to train medical students and faculty members on how to integrate
community participation into research projects. The Spanish, Portuguese, and English versions
have each been integrated into the empowerment, social participation, and participatory research
curriculum (in three languages) on the UNM Center for Participatory Research website.
8
Finally, the conceptual model is being used as a visioning and planning tool for new part-
nerships to brainstorm their desired outcomes and the partnering processes they would like to
have. New teams often start with brainstorming in the fourth domain, the outcomes they would
like to see. They then return to the rst two domains of the model: identifying core contex-
tual issues important to their communities and discussing partnership dynamics, that is, how
they plan to integrate CBPR principles and strategies into their partnering practices or whether
they need or want to develop formal agreements. They can then think ahead as to how their
decision-making practices will affect their interventions and research design and methods, and
ultimately, return to desired outcomes.
This newer use of the model as a reection tool for setting a planning or evaluation agenda
provides partnerships an opportunity to adapt the model for their own use. For CBPR visioning
facilitation guides for planning and evaluation purposes, see http://cpr.unm.edu/research-
projects/cbpr-project/facilitation_tools.html.
These self-created plans can then be revisited on an annual basis and form part of an ongoing
cycle of evaluation and reection opportunities for recognition of achievements and recom-
mendations for the future. As a living, breathing document, we hope that the CBPR conceptual
model can be useful for your own reections and actions in current and future collaborative
research endeavors.
CONCLUSION
Future stages of work on the conceptual model include evolution of how best to apply the model
for planning, collective evaluation, and ongoing reection on partnering practices and outcomes.
Cross-partnership dialogue about model use may lead to further evolution or potential reinter-
pretation of the model. Future research will focus on better understanding the pathways among
variables in the domains or better identifying theories of change that lead to system, capacity, and
social justice outcomes. We hope that partnerships can be better positioned to make deliberate
choices about which context, relationship, or structural processes or other partnering factors are
important to them and their research, in order for them to achieve their own desired outcomes.
QUESTIONS FOR DISCUSSION
1. What is the value of the CBPR conceptual model? How can it be used?
2. How has the evolution of this model supported a larger CBPR research agenda, including
improving CBPR science?
3. What are the potential dangers of putting forth a model of CBPR (even if you acknowledge
variability and no one “right” way)?
92 Community-Based Participatory Research for Health
ACKNOWLEDGMENTS
The research described in this chapter was supported by NARCH (U261HS300293;
U261IHS0036-04-00), with Indian Health Service in partnership with the National Institute of
General Medical Sciences, National Institute of Minority Health and Health Disparities, National
Institute on Drug Abuse, National Center for Research Resources, Ofce of Behavioral Social
Sciences Research, National Cancer Institute, and Health Resources Services Administration. We
thank the research team and members of the think tank and community scientic advisory board
for their collaboration. We also appreciate Dr. Malia Villegas who stepped in as PI for Dr. Sarah
Kastelic, when Sarah left the directorship of NCAI’s Policy Research Center. Most important,
we thank the academic and community partners who participated in the surveys and case studies.
NOTES
1. See www.nigms.nih.gov/Research/CRCB/NARCH/Pages/default.aspx.
2. See www.ncai.org/policy-research-center/about-prc/mission.
3. See quantitative and qualitative instruments at http://cpr.unm.edu/research-projects/cbpr-project/
research-for-improved-health.html.
4. See www.ncai.org/policy-research-center/initiatives/projects/narch.
5. http://cpr.unm.edu/research-projects/cbpr-project/background-to-teeth-tales.html.
6. See http://rochesterhealthy.org/website/.
7. http://cpr.unm.edu/research-projects/cbpr-project/cbpr-model.html.
8. See http://cpr.unm.edu/curricula--classes/empowerment-curriculum.html.
REFERENCES
Ahmed, S. M., & Palermo, A. G. (2010). Community engagement in research: Frameworks for education and peer review.
American Journal of Public Health, 100(8), 1380–1387. doi:10.2105/AJPH.2009.178137
Barkin, S., Schlundt, D., & Smith, P. (2013). Community-engaged research perspectives: Then and now. Academic Pediatrics,
13(2), 93–97.
Belone, L., Lucero, J. E., Duran, B., Tafoya, G., Baker, E. A., Chan, D.,...Wallerstein, N. (2016). Community-based participa-
tory research conceptual model: Community partner consultation and face validity. Qualitative Health Research, 26, 117–135.
Devia, C., Baker, E., Sanchez-Youngman, S., Barnidge, E., Golub, M., Motton, F., Muhammad, M., Ruddock, C., Vicuña,
B., & Wallerstein, N. (2017). CBPR to advance social and racial equity: Urban and rural partnerships in black and Latino
communities. International Journal for Equity in Health, 16, 17. doi:10.1186/s12939-016-0509-3
Duran, E., & Duran, B. (1995). Native American postcolonial psychology. Albany State University of New York Press.
Freire, P. (1970). Pedagogy of the oppressed. New York, NY: Seabury Press.
Freire, P. (Ed.). (1982). Creating alternative research methods: Learning to do it by doing it. Toronto, Canada: Participatory
Research Network.
Greenlund, K. J., & Giles, W. H. (2012). The Prevention Research Centers program: Translating research into public health
practice and impact. American Journal of Preventive Medicine, 43(3 Suppl 2), S91–S92. doi:10.1016/j.amepre.2012.06.002
Hicks, S., Duran, B., Wallerstein, N., Avila, M., Belone, L., Lucero, J.,...White Hat, E. W. (2012). Evaluating community-
based participatory research to improve community-partnered science and community health. Progress in Community
Health Partnership: Research, Education, and Action, 6, 289–299.
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (Eds.). (2013). Methods in community-based participatory research for
health (2nd ed.). San Francisco, CA: Jossey-Bass.
Socio-Ecologic Framework for CBPR 93
Kaplan, S. A., Ruddock, C., Golub, M., Davis, J. D., Foley, R.C.D.,...Calman, N. (2009). Stirring up the mud: Using a
community-based participatory approach to address health disparities through a faith-based initiative. Journal of Health
Care for the Poor and Underserved, 20, 1111–1123.
Lucero, J., Wallerstein, N., Duran, B., Alegria, M., Greene-Moton, E., Israel, B.,...White Hat, E. (2016). Development of
a mixed-methods investigation of process and outcomes of community-based participatory research. Journal of Mixed
Methods Research. Advance online publication. doi:10.1177/1558689816633309
Lucero, J., et al. (under review). CBPR as negotiation: A cancer screening case study from Chinatown, San Francisco. Journal
of Health Psychology.
Michener, L., Cook, J., Ahmed, S. M., Yonas, M. A., Coyne-Beasley, T., & Aguilar-Gaxiola, S. (2012). Aligning the goals
of community-engaged research: Why and how academic health centers can successfully engage with communities to
improve health. Academic Medicine, 87(3), 285–291. doi:10.1097/ACM.0b013e3182441680
Minkler, M., & Wallerstein, N. (Eds.). (2008). Community-based participatory research for health: From process to outcomes
(2nd ed.). San Francisco, CA: Jossey-Bass.
Oetzel, J. G., Villegas, M., White Hat, E., Duran, B., & Wallerstein, N. (2015). Governance of community-engaged research:
Exploring the associations of nal approval with processes and outcomes. American Journal of Public Health, 105,
1161–1167.
Oetzel, J. G., Wallerstein, N., Duran, B., Villegas, M., Sanchez-Youngman, S., et al. (in press). Community-engaged research
for health: A test of the CBPR conceptual model. BioMed Research International.
Pearson, C., Duran, B., Martin, D., Lucero, J., Sandoval, J., Oetzel, J., Tafoya, G., Belone, L., Avila, M., Wallerstein, N., &
Hicks, S. (2011). CBPR variable matrix: Research for improved health in academic-community partnerships [Interactive
model]. Retrieved from http://ces4health.info/index.aspx
Pearson, C. R., Duran, B., Oetzel, J., Margarati, M., Villegas, M., Lucero, J., & Wallerstein, N. (2015). Research for improved
health: Variability and impact of structural characteristics in federally funded community engaged research projects.
Progress in Community Health Partnerships: Research, Education, and Action, 9, 17–29.
Sandoval, J. A., Lucero, J., Oetzel, J., Avila, M., Belone, L., Mau, M., & Wallerstein, N. W. (2012). Process and outcome con-
structs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education
Research, 27, 680–690.
Schulz, A. J., Israel, B. A., & Lantz, P. (2003). Instrument for evaluating dimensions of group dynamics within
community-based participatory research partnerships. Evaluation and Program Planning, 26, 249–262.
Selby, J. V., Beal, A. C., & Frank, L. (2012). The Patient-Centered Outcomes Research Institute (PCORI) national priorities
for research and initial research agenda. JAMA, 307(15), 1583–1584. doi:10.1001/jama.2012.500
Trickett, E. J. (2011). Community-based participatory research as worldview or instrumental strategy: Is it lost in translation(al)
research? American Journal of Public Health, 101(8), 1353–1355. doi:10.2105/AJPH.2011.300124
Tuhiwai Smith, L. (1999). Decolonizing methodologies: Research and Indigenous peoples. New York, NY: Zed Books.
Viswanathan, M., Ammerman, A., Eng, E., Garlehner, G., Lohr, K. N., Grifth, D., . . . Whitener, L. (2004, August).
Community-based participatory research: Assessing the evidence summary (AHRQ Pub. No. 04-E022-1). Rockville,
MD: Agency for Healthcare Research and Quality. Retrieved from https://archive.ahrq.gov/clinic/epcsums/cbprsum.pdf
Wallerstein, N., & Auerbach, E. (2004). Problem-posing at work: Popular educators guide. Edmonton, Canada: Grass
Roots Press.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal Public Health, 100(Suppl 1), S40–S46.
Wallerstein, N., Oetzel, J., Duran, B., Magarati, M., Pearson, C., Belone, L., Davis, J., Dewindt, L., Lucero, J., Ruddock,
C., Sutter, E., Villegas, M., Dutta, M. (under review). Conceptualizing and measuring the culture-centered approach in
community based participatory research. Social Science and Medicine.
Wallerstein, N. B., Oetzel, J., Duran, B., Tafoya, G., Belone, L., & Rae, R. (2008). What predicts outcomes in CBPR? In
M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes
(pp.371–394). San Francisco, CA: Jossey-Bass.

7
CHAPTER
YOUTH-LED PARTICIPATORY ACTION research (YPAR) is an approach to inquiry and
social change that engages young people in identifying problems relevant to their own lives,
conducting research to understand the problems, and advocating for changes based on research
evidence (Brown & Rodríguez,2009; London, Zimmerman, & Erbstein,2003; Ozer & Doug-
las,2015). YPAR, similar to other forms of community-based participatory research (CBPR),
is focused on increasing the power of marginalized groups in improving real-world problems
via iterative cycles of inquiry and action (Minkler & Wallerstein,2003). YPAR research and
practice has grown in recent years: a 2016 Psychinfo database search, for example, shows
more than three hundred citations using the term youth-led participatory action research.
YPAR spans elds including public health, education, and community psychology, with youth
researchers addressing diverse topics, such as neighborhood food access (Breckwich Vásquez
et al., 2007), invasive pest management in the Ecuadorian Andes (Dangles et al., 2010),
educational inequalities (Ozer & Wright,2012), water quality in a rural Colombian watershed
(Roa García & Brown,2009), and community education about the judicial system (Stovall &
Delgado,2009).
YOUTH-LED PARTICIPATORY
ACTION RESEARCH (YPAR)
PRINCIPLES APPLIED TO THE US AND DIVERSE
GLOBAL SETTINGS
EMILY J. OZER AND AMBER AKEMI PIATT
96 Community-Based Participatory Research for Health
CBPR focuses on equity and empowerment, as well as generating knowledge that is
informed by insider experts on the nature of the problems studied. YPAR deserves specic
consideration for how it can contribute positively to the development of children and adoles-
cents who participate (Ozer, 2016; Ozer & Russo,2016). YPAR is a particularly promising
approach for disadvantaged youth in early to mid-adolescence because these are developmental
periods characterized by uidity and transition for individual and collective senses of iden-
tity and purpose (Damon, Menon, & Cotton Bronk,2003; Ozer, Ritterman, & Wanis,2010).
YPAR that involves youth in analyzing and changing the conditions that inuence their schools
and communities provides opportunities for youth to identify as leaders with purpose (Damon
etal.,2003; Spencer, Fegley, & Harpalani,2003), rather than seeing themselves in terms of neg-
ative stereotypes held by others (Cahill, Rios-Moore, & Threatts,2008). Further, YPAR seeks to
enhance critical consciousness—critical reection, motivation, and action—that pushes youth
to investigate broader structural conditions that shape behavior rather than just individual-level
explanations (Watts, Diemer, & Voight,2011).
A small but growing research literature indicates that YPAR is well suited to create and
strengthen opportunities for youth to enhance their own knowledge, skills, and motivation;
address inequities in health, education, and other systems; and expand the opportunities for
meaningful inuence in the settings in which young people grow and develop (Berg, Coman,
& Schensul,2009; Cargo et al.,2003; Holden, Evans, Hinnant, & Messeri,2005; Mitra,2004;
Ozer & Douglas, 2013). Individual-level gains found in qualitative YPAR research include
increases in adolescents’ sense of purpose, perceived support from caring adults, and positive
attitudes toward school (Mitra,2004; Wilson et al.,2007).
In this chapter, we provide an overview of key YPAR practices, examples of YPAR proj-
ects from around the world, and important choice points and challenges that are likely to
be faced in practice. Similar to other researchers, we view YPAR as multidimensional: an
intervention to promote positive youth development and improve inequitable conditions that
undermine it, a re-visioning of young people not as problems to be “xed” but rather as
expert cocreators of knowledge, and an approach toward engaging youth and their exper-
tise in research conducted about them. In practice, YPAR projects can vary with respect
to focusing more explicitly on political empowerment versus enhancing youth’s inquiry
and action skills and their participation in improving and designing settings and programs
intended to serve them.
KEY YPAR PRINCIPLES
As in any research, there are many paths and choice points in YPAR. YPAR needs to be respon-
sive to the context of youth, particularly to the resources and limitations of the institutions
and communities engaged in efforts related to youth participation, and thus by denition will
not look exactly the same across settings. That said, there are core principles and practices in
this approach that are important to articulate, including (1) bringing youth participants into the
training and practice of research, critical thinking, and change strategy; (2) carefully attending
to intentional power sharing between youth and adults, especially considering that youth do not
exert the same power in school or out-of-school contexts; and (3) integrating iterative research
and action phases into the project (Ozer et al.,2010).
Youth-Led Participatory Action Research (YPAR) 97
Context: Youth as Experts and Knowledge Creators
Regardless of specic emphases, all YPAR projects assert that youth are capable of generating
expert knowledge of value in addressing problems that affect their development and well-being.
Youth can be valued partners in the scientic enterprise and agents for changes in systems and
communities beyond the traditional role of serving as passive participants in research that seek
to affect them. Positive views of youth—particularly youth of color—as providing expertise and
leadership potential run counter to dominant stereotypical views of adolescents as sources of
worry or threat (Camino & Zeldin,2002) and as a group lacking in agency, wholly governed by
hormones and peer pressure.
Researchers who study youth development with YPAR have identied how research validity
is strengthened via partnership with youth researchers, including in dening research questions,
developing instruments, and interpreting ndings (Fine,2008; Langhout & Thomas,2010). The
role of YPAR in providing an insider phenomenological perspective on youth development,
especially for the investigation of sensitive, hidden, or hard-to-report phenomena, is discussed
in greater detail in Ozer (2016).
Relationships: Adult-Youth Power Sharing
Sharing of power between adult facilitators and youth researchers requires intentionality and
care given the inequality of adult-youth relationships, especially within the inherent hierarchy
of K–12 school settings (Kohfeldt, Chhun, Grace, & Langhout,2011; Ozer, Newlan, Douglas,
& Hubbard,2013; Zeldin, Christens, & Powers,2013). We note that power sharing regarding
key decisions and processes in YPAR does not mean that all ideas made by the youth should
be followed uncritically. Rather, it means that the perspectives and interpretations of the youth
researchers must be considered by the group for their strengths and limitations rather than
outright overruled by an adult. The plan and process for decision making should be discussed
openly and followed so that there are no surprises.
Engaging in YPAR requires preparing the ground early through activities that develop
trusting relationships and communication skills among the youth participants and between
the adult and youth participants (see Mirra, Garcia, & Morrell [2015] for in-depth analysis of
building trust and negotiating power within a long-term educational partnership for YPAR).
Conducting YPAR calls for effective adult facilitators who can train and guide teams of youth
researchers on the journey without fully taking over steering the ship. Our research, and that of
others concerned with the balance of power in youth development programs (Larson, Walker,
& Pearce,2005), analyzes how effective adult facilitators use strategies to maintain youth con-
trol over key aspects of the YPAR projects, such as dening the problem, choosing the design,
interpreting data, and deciding on action steps, while at the same time providing helpful struc-
ture, such as breaking down tasks and keeping timelines. Importantly, in addition to guiding the
organizational and learning processes of research and action, effective adult facilitators help
students resolve conicts—substantive and personal—and navigate the political complexities of
seeking to make changes in institutions such as schools in which they have little power.
In addition to these “non-negotiables,” other youth development activities that generally
occur as part of high-quality YPAR projects include skill-building exercises related to working
in groups to achieve goals and the expansion of youth’s social network with peers and adult
leaders (Ozer & Douglas,2015).
98 Community-Based Participatory Research for Health
Balancing Research and Action
Although this chapter focuses on YPAR, there are other approaches, such as youth organizing,
action civics, and city planning, that often similarly emphasize equity and social change
(Center for Cities and Schools,2016; Generation Citizen,2016; Kirshner,2015; Kirshner &
Ginwright,2012). Of these related approaches, YPAR tends to be the most focused on gen-
erating and engaging with data—coupled with taking action based on those data. Because
YPAR projects differ in context, group dynamics, issues, methods, and opportunity for social
change, there is no easy formula for how to best integrate iterative cycles of research and
action in a YPAR project. Research and action are not mutually exclusive: actions driven
by well-designed and well-implemented research can deliver more targeted, meaningful
impacts, and research that is driven by an action-oriented agenda can often be more relevant
and useful.
YPAR PHASES AND SUPPORT RESOURCES
There are multiple curricula that can help scaffold groups interested in conducting YPAR proj-
ects; these curricula provide interactive activities that can be adapted to various development
and educational levels. For our initial UC Berkeley–SF Peer Resources Project (2003–2011)
that supported and studied YPAR in public high schools (Ozer & Douglas, 2013; Ozer
etal.,2008), we drew from existing curricula (Anyon et al.,2007; London,2001; Schensul,
Berg, & Sydlo,2004) to create a hybrid that t the goals and pedagogical approaches of SF
Peer Resources’ middle and high school elective classes. In our recent efforts to develop an
interactive web platform—the YPAR Hub—to help diffuse YPAR, we synthesized the con-
tributions of multiple curricula; the result is a website with downloadable lesson plans and
practical tips for adult facilitators, as well as examples of YPAR in the United States and inter-
nationally. Some of these resources are discussed in the following sections as we walk through
phases of YPAR.
Issue Selection
It is critical that the issues tackled by the YPAR groups reect the authentic concerns of the
youth researchers—in other words, that the problems or questions are ones that they genuinely
care about and want to inuence. Before deciding on a topic, however, it is also important for
the adult facilitators and youth researchers to be strategic in considering the potential allies,
resources, and time they would have for any given issue. Who else will care about this issue?
What are the existing governance structures and opportunities for the group to report back their
ndings? Even in the early stages of YPAR projects, thinking ahead to possible action steps and
to the timing for getting on the calendar of key stakeholders for reporting back is highly recom-
mended to make sure that there will be an audience for the results.
Multiple strategies can help support young people to identify an issue that they are moti-
vated to work on and that is addressable within the time frame of the project. Although some
YPAR groups target big community-level issues, such as reducing the number of liquor stores
or air pollution in their neighborhoods, others take on more discrete issues, such as having clean
bathrooms, drinking fountains, or adequate athletic equipment at their schools. Many examples
of successful YPAR projects start with an open-ended issue selection process, guided by (1)
Youth-Led Participatory Action Research (YPAR) 99
dening their community and then (2) assessing the strengths and problems of that community.
Once the group has agreed on a more narrow area of interest, they can then dene their research
questions, hypotheses, and methods.
For example, when Voces y Manos conducted a YPAR project with Indigenous youth in
rural Guatemala, they used a layered issue selection process. First, a small group of the older
adolescents in the organization developed and facilitated internal focus groups with the younger
adolescents who were guided by open-ended questions to learn what topics mattered to the
group. The older adolescents recorded and transcribed the sessions, then identied the themes
that emerged. They brought back the main emergent themes to the full group of adolescents—
burdensome cost of school-related resources, lack of trust with teachers, fear of free expression
in schools, gender inequities, and subjectivity of classroom grading—to dig into creating indi-
cators for each of the issue areas. The full group then developed a survey that was later admin-
istered to a random sample of high school students in the municipality.
Although YPAR projects often start with an open-ended issue selection process, it is
also common that the choice of topics is more constrained. This can occur for many reasons,
such as when the YPAR project is developed in the context of an existing initiative to study a
particular issue or evaluate services, or when the organization has a specic mandate to jus-
tify its existence or funding. For example, in the UC Berkeley–SF Peer Resources study, stu-
dent cohorts sometimes began the school year knowing they were charged with addressing a
particular topic, such as supporting youth of color with the transition to high school. The fact
that these YPAR projects were conducted in elective high school classes meant that new stu-
dents entered into the project every year or even every semester. When the prior year’s YPAR
cohort had made progress, such as increasing the ethnic diversity of the school or working to
improve the cultural responsiveness of the teaching, there was a clear benet to sticking with
the same issue across cohorts to better sustain traction on inuencing policies and practices. At
the same time, there was recognition that it was important for new cohorts to work on issues
that they genuinely wanted to change rather than solely carrying the torch of the prior cohort.
In examining constrained cases of “bounded empowerment,” we identied processes that facili-
tated youth ownership and sustained work, such as teachers’ framing and buy-in strategies (e.g.,
asking students to further rene an existing research question or shape unnished phases of
a project); micro-power compensation (e.g., providing opportunities for autonomous decision
making on specic tasks within the predetermined project); and alignment of student interests
across cohorts (i.e., natural agreement across cohorts on what an important issue focus would
be in their community) (Ozer et al.,2013). Thus, even when the topic is constrained, it is impor-
tant that each youth cohort selects or adapts an issue that matters to it and is feasible to advance
within the time frame.
Once an issue has been identied, it must be framed strategically. YPAR seeks to engage
young people in social-ecological analyses to address issues that matter to them while identi-
fying the root causes that create and perpetuate those problems. By identifying root causes as
best as they can, youth researchers and adult facilitators seek to enact solutions that address the
upstream sources of problems in order to foster meaningful, sustainable change. The framing
of the issue shapes the research design, methodology, analysis, and action agendas; it also com-
municates the parameters of possible solutions to researchers, stakeholders, allies, and afliates.
For example, the framing of issues can inadvertently reinforce negative attitudes toward youth
100 Community-Based Participatory Research for Health
by placing blame on the individual (e.g., “local students steal from neighborhood convenience
stores at high rates”) rather than acknowledging the inuence of the conditions in which youth
live (e.g., “local students experience high poverty because of the elimination of city rent control
policies and subpar minimum wages”).
Research Design and Methods
After landing on a topic with the guidance of adult facilitators, youth researchers engage in
decision-making processes about the research design, methods, and interpretation of the data
collected. Any issue can be studied with many designs and methods, so it is important to be
strategic and inclusive in this core phase of YPAR. YPAR projects often focus on complex
areas of inquiry and thus can be sliced many ways. Further, given that the researchers likely
have personal experience with a limited range of methods—surveys, for example, are most
common—it is important to use curricula that expose them to the rationales for prioritizing dif-
ferent types of research methods and data. Understanding the relative advantages and disadvan-
tages of different forms of data is important not only for gaining insight into the issue that youth
researchers are working on but also for promoting important intellectual competencies related
to critical thinking and arguing from evidence, areas that are central to current educational
standards and priorities in the United States and other countries (Kornbluh, Ozer, Kirshner, &
Allen,2015).
After deciding on an issue and dening a research question, one of the rst steps that the
research team must take is to search for existing data available to answer their question. Youth
researchers may decide that they will be informed by existing data sets while also generating
some new data on a particular aspect of the issue that needs to be understood through data from
their own school or community. For example, youth interested in violence prevention might
start with understanding published data on county crime levels and then decide to conduct sur-
veys or observations in their own school or neighborhood to inform local action steps. Fortu-
nately, there are new online resources that provide guidance in identifying and understanding
existing data sets regarding health, education, housing, civic life, and other areas of interest
(Center for Regional Change,2014; YPAR Hub,2015).
If new data are needed, selecting research methods that best shine a light on the issue at
hand can necessitate balancing many competing needs and constraints, such as funding, equip-
ment, time, and expertise. To support this process, the YPAR Hub has a decision tree to help
guide groups through some of the choice points inherent to YPAR. Some research methods
commonly used within the YPAR approach include focus groups, interviews, mapping, obser-
vations, photovoice, and surveys. Mapping, for example, is best suited for investigating issues
that are tied to geographic locations whereas photovoice works well with issues that can be
represented visually, either literally or symbolically (see Langhout, Fernandez, Wyldbore, &
Savala [2015] for a detailed case example). Surveys generally enable researchers to gather data
from a larger number of people cost-effectively whereas interviews provide for more in-depth
investigation into individuals’ experiences and opinions. Many projects opt to employ multiple
methods to capitalize on the benets of each.
As an example of choosing research methods, we consider Viramundo, a nongovernmental
organization in Brazil that conducted YPAR to document disparities between wealthy neighbor-
hoods in Rio de Janeiro and the neighboring slums, or favelas, in Rocinha (F. Wittlin, personal
Youth-Led Participatory Action Research (YPAR) 101
communication, October 10, 2015). The research team opted to use community communica-
tion technologies, such as participatory photography and videography, in their data collection.
They videotaped interviews with community members on the streets and in homes in the city
and in the slums responding to questions about bias and discrimination against the favelas. The
research team then compiled and edited the content into a publicly available video. The viewer
is thus able to not only gather the text content of what the respondents say but also their non-
verbal communication (e.g., raised eyebrows, shrugged shoulders) and their settings (e.g., busy
commercial street, dilapidated home). This visually oriented method facilitated Viramundo’s
ability to best answer their specic research question and also gave them powerful material to
engage with the media as part of their action plan for change. (See also Chapter23 on interna-
tional youth mapping.)
Data Analysis and Interpretation
A key point to consider in working with and interpreting data is how to do high-quality gener-
ation and analysis of evidence that is appropriate to the developmental and educational level of
the research team and viable within time and nancial constraints. It is important to make this as
fun and interactive as possible, especially given that some youth may come to the project with
negative experiences with learning with numbers in math and science. Even the term research
may have negative connotations; it is better to focus on questions they want to answer rather
than framing the process as a “big research project.” Fortunately, data analysis does not need to
be complicated to be systematic. For groups that want to keep it simple and do not have access
to the Internet, much can be learned by looking at patterns using basic statistics such as means,
medians, and ranges for different groups. Qualitative analysis of data can also be conducted
through activities such as having youth sort hard copies of quotes in envelopes or tables around
a room as part of a thematic coding process. For groups with access to the Internet, there are
good free versions of computer programs, such as SurveyMonkey, that enable respondents to
enter numeric or text survey data directly into the computer program; this saves time on data
entry and can be used for easy generation of tables and graphs.
One way to reduce the pressure of data interpretation is to invite students to reect on
surprises between what they expected versus what they found as well as patterns among their
sample. Guided questions can help youth researchers to highlight the key points of their nd-
ings and to note any meaningful differences among subjects (e.g., “Would you have expected
English language learners to report more bullying than native English speakers? Do male and
female students feel equally safe at school?”). Arguing from evidence is an important criti-
cal thinking and educational competency; thus, strategies in data interpretation in which youth
researchers state a claim and provide supporting evidence help prepare the research team to
provide a compelling report back to stakeholders and develop skills for weighing evidence. See
the YPAR Hub home page (http://yparhub.berkeley.edu) for a video of how youth researchers
gathered supporting evidence to improve teaching practices.
Voces y Manos, the organization in Guatemala previously discussed, provides an excel-
lent example of the use of survey methods in an international context. The youth researchers
surveyed high school students in their municipality to learn more about their issue from a
maximum number of people at a minimal nancial cost. After data collection, adult facilitators
provided youth researchers with hands-on training in analyzing data, and the youth learned
102 Community-Based Participatory Research for Health
skills such as generating graphs from survey data. In the data interpretation and analysis phase,
the youth researchers realized that the results pointed to multiple manifestations of systemic
issues related to poverty and disempowerment in their communities. Though many students
chronically struggled with similar issues (e.g., lack of trust with teachers), they did not have
a centralized place where they could safely seek support or request a review of their schools’
practices. They concluded that the themes they studied were symptoms of a lack of infrastruc-
ture expressly designed to support local youth, and the youth researchers decided to focus their
action phase on pressuring elected ofcials to commit to fund a preexisting but unfunded Ofce
of Childhood and Adolescence. This ofce could then be reasonably charged with sustainably
addressing and alleviating issues for youth in their community.
Outcomes: Reporting Back and Taking Action
After data collection and interpretation are complete, youth researchers and adult facilitators
identify specic actions that they can take to address the problem, work to report their nd-
ings and proposals to relevant stakeholders, and negotiate the political and logistical complex-
ities of working for change. For example, YPAR groups in the UC Berkeley Peer Resources
project used report back activities such as peer education presentations to students, student-led
professional development sessions for teachers, and slideshow presentations of key ndings to
teachers, school administrators, district decision makers, university partners, and funders.
Voces y Manos also employed a creative report back strategy that advanced their specic
action plan. After deciding that the group wanted to use their data to make policy and budget
recommendations for their municipality, they knew they needed to engage the target that
could implement their requested change: their local mayoral candidates. As such, the youth
researchers held a public forum to present their ndings and policy proposal. They worked with
a coalition of local organizations and youth organizers and involved local radio, television out-
lets, and social media to ensure that the forum reached a large number of residents and raised
the prole of the event. Furthermore, students received trainings in digital literacy, print literacy,
and numeracy (demonstrated in their PowerPoint presentations) that enabled them to engage in
scientic discourse. Furthermore, the public forum was livestreamed for those who could not
attend in person (e.g., Voces y Manos alumni, international donors). In all, 250 people in their
small community participated in person—including all seven mayoral candidates—and an addi-
tional six hundred people watched remotely. By the end of the public forum, all mayoral candi-
dates signed an agreement that they would implement the youth researchers’ policy proposal to
fund their Ofce of Childhood and Adolescence.
Another innovative report back was implemented by the Dream Teens, a national project in
Portugal seeking to integrate youth voice into public policies that affect their lives and commu-
nities (Aventura Social,2015). After working online in small groups with support from university
teams to conduct the research, all youth researchers convened in person to reect on and deliver
recommendations to the National Secretary of Health. Following this event, the government
ministry posted the Dream Teens’ recommendations on their website, and key ofcials reported
that the recommendations were “crucial” for tailoring national policies related to youth.
Finally, YPAR projects can nd inspiration for report back strategies in the larger CBPR
eld. For example, a campaign against discriminatory police practices in New York with the
CUNY Public Science Project projected ndings onto the sides of buildings at night, and the
Youth-Led Participatory Action Research (YPAR) 103
Morris Justice Project in New York City created portraits of community members that chal-
lenged negative stereotypes about their neighborhood and distributed postcards with statistics
comparing disproportionate unwarranted police stops in their neighborhood to those in a high-
income neighborhood.
Scaling, Embedding, and Institutionalizing Change
Beyond promoting the skills and empowerment of the youth who participate in YPAR, a key
goal of most YPAR projects is to make a meaningful difference in the problem that the youth
set out to address. As noted in the academic literature (Sarason,1996) and known all too well
by those in practice, changing policies and institutions that affect the lives of youth is dif-
cult—for well-connected adults let alone youth who do not enjoy the same rights and privileges
as adults. Despite the challenges, there are important examples of YPAR projects that made a
difference in inuencing settings, policies, and systems that we consider here and on the YPAR
Hub. In the United States, there are published examples of youth research and evaluation being
integrated into the work of youth-serving entities such as San Francisco’s Department of Chil-
dren, Youth, and Their Families (Youth IMPACT,2001) and organizations such as Girls, Inc.
(Chen, Weiss, & Nicholson,2010). Educational systems have been a major site of YPAR in the
United States (Cammarota & Fine,2008; Kirshner,2007; Ozer & Douglas,2013). In other work
(Ozer,2016; Ozer et al.,2010), we used social-ecological and developmental theoretical frames
to consider how YPAR can help address the “developmental mismatch” of secondary schools
(Eccles & Roeser,2011) by promoting greater opportunities for youth agency and inuence
through meaningful roles in school governance (Ozer & Douglas,2013; Ozer & Wright,2012).
An important challenge for YPAR is embedding YPAR and related participatory youth
approaches into systems-change efforts to expand the impact on policies and practices that
affect youth development while simultaneously maintaining the integrity of YPAR’s key princi-
ples and rigor. In addition to the web platforms already discussed in this chapter, there are note-
worthy efforts under way to bring YPAR and other youth voice efforts to scale—some of which
rely on social media to connect youth across schools, communities, and even countries (Aven-
tura Social,2015; Kornbluh, Neal, & Ozer,2016). For example, UNICEF recently launched U
Report, a text message–based platform focused on engaging young people in developing coun-
tries to provide data on important issues.
In Australia, the Improving Children’s Lives Initiative at the University of Melbourne
formed a partnership with Behind the News, a children’s news program that is broadcast into
K–12 schools by the Australian Broadcast Commission (L. Gibbs, personal communication,
March 10, 2016; The University of Melbourne,2016). Behind the News has developed an inter-
active approach to news journalism with students. Working with University of Melbourne as a
research partner, the program will invite children to identify and respond to issues of concern
to them, and the university team will then analyze the responses and report back to students in
order to support further action.
Finally, another step that should aid the scaling of YPAR is the recent launch of the Kids in
Action network by the International Collaboration for Participatory Health Research (ICPHR)
to invite registration of participatory health research projects with children up to age fourteen
years to use a peer support process that will promote best practices and facilitate positive local
and collective outcomes (www.icphr.org/kids-in-action.html).
104 Community-Based Participatory Research for Health
CONCLUSION
This chapter provided an overview of YPAR’s key processes and phases, with a focus on illus-
trative examples from the United States and other countries, such as Guatemala, Brazil, Portu-
gal, and Australia, while identifying relevant curricular activities for each phase. We proposed
that YPAR has value in promoting positive youth development, particularly for the majority of
young people in the world who must negotiate racism, economic inequity, violence, and other
threats to their well-being. We suggested that the potential benets of YPAR are multidimen-
sional; it is not just an approach for strengthening young people’s learning and development
while improving community conditions but also for engaging young people’s expertise in
scientic inquiry about youth development and health. Finally, we considered current steps to
scale YPAR that aim to deepen its broad impact, capitalizing on social and web-based platforms
while seeking to maintain the integrity and spirit of the approach.
QUESTIONS FOR DISCUSSION
1. Considering the principles and complexities of YPAR, what might be some challenges to
conducting YPAR at scale with large numbers of students across communities, and what
current strategies and platforms are being used to help address these challenges?
2. Think about a school that you currently attend or did in the past. If you were to pick an
area to improve, what would be on your short list? Pick one to reect on in a YPAR thought
experiment. Drawing on the examples in the chapter, including web resources, consider
the stakeholders you would want to engage in this research and what kinds of research
designs and methods might generate actionable evidence to help support improvements.
ACKNOWLEDGMENTS
The rst author’s research on YPAR described here was supported by a William T. Grant
Scholars’ Award and the Centers for Disease Control and Prevention. The authors thank Michael
Bakal, Flavio Wittlin, and Lisa Gibbs for details about their work; Julia Levinson for research
assistance; the high school students who participated in YPAR projects; SF Peer Resources
(especially Elizabeth Hubbard, Gary Cruz, Adee Horn, Morgan Wallace, and Pui Ling Tam);
SFUSD for research collaboration; and the UC Berkeley student teams.
REFERENCES
Anyon, Y., Brink, K., Crawford, M., Fernández, M., Hofstedt, M., Osberg, J., & Strobel, K. (2007). Youth Engaged in Lead-
ership and Learning (YELL): A handbook for program staff, teachers, and community leaders. Stanford, CA: John W.
Gardner Center for Youth and Their Communities.
Aventura Social. (2015). Dream Teens. Retrieved from www.dreamteens-en.aventurasocial.com/
Berg, M., Coman, E., & Schensul, J. J. (2009). Youth action research for prevention: A multi-level intervention designed
to increase efcacy and empowerment among urban youth. American Journal of Community Psychology, 43, 345–359.
Breckwich Vásquez, V., Lanza, D., Hennessey-Lavery, S., Facente, S., Halpin, H. A., & Minkler, M. (2007). Addressing
food security through public policy action in a community-based participatory research partnership. Health Promotion
Practice, 8(4), 342–349.
Youth-Led Participatory Action Research (YPAR) 105
Brown, T. M., & Rodríguez, L. F. (2009). Youth in participatory action research. San Francisco, CA: Jossey-Bass.
Cahill, C., Rios-Moore, I., & Threatts, T. (2008). Open eyes-different eyes: PAR as a process of personal and social trans-
formation. In J. Cammarota & M. Fine (Eds.), Revolutionizing education: Youth participatory action research in motion.
New York, NY: Routledge.
Camino, L., & Zeldin, S. (2002). From periphery to center: Pathways for youth civic engagement in the day-to-day life of
communities. Applied Developmental Science, 6(4), 213–220.
Cammarota, J., & Fine, M. (Eds.). (2008). Revolutionizing education: Youth participatory action research. New York, NY:
Routledge.
Cargo, M., Grams, G., Ottoson, J., Ward, P., & Green, L. (2003). Empowerment as fostering positive youth development and
citizenship. American Journal of Health Behavior, 27(Supplement 1), S66–S79.
Center for Cities and Schools. (2016). Y-PLAN. Retrieved from http://y-plan.berkeley.edu/
Center for Regional Change. (2014). Welcome to the UC Davis Center for Regional Change. Retrieved from http://regional-
change.ucdavis.edu/
Chen, P., Weiss, F. L., & Nicholson, H. J. (2010). Girls Study Girls Inc.: Engaging girls in evaluation through participatory
action research. American Journal of Community Psychology, 46(1–2), 228–237.
Damon, W., Menon, J., & Cotton Bronk, K. (2003). The development of purpose during adolescence. Applied Developmental
Science, 7(3), 119–128.
Dangles, O., Carpio, F. C., Villares, M., Yumisaca, F., Liger, B., Rebaudo, F., & Silvain, J. F. (2010). Community-based par-
ticipatory research helps farmers and scientists to manage invasive pests in the Ecuadorian Andes. Ambio, 39(4), 325–335.
Eccles, J. S., & Roeser, R. (2011). Schools as developmental contexts during adolescence. Journal of Research on Adoles-
cence, 21, 225–241.
Fine, M. (2008). An epilogue of sorts. In J. Cammarota & M. Fine (Eds.), Revolutionizing education: Youth participatory
action research in motion (pp. 213–234). New York, NY: Routledge.
Generation Citizen. (2016). Generation Citizen. Retrieved from www.generationcitizen.org/
Holden, D., Evans, W. D., Hinnant, L., & Messeri, P. (2005). Modeling psychological empowerment among youth involved in
local tobacco control efforts. Health Education and Behavior, 32(2), 264–278.
Kirshner, B. (2007). Supporting youth participation in school reform: Preliminary notes from a university-community part-
nership. Children, Youth and Environments, 17(2), 354–363.
Kirshner, B. (2015). Youth activism in an era of education inequality. New York: New York University Press.
Kirshner, B., & Ginwright, S. (2012). Youth organizing as a developmental context for African American and Latino adoles-
cents. Child Development Perspectives, 6(3), 288–294.
Kohfeldt, D., Chhun, L., Grace, S., & Langhout, R. D. (2011). Youth empowerment in context: Exploring tensions in school-
basedyPAR. American Journal of Community Psychology, 47(1–2), 28–45.
Kornbluh, M., Neal, J. W., & Ozer, E. J. (2016). Scaling-up youth-led social justice efforts through an online school-based
social network. American Journal of Community Psychology, 57(3–4), 266–279.
Kornbluh, M., Ozer, E. J., Kirshner, B., & Allen, C. D. (2015). Youth participatory action research as an approach to socio-
political development and the new academic standards: Considerations for educators. Urban Review, 47(5), 868–892.
Langhout, R. D., Fernandez, J. S., Wyldbore, D., & Savala, J. (2015). Photovoice and house meetings as tools within partici-
patory action research. In L. A. Jason & D. S. Glenwick (Eds.), Handbook of methodological approaches to community-
based research: Qualitative, quantitative, and mixed methods (pp. 82–92). New York, NY: Oxford University Press.
Langhout, R. D., & Thomas, E. (2010). Imagining participatory action research in collaboration with children: An introduc-
tion. American Journal of Community Psychology, 26(1–2), 60–66.
Larson, R., Walker, K., & Pearce, N. (2005). A comparison of youth-driven and adult-driven youth programs: Balancing
inputs from youth and adults. Journal of Community Psychology, 33(1), 57–74.
London, J. (2001). Youth REP: Step by step: An introduction to youth-led evaluation and research. Oakland, CA:
Youth in Focus.
London, J., Zimmerman, K., & Erbstein, N. (2003). Youth-led research and evaluation: Tools for youth, organizational, and
community development. New Directions for Evaluation, 2003(98), 33–45.
Minkler, M., & Wallerstein, N. (2003). Introduction to community-based participatory research. In M. Minkler & N. Waller-
stein (Eds.), Community-based participatory research for health (pp. 3–26). San Francisco, CA: Jossey-Bass.
106 Community-Based Participatory Research for Health
Mirra, N., Garcia, A., & Morrell, E. (2015). Doing youth participatory action research: Transforming inquiry with researchers,
educators, and students. New York, NY: Routledge.
Mitra, D. L. (2004). The signicance of students: Can increasing student voice in schools lead to gains in youth development?
Teachers College Record, 106(4), 651–688.
Ozer, E. J. (2016). Youth-led participatory action research: Developmental and equity perspectives. In S. S. Horn, M. D. Ruck,
& L. S. Liben (Eds.), Advances in child development and behavior (pp. 189–207). Burlington, MA: Academic Press.
Ozer, E. J., Cantor, J. P., Cruz, G. W., Fox, B., Hubbard, E., & Moret, L. (2008). The diffusion of youth-led participatory
research in urban schools: The role of the prevention support system in implementation and sustainability. American
Journal of Community Psychology, 41(3–4), 278–289.
Ozer, E. J., & Douglas, L. (2013). The impact of participatory research on urban teens: An experimental evaluation. American
Journal of Community Psychology, 51, 66–75.
Ozer, E. J., & Douglas, L. (2015). Assessing the key processes of youth-led participatory research: Psychometric analysis and
application of an observational rating scale. Youth & Society, 47(1), 29–50.
Ozer, E. J., Newlan, S., Douglas, L., & Hubbard, E. (2013). “Bounded” empowerment: Analyzing tensions in the practice of
youth-led participatory research in urban public schools. American Journal of Community Psychology, 52(1–2), 13–26.
Ozer, E. J., Ritterman, M., & Wanis, M. (2010). Participatory action research (PAR) in middle school: Opportunities, con-
straints, and key processes. American Journal of Community Psychology, 46, 152–166.
Ozer, E. J., & Russo, I. (2016). Development and context across the lifespan: A community psychology synthesis. In
M. A. Bond, C. B. Keys, & I. Serrano-Garcia (Eds.), Handbook of community psychology (pp. 421–436). Washington, DC:
American Psychological Association.
Ozer, E. J., & Wright, D. (2012). Beyond school spirit: The effects of youth-led participatory action research in two urban
high schools. Journal of Research on Adolescence, 22(2), 267–283.
Roa García, C. E., & Brown, S. (2009). Assessing water use and quality through youth participatory research in a rural
Andean watershed. Journal of Environmental Management, 90(10), 3040–3047.
Sarason, S. B. (1996). Revisiting “The culture of the school and the problem of change.” New York, NY: Teachers College Press.
Schensul, J. L., Berg, M. J., & Sydlo, S. (2004). Core elements of participatory action research for educational empowerment
and risk prevention with urban youth. Practicing Anthropology, 26(2), 5–9.
Spencer, M. B., Fegley, S. G., & Harpalani, V. (2003). A theoretical and empirical examination of identity as coping: Linking
coping resources to the self processes of African American youth. Applied Developmental Science, 7(3), 181–188.
Stovall, D., & Delgado, N. (2009). “Knowing the ledge”: Participatory action research as legal studies for urban high school
youth. New Directions for Youth Development, 2009(123), 67–81.
The University of Melbourne. (2016). Children’s Lives Research Initiative. Retrieved from http://research.unimelb.edu.au/
hallmark-initiatives/childrens-lives-research-initiative—welcome
Watts, R. J., Diemer, M. A., & Voight, A. M. (2011). Critical consciousness: Current status and future directions. New Direc-
tions for Child and Adolescent Development, 2011(134), 43–57.
Wilson, N., Dasho, S., Martin, A., Wallerstein, N., Wang, C., & Minkler, M. (2007). Engaging young adolescents in social
action through photovoice: The Youth Empowerment Strategies (YES!) project. The Journal of Early Adolescence,
27(2), 241–261.
Youth IMPACT. (2001). Youth voices inspiring creative change. Retrieved from www.whatkidscando.org/archives/images/
studentwork/YouthImpactReport.pdf
YPAR Hub. (2015). Investigate. Retrieved from http://yparhub.berkeley.edu/investigate-curriculum/
Zeldin, S., Christens, B. D., & Powers, J. L. (2013). The psychology and practice of youth-adult partnership: Bridging gen-
erations for youth development and community change. American Journal of Community Psychology, 51(3–4), 385–397.
8
CHAPTER
PARTNERSHIP, TRANSPARENCY,
AND ACCOUNTABILITY
CHANGING SYSTEMS TO ENHANCE RACIAL
EQUITY IN CANCER CARE AND OUTCOMES
EUGENIA ENG, JENNIFER SCHAAL, STEPHANIE BAKER, KRISTIN BLACK,
SAMUEL CYKERT, NORA JONES, ALEXANDRA LIGHTFOOT, LINDA ROBERTSON,
CLEO SAMUEL, BETH SMITH, AND KARI THATCHER
AS NOTED BY the Sullivan Commission (Sullivan,2004), many visible racial barriers of the
US health care system were eradicated by the civil rights era, but today’s effects from insti-
tutional racism are subtle and require careful recognition. Institutional racism is a process of
advantage and oppression, conscious or not, functioning as “a system of structuring opportunity
and assigning value based on race phenotype, that unfairly disadvantages some..., unfairly
advantages others..., and undermines the...potential of the whole society...” (Jones,2003,
p. 10). Race, a biologically specious construct, does little to describe the specic origins and
causal pathways of race-specic inequities in quality and completion of health care (Williams &
Rucker,2000).
Despite decades of documenting racial disparities in cancer survival in the United States,
variations in treatment persist. African American breast cancer patients continue to initiate
treatment later (Gorin, Heck, Cheng, & Smith,2006) and receive less treatment than their white
counterparts (Bickell et al.,2006; Hershman et al.,2005; Voti et al.,2006). Non–small cell lung
108 Community-Based Participatory Research for Health
cancer represents more than 80 percent of all cases (Jemal et al.,2007), and the only reliable
curative treatment for it is surgical resection, with ve-year survival rates at about 50 percent
for localized disease and 21 percent for regional (Ries et al.,2007). Alone or in consultation
with their physicians, 24 percent of white patients and 36 percent of African American patients
with Stage 1 or 2 disease decide not to pursue surgical resection (Bach, Cramer, Warren, &
Begg,1999; Cykert et al.,2010; Farjah et al.,2009) treatment. Patients who do not undergo
appropriate lung resection surgery are limited to a median survival rate of less than one year
(Bach et al.,1999). This racial variation in surgery has been directly linked to excess lung can-
cer mortality (Bach et al.,1999).
Although used for decades by community organizers working for civil rights and social
change, the relevance of the antiracism framework to health care inequity has rarely been exam-
ined or applied to health systems change. This chapter is a case study of building a community-
academic-health agency research partnership on antiracism training and collaborative processes
within two cancer centers located in Greensboro, North Carolina, and Pittsburgh, Pennsylvania.
Emphasis is given to how our partnership identied system-level barriers to transparency and
accountability for racial equity in quality and completion of cancer care, which informed our
design and testing of a system change intervention at both cancer centers. Finally, we offer
insights on the potential of integrating CBPR principles and an antiracism framework as a part
of the growing system change movement within US medical care and the National Institutes of
Health (NIH).
HISTORY OF THE INTERSECTION OF CBPR AND ANTIRACISM
TRAINING IN GREENSBORO
Citizens of Guilford County, North Carolina, have played a pivotal role in this nation’s history
of civil rights. On February 1, 1960, four students from NC A&T University conducted the rst
lunch counter sit-in. Also in Guilford County, Dr. George Simkins Jr. led African American doc-
tors, dentists, and patients to prosecute the largest white-owned and white-serving-only hospital
in the county, Moses Cone Memorial Hospital, for discrimination by maintaining racially sep-
arate medical facilities with taxpayers’ money. The 1963 Simkins v. Cone Health decision
marked the rst time that federal courts applied the Equal Protection clause of the Fourteenth
Amendment to prohibit racial discrimination by a private entity (Powell,2006). The following
year, Congress passed the Civil Rights Act of 1964, ofcially prohibiting private discrimination
in public places.
The county seat is Greensboro, with a population of 282,586 (2014 estimate): 48.4 percent
of residents are white and 40.6 percent are African American; 87.7 percent of residents have at
least a high school diploma, and 35.7 percent have a bachelor’s or higher degree. About one in
ve Greensboro residents (20.3 percent) live below poverty (US Census Bureau,2015).
In 1997, The Partnership Project (TPP) was formed by three local organizations: Project
Greensboro, Guilford College, and the City of Greensboro. TPP’s mission was to deepen the
capacity of fragile neighborhoods to take responsibility for community improvement. TPP’s
rst director encouraged board members and staff members to attend the People’s Institute
for Survival and Beyond (PISAB) antiracism training in New Orleans to better understand
the history of racism in the United States and address its current institutional manifestations.
Partnership, Transparency, and Accountability 109
The PISAB’s two-day training focuses on a racial analysis of how and why institutions from
all sectors in our society interact in maintaining a race-based hierarchy. The rationale is that
gatekeepers from institutions work for equity with different understandings of racism, relying
on discipline-specic frameworks, personal feelings, and popular opinion. A gatekeeper is
anyone who works in an institution and has the power to give and deny access to their institu-
tion’s resources or equity—ranging from information and services to use of the bathroom key.
Regardless of the size of the gate, it is not owned by the gatekeepers but by the institution.
Gatekeepers, however, are in control of who has access and when, by virtue of their work or
personal relationship with patients and clients. Using this racial analysis, participating organiza-
tions establish a common lens and vocabulary to (1) critically analyze structural issues of race
and class, rather than characteristics of individuals and groups, and (2) address the explicit and
subtle ways that racialized patterns in American history, culture, and policies permeate struc-
tures and practices within and across systems, such as education, criminal justice, and health
care, which create and sustain inequities (www.pisab.org).
TPP organized to bring the PISAB training to Greensboro. The rst training was sponsored
in 1997. The PISAB analysis took root and local community members built on it forming the
Racial Equity Institute (REI), which now conducts quarterly trainings in Greensboro. Although
TPP began as a community-building organization, introduction to PISAB’s racial analysis
transformed TPP to an antiracism training organization with the mission to educate community
members and organizational leaders in understanding institutional racism and development of
strategic actions to benet communities. In 2007, TPP was reorganized as a 501(c)3 corporation.
TPP’s mission was validated with empirical ndings published in the Institute of Medicine
(IOM) report, Unequal Treatment (Smedley, Stith, & Nelson,2003). Reviewing ten years of
studies on patient and provider attitudes, expectations, and behaviors, the IOM panel concluded
that race and ethnicity of patients remained signicant predictors of the quality of health care
received, even after accounting for access to care and issues that arise from differing socio-
economic conditions. The panel offered recommendations for system-change improvements
in medical care nancing, allocation of care, availability of language translation, community-
based care, and others.
Bolstered by these ndings, TPP leaders sought funding from the Moses Cone-Wesley Long
Community Health Foundation to build a coalition grounded in antiracism training and driven
by community voices to address health inequities in Greensboro. The foundation encouraged
TPP to approach the UNC’s School of Public Health to recruit academic researchers for future
collaboration. TPP invited faculty members Geni Eng and Anissa Vines and postdoctoral fellow
Derek Grifth, given their record of CBPR health inequities research. Together, they applied
successfully for an eighteen-month planning grant, awarded by the foundation in 2004 to TPP
with a subcontract to UNC (Yonas et al.,2006). After eighteen months, thirty-four persons (50
percent community-based, 50 percent representing health agencies and academic institutions)
had completed antiracism training, signed a “full-value contract” formalizing a commitment to
shared goals, expectations, and values for working together and an agreement that all products
generated, research or otherwise, belong to the group.
After completing training on how to apply for NIH funding, and on CBPR, the newly
formed collaborative agreed to focus on documenting race-specic inequities in the local cancer
care system, applying for an R21 for formative research to the National Cancer Institute (NCI).
110 Community-Based Participatory Research for Health
We established ourselves as the Greensboro Health Disparities Collaborative (GHDC) with the
mission to create structures and processes that respond to, empower, and facilitate communities
in dening and resolving issues related to disparities in health. Working in subcommittees, we
designed the Cancer Care and Racial Equity Study (CCARES), which NCI funded in 2006 to
answer the following research questions:
Did African American and White women with breast cancer in Guilford County, North
Carolina, receive treatment at Cone Cancer Center that was the same?
If the breast cancer care was not the same, how was it different and what could have been
the reasons?
It is noteworthy that although the executive vice president of the Cone Health System had
reviewed our CCARES application and submitted a letter of support for providing access to the
facility’s breast cancer patients and cancer registry database, the Cone Health Cancer Center
(CHCC) was not yet a health agency partner with GHDC and UNC, although GHDC mem-
bers included physicians and nonclinical staff members employed by Cone Health. Hence,
GHDC orchestrated a community press conference to announce NCI funding of CCARES and
invited Cone Health’s vice president for oncology services and the CHCC medical director.
Both attended the press conference, recognized the potential implications of CCARES ndings
for their cancer center, requested to join GHDC, and completed the two-day antiracism training.
ENGAGING CANCER CENTERS AS EQUAL PARTNERS
IN SYSTEM CHANGE RESEARCH FOR HEALTH EQUITY
CCARES’ formative research ndings revealed a six-month delay in reporting cancer registry
data to CHCC staff. Registry data revealed racial differences in histological tumor grade, sur-
gical outcomes, insurance status, and physician recommendation of hormone therapy, chemo-
therapy, and radiation therapy (Yonas, Aronson, Schaal, et al.,2013). Associations with racial
differences in treatment outcomes could not be examined because cancer registry data did not
include hormone receptor status, patient refusal of treatment, dates for initiating and discontinu-
ing or completing treatment, or discontinuing follow-up care. Cone Health’s cancer care system
lacked transparency on equity in quality and completion of care. Additionally, critical incident
interviews with white (n = 27) and African American (n = 23) breast cancer patients treated at
CHCC during the same period revealed 861 specic encounters described as having an impact,
positive and negative, on their cancer care experience (Yonas, Aronson, Schaal, et al.,2013).
Subtle but important racial differences on the impact from patient encounters within the cancer
care system indicated lack of accountability for equity in quality of care. Implications from
CCARES ndings suggested the need for a prospective study to monitor each patient encounter
during treatment, by race, to identify systemic causes for less than optimal care for African
American patients.
Following the CBPR approach, GHDC presented and discussed the implications of
CCARES ndings to the fty breast cancer survivors interviewed and CHCC administrators and
clinicians before disseminating to the public. With a small grant from a local foundation, GHDC
and UNC sponsored a private dinner for interviewees, a private meeting with CHCC staff mem-
bers, and a public forum at the public library in Greensboro. Among the benets of a separate
Partnership, Transparency, and Accountability 111
meeting with CHCC staff members was the opportunity for the medical director and vice
president for oncology services to commit to serving as an equal partner with GHDC and UNC
in designing a follow-up system-change intervention study, informed by CCARES ndings,
and applying for NCI funding through the RO1 mechanism. During this period between fund-
ing, GHDC continued to meet monthly, planning and conducting activities toward achieving its
mission, including academic and community presentations, developing community outreach,
support of academic partners and their students, and establishing Sisters Network Greensboro
(SNG), a local chapter of a national survivorship organization for African American breast can-
cer survivors.
THE SYSTEM CHANGE STUDY: ACCOUNTABILITY FOR CANCER
CARE THROUGH UNDOING RACISM AND EQUITY (ACCURE)
In 2009, Dr. Yonas, the postdoctoral fellow integrally involved with CCARES, accepted a fac-
ulty position with the University of Pittsburgh Medical Center (UPMC) and recruited that can-
cer center as a CBPR partner to serve as the second site for the study. Our partnership submitted
two RO1 applications to NCI. The second was revised, resubmitted, and funded in 2012.
Applying CBPR Principles to Prepare for Resubmitting Application
To organize for the resubmission to NCI, we divided into writing groups to revise specic sec-
tions, including specic aims, signicance, preliminary studies, intervention, and research
strategy. Following CBPR principles, each group included a representative from each of our
academic, community, and cancer center partners. We held weekly conference calls to appraise
one another on progress in thinking, and co–principal investigator (co-PI) Eng served as the
coordinator for synthesizing written texts.
ACCURE System Change Study Design
ACCURE’s research question was, “What are the structures built into cancer care systems that
trigger vulnerabilities to implicit bias, and how can they be changed to reduce race-specic
inequities in quality and completion of breast and lung cancer care?” Our ACCURE interven-
tion study directed public health and translational clinical research attention to the concepts of
transparency and accountability as mechanisms of systems change to achieve racial equity in
cancer care.
We conducted a ve-year study using interrupted time-series design, with an embedded
randomized control trial (RCT) to test the effectiveness of the ACCURE intervention on opti-
mizing therapy and narrowing treatment disparities between white and African American
patients with a rst diagnosis of Stage 1–2 breast and lung cancer receiving treatment at Greens-
boro’s CHCC and the UPMC Cancer Center that contribute to excess mortality. For the RCT,
a cohort of 150 Stage 1–2 breast and Stage 1–2 lung cancer patients from the two centers were
randomized to the ACCURE navigator or usual care navigator.
The ACCURE intervention had two transparency (1 and 2) and two accountability (3 and 4)
components: (1) an analysis of power and authority with cancer patients, (2) health care equity
education and training (HEET) quarterly sessions with oncology providers and staff members,
(3) a full-time ACCURE navigator at each center to act as a two-way communication bridge
112 Community-Based Participatory Research for Health
between patients and their encounters with the cancer care system, and (4) race-specic clini-
cian feedback to physician champions (one for breast and one for lung cancer) at each cancer
center. Components (3) and (4) used a real-time warning system derived from electronic health
records that immediately indicated if a patient either missed an appointment or did not reach
expected milestones in care.
As a rst step in launching ACCURE, GHDC members were offered alternate human sub-
jects research ethics training, developed and approved by UNC’s institutional review board (IRB)
for nontraditional investigators (Yonas, Aronson, Coad, et al.,2013). This training provided a
community-friendly set of slides that covered the human subjects protections content of the
web-based collaborative institutional training initiative and was delivered by an ACCURE co-PI
with examples specic to ACCURE. Twenty-six GHDC members completed the training, indi-
cating strong community interest in contributing to ACCURE’s implementation. Their names
and contact information were entered into the UNC IRB database. Being trained and certied
enabled community members of GHDC to actively engage in all data collection and analysis
throughout the ACCURE study. By ensuring community input alongside academic and can-
cer center input, the authenticity of data and the relationships among ACCURE partners were
enhanced and strengthened. The ACCURE grant was administered by a steering committee
with representatives from all academic, community, and cancer center partners who met weekly
via conference calls and reported monthly to the GHDC.
Transparency Intervention Components
The antiracism training that is foundational to the GHDC posits that lack of transparency and
accountability are the mechanisms that prevent systems from adequately addressing racial dis-
parities. We began ACCURE by exploring the functioning of the system to make it transparent
to the investigators.
Analysis of Power and Authority To understand similarities and differences in the delivery
of cancer care between the two centers, our intervention began with ACCURE staff members
shadowing usual-care nurse navigators for breast and lung cancer patients at each cancer center.
From these observations and personal experiences, members of GHDC and SNG developed a
visual representation of the cancer care system for ACCURE’s “power analysis,” an antiracism
diagnostic tool that examines the origins and pathways within “systems of power and authority”
that produce inequity. Figure8.1 is the resulting diagram of the cancer care system, used during
small-group discussions with white and African American cancer patients on encounters with
gates and gatekeepers that encouraged or discouraged them from continuing their care.
For ACCURE’s focus groups, we recruited forty-two white and African American patients
who initiated treatment in January–December 2011 for their rst diagnosis of Stage 1–2 breast
or lung cancer at both cancer centers. Eligible participants, grouped by race, gender, and type of
cancer, received a $15 incentive for a ninety-minute session to discuss these questions: “During
your treatment these past [three or six] months, what were the things that were done—or not
done—that made you think you were getting treated well? That made you think you were not
getting treated well?” Two racially concordant TPP consultants, experienced in conducting a
power analysis, served as the moderator and note taker at both sites. Discussions were digitally
recorded and transcribed verbatim.

Partnership, Transparency, and Accountability 113
For the analysis, eight pairs of academic and community partners were trained to code all
transcripts. A small group of community and academic partners then used Atlas.ti, a text anal-
ysis software, to enter and retrieve coded text from verbatim transcripts and compare power
analysis ndings, by race and site, to identify “pressure point encounters.” The greater the
overlap in pressure point encounters reported by patients, the stronger the association by race
on timely initiation of recommended care, adherence to, and completion of care (see Schaal
et al.,2016, for more details). The ndings from this power analysis were used to inform the
remaining three components of ACCURE’s intervention.
Healthcare Equity Education and Training (HEET) Sessions For system-wide application of
ndings from the power analysis on origins and pathways that undermine racial equity in cancer
care, we offered quarterly one-hour HEET sessions for certied continuing education credit to
TREATMENT
OTHER EXPERIENCES
PRIMARY CARE/GYN
DIAGNOSIS
Experience with Surgery
Follow Up Imaging / X-rays
Emergency Room Visits
Complications
Telephone
Communications
Support Groups
Screening/Chest X-ray /
Mammogram
Symptoms / Mass
Referral to Specialist
CT Scan / MRI /
Needle Biopsy
“The Phone Call”
or Office Visit
Radiation Oncology
Radiation Oncologist
Radiation Treatment
Testing/Diagnostic
Mammogram
Surgeon
Hospital Staff
Hospital Facility
Oncology Center
Front Desk
Nursing Staff
Laboratory
Navigator
Medical Oncology
Medical Oncologist
Chemotherapy
Chaplain
Social Worker
Other Support Services
Billing Process/Personnel
FIGURE 8.1 Cancer Journey Diagram
Note: The cancer journey diagram, developed by GHDC and Sisters Network Greensboro, a local afl-
iate of a national African American breast cancer survivorship organization, was a focal point for power
analysis discussions and data analysis. It depicts a patient’s journey through cancer care, beginning in the
community, from diagnosis through therapy and return to the community following treatment.

114 Community-Based Participatory Research for Health
cancer center staff members at each site, beginning in year 2. These sessions presented and dis-
cussed principles gleaned from antiracism trainings and shared intermediate ACCURE ndings
by race on missed appointments, delays on treatment initiation, and premature discontinuation
of recommended therapies. In addition, HEET sessions educated staff members regarding their
roles as gatekeepers within their institutions.
A HEET planning committee, including representatives from TPP, REI, and ACCURE
staff members from each cancer center, was responsible for publicizing, evaluating, designing
the content, and selecting REI, community, and academic presenters. Figure8.2 displays the
content. We had projected that 50 percent of staff members at each cancer center would have
attended HEET sessions by the end of the intervention. However, differences in the dissemina-
tion of information within an academic hospital versus a community hospital required modi-
cations in the delivery format.
Accountability Intervention Components
In addition to transparency, systems must be accountable to their constituents to achieve equity.
By establishing mechanisms for accountability, the health care system can begin to address
racial disparities.
ACCURE Navigator Review of job descriptions for cancer patient nurse navigators at both can-
cer centers revealed variation in educational backgrounds (e.g., high school diploma, RN) and
SESSION I:
Exercise in shifting the
paradigm and thinking
outside the box about
causes of cancer health
outcomes
Examine the role of
gatekeeping in more
depth
Examine manifestations
of implicit bias in their
own cancer center
through gatekeeping
Examine race-specific findings from their
own cancer center’s past cancer registry
data and engage staff members in “power
analysis” of their own system of cancer
care
Examine race-specific
findings from their own
cancer center’s
patients’ “power
analysis”
Introduce concepts of
implicit bias
SESSION II:
SESSION III:
SESSION IV:
Overview of
ACCURE
Healthcare
Equity
Education and
Training
SESSION V:
SESSION VI:
FIGURE 8.2 Healthcare Equity Education and Training Sessions
Partnership, Transparency, and Accountability 115
scope of responsibilities. The range of duties included direct patient contact, initial greeting and
comfort care, social work tasks, follow-up to missed appointments, administrative responsibil-
ities, and tasks related to protection of the institution.
Our grant complemented the usual care offered by a navigator by hiring and training an
ACCURE navigator to serve as a two-way communication bridge to optimize accountability for
(1) hearing how patients understand (health literacy) and how patients feel (medical mistrust)
about the plan of care outlined for them and the policies and procedures they had recently and
were currently encountering, (2) eliciting patient suggestions for reducing the impact of negative
experiences, and (3) communicating solutions back to the cancer center. The ACCURE navi-
gator was an experienced cancer care provider and educator with a bachelor’s degree in nursing.
We provided training designed to address specic issues interfering with completion of care
that were uncovered by our previous studies and patient focus groups. Whereas the job descrip-
tions for usual care navigators involved a reactive posture to respond to expressed patient con-
cerns, the ACCURE navigator proactively reviewed the care plan with the patient face-to-face at
the initiation of care and by telephone every two months thereafter. The purpose was to solicit
patient understanding and specically address questions and concerns raised by patients before
a break in care occurs (i.e., before an appointment is missed). In addition to antiracism training,
the ACCURE navigator was trained in the “ask-advise-assist” counseling technique to conrm
patients’ understanding of prognosis, treatment, and the follow-up care process.
To work system-wide, the ACCURE navigator was trained to use our specially devel-
oped automated real-time registry (RTR). RTR is a digital uploading process through which
the ACCURE navigator obtained visit and procedure appointments for all consented patients.
Automated warnings were transmitted to the navigator if a patient missed an appointment or
an anticipated treatment milestone did not occur. With the warning trigger, the ACCURE navi-
gator would contact the patient to address concerns or barriers related to missed appointments.
For missed milestones, the care team, often using the ACCURE physician champion, would be
informed and discussions would ensue on fullling the milestone.
Available as a resource to the ACCURE navigator at each cancer center were two oncol-
ogists (one for lung and one for breast cancer) designated as physician champions not only
for their clinical expertise but also to assist in following up with providers when patients miss
milestones in care. Because the ACCURE navigator and physician champions at each cancer
center attended weekly clinical breast and thoracic oncology conferences, they brought RTR
warnings, alerts, and patient insights directly to the clinical team regarding the lack of expected
care progress for resolution in real time. The combination of accrued RTR data and ndings
from the analysis of power and authority were used to inform HEET sessions and the clinical
performance reports, described in the following section.
Race-Specific Clinical Performance Reports (CPRs) In recent years, ACCURE’s two cancer
centers installed electronic medical record (EMR) software, designed specically for med-
ical oncology, providing a clear, fast, and exible means of documenting patient information
throughout the medical assessment and chemotherapy administration process. With the ability
to include diagnostic images, lab results, full-featured scheduling, and external documentation,
the software could provide (1) a complete picture of patient care and (2) generate a clinician
worksheet to help medical oncologists efciently plan, accurately order, and carefully monitor
the chemotherapy process.
116 Community-Based Participatory Research for Health
EMR data through successive denitions of meaningful use enabled real-time identication
by ACCURE of patients who, through non-adherence, misperception, or nonstandard recom-
mendation, fell out of accepted parameters of care. Table8.1 displays the parameters dened for
ACCURE with structured data that were pulled by automated reports. We used date of patho-
logic diagnosis or abnormal chest computerized tomography as the initiating trigger, determined
reasonable parameters for therapeutic starting points, and incorporated accepted standards of
care for effective therapy to dene milestones and outcomes.
From these data, each cancer center generated CPRs that were specic to the institution as
a whole. Each CPR presented race-specic data as shown in Table8.1 on patients treated that
time period, aggregated for all providers. Data from CPRs were disseminated quarterly through
ACCURE’s HEET sessions.
RESULTS AND LESSONS LEARNED
At the time of this writing, ACCURE is in its fth and nal year, and we are still completing our
analyses of process and outcome evaluation data. Presented here are the outcome results from
our embedded RCT of the ACCURE navigator intervention component with early-stage lung
cancer patients.
ACCURE achieved parity that narrowed historical racial gaps in treatment and, at the same
time, raised treatment completion rates for both races. We compared race-specic rates of com-
pleting potentially curative treatment (e.g., stereotactic body radiation or surgical resection)
within four months of diagnosis of (1) 2,044 baseline patients at both cancer centers, who had
received treatment, 2007–2011, before ACCURE began; (2) 393 patients randomly assigned to
“usual care navigators,” and (3) one hundred patients randomly assigned to the ACCURE nav-
igators. Table8.2 displays the results. Among baseline patients, we found a signicant racial
gap of 76 percent white versus 64 percent African American (p < .05) who received potentially
curative lung cancer treatment. Among patients assigned to ACCURE navigators, this eleven
percentage point racial gap disappeared; 96 percent of white (n = 75) and African American
(n = 25) patients completed potentially curative treatment. Among the “usual care navigator”
patients, we also saw a signicant improvement (p < .05) in completion of potentially curative
care, when compared to baseline. This nding may be the result of a spillover effect at the two
cancer centers, whereby ACCURE navigator sensibilities and training may have inuenced staff
members outside of the project.
At a monthly GHDC meeting, one of ACCURE’s physician champions, Dr. Matthew
Manning, proposed submitting an abstract on these ndings to be presented at the 2016 annual
meeting of the American Society for Thoracic Radiation Oncology (ASTRO). He obtained
approval from the GHDC Publications and Dissemination Committee, and several GHDC
members served as coauthors. ASTRO accepted the abstract and designated it to be one of
three presentations to receive a press conference. At a subsequent GHDC monthly meet-
ing, Dr. Manning presented the PowerPoint slides, rehearsed the presentation, and received
substantive constructive feedback from community and academic members on terminology
used to describe the science and practice of ACCURE’s intervention and the logical progres-
sion of the “story” to be told about ACCURE’s CBPR approach. (For further information on

Partnership, Transparency, and Accountability 117
TABLE 8.1 Breast and Lung Cancer Treatment Outcome Measures
Outcome Measure Cancer Diagnosis Definition
Adequate completion of
chemotherapy treatment
Breast Yes, if 80 percent of chemotherapy
visits were completed
No, otherwise
Stage 1b or 2 lung Yes, if three out of four chemotherapy
visits were completed
No, otherwise
Surgery completed Lung Yes, if surgery completed within four
months of diagnosis
No, otherwise
Adherence to medical
oncology follow-up
appointments
Stage 1 and 2 breast
and lung
No, if three consecutive missed
appointments
Yes, otherwise
Days to treatment initiation Breast Number of days from diagnosis to
chemotherapy treatment initiation
Treatment started on time Breast or lung Yes, if chemotherapy started within
120 days of diagnosis (date of
path report)
No, otherwise
Surgery completed Breast Number of days from diagnosis
to surgery
Start radiation therapy Breast with lumpectomy
(not mastectomy)—
younger than age seventy
Yes, if patients start treatment
No, otherwise
Completed radiation therapy Breast with lumpectomy
(not mastectomy)—
younger than age seventy
Yes, if 80 percent of
sessions completed
No, otherwise
Adequate completion of
chemotherapy treatment
Stage 3 colon Yes, if six treatments completed within
six months diagnosis
No, otherwise
Note: Primary outcomes in italics text.
118 Community-Based Participatory Research for Health
Dr. Manning’s presentation see www.medscape.com/viewarticle/869840?nlid=109754_2981
&src=wnl_dne_161006_mscpedit&uac=241217HR&impID=1210188&faf=1.) As a result of
this preliminary success, additional system changes are being considered at Cone Health, for
example, identifying potential transparency and accountability factors to racial differences in
receiving low-dose CT scan screening for lung cancer.
Who beneted? By joining the principles of antiracism with CBPR in a clinical trial of a
system change intervention, quality and completion of treatment was improved for early-stage
cancer patients of all races. To achieve equity for African American patients, our intervention
was intentionally focused on enhancing the cancer care system’s transparency and account-
ability for the quality and completion of treatment received by African American patients. At
both cancer centers we introduced innovations in (1) health care informatics that analyzed their
own data by race (i.e., RTR, CPRs) and (2) patient-centered communication structures that
were informed by antiracism training (i.e., specially trained nurse navigators and physician
champions and HEET sessions for all staff members). Our preliminary outcome data indicate
that, through systems change, all early-stage lung cancer patients beneted, achieving parity
with 96 percent completing potentially curative treatment within four months of diagnosis.
Although ndings from our process evaluation are promising, we note differences in the
type of staff members who attended HEET sessions. At the cancer center afliated with an
academic teaching hospital, HEET sessions were offered during grand rounds, and HEET par-
ticipants were primarily physicians. The other cancer center was a regional hospital that did
not offer grand rounds, and HEET sessions were presented at the end of a workday and were
attended by nurses, social workers, and other auxiliary staff members. We had intended to reach
at least 50 percent of staff members at each cancer center with HEET sessions, but we had not
anticipated how the preexisting culture and different structures for continuing education would
shape participation.
What were the challenges and lessons learned? Our GHDC partnership and ACCURE
research team were fully aware that securing NIH funding for a longitudinal clinical trial of a
systems-change intervention to eliminate persistent racial inequities in cancer outcomes within
medical care settings was a lofty goal. Nonetheless, we were certain that we could offer, at the
very least, lessons learned on the dynamics of attempting to integrate the CBPR approach into a
broader antiracism movement that would be relevant for achieving health equity.
TABLE 8.2 Early Stage Lung Cancer Treatment Rates (Stereotactic Body Radiation
Therapy and Surgical Resection) by Race and ACCURE Intervention Arm, by Percent
Race
Baseline:
R + SBRT
Baseline:
R
ACCURE:
R + SBRT
ACCURE:
R
Usual Care:
R + SBRT
Usual Care:
R
Black 64 55 96
a
80
a
85
a
57
White 76 61 96
a
79
a
87
a
55
R = surgical resection.
a
p < .05 compared with baseline.
Partnership, Transparency, and Accountability 119
One lesson is to nd a balance between following the details of CBPR while not losing sight
of the long-term vision of challenging the overarching context of antiracism. It was essential for
us to recognize that GHDC’s antiracism mission is broader than ACCURE’s specic aims. Any
study conducted by GHDC is a means toward an end. Although ACCURE established a steering
committee who met weekly to guide administration and management of study activities and
the budget, the nal decision-making power rested with GHDC members on deviations from
the initial proposal, personnel changes, interpretation of ndings, publications and presenta-
tions, and proposed supplements. At the same time, GHDC leaders observed that the agendas
for monthly GHDC meetings were so focused on the CBPR details of ACCURE that GHDC’s
antiracism mission was becoming eclipsed. As a solution, each GHDC meeting begins with a
cochair raising a current societal event that is relevant to antiracism, ranging from voter registra-
tion to House Bill 2 in NC. In addition, bimonthly, short interactive exercises are designed and
presented by GHDC’s outreach committee on antiracism issues, such as microaggressions or a
time line of our family’s cultural roots.
A second lesson is to negotiate the balance of community and academic members in a
long-term CBPR partnership. Over time, because of the innovative nature of this work, GHDC
has drawn more and more membership from academic institutions. Additionally, community
members have developed research experience and have been hired into institutional roles dur-
ing ACCURE, subtly shifting the balance of voices around the table. As a result, GHDC is
engaged in an ongoing conversations about who among us is, and is not, currently in a position
to authentically speak from a community perspective. This question dees a categorical answer
and charges us to use the analysis of power and authority as a mirror to reect on our partner-
ship and our gatekeeping.
A third lesson is to anticipate the gatekeeping role of academic CBPR partners during
the post-award period. After receiving funding for ACCURE, it was essential for us to recog-
nize that ACCURE’s subcontracts between UNC and the two cancer centers were “business as
usual,” whereas, the subcontract with TPP, ACCURE’s community-based organization partner,
was not. With minimal cash ow and one part-time accountant, TPP has limited resources to
adjust to changes in policies and procedures from NIH (e.g., new conditions for reconciling
cash advances versus invoicing for reimbursing receipts), UNC’s Ofce of Sponsored Research
(e.g., newly required criminal background checks for paying community consultants), and
UNC’s IRB (e.g., no longer allowing cash incentives for participants and mandating gift cards
for which merchants can demand a photo ID with no legal basis). Such adjustments placed extra
burdens on ACCURE’s project manager and co-PIs, who served as gatekeepers faced with the
dilemma of how to serve as advocates for TPP, UNC, or both. Details on ACCURE’s solutions
can be found in Academic Researcher’s Guide for Pre- and Post-Award Grants Management
When Conducting Community Engaged Research (https://tracs.unc.edu/docs/cares/CAGAT_
Academic_Researchers_Guide_v20150929.pdf). This guide was designed for academic
researchers at UNC interested in gaining a greater understanding of, and information about,
the grant submission and management process when conducting federally funded community-
engaged research.
In conclusion, this case study of ACCURE is built on an understanding of the importance of
structural racism and the integration of antiracism training and collaborative processes of CBPR
within the two cancer centers. We have described and reected on how involving cancer center
120 Community-Based Participatory Research for Health
providers and staff members to join a thirteen-year-old CBPR partnership, grounded in anti-
racism training and CBPR, enabled us, in general, to investigate race-specic patient experiences
with quality and completion of cancer care and, in particular, to uncover and address major bar-
riers for African American patients.
QUESTIONS FOR DISCUSSION
1. The ACCURE case study is focused on the health care system. Which concepts, methods,
and lessons learned from ACCURE would be relevant for addressing inequities within
other systems, such as education, criminal justice, social welfare, and for-prot business?
2. The authors refer to gatekeeping roles among health care staff within a cancer center and
partners within a CBPR partnership. Thinking back to your own experiences, how have
you served as a gatekeeper? Moving forward, how do you foresee yourself, as an enlight-
ened gatekeeper, to use your power and accountability for breaking down health inequities?
REFERENCES
Bach, P. B., Cramer, L. D., Warren, J. L., & Begg, C. B. (1999). Racial differences in the treatment of early-stage lung cancer.
New England Journal of Medicine, 341, 1198–1205.
Bickell, N. A., Wang, J. J., Oluwole, S., Schrag, D., Godfrey, H., Hiotis, K., Mendez, J., & Guth, A. A. (2006). Missed oppor-
tunities: Racial disparities in adjuvant breast cancer treatment. Journal of Clinical Oncology, 24, 1357–1362.
Cykert, C., Dilworth-Anderson, P., Monroe, M. H., Walker, P., McGuire, F. R., Corbie-Smith, G., Edwards, L. J., & Bunton,
A. J. (2010). Modiable factors associated with decisions to undergo surgery among newly diagnosed patients with early
stage lung cancer. Journal of the American Medical Association, 303, 2368–2376.
Farjah, F., Wood, D. E., Yanez, N. D., III, Vaughan, T. L., Symons, R. G., Krishnadasan, B., & Flum, D. R. (2009). Racial
disparities among patients with lung cancer who were recommended operative therapy. Archives of Surgery, 144, 14–18.
Gorin, S. S., Heck, J. E., Cheng, B., & Smith, S. J. (2006). Delays in breast cancer diagnosis and treatment by racial/ethnic
group. Archives of Internal Medicine, 166, 2244–2252.
Hershman, D., McBride, R., Jacobson, J. S., Lamerato, L., Roberts, K., Grann, V. R., & Neugut, A. I. (2005). Racial disparities
in treatment and survival among women with early-stage breast cancer. Journal of Clinical Oncology, 23, 6639–6646.
Jemal, A., Siegel, R., Ward, E., Murray, T., Xu, J., & Thun, M. J. (2007). Cancer statistics, 2007. CA: A Cancer Journal for
Clinicians, 57, 43–66.
Jones, C. P. (2003). Confronting institutionalized racism. Phylon, 50(1–2), 7–22.
Powell, W. (2006). Encyclopedia of North Carolina. Chapel Hill, NC: University of North Carolina Press.
Ries, L.A.G., Melbert, D., Krapcho, M., Mariotto, A., Miller, B. A., Feuer, E. J., & Reichman, M. (2007). SEER cancer
statistics review, 1975–2004. Bethesda, MD: National Cancer Institute. Retrieved from seer.cancer.gov/csr/1975–2001
Schaal, J. C., Lightfoot, A. F., Black, K. Z., Stein, K., White, S. B., Cothern, C., Gilbert, K., Hardy, C. Y., Jeon, J. Y., Mann, L.,
Mouw, M. S., Robertson, L., Waters, E. M., Yonas, M. A., & Eng, E. (2016). Community-guided focus group analysis on
cancer disparities. Progress in Community Health Partnerships: Research Education Action, 10(1), 159–166.
Smedley, B. D., Stith, A. Y., & Nelson, A. R. (Eds.). (2003). Unequal treatment: Confronting racial and ethnic disparities in
health care. Washington, DC: National Academies Press.
Sullivan, L. W. (2004). Missing persons: Minorities in the health professions; A report of the Sullivan Commission on Diver-
sity in the Healthcare Workforce. Alexandria, VA: The Sullivan Alliance to Transform the Health Professions.
US Census Bureau. (2015) State & county quick facts: Guilford County, North Carolina. Retrieved from http://quickfacts
.census.gov/qfd/states/37/37081.html
Partnership, Transparency, and Accountability 121
Voti, L., Richardson, L. C., Reis, I., Fleming, L. E., Mackinnon, J., & Coebergh, J. W. (2006). The effect of race/ethnicity
and insurance in the administration of standard therapy for local breast cancer in Florida. Breast Cancer Research and
Treatment, 95, 89–95.
Williams, D. R., & Rucker, T. D. (2000). Understanding and addressing racial disparities in health care. Health Care
Financing Review, 21, 75–90.
Yonas, M. A., Aronson, R. E., Coad, N., Eng, E., Jones, N., Petteway, R., Schaal, J., & Webb, L. (2013). Infrastructure
for equitable decision-making in research. In B. A. Israel, E. Eng, A. J. Schultz, & E. A. Parker (Eds.), Methods for
community-based participatory research for health (2nd ed.). San Francisco, CA: Jossey-Bass.
Yonas, M. A., Aronson, R., Schaal, J., Eng, E., Hardy, C., & Jones, N. (2013). Critical incident technique: An innovative
participatory approach to examine and document racial disparities in breast cancer healthcare services. Health Education
Research, 28(5), 748–759.
Yonas, M. A., Jones, N., Eng, E., Vines, A. I., Aronson, R., Grifth, D. M., White, B., & DuBose, M. (2006). The art and sci-
ence of integrating undoing racism with CBPR: Challenges of pursuing NIH funding to investigate cancer care and racial
equity. Journal of Urban Health, 83(6), 1004–1012.

9
CHAPTER
SOUTH VALLEY PARTNERS FOR
ENVIRONMENTAL JUSTICE
A STORY OF ALIGNMENT AND
MISALIGNMENT
MAGDALENA AVILA, SHANNON SANCHEZ-YOUNGMAN, MICHAEL
MUHAMMAD, LAURO SILVA, AND PAULA DOMINGO DE GARCIA
AS THE ORIGINAL settlement of Albuquerque, New Mexico, the South Valley has been
home to generations of Chicano-Hispanic farmers and more recent Mexican immigrants. The
South Valley is composed of many historic sub-neighborhood communities that have a long-
established legacy of community organizing for social justice. Much of this history is rooted in
the culture and tradition of New Mexican land grants and their long-term inuence on the lives
of residents. Faced with many economic and health disparities encountered by downstream
communities, South Valley residents have also historically struggled with institutional and envi-
ronmental racism, including no public services for multiple Mexican colonias and contamina-
tion from heavy industrial development within residential neighborhoods. Industries, such as
wrecking yards and petrochemical storage, over the last several decades, have generated brown-
elds and two Superfund sites.
The South Valley Partners for Environmental Justice (SVPEJ) originated as a CBPR part-
nership among community-based organizations, the county environmental health department,
and the University of New Mexico. This project received two cycles of National Institute of
124 Community-Based Participatory Research for Health
Environmental Health Sciences (NIEHS) funding to map conditions and empower residents
to address environmental justice issues. SVPEJ achieved multiple grant goals, including the
training and empowerment of a cadre of research promotores (lay health workers) to provide
environmental education within some of the most economically, socially, and politically vulner-
able neighborhoods.
Despite this longevity, SVPEJ stakeholders identied multiple challenges for reaching their
policy goals. These included the historical context, an inhospitable policy environment, and the
impact of these contexts on issues of alignment and misalignment among the different part-
ners and between the partnership and the community. Alignment is dened here as the eth-
ical adjustments of a partnership to t with the perspective of community partners about their
sociocultural, historical, and political context to ensure the maximum potential for collectively
producing knowledge for equity. This chapter demonstrates that different, and sometimes clash-
ing, perspectives of key community leaders, promotores, academics, and policy makers toward
their context, the purpose of the research, group decision making, governance, and community
authority can impede CBPR efforts to achieve environmental justice. However, even when part-
nerships falter, effective community leadership can seed differential consciousness among activ-
ists. Although possibly not intended, differential consciousness, dened by Sandoval (1991)
as an empowering mental state that prepares members of an oppressed group to undermine,
reform, or overthrow a dominant system, became one of its most important accomplishments.
ENVIRONMENTAL JUSTICE IN THE UNITED STATES
The environmental health justice movement and CBPR are tightly linked in practice and through
their institutional development (Brugge & Hynes,2005; Corburn,2005; Minkler et al.,2010;
O’Fallon & Dearry, 2002). This approach fuses academic and community insights to dene
problems and research questions enabling collaboration to gather and analyze data and use grass-
roots organizing strategies to advocate for health justice issues. Through a process of coproduc-
tion of research and community action, CBPR and environmental health partnerships have the
potential to reveal the contingency of knowledge and expertise and offer an innovative platform
to inuence community and political transformation. Importantly, the environmental justice
movement preceded CBPR, with the NIEHS being the rst institute to fund community-based
research projects incorporating CBPR in 1995. At the federal level NIEHS initiated an innovative
research approach that brought together environmental health, CBPR, and social justice.
The civil rights movement of the sixties was the precursor to the mainstream environmental
justice movement that crystalized in the mid-1980s (Brown, 2015; Brulle & Pellow, 2006).
Adopting an expansive view of equity, young leaders of color mobilized on toxic contamination,
substandard housing, access to green space, land use and smart growth policy, food justice, and
jobs (Faber & McCarthy,2003). Using street science to advance their claims, lay community
leaders made observations of health effects and pollutants, hypothesized connections, organized
community groups, and brought in legal experts for advocacy and policy reforms. With a clear
sense of structural determinants, movement groups typically framed their concerns in individual
and collective terms. Battles about land use, for example, were not just about individual impacts
but also stressed the impact on social cohesion and the well-being of communities of color.
Insum, those communities experiencing the greatest environmental and health inequities asserted
South Valley Partners for Environmental Justice 125
that their lived experiences, coping strategies, and cultural traditions qualied them as copro-
ducers of environmental and health decision making (Corburn,2007).
Alongside these developments, mainstream environmental organizations, predominantly
representing interests of white, upper-middle-class liberals, fought to protect wilderness,
endangered species, clean air and water, and often ignored the structural inequalities faced by
people of color (Schlosberg & Carruthers,2010). In 1991, the rst People of Color Summit of
Environmental Justice challenged these mainstream environmentalists by establishing seven-
teen environmental justice principles. In an act of differential consciousness, people of color
and vulnerable communities named the issue of environmental racism, using their own oral his-
tories, and identied siting of toxic waste in communities of color. Citing multiple conditions of
oppression faced by people of color, these activists also called for new and multiple strategies to
achieve equity. This critical act of resistance redened environmental justice as a civil right and
a social justice and human rights issue in the eyes of governmental funding agencies such as the
NIH (Brulle & Pellow,2006).
Building on these efforts, the environmental justice health movement also began to call
for “recognition” as another crucial element of environmentalism (Gibson-Wood & Wake-
eld,2012). In effect, Indigenous activists called for the inclusion of alternative ways of know-
ing in dening and solving environmental problems to promote broader environmental justice
(Corburn,2007; Haluza-Delay,2008). They asserted that ignoring alternative ways of naming
and framing environmental problems was unjust because it denied equal voice to those whose
understandings and experiences of “the environment” were outside of dominant experiences.
Indigenous calls for a politics of recognition presented a natural t for one of CBPR’s major
strategies to recognize the critical role of local culture and context in designing and implement-
ing interventions with local ways of knowing (Belone et al.,2016; Wallerstein & Duran,2010;
Wallerstein et al., under review). For CBPR practitioners, lived experiences provide crucial venues
to understand environmental health concerns from multiple vantage points. Further, the coproduc-
tion of knowledge disrupts power imbalances among academics, policy makers, and lay people,
and alternative ways of knowing problematize the origins and substance of policy issues by high-
lighting that scientic legitimacy is a social, political, and material phenomena. Most critically,
local ways of knowing give communities the agency to transform the social, political, and ethno-
racial stratication systems that have subjugated their community knowledge (Dutta,2008).
SOCIOCULTURAL RELATIONS AND ENVIRONMENTAL ACTIVISM
IN THE SOUTH VALLEY
The South Valley (SV) is a vibrant, culturally rich community that intersects urban and rural
living with pockets of neighborhoods that still have livestock in the backyard with those that are
a bit trendier in their modernization. Latinos of New Mexican heritage and Mexican immigrants
comprise the biggest percentage of SV residents. Although the majority of its residents are
socioeconomically disadvantaged, there is also a long history of land-based ownership among
the many New Mexican families who have made the SV home for generations.
The sociopolitical history of the SV is one that is deeply immersed, similar to the rest of
New Mexico, in a history of community empowerment and the struggle for social justice related
to land grant status, going back to the Treaty of Guadalupe in 1848. Through land grants, native
126 Community-Based Participatory Research for Health
New Mexican community identities have been rooted in a long legacy of land-based people’s
struggles for the right to their lands, their water rights, and their perceived cultural inheritance.
SV community leadership is also an attribute of generations of families who have spoken up
for their rights as political activists and as elected ofcials at the county and state levels. More
recent organizing related to environmental contamination has brought together local predom-
inantly Latino advocacy organizations in formal and informal coalitions to advocate for the
cleanup of two Superfund sites. With the increase of Mexican low-income immigrants in the SV
over the last twenty years, the differences between immigrants and politically powerful native
New Mexicans have created a complex constellation of cultural factors and values and princi-
ples that are often confusing to outside researchers and public health ofcials.
The SVPEJ originated as a research group in 2000 as a response to a request for pro-
posals from NIEHS. Consisting of four partners—the University of New Mexico, Bernalillo
County’s Ofce of Environmental Health, the Rio Grande Community Development Cor-
poration (RGCDC), and South Valley promotores—SVPEJ was successfully funded for two
NIEHS grant cycles (2000–2004, 2005–2009). The research partnership came together to
seek reductions of environmental health hazards and risks in the South Valley by bridging
communication gaps among community residents, health care providers, policy makers, and
environmental health researchers. In the rst grant, the county was the principal investigator
(PI) and worked in collaboration with the community to identify, dene, and assess the dispro-
portionate burden of environmental health risks and health inequities faced by Latino families.
In the second grant, the community became the PI after community members challenged
aspects of the rst grant cycle. In the second phase, the goals were to develop a communication
model, identify venues to better inform and engage SV residents on local land-use zoning and
planning issues, and seek greater community participation in decision making on these zoning
and policy issues. Key grant outcomes included increased understanding of the local land use
zoning and policy process, the update and revision of a dated neighborhood sector plan that
was decades old, and a communication model to better inform residents as part of an informed
policy-making process. This increased capacity building among promotores, but after ten years
of multiple fractures, the partnership dissolved.
These fractures, which emerged through conscious and unconscious practices, deepened
throughout the ten-year project period. In the beginning, they emerged as almost invisible hairline
cracks. Although seemingly unnoticed, they cumulatively contributed to misalignment between
community and the academic and county partners. As these fractures expanded, they led to a major
dissention and disagreements about how the research and advocacy was carried out in the SV.
METHODS
In 2012, the SVPEJ research project was selected as a case study from a larger National Insti-
tute of Health investigation known as the Research for Health (RIH) Project, led by the Uni-
versity of New Mexico (UNM) Center for Participatory Research. RIH sought to test a CBPR
conceptual model, assess the variability of CBPR partnerships nationwide, and identify asso-
ciations between contexts, partnering characteristics, research, and health outcomes (Hicks
etal.,2012; Pearson et al.,2015). Data collection for the SV as part of the RIH case study took
twelve months and included fteen semi-structured individual interviews, one focus group, a
South Valley Partners for Environmental Justice 127
document review, and a historical time-line exercise with case study partners (see Chapters6
and17 for more discussion of RIH case study methods).
DISCUSSION: TENSIONS AND FRACTURES
Environmental justice research and advocacy is a complex and challenging area—especially when
collaborative partnerships are composed of such a unique constellation of interests, aims, and
motivations. The SVPEJ partnership reveals how conicting ways of knowing and divergent social
justice tactics contributed to a series of fractures that ultimately eroded the partnership. As the
next sections illustrate, the SVPEJ project represents an example in which academics and county
policy makers missed several opportunities to recognize and build on the layers of community
understandings of water and land use in New Mexico. These community understandings are criti-
cal sources of survival, political, and cultural identity, nation-state making, and become central
metaphors that encapsulate generations of struggle(s) against stratication systems that continue
to ripple on the basis of class, citizenship, ways of living, and ethno-racial dynamics.
Divergent Worldviews on Environmental Problems and Solutions
Seeding the development of these fractures, interviews with academic and county partners
showed they approached the aims of the project through a distributive justice lens, which was
informed by white, liberal environmentalism and their obligations as county ofcials. Aca-
demics and county representatives shared the community’s values of reducing environmental
racism. For them, the project presented the opportunity to fold in community member partic-
ipation into ongoing struggles to promote equitable land use. They suggested that the project
would use traditional tactics of agenda setting and policy advocacy at the county level to alle-
viate environmental ills.
A second aim was to cooperate with community members to achieve a unied vision of
environmental justice. Academic and county partners imagined a process in which experts
would develop the community’s skills to identify environmental risks to advocate and inform
community residents about how to build safer neighborhoods. Building community capacity
meant teaching promotores to take air and water samples, develop their leadership skills, and
use storytelling to inuence formal policy reform. When reecting on the major aims of these
policy efforts, one county person said, “I think the purpose was developing skills amongst the
community around land use issues. For instance, we did a training on when somebody submits
a permit, what’s the process that it goes to before becoming approved.”
These county-driven aims were largely a response to their own bureaucratic constraints
that limited their political advocacy. Guided, therefore, by technical approaches to policy
advocacy, academic and county partners assumed that their role was to educate the community
to become active participants in their local advocacy efforts. The shortcoming of this approach
was that it implied that experts would provide information to vulnerable communities to create
policy change.
Academics and policy makers also viewed the grant as a mechanism to provide resources
to the community to improve local environmental conditions. For instance, the county leveraged
funds to initiate several cleanup projects as part of the project. According to a local county ofcial,
“we wrote a grant to provide containers to do a community cleanup on Pajarito Mesa. But then of
128 Community-Based Participatory Research for Health
course, the community used them for gas and other things. So we did a training—all in Spanish
and they learned how to use them.” The presumption here is that the partnership provided the
opportunity to promote individual behavior change in the community through culturally sensitive
trainings. Although the resources provided were valuable for environmental cleanup, they down-
played the necessity to resist the unhealthy structures faced by community residents.
In the political sphere, academic and county partners often situated their analysis of local
power relations on political corruption and sexism. According to county and academic part-
ners, some major obstacles to their partnership’s success were embedded in the “machismo”
of Latino political leadership in the area and entrenched patronage politics between old New
Mexican families and business owners. From their point of view, the partnership would leverage
the perspectives of Chicano community leaders to ght against patronage politics and to ght
against male control of the political agenda. One county ofcial noted the following:
Historically, a lot of the organizations that worked in the South Valley were male dominant.
Ithink that there is some bias from attitudes like “you females, you are trying to change us and
our power.” And, I’m sorry, the Bernalillo County at that time was very male dominant in power.
I don’t think there was one female who had a leadership role in the county.
The community’s vision of social justice, however, was premised on harnessing the lived
experiences of immigrant and Chicano-Latino communities to ght for multiple reforms.
Informed by oral stories passed on through generations, community members described water
and land use struggles as multilayered issues embedded within deep historical struggles of
community identity, distribution of material resources, and communal ways of living. One
community member interviewee described the SV acequia (irrigation ditches) movement:
For me, the acequia movement is another movement of struggle altogether that is currently
happening. There is the association of acequias, because with a water problem, it’s a movement
based on tradition, and dealing with tradition. It’s a New Mexican movement; the struggle for
water, and that water is life, “se deende no se vende,” “Water is to defend, not to sell.”
As this quote suggests, the community’s struggle over water not only sought to preserve
and reproduce a way of life but also entailed a struggle for political voice and autonomy for suc-
cessful community functioning and independence.
Representing a movement premised on the decolonization of knowledge and political
advocacy, community activists in the SV drew from the political skills of women and men of
color that emanated from their everyday resistance. For community partners, a major aim of the
project was to build from community resilience rooted in cultural practices to ght against envi-
ronmental racism. One activist scholar stated the following:
I think my approach and how I saw the project is rst of all, it’s certainly not a decit model of
knowledge from a community perspective, but rather a capacity model. There’s already tremen-
dous knowledge from what I call organic venues within the community. So when we’re going
to tap into those venues it’s which one are we going to tap? How are we going to tap it? How
do we acknowledge the depth and width of expertise? So it always comes from a model that
acknowledges the foundation of knowledge that comes from a community...It’s like con-
stantly mapping. Always mapping the movement with the community.
South Valley Partners for Environmental Justice 129
Community partners did not envision their work as simply demanding formal legal
equality through a multisector plan. Rather, a central task was to facilitate critical conscious-
ness among community members and their academic and county allies to advocate for rights.
Akey community project leader saw educating the community as an exercise in “deconstruct-
ing a policy manual and working to educate the community about what a sector plan does and
by taking it apart informing people of their rights.”
Divergent Tactics for Environmental Justice
Community activists advocated for strategies encompassing a more holistic vision of social jus-
tice that promoted social, political, and economic actions that linked solutions to broader social
change. For community leaders, this involved having the exibility to read multiple situations
and consciously choose strategies best suited to push against multiple forms of oppression. For
these folks, organizing for change was neither linear nor utilitarian, and the goal was to mobi-
lize community members to adopt a variety of organizing tactics, ranging from advocating for
formal legal reforms to mobilizing against a broader eld of unequal conditions that produced
environmental injustices in the South Valley.
Informed by a more radical lens compared to academic and county partners, community
residents felt that a bias existed in favor of industrial investment supported by elected policy of-
cials. They argued that this conicted with the traditional land use among Indigenous community
members, placing community residents at greater health risks. As a result, community partners
saw the community PI as a champion who would adopt a more hard-line position against per-
ceived encroachments to SV self-determination. Promotores especially felt that researchers and
county-level bureaucrats who preferred top-down approaches ultimately upheld the status quo
of public health institutions:
Well, I think it was real benecial for me to be a promotor and to be a part of this process;
and I think the leadership, the principal investigator of the promotores, I think he was one of
these elders of the community that was connected, and that he did have a lot of knowledge of
the community, a lot of knowledge about the university and with the county. He had a lot
ofexperience, and I think that was really important. I don’t think the community partners, as the
principal investigators, would have been successful had it not been for somebody, for an elder
that knows, that’s been part of the community.
In contrast to the promotores who viewed the community PI as a powerful elder, academic
and county partners suggested that the community PI’s advocacy strategies were conictual and
ignored the science of public health. They argued that his conictual advocacy-based approach
ultimately decreased their participation in the project. A member from the academic team stated
the following:
The trust actually disintegrated towards the end. The promotores weren’t trustful of me, because
I was representing the university. I wasn’t trustful of the community PI because he was pulling
this power thing. And it really disintegrated quite a lot. We tried talking to the community PI
about wanting to really have it be participatory. He was a guy that really held things close to his
chest. And so it really wasn’t a partnership towards the end. I think that we were ready to bag
it and just call it a day.
130 Community-Based Participatory Research for Health
For academic and community partners, advocating against environmental racism would
have been more straightforward if community members had agreed to set timely goals with
measurable outcomes. For them, CBPR offered the space to include community members in
the process of linking science to policy. In fact, academic and county partners suggested that a
major shortcoming of the project was its lack of linearity:
I’m not a process person. And I’m a very structural person. So like I have “to do” lists. So this
was a bit different for me, very different for me. And I had a difcult time seeing the end result,
and I was impatient with some of the very loose dynamics that occurred, which I think are part
of community work. And I recognize that. I think it wasn’t as well-dened as it could have been.
And to me that was a huge frustration...we didn’t have time lines...we didn’t have measure-
ments...And I think without those time lines and without the structural components...we
didn’t achieve as much as we could have.
Why? I think it was learning curve of the community people. They had done some
community organizing, but did not have an academic base in public health or CBPR.
This quote highlights that some of the county or academic participants privileged results
over process and ultimately felt that more structured approaches provided a better framework to
produce policy change.
Ruptures in Ways of Knowing
A comparison of community, academic, and county partners’ ways of naming, framing, and
addressing environmental justice revealed important differences and misalignments among
members of the SVPEJ project. Though CBPR as a eld depends on the valuing of coproduc-
tion of knowledge, this case study reveals ways in which coproduction faltered throughout the
ten-year period, reducing the partnership’s effectiveness, in two primary ways.
As said previously, the county public health professionals and academics implicitly held a
decit-based approach to the community by believing that their technical resources and trainings
would provide the necessary skill building for policy change. Indeed, this top-down approach
was established by academic and county members in the initial design and early implemen-
tation of the grant. When promotores were recruited to participate, the rst county leadership
did not fully explain the aims of the project in an inclusive manner. This created early tensions
because promotores perceived this omission as condescending. Academic and county partners
also excluded promotores from research meetings, organized antiracism trainings for promo-
tores without academic and county participation, and used promotores as interpreters among
stakeholders. These actions discredited them as community knowledge holders. According to
the community PI of the second grant,
I think it’s a question of basically community partners not having the respect that they deserve
and the trust that they deserve. The academics didn’t trust the community. And it’s hard for aca-
demics to trust community. Community distrusts academics because they come in and mine the
resources of the community and run away with it and don’t leave anything behind.
By contrast, academic and county partners repeatedly expressed their frustration with the lack
of “professionalism” and focus among the community partners. This skeptical view of community
knowledge perpetuated the notion that science was the primary mechanism to speak truth to power.
South Valley Partners for Environmental Justice 131
Academic and policy partners also missed crucial opportunities to create meaningful dia-
logue with community partners about broader solutions that promoted social, political, and
economy integration in the SV. By focusing on the narrower objectives of distributive environ-
mental justice, they inadvertently didn’t understand the deep and multifaceted politics of water
and land in the Rio Grande region. In short, their proposed solutions adhered to mainstream
conceptions of environmentalism that were individual and consumption based. This subtly
reected the biases of liberal environmentalism and ignored the reality that community mem-
bers often lacked the basic infrastructure to meet their everyday living needs. As the community
partners pointed out, the danger of tinkering with zoning laws did not necessarily change the
key conditions of vulnerability in the South Valley.
This top-down approach had far-reaching consequences. Academic and county partners
reproduced a mainstream science narrative that linked traditional forms of advocacy with
progress and social transformation. From the community’s perspective, the partnership failed
to foster spaces for social change and structural transformation because academic and county
participants did not leverage Indigenous knowledge to understand problems and solutions. By
refusing to relinquish their control of the research process, promotores and community leaders
argued that the process became paternalistic. According to one promotora,
Towards the end of partnership you could see the true colors of the organizations when the
community had the chance to be in the driver seat; and I don’t think the partners—the uni-
versity and the academic partners—were comfortable with it and I think their egos were hurt
because these uneducated people were talking about publishing papers and having their names
put on these publications that these professors need to have tenure...and that the county
needs to show that they’re doing something for the community. And so it is a very paternalistic
relationship that is like, “We are taking care of you guys. We’ll take care of this.” And we’re
like, “No, we can put our names on the papers too we’re doing the research or whatever else.”
Community leaders also described how the partnership reproduced power asymmetries
between structural positions of the white feminists and community members. For community
activists, the project ultimately reinforced the status quo in academic-community interactions
because the power to name, frame, and organize remained in the hands of the academy and in
public health county bureaucratic institutions. According to one female academic,
The PIs are white, the assistant PIs are white, everybody’s white for the most part. And then
what do you have? Again that, what do you call it?...that sister relationship, but the Great
White Hope is holding the hand. It can’t be that way. I’m just tired of seeing that. You cannot
be afraid to give up your power. And I think for me that’s my greatest test. I ask myself, “Am I
afraid to be replaced or am I afraid to be questioned?” We need the community to challenge us.
They’re going to know stuff we don’t know. Yeah, we have to develop more Indigenous experts.
That’s what’s going to change the pendulum.
Community Resilience
In spite of the partnership’s dissolution, community leaders were successful in empowering
a cadre of research promotores that reappropriated the term of environmentalism and rede-
ned it according to their lived realities at ground zero. Promotores and other community
132 Community-Based Participatory Research for Health
members did not agree with how the county and academic environmentalism was mirroring
their struggle, so they took charge and completely redened the aims of the project. This is an
example of differential consciousness when communities of color experience, perceive, dene,
and advocate an environmentalism that was not aligned with the perceptions and social norms
of mainstream environmentalism. Through their differential consciousness and struggles within
the partnership and through the leadership of community leaders, promotores expressed an
awakening of deep and profound knowledge that included shaking off oppressive practices that
they saw and experienced through the research process. Through consciousness raising in dia-
logue with community leaders, promotores said that their critical lens changed on a daily basis
as they became more condent in operational research methods. In the words of a key facilitator
of this process,
The SVPEJ started like a ripple when you throw the pebble into the pond and then it became a
tsunami of intellectual and political force that left in its stead an innite amount of ripples that
hit at the mind, the soul, the spirit, the heart, the feet, and the legacy of each and every one
of the promotores. Those are the elements of critical thinking in our communities that shift the
alignment and that shocks those benevolent minds who have absolutely no understanding of its
force and whence it comes. CBPR is an awakening from a total different point of consciousness
and intellect than it is for the academic partners. The seed was planted and it came to fruition
regardless of what anyone thinks; this was the success that can’t be empirically measured. It
is a seed of a movement. To me this is the greatest gift or seeding of what CBPR research can
bring—such a degree of reexivity that it opens the doors that oppression has closed. It reignites
the spark. It’s more than data...it’s a social movement.
LESSONS LEARNED
Although these fractures and tensions challenged the success of the SV partnership, they also
raised important lessons for other CBPR partnerships.
Establish structural mechanisms that promote mutuality from the outset. A fundamental
principal of CBPR is to leverage the research process to bring everyone forward and create
venues that equalize power differentials between academics and community members. Key
to promoting a successful and equity-based partnership is demystifying and deconstruct-
ing the research process. A rst step is for academics and community members to copro-
duce research documents, beginning with the research proposal. Most proposals consist of
professional and technical language that is unfamiliar to community-based partners. Rather
than conning proposal writing to academics, cowriting grants (or creating agreements) can
seed the possibilities for meaningful change, and it establishes an equity-based framework
from the outset.
Enter communities with humility. Academic partners must avoid entering communities
with a “follow me and learn” attitude. They should listen, observe, and adopt a “let’s walk
together” approach to foster collaborative learning and collective empowerment. As the SV
case study demonstrates, community partners do not see activities such as translating and inter-
preting as a newly acquired research skill but rather as part of their existing culturally based
skill set. Effective partnerships promote community capacity by recognizing and building
South Valley Partners for Environmental Justice 133
from community assets rather than appropriating cultural knowledge as a form of research
skill development.
Embrace tensions. Working in a collaborative research partnership may give the impres-
sion that relational processes are always healthy and that all members should strive to maintain
partnership perfection. Partnerships, similar to any relationship, often fall victim to maintain-
ing the false perception that all is well. Yet, fractures and tensions may present some of the
most valuable lessons for collaborative research processes. Genuine collaborations require
continual collective reexivity among all partners. This includes providing the space for mem-
bers to reect on and revise their roles and levels of input throughout the project. It means
being conscious of institutional positions and the limitations and opportunities within each. It
is imperative to recognize that the partnerships’ conguration will not stay the same for the
duration of the research project. If anything, the partnership pendulum will swing back and
forth, and it should be accepted and perceived as a healthy indicator of a collaborative partner-
ship process.
Differential consciousness is a catalyst for community-based research and social transfor-
mation. In a collaborative research partnership, it is critical that equal value be given to multiple
ways of knowing to produce decolonized research and social transformation. This provides the
intellectual engine for the team. Valued scholarship must be equally based and not anchored in
condescending or patronizing approaches that are masked to pass as genuine. Community-based
partners (i.e., promotores) did not want to be written about, but they wanted to participate in
dissemination of knowledge by being treated and approached as scholarly partners. Promotores
found out about project articles being discussed for publication that they were never invited
to participate in. They felt they were not valued, and their perspective was seen as outside the
dominant norm.
CBPR is like a prism that encourages different and changing viewpoints. It is a con-
tinuum that provides different anchor points to the research among the different partners.
CBPR grows in its value and importance as communities take more ownership of the process
and can change the merits of the research outcomes. Academic partners must be exible and
be prepared to accommodate this changing lens. Inexibly forcing a linear research approach
can produce unexpected levels of challenges, including partnership fractures, punctures,
and tensions.
CONCLUSION
This case study demonstrates the issues that arise as a result of partnership alignment and mis-
alignments. All research partnerships have challenges and, even when those challenges turn
into tensions, fractures, and ruptures that derail the initial goals of the project, there are still
lessons to be learned and successes to be gained. CBPR is a research orientation that promises
equity and equanimity. Those who use this approach will be held to a higher standard from
a community perspective than other traditional research approaches. Research can produce
differential consciousness at a grassroots community level. CBPR therefore has within its very
foundation the essential constructs to go beyond a canned approach and to give greater voice to
organic narratives and knowledge.
134 Community-Based Participatory Research for Health
QUESTIONS FOR DISCUSSION
1. All research partnerships will face challenges along the way, with larger and more diverse
partnerships perhaps facing a more challenging journey. Given this reality, how would
you as a research team member identify and address potential threats based on your per-
ception of tensions and fractures? How would you differentiate perceived problems from
actual problems?
2. What strategies would you develop to address tensions, fractures, and ruptures within
a partnership? What strategies would you use to communicate this to community and
academic team members, including identifying indicators of tensions early on?
ACKNOWLEDGMENTS
The authors of this chapter would like to acknowledge NIEHS for the two grants that they
funded (2001–2009, #1r25eso14347-03), the NIEHS program ofcer, Liam O’Fallon, the South
Valley Partners for Environmental Justice (SVPEJ), and the South Valley Community. Thanks
also to the promotoras, and the many other partners who remain committed to health equity
work from Bernalillo County, the University of New Mexico and the Rio Grande Community
Development Corporation. Environmental justice will not be possible without all the collabora-
tion and shared work. Thank you to all.
REFERENCES
Belone, L., Lucero, J., Duran, B., Tafoya, G., Baker, E., Chan, D., Chang, C., Greene-Moton, E., Kelley, M., & Wallerstein,
N. (2016). Community-based participatory research conceptual model: Community partner consultation and face validity,
Qualitative Health Research, pp. 1–19.
Brown, P. (2015). Integrating medical and environmental sociology with environmental health: Crossing boundaries and
building connections through advocacy. Journal of Health and Social Behavior, 54, 145–164.
Brugge, D., & Hynes, P. (2005). Community research in environmental health: Studies in science, advocacy and ethics.
Burlington, MA: Ashgate Publishing.
Brulle, R., & Pellow, D. (2006.) Environmental justice: Human health and environmental inequalities. Annual Review of
Public Health, 27, 103–123.
Corburn, J. (2005). Street science: Community knowledge and environmental health justice. Cambridge, MA: MIT Press.
Corburn, J. (2007). Community knowledge in environmental health science: Coproducing policy expertise. Environmental
Science and Policy, 10, 150–161.
Dutta, M. J. (2008). Communicating health: A culture-centered approach. Malden, MA: Polity Press.
Faber, D., & McCarthy, D. (2003). Neoliberalism, globalization and the struggle for ecological democracy: Linking sustain-
ability and environmental justice. In J. Agyeman, R. D. Bullard, & B. Evans (Eds.), Just sustainabilities: Development in
an unequal world. Cambridge, MA: MIT Press.
Gibson-Wood, H., & Wakeeld, S. (2012). Participation, white privilege and environmental justice: Understanding environ-
mentalism among Hispanics in Toronto. Antipode, 45, 641–662.
Haluza-DeLay, R. (2008). A theory of practice for social movements, environmentalism and ecological habitus, Mobilization:
An International Quarterly, 13, 205–218.
Hicks, S., Duran, B., Wallerstein, N., Avila, M., Belone, L., Lucero, J., Magarati, M., Mainer, E., Martin, D., Muhammed,
M., Oetzel, J., Pearson, C., Sahota, P., Simonds, V., Sussman, A., Tafoya, G., & White Hat, E. (2012). Evaluating
South Valley Partners for Environmental Justice 135
community-based participatory research to improve community-partnered science and community health. Progress for
Community Partnerships, 6, 289–311.
Minkler, M., Garcia, A. P., Williams, J., LoPresti, T., & Lilly, J. (2010). Si se puede: Using participatory research to promote
environmental justice in a Latino community in San Diego, California. Journal of Urban Health, 87, 796–812.
O’Fallon, L. R., & Dearry, A. (2002). Community-based participatory research as a tool to advance environmental health sci-
ences. Environmental Health Perspectives, 110(Supp 2), 155–159.
Pearson, C. R., Duran, B., Oetzel, J., Margarati, M., Villegas, M., Lucero, J., & Wallerstein, N. (2015). Research for improved
health: Variability and impact of structural characteristics in federally funded community engaged research projects.
Progress in Community Health Partnerships: Research, Education, and Action, 9, 17–29.
Sandoval, C. (1991). Methodology of the oppressed. Minneapolis, MN: Minnesota University Press.
Schlosberg, D., & Carruthers, D., (2010). Indigenous struggles, environmental justice, and community capabilities, Global
Environmental Politics, 10(4), 12–35.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100, S40–S46.
Wallerstein, N., Oetzel, J., Duran, B., Margarati, M., Pearson, C., Davis, J., DeWindt, L., Lucero, J., Ruddock, C., Sutter, E.,
Villegas, M., & Dutta, M. (under review). Culture-centeredness in community-based participatory research: Implications
for psycho-social health interventions. Social Science and Medicine.

4
PART
PROMISING PRACTICES:
INTERVENTION
DEVELOPMENT AND
RESEARCH DESIGN
The impacts of context and partnering processes and practices are most often seen on the
development of interventions and research designs. Stated most directly, if there is no or
minimal engagement with key community stakeholders, intervention and research meth-
odologies suffer isolation from critical community knowledge, priorities, and input on what
would succeed for any particular geographic, policy, organizational, and cultural context. NIH
has acknowledged the importance of community engagement for precisely ensuring that data
138 Part 4
instruments, intervention components, and understanding of local implementation contexts
can be recognized and incorporated into the research in order to make a difference in reducing
health inequities.
CBPR takes engagement further than just input and looks to shared leadership, copro-
duction, and community-driven theories and interventions in these all-important knowledge
appraisals. Judgements about the usefulness or validity of knowledge are increasingly recog-
nized (by academics and communities) as being embedded in community contexts, not simply as
images or beliefs but as dynamic processes of social and cultural reproduction. Communication
scholar Mohan Dutta, as noted in Chapters1 and2, has proposed the language of “culture-
centeredness” to represent community voice, agency, decision making, and reflexivity as key
for creating interventions and research designs to transform top-down academic assumptions
and other inequitable conditions. Coproducing knowledge not only improves intervention or
research method fit within the community but also facilitates greater community ownership,
research capacity, and program sustainability after grant funding might end. Valuing community
culture and knowledge is also key to promoting the goal of knowledge democracy, which rec-
ognizes and celebrates the importance of multiple knowledge systems, such as organic, organi-
zational, land-based, and spiritual systems, and frameworks emerging from social movements,
and knowledges of the marginalized and excluded.
The four chapters in this section beautifully illustrate the opportunities for integrating CBPR
principles and processes, with community knowledge, cultural agency, understanding of imple-
mentation contexts, and academic evidence in creating successful interventions. Case studies
and vignettes are provided as examples and as inspiration for others.
In Chapter10, Margarita Alegría and colleagues provide guidance for applying CBPR to
the growing arena of health services research, with its diverse stakeholders of health care pro-
viders, payers, patients, patient advocacy groups, families, and other caregivers. They start with
challenges, including limited CBPR training for health service researchers, and present useful
implementation strategies for incorporating CBPR principles at different research stages. Three
vignettes are presented: Community Partners in Care (CPIC), a randomized comparative effec-
tiveness trial of two interventions to support depression quality improvement across health care
and community-based agencies in Los Angeles; a PCORI-funded trial at Massachusetts General
Hospital and thirteen clinics examining effectiveness of improved patient-provider behavioral
Part 4
139
health shared decision making through encouraging patients to ask questions and providers to
be more receptive; and efficacy of a community health worker intervention to improve type 2
diabetes within the Bangladeshi American community in New York City. All three had extensive
partnerships and illustrate how to better integrate CBPR within health care and agency settings.
In Chapter11, Steven Barnett and colleagues present their experience at the National Center
for Deaf Health Research, in Rochester, New York, a city with a large, vibrant, and diverse Deaf
population. They showcase how they’ve developed and sustained CBPR research with mem-
bers of the Deaf community, who are defined as having a Deaf culture and sign language and
not by hearing acuity. The chapter starts with an overview of the cultural dimensions and con-
text of this overlooked population and provides multiple examples of CBPR research with Deaf
and hearing researchers, staff members, students, and community members on how they select
health research priorities; adapt research methods, measures, and interventions to be language
and culturally accessible and appropriate while maintaining scientific rigor; and translate and
disseminate their findings to broad stakeholder audiences. Their lessons learned in terms of
deeply connecting to the knowledge, values, language, and culture of the community within
CBPR are applicable to other minority populations.
In Chapter12, Nadia Islam and colleagues discuss CBPR with Asian Americans, the fastest
growing racial-ethnic group in the United States. CBPR approaches are well suited for Asian
American populations, whose contexts vary greatly by subgroup, who often reside in concen-
trated ethnic enclaves, and who possess rich cultural knowledge integral to conducting quality
research and developing effective interventions. The authors present two case studies. The first
case study focuses on a national-level, multiethnic approach based at the Center for the Study
of Asian American Health at New York University and shares principles and lessons learned
from sustaining multiple CBPR partnerships over many years. The second case study focuses
on a study of health and working conditions in San Francisco Chinatown restaurants involving
immigrant workers as key community researchers, with a local community-activist organization,
university, and the local health department. Lessons are shared for building community capacity
and successfully advocating for a major municipal worker protection policy.
In Chapter13, Scott D. Rhodes and colleagues describe the development and refining of
a thirteen-step ENGAGED for CHANGE strategy that provides a collaborative framework for
CBPR intervention development. ENGAGED for CHANGE is a process that incorporates the lived
140 Part 4
experiences and decision making of community members and service practitioners working
in these communities to ensure culture-centered and contextually appropriate interventions.
Based on their fifteen-year experiences as a CBPR collaborative creating sexual health and
HIV-prevention interventions for Latino gay and bisexual men, men who have sex with men
(MSM), transgender persons, and Latina women, they provide examples for each step of how
to incorporate community knowledge with evidence-based strategies in the design, piloting,
implementation, and evaluation of their interventions. They hope others can benefit from this
approach to maximize the potential for reducing and eliminating health disparities.

10
CHAPTER
CBPR IN HEALTH
CARE SETTINGS
MARGARITA ALEGRÍA, CHAU TRINH-SHEVRIN, BOWEN CHUNG, ANDREA AULT,
ALISA LINCOLN, AND KENNETH B. WELLS
DESPITE SCIENTIFIC ADVANCES since the 1990s, the translation of evidence-based research
into clinical and community practice has been limited (Committee on Quality of Health Care in
America, 2001; Pearson, Jordan, & Munn,2012). Understanding what works in these settings
requires moving beyond controlled research designs and settings into community and practice-
embedded research partnerships. In the context of health care system research in communi-
ties experiencing health disparities, genuine community engagement throughout the research
process is required to ensure improved translation of efcacy and effectiveness ndings into
adoption and practice (Mullins, Abdulhalim, & Lavallee,2012; Wallerstein & Duran,2010).
Community-based participatory research (CBPR) can elucidate the mechanisms and strategies
to support this translation and generate the practice-based evidence to disseminate and scale
clinically proven strategies, particularly in under-resourced communities and vulnerable popu-
lations (D’Alonzo,2010; Wallerstein & Duran,2010).
In recent years, new directions and renewed interest in CBPR approaches have emerged
with a focus on patient-centered outcomes research that emphasizes reaching out to patients
for their perspectives and the perspectives of caregivers in the research process. With the
recent movement toward patient-centered research, the application of CBPR to health
services (HS) research has expanded to include health care providers and payers as well as
patients, patient advocacy groups, families, and other caregivers and community members as
stakeholders (Concannon et al.,2012).
142 Community-Based Participatory Research for Health
Further, national efforts and discussions about patient-centered research have emphasized
authentic stakeholder engagement (Woolf, Zimmerman, Haley, & Krist, 2016), supporting
processes and mechanisms that ensure that stakeholder perspectives are integrated throughout
the health care system research process and are reective of CBPR principles. Although interest
in patient and family engagement in HS and clinical effectiveness research has increased, there
is a dearth of information related to appropriate tools for the measurement and evaluation of
engagement in such research, including economic analyses of associated costs of engagement
(Domecq et al.,2014; Mockford, Staniszewska, Grifths, & Herron-Marx,2012) as well as best
practices for engagement. The dearth of information results from a general lack of comparisons
of engagement approaches (Domecq et al.,2014) and the limited availability of CBPR training
for HS researchers (Mockford et al.,2012).
This chapter proposes that rigorous HS interventions and research can incorporate CBPR
principles and practices to better embrace patient and stakeholder engagement. CBPR can
help address the preferences of these multiple stakeholders to accelerate implementation and
problem-solve challenges. This chapter summarizes three case studies and uses examples from
each study to offer guidance for scholars and practitioners in CBPR implementation within
HS research.
USING CBPR PRINCIPLES TO ADVANCE HEALTH SERVICES RESEARCH
The Patient-Centered Outcomes Research Institute (PCORI), funded through the Affordable
Care Act, seeks to improve the relevance of comparative effectiveness research for patient-
prioritized outcomes and interventions. As such, it has explicit grant requirements to include
patients, family, community members, and health care stakeholders in all aspects of study
development, governance, implementation, and dissemination (Hickam et al.,2013).
Much like other forms of community-engaged research (see Chapter1), traditional HS
research has varied in the level of community engagement—from conducting focus groups and
interviews with patients regarding outreach and recruitment strategies (minimal involvement),
to stakeholders serving as advisors for research design and evaluation (medium involvement),
to stakeholders driving the research questions and strategies as part of the decision-making
team (high involvement). Several core CBPR principles (see Table10.1, with full description in
Chapter3) address the importance of community-framed and community-driven identication
of issues for study at the local level and balancing data generation and research with action-
oriented solutions and programming efforts in HS research. Understanding patient barriers and
facilitators for health improvement includes not only a comprehension of the disease but also the
social ecology that predisposes vulnerability and enables disease prevention, treatment adher-
ence, support to tackle comorbid health and social factors, as well as an attention to community
preferences and cultural context for health. Dimensions such as social position, race, English
language prociency, or immigration status have substantial impact on the identication of
patient priorities and outcomes. By drawing on the core CBPR theme of stakeholders deter-
mining priorities, HS studies have the opportunity to advance our understanding of “patient-
driven” outcomes beyond those that are clinical or physiological in nature. For example, the
National Institute of Mental Health Affective Disorders Work Group developed and vali-
dated the Individual Burden of Illness Index for Depression and found that the inclusion of
CBPR in Health Care Settings 143
TABLE 10.1 CBPR Principles, Strategies, and Examples in Health
Services Research
CBPR Principle
Strategies in Health
Services Research Examples from the Literature
Create collaborative,
equitable partnerships
in all research phases.
■ Include patients, caretakers,
and patient advocacy group
as research coleads.
■ Partner with patient
stakeholders in
study decision-making
and dissemination
processes.
■ PatientsLikeMe (Fourie, Biller-
Andorno, & Wild,2014)
■ Disease-specific foundations,
particularly for rare conditions,
can be important partners
(Ginsberg,2017; Sharpe,2013).
Community is the unit
of identity—focus is on
the community.
■ Create a stakeholder board
representing diverse patient
and caretaker perspectives.
■ Use multiple strategies
(Islam et al.,2012) to
include diverse constituent
and stakeholder
perspectives.
■ The DREAM Project coalition
involved patients, providers,
and other multisector
stakeholders serving the New
York City Bangladeshi American
community.
Build on strengths of
community.
■ Use an asset-based
approach to develop
interventions with
patients, their families,
and providers.
■ Use community health workers:
Positive Minds-Strong Bodies
Project (Alegría et al.,2016).
Foster co-learning and
capacity building.
■ Conduct learning exchanges
in which researchers and
stakeholders contribute to
the research process.
■ Patient testimonials and
narratives were tools in
community mobilization
around hypertension:
Project AsPIRE (Trinh-
Shevrin,2014).
Focus on problems of
local relevance.
■ Conduct a multi-method
formative assessment to
incorporate stakeholder
perspectives in the study
design, analysis, and
interpretation.
■ A cancer screening study (Woolf
et al.,2016) used formative
assessments and ongoing
stakeholder engagement
to increase acceptability
and reach.
(Continued )
144 Community-Based Participatory Research for Health
functioning, perceived suffering, and quality of life indicators along with symptom severity
more comprehensively captured patient perspectives of the impact of treatment on depressive
symptoms (Cohen, Greenberg, & IsHak,2013).
The idea of reciprocal capacity building is an essential component of CBPR and stems
from the notion that as equal partners, community and academic partners have unique strengths
and contributions that can be harnessed as well as learning needs that must be addressed
(Minkler,2010; Trinh-Shevrin et al.,2007). In the context of HS, and particularly in light of
“big data” initiatives driven by PCORI and the Agency for Healthcare Research and Quality,
patient stakeholders may benet from capacity building in the use of big data initiatives
(Fleurence et al.,2014), whereas researchers may need a better understanding of contextual
factors, such as familial, neighborhood, and cultural inuences that affect patient health and
caregiving negatively and positively (Wallerstein & Duran,2010).
CBPR Principle
Strategies in Health
Services Research Examples from the Literature
Balance knowledge
generation and benet.
■ Explore study designs
that balance scientific
rigor with benefits to
participants and perceived
community concerns.
■ Such designs include
comparative-effectiveness trials
that compare two or more
relevant strategies, cross-over
control, or wait-list control
designs so no one is denied a
beneficial strategy.
Use a cyclical and
iterative process of
improving the study.
■ Work with stakeholders
to identify challenges and
potential solutions.
■ In Projects AsPIRE and DREAM,
coalitions met monthly to ensure
progress and address challenges.
Partners are involved in
dissemination.
■ Disseminate findings
through multiple vehicles
and strategies, ranging
from patient narratives and
forums, newspapers, policy
briefs, community forums,
and peer-reviewed articles.
■ Cancer survivors’ narratives
about treatment choices can be
more compelling than reviewing
recommended guidelines for
patients grappling with similar
decisions (Dohan et al.,2016).
Embrace a
commitment to
sustainability.
■ Prioritize sustainability from
project inception.
■ Commitment to the
sustainability of the community’s
capacity to remain engaged in
research increases investment
(Hacker et al.,2012).
TABLE 10.1 (CONTINUED)
CBPR in Health Care Settings 145
IMPLEMENTING CBPR IN HEALTH CARE SETTINGS: CHALLENGES
AND OPPORTUNITIES
Implementing community-partnered approaches in the design of health care interventions poses
opportunities and inherent challenges. Populations engaged in research may be more committed
to its use, particularly for HS (Chung et al.,2008). Engagement may increase attention to par-
ticipants’ life circumstances and cultures when designing interventions, which could yield more
acceptable interventions for minority populations (Schensul,2009). Research may be more fea-
sible if community members are engaged in its development (Halpern, Johnson, Miranda, &
Wells,2004).
Potential challenges to the application of CBPR principles in HS research can arise when
implementing evidence-based practices. These practices may or may not have been developed
with community input; the treatments and language to describe them may not be familiar to
stakeholders; they may compete with alternative practices in the community; or, they may raise
concerns about addressing health issues that are stigmatized and difcult to discuss. Overall,
there may be a greater risk that researchers will approach implementation from a top-down or
expert-driven approach.
A CBPR approach would emphasize a two-way knowledge exchange within equitable
partnerships, in which the clinical practice and research expertise is balanced with community
expertise in lived experience, cultural adaptation, and context. Given genuine engagement,
the system or research expert becomes part of the community of equal stakeholders, who
then can incorporate local ecology and community values in the partnership and interventions
(Trickett,1998).
Research partnerships that aim to develop new interventions or adapt existing, evidence-
based interventions for translation and dissemination to eliminate health disparities often
contend with practical constraints in under-resourced communities that have important implica-
tions for study design and methods. Innovative research methods need to be used to address the
numerous methodological challenges to ensure the rigorous design and analysis of interventions
in the health eld, which are appropriate to the community:
■ Decisions to randomize at levels above the individual (e.g., clinic, community) require
attention to potential cross-contamination effects and the feasibility of including a
sufcient number of units to achieve adequate precision in cluster randomized designs
(Murray,2015).
■ Improving the validity, reliability, and efciency of measurement means attention to mul-
tiple levels in diverse populations and low resource settings (Charns et al.,2012)
■ A CBPR process may require pre-specifying a participatory process to nalize a design
protocol, even when there has been substantial stakeholder input into developing the initial
research proposal.
■ High attrition or poor adherence to study protocols can bias standard intent-to-treat
analyses and especially affect racial-ethnic minorities living in under-resourced commu-
nities (Honas, Early, Frederickson, & O’Brien,2003; Zeller et al.,2004).
Table10.2 presents a brief summary of these challenges, research designs, and potential
solutions.
TABLE 10.2 Types of Study Designs and Pros and Cons for the Community
Study
Design
Randomized
Controlled Trials
Stepped Wedge
(or Lagged) Design
Pragmatic
Randomized Trials
Randomized
Encouragement Design
Design
description
May involve random
assignment to usual care
or no care condition, strict
inclusion or exclusion
criteria, controlled setting,
rigid interventions
Tested intervention is
rolled out randomly to
participants over a number
of time periods so that
everyone eventually gets
the intervention.
Tests the effectiveness of
an intervention in a broad
range of settings in order
to examine “if and how
an intervention works,”
controlling for “all known
biases and confounders,”
so that the intervention’s
effect is maximized
An encouragement trial
randomizes participants
to the control group
or to an opportunity
or encouragement to
receive an intervention.
Participants randomized
to the opportunity or
encouragement can
then decide whether to
engage and adhere to
the intervention (West
et al.,2008).
Strengths Strong internal validity All participants will receive
intervention; they can
model the effect of time
on an intervention as a
variable in assessing the
effectiveness.
Strong external validity
because of exible inclusion
or exclusion criteria and
testing interventions in
diverse, real-world settings
Strong internal and external
validity; addresses practical
and ethical challenges
associated with participants
engaging in interventions
inconsistent with their
preferences and evaluates
the acceptability to engage
in diverse interventions
Challenges Control condition group
receives no intervention
or an enhanced control
condition; limited external
validity because of
likelihood study will be
limited to participants with
one health condition (e.g.,
hypertension alone versus
hypertension, depression,
and diabetes) or limited
to one setting (e.g.,
primary care only versus
primary care, church, social
services settings)
Participant groups may
face delay in receiving
intervention; contamination
and extended learning
effects in participants
receive intervention later.
Participants could be
exposed to the general
idea of interventions, and
the single-blind approach
may lead to diminished
internal validity.
Potential difculty
drawing causal inferences;
involves randomization of
participants to different
interventions that may be
unacceptable for ethical
reasons and difcult
to implement
Study data collection
costs may be higher
because of requiring larger
number of participants
caused by smaller effect
sizes and greater within-
group variance, as well
as needing qualitative
and quantitative data on
compared intervention
implementation.
(Continued )
TABLE 10.2 (CONTINUED)
Study Design
Nonrandom Quantitative
Intervention Assignment Quasi-Experimental Designs Observational Studies
Design
description
Assigns participants to
particular groups based
on a numerical rank (e.g.,
community, household
income, level of risk); the
quantitative variable used
to assign groups and the
outcome variable of interest
used for causal modeling,
with separate modeling for
the different groups to enable
inferences regarding treatment
effect to be made
Participants are not randomly assigned to intervention
or control groups but are compared to the
intervention groups. Matching methods (e.g., using
propensity scores) to select controls can improve the
design validity, but it requires signicant details on
relevant sociodemographic and clinical characteristics
of a large population of individuals in a comparison
condition. Examples of studies include natural
experiments in which a policy or an intervention
is given to one community or group of individuals
while another similar group does not receive an
intervention, such as public insurance benets
or unconditional cash transfers (Costello, Erkanli,
Copeland, & Angold,2010).
Observes an aspect of
interest among a group of
participants over time
Strengths Addresses practical and ethical
concerns of randomized
studies; intervention can be
assigned based on meaningful
variables such as level of risk
Leverages existing differential policy implementation
in demographically equivalent groups for
evaluation purposes
Addresses practical and
ethical challenges of
randomized designs
Challenges May be difcult to interpret
study outcomes because of
the challenge of discerning the
precise relationship between
the quantitative assignment
variable and the outcome
variable of interest
Funding to respond in real time to evaluate
natural experiments may be difcult. Systematic
or unmeasured differences between compared
groups, such as secular trends or neighborhood or
community characteristics, may make it difcult to
interpret results and determine the impact of policy
or program.
Difcult to draw causal
inferences
CBPR in Health Care Settings 149
SHARED ANALYSIS, INTERPRETATION, AND DISSEMINATION
OF RESULTS
For more traditional HS or clinical researchers not familiar with CBPR processes, inclusion
of nonscientists or community partners in data analyses may seem particularly challenging.
Researchers may worry about compromised scientic integrity because of the limited capacity
of community partners to contribute meaningfully to the technical aspects of data analysis, or
the lack of “efciency” of data analysis with partners unfamiliar with statistical or qualitative
analyses. However, community members might be concerned about the lack of contextual and
historical knowledge that researchers bring to these partnerships.
What are the options to structure complementary roles and skills for academic and
community partners to work together in data analysis? Similar to all processes in a participatory
research project, community partners’ roles in data analysis and interpretation should be deter-
mined collaboratively, and, depending on the partnership, these roles may vary. For example,
if a partnership is new, expanding resources to cover partners’ participation may improve the
overall quality of the shared data. Multiple institutions have developed “Research 101” train-
ings or resources for nonscientists that provide an easy-to-understand overview of different
research methods. For example, PCORI’s “Methodology 101 Training Booklet and Resource
Guide” reviews study design, analysis, and interpretation for comparative effectiveness research
(PCORI, 2014). Training and resource manuals have also been created for clinicians on col-
laborating with researchers in HS research (Potter et al.,2010). Less has been done to train
researchers on how to learn about the ecology of lives in community settings.
Often if the technical data analyses are conducted by university partners, then data interpre-
tation can be done collaboratively. This generates trust and understanding of the research pro-
cess and ndings and further develops health care research that has greater external validity by
virtue of being more relevant and reective of partners’ perspectives and priorities.
Another potential benet of including community partners in data analysis and interpreta-
tion is the increased capacity of the partnership to conduct more effective research over time
through the augmentation of research skills. As one community partner in the Community Part-
ners in Care project noted, “Even though I didn’t completely understand all of the statistical
programming and numbers the rst time around, I felt that taking the time to have all of us
work together was important in building trust and making sure that we could do the work more
quickly the next time around.” In CBPR, it can be helpful to view research as two-way capacity
building in a shared process of exchanging expertise. For example, while sharing and training
community or patient stakeholders in analysis principles, it may be effective to have stake-
holders train academic partners on the meaning of concepts in community context or share
information on community resources and culture. In this way, all participants are valued in an
ongoing process of development, using a strength-based paradigm. Developing such a strategy
for partnered analysis can benet from intentional planning for inclusion of CBPR principles
into all phases of research design, including budgeting activities.
Partnered analysis goes hand-in-hand with partnered research presentations and publica-
tions, which also require preparation and anticipation of budgets (e.g., for travel to meetings).
In addition to traditional peer-reviewed approaches to dissemination, participatory research
projects in health care require approaches that share ndings and lessons learned with groups
150 Community-Based Participatory Research for Health
directly affected by the results (e.g., patients, community members), who might not read or have
easy access to academic journals or conferences. In developing a dissemination approach with
community collaborators, researchers must be open to a diversity of different partnerships. For
example, the Los Angeles health advocacy organization Healthy African American Families
(HAAF) II has partnered with hundreds of researchers over the last twenty-ve years and holds
all-day conferences in local community settings, such as churches or in the meeting rooms of
local community agencies for the local population. All events are free and invitations are sent
to nearly fty thousand individuals on their e-mail list. Individuals attending these conferences
range from the general public to policy makers, representatives of local community agencies,
health care clinics, mental health clinics, and churches. In order to incentivize attendance, audi-
ence members are offered free food or rafed prizes, such as gift cards, computer equipment,
or televisions. Continuing education credits are offered for the wide array of professionals in
attendance. The events often cover a particular health condition, such as cancer, depression,
diabetes, or autism, and the content of each conference is reective of the stage of implementa-
tion that HAAF II has reached with a research institution at the time. For conferences devoted to
disseminating the results of a recently completed research study, presentations range from tra-
ditional academic style presentations that summarize design, goals, outcome measures, results,
and interpretation of study ndings to small-group discussions on how attendees would interpret
the study ndings and what the potential implications for the ndings may be for community
members. This has been the case for a PCORI-funded study, DECIDE (Alegría, Grant ID 4187).
Other approaches include printed or e-mailed newsletters, presentation of study results in
local media (e.g., newspapers, radio, television), social media reports, or even through the art
initiatives. For example, one researcher supported adolescent patients’ work by collaborating
with a professional drama teacher to disseminate study ndings on improving hospital care
for adolescents with chronic health conditions. “A group of nine young people worked with
a professional drama teacher to create the play, using role-play and improvisation...Their
self-created rap urged the hospital board to listen to young people and adjust care to their needs”
(Van Staa, Jedeloo, Latour, & Trappenburg,2010). The key for ensuring appropriate dissemi-
nation is to actively collaborate on all aspects of dissemination so that the approaches, format,
and language used in the dissemination of results will be understood by and accessible to the
intended recipients.
VIGNETTES
In the following sections, we present three vignettes to illustrate the ideas we elaborate on in
this chapter.
Community Partners in Care (CPIC)
Community Partners in Care (CPIC) was a program-level randomized comparative effective-
ness trial of two interventions to support depression quality improvement across health care and
community-based agencies in Los Angeles. To our knowledge, CPIC is the rst randomized
US-based study of the added value of community engagement and planning beyond a tradi-
tional approach to implementing depression collaborative care (Ngo et al.,2016). According to
a Cochrane Collaborative Review, it is one of the few such comparative studies internationally
CBPR in Health Care Settings 151
in any eld of health (Anderson et al.,2015) that uses a community engagement intervention
that was implemented using a community-partnered participatory research (CPPR) approach,
a manualized form of CBPR developed in South Los Angeles, with community and academic
partners coleading under equal authority in all aspects of research. CPPR emphasizes princi-
ples such as equal partnership and power sharing between partners, which are reinforced in
a memorandum of understanding in all research phases. The study was designed and imple-
mented by the CPIC Council, co-led by UCLA, RAND, HAAF II, Behavioral Health Services,
Queens Care Health, Faith Partnership, and fty other agencies providing safety-net services.
The monthly meetings of the CPIC Council and working groups were supplemented as needed
by telephone, text, online, or e-mail voting to facilitate timely decision making in all phases
of research, following principles of CBPR (trust building, strength based, two-way knowledge
exchange, inclusive partnerships with full and equitable participation). Larger decisions were
discussed for further input with larger community groups in an open forum, such as a church,
museum, or movie theater. This reinforced that the community or patient representatives were
viewed as the primary stakeholders for major decisions. In these presentations, community and
academic partners as well as patients or family members presented what the council and work
groups had deliberated and provided their synthesized opinions and outlined pros and cons.
This process was used in nalizing the design for CPIC, developing the nal plan for interven-
tions, and presenting study ndings.
Both interventions were based on evidence-based depression quality improvement (QI) tool
kits, using a stepped-care approach with case management tool kits. Community engagement
and planning (CEP) supported networks of programs in tailoring tool kits to local communities
in a four- to six-month planning period followed by training in depression QI; resources for
services (RS) offered each program the opportunity to participate in twelve webinars and pri-
mary care site visits on depression collaborative care. Health care providers received training on
treatment (including assessment, therapy, and medication) and case managers and non-licensed
staff members received training on screening, referral, education, and behavioral management
skills. This approach could support patient engagement in evaluation and treatment regardless
of the door of entry to services.
The active inclusion of partners at all levels, but especially community and policy part-
ners, led to the rapid dissemination of the CPIC approach and ndings into health care policy
in two large urban areas: the County of Los Angeles (LAC) and city of New York’s public
health care systems. In Los Angeles, the Department of Mental Health with the Departments
of Public Health and Health Services proposed the Health Neighborhood Initiative to increase
service capacity for behavioral health homes under expanded Medicaid services. The Health
Neighborhood Initiative was added to the LAC Strategic Plan by the LAC board of supervisors
in 2014 and proposes to coordinate county services for shared behavioral health clients while
engaging neighborhood coalitions to address one or more locally prioritized social determinants
of mental health. This project is currently being supported by a $100 million investment through
the California Mental Health Services Act. Similarly, the city of New York’s Ofce of Health
and Mental Health has been actively exploring using the CPIC model as an approach to inte-
grate health care, mental health, and non-health-care community agencies to address depression
as part of their mental health road map or ThriveNYC initiative. This illustrates the potential of
CBPR to generate stakeholder engagement and support sustainability.
152 Community-Based Participatory Research for Health
PCORI
The PCORI-funded “Effectiveness of DECIDE in Patient-Provider Communication, Therapeutic
Alliance & Care Continuation” examined the combined effectiveness of a patient and provider
intervention designed to improve shared decision making (SDM), the working alliance, and
communication between patients with behavioral health issues and their providers. The patient
intervention (DECIDE-PA) was designed to encourage patients to ask questions in their clinical
sessions and increase their level of involvement in the management of their own care. This project
was the result of a partnership among Massachusetts General Hospital, the Disparities Research
Unit, thirteen clinics, and the community advisory board (CAB) of the overall study. The provider
intervention (DECIDE-PC) coached providers on how to be more receptive to their patients’
questions and concerns. The study took place in thirteen outpatient behavioral health clinics in
the Northeast region of the United States. Patient participants were between the ages of eigh-
teen and eighty; spoke English, Spanish, or Mandarin Chinese; and received behavioral health
care (e.g., psychotherapy, psychopharmacology, or counseling) from behavioral health providers
(e.g., psychiatrists, psychologists, social workers, addiction counselors, and mental health nurse
practitioners) enrolled in the study. The study recruited 312 patients and 74 providers.
Guided by principles of CBPR, the study was committed to involving patients, providers,
and other stakeholders throughout the course of the study, ensuring that they had a purposeful
and equal voice in the research. Stakeholder engagement efforts were led by the CAB, which
was composed of a patient, a patient caregiver or patient advocate, behavioral health clinicians,
and a community-academic liaison. CAB members met with the PI and leaders of the research
team on a bimonthly (sometimes monthly) basis throughout the course of the study and were all
equally compensated for their time helping design and implement the study.
First-year CAB activities included identifying strategies for clinic, provider, and patient
recruitment and reviewing and editing the provider’s and patient’s assessment questionnaires.
CAB members were also instrumental in shaping the patient and provider assessments so that
the data gathered could help produce ndings more relevant to diverse stakeholder groups. For
example, the CAB identied the need to add questions related to patient stigma about seeking
mental health care and issues related to continuity of care. The CAB also helped ensure the
comprehension of our assessment measures and other study materials, such as patient recruit-
ment yers.
In year 2, the CAB began to think about how best to disseminate study ndings, with many
suggesting peer conferences they could attend to present study ndings as well as ideas for
papers they wanted to write (in addition to helping with writing the main paper for the study).
The engagement of the CAB in paper writing started off with a formal introduction of writing
research papers from the study’s PI and project director, because some members of the CAB
had no prior experience in writing research papers. Beginning in year 3, CAB members played a
major role in planning focus groups to help disseminate preliminary study ndings, allowing the
study to get feedback from provider and patient stakeholders on their respective interpretation of
the ndings. Overall, the engagement of the CAB helped to make the study successful in recruit-
ing a wide range of clinics, providers, and patients. It facilitated the creation of assessment ques-
tionnaires that were more relevant to diverse stakeholder groups and dissemination activities that
provided contextual, real-world feedback on how to make the intervention practical and effective
for patients, providers, and other key stakeholders.
CBPR in Health Care Settings 153
DREAM (Diabetes, Research, Education, and Action for Minorities) Project
The DREAM Project, established in 2009, was a CBPR study developed in a partnership between
the NYU Center for the Study of Asian American Health (CSAAH) and a community coalition
serving the Bangladeshi American community in New York City (NYC). The overall goal of the
DREAM Project was to develop, implement, and test the efcacy of a community health worker
(Tomfohr, Schweizer, Dimsdale, & Loredo,2013) intervention designed to improve type 2 diabetes
mellitus control and management in the Bangladeshi community. The DREAM Coalition played
a critical role in informing intervention design—selecting a community health worker (CHW)
approach as a strategy to build on community assets and strengthen community leadership for
diabetes prevention and control. In developing this approach, community partners agreed to use
a rigorous methodology that balanced their concerns regarding the ethics of research design with
an understanding of the need for scientic rigor. This approach helped support the development
of an evidence base and policies for CHW integration in health care for underserved populations.
Using a two-arm randomized controlled trial (RCT) design, study participants were recruited
from hospitals, community health centers, primary care practices, and community settings,
including faith-based organizations (FBOs) and community-based organizations (CBOs). Partici-
pants were randomly assigned to either the control or treatment group. In a six-month intervention
program, treatment group participants received ve monthly educational sessions with an over-
view of diabetes, nutrition, physical activity, complications of diabetes, and stress management
and family support. In addition, CHWs conducted two one-on-one meetings with treatment group
participants to develop and implement individualized goal-setting plans.
CBPR principles were integrated into all phases of the DREAM study and operationalized
through a coalition partnership. This coalition included a diverse stakeholder group of those with
lived experiences as members of the community, as members living with or having family mem-
bers who have diabetes, FBOs, CBOs, health providers, ethnic media, and academic partners
serving the Bangladeshi community. The coalition, which met on a monthly basis, ensured that
the study maintained a delicate balance between academic research, community interests, and the
linguistic and cultural appropriateness of the research. A key participatory feature of DREAM
has been the integration of CHWs into the coalition and study team. The DREAM Project inter-
vention was delivered by four trained bilingual Bangladeshi CHWs who were trusted community
members and leaders with shared ethnicity, language, culture, and life experiences as study par-
ticipants. They served as a vital source of community knowledge and were closely involved in all
aspects of the study, including the development of study instruments, data collection, informing
research design, and interpreting study results. Throughout the intervention period, CHWs not
only worked with the participants but also with the participants’ care providers, family mem-
bers, support groups, and others to assist participants with diabetes control and management.
CHWs also played a key role in dissemination of the intervention through community forums
and the ethnic media. In addition to reporting results of the intervention back to the community,
community forums were also conducted in response to the community’s concerns and questions,
regarding new policies and initiatives (e.g., Affordable Care Act). Finally, CHWs also played
a capacity-building role in clinical settings by conducting cultural competency trainings with
medical students, residents, and health care providers at clinical sites to enhance knowledge
and understanding about unique religious and cultural practices that might inuence diabetes
management among Bangladeshi Americans.
154 Community-Based Participatory Research for Health
By employing CBPR approaches, the DREAM Project was able to ensure cultural and
social relevance for the community and facilitated linkages to the health care system in mean-
ingful ways that built on community assets and addressed concerns related to diabetes control.
The DREAM Project is now an established, trusted, and recognized community resource with a
high level of popularity in the New York City Bangladeshi community.
CONCLUSION AND RECOMMENDATIONS
There have been multiple calls for the increased involvement of community members in research
addressing health and well-being. Patient and consumer groups have long advocated for their
inclusion in the research process across multiple health outcomes including HIV/AIDS, mental
illness, diabetes, and environmental health concerns. These efforts often grew from those who
felt marginalized and disengaged from the research being conducted on their communities.
Later, researchers and policy makers joined these efforts because the benets to the quality
of the research process and the scope and impact of the research were seen to be improved by
increased community participation and the use of CBPR.
This chapter addressed the benets to HS research, particularly those engaged in clinical
trials, to broaden their research strategies and designs by using methods to increase community
involvement through the addition of patients or service users, their families and caretakers, cli-
nicians and administrators, and the communities within which research occurs. In fact, CBPR
is an effective tool for generating knowledge and developing models of care and treatment pro-
grams as well as policies to meet the needs of traditionally under-resourced and marginalized
populations. Through community partnerships, the design and conduct of research is strength-
ened and the impact of ndings on policy and practice is bolstered. Community involvement
in the development of research questions can increase the study’s relevance to patients and
service users and help researchers to be condent that they are addressing areas of real concern
to communities.
This chapter presented illustrative case studies for reecting on the inclusion of the
community in multiple study designs as well as the challenges these study designs could
present. We have described how community partners can contribute in meaningful and criti-
cal ways to the development of research, ensuring that assessment tools are appropriate and
respectful to patients in HS studies. In addition, we have shown how community involve-
ment in design, such as choosing appropriate recruitment strategies, can be critical to suc-
cessful research, because patients’ lived experiences of engaging with our health care systems
can help to identify appropriate points of interface with researchers at clinical sites; but more
important, bringing the voice of diverse stakeholders ensures that research is meaningful for
the different stakeholders.
As we continue to explore innovative models for the delivery and nancing of health care
services, we must be vigilant in ensuring that these services and approaches to deliver them meet
the needs of our most vulnerable populations. Inclusion of stakeholders in the research pro-
cess through CBPR may be one of our most powerful tools for this endeavor. This work is not
without its challenges, and efforts to increase community involvement in research should draw
on the success and challenges identied by previous HS researchers to improve our capacity for
integrating CBPR within health systems research.
CBPR in Health Care Settings 155
QUESTIONS FOR DISCUSSION
1. How do community partners benet from being included in the analysis and interpretation
of study results? How do academic partners benet from their inclusion?
2. Using Table10.1 as a reference, can you comment on the CBPR principles each vignette
portrays and any similarities or differences you see between CBPR in health care settings
versus community settings?
REFERENCES
Alegría, M., Alvarez, K., Ishikawa, R. Z., DiMarzio, K., & McPeck, S. (2016). Removing obstacles to eliminating racial and
ethnic disparities in behavioral health care. Health Affairs, 35(6), 991–999.
Anderson, L. M., Adeney, K. L., Shinn, C., Safranek, S., Buckner-Brown, J., & Krause, L. K. (2015). Community coalition-
driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database of
Systematic Reviews, 6, 1–189.
Charns, M. P., Foster, M. K., Alligood, E. C., Benzer, J. K., Burges s, J. F., Jr., Li, D., Mcintosh, N. M., Burness, A., Partin, M. R.,
& Clauser, S. B. (2012). Multilevel interventions: Measurement and measures. Monographs: Journal of the National
Cancer Institute, 2012(44), 67.
Chung, B., Jones, L., Campbell, L. X., Glover, H., Gelberg, L., & Chen, D. T. (2008). National recommendations for
enhancing the conduct of ethical health research with human participants in post-disaster situations. Ethnicity & Disease,
18(3), 378–383. Retrieved from www.ncbi.nlm.nih.gov/pubmed/18785455
Cohen, R. M., Greenberg, J. M., & IsHak, W. W. (2013). Incorporating multidimensional patient-reported outcomes of
symptom severity, functioning, and quality of life in the Individual Burden of Illness Index for Depression to measure
treatment impact and recovery in MDD. JAMA Psychiatry, 70(3), 343–350.
Concannon, T. W., Meissner, P., Grunbaum, J. A., McElwee, N., Guise, J.-M., Santa, J., Conway, P. H., Daudelin, D., Morrato,
E. H., & Leslie, L. K. (2012). A new taxonomy for stakeholder engagement in patient-centered outcomes research.
Journal of General Internal Medicine, 27(8), 985–991.
Costello, E. J., Erkanli, A., Copeland, W., & Angold, A. (2010). Association of family income supplements in adolescence
with development of psychiatric and substance use disorders in adulthood among an American Indian population. JAMA
Psychiatry, 303(19), 1954–1960.
D’Alonzo, K. T. (2010). Getting started in CBPR: Lessons in building community partnerships for new researchers. Nursing
Inquiry, 17(4), 282–288.
Dohan, D., Garrett, S. B., Rendle, K. A., Halley, M., & Abramson, C. (2016). The importance of integrating narrative into
health care decision making. Health Affairs, 35(4), 720–725.
Domecq, J. P., Prutsky, G., Elraiyah, T., Wang, Z., Nabhan, M., Shippee, N., Brito, J. P., Boehmer, K., Hasan, R., Firwana,
B., & Erwin, P. (2014). Patient engagement in research: A systematic review. BMC Health Services Research, 14(1), 1.
Fleurence, R. L., Beal, A. C., Sheridan, S. E., Johnson, L. B., & Selby, J. V. (2014). Patient-powered research networks aim to
improve patient care and health research. Health Affairs, 33(7), 1212–1219.
Fourie, C., Biller-Andorno, N., & Wild, V. (2014). Systematically evaluating the impact of diagnosis-related groups (DRGs)
on health care delivery: A matrix of ethical implications. Health Policy, 115(2–3), 157–164.
Ginsberg, S. (2017). Arthritis Patient Partnership with Comparative Effectiveness Researchers (AR-PoWER). Retrieved from
www.pcori.org/research-results/2013/arthritis-patient-partnership-comparative-effectiveness-researchers-ar-power
Hacker, K., Tendulkar, S. A., Rideout, C., Bhuiya, N., Trinh-Shevrin, C., Savage, C. P., Grullon, M., Strelnick, H., Leung, C.,
& DiGirolamo, A. (2012). Community capacity building and sustainability: Outcomes of community-based participatory
research. Progress in Community Health Partnerships: Research, Education, and Action, 6(3), 349.
Halpern, J., Johnson, M. D., Miranda, J., & Wells, K. B. (2004). The partners in care approach to ethics outcomes in quality
improvement programs for depression. Psychiatric Services, 55(5), 532–539.
Hickam, D., Totten, A., Berg, A., Rader, K., Goodman, S., & Newhouse, R. (2013). The PCORI methodology report.
Washington, DC: Patient-Centered Outcomes Research Institute.
156 Community-Based Participatory Research for Health
Honas, J. J., Early, J. L., Frederickson, D. D., & O’Brien, M. S. (2003). Predictors of attrition in a large clinic-based
weight-loss program. Obesity Research, 11(7), 888–894.
Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new
health system for the 21st century. Washington, DC: Author.
Islam, N. S., Tandon, D., Mukherji, R., Tanner, M., Ghosh, K., Alam, G., Haq, M., Rey, M., & Trinh-Shevrin, C. (2012).
Understanding barriers to and facilitators of diabetes control and prevention in the New York City Bangladeshi community:
A mixed-methods approach. American Journal of Public Health, 102(3), 486–490.
Meade, C. D., Menard, J. M., Luque, J. S., Martinez-Tyson, D., & Gwede, C. K. (2009). Creating community-academic part-
nerships for cancer disparities research and health promotion. Health Promotion Practice, 12(3), 456–462.
Minkler, M. (2010). Linking science and policy through community-based participatory research to study and address health
disparities. American Journal of Public Health, 100(S1), S81–S87.
Mockford, C., Staniszewska, S., Grifths, F., & Herron-Marx, S. (2012). The impact of patient and public involvement on UK
NHS health care: A systematic review. International Journal for Quality in Health Care, 24(1), 28–38.
Mullins, C. D., Abdulhalim, A. M., & Lavallee, D. C. (2012). Continuous patient engagement in comparative effectiveness
research. JAMA Psychiatry, 307(15), 1587–1588.
Murray, D. M. (2015). Design and analysis of studies to evaluate multilevel interventions in public health and medicine.
National Institutes of Health. Retrieved from https://prevention.nih.gov/docs/programs/mind-the-gap/mtg2015-murray-
presentation.pdf
Ngo, V. K., Sherbourne, C., Chung, B., Tang, L., Wright, A. L., Whittington, Y., Wells, K., & Miranda, J. (2016). Community
engagement compared with technical assistance to disseminate depression care among low-income, minority women:
A randomized controlled effectiveness study. American Journal of Public Health, 106(10),1833–1841.
Patient-Centered Outcomes Research Institute (PCORI). (2014). Methodology 101: Training for patients and stakeholders
[training booklet and resource guide]. Retrieved from www.pcori.org/sites/default/les/PCORI-Methodology-101-Training-
Booklet-and-Resource-Guide.pdf
Pearson, A., Jordan, Z., & Munn, Z. (2012). Translational science and evidence-based healthcare: A clarication and recon-
ceptualization of how knowledge is generated and used in healthcare. Nursing Research and Practice, 2012, 1–6.
Potter, M., Handley, M., Goldstein, E., Abrams, D., Alvarez, R., Benson, M., Benton, L. D., Bird, W., Fischer, D., & Raine-
Bennett, T. (2010). Community-engaged research with UCSF researchers: A resource manual for community-based clini-
cians. Retrieved from https://accelerate.ucsf.edu/les/CE/manual_for_clinicians.pdf
Schensul, J. J. (2009). Community, culture and sustainability in multilevel dynamic systems intervention science. American
Journal of Community Psychology, 43(3–4), 241–256.
Sharpe, R. (2013). Establishing a patient-centered research community for cystic brosis. Retrieved from www.pcori.org/
research-results/2013/establishing-patient-centered-research-community-cystic-brosis
Tomfohr, L. M., Schweizer, C. A., Dimsdale, J. E., & Loredo, J. S. (2013). Psychometric characteristics of the Pittsburgh
Sleep Quality Index in English-speaking non-Hispanic whites and English and Spanish-speaking Hispanics of Mexican
descent. Journal of Clinical Sleep Medicine, 9(1), 61.
Trickett, E. J. (1998). Toward a framework for dening and resolving ethical issues in the protection of communities involved
in primary prevention projects. Ethics & Behavior, 8(4), 321–337.
Trinh-Shevrin, C. (2014). Community health workers offer culturally tailored interactive workshops and counseling to Fili-
pino Americans, leading to improvements in medication adherence and cardiovascular risk factors. Retrieved from https://
innovations.ahrq.gov/proles/community-health-workers-offer-culturally-tailored-interactive-workshops-and-counseling
Trinh-Shevrin, C., Islam, N., Tandon, S. D., Abesamis, N., Hoe-Asjoe, H., & Rey, M. (2007). Using community-based
participatory research as a guiding framework for health disparities research centers. Progress in Community Health
Partnerships: Research, Education, and Action, 1(2), 195–205.
Van Staa, A., Jedeloo, S., Latour, J. M., & Trappenburg, M. J. (2010). Exciting but exhausting: Experiences with participatory
research with chronically ill adolescents. Health Expectations, 13(1), 95–107.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(S1), S40–S46.
West, S. G., Duan, N., Pequegnat, W., Gaist, P., Des Jarlais, D. C., Holtgrave, D.,...Clatts, M. (2008). Alternatives to the
randomized controlled trial. American Journal of Public Health, 98(8), 1359–1366.
Woolf, S. H., Zimmerman, E., Haley, A., & Krist, A. H. (2016). Authentic engagement of patients and communities can
transform research, practice, and policy. Health Affairs, 35(4), 590–594.
Zeller, M., Kirk, S., Claytor, R., Khoury, P., Grieme, J., Santangelo, M., & Daniels, S. (2004). Predictors of attrition from a
pediatric weight management program. The Journal of Pediatrics, 144(4), 466–470.
11
CHAPTER
NATIONAL CENTER FOR DEAF
HEALTH RESEARCH
CBPR WITH DEAF COMMUNITIES
STEVEN BARNETT, JESSICA CUCULICK, LORI DEWINDT,
KELLY MATTHEWS, AND ERIKA SUTTER
DEAF SIGN LANGUAGE users and people with hearing loss comprise health disparity popu-
lations overlooked by most public health research, surveillance, and programs (Barnett, McKee,
Smith, & Pearson,2011). The mission of the Rochester Prevention Research Center (RPRC) is
to promote health and prevent disease with populations of Deaf sign language users and people
with hearing loss through community-based participatory research (CBPR). These two popula-
tions differ in many aspects, including language, culture, and lived experience. Three similarities
are risk for health inequities, barriers to health care communication, and limited engagement
with public health. In this chapter, we focus on research conducted with Deaf sign language
users in Rochester, New York, by RPRC’s National Center for Deaf Health Research (NCDHR).
INTRODUCTION TO DEAF COMMUNITIES
Deaf communities. The word Deaf refers to identity and culture, not hearing acuity. This distinction
is sometimes indicated with an uppercase D. Use of sign language is a prime characteristic of being
Deaf. An individual’s audiogram is not relevant. For example, hearing children with Deaf parents are
often also Deaf. Most Deaf sign language users were born deaf or became deaf in early childhood.
Deaf culture, mores, and folkways come from a worldview shaped by common experiences and a
shared understanding of those experiences. Sign language is part of that shared experience.

158 Community-Based Participatory Research for Health
Language. American Sign Language (ASL) is the primary language used in US Deaf commu-
nities. ASL is indigenous to the United States and is not universally used by Deaf people around
the world. ASL is a natural, living language that evolved with US Deaf communities over time.
ASL and English are different languages; ASL is not a form of English. Similar to other languages,
ASL has “accents” and other regional variations, variations by social groups (such as age), and
jargon, such as specialized technical terminology used by Deaf professionals in a particular eld.
Diversity. The broad range of human diversity is expressed within Deaf populations,
including race, ethnicity, gender, sexual orientation, age, educational attainment, income, and
presence of physical disabilities and health conditions. The distribution of that diversity in Deaf
populations differs from the distribution in the US general population.
Early experiences. Most deaf children have hearing parents, and most hearing parents with
a deaf child do not become ASL uent. Many hearing people view being deaf in the context of a
medical model that wants to x being deaf. The attempts to “x” the child often occur in health
care settings and in school settings. These early experiences likely inuence a Deaf adult’s per-
ception of health care institutions and educational institutions. These perceptions, in turn, likely
inuence a Deaf person’s willingness to engage with health researchers, who are often from
university medical centers (a health care and educational institution).
Communities of Deaf ASL users are in some ways similar to, though also different from,
other language minority populations (Barnett,1999; Steinberg et al.,2006). Familiarity with
these similarities and differences is relevant to doing community-based participatory health
research with Deaf ASL users (Table11.1).
TABLE 11.1 Comparison of Deaf ASL-Using Communities and Some Other
Language Minority Groups
Similarities CBPR Relevance
Social
■ Use of a non-English language
■ Socialize and partner or marry
within community
■ Sociocultural norms different than
those of the majority community
■ Children often become bicultural
and bilingual.
■ Language minority model (cultural
model) approach fits better than a
medical model or disability model.
Health care
■ Infrequently encounter a doctor
from their own cultural group
■ Language differences and health
knowledge limitations are often
barriers to appropriate health care.
■ Many have poorer health than
those in the general population.
■ Less likely to visit a physician than
those in the general population
■ Inclusion of Deaf people on
the research team will be
welcomed and appreciated by
community members.
■ Low health literacy is common.
■ Research recruitment from
community settings will likely
work better than recruitment from
health care settings.
National Center for Deaf Health Research 159
Similarities CBPR Relevance
Opportunity
■ Lower education level,
socioeconomic status, and English
literacy than the general population
■ Often encounter prejudices that
limit opportunities
■ Limited access to English
language–based information
■ Written English recruitment
materials may have limited reach;
consider direct person-to-person
interactions in ASL; consider
videos in ASL.
Assimilation
■ Children forbidden to use
their language
■ Children taught that their language
is inferior
■ Some research terms (e.g.,
community voice) are reminders of
social and institutional oppression.
Research
■ History of oppression and
mistreatment influences
perceptions of research
■ Limited experience with survey
research and public health
surveillance
■ Negative experiences in health care
during childhood (to “fix” being
deaf) may explain some of the adult
suspicions of health researchers.
■ Common research practices (e.g.,
randomization, repeated measures)
may be unfamiliar and will likely
need explanation.
Biology
■ Biology sometimes used to justify
bias, barriers, and the existence of
social inequalities
■ Health research with deaf people
often focuses on ears and hearing,
rather than health.
Differences CBPR Relevance
Expectations Unlike members of other language
minority groups, Deaf people are
expected to do the following:
■ Have fluency in written English
■ Communicate with clinicians by
writing notes in English
■ Communicate with clinicians by
speech-reading in English
■ Language-congruent approaches
will be welcomed and will enhance
connection and recruitment.
■ Research teams that include
Deaf community members will
be welcomed and will enhance
connection and recruitment.
Cultural
transmission
■ Deaf culture and ASL are usually
transmitted horizontally (from
peers) rather than vertically
(from parents).
■ Health information (e.g., about
breastfeeding) likely comes from
Deaf peers and community leaders,
rather than hearing parents and
grandparents.
(Continued )
160 Community-Based Participatory Research for Health
CBPR FOR HEALTH WITH ROCHESTER DEAF COMMUNITIES
Rochester, New York, has a large, vibrant, and diverse Deaf population with deep local histor-
ical roots. The Rochester School for the Deaf (RSD), established in 1876 and still operating
today, works with deaf and hard-of-hearing children and their families. RSD also employs Deaf
teachers and staff members and has an active alumni association. The National Technical Insti-
tute for the Deaf (NTID) was established as one of the colleges of Rochester Institute of Tech-
nology (RIT) in 1966 to provide postsecondary technical education to people who are Deaf or
hard of hearing. NTID is the largest technical college for Deaf and hard-of-hearing students in
the United States, with about 1,400 NTID students included in the more than fteen thousand
RIT students. NTID and RIT employ faculty and staff members who are Deaf, and a number
of NTID/RIT graduates remain in Rochester. The critical mass of Deaf people inuences the
local Rochester economy, and many local companies hire qualied Deaf people for blue- and
white-collar jobs, and local service industries, such as restaurants, are comfortable with Deaf
customers. University of Rochester research and clinical training programs include Deaf grad-
uate students, medical students, and fellows. Deaf people migrate to Rochester, attracted by the
economic, social, and educational opportunities.
Similarities CBPR Relevance
Language
deprivation
■ Many Deaf children experience
limited exposure to accessible
language during the critical period
for language development.
■ Cognitive and interpersonal
consequences of early language
deprivation are associated
with health risks, conditions,
and outcomes.
■ Cognitive and interpersonal
consequences of early language
deprivation are relevant to
the relationship building
required for CBPR.
Legal
■ Guidelines for health care
communication with Deaf people
come from the Department of
Justice (DOJ).
■ Guidelines for health care
communication with others who
have low English proficiency come
from the Department of Health
and Human Services.
■ Legal guidelines from the DOJ
apply to health research.
■ There is no standard approach used
by funders regarding budgets for
communication access services.
Source: Adapted from Barnett (1999) and Steinberg et al. (2006).
TABLE 11.1 (CONTINUED)
National Center for Deaf Health Research 161
The Rochester Deaf Health Task Force (RDHTF) is the immediate precursor to the
community-academic collaboration that became RPRC/NCDHR. The RDHTF was a diverse
stakeholder group formed in 2003 to identify local health and health care priorities with Roch-
ester’s large Deaf population (Rochester Deaf Health Task Force, 2004). RDHTF included rep-
resentatives from Deaf communities, community-based organizations, health care (including
clinicians and insurers), public health, and academic institutions.
The RDHTF identied the absence of health data from Deaf communities as a major lim-
itation to identifying priorities. RDHTF members decided to address this lack of data and sub-
mitted a proposal to CDC to establish RPRC/NCDHR, with an initial core research project to
develop accessible health surveillance to collect basic health data from Deaf ASL users. The
CDC Prevention Research Centers (PRC) Program funded RPRC/NCDHR in 2004, and many
from the RDHTF became members of the RPRC/NCDHR Deaf Health Community Committee
(DHCC) or one of the other RPRC/NCDHR committees.
With the establishment of RPRC/NCDHR and a focus on creating accessible surveil-
lance, community-academic collaboration grew. Researchers and DHCC members worked
together to prioritize topics to include in the Rochester Deaf Health Survey, translated
English language survey questions (Graybill et al.,2010) and developed new survey ques-
tions, recruited community members to help RPRC/NCDHR evaluate and improve the survey,
recruited community members to take the survey, interpreted preliminary ndings, dissem-
inated research ndings to local and national stakeholder audiences, and chose next steps
in the research process. RPRC/NCDHR dissemination includes coupling RPRC/NCDHR
academic journal articles (Barnett, Klein, et al.,2011; Barnett, McKee, et al.,2011) with
videos that present in ASL the content of the written English article (Table11.2; at the end of
the chapter).
With data from the rst Rochester Deaf Health Survey, Rochester’s Deaf communities
could, for the rst time, select health research priorities based on their own data. RPRC/NCDHR
and DHCC members hosted community forums to share ndings of the 2008 Rochester Deaf
Health Survey, discuss interpretation of ndings, and identify next steps. Deaf community
members selected three health priorities based on ndings from the 2008 Rochester Deaf Health
Survey: obesity, partner violence, and suicide risk (Barnett, Klein, et al.,2011). RPRC/NCDHR
successfully obtained research funding for all three priorities. RPRC/NCDHR’s second core
research project focused on obesity: the Deaf Weight Wise clinical trial.
CBPR, INTERVENTION DEVELOPMENT, AND RESEARCH DESIGN
For the RPRC/NCDHR Deaf Weight Wise (DWW) clinical trial, we adapted for use with Deaf
adult ASL users a healthy lifestyle intervention (Weight Wise) previously demonstrated to be effec-
tive with a different population (rural women in North Carolina) (Samuel-Hodge et al., 2009). Deaf
and hearing researchers and community members worked together to adapt interventions materials,
measures, and methods to be culturally appropriate and language congruent. Key to the success of
the two-year DWW clinical trial are the Deaf people on the research team, including as research
coordinators and other research staff members.
Deaf and hearing RPRC/NCDHR research team members worked with DHCC members to
make important decisions on research trial design. Following are three examples.
162 Community-Based Participatory Research for Health
DWW intervention. Researchers and community members agreed that all DWW interven-
tion leaders must be Deaf and not hearing people working with interpreter services or hearing
people who are ASL uent. Team members felt strongly that having DWW group meetings con-
sist only of Deaf people, including a Deaf person as the intervention group leader, would be a
benet to the intervention. Designing the trial with Deaf people as intervention leaders provided
another opportunity for RPRC/NCDHR to “give back” to the community by providing training
and employment. RPRC/NCDHR trained and employed ten Deaf people to be DWW coun-
selors during the two-year clinical trial.
Delayed-start design. Researchers and community members discussed the need to com-
pare those who received the DWW intervention with those who did not. Randomization to
“usual care” would mean that half the people enrolled in the trial would not receive an inter-
vention at all. Whereas hearing people have access to myriad healthy lifestyle interventions,
there are no healthy lifestyle interventions designed for use by Deaf people. RPRC/NCDHR
researchers and community members agreed that the DWW randomized trial design would
assign people to either immediate intervention or intervention delayed one year. This approach
permitted research comparison, at the trial midpoint, of those who participated in the DWW
intervention and those who had not yet. The delayed-start design also meant that everyone in
the trial would participate in the DWW intervention, important because there are no accessible
alternative interventions.
Informed consent information. Research informed consent information presented in writ-
ten English is often challenging to understand for many people. It is best to present research
consent information in the primary language of the person considering research participation.
Prior to DWW, RPRC/NCDHR presented research study information in a video monologue
in ASL. The study information video for the 2008 Rochester Deaf Health Survey was seven
minutes long, and many Deaf Health Survey participants complained about the video length.
Researchers and DHCC members discussed informed consent processes for the DWW clinical
trial. The research detail required to make an informed decision about participation in a two-
year clinical trial would result in an ASL video that was twice as long as the video for the 2008
Rochester Deaf Health Survey. The group decided to use a video novella approach to presenting
research consent information. The video novella has been used to present health information in
ASL to Deaf audiences (Pollard, Dean, O’Hearn, & Haynes,2009) and in spoken Spanish to
Hispanic audiences (US Food and Drug Administration,2014). RPRC/NCDHR worked with
the University of Rochester institutional review board (IRB) to adapt the video novella approach
for use in research informed consent. The DWW consent video novella was successful in terms
of presenting information needed for viewers to make a decision about DWW participation and
in terms of the viewers’ experience of the video. The DWW consent video was eighteen min-
utes long, and no one complained that the video was too long (see Table11.2).
RPRC/NCDHR growth and success during this period meant that RPRC/NCDHR was con-
ducting multiple research projects simultaneously. Some research participants found it difcult
to keep track of which RPRC/NCDHR research projects they had already participated in, in part
because the computer-based surveys looked similar. A project-specic logo, developed in col-
laboration with Deaf artists, became a communication aid to help RPRC/NCDHR research staff
members to identify the different projects with participants and to provide a visual memory aid
to help research participants remember whether they had participated in a specic project. The

National Center for Deaf Health Research 163
logo development process enhanced the feeling of shared project ownership by community and
research team members and provided an opportunity for RPRC/NCDHR to employ Deaf artists
and graphic designers (Figure11.1).
RPRC/NCDHR CAPACITY BUILDING
Building relationships is essential for successful CBPR. RPRC/NCDHR facilitates this by
bringing together community members with researchers and Deaf people with hearing people.
The process of learning about each other builds trust needed for CBPR.
Deaf people work in RPRC/NCDHR in a variety of roles, including as faculty and staff mem-
bers, trainees, teachers, community members, advisors, and RPRC/NCDHR committee mem-
bers, including the executive committee. RPRC/NCDHR community committees bring together
Deaf and hearing individuals and organizations that would otherwise not interact. RPRC/NCDHR
community engagement with DHCC focused primarily on collaboration with individuals. We
created the local partner advisory board (LPAB) to better engage with community organizations
and institutions, such as Rochester School for the Deaf, the local county health department, and
health insurers. Center-wide retreats include diverse stakeholders and encourage dialogue and
feedback to inform RPRC/NCDHR development.
Relationship building is one facet of growing capacity; research training is another. RPRC/
NCDHR worked with DHCC to create a training program to teach Deaf community members
about research ethics and to develop together the Cross-Cultural Research Competencies Cur-
riculum (Table11.2) to teach hearing researchers about CBPR with Deaf communities. Summer
internship programs foster the interest of deaf and hearing college students in CBPR and public
health research. RPRC/NCDHR summer interns have subsequently gone on to medical and
nursing schools and research PhD programs. Deaf and hearing graduate students, postdoctoral
fellows, faculty members with research career development awards, and community members
do research training with RPRC/NCDHR.
Communication is vital to RPRC/NCDHR capacity building, as is the funding to support
communication access services. Interpreter services are needed for all communication that
includes Deaf ASL users and people who do not know ASL. This includes communication
General NCDHR logo. The image depicts
the ASL sign for “health.”
Logo for the Deaf Weight Wise (DWW)
clinical trial with Deaf people ages 40–70.
The person is showing the ASL sign for
“success.”
Logos © University of Rochester
FIGURE 11.1 Examples of RPRC/NCDHR Logos Designed by Deaf Community Partners
164 Community-Based Participatory Research for Health
during weekly RPRC/NCDHR staff meetings, RPRC/NCDHR committee meetings and
retreats, trainings that include Deaf teachers or Deaf students with people who do not know
ASL, professional conferences and research networking opportunities, and telephone calls and
other interactions with funders. If the costs of communication access come from core program
budgets, accessible programs will have fewer resources for research or programs, and this per-
petuates disparities. RPRC/NCDHR continues to explain to funders and other audiences the
necessity of communication access services and has successfully advocated with some funders
to provide budget supplements to support communication access services.
Capacity building related to communication also includes supporting the development of
ASL skills among faculty and staff members who are not ASL uent. RPRC/NCDHR includes
Deaf people as staff members, trainees, and faculty members, working alongside hearing people
with a range of ASL skills. RPRC/NCDHR hires qualied Deaf teachers to tutor RPRC/NCDHR
faculty and staff members who are interested in learning ASL or improving their ASL skills.
RPRC/NCDHR’s commitment to tutoring demonstrates an appreciation of the value of ASL,
important for relationships and trust. The tutoring program supports informal communication
that builds relationships and trust, in the workplace and with communities. Clear communication
is paramount, and RPRC/NCDHR works with interpreter services for formal workplace commu-
nication that includes people not ASL uent and for RPRC/NCDHR-sponsored events.
RPRC/NCDHR growth and capacity building also requires collaboration with IRBs. CBPR
health research with Deaf adult ASL users was new for the University of Rochester IRB, and
standard IRB-required training was not accessible to some Deaf ASL users. RPRC/NCDHR
researchers, DHCC members, and the University of Rochester IRB agreed to an approach to
adapt the content of existing written English-language CITI training modules into ASL. This
process enabled RPRC/NCDHR to include more DHCC members as research team members.
To ensure appropriate IRB review of ASL materials, RPRC/NCDHR met with IRB lead-
ership to develop ways to ensure that research participants were safe and that informed con-
sent information was accessible. We discussed approaches to evaluating the ASL measures and
certifying the accuracy of the translations. The University of Rochester IRB agreed to assign
one IRB specialist to all RPRC/NCDHR research; the continuity was helpful for relationship
building and efciency and added a level of cultural awareness to the University of Rochester
IRB team. The University of Rochester IRB and RPRC/NCDHR worked together to develop
mutually agreeable approaches to documenting informed consent that did not require Deaf adult
ASL users to sign their names to written English consent forms (See Figure11.2 below).
RPRC/NCDHR sometimes needed to navigate potential conicts between research needs
and relationship needs. One example from the DWW clinical trial involved inclusion criteria.
DWW had strict parameters regarding eligibility for the clinical trial, including age range
(40–70) and BMI (25–45). Some Deaf individuals wanted to enroll in the trial but were ineligible
because of age or BMI. It was a challenge for RPRC/NCDHR to turn people away, especially
because there were no accessible alternative programs to refer people to. Some RPRC/NCDHR
faculty and staff members also work as clinicians in the University of Rochester Department
of Psychiatry’s Deaf Wellness Center (DWC). RPRC/NCDHR and DWC worked together to
create an accessible alternative to DWW, called the Mindful Eating Group. The DWC Mind-
ful Eating Group was led by ASL-uent therapists who used psychotherapeutic techniques to
encourage healthy choices, and the cost to participate was covered by some health insurance
National Center for Deaf Health Research 165
policies. This solution was good for relationships, research, and institutional and community
capacity building.
CULTURE-CENTEREDNESS APPROACH
The RPRC/NCDHR experience of CBPR with Rochester Deaf communities ts the culture-
centeredness approach (CCA) (see Chapter 2; Dutta, 2008; Wallerstein et al., under review).
The collaboration creates space for and encourages agency through shared decision making and
Deaf Weight Wise Research Study: Consent Form with Signatures
Documentation of Consent
■ I have watched a video about Deaf Weight Wise. I was given a copy of the video.
■ I understand what it means to be involved in the Deaf Weight Wise research study.
■ I agree that it is my choice to participate in the Deaf Weight Wise research study.
■ I will get a signed copy of this form and information letter.
Research Subject:
___________________________________________________________
Print Name
___________________________________________________________
Signature
Person Obtaining Consent (Research Staff)
■ The person watched a video in sign language about the Deaf Weight Wise study.
■ The person was able to ask questions and all questions were answered.
■ The person understands the Deaf Weight Wise study.
■ I will provide the person with a copy of this consent form.
___________________________________________________________
Print Name and Title
___________________________________________________________
Signature
____________ Research subject watched video no.: _____________
Date
FIGURE 11.2 Documentation of Consent Signature Form
166 Community-Based Participatory Research for Health
acknowledging the expertise in communities. The Rochester collaboration values and fosters
the trust necessary for critical reection that occurs during retreats, committee meetings, and
community forums. Working together, the Rochester collaboration transformed some dominant
practices in research culture, such as the IRB changing processes and academic journals pub-
lishing ASL videos to accompany written English articles about Deaf communities. Clear com-
munication and safe, bidirectional sharing of knowledge has been essential to our collaboration.
LESSONS LEARNED
We have learned a great deal about community-researcher collaboration to do CBPR with Roch-
ester Deaf communities, and those lessons inform non-research collaborations and research with
other communities. We have listed some key lessons that contributed to our growth and success.
Work with Deaf people. RPRC/NCDHR conducts research with Deaf people, not for Deaf
people, and not on Deaf people. The collaboration is a partnership with shared decision making.
The collaborative process begins early in a project, with research topic selection and research
project design. Each project provides opportunities to learn, strengthen relationships, and build
trust. New projects build on the foundation created by prior projects; the investment in the
current project contributes to the current project and to future projects. We list this lesson rst
because of its paramount importance. This lesson also permeates other lessons listed in the fol-
lowing paragraphs.
Shared ownership. RPRC/NCDHR research works best when Deaf and hearing people,
working together, feel shared ownership for the project. Having you work on my project, or hav-
ing me work on your project, does not work as well as having us work together on our project.
Achieving shared ownership often requires early collaboration and mutual development of a
project, which builds trust and meaningful relationships.
Cultivate relationships. The infrastructure of RPRC/NCDHR is built on relationships.
We recognize that relationships are the primary resource for our CBPR work. Relationships
require attention. One way we nurture relationships is by working with Deaf communities,
and acknowledging the value they add to our research together. Clear, accurate, and accessible
communication is vital to relationships. RPRC/NCDHR commits resources for communication
access services, including sign language interpreter services and tutoring in ASL, to support an
environment that nurtures relationships. Experiences of present-day collaborations have roots
in history. Knowing about the historical context can help build relationships (Table11.3; at the
end of the chapter).
Find common values. A goal of RPRC/NCDHR research is to promote health and
well-being. This is consistent with a value in Deaf communities to “give back,” such as to
provide a needed service. RPRC/NCDHR research “gave back” with a breastfeeding project
(see Box 11.1), providing accessible information and support to Deaf mothers. RPRC/NCDHR
“gave back” with the Mindful Eating Group, providing an accessible alternative program to
Deaf Weight Wise for those who did not qualify for the research trial. For some researchers,
“giving back” initially felt outside of their scope as researchers, but when viewed in the frame
of “common values,” the process of “giving back” was recognized as being consistent with
“promoting health and well-being.”
National Center for Deaf Health Research 167
Recognize community strengths. RPRC/NCDHR researchers and community members
work together to identify and prioritize disparities for research and intervention. Although
RPRC/NCDHR grant proposals often emphasize disparities to successfully compete for grants,
RPRPC/NCDHR research also seeks to identify community strengths. These strengths, and
sharing information about these strengths, have inherent value, cultivate relationships, empower
individuals and communities, and support a sense of self-worth. Sometimes collaborative discus-
sions of community strengths identify strategies and resources that will help address disparities.
These lessons learned reinforce RPRC/NCDHR’s commitment to the values of CBPR and
help ground us in our efforts to work together with communities to promote shared ownership
of health research in order to achieve our mutual goal to improve health and well-being with and
within Deaf communities.
QUESTIONS FOR DISCUSSION
1. Think about the following two true statements:
A. Throughout history (including today), hearing people routinely have devel-
oped and still use visual communication systems in situations in which sound is
Box 11.1 Deaf Moms and Infant Care Project
RPRC/NCDHR research topics are selected in collaboration with communities. Some research topics
are identied from community forums to share and discuss RPRC/NCDHR research data, other topics
come from discussions during community meetings, and some are selected based on recent events or
experiences. The Deaf Moms and Infant Care project came about from the last category.
During an RPRC/NCDHR executive committee meeting, the chair of the Deaf Health Community
Committee (DHCC), a Deaf woman who was currently pregnant, wondered about the infant care
knowledge and experiences of other Deaf women and their sources of information. The RPRC/NCDHR
director and the rest of the RPRC/NCDHR executive committee agreed that this was a great topic
for research. The DHCC chair began attending the weekly meetings of the RPRC/NCDHR research
committee to learn more about research. RPRC/NCDHR devoted resources to the project and facilitated
a connection with hearing faculty mentors with related research interests and relevant research expertise
to work with the DHCC chair and other Deaf women who joined the project. Communication during
these project team meetings was facilitated by interpreter services funded by RPRC/NCDHR. The project
team adapted qualitative research methods to be accessible for use in research with Deaf people.
The DHCC chair presented ndings from the project at national public health conferences and an
international Deaf conference. The project ndings were published in written English in a peer-reviewed
health journal (Chin et al.,2013). The project team and research participants also shared ndings with
other Deaf women through the production of informational videos in ASL regarding breastfeeding.
RPRC/NCDHR provided video-editing support and facilitated posting the completed videos online to
make them broadly available (Table11.2).
168 Community-Based Participatory Research for Health
inadequate, inappropriate, or unavailable for clear and accurate communication.
Some examples:
• Hand and body signals used in baseball by umpires, coaches, and players
• Signal mirrors used by hikers, militaries, and others
• Hand signals used by underwater divers
B. Throughout history (including today), some deaf people have been forbidden to use
sign language, even though sound is unavailable and inadequate for clear and accurate
communication. Speech reading, a form of visual communication, is visually limited
compared with the visual range available in American Sign Language.
How do you explain the two different approaches to visual communication?
How would you feel if society prevented you from using a communication modality
that worked for you?
How likely would you be to engage with health researchers from that society?
When you answered that question, did you assume the “health researchers” were hearing?
What do the assumptions about “health researchers” teach us about bias?
Do you think whether a health researcher is Deaf or hearing would make a difference
in terms of Deaf community members’ willingness to engage? What other factors
might inuence that engagement?
2. Personal experiences of discrimination can inuence an individual’s trust. Historical
events, such as the Tuskegee Syphilis Study and the slow US response to the AIDS epi-
demic in the 1980s (predominantly affecting gay communities and other minority commu-
nities), can inuence a community’s trust for generations.
In what ways do you think this is true with Deaf communities?
In what ways do you think Deaf communities might be different than some other
minority communities? What about minority Deaf communities, such as African
American Deaf communities or LGBT Deaf communities?
TABLE 11.2 Online Resources Related to CBPR for Health with Deaf Communities
Resource Link
General Information about RPRC/NCDHR
Rochester Prevention Research Center: National
Center for Deaf Health Research
(RPRC/NCDHR) website
www.urmc.edu/ncdhr
RPRC/NCDHR Cross-Cultural Research
Competencies Curriculum
www.urmc.rochester.edu/ncdhr/information/
training/cross-cultural-competency.aspx
National Center for Deaf Health Research
YouTube Channel
www.youtube.com/user/NCDHResearch
National Center for Deaf Health Research 169
Resource Link
General Information about RPRC/NCDHR
American Sign Language Video-Blogs (“vlogs”) about Research Concepts, Produced by
RPRC/NCDHR
How do I become a research volunteer?
What is a randomized controlled trial?
What is informed consent?
What is a cognitive interview?
Peer-driven recruitment
www.youtube.com/watch?v=AB5ULOxpPhI
www.youtube.com/watch?v=9MRKgdXiOP8
www.youtube.com/watch?v=uqobwRzqiLg
www.youtube.com/watch?v=vGyBEitJvS0
www.youtube.com/watch?v=lFDm1Q4TLlM
American Sign Language Video Adaptions of Published Academic Articles
Barnett, S., Klein, J. D., Pollard, R. Q., Jr., Samar,
V., Schlehofer, D., Starr, M.,...Pearson, T. A.
(2011). Community participatory research with
deaf sign language users to identify health
inequities. American Journal of Public Health,
101(12), 2235–2238.
An American Sign Language video adaption
of this article was also created by RPRC/
NCDHR and the Deaf Health Community
Committee. The video is available in the journal’s
online appendix.
Full article:
www.ncbi.nlm.nih.gov/pmc/articles/
PMC3222424/pdf/2235.pdf
ASL video adaption of article available in online
appendix (scroll to bottom of page):
http://ajph.aphapublications.org/page/
VideoArchive
ASL video adaptation also posted here: www.
urmc.rochester.edu/ncdhr/research.aspx
Barnett, S., McKee, M., Smith, S. R., & Pearson,
T. A. (2011). Deaf sign language users, health
inequities, and public health: Opportunity for social
justice. Preventing Chronic Disease, 8(2), A45.
An American Sign Language video adaption of
this article was also created by the RPRC/NCDHR
and community partners. The two-part video
is posted on the journal’s web page along with
the article.
Full article: http://cdc.gov/pcd/issues/2011/
mar/10_0065.htm
ASL video adaption of article:
www.cdc.gov/pcd/issues/2011/mar/10_0065.
htm#Appendix
ASL video adaptation also posted here:
www.urmc.rochester.edu/ncdhr/research.aspx
Community-driven Health Information in ASL
Deaf Breastfeeding Project
Breastfeeding facts and stories from the
Deaf community
Breastfeeding facts: Information for Deaf moms
Main page: www.youtube.com/channel/
UChEfH47LLsnrgRdV3WgjN_A
Video 1: www.youtube.com/
watch?v=m36FCJLQLGs
Video 2: www.youtube.com/
watch?v=P53LvHkJrYE
(Continued )
170 Community-Based Participatory Research for Health
Resource Link
General Information about RPRC/NCDHR
Research Informed Consent in ASL
The Deaf Weight Wise Study: informed consent
in American Sign Language
www.youtube.com/watch?v=ZVGSOGcQRNU
American Sign Language Video-Blogs (“vlogs”) about the Importance of Public Health
Surveillance with Deaf Communities
Deaf Health Survey 2013 movie www.urmc.rochester.edu/ncdhr/research/deaf-
health-survey-2013.aspx
Deaf Health Survey 2013 vlog in American
Sign Language
www.youtube.com/watch?v=gggDQm4DaRw
Education and Training Programs
Rochester Bridges to the Doctorate program http://deafscientists.com/
Rochester Postdoc Partnership: Rochester
Partnership for Research and Academic Career
Training of Deaf Postdoctoral Scholars
www.deafpostdoc.urmc.edu
TABLE 11.3 Significant Historical Events Relevant to Community-Based
Participatory Research for Health with Deaf Communities
Year Event
Relevance to CBPR for Health
with Deaf Communities
1817 American School for the Deaf: The
rst permanent school for Deaf people
in the United States established in
Hartford, Connecticut (now called the
American School for the Deaf). The
founders include Laurent Clerc, a Deaf
man and a graduate of and teacher
at the Royal Institute for the Deaf in
Paris, and Thomas Hopkins Gallaudet,
a hearing American from Hartford who
visited Paris to learn about educating
Deaf children.
■ Acknowledges and demonstrates the
value of specific programs developed by
and for Deaf people
■ Social determinants of health: access to
education and employment
■ Successful collaboration of deaf and
hearing people
TABLE 11.2 (CONTINUED)

National Center for Deaf Health Research 171
Year Event
Relevance to CBPR for Health
with Deaf Communities
1864 Gallaudet College: The rst college for
Deaf people in the world established
in Washington, DC (now Gallaudet
University).
■ Social determinants of health: access to
education and employment
■ Many past and current Deaf community
leaders are Gallaudet graduates.
■ Successful collaboration of deaf and
hearing people
1876 Rochester School for the Deaf
established.
■ One institution that led to the rise of
Rochester’s Deaf communities
■ Social determinants of health: access to
education and employment
1876 Telephone invented. The telephone
connected hearing people with other
hearing people. Deaf people did not
communicate directly over telephone
lines until the development of the
teletypewriter (TTY) and acoustic coupler
nearly one hundred years later.
■ Amplified the separation of hearing and
Deaf people and institutions
1880 Milan Conference: endorses spoken
language over sign language for
education of Deaf students. Of the 164
participants, from the United States and
some European countries, one was Deaf.
The conference’s endorsement of spoken
language was not unanimous.
■ Social determinants of health: changes
in education approach associated with
worsening of educational attainment,
literacy, and employment, still evident today
■ Loss of Deaf role models, including Deaf
teachers and other successful Deaf adults
■ Hearing people not valuing ASL
■ Hearing people making decisions for Deaf
people, especially for Deaf children
■ Some research terms (e.g., community
voice) are reminders of social and
institutional oppression.
1880 National Association of the Deaf (NAD)
is established by Deaf Americans “to
deliberate on the needs of the deaf as
a class.” NAD continues to advocate
today for the needs of Deaf communities,
including opposing the suppression of
sign language.
■ Self-determination
■ Self-advocacy
■ Community leadership
(Continued )
172 Community-Based Participatory Research for Health
Year Event
Relevance to CBPR for Health
with Deaf Communities
1966 National Technical Institute for the Deaf
(NTID) established at Rochester Institute
of Technology (RIT). NTID is the largest
technical college for Deaf and hard-of-
hearing students in the United States.
■ One institution that contributed to the
rise of Rochester’s Deaf communities
■ Social determinants of health: access to
education and employment
■ Many Deaf community leaders are NTID/
RIT graduates.
■ Successful collaboration of deaf and
hearing people
1960s Teletypewriter (TTY) invented. The TTY,
developed by a Deaf engineer, made it
possible for Deaf people to communicate
directly over telephone wires via typing.
■ Access to information
■ Access to community
■ Telecommunication led to changes in
in-person communication
■ Led to changes in the roles of local
Deaf clubs
1973 Rehabilitation Act: federal law that
forbids discrimination and mandates
access in programs that receive federal
funding; as with other civil rights laws,
societal change was not immediate
■ Social determinants of health:
acknowledges barriers to access to
education, health care services, and
employment
1988 Deaf President Now (DPN): Gallaudet
students led a movement that
successfully advocated that one of the
qualied Deaf candidates be selected
as the rst Deaf president of Gallaudet
University.
■ Self-determination
■ Self-advocacy
■ Successful broad collaboration
1990 Americans with Disabilities Act (ADA):
federal law that forbids discrimination
and mandates access across a variety
of societal entities (public and
private) and infrastructure; mandates
telecommunication relay services to make
telephone networks accessible; as with
other civil rights laws, societal change
was not immediate
■ Social determinants of health:
acknowledges barriers to access to
education, health care services, and
employment
TABLE 11.3 (CONTINUED)
National Center for Deaf Health Research 173
ACKNOWLEDGMENTS
The work described here was funded in part by the CDC Prevention Research Centers Program
(U48 DP000031, U48 DP001910, and U48 DP005026), a CDC Community Transformation
Grant (U58 DP003599), and a grant from the Association of Teachers of Preventive Medicine
(ATPM) in collaboration with CDC (TS-0817). The ndings and conclusions in this chapter are
those of the authors and do not necessarily represent the ofcial position of the funders.
Thank you to the staff and faculty members, students, Deaf Health Community Committee
(DHCC) members, research participants, other community members, other stakeholders, and
funders who contributed to the success of the Rochester Prevention Research Center: National
Center for Deaf Health Research. We also thank our partners, including the National Technical
Institute for the Deaf at the Rochester Institute of Technology. With deep gratitude we thank
Thomas A. Pearson, the founding director of RPRC/NCDHR.
REFERENCES
Barnett, S. (1999). Clinical and cultural issues in caring for deaf people. Family Medicine, 31(1), 17–22.
Barnett, S., Klein, J. D., Pollard, R. Q., Jr., Samar, V., Schlehofer, D., Starr, M.,...Pearson, T. A. (2011). Community partic-
ipatory research with deaf sign language users to identify health inequities. American Journal of Public Health, 101(12),
2235–2238.
Barnett, S., McKee, M., Smith, S. R., & Pearson, T. A. (2011). Deaf sign language users, health inequities, and public health:
Opportunity for social justice. Preventing Chronic Disease, 8(2), A45.
Chin, N. P., Cuculick, J., Starr, M., Panko, T., Widanka, H., & Dozier, A. (2013). Deaf mothers and breastfeeding: Do unique
features of deaf culture and language support breastfeeding success? Journal of Human Lactation, 29(4), 564–571.
Dutta, M. J. (2008). Communicating health: A culture-centered approach. Malden, MA: Polity Press.
Graybill, P., Aggas, J., Dean, R., Demers, S., Finigan, E., & Pollard, R. (2010). A community-participatory approach to adapt-
ing survey items for deaf individuals and American Sign Language. Field Methods, 22(4), 429–448.
Pollard, R. Q., Dean, R. K., O’Hearn, A., & Haynes, S. L. (2009). Adapting health education material for deaf audiences.
Rehabilitation Psychology, 54(2), 232–238.
Rochester Deaf Health Task Force. (2014, August). Deaf Health Task Force report. Rochester, NY: Finger Lakes Health
Systems Agency. Retrieved January 30, 2017, from www.urmc.rochester.edu/ncdhr/information/documents/FLHSARD-
HTFreport2004.pdf
Year Event
Relevance to CBPR for Health
with Deaf Communities
2004 National Center for Deaf Health
Research (NCDHR) is established in
Rochester, New York.
■ CBPR for health applied to work with
Deaf communities
■ Engages, trains, and employs Deaf
people in health research and programs
■ Raises awareness with agencies in the
US Department of Health and Human
Services regarding disparities
■ Successful broad collaboration
174 Community-Based Participatory Research for Health
Samuel-Hodge, C. D., Johnston, L. F., Gizlice, Z., Garcia, B. A., Lindsley, S. C., Bramble, K. P.,...Keyserling, T. C. (2009).
Randomized trial of a behavioral weight loss intervention for low-income women: The Weight Wise Program. Obesity,
17(10), 1891–1899.
Steinberg, A. G., Barnett, S., Meador, H. E., Wiggins, E. A., & Zazove, P. (2006). Health care system accessibility. Experi-
ences and perceptions of deaf people. Journal of General Internal Medicine, 21(3), 260–266.
US Food and Drug Administration. (2014, December 2). ¡Nunca Más! Novelas. Retrieved January 31, 2017, from www.fda.
gov/ForConsumers/ByAudience/ForWomen/ucm269846.htm
Wallerstein, N., Oetzel, J., Duran, B., Magarati, M., Pearson, C., Belone, L., Davis, J., DeWindt, L., Lucero, J., Ruddock, C.,
Sutter, E., Villegas, M., Dutta., M. (under review). Culture centeredness in community-based participatory research: Its
impact on psycho-social health interventions. Social Science and Medicine.
12
CHAPTER
ASIAN AMERICANS (AAs) COMPRISE 5.6 percent of the US population, and in metropolitan
areas make up between 13 percent (New York City and Los Angeles) to 33 percent (San
Francisco) (Hoeffel, Rastogi, Kim, & Shahid,2012). The AA category includes East Asian (e.g.,
Chinese, Japanese, Korean); South Asian (e.g., Bangladeshi, Indian, Pakistani); Southeast Asian
(e.g., Filipino, Cambodian, Thai, Vietnamese); and sometimes Pacic Islander Americans (e.g.,
Native Hawaiians, Chamorros, Marshallese), denoting a vastly diverse array of subpopulations
with unique ethnic, cultural, linguistic, and historical proles, stretching across the Asian con-
tinent and its millions of islands. The US AA population is projected to double in size to more
than 43 million by 2050 and comprise approximately 40 percent of the country’s immigrant
population (Hoeffel et al.,2012). More than 65 percent of AAs are foreign-born immigrants
and refugees who come from low-income, limited-English- procient (LEP) backgrounds, com-
pounding the unique challenges faced by these communities (Ortman & Guarneri,2009).
Given the diversity of the AA community and a changing history of how racial and ethnic
groups have been categorized, the use of consistent terminology regarding the AA community
presents a challenge. AAs are dened here using the US Census 2000 classication as a race of
“individual people having origins in any of the original peoples of the Far East, Southeast Asia,
or the Indian subcontinent.” In this chapter, we did not include Native Hawaiian and Pacic
Islanders (NHPIs) because of their different political realities and major disparities that are
masked when aggregated with the AA population and, as such, contend that CBPR efforts in
NHPIs warrant exclusive attention.
CBPR IN ASIAN AMERICAN
COMMUNITIES
NADIA ISLAM, CHARLOTTE YU-TING CHANG, PAM TAU LEE, AND CHAU
TRINH-SHEVRIN
176 Community-Based Participatory Research for Health
CBPR’S RELEVANCE FOR AA COMMUNITIES
Tandon and Kwon’s (2009) review of fty-three articles on CBPR in AA communities high-
lighted key reasons why CBPR approaches are appropriate and relevant for AA communities.
AAs are subject to the “model minority myth.” AAs have been unfairly portrayed as a
“model minority” in many societal outcomes. From a broad perspective, this stereotype
implies that Asian Americans are not an underprivileged racial-ethnic minority because of
their economic success compared with other racial-ethnic groups; accordingly, Asian Ameri-
cans merit neither resources nor attention as an ethnic minority group within the American
population. The persistence of this myth is also reected in continued portrayals of Asian
Americans in the media as overachieving, successful, and without problems (Kristof,2015;
Murphy,2011; Powell,2011). In health, this is driven by and a result of a systematic lack
of collection, reporting, and analysis of AA data (Islam et al., 2010; Yi, Kwon, Sacks, &
Trinh-Shevrin,2016). Prior to 2010, there were few epidemiologic studies of AA health in the
United States, with most data part of studies examining multiple racial-ethnic groups. Recent
large-scale AA studies have documented health status diversity, though analysis on any aggre-
gated AA sample still masks disparities across and among subgroups. CBPR studies, with the
principles of dening communities of identity and local context, have therefore played impor-
tant roles in documenting these health disparities that traditional epidemiologic research fails
to capture.
AAs represent many separate racial and ethnic groups. CBPR approaches enable researchers
to take differences across Asian subgroups into account with each aspect of the research process.
CBPR strategies involving community health workers (CHWs) have strengthened the ability to
engage Bangladeshi and Korean populations in cardiovascular disease and diabetes prevention.
Bangladeshi CHWs have leveraged the cultural value of niyiom (“rules to live by”) to moti-
vate community members’ commitment to engaging in healthy behaviors. Korean American
populations’ preferences for health-promotion efforts delivered by health professionals led to
the use of a team-based care approach with CHW-led diabetes prevention and control studies.
Although cultural awareness is critical, CBPR approaches also call for reexivity and cultural
humility. This requires a balance between incorporating important cultural norms and beliefs
into research and interventions while avoiding cultural stereotypes.
AAs often live in densely populated “ethnic enclaves.” Asian ethnic groups often reside
heavily in centralized geographic locations, particularly in urban areas, thereby creating ethnic
enclaves. These communities’ close geographical proximity lends itself to working within
community contexts in CBPR.
CBPR is an asset-based and community-building approach that is particularly relevant
for immigrant communities. Recent AA immigrants often feel disempowered by traditional
top-down research and wary of research because of their immigration status. By contrast, CBPR
validates community members’ expertise and capabilities as researchers and agents for social
change to engage the entire community. In our work in New York City and New Jersey Filipino
communities, coalition development efforts focused on inclusion of a broad range of stake-
holders organized around wellness (Aguilar et al.,2010). In immigrant communities, the role
of storytelling and personal narratives (Trinh-Shevrin, 2014) have been compelling ways to
engage communities already marginalized by their social position.
CBPR in Asian American Communities 177
An updated literature search (2007–2015) found an additional 266 publications that described
a CBPR or community-engaged framework in AA communities, with approximately half explic-
itly using a CBPR approach.
CBPR CASE STUDIES
First, we highlight a federally funded research center rooted in a CBPR approach with AA com-
munities at local, regional, and national levels. Second, we highlight a local effort to demonstrate
how a CBPR partnership involving Asian immigrant workers built community capacity, lead-
ership, and equitable participation while also organizing the community toward policy change.
Case Study 1: National Research Center of Excellence in Asian American
Communities: NYU Center for the Study of Asian American Health
In 2003, the NYU Center for the Study of Asian American Health (CSAAH) was established
with funding from the National Center for Minority Health and Health Disparities (NCMHD)
Project EXPORT initiative. In the following sections, we describe our evolution as a federally
funded research center rooted in CBPR principles and our impact on improving the health of
Asian Americans.
Phase 1 The funding of CSAAH in 2003 formalized a long-standing relationship among the
New York University School of Medicine and several community partners that promote health
research and access in underserved AA communities across New York City (NYC) (Trinh-
Shevrin et al.,2007). CSAAH and its community partners were interested in conducting AA
health disparities research using CBPR. Given the considerable cultural variations among
AA ethnic groups, political dynamics among the community-based organizations (CBOs),
fragmentation among the AA population, and paucity of pan-Asian CBOs, it was critical to
nurture existing relationships and create new relationships with community partners during the
establishment of the center.
Three key principles guided CSAAH’s relationship building with NYC AA community
partners: (1) creating and sustaining multiple partnerships, (2) promoting equity in partnerships,
and (3) commitment to action as well as research (Trinh-Shevrin et al.,2007,2015). Each of
these principles aligned with a CBPR approach.
Creating and Sustaining Multiple Partnerships Building on the central CBPR tenet of engaging
multiple and diverse stakeholders in the research process (see Chapter1; Israel, Eng, Schulz, &
Parker,2013; Parker et al.,2010), one of CSAAH’s guiding principles was to create and sustain
partnerships with multiple CBOs and leaders serving NYC’s AA community. First, CSAAH
developed or participated in ethnic-specic and pan-Asian advisory groups. In developing advi-
sory boards, we recruited stakeholders from health and non-health sectors (e.g., worker’s rights,
faith, arts and cultures) to ensure that members could provide nuanced and context-driven
perspectives. We also developed operational norms, guidelines, and bylaws for each coalition that
were driven by coalition members, particularly community stakeholders, to facilitate consensus
building and communication and dene partner roles, thus enhancing accountability among
178 Community-Based Participatory Research for Health
members. Partnership roles were further delineated through letters of support for grant applications
and memoranda of understanding that formalized the roles, responsibilities, and activities of
respective partners. Finally, outside of the work of the coalition, CSAAH staff members and
investigators engaged in reciprocal support through participation in CBO activities, joining CBO
advisory or executive boards, or cosponsoring health events. Engagement in CBOs, from the
Chinatown YMCA, the Korean American Services of Metropolitan NYC, the DREAM Coalition,
the Kalasugan Coalition, to pan-ethnic boards, such as Project CHARGE, strengthened our
voices in community efforts and deepened the acceptance and legitimacy of our collective work
to advance health and well-being. Together, these steps were important in demonstrating mutual
understanding, respect, and reciprocity between CSAAH and its community partners and
establishing processes and norms for the academic-community collaboration.
Promoting Equity in Partnerships A central strategy in building equity was to ameliorate
negative stereotypes that stemmed from the historical lack of attention to immigrant and AA
needs by academics, particularly in NYC. Using a multipronged approach, we built capacity
within the center to understand diverse communities through the hiring of diverse staff members
and investigators, as well as promoting institutional understanding through seminars, symposiums,
and trainings for faculty members and leadership.
To establish equity in grants development and the distribution of resources, we undertook
two action steps. First, we created spaces and mechanisms for partners to play an equal role in
pursuing grants and research projects, including identifying the research priorities and method-
ologies. By engaging partners at the beginning to ensure their ownership of a research project
through meetings, brainstorming sessions, and joint grant writing, we have successfully main-
tained the active participation of community partners throughout several CBPR projects they
and CSAAH have initiated. For example, our research on the role of CHWs in reducing chronic
disease disparities among AA populations was driven by community partners’ desires to build
on the strong history of community organizing and lay leadership in many Asian immigrant
communities. We have, therefore, developed and tailored CHW interventions for the Chinese,
Korean, Filipino, Bangladeshi, and Asian Indian communities in response to our partners’ needs
and perspectives. Second, we negotiated distribution of research funds depending on the roles
and responsibilities by CSAAH and community partners. Because all partners helped develop
research priorities and methods, they gained a greater appreciation for resources they would
need to implement outreach, training, and research activities. Furthermore, to promote co-
learning, academic and community partners received education and training on grant writing,
budgeting, research design, and community engagement. As a result of learning exchanges, we
have been able to more condently and accurately estimate the funding partners need on an
ongoing basis to engage in research activities.
Commitment to Action as Well as Research A key feature of CBPR is a commitment to
turning research results into impactful action. To accomplish this, we maintained a strong
commitment to community-level dissemination by engaging with ethnic media as a primary
source of health and other information within AA communities. Second, CSAAH built advocacy
efforts into our research platform early, including encouraging locally elected ofcials to attend
CSAAH events, recognizing them for their support, educating them on AA health issues, and
CBPR in Asian American Communities 179
working with legislators directly to increase their awareness of AA health disparities. CSAAH
also mobilized community partners to advocate for funding on specic health disparities issues
to deepen coalition efforts to ensure sustainability beyond the research partnership.
Phase 2 In 2007, CSAAH received renewal funding from NIMHD to establish itself as a National
Research Center of Excellence. Although this offered an opportunity to ensure AA health dis-
parities were addressed at the national level, it also presented the challenge of balancing the
evolving needs of a federal institutional stakeholder (NIH) with those of community and public
health stakeholders and ensuring sustained community ownership of CSAAH research prior-
ities and framework based on CBPR principles. In doing so, CSAAH used a population health
equity framework to maximize the impact of our work in promoting population health while
remaining grounded in participatory, context-driven approaches to address health disparities in
AA communities (Trinh-Shevrin et al.,2015).
Apply a Social Determinants of Health Perspective to Research For community partners
across all Asian subgroups and sectors, the social determinants approach for equity is especially
relevant because they are confronted on a daily basis with the role that social inequities and
position play, including immigration and refugee status, racism, and discrimination. For AA
communities that are predominantly rst- and second-generation immigrants, a transnational
approach that integrates life course frameworks allows for greater elucidation of the role of
migration, immigration, and acculturative experiences on health and how they differ across
generations and are aligned with CBPR’s focus on context-driven research and action (Acevedo-
Garcia, Sanchez-Vaznaugh, Viruell-Fuentes, & Almeida,2012; Spallek, Zeeb, & Razum,2011).
For example, CSAAH has supported pilot studies to understand the impact of early childhood–
intervention programs in Chinese and Bangladeshi communities (Huang, Calzada, Cheng, &
Brotman,2012) and has initiated mixed-methods needs assessments in youth and older adult
populations to better understand contextual factors affecting the health of these communities.
Intergenerational strategies have been profoundly inuential in mobilizing Filipino American
community members to the Kalusugan Coalition and strengthening CSAAH’s outreach,
recruitment, and retention efforts for various studies (Aguilar et al.,2010).
Use a Multi-Sectorial (Health in All Policies) Approach With multi-sector coalitions, CSAAH
was well positioned to consider a health in all policies approach that integrates health considerations
into decision making on policies within health and other sectors. From 2012 to 2014, CSAAH
co-led the innovative CDC-funded Strategies to Reach and Implement the Vision of Health Equity
(STRIVE) program, which worked with fteen CBOs serving AAs and NHPIs across the United
States. Guided by a multi-sector coalition, each site led the development and implementation of
culturally relevant and sustainable, high-impact, policy, systems, and environmental strategies to
improve access to healthy food and increase physical activity within their local communities,
reaching an estimated 1,472,373 people across the United States (Patel et al.,2014).
Invest in Asset-Based Approaches That Build Human and Social Capital We used a CBPR
assets-based approach at the local level to recognize the role of lay leaders such as CHWs,
frontline public health professionals who have a unique understanding of and are trusted
180 Community-Based Participatory Research for Health
members of the community. Several of CSAAH’s NIH and CDC research studies have
demonstrated the efcacy and effectiveness of a CHW model to improve access to health care
and cardiovascular disease and diabetes-related outcomes for Filipino (Ursua et al., 2014),
Bangladeshi (Islam, Wyatt, et al.,2013), Asian Indian (Islam et al.,2014), and Korean (Islam,
Zanowiak, et al., 2013) populations. Using a CBPR framework, studies have elucidated the
cultural and social mechanisms through which CHWs affect health outcomes. For instance, in
their study of a CHW intervention on diabetes management among Bangladeshi individuals
in NYC, Islam and colleagues found statistically signicant increases in reported self-efcacy
in accessing health care. Qualitative ndings provided support by demonstrating specic
mechanisms through which CHWs were able to enhance self-efcacy, such as assisting female
participants with learning to access and navigate public transportation systems so that they were
able to attend regular doctor visits without relying on family or friends (Islam, Wyatt, et al.,2013).
Build Sustainability through Internal Structures To ensure that research is action driven, CBPR
calls for research partners to address and build in sustainability, including strengthening CBO
infrastructure, from the outset of program development. Through a subcontract with the UNITED
SIKHS, a major community partner serving the South Asian communities in NYC and nationally,
CSAAH investigators invested approximately $198,000 over the course of ve years to support the
implementation and development of a CHW initiative housed within the organization. By
enhancing the capacity of the organization to engage in health programming and evaluation efforts
and supporting CHWs as part of the organization’s staff, UNITED SIKHS has subsequently been
successful in initiating new efforts to address oral health, policy, systems, and environmental
strategies to improve access to healthy foods and access to care in the South Asian community.
UNITED SIKHS acquired more than $600,000 in additional funding as either a lead or
subcontracted agency. Similarly, of the fteen funded CBO partners of the STRIVE program, six
have gone on to successfully receive a CDC grant as the lead agency to implement, enhance, and
strengthen existing policy, systems, and environmental strategies to address chronic disease-related
risk factors affecting AA and NHPI local communities. In the case of several of our community
partners, sustainability moved beyond the immediate interventions and also encompassed
sustaining the core infrastructure to support organization’s efforts independent of CSAAH funds.
Thus, though CSAAH experienced an evolution in terms of structure, scope, and purpose,
a commitment to employing CBPR principles through all phases of our center’s development
enabled us to develop action-oriented research, programs, and policies across diverse AA com-
munities at the local and national levels.
Case Study 2: Developing Worker Leaders, Adapting CBPR Principles,
and Moving Policy Action at the Local Level: San Francisco Chinatown
Restaurant Worker Health and Safety Study
The San Francisco Chinatown Restaurant Worker Health and Safety Study was conducted by
a community-university–health department collaboration that undertook extensive efforts to
facilitate equitable participation among its members, in particular with its immigrant worker
partners. The partnership’s experience underscored that participation of non-English-speaking
immigrant community members cannot be taken for granted given the complex power dynamics
CBPR in Asian American Communities 181
at play within diverse partnerships. The “participatory starting points” (Chang et al.,2013) or
“participatory readiness” (Belone et al.,2016) of immigrant communities, may be affected by
members’ language and civic skills as well as the larger “contexts of reception,” or economic,
social, and political opportunity structures and societal signals of inclusion or exclusion in
which they are embedded (Bloemraad,2006).
This case study describes the worker leadership development process and the application
and adaptations of CBPR principles of the partnership that took into account the participatory
starting points of immigrant worker partners. The research effort ultimately ended with ground-
breaking policy change addressing wage theft at the city level and with the building of critical
community capacity at multiple levels. It serves as an example of how efforts initiated in one
immigrant community can have broader societal impact in helping to lift up conditions beyond
the ethnic enclave.
Research Context: Setting and Partnership Restaurants are the largest employer of Chinese
immigrants in San Francisco’s Chinatown district. Health issues in restaurants include traditional
occupational health concerns such as cuts, burns, falls, and on-the-job stress (Jayaraman,2013;
Webster,2001) and also encompass serious economic and social risk when employers engage
in “wage theft” by not paying the legal minimum wage or delaying or withholding payment of
wages or benets earned by employees (Minkler et al.,2014).
Building on previous collaborations, a partnership was formed in 2007 to carry out a CBPR
study of working conditions and health among Chinatown restaurant workers. The research used
an ecological approach and included focus groups with restaurant workers, a survey of working
conditions and health among 433 Chinatown restaurant workers, observations of working con-
ditions in 106 of the 108 neighborhood restaurants, and a mixed-methods evaluation of the part-
nership (Gaydos et al.,2011; Minkler et al.,2014).
Partners included the Chinese Progressive Association of San Francisco (CPA), a grass-
roots CBO; two universities (the University of California, Berkeley, School of Public Health
and its Labor Occupational Health Program [LOHP] and the University of California, San Fran-
cisco, School of Medicine); and the Occupational and Environmental Health Section of the San
Francisco Department of Public Health (SFDPH). Notably, in addition to the professional staff
members participating at CPA, nine current and former immigrant Chinese restaurant workers
provided on-the-ground community expertise to the research, analysis, and action components.
The study presented an important opportunity for each of the partners involved. Community-
based partners would be able to leverage scientic research in their work to address the ongoing
economic hardship workers in the Chinese immigrant community were facing and in the pro-
cess build worker leadership capacity. And university and health department partners commit-
ted to community-driven research and action and focused on issues of work and health were
able to collaborate with trusted community partners on the effort.
Contexts of Reception and Participatory Starting Points Contexts of reception were men-
tioned by worker partners in evaluation interviews as potentially affecting the “participatory
starting points” of community participants in the project, for themselves in the partnership and
for survey respondents. Relevant contexts included limited job opportunities, social marginaliza-
tion, and discrimination, which worker partners tended to link to a lack of English language skills.
182 Community-Based Participatory Research for Health
Work-related challenges were identied by worker partners as among their and their
community’s most pressing problems. They described how people often could not transfer
their job skills from their countries of origin to the US labor market because of language bar-
riers. Reecting on the economic vulnerability of new immigrants in particular, they noted how
seldom people questioned difcult or problematic working conditions as a result. Key among
these was wage theft, which had been a critical issue in the community for years. Worker part-
ners additionally described experiences of feeling not fully incorporated into broader society
or of being actively rejected or discriminated against in public spaces and social interactions,
again, primarily because of English language limitations.
Regarding challenges to their own participation in the project, worker partners again drew the
connection to language, reecting the relative positions of privilege within the partnership based
on English language facility, though also on the basis of scientic training. One worker described
feeling nervous and intimidated when joining in project meetings with the rest of the partners even
after undergoing trainings with CPA staff members on the project and even when Chinese was the
primary language used during meetings because she felt “everyone else’s English was so good.”
Worker Leadership Development Based on years of organizing in the community, CPA
staff partners anticipated challenges that a research partnership in particular would present
for worker participation. Together with the project director from LOHP, who played a critical
bridging role having grown up in Chinatown and with deep ties to the community, CPA staff
partners designed a worker partner recruitment and training plan to support worker engagement
in the project as well as in CPA’s longer term organizing efforts for preventing wage theft and
increasing labor rights.
Workers partners engaged in an initial eight-week training followed by biweekly meet-
ings with CPA staff members that facilitated their in-depth participation throughout the
project. The trainings and leadership development component of the project used a popular
education approach with interactive, participatory, and learner-centered activities that incor-
porated critical reection and community action (Chang et al.,2012). Activities included risk
mapping (Brown,2008), power mapping (Ritas, Minkler, Ni, & Halpin,2008), workshops on
policy making, mock food inspections in a simulated kitchen, and the use of visual triggers
for discussion (images of Chinese restaurant workers in various work-related situations). The
exercises supported workers in drawing connections between their own lives and the study and
CPA-organizing goals and helped to draw out their knowledge and expertise.
In addition to enhancing participation and building community capacity, the worker leader-
ship development component provided critical co-learning opportunities for the entire partnership.
Workers’ active participation and contributions yielded rich information and insights throughout
the research and action phases, from developing the survey and checklist tools and procedures to
data interpretation and in planning for and taking action.
Application and Adaptations of CBPR Principles Acknowledging variations in local context,
CBPR principles encourage individual partnerships to adapt their approaches to collaboration
because “no one set of CBPR principles is applicable to all partnerships” (see Chapter3).
One example of the partnership’s adaptations was alterations to its collaborative struc-
tures, following the recommendations of CPA staff partners. They moved toward a more
CBPR in Asian American Communities 183
separate and parallel process in which there were meetings of the primarily English- speaking
institutional partners (university, CPA staff members, DPH) and meetings of primarily
Chinese-speaking partners (worker partners, CPA staff members, and university members).
English-speaking university and health department partners would individually attend and
participate in the worker partner meetings and trainings from time to time, and full “steering
committee” meetings of all partners together occurred twice during the project.
This adaptation created space for community members to safely participate on their own
terms and to develop skills and engage in transformative critical reection and action, while
forming their own relationships to the project and to each other. In this arrangement, trusted
facilitators playing critical bridging roles, such as CPA staff members and the LOHP project
director, became even more central to facilitating effective communication among all partners.
During the two full steering committee meetings when all project partners were present,
the sessions were conducted in Cantonese with simultaneous translation provided to English-
only speakers. Prior to the meetings, partners from CPA, the university, and the DPH also
discussed and prepared for “stepping back” their own participation to make more space for
worker partners.
Policy and Community Capacity Outcomes In addition to building worker leadership capacity,
the Chinatown study from the beginning was focused on generating data for policy and practice
that could help promote change (Minkler et al.,2014). DPH partners reached out to several key
agencies with study results urging stronger enforcement of existing labor laws, began verifying
workers compensation insurance when issuing new business licenses to restaurants (Gaydos
etal.,2011), and later would coordinate with the Ofce of Labor Standards Enforcement to
suspend health permits of food facilities across the city with outstanding labor law violations
( Minkler et al.,2014). At the same time, CPA cofounded the Progressive Workers Alliance
(PWA), which developed a “low-wage worker bill of rights” and pushed the San Francisco
board of supervisors to pass an anti-wage theft ordinance in 2011, followed by a dedicated
Wage Theft Ordinance Task Force in 2012. These actions would be pivotal to the success of sev-
eral important campaigns in subsequent years, including one involving a $4 million settlement
between a major Chinese restaurant and its workers in 2014 (Hua,2015).
In addition to policy gains, a major outcome of the Chinatown study was the individual,
organizational, and community capacity built through the training and active engagement of
the worker partners and community members in the study. Worker partners described over-
coming fear of engaging with new people, gaining experience speaking in public, and a gener-
alized sense of “courage,” condence, and ability to think about social issues. They additionally
reported learning about worker rights, labor laws, and Chinatown restaurant working conditions.
CPA acquired new grants and trained a new generation of worker leaders, several of whom
remain active as the community leadership core with the organization. CPA has continued to
organize on wage theft and other issues of importance to the community, while also forging
alliances and expanding its national-level movement building efforts on other economic and
racial justice issues. Through the project, critical transformation took place at the individual
level for members of the partnership, including worker partners, as well as at the organiza-
tional, community, and the broader society levels through its contributions to policy change and
continued organizing efforts.
184 Community-Based Participatory Research for Health
CONCLUSION: OPPORTUNITIES AND FUTURE CONSIDERATIONS FOR
CONDUCTING CBPR IN ASIAN COMMUNITIES
As demonstrated throughout this chapter, there are robust CBPR efforts in AA communities
at national and local levels. Nationally, a growing commitment to the CBPR approach in AA
communities, evidenced by the exponential growth in the published literature and the funding
of research infrastructures to support community-engaged research in Asian communities, pro-
vides researchers, advocates, and funding agencies with key evidence that CBPR produces sus-
tainable efforts that amplify and address the health needs of this growing population ( Hoeffel
et al.,2012; Ortman & Guarneri,2009). As highlighted in our second case study, CBPR efforts
at the local level require a deep commitment to multi-sector engagement that is iterative, mul-
tistep, and reective in nature. Moreover, careful attention to integrating capacity-building
efforts into all stages of the research process is crucial. Whereas the local CBPR effort focused
on a single AA community of interest, the national example illustrates clearly the increased
complexity of collaborating over time with multiple AA communities and the opportunities
and challenges of pan-ethnic work. Community participation helps ensure that unique cultural
perspectives and strengths are built into interventions. From national and local examples, prac-
titioners have a wealth of best practices from which to draw in initiating CBPR in their own
communities.
In addition to the benets and strengths of CBPR, our case studies demonstrate some of
the unique challenges faced in using this approach in AA communities, such as those related to
inclusivity and addressing diversity across myriad AA ethnic groups, immigrant statuses, and
language prociencies.
We anticipate that these challenges and strategies used to address them will serve as a
basis for key future considerations in conducting CBPR in AA communities, incorporating
multilevel and equity-based strategies. Some of these considerations are highlighted in the
following:
■ The United States is facing the growth of new waves of emerging, smaller AA immigrant
groups throughout the country (such as the Himalayan and Burmese communities). Many
of these populations have migrated as refugees and have acute health needs, yet their
relatively small size may mask their disparities and issues in regional and local research
efforts. CBPR researchers working in AA communities must maintain a commitment to
engaging and building capacity in new and emerging communities while continuing to
engage with more established communities, which can be challenging in the context of
limited resources. In doing so, there are opportunities to share best practices and capacity-
enhancing models across communities, new and established.
■ Particularly concerning may be the growth of discriminatory language and fears, such as
Islamophobia, which will affect a growing number of refugees and immigrants with Islamic
religious backgrounds. CBPR partnerships may have to strengthen our determination to
raise sensitive issues and confront the norms and values as well as the structural inequalities
that face diverse populations. CBPR may be more important than ever to systematically
document the health risks and concerns these communities may be experiencing and allow
CBPR in Asian American Communities 185
communities under attack to have voice and self-determination in understanding and acting
on issues affecting them.
■ Though rst- and second-generation Asian immigrant populations will continue to grow,
areas with long-term AA settlement will concurrently experience growth in third- and
fourth-generation AA communities. Accounting for the multigenerational nature of AA
citizenship and incorporating diverse perspectives into CBPR efforts will be critical. Sim-
ilarly, the growth in multiracial communities will necessitate researchers and communities
alike to challenge their notions of identity in initiating CBPR efforts.
■ Finally, ongoing and future efforts should consider building alliances across communities
of color. Given the emphasis of CBPR on equity promotion, there is a unique opportunity
in the multiethnic context of the United States to recognize that justice denied for anyone is
justice denied for all—and to build research programs accordingly.
As the diversity and attendant complexity of the AA population grow in the coming
decades, CBPR principles will continue to provide an important means of ensuring research is
meaningful, context driven, and action oriented for this community.
QUESTIONS FOR DISCUSSION
1. What were the different CBPR-related opportunities and challenges that CSAAH faced as
it grew from a new initiative in 2003 to becoming an NIMHD National Research Center of
Excellence? How did it address these? What other changes might occur in Asian American
communities or among academic and other partners that have implications for using a
CBPR approach?
2. Why might you need to make adaptations to CBPR principles when working with Asian
American communities? Are there any adaptations that would not be acceptable for a CBPR
approach? Why or why not?
ACKNOWLEDGMENTS
We sincerely thank Julie Kranick for her assistance with this chapter. The efforts of Drs. Islam
and Trinh-Shevrin are supported by the National Institutes of Health National Institute on
Minority Health and Health Disparities (NIH NIMHD) grants P60MD000538; National Insti-
tutes of Health National Center for the Advancement of Translational Science (NCATS) Grant
UL1TR000038; and Centers for Disease Control and Prevention (CDC) Grants U48DP001904
and U58DP005621. The San Francisco Chinatown Restaurant Worker Health and Safety Study
was supported by the National Institute for Occupational Safety and Health/Centers for Dis-
ease Control and Prevention Grant (R219081) and the California Endowment, with additional
support from the Occupational Health Internship Program. We dedicate this chapter to the
numerous community partners we have had the privilege of working with over the past two
decades. Their commitment and dedication to improving the lives of Asian American commu-
nities is awe-inspiring.
186 Community-Based Participatory Research for Health
REFERENCES
Acevedo-Garcia, D., Sanchez-Vaznaugh, E. V., Viruell-Fuentes, E. A., & Almeida, J. (2012). Integrating social epidemiology
into immigrant health research: A cross-national framework. Social Science Medicine, 75(12), 2060–2068. doi:10.1016/j.
socscimed.2012.04.040
Aguilar, D. E., Abesamis-Mendoza, N., Ursua, R., Divino, L. A., Cadag, K., & Gavin, N. P. (2010). Lessons learned and chal-
lenges in building a Filipino health coalition. Health Promotion Practice, 11(3), 428–436. doi:10.1177/1524839908326381
Belone, L., Lucero, J. E., Duran, B., Tafoya, G., Baker, E. A., Chan, D.,...Wallerstein, N. (2016). Community-based partici-
patory research conceptual model: Community partner consultation and face validity. Qualitative Health Research, 26(1),
117–135. doi:10.1177/1049732314557084
Bloemraad, I. (2006). Becoming a citizen in the United States and Canada: Structured mobilization and immigrant political
incorporation. Social Forces, 85(2), 667–695.
Brown, M. P. (2008). Risk mapping as a tool for community-based participatory research and organizing. In M. Minkler &
N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes (pp. 453–457, 2nd
ed.). San Francisco, CA: Jossey-Bass.
Chang, C., Salvatore, A., Lee, P., Liu, S. S., & Minkler, M. (2012). Popular education, participatory research, and community
organizing. In M. Minkler (Ed.), Community organizing and community building for health. San Francisco, CA: Jossey-Bass.
Chang, C., Salvatore, A. L., Lee, P. T., Liu, S. S., Tom, A. T., Morales, A.,...Minkler, M. (2013). Adapting to context
in community-based participatory research: “Participatory starting points” in a Chinese immigrant worker community.
American Journal of Community Psychology, 51(3–4), 480–491. doi:10.1007/s10464-012-9565-z
Gaydos, M., Bhatia, R., Morales, A., Lee, P. T., Liu, S. S., Chang, C.,...Minkler, M. (2011). Promoting health and safety in
San Francisco’s Chinatown restaurants: Findings and lessons learned from a pilot observational checklist. Public Health
Reports, 126(Suppl 3), 62–69.
Hoeffel, E. M., Rastogi, S., Kim, M. O., & Shahid, H. (2012). The Asian population: 2010 census briefs. Retrieved from
http://census.gov/prod/cen2010/briefs/c2010-11.pdf
Hua, V. (2015). The dim sum revolution. San Francisco Magazine, 62(4).
Huang, K. Y., Calzada, E., Cheng, S., & Brotman, L. M. (2012). Physical and mental health disparities among young children
of Asian immigrants. Journal of Pediatrics, 160(2), 331–336. doi:10.1016/j.jpeds.2011.08.005
Islam, N. S., Khan, S., Kwon, S., Jang, D., Ro, M., & Trinh-Shevrin, C. (2010). Methodological issues in the collection, anal-
ysis, and reporting of granular data in Asian American populations: Historical challenges and potential solutions. Journal
of Health Care for the Poor and Underserved, 21(4), 1354–1381. doi:10.1353/hpu.2010.0939
Islam, N. S., Wyatt, L. C., Patel, S. D., Shapiro, E., Tandon, S. D., Mukherji, B. R.,...Trinh-Shevrin, C. (2013). Evaluation
of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2
diabetes in New York City. Diabetes Education, 39(4), 478–493. doi:10.1177/0145721713491438
Islam, N. S., Zanowiak, J. M., Wyatt, L. C., Chun, K., Lee, L., Kwon, S. C., & Trinh-Shevrin, C. (2013). A randomized-
controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community.
Journal of Community Health, 38(6), 1030–1041. doi:10.1007/s10900-013-9711-z
Islam, N. S., Zanowiak, J. M., Wyatt, L. C., Kavathe, R., Singh, H., Kwon, S. C., & Trinh-Shevrin, C. (2014). Diabetes
prevention in the New York City Sikh Asian Indian community: A pilot study. International Journal of Environmental
Research and Public Health, 11(5), 5462–5486. doi:10.3390/ijerph110505462
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (2013). Methods in community-based participatory research for health
(2nd ed.). San Francisco, CA: Jossey-Bass.
Jayaraman, S. (2013). Beyond the kitchen door. Ithica, NY: ILR Press.
Kristof, N. (2015). The Asian advantage. New York Times (October 10). www.nytimes.com/2015/10/11/opinion/sunday/the-
asian-advantage.html?_r=1
Minkler, M., Salvatore, A. L., Chang, C., Gaydos, M., Liu, S. S., Lee, P. T.,...Krause, N. (2014). Wage theft as a neglected
public health problem: An overview and case study from San Francisco’s Chinatown district. American Journal of Public
Health, 104(6), 1010–1020. doi:10.2105/AJPH.2013.301813
Murphy, P. A. (2011). Tiger moms: Is tough parenting really the answer? Time (January 20). http://content.time.com/time/
magazine/article/0,9171,2043477,00.html
CBPR in Asian American Communities 187
Ortman, J. M., & Guarneri, C. E. (2009). United States population projections: 2000 to 2050. Washington, DC: US
Census Bureau.
Parker, E. A., Chung, L. K., Israel, B. A., Reyes, A., & Wilkins, D. (2010). Community organizing network for environmental
health: Using a community health development approach to increase community capacity around reduction of environ-
mental triggers. Journal of Primary Prevention, 31(1–2), 41–58. doi:10.1007/s10935-010-0207-7
Patel, S., Kwon, S., Tepporn, E., Arista, P., Rideout, C., Linkin, F., . . . Trinh-Shevrin, C. (2014). Strategies to Reach
and Implement the Vision of Health Equity (STRIVE) project: Qualitative ndings about the process of implement-
ing evidence-based strategies in local AANHPI communities. In A.P.H. Association (Ed.), Strengthening communities
through participatory research (APHA 142nd Annual Meeting & Expo ed.). New Orleans, LA: Author.
Powell, B. (2011). An American dad on raising a tiger daughter. Time (January 20). http://content.time.com/time/magazine/
article/0,9171,2043420,00.html
Ritas, C., Minkler, M., Ni, A., & Halpin, H. A. (2008). Using CBPR to promote policy change: Exercises and online resources.
In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes
(2nd ed., pp. 459–463). San Francisco, CA: Jossey-Bass.
Spallek, J., Zeeb, H., & Razum, O. (2011). What do we have to know from migrants’ past exposures to understand their health
status? A life course approach. Emerging Themes in Epidemiology, 8(1), 6. doi:10.1186/1742-7622-8-6
Tandon, S. D., & Kwon, S. C. (2009). Community-based participatory research. In C. Trinh-Shevrin, N. S. Islam, & M. J.
Rey (Eds.), Asian American communities and health: Context, research, policy, and action (pp. 464–503). San Francisco,
CA: Jossey-Bass.
Trinh-Shevrin, C. (2014). Community health workers offer culturally tailored interactive workshops and counseling to Fili-
pino Americans, leading to improvements in medication adherence and cardiovascular risk factors. Retrieved from https://
innovations.ahrq.gov/proles/community-health-workers-offer-culturally-tailored-interactive-workshops-and-counseling
Trinh-Shevrin, C., Islam, N. S., Nadkarni, S., Park, R., & Kwon, S. C. (2015). Dening an integrative approach for health
promotion and disease prevention: A population health equity framework. Journal of Health Care for the Poor and Under-
served, 26(2 Suppl), 146–163. doi:10.1353/hpu.2015.0067
Trinh-Shevrin, C., Islam, N., Tandon, S. D., Abesamis, N., Ho-Asjoe, H., & Rey, M. J. (2007). Using community-based par-
ticipatory research as a guiding framework for health disparities research centers. Progress in Community Health Partner-
ships: Research, Education, and Action, 1(2), 195–205.
Trinh-Shevrin, C., Kwon, S. C., Park, R., Nadkarni, S. K., & Islam, N. S. (2015). Moving the dial to advance population
health equity in New York City Asian American populations. American Journal of Public Health, 105(Suppl 3), e16–e25.
doi:10.2105/AJPH.2015.302626
Ursua, R. A., Aguilar, D. E., Wyatt, L. C., Katigbak, C., Islam, N. S., Tandon, S. D., . . . Trinh-Shevrin, C. (2014).
A community health worker intervention to improve management of hypertension among Filipino Americans in New
York and New Jersey: A pilot study. Ethnicity and Disease, 24(1), 67–76.
Webster, T. (2001). Occupational hazards in eating and drinking places. Compensation and Working Conditions (Summer).
Retrieved from www.bls.gov/opub/mlr/cwc/occupational-hazards-in-eating-and-drinking-places.pdf
Yi, S. S., Kwon, S. C., Sacks, R., & Trinh-Shevrin, C. (2016). Commentary: Persistence and health-related consequences of
the model minority stereotype for Asian Americans. Ethnicity and Disease, 26(1), 133–138. doi:10.18865/ed.26.1.133

13
CHAPTER
ENGAGED FOR CHANGE
AN INNOVATIVE CBPR STRATEGY TO
INTERVENTION DEVELOPMENT
SCOTT D. RHODES, LILLI MANN, FLORENCE M. SIMÁN, JORGE ALONZO,
AARON T. VISSMAN, JENNIFER NALL, AND AMANDA E. TANNER
ALTHOUGH CBPR IS committed to equitable partnering practice and science to promote health
equity within complex sociocultural, political, and economic contexts, the challenge remains
for academics to engage with communities to develop, implement, and evaluate individual-,
community-, system-, and policy-level interventions designed to reduce health disparities and
increase health equity. Intervention development is difcult, and little guidance exists in terms
of strategies and processes, especially in involving community members as experts in their own
community and culture to co-develop interventions designed to promote health and prevent
disease. The science behind intervention development remains largely underdeveloped, and
there is a profound need for evidence-based strategies to guide the development of interventions
(Bartholomew, Parcel, Kok, & Gottlieb,2001; Hoddinott,2015; Wallerstein & Duran,2010;
Yardley, Morrison, Bradbury, & Muller,2015).
In this chapter, we outline the intervention research that our long-standing and well-established
partnership has been conducting and describe a multistep process that we have developed to pro-
vide guidance to intervention development through CBPR. The process provides a framework for
developing an intervention that is well informed by the lived experiences of community members,
the experiences of representatives from service- and practice-based organizations, and sound sci-
ence. The process ensures the culture-centeredness of interventions. Rather than an intervention
190 Community-Based Participatory Research for Health
that merely incorporates appropriate language, beliefs, and images, culture-centeredness locates
culture at the center of the intervention including identities, meanings, and experiences, which are
grounded in historical and social contexts (Dutta,2008), as described in Chapter2.
OUR CBPR PARTNERSHIP’S EXPERIENCE WITH INTERVENTION
DEVELOPMENT
Our CBPR partnership is located in western North Carolina. North Carolina has one of the fast-
est growing Latino populations in the country. Members of our partnership focus on the health
of ethnic-racial, sexual, and gender minorities and economically disadvantaged communities,
with HIV incidence rates in North Carolina 40 percent higher than the national rate. Since the
new millennium, our partnership has evolved to reect demographic trends and the evolving
impact of the HIV epidemic. Many of our CBPR studies focus on promoting sexual health and
preventing HIV among Latino communities and gay, bisexual, and other men who have sex
with men (MSM). Current partners include representatives from North Carolina public health
departments (local and state level); AIDS service organizations; community-based organiza-
tions, including Latino soccer leagues and teams, a local lesbian, gay, bisexual, and transgender
(LGBT) pride organization, and Latino-serving organizations; a local LGBT foundation; local
businesses, including media organizations, Internet applications (“apps”), bars, and clubs, a
video production company, and tiendas (Latino grocers); the Centers for Disease Control and
Prevention (CDC); and three universities. Our partnership consists of a variety of members
working on multiple projects. Members may be involved with and committed to different proj-
ects; however, our partnership is not study-specic. Members may join and leave, and be more
or less involved, but despite transitions, the partnership remains.
Our partnership has developed multiple interventions designed to address community-
identied health priorities:
■ HoMBReS (Hombres Manteniendo Bienestar y Relaciones Saludables; Men Maintaining
Well-being and Healthy Relationships), designed to promote sexual health and HIV pre-
vention through social networks of Latino men who are members of recreational soccer
leagues (Rhodes, Leichliter, Sun, & Bloom,2016)
■ CyBER/M4M (Cyber-based Education and Referral/Men for Men), designed to increase
knowledge of HIV among gay and bisexual and other MSM who use online chat rooms for
social and sexual networking (Rhodes et al.,2010)
■ C-CAPRELA (Cervical Cancer Prevention for Latinas), designed to reduce cancer-related
health disparities through social networks of Latina women living within the same housing
communities (Rhodes, Kelley, et al.,2012)
■ CyBER/testing, designed to increase HIV testing among gay, bisexual, and other MSM
and transgender persons who use social media for social and sexual networking (Rhodes,
McCoy, et al.,2016)
■ MuJEReS (Mujeres Juntas Estableciendo Relaciones Saludables; Women United Establish-
ing Healthy Relationships), designed to promote sexual health through social networks of
Latina women (Rhodes, Kelley, et al.,2012)
■ HoMBReS por un Cambio (Men for Change), designed to promote sexual health and
advocate for social justice through mobilizing and organizing social networks of Latino
men who are members of recreational soccer leagues (Rhodes, Leichliter, et al.,2016)
ENGAGED for CHANGE 191
■ HOLA, designed to reduce HIV-related health disparities among Latino gay, bisexual, and
other MSM and Latina transgender women (Rhodes, Daniel, et al.,2013)
■ HOLA en Grupos, designed to reduce HIV-related health disparities through social net-
works of Latino gay, bisexual, and other MSM and Latina transgender women (Rhodes,
Alonzo, Mann, Freeman, et al.,2015)
■ MAP’T (Mobile Apps to Promote Testing), designed to increase HIV testing through the
use of mobile applications (e.g., A4A/Radar, Grindr, Jack’d, and SCRUFF) commonly used
for social and sexual networking among gay, bisexual, and other MSM and transgender per-
sons (Sun et al.,2015)
■ weCare, designed to support the health and well-being of young racially ethnically diverse
gay, bisexual, and other MSM and transgender persons with HIV through social media
(Tanner et al.,2016)
■ ChiCAS (Chicas Creando Acceso a la Salud; Girls Creating Access to Health), designed to
promote the sexual and transition-related health of Latina transgender women
During the development, implementation, and evaluation of these interventions since the
new millennium, our CBPR partnership developed a process for intervention development that
evolved and became more sophisticated (Rhodes, Alonzo, Mann, Freeman, et al.,2015; Rhodes,
Daniel, et al.,2013; Rhodes, Duck, Alonzo, Daniel, et al.,2013; Rhodes, Duck, Alonzo, Downs,
et al.,2013; Rhodes et al.,2006,2007).
Although our initial processes followed typical steps of partnership trust building, devel-
oping, adapting, pilot-testing, and launching interventions, we also created a grid of resources
for intervention development (GRID). This GRID enabled us to outline existing interventions
and related programs and documented how activities met intervention objectives; explored
whether existing approaches or activities met local priorities; and began the process of thinking
creatively about the intervention strategies, activities, theories, and logic model development.
Since the earlier processes, however, we have worked to better deconstruct, clarify, and
codify our intervention development process throughout our ongoing intervention research. We
do not assume that what worked in the past will work in the future; we are reective and do not
work on “auto-pilot.” Furthermore, we wanted to support other partnerships that want to apply
a systematic and engaged approach to intervention development and maximize the potential
impact of their interventions.
STEPS IN INTERVENTION DEVELOPMENT THROUGH CBPR
We have developed a rened and enhanced thirteen-step process that is known as ENGAGED
for CHANGE, with each letter signifying one step within the intervention development process.
These steps are outlined in Table13.1.
Expand the Partnership
The rst step in the process involves expanding the partnership. Often CBPR partnerships lack
sufcient representation of key community or academic partners. Our partnership has learned
that we may not always have the expertise, connections, or other resources that are needed to
move an intervention project forward. Although our partnership already had some Latino mem-
bers, during our initial CBPR study focusing on Latino men’s health, we realized that to be
successful, we needed to expand participation by increasing representation of Latino men who

192 Community-Based Participatory Research for Health
TABLE 13.1 ENGAGED for CHANGE: A Stepped Approach to Intervention
Development
Step Objective
E Expand the partnership. To ensure that necessary key partners and perspectives
are not missing from the partnership
N iNtervention team established. To assign responsibility to a small team representing
the partnership and its diversity that will move the
intervention development process forward
G Gather existing literature and data. To build on what is already known in terms of
epidemiologic data; existing local, regional, national,
and global data; and so on
A Assess community needs, priorities,
and assets.
To ensure that community needs, priorities, and assets
are blended with existing data
G Generate and rene intervention
priorities.
To begin the process of focusing intervention goals
based on community needs and priorities
E Evaluate and incorporate
appropriate and meaningful theory.
To apply theory when appropriate; to ensure the
intervention is informed by theory
D Design an intervention conceptual
or logic model.
To describe the logic of the intervention (what is
expected to happen)
for
C Create objectives and craft activities
and materials.
To develop and rene intervention objectives and all
necessary activities and materials, ensuring activities
and materials are clearly linked to objectives
H Hone and pretest all activities and
materials.
To ensure activities and materials make sense for
those for whom they are designed
A Administer intervention pilot test. To ensure intervention components t together
coherently
N Note process of implementation
during the pilot test.
To document challenges, problems, weaknesses, and
successes identied through the pilot test
G Gather feedback from the pilot
and those who conducted and
participated in the pilot.
To include all perspectives in the intervention
editing step
E Edit the intervention based
on feedback.
To rene, enhance the intervention based on lessons
learned from the pilot
ENGAGED for CHANGE 193
were involved in local recreational soccer leagues. Of course, the expansion of representation
is not easy. It can take months to identify potential members, build trust, and increase under-
standing of the rationale for CBPR partnerships and the relevant processes, history, and goals.
Although networking and building trust to expand a partnership is a challenge (Becker,
Israel, & Allen,2005), within some communities, networking and building trust can be particu-
larly complicated. As we learned in our work with Latinos in North Carolina, some community
members were hesitant to participate in a process they initially did not understand or trust;
some were undocumented, others were not, but many shared a fear of engagement within a
state in which there were high levels of racism and anti-immigration sentiment (Rhodes, Mann,
et al.,2015; Rhodes et al.,2006). This is also true for working with sexual and gender minor-
ities. Partnering with gay, bisexual, and other MSM and transgender persons requires careful
consideration and effort given the intersectionality of identities and stigmas.
Intervention Team Established
The second step is establishing an intervention team, which is a smaller working group, tasked
with overseeing the entire intervention development process. The team works collaboratively
with the partnership, providing updates and brainstorming solutions to challenges faced. This
team must have broad and diverse representation from the partnership; its work cannot be done
in isolation and requires thorough involvement of members representing all partner types,
including community members, organization representatives, and academic researchers.
Gather Existing Literature and Data
This next step allows for the intervention team and partnership to build on what is known through
collection and interpretation of existing literature and data describing community needs, pri-
orities, and assets. These may include community assessments that are regularly conducted by
public health departments, hospitals, and local foundations; epidemiologic and disparities reports
from state and national agencies; data collected and synthesized by community-based orga-
nizations used in their own service delivery and grant proposals; and other sources, including
those from traditional academic research efforts (e.g., peer-reviewed publications). A partnership
approach to this step is important because different members will be aware of and have access to
different types of existing literature and data depending on their different roles (e.g., organization
representatives and academics), and gathering information from a broad range of sources helps
to have a more complete picture of the current community landscape and inequities.
Assess Community Needs, Priorities, and Assets
Because not all necessary literature and data may be readily available, the partnership also
must examine the needs, priorities, and assets of communities themselves. For example, in the
early 2000s, Latino communities in the southern United States, often referred to as “new Latino
settlement states,” were not well understood and remained relatively isolated (Gill,2010). Thus,
working with community members to understand community needs, priorities, and assets was a
key component of our early work.
We used multiple research methodologies. One approach was photovoice, an empowerment-
based qualitative method of inquiry that enables participants to record and reect on their
personal and community strengths and concerns through group discussions and photographs.

194 Community-Based Participatory Research for Health
Not only does it provide images of lived experiences but also the space for participants and
others who may be able to support action to collaboratively identify next steps (Hergenrather
et al., 2009). Our partnership has successfully used photovoice with Latino adolescents (Streng
et al., 2004), Latino men (Rhodes et al.,2009), persons living with HIV (Rhodes, Hergenrather,
Wilkin, & Jolly,2008), African American–Black men with HIV, and Latina transgender women
(Rhodes, Alonzo, Mann, Sun, et al.,2015).
In our photovoice project with Latina transgender women, nine transgender women docu-
mented their daily experiences through photography, engaged in discussions about their pho-
tographs, and organized a bilingual community forum to move knowledge to action. From
the participants’ photographs and words, eleven themes emerged in three domains: daily
challenges (e.g., health risks, uncertainty about the future, discrimination, and anxiety about
family reactions); needs and priorities (e.g., health and social services, emotional support, and
collective action); and community strengths and assets (e.g., supportive individuals and institu-
tions, wisdom acquired through lived experiences, and personal and professional goals).
As an example of the health risks Latina transgender women often take, a participant took
and shared with the group a photo (Figure13.1) of hormones that she had purchased at a tienda
(Mexican grocery store) and injected without the guidance of a medical professional. This res-
onated with other participants and triggered a discussion about health risks that many Latina
transgender women take (e.g., unsafe hormone use), the reasons that they take these risks (e.g.,
barriers to care), and the need to increase access to affordable and culturally congruent transition-
related health services.
FIGURE 13.1 Latina Transgender Women’s Photovoice Project Photograph and
Corresponding Quotation, “It Is Important to Go down the Right Path and to Not Just
Inject Yourself with Whatever.”
ENGAGED for CHANGE 195
At the community forum, sixty inuential advocates, including Latina transgender women,
community-based organization staff members, health and social service providers, and law
enforcement, reviewed ndings and developed ten recommended actions. These included edu-
cating staff members at the Mexican Consulate in Raleigh about the lives of Latina transgender
women in order to reduce discrimination they felt when seeking consulate services; increasing
health promotion programming in specic priority areas, that is, linking HIV, sexual health, and
transition-related services; and raising consciousness about negative experiences with police
about intimate partner violence. Overall, photovoice served to obtain rich qualitative insight of
Latina transgender women that was then shared with local leaders and agencies to help address
priorities (Rhodes, Alonzo, Mann, Sun, et al.,2015).
Gaps can also be lled by collecting data using innovative quantitative methods, such as
respondent-driven sampling, which uses chain referrals or initial respondents as “seed” to yield
representative samples and prevalence estimates for populations that may be considered “dif-
cult to reach” by researchers or other outsiders or for which no sampling frame exists (Rhodes,
McCoy, et al.,2012; Song et al.,2012).
Generate and Refine Intervention Priorities
Based on existing data and data uncovered by the previous step, the intervention team generates
priorities, presents them to the entire CBPR partnership, and iteratively renes intervention pri-
orities based on feedback. For example, our photovoice project in partnership with Latina trans-
gender women uncovered the need for more access to sexual health information and services,
a nding that aligns with the literature on high rates of HIV among transgender women, espe-
cially among racial-ethnic minorities. However, access to transition-related health care services,
including safe hormone use, emerged as a more salient and urgent priority for photovoice par-
ticipants, particularly given existing barriers because of high un-insurance and limited English,
much less culturally congruent and transgender-specic services. Thus, our partnership devel-
oped the ChiCAS intervention to focus jointly on sexual health and transition-related health
based on these qualitative data and on our enhanced understanding that transition-related needs
must be met rst. In addition, the community forum that was the culmination of the photovoice
project identied community organizations, which already offered low-cost hormone therapy,
where future intervention participants could be referred for transition-related health care.
Evaluate and Incorporate Appropriate and Meaningful Theory
Discussions of theory enable partners to understand processes of change, at whatever level,
from a systematic perspective and identify where and how theory ts into their lived experi-
ences. Understanding theory and integrating it with community member perspectives on the
lived experiences of community members is critical to making informed decisions about inter-
ventions. This blending of perspectives and integration of theory reects knowledge democracy
as described in Chapter2.
For example, through the exploration of theory and its uses, our partnership determined
that to support sexual health of Latino gay, bisexual, and other MSM and Latina transgender
women, two theories “t” our desired approach: social cognitive theory (Bandura,1986) and
empowerment education (Freire,1970,1973; Wallerstein,1994). We also decided that using
a lay health advisor model would enable us to reach a larger number of Latino gay, bisexual,
196 Community-Based Participatory Research for Health
and other MSM and Latina transgender women with an approach that was authentic to how
these communities convene. Thus, our HOLA intervention was designed to train members from
the community across North Carolina to promote sexual health through their naturally exist-
ing social networks (i.e., through their friends), and our approach to training and supporting
these lay health advisors drew on constructs from both theories. This approach also enables the
knowledge to live in the community (in this case through the lay health advisors) even after a
project is complete.
Design an Intervention Conceptual or Logic Model
Designing an intervention conceptual or logic model helps partnership members visually depict
the links among determinants of health (e.g., HIV risk and use of unsafe transition-related prac-
tices among Latina transgender women); the intervention strategies designed to address these
determinants; and expected immediate, intermediate, and long-term outcomes. The conceptual
or logic model enables partnership members to visually depict and see the logic in their thinking,
discuss their assumptions, and engage in a process of blending perspectives, insights, and expe-
riences with science while keeping an eye on outcomes. Table13.2 provides an abbreviated
logic model from our HOLA en Grupos HIV prevention intervention for gay, bisexual, and
other MSM and Latina transgender women.
During these discussions, community members may describe their real-world experiences
and perspectives on health and risk within contexts and evaluate what might and might not work
to reach expected outcomes. Service providers, including representatives from community-
based organizations, may provide insights based on their rich experience in service provision,
and academic researchers will synthesize the literature and provide expertise in health behavior
theory and health promotion. During development of the logic model, new variables may be
identied for measurement, including mediating and moderating variables and outcomes.
Create Objectives and Craft Activities and Materials
Intervention team members collaboratively draft objectives and craft activities and materials.
In this step, the team develops a general outline for the intervention including goals, objec-
tives, key messages, and theoretical underpinnings. Intervention activities are then outlined,
rened, and developed. Necessary culturally congruent materials (e.g., use of penis models for
practicing condom use) also are developed at this stage. This process is iterative with multiple
opportunities for intervention team and partnership members to provide feedback.
Hone and Pretest All Activities and Materials
We have learned that over time, partnership members, even those who represent the community,
become more alike others within the partnership (including organization representatives and
academic researchers) and may become out of touch with their peers in the community. Thus,
we have found it critical to pretest intervention activities and materials with community mem-
bers outside of the partnership who may be naive to the research and the partnership.
For example, we developed a condom tips card designed to support proper condom use
among Latino gay, bisexual, and other MSM. Our partnership debated how “real” to make the
illustrations, with the partnership deciding that the illustrations of the receptive partner should
be unclear so that the gender was vague. Our rationale was that we did not want to put at risk
anyone who might forget the tips card in his pants pocket or car, as examples, for someone else

ENGAGED for CHANGE 197
TABLE 13.2 An Abbreviated, Sample Logic Model from Our Partnership’s HOLA en Grupos Intervention
Problem statement: The US South carries disproportionate HIV burden compared to other parts of the United States. Spanish-speaking Latino
gay, bisexual, and other MSM and Latina transgender women in the South are at increased risk for HIV. Unfortunately no efcacious culturally
congruent behavioral interventions exist to reduce risk among these communities. HOLA en Grupos is designed to increase consistent condom
use and HIV and STD testing among Spanish-speaking Latino gay and bisexual men, MSM, and transgender persons ages eighteen years
and older.
Behavioral Determinants
Factors that affect risk and
protective behaviors
Activities
To address behavioral determinants
Outcomes
Expected changes as a result of
activities targeting behavioral
determinants
Immediate
Outcomes
Intermediate
Outcomes
1. Knowledge of HIV and STDs
(including magnitude and
impact on communities); the
types of infections; modes of
transmission; signs; symptoms;
and prevention strategies
2. Knowledge of available health
care services and eligibility
3. Perceived access to available
health care and related services
4. Condom use skills and
self-efficacy
5. Sexual communication skills
and self-efficacy
6. The sociocultural environment
(e.g., reactions to machismo,
fatalism, homophobia, and
discrimination)
Module 1: General information about the intervention and
an introduction to sexual health
Activities: 1. Icebreaker, introduction to the intervention,
and group introductions; 2. Ground rules; 3. Magnitude
of HIV and STDs; 4. “Find someone who” game; 5. HIV/
STD presentation and discussion, distribution of STD and
health department brochures; 6. HIV/STD vocabulary game
Activities correspond to determinants 1 and 2.
Module 2: Protecting Yourself and Your Partners
Activities: 1. Discussion of module 1; 2. Demonstrating
and practicing correct condom use; 3. Practical advice
about condoms; 4. Putting condom use steps in correct
order; 5. Condom use DVD and discussion; 6. Internal
condom use DVD and discussion; 7. Why some people
use and some do not use condoms activity in pairs; 8.
Condom negotiation role-plays; 9. Homework (learning
about different types of condoms)
Activities correspond to determinants 3, 4, and 5.
Increased knowledge
of HIV and STDs
Increased levels of
correct knowledge
about HIV and STDs:
the types of diseases,
modes of transmission,
signs, symptoms, and
prevention strategies
Increased condom
use skills, self-efcacy,
and intention
Increased sexual
communication and
safer sex negotiation
skills and self-efcacy
Increased
consistent
condom use
during anal
and vaginal sex
Increased
communication
with sexual
partners about
condom use
Increased
HIV and STD
testing and
receipt of
test results
(Continued )

198 Community-Based Participatory Research for Health
Module 3: Cultural Values That Affect Our Health
Activities: 1. Discussion of module 2; 2. Group discussion
of what it means to be Latino/a and gay or transgender;
3. How Latino cultural values inuence behavior; 4.
Confronting health-compromising attitudes and beliefs; 5.
Overcoming sociocultural obstacles to accessing medical
services discussion and accessing health department HIV
and STD testing services DVD.
Activities correspond to determinants 2, 3, 5, and 6.
Module 4: Review activities: 1. Group discussion of
previous module; 2. Review of HIV and STD transmission
and prevention; 3. Distinguishing between HIV and STD
myths and realities; 4. Living with HIV DVD and group
discussion; 5. Discussion about abstinence; 6. Conclusions
Activities correspond to determinants 1, 2, 3, 4, 5, and 6.
Decreased negative
and increased
positive attitudes
toward condoms
Reduced adherence
to traditional notions
of masculinity
and fatalism
Decreased
homo-negativity
Increased ethnic
group pride
Reduced perceived
barriers to HIV testing
TABLE 13.2 (CONTINUED)
Behavioral Determinants
Factors that affect risk and
protective behaviors
Activities
To address behavioral determinants
Outcomes
Expected changes as a result of
activities targeting behavioral
determinants
Immediate
Outcomes
Intermediate
Outcomes
ENGAGED for CHANGE 199
to nd. However, when pretesting the card, Latino gay, bisexual, and other MSM reported that
the clearer images spoke to them. They were less worried about safety and prioritized the card’s
meaningfulness.
Administer Intervention Pilot Test
Pilot testing is essential to analyzing activities and materials for attention, comprehension,
personal relevance, credibility, and acceptability by those for whom the activities and mate-
rials are developed (Bartholomew et al.,2001; National Cancer Institute,1989; Rhodes et al.,
2006,2007). Questions include (1) Do activities and materials motivate and sustain the partic-
ipants’ attention and interest? (2) Are activities and materials perceived as they were intended?
(3) Is there anything offensive in them? (d) Do the participants recognize and identify with the
activities and materials? (Rhodes, Kelley, et al.,2012; Rhodes et al.,2006,2007). Results of
this step are used in the last step (editing of intervention).
Note Process of Implementation during the Pilot Test
It is critical to learn as much as one can from the pilot test. For this reason, it is recommended that,
in addition to those partnership members who are involved directly in implementing the intervention
during the pilot test, other partnership members be present to observe the process of implementa-
tion. They may complete observer’s logs to capture details of implementation in a systematic way.
These details may identify where the intervention curriculum is vague, unclear, or confusing for
those who are delivering the intervention. Instructions may need to be rened, for example.
Gather Feedback from the Pilot and Those Who Conducted
and Participated in the Pilot
Discussions with those who implemented the pilot are vital to explore how they felt about
the process, what worked well, and what did not from their perspectives. We have conducted
qualitative interviews with pilot participants to better understand what worked and what did not
work well. With participants for whom the intervention worked well, we conducted interviews
that we referred to as “stories of success,” and with participants for whom the intervention did
not work well, we conducted interviews that we referred to as “stories of learning.” This process
ensured that we explored the strengths and weaknesses of the intervention during the pilot phase.
Edit the Intervention Based on Feedback
Based on the feedback and results from the pilot test, the intervention team edited and revised
intervention activities, strategies, and implementation processes. This may be an iterative pro-
cess with the intervention team revisiting previous steps of the ENGAGED for CHANGE
model. This editing process is crucial to ensure that the most-promising intervention—based on
science and the unique needs of the community—is used and evaluated.
CONCLUSION
There continues to be profound need to move from knowledge generation to the translation of
knowledge into interventions designed to promote community health. The strategy outlined in
this chapter can serve as a guide for other CBPR partnerships. Each step is complex, and our
200 Community-Based Participatory Research for Health
partnership’s work has not been without challenges. Members face the realities of health dis-
parities and inequities every day and know that something must be done for the communities
we each belong to. The slow pace of securing research funding and conducting sound research
is an ongoing frustration. Furthermore, communities themselves are not infallible; community
members and members of research partnerships may have strongly held prejudices about one
another that require ongoing attention and work highlighting the need to return to trust building
throughout the course of the partnership. Although there has been much literature on approaches
to address differences among partners, we have used team-building exercises, regular in-person
meetings to develop and nurture relationships, and celebrations of partnership successes as well
as life events (e.g., birthdays and births of babies).
Of course, the thirteen steps that we outline rely on a foundation of trust, transparency, clear
communication, and ongoing commitment by partnership members. Partnership principles were
not outlined in this chapter, but there are multiple places to nd examples of these principles
(including Chapter3 and Appendices 2 to 4), which are designed to support processes that facil-
itate equal participation in research among community members, organization representatives,
and academic researchers (Rhodes et al.,2011,2014; Seifer & Maurana,2000). Moreover, the
steps may overlap and be iterative.
It is also essential that once partnerships develop interventions, they rigorously evaluate
those interventions. Though there are strong arguments for why using a CBPR approach to
develop interventions may help increase intervention efcacy, outcome evaluation to measure
the effectiveness of interventions, as well as process evaluation, are essential for having an
impact on community and population health. Evaluation ndings can inform dissemination
and adaption of those interventions that are found to be effective and help ensure intervention
delity. Strong collaborations and diverse perspectives among partnership members are impor-
tant in evaluation also, including development of instruments; data collection, analysis, and
interpretation; and dissemination of ndings (Cashman et al.,2008; Schaal et al.,2016).
We are committed to this innovative CBPR approach to intervention development because
it maximizes the probability that our work as a partnership is based on what community mem-
bers identify as priorities; is more informed because of the sharing of broad perspectives,
insights, and experiences; builds capacity of all partners to solve community problems, harness
community assets, and conduct meaningful research; and promotes sustainability. We also think
that working together in partnership and building on the strengths of communities, organiza-
tion representatives, and academic researchers is ethical. Health disparities, such as HIV, for
example, require that we develop interventions that have the highest likelihood of success to
ensure the reduction and elimination of disparities over time. We must maximize our potential
for change.
QUESTIONS FOR DISCUSSION
1. What are the strengths of using ENGAGED for CHANGE as a strategy for intervention
development?
2. What challenges do you see with applying this strategy to developing interventions, and
how could these challenges be overcome?
ENGAGED for CHANGE 201
REFERENCES
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Bartholomew, L. K., Parcel, G. S., Kok, G., & Gottlieb, N. H. (2001). Intervention mapping: Designing theory- and evidence-
based health promotion programs. New York, NY: McGraw-Hill.
Becker, A. B., Israel, B. A., & Allen, A. J. (2005). Strategies and techniques for effective group process in CBPR partnerships.
In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods in community-based participatory research for health
(pp. 52–72). San Francisco, CA: Jossey-Bass.
Cashman, S. B., Adeky, S., Allen, A. J., Corburn, J., Israel, B. A., Montaño, J.,...Eng, E. (2008). The power and the promise:
Working with communities to analyze data, interpret ndings, and get to outcomes. American Journal of Public Health,
98(8), 1407–1417.
Dutta, M. J. (2008). Communicating health: A culture-centered approach. Malden, MA: Polity Press.
Freire, P. (1970). Pedagogy of the oppressed. New York, NY: Herder and Herder.
Freire, P. (1973). Education for critical consciousness. New York, NY: Seabury Press.
Gill, H. (2010). The Latino migration experience in North Carolina: New roots in the old north state. Chapel Hill, NC:
University of North Carolina.
Hergenrather, K. C., Rhodes, S. D., Cowan, C. A., Bardhoshi, G., & Pula, S. (2009). Photovoice as community-based
participatory research: A qualitative review. American Journal of Health Behavior, 33(6), 686–698. doi:10.5555/
ajhb.2009.33.6.686 [pii]
Hoddinott, P. (2015). A new era for intervention development studies. Pilot and Feasibility Studies, 1(36), doi:10.1186/
s40814-40015-40032-40810.
National Cancer Institute. (1989). Making health communications work: A planner’s guide. Bethesda, MD: US Department
of Health and Human Services.
Rhodes, S. D., Alonzo, J., Mann, L., Freeman, A., Sun, C. J., Garcia, M., & Painter, T. M. (2015). Enhancement of a locally
developed HIV prevention intervention for Hispanic/Latino MSM: A partnership of community-based organizations, a
university, and the Centers for Disease Control and Prevention. AIDS Education and Prevention, 27(4), 312–332.
Rhodes, S. D., Alonzo, J., Mann, L., Sun, C. J., Simán, F. M., Abraham, C., & Garcia, M. (2015). Using photovoice, Latina
transgender women identify priorities in a new immigrant-destination state. International Journal of Transgenderism,
16(2), 80–96.
Rhodes, S. D., Daniel, J., Alonzo, J., Duck, S., Garcia, M., Downs, M.,...Marsiglia, F. F. (2013). A systematic community-
based participatory approach to rening an evidence-based community-level intervention: The HOLA intervention for
Latino men who have sex with men. Health Promotion Practice, 14(4), 607–616.
Rhodes, S. D., Duck, S., Alonzo, J., Daniel, J., & Aronson, R. E. (2013). Using community-based participatory research to
prevent HIV disparities: Assumptions and opportunities identied by The Latino Partnership. Journal of Acquired Immu-
nodeciency Syndromes, 63(Supplement 1), S32–S35.
Rhodes, S. D., Duck, S., Alonzo, J., Downs, M., & Aronson, R. E. (2013). Intervention trials in community-based participa-
tory research. In D. Blumenthal, R. J. DiClemente, R. L. Braithwaite & S. Smith (Eds.), Community-based participatory
research: Issues, methods, and translation to practice (pp. 157–180). New York, NY: Springer
Rhodes, S. D., Hergenrather, K. C., Duncan, J., Ramsey, B., Yee, L. J., & Wilkin, A. M. (2007). Using community-based par-
ticipatory research to develop a chat room-based HIV prevention intervention for gay men. Progress in Community Health
Partnerships: Research, Education, and Action, 1(2), 175–184.
Rhodes, S. D., Hergenrather, K. C., Duncan, J., Vissman, A. T., Miller, C., Wilkin, A. M.,...Eng, E. (2010). A pilot inter-
vention utilizing Internet chat rooms to prevent HIV risk behaviors among men who have sex with men. Public Health
Reports, 125(Supplement 1), 29–37.
Rhodes, S. D., Hergenrather, K. C., Grifth, D., Yee, L. J., Zometa, C. S., Montaño, J., & Vissman, A. T. (2009). Sexual and
alcohol use behaviours of Latino men in the south-eastern USA. Culture, Health & Sexuality, 11(1), 17–34.
Rhodes, S. D., Hergenrather, K. C., Montano, J., Remnitz, I. M., Arceo, R., Bloom, F. R.,...Bowden, W. P. (2006). Using
community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men.
AIDS Education and Prevention, 18(5), 375–389.
Rhodes, S. D., Hergenrather, K. C., Vissman, A. T., Stowers, J., Davis, A. B., Hannah, A.,...Marsiglia, F. F. (2011). Boys
must be men, and men must have sex with women: A qualitative CBPR study to explore sexual risk among African
American, Latino, and white gay men and MSM. American Journal of Men’s Health, 5(2), 140–151.
202 Community-Based Participatory Research for Health
Rhodes, S. D., Hergenrather, K. C., Wilkin, A. M., & Jolly, C. (2008). Visions and voices: Indigent persons living with HIV in
the southern United States use photovoice to create knowledge, develop partnerships, and take action. Health Promotion
Practice, 9(2), 159–169.
Rhodes, S. D., Kelley, C., Simán, F., Cashman, R., Alonzo, J., Wellendorf, T.,...Reboussin, B. (2012). Using community-
based participatory research (CBPR) to develop a community-level HIV prevention intervention for Latinas: A local
response to a global challenge. Women’s Health Issues, 22(3), 293–301.
Rhodes, S. D., Leichliter, J. S., Sun, C. J., & Bloom, F. R. (2016). The HoMBReS and HoMBReS Por un Cambio interven-
tions to reduce HIV disparities among immigrant Hispanic/Latino men. MMWR, 65(1), 51–56.
Rhodes, S. D., Mann, L., Alonzo, J., Downs, M., Abraham, C., Miller, C.,...Reboussin, B. A. (2014). CBPR to prevent
HIV within ethnic, sexual, and gender minority communities: Successes with long-term sustainability. In S. D. Rhodes
(Ed.), Innovations in HIV prevention research and practice through community engagement (pp. 135–160). New York,
NY: Springer.
Rhodes, S. D., Mann, L., Simán, F. M., Song, E., Alonzo, J., Downs, M.,...Hall, M. A. (2015). The impact of local immigra-
tion enforcement policies on the health of immigrant Hispanics/Latinos in the United States. American Journal of Public
Health, 105(2), 329–337.
Rhodes, S. D., McCoy, T. P., Hergenrather, K. C., Vissman, A. T., Wolfson, M., Alonzo, J.,...Eng, E. (2012). Prevalence esti-
mates of health risk behaviors of immigrant Latino men who have sex with men. Journal of Rural Health, 28(1), 73–83.
Rhodes, S. D., McCoy, T. P., Tanner, A. E., Stowers, J., Bachmann, L. H., Nguyen, A. L., & Ross, M. W. (2016). Using social
media to increase HIV testing among gay and bisexual men, other MSM, and transgender persons: Outcomes from a
randomized community trial. Clinical Infectious Diseases, 62(11), 1450–1453. doi:10.1093/cid/ciw127
Schaal, J. C., Lightfoot, A. F., Black, K. Z., Stein, K., White, S. B., Cothern, C.,...Eng, E. (2016). Community-guided focus
group analysis to examine cancer disparities. Progress in Community Health Partnerships, 10(1), 159–167. doi:10.1353/
cpr.2016.0013
Seifer, S. D., & Maurana, C. A. (2000). Developing and sustaining community-campus partnerships: Putting principles into
practice. Partnership Perspectives, 1(2), 7–11.
Song, E. Y., Vissman, A. T., Alonzo, J., Bloom, F. R., Leichliter, J. S., & Rhodes, S. D. (2012). The use of prescription medica-
tions obtained from non-medical sources among immigrant Latinos in the rural southeastern US. Journal of Health Care
for the Poor and Underserved, 23(2), 678–693.
Streng, J. M., Rhodes, S. D., Ayala, G. X., Eng, E., Arceo, R., & Phipps, S. (2004). Realidad Latina: Latino adolescents, their
school, and a university use photovoice to examine and address the inuence of immigration. Journal of Interprofessional
Care, 18(4), 403–415.
Sun, C. J., Stowers, J., Miller, C., Bachmann, L. H., & Rhodes, S. D. (2015). Acceptability and feasibility of using established
geosocial and sexual networking mobile applications to promote HIV and STD testing among men who have sex with
men. AIDS and Behavior, 19(3), 543–552.
Tanner, A. E., Mann, L., Song, E., Alonzo, J., K., S., Arellano, E.,...Rhodes, S. D. (2016). weCare: A social media-based
intervention designed to increase HIV care linkage, retention, and health outcomes for racially and ethnically diverse
young MSM. AIDS Education and Prevention, 28(3), 216–230.
Wallerstein, N. (1994). Empowerment education applied to youth. In A. C. Matiella (Ed.), The multicultural challenge in
health education (pp. 153–176). Santa Cruz, CA: ETR Associates.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(Suppl 1), S40–S46.
Yardley, L., Morrison, L., Bradbury, K., & Muller, I. (2015). The person-based approach to intervention development:
Application to digital health-related behavior change interventions. Journal Medical Internet Research, 17(1), e30.
doi:10.2196/jmir.4055

5
PART
PROMISING PRACTICES:
ETHICAL ISSUES
Ethics of health research traditionally focuses on the protection of human participants as car-
ried out by institutional review boards (IRBs) (e.g., university IRBs or Indian Health Service
IRBs). These protections primarily emphasize the Belmont principles of respect for persons
(voluntary participation), beneficence (maximizing benefits), and justice (balancing risks and
benefits) (see Chapter15). Such focus can be categorized as research regulation. These legal
protections are certainly an important part of any research project, and yet the ethical focus in
CBPR expands beyond the rights of individual research participants.
A number of scholars in the past decade have sought to expand the discussion of CBPR
ethics beyond simply IRB regulations (Banks & Brydon-Miller, 2018; see also Chapters14 to16).
For example, the stewardship of CBPR through governance can be an ethical stance (see Chapter
16). Stewardship includes the protection of community (and individual) interests, enhances the
204 Part 5
development of equitable partnerships and effective collaboration, provides legitimacy for the
research by ensuring appropriate approvals are obtained, builds capacity in the community, and
ensures the community and cultural perspective is provided throughout the research process to
increase the quality of the research and the effectiveness of interventions.
Stewardship can be provided by a number of sources. In Native communities, the use of
tribal research review boards and IRBs introduce requirements for community protections and
benefits along with cultural fit and focus of the research. They also require collaboration in all
phases of the research including the dissemination of research. In Native and non-Native com-
munities, advisory boards are often used to steward research. Further, partnership agreements
and evaluation frameworks also help to steward the research.
The three chapters in this section further contribute to this expansion of ethical issues
beyond simple research regulation. In Chapter14, Myra Parker describes how the application
of CBPR principles enhances research and cultural ethics in American Indian and Alaska Native
(AI/AN) communities. She argues that cultural issues are critical for AI/AN communities and that
CBPR principles and practices enable researchers and community members to integrate culture
into the research and intervention process. This integration enables partnerships to improve
the quality and impact of the research and intervention and hence meet an ethical obligation
of community benefit. Further, she suggests that CBPR principles and practices throughout the
research and dissemination process ensure ethical research protocols are used and help to avoid
research violations and unintended consequences such as stigma for the community.
In Chapter15, Rachel Morello-Frosch, Phil Brown, and Julia Green Brody discuss how CBPR
(re)shapes the ethical oversight of human subjects protection in research. They argue that strict
and traditional IRB review of CBPR can result in unintended violations of the very ethical princi-
ples review committees are charged to uphold. They argue this is in part because of the seeking
of IRBs to protect research participants as individuals, whereas CBPR seeks to protect individuals
and communities. This ethical tension has profound implications for the viability and logistics of
CBPR projects. The authors suggest ways to manage these tensions to ensure that CBPR projects
are supported, which is especially important given the increased uptake of community-engaged
methods in biomedical and social science research.
In Chapter16, Sarah Flicker, Adrian Guta, and Robb Travers broaden the focus of ethics
beyond IRBs to examine “everyday ethics” of CBPR. Specifically, they note that many of the
Part 5
205
ethical issues faced by CBPR practitioners fall outside the traditional purview of IRBs. It is in
the everyday choices about how to engage communities (with myriad “right” and “wrong”
answers) that morals, ethics, values, and principles may conflict. The authors identify and discuss
four key points in the life cycle of a typical CBPR project: (1) laying the groundwork; (2) get-
ting “permission,” governance as stewardship, and honoring community protocols; (3) project
implementation and working with peer researchers; and (4) sharing work and ending the cycle.
They illuminate each challenge and offer a brief case study for consideration and reflection to
explore the idea of researchers “as active moral agents.”
REFERENCE
Banks, S. and Brydon-Miller, M. (Eds.). (2018). Ethics in participatory research for health and social well-being, London,
Routledge.

14
CHAPTER
AMERICAN INDIAN/ALASKA NATIVE (AI/AN) communities and individuals have expe-
rienced harm from research, medical practitioners, and health systems, leading to distrust
of research and medicine. Over three thousand AI/AN women were sterilized without their
knowledge or consent during the 1960s and through the 1970s, some as young as sixteen years
old (Lawrence,2000). Indian Health Service physicians recommended sterilizations based on
discriminatory views of AI/AN people. In research, Arizona State University researcher Therese
Ann Markow obtained DNA samples from Havasupai tribal members to use in a diabetes study
in the early 1990s (Garrison,2013). She gave samples to researchers at ASU and other labs
across the country. Study participants and the tribe assert they were not informed these samples
would be given to other researchers or that they would be used to study mental health problems,
consanguinity, and tribal migrations. They further stated in court documents that these practices
resulted in individual and community harm from stigma, as well as from a lack of informed
consent, and went against important cultural beliefs.
These cases raise issues about the ethics of research processes, particularly the informed
consent process required of research participants. Beyond research ethics specied in the
Common Rule, it is also important to consider the cultural elements of research that may not t
neatly into an ethics discussions. The Common Rule refers to the federal regulations govern-
ing human subjects research. These cultural elements shape the nature of health problems and
CBPR PRINCIPLES AND
RESEARCH ETHICS IN
INDIAN COUNTRY
MYRA PARKER
208 Community-Based Participatory Research for Health
interventions and the rights of people to dene those problems and interventions. Research
ethics discussions limited to the Common Rule focus exclusively on individual informed con-
sent and other Belmont principles rather than considering culture and community benets, two
critical aspects of research with AI/AN communities and individuals.
Community-based participatory research (CBPR) principles (see Chapter 3) reinforce
Indigenous research ethics and help to bring Western and Indigenous research ethics into an
integrated perspective (Pearson, Parker, Fisher, & Moreno,2014). CBPR ensures inclusion of
AI/AN cultures and social and environmental considerations unique to Indian Country through
every stage of the research process. Adhering to CBPR principles helps researchers and AI/AN
communities to accurately assess potential harms and benets from research methods, partic-
ipation, and dissemination; improves research knowledge for AI/AN in general; and can help
improve external validity of research ndings. For example, using CBPR principles can ensure
inclusion of subgroups within the community, such as elders, who may not be part of a non-
CBPR approach. Inclusion of these subgroups helps research teams gather comprehensive per-
spectives of public health needs and possible contributing factors, enhancing generalizability
across the entire AI/AN population of interest (Wallerstein & Duran,2010). Thus, CBPR can
provide an important approach for addressing cultural issues throughout the research process in
a meaningful and appropriate way.
INCORPORATING CULTURAL ELEMENTS THROUGH CBPR PRINCIPLES
One of the most important contributions of CBPR is to ensure the inclusion of culture and
cultural diversity in the research process. Specically, a culture-centered approach encourages a
recognition of the importance of culture, the voice or agency of community members in dening
problems and solutions, and societal transformations related to culture and agency (Dutta,2007;
Wallerstein et al., under review). Not only does a culture-centeredness approach and under-
standing of the culture(s) of participating communities support improved research ethics, but
also it improves the overall t and quality of the research. Kagawa-Singer, Dressler, George,
and Elwood (2016) recognize culture as follows: (1) is a schema created by humans, (2) helps to
support community members’ survival and well-being, and (3) helps group members interpret
the world through social norms of beliefs, attitudes, spiritual and emotional explanations, and
practices. These authors further argue that our cultural frameworks operate through multiple
dimensions. Not only do they integrate biological, psychological, and sociological aspects of
our communities but also they rely on our relationships with the world around us, including
the natural world. Cultures are complex and necessarily incorporate aspects of surrounding
geography, historical realities, social norms and trends, and the political realm (Kagawa-Singer
etal.,2016).
Research translation, application, and dissemination benet from culture-centeredness in
the research process. Ignoring culture when conducting research in diverse communities can
result in a poor t for health interventions and lower uptake of intervention content (Vaeth,
Wang-Schweig, & Caetano,2017), let alone ethical violations of informed consent and related
issues such as in the Havasupai Diabetes Study. The principal investigator in the Havasu-
pai Diabetes Study failed to obtain informed consent from individual tribal participants for
research on their DNA samples for health conditions and tribal characteristics outside the
CBPR Principles and Research Ethics in Indian Country 209
scope of diabetes research originally specied. In fact, paying attention to key cultural ele-
ments can have positive health impacts. This section explores several components of Kagawa-
Singer et al.’s (2016) denition of culture to illustrate how cultural elements can work with
CBPR principles to shape health outcomes.
Kagawa-Singer et al. (2016) describe how culture is related to several key domains that in
turn affect health behaviors including (but not limited to) spiritual and emotional explanations
of health and well-being and health knowledge and practices. Spiritual and emotional expla-
nations of health and well-being can inuence health behaviors. For example, use of tradi-
tional healers is a spiritual and emotional approach to addressing health issues and varies across
tribes. In a study of two large tribes, Southwest tribal members experiencing lifetime substance
abuse disorder and lifetime comorbid depression or anxiety and substance disorders turned to
traditional healers more frequently than members of a Northern Plains tribe (Beals etal.,2005).
Using CBPR to understand these differences by involving community members early in the pro-
cess and building from community strengths could help improve access to traditional healers,
improve partnerships between traditional healers and mental health and medical professionals,
and perhaps destigmatize mental health services and substance disorder treatment. AI/AN
spiritual leaders involved through an advisory board or other meaningful roles may provide
the cultural context relevant to AI/AN help-seeking behaviors, specically for mental health or
substance use issues. Such an approach helps to avoid an erroneous assumption that different
tribal groups use traditional healers at the same rate, thus ensuring the CBPR principle of “t
to the local cultural context.” Involving spiritual leaders and other stakeholders from both tribal
communities could support hypothesis development of the circumstances under which tribal
members would be likely to seek care.
A second key cultural element is health understanding and knowledge as it relates to health
practices. For example, a recent study examined AI/AN parents, youth, and health providers’
understanding of human papillomavirus (HPV) screening. Teens, the most at-risk group in the
study, were less likely to endorse the statement that HPV can cause cervical cancer. By con-
trast, young adults were most likely to indicate HPV can cause cervical cancer, even compared
to Indian Health Service (IHS) providers. No teens indicated that they believed HPV to be a
rare infection, whereas about 40 percent of parents, young adults, and IHS providers indicated
they believed it to be rare (Schmidt-Grimminger et al.,2013). Given the disparity of health
knowledge across high-risk groups, parents, and providers, community partnerships supported
through CBPR processes could represent an important step to improve HPV knowledge in this
community. In non-Native communities, addressing these knowledge differences might include
having open dialogue to enhance comprehension. However, in some AI/AN communities, dis-
cussing sexual practices may be considered taboo. Relying on a non-Native approach might
dissuade participants from learning important information. Facilitating collaborative processes
in all phases of the research, one of the CBPR principles, could support understanding of key
cultural beliefs and norms, resulting in improved interventions and education and avoiding any
unintended consequences to enhance the knowledge of HPV.
A nal illustration of Kagawa-Singer et al.’s (2016) notion of culture includes structural
and ecological elements. CBPR supports research partnerships in the process of integrating
broader social, economic, and other environmental factors that affect population health into
research plans. For example, an AI/AN family of ve living ten miles outside of downtown
210 Community-Based Participatory Research for Health
Seattle and without a car may need to travel two hours by bus, one way, for their children to
see the doctor at the only medical facility that offers IHS-subsidized care in Seattle. Thus, the
structural limitations of the Seattle urban transportation system disproportionately affect fam-
ilies living in poverty, resulting in barriers to health care for these families. By combining this
perspective with cultural humility, researchers can gain a more comprehensive understanding
of the challenges communities face, resulting in improvements in research planning, imple-
mentation, and community t. Cultural humility (see Appendix 4) includes committing to an
ongoing relationship with communities, acknowledging the uidity and subjectivity of culture,
and thereby challenging individuals and institutions to address inequalities (Fisher-Borne, Cain,
& Martin,2015). Cultural humility represents an important competency to achieve adherence to
the spirit of CBPR and also ensures a strong t with community ethics perspectives.
ENSURING ETHICS THROUGH THE APPLICATION OF CBPR PRINCIPLES
Although the previous section illustrates how application of CBPR principles can address
ethical issues related to cultural elements, this section highlights how CBPR principles and
practices can ensure broader ethical adherence throughout stages in the research. The CBPR
principle of using a cyclical and iterative process presents opportunities to revisit study t and
the ethics of study decisions throughout the research process. From the conceptualization stage
through dissemination, communities have important insight in the research that affects their
communities (James et al.,2014).
Recognizing the community as a unit of identity constitutes an important rst step. For
AI/AN communities, some may be dened by reservation boundaries, and others, such as urban
Indian communities, may be dened by community members. Dening community informs
how IRBs or other research-approval entities may review human subject involvement on behalf
of the community partner. Such a recognition helps to avoid unintended ethical violations and
also ensures the cultural perspective of community boards are included in the research ethics
processes.
Discussing research ideas constitutes a critical next step in working with AI/AN commu-
nities. All too often researchers have made decisions about research questions or selected their
own priorities for health research in AI/AN communities (Walters & Simoni,2009). Incorpo-
rating community input in the problem-denition phase could include feedback on the initial lit-
erature reviews to describe the public health issues, identifying appropriate scientic resources,
and recognizing that “gray literature,” non-peer-reviewed materials such as government reports,
tribal reports, and Indigenous or other community resources, may provide critical information.
Scientic methodology and research design may also benet from reliance on the CBPR
framework. Communities have preferences in choosing the research design, identifying the
sample, providing input on recruitment strategies, and identifying or giving feedback on the
measures used for health outcomes and cofactors (Corbyn,2011). Discussing human subjects’
protections with community stakeholders ts in with CBPR practices (Harding et al.,2012;
Quigley, 2015). Establishing informed consent requirements, ensuring cultural norms and
expectations are met, and understanding the unique vulnerabilities without stigmatizing com-
munities all contribute to a clear, mutual understanding of how research ethics will be upheld.
CBPR approaches can support development of the plan for analysis to ensure community input.
CBPR Principles and Research Ethics in Indian Country 211
Many diverse communities, including AI/AN communities, are ambivalent about randomized
controlled trials (RCT) (Massey & Kirk, 2015). Although communities understand that the
RCT is the “gold standard” for ensuring unbiased results, they also recognize that the require-
ments for an RCT may be challenging for community members. Discussing the methodology
and analysis offers all partners opportunities to discuss potential risks and benets, build
trust, and to clarify everyone’s expectations of the research process, and concerns about
individual- and community-level risks.
Including community input in the study dissemination plan supports trust building
(Lucero,2013; Chapter5), which is an important CBPR principle. Many AI/AN communities
require community review and approval of publications and presentations prior to dissemination
(Brugge & Missaghian,2006; Foster et al.,1999; Navajo Nation IRB,2003; Tribal IRBs,2008).
In addition to supporting human subjects and community protections, community contribu-
tions can assist and support meaningful dissemination (Chen, Diaz, Lucas, & Rosenthal,2010).
Academic publications may be useful for researchers or physicians, but most communities
require research results in a different format for decision making, program development, and
community capacity building. This may necessitate translation of research results into mate-
rials, building on community strengths, with content easily used by community stakeholders.
These efforts guard against stigmatization and other community-level harms as well as ensure
an equitable role in decision making for AI/AN communities.
Culture-centeredness, as a CBPR principle, represents CBPR praxis and, in research proj-
ects involving AI/AN communities, a key CBPR outcome. As CBPR praxis (or the cycle
of reection, action, reection practice), it means developing, relying on, and incorporating
a meaningful process in the research to ensure community decision making and cultural
knowledge in formulating interventions and research designs. As a key CBPR outcome, culture-
centeredness, brought about by the amalgamation of culture, community agency, and voice,
can lead to community benets such as cultural revitalization and community transformations.
Community voice and decision making about the use of data in general, and not just about
specic cultural practices, embody an important CBPR principle that recognizes the impor-
tance of cultural and community worldviews for decision making. One example is establishing
a clear, multidirectional process for summarizing study results aimed to inform tribal partners.
This process ensures knowledge democracy across partners and supports community action for
improved health outcomes.
Incorporating community voice in decision making operationalizes another CBPR prin-
ciple of supporting community empowerment. Community voice can facilitate agreement
across the research partnership as to the best steps and deliverables for community use. Tribal
decision making may vary by stakeholder, given the results of a research study. As an example,
for a study involving elementary school children, tribal program managers may have a different
need and focus for the data as compared to tribal leaders. Data at the level of the school district
may reect a high degree of school absenteeism, which may support a conclusion that improved
school engagement is needed to incentivize school attendance and make the content more rele-
vant for students. Thus, a tribal program manager would work to integrate tribal culture(s) into
the educational materials.
By contrast, tribal leaders may examine the overall population-level data and identify the
public health need—for example, to reduce the risk of underage alcohol use. Tribal leadership
212 Community-Based Participatory Research for Health
may then be able to authorize additional funding to after-school programs to ensure children
have a safe alternative to settings in which alcohol use may be promoted. In this example, the
research ndings may focus on alcohol use and school absenteeism as major outcomes, which
are then translated by tribal stakeholders into action to support improvements in overall health
and well-being for elementary school students. This process supports the Indigenous research
ethics principle of “doing good” across the community to ensure community benet, which
contrasts with the principle of benecence in the Belmont Report, which espouses the notion of
“do no harm” to individuals participating in research (see Figure14.1).
CONCLUSION
Culture matters in public health research with AI/AN communities as well as in research imple-
mentation, translation, and dissemination. CBPR principles, in combination with human subject
protection principles, help to include culture in public health research for improved relevance and
benet to AI/AN communities involved in the research. CBPR also reinforces adherence to ethics
principles, supporting diverse communities by offering a meaningful opportunity to discuss and
make decisions about what research makes sense for them and the community as a whole.
QUESTIONS FOR DISCUSSION
1. In the following scenario, how do CBPR principles inform research decisions?
2. How do ethics principles and CBPR principles relate to the community context described
in the scenario?
3. How does culture play a role in understanding CBPR and ethics applications?
4. How could an understanding of structural inequities and context inform research decisions?
Tribal Program Managers Tribal Leaders
Actions
Culture included
in program
Elders volunteer
Interpretation
High risk Low resources
Results
By district By school
Actions
Authorize funding
Explore new
partnerships
Interpretation
Public health
need
Available
resources
Results
Overall tribeCost per child
FIGURE 14.1 Integrate Knowledge and Action for the Mutual Benefit of All Partners

CBPR Principles and Research Ethics in Indian Country 213
REFERENCES
Beals, J., Manson, S. M., Whitesell, N. R., Spicer, P., Novins, D. K., & Mitchell, C. M. (2005). Prevalence of DSM-IV disorders
and attendant help-seeking in two American Indian reservation populations. Archives of General Psychiatry, 62, 99–108.
Brugge, D., & Missaghian, M. (2006). Protecting the Navajo people through tribal regulation of research. Science and
Engineering Ethics, 12, 491–507.
Chen, P. G., Diaz, N., Lucas, G., & Rosenthal, M. S. (2010). Dissemination of results in community-based participatory
research. American Journal of Preventive Medicine, 39, 372–378.
Corbyn, Z. (2011). Science education: Research on the reservation. Nature, 471, 25–26.
Dutta, M. J. (2007). Communicating about culture and health: Theorizing culture-centered and cultural sensitivity approaches.
Communication Theory, 17, 304–328.
Fisher-Borne, M., Cain, J. M., & Martin, S. L. (2015). From mastery to accountability: Cultural humility as an alternative to
cultural competence. Social Work Education, 34, 165–181.
Foster, M. W., Sharp, R. R., Freeman, W. L., Chino, M., Bernsten, D., & Carter, T. H. (1999). The role of community review
in evaluating the risks of human genetic variation research. The American Journal of Human Genetics, 64, 1719–1727.
Garrison, N. A. (2013). Genomic justice for Native Americans. Science, Technology, & Human Values, 38, 201–223.
Harding, A., Harper, B., Stone, D., O’Neill, C., Berger, P., Harris, S., & Donatuto, J. (2012). Conducting research with tribal
communities: Sovereignty, ethics, and data-sharing issues. Environmental Health Perspectives, 120, 6–10.
James, R., Tsosie, R., Sahota, P., Parker, M., Dillard, D., Sylvester, I.,...Kiana, G. (2014). Exploring pathways to trust:
A tribal perspective on data sharing. Genetics in Medicine, 16, 820–826.
Kagawa-Singer, M., Dressler, W. W., George, S. M., & Elwood, W. N. (2016). The cultural framework for health: An integra-
tive approach for research and program design and evaluation. National Institutes of Health. Retrieved from https://obssr.
od.nih.gov/about-us/publications/
- Study proposes to use infant data.
- The study examines parent-child relationship and obesity.
- Infant room teacher is married to tribal chair.
- Tribal chair opposes health research.
- Tribe is unhappy with federal government–run IHS.
- The tribal election will occur within weeks.
- The assistant position is a political appointment.
- The reservation unemployment rate is 60%.
- Uncle’s position is up for reelection.
- There is a poor relationship with the health committee chair.
Mother
works at
IHS clinic.
Daughter
attends
tribal
school.
Clan
uncle sits
on tribal
council.
Aunt is
Administrative
assistant
for tribe.
Research Scenario: Applying CBPR in a Tribal Setting
214 Community-Based Participatory Research for Health
Lawrence, J. (2000). The Indian Health Service and the sterilization of Native American women. American Indian Quarterly,
24, 400–419.
Lucero, J. (2013). Trust as an ethical construct in community-based participatory research partnerships. Unpublished doc-
toral dissertation. University of New Mexico.
Massey, A., & Kirk, R. (2015). Bridging Indigenous and western sciences: Research methodologies for traditional, comple-
mentary, and alternative medicine systems. SAGE Open, 5.
Navajo Nation IRB. (2003). Navajo Nation IRB: A unique human research review board has three primary concerns: Protect-
ing its community, its people, and its heritage. Protecting Human Subjects, pp. 1–2.
Pearson, C. R., Parker, M., Fisher, C. B., & Moreno, C. (2014). Capacity building from the inside out: Development and
evaluation of a CITI ethics certication training module for American Indian and Alaska Native community researchers.
Journal of Empirical Research on Human Research Ethics, 9, 46–57.
Quigley, D. (2015). Promoting human subjects training for place-based communities and cultural groups in environmental
research: Curriculum approaches for graduate student/faculty training. Science and Engineering Ethics, 21, 209–226.
Schmidt-Grimminger, D., Frerichs, L., Black Bird, A. E., Workman, K., Dobberpuhl, M., & Watanabe-Galloway, S. (2013).
HPV knowledge, attitudes, and beliefs among Northern Plains American Indian adolescents, parents, young adults, and
health professionals. Journal of Cancer Education, 28, 357–366.
Tribal IRBs. (2008). Tribal IRBs shape research in Native populations. IRB Advisor. Retrieved from www.ahcmedia.com/
articles/15543-tribal-irbs-shape-research-in-native-populations?trendmd-shared=0
Vaeth, P. A., Wang-Schweig, M., & Caetano, R. (2017). Drinking, alcohol use disorder, and treatment access and utilization
among U.S. racial/ethnic groups. Alcoholism: Clinical and Experimental Research, 41, 6–19.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(Suppl 1), S40–S46.
Wallerstein, N., Oetzel, J. G., Duran, B., Magarati, M., Pearson, C., Belone, L., et al. (under review). Conceptualizing and
measuring the culture-centered approach in community based participatory research. Social Science & Medicine.
Walters, K. L., & Simoni, J. M. (2009). Decolonizing strategies for mentoring American Indians and Alaska Natives in HIV
and mental health research. American Journal of Public Health, 99(Suppl 1), S71–S76.
15
CHAPTER
THE BENEFITS OF CBPR for community partners have been well documented and include
enhanced co-learning between community members and scientists, informing organizing
efforts, and linking research to policy action. Less, however, has been written on how CBPR
(re)shapes the scientic enterprise itself by improving its rigor, relevance, and reach (Balazs&
Morello-Frosch, 2013). Rigor refers to the practice and promotion of good science—in the
study design, data collection, and interpretation phases of research. Relevance refers to
whether science is asking the right questions and how it elucidates opportunities for individual
action or collective change. Reach encapsulates the degree to which knowledge is dissemi-
nated to diverse audiences and translated into useful tools for the scientic, regulatory, policy,
and lay arenas. Moreover, by advancing the three Rs, CBPR not only facilitates translational
DEMOCRATIZING ETHICAL
OVERSIGHT OF RESEARCH
THROUGH CBPR
RACHEL MORELLO-FROSCH, PHIL BROWN, AND JULIA GREEN BRODY
Sections of the chapter have been adapted from the following articles with permission: Morello-Frosch, R., Varshavsky, J.,
Liboiron, M., Brown, P., & Brody, J. G. (2015). Communicating results in post-Belmont era biomonitoring studies: Lessons from
genetics and neuroimaging research. Environmental Research, 136, 363–372. https://doi.org/10.1016/j.envres.2014.10.001;
and Brown, P., Morello-Frosch, R., Brody, J. G., Altman, R. G., Rudel, R. A., Senier, L.,...Simpson, R. (2010). Institu-
tional review board challenges related to community-based participatory research on human exposure to environmental toxins:
Acase study. Environmental Health: A Global Access Science Source, 9, 39. https://doi.org/10.1186/1476-069X-9-39.

216 Community-Based Participatory Research for Health
research (i.e., application of research ndings to community stakeholders and policy makers) but
also, more important, transformational research, which changes the nature of and approach to
scientic inquiry itself. Figure15.1 displays a continuum from translational to transformational
research. On the left side, traditional scientic methods collect community data or conduct
research translation but treat community members as passive study participants. Toward the
right, community engagement increases, as members move from being mere study participants
to being active research partners.
This transformative potential of CBPR also extends to the realm of research ethics and
oversight of human subject protections. In general, institutional review board (IRB) review of
human subjects research encourages investigators to systematically assess the ethical implica-
tions of their proposed projects. This process involves feedback and revisions of study protocols
to ensure that ethical concerns are thoroughly vetted. In addition to encouraging researchers to
reect on the ethics of their work, IRB members themselves often learn about novel methodo-
logical approaches to research, such as CBPR, and their unique ethical nuances.
Increasing uptake of community-engaged methods in biomedical and social science
research makes it particularly important that scientists, funders, community members, and uni-
versity administrators work toward dening human subjects’ protection procedures that support
CBPR projects instead of inadvertently hindering them.
OVERSIGHT OF PROTECTION OF STUDY PARTICIPANTS IN RESEARCH
In 1979, the Belmont Report established principles for the use of human subjects in scientic
research. Developed partly in response to the notorious Tuskegee syphilis study on poor African
American men, Belmont identied three basic principles governing the ethical use of human
Context influences
study design,
research questions,
and ethics oversight
Participatory
Science
Traditional
Science
No influence on
research design
or ethics
oversight
Participation in
dissemination of results
and some input on
protocol ethics
Opinions actively
solicited through pre-
and post-data collection
Level of Community Engagement
Leverage research and
partnerships to
promote policy change
and transform research
ethics frameworks
From Translational Research …… to Transformational Research
Partners in research
protocol design,
ethics oversight, data
collection, results
interpretation
FIGURE 15.1 The Three Rs of CBPR: Rigor, Relevance, and Reach
Source: Adapted from Balazs and Morello-Frosch (2013).
Democratizing Ethical Oversight of Research through CBPR 217
research subjects: (1) “respect for persons,” or voluntary participation and special protection
for those who lack the capacity to make their own decisions; (2) “benecence,” or maximizing
benets and reducing risk to participants; and (3) “justice,” or balancing risk and benets and
selecting study participants only “for reasons directly related to the problem being studied” (US
Department of Health and Human Services,1979).
Implementation of the Belmont Report principles falls to IRBs that protect individual
research participants through condentiality, informed consent, and oversight of research design
and communications with participants. But although IRBs have been the traditional enforcers
of the Belmont principles, they are not the only place where those principles have found expres-
sion. Those same principles form the basis of CBPR, with affected communities engaging
more directly in research design and the collection and analysis of individual-level human data.
CBPR explicitly focuses on problems that affect whole communities—environmental toxics, for
example—and thus is different from most biomedical research, which takes the individual as its
primary subject. In CBPR, researchers work closely with community members and community-
based organizations to develop research agendas, conduct analyses, and disseminate results and
information. This merging of community interests and community action reects another dis-
tinct quality of CBPR: its commitment to advocacy for the public good and creating open access
to information (Morello-Frosch et al.,2015).
CBPR takes “respect for persons” to a new level: not only do study participants voluntarily
participate in research but also they actively collaborate to carry it out. This inclusion reects
CBPR’s commitment to the principles of “benecence” and “justice,” because the active involve-
ment and scrutiny of study participants encourages the fair assessment and distribution of the
research’s risks and benets. Further, the CBPR concept of data as co-owned and the practice
of giving research participants the right to decide whether to have full access to research results
helps ensure they have sufcient information to make informed choices during and after the study
and is thus consistent with Belmont’s emphasis on informed consent. In the process, research
“subjects” are transformed into research “participants.” CBPR thus enters a “post-Belmont era,”
blurring the traditional roles of researcher and subject and taking seriously the insight, energy,
and objectives that members of the affected community bring (Morello-Frosch et al.,2015).
CBPR further embodies the “respect for persons” principle by protecting research partici-
pants from being objectied and dehumanized. By encouraging the active involvement of study
participants in the research process, CBPR greatly reduces the chances that they will be objec-
tied in the rst place. As participants in the design and implementation of the research plan,
members of the affected community have a level of “informed consent” far deeper than typi-
cally occurs in conventional research. Thus CBPR achieves “respect for persons” by democra-
tizing the research process and encouraging scientist experts to work alongside communities,
rather than treating them as objects of study.
Despite these characteristics, however, IRB review of CBPR projects can result in unin-
tended violations of the very principles they seek to uphold. This is in part because of implicit
assumptions embedded in the Belmont Report that were adopted by IRBs but that contradict
other CBPR principles. For example, IRBs, following Belmont, assume that the research par-
ticipant is an individual, whereas CBPR sees research participants as individuals and as a
community of individuals (Deeds et al.,2008). This difference has profound implications for
condentiality, the dissemination of information, and the assessment of risks and benets.
218 Community-Based Participatory Research for Health
The differing assumptions and discord that CBPR researchers and IRBs bring to the
research process come into sharpest relief in the context of two particular CBPR practices: (1)
direct community participation in research and (2) the reporting back of individual results to
study participants who want them. With regard to the rst issue, some clinical researchers form
community or patient advisory boards to promote more communication with study participants
and broader community benets of research. Still, CBPR represents a much deeper form of
engagement with study communities that makes it qualitatively different. CBPR’s inclusion of
laypersons and others traditionally outside the research process means university IRBs must
consider collaborators who are outside their conventional jurisdiction. As a result, IRBs may
be reluctant to oversee human subjects’ protection compliance for such outside partner organi-
zations. This can lead to misunderstandings and unnecessary delays as IRBs deliberate about
whether and how to extend their jurisdiction into new territory, and, if accommodation is not
reached, it can restrict the roles that community members can play or force partner organi-
zations to pay for independent IRB coverage. In terms of the second issue, IRBs may object
when a community-based organization challenges traditional academic norms by engaging in
research and advocacy. Moreover, the CBPR practice of reporting back, and the philosophy of
openness that informs it, challenges IRB assumptions about who controls the ow of data pro-
duced in human subjects research, when and whether those data should be made available to
members of an affected community, and what the nature and duration of the researcher–study
participant relationship should be.
These differences and the unfamiliarity of many IRBs with CBPR can create undue obstacles
and extensive delays to conducting research, diminish the benet of research for study participants,
and potentially cause them harm as they anxiously await unnecessarily long periods of time to
receive results that could inform strategies for protecting their future health and that of their families
and communities. Not surprisingly, some researchers have criticized the rigidity of IRB reviews,
particularly for low-risk, non-intrusive research (Bosk & DeVries,2004; Brown et al.,2010).
UNCERTAINTY OF STUDY RESULTS AND PARTICIPANTS’
RIGHT TO KNOW
A great tension in the ethical oversight of CBPR entails reporting back individual-level results
with scientic uncertainty regarding implications for health. This is particularly the case in the
realm of environmental health research, specically in studies that characterize human expo-
sures to a diverse array of environmental chemicals, through biomonitoring, for example. Since
World War II, more than eighty-three thousand chemicals have been registered for commercial
use in the United States, three thousand of which are produced or imported at 1 million pounds
or more per year (Environmental Protection Agency,2010,2011). Most of these chemicals have
little to no toxicity testing data, and information on exposure sources, mitigation strategies, and
health implications remains elusive in many cases. Although we increasingly know more about
the effects of chemicals on health, signicant data gaps remain and raise ethical and scientic
challenges for whether and how to report biomonitoring results to study participants. As our
analytic capacity to detect chemicals in humans surpasses our ability to interpret results, sci-
entists and IRB members have raised the question of whether it may be detrimental to share
individual biomonitoring results with study participants. Hypothetically, a participant might be
Democratizing Ethical Oversight of Research through CBPR 219
psychologically harmed by receiving results if their clinical signicance is unknown or if no
valid options exist to address the potential health risks they reveal (Shalowitz & Miller,2005).
Indeed, the National Bioethics Advisory Committee issued guidelines directing researchers
to report biomarkers only when health implications are signicant and recourse is available
(National Bioethics Advisory Committee, 1999). These discussions may not, however, have
adequately considered the distinction between communications related to genetic biomarkers,
which are not modiable, and chemical exposures, many of which are modiable. When these
clinical guidelines are applied to chemical exposure research, people are left unaware of the
presence in their own bodies of environmental chemicals, often known to be harmful in animal
studies and sometimes in in vitro and human studies.
From the perspective of CBPR, such rigid reporting-back guidelines are an affront to indi-
viduals’ and communities’ right to know, and by extension they tarnish the scientic process.
More recently, several guidance documents, including the National Academy of Sciences bio-
monitoring report, now support participants’ right to know their personal chemical biomonitor-
ing results (Brody et al.,2014). Nevertheless, tensions between participants’ right to know their
exposure results and their capacity or right to act to reduce those exposures can raise ethical
challenges when developing results communication protocols. For example, in some occupa-
tions (e.g., farm workers or custodians) study participants may not be able to take action to
reduce their chemical exposures, either through the use of personal protective equipment or
the substitution, reformulation, and purchasing of less-toxic products used at the workplace
(Holmes,2013; Senier, Mayer, Brown, & Morello-Frosch,2007).
Research on reporting back in personal exposure studies and genetics research has also
explored study participant perspectives and expectations, and evidence indicates that although
some participants might opt out of learning their results, the vast majority believe they have a
right to know. One study reported that 97 percent of participants wanted their personal exposure
results even if the health implications of the data were not clear (Brody et al., 2007), mir-
roring the strong desire of study participants in other environmental health studies to receive
results (Quandt et al.,2004). As in chemical biomonitoring studies, public attitudes about ge-
netic research also support the return of individual results. A poll concluded that for many study
participants, learning their results was a large motivating factor for enrolling in such studies,
with 75 percent of 4,500 respondents in one study indicating they would be less likely to vol-
unteer if individual results were not provided (Kaufman, Murphy, Scott, & Hudson, 2008).
Despite this evidence, individualized reporting back remains controversial because many IRBs
question whether scientic uncertainty regarding health implications of genetic or chemical
biomonitoring results can cause undue stress among study participants. This concern may not
be warranted. A randomized study investigating the psychological effects of disclosure of an
apolipoprotein E (APOE) allele associated with Alzheimer’s disease revealed that participants
who were informed that they had a genetic predisposition did not show more symptoms of
anxiety or depression compared to participants who did not get their screening results (Green
etal.,2009). Similarly, evaluation of reporting back in community-engaged chemical biomoni-
toring studies indicates that participants who learn about their chemical exposures gain valuable
knowledge about environmental health, which results in behavioral changes (e.g., in purchasing
decisions) and engagement in the policy process (e.g., public testimony to inuence industrial
permitting decisions) (Adams et al.,2011; Altman et al.,2008).
220 Community-Based Participatory Research for Health
Although the biomedical-driven research approach may recommend only reporting back
when health implications are clear, a CBPR right-to-know approach empowers study par-
ticipants with knowledge, addresses community-level concerns such as stigmatization, and
promotes policy change. Moreover, biomedical ethics are evolving to promote more open com-
munication between patients and health care providers, which has begun to inuence com-
munication strategies in environmental health science. For example, through the Open Notes
project, patients who were given electronic access to their doctors’ notes reported feeling more
informed and in control of their health care, which in turn fostered more productive commu-
nication and shared decision making with their health care providers (Delbanco et al.,2012).
Digital communication interfaces used in the clinical setting can be adapted for applications
to report back individual results in CBPR projects by providing options for receiving results,
including views using text or graphs, in different languages, and aimed at diverse literacy levels
(Boronow et al.,2017). Key to this reporting-back process is a collective consensus about who
represents the interests of study communities and how their priorities can be effectively incor-
porated into protocol development.
IRB CHALLENGES RELATED TO INDIGENOUS RESEARCH
Scientic research has a sordid history in the colonization of Indigenous peoples within the
United States and internationally through the devaluation, appropriation, and desecration of
their beliefs, cultural practices, knowledge, environments, and bodies (Smith, 2012; Tall-
bear, 2013). Yet because tribes and other Indigenous peoples insist on their status as sover-
eigns, they also resist, regulate, initiate, collaborate in, and govern ethics in research in ways
that support self-governance, cultural-centeredness, and sovereignty. (See Chapter 14.) For
example, CBPR has been used to carry out innovative environmental health research projects
with Native Americans and Alaska Natives in the United States (Hoover et al.,2012). US law
requires extensive review by multiple IRBs; the Indian Health Service tasks area IRBs and tribal
epidemiology centers with evaluating research projects involving American Indians and Alaska
Natives. These committees generally include Native and non-Native members, researchers, cli-
nicians, and community leaders (Saxton et al.,2015). In addition, tribes often have their own
internal IRBs or tribal government approval processes to vet research projects to ensure that
they align with their own priorities as well as legal and cultural standards (Becenti-Pigman
etal.,2008; Macaulay et al.,1998; Sharp & Foster,2002).
Although tribal IRBs seek to protect the sovereignty and interests of Indigenous commu-
nities, some external IRBs universalize ethical frameworks in ways that “homogenize” Indig-
enous communities as inherently vulnerable without regard to their interests, relationships to
researchers, and leadership roles on research projects. These cases have been characterized as
a form of “ethical imperialism” that undercuts the research priorities and methods advanced by
Indigenous communities (Saxton et al.,2015). For example, a tribal collaboration with university
researchers and a nongovernmental organization to conduct a CBPR breast milk biomonitoring
study among Alaska Native communities was thwarted by the Alaska area IRB, despite clear
support from tribal leadership, on the grounds that the study might discourage breastfeeding.
For nearly ve years, tribal and university researchers sought to alleviate these ethical concerns
by demonstrating to the area IRB that their biomonitoring study protocol would report results to
Democratizing Ethical Oversight of Research through CBPR 221
participants while actively encouraging the continuation of breastfeeding. After several rounds
of protocol review, the study was effectively thwarted by the Alaska area IRB. The rigidity of
the IRB review in effect undermined key Belmont tenets, including autonomy, benecence, and
justice, by hindering the project, which sought to address Alaska Native communities’ concerns
about exposures to environmental chemicals in the Arctic region (Saxton et al.,2015).
Most tribal research rules of conduct and reviews strongly encourage reporting back of
ndings to individual research participants and the tribe (American Indian Law Center,1999;
Freeman,2004). Reporting back is viewed as a continuous process rather than something that
occurs only at the conclusion of a research project (American Indian Law Center,1999). The
Indigenous Rights Protection Act (Indigenous Peoples Council on Biocolonialism,2000) stip-
ulates that researchers must provide a detailed plan on how they will communicate aggregate
study results to diverse audiences and personal results to individual participants and how the
community at large will be educated or empowered by their proposed study. A description of
the frequency and manner by which the aggregate data and progress reports will be shared with
research review committees along with a communication plan for presenting aggregate results
to the community at large must be included in study protocols. These requirements afrm the
notion of community engagement in the development of results communication protocols and
the reporting back of results as a reexive and iterative process.
DEMOCRATIZING ETHICAL OVERSIGHT OF RESEARCH
The problems that arise in IRB reviews of CBPR projects stem from the different assumptions
and objectives of diverse parties and institutions. Therefore, effective solutions require engage-
ment by all research stakeholders to successfully navigate ethical review of multi-partner CBPR
projects: IRBs, CBPR researchers, community and CBO partners, study participants, and fund-
ing agencies. Researchers need to educate those IRB members who may be unfamiliar with
CBPR in its basic principles, its scientic and community benets, and the unique ethical con-
siderations it raises. CBPR scientists can connect community partners with IRB staff members
to demonstrate the community’s involvement in the research process and how their perspec-
tive on human subjects’ protection is key to the project’s success. This might include inviting
community partners to meetings with the IRB. Research partners can include this “community
consent” in their IRB application. If the IRB lacks the familiarity, experience, or the skill set
necessary for assessing the ethical issues posed by a research project, an outside expert should
be brought in to educate the board.
Funding institutions, including National Institutes of Health and National Science
Foundation, should offer human subjects guidance specic to CBPR research and should sen-
sitize universities to the importance of supporting community groups. (See Appendix 8 for
community CITI trainings.) University IRBs should be aware that community organizations
may operate on different time lines and that the intense and lengthy university IRB-reporting
process can create conicts for them. Even when giving this guidance to IRBs, researchers
doing grant-funded community-based research should include ample time for IRB review in
their grant proposals. Similarly, funding agencies should encourage academic institutions to
provide IRB oversight to academic and community partners to avoid unnecessary delays and
expenses in protocol reviews. They may want to promote consortium-based approval whereby
222 Community-Based Participatory Research for Health
one institution’s IRB is accepted by others in the consortium; indemnication may be necessary
so that universities do not bear responsibility for the actions of community partners.
IRBs need to better regulate potential conicts of interest their members may bring to the
review process, particularly when an institution might have a vested interest in the outcome
of a proposed study (because of its implications for a state public health agency action, for
example). A survey of 893 IRB members at one hundred academic institutions found that 36
percent had at least one relationship with industry in the previous year, of which only two-thirds
had been disclosed to the IRB. Of those reporting conicts, nearly one-third had participated in
the reviews anyway (Campbell et al.,2006).
Finally, IRBs must reexamine how they address situations in which participants want access
to and disclosure of their own study results. In some cases, this necessitates continued interac-
tion between researchers and participants, a process that IRBs have traditionally been reluctant
to allow and are poorly designed to manage. In the case of environmental health research, iter-
ative rounds of approval for ongoing communication with study participants can create delays
that undermine researchers’ relationships with participants and harm participants’ capacity to
take timely action to reduce their exposures. To address this challenge, IRBs can review proto-
types of such communication protocols without having to repeat reviews with every iteration.
Participants may also want to share their personal results with other study participants and have
the collective power to disseminate their results through their own networks and broader public
forums. Putting the brakes on individual reporting back could push condentiality protections
to collide with the principle of benecence. Thus, CBPR challenges IRBs to reassess the seem-
ingly contradictory elements of the Belmont principles and develop alternatives that do not
require choosing one principle over another.
WORKING WITH COMMUNITY AND TRIBAL IRBS
University IRBs are not the only forums in which community benets and risks of research may
be assessed. Some tribes convene their own review boards to evaluate collectively whether pro-
posed research is justied and benets the community (Quigley,2006). Although tribal IRBs
have the power of regular IRBs, other community review boards do not meet the requirements
for oversight of federally funded research, requiring an additional IRB to provide formal guar-
antees. Academic IRBs reviewing research proposals on behalf of such communities need to
understand their form and organization, their needs and vulnerabilities, and their governance
and communication structures for disseminating research (Weijer,1998).
Community representation in the review process would be helpful not only to those explic-
itly engaged in CBPR but also to those engaged in individual research who may not have con-
sidered the effects of their research on communities. NIH rules were claried in 1998 to ensure
that IRBs have “knowledge of the local research context,” but although one member of the IRB
must be from outside the institution, direct community representation is not required (National
Institutes of Health, 1998). Community representation on academic IRBs usually takes the
form of large, well-established organizations rather than grassroots groups and does not usu-
ally reect the demographic composition of the communities under study. We recommend that
IRBs recruit not just any community members but those who have experience in either CBPR
or other community-engaged research. This can provide benets to many IRB reviews because
Democratizing Ethical Oversight of Research through CBPR 223
of the creativity, exibility, and respect for human subjects’ protection that comes with CBPR
experience.
CONCLUSION
The very CBPR practices that concern many IRBs are exactly those that make community-
engaged work so valuable for communities and the scientic enterprise and that enhance eth-
ical oversight of research. Yet, ethical tensions emerge when communities that seek to conduct
research with scientic collaborators face roadblocks by IRBs, which delay or deny approval of
study protocols and hinder investigations of potentially signicant public questions that affect
them. Efforts to overcome these IRB challenges require a holistic understanding of how CBPR
researchers and study communities (whether dened by geography, class, ethnicity, or other
socially salient distinctions) collaborate in ways that empower the latter to play a central role
in the scientic enterprise, which includes ethical oversight of research. Ultimately, IRBs will
need to go beyond simply modifying traditional review procedures to fundamentally incorpo-
rate how CBPR ethics redenes the scientic enterprise itself, including researcher-participant
relationships, academic-community interactions, and the right to know the signicance of study
results for individual and collective action to improve public health.
QUESTIONS FOR DISCUSSION
1. What are the elements of CBPR that can advance ethical oversight of public health and
medical research?
2. How can IRBs do more to integrate ethical protections for study communities and
individual study participants?
REFERENCES
Adams, C., Brown, P., Morello-Frosch, R., Brody, J. G., Rudel, R., Zota, A.,...Patton, S. (2011). Disentangling the exposure
experience: The roles of community context and report-back of environmental exposure data. Journal of Health and
Social Behavior, 52(2), 180–196. https://doi.org/10.1177/0022146510395593
Altman, R. G., Morello-Frosch, R., Brody, J. G., Rudel, R., Brown, P., & Averick, M. (2008). Pollution comes home and gets
personal: Women’s experience of household chemical exposure. Journal of Health and Social Behavior, 49(4), 417–435.
American Indian Law Center. (1999). Model tribal research code: With materials for tribal regulation for research and check-
list for Indian health boards (3rd ed.). Albuquerque, NM: Author.
Balazs, C. L., & Morello-Frosch, R. (2013). The three R’s: How community-based participatory research strengthens the
rigor, relevance and reach of science. Environmental Justice, 6(1). https://doi.org/10.1089/env.2012.0017
Becenti-Pigman, B., White, K., Bowman, B., Palmenteer-Holder, N. L., & Duran, B. (2008). Research policies, processes and
protocol: The Navajo Nation Human Research Review Board. In M. Minkler & N. Wallerstein, Community-based partici-
patory research for health: Processes and outcomes (2nd ed., pp. 441–446). San Francisco, CA: Jossey-Bass.
Boronow, K. E., Sussman, H. P., Gajos, K. Z., Rudel, R. A., Arnold, K. C., Brown, P., Morello-Frosch, R., Havas, L., & Brody,
J. G. (2017). DERBI: A digital method to help researchers offer “right-to-know” personal exposure results. Environmental
Health Perspectives, 125(2), A27–A33.
Bosk, C., & DeVries R. (2004). Bureaucracies of mass deception: Institutional review boards and the ethics of ethnographic
research. Annals of the American Academy of Political and Social Science, 595, 249–263.
224 Community-Based Participatory Research for Health
Brody, J. G., Dunagan, S. C., Morello-Frosch, R., Brown, P., Patton, S., & Rudel, R. A. (2014). Reporting individual results
for biomonitoring and environmental exposures: Lessons learned from environmental communication case studies. Envi-
ronmental Health: A Global Access Science Source, 13, 40. https://doi.org/10.1186/1476-069X-13-40
Brody, J. G., Morello-Frosch, R., Brown, P., Rudel, R. A., Altman, R. G., Frye, M.,...Seryak, L. M. (2007). Improving dis-
closure and consent. American Journal of Public Health, 97(9), 1547–1554. https://doi.org/10.2105/AJPH.2006.094813
Brown, P., Morello-Frosch, R., Brody, J. G., Altman, R. G., Rudel, R. A., Senier, L.,...Simpson, R. (2010). Institutional
review board challenges related to community-based participatory research on human exposure to environmental toxins:
A case study. Environmental Health: A Global Access Science Source, 9, 39. https://doi.org/10.1186/1476-069X-9-39
Campbell, E. G., Weissman, J. S., Vogeli, C., Clarridge, B. R., Abraham, M., Marder, J. E., & Koski, G. (2006). Finan-
cial relationships between institutional review board members and industry. New England Journal of Medicine, 355(22),
2321–2329. https://doi.org/10.1056/NEJMsa061457
Deeds, B. G., Castillo, M., Beason, Z., Cunningham, S. D., Ellen, J. M., Peralta, L., & Adolescent Trials Network for HIV/
AIDS interventions. (2008). An HIV prevention protocol reviewed at 15 national sites: How do ethics committees pro-
tect communities? Journal of Empirical Research on Human Research Ethics, 3(2), 77–86. https://doi.org/10.1525/
jer.2008.3.2.77
Delbanco, T., Walker, J., Bell, S. K., Darer, J. D., Elmore, J. G., Farag, N.,...Leveille, S. G. (2012). Inviting patients to read
their doctors’ notes: A quasi-experimental study and a look ahead. Annals of Internal Medicine, 157(7), 461. https://doi.
org/10.7326/0003-4819-157-7-201210020-00002
Environmental Protection Agency. (2010). HPV chemical hazard data availability study. Retrieved October 15, 2011, from
www.epa.gov/HPV/pubs/general/hazchem.htm
Environmental Protection Agency. (2011). TSCA chemical substance inventory. Retrieved December 17, 2012, from www.
epa.gov/oppt/existingchemicals/pubs/tscainventory/index.html
Freeman, W. L. (2004). The protection of potential individual volunteers and tribal communities in research involving the
Indian Health Service (IHS) (IRB appendix). Portland, OR: Northwest Portland Area Indian Health Service Institutional
Review Board.
Green, R. C., Roberts, J. S., Cupples, L. A., Relkin, N. R., Whitehouse, P. J., Brown, T.,...Farrer, L. A. (2009). Disclosure
of APOE genotype for risk of Alzheimer’s disease. New England Journal of Medicine, 361(3), 245–254. https://doi.
org/10.1056/NEJMoa0809578
Holmes, S. (2013). Fresh fruit, broken bodies. Berkeley CA: University of California Press.
Hoover, E., Cook, K., Plain, R., Sanchez, K., Waghiyi, V., Miller, P.,...Carpenter, D. O. (2012). Indigenous peoples of North
America: Environmental exposures and reproductive justice. Environmental Health Perspectives, 120(12), 1645–1649.
https://doi.org/10.1289/ehp.1205422
Indigenous Peoples Council on Biocolonialism. (2000). Indigenous Research Protection Act. Retrieved January 15, 2017
from www.ipcb.org/
Kaufman, D., Murphy, J., Scott, J., & Hudson, K. (2008). Subjects matter: A survey of public opinions about a large genetic
cohort study. Genetics in Medicine: Ofcial Journal of the American College of Medical Genetics, 10(11), 831–839.
https://doi.org/10.1097/GIM.0b013e31818bb3ab
Macaulay, A. C., Delormier, T., McComber, A. M., Cross, E. J., Potvin, L. P., Paradis, G., Kirby, R. L., Saad-Haddad, C., &
Desrosiers, S. (1998). Participatory research with native community of Kahnawake creates innovative code of research
ethics. Canadian Journal of Public Health, 89, 105–108.
Morello-Frosch, R., Varshavsky, J., Liboiron, M., Brown, P., & Brody, J. G. (2015). Communicating results in post-Belmont
era biomonitoring studies: Lessons from genetics and neuroimaging research. Environmental Research, 136, 363–372.
https://doi.org/10.1016/j.envres.2014.10.001
National Bioethics Advisory Committee. (1999). Research involving human biological materials: Ethical issues and policy
guidance. Rockville, MD: National Institutes of Health.
National Institutes of Health. (1998). IRB knowledge of local research context. Bethesda, MD: Division of Human Subjects
Protection OPPR.
Quandt, S. A., Doran, A. M., Rao, P., Hoppin, J. A., Snively, B. M., & Arcury, T. A. (2004). Reporting pesticide assessment
results to farmworker families: Development, implementation, and evaluation of a risk communication strategy. Environ-
mental Health Perspectives, 112(5), 636–642.
Quigley, D. (2006). A review of improved ethical practices in environmental and public health research: Case examples from
native communities. Health Education and Behavior, 33, 130–147.
Democratizing Ethical Oversight of Research through CBPR 225
Saxton, D. I., Brown, P., Seguinot-Medina, S., Eckstein, L., Carpenter, D. O., Miller, P., & Waghiyi, V. (2015). Environmental
health and justice and the right to research: Institutional review board denials of community-based chemical biomonitor-
ing of breast milk. Environmental Health, 14, 90. https://doi.org/10.1186/s12940-015-0076-x
Senier, L., Mayer, B., Brown, P., & Morello-Frosch, R. (2007). School custodians and green cleaners new approaches to
labor-environment coalitions. Organization and Environment 20, 304–324.
Shalowitz, D. I., & Miller, F. G. (2005). Disclosing individual results of clinical research: Implications of respect for partici-
pants. Journal of American Medical Association, 294(6), 737–740.
Sharp, R. R., & Foster, M. W. (2002). Community involvement in the ethical review of genetic research: Lessons from
American Indian and Alaska Native populations. Environmental Health Perspectives, 110, 145–148.
Smith, L. T. (2012). Decolonizing methodologies: Research and indigenous peoples. London, UK: Zed Books.
Tallbear, K. (2013). Native American DNA: Tribal belonging and the false promise of genetic science. Minneapolis, MN: The
University of Minnesota Press.
US Department of Health and Human Services. (1979). The Belmont report: Ethical principles and guidelines for the pro-
tection of human subjects of research. Bethesda, MD: The National Commission for the Protection of Human Subjects of
Biomedical and Behavioral Research.
Weijer, C. (1998). Protecting communities in research: Philosophical and pragmatic challenges. Cambridge Quarterly of
Healthcare Ethics, 8, 501–513.
16
CHAPTER
IN 2007 WE began to reect on the mismatch between traditional research ethics and institu-
tional review board (IRB) guidelines and the kinds of issues that are encountered in community-
based participatory research (CBPR) (Flicker et al., 2007). Although we recognized the
importance of ethics review and the need for researchers to be accountable for their practices,
we were able to show that the dominant biomedical orientation of review processes was cre-
ating challenges given the exible, collaborative, and relational approaches found in CBPR.
After assessing the applicability of institutional research ethics review to CBPR principles, we
proposed suggestions for improving their relevance. Since then, Canadian research ethics board
practices are demonstrating slow but promising paradigmatic and policy shifts (Guta, Wilson,
et al., 2010). Many US IRBs are also improving their procedures for more effective and relevant
reviews of CBPR research.
In continuing to study ethics in the context of CBPR, we have become increasingly con-
vinced that IRB institutional changes are only one piece of the ethics puzzle. Many ethical
challenges and daily dilemmas faced by CBPR practitioners fall outside the purview of review
boards (Mikesell, Bromley, & Khodyakov,2013). It is in the everyday choices about how to
engage community, with myriad “right” and “wrong” answers, that ethics, morals, values, and
principles may conict.
EVERYDAY CHALLENGES IN
THE LIFE CYCLE OF CBPR
BROADENING OUR BANDWIDTH ON ETHICS
SARAH FLICKER, ADRIAN GUTA, AND ROBB TRAVERS
228 Community-Based Participatory Research for Health
In response to the ways in which conventional research has historically been conducted on
community (rather than with or alongside), CBPR has been positioned as an ethical alternative,
based on core principles (see Chapter3), that seeks to engage those most affected by health ineq-
uities in the research process as full and engaged partners. These principles codied a “new”
way of operating that privileged relationality, multiple voices, and different ways of knowing.
IRBs were never in a position to monitor these sets of ethical commitments, nor should they
be. And yet, these ethical commitments have become for many CBPR practitioners a moral
compass that guides our work. In choosing to describe our work as CBPR, community and
academic practitioners actively align themselves with this principled promise that boasts the
potential for transformational outcomes.
However, these principles do not always work congruently and sometimes may be in
tension with each other (Travers et al.,2013). It is in these moments of tension, and in the quest
to honor these values, that new ethical dilemmas emerge. Work in, and with, community is
often messy, complicated, and hard. In contrast to romanticized notions of empowered citizens
engaging in transformational social justice work, we often become mired in the slow, tedious
work of making hard quotidian decisions ranging from resource allocation to data analysis.
However, the ways we go about making decisions on these matters is not trivial. As Eikeland
(2006) so eloquently writes,
the ethical questions that concern action research often seem to operate on a smaller scale,
such as: who is to be involved; how and why; who makes decisions and how; whose interpre-
tations are to prevail and why; how do we write about and publish on people involved; who
owns the ideas developed; etc....The consequences of letting such questions pass unattended
may be—intended or not—the spontaneous, habitual emergence of subtle power structures on
a micro-level, not clearly visible in the beginning, but accumulating and “petrifying” over time
into larger unwanted patterns. (pp. 38–39)
Thus, in this chapter, we pay attention to what Banks and her colleagues (2013) call the
“everyday ethics” of CBPR. The small and everyday decisions that represent choices about
power, equity, and justice often operate at the microlevel of weighing these moment-to-moment
alternatives. Together, these everyday decisions inform how CBPR practitioners understand
themselves as moral agents and engage community in ethical ways.
LAYING THE GROUNDWORK
The rst step in beginning a CBPR project, of gathering and establishing your team, can be one
of the most ethically fraught. It brings up many questions about “who represents a community?”
(Jewkes & Murcott,1998) and who has the authority to speak or make decisions on behalf of his
or her peers. These questions are particularly challenging to answer in contexts in which there is
no elected or ofcial leadership body. For many stigmatized and marginalized communities, there
may be few entities that purport to represent them, and they are unlikely to reect the diversity
of community experience. In such cases, the “community” may be represented by elected of-
cials, government bureaucrats, staff members, volunteers, board members of community-based
organizations, or those with lived experience of the issue under study. If research foci are contro-
versial, there may be strong differences of opinion and political histories between communities

Everyday Challenges in the Life Cycle of CBPR 229
that are fractured and divided by the issues under study. Decisions about representation and gov-
ernance will have powerful implications for the kinds of questions that get asked and the ways
they get answered. For researchers who may be “outsiders” the complications multiply: they
may not immediately realize the complexities of the landscape (D’Alonzo,2010). For example,
a group of CBPR practitioners were surprised to discover the range of perspectives about sub-
stance use within a small health care facility and inadvertently created conict between clients
(Strike et al.,2016). They ultimately had to redesign their project and implemented new steps to
ensure participants felt supported.
Sorting out representation, governance, and human resource policies can be a fraught matter.
Projects may decide to include community members as coinvestigators, create community advi-
sory boards, hire community members as core staff, or all three. There is a wide range of the
degree to which each project takes up participatory principles and is successful in democra-
tizing power. In “Case Example16.1: Trans PULSE,” the research team intentionally developed
a governance structure that ensured that trans community members’ voices would always be in
the majority.
CASE EXAMPLE 16.1 Trans PULSE
The Trans PULSE Project is a CBPR project that investigates the impact of social exclusion and
discrimination on the health of trans people in Ontario, Canada. The project was initiated by trans
community members with support from an ally who worked at a local health center. Together,
these community partners sought out academic partners and built a governance model in which
key decisions had to be approved in contexts when 50 percent +1 of the vote came from trans
members of the investigator’s team.
Source: Travers et al. (2013).
GETTING “PERMISSION”: GOVERNANCE AS STEWARDSHIP
AND HONORING COMMUNITY PROTOCOLS
As a result of the ongoing colonial violence done in the name of research, many Indigenous
communities are now demanding that research done in, and with, their communities formally
seek tribal permission and adopt more participatory practices. CBPR’s decolonizing potential
(Darroch & Giles,2014) has excited many scholars who are actively trying to adapt methodol-
ogies to local contexts (Castleden, Garvin, & First Nation,2008; Simonds & Christopher,2013).
In addition to the original principles laid out by Israel et al. (1998), CBPR projects operating in
Indigenous contexts must also acknowledge history, context, tribal sovereignty, and Indigenous
ways of knowing (LaVeaux & Christopher,2009).
Furthermore, the idea of CBPR governance as stewardship has gained popularity. “Gov-
ernance as stewardship enhances protection of the community, helps foster research partner-
ships and appropriate...approval of research by community bodies, ensures benet for the
community, provides legitimacy and shares responsibility for the research, provides community
control, and builds research capacity in communities” (Oetzel et al.,2015, p. 1161).

230 Community-Based Participatory Research for Health
Tribal and community review boards have sprung up to offer additional community rel-
evant protections beyond traditional ethics review, attending to such issues as cultural safety,
community consent, and important process concerns (Shore et al.,2011). Moreover, in Canada,
research policy now requires researchers seeking to do research with Indigenous communities to
rst obtain formal permission from those communities (Tri-Council of Canada,2010). Although
recognizing Indigenous sovereignty, this has been complicated to put into practice. Many
reserve communities have formal leadership structures or research councils, yet those seeking
to do research with urban Aboriginal people may nd guring out “whom to ask” difcult. Nev-
ertheless, this model of showing clear respect for communal rights to self- determination may
be an important one to pursue when working with other groups that have also suffered colonial
(and other forms) of oppression. In “Case Example16.2: Taking Action! Building Aboriginal
Youth Leadership for HIV Prevention,” the research team sought informed communal consent
from several formal bodies and informal stakeholders to ensure that their protocol was ethical,
culturally safe, and respectful in specic local contexts.
CASE EXAMPLE 16.2 Taking Action! Building Aboriginal Youth Leadership
for HIV Prevention
This CBPR project worked with six Indigenous communities across Canada. The project was
governed by a national Indigenous youth council and the Canadian Aboriginal AIDS Network’s
National Research Advisory Committee, made up of diverse community stakeholders. In addition
to formally getting approval through multiple university-based research ethics boards, the project
also sought formal permission from various local entities. In urban centers, project leads met with
local community-based organizations and sought permission. In a northern Inuit community, they
received approval from the mayor and elected ofcials. In multiple First Nations communities,
Taking Action approached local and regional research councils (if constituted) and band councils.
Source: Flicker et al. (2014).
PROJECT IMPLEMENTATION
Gathering data in marginalized communities can be extremely challenging. Sometimes those
with lived experience of the issue under study are in the best position to navigate hidden net-
works. Peer researchers (PRs) are members of a research project’s target population who are
trained to participate as coresearchers (Flicker, Roche, & Guta, 2010; Greene et al., 2009).
Recruiting, hiring, and managing peer researcher involvement can present unique ethical chal-
lenges (Guta, Flicker, & Roche,2010).
Similar to all new staff members in a research project, peer researchers require extensive
training. For some PRs, it may be the rst time that they are working in professional environ-
ments, and additional supports may be necessary. This is particularly true for peer researchers
who may be unintentionally triggered by the nature of their work duties (e.g., drug users collect-
ing drug-related data). Because PRs may be navigating their own personal networks or operating

Everyday Challenges in the Life Cycle of CBPR 231
in very small, tight-knit communities, special attention to helping PRs manage boundaries (e.g.,
maintaining condentiality) may be challenging.
Despite the fact that PR positions may be seen as a step toward inclusion and increasing
participation, care needs to be taken to think through the possibilities for real and meaningful
power sharing (particularly when PRs are operating in a traditional, bureaucratic employee
structure). As we have noted elsewhere, “Care should be taken to avoid research practices that
benet extensively from the labor and expertise of peer researchers, but offers little in return in
the way of recognition, remuneration, or a sense of ownership of the work” (Flicker et al.,2010,
p. 3). In “Case Study16.3: Women’s CBR Study,” the research team had to change their original
plans to accommodate the unique inclusion needs of their peer researchers.
Finding creative strategies for engaging PRs, and community partners in general, in
data analysis has the potential to enrich analyses and interpretation and dissemination strat-
egies (Cashman et al.,2008; Flicker,2008). Evaluations reveal that this tends to be an area in
which many projects fall short of their participatory promise (Flicker, Savan, Mildenberger, &
Kolenda,2008; Flicker et al.,2008); leaving PRs out of analysis can be unintentionally disem-
powering to those who are excluded (Travers et al.,2013).
CASE STUDY 16.3 Women’s CBR Study
Women living with HIV were hired to conduct and facilitate focus groups with other HIV+
women. However, because of HIV-related stigma and complicated community relationships, the
peer researchers did not want their names associated with project recruitment or dissemination
materials. They were also reluctant to take leadership roles in focus group facilitation because
many of them felt uncomfortable about the power dynamics this might set up with their peers.
Peer researchers needed a number of additional (social, psychological, physical, and monetary)
supports in place in order to succeed at their jobs.
Source: Logie, James, Tharao, and Loutfy (2012).
SHARING YOUR WORK AND ENDING THE CYCLE
The end of a project phase presents new ethical issues when thinking about how to share
research ndings in respectful and accessible formats, how to credit participation, and how to
close a project. Some partners, particularly those from marginalized communities, may not see
the utility of investing precious project time and resources into academic publications. Many
may want to publicize results in more accessible ways (e.g., newsletters, press releases, blog
posts, social media) to get the word out. Developing a comprehensive knowledge translation
and exchange plan (Nixon, Casale, Flicker, & Rogan,2012) that species data sharing and own-
ership protocols (Schnarch,2004), often through memoranda of understanding—in advance—
can be a useful strategy for guring out who needs to be reached how and with what messages.
Then, difcult conversations need to be had about how project resources will be allocated to
realize these ambitions.
232 Community-Based Participatory Research for Health
Another end-of-project issue is how people will get recognized and credited for their work.
Academics and staff members from community-based organizations are often happy to have their
job titles acknowledged. However, this may be more complicated when team members belong
to stigmatized communities (e.g., drug using, sex working, HIV+). They may have invested sub-
stantial time and intellectual capital but have very mixed feelings about attaching their names
to documents that may live on in the public record. For instance, a youth who is currently street
involved and an activist on the project may not want to be afliated as “the homeless youth” on
a report or conference presentation years later when he or she may no longer identify with that
experience. The traumas of disclosure may also have real legal implications for some. Care needs
to be taken to carefully negotiate a plan for acknowledgment that takes into account pres ent
and potential future conditions. For instance, in “Case Study16.4: Healing Home,” the research
team took extra precautions to ensure the long-term condentiality and anonymity of previously
homeless participants when a book about their project was being published.
Last, although academics and service providers often move from one project to another
(following funding cycles), these research projects often become meaningful interventions for
community members involved. They can provide structure, purpose, employment, and social
support and referrals for health care, housing, and social services. Some community members
invoke “family” when describing CBPR projects; these research projects can become a lifeline
for more marginalized members of the team. Carefully planning for the end-of-project funding
and creating a transition plan for all members of a team is a necessary ethical requirement.
CASE STUDY 16.4 Healing Home
Homeless young women were involved in a project that looked at social and structural barriers and
facilitators to their health and well-being. At the time of their participation, the youth were all very
excited about the project and proud of their role in it. However, a few years later, when the project
was being turned into a book, some of the participants who had subsequently found housing and
stability were very worried about the possible implications of being identied by current friends,
partners, or employers. Extra caution was taken to ensure their anonymity.
Source: Oliver (2013).
CONCLUSION
The issues we have discussed are complex, and there are no “absolute” right ways of approach-
ing them; careful ethical reection throughout the research process can lead to creative and
equitable responses. Reection on the ways power operates in these micro moments can lead to
strategies for opportunities to share control. For example, when a CBPR project is submitted for
institutional ethics review, community partners may feel a sudden shift in power toward the uni-
versity. Sharing full control in such moments is very likely not possible, but providing the space
to discuss people’s feelings in relation to the shift is possible (and necessary). Paying attention
to such “relational” challenges in the life of a CBPR project is crucial.
Everyday Challenges in the Life Cycle of CBPR 233
As Banks and colleagues (2013) write, “This way of constructing the ‘ethical’ is to see the
moral agent not just as an impartial deliberator, but also as an embedded participant with situated and
partial relationships, responsibilities, values and commitments that frame and constrain ways of see-
ing, judging and acting in particular situations. Thus the ‘ethical’ is present in ways of being as well
as acting, and in relationships and emotions, as well as conduct” (p. 266). In order for CBPR to truly
be about reparative justice, we need to be “actuating a new type of ethical practice through mutuality,
equity, and shared responsibility” (Bromley, Mikesell, Jones, & Khodyakov,2015, p. 902).
QUESTIONS FOR DISCUSSION
Imagine you are building a new CBPR team and don’t want to be caught off guard with unfore-
seen ethical challenges.
1. What governance, decision-making, and conict resolution models will your team adopt
to transform traditional power structures in ways that are reasonable and feasible? What
could a partnership agreement cover to be helpful? What ethical principles are important
for your team to uphold?
2. What kinds of training and supports will you put in place for peer researchers and other
community members? How will you ensure that your research approach does not further
stigmatize communities?
3. How will you plan for the end life of a project? What strategies can you build in to ensure
a smooth transition for all team members?
REFERENCES
Banks, S., Armstrong, A., Carter, K., Graham, H., Hayward, P., Henry, A., . . . McNulty, A. (2013). Everyday ethics in
community-based participatory research. Contemporary Social Science, 8(3), 263–277.
Bromley, E., Mikesell, L., Jones, F., & Khodyakov, D. (2015). From subject to participant: Ethics and the evolving role of
community in health research. American Journal of Public Health, 105(5), 900–908.
Cashman, S., B., Adeky, S., Allen, A., J., Corburn, J., Israel, B. A., Montaño, J.,...Wallerstein, N. (2008). The power and the
promise: Working with communities to analyze data, interpret ndings, and get to outcomes. American Journal of Public
Health, 98(8), 1407–1417.
Castleden, H., Garvin, T., & First Nation, H.-a.-a. (2008). Modifying photovoice for community-based participatory Indig-
enous research. Social Science & Medicine, 66(6), 1393–1405. doi:https://dx.doi.org/10.1016/j.socscimed.2007.11.030
D’Alonzo, K. T. (2010). Getting started in CBPR: Lessons in building community partnerships for new researchers. Nursing
Inquiry, 17(4), 282–288.
Darroch, F., & Giles, A. (2014). Decolonizing health research: Community-based participatory research and postcolonial
feminist theory. The Canadian Journal of Action Research, 15(3), 22–36.
Eikeland, O. (2006). Condescending ethics and action research. Action Research, 4(1), 37–47. doi:10.1177/147675030606054
Flicker, S. (2008). Who benets from community-based participatory research? Health Education & Behavior, 35(1), 70–86.
Flicker, S., Danforth, J., Oliver, V., Konsmo, E., Wilson, C., Jackson, R.,...Mitchell, C. (2014). “Because we have really
unique art”: Decolonizing research with Indigenous youth using the arts. International Journal of Indigenous Health,
10(1), 16–34.
Flicker, S., Roche, B., & Guta, A. (2010). Peer research in action III: Ethical issues. Toronto, Canada: Wellesley Institute.
Flicker, S., Savan, B., McGrath, M., Kolenda, B., & Mildenberger, M. (2008). If you could change one thing . ..What
community-based researchers wish they could have done differently. Journal of Community Development, 43(2), 239–253.
234 Community-Based Participatory Research for Health
Flicker, S., Savan, B., Mildenberger, M., & Kolenda, B. (2008). A snapshot of community-based research in Canada: Who?
What? Why? How? Health Education Research, 23(1), 106–114.
Flicker, S., Travers, R., Guta, A., Macdonald, S., & Meagher, A. (2007). Ethical dilemmas in community-based participa-
tory research: Recommendations for institutional review boards. Journal of Urban Health, 84(4), 478–493. doi:10.1007/
s11524-007-9165-7
Greene, S., Ahluwalia, A., Watson, J., Tucker, R., Rourke, S. B., Koornstra, J.,...Byers, S. (2009). Between skepticism and
empowerment: The experiences of peer research assistants in HIV/AIDS, housing and homelessness community-based
research. International Journal of Social Research Methodology, 12(4), 361–373.
Guta, A., Flicker, S., & Roche, B. (2010). Peer research in action II: Management, support and supervision. Toronto, Canada:
Wellesley Institute.
Guta, A., Wilson, M., Flicker, S., Travers, R., Mason, C., Wenyeve, G., & O’Campo, P. (2010). Are we asking the right ques-
tions? A review of Canadian REB practices in relation to community-based participatory research. Journal of Empirical
Research on Human Research Ethics, 5(2), 35–46.
Israel, B., Schulz, A., Parker, E., & Becker, A. (1998). Review of community-based research: Assessing partnership
approaches to improve public health. Annual Reviews Public Health, 19(1), 173–194.
Jewkes, R., & Murcott, A. (1998). Community representatives: Representing the “community”? Social Science and Medicine,
46(7), 843–858.
LaVeaux, D., & Christopher, S. (2009). Contextualizing CBPR: Key principles of CBPR meet the Indigenous research con-
text. Pimatisiwin, 7(1), 1.
Logie, C., James, L., Tharao, W., & Loutfy, M. R. (2012). Opportunities, ethical challenges, and lessons learned from working
with peer research assistants in a multi-method HIV community-based research study in Ontario, Canada. Journal of
Empirical Research on Human Research Ethics, 7(4), 10–19.
Mikesell, L., Bromley, E., & Khodyakov, D. (2013). Ethical community-engaged research: A literature review. American
Journal of Public Health, 103(12), e7–e14.
Nixon, S. A., Casale, M., Flicker, S., & Rogan, M. (2012). Applying the principles of knowledge translation and exchange to
inform dissemination of HIV survey results to adolescent participants in South Africa. Health Promotion International,
28(2), 233–243.
Oetzel, J. G., Villegas, M., Zenone, H., White Hat, E. R., Wallerstein, N., & Duran, B. (2015). Enhancing stewardship of
community-engaged research through governance. American Journal of Public Health, 105(6), 1161–1167.
Oliver, V. (2013). Healing home: Health and homelessness in the life stories of young women. Toronto, Canada: University
of Toronto Press.
Schnarch, B. (2004). Ownership, control, access, and possession (OCAP) or self-determination applied to research: A critical
analysis of contemporary First Nations research and some options for First Nations communities. Journal of Aboriginal
Health, 1(1), 80–95.
Shore, N., Brazauskas, R., Drew, E., Wong, K. A., Moy, L., Baden, A. C.,...Seifer, S. D. (2011). Understanding community-
based processes for research ethics review: A national study. American Journal of Public Health, 101(S1), S359–S364.
Simonds, V. W., & Christopher, S. (2013). Adapting Western research methods to Indigenous ways of knowing. American
Journal of Public Health, 103(12), 2185–2192.
Strike, C., Guta, A., de Prinse, K., Switzer, S., & Carusone, S. C. (2016). Opportunities, challenges and ethical issues
associated with conducting community-based participatory research in a hospital setting. Research Ethics, pp. 1–9.
doi:10.1177/1747016115626496
Travers, R., Pyne, J., Bauer, G., Munro, L., Giambrone, B., Hammond, R., & Scanlon, K. (2013). “Community control” in
CBPR: Challenges experienced and questions raised from the trans PULSE project. Action Research, 11(4), 403–422.
Tri-Council of Canada. (2010). Tri-Council policy statement 2: Ethical conduct for research involving humans. Retrieved
May 11, 2017, from www.pre.ethics.gc.ca/pdf/eng/tcps2/TCPS_2_FINAL_Web.pdf
6
PART
PROMISING PRACTICES
TO OUTCOMES: CBPR
CAPACITY AND HEALTH
The importance of evaluation and assessment of the added value of equitable participatory
practices among community, agency, other social actors and academic researchers has grown
in this last decade of the consolidation of CBPR and community-engaged research approaches.
An increased number of systematic reviews have identified multilevel outcomes and effective
partnership practices (see Chapter1). Although many of us are part of these national evaluation
efforts, including identifying mixed-methods instruments and measures or metrics of engage-
ment and partnering (see Appendix 10), the caution still exists to recognize the importance of
contexts under which specific partnerships operate. Key questions to consider remain: (1) under
what conditions and contexts do partnerships choose which practices are “best” or promising
236 Part 6
in their experience, and (2) how will their chosen practices affect research designs and interven-
tions to produce their desired (and also possibly unintended) outcomes within communities and
the academy?
This section of the book provides three chapters on research and evaluation methodologies,
measures, and outcomes as a result of using CBPR approaches. Chapter17 by John G. Oetzel and
colleagues presents the next stage of the national Research for Improved Health (RIH) study to
identify measures and analyses of partnering practices and outcomes, using constructs from the
four domains of the CBPR model introduced in Chapter6. With a mixed methodology of Inter-
net surveys of two hundred partnerships and seven diverse case studies, the authors present
empirical data of associations of promising practices with outcomes, as well as options for how
other partnerships can adapt the model and measures for their own evaluations.
Chapter18 by Noelle Wiggins and colleagues compares and contrasts participatory eval-
uation with CBPR using two community health worker (CHW) initiatives, one in the United
States and one in Nicaragua. The authors present a transformational participatory evaluation
approach, as closest to CBPR’s philosophy, which also incorporates decolonizing approaches to
evaluation. They offer a cycle of participatory evaluation steps that enables all stakeholders,
including the CHWs, to participate in all stages of the evaluation, including interpreting and
dissemination of data for health improvements in their communities, and they end with lessons
learned to ensure authentic participation of community.
Chapter19 by Lorenda Belone, Derek M. Griffith, and Barbara Baquero takes a personal
approach to outcomes by describing the role of CBPR training and research opportunities
as pipelines to their own academic success as faculty members of color. These opportunities
enabled their success in integrating their academic careers with a life calling of service to com-
munities. Personal outcomes for participants in the research process, whether from the academy
or community, are important human development outcomes, and, in this case, they served to
strengthen the sustainability of CBPR within the larger research enterprise at the same time as
diversifying the academy.

17
CHAPTER
EVALUATION OF
CBPR PARTNERSHIPS
AND OUTCOMES
LESSONS AND TOOLS FROM THE RESEARCH
FOR IMPROVED HEALTH STUDY
JOHN G. OETZEL, BONNIE DURAN, ANDREW SUSSMAN, CYNTHIA PEARSON,
MAYA MAGARATI, DMITRY KHODYAKOV, AND NINA WALLERSTEIN
AS NOTED IN previous chapters, community-based participatory research (CBPR) is a popular
approach that uses equitable research partnerships to engage in community health improvement
and reduce health inequities when working with underserved communities, Indigenous commu-
nities, communities of color, and other communities facing inequities in health or experiencing
mistrust for past research issues (Atalay,2010; Lorway et al.,2013). Despite the popularity of
CBPR in practice, the science of CBPR has lagged behind. Although CBPR can and should
be implemented based on social justice values (rather than simply utilitarian values) (Trick-
ett,2011), there is also a need to establish the conceptual and empirical rationale for its use. The
development of several frameworks, the CBPR conceptual model (Chapter6), a logic model
emphasizing partnership synergy (Khodyakov et al.,2011) and a realist review of CBPR research
(Jagosh et al.,2012), have advanced the theorizing and conceptual explanation of CBPR.
238 Community-Based Participatory Research for Health
The empirical rationale for CBPR is starting to grow as well. As noted in Chapter1, recent
reviews demonstrate the positive impacts of community-engaged research (CEnR) in general
and CBPR in particular for health outcomes (Cyril, Smith, Possamai-Inesedy, & Andre,2015;
O’Mara-Eves et al.,2015). These reviews provide strong justication for the benet of CBPR
and some evidence of its impact. At the same time, these reviews do not provide sufcient
information about why CBPRs lead to health outcomes or how to evaluate the various elements
of CBPR to improve partnership capacity and partnering. Further, effective evaluation requires
a range of quantitative and qualitative tools. There are a number of evaluation frameworks in the
literature, and yet some of the tools in these frameworks lack evidence of reliability and validity
(Sandoval et al.,2012). (See Appendix 10 for further tools.)
The purpose of this chapter is twofold. First, we share the methods and measures that we
developed in the Research for Improved Health (RIH) study. The quantitative and qualitative
measures are valid and reliable evaluation tools that partnerships and outside evaluators can use
toassess partnering process and outcomes. Second, we present evidence from the RIH study
linking CBPR processes and contexts with outcomes, including CBPR capacity and system out-
comes, community transformation, and health improvement. The chapter begins with a discussion
of a previous different project that served as foundational for the evaluation tools and outcome
data presented in the RIH study. We then discuss specic evaluations tools and outcomes of the
RIH study and conclude by discussing how these tools can be used for evaluation purposes.
STUDY OF PARTNERSHIP SYNERGY
As part of the NIMH Partnered Research Center for Quality Care (PRC) in Los Angeles, a team
of academic and community partners conducted the Partnership Evaluation Study (PES), which
explored the process and outcomes of community engagement (CE) in research (Khodyakov
et al.,2011,2013). PES was conducted in 2010, and at that time, there was no rigorous empirical
research that measured the extent to which community partners were engaged in the process of
conducting research or evaluated the impact CE has on outcomes of partnered research projects.
Grounded in the early conceptual model of community-academic partnerships (Wallerstein &
Duran, 2010; Wallerstein et al., 2008), an existing measure of partnership synergy (Lasker,
Weiss, & Miller,2001; Weiss, Anderson, & Lasker,2002) was supplemented with newly devel-
oped measures of CE in research and outcomes of partnered research projects.
Partnership synergy is an outcome of partnership functioning that facilitates the accomplish-
ment of more than what can be done by individual partners on their own (Lasker et al.,2001;
Weiss et al.,2002). On partnered research projects, academics contribute their research exper-
tise and knowledge of evidence-based interventions, whereas community partners bring their
understanding of community needs, local sociocultural contexts, and knowledge of community-
and practice-based evidence. By beneting from complementary strengths and areas of exper-
tise, community-academic collaborations develop partnership synergy, which ultimately results
in more comprehensive and sustainable programs as well as stronger relationships with the
community at large. In a realist review of twenty-three partnerships, Jagosh et al. (2012) also
found the importance of partnership synergy as a middle-range theory to explain the contri-
bution of partnering processes to outcomes of culturally appropriate research, sustainability,
capacity, and system changes. (See Appendix 6 for discussion of realist review methodology.)
Evaluation of CBPR Partnerships and Outcomes 239
The rst step in the PES was the development of a logic model to link partnership charac-
teristics (e.g., the extent of CE in research, partnership size, and duration); partnership func-
tioning (e.g., leadership, decision making, efciency, management, resources, and challenges
encountered); partnership synergy; and partnership outcomes at a community and policy level
(e.g., improved access and improved health) and personal level (e.g., professional development).
A series of semi-structured interviews with academic and community leaders working on thirty-
nine out of seventy-two mental health and substance abuse partnered projects afliated with the
PRC were conducted (details available in Khodyakov et al.,2011,2013).
The primary goal of the interviews was to develop measures of CE in research and out-
comes of partnered research projects to be used in the survey, which led to two approaches to
measuring CE in research: (1) the community engagement in research index (CERI), which
offers a multidimensional view of community participation in the research process, and (2) a
three-model approach that differentiates among the levels of community participation (Khodya-
kov et al.,2013). The CERI included research steps from grant proposal writing and conduct-
ing background research; to developing sampling procedures and recruitment; to implementing
the intervention and designing interview and survey questions, collecting, analyzing, and inter-
preting study ndings; to dissemination. Then, three partnership models were created (Baker,
Homan, Schonhoff, & Kreuter,1999): (1) community partners only provide access to study
participants and are not engaged in the research aspects of the project, (2) community part-
ners are consulted and act as advisors but do not make any research-related decisions, and (3)
community partners engage in the research activities. These three models became the response
set for the activities in the CERI (1 = “Community partners did not participate in this activity”;
2 = “Community partners consulted on this activity”; 3 = “Community partners were actively
engaged in this activity.”). The CERI results in an index by summing the scores across the
twelve research activities and dividing by three (4 = low engagement to 12 = high engagement).
The study ndings suggested that more active engagement of community partners in
research is positively associated with a number of perceived community- and policy-level out-
comes, including more sustained partnerships among agencies, policy changes, and public rec-
ognition and acknowledgment from local policy makers and government ofcials. Moreover,
partnerships with higher levels of community engagement in research are more likely to con-
tribute to the perception of positive professional development of their members, whereas larger
partnerships with higher levels of synergy may positively affect partners’ perception of personal
capacity. Finally, larger projects that actively engage community partners in research and have
higher levels of synergy may yield higher levels of perceived political impact and a greater
number of perceived community- and policy-level outcomes (Khodyakov et al.,2011).
Given the strength of these ndings and the quality of measurement, the CERI, partnership
synergy, partnership process measures, and several outcome measures were included in the RIH
study. RIH researchers did change how we used the CERI by focusing on three different dimen-
sions of what we called community involvement in research.
RIH STUDY METHODS
The research design for the RIH was a mixed-method, iterative integration design; we describe
this as an Indigenous-transformative framework with full details found elsewhere (and more
240 Community-Based Participatory Research for Health
briey in Chapter6) (Hicks et al.,2012; Lucero et al.,2016; Oetzel, Zhou, et al.,2015; Pearson
et al.,2015). The sampling frame for the study was developed in the rst instance with a series
of steps. A computer algorithm was used to screen 103,250 federally funded extramural proj-
ects funded in 2009 to identify projects that involved CEnR or CBPR. Staff review of abstracts
provided further validation of the inclusion of projects. The projects were research-based proj-
ects from a range of health topics and funding agencies. From this search, 333 projects were
identied. Among the invited projects, only 294 actually involved CBPR or CEnR (based on
self-identication or rescreening of nonparticipating abstracts).
From this sample, we initiated the two key data collection elements: qualitative case study
and cross-sectional survey. We selected seven partnerships for an in-depth qualitative case
study. The case studies were included to account for complexity in contextual, dynamic, and
temporal features and processes of the conceptual model that the cross-sectional survey could
not capture. The seven cases were selected (see Chapter6) to include successful partnerships
from a range of health topics and ethnic-racial communities. The data collection involved two
research team members visiting partnerships and in particular the community where the project
was located. During these visits, ten to fteen interviews and one to two focus groups were con-
ducted with team and advisory board members. Further, observations of meetings and review of
documents were completed. Three case studies were completed prior to initiating the survey, so
we also used these data to inform and change the cross-sectional survey, particularly when no
previous measures could be identied. The two components continued in parallel until the com-
pletion, at which time the qualitative and quantitative ndings informed each other and provided
triangulation of conclusions.
The cross-sectional survey involved a two-stage sample. First, two hundred (68.0 percent)
of the principal investigators (PIs) or project directors (PDs) participated in a key informant
survey (KIS) during the latter part of 2011. The KIS asked the PIs to identify project character-
istics and also up to four partners (one academic and three community) to participate in the sec-
ond survey, the community engagement survey (CES). The PIs identied 404 partners, and 312
completed the survey. Of the 200 eligible PIs, 138 completed the CES. These 450 participants
represented 82 percent of the total projects in which a KIS was completed and 56 percent of
the original 294 projects. In addition, the PIs and PDs were invited to complete the CES and to
nominate community partners to complete the CES. All data were collected via DatStat Illume,
a web-based survey platform.
All research processes and measures were developed in consultation and collaboration with
two advisory groups of academic and community partners with expertise in CBPR. One group
focused on the qualitative measures and research design, and the other group focused on the
quantitative elements. These steps allowed for the creation of items with face and content validity
consistent with the CBPR conceptual model. The specic measures and tools are described in the
following three sections, and URLs for these and other tools can be found in Appendix 10 and in
http://cpr.unm.edu/research-projects/cbpr-project/research-for-improved-health.html.
QUALITATIVE MEASURES AND TOOLS
We employed a multi-method data collection strategy during the case studies. The purpose of
this approach was to triangulate varied sources of data from different stakeholders as well as
Evaluation of CBPR Partnerships and Outcomes 241
create more visually engaging and interactive opportunities to ensure participation from part-
nership members who may have different preferences for sharing their views. The qualitative
tools involved two primary components: interview guides and historical time lines.
The qualitative interview guides—individual and focus group—were developed following
an iterative process of review and renement with multiple study team stakeholders. The CBPR
conceptual model grounded this effort because it provided a foundational base from which to
create relevant questions across the domains. Given that our goal was to conduct interviews and
focus groups with a diverse range of partnership participants—university as well as community
members—we recognized that the interview guides needed to be exible and adaptive to the
respondents’ specic role. The overarching purpose of the guides was to link stakeholder per-
spectives and actions to broader historical, cultural, and political contexts, partnership func-
tioning, group dynamics, specic implementation strategies, and a range of potential outcomes
(e.g., personal, health, and policy).
A common and effective strategy in the development of qualitative interview guides is to
begin by eliciting narrative reection and stories through personal engagement and experi-
ence. We recognized that interviewees across the partnership spectrum may not have engaged
in a process of considering their own personal roles in these projects or how such efforts have
been inuenced by larger sociohistorical and interactional forces. Therefore, questions in the
domains concentrated on probing descriptions of existing conditions and partnership dynamics
derived from actual experience rather than focusing on more abstract associations among model
components. Once nal draft guides were developed, we conducted a series of pilot interviews
with CBPR partnership members connected to our research team as a way to test and modify
the guides. We reviewed these initial transcripts as a team to modify the content and sequencing
of questions until we reached consensus on a nal version. Individual interviews were con-
ducted with a broad cross-section of partnership members, and focus group sessions were held
with typically a core group of academic and community members, emphasizing group dynamic
processes over individual perceptions and roles.
During a previously agreed time during the case study visit, we gathered academic and
community partnership members together and guided them through a historic time line exercise.
A research team moderator instructed the group to consider the most salient events that have
inuenced the historical development of the partnership. We informed them that there was no
predetermined start or end date to this time line. Participants were free to consider past histor-
ical events as relevant ranging from broader political-economic structures that inuence social
conditions, receipt of grant funding, or the arrival or departures of partnership members. To
enhance the experience, we typically gave people a large piece of butcher paper (or several
pieces taped together) to either lay on a table or tape to a wall (3 ft × 9–12 ft) and handed out
markers. There was very little direct research team facilitation for this exercise, and after some
initial hesitation, participants began interacting with each other about specic events and dates
while reecting further on their partnership history. Appendix 7 displays the historical time line
(also known as the River of Life tool).
We found this exercise to be a rich complement to other sources of data collection. In some
case studies, participants began the time lines several decades before the present time period and
a few traced the origins of their collective interests back well over a century. For example, one
case study site identied slavery and the civil rights movement as foundational to partnership
242 Community-Based Participatory Research for Health
activities. Following the completion of the time line (which usually took about an hour), we
then moderated a semi-structured focus group to explore the items and events featured on the
scroll. These sessions were highly interactive because they provided an opportunity for partner-
ship members to learn from each other and to assess where the partnership came from and what
progress has been made.
KEY INFORMANT SURVEY
Guided by the CBPR conceptual model, we rst identied project-level measures that included
project descriptors and structural features that could be collected via self-report from the PI or
abstracted from the RePORTER database. We obtained measures from a library of available
CBPR measures that mapped onto constructs and domains represented in the CBPR conceptual
model (Pearson et al.,2011).
Project descriptive measures were primarily gathered from RePORTER and included
funding for specic areas of research, conditions, or diseases; specic organizations; specic
geographical regions; application success rates; and information on the researcher (PI) and
his or her organization, project details including abstracts, key words, start and end dates, and
type of award (R: research, K: career development, U: center grants) mechanisms used by the
National Institutes of Health, and so on.
Structural features included measures to address the nature of agreements among partners
and the ways that the partners work together. They included the following elements:
■ Project features (twelve items: for example, length of partnership and condence in goal
achievement)
■ Resource control and power sharing (four items: for example, who hires personnel and
decides how the resources are shared)
■ Research integrity (three items: for example, research ethics training and guidelines on con-
dentiality)
■ Formal agreements (seven items: for example, memoranda of understanding or written agree-
ment and the contents of those agreements)
■ Formal trainings or substantial discussions (eight items: for example, training about cultural
humility, privilege, and power and conict resolution)
■ Partnership roles and involvement (thirteen items: for example, CERI items with one
new item).
■ Research outcomes (four items: for example, papers in press or published, additional research,
or funding)
COMMUNITY ENGAGEMENT SURVEY
The CES measures academic and community partners’ perceptions of partnership context,
processes, research design, and outcomes as guided by the CBPR conceptual model. Overall,
there were twenty-two measures with 101 items included in the CES. For the partnership
context domain, the CES included (1) a measure of the capacity of the partnership to meet its
aims; and (2) a measure of the degree of trust at the beginning of the partnership.
Evaluation of CBPR Partnerships and Outcomes 243
For the partnership processes domain, the CES contained (1) four measures of structural and
individual features and (2) eight measures of relational dynamics. The structural and individual
measures comprised the following: bridging social capital, alignment with CBPR principles-
partner focus, alignment with CBPR principles-community focus, and partner values (degree of
agreement with the mission of the project). Relational dynamics included the following mea-
sures: cooperation, participation, respect, trust, inuence, participatory decision making, lead-
ership effectiveness, and resource management.
For the intervention and research design domain, the CES had a measure of partnership syn-
ergy from PES and measures of community involvement in background research, community
involvement in data collection, and community involvement in analysis and dissemination (the
last three derived from the CERI). For the partnership outcomes, we included four measures of
systems and capacity changes: individual capacity building, agency capacity building, shared
power relations in research, and sustainability. We also provided two measures of long-term
outcomes: community transformation and community health improvement.
We conducted a rigorous assessment of the psychometric properties of these scales (Oet-
zel, Zhou, et al.,2015). Conrmatory factor analysis demonstrated that the twenty-two mea-
sures have strong factorial validity, and Pearson correlation analysis established convergent
and discriminant construct validity. Internal consistency was strong, with eighteen of twenty
measures with multiple items achieving at least a .78 Cronbach’s alpha (two measures were
single items).
Finally, we also developed a measure of culture-centeredness based on the CES measures
and qualitative methods (Wallerstein et al., under review). Ensuring cultural t of research
methods, design, and co-development of interventions is necessary for meaningful research
outcomes, research integrity, ethical conduct, external validity, and effectiveness to enhance
health equity. The culture-centered approach identies communication processes that mar-
ginalize certain communities and suggests three core constructs that challenge this marginal-
ization by validating communication knowledge: community voice and agency (inclusion of
community perspective in dening problems and identify solutions), reexivity (awareness of
unstated power and privilege), and structural transformation (changing rules and resources)
(Dutta,2007). The measure includes seven subscales related to these three core constructs.
KEY OUTCOMES
The quantitative and qualitative analyses have been conducted in an integrative manner and
aligned with the CBPR conceptual model. We organize the ndings on four key areas: (1) con-
ceptualizing outcomes, (2) promising practices, (3) context and culture, and (4) structure and
governance. A fth key evaluation area was the testing of the conceptual model itself, using
structural equation modeling, which is presented in Chapter6.
Conceptualizing Outcomes
Our qualitative and quantitative analyses identied a series of outcomes, reecting different
levels of change and values. The initial desired outcome for a partnership might be the health or
research outcome as identied in the specic objectives of a project or grant. Yet, CBPR proj-
ects have a potentially much greater breadth of outcomes, including advances toward social
244 Community-Based Participatory Research for Health
justice goals of reduced inequities and knowledge democracy. Qualitative analyses from the
case studies showcased this range. Case study participants noted the importance of community
and system transformation as core desired intermediate and long-term outcomes of their part-
nership. These outcomes related to changes in the policy environment, that is, greater recogni-
tion of the community partners’ strengths as sources of data and as advocates with inuence,
specic policy changes (e.g., local ordinance enacted by policy makers based on partnership
data and advocacy), or improved services and programs. At an intermediate level, case studies
identied outcomes in the university environment through changes in IRB processes, for
example, as well as community capacity outcomes, such as increased skills in partner agencies
related to research. On a personal level, we found that involvement in partnership activities
led to positive changes for community members, such as new motivations for pursuing further
education or new skills to enhance personal and professional goals. Through the historical time
line, we also found greater interest in evaluating the partnership itself in terms of which prac-
tices led to greater partnership synergy and effectiveness.
These ndings relate closely with our conceptualization of quantitative outcomes at three
different levels: (1) short term, (2) intermediate, and (3) long term (Oetzel, Zhou, et al.,2015).
Short-term outcomes are the immediate output of partnership dynamics and include partner-
ship synergy. Intermediate outcomes consist of system and capacity outcomes of individual and
agency capacity building, shared power relations in research, and sustainability. The long-term
outcomes are the community transformations, such as improved programs, policies, and ser-
vices, and improving the status of the community health issue being addressed.
Promising Practices
One of our specic aims of the RIH study was to identify a set of promising practices for
CBPR. These promising practices are contextual and process variables for partnering that are
associated with the three different types of outcomes. Building on community consultations
(Belone et al.,2016), we categorize these promising practices in congruence with our model:
context (partnership has capacity to meet aims); partnership structures (which ensure bridg-
ing social capital, value alignment, and power sharing through written agreements and control
of resources); relationships (mutual dialogue, inuence, ethical management, and trust); and
research-intervention (ensuring community involvement in all research phases).
We completed a multilevel multiple regression analysis of the KIS and CES data to identify
which of these promising practices is associated with each of the specic outcomes including
a composite outcome (a combination of the seven outcomes). These practices accounted for
21 to 67 percent of the variance in the specic outcomes. For example, the following specic
constructs were associated with the composite outcome: (1) having a formal written agreement,
(2) having shared academic and community control of resources, (3) a partnership with strong
capacity, (4) following CBPR principles, (5) community involvement in multiple stages of the
research, (6) partners having inuence on the project, (7) effective leadership, and (8) effective
resource management (Duran et al.,under review).
The qualitative analysis also explored promising practices, particularly related to partner
dynamics. We specically sought examples of how partnerships built and nurtured rela-
tionships of trust and used a trust typology to categorize varying stages of this process (see
Chapter5). Trust is an essential component of partnership synergy yet remains a fragile and
Evaluation of CBPR Partnerships and Outcomes 245
ongoing dynamic that requires nurturing in even experienced partnerships. Other aspects of
group dynamics included strategies for collaborative decision making and how partnerships
managed and distributed relationships of power. Finally, we identied the importance of “bridg-
ing characteristics” of certain partnership members (often academic staff members who come
from similar communities that the partnership works with). Bridging social capital was seen as
an essential quality given the importance of effective communication and “translation” across
the academic-community boundary and across ongoing structural barriers of institutional rac-
ism and privileged academic knowledge (see Chapter4).
Context and Culture
Perhaps the most overarching nding in the qualitative analysis related to the social and histor-
ical context in which partnerships developed and ultimately drove priorities and goals (Muham-
mad et al., 2015). Community members cited a deep historical awareness of the processes
leading to disparities and current needs. Indeed, without exception, all of the intervention and
policy projects we encountered were directly linked to these dynamics and were rooted in
cultural knowledge. Although the case studies varied across a range of sociopolitical climates,
we found that there was a high degree of recognition regarding how contextual factors inu-
enced project and partnership decisions. The quantitative analysis included limited contextual
elements because context is hard to measure across partnerships (quantitative exceptions were
partnership capacity and trust at beginning of partnership).
We also identied culture-centeredness as a central feature of partnership project devel-
opment and adhering to core CBPR principles (Muhammad et al., 2015; Wallerstein et al.,
under review). Themes of cultural revitalization and identity were consistently reported across
the case studies. In some cases, the importance of culture-centeredness related to grounding
program and research materials within linguistic and social norms of communities, whereas
in other settings, recognition of historical and structural racism served as a common basis to
function as a social movement aimed at achieving forms of justice (Devia et al.,2017). The
lack of culture-centeredness would be a signicant deterrent to positive group dynamics and
mutuality in academic-community member relationships. Our measure of culture-centeredness
validates this conclusion because it was moderately correlated with group dynamics constructs.
Further, the measure was also moderately correlated with intermediate and long-term outcomes.
Structure and Governance
Another major thematic focus included processes of structure and governance. We were inter-
ested in understanding how projects were conceptualized and approved as well as in identifying
the relevant advisory structures for decision making and reporting. The issue of governance was
particularly salient in Native (American Indian, Alaska Native, or Native Hawaiian) partner-
ships given the central role of such processes as a fundamental basis for engaging in partner-
ship efforts and respecting Native sovereignty. In non-Native partnerships, we observed other
oversight processes, though these were typically less formal and based on the context of the
partnership itself.
Our quantitative ndings showed that Native-serving projects receive less funding com-
pared to other communities of color and multiple race–unspecied groups (Pearson et al.,
2015). However, the research outputs in Native communities were no different than those in
246 Community-Based Participatory Research for Health
other communities. This may be explained by the fact that Native communities were more
likely to have a written agreement, and perhaps these protected the resources and time of the
community partners.
A key aspect of governance is the stewardship of projects (Oetzel, Villegas et al.,2015).
Much of governance of research projects focused on research ethics. However, this is insuf-
cient oversight of the research project. Stewardship means ensuring that the research project is
administered appropriately to meet specic aims and is accountable to community values and
priorities. Our research explored the approval of a project as a form of stewardship. We found
that projects approved by a tribal government or health board were more likely to have control
of resources, written agreements, and agreements about publishing compared to other types of
approval, such as advisory boards, agencies, or individuals. These steps help to ensure that the
project is well resourced and thus benets the community.
MEASURES AND TOOLS FOR EVALUATION
Collectively, all of these ndings demonstrate a robust set of measures and tools that identify
key and promising CBPR practices. The constructs we have measured have empirical evidence
of relevance for the various outcomes. Further, the combined qualitative and quantitative results
provide a level of triangulation and also complementarity.
We end the chapter with recommendations on how to use the model as a planning and quality
improvement and reection tool for ongoing evaluation of community-engaged partnerships in
innovative and simple ways. For example, community-academic partnerships can use these valid
and reliable measures, with qualitative interview guides, to self-assess their partnership practices
and outcomes in order to strengthen their partnerships to achieve desired outcomes. Partners can
use their own data results to choose the constructs they perceive best t their project and partner-
ship needs by (1) assessing where their partnership stands for a particular construct of interest
compared to national community-engaged project data (e.g., based on empirical results from
our cited studies) and prioritizing strategies to address that particular partnering process and (2)
evaluating the quality of the measures in relation to other constructs within their own partnership
(e.g., are higher levels of participation related to higher capacity building?).
To use the model as a visioning tool for planning or to create an evaluation strategy, there
are inductive and deductive approaches. Inductively, partnerships can use the four domains
(context, partnership processes, intervention and research, and outcomes) as the starting point
to drive their planning, beginning from their own interests and contexts. For example, part-
ners could rst reect on their “desired outcomes,” reecting on which constructs resonate and
which need to be changed. They then can return to contexts and continue with partnership
processes and intervention and research issues, identifying constructs that resonate or new ones.
The result is an adapted model specic to their partnership. If the partnership is just starting,
the same approach would lead to documenting desired outcomes, then brainstorming issues in
their context, their desired strategies for creating equitable relationships, the potential impact on
research design, and revisiting outcomes (see http://cpr.unm.edu/research-projects/cbpr-project/
facilitation_tools.html).
A deductive approach might start with a set of outcomes the partnership is interested in
(e.g., agency capacity building and shared power relations in research). Examining the identied
Evaluation of CBPR Partnerships and Outcomes 247
promising practices from RIH (Duran et al.,under review), there are a set of processes associ-
ated with each of these outcomes. The partnership can administer these measures to see where
they currently stand and whether there are areas for growth.
In 2015, we were invited by Mayo Clinic partners to work with the ten-year-old Roches-
ter Healthy Community Partnership, a collaboration between local community organizations
and health researchers in Rochester, Minnesota to undertake such an application of our work.
Through an iterative process of meetings and document review, they created their own version
of the model (http://cpr.unm.edu/research-projects/cbpr-project/rhcp-cbpr-model-nal-ppt.pdf)
and modied existing instruments—individual and focus group guides, historical time line, and
surveys—to evaluate partnership functioning and future goals. Our RIH instruments served as
templates representing a range of domains that a partnership could select from and adapt to
their needs and priorities. Analysis of eleven interviews and thirty-six surveys led to community
voices reports of core areas of strength and challenge (comparing their response to RIH national
averages) and of questions for the partnership to reect on as they use the evaluation for their
future directions. To use the model as a visioning tool for evaluating existing partnerships, also
see http://cpr.unm.edu/research-projects/cbpr-project/facilitation_tools.html.
We are fortunate to have received further funding (2015–2020) for the next iteration of
our project. In this new R01 funding called Engage for Equity (E
2
), from the National Insti-
tute of Nursing Research, we are revising, improving, and translating into Spanish our KIS
and CES measures. For the KIS, we have developed new measures of stewardship, community
organizing capacity to complement community partnership capacity, academic practices, and
advisory boards. For the CES, we enhanced measures of inuence, culture centeredness, short-
ened many relational measures while also adding reexivity, time commitment, satisfaction,
and personal costs.
We are also developing a two-day workshop and web-based tools for partnerships at var-
ious stages on how to engage in self-assessment and reection to strengthen their practice and
achieve their own goals. The underlying assumption of the workshop and tools is that reexivity
(using Freirean empowerment methodologies) about one’s partnership practices strengthens
equitable practices, enabling partners to be more effective in reaching their goals. The tools
for reexivity, including evaluation quantitative measures, qualitative guides, and other
resources, are being tested and rened and then will be made available to partnerships for use
and adaptation to their own priorities and contexts (http://cpr.unm.edu/research-projects/cbpr-
project/index.html). These tools are also complemented by the empowerment, social participa-
tion, and CBPR curriculum, available in English, Spanish, and Portuguese (http://cpr.unm.edu/
curricula--classes/empowerment-curriculum.html).
In conclusion, this chapter, along with tools in Appendices 7, 10, and 11, identied
methods, measures, and tools from RIH (the rst national study of two hundred federally
funded partnerships) that are useful for evaluation of community engagement, which can
be started at baseline and maintained over time. We reported some of the key ndings and
psychometric properties to support the CBPR conceptual model as a guide for evaluation.
These ndings illustrate demonstrable outcomes of CBPR contexts and partnering practices
that together can lead to enhanced recognition of the power of community and academic
knowledge working together to reach specic grant goals as well as the broadest goal of
health equity for all.
248 Community-Based Participatory Research for Health
QUESTIONS FOR DISCUSSION
1. Think about your community and imagine a community-engaged intervention being done
there (or think about an actual intervention you have read about or experienced). How
would you suggest you evaluate that project?
2. Imagine you are a member of a participatory research project. How would you go about
using the tools and methods presented here? How would you use them to engage in critical
self-reection? How would you ensure that the evaluation process is participatory?
ACKNOWLEDGMENTS
The research described in this chapter was supported by NARCH: (U261HS300293;
U261IHS0036-04-00), with Indian Health Service in partnership with the National Insti-
tute of General Medical Sciences, National Institute of Minority Health and Health Dispar-
ities, National Institute on Drug Abuse, National Center for Research Resources, Ofce of
Behavioral Social Sciences Research, National Cancer Institute, and Health Resources Services
Administration. Engage for Equity (1R01NR015241-01A1) is funded by the National Insti-
tute of Nursing Research. We thank members of each research team, the think tank, and the
academic and community partners who participated in the surveys and case studies.
REFERENCES
Atalay, S. (2010). “We don’t talk about Catalhoyuk, we live it”: Sustainable archaeological practice through community-
based participatory research. World Archaeology, 42, 418–429.
Baker, E., Homan, S., Schonhoff, R., Sr., & Kreuter, M. (1999). Principles of practice for academic/practice/community
research partnerships. American Journal of Preventive Medicine, 16(3), 86–93.
Belone, L., Lucero, J., Duran, B., Tafoya, G., Baker, E., Chan, D., et al. (2016). Community-based participatory research
conceptual model: Community partner consultation and face validity. Qualitative Health Research, 26, 117–135.
Cyril, S., Smith, B. J., Possamai-Inesedy, A., & Andre, M.N.R. (2015). Exploring the role of community engagement in
improving the health of disadvantaged populations: A systematic review. Global Health Action, 8, 1–12.
Devia, C., Baker, E., Sanchez-Youngman, S., Barnidge, E., Golub, M., Motton, F., Muhammad, M., Ruddock, C., Vicuña,
B., & Wallerstein, N. (2017). CBPR to advance social and racial equity: Urban and rural partnerships in black and Latino
communities. BMC International Journal of Health Equity, 16, 17. doi:10.1186/s12939-016-0509-3
Duran, B., Oetzel, J. G., Pearson, C., Magarati, M., Zhou, C., Villegas, M., & Wallerstein, N. (under review). Promising prac-
tices in community-based participatory research: Evidence from a national study. Progress in Community Health Partner-
ships: Research, Education, and Action.
Dutta, M. J. (2007). Communicating about culture and health: Theorizing culture-centered and cultural sensitivity approaches.
Communication Theory, 17, 304–328.
Hicks, S., Duran, B., Wallerstein, N., Avila, M., Belone, L., Lucero, J., et al. (2012). Evaluating community-based participa-
tory research to improve community-partnered science and community health. Progress in Community Health Partner-
ships: Research, Education, and Action, 6, 289–299.
Jagosh, J., Macaulay, A. C., Pluye, P., Salsberg, J., Bush, P. L., Henderson, J., et al. (2012). Uncovering the benets
of participatory research: Implications of a realist review for health research and practice. The Milbank Quarterly,
90, 311–346.
Khodyakov, D., Stockdale, S., Jones, A., Mango, J., Jones, F., & Lizaola, E. (2013). On measuring community participation
in research. Health Education & Behavior, 40, 346–354.
Evaluation of CBPR Partnerships and Outcomes 249
Khodyakov, D., Stockdale, S., Jones, F., Ohito, E., Jones, A., Lizaola, E., et al. (2011). An exploration of the effect of
community engagement in research on perceived outcomes of partnered mental health services projects. Society and
Mental Health, 1(3), 185–199.
Lasker, R., Weiss, E., & Miller, R. (2001). Partnership synergy: A practical framework for studying and strengthening the
collaborative advantage. The Milbank Quarterly, 79, 179–205.
Lorway, R., Thompson, L. H., Lazarus, L., du Plessis, E., Pasha, A., Fathima Mary, P., et al. (2013). Going beyond the clinic:
Confronting stigma and discrimination among men who have sex with men in Mysore through community-based partici-
patory research. Critical Public Health, 24(1), 1–15.
Lucero, J., Wallerstein, N., Duran, B., Alegria, M., Green-Moten, E., Israel, B. A., et al. (2016). Development of a mixed
methods investigation of process and outcomes of community-based participatory research. Journal of Mixed Methods
Research. doi:10.1177/1558689816633309
Muhammad, M., Wallerstein, M., Sussman, A. L., Avila, M., Belone, L., & Duran, B. (2015). Reections on researcher iden-
tity and power: The impact of positionality on community-based participatory research (CBPR) processes and outcomes.
Critical Sociology, 41, 1045–1063.
O’Mara-Eves, A., Brunton, G., Oliver, S., Kavanagh, J., Jamal, F., & Thomas, J. (2015). The effectiveness of community
engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health, 15(1), 1352.
Oetzel, J. G., Villegas, M., Zenone, H., White Hat, E. R., Wallerstein, N., & Duran, B. (2015). Enhancing stewardship of
community-engaged research through governance. American Journal of Public Health, 105(6), 1161–1167.
Oetzel, J. G., Zhou, C., Duran, B., Pearson, C., Magarati, M., Lucero, J., Wallerstein, N., Villegas, M. (2015). Establishing the
psychometric properties of constructs in a community-based participatory research conceptual model. American Journal
of Health Promotion, 29, e188–e202.
Pearson, C., Duran, B., Lucero, J., Sandoval, J., Oetzel, J., Tafoya, G., Belone, L., Avila, M., Martin, D., Wallerstein, N., &
Hicks, S. (2011). CBPR variable matrix: Research for improved health in academic/community partnerships. CES4Health.
info. Retrieved from http://ces4health.info/nd-products/view-product.aspx?code=FWYC2L2T
Pearson, C., Duran, B., Oetzel, J., Magarati, M., Villegas, M., Lucero, J., & Wallerstein, N. (2015). Research for improved
health: Variability and impact of structural characteristics in federally-funded community engaged research. Progress in
Community Health Partnerships, 9, 17–29.
Sandoval, J. A., Iglesias Rios, L., Wallerstein, N., Lucero, J., Oetzel, J., Avila, M., et al. (2012). Process and outcome con-
structs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education
Research, 27, 680–690.
Trickett, E. J. (2011). Community-based participatory research as worldview or instrumental strategy: Is it lost in translation(al)
research? American Journal of Public Health, 101, 1353–1355.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100, S40–S46.
Wallerstein, N., Oetzel, J. G., Duran, B., Magarati, M., Pearson, C., Belone, L., Davis, J., Dewindt, L., Lucero, J., Ruddock,
C., Sutter, E., Villegas, M., Dutta., M. (under review). Conceptualizing and measuring the culture-centered approach in
community based participatory research. Social Science and Medicine.
Wallerstein, N., Oetzel, J. G., Duran, B., Tafoya, G., Belone, L., & Rae, R. (2008). CBPR: What predicts outcomes? In
M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes (2nd
ed., pp. 371–392). San Francisco, CA: Jossey-Bass.
Weiss, E., Anderson, R., & Lasker, R. (2002). Making the most of collaboration: Exploring the relationship between partner-
ship synergy and partnership functioning. Health Education & Behavior, 29, 683–698.

18
CHAPTER
PARTICIPATORY EVALUATION
AS A PROCESS OF
EMPOWERMENT
EXPERIENCES WITH COMMUNITY HEALTH
WORKERS IN THE UNITED STATES AND
LATIN AMERICA
NOELLE WIGGINS, LAURA CHANCHIEN PARAJÓN, CHRIS M. COOMBE, AILEEN
ALFONSO DULDULAO, LETICIA RODRIGUEZ GARCIA, AND PEI-RU WANG
PARTICIPATORY EVALUATION IS an approach to assessing the strengths and weaknesses
of a program, intervention, or activity and making recommendations for improvements that
involve those directly affected in the evaluation process. It can be considered a subeld of par-
ticipatory research and a discipline in its own right. Given the proper combination of skills, rela-
tionships, conditions, and value orientations, participatory evaluation can produce more valid
and actionable results than more conventional approaches to evaluation, while at the same time
contributing to the empowerment of individuals and communities.
In this chapter, we will provide a solid grounding in the fundamentals of participatory eval-
uation as distinct from research, explore transformative participatory evaluation as most consis-
tent with CBPR, offer a cyclical process for conducting transformative participatory evaluation,
252 Community-Based Participatory Research for Health
and end with two examples of how participatory evaluation is being used in two community
health worker (CHW) programs, one in the United States and one in Nicaragua. Throughout, we
seek to demonstrate how context, skills, and values inuence how we conduct empowerment-
oriented participatory evaluation and research.
WHAT IS EVALUATION?
There are many ways of thinking about the relationship between evaluation and research; the
development of new paradigms for research over the last thirty years has further blurred an
already hazy distinction. Nonetheless, differences remain, and it is important to understand
those differences in order to conduct effective evaluations (Springett & Wallerstein,2008).
Perhaps the key difference between evaluation and research lies within the word evalua-
tion. At its heart, evaluation is a systematic process of assigning value or making a judgment
about a program, intervention, or activity to improve effectiveness or inform decision making
(Morelli & Mataira,2010). Although most practitioners now agree that research is never value-
free, assigning value is not an inherent function of research.
Because evaluation is conducted about a specic program, evaluators must constantly take
context into account, whereas some researchers (though not those inuenced by CBPR) try to
exclude context. Although participatory researchers may have additional goals, a central goal
of research is the creation of new knowledge (and ensuring the external validity of ndings),
whereas a central goal of evaluation is program improvement (and ensuring the internal validity
of ndings) (Levin-Rozalis,2003).
Many of these factors—the explicit goal of assigning value, the inuence of context, the
orientation of service to some group—mean that evaluation is inherently political. Evaluators
therefore must be prepared to understand and mitigate the effects of power, especially participa-
tory evaluators who wish to contribute to empowerment.
WHAT IS PARTICIPATORY EVALUATION?
Cousins and Chouinard (2012) dene participatory evaluation as a range of collaborative
approaches to evaluation “in which trained evaluators work in partnership with [program] stake-
holders to produce evaluative knowledge” (p. 10). This range includes the empowerment eval-
uation pioneered by Fetterman (2000). They contrast these approaches to more conventional
approaches to evaluation in which the evaluator is an outsider who strives to maintain “objec-
tivity” and distance from the program being evaluated. Based on a positivist or post- positivist
worldview, conventional forms of evaluation assume that objective truth exists and can be
known through hypothesis generation and testing. Participatory and collaborative approaches to
evaluation are based on a worldview that “includes the ways in which the people involved with
facts perceive them” and acknowledges that “concrete reality is the connection between subjec-
tivity and objectivity, never objectivity isolated from subjectivity” (Freire,1982, p. 30).
Cousins and Chouinard (2012) divide the range of participatory evaluation into two
principal streams: practical participatory evaluation (P-PE) and transformative participatory
evaluation (T-PE). P-PE is motivated primarily by a pragmatic philosophy and a desire to pro-
duce valid ndings that can be used for program improvement (Brisolara,1998). P-PE is based
Participatory Evaluation as a Process of Empowerment 253
on a democratic pluralist theory of power, which assumes people choose to participate or not
based on free will. By contrast, T-PE grows out of a desire, originally from Latin America,
South Asia, and Africa, to create a just society by challenging unequal power structures. (See
Chapter2 for analogous Northern and Southern participatory research traditions.)
TRANSFORMATIVE PARTICIPATORY EVALUATION
In terms of its historical antecedents and its current uses, T-PE is the participatory evaluation
stream most in line with CBPR and thus is the focus of this chapter. T-PE has two primary
sources: the participatory action research (PAR) work conducted by Colombian sociologist
Orlando Fals-Borda and colleagues in Latin America in the 1960s to 1990s (Fals-Borda & Rah-
man,1991) and the participatory research and evaluation work conducted by Walter Fernandes
and Rajesh Tandon (1981) and colleagues in South Asia during roughly the same period of
time (Hall et al.,2013). These practitioner authors were working in the context of community
development amid the social-political ferment occurring in many parts of the Global South.
Inuenced by thinkers such as Marx, Engels, Gramsci (1971), and Frankfurt School theorists,
these researchers identied mechanisms that maintain inequity and developed research and
evaluation strategies for empowering those most marginalized in society by ceding power to
them and making them the agents, rather than the objects, of research (Brisolara,1998).
Although the historical context of the United States is different, similar disparities of wealth,
power, and control produced the need for participatory research and evaluation, inspiring prac-
titioner academics such as John Gaventa (1980, 1991), along with popular educators at the
Highlander School for Research and Education, such as Myles Horton (2003), to produce par-
ticipatory research that bears many similarities to the approach developed in the Global South.
These approaches are closely connected to the popular education methodology that was sys-
tematized and disseminated by Brazilian educator Paulo Freire (Freire,2003; Wallerstein &
Auerbach,2004; Wiggins,2012; Wiggins et al.,2014). Popular education can help to create an
organizational and community climate that promotes and sustains participatory evaluation and
is proled in the case studies.
Power is a central issue in participatory evaluation generally. In the context of community
health programs and interventions, power takes on added signicance. With lack of power
understood as an overarching disease risk factor (Wallerstein,1992), it stands to reason that the
way to reverse health inequities is to shift and balance power between dominant and oppressed
communities. This occurs through the process of empowerment, which is understood in public
health not as a process that is done by the powerful to or for those lacking power but rather
as a process that communities most affected by inequities do for and with themselves. Public
health studies suggest that empowerment independently predicts better self-reported health and
decreased depressive symptoms (Wallerstein,2006) and that popular education is an effective
way of increasing empowerment and improving community health (Wiggins,2012).
DECOLONIZING PARTICIPATORY EVALUATION
T-PE developed in the Global South as it emerged from colonization and has always been
concerned with the question of who gets to assign value and dene knowledge. In 1991,
254 Community-Based Participatory Research for Health
Rahman wrote of the need to “return to the people the legitimacy of the knowledge they are
capable of producing through their own verication systems, as fully scientic” (p. 15). This
statement pregures the “decolonizing methodologies” of Indigenous scholar Linda Tuhiwai
Smith (1999), who states that “imperialism and colonialism brought complete disorder to colo-
nized peoples, disconnecting them from their histories, their landscapes, their languages, their
social relations and their own ways of thinking, feeling and interacting with the world” (p. 29).
One of the insights of a decolonizing approach is that research and evaluation are critical and
important sites of struggle where colonization and Western science can be challenged and Indig-
enous ways of knowing centralized (Kawakami et al.,2007; Morelli & Mataira,2010; Tuhiwai
Smith,1999; Zavala,2013). A decolonizing approach changes the Western paradigm of evaluation
by challenging the meaning of value, what constitutes value, and whether an intervention should
be improved on or cease to exist. It empowers communities to set evaluation agendas; incorporate
historical, cultural, spiritual, social, environmental, and emotional “data”; and have their evalu-
ation ndings returned to their communities (Kawakami et al.,2007; Morelli & Mataira,2010).
Adopting a decolonizing approach to evaluation represents a return to the roots of transformative
participatory evaluation, as well as a further step toward conducting evaluation from within the
worldview of those most directly affected by the program, intervention, or activity under study.
A PROCESS FOR CARRYING OUT TRANSFORMATIVE
PARTICIPATORY EVALUATION
Similar to CBPR, T-PE is not a specic methodology but rather an approach to evaluation based
on a worldview and set of key principles that guide evaluation design, process, and methods
(Shulha et al.,2016). A number of frameworks have been developed that lay out key steps in
participatory evaluation (Coombe,2012; Fawcett et al.,1996; Fetterman, Kaftarian, & Wan-
dersman,2015; Maltrud, Polacsek, & Wallerstein,1997; Springett & Wallerstein,2008). Rep-
resented initially as sequential steps in Coombe (2012; see Figure18.1), T-PE is in practice a
cyclical, iterative process of learning from the past, applying new understandings to the future,
and cycling back through processes as needed.
Step 1: Identify Purpose and Commit to Participatory Evaluation
Together, those groups and organizations with a vested interest in the program, intervention,
or activity identify the purpose and objectives of the evaluation, decide whether to commit to a
participatory approach, and determine the extent and type of participation by different groups.
Important considerations are the project’s stage of development, past experience with evalua-
tion and research, resources available and needed, and potential benets of carrying out a par-
ticipatory evaluation.
Community, program, and institutional contexts are essential considerations throughout the
process. Contextual factors include power relationships between and among community mem-
bers, funders, outside evaluators, and policy makers; the level at which the program is being
conducted (e.g., local, state, national); and support or lack thereof for the participatory process
from program funders and organizational leaders. In participatory evaluation there is “a role for
program sponsors/funders to support the inquiry in ways that move well beyond the provision
of scal resources” (Cousins & Chouinard,2012, p. 130).

Participatory Evaluation as a Process of Empowerment 255
Step 2: Build the Participatory Evaluation Team
Collaborative partnerships require a shared commitment to equity and adequate time and skills
to establish and maintain relationships, build mutual trust, understand differences, and resolve
conicts. Laying the proper groundwork is critical to success and involves four key tasks:
1. Core team. It is important to formally identify who will be involved, the level and nature of
participation expected, and what personal and institutional resources each partner brings
to the table. Although diverse stakeholder groups can generally produce more credible
and valid ndings, extremely unequal levels of power and privilege among stakeholders
can complicate the goal of transformation. Guiding principles and operating norms can
help address power differentials to foster equitable participation and make the best use of
everyone’s time.
2. Roles and multiple mechanisms for participation. Identifying the roles and strategies for
substantive participation is an important early step for an equitable and high-quality evalu-
ation. In some projects, stakeholders participate in certain stages (e.g., data collection, dis-
semination, etc.) and in others they are involved throughout. Also, depth of participation
can vary over time. To accomplish the goals of T-PE, evaluation facilitators often work in
teams and employ a constellation of skills that include facilitation, popular or liberating
E
v
a
l
u
a
t
e
P
E
p
r
o
c
e
s
s
e
s
a
n
d
o
u
t
c
o
m
e
s
1. Identify purpose
and commit to
participatory
evaluation
2. Build the
evaluation
team
Empowering and
capacity-
building
processes
Transformation
and sustainability
3. Agree on what
to evaluate
4. Create a plan
for collecting
data
5. Collect data
and track
progress
6. Feed rack
and interpret
findings
7. Communicate
results
8. Apply
findings for
action
E
v
a
l
u
a
t
e
P
E
p
r
o
c
e
s
s
e
s
a
n
d
o
u
t
c
o
m
e
s
u
t
c
o
m
u
a
a
t
t
e
1. Identify purpose
and commit to
participatory
evaluation
2. Build the
evaluation
team
Empowering and
capacity-
building
processes
Transformation
and sustainability
3. Agree on what
to evaluate
4. Create a plan
for collecting
data
5. Collect data
and track
progress
6. Feedback
and interpret
findings
7. Communicate
results
8. Apply
findings for
action
FIGURE 18.1 Key Steps in Participatory Evaluation Process
256 Community-Based Participatory Research for Health
education, team building, negotiation, conict resolution, stakeholder involvement, and
coordination (Burke,1998).
3. Capacity building. Creating a plan to enhance skills and knowledge of all partners fosters
co-learning, reexivity about power, equitable participation, and sustainability. External
evaluators and funders must gain a deep understanding of the community, the historical
and current context, and the program (Shulha et al.,2016). Workshops based on popular
education can help build skills and knowledge of participatory evaluation while empha-
sizing that all bring knowledge to the table. Evaluation facilitators who are working across
languages or with participants who require accommodations need to allocate sufcient
time and resources to ensure that all can participate fully.
4. Relationships with constituencies. Finally, participants should engage their broader con-
stituencies early on to build trust and ownership of the evaluation process beyond the core
team, inspire condence and vision, address concerns, and build a culture of transforma-
tive evaluation and learning.
Step 3: Agree on What to Evaluate
If program assumptions and theory, goals, objectives, and targets of change have been spelled out
using a participatory process, then the evaluation team can review and adjust what was initially
proposed. If goals and objectives were not clearly specied or developed without participation,
evaluation facilitators can guide discussion to make explicit the community’s implicit theory
(Weiss,1995). Objectives and evaluation criteria emerge from jointly exploring what results are
desired and how participants will know if progress is being made. Along with program-specic
outcomes such as improved health, it is important to measure process and systems outcomes
such as participation (Rifkin,2014), collaboration (Granner & Sharpe,2004), empowerment and
community control (Cyril, Smith, & Renzaho,2015; Wallerstein,2006), and community compe-
tence or capacity (Eng & Parker,1994; Goodman et al.,1998; Liberato et al.,2011).
Step 4: Create a Plan for Collecting Data
The participatory evaluation team collaboratively develops a design and methodology for the
evaluation that is made up of quantitative and qualitative methods for collecting information
to track progress and document change. Feuerstein (1988) recommends building condence in
participants by starting with existing methods of monitoring. The evaluation plan needs to be
feasible and make the best use of community resources while ensuring that results are valid and
credible. Popular education activities can be used to develop an evaluation design that values
and integrates multiple ways of knowing.
Step 5: Collect Data and Track Progress
T-PE involves community members in documenting the program and its effects. Systems for
recording activities and events as they unfold should be developed with those who will be using
them, including partner organizations to enhance sustainability (Zukoski & Luluquisen,2002).
Use of technology and online resources, such as handheld devices for recording data in the eld
(Gravlee et al.,2006), expand the community’s ability to create and use knowledge. See for
example, the Community Tool Box Online Documentation System (see Appendix 11).
Participatory Evaluation as a Process of Empowerment 257
Step 6: Feedback and Interpret Findings Collectively
Making sense of the data is a collaborative effort that combines technical expertise, experiential
knowledge, and deep understanding of the community. The evaluation facilitator and project
staff members organize different types of data into a common body of information that partici-
pants can check for meaning and validity and then identify gaps or connections among the data.
The aim is to build consensus and incorporate preliminary implications and recommendations
to set the stage for moving from knowledge to action using a decolonizing lens, incorporating
larger structural factors into the analysis.
Step 7: Communicate Results to Relevant Audiences
Participatory evaluation communicates ndings to key insider and outsider stakeholders in mul-
tiple ways and at multiple time points. Sharing achievements as they occur and framing evalu-
ation data in terms of strengths rather than weaknesses can energize the community and build
trust and commitment to the project. Creative media, such as video, theater, art, posters, web-
sites, and social media, using the expertise of community team members, may communicate
results more effectively than reports and presentations.
Step 8: Apply Findings for Action
Using the lessons learned, the group can strengthen or expand community efforts, institution-
alize changes, and plan future actions. Valuable information on program processes and out-
comes may lead the project to redene objectives, redirect scarce resources or seek out new
ones, modify strategies, and strengthen leadership structures. Community efforts that aim
for transformative change focus on evaluating collective power, equity, systems change, and
policy advocacy (Cheezum et al.,2013; Israel et al.,2010; Minkler, Garcia, Rubin, & Waller-
stein,2012).
CASE STUDY ONE: THE OREGON COMMUNITY EDUCATION
WORKER (CEW) PROGRAM
In the following, we provide two case studies of how participatory evaluation is being used to
foster and facilitate empowerment in two community health worker programs. The case studies
provide concrete applications of the theory and action steps previously described.
Background and Lead Partners
The Community Education Worker (CEW) Program, based in Multnomah County, Oregon, is
a two-year-old partnership between culturally specic and mainstream community-based orga-
nizations (CBOs), a public agency, and several local funders. The CEW Program is the result
of a community-based process that aimed to ensure that all children in Multnomah County can
achieve educational success and obtain a fullling career that pays a living wage.
The idea for the CEW Program came from a Latina mother, who expressed a need for
people from her own community who could help her prepare her children to succeed in kin-
dergarten. In response, the “Ready for Kindergarten (R4K) Collaborative” decided to adapt the
CHW model. In its rst year, individuals who had participated in a CHW-certication course
258 Community-Based Participatory Research for Health
using popular education were hired by three culturally specic agencies: Native American
Youth and Family Association (NAYA), Latino Network, and the Urban League of Portland.
The Immigrant and Refugee Community Organization (IRCO) added CEWs serving the Zomi
(Burmese) and Somali communities in year 2. CEWs conduct visits with families, facilitate
parent-child learning groups, serve as cultural mediators between families and systems, and
organize parents to address early childhood education inequities.
The Multnomah County Community Capacitation Center (CCC) was chosen by the R4K
Collaborative to lead the CEW Program and conduct the evaluation. For fteen years, the CCC
has supported communities most affected by inequities to identify and address their own most
pressing health issues, using popular education, the CHW model, and community-based partici-
patory research and evaluation (CBPR/E). As the staff members and communities involved have
grown and become more diverse, the theoretical framework of the CCC has expanded from
its original Latin American inuences to include the civil rights movement, disability rights
movement, and movements to decolonize evaluation and community practice.
To date, the participatory evaluation experience of the CEW Program can be divided into
two phases. In year 1, CCC developed an evaluation plan that, although it had participatory ele-
ments, was largely driven by the CCC staff members. During year 2, CCC is deepening stake-
holder participation to develop a truly participatory evaluation. The experience of the CEW
Program demonstrates how an evaluation can progress along a continuum from evaluator-driven
to community-driven.
Context
Portland, Oregon, is the whitest major city in the United States (Badger, 2015). Although Oregon
has a reputation (at least in dominant culture) for being politically progressive, this reputation
obscures a history of oppression and exclusion directed at people of color and immigrants. As
Portland has become a highly desirable place to live, gentrication and an acute shortage of afford-
able housing have led to substantial displacement and homelessness among low-income people of
color. Families of color are now moving into areas where they have not traditionally lived, where
they do not feel welcome, and where schools are ill-prepared to effectively serve their children.
Initial Steps in the T-PE Process
After the idea for the CEW Program had been developed, CCC staff members and a super-
visor at one of the culturally specic agencies co-facilitated a workshop at an R4K meeting
to develop a logic model. This resulted in a draft set of desired outcomes as well as short-,
medium-, and long-term indicators for these outcomes. Social Venture Partners (SVP) Portland,
one of the local funders, contributed other intermediate and long-term outcomes associated with
kindergarten readiness.
The CCC proposal for year 1 evaluation funding to SVP was not yet participatory because
CEWs had not yet been hired. CCC included a proviso in the proposal that a commitment to
developmental and participatory evaluation would likely mean changes in the future based on
CEW and community input.
Once the CEWs were hired, the next step was to begin to bring them into the evaluation
process, which occurred during their initial training. Following discussions on how assessment
can be used as a tool for oppression or for empowerment, the new CEWs were introduced to
Participatory Evaluation as a Process of Empowerment 259
the logic model, which was compared to a “road to educational equity,” starting at “now” and
ending twenty to twenty-ve years in the future. On the far right were outcomes such as “all
children graduate from high school.” In the middle were indicators such as “families express
increased ability to advocate for their children with systems.” On the left were short-term mea-
sures such as “children have a primary care home.” CEWs were given placards with the out-
comes and indicators. They were asked to read their outcome or indicator and then place it on
the road. They started on the far right and worked backward so that they could see what the
program’s ultimate goals were and how their actions as CEWs would contribute to achieving
the long-term goals. Finally, the group reected on several questions: (1) How does our work
now contribute to achieving outcomes twenty and twenty-ve years into the future? (2) What
do you think about these outcomes? and (3) In order to show that we are moving along this time
line, what do we have to do?
The “road to educational equity” activity set the stage for the participatory development of
tools to track outcomes and indicators. In a series of meetings conducted separately with both
major language groups (Spanish and English), a draft set of tracking forms was workshopped
with the CEWs. At each stage, changes made with one language group were translated into
the other language and reviewed by the other language group until initial forms were devel-
oped. Forms have continued to change based on input from CEWs, such as simplifying “case
management” sections to allow more exibility for CEWs and participants to record and track
their goals and activities.
Deepening Participatory Processes
In year 2, evaluation staff members expressed a desire at a steering committee meeting to make the
evaluation a fully participatory process. Despite the extra time involved for frontline and super-
vision staff members, whose time was already limited, they supported this idea. An e-mail invi-
tation was sent to key stakeholders, who included CEWs, supervisors, and funders. Since then,
meetings of the participatory evaluation team have been held monthly. In these fully bilingual
meetings, popular education has been used to build collective knowledge about topics such as
(1) the meaning of evaluation and the range of evaluation paradigms; (2) how beliefs about truth,
knowledge, and values inuence approaches to evaluation; (3) the role of evaluation questions; (4)
evaluation design; and (5) data collection methods. The year 1 evaluation plan has been used as an
example of the phenomena the team is discussing. Participants have expressed excitement about
learning to use terms such as ontology and epistemology (in two languages) and satisfaction that
no assumptions were made about their interest in or ability to learn these concepts. The team has
made changes to better reect the collective paradigm and revised evaluation questions.
The process of developing a participatory evaluation for the CEW Program reects many
of the lessons described in the background section of this chapter. Despite their heavy work-
load, CBO staff members, including CEWs, have been eager to engage in the participatory
process, as long as meetings are fully accessible to them and their time is well spent. They
bring insights from their cultural groups that could not be accessed if they were not a part of
the process, leading to better evaluation questions and stronger outcomes. Staff members and
partners from SVP have not only supported the process but also have eagerly participated in it.
Because many of the evaluation team members, including CEWs, have extensive experience
with popular education, there is a shared, preexisting commitment to popular education values
260 Community-Based Participatory Research for Health
including solidarity, compassion, humility, and love for the cause of the people. This commit-
ment provides solid grounding for the participatory evaluation process.
CASE STUDY TWO: AMOS HEALTH AND HOPE, NICARAGUA
This case study describes the T-PE approach of a community-based nonprot public health orga-
nization in Nicaragua called AMOS Health and Hope (www.amoshealth.org). Despite being in
a low-resourced global health setting, AMOS has prioritized T-PE as an integral part of the
CBPR conceptual model (see Chapter6) to improve program impact and facilitate community
empowerment.
Context
Nicaragua is the second poorest country in Latin America and has a long history of man-made
and natural disasters. Starting with the death of the majority of the Indigenous populations during
Spanish colonization, followed by years of dictatorship under the Somozas, a revolution in the
1980s, and earthquakes, hurricanes, and International Monetary Funds (IMF) structural adjust-
ment policies in the 1990s, the country is characterized by extreme disparities in wealth and health.
Passionate about reducing health inequities and informed by the work of global health,
popular education, and public health practitioners, AMOS cofounder, the late Dr. Gustavo Para-
jón, pioneered the rst Nicaraguan CHW program and later gave the best advice possible: “A
doctor in Nicaragua should not be a doctor but a teacher to share our knowledge and empower
others to serve.” In this spirit, AMOS was founded as a place to learn alongside communities
to continuously evaluate, reect, and improve the practice of CBPR, community empower-
ment, and participatory evaluation. AMOS currently works in twenty-six communities and four
departments throughout Nicaragua, serving a population of thirteen thousand people.
CHW and Staff Training for CBPR and Participatory Evaluation
When the current codirectors cofounded AMOS in 2006, an emphasis was placed on designing
the program using CBPR principles, including participatory evaluation. Not having funds for an
evaluator, AMOS integrated participatory evaluation into every aspect of the program. CHWs
are trained using popular education methodologies and often refer to themselves as “agents of
change” who work to transform root causes of inequities in their own communities. The CHWs
in each of the communities comprise a community health promoter, community leaders, and
volunteer mothers who form a community health committee. The current evaluation staff mem-
bers at AMOS mentor and annually train eld staff members and CHWs to ensure that the prin-
ciples of T-PE occur throughout the organization.
AMOS’s multidisciplinary staff members comprise CHWs, nurses, doctors, and nutrition-
ists from a range of social classes, ethnicities, and countries and are conscious of colonization,
the bidirectionality of relationships between communities and themselves, and the continuous
need to inspire and be inspired using transformative educational methods.
Participatory Evaluation Processes
AMOS’s approach is to start by developing trust with the communities, understanding the
geographic boundaries of the community (which often may not be the same as governmental
Participatory Evaluation as a Process of Empowerment 261
boundaries), as well as developing an inventory to identify community strengths. The approach
is assets-based and seeks to bring together multi-sectoral collaboration for increased impact
through a three-way partnership: the community identifying their key community priorities
and issues, the government providing top-down policy guidance and epidemiological priority
guidance, and nongovernmental partners such as nonprots and churches offering the support
and facilitation for participatory processes and evaluation.
Once the three-way partnership is established, a health committee (HC) is formed by
community leaders representing diverse geographic, political, and cultural groups and who
receive training by AMOS staff members using popular education methods. The cornerstone
of the community’s participatory evaluation process is the census, which is based on the motto
“Every person is counted, and every person counts.” Conducted by community members, the
census is analyzed in coordination with AMOS staff members, who do the initial tabulation
of data. Once data are interpreted with the community, the HC develops a community plan of
action. Communities have developed priority projects, such as installation of clean water lters,
clean-up campaigns for vector control, and community advocacy to close down bars.
A balance of community-driven priorities (such as clean water projects) and the govern-
mental epidemiological priorities (such as ensuring systematic home visitation of pregnant
women and newborns to prevent high neonatal mortality rates) is facilitated by AMOS support
staff members, who visit communities monthly. Community data are analyzed by the health
promoter and HC on a quarterly and annual basis. Popular education methodologies such as the
River of Life (see Appendix 7) are used to support participatory evaluation. The process is iter-
ative with several steps done annually to prioritize issues, implement a community health plan,
and evaluate impact together.
Many lessons have been learned over the years:
1. “Staff not stuff” approach. Participatory evaluation requires staff time and resources to
organize and integrate real-time data into an understandable form to allow for deeper
discussion at the community level. This is a challenge in low-resource international health
settings where donors tend to give money for “stuff”—commodities such as vitamins,
vaccines, educational ipcharts, deworming pills—but not for trained and committed staff
members needed for CBPR and participatory evaluation. With many competing needs
for funding, strong organizational leadership and a commitment to CBPR is necessary to
ensure adequate staff and resources for T-PE.
2. Continuing education for T-PE. Despite Latin America being the birthplace of many
transformative education methodologies, most education still uses “banking” method-
ology (Freire,2003). Intensive CBPR training for new staff members followed by ongoing
training and mentoring is key to ensuring T-PE becomes part of the organizational culture.
Having a T-PE-oriented evaluator on staff to facilitate this process is key!
3. Balancing epidemiological and community priorities. In the framework of transformational
community development work, epidemiological priorities often must be balanced with
community priorities. For example, patients who have walked three hours carrying their
child to the clinic expect curative services, such as antibiotics for a common cold, even
though international protocols prohibit this use. Communities don’t clamor for preventive
care even though it is more cost-effective. Through the T-PE process, AMOS has ensured
262 Community-Based Participatory Research for Health
that data collected on the use of antibiotics is shared with the community. This practice,
combined with educational messages using popular education methodologies, has resulted
in signicant improvement on the rational use of antibiotics in communities. Balancing
these two priorities is a long-term process that includes the use of T-PE to help establish
priorities based on real data that can be used to change social and cultural norms.
4. Real-time data use by communities. For T-PE to create momentum for change in commu-
nities, there is a need for constant feedback of data to communities, which can be very
time-consuming when a paper-based system is used. Future plans at AMOS include seek-
ing funding to design and implement robust mobile data collection and evaluation systems
that can provide real-time data for CHWs and training CHWs to use these mobile data
systems with their community evaluation teams in order to enhance the impact of T-PE
processes.
AMOS provides lessons for practitioners and researchers in the development of partic-
ipatory evaluation tools for low-resource settings. Participatory evaluation as practiced by
AMOS is not a separate project or intervention, but a way of life. In the words of one CHW:
“We are investigators because we collect information on what is going on in our own commu-
nities. And because we know, we can take that knowledge and make a difference in our own
communities.”
CONCLUSION
Transformative participatory evaluation is a process of skill building and power sharing that,
when conducted with intention and integrity, can promote the empowerment of individuals and
communities, as well as contribute to a range of other desirable outcomes. Facilitation of a suc-
cessful participatory evaluation process requires careful attention to composition of the stake-
holder group, relationship building across a range of stakeholders, deep awareness of one’s own
cultural worldviews, open acknowledgment and constant renegotiation of power and control,
use of liberatory educational philosophies and methods, selection of appropriate data collection
methods, and prevention of stakeholder burnout through optimal use of their time. It carefully
balances education, investigation, and action, and in so doing, it provides a crucial opportunity
to challenge assumptions of value and shift and balance power.
QUESTIONS FOR DISCUSSION
1. What are the key differences between transformative participatory evaluation and more
conventional approaches to evaluation? How does T-PE challenge dominant Western
assumptions about value and the meaning of knowledge?
2. Based on your experience as well as what you read, why is it important to constantly
attend to power relationships when working on diverse teams? What strategies can we use
to do this?
3. How do you reconcile balancing epidemiological priorities with community priorities in a
participatory evaluation process?
Participatory Evaluation as a Process of Empowerment 263
REFERENCES
Badger, E. (2015, March 24). How the whitest city in American appears through the eyes of its black residents. Washington Post. Avail-
able at: https://www.washingtonpost.com/news/wonk/wp/2015/03/24/how-the-whitest-city-in-america-appears-through-
the-eyes-of-its-black-residents/?utm_term=.0c2665705ec2
Brisolara, S. (1998). The history of participatory evaluation and current debates in the eld. In E. Whitmore (Ed.), New direc-
tions for evaluation: Understanding and practicing participatory evaluation, 80, 25–37.
Burke, B. (1998). Evaluating for a change: Reections on participatory methodology. In E. Whitmore (Ed.), New directions
for evaluation: Understanding and practicing participatory evaluation, 80, 43–55.
Cheezum, R. R., Coombe, C. M., Israel, B. A., McGranaghan, R. J., Burris, A. N., Grant-White, S., . . . Anderson, M. (2013).
Building community capacity to advocate for policy change: An impact evaluation of the Neighborhoods Working in Part-
nership Project in Detroit. Journal of Community Practice, 21(3), 228–247.
Coombe, C. M. (2012). Participatory approaches to evaluating community organizing and coalition building. In M. Minkler
(Ed.), Community organizing and community building for health and welfare (pp. 346–365). New Brunswick, NJ: Rutgers
University Press.
Cousins, J. B., & Chouinard, J. A. (2012). Participatory evaluation up close: An integration of research-based knowledge.
Charlotte, NC: Information-Age Publishing.
Cyril, S., Smith, B. J., & Renzaho, A. M. (2015). Systematic review of empowerment measures in health promotion. Health
Promotion International (2015), 1–18.
Eng, E., & Parker, E. (1994). Measuring community competence in the Mississippi Delta: The interface between program
evaluation and empowerment. Health Education & Behavior, 21(2), 199–220.
Fals-Borda, O., & Rahman, M. A. (1991). Action and knowledge: Breaking the monopoly with participatory action research.
New York, NY: The Apex Press.
Fawcett, S. B., Paine-Andrews, A., Francisco, V. T., Schultz, J. A., Richter, K. P., Lewis, R. K., . . . Fisher, J. L. (1996).
Empowering community health initiatives through evaluation. In D. M. Fetterman, S. J. Kaftarian, & A. Wandersman
(Eds.), Empowerment evaluation: Knowledge and tools for self-assessment and accountability (pp. 161–187). Thousand
Oaks, CA: Sage
Fernandes, W., & Tandon, R. (1981). Participatory research and evaluation: Experiments in research as a process of
liberation. New Delhi, India: Indian Social Institute.
Fetterman, D. M. (2000). Foundations of empowerment evaluation. Thousand Oaks, CA: Sage.
Fetterman, D. M., Kaftarian, S. J., & Wandersman, A. (2015). Empowerment evaluation: Knowledge and tools for self-assessment
and accountability (2nd ed.). Thousand Oaks, CA: Sage.
Feuerstein, M. T. (1988). Finding the methods to t the people: Training for participatory evaluation. Community Development
Journal, 23(1), 16–25.
Freire, P. (1982). Creating alternative research methods: Learning to do it by doing it. In B. Hall, A. Gillette, & R. Tandon
(Eds.), Creating knowledge: A monopoly? Participatory research in development (pp. 29–37). New Delhi, India: Society
for Participatory Research in Asia.
Freire, P. (2003). Pedagogy of the oppressed. New York, NY: Continuum.
Gaventa, J. (1980). Power and powerlessness: Quiescence and rebellion in an Appalachian valley. Chicago: University of
Illinois Press.
Gaventa, J. (1991). Toward a knowledge democracy: Viewpoints on participatory research in North America. In O. Fals-
Borda & M. A. Rahman (Eds.), Action and knowledge: Breaking the monopoly with participatory action-research
(pp. 121–131). New York, NY: The Apex Press.
Goodman, R. M., Speers, M. A., McLeroy, K., Fawcett, S., Kegler, M., Parker, E., Sterling, T., & Wallerstein, N. (1998).
Identifying and dening the dimensions of community capacity to provide a basis for measurement. Health Education &
Behavior, 25(3), 258–278.
Gramsci, A. (1971). Selections from the prison notebook of Antonio Gramsci. Q. Hoare & G. N. Smith (Eds.). London, UK:
The Electric Book Company.
Granner, M. L., & Sharpe, P. A. (2004). Evaluating community coalition characteristics and functioning: A summary of
measurement tools. Health Education Research, 19(5), 514–532.
Gravlee, C. C., Zenk, S. N., Woods, S., Rowe, Z., & Schulz, A. J. (2006). Handheld computers for direct observation of the
social and physical environment. Field Methods, 18(4), 382–397.
264 Community-Based Participatory Research for Health
Hall, B., Jackson, E., Tandon, R., Fontan, J. M., & Lall, N. (2013). Knowledge, democracy, and action: Community-university
partnerships in global perspectives. Manchester, UK: Manchester University Press.
Horton, M. (2003). The Miles Horton reader: Education for social change. D. Jacobs (Ed.). Knoxville, TN: The University
of Tennessee Press.
Israel, B. A., Coombe, C. M., Cheezum, R. R., Schulz, A. J., McGranaghan, R. J., Lichtenstein, R., . . . Burris A. (2010).
Community-based participatory research: A capacity building approach for policy advocacy aimed at eliminating health
disparities. American Journal of Public Health, 100(11), 2094–2102.
Kawakami, A. J., Aton, K., Cram, F., Lai, M. K., & Porima, L. (2007). Improving the practice of evaluation through Indige-
nous values and methods: Decolonizing evaluation practice returning the gaze from Hawai’i and Aotearoa. Hülili: Multi-
disciplinary Research on Hawaiian Well-Being, 4(1), 319–348.
Levin-Rozalis, M. (2003). Evaluation and research: Differences and similarities. The Canadian Journal of Program Evalua-
tion, 18(2), 1–31.
Liberato, S. C., Brimblecombe, J., Ritchie, J., Ferguson, M., & Coveney, J. (2011). Measuring capacity building in commu-
nities: A review of the literature. BMC Public Health, 11(1), 1–10.
Maltrud, K., Polacsek, M., & Wallerstein, N. (1997). Participatory evaluation workbook for community initiatives: A toolkit
for healthy communities in New Mexico. Albuquerque, NM: University of New Mexico, MPH Program.
Minkler, M., Garcia, A. P., Rubin, V., & Wallerstein, N. (2012). Community-based participatory research: A strategy for
building healthy communities and promoting health through policy change. Retrieved from www.policylink.org/sites/
default/les/CBPR.pdf
Morelli, P. T., & Mataira, P. J. (2010). Indigenizing evaluation research: A long-awaited paradigm shift. Journal of Indigenous
Voices in Social Work, 1(2010), 1–12.
Rahman, M. A. (1991). The theoretical standpoint of PAR. In O. Fals-Borda & M. A. Rahman, Action and knowledge:
Breaking the monopoly with participatory action-research (pp. 13–23). New York, NY: The Apex Press.
Rifkin, S. B. (2014). Examining the links between community participation and health outcomes: A review of the literature.
Health Policy and Planning, 29(2014), ii98–ii106.
Shulha, L. M., Whitmore, E., Cousins, J. B., Gilbert, N., & Al Hadib, H. (2016). Introducing evidence-based principles to guide
collaborative approaches to evaluation results of an empirical process. American Journal of Evaluation, 37(2), 193–215.
Springett, J., & Wallerstein, N. (2008). Issues in participatory evaluation. In M. Minkler & N. Wallerstein (Eds.), Community-
based participatory research for health: From process to outcomes (pp. 199–220). San Francisco, CA: Jossey-Bass.
Tuhiwai Smith, L. (1999). Decolonizing methodologies: Research and Indigenous peoples. New York, NY: St. Martin’s Press.
Wallerstein, N. (1992). Powerlessness, empowerment, and health: Implications for health promotion programs. American
Journal of Health Promotion, 6(3), 197–205.
Wallerstein, N. (2006). What is the evidence on effectiveness of empowerment to improve health? Retrieved from www.euro.
who.int/__data/assets/pdf_le/0010/74656/E88086.pdf
Wallerstein, N., & Auerbach, E. (2004). Problem-posing at work: Popular educator’s guide. Edmonton, Alberta: Grass
Roots Press.
Weiss, C. H. (1995). Nothing as practical as good theory: Exploring theory-based evaluation for comprehensive community
initiatives for children and families. New Approaches to Evaluating Community Initiatives: Concepts, Methods, and Con-
texts, 1(1995), 65–92.
Wiggins, N. (2012). Popular education for health promotion and community empowerment: A review of the literature. Health
Promotion International, 27(3), 356–371.
Wiggins, N., Hughes, A., Rodriguez, A., Potter, C., & Rios-Campos, T. (2014). La Palabra es Salud (The word is health):
Combining mixed methods and CBPR to understand the comparative effectiveness of popular and conventional educa-
tion. Journal of Mixed Methods Research, 8(3), 278–298.
Zavala, M. (2013). What do we mean by decolonizing research strategies? Lessons from decolonizing; Indigenous research
projects in New Zealand and Latin America. Decolonization: Indigeneity, Education & Society, 2(1), 55–71.
Zukoski, A., & Luluquisen, M. (2002). Participatory evaluation: What is it? What are the challenges? Community-Based
Public Health, 5(2002), 1–6.

19
CHAPTER
Since 2003, the Institute of Medicine (IOM) (Gebbie, Rosenstock, & Hernandez,2003), the
W.K. Kellogg Foundation and others have declared community-based participatory research
(CBPR) to be an essential area of education for public health professionals. One of the core out-
comes of CBPR partnerships is in fact the development of personal skills and capacities among
all stakeholders, leading often to more formal education for community partners, students, or
junior researchers. For academics, training researchers to use a CBPR approach, however, is
complex, and it is particularly complex for faculty members of color. Few formal programs
have sought to train doctoral-level researchers, especially scholars of color, to achieve the met-
rics necessary for success in university or other academic research settings through a CBPR
approach. This chapter will introduce three formal training programs as experienced by three
faculty members of color while using a CBPR approach.
Fortunately, there has been the Native American Research Centers for Health (NARCH)
initiative funded by the National Institutes of Health (NIH) in partnership with the Indian
Health Service (IHS), and two W.K. Kellogg Foundation–funded postdoctoral training pro-
grams focused on the use of CBPR: the Community Health Scholars Program and the Kellogg
Health Scholars Program. In this chapter, as faculty of color, we discuss some of the unique
ACADEMIC POSITIONS FOR
FACULTY OF COLOR
COMBINING LIFE CALLING, COMMUNITY
SERVICE, AND RESEARCH
LORENDA BELONE, DEREK M. GRIFFITH, AND BARBARA BAQUERO

266 Community-Based Participatory Research for Health
challenges and benets of employing a CBPR approach. We begin by briey describing each
program and the scholar representing the program. We discuss our own history and culture and
how that has led each of us to see CBPR research as not only a job but as a life calling and a
service to communities of color. We conclude by offering some collective reections on how
CBPR makes research more meaningful in our ability to simultaneously serve our own commu-
nities as well as the scientic community.
THE NATIVE AMERICAN RESEARCH CENTERS FOR HEALTH (NARCH)
Since 2000, the purpose of NARCH has been to fund American Indian/Alaska Native
(AI/AN) research, reduce AI/AN health disparities, address the distrust of research, and
support a pipeline for Native researchers. To date, there have been nine NARCH fund-
ing cycles (www.nigms.nih.gov/Research/CRCB/NARCH/Pages/default.aspx). Unlike any
other NIH-funding mechanism, NARCH funding requires tribes or inter-tribal organizations
to be the principal investigator of a NARCH Center, which can have multiple research and
training components.
Lorenda: An Indigenous Scholar and the Contribution of NARCH
I am a Navajo woman, raised in a matriarchal society that focuses on the importance of clan relationships
and the roles of daughters, mothers, grandmothers, etc., which are central to one’s identity. As a child
I had very loving grandparents who raised me, which is not uncommon in Navajo childrearing. Navajo
grandparents often take on a very active role in raising grandchildren, something I proudly do as a
grandmother of a four-year-old granddaughter. I grew up in a home where education was highly
valued. I was fortunate, due to the fact that in other Navajo homes education was viewed as traumatic
due to prior abusive boarding school experiences. My grandfather was a life-long learner who instilled
this passion in me, along with the values of respect and the importance of service to my community.
As a Native researcher who instills the importance of service to Native communities, I utilize a
community-based participatory research approach with an Indigenous paradigm. For the past seventeen
years, I have been engaged in health disparities research with Native communities of the Southwest.
For twelve of the seventeen years I have collaborated in the creation, piloting, and now rigorous testing
of an intergenerational family prevention program with three tribal sovereign nations. In addition, for
eleven years I have coinvestigated the examination of the partnering processes of CBPR across the
country in the hopes of improving health equity.
As a Native scholar I obtained research experience, skills, and mentoring while a master’s and
then doctoral student on federally funded Centers for Disease Control and NARCH studies, each
study involving a New Mexico Native community, although none of these communities were my own.
Though I did not ofcially participate in a NARCH training component, the training I received from
mentorship from faculty members at UNM’s Center for Participatory Research, and on-the-job research
eld experiences were invaluable. When I was a pre- and postdoctoral fellow, this training led to me
becoming a principal investigator on a NARCH V study with an Apache community, and I then began
to participate in the national NARCH investigator network.
Academic Positions for Faculty of Color 267
W.K. KELLOGG COMMUNITY HEALTH SCHOLARS (CHSP) AND KELLOGG
HEALTH SCHOLARS PROGRAMS (KHSP)
From 1998 to 2007, the W.K. Kellogg Community Health Scholars Program (CHSP) provided
postdoctoral training fellowships to develop and enhance their CBPR research skills in working
with communities while concurrently following the core principles of CBPR by contrib-
uting to the health of communities where scholars were trained (Baquero et al.,2014; Grifth
My dissertation examined the communicative dialectical tensions and paradoxical situations faced
by other Native scholars across the county and found that they experienced multiple communicative
struggles while conducting research with Native communities (Belone,2010). A major struggle included
the tension of being both insider-outsider on research involving tribal communities and serving these
communities yet being held to academic requirements of publishing. Native scholars also stated they
struggled with the paradox of wanting to walk the talk in the academy (for those who used a CBPR
approach), which was appropriate in community settings, but not fully rewarded in the academy, and
the challenges of navigating when to have (or not have) open and honest communication within
academic departments about the additional accountability to the community.
As an Indigenous disparities researcher, I incorporate the centering of culture in the design and
dissemination of research and when possible utilize a decolonizing methodological process with a
public health socioecological holistic framework. For the past twelve years, I have been actively engaged
with three New Mexico Native communities. Being responsive to these communities’ voices have
spurred the creation of culturally specic Navajo, Pueblo, and Apache intergenerational family curricula
called the Family Listening/Circle Program (FL/CP) that was built upon the empirically supported and
culturally embedded intervention work of Whitbeck and the Anishinabe Tribe of Minnesota. The CBPR
development and piloting of the culturally specic FL/CP intervention was funded by NARCH III and V
(Belone et al.,2016). The ndings from these pilots included the importance of acknowledging and
overcoming historical negative research experiences; using community resources; listening to the voices
of the young and old in guiding the family prevention program; maintaining a continuing presence
in the community, even during periods without funding; and transforming each tribe’s community
advisory board to an effective tribal research team.
This collaborative work resulted in a continued commitment to the tribal-university partnership and
the collective decision to submit and successfully obtain an NIH R01 study to test the effectiveness of
FL/CP with the tribal communities. Our intention has been to establish an empirically tested program,
co-developed using CBPR processes with tribal research teams, that could eventually be offered as a
nationally acknowledged evidence-based program. Historically, tribes do not have options to choose
Indigenous-centered programs when using federal funds for prevention-intervention programs. The
rigorous testing, therefore, of FL/CP would have huge implications for tribes across the country to
adopt and then adapt their own version of the culture-centered prevention-intervention program. This
result not only holds the promise of improved health outcomes for tribal communities but also makes
a strong contribution to health disparities research with AI/AN populations. As a Native scholar I am a
proud product of the NARCH initiative.
268 Community-Based Participatory Research for Health
et al., 2009). The CHSP grew out of the experience of an earlier Kellogg-funded program,
the community-based public health initiative (CBPHI). The initial aim of the program was to
enhance community understanding of social determinants of health, identify and map Indige-
nous leadership, build coalitions, and increase competency in working in cross-cultural settings
(www.kellogghealthscholars.org).
As the CHSP program was ending, the W.K. Kellogg Foundation decided to create the Kel-
logg Health Scholars program, beginning in 2007. Building on the success of CHSP, the KHSP
helped scholars build skills in working with communities and in translating the ndings of
CBPR into policy. The KHSP also sought to strengthen the capacity of community-based orga-
nizations working in communities experiencing health disparities to initiate and participate in
health disparities research, to apply this research in addressing their own health challenges, and
to advocate effectively for policy changes that address these disparities. As part of the agenda
of the annual networking meeting in Washington, DC, KHSP scholars and their academic and
community mentors participated in a “hill walk,” visiting with members of Congress, staffers,
and advocacy organizations to share their work and establish relationships with these policy
makers and advocates. At each of these visits, scholars and their accompanying mentors shared
one-page summaries of their work and its application to policy. The program ended in 2012
after training a number of scholars in CBPR who also understood how to inuence policy.
Barbara: A Latina Scholar and the Contribution of KHSP
I emigrated from Venezuela with a degree in clinical psychology to pursue my graduate education
in 1998, receiving my MPH and doctoral degree from the University of California, San Diego and
SanDiego State University.
Living in Southern California as a Latina, I now realize I had many privileges and was shielded from
racial-ethnic discrimination that occurs in other parts of the country. I am the daughter of immigrants;
my parents and nuclear family immigrated from Colombia to Venezuela in the early 1970s to look for
better opportunities; twenty years later I did it myself. These experiences have shaped and inuenced my
pre- and postdoctoral research training and career. My research focuses on addressing health disparities
in obesity and cancer prevention and control through the design, implementation, and evaluation of
community-based interventions to promote healthy eating and active lifestyles for Latinos and rural
communities in the United States.
As an immigrant, training with mentors committed to Latino health and working in a diverse and
Latino majority community, I was able to leverage my cultural background, immigrant experience,
language skills, and passion for research toward learning about and addressing Latino public health
issues. As a complement, my predoctoral training consisted of health behavior intervention design
and implementation, with an emphasis on CBPR. Mentors, professors, and supervisors shared their
power with me and used their power and privilege to offer me opportunities and connection to their
networks. They took the time to polish my talents, trained me as a scientist, and supported me to
continue in academia. This environment proved to be important in my development as a Latina scholar.
Training in that environment made it possible for me to see myself as a researcher and allowed me to
believe I could achieve that goal.

Academic Positions for Faculty of Color 269
From that foundation, I was able to secure a spot in the W.K. Kellogg Health Scholar Program (KHSP)
in CBPR. I would describe my experience as a scholar as empowering, eye opening, and challenging.
Coming from an academic community where I was part of the dominant group, then moving to UNC,
Chapel Hill was a culture shock not only because the academic experience was different but also because
it was a different state with different cultural politics and history. This challenged me to think about the
experiences of Latinos who do not live in California and my own power and privilege as being a highly
educated Latina who shared cultural and immigrant experiences but at the same time was an outsider
to the same Latino community. Realizing my outsider-insider roles as Latina and a researcher has helped
me to stay grounded and connected to my Latino and academic communities. From these roles, I have
drawn strength to continue my work and advocate for issues I consider important without assuming
that I can represent the Latino community as a whole. But also having these roles and understanding my
experience have been taxing as I am never an insider nor an outsider in either community.
Professionally, the KHSP provided me the opportunity to train and practice CBPR and to nd an
identity as an independent researcher. The combination of having academic and community mentors
taught me how to navigate and integrate both worlds into my research and to negotiate the demands
and resources of each.
Personally, I have beneted from the networks I have created, the new prestigious mentors I gained,
and the reputation I acquired from being in the KHSP. As a scholar of color, I have borrowed power from
academic and community mentors who have provided the currency to gain entry and acceptance into the
academic community. I realize now that when I introduce myself to a new group I include my postdoctoral
training as a Kellogg scholar to validate my CBPR expertise and presence in the room. In addition, the
training and networks allowed for the growth of my professional and peer network of like-minded and
racial-ethnic diverse researchers and scholars. I am now a part of a far-reaching network of CBPR researchers
who work all across the country with whom I can collaborate and obtain support and mentorship that
I would not have if I had not participated in the program. Among this diverse and rich network, I know
people like me, who share similar professional experiences and work toward the same goals.
Derek: An African American Man and the Contribution of CHSP and KHSP
I am an African American man who is second-generation American. My parents immigrated here
from Jamaica and Guyana and both have had careers in the health eld. My interest in racial and
gender disparities in health grew out of a desire to understand the relationship between racism
and health and how we could reduce and eliminate racial disparities in health. I earned a PhD in
clinical-community psychology from DePaul University, where my research explored people’s capacity
to envision and act to change political and social systems.
From this work on activism and social change, I successfully competed for a position in the CHSP,
where I trained at the UNC School of Public Health. During this time, I began to study institutional
racism in public health systems, and I started exploring social determinants of African American
men’s health. This work led to me developing an academic career studying social determinants
of health, strategies to achieve health equity, and men’s health disparities, rst at the University

270 Community-Based Participatory Research for Health
CONCLUSION
Faculty of color who use a CBPR approach face even greater challenges than colleagues who
use more traditional approaches (Belone, 2010; Walters & Simoni, 2002). As we illustrate
in this chapter, one tool that has been instrumental in the professional success of faculty of
color who are committed to using a CBPR approach in academia has been their participation
in formal funding programs that have a pipeline orientation, such as the NARCH initiative, and
of Michigan School of Public Health then at Vanderbilt University. During my time on the faculty at
Michigan, I also had the honor of becoming an academic mentor at Michigan in the CHSP and KHSP
programs. I mentored three postdoctoral fellows, alongside my community co-mentor, Mrs. Bettina
Campbell, the executive director of YOUR Center.
In my experience, being a faculty person of color presents three unique challenges and
opportunities. First, while many of us bring strong political and philosophical beliefs about fairness,
justice, and equity to the work, the role of a professor is not that of a philosopher or activist who
operates solely on opinion. Our jobs are to use science and scholarship to inform and make change,
and we have to prioritize publishing and funding this science if we want the opportunity to use
our platform to make social change. Thus, it is critical to recognize that what allows you to keep
your job is meeting and exceeding the expectations of promotion and tenure in the form of peer-
reviewed publications and grants. Second, while recognizing this context and its constraints, it is
critical to be present in the community, all the while being transparent about who we are and what
we are doing. Trust is difcult to earn, easy to lose, and hard to regain once broken. Being true to
CBPR principles and successful in academia may seem at odds, but they are more complicated if you
try to solve these problems without sharing them with your community partners. Good community
members are willing to work with you to balance their needs and your professional needs, and part
of doing this work is having enough faith in them to be honest about what you need and willing
to nd ways that both of you can achieve goals that are mutually benecial. There may be some
potential partners who reject this notion, but perhaps that person should not be your primary
partner in this work.
Third and nally, CBPR approaches to public health research and health promotion are personal.
When we do this work, we are affecting the lives of real people and their friends and loved ones who
eventually should become people whom you love and care about, too. It is incumbent upon us to utilize
the best of our skills and the best of ourselves, along with the resources we can marshal, to not only
do the best work we can but to help others in the process. There will be community members whom
you may be able to help learn about educational opportunities, jobs, and careers, not to mention junior
colleagues who would benet from your ear, support, and opinions, which are hopefully reecting
wisdom. Doing this work, as I have learned from my mentors, is not just about the job but recognizing
the awesome opportunity and responsibility that we have to be successful in our careers and also to
make tangible change where possible, leaving the communities better than when we arrived. We also
should recognize that if you leave this work or the communities of interest without relationships that
extend beyond the professional, you are likely doing something wrong.
Academic Positions for Faculty of Color 271
more formal training programs, such as the CHSP and the KHSP. These programs provided
the opportunities, supports, networks, and mentoring—during and after the formal training—
that have propelled us and other scholars into successful academic careers. CBPR reects the
embodiment of specic goals, values, and beliefs, and the motivation to employ this approach
as a way to realize how generations of sacrice and struggle can be honored through not only
what work we do but also how we do it. In this way, scholarship created using a CBPR approach
takes on more substance and meaning by the scholars and the communities they serve or repre-
sent by creating the space for bidirectional learning for new levels of critical thinking and action
(Muhammad et al.,2014).
QUESTIONS FOR DISCUSSION
1. This chapter shared training opportunities that supported the authors to be trained in
CBPR and to be able to conduct CBPR research. Can you identify additional training
opportunities in CBPR that were not mentioned?
2. From your experience as a scholar or community member, how can you support advancing
scholars of color to engage in CBPR?
REFERENCES
Baquero, B., Goldman, S. N., Siman, F., Muqueeth, S., Eng, E., & Rhodes, S. D. (2014). Mi Cuerpo Nuestro Responsabili-
dad: Using photovoice to describe the assets and barriers to sexual reproductive health among Latinos. Journal of Health
Disparities Research and Practice, 7(1 Special Issue).
Belone, L. (2010). An examination of communicative dialectical tensions and paradoxes encountered by Native American
researchers in the eld and in the academy. Dissertation, Communication and Journalism, University of New Mexico,
Albuquerque, NM.
Belone, L., Tosa, J., Shendo, K., Toya, A., Straits, K., Tafoya, G., Rebecca, Rae, Noyes, E., Bird, D., & Wallerstein, N. (2016).
Community-based participatory research for co-creating interventions with Native communities: A partnership between
the University of New Mexico and the Pueblo of Jemez. In N. Zane, G. Bernal, & F. T. L. Leong (Eds.), Evidence-
based psychological practice with ethnic minorities: Culturally informed research and clinical strategies (pp. 199–220).
Baltimore, MD: United Book Press.
Gebbie, K., Rosenstock, L., & Hernandez, L. M. (2003). Who will keep the public healthy? Educating public health profes-
sionals for the 21st century. Washington, DC: The National Academies Press.
Grifth, D. M., Citrin, T., Jerome, N. W., Bayer, I., & Mebane, E. (2009). The origins and overview of the W.K. Kellogg
community health scholars program. Progress in Community Health Partnerships: Research, Education, and Action,
3(Winter), 335–348. doi:10.1353/cpr.0.0098
Muhammad, M., Wallerstein, N., Sussman, A. L., Avila, M., Belone, L., & Duran, B. (2014). Reections on researcher
identity and power: The impact of positionality on community-based participatory research (CBPR) processes and
outcomes. Critical Sociology, 41(7—8), 1045–1063.
Walters, K. L., & Simoni, J. M. (2002). Reconceptualizing native women’s health: An “Indigenist” stress-coping model.
American Journal of Public Health, 92(4), 520–524.

7
PART
PROMISING
PRACTICES TO
OUTCOMES: HEALTHY
PUBLIC POLICY
As illustrated throughout this book, a distinguishing feature of community-based participa-
tory research (CBPR) is its commitment to action as part of the research process itself and not
something simply left for others to do once the study is complete. By understanding policy
change as a potent “action component,” CBPR has the potential for improving the lives and the
health of large numbers of people, beyond the partners involved or the particular communities
and populations they serve.
274 Part 7
One of the most celebrated examples of the potency of community-driven and policy-
focused CBPR in the United States began almost forty years ago, when residents of Woburn,
Massachusetts, worried about the high rates of childhood leukemia in their neighborhood. They
gathered data that led them to suspect a link to the community’s water supply and tried, unsuc-
cessfully, to convince local government authorities to test the water. Undeterred, community
members then approached researchers at Harvard University’s School of Public Health, and
a partnership was born. Harvard team members worked collaboratively with the community
in data gathering while also conducting their own epidemiological analyses to document
what the community had long suspected. Not only did community members in Woburn win a
multimillion-dollar civil suit against corporations that had, for years, dumped harmful chemicals
in the local water supply, but the partnership’s work played a key role in the federal govern-
ment’s decision to reauthorize Superfund legislation for toxic cleanups around the country.
In Chapter20, Lisa Cacari-Stone and her colleagues provide an overview of CBPR and policy
making, with particular attention to health equity. As they point out, although a “fundamental
disconnect” often exists between researchers and policy makers, CBPR’s engagement of a diver-
sity of stakeholders including constituents most affected by a problem can build bridges among
research, policy, and practice to help bring about needed change. After viewing CBPR within
the context of the social ecology of research use, Chapter20 offers and illustrates Cacari-Stone
et al.’s conceptual model for CBPR in policy making. Building in part on earlier “steps and
stages” frameworks, the new model moves from the contexts in which CBPR is embedded, to
partnership dynamics and the roles of scientific evidence and civic engagement, to the roles
partnerships may play in different phases of the policy-making process, and finally, to multi-
level outcomes. An environmental justice case study illustrates the model’s utility in practice,
and principles of CBPR are revisited through the lens of equity policy. The chapter ends with
policy competencies for CBPR partnerships interested in helping effect change on this critical
macro level.
Chapter21 by Meredith Minkler and colleagues again puts CBPR policy theory into action,
analyzing a case study of food insecurity and tobacco saturation in neighborhoods that depend
on small corner stores for food access. A healthy retail coalition in San Francisco’s low-income
Tenderloin neighborhood is examined with a focus on the roles of community, academic, health
Part 7
275
department, and other coalition partners in collecting data critical to building the local evidence
base, engaging residents and merchants, and helping craft, pass, and implement a healthy retail
policy enabling store conversions in such neighborhoods. The pathways model of CBPR and
policy making introduced in Chapter20 is used together with Kingdon’s three streams in the
policy-making process, to explore the contexts, dynamics, and diverse policy roles played by
partnership members and their allies. Diverse outcomes, including successful policy passage on
the municipal level, the conversion of nine initial stores to healthy retail, enhanced community
and partnership capacity, and substantial increases in the availability of healthy produce and
decreases in tobacco advertising and sales, also are presented, as are findings of a ripple effect
in other neighborhood stores. The key role of the coalition “food justice leaders” in monitoring
outcomes is discussed, as are challenges and implications for other municipalities interested in a
healthy retail approach to food justice.
In Chapter22 by Saneta deVuono-Powell and colleagues, we turn to an area in which health
and social inequities in the United States are among the sharpest: the differential treatment
of African Americans and Latinos in the criminal justice system. Following a brief review of
the dimensions of this reality, the need for a broader, public health approach to criminal jus-
tice reform is emphasized. This broad approach is illustrated through participatory research
studies of and by recently incarcerated people of color in Richmond, California, and by African
Americans and Latinos in the South Bronx, New York. The two cases highlight policy outcomes,
including Richmond’s creation of one of the strongest “ban-the-box” measures in the country
(stopping employers from asking about criminal convictions in the application and hiring pro-
cess), and in the Bronx, ending such racial-profiling practices as police “stop-and-frisk” in private
apartment buildings. Although the role of partnerships in such outcomes are best assessed in
terms of contribution, rather than attribution, multiple data sources suggest the importance of
each partnerships’ efforts in bringing about these critical policy changes. Both case studies used
the term participatory action research (PAR) and use methods, such as surveys and interviews,
“sidewalk science,” and other methods to gather actionable data for change. Although a dif-
ferent term than used in the rest of the book, PAR shares similar values and principles to CBPR
and offers similar promise for improving the processes and outcomes of equity-focused research
on the policy level.
276 Part 7
In Chapter23, Jason Corburn and colleagues broaden our gaze to explore two case studies
of community-driven mapping in the global South, where slum or informal settlement dwellers
and their outside partners have long mobilized to map their social and health conditions and
use findings to advocate for policy change The first case study, in a large slum settlement in
Rio de Janeiro, Brazil, illustrates how youth-led digital mapping, with the support of partners
at UNICEF and CEDAPS, a local Non-Government Organization (NGO), involved mapping tools,
including mobile phones for youth to photograph and upload images of risk in their commu-
nities to Google Maps and create a symbolic spatial representation of areas of environmental
risk. They subsequently use key findings to graphically make the case to government policy
actors for improvements in sanitation, reclaimed play spaces, and safer paths. In the second case
study, we learn how the residents of the Mathare informal settlement in Nairobi, Kenya, have
for years worked with partners at the University of Nairobi and the University of California,
Berkeley, to spatially map communities, help design place-based physical and social improve-
ments, and advocate for policies to increase health equity. The mapping led to tangible out-
comes (e.g., beginning implementation of a community-designed water plan and road building
and upgrades). Part of their success was their ability to help government decision makers recog-
nize the role that settlement youth could play, working collaboratively with adult academic and
other research partners to provide accurate and relevant data for policy deliberations.
Although each chapter discusses challenges, they also make the case for strong, often
community-led research partnerships for collecting and translating policy-relevant data and
using the findings to promote equity-focused policy change. Particularly in the unchartered
waters that characterize the current historical epoch, civic engagement on all levels and in all
sectors, including high-level engagement in research to inform and advocate for policy pro-
moting health and social equity, cannot be overstated.

20
CHAPTER
COMMUNITY-BASED
PARTICIPATORY RESEARCH
FOR HEALTH EQUITY
POLICY MAKING
LISA CACARI-STONE, MEREDITH MINKLER, NICHOLAS FREUDENBERG,
AND MAKANI N. THEMBA
DESPITE DECADES OF evidence of the disproportionately adverse impacts of social disad-
vantage on the health of diverse populations in the United States, insufcient attention has been
paid to how research can be leveraged with community partnerships to promote sound policies
that advance health equity. Although research plays an important role in documenting racial and
ethnic health inequities, there are ongoing challenges to moving evidence into a strategic policy
agenda and focused political action. First, a fundamental disconnect typically exists between
policy makers and researchers. A study of policy makers demonstrated the need for improving
their understanding of the relative merits of different evidence and for researchers to better under-
stand the demands on policy makers to better provide customer-sensitive products (Rigby, 2005).
Second, research competes with other political and world events, such as institutional con-
straints and rules, interest group pressure, and citizens’ values (Campbell et al., 2007). The
likelihood for evidence to be used in the policy-making process is increased if the research is per-
ceived as useful to policy makers (Lavis Lomas, Hamid, & Sewankambo,2006). Policy makers
need real-life timely analysis, availability of nancial and staff resources to meet demands, high
278 Community-Based Participatory Research for Health
technical quality, research tailored to different needs and users, and translation into user-friendly
materials (Rigby,2005).
Third, moving data into policy making requires more than the skills of researchers to
package and disseminate their research for use. Northington-Gamble and Stone (2006) argue
for the role of political action as a catalyst for research and policy:
Thirty years of scholarship on agenda-setting and issues framing have shown that societal prob-
lems do not become policy issues just because they exist as problems or because careful scientic
research has documented that they are problems. They must be converted into political issues by
an array of leaders and dened in a way that government can do something about them. (p. 95)
To bridge the divide between scientic knowledge and policy actions, research must be shep-
herded through the policy-making process, from policy formulation to evaluation (Longest, 2006).
The inuence of research on evidence-based health equity policies relies on political momentum
and civic engagement of minority populations experiencing disproportionate health inequities
to move the disparities agenda from low to high importance. Community-based participatory
research (CBPR) spans the division among research, policy, and practice by engaging diverse
stakeholders, including those who are most affected by a policy problem of concern.
CBPR policy–focused efforts aimed at advancing health equity share values rooted in social
justice and human rights, connecting people to social resources, power, or prestige. CBPR links
to these values through policy-directed action. Many CBPR policy partnerships, especially
those that focus on environmental and occupational justice, also highlight the utility of bridg-
ing “street science” with academic-based evidence and advocacy (Garcia et al.,2013; Gonzalez
et al., 2011; see Chapter23).
This chapter briey reviews the role of CBPR in the social ecology of research use, presents
a CBPR policy conceptual model for illustrating the role of CBPR in policy making, and reviews
principles of CBPR within an equity policy framework. It then recommends equity policy com-
petencies for CBPR partnerships that are critical for taking action. As this chapter demonstrates,
although not all CBPR lends itself to policy change, CBPR partnerships with explicit goals of
working within the policy arena and incorporating political action hold promise for advancing
structural and systemic changes for health equity.
THE SOCIAL ECOLOGY OF RESEARCH USE
Tseng (2012, p. 7) describes the social ecology of research use as the process by which “research
unfolds through linkages of relationships, organizational settings, and political and policy con-
texts in which policy decisions are made.” In a landmark report, Prewitt, Schwandt, and Straf
(2012) highlight the uncertain connection between scientic knowledge and how it is used in
public policy and how it can be more effectively used. Shonkoff (2000) describes the transmis-
sion of knowledge to policy making as a complex process characterized as a daunting challenge
because of the three different cultures involved (human services practice, research, and policy).
Each embodies distinct cultures that it needs to learn and adapt in an atmosphere of mutual
respect and understanding of a common purpose (Shonkoff,2000).
For policy making, academic research needs to be enhanced by the knowledge and voice
of those communities who can speak to their real-world experience. Research evidence needs
Community-Based Participatory Research for Health Equity Policy Making 279
to be locally relevant with links to local cultural and political context. Empirically supported
policy interventions in the western mainstream culture may not translate to Indigenous cul-
tures, especially if culturally supported interventions, theories, and local context are excluded
from the research (Nelson, Lefer, & Hansen,2009). Our denition of evidence within a CBPR
approach embraces a variety of forms of evidence including social and basic science research;
expert testimony and local cultural stories; street science; practitioner knowledge; and parent,
youth, and community input.
CBPR creates a pathway by which community members or practitioners, researchers, and
policy makers acquire, interpret, and use research in policy making to advance health equity.
CBPR partnerships have the potential to bridge the “know-do” gap illustrated in Table20.1
by fostering integration and translation of three types of cultures that can be linked to policy
making to reduce social inequalities: (1) science, (2) policy, and (3) community-practice. This
involves bringing together the three types of partners to pursue a course of targeted action that
transcends deeply rooted, and sometimes self-serving, interests of politicians or scientists and
researchers to advance their own agendas or keep political or academic power within their
respective circles. CBPR partnerships rooted in equity policy change can help facilitate the will-
ingness of social scientists to engage in the political process with their community partners and
help forge the willingness of politicians to engage with a set of ideas beyond their class interests
(Cacari Stone, Wallerstein, Minkler, & Garcia,2014).
Although CBPR has the capacity to bridge the gap between science and practice
through community engagement and social action to increase health equity (Wallerstein &
Duran, 2010), fewer CBPR partnerships in the nation have explicitly targeted policy
change. As discussed in Appendix 5, funders investing in CBPR have traditionally come
TABLE 20.1 The “Know-Do” Gap in Advancing Health Equity
How Policy Makers
Perceive Research
How Researchers
Perceive Policy
How Communities and
Practitioners Perceive
Policy and Research
■ Lack of timeliness
■ Politically
irrelevant research
■ Research for the sake
of research
■ Too much focus on
describing and managing
the problem
■ Lack of applicability to
“real-life” solutions
■ Decisions based
on political
preferences and money
■ Lack of scientific evidence
■ Too much partisanship
■ Manipulation of data
to support a political
position or agenda
■ Lack of political
will or action
■ Both disconnected from
real lived experiences of
the persons on whom
they are doing research
or for whom they are
making policy
■ Lack of personal contact
among researchers, policy
makers, and those most
affected by the problem
■ Not enough action
Source: Cacari Stone (2016).
280 Community-Based Participatory Research for Health
from federal agencies, which have slowly begun to support research in environmental and
structural determinants of health. This investment in CBPR in turn has manifested in an
increased interest in a health-in-all-policies approach, which integrates health consider-
ations into policy making and programming to improve the health of all communities and
people (ASTHO,2016).
Two important studies have highlighted the importance of CBPR and health policy. In 2007
and 2012, the W.K. Kellogg Foundation and the California Endowment/Policylink, together with
the School of Public Health, University of California, Berkeley, published reports highlighting
sixteen case studies of CBPR as a strategy for promoting health through policy change. The cases,
in diverse parts of the United States (n = 10) and California (n = 6), respectively (Minkler, Garcia,
Rubin, & Wallerstein,2012; Minkler et al.,2008), were selected in part for their contributions
to successful policy outcomes and with input from national and statewide advisory committees.
Using in-depth, multi-method case study data collection and analysis, the partnerships ranged
geographically from South Central Los Angeles; to Tar Creek, Oklahoma; to East Harlem, New
York. Topics included air pollution and childhood asthma, coercive institutionalization of people
with disabilities, lead paint exposure in Native and rural communities, food insecurity, and an
unusual partnership with homeless skid row youth for education and criminal justice reform to
end punitive practices.
THE LINK BETWEEN CBPR AND POLICY MAKING
To understand the pathways and linkages between community-based participatory research
and healthy public policy, new theoretical frameworks and their testing through the use of
“real-time” policy-focused CBPR projects are needed.
A Conceptual Model
As one important bridge, we present a conceptual model on CBPR and policy making that
has proved useful in theorizing about and in exploring the interplay among civic engage-
ment, political participation, and evidence as it contributes to policy changes that reduce social
inequalities (Cacari Stone et al.,2014) (see Figure20.1). Initial testing of the model focused on
two environmental justice CBPR partnerships in California, one of which, the Environmental
Health Coalition’s (EHC) Toxic Free Campaign in the heavily Latino Old Town National City
(OTNC), San Diego County, is used here to briey illustrate the model. The coalition and its
partners sought to change policy at the local level, the arena most accessible to community-
based participants, and particularly at the stage of building an equity-focused agenda with mul-
tiple partners and sectors.
The majority of policy strategies developed by diverse policy partners across this and
other sites were instrumental in facilitating policy formulation through systematic problem
identication, creating public awareness and bringing “legitimate” attention to the issues
affecting the communities, constructing policy alternatives, and adopting politically feasible
policy objectives. Following is a brief description of the CBPR conceptual model along with
examples from the OTNC project that illustrate how CBPR engages partners who intentionally
set data-informed policy goals and direct strategies toward policy-oriented outcomes (Cacari
Stone et al.,2014; Minkler et al.,2010).
281
CBPR Processes
POLICY MAKING
OutcomesContexts
Macro
Participatory Research
Partnership
Dynamics
Political Action
Policies (formal
/
informal)
Policy Landscape
•Procedural justice
•Distributive justice
∆
∆
∆
Policy
Formulation
Alternatives
Policy
Implementation
Policy Evaluation
& Modification
Problem
Definition
Public Awareness
Agenda-Setting
Health Equity
Outcomes
Policy Change
Adoption
Problem(s)
Policy
Window of Opportunity
Trust/Mistrust
Capacity & Readiness
History
-Economic, Social &
Political
∆
Role of Civic
Engagement
/
Political
Participation
Role of Evidence
FIGURE 20.1 CBPR Policy Model
Source: Reprinted with permission from Cacari Stone, L., Wallerstein, N., Garcia, A., & Minkler, M. (2014). The promise of community-based participa-
tory research for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health, 104(9), 1615–1623.
282 Community-Based Participatory Research for Health
To create our CBPR policy model, we drew on the stages approaches of Kingdon (2003),
Bardach (2000), and Longest (2006). Using varied terminology, each of these models included
(1) problem denition, (2) creating awareness and setting (or getting on) policy-maker agendas,
(3) constructing policy alternatives, (4) deciding on the policy to pursue, (5) implementing the
policy, and (6) evaluation. Although some policy scholars have criticized these steps for over-
simplifying complex political processes (Sabatier,2007), they contributed practical insights,
emphasizing the cyclical and interconnected nature of policy making, and the role of contex-
tual factors and “windows of opportunity” when factors converge to increase the likelihood of
policy change (Breckwich Vasquez et al.,2007; Longest,2006).
The rst oval, “Context,” refers to macro-contextual factors (e.g., the socio-cultural-
economic environments, political leadership and power, public attitudes, and policy trends) and
the participatory research context. The latter includes patterns of trust (or distrust) among com-
munities, agencies, and university partners; organizational characteristics; and their capacity
for high-quality collaborative research. For instance, the macro context in OTNC included a
decades’ earlier decision by an all-white San Diego city council to transform the neighborhood
from a residential community to a “light industrial/mixed-use neighborhood,” enabling pollut-
ing industries to move into this low-income area (Environmental Health Coalition,2005).
The second oval, “CBPR Processes,” includes partnership (stakeholder) dynamics and
addresses questions such as “Are there policy makers who are already committed to the issue?”
and “Are there democratic decision-making processes in place among partners?” It also includes
the dynamic interplay between the role of science and evidence and the role of civic engage-
ment. Such work includes traditional outside expert–driven research studies and compelling
street science, in which community members take the lead in collecting data capturing their
often-sophisticated understanding of issues affecting their neighborhoods. Civic engagement
refers to the role of community partners in organizing and advocacy, roles that may be more dif-
cult or restricted for academic or government agency partners, and how community partners
can integrate evidence into their organizing strategies.
The EHC in OTNC included multiple research methods in its Toxic Free Campaign, for
example, secondary data analysis, geographic information systems (GIS) mapping, surveys,
and air sampling. Resident members of the coalition conducted door-to-door surveys and col-
lected data on ultrane particulate matter, which an academic partner had linked to adverse
lung development. A staff member further created “visual footprints” from GIS mapping,
which graphically compared toxic releases for OTNC with those of adjacent areas with star-
tling results: 23,000 pounds of toxic air contaminants were released in OTNC in 2005, whereas
nearby footprints contained 6,000, 3,500, and 0 pounds. Trained community partners not only
understood these data but also presented them at city council meetings and in other venues
(Environmental Health Coalition,2005).
The “Policy Making” circle includes in the center the problem(s) to be addressed and,
around the periphery, the stages in which CBPR partnerships may be engaged. The policy-
formation stage involves multiple dynamic strategies, which are not necessarily linear. These
include agenda-setting; dening and prioritizing the problems within a given political envi-
ronment, creating awareness of the issue(s) among key policy makers and the public, con-
structing policy alternatives based on what is timely and feasible, deciding which policies to
pursue, and advocating for proposed changes and policy adoption. The last stages in particular
Community-Based Participatory Research for Health Equity Policy Making 283
typically involve drawing on research ndings and community members’ stories and experi-
ences. Choices tend to be made when the right combination of conditions, politics (e.g., moods
or leadership turnover), and policies (acceptance of ideas by policy makers) converge, creating
“policy windows” of opportunity. These windows may open at any stage of the policy-making
process (Kingdon,2003).
The EHC’s (2005) publication of surveys, GIS ndings, and recommendations in a widely
cited report was described by policy makers as having played an important role in formulating
policy strategies, such as media advocacy, door-knocking, brieng public ofcials, and testi-
fying at hearings. Although the academically trained research partners participated in testimony,
promotoras and other residents were at the center of such efforts, including identifying policy
strategies most likely to be effective (Minkler et al.,2010).
Finally, the “Outcomes” circles include policy changes, such as catalyzing political activity
(i.e., new leadership, increased civic engagement), formal and informal policies (ordinances,
action plans), and changes in the policy landscape. These outcomes, in turn, may increase the
likelihood of future policy change and greater opportunity for two forms of justice: distributive
justice, or equal protection and fair allocation of burdens and resources, and procedural justice,
or fairness in how the decision-making process takes place, with marginalized communities
participating in the policy-making process (Minkler,2010; see Chapter21).
In OTNC, policy maker and other stakeholder interviews, review of mass media, docu-
ments, and observations at hearings suggested that the EHC partnership played a key role in the
unanimous passage, by the city council, of an amortization ordinance, requiring that polluting
businesses be relocated outside the community within a specied period of time. The partner-
ship’s continued efforts further contributed to OTNC’s becoming the rst city in the state to
include environmental justice in its general plan (Minkler et al.,2010). Evidence of increased
procedural justice also was seen, including enhanced involvement of community members in
city council meetings, growing youth interest in advocacy work their parents began, and one
former promotora not only winning a seat on the city council but also going on to serve twice as
the town’s vice mayor (Minkler et al.,2010).
TAKING ACTION TO ADVANCE HEALTH EQUITY: CBPR POLICY
PRINCIPLES, GOALS, STRATEGIES, TARGETS, AND TOOLS
In addition to using the CBPR policy model to identify partnership contexts, participatory strat-
egies, and policy actions for an equity vision, CBPR partnerships may also consider several
benchmarks for readiness: (1) adapting principles of equity that challenge the underlying ide-
ologies that inuence the decisions made by powerful industries, political insiders, and elites;
(2) framing a policy goal from an equity lens; (3) selecting policy strategies; (4) identifying a
target; and (5) using policy analysis tools.
Adapting Principles of Equity That Challenge the Underlying Ideologies That
Influence the Decisions Made by Powerful Industries, Political Insiders, and Elites
In applying CBPR for policy change, we underscore the importance of a partnership’s adoption
of principles that span three approaches: CBPR, equity, and equity policy (see Box20.1). CBPR

284 Community-Based Participatory Research for Health
partnerships often have principles that value the rich diversity and contributions of partners. Yet,
this may not necessarily carry over into work for more distal structural changes that tackle the
unfair distribution of resources or systemic issues related to power and privilege.
The complementarities of CBPR and policy-focused change are well captured in social
justice concerns with distributive justice and procedural justice. Freudenberg expands on
the principle of equity in policy by calling for identifying intersectional positions of power
and privilege (see Chapter4) and cultural humility (see Appendix 4) in modifying the social
Box 20.1 Adding Principles of Equity and Equity Policy to CBPR Principles
Health Equity
■ Recognizes the human right to health, dened as the right to attain the highest possible standard
of health—remove obstacles to health in any sector (e.g., education, housing, or transportation)
(Whitehead,1992)
■ Embraces nondiscrimination and equality—everyone has equal rights, and governments are
obligated to prohibit policies that have either the intention or the effect of discriminating against
particular social groups; prohibit de facto (unintentional or structural) as well as intentional
discrimination
■ Addresses social justice in health—striving for the highest possible standard of health for all
people and giving special attention to the needs of those at greatest risk of poor health and who
are economically and socially disadvantaged (Braveman et al.,2017)
Equity Policy
■ Commits to distributive justice, equal protection and fair allocation of burdens and resources and
procedural justice or fairness in how the decision-making process takes place with marginalized
communities participating in the policy-making process (Minkler,2010); beyond (re)allocation of
resources, includes equal concerns about the nature of relationships among persons (Powers &
Faden,2006)
■ Respects mutuality in relationships
■ Equalizes power dynamics among diverse partners in the policy-making process
■ Confronts social subordination as a threat to social justice and human rights
■ Counteracts stigma of diverse populations, especially those who have been traditionally dened
as “other”
■ Supports capacities for self-determination
■ Recognizes the role of intersectional positions of power and privilege and cultural humility in
conducting community and applied research policy research
■ Leverages social policies to ameliorate economic or social disadvantage, such as minimum wage
laws, progressive taxation, and statutes barring discrimination in housing or employment based
on race, gender, disability, or sexual orientation
Community-Based Participatory Research for Health Equity Policy Making 285
determinants of health (Freudenberg & Tsui,2014). To best realize this potential, however,
a deeper understanding of key factors is needed. These include the roles of scientic evi-
dence and political power in bringing about policy change; the appropriate scales for policy
change, from community to global; and the participatory processes that best acknowl-
edge the interplay between power and evidence. Themba (1999) argues that community-
academic partnerships should address power and help move accountability, pushing the
public debate to the next level by growing and moving the parameters of research into the
political realm.
To complement the principles of CBPR discussed in this book (see Chapter3), principles of
equity and equity policy may help further strengthen policy-focused CBPR practice.
Framing a Policy Goal from an Equity Lens
The rst step in a CBPR partnership is to establish processes for the community to identify
and frame the goal from an equity lens. In the National Academy of Sciences publication “Get
Ready for Equity,” Burke (2016) lists several central “equity competencies”: common language,
historical context, privilege and oppression, and policy and commitment to ongoing learning.
In agreeing on a common language, partners should nd a shared meaning in ways that support
the intent of the collaboration. Going beyond the use of the term disparities, as the noting of
differences, for example, the term equity connotes unfair and avoidable conditions, with deep
understanding of the historical context of oppression, power suppression, and their intergener-
ational impacts on communities. To build collective wisdom and insights on systemic patterns
in inequitable relationships, Jones (2016) underscores the importance of recognizing and rec-
tifying historical injustices as a fundamental action step toward achieving health equity. In a
comparison of an urban and rural CBPR case study, Devia and colleagues (2017) report how
partners shaped social justice strategies for policy change based on analyses of local histories
and root causes of inequities.
Setting a goal to address privilege and oppression is another avenue for developing an
equity lens. It is important to name racism, sexism, homophobia, ableism, xenophobia, and
Islamophobia as forces in determining how these social determinants are distributed within a
given geography or community. Collective insights as to how power and oppression interplay at
the personal, community, and systemic levels are core to evaluating, developing, or implement-
ing policy. It is important to embrace ongoing learning and a commitment to humility in seeking
growth in knowledge and skills among partners. Talking about privilege, oppression, and histor-
ical injustices such as racism and genocide can be challenging for diverse audiences, yet they
are core to creating a policy goal from an equity lens.
Selecting Policy Strategies
After adapting principles of equity policy and selecting a policy goal, CBPR partners will need
to determine who has the power to make the change, whether that be an elected ofcial, a
planning commission, or a business. Although the focus of this chapter is primarily on efforts
to inuence local public policy, efforts to bring about similar policy changes at higher levels or
in relevant private sector arenas should also be considered, especially in partnership with other
CBPR or advocacy groups in other jurisdictions. Let us now look at a range of possible policy-
related strategies.
286 Community-Based Participatory Research for Health
Voluntary Agreements Voluntary agreements are “pacts between a community and one or
more institutions that outline conditions, expectations, or obligations without the force of law”
(Themba,1999, p. 91). Such agreements provide a useful alternative to more formal regula-
tions when there is not sufcient support for enacting such regulations. A voluntary agreement
may be an interim step toward more meaningful changes in policy, either because the voluntary
agreements do not solve the problem or because some large organizations prefer public policy
change to negotiating many agreements with many communities. Ideally, a written memo-
randum of understanding (MOU) should be developed that clearly spells out the conditions of
each agreement, with appropriate oversight of implementation.
Prior to working for a healthy retail measure in San Francisco, incentivizing merchants
in low-income “food swamps” to offer less alcohol and tobacco and more fresh produce (see
Chapter21), a CBPR partnership in one low-income neighborhood campaigned to get local
merchants to sign voluntary agreements to stock healthier foods. These agreements led to
improvements in nutritional choices for local residents and helped provide some of the evidence
base for later efforts to pass legislation supporting a more formalized program citywide (Breck-
wich Vasquez et al.,2007; Chapter21).
Legal Actions Well-framed legal actions, such as lawsuits and other court actions, can also
accomplish signicant long- and short-term goals, even if they simply result in getting the other
party to the table. Yet such actions can be tedious and expensive as well as a major distraction
if not integrated into a broader community agenda (Themba,1999). Further, failure to identify
the right defendants (for example, the parent company of a major local polluter) can lead to
embarrassing and demoralizing defeats. In lieu of (or in addition to) bringing a lawsuit, simply
ling complaints about bad or illegal practices with the appropriate regulatory agency can be
an effective policy approach. In recent years, community and advocacy groups have used legal
action against the food, pharmaceutical, and tobacco industries (Freudenberg,2014) and against
local governments. In the South Bronx, New York, the Morris Justice Project (MJP) is a par-
ticipatory research partnership of residents, academics, lawyers, artists, and activists. Although
legal challenges have not been central to their work, the MJP was in fact born in 2011 after
local mothers, upset about the frequency of police harassment experienced by their sons under
a “stop-and-frisk” policy, took part in a court case that effectively challenged such policing in
private apartment buildings (see Chapter22). More recently, the MJP worked with the law rm
helping a California city successfully call for the reform of a controversial police “carding”
policy, which also had been based on racial proling.
Studies and Moratoriums Mandated studies and moratoriums pending data collection can be
helpful under certain circumstances. Although CBPR can uncover valuable information about
an unhealthy or unlawful institutional practice, far more extensive study may be necessary to
collect the hard data needed to support a policy change. In such instances, CBPR partners may
identify a policy goal of getting a mandated study or other data collection activity performed
(or protecting what is currently being collected, such as data on racial or ethnic disparities
in health).
Relatedly, a useful policy approach may involve calling for a moratorium on continued
enactment of existing policy until more data are available. For example, during conicts about
Community-Based Participatory Research for Health Equity Policy Making 287
local and state laws that would dictate the process for locating polluting facilities, environ-
mental justice activists in West Harlem called for a moratorium on siting new facilities in their
neighborhood to protect their community and to set a precedent that could guide future action.
The breathing time allowed by a moratorium may also permit CBPR partners to organize neigh-
borhood hearings or town hall meetings, with stories and numbers, for legislators in attendance
(Wallack, Woodruff, Dorfman, & Diaz,1999).
Electoral Strategies Electoral strategies, similar to legal approaches, tend to be time- consuming
and labor intensive. Yet such approaches, including ballot initiatives, referendums by citizens,
and even support of candidates, can have a considerable payoff over the longer term. There
may be short-term payoffs as well. Electoral campaigns can raise the prole of an issue, attract
volunteers, and pull an issue out of the purview of non-supportive policy makers and place it
directly before a more supportive public. CBPR partners can often facilitate bringing an issue
to public attention.
Each of these policy-related approaches—voluntary agreements, legal actions, mandated
studies, moratoriums, and electoral strategies—has advantages and disadvantages that must
be carefully weighed by CBPR partners in their efforts to select the alternative most likely
to succeed.
Identifying a Target
As noted, decisions about the particular policy approach best suited to a given CBPR effort
should be driven, in part, by a careful analysis of the most appropriate change target or decision-
making body with the power to bring about the changes sought. Several key questions may be
helpful to community members and their outside research partners as they choose an appro-
priate target:
■ Who or what institutions have the power to solve or ameliorate the problem and grant the
community’s demands?
■ Are there key actors who must be approached rst as gatekeepers to the people with
real power?
■ What are the most powerful and strategic inuences on the targets (for example, voters,
consumers, faith-based organizations, investors, neighborhood organizations)?
■ Who would have jurisdiction if you redened the issue (for example, if you turned a
tobacco advertising issue into a question of fair business practices)? Would this increase
your likelihood of success? (Themba,1999).
As these questions suggest, each decision-making body or target selected will require differ-
ent organizing strategies to move it to action. A critical part of the CBPR process will, therefore,
be conducting strategic analyses to narrow down potential targets and researching each target’s
self-interests, strengths, and vulnerabilities (Appendix 12). Not infrequently, such research will
reveal the existence of a more vulnerable primary target with whom the possibility of success is
greater. In other instances, CBPR partners may need to identify additional, secondary targets to
bring about the desired change.
Finally, CBPR participants need to assess the capacities of their partnership and identify the
existing competencies and needed training for conducting policy analysis.
288 Community-Based Participatory Research for Health
Using Policy Analysis Tools
In CBPR partnerships, tools for achieving policy-oriented outcomes include raising public
awareness of the impact of socioeconomic factors in health; engaging low-resourced and racial-
ethnic communities in policy-making activities; building momentum of coalitions for grassroots
organizing; applying media advocacy; and strengthening leadership, research, and policy-
advocacy skills of communities.
CBPR partnerships need to invest in their ability to conduct policy analysis using various
forms of evidence to make the case for change. Our CBPR policy model overemphasizes the
role of CBPR in policy making and underemphasizes other factors that usually dominate the
agendas and decision-making process. These include economic pressures, the role of the media,
and other social and political forces that have independent and direct paths to the policy-making
process. CBPR partners may wish to conduct a strategic power analysis to determine who has
the power to make the change at the local or larger jurisdiction. Power mapping (see Appendix
12) and other tools are useful in enabling partners to become well versed in determining and
analyzing the key set of players in the policy-making process.
It is also important for CBPR partnerships to diversify their focus of analysis beyond pro-
grammatic, clinical, or community-based interventions to a focus on the “structures” that deter-
mine health (systems and policies) (WHO,2005). The use of qualitative and quantitative data
may be necessary to link the interrelationships between factors at the individual level and within
the social context that increase the likelihood of achieving and maintaining good health. Tools
such as health equity impact assessments, digital storytelling, and mapping of visual data (see
youth mapping environmental hazards in Brazil, Chapter23), geocoding, and development of
indices or measures of the SDoH (e.g., racial segregation indices, redlining) may be useful here.
Similarly, the use of storytelling and side-by-side comparisons of promising or evidence-based
policy interventions that list each of their trade-offs (human, economic) often are instrumental
in equity-focused policy analyses.
Finally, through the use of social media and alternative communication strategies (e.g.,
radio, storytelling, infographics), CBPR expands the potential for translation and dissemination
of various forms of evidence across diverse communities through strategies to redress power
imbalances (Wallerstein & Duran,2010). CBPR presents exciting opportunities for multimedia
and multi-sectoral dissemination of research results and policy change, especially concerning
the impact of research on health equity for underrepresented populations.
CONCLUSION
CBPR has been an important asset in bridging the gap among researchers, policy makers,
and community members and practitioners. CBPR partners have identied, made visible, and
legitimized issues so that they get on the public’s agenda. It has also helped community advo-
cates and their CBPR partners to attract media attention for long-standing but long-ignored
issues when there are newsworthy ndings. The best initiatives use research as a means of
documenting and elucidating problems that are already of concern to communities, and they
do so in ways that build condence in community-based knowledge and ways of knowing
(Chapter2).
Community-Based Participatory Research for Health Equity Policy Making 289
CBPR focused on policy change faces numerous obstacles, including the reluctance of some
partners to participate, believing that they cannot legally do so, or that policy is too abstract to
deal with effectively. Further, even powerful community data may be addressed informally yet
discounted in policy considerations as not being rigorous enough to inform decision making.
Despite such constraints, however, CBPR can be an agent for the democratization of information
through bringing about the active involvement of communities in data gathering and by giving
community-based groups equal access to the kinds of data that drive policy making. It can help
communities inuence the policy process in ways that can benet the groups of which they are
a part. CBPR partnerships are, of course, only one inuence on policy. Yet, as examples in this
and other chapters illustrate, community groups, academic researchers, and policy makers who
are intentional about setting and achieving equity policy outcomes from the beginning can build
CBPR projects that result in lasting, formal changes that, in turn, can promote health and help
tackle structural and historical inequities.
QUESTIONS FOR DISCUSSION
1. Although its action orientation would seem to make policy work a natural for CBPR,
community and academic partners may be reluctant to move into this area. What are some
reasons for this reluctance? As a partner who sees potential for engaging in a policy-related
action, what arguments might you make to encourage your partners to consider becoming
engaged in this arena?
2. In what ways are goals different between CBPR partnerships that seek to advance population
health (at individual, organizational, or community levels) and those that explicitly set an
equity vision toward policy change? (Compare examples of CBPR partnerships you know
or are described this book.)
3. Using the CBPR policy model, divide into groups based on common interests (for example,
reproductive rights, environmental justice, or health care for the uninsured). Think of a real
or hypothetical policy you would like to see enacted and identify where in the policy-
making process is the leverage point of action (for example, agenda setting, modifying an
existing policy to include equity-oriented provisions). Brainstorm strategies described in
this chapter that your partnership could take to make policy, strengthen your allies, and
help bring about the change you seek.
REFERENCES
Association of State and Territorial Health Ofcials (ASTHO). (2016). Triple aim: Implementing a “health in all pol-
icies” approach with health equity as the goal. Retrieved February 22, 2017, from www.astho.org/Health-Equity/2016-
Challenge/Implementing-a-health-in-all-policies-approach-with-health-equity-as-the-goal/
Bardach, E. (2000). A practical guide for policy analysis: The eightfold path to more efffective problem solving. New York, NY:
Chatham House.
Braveman, P., Arkin, E., Orleans, T., Proctor, D., & Plough, A. (2017). What is health equity? And what difference does a
denition make? Princeton, NJ: Robert Wood Johnson Foundation.
290 Community-Based Participatory Research for Health
Breckwich Vasquez, V., Lanz, D., Hennessey Lavery, S., Facente, S., Halpin, H. A., & Minkler, M. (2007). Addressing
food security through public policy action in a community-based participatory research partnership. Health Promotion
Practice, 8(4), 342–349.
Burke, N. (2016). Get ready for equity. Framing the dialogue on race and ethnicity to advance health equity. Proceedings of
a Workshop. National Academy of Sciences.
Cacari Stone, L. (2016). Lost in translation learning module: Health policy, politics and social justice. PH 554. Albuquerque,
NM: College of Population Health, University of New Mexico.
Cacari Stone, L., Wallerstein, N., Garcia, A., & Minkler, M. (2014). The promise of community-based participatory research
for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health, 104(9),
1615–1623. doi:10.2105/AJPH.2014.301961
Campbell, S., Benita, S., Coates, E., Davies, P., & Penn, G. (2007). Analysis for policy: Evidence-based policy in practice.
London, UK: Government Social Research Unit.
Devia, C., Baker, E., Sanchez-Youngman, S., Barnidge, E., Golub, M., Motton, F., Muhammad, M., Ruddock, C., Vicuña, B.,
& Wallerstein, N. (2017). CBPR to advance social and racial equity: Urban and rural partnerships in Black and Latino
communities. BMC International Journal of Health Equity, 16, 17. doi:10.1186/s12939–016–0509–3
Environmental Health Coalition. (2005). Reclaiming Old Town National City: A community survey. National City, CA: Author.
Freudenberg, N. (2014). Lethal but legal: Corportations, consumption, and protecting public health. Oxford, UK: Oxford
University Press.
Freudenberg, N., & Tsui, E. (2014). Evidence, power, and policy change in community-based participatory research.
American Journal of Public Health, 104(1), 11–24.
Garcia, A. P., Wallerstein, N., Hricko, A., Marquez, J. N., Logan, A., Nasser, E. G., & Minkler, M. (2013). THE (Trade,
Health, Environment) Impact Project: A community-based participatory research justice case study. Environmental
Justice, 6(1), 17–26.
Gonzalez, P. A., Minkler, M., Garcia, A. P., Gordon, M., Garzon, C., Palaniappan, M.S.C., Prakash, S., & Beveridge, B.
(2011). Community-based participatory research and policy advocacy to reduce diesel exposure in West Oakland,
California. American Journal of Public Health, 101(S1), S166–S175.
Jones, C. (2016, November). Keynote address to the American Public Health Association, Denver, Colorado.
Kingdon, J. W. (2003). Agendas, alternatives, and public policies (2nd ed.). New York, NY: Longman.
Lavis, J. N., Lomas, J., Hamid, M., & Sewankambo, N. K. (2006). Assessing country-level efforts to link research to action.
Bulletin of the World Health Organization, 84(8), 620–628.
Longest, B. B., Jr. (2006). Health policymaking in the United States (4th ed.). Chicago, IL: AUPH/Health Administration Press.
Minkler, M. (2010). Linking science and policy through community-based participatory research to study and address health
disparities. American Journal of Public Health, 100(S1), S81–S87.
Minkler, M., Breckwich Vásquez, V., Chang, C., et al. (2008). Promoting healthy public policy through community-based
participatory research: Ten case studies. Oakland, CA: PolicyLink.
Minkler, M., Garcia, A., Rubin, V., & Wallerstein, N. (2012). Community-based participatory research: A strategy for
building healthy communities and promoting health through policy change. Oakland, CA: PolicyLink. Retrieved February
22, 2017, from www.policylink.org/sites/default/les/CBPR.pdf
Minkler, M., Garcia, A. P., Williams, J., LoPresti, T., & Lilly, J. (2010) Si Se Puede: Using participatory research to promote
environmental justice in a Latino community in San Diego, California. Journal of Urban Health, 87(5), 796–812.
Nelson, S. R., Lefer, J. C., & Hansen, B. A. (2009). Toward a research agenda for understanding and improving the use
of research evidence. Portland, OR: Northwest Regional Educational Laboratory. Retrieved from www.nwrel.org/
researchuse/report.pdf
Northington-Gamble, V., & Stone, D. (2006). U.S. policy on health inequities: The interplay of politics and research. Journal
of Health Politics, Policy and Law, 31(1), 93–126.
Powers, M., & Fadden, R. (2006). Social justice: The moral foundations of public health and health policy. Oxford, UK:
Oxford University Press.
Prewitt, K., Schwandt, T. A., & Straf, M. L. (2012). Research on the use of science in policy: A framework. Using science as
evidence in public policy (Chap. 4, pp. 53–63). Washington, DC: National Research Council, The National Academies
Press. doi:https://doi.org/10.17226/13460
Community-Based Participatory Research for Health Equity Policy Making 291
Rigby, E. (2005). Linking research and policy on Capitol Hill: Insights from research brokers. Evidence and Policy,
1(2), 195–213.
Sabatier, P. A. (2007). Theories of the policy process (2nd ed.). Boulder, CO: Westview Press.
Shonkoff, J. P. (2000). Science, policy and practice: Three cultures in search of a shared mission. Child Development,
71(1), 181–187.
Themba, M. N. (1999). Making policy, making change: How communities are taking law into their own hands. San Francisco,
CA: Jossey-Bass.
Tseng, V., & the Senior Program Team. (2012). The use of research in policy and practice. William T. Grant Foundation Social
Policy Report, 26(2).
Wallack, L., Woodruff, K., Dorfman, L., & Diaz, I. (1999). News for a change: An advocate’s guide to working with the
media. Thousand Oaks, CA: Sage Publications.
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(S1), S40–S46.
doi:10.2105/AJPH.2009.184036
Whitehead, M. (1992). Concepts and principles of health equity. Health Promotion International, 6(3), 216–228.
WHO. (2005). Priorities for research to take forward the health equity policy agenda. WHO Task Force on Research Priorities
for Equity in Health WHO Equity Team. Bulletin of the World Health Organization, 83, 948–995.

21
CHAPTER
IMPROVING FOOD SECURITY
AND TOBACCO CONTROL
THROUGH POLICY-
FOCUSED CBPR
A CASE STUDY OF HEALTHY RETAIL IN
SAN FRANCISCO
MEREDITH MINKLER, JENNIFER FALBE, SUSANA HENNESSEY LAVERY,
JESSICA ESTRADA, AND RYAN THAYER
FOOD INSECURITY, OR “limited or uncertain access to adequate food” (Coleman-Jensen,
Gregory, & Singh,2014, p. 4), is a fact of life for one in seven Americans. As Farley and Sykes
(2015) point out, however, “the problem in poor neighborhoods isn’t a shortage of food, but a
shortage of healthy food” (p. A19). Although half of high-income zip codes have at least one
supermarket, just one in six low-income zip codes do. Further, although supermarkets in high-
income zip codes devote an average of almost 280 feet of shelf space to fresh produce, small
stores had just 9 feet, with three times as much space going to chips, sugary beverages, candy,
and the like (Farley et al.,2009).
294 Community-Based Participatory Research for Health
In neighborhoods such as San Francisco’s low-income Tenderloin District, the problem
of food insecurity intersects with an overabundance of advertising, display, and availability of
alcohol and tobacco in the local retail environment. Poor diets, smoking, and heavy drinking
contribute to the disproportionately high rates of morbidity and premature mortality (San Fran-
cisco Department of Public Health [SFDPH],2012). This chapter begins with a brief overview
of San Francisco’s Tenderloin neighborhood and the Tenderloin Healthy Corner Store Coali-
tion (the coalition). We then present the conceptual framework and methods used to explore
the coalition’s CBPR processes, ndings, and contributions to neighborhood and policy-level
change (e.g., through municipal legislation creating a successful healthy corner store retail
program). We conclude by discussing some of the challenges and takeaway lessons from this
case study.
OVERVIEW OF THE TENDERLOIN AND ITS HEALTHY CORNER
STORE COALITION
The Tenderloin is one of San Francisco’s poorest neighborhoods, with 35 percent of its thirty-
two thousand residents living below the federal poverty line compared to a citywide average
of 14 percent (City Data, 2015). With no full-service grocery store and more than seventy
corner stores primarily stocking prepackaged food, sodas, tobacco, and alcohol, lack of access
to healthy food is a signicant problem. The Tenderloin also has by far the highest tobacco
and alcohol outlet density in the city and correspondingly elevated rates of tobacco use and
alcoholism (SFDPH,2012). Together with deep health and social inequities and the chronic
stressors associated with life in poor neighborhoods, these forces are key contributors to the
poor health of residents, who have some of San Francisco’s highest rates of heart disease, can-
cer, and premature death (SFDPH,2012).
The precursor to what was to become the Tenderloin Healthy Corner Store Coalition (www.
healthyTL.org) evolved in 2011 from a tobacco-free initiative in the neighborhood. When a
youth-driven assessment graphically illustrated the plethora of tobacco advertising and avail-
ability and poor access to healthy foods in the neighborhood’s corner stores, it resonated with
several community-based organizations and agencies, which began meeting to discuss the
problem. Formalized the following year, the coalition was initially co-led by two organiza-
tions—the Vietnamese Youth Development Center (VYDC) and the Tenderloin Neighborhood
Development Corporation (TNDC)—and included diverse community-based organizations,
staff members from the local health department (DPH), and other city agencies, local residents,
and university partners from UC Berkeley and UCSF.
Central to the work of the coalition was the training and hiring of ve local residents as “food
justice leaders” (FJLs). Modeled in part on the food guardians active in the similarly food insecure
Bayview Hunters Point neighborhood through its Southeast Food Access (SEFA) coalition (www.
southeastfoodaccess.org), FJLs are local residents hired and trained for their roles as participatory
researchers, community organizers, and advocates. Their detailed corner store assessments, resi-
dent surveys, merchant and resident education, organizing, and policy advocacy, together with the
work of the larger coalition and its allies, played an important role in helping secure the passage
and implementation of legislation in fall 2013, creating the city’s Healthy Food Retailer Incentive
Program (www.HealthyRetailSF.org) described in this chapter.
Improving Food Security and Tobacco Control through Policy-Focused CBPR 295
CONCEPTUAL FRAMEWORK
To explore the processes and outcomes of the coalition and its work, particularly in helping
effect policy change and monitor and evaluate implementation outcomes, we used a theoretical
framework that combined Kingdon’s (2003) model of the three streams in the policy-making
process with the CBPR and policy engagement model described in Chapter20 (see also Cacari
Stone, Wallerstein, Garcia, & Minkler,2014).
Although policy making proceeds in a nonlinear fashion and is embedded within chang-
ing sociohistorical contexts (Bardach,2005; Birkland,2015; Cacari Stone et al.,2014), several
policy steps “shape the content, course, pace, and development of policy” (Breckwich Vásquez
et al.,2007, p. 358). Typically, they include problem denition or identication of an issue, cre-
ating awareness and getting on the policy makers’ agenda, considering different policy options
and deciding on one to pursue, negotiating for a policy win, and implementing the policy.
Finally, and although not included in all policy-making models, monitoring and evaluating out-
comes of policy implementation is a critical part of the process.
Kingdon (2003) combined these steps into three streams: the problem stream, convincing
decision makers a problem exists and building awareness; the politics stream, proposing fea-
sible, politically attractive solutions; and the policy stream, negotiating the politics to get
approval of a proposed measure. Kingdon further noted that when positive developments
occur in all three streams, a policy window of opportunity opens, increasing the likelihood
of success.
As described in Chapter20, Cacari Stone and her colleagues’ (2014) pathways model of
how CBPR can help promote policy change builds on the broader CBPR model used through
much of this book, while adding an explicit focus on policy-making stages. It highlights, as
well, “the interaction between evidence and civic engagement to shift political power” toward
equity-focused policy outcomes (Cacari-Stone et al.,2014, p. 1621).
ROLE OF THE COALITION IN LINKING CBPR AND POLICY MAKING
Drawing on Kingdon’s (2003) three streams in the policy-making process, and Cacari-Stone
et al.’s (2014) pathways model of CBPR and policy making previously described, we now
examine the role and functioning of the Tenderloin Healthy Corner Store Coalition and its
CBPR efforts and contributions to policy and related change.
The “Problem Stream” and Creation of a Grassroots Coalition
Although substantial literature exists on the associations among tobacco marketing, lack of
access to healthy foods, and poor health (Butler, Aboelata, Cohen, & Spilker, 2013; Farley
et al.,2009; Feeding America,2014), to effectively create awareness of the problem and reach
the public and policy makers, local data that “hit home” are particularly useful.
In the Tenderloin, an “apple map” created by the Vietnamese Youth Development Center,
with support from DPH, was exemplary. Based on data they had collected from thirty-ve of the
Tenderloin’s then seventy-three corner stores, the youth created an apple map by using Google
Maps, using the image of an apple, half an apple, and most often, a rotten apple core to help bring
their ndings alive. They showed that 42.4 percent of stores had no fresh produce, 85 percent
296 Community-Based Participatory Research for Health
lacked the required “no smoking” signs posted, and 75.8 percent had more than one-third of
their storefronts covered with advertising, mostly for alcohol, tobacco, sugary drinks, and junk
food. In all, just 19 percent of the stores received a “good apple” rating, with close to two-thirds
(65.6 percent) rated “rotten apples” (Estrada & Mathews,2012). Together with earlier CBPR
studies on the lack of healthy food access and heavy tobacco concentration in the city’s Bay-
view neighborhood (Breckwich Vásquez et al.,2007; Hennessey Lavery et al.,2005), this local
evidence attracted attention and helped effect change. On the neighborhood level, the DPH
encouraged the youth researchers to distribute the mandatory no smoking signs to all of the
stores that were not in compliance, an action that boosted compliance by 82 percent (Estrada &
Mathews,2012).
Effective sharing of their data also increased policy maker attention to the problem. After
seeing the apple map, a local supervisor visited the Tenderloin and commented, “A lot of stores
are covered in cigarette and alcohol ads, or junk food and drink ads... I’ve really come to see
food access as a civil rights issue. Many people don’t have access to affordable, good-quality
food at a fair price, and corner stores are a key part of this.”
In CBPR, as Cacari Stone et al. (2014) note, partnership dynamics affect the roles of evi-
dence, and civic engagement and political participation. To involve more community residents
and organizations in further rening the problem and identifying potential ways to approach it,
a community meeting was called by a local agency—the Community Benets District—which
was among several organizations for which the youths’ apple map was a catalyst to action.
Attended by about sixty residents and representatives of the DPH and local community-based
organizations (CBOs), the meeting generated considerable interest. As a convener commented,
“we had various topics for the community to give input on, but converting the corner stores
from something negative into having a positive inuence on the neighborhood had the greatest
support” (Flood et al.,2015, p. 660). This desire for ownership, coupled with the shared goal of
creating broader awareness and understanding of the problem to effect change, culminated in
the formalization and naming of the Tenderloin Healthy Corner Store Coalition.
The coalition’s regular organizational and individual members met monthly, sometimes
joined by an architect interested in healthy retail and members of a local mosque and of the
Arab American Grocers Association. Described by an early coleader as a “very, very, very
diverse” group, the coalition sometimes experienced tensions based, in part, on this diversity.
Yet it quickly emerged as a highly effective organization because of its strong inclusive leader-
ship and its members’ unifying belief that “food is a health equity issue” (Gomez et al.,2013).
Finally, and commenting on the collaborative, community-driven process, a participant noted
that for regular coalition meetings, members “drop [personal or organizational] agendas at the
door” and focus on activities they are conducting in support of their collective goal.
The “Politics Stream” and the Coalition’s Research and Advocacy Contributions
Building on the early apple map data, and lessons learned from the Bayview work, the coalition
further honed in on the goal of improving access to healthy foods and decreasing availability of
tobacco and other unhealthy products in a form that made sense within the community: turning
corner stores into community assets through conversion to healthy retail.
To make the case for action promoting healthy retail, food justice leaders led in gathering
more data on the needs and concerns of local residents to be shared locally and with policy
Improving Food Security and Tobacco Control through Policy-Focused CBPR 297
makers. A 2012 multilanguage survey of 640 residents revealed that most participants shopped
outside the neighborhood for staples (e.g., produce, dairy, meat and poultry, and grains), repre-
senting close to 50 percent of their total grocery expenditures. Extrapolating from these gures,
TNDC staff members estimated that the neighborhood was losing some $11 million in revenue
each year (Gomez et al.,2013). These stark realities, and the fact that close to 80 percent of
respondents reported that they would buy healthy food locally if it were available and afford-
able, were seen by coalition members as underscoring the need for healthier, more comprehen-
sive food options locally, which could also strengthen the local revenue base.
The Vietnamese Youth Development Center (VYDC) and the coalition held a joint press
conference in December 2012 sharing their survey ndings and those of the earlier apple map
study to help leverage support for change (Estrada & Mathews,2012). Coverage included a
piece on local public radio featuring the voices of several involved youth and an article in a
district supervisor’s newsletter. As another policy maker remarked, “The fact that local people
provided actual numbers and facts from work on-the-ground made a difference,” because any
proposed policy measure “has to have support from the community.”
Community support, however, also needed to come from local merchants, who could be
resistant to a policy measure that might discourage the selling of what many perceived as their
most protable items: tobacco and alcohol. The coalition, SFDPH, and a nonprot design and
architecture rm specializing in grocery store retailers, Sutti & Associates, educated merchants
about the strong prot margins on dairy, bread, meat, and fresh produce (25 to 50 percent, and
sometimes exceeding 100 percent for precut fruit and salads), compared to 15 to 25 percent on
tobacco and alcohol (PolicyLink,2013, p. 8). They also reminded merchants of the voluntary
nature of the proposed program.
A key legislative aide further noted that to get buy-in from all stakeholders, “we sent differ-
ent iterations of the [proposed] legislation around to the Arab American Grocers’ Association
(AAGA), the coalition, and others to talk through the language of the measure.” This inclusive
approach proved critical with a particularly important player: the AAGA, representing 450
stores in the city, many of them in the Tenderloin and Bayview Districts, which eventually
endorsed the proposed ordinance.
Merchants also were involved with DPH, the coalition, San Francisco Ofce of Economic
and Workforce Development (OEWD), and other partners in working out details of the legis-
lation. The nal product of this collaborative effort was the Healthy Retailer Incentive Ordi-
nance, which would provide technical assistance with redesigns and other benets for selected
stores that, in turn, would commit to changes (e.g., shifting their business plan) to meet the
denition of a healthy retailer in the legislation. That denition included devoting at least 35
percent of selling space to healthy foods and no more than 20 percent to alcohol and tobacco
combined while removing specied amounts of their cigarette and alcohol advertising and pay-
ing minimum wage to workers (www.sfsbdc.org/HealthyRetailSF).
To make the proposed healthy retail measure politically attractive and feasible (King-
don,2003), the roles of different players were clearly laid out and the need for only a small
monetary investment from the city highlighted. OEWD would house the program and con-
tribute just $60,000 annually for the physical and business operations, technical assistance, and
equipment. OEWD would work closely with the DPH in running the program, with the latter
also contributing community engagement resources and materials. The fact that the coalition
298 Community-Based Participatory Research for Health
had already brought in a small foundation grant in support of healthy retail, including funding
for an initial pilot store conversion, further underscored the commitment of diverse stakeholders
to assisting the city in this endeavor. This bundling of resources supported the HealthyRetail
SF (HRSF) model, which emphasized community engagement, physical redesign of stores, and
improved business operations.
Detailed methods were described in the legislation for ensuring store and program
accountability, monitoring, and evaluation, including, in addition to point-of-sale data, “report
cards” to be completed by the FJLs in each participating store biweekly. Further, and prior to
the legislation’s passage, a fty-four-item Standards for Health and Sustainability Tool (http://
southeastfoodaccess.org/138) introduced by DPH and piloted in the Bayview was revised min-
imally and conducted by the coalition’s FJLs in two-thirds of the Tenderloin’s seventy-plus
corner stores. The FJLs’ strong relationships with local store owners and managers helped
achieve this high level of participation. Findings were made accessible to residents and mer-
chants through an eleven-page Tenderloin Corner Store Shopping Guide, which included a
color picture of each store, its data-based rating on a one- to four-star scale, and a summary of
its “healthy highlights” (e.g., low-fat dairy, no tobacco, and acceptance of Electronic Benets
Transfers or food stamps). In addition to capturing baseline data for studying changes in the
stores over time, the initial ndings (e.g., that the majority of stores received a rating of just
one to two stars, with only one receiving four stars) provided additional evidence of the need
for the proposed legislation.
The importance of sustaining trusting relationships with participating stores and growing
community engagement while building the evidence base for policy change (Cacari Stone
et al.,2014; Minkler,2014) remained evident in this second phase of the policy-making pro-
cess. The FJLs, for example, shared copies of the shopping guide rst with the merchants as
part of individualized feedback packets and one-on-one education. They then distributed the
shopping guide at a large community forum attended by about 150 residents and others, with
tabling by twelve CBOs, a nutritious meal along with recipes provided by a coalition member
organization, and speeches by a supervisor and another’s legislative aide about the proposed
healthy retail ordinance and how it would benet the neighborhood.
The “Policy Stream” and a Window of Opportunity
In the nal stream of the policy-making process, the FJLs and other coalition members, together
with their counterparts in the Bayview, spoke with policy makers in person and at hearings
before the full board of supervisors and relevant subcommittees to advocate for the healthy retail
legislation. Reecting on the importance of their testimony at a land use hearing shortly before
a vote of the full board of supervisors, a policy maker commented on how coalition members’
words seemed to resonate with some members of the board who had not paid much attention to
the issue of lack of access to healthy foods. As he noted, “It also brought up things not apparent
[to them]. So much publicity about [the city’s] great restaurants, the food culture, but hearing
from people who couldn’t get healthy food in their own neighborhood was something else.”
A supervisor cosponsor of the legislation later reected that “the coalition was extremely
inuential in drafting, rening, and then passing the healthy retailer ordinance” in part because it
“brought members in to educate the legislators [and] had very clear ideas in working with our staff
on what the measure should look like.” Their collective work paid off, and on September 1, 2013,
Improving Food Security and Tobacco Control through Policy-Focused CBPR 299
the board of supervisors unanimously passed the Healthy Food Retailer Incentive Program Ordi-
nance, which was then signed into law by the mayor.
In retrospect, a policy “window of opportunity” (Kingdon,2003) may have helped with
the legislation’s passage. As a policy maker noted, city hall–based priorities of redevelopment,
reducing community violence, and “doing something” about growing inequalities and hunger in
this afuent city provided an ideal environment for getting the absence of healthy retail in the
city’s poorest neighborhoods on the policy agenda in the problem stream. In the politics stream,
the design of a low-cost measure, with the ability to bring together multiple stakeholders and
public-private partnerships, and with grounding in scientic evidence and strong community
engagement, was promising. Finally, in the policy stream, a progressive board of supervisors,
several of whose members prioritized food insecurity; a mayor concerned about the city’s poor
but also the needs of small business; and effective media and policy advocacy (see for example,
Lagos,2013) proved critical.
Policy Implementation, Monitoring, and Evaluation
Passing legislation, and particularly municipal ordinances that may “lack teeth,” must be fol-
lowed by timely implementation, including detailed measures for monitoring, evaluating, and
suggesting course corrections where needed (Bardach,2005; Breckwich Vasquez et al.,2007).
Soon after the ordinance’s passage, the HRSF program infrastructure, including a rened model
and ve implementation steps, was established, along with stafng and the creation of a central-
ized resource center (see www.Healthyretailsf.org). A HRSF program advisory committee also
was established to review progress to date and offer guidance to OECD and DPH in program
decision making. Importantly, three representatives of the coalition were invited to join the
advisory committee, meeting quarterly in city hall with government representatives and other
key stakeholders.
Implementation of HRSF included the conversion of nine corner stores by the end of 2016,
ve of them in the Tenderloin, and technical assistance to an additional six stores receiving
more limited improvements. But successfully translating the ordinance into practice further
included engaging more than four thousand community residents in nutrition education and
healthy retail efforts, food advocate training and workforce development, the strengthening of
healthy retailer skills and collaborations, and the development of new local partnerships with
other demand-side projects, for example, a free municipal healthy food voucher program (www.
EatSF.org). Finally, implementation also involved sharing promising practices and preliminary
ndings through sponsorship of a Bay Area convening; media advocacy including at least four-
teen press events in 2014–2015 alone; and coalition member presentations at state, national,
and international professional meetings. Several articles for peer-reviewed journals also were
begun, with academic, community, and health department partners as coauthors.
Ongoing efforts at monitoring and evaluating progress and outcomes of the work on the
levels of the corner store, the coalition, the neighborhood, and municipal policy (HRSF) were
put into place. These included the FJLs’ observational assessments in two-thirds of the Ten-
derloin’s corner stores again in 2014, 2015, and 2017, enabling analysis of changes over time.
The addition of ten new observational items on tobacco advertising, availability, and display,
including e-cigarettes and small cigars beginning 2014, also enabled additional data collection
as new tobacco control legislation was passed and then enforced.
300 Community-Based Participatory Research for Health
The major hypothesis of this case study research was that the coalition’s work and HRSF
implementation activities and events would have a ripple effect among other Tenderloin corner
stores. We thus expected to see improvements in aggregate corner store assessment scores not
only in the ve Tenderloin stores participating in HRSF but also in many of those that applied
but weren’t accepted into the program or expressed no interest in healthy retail. Initial data
suggest that this ripple effect was indeed taking place. From the 2013 baseline through 2015,
the number of stores with a poor composite healthy retail assessment score (one to two stars)
decreased from forty-three to twenty-ve, and the number of stores with a good rating (three or
four stars) increased from thirteen to thirty. Subsequent interviews with the owners or managers
of fteen stores not participating in the program further supported a ripple effect, with most
reporting that they had made some healthy changes (e.g., offering some fresh fruit or reducing
cigarette advertising). Reasons given typically included wanting to stay competitive, hoping to
get into HRSF in the future, and not infrequently, because “my customers deserve it.”
Comparison of baseline point-of-sale data from the rst four Tenderloin HRSF stores with
data from their monthly POS printouts, collected quarterly thereafter, also showed promise.
The average units of produce sold per month in these stores increased from 6,025 at baseline
to 7,489 by month six and beyond in the program. One store that did not sell any produce at
baseline increased average monthly units sold to 1,438 between months six and ten. The stores
decreased absolute units of tobacco sold per month, although tobacco as a percent of total sales
in a fourth store remained similar. More data are needed to examine uctuations in sales because
of the seasonality of some items, store launches and other community events, and the passage
and enforcement of new state and local tobacco legislation (e.g., placing more restrictions on
e-cigarette advertising and display, increasing excise tax on cigarettes, and increasing minimum
age from eighteen to twenty-one). These and other initial ndings, however, are encouraging.
Further, as a DPH partner commented, tools like the biweekly store report cards, although help-
ful for data analysis, also are critical to the program in other ways, “[enabling] FJLs to help
merchants receive feedback and problem solve, while tracking changes.”
Data collection on the coalition and its functioning also are yielding useful ndings.
Although many of the facilitating factors contributing to the coalition’s work are discussed
previously, detailed analysis of these and of key challenges faced are still under way. In the
meantime, however, some of the striking obstacles that surfaced should be underscored. Among
these are severe limitations in scal and human resources that constrain the amount that can
be accomplished by the coalition and by HRSF. Although the conversion of ve Tenderloin
stores to healthy retail in 2014–2016 is impressive, against the background of need, ve corner
stores out of about seventy remain a drop in the bucket. Additionally, as some merchants noted,
practices such as the recent and well-intentioned distribution of fresh fruits and vegetables by
local volunteer programs may result in customers’ not purchasing these items in the stores, with
stores in turn seeing fresh produce go bad. One further commented that by failing to require
that “food stamps” be spent primarily on healthy foods, this critical government program was
thwarting the sale and consumption of healthier fare. Finally, merchant incentives from the
tobacco and sugary drink industries to display ads or in other ways promote their products also
were seen as barriers to healthier retail.
A major strength of the coalition was its emphasis on building individual and community
capacity and receipt of a large three-year Tobacco-Related Disease Research Program grant by
Improving Food Security and Tobacco Control through Policy-Focused CBPR 301
the academic PI in 2014, with two-thirds of the funding subcontracted for the coalition, further
contributing to such capacity building. The grant enabled a doubling of the time of coalition
coleaders, increased the number of FJLs from four to eight, and funded more multilingual
community materials and outreach to more broadly and deeply engage additional residents. The
grant also made possible more rigorous quantitative and qualitative data collection and analysis
and added a coalition participatory evaluation subcommittee to help study the functioning of the
partnership and its contributions to achieving project aims. As FJLs and other coalition mem-
bers and staff members enhanced their skills in research and evaluation, they made new con-
tributions to the work and increased their condence in the importance of the lived experience,
community trust, and social networks they brought to bear.
Although coalition leaders and DPH staff members facilitated important capacity building
in areas such as testifying and media advocacy among their members, challenges also emerged
in this area. As coalition members commented, for example, although being able to testify at
hearings was “huge,” in reality, conicting family and other obligations, mobility limitations,
and the frustrating tendency for hearings to be cancelled or delayed for hours without notice are
often major barriers to participation. With policy makers and other stakeholders reaching out
to the FJLs and other coalition members for testimony and support on other issues related to
healthy retail (e.g., a soda tax and new tobacco control measures), the importance of addressing
such barriers, for those who wish to increase their civic participation in this way, is underscored.
CONCLUSION
At their Health Equity Summit in 2013, the California Department of Public Health and the
California Tobacco Control Program emphasized the importance of “endorsing a paradigm shift
in how to look at equity. For example, supporting and building communities’ ability to engage
in reducing inequities at the state and local level; identifying creative ways to eliminate ineq-
uities; and measuring equity differently...” (Butler et al.,2013, p. 5).
In this chapter, we examined how a neighborhood coalition and its partners demonstrated
this “paradigm shift” through their focus on CBPR and policy change to address food justice
and inequities in exposure to tobacco and other unhealthy products in low-income neighbor-
hoods. We further illustrated how the coalition and other actors helped affect each stream of the
policy-making process, culminating in their work on helping to pass, implement, and evaluate
HealthyRetail SF.
The power of youth voices and participation in CBPR as a catalyst for change emerged early
in this case study and has also been widely demonstrated in studies with homeless youth (Garcia
et al.,2013) and those in other low-income and marginalized communities (Berg, Coman, &
Schensul,2009; Ozer, Lavi, Douglas, & Wolf,2015; Wilson et al.,2007; see Chapter8).
The role of the coalition’s “partnership dynamics” in strengthening the evidence base and
civic engagement for change (Cacari Stone et al.,2014) was also well illustrated in our case
study. Respectful, interactive trainings of the coalition’s FJLs in research methods and related
areas, co-led by a DPH partner and later supplemented by additional trainings in participatory
evaluation with UC Berkeley researchers, emphasized the bidirectional nature of learning and
data collection, interpretation, and dissemination.
302 Community-Based Participatory Research for Health
As in other CBPR efforts (Minkler, 2014), there were multiple challenges of time and
resources, including some that involved clashes between grant deliverables and preexisting
community priorities. Additionally, rapid gentrication of the neighborhood, although positive
in bringing in a stronger local revenue base and new customers for stores stocking healthier
fare, also raised questions about whether a project such as HRSF may inadvertently contribute
to further squeezing out of low-income residents and small businesses. Although the community
engagement leg of the HRSF model is key in buffering against the displacement of local resi-
dents and increasing community pride, more attention to gentrication and how it might equi-
tably be addressed should be explored.
Cacari Stone et al.’s (2014) model of CBPR as a strategy for policy change and King-
don’s (2003) three streams of the policy-making process proved useful conceptual frameworks
for studying the processes and outcomes of the coalition and of the HRSF program it helped
craft and bring to fruition. As this case study has illustrated, the use of multiple methods of
evaluative data collection (e.g., interviews with policy makers and other stakeholders, focus
groups, archival review, and ongoing participant observation) “can together improve a partner-
ship’s assessment of its contributions to changing a policy or the policy environment” (Minkler,
Garcia, Rubin, & Wallerstein,2012, p. 46).
Another takeaway from this case study was the imperative of community-led data gathering
and high-level involvement in all phases of the project. FJLs had trusting relationships with, and
therefore much greater access to, merchants than outside academics or health professionals. It
was that trust and access that enabled the FJLs’ detailed observational assessments in two-thirds
of stores three years in a row, with more to follow. Indeed, one merchant commented that when
strangers want to write down what he’s stocking, “I throw them out.”
Local members of the coalition also knew what to ask, how to ask it, and which organiza-
tions to go through in getting hundreds of residents to take part in a survey of their shopping
habits and concerns. Their sharing of ndings proved critical in reaching the media, the broader
public, and policy makers. Further, and whether educating merchants, helping lead large
community forums, or speaking out at municipal hearings and helping advise the city on imple-
mentation and sustainability, community leadership is the life blood of efforts like this one.
The imperative of doing your homework before pushing for a policy measure that requires
broad-based support from diverse constituents (Minkler,2014) also was demonstrated. For mer-
chants who often saw alcohol and tobacco as important sources of income, for example, the FJLs’
ability to understand and discuss the prot margins on these products, compared to the much more
favorable margins for fresh produce, was critical. Similarly, the coalition, DPH, and other part-
ners’ working out in advance the means for monitoring implementation and measuring progress
and outcomes helped underscore for policy makers that this was a well-thought-out proposal to
which key supporters continue to contribute well beyond the implementation phase. Particularly
in uncertain or difcult economic times, the importance of accenting for government, potential
funders, and other key players the sustainability of a new project also is critical. As noted, ongoing
collaboration between DPH and the coalition, and later with academic partners, helped raise the
foundation and other support for HRSF beyond the modest resources available through the city.
Local leadership development, community capacity building, and increased visibility
through the media and professional and academic channels helped keep the coalition and the
city’s HRSF program in focus. Together with organizations such as SEFA (now the Healthy
Improving Food Security and Tobacco Control through Policy-Focused CBPR 303
Southeast Coalition) in the Bayview and DPH, the Tenderloin Healthy Corner Store Coalition
and its partners remain viable and thriving contributors to the ght against inequities in who
can access healthy food and who has greater neighborhood saturation with tobacco, alcohol,
and other unhealthy offerings. “Food insecurity is a civil rights issue,” just as tobacco control is
a health equity issue, if poor neighborhoods are no longer to bear the brunt of disproportionate
exposure to the advertising and availability of these products. Policy-focused CBPR can play
an important role in helping study and address such injustices and building community capacity
and visibility as key players in helping make change happen.
QUESTIONS FOR DISCUSSION
1. Thinking back on the “three stages in the policy-making process” illustrated in this chapter
(the problem, politics, and policy stages), discuss whether and how you see this model as
relevant to your own work or other policy-focused CBPR with which you are familiar.
2. Some argue that having community residents take the lead in data collection may compro-
mise the rigor of the research. Discuss this concern, and describe one to two ways in which
the key data collection role of local FJLs in this case study may have improved research
quality and utility.
ACKNOWLEDGMENTS
The authors gratefully acknowledge our fellow members of Tenderloin Healthy Corner Store
Coalition and, particularly, the FJLs, without whom this work would not have been possible.
We thank, as well, the Tenderloin Neighborhood Development Corporation, the San Francisco
Department of Public Health, the SF Ofce of Economic and Workforce Development, and
Sutti & Associates for their support, and the Food Guardians and Bayview Heal Zone for paying
the way for healthy retail efforts in the Bayview neighborhood. The Tobacco-Related Disease
Research Program provided funding for much of the research and policy analysis described
in this study, with additional support from the California Endowment and an American Heart
Association postdoctoral fellowship. We are deeply grateful to Metta Fund, San Francisco
Foundation, and Dignity Health for their early and continuing support of the coalition and to
Patricia Wakimoto and Gladis Chavez for their assistance. Finally, we owe deep thanks to the
residents and merchants of the Tenderloin and to former Supervisor Eric Mar for their contribu-
tions to making healthy retail an increasing reality in San Francisco food swamps and beyond.
REFERENCES
Bardach, E. (2005). A practical guide for policy analysis: The eightfold path to more effective problem solving. New York,
NY: Chatham House.
Berg, M., Coman, E., &. Schensul, J. J. (2009). Youth action research for prevention: A multi-level intervention designed to
increase efcacy and empowerment among urban youth. American Journal of Community Psychology, 43(3–4), 345–359.
Birkland, T. A. (2015). An introduction to the policy process: Theories, concepts and models of public policymaking (3rd ed.).
New York, NY: Routledge.
304 Community-Based Participatory Research for Health
Breckwich Vásquez, A., Lanza, D., Hennessey Lavery, S., Facente, S., Halpin, H. A., & Minkler, M. (2007). Addressing food
security through public policy action in a CBPR partnership. Health Promotion Practice, 8(4), 342–349.
Butler, D., Aboelata, M., Cohen, L., & Spilker, S. (2013). Advancing health equity in tobacco control. Proceedings.
Health Equity Summit, June 25–26. Sacramento, CA: California Department of Public Health and California Tobacco
Control Program.
Cacari Stone, L., Wallerstein, N., Garcia, A. P., & Minkler, M. (2014). The promise of community-based participatory
research for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health,
104(9), 1615–1623.
City Data. (2015). Tenderloin neighborhood in San Francisco, CA, 94702, 94703, 94109 detailed prole. www.city-data.com/
neighborhood/Tenderloin-San-Francisco-CA.html
Coleman-Jensen, A., Gregory, C., & Singh, A. (2014). Household food security in the United States in 2013. USDA-ERS
Economic Research Report (173).
Estrada, J., & Mathews, G. (2012, December 3). Finding the good apples in the Tenderloin: Tenderloin youth and new
community coalition launch healthy retail program. Unpublished press release.
Farley, T. A., Rice, J., Bodor, J. N., Cohen, D. A., Bluthenthal, R. N., & Rose, D. (2009). Measuring the food environment:
Shelf space of fruits, vegetables, and snack foods in stores. Journal of Urban Health, 86(5), 672–682. doi:10.1007/
s11524-009-9390-3
Farley, T. A., & Sykes, R. (2015). See no junk food, buy no junk food. New York Times (March 21): A19.
Feeding America. (2014). Hunger in America. Retrieved from www.feedingamerica.org/hunger-in-america/our-research/
hunger-in-america/
Flood, J., Minkler, M., Hennessey Lavery, S., Estrada, J., & Falbe, J. (2015). Healthy retail as a strategy for tobacco control
and food justice: A case study of collective impact. Health Education and Behavior, 42(5), 654–668.
Garcia, A. P., Cardenas, Z., Porter, C., Grills, C., & Minkler, M. (2013). Engaging homeless youth in community-based partic-
ipatory research: A case study from skid row, Los Angeles. Health Promotion & Practice, 15(1), 18–27.
Gomez, A., Loresca, E., Myer, F., Payan, K., Sanseau, E., & Selpides, P. (2013). Healthy foods at the corner store:
A community project by the Tenderloin Healthy Corner Store Coalition (Unpublished report for the PRIME program).
Berkeley: University of California, Berkeley, Joint Medical Program.
Hennessey Lavery, S., Smith, M. L., Esparza, A. A., Hrushow, A., Moore, M., & Reed, D. F. (2005). The community action
model: A community-driven model designed to address disparities in health. American Journal of Public Health,
95(4), 611–616.
Kingdon, J. W. (2003). Agendas, alternatives, and public policies (2nd ed.). New York, NY: Longman.
Lagos, M. (2013). Measure to help corner stores sell healthy fare. San Francisco Chronicle (July 7).
Milio, N. (1998). Priorities and strategies for promoting community-based prevention policies. Journal of Public Health
Management and Practice, 4(3), 14–28.
Minkler, M. (2014). Enhancing data quality, relevance and use through community-based participatory research to improve
data relevance, quality and use to effect change. In N. Cytron, K. Petit, & G. T. Kinglsey (senior eds.), What counts?
Harvesting data for American’s communities (pp. 245–259). San Francisco, CA: Federal Reserve Bank of San Francisco
and the Urban Institute.
Minkler, M., Garcia, A., Rubin, V., & Wallerstein, N. (2012). Community-based participatory research: A strategy for
building healthy communities and promoting health through policy change. Oakland, CA: PolicyLink. Retrieved from
www.policylink.org/sites/default/les/CBPR.pdf
Ozer, E. J., Lavi, I., Douglas, L., & Wolf, J. P. (2015). Protective factors for youth exposed to violence in their communities:
A review of family, school, and community moderators. Journal of Clinical Child & Adolescent Psychology, pp. 1–26.
PolicyLink. (2013). Economic and community development outcomes of healthy food retail. PolicyLink, p. 8. Retrieved from
www.policylink.org/sites/default/les/FINAL_HER_ECONOMIC_WHITE_PAPER_FINAL_1%2018%2013.PDF
San Francisco Department of Public Health. (2012). Community health status assessment: City and county of San Francisco.
Retrieved from www.cdph.ca.gov/data/informatics/Documents/San%20Francisco%20CHSA_10%2016%2012.pdf
Wilson, N., Dasho, S., Martin, A., Wallerstein, N., Wang, C., & Minkler, M. (2007). Engaging young adolescents in social
action through photovoice: The Youth Empowerment Strategies (YES!) project. Journal of Early Adolescence, 27(2).

22
CHAPTER
CRIMINAL JUSTICE REFORM
THROUGH PARTICIPATORY
ACTION RESEARCH
SANETA DEVUONO-POWELL, MEREDITH MINKLER, EVAN BISSELL, TAMISHA
WALKER, LAVERN VAUGHN, ELI MOORE, AND THE MORRIS JUSTICE PROJECT
WITH AN ESTIMATED 2.3 million of its people behind bars, the United States has the highest
incarceration rate in the world (Wagner & Rabuy,2016). Despite a recent decline, the more than
quadrupling of the number of people in jail or prison from 1980 to 1990—driven by such factors
as a proliferation of new felony designations, mandatory minimum sentencing, increased crim-
inalization of drug violations, and the political capital gained through “tough-on-crime” pol-
icies and narratives—set the stage for the unfortunate “incarceration capital” designation the
country holds today (Alexander,2010). The Trump administration, led by Attorney General Jeff
Sessions, has committed to increasing, rather than decreasing, arrests for minor drug and other
offenses as well as the length of prison and jail terms. This policy stands in sharp contrast to
the Obama administration’s mandating that federal prosecutors evaluate “the unique facts and
circumstances of each case” and “select charges and seek sentences that are fair and propor-
tional based upon this individualized assessment” (Dominguez,2017, p. 1). Further, the Trump
administration’s criminal justice policy builds on and reects historical systems of racialized
connement including reservations, slavery, and internment camps.
Although white males born in the United States in 2001 had a one in seventeen chance of
imprisonment, the predicted odds increased to one in six for Latino males and to an astonishing
one in three for Black males (The Sentencing Project,2013). Similar racial disparities in rates
306 Community-Based Participatory Research for Health
of incarceration exist for women, although the gap has declined since 2001 (Mauer & Sabrina
Jones,2013). Just 15 percent of people detained can afford to pay bail and more than half of
individuals in jail are below the poverty line (Wagner & Rabuy,2016). Indeed, low income
helps explain why less than two hundred thousand of the 11 million jail admissions a year are of
people who have actually been convicted (Wagner & Rabuy,2016).
Prisons and jails are only one part of the criminal justice apparatus. It also encompasses inter-
locking systems and institutions, including immigration, juvenile detention centers, probation,
parole, policing, and punitive aspects of child services, welfare, public housing, and third-party
policing. The impact of these systems extends beyond the individual, affecting families and
entire communities (Alexander,2010; Gaber & Wright,2016). Forty-four percent of African
American women have an incarcerated family member (Lee, McCormick, Hicken, & Wildeman,
2015), and an estimated 10 million children experience parental incarceration during their lives
(Pew Charitable Trusts,2010). By 2012, three in ten Americans were under community super-
vision, leading to estimates that close to a third of US adults have some criminal justice record
(US Bureau of Justice,2012).
In this chapter, we summarize evidence that the criminal justice system constitutes a major
public health problem. We then highlight such positive developments as the momentum for
change created by Black Lives Matter and efforts to “realign” government funds away from
prison and jail expansion toward community-based organizations (CBOs) and resources for
prevention and successful reentry. Although situating such efforts within a public health frame-
work, we argue that many widely heralded reform efforts focus too narrowly on individual
behavior change and fail to engage those most directly affected by mass incarceration and
police brutality in broader systems change. We present two contemporary case studies, driven
respectively by formerly incarcerated individuals in Richmond, California, and residents
of the Bronx, New York, ghting aggressive policing. Both partnerships consciously use the
term participatory action research (PAR) rather than CBPR because of the former’s explicit
emphasis on the centrality of action in the research process. As discussed further on, however,
the terms PAR and CBPR often are used interchangeably, and they share common principles
and commitments such as addressing issues that matter locally, engaging community members
throughout the research process, and using ndings to help effect change (see also Chapters1
and2). We examine how these two projects collected meaningful insider data and worked for
community and policy-level change while promoting personal transformation among partici-
pants. Finally, we discuss the lessons learned and their potential relevance for other CBPR-PAR
efforts addressing criminal justice reform.
MASS INCARCERATION AND THE PUBLIC’S HEALTH
Increasingly, private and public discourse has focused on reforming our criminal justice
system. The United States spends more than $80 billion on incarceration annually—more than
six times the expenditures of other OECD countries (National Association of State Budget
Ofcer, 2013)—yet remains one of the most violent developed countries in the world (Pew
Charitable Trusts,2011). Harsher sentencing laws had limited effect on crime rates from 1990
to 2000 and no effect since 2000 (Roeder, Eisen, & Bowling,2015). The rehabilitative failures
of incarceration also have been documented, with close to half of those released re-incarcerated
Criminal Justice Reform through Participatory Action Research 307
within three years (Pew Charitable Trust,2011). Further, educational and other programs that
have shown lowered recidivism and greater cost savings have, with few exceptions, received
little support (Anderson,2015; Fine & Torre,2006).
Incarceration also exacerbates negative health outcomes and poses public health risks
(Binswanger, Krueger, & Steiner, 2009; Gaber & Wright,2016). Since 2000, suicide has been
the leading cause of death in local jails (Noonan, Rohloff, & Ginder,2015). Living in neighbor-
hoods with high incarceration rates—even for those who have never been incarcerated—puts
one at signicant risk for major depressive disorder and general anxiety disorder (Hatzenbuehler
et al.,2015).
In many of the largely Black and Latino low-income neighborhoods, coercive and lethal
policing also are concentrated. Similar to high rates of incarceration, the impact of police bru-
tality and killings on communities imposes stressors and can erode social cohesion. The need
for hypervigilance in such neighborhoods can contribute to depression and other mental health
problems as well as to HIV risk-taking, obesity, and a range of chronic diseases (Sewell &
Jefferson,2016).
MOVING TOWARD A BROADER PUBLIC HEALTH APPROACH
Despite strong public outcry epitomized by Black Lives Matter, residents of Ferguson and
manyother groups across the country, the lack of judicial interest in prosecuting or convicting
police who kill people of color is a stark indicator of institutional bias and the insecurity people
of color often experience within the criminal justice system. Further, and despite limited recent,
high-prole examples of police being held accountable, the continuing norm of institutional
bias also reects how a fear of the non-white “other” helps dene notions of crime and “reason-
able” police action. Further, it shines a spotlight on the need to address historical racism in any
public health approach to arenas such as criminal justice (see Chapter4).
Actions for reform of the criminal justice system have resulted in some important vic-
tories; between 2001 and 2009 the rate of growth in the prison population declined signicantly
(Mauer & Sabrina Jones,2013). By 2013, seventeen states—supported by the Department of
Justice and led by governors and legislators of both parties—had directed funding away from
prison construction and toward evidence-based programs and services, including treatment
and supervision (Goode,2013). States from California to Florida have reduced sentences and
eliminated enhancements for drug offenses. Laws that promulgate “collateral consequences”
of felony convictions also are being challenged and changed (Mauer & Jones2013; Sewell &
Jefferson,2016; Travis,2002). These include the role of police in public housing (Davis v. City
of New York); private housing (Ligon v. City of New York); the exclusion of those carrying felony
convictions from public housing and private rental housing, food stamps, and many jobs (US
Department of Housing and Urban Development Ofce of Public and Indian Housing,2015);
and the growth of the “ban-the-box” movement to prohibit employers from asking applicants
about prior convictions.
A diversity of states, cities, businesses, and universities also has responded to the pressure
of grassroots movements to divest from prisons and prison construction. In 2015, San Francisco
supervisors unanimously voted to return $80 million of state funds for the construction of a new
jail. Columbia University was the rst to divest from private prisons in 2015, an important step
308 Community-Based Participatory Research for Health
despite the small percentage of people held in private prisons nationwide. Californians are also
organizing to ensure that savings generated by recent laws and rulings reducing the incarcer-
ated population are not spent on the construction of new jails but go toward alternatives such as
treatment programs or community supervision.
Concurrently, movements against police brutality have grown locally and nationally
through the frequent use of direct action, increased documentation, and data collection and
dissemination. Most visible is the aggregate actions of Black Lives Matter, whose ideological
and political interventions challenge systemic anti-Black racism (see https://policy.m4bl.org/).
Although challenges to police misconduct have been made for decades, increased community
documentation of police violence and direct action responses have helped move the issue onto
the policy agenda (Kingdon,2003). This includes “The Counted,” the most reliable database
to date of fatal killings by police (The Guardian,2015), which documented 863 such killings
in 2016 and l,134 the preceding year. Responses to community activism have also included
requiring dashboard or lapel cameras on police, the right to have a lawyer at bookings in police
departments, justice department investigations of municipal police departments, and consent
decrees mandating changes in policing practices.
As noted previously, however, such encouraging developments are now being accompa-
nied by a return to more punitive measures under the Trump White House, with many more
(and longer-term) jail and prison terms for minor offenses. Overturning criminal justice reforms
under the Obama administration, the Justice Department’s “Charging and Sentencing Policy”
under President Trump stated that “prosecutors should charge and pursue the most serious,
readily provable offense” and invoke the most severe penalties possible (Dominguez,2017, p.1).
Further, and independent of the often draconian measures of the Trump administration, many
reform efforts have continued to focus downstream, emphasizing changing criminal behavior
without acknowledging structural issues of racism and violence. Hybrid programs also have
gained traction, most notably the widely heralded CeaseFire program (also called Cure Violence),
which began in Chicago more than twenty years ago and now is operating in two dozen cities and
several other countries, including Canada, the United Kingdom, and Iraq (www. cureviolence.
org). CeaseFire involves former gang members and felons whose “street cred” enables them
to reenter their communities as “interrupters” of retaliatory ghts and other violence before it
happens. Rigorous early research in three Chicago communities showed a reduction in violent
crime of 41 to 73 percent over a three-year period (Skogan, Harnett, Bump, & Dubois,2009).
A hallmark of CeaseFire’s efforts is the involvement of local police, who typically accom-
pany the interrupters on night walks and in other capacities. Such partnerships, however, are
fraught for some communities distrustful of law enforcement. In some instances, local community
groups have pulled out of CeaseFire, concerned that the decreases in violence may be largely a
result of increased arrests facilitated by the program’s strong police presence. Further, CeaseFire
limits its members to the downstream role of interrupters on the ground. They are not engaged
in discussions of the root causes of violence and mass incarceration, let alone invited to partici-
pate in developing and promoting upstream changes in policy for more-lasting, population-level
health and social outcomes (personal communication from G. Slutkin, November 4,2015).
To facilitate efforts to move upstream in the ght against mass incarceration and police
violence, a broader public health approach is needed that will ensure access to resources for
living, such as healthy food, education, adequate housing, and health care. But a public health
Criminal Justice Reform through Participatory Action Research 309
approach also includes changing upstream, political economic factors, such as structural vio-
lence and racism. Nancy Krieger’s (2011) “ecosocial approach” is a helpful tool in this regard.
Ecosocial analysis recognizes that “people literally embody, biologically, their lived experi-
ence and the societal and ecological context of the material and social world in which we live”
(p. 214). “Social trauma,” exemplied by incarceration and aggressive policing, is one of the
pathways of embodiment toward ill-health (p. 215).
Finally, a broader, ecosocial and community-partnered approach to prevention and public
health can advance solutions that are “rooted in community wisdom—the combined knowledge,
assets, intuition, and skills of community members” and will “alter policies, institutional prac-
tices, and physical environments to catalyze norms change” to support “equity, health, and
safety” (Cohen,2017). The following two case studies showcase how community-driven PAR
is a strategy for helping develop and implement policies that promote, rather than thwart, social
justice in the critical arena of criminal justice reform.
THE SAFE RETURN PROJECT
Just being involved with Safe Return, the impacts of how things change for
people who are coming home. The changing attitude of people, telling our
story, and watching a whole room of people in tears; it really was the best job
I have ever had, where I felt the most useful and made an impact.
L. V.
Based in Richmond, California, the Safe Return Project is rooted in the region’s unique history.
With 107,000 residents, Richmond has seen not only high levels of violence and incarceration
but also robust community organizing and engagement in progressive politics.
In 2010, the Safe Return (SR) Project was formed as a response to city and county discus-
sions about realignment of funds. The project’s founders were concerned that the populations
that would be most affected by these changes—currently and formerly incarcerated people and
their families—were not included in the conversation. The goal of Safe Return was to engage
formerly incarcerated residents in PAR, leading to action on issues that affected their lives. In
the seven years since its inception, Safe Return has conducted research, published reports, and
advocated for and seen policy changes to improve the lives of those coming home from prison
and jail (www.safereturn.org; deVuono-Powell,2016).
SR began with a strong commitment to community-driven PAR with three organizations—
the city of Richmond’s Ofce of Neighborhood Safety, the nonprot Contra Costa Interfaith
Supporting Community Organization (CCISCO), and a research organization, the Pacic Insti-
tute. With funding from The California Endowment and two nonprots, the partners hired a
team of eight individuals who had recently returned from prison or jail to work part-time at a
living wage. Organizational partners engaged the team in more than seventy-ve hours of initial
trainings that promoted trust and a sense of community and helped members develop skills that
would facilitate community research, organizing, and advocacy. The meetings began with dis-
cussions about salient issues that team members faced in adjusting to life outside. Topics, such
310 Community-Based Participatory Research for Health
as how to deal with conict, trauma, and legal challenges, were used to develop other tools and
skills that informed their research and their understanding of what issues and concerns they
shared with other members of the team. Concurrently, the group began to conduct informal
interviews with community members and city ofcials and to develop the survey instrument
they would later use to understand the issues faced by other formerly incarcerated people when
they came home. As part of developing the survey instrument, the team was further trained
in conducting interviews and other research methods. Although no formal institutional review
board (IRB) process was required, team members also were taught about ethical considerations
in conducting research and how to reect these in their work.
Using their survey instrument, team members interviewed 450 Richmond residents and
101 adults who were on probation or parole. Among their ndings were that fully 70 percent
of those released in the last three to eighteen months had unstable housing and 78 percent were
unemployed, compared to 16.5 percent citywide (Safe Return,2011).
To create awareness and get policy makers’ attention, the team published research nd-
ings, stories, and recommended action steps in a fteen-page report, Speaking Truth on Coming
Home (Safe Return, 2011), which was presented at a community meeting attended by 150
community residents and six public ofcials. In response to a major identied problem—job
applications requiring felons to indicate their status—the SR team played a leading role, with
other stakeholders, in helping craft and pass “ban-the-box” legislation in Richmond. SR team
members did their homework, nding out that the municipal government was Richmond’s third
largest employer, which itself required “the box” on job applications. During this rst problem
stage in the policy-making process, SR and its allies helped create increased awareness of the
adverse consequences of “the box” on the economic well-being of many of Richmond’s resi-
dents, families, and neighborhoods.
In the subsequent politics stage, SR worked with city council members and the city attor-
ney’s ofce to develop a policy that was politically attractive (e.g., low cost and popular). The
proposed measure would prohibit the city, or employers with city contracts, from asking about
criminal history, not only on job applications but also at any point in the hiring process. During
the politics and subsequent policy stage, SR and its allies continued to testify, meet with key
stakeholders, and secure public and media support for the ordinance, in part by arguing that it
would be among the most comprehensive in the country (Safe Return,2011). The ban-the-box
measure passed two years after SR began its efforts, and Safe Return continues to be acknowl-
edged as a major player in this successful campaign.
The SR team also partnered with local service providers and government ofcials to
advocate for and address another of its priority issues: creating a “one-stop shop” for reentry
services. To make such a center politically feasible, SR helped lead the ght to prevent county
funds from being used for jail expansion, instead making them available for substance abuse
and other health and social services for people at risk of incarceration or re-incarceration. In
2015, the city celebrated the opening of the Richmond Reentry Success Center—a comprehen-
sive center that was something every member of the Safe Return team had wished for when they
were released. SR continues to work on strategies to help formerly incarcerated people. Led
by one of its rst formerly incarcerated members, the project now runs a biannual leadership
academy for cohorts of thirty recently released individuals, who are committed to developing
their personal skills and helping effect systems change.
Criminal Justice Reform through Participatory Action Research 311
Although not without challenges, including member and staff turnover and fund-raising
difculties for this nontraditional organization, the effective work of Safe Return is a result of
its full engagement of participants and their ability to bring their lived experience and insider
knowledge to the table. Further, and although not a traditional research project that needed
to conform to IRB requirements and the like, the collaborative of community organizers
with Pacic Institute researchers and city staff members created a promising model of ethi-
cally informed on-the-ground research that other communities have shown interest in adapting
(deVuono-Powell et al.,2016).
THE MORRIS JUSTICE PROJECT
Dear NYPD, This is the Morris Justice Project . . .
This is our home! We live here. 50% of us were asked to show I.D. outside our
homes. We raise our children here. 75% of community members who took our
survey were stopped by the police. 25% of those were stopped for the 1st time
when they were 13 or younger . . .
On the side of a twenty-story public housing building in the South Bronx, a giant bat signal
illuminates the night. The projection ashes statistics and text as members of the Morris Jus-
tice Project read an open letter detailing their ndings about the New York Police Department’s
(NYPD’s) racially targeted practices of “stop-and-frisk” policing in the neighborhood. As the
data performance gains momentum, with people leaning out of windows and slowing on the
sidewalk, police show up and shut down the event. Such is the nature of public science and PAR
focused on aggressive policing practices by the nation’s largest police department in a heavily
policed New York neighborhood.
The Morris Justice Project (MJP) is a PAR collective of South Bronx residents, academics
from the City University of New York (CUNY) Graduate Center, John Jay College, as well
as lawyers, artists, and activists. MJP’s core collective is composed of about twelve people—
parents and grandparents, youth, faculty members, and students. The group operates with no
formal structure or consistent funding source. MJP formed to gather neighborhood thoughts and
experiences on aggressive police practices in order to speak back to the police and intervene
against harassment of area residents.
MJP’s process is rooted in the organizing call for “no research about us, without us” (Charl-
ton,1998) or what Arjun Appadurai (2006) has called the “right to research.” Consistent with
the philosophy of PAR (Cornwall & Jewkes,1995), this notion expands conventional concep-
tualizations of expertise, insisting that those who have been traditionally the objects of research
be repositioned as architects of research—designing, conducting, interpreting, and reporting the
ndings (Appadurai,2006). Following this, at each stage of research, MJP members work col-
laboratively and iteratively.
MJP was formed in 2011 after neighborhood mothers sought to respond, in part through
a successful lawsuit, to frequent police harassment of their sons because of NYPD’s stop-and-
frisk practice. Known colloquially as “broken windows” policing, stop-and-frisk, as practiced
312 Community-Based Participatory Research for Health
by the NYPD, required police ofcers to meet a quota of stops and resulted in disproportionate
harassment of Black and Latino residents. The mothers were introduced by their lawyers to
researchers at the Public Science Project (PSP; publicscienceproject.org). A PAR research
center at the CUNY Graduate Center, the PSP was interested in partnering with the mothers,
and the Morris Justice Project was formed. Community activists, including MJP, saw a major
victory in the 2014 decision in Floyd v. City of New York; how the NYPD practiced stop-and-
frisk was shown to exhibit racial bias and was found to be in violation of the 4th and 14th
amendments of the US Constitution.
MJP employs and develops context-specic participatory research methods for a forty-two-
block neighborhood dened by the group. After outlining this geographic area, the partnership
went through an iterative process of developing a community survey, accountable to the exper-
tise of area residents and the university IRB. The survey was systematically distributed by mem-
bers throughout the neighborhood and attracted 1,030 respondents. The survey process created
opportunities for additional neighborhood residents to join, and this expanded group analyzed the
results from the surveys through a “stats-’n-action” collaborative data analysis process (Stoudt &
Torre,2014). MJP members then designed a “back-pocket” report, which could be folded up and
put in one’s back pocket, for ease of distribution on neighborhood streets (see morrisjustice.org).
This back-pocket report included a summary of quantitative and qualitative ndings, an overview
of the project, sample demographics, and a comparative analysis of their Bronx neighborhood
with a whiter, more afuent neighborhood in lower Manhattan. The ndings cast in stark relief the
highly disproportionate policing of the MJP neighborhood, with 75 percent of residents surveyed,
for example, reporting that they personally had been stopped by police prior to age twenty-six.
Given limited public space in the neighborhood, MJP next designed a strategy to share and
gather research that it calls sidewalk science. Sidewalk science actions are iterative practices
of sharing and collecting data through temporary installations on street corners, school fences,
outside the adjacent Yankee Stadium, and other slivers of public space (Stoudt & Torre,2014).
Consistent with PAR-CBBR’s emphasis on translational research to educate and help inform
policy and community change, during summer 2014 after stop-and-frisk was found unconsti-
tutional in the way it was practiced, MJP created posters (see Photo22.1), stickers, letters, and
interactive displays installed throughout the neighborhood that connected stop-and-frisk and
the broader, but lesser known, police strategy in which it sits—order-maintenance policing or
broken windows policing. This also included the collection of new data about resident visions
of a safe and healthy neighborhood (see Photo22.2).
Sidewalk science actions create what MJP’s María Elena Torre (2010) calls “contact zones,”
in which connection across difference generates knowledge across and through those differences.
As a result, the zones become a container for communication, relationship building, debate, and
data collection. As highly visible actions in a heavily policed area, these actions are reclamations
of public space and an assertion of the need for community safety beyond policing. Although data
are aggregated and condential, participation may bring increased police or community attention.
To address this, MJP works in larger groups, partners with lawyers while in public, and members
text and call each other at the end of meetings and actions to make sure everyone is home safe.
The role of MJP actions in contributing to outcomes is based on using its sidewalk science,
data collection, and other participatory research methods in multiple policy, legal, and orga-
nizing arenas. As only one player in a broad movement to challenge police practices, it is

Criminal Justice Reform through Participatory Action Research 313
difcult, and perhaps unnecessary, to trace linear or direct policy, legal, and political outcomes
precipitated by MJP’s work. MJP members, however, actively speak about their ndings at
local town halls, rallies, and block parties as well as through various media (Pabon,2013; Tuttle
& Schneider,2012). As MJP has expanded its audience, it embarked on a series of academic
papers, including a twelve-coauthored journal article on the potential of PAR for policy making
that was created through a process of interviews, group writing, and editing (Stoudt et al.,2015).
MJP has been invited to present in close to a dozen academic and professional gatherings
across the United States, including keynotes and presentations in venues ranging from Bronx
Community College to a 2015 Citizen Science Forum at the White House.
The work of MJP included its key role in the coalition Communities United for Police
Reform (CPR) (changethenypd.org), founded in 2011 to build public support for police
reform legislation and legal challenges to aggressive policing. As a member, MJP infused
PHOTO 22.1
Source: María Elena Torre.
Photo Credit: Morris Justice Project

314 Community-Based Participatory Research for Health
data and research into demonstrations, policy discussions, council votes, press conferences,
and press releases, including compiling reports on court hearings for the stop-and-frisk
case (see morrisjustice.org/watching-oyd). This work contributed to the passage of the
Community Safety Act legally ending discriminatory proling and providing independent
oversight of the NYPD. The appointment of a MJP member to the judge’s community advi-
sory board tasked with overseeing the joint remedial reform process of stop-and-frisk further
underscored the visibility of and respect in which MJP and its work was held.
MJP’s prioritization of resident expertise in all stages of research, its responsive iterations
of research forms, and emphasis on sharing back research from where it was gathered have
informed other studies. Researchers for Fair Policing (RFP), to which two of MJP’s academic
researchers also belong, drew from MJP’s process in its survey development on youth experi-
ences with policing in New York. As a result of its impressive work, RFP went on to gain rep-
resentation on President Obama’s Task Force on 21st Century Policing. Finally, and although
MJP is focused on a local area, it also worked with the law rm assisting the city of Toronto,
Canada, in reforming its “carding” policy, which was resulting in racially discriminatory pro-
ling. As part of its police reform efforts, Toronto further adapted the work of MJP for a study
on carding abuse in its communities of color (Meng,2014).
Such developments are encouraging, as is the dramatic drop in New York City’s ofcially
recorded police stops, from 685,724 in 2011 to 22,939 in 2015 (New York Civil Liberties
PHOTO 22.2
Photo Credit: Morris Justice Project
Criminal Justice Reform through Participatory Action Research 315
Union,2015). However, signicant concerns remain that the decline doesn’t capture the actual
stops experienced by residents and that formal reform efforts tend to tokenize resident participa-
tion. Nearly a year after the successful legal challenge to how NYPD practiced stop-and-frisk,
the widely publicized murder of an unarmed Black man, Eric Garner, at the hands of police and
the ofcers’ acquittal, made horrically clear how much work remains. The reform of policing
is not an end, but conversely, as an MJP researcher recently commented, “We are just beginning
with this.” MJP recognizes that deep, lasting change necessitates critical analysis and action on
schools, surveillance, gentrication, and the structures that create the social conditions of the
South Bronx, particularly in the current sociopolitical climate.
CONCLUSION
The criminal justice system encompasses a complex set of institutions, policies, and dynamics,
reected in community policing, incarceration, and surveillance and how judicial systems dene
and punish crimes. It is therefore easy to lose sight of the upstream causes of the overlapping
issues of mass incarceration and aggressive, sometimes lethal, policing in low-income, mostly
Black and Latino communities. As discussed in this chapter, many new efforts at reforming
some of the most obvious failures of the criminal justice system are gaining traction. Unfortu-
nately, many of these strategies that gain mainstream acceptance are focused on downstream
efforts that do little to address deeply rooted causes of and contributors to these problems.
Health professionals and academic health researchers increasingly have recognized the
need to study and help address criminal justice reform, as illustrated in recent special issues
of the Journal of Urban Health (April 2016) and the Journal of Health Care for the Poor and
Underserved (Spring 2016). Further, as Smith and Braithwaite (2016) suggest in their “Call to
Action,” academic health researchers concerned with criminal justice reform should include
participatory research as one of six top priorities.
Both partnerships explored in this chapter intentionally chose to use the term participatory
action research in place of CBPR, given the former’s more explicit emphasis on the centrality
of action as part of the research process. Yet as noted, CBPR and PAR share a core set of values
and principles, key among them beginning with an issue of local relevance and importance,
engaging residents throughout the research process, building capacity, and using study ndings
to help effect change, often including change on the policy or systems level (see Chapters1
and20). In the United States, research labeled CBPR is more likely to be university funded or
negotiated than PAR and to include the formal development and approval of an IRB protocol to
help ensure that the partnership upholds high ethical standards in research. Yet even when there
is no university or related partner, PAR (or CBPR) efforts are committed to ethical practices in
survey and other data collection, maintaining condentiality when appropriate, and so on.
The efcacy of CBPR and PAR for studying and helping address a wide range of health
problems is well established. But with some important exceptions (e.g., deVuono-Powell,
Schweidler, Walters, & Zohrabi,2015; Freudenberg, Rogers, Ritas, & Nerney,2005) its appli-
cation in the criminal justice context is relatively underdeveloped. Conceived by three Oak-
land, California, community-based organizations (deVuono-Powell et al.,2015), reports on how
trained community researchers conducted more than one thousand interviews with formerly
incarcerated persons, family members, and other stakeholders in fourteen states and close to
316 Community-Based Participatory Research for Health
three dozen focus groups. Among their ndings were that apart from immediate expenses, the
costs to families of a member’s incarceration often equal the annual household income, with
pronounced gender differences. Fully 83 percent of family members responsible for a member’s
legal and other fees while incarcerated were women.
Through the two studies highlighted in this chapter, we examined how the use of PAR
produced community-driven and evidence-based research and advocacy while employing
novel means of community education and personal transformation, contributing to policy and
community change. Efforts by Safe Return and MJP to carry a participatory ethos through all
aspects of the work emphasize a political and epistemological challenge to dominant forms of
research and knowledge production, particularly those that have supported mass incarceration
and aggressive policing.
As these two examples illustrated, although typically cast as the “other,” formerly incar-
cerated residents and those living in Black and Latino neighborhoods most affected by aggres-
sive policing have a critical role to play. Community team members’ knowledge and personal
experiences frequently reveal deeper insights into the problems faced, connect the research with
others affected by aggressive policing or incarceration, and build innovative educational- and
systems-level movements for change.
Understanding the role of policy as a catalyst for promoting what the Prevention Institute
describes as the “norms of equity, health and safety” (www.preventioninstitute.org/about-us/our-
approach) was also demonstrated in the two case studies. For MJP, community-led education,
research, and action with artists, lawyers, and other actors helped people think differently, and
more deeply, about root causes of aggressive policing, including systemic racism and exclusionary
forms of leadership and decision making. Their work helped catalyze change by contributing to
policies that privilege “equity, health and safety,” regardless of one’s color or zip code. Finally,
Safe Return and the Morris Justice Project offer not only lessons on reforming the failed criminal
justice system but also how “upstream” intervention can occur, as well as what it can help achieve.
Among these lessons are the need to do the following:
■ Prioritize the leadership and knowledge of those most directly affected by unjust and ineq-
uitable systems.
■ Design data collection processes that are rigorous enough to capture complex collateral
consequences of practices, such as mass incarceration and aggressive policing, and produce
data outcomes relevant to those affected by the system.
■ Create a research process that simultaneously focuses on policy and legal avenues to change
as well as contributing to the capacity, leadership, and healing of community researchers.
■ Produce accessible and creative means of disseminating knowledge created through the
research to diverse audiences, from community residents through policy makers, toward the
end of equity-focused sustainable change.
■ Increase nancial and other support for community-level, CBPR-PAR groups and partner-
ships to thrive and contribute their gifts to helping study and address problems that matter
locally and beyond. In the case of projects such as MJP and Safe Return, because those
conducting this critical work tend to live in largely Black and Brown heavily policed neigh-
borhoods, support should include helping ensure that their participation does not contribute
to increased surveillance and harassment—and engaging the media and other sectors to
shine a spotlight on such harassment, if and when it occurs.
Criminal Justice Reform through Participatory Action Research 317
Despite the Trump administration’s efforts to roll back recent reforms at the federal level
(Dominguez,2017), we are encouraged that many policy makers, particularly on the state and
local levels, are nally grappling with the criminal justice system and related problems that con-
tribute to violence, including police violence, and the unrelenting cycle of poverty and loss they
exacerbate. Particularly in efforts to effect authentic and sustainable change, the engagement of
affected community members as leaders and key PAR-CBPR partners in disrupting policy as
usual cannot be overstated.
QUESTIONS FOR DISCUSSION
1. You are an academically trained researcher, have access to seed funding for a CBPR project,
and have reached out to a community group about possibly doing a project together to
address your mutual concerns with lethal policing. Members seem interested but have only
heard of participatory action research and wonder what the differences are between PAR
and CBPR. How would you react if they want to use the term PAR, but your funder is a
rm believer in the lexicon of CBPR?
2. Many groups and individuals address issues such as inequities in incarceration and other
aspects of the criminal justice system through direct advocacy and organizing. What role
does research have in relation to these issues? Why include research instead of just action?
3. How do the case studies address upstream factors related to the criminal justice system?
Why do the authors critique CeaseFire as a downstream approach?
ACKNOWLEDGEMENTS
We gratefully acknowledge the members of the Safe Return Project and the Morris Justice
Project, and the many other participants in and supporters of their work. For the Safe Return
Project, special thanks go to Richard Boyd and Sam Vaughn, and to others interviewed for this
chapter. We also are deeply grateful to The California Endowment and the Robert Wood John-
son Foundation for their major support. For the Morris Justice Project, we thank the following
members of MJP for ongoing conversations about this work and guidance on this chapter: Paul
Bartley, Fawn Bracy, Anthony Downs, Cory Greene, Prakriti Hassan, Nadine Sheppard, Brett
Stoudt, María Elena Torre, and Jacqueline Yates.
Finally, our deep thanks go to Black Lives Matter, the Sentencing Project, and the numerous
other individuals and organizations who have made imperative ending police brutality and mass
incarceration. Angela Glover Blackwell, Leonard Cavise, and Larry Cohen are among those to
whom we are especially grateful for insights and contributions.
REFERENCES
Alexander, M. (2010). The new Jim Crow: Incarceration in the age of mass incarceration. New York, NY: The New Press.
Anderson, N. (2015, July 31). A diploma really is a crime-stopper. Feds aim to fund inmate education. Washington Post.
Appadurai, A. (2006). The right to research. Globalisation, Societies and Education, 4(2), 167–177. http://doi.
org/10.1080/14767720600750696
318 Community-Based Participatory Research for Health
Charlton, J. I. (1998). Nothing about us without us: Disability oppression and empowerment. Berkeley: University of
California Press.
Clear, T., Frost, N. A., Carr, M., Dhondt, G. D., Braga, A., & Wareld, G. (2014). Predicting crime through incarceration: The
impact of rates of prison cycling on rates of crime in communities. Washington, DC: US Department of Justice.
Cohen, L. (2017). Prevention institute: Our approach. Retrieved January 31, 2017, from www.preventioninstitute.org/
about-us/our-approach
Cornwall, A., & Jewkes, R. (1995). What is participatory research? Social Science & Medicine, 41(12), 1667–1676. http://doi.
org/10.1016/0277–9536(95)00127-S
deVuono-Powell, S., Schweidler, C., Walters, A., & Zohrabi, A. (2015). Who pays? The true cost of incarceration on families.
Oakland, CA: Ella Baker Center, Forward Together, Research Action Design. Retrieved from http://whopaysreport.org/
who-pays-full-report/
deVuono-Powell, S., Vaughn, L., Walker, T., Moore, E., & Minkler, M. (2016). Home with a purpose: A history of the Safe
Return Project. The Haas Institute for a Fair and Inclusive Society. Retrieved from http://haasinstitute.berkeley.edu/sites/
default/les/safereturncasestudy_publish.pdf
Dominguez, I. (2017). AG Sessions issues retrograde charging policy, seeks return to 20th century’s so-called war on drugs
and the age of mass incarceration. Washington Post (May 12), p. 1.
Fine, M., & Torre, M. (2006). Intimate details: Participatory action research in prison. Action Research, 4(3), 253–269.
Freudenberg, N., Rogers, M. A., Ritas, C., & Nerney, M. (2005). Policy analysis and advocacy: An approach to community-
based participatory research. In B. A. Israel, E. Eng, A. J. Schulz, & E. A. Parker (Eds.), Methods in community-based
participatory research for health (pp. 349–370). San Francisco, CA: Jossey-Bass.
Gaber, N., & Wright, A. (2016). Protecting urban health and safety: Balancing care and harm in the era of mass incarceration.
Journal of Urban Health, 93(Suppl 1), 68–77. doi:10.1007/s11524-015-0009-6
Goode, E. (2013, July 25). U.S. prison populations decline, reecting new approach to crime. New York Times. Retrieved from
www.nytimes.com/2013/07/26/us/us-prison-populations-decline-reecting-new-approach-to-crime.html
Hatzenbuehler, M. L., Keyes, K., Hamilton, A., Uddin, M., & Galea, S. (2015). The collateral damage of mass incarceration:
Risk of psychiatric morbidity among nonincarcerated residents of high-incarceration neighborhoods. American Journal
of Public Health, 105(1), 138–143.
Kingdon, J. W. (2003). Agendas, alternatives, and public policies (2nd ed.). New York, NY: Longman Press.
Krieger, N. (2011). Epidemiology and the people’s health: Theory and context. Oxford, UK: Oxford University Press.
Lee, H., McCormick, T., Hicken, M. T., & Wildeman, C. ( 2015). Racial inequalities in connectedness to imprisoned individ-
uals in the United States. Du Bois Review, 12(2), 269–282.
Mauer, M. (2013). The changing racial dynamics of women’s incarceration. Washington, DC: The Sentencing Project.
Retrieved from www.sentencingproject.org/publications/the-changing-racial-dynamics-of-womens-incarceration/
Mauer, M., & Sabrina Jones, M. (2013). Race to incarcerate: A graphic retelling (3rd ed.). New York, NY: The New Press
Meng, Y. (2014). Racially biased policing and neighborhood characteristics: A case study in Toronto, Canada. Cybergeo:
European Journal of Geography. Retrieved May 23, 2017, from https://cybergeo.revues.org/26165
National Association of State Budget Ofcer. (2013). State spending for corrections: Long-term trends and recent criminal jus-
tice policy reforms. Retrieved from www.nasbo.org/sites/default/les/pdf/State%20Spending%20for%20Corrections.pdf
New York Civil Liberties Union. (2015). Stop-and-frisk data. Retrieved from www.nyclu.org/content/stop-and-frisk-data
Noonan, M., Rohloff, H., & Ginder, S. (2015). Mortality in local jails and state prisons, 2000–2013 statistical tables. Bureau
of Justice Statistics. Retrieved from www.bjs.gov/index.cfm?ty=pbse&sid=76
Pabon, J. (2013, April 22). South Bronx continues to organize against “stop & frisk.” Hufngton Post. Retrieved May 24,
2016, from www.hufngtonpost.com/julio-pabon/stop-and-frisk-south-bronx_b_3123403.html
Pew Charitable Trusts. (2010). Collateral costs: Incarceration’s effect on economic mobility. Washington, DC: The Pew Char-
itable Trusts. Retrieved from www.pewtrusts.org/˜/media/legacy/uploadedles/pcs_assets/2010/collateralcosts1pdf.pdf
Pew Charitable Trusts. (2011). State of recidivism: The revolving door of America’s prisons. Retrieved from www.pewtrusts.
org/en/research-and-analysis/reports/0001/01/01/state-of-recidivism (p. 2).
Roeder, O., Eisen, L., & Bowling, J. (2015). What caused the crime decline? Brennan Center for Justice. Retrieved from
www.brennancenter.org/publication/what-caused-crime-decline
Safe Return. (2011). Speaking truth on coming home: Research ndings and recommendations on reentry in Richmond.
Retrieved from www.pacinst.org/wp-content/uploads/sites/21/2013/02/reentry_report3.pdf
Criminal Justice Reform through Participatory Action Research 319
Sewell, A. A., & Jefferson, K. A. (2016). Collateral damage: The effects of invasive police encounters in New York City.
Journal of Urban Health, 93(Suppl 1), 42–67.
Skogan, W., Harnett, S. M., Bump, N., & Dubois, J. (2009). Evaluation of CeaseFire—Chicago. Washington, DC: National
Institute of Justice.
Smith, S. A., & Braithwaite, R. L. (2016). Introduction to public health and incarceration: Social justice matters. Journal of
Health Care for the Poor and Underserved, 27(2A), 1–4.
Stoudt, B. G., & Torre, M. E. (2014). The Morris Justice Project. In P. Brindle (Ed.), Sage cases in methodology. Thousand
Oaks, CA: Sage Publications.
Stoudt, B. G., Torre, M. E., Bartley, P., Bracy, F., Caldwell, H., Downs, A., Greene, C., Haldipur, J., Hassan, P., Manoff, E.,
Sheppard, N., & Yates, J. (2015). “We come from a place of knowing”: Experiences, challenges, advantages and possibil-
ities of participating in Morris Justice Project. In C. Durose & L. Richardson (Eds.), Re-thinking public policy making:
Why co-production matters. Bristol, UK: Policy Press.
The Guardian view on killings by US police: Why we must keep counting (2015, December 31). The Guardian. Retrieved
from www.theguardian.com/us-news/2015/dec/31/the-counted-killings-by-police-editorial
The Sentencing Project. (2013). Report of the Sentencing Project to the United Nations Human Rights Committee regarding
racial disparities in the United States criminal justice system. Retrieved from http://sentencingproject.org/wp-content/
uploads/2015/12/Race-and-Justice-Shadow-Report-ICCPR.pdf
Torre, M. E. (2010). The history and enactments of contact in social psychology. Ann Arbor, MI: UMI Dissertations
Publishing.
Travis, J. (2002). Invisible punishment: An instrument of social exclusion. In M. Mauer & C.-L. Meda (Eds.), Invisible pun-
ishment: The collateral consequences of mass imprisonment (pp. 15–36) New York, NY: The New York Press.
Tuttle, R., & Schneider, E. (2012, October 8). Stopped-and-frisked: “For being a f**king mutt” [Video]. The Nation. Retrieved
from www.thenation.com/article/stopped-and-frisked-being-fking-mutt-video/
US Bureau of Justice Statistics. (2012). Survey of state criminal history information systems, 2012. US Department of Jus-
tice, Ofce of Justice. Retrieved from www.ncjrs.gov/pdfles1/bjs/grants/244563.pdf
US Department of Housing and Urban Development Ofce of Public and Indian Housing. (2015). Notice PIH 2015–19
guidance for public housing agencies (PHAs) and owners of federally assisted housing on excluding the use of arrest
records in housing decisions. Retrieved from https://portal.hud.gov/hudportal/documents/huddoc?id=PIH2015–19.pdf
Wagner, P., & Rabuy, B. (2016). Mass incarceration: The whole pie 2016. Prison Policy Initiative. Retrieved from www.
prisonpolicy.org/reports/pie2016.html

23
CHAPTER
GLOBAL HEALTH POLICY
SLUM SETTLEMENT MAPPING IN NAIROBI
AND RIO DE JANEIRO
JASON CORBURN, IVES ROCHA, ALEXEI DUNAWAY, AND JACK MAKAU
IN COMMUNITIES ACROSS the Global South, the urban poor are organizing to map the
physical and social conditions in which they live and using visualization to advocate for
improved health. There is a long tradition in urban public health of mapping social conditions,
exposures, and morbidity and mortality, ranging from John Snow’s historic mapping of cholera
cases and resultant removal of a contaminated water pump in nineteenth-century England to the
twenty-rst-century use of geographic information system (GIS) science to analyze and model
potential interactions among biophysical, built, and social environmental factors across time
and space (Brown, McLafferty, & Moon,2010). Community-based organizations (CBOs) are
increasingly partnering with universities and others to combine their local knowledge of place
with computer-aided data collection and mapping tools. One result is that community-driven
mapping is shaping global health interventions and policy making in new ways because map
making is including new participants in the action research process and revealing information
by and about communities previously ignored in global health discourses.
In this chapter, we suggest that map making is as much a process as a product and that both
help community members and researchers organize and prioritize information, make visible key
data, challenge professional characterizations of whether or not a place is “healthy,” and con-
tribute to the important narratives of healthy policy making. Using case studies of community-
driven mapping from Rio de Janeiro, Brazil, and Nairobi, Kenya, respectively, we highlight
322 Community-Based Participatory Research for Health
how map making can support CBPR and vice versa only when the process reects norms of
democratic science. These include a commitment to transparency, an openness to critical scru-
tiny, a skepticism toward claims that too neatly support reigning values, a willingness to listen
to countervailing opinions, a readiness to admit uncertainty and ignorance, and a respect for evi-
dence gathered by local and professional experts (Corburn,2009).
Ensuring that map making is a democratic process owned and controlled by community
members requires that local people, not outside researchers, dene the geographic or other
boundaries over what counts as part of the “community.” The collaborative partnerships and
knowledge generated through action research must be oriented toward existing community
organizing goals, focus on mapping assets and hazards, and aim to highlight issues that may
be ignored or given scant attention by outsiders, particularly policy makers. In this process,
mapping can facilitate learning about place and health equity relationships by researchers
and community members, particularly if the process is ongoing and dynamic, rather than a
static, one-time effort. Finally, map making that extends CBPR must capture the broad, often
cumulative, determinants of health in places and communicate this complexity easily and
widely to residents and others beyond the community’s boundaries.
PLACE AND MAPPING IN A RELATIONAL VIEW
Mapping is necessary (but perhaps insufcient) for capturing the complexities of places that
inuence health inequities and thus can lead to interventions that more fully characterize the
determinants of health. Much work in public health, dened as “built environment and health,”
in fact tends to conate neighborhood characteristics (often using static variables) with place
(Ellaway et al.,2012; Kimbro & Denney,2013). These studies aim to explore for signicant
“neighborhood effects” on well-being using a subset of quantitative variables. When little or no
statistical inuence is found, they often conclude that individual biology, behaviors, or genes
must be responsible for health status, not “neighborhood characteristics.” In neighborhood-
effects research, the most proximate scale is used often because of the relative ease in access-
ing administrative data (i.e., census or health surveys). However, this may miss community
knowledge or forces outside the neighborhood or local place, such as national and international
policies, which can inuence local access to a health-promoting good, such as affordable food.
Distance under the relational view ought to include physical and social relations and view
populations and places embedded within networks. This concept of distance is important for
health promotion, and although distance typically is seen as posing a barrier for people without
close proximity to needed health or social services, the converse may also be true. The poor, for
example, may not access a service that is physically close to them, especially if they perceive it
as not being culturally appropriate or affordable or if traveling far away from one’s home might
reduce the chances of being stigmatized for being treated for a disease in one’s community
(Popay, Williams, Thomas, & Gatrell,1998).
In the relational view of place taken here, there are mutually reinforcing relationships be -
tween places and people and the position of places relative to each other. Further, the place effects
on health ought to be understood as a result of endogenous and exogenous processes operating
at a variety of spatial scales, not just the neighborhood scale (Cummins, Curtis, Diez-Roux, &
Macintyre,2007). Healey (2007, pp. 3–4) describes the relational approach as emphasizing
Global Health Policy 323
... the dynamic diversity of the complex co-location of multiple webs of relations that transect
and intersect across an urban area, each with their own driving dynamics, history and geog-
raphy...This involves moving beyond an analysis of the spatial patterns of activities as organ-
ised in two-dimensional space, the space of a traditional map. Instead, it demands attention to
the interplay of economic, socio-cultural, environmental and political/administrative dynamics as
these evolve across and within an urban area.
CBPR mapping can reveal the “double construction” of places: rst through material and
physical building (the buildings, streets, parks, etc., of the “built environment”) and second
through the shaping of social processes that assign meanings, interpretations, narratives, per-
ceptions, feelings, and imaginations within places. CBPR projects have a natural afliation
for the relational view and frequently capture the multiple features and meanings in places
( Cashman, Adeky, & Allen,2008; Rambaldi et al.,2006).
Importantly, these meanings are contingent and contested, constantly being constructed and
reconstructed as, for instance, when new population groups and cultures move into a place.
Differences in social processes, such as power, inequality, and collective action, are often
revealed through the construction and reconstruction of the material forms and social meanings
of places, and a nuanced understanding of these processes is required for health equity planning
( Emirbayer, 1997; Escobar,2001). The contingent and contested characteristics of place mean-
ings suggest an anti-essentialist view of places or the notion that there is no one single set of
place characteristics, meanings, or relationships that will make all cities and neighborhoods
healthy. Such a perspective further underscores the necessity of understanding the history of
places and the biographies of people living there if health equity is to be seriously understood,
sought, and achieved.
RIO DE JANEIRO CASE STUDY
The Mapeamento Digital Liderado por Adolescentes e Jovens (Youth-Led Digital Mapping)
was a joint initiative implemented between 2011 and 2015 by UNICEF and a Brazilian non-
governmental agency (NGO), the Centro de Promoção da Saúde (Center for Health Promotion,
CEDAPS).
1
The project directly involved 550 people in nineteen poor communities throughout
the country and invited youth to explore and map socio-environmental health risks as a tool for
advocacy and community mobilization. In doing so, the mapping process aimed to help youth
move from passive observers into arbiters of local knowledge and principal agents of local
social transformation.
Three mapping methodologies were used. The rst employed mobile phones to identify and
geo-locate specic health risks, uploaded to a Google Maps–based interactive platform. The
second built a non-cartographic but symbolic spatial representation of important community
areas. Finally, the third used an aerial kite-and-camera rig to modernize outdated satellite
images and validate the existence and true size of neighborhoods. Together, these methodol-
ogies elevated community expertise in the denition of place and provided an alternate episte-
mology that drove local community mobilization and government action.
Throughout the implementation of the initiative, collaborative engagements among youth,
local associations, civil society, and government partners were instrumental in ensuring concrete,

324 Community-Based Participatory Research for Health
integrated results. Using networks built through the mapping process, local community associa-
tions spearheaded initiatives to reduce trash levels, in one instance removing two tons of refuse
and in another redistributing trash collection points through the neighborhood.
CEDAPS Methodology
The rst and primary focus of the youth-led digital mapping was to build an interactive, digital
map showing specic socio-environmental health risks in favelas (slums) and to subsequently
build action plans for communities, civil society actors, and government.
2
In workshops with
twenty-ve youth at a time, CEDAPS invited participants to interrogate conceptual categories
of risk and identify those that were most pressing in their communities. The youth then took
pictures of these theme-based risks to populate a map of their environment through an Android
application built with the assistance of MIT Media Lab and InSTEDD. The application enabled
each user to take a picture, write a tagline and any commentary, and geo-locate the information.
When the cellphone connected to the Internet, all the mapped items synchronized with the
UNICEF-GIS mapping server.
3
(See Picture23.1.)
When the group members were younger or averse to using technological tools, CEDAPS
used a second technique: the Mapa Falante (Talking Map), which is a hand-drawn map offering
a symbolic, graphic representation of local points of interest. Although it lacks cartographic
rigor, this process allows community residents to register how they think about their neighbor-
hood, to highlight those areas of high risk, community strengths, and potential interventions,
thus adding a layer of social meaning—from the perspective of those who experience and live
in the territory—to the two-dimensional space of a traditional map.
PICTURE 23.1 Recycle Project: Young Mapper Using “Voices of Youth Maps”
App to Document Garbage Accumulation.
Source: © CEDAPS/Ives Rocha.
Global Health Policy 325
The third form of community mapping was an aerial mapping technique developed by the
Public Laboratory for Open Technology and Science (http://publiclab.org/) and adapted for this
project. Held securely within an aerodynamic capsule, a digital camera was attached to the line
of a delta kite and set to take a picture every second as it rose into the air. Once downloaded,
the individual photos could be manipulated and stitched together to form a complete picture
that was often several years more current than existing Google satellite footage. That picture
showed houses and the extension of the community where there had been no previous record,
thus providing community residents with concrete evidence, or “proof of place,” that could be
leveraged to demand government services.
After the digital and aerial mapping, youth participants met with CEDAPS and local part-
ners to dene action plans addressing the identied risks in the form of youth-led community
mobilizations as well as political advocacy, where they presented their data-backed demands to
the municipal government. Taken together, these mapping techniques offered opportunities for
youth participants to know and redene their space. By using their realities as teaching mate-
rials, the training aimed to offer participants new perspectives to problematize and debate their
surroundings: as the technical coordinator of the initiative noted, “in registering their reality
through image and proposing concrete changes, boys and girls see themselves not only as sub-
jects able to critically analyze their reality but also as actors responsible for its transformation”
(Rocha,2014).
Mapping Successes
Of all the themes mapped (poor accessibility, trash accumulation, frayed or knotted electrical
lines, risks of housing collapse and landslides, open sanitation, and gender-based violence),
only one was present across all communities: the accumulation of trash. The density of housing
in favelas in Rio de Janeiro, broken only by narrow footpaths, means that these low-income
communities are often deprived of effective public trash collection. With no trashcans or dump-
sters in sight, refuse accumulates on hillsides, wells, and the public paths snaking between
homes—by providing nooks and crannies for bacteria and mosquitos to thrive, the piles of trash
contribute to high rates of various preventable diseases, including dengue and Zika.
It should be no surprise then that trash served as a lightning rod for mobilization in mul-
tiple communities following the mapping process. In Morro dos Prazeres, a favela climbing the
hills above the historic Santa Teresa neighborhood, CEDAPS partnered with a local association,
Galera.com, to draw attention to a massive trash heap that had caused a landslide earlier that
year. Branding their project Acredite e Faça Acontecer (“Believe and Make It Happen”), Galera.
com invited the government trash collection agency to a clean-up day they organized with res-
idents. With the support of the municipal government, they removed two tons of trash. In part-
nership with UNICEF and CEDAPS, Galera.com and other local institutions then mobilized the
same youth participants to renovate the open space next to the former dump, turning it into a
community recreation space (see Picture23.2). Dozens of other activities similar to these were
planned and executed in two other favelas, Morro de Macacos and Morro de Borel. In both,
the local housing associations distributed trash cans throughout the community and lobbied the
municipality to move the dumpster sites where they collect trash to more convenient areas.
In one case in 2015, a public school launched the youth-led digital mapping as an elective
course for students. The course was instituted at Ginásio Olímpico Juan Samaranch in the Rio

326 Community-Based Participatory Research for Health
Comprido neighborhood through the initiative of the geography teacher. Every week for fty min-
utes students carried out each stage of the mapping process. The semester commenced with twelve
students and ended with thirty-three, plus a waiting list. As in the mapped favelas, the principal
problem students identied was the inadequate disposal of solid refuse in the three favelas around
the school. As part of the mitigation action plan, the students launched an educational campaign
themed “a little gesture makes a big difference,” which sought to sensitize all ve hundred stu-
dents and the almost eight thousand people who transited around the school daily.
The youth-led digital mapping project also was successful in pushing the municipality of
Rio de Janeiro to take limited action. In one instance, youth participants in the Morro de Praz-
eres took a particularly impactful picture of young girl crossing a deteriorating wood bridge,
just steps away from a gaping hole. When the director of the project’s government partner saw
the picture, he ordered the bridge rebuilt out of concrete.
Lessons from CEDAPS Mapping
Although many lessons were learned from the described youth-engaged mapping and action
experiences, ve stand out as particularly important:
Location-specic approaches to community issues galvanize mobilization more than
higher-level ones. Across all the methodologies used, youth participants were invited to criti-
cally consider the pressing issues facing their communities. Of the three types of mapping, the
PICTURE 23.2 Recycle Project: João Tuteia Square—From Dump Site to Recreation
Place in Two Years of Mobilization and Action.
Source: © CEDAPS/Ives Rocha.
Global Health Policy 327
two that elicited the greatest positive responses by participants were the digital map and the
Talking Map, through which they highlighted and located the risks that youth face every day.
For external partners, the digital map was of most interest, because it provided a traditional geo-
graphic perspective and the layer of social meaning ascribed by the community. Youth could not
relate as directly to the aerial map, perhaps because non-recognition by government was less
immediately pressing than other, more-common injustices.
Local leaders are needed to act as intermediaries to legitimize community knowledge
and promote follow-through. The collaborative partnership with local leaders (coming from
institutions such as community associations, housing associations, women’s associations, and
schools) was a critical success factor in three respects. First, they were necessary to secure the
buy in of residents; almost always, youth participants needed to overcome the distrust of resi-
dents who had witnessed years of frustrated attempts to implement change. Second, strong local
institutional backing was necessary for the implementation of the action plans derived by the
youth. Such backing, in fact, proved critical in helping keep participants motivated and together
beyond the workshop. When such backing was not present, youth engagement fell off, with
some groups disbanding. Finally, participants’ recognition and power outside the community
bridged the gap between residents and government authorities. They helped mitigate one of the
most-complex challenges faced: guaranteeing that the voice and self-determination of youth
was respected while ensuring a collaborative partnership. Each time the initiative was launched
in a new site, the advice and feedback of all local actors was included, including youth and ado-
lescents. Further, because each neighborhood was unique, adjustments were always necessary.
Government involvement is critical, even though it sometimes creates bottlenecks. From
the beginning of the youth-led digital mapping, the team partnered with the Defesa Civil (Civil
Defense), a government body tasked with designing, coordinating, and implementing projects
to reduce disasters in the city. This partnership proved critical to the success of the mapping and
to the follow-up coordination with government entities, because Civil Defense made contacts,
built bridges, and pushed for action. At the same time, there is a large discrepancy between the
urgency felt by community residents (particularly youth and adolescents) and the bureaucratic
delays involved with making requests of—and getting action from—the city government. In this
regard, too, the policy mentorship (see Chapter20) provided by Civil Defense was valuable in
helping youth participants better understand, and not give up on, the politics of helping effect
change at the municipal level.
The different epistemologies of government agencies and communities can cause tension
and delays. Although the Civil Defense recognized the value of community youth perspec-
tives, the information generated was not considered sufciently systematic or technical. Thus,
despite its support, this organization proved unable to integrate the mapping database in its
original form and was forced by internal policy to reevaluate the mapped points, particularly
those that spoke about risks of landslides or housing collapse. Although partnership members
were still able to organize for action with the assistance of Civil Defense, the data were not used
as a foundation of policy decisions. This highlights a common challenge with CBPR, namely,
that information generated by communities can be seen as inferior to that generated by tech-
nocrats. This perception also underscores the importance of bringing government partners into
project design early to help ensure that the information generated will be in a form that meets
their needs.
328 Community-Based Participatory Research for Health
Pilot projects require responsive technical partners and back-up plans. As with any pilot
of a new tool, CEDAPS frequently faced challenges in the eld while sorting out bugs in the
technology. The implementing partnership’s success was, in part, because of highly engaged
technical partners, whose involvement allowed for rapid iteration and technical support. Even
with such assistance, however, delays sometimes were faced when the mapping application
was not functional, non-digital methodologies had to be employed, or when a return to the
community another day to redo the mapping was necessary.
Despite such limitations, however, this case study provides a useful illustration of the
impressive role youth can play as partners in digital and other mapping for information and
action, even in extreme resource-poor environments.
CASE TWO: NAIROBI, KENYA: SHACK/SLUM DWELLERS
INTERNATIONAL (SDI) IN THE MATHARE VALLEY
In Nairobi, Kenya, close to 65 percent of the population lives in informal settlements, or slums,
on about 10 percent of the city’s land area. Children under ve living in Nairobi’s slums are
almost three times as likely to die as their counterparts in the rest of the city, and women expe-
rience disproportionate health burdens compared to men. For example, more than a quarter of
all women and girls in Nairobi’s slums reported an episode of diarrhea in the past month, com-
pared to about one-fth of all Kenyans. More than 36 percent of slum-dwelling women report
being physically forced to have sex, and more than one-third report being sexually abused
(Swart,2012). This case study describes work in and with the Mathare informal settlement
located about six kilometers from the city center, with about 260,000 people, and composed of
thirteen different villages: Mashimoni, Mabatini, Village No. 10, Village 2, Kosovo, 3A, 3B,
3C, 4A, 4B, Gitathuru, Kiamutisya, and Kwa Kariuki.
From 2009 to 2014, Shack/Slum Dwellers International (SDI), an international NGO, part-
nered with and supported the Kenyan federation of the urban poor, called Muungano wa Wanavijiji
(Muungano). SDI and Muungano developed an action-research partnership with the University of
California, Berkeley, and the University of Nairobi to document living conditions in Mathare and
advocate for change. SDI, established in 1996, is a global network of community-based organiza-
tions of the urban poor with its origins in India, but it now has a presence in thirty-three countries in
Africa, Asia, and Latin America (http://sdinet.org). In Kenya, SDI supports Muungano, the national
federation of the urban poor with hundreds of community-based afliates. SDI assists Muungano’s
community-based organizations and the entire federation to organize residents, conduct research,
collaboratively advocate and negotiate with governments to deliver life-supporting services, and
address issues of tenure security, safety, and social and political exclusion (sdinet.org).
The aims of the Mathare collaboration were to develop and sustain community mobiliza-
tion that contributed to an alternative development plan and advocacy strategy for the entire
informal settlement, not just a specic mapping project. Multiple participatory data gathering
and mapping processes were employed, including household enumerations, spatial mapping,
designing place-based physical and social improvements, and drafting new plans and policies. In
these ways, data gathering and mapping explicitly included different groups: youth documented
safety; and women documented food, water, and sanitation locations; and schools were enrolled
to capture student and teacher perspectives. Resident planning teams were organized in each
village to organize a surveying and eld-mapping process (Makau, Dobson, & Samia,2012).

Global Health Policy 329
Making the Invisible Visible
In 2008–2009, the United Nations Environment Programme (UNEP) and the Kenyan National
Environment Management Authority (NEMA) proposed to clean up the Nairobi River and its
tributaries, citing health and environmental risks. A concern of Muungano and its network
of slum dwellers was that tens of thousands of urban poor residents living alongside water-
ways in Nairobi would be evicted through this river clean-up program (All Africa, 2008;
Weru,2012).
Muungano and the universities designed and implemented a detailed household survey,
training and employing residents in data gathering. A separate team generated aerial photos
using a camera attached to a balloon that was own over the entire Mathare settlement.
This created more than 5,400 detailed images of the community in much more detail than a
Google Earth image could provide. These images were “stitched together” digitally to create
a high-resolution “base map” that enabled residents to see their community in a new way.
The detailed aerial images highlighted potential health hazards not well documented before,
such as the presence of cooking near open drains (see Picture23.3). These and other ndings
were discussed in focus groups and directed ground-level mapping teams in their data collec-
tion efforts.
PICTURE 23.3 Balloon Captured Aerial Image Showing Cooking Pots (Round White
Circles Adjacent to Open Drain), Later Found to Contain High Amounts of Human Waste
Source: Edwin Simiyu. Used with permission.
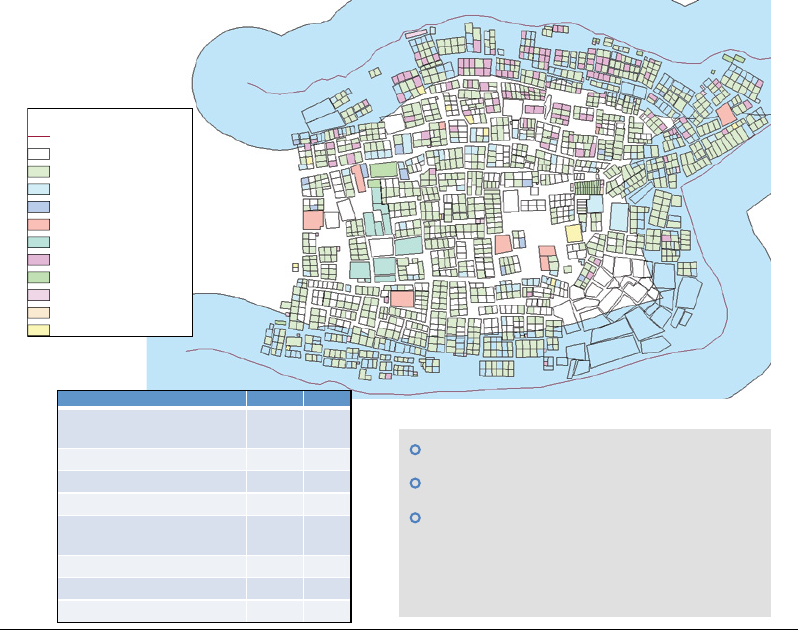
330 Community-Based Participatory Research for Health
The community satellite images and focus group discussions over community health pri-
orities were used to inform eld-based mapping, where teams of residents and students walked
every meter of the community to document the locations of each water point, toilet, electricity
power pole, food vendor, dump site, school, community facility, and other assets and hazards.
Student interns from the University of Nairobi worked with residents, and university courses,
co-led by UC Berkeley and University of Nairobi faculty members and involving tens of stu-
dents, were organized to conduct participatory mapping and data gathering.
First, data and maps were generated to highlight the number of people and types of
community activities that would be displaced by the UNEP river program (Figure23.1). These
data were presented to UN and local government, and residents marched to the Nairobi City
Council to prevent evictions. The data visualization combined with community mobilization
resulted in a temporary stay of planned evictions in Mathare. One result was a recognition by
the state, for the rst time, that community residents, working in partnership with universities,
could produce policy-relevant data.
Legend
Nairobi river
Missing/unknown
Residential 445 77.3
1,441 people (42.8% children)
753 total structures
92.5% tenants
N%
Business 17 3.0
Residential and business 2 0.4
Church 1 0.2
Vacant 79 13.7
Toilet or bathroom 29 5.0
Other 3 0.5
Unknown/missing data 215
Residential
Business
Residential and business
Church
Institution
Vacant
Bathroom
Waterpoint
Other
Toilet
FIGURE 23.1 Data Map of Potential Displacement of People and Activities
Source: Muungano wa Wanavijiji. Used with permission.
Global Health Policy 331
Sanitation and Women’s Health
A second key result of the processes in Mathare was a nding that girls and women were dis-
proportionately burdened from inadequate sanitation. Our map-making processes revealed the
uneven access to toilets across Mathare. However, it was survey and focus group data that com-
plemented the spatial mapping to highlight the serious health consequences of the maps. For
example, household survey data revealed that more than 83 percent of Mathare residents relied
on an unimproved pit latrine and that more than 60 percent used a “ying toilet,” defecating into
a plastic bag and throwing it into an open dump.
The team also heard in focus groups with Mathare women about the indignity they endured
from a lack of private, safe, well-lit, nearby toilets. One women noted:
Past eight, we can’t go out to use the toilet. There is no lighting and the men drinking Chang’aa
[local alcohol] on that side, get violent with us, even girls. We are forced to use a bucket...a
bucket in one room in front of your children, fathers and brothers. Can you imagine? Some-
times we use the “ying toilets” at night but your neighbors don’t like this. Without any gar-
bage collection, I wake up at dawn and sneak away to empty the bucket or dispose the bag.
There is no dignity in our toilet situation.
Team members also heard in focus groups with girls that they were more likely than boys
to miss school because of sanitation-related illness and lack of safe, private, and hygienic toilets
at their school. A lack of adequate toilets in schools decreases the attendance of girls especially
during their menstrual cycle (Chebbii,2014). One schoolgirl noted:
As girls, when we don’t have a toilet in school, we are forced to stay with one pad for a whole
day. I know many girls who just do not come to school during those days. Even if we have a
toilet at school and we have to share them with boys, girls will avoid them and stay home. We
do not have a bath place so I know when you have your period you do not want to smell in
school, so us girls avoid it.
For girls and women in Mathare, toilets are a relational issue of inadequate infrastructure,
safety, economic opportunity, stigma, dignity, and human health.
Collaborative Analysis and Policy
All maps and data were shared in draft form with community planning teams and during in-depth
discussions with residents over the meaning of the maps and how the information should be
used. For example, maps of the distribution of water points were used to advocate with the
Nairobi Water and Sewer Company to install new piped water service to residents. Muungano
used the data to not only advocate for piped water but also for a community-run management
scheme, so that economic opportunities and oversight responsibilities would go to local res-
idents. The campaign was successful and now acts as the Mathare-Kosovo Water Model and
is used in other urban slums across Kenya (Kenya Water Services Trust Fund [WSTF],2010).
All maps and data contributed to the Mathare Zonal Plan, a comprehensive upgrad-
ing plan for the community that was used to advocate for investments and organize disparate
improvement efforts (SDI, 2012). Two years after the publication of the report, the World Bank

332 Community-Based Participatory Research for Health
approached the university about the spatial data they created for upgrading sanitation, namely,
the trunk sewers. The GIS shape les were shared with the bank and the Athi Water Services
Board, and by 2014, ten kilometers of the community-designed sewer plan were constructed
in Mathare. In January 2015, the president of Kenya, Uhuru Kenyatta, came to Mathare and
launched a new project of the National Youth Service (NYS) to upgrade roads. The NYS also
used the Mathare Zonal Plan to determine where to formalize and tarmac new roads in Mathare.
Although data collection and mapping by slum dwellers continues in Nairobi’s informal set-
tlements, the work in Mathare has delivered tangible improvements to the living conditions
of residents and has given them “data” to negotiate with the state for greater recognition and
health-promoting resources (Picture 23.4).
ONGOING CHALLENGES AND OPPORTUNITIES
In both case studies, it is clear that mapping technologies have expanded beyond desktop GIS, with
capacity for community generation of data using free and publicly accessible web-based mapping
tools such as Google Maps, MapServer, OpenStreetMap, and GRASS GIS to only name a few
(maps.google.com, Mapserver.org, openstreetmap.org, grass.fbk.eu). These web-based tools have
made sophisticated mapping available to community and nonprot groups with limited resources,
in part because they have centralized and made freely available very high resolution background
geographic data, including satellite data, street photography, and building outlines.
PICTURE 23.4 Mathare Residents Review Maps During Community Planning Forum.
Source: Jason Corburn. Used with permission.
Global Health Policy 333
Importantly for CBPR, new social media, sometimes linked to mapping technologies, are
reshaping denitions of community and how people see themselves in relationship with their
surroundings, neighbors, and institutions by mapping things such as access to food or the respon-
siveness of government agencies. For example, individuals and community-based organizations
have mobilized citizens to send text messages and photos from mobile phones to track a range of
community health “eld” data that can be located on a map, many with addition geo-referenced
data, such as incidents of violence, housing code complaints, dangerous streets and intersections,
and pedestrian injuries (see crimemapping.com, www.everyblock.com, www.seeclickx.com,
www.infrastructurist.com/f-this/, www.appsfordemocracy.org/stumble-safely, www.mybikelane.
com, healthycity.org). Software developed by groups such as Ushahidi
(www.ushahidi.com)
are enabling community map makers to track identied community hazards and assets through
time (i.e., at what time of day a report was sent) and space (i.e., geographic location)—giving
rise to sophisticated “time-space health biographies.” These, in turn, are enabling collaborative
researchers to suggest that movement, and thus exposure, varies from person to person (e.g.,
elderly versus adult versus young person) living in the same place.
As suggested throughout this chapter, map making using CBPR should be open to engaging
with new technologies while also acknowledging its inherent limitations, because low-cost
mapping technology can help achieve multiple important ends:
■ Ensuring that community residents are valued coproducers of health knowledge
■ Offering a platform for community residents to express what matters to them and share this
with a world of potentially new listeners and allies
■ Providing new forums for residents and researchers to collaboratively generate innovative
solutions for persistent health inequities
■ Raising awareness among community members of the benets and pitfalls of technology,
such as the potential for overwhelming residents with too much information and creating a
dependency on technology
The cases presented here also raise some challenges for community members, activists,
academics, and others attempting to use mapping to extend CBPR for health equity. First,
organizing youth on scientic and health issues can be challenging, especially when engaged
research projects demand long-term, multiyear commitments and young people may have
limited available time (also see Chapter7). However, one recommendation from our experi-
ence is that the mapping process should engage young people early and often, especially as new
technologies, web, and social media geared toward youth become commonplace as mapping
tools. Partnering with youth can also help ensure that map making is fun, tied to local culture,
and even to a broader fund-raising strategy, as CEDAPS recognized. Engaging youth can also
support mapping as a strategy to build new organizational capacity, leadership, and power, espe-
cially when community members drive the research questions, selection of appropriate data,
and interpretation and presentation and use of results.
A second challenge is that the rapid pace of technological change and sophistication may
lead some groups to choose to leapfrog and start with the latest, most advanced tools. Our expe-
rience suggests that this rarely builds on local knowledge and may create an overdependency of
community groups on technology and outside expert advisors. Hence, we suggest that mapping
processes are most successful when they build incrementally from smaller to larger scale, from
334 Community-Based Participatory Research for Health
less to more complex, and from lower to higher technology. This trajectory can be rather quick
with skilled partnerships and collaborations, as shown by when CEDAPS quickly led from
the Talking Map into a digital one. Ultimately, mapping can act as a key piece of an ongoing
community-led research program.
A third challenge for mapping processes is to focus on bonding and bridging social capital
(Briggs1998), where bonding helps different CBOs and community members build trust and
partnerships among themselves and bridging allows mapping process and outputs to engage
with unlikely allies and change agents, such as regulators and academic scientists. Often, the
goal of a community mapping effort is to build community alliances and gather local knowledge
or challenge an inaccurate characterization of a place done by outsiders, but not both. The cases
presented here suggest that a both-and approach be explicit from the outset and designed into
the mapping process.
Fourth, linking concrete community health concerns with broader policy frames and cam-
paigns is another challenge of map making. Characterizing one’s community by selecting
certain features to map always requires value judgments over what to leave out. Instead of
viewing this as a weakness or limitation, we suggest that a community map-making process be
explicit about their issues and policy objectives from the outset, with place-based health ineq-
uities being one logical policy frame.
CONCLUSION: COMMUNITY MAPPING FOR HEALTH EQUITY
Community mapping can act as a core method and process when using a CBPR approach and
should be considered by all practitioners interested in building community knowledge and using
that knowledge to inform action, leadership, organizing, and ultimately improving the science
of assessing health burdens in places. As these two case studies have shown, when mapping
processes embody the core principles of CBPR, they can contribute to the following:
■ Building a power or organizing base in communities of color
■ Reframing community organizing priorities
■ Highlighting local knowledge
■ Linking the work to health equity
■ Demystifying research and environmental regulations
■ Changing policy and improving lives
Community mapping is one important tool to organize residents and extend CBPR’s
emphasis on ensuring that research contributes to action (Israel et al.,1998). As global public
health practitioners and social epidemiologists recognize that “place matters” for understanding
why some populations in some places get sick more often and die prematurely, community
mapping will be increasingly important for gathering information on the features and charac-
teristics of places that inuence well-being and moving from research to policy. Capturing haz-
ards and assets is crucial, and a CBPR approach is vital for ensuring residents and researchers
engage in a collaborative process for deciding what information to capture, what role different
technologies can play, what to display on maps, and how to share visual information within and
outside the community. What is crucial is that community members consider mapping as one
part of an ongoing global health equity advocacy and policy change strategy.
Global Health Policy 335
QUESTIONS FOR DISCUSSION
1. How can map making help community-driven research capture crucial knowledge that
other public health research methods might overlook?
2. What roles do public health professionals have in facilitating CBPR mapping processes?
3. How might map making help the poor develop new skills while also improving the
scientic evidence based behind public health interventions and policy making?
NOTES
1. CEDAPS is a NGO founded in 1993, based in Rio de Janeiro and active in several states of Brazil.
CEDAPS works with two strategies of health promotion: empowering communities in order for
them to become active social actors, generating local solutions, and proposing and developing inter-
vention strategies toward building and enhancing community-based public policies. Read more on
http://cedaps.org.br/.
2. CEDAPS used the Construção Compartilhada de Soluções Locais (Shared Contribution to Local
Solutions) methodology it has developed over years of operation (Edmundo & Nunes,2014).
3. Map visible at http://rio.unicef-gis.org/.
REFERENCES
All Africa. (2008). Kenya: Slum dwellers along Nairobi rivers face eviction (July). Retrieved from http://allafrica.com/
stories/200807090331.html
Briggs, X. S. (1998). Brown kids in white suburbs: Housing mobility and the many faces of social capital. Housing Policy
Debate, 9(1), 177–121.
Brown, T., McLafferty, S., & Moon, G. (Eds.). (2010). A companion to health and medical geography. Malden, MA: Wiley-
Blackwell.
Cashman, S. B., Adeky, S., Allen, A. J., III, et al. (2008). The power and the promise: Working with communities to analyze
data, interpret ndings, and get to outcomes. American Journal of Public Health, 98(8), 1407–1417.
Chebbii, S. J. (2014). Menstruation and education: How a lack of sanitary towels reduces school attendance in Kenyan slums.
BUWA (October). Retrieved from www.osisa.org/sites/default/les/27–31.pdf
Corburn, J. (2009). Toward the healthy city: People, places and the politics of urban planning. Cambridge, MA: MIT Press.
Cummins, S., Curtis, S., Diez-Roux, A. V., & Macintyre, S. (2007). Understanding and representing “place” in health
research: A relational approach. Social Science & Medicine, 65(9), 1825–1838.
Edmundo, K., & Nunes, N. R. (2014). Construção compartilhada de soluções locais: Guia de elaboração e gestão de proje-
tos sociais. Rio de Janeiro, Brazil: CEDAPS.
Ellaway, A., Benzeval, M., Green, M., Leyland, A., & Macintyre, S. (2012). “Getting sicker quicker”: Does living in a more
deprived neighbourhood mean your health deteriorates faster? Health and Place, 8(2), 132–137.
Emirbayer, M. (1997). Manifesto for a relational sociology. American Journal of Sociology, 103(2), 281–317.
Escobar, A. (2001). Culture sits in places: Reections on globalism and subaltern strategies of localization. Political Geog-
raphy, 20(2), 139–174.
Healey, P. (2007). Urban complexity and spatial strategies: Towards a relational planning for our times. London, UK:
Routledge.
Israel, B., et al., (1998). Review of community-based research: Assessing partnership approaches to improve public health.
Annual Review of Public Health,19,173–202.
336 Community-Based Participatory Research for Health
Kenya Water Services Trust Fund (WSTF). (2010). Formalising water supply through partnerships: The Mathare Kosovo
water supply model. Nairobi, Kenya: Author.
Kimbro, R. T., & Denney, J. T. (2013). Neighborhood context and racial/ethnic differences in young children’s obesity: Struc-
tural barriers to interventions. Social Science and Medicine, 95, 97–105.
Makau, J., Dobson, S., & Samia, E. (2012). The ve-city enumeration: The role of participatory enumerations in developing
community capacity and partnerships with government in Uganda. Environment and Urbanization, 24(1), 31–46.
Popay, J., Williams, G., Thomas, C., & Gatrell, A. (1998). Theorizing inequalities in health: The place of lay knowledge.
Sociology of Health and Illness, 20, 619–644.
Rambaldi, G., Corbett, J., Olson, R., et al. (2006). Mapping for change: Practice, technologies and communication. Participa-
tory Learning and Action (54). London, UK: IIED and CTA.
Rocha, I. (2014). Mapeamento digital liderado por adolescentes e jovens: Guia do facilitador. Rio de Janeiro: CEDAPS.
Retrieved from www.unicef.org/brazil/pt/guia_mapeamento_pcu1316.pdf
Swart, E. (2012). Gender-based violence in a Kenyan slum: Creating local, woman-centered interventions. Journal of Social
Service Research, 38(4), 427–438.
Weru, G. (2012). Nairobi rivers pose health, safety hazards. Daily Nation (May 26). Retrieved from www.nation.co.ke/News/
Nairobi+rivers+pose+health+safety+hazards+/-/1056/1414258/-/39258y/-/index.html
1
APPENDIX
CHALLENGING OURSELVES
CRITICAL SELF-REFLECTION ON POWER
AND PRIVILEGE
CHERYL HYDE
Source: Adapted from Hyde, Cheryl A. “Appendix 3: Challenging Ourselves: Critical Self-Reection on Power and
Privilege” in Community Organizing and Community Building for Health and Welfare, edited by Meredith Minkler.
Copyright © 2012 by Meredith Minkler. Reprinted by permission of Rutgers University Press.
One of the more common, and mistaken, assumptions that community practitioners make is
thinking that because they are “ghting the good ght,” they do not need to address issues regarding
their own power and privilege. Yet engaging in practice under the banner of social justice (or any
other “right” reason) does not result in an automatic community of shared interests. Nor does it
inoculate against the dividends that one might accrue because of race, class, gender, sexual orien-
tation, or other aspect of an individual’s cultural identity. Because so much of community practice
is relational (see Chapters4,5, and6), I suggest that it is essential for practitioners to undertake
in some rigorous self-exploration as part of their broader anti-oppression work. In this appendix,
I offer one approach to such critical reection that I have used in teaching and training efforts.
Similar to many individuals who engage in anti-oppression teaching and practice, I ground
much of my thinking in Peggy McIntosh’s (1989) classic essay, “White Privilege: Unpacking the
Invisible Knapsack.” By delineating the many ways in which white individuals benet from usu-
ally unrecognized or unacknowledged everyday expectations, rituals, and processes (e.g., “I am
338 Appendix 1
never asked to speak for all the people of my racial group” [p. 11]), McIntosh connects the
personal with broader structures that promote or protect racism and then issues a call to action:
“A ‘white’ skin in the United States opens many doors for whites whether or not we approve of
the way dominance has been conferred on us. Individual acts can palliate, but cannot end, these
problems. To redesign social systems we need rst to acknowledge their colossal unseen dimen-
sions. The silences and denials surrounding privilege are the key political tool here” (p. 12).
Part of the power of McIntosh’s essay is that the reader needs to contend with the cumulative
impact that seemingly minor activities can have on the perpetuation of racism. In demanding that
whites dissect their racial privilege, and then take steps to challenge it, she provided a foundation
for much of the anti-oppression work that followed. Comparable examinations can happen
for other privileges based on class, gender, sexual orientation, and so forth; indeed, there are
many, many examples in the literature (for varying approaches see Adams, 1997; Connell, 2005;
Gerschick, 1993; Goodman, 2001; hooks, 2000a, 2000b; Tappan, 2006; Wallerstein, 1999).
Although McIntosh’s contribution to antiracism work cannot be underestimated, her approach
does, I think, fall short in four important ways. First, it does not distinguish between how we see
our own privilege and how others might perceive or experience our identity. McIntosh is focused
on the former, yet those with whom we interact also bring to the encounters an awareness (or
not) of privilege as beneciaries or as those denied such benets. Second, she is focused on race
and racism, which is understandable but incomplete. Race is not the only attribute that shapes
how we negotiate the world. Third, because of this primary focus on race, McIntosh does not
capture how different cultural attributes interact and differentially shape privilege. For example,
a white middle-class woman and a white working-class woman both hold racial privilege, yet the
manifestation of that privilege will present differently because of class. And fourth, even though
McIntosh notes that “unseen dimensions” support societal structures, she nonetheless neglects
the broad, systemic impact of labor market, educational, residential, and other forms of institu-
tionalized racism (Jones, 2000). Fundamentally, hers is an intrapersonal framework for address-
ing racism: certainly critical but not sufcient. Grappling with these points, while still employing
the essential insights of McIntosh, became the catalyst for the approach that I use.
ONE APPROACH TO CRITICAL SELF-REFLECTION
Before outlining my approach to a critical self-reection for community practitioners, I want to
emphasize, rst, that this is a framework that I have found useful as a learner, teacher, trainer,
and practitioner. It is not, however, the only model out there, and it is well worth the effort to
nd a process that works well and authentically challenges you as a community practitioner.
Second, two assessments have been constructed for this appendix (see TablesA1.1 andA1.2),
but they are adapted from tools that others and I have developed (Axner, n.d.; Burghardt, 2011;
Katz, 1978; McIntosh, 1989). These tools work best when the individual pushes him- or herself
to honestly complete them and then when a group debrieng can support further exploration
and exchange of ideas.
Step 1: Our Complex Cultural Selves
The rst step in this process is to understand the basics of one’s culture and the impact on iden-
tity. Here, I am referring to the values, attitudes, beliefs, practices, and rituals that shape who we

Appendix 1 339
are and how we act, all of which ow from the various groups of which we are members. The
primary cultural dimensions that I focus on are race, gender, citizenship status (in the United
States), sexual orientation, class, religion, and physical or mental ability. There may be other
dimensions that are important to an understanding of the cultural self (e.g., region of the country
or level of education), but I nd that these are the signicant ones and serve as important spring-
boards to self-awareness.
So turn to the Cultural Identity Inventory (Table A1.1) and consider the rst three col-
umns: “cultural dimensions,” “manifestations, and “interactions.” For each dimension, indi-
cate what you are (note any conicting messages or challenges to this self-identication) and
whether there are any important values, messages, or actions associated with that dimension.
For example, if you are a lesbian, did you receive messages of acceptance or condemnation? Or
if you are a male, were you told that certain emotions or displays of emotion were not manly
TABLE A1.1 Cultural Identity Inventory
Cultural
Dimensions Manifestations Interactions
Domination or
Subordination Vantage Points
Indicate for each
(note any conict
concerning this
identier)
What values,
actions, or
messages are
associated with
the dimension?
Does the effect
of this dimension
interact with any
other dimension?
How so?
If dominant—
what privileges
do you have?
How have you
responded?
If subordinate—
what have you
been denied?
How have you
responded?
How do you
understand
this aspect
of yourself?
How do
you think or
experience
the way
others see you?
Gender
Race
Class
Sexual
orientation
Citizenship
Religion
Physical or
mental ability
Other?
340 Appendix 1
(i.e., unacceptable)? As you start this inventory, you may be able to see how different aflia-
tions inuence one another, for example, how messages about being female are shaped by one’s
religion. You should note these connections as they became apparent. What should begin to
become apparent is that we are more than just one or two cultural attributes. The foundation of
our cultural selves is the complex whole that is generated from these dimensions.
Review and reect on your inventory. Consider these questions:
1. What are your overall reactions to this information (any afrmations, surprises, points of
confusion)?
2. Does any dimension stand out as particularly important to your overall cultural iden-
tity and why?
3. What have you learned about yourself? What next steps in this process do you see your-
self taking?
It also is important to understand that the level of inuence exerted by these dimensions on
one’s cultural self might not be the same and can vary over time. You might even want to note
if a particular dimension is exerting a relatively strong (or weak) effect on you and why. If we
imagine these dimensions arrayed in a pie chart, some wedges will be larger than others, and,
sometime in the future, these wedges could be resized. This is one reason why it is unwise (and
even foolish) to assume that you know a person’s culture based on just one or two character-
istics. What is important to you may not be as signicant to another, because that individual is
perhaps more concerned with, or inuenced by, a different cultural dimension. There is uidity
to the components of one’s identity, depending on specic challenges of a given time and place
as well as negotiating daily life.
Step 2: Privilege and Power
Within each of these dimensions there is a dominant and a subordinate group (see TableA1.1,
column 4). A dominant group is one that as a group has access to economic, social, political,
and civic privileges. This access is temporal and systemic, and the privileges may be con-
sciously sought or unconsciously acquired. The point is not whether each individual in a given
group always (and knowingly) enjoys privilege or even wants it (or asked for it). It is about the
societal group, which, through its collective activity, turns that privilege over time into soci-
etal power. So in twenty-rst-century America, the privileged groups include men, whites, the
middle and upper classes, heterosexuals, citizens, the able-bodied, and Christians. Continuing
with the Cultural Identity Inventory, indicate whether you are a member of the dominant or sub-
ordinate group for each cultural dimension in column 4.
Individuals who nd themselves mostly or exclusively in dominant-status groups are not
bad or evil. Rather, by virtue of these group memberships, they have beneted from various
societal “perks,” whether they asked for them or not. But once such privilege is revealed, these
individuals have an obligation to question, challenge, and otherwise act in good faith to work
toward the dismantling of a system that generates such disproportionate rewards based on group
membership. And the key here is taking action; wallowing in guilt or engaging in excessive
Appendix 1 341
hand-wringing does nothing to contribute to anti-oppression work (indeed, such responses just
further underscore one’s privileges).
Conversely, the individuals who nd themselves mostly or exclusively in subordinate-status
groups do not have license to claim victimhood and then withdraw from any constructive action.
The tasks for those with less privilege is to understand the injuries, hidden or explicit, that group
subordination may have caused (for an excellent analysis of this, see Sennett and Cobb’s [1972]
classic work, The Hidden Injuries of Class). How, for example, has one addressed internalized
oppression? Individuals from subordinate-status groups also need to take action against oppres-
sive structure and processes, though their paths to, and strategies for, that action will likely dif-
fer from the work that dominant-group individuals undertake.
For most of us, however, it isn’t a matter of being in either all-dominant or all-subordinate
groups. Instead, our cultural identities are composed of a mix. So we might have access to racial
or gender privilege, yet be in subordinate groups for religion and sexual orientation. To further
complicate this understanding, as noted, not all dimensions have equal weight on our overall
identity. We should not, however, let this complexity become an excuse for not owning the priv-
ilege that we may have. Yes, I may need to contend with a disability or gender discrimination,
yet I also need to be mindful that as a white, professional person, I benet from race and class
privilege. Moreover, these societal dividends provide me with some resources with which to
address or cope with subordination that results from membership in other groups. It is essential
that we push ourselves to understand the implications of this complexity.
Step 3: Understanding Different Vantage Points
A nal factor that I consider in this particular approach to understanding cultural identity
focuses on how we see ourselves versus how others perceive us. Although it is tempting to think
that we have primary or sole control over the making of our cultural identity, we do not. When
we interact with, or are simply in the presence of, others, our cultural identity is being shaped by
that individual’s ideas, beliefs, attitudes, experiences, and so forth. This may not always be fair,
but in relationship building, we are always negotiating the perceptions and reactions of others
and hopefully in the process can address any misperceptions.
Referring again to the Cultural Identity Inventory, column 5, push yourself to consider
your subjective (self-)understanding of each cultural dimension and then the understandings of
others. If you are white, how do you view this and how do you experience others viewing that?
If you have a disability that is not readily apparent, how do you understand this and how might
others (if at all)? The point of this aspect of the inventory is to understand that how you move
through life does not necessarily correspond with how others see that journey. What you think
might be central to your identity may not even register with someone else. Conversely, what
you minimize (such as racial privilege) may be of central import to others. Making the genuine
effort to understand how others experience you is critical to relationship building and essential
if you want to deconstruct and challenge your own societal privileges.
Step 4: Synthesis and Next Steps
Now comes the difcult work—digesting and then acting on what you have uncovered by virtue
of doing this inventory. Consider these three questions: (1) What are your overall reactions
342 Appendix 1
to this inventory? (2) Does any dimension stand out as particularly important to your overall
cultural identity and why? and (3) What have you learned about yourself and what next steps in
this process do you see yourself taking? In other words, the inventory, in itself, does not con-
stitute anti-oppression work. It is the precursor to anti-oppression actions. If you have pushed
yourself to be honest and reective thus far, then you have laid a foundation for considering
what you need to do. Perhaps education is needed—if so, how will you go about getting it?
Maybe an important relationship needs to be repaired—how might you take the steps to make
amends? Or perhaps the inventory revealed that some skills, such as assertiveness training, are
needed—where will you obtain this? Did you become aware of new potential problems or chal-
lenges for other groups, and if so, how might you respond?
It is tempting, and perhaps even human nature, to try to minimize the inventory messages
that we don’t want to know. It is not easy to think of oneself as “privileged,” particularly if
we don’t ask for it or believe we use that privilege to our advantage. Often, we become more
focused on those parts of our identity associated with subordinate-group membership and then
don’t see the privilege we might have. We also run the risk of becoming paralyzed by building
an identity of victimization. Self-awareness, exibility, empathy, and openness are essential, but
perhaps most important is understanding that anti-oppression work takes time (Burghardt, 2011;
hooks, 2003). Be patient with yourself and others as more authentic relationships are built.
CONNECTING TO COMMUNITY PRACTICE
Community practitioners would be wise to take a page from the training manual of most clinical
social workers, therapists, and counselors who are trained to be cognizant in the “use of self.”
Use of self may be dened as the knowledge and skill sets employed by the practitioner in such
a way that he or she becomes an instrument to facilitate change (Heydt & Sherman, 2005).
Within the parameters of the therapeutic relationship, the practitioner is able to model and
reect transformative possibilities for the client. Yet this approach is not without its dangers,
and considerable self-awareness is necessary if the practitioner wishes to minimize unneces-
sarily complicated or messy relationships with clients. As part of this training, these practi-
tioners learn to recognize and address the emotions generated in the therapeutic relationship;
identify what client actions might “push buttons”; negotiate expectations of the client, including
the maintenance of “appropriate” boundaries; and work through resistance and reluctance. The
cultural selves of practitioner and client signicantly affect these dynamics as cultural varia-
tions in seeking help, dealing with authority and power, and building relationships come into
play (Heydt & Sherman, 2005; Reupert, 2007). Thus, the use of self is actually the use of the
cultural self.
How does this translate to community practice? The strategic use of self is concerned with
relationship building that encourages constructive change, which in many respects is the core
of community practice. In order to be an effective community organizer or other practitioner
who can build the relationships necessary for increasing community capacity, that individual
needs to understand how his or her cultural identity affects facilitating and sustaining rela-
tionships. The assumption is that if one does not acknowledge or address the affect of priv-
ilege, then one risks poisoning this critical aspect of practice. Moreover, the ability to build

Appendix 1 343
authentic connections rests on how well one understands oneself. Many practitioners want to
move quickly to nding commonalities, but the realities of oppression—including the personal
side—need to be addressed rst (Burghardt, 2011). Time, patience, and humility are essential
ingredients in this process.
Building on the insights from the Cultural Identity Inventory, one needs to turn to making
connections between that awareness and community practice. For this, another assessment is
suggested (see TableA1.2). Adapted from Axner’s (n.d.) exercise, the goal is to identify how
one’s cultural identity helps and hinders one’s community practice abilities and then extend
these ndings by determining what one needs to continue with his or her development. This
information is then linked to an emerging use of self. By systematically engaging in this self-
assessment, one will not only understand how cultural attributes of the practitioner become part
of practice (for better or worse) but also begin to think strategically about how to maximize the
assets and minimize the concerns.
TABLE A1.2 Assessment: Connecting Cultural Identity to Community Practice
Cultural Dimension
As Strength or
Asset to My
Community Practice
As Challenge or
Concern to My
Community Practice
What Do I Need
to Continue My
Development?
Gender
Race
Class
Sexual orientation
Citizenship
Religion
Physical or
mental ability
Other?
Note the ways in which the different components of your cultural identity have inuenced you as a community
practitioner. Specically, record how that attribute has (1) given you strengths or assets and (2) provided challenges
or concerns.
A. Indicate what you need to continue your development (i.e., how can you build on your strengths or address
concerns?).
B. How does this assessment inform your cognizance of “use of self”?
Adapted from M. Axner, Diversity and Community Strengths (Lawrence, KS: Work Group for Community
Health and Development, University of Kansas, 2011); Community Tool Box, http://ctb.ku.edu/en/tablecontents/
sub_ section_tools_1170.aspx. Used with permission from the Work Group for Community Health and Develop-
ment, University of Kansas.
344 Appendix 1
SUMMARY
Community practitioners typically are concerned with, and adept at analyzing, the power struc-
tures and processes that affect their constituencies. In this appendix, I have challenged practi-
tioners to look at a more personal aspect of power—the privileges derived from membership
in dominant-status groups. I have argued that one’s cultural identity largely is determined by
these memberships, and I have highlighted the need for reecting on the multiple and often
intersecting identities we hold (woman, Latina, middle class, etc.). With a more comprehensive
understanding of our cultural identities, including the ways in which the various dimensions
can change and be challenged over time, we are better situated to build authentic relationships
with constituents and community members. In more fully understanding how we benet from
oppressive systems, we are more likely to nd the tools to dismantle the attendant structures
and processes. This is a critical aspect of “ghting the good ght” and takes time, self-patience,
and an openness to continued learning. In doing so, we forge better bonds with our partners and
allies and, ultimately, create better communities for us all.
REFERENCES
Adams, M. (1997). Pedagogical frameworks for social justice education. In M. Adams, L. A. Bell, & P. Grifn (Eds.),
Teaching for diversity and social justice: A sourcebook (pp. 30–43). New York, NY: Routledge.
Axner, M. (n.d.). Diversity and community strengths. Community Tool Box. Retrieved from http://ctb.ku.edu/en/tablecontents/
sub_section_tools_1170.aspx
Burghardt, S. (2011). Why can’t we all just get along? Building effective coalitions while resolving the not-so-hidden real-
ities of race, gender, sexuality, and class. Macro practice in social work for the 21st century (pp. 176–214). Thousand
Oaks, CA: Sage.
Connell, R. W. (2005). Masculinities (2nd ed.). Berkeley: University of California Press.
Gerschick, T. (1993). Should and can a white, heterosexual, middle-class man teach students about social inequality and oppres-
sion? In D. Schoem, L. Frankel, X. Zuniga, & E. Lewis (Eds.), Multicultural teaching in the university (pp. 200–207).
Westport, CT: Praeger.
Goodman, D. J. (2001). Promoting diversity and social justice: Educating people from privileged groups. Thousand
Oaks, CA: Sage.
Heydt, M. J., & Sherman, N. E. (2005). Conscious use of self: Tuning the instrument of social work practice with cultural
competence. Journal of Baccalaureate Social Work, 10(2), 25–40.
hooks, b. (2000a). Feminist theory: From margin to center (2nd ed.). Boston, MA: South End Press.
hooks, b. (2000b). Where we stand: Class matters. New York, NY: Routledge.
hooks, b. (2003). Teaching community: A pedagogy of hope. New York, NY: Routledge.
Jones, C. P. (2000). Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health, 8,
1212–1215.
Katz, J. (1978). White awareness. Norman, OK: University of Oklahoma Press.
McIntosh, P. (1989). White privilege: Unpacking the invisible knapsack. Peace and Freedom (January/February), 10–12.
Reupert, A. (2007). Social worker’s use of self. Clinical Social Work Journal, 35, 107–116.
Sennett, R., & Cobb, J. (1972). The hidden injuries of class. New York, NY: W. W. Norton.
Tappan, M. B. (2006). Reframing internalized oppression and internalized domination: From the psychological to the socio-
cultural. Teachers College Record, 108(10), 2115–2144.
Wallerstein, N. (1999). Power between evaluator and community: Research relationships within New Mexico’s healthier
communities. Social Science and Medicine, 49, 39–53.
APPENDIX
2
GUIDING CBPR PRINCIPLES
FOSTERING EQUITABLE HEALTH
CARE FOR LGBTQ+ PEOPLE
MIRIA KANO, KELLEY P. SAWYER, AND CATHLEEN E. WILLGING
With transphobia and homophobia, a lack of knowledge
can be just as damaging as a slur.
1
Although often focused on ethnic-racial minorities, community-based participatory research
(CBPR) approaches are equally benecial to address health inequities faced by other vulner-
able communities that face stigma and social marginalization. In 2014, we received a PCORI
Pipeline to Proposal award to address health inequities faced by lesbian, gay, bisexual, trans-
gender, and queer (LGBTQ+) people in urban and rural areas of New Mexico. The community-
academic partnership was formalized as the New Mexico LGBTQ+ Health Collaborative (the
collaborative), a fteen-person advisory board of health care advocates, patients, providers, and
health services researchers from across the state, whose stated purpose is to improve quality of
care for LGBTQ+ people based on their lived experiences. To promote community-partnered
research, optimal stakeholder communication, and better health care, the collaborative authored
Guidelines for Healthcare Research with LGBTQ+ Individuals and Communities in New Mexico
(see online resource at http://hsc.unm.edu/programs/nmcareshd/docs/LGBTQ-guidelines.pdf).
2
346 Appendix 2
This appendix provides a brief overview of this process and our key principles for positive and
productive partnerships.
Compared to their heterosexual, cisgender
3
counterparts, LGBTQ+ people are more likely
to suffer from mental health and substance abuse problems, eating and body-related disorders,
sexually transmitted diseases, poor diet and exercise, and are less likely to benet from preven-
tative services (Hembree et al.,2009; McNair & Hegarty,2010). Recent reviews of existing
guidelines to promote LBGTQ+ competence across clinical services have highlighted insuf-
cient inclusion of LGBTQ+ patient and provider perspectives in their design and implementa-
tion (McNair & Hegarty,2010).
Historical discrimination within health care services, including from cultural stigma
concerning sex and gender atypicality, have generated distrust by LGBTQ+ people of med-
ical institutions and research enterprises (Eckstrand & Sciolla,2015). Over the last fty years,
LGBTQ+ people have experienced denial of treatment for HIV/AIDS (Wright,2013), inva-
sive and damaging genital surgeries and hormone treatments to normalize sex and gender in
babies with ambiguous genitalia (Kessler et al., 1998), and ongoing damaging “reparative
therapies” (Berger,1994). Such commonplace experiences, also embedded in discriminatory
laws, policies, and care-giving practices, pathologize sexual and gender difference and alienate
LGBTQ+ patients.
DEVELOPING LGBTQ+ GUIDELINES
These guidelines were created to promote bidirectional learning, effective communication, and
trust among members of the LGBTQ+ community, health care providers, and health services
researchers to inspire health equity and catalyze social change. The collaborative developed a
series of semi-structured interview questions, UNM HRPO (14–077), to guide one-on-one dis-
cussions, and a collection of vignettes from LGBTQ+ individuals from New Mexico tapped to
discuss relational and participatory needs of sexual and gender minority research participants
from rural and urban areas of the state.
In 2015, a contracted ethnographer interviewed twenty LGBTQ+ New Mexicans. Partici-
pants were twenty-seven to sixty-ve years old, with a range of gender, sexual, and ethnic-racial-
cultural identities. Most resided in Albuquerque, but many were originally from rural and tribal
communities. Many had explicit interests in health research, with specialties of nursing, mental
health, and surgery. Other participants were students, advocates, activists, and self-described
“regular” members of an LGBTQ+ community.
Interview participants and members of the collaborative cited examples of research and
health care–related encounters that were “homophobic,” “transphobic,” “biased,” “discrimina-
tory,” and “insensitive.” Many suggested that such encounters could be avoided if researchers
and clinicians had greater exposure to and more information about LGBTQ+ communities and
more effective training in inclusive communication practices within health care and research.
For Native American or Hispanic participants, issues of research misconduct were brought to
the fore, as were calls to use CBPR, with special attention to negative historical relationships
Appendix 2 347
between the community and local universities in research. One participant stressed having
ongoing relationships with communities:
We would love to work with researchers on [LGBTQ+] issues, as long as the researcher will stick
around, and give something back to the community. Some have come in to research the trans
community. They gather information and just disappear. How does that help our community?
It just reinforces stigma, our sense of outsiderness, and negative feelings about research and
privilege on the part of academics.
The following three themes were considered essential in building research relationships
with LGBTQ+ communities.
Be Aware of the Link between Historical Trauma and Individual
Experiences of Trauma
Historical trauma theories posit that past violence and assaults (e.g., the colonization of the
Americas and slavery) have undermined physiological and psychological health, leading to
personal trauma among many in these same communities today. They also contend that histor-
ical oppression has led to a “weak mainstream political will to ameliorate [these disparities]”
(Chávez et al.,2008, p. 96). Although theories of historical trauma have been developed to
explain the colonization of Indigenous peoples and internment and genocide of Jewish peoples,
persons contributing to these guidelines were adamant that they be applied to past violence and
attempts to oppress LGBTQ+ populations.
The “humanity” of LGBTQ+ people has been dened historically in opposition to sexual
and gender roles considered “normal” by a dominant Western standard. Medical pathologiza-
tion of LGBTQ+ people, through the Diagnostic and Statistical Manual of Mental Disorders,
has been a source of historical trauma and contributes to gender- and sexuality-based social
trauma and violence. Collaborative members and participants provided insight into how such
trauma is internalized for LGBTQ+ individuals. One participant explained:
We are already pretty unhealthy in our community: smoking, substance use, obesity...but
there has to be a high level of understanding as to why that is. Systemic things and hardcore
trauma have created this. Please, don’t just tell people not to smoke, or to exercise more. This
really starts at healing from trauma.
Although LGBTQ+ communities and their allies may be well aware of endured traumas
that lead to health disparities, one participant observed, “The roots are not widely under-
stood by health care professionals.” Constant reinforcement of traumatic experiences can
lead to internalized trauma and “minority stress” for LGBTQ+ individuals excluded from
benets and protections offered to heterosexual and cisgender people (Meyer,2003). This
context must be understood by researchers to build strong and lasting partnerships with
community members.
348 Appendix 2
Understand the Intersectional and Diverse Identities and Experiences
of LGBTQ+ Individuals with Whom You Are Working
Although the umbrella term LGBTQ+ is often used as a cohesive category, it encompasses a
broad spectrum of diversity. Some LGBTQ+ individuals may experience gender and sexuality
as stable, identifying with certain categories throughout their lives, and others will experience
uidity, occupying different categories during their lifetimes.
“Sexual diversity means more than gay or straight,” stated one participant, adding that
“poly and kinky people can sometimes still feel stigmatized or sensationalized and not as free to
speak about their sexual lives and relationships.” A second addressed the “B” in LGBTQ+, clar-
ifying that “bisexual people have traditionally been largely ignored and often feel marginalized
and judged within the LGBTQ community [and research].” A third expressed concerns in terms
of cisgenderism and binary bias (versus inclusion) within LGBTQ+ health care and research:
I worry about non-binary folks...a lot of our work deals with more binary trans people, and
these folks get left behind more than anyone else; a lot of times it’s butch lesbians [and those
with] non-normative gender presentations who get the weirdest, most uncomfortable reactions.
For CBPR to be successful in LGBTQ+ communities, recruitment, data collection, and anal-
ysis must include diversity along the sexual and gender minority continuum while remaining
mindful of intersecting identities. Partnering with community leaders, advocates, and LGBTQ+
persons allows researchers to understand how gender and sexuality intersect with race, economic
position, regional and rural-urban locales, age, (dis)ability, and local contexts. For some, resi-
dency in rural areas, economic disadvantage, and even tribal afliation, can intersect to create
isolation and compound disparities in health and access to care. Others may nd rural residency
preferable, experiencing resilience through kinship networks from the local culture.
When working with LGBTQ+ people, investigators may encounter unique challenges, and
as a participant remarked, “We have to get creative to address the intersectionality of New
Mexico’s queer communities: for trans people living on the streets, we have to nd out how
to reach these individuals.” Describing the reticence some sexual- and gender-minority Native
Americans have in participating in research, one participant said, “Being labeled in general is
difcult for Native people—we had our names thrust upon us. So even adding 2S (Two-Spirit)
onto acronyms is challenging and not particularly accurate for a lot of us.” She added, “Maybe
that’s why we don’t get more Native [research] participation; with colonization and sovereignty
struggles—with the US governmental system that was pushed upon us.”
When Working in LGBTQ+ Communities, Using Preferred Terminology
and Maintaining Respectful Attitudes Are Important
For nonheterosexual and gender-nonconforming people, sexualized and gendered labels and
categories are not merely descriptive, they are deeply social and political identities. Identity
labels and pronouns are hotly debated within and outside LGBTQ+ communities. As one par-
ticipant explained, “Researchers should probably be aware of the internal politics and ten-
sions...In activist circles we pay great attention to language and pronouns.”
Persons sharing the same identities may identify differently from each other, and indi-
viduals who vary in identities or attraction may use the same label. For example, a cisgender
Appendix 2 349
women who sleeps with other cisgender women may identify as a lesbian, while another may
identify as queer. A transgender man in a relationship with a cisgender man may identify as gay,
as do many cisgender men in relationships together. A transgender woman in a relationship with
a cisgender man may also identify as gay.
Mislabeling someone may cause harm or repeat patterns of trauma. Gender-nonconforming con-
tributors to these guidelines cited ignorance or misuse of pronouns as a major source of misunder-
standing and harm in interactions with researchers and health care providers. One participant used an
example of seeking gynecological care to illustrate why it is important to be aware of pronoun use.
Already uncomfortable as a trans man and confronting past body and identity-related trauma, he had
put off seeking such care until the situation became life-threatening. At the appointment where he
learned that he would need an emergency hysterectomy, nurses repeatedly referred to him as “Miss.”
He said, “It added more trauma to the experience.” Participants unanimously agreed that a good rule
of thumb is for researchers and health providers to talk to research partners, ask what they call them-
selves, and avoid assuming identications based on how they present themselves.
QUICK TIPS FOR FOSTERING EQUITABLE RESEARCH PARTNERSHIPS
WITH LGBTQ+ COMMUNITIES
■ Begin by developing meaningful partnerships with community members and understand
the needs of the community in which you are conducting research.
■ Partner with leaders, advocates, and community members to dene research questions and
culturally sensitive research methodologies.
■ Incorporate inclusive, community-preferred language in consent documents and research
instruments. Acceptable pronouns may include they, them, ze, zhe, zir, hir, her, and him.
■ Use open-ended demographic forms: let participants dictate preferred names, pronouns,
labels, behaviors, what they call their relationships, and why.
■ Understand historical trauma within the LGBTQ+ community and how this trauma inter-
acts with other axes of historical trauma and oppression.
■ Train all CBPR team members (e.g., researchers, providers, and community members) in
LGBTQ+ competency.
■ Know the relationship between the community and your research institution (power dynamics
are often long-standing between institutions and communities).
Our experiences suggest that CBPR is an effective method for developing positive,
respectful, and long-term relationships with members of the LGBTQ+ community. The
CBPR approach provides a space for people with multiple intersecting identities to work
together to inform research projects with potential to create sustainable and equitable health
care experiences for LGBTQ+ people while simultaneously advancing the science of health
disparities.
ACKNOWLEDGMENTS
These guidelines were made possible through support by the Community Engagement Core of
NM CARES HD (http://hsc.unm.edu/programs/nmcareshd/cec.shtml#tabs1-toolkits).
350 Appendix 2
See research guidelines for Latino border communities at this same website: http://hsc.
unm.edu/programs/nmcareshd/docs/CECFINALGuidelinesHealthResearchBorderPromo-
tores10.03.15.pdf.
Spanish version for Latino border communities: http://hsc.unm.edu/programs/nmcareshd/
docs/CECFINALInvestigacionsaludFronterizasPromotores10.03.15.pdf.
The authors thank members of the New Mexico LGBTQ+ Health Collaborative, Edward
Fancovic, Rebecca Dakota, Greg Gomez, Barbara Cichosz, Amber Royster, Cameron Crandall,
Nathaniel Sharon, Beverly Gorman, Adrien Lawyer, Alma Rosa Silva-Bañuelos, and Robert
Sturm for their expert recommendations.
NOTES
1. K. Sawyer, personal communication with research participant (September 15, 2015).
2. Also see “Acknowledgments” for guidelines for Latino border communities.
3. Cisgender refers to individuals whose sex assigned at birth aligns with their gender identity.
REFERENCES
Berger, J. (1994). The psychotherapeutic treatment of male homosexuality. American Journal of Psychotherapy, 48(2), 251–261.
Chávez, V., Duran, B., Baker, Q. E., Avila, M. M., & Wallerstein, N. (2008). The dance of race and privilege in CBPR. In
M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to outcomes
(2nd ed., pp. 91–106). San Francisco, CA: Jossey-Bass.
Eckstrand, K. L., & Sciolla, A. F. (2015). History of health disparities among people who are or may be LGBT, gender non-
conforming, and/or born with DSD: A resource for medical educators. In A. D. Hollenbach, K. L. Eckstrand, & A. Dreger
(Eds.), Implementing curricular and institutional climate changes to improve health care for individuals who are LGBT,
gender nonconforming, or born with DSD (pp. 10–21). Washington, DC: Association of American Medical Colleges.
Hembree, W. C., Cohen-Kettenis, P., Delemarre-van de Waal, H. A., Gooren, L. J., Meyer, W. J., III, Spack, N. P., Tangpricha,
V., & Montori, V. M. (2009). Endocrine treatment of transsexual persons: An Endocrine Society clinical practice guide-
line. The Journal of Clinical Endocrinology and Metabolism, 94(9), 3132–3154.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues
and research evidence. Psychological Bulletin, 129(5), 674–697.
McNair, R. P., & Hegarty, K. (2010). Guidelines for the primary care of lesbian, gay, and bisexual people: A systematic
review. Annals of Family Medicine, 8(6), 533–541.
Wright, J. (2013). Only your calamity: The beginnings of activism by and for people with AIDS. American Journal of Public
Health, 103(10), 1788–1798.
APPENDIX
3
QUALITY CRITERIA OF
THE INTERNATIONAL
COLLABORATION FOR
PARTICIPATORY HEALTH
RESEARCH (ICPHR)
MICHAEL T. WRIGHT
Participatory approaches to health research are increasingly drawing the attention of funders,
decision makers, researchers, and civil society worldwide. There is a great diversity among
these approaches in terms of intention, theory, process, and outcome. Community-based partic-
ipatory research (CBPR) is an important contribution to these approaches from North America;
in other parts of the world there are other traditions of participatory research going by different
names (e.g., participatory action research, participatory research, action research, collabora-
tive inquiry). This diversity reects the large variety of people, places, and issues involved in
participatory health research (PHR) in many different countries and under widely varying con-
ditions. PHR is often viewed as being a means for achieving positive transformation in society
in the interest of people’s health, for example, by changing the way health professionals are
educated, the way health care institutions work, and the politics and policies affecting the health
of society.
352 Appendix 3
The International Collaboration for Participatory Health Research (ICPHR, www.icphr.org)
was created in 2009 as a place to bring together international learning about the application of
participatory research approaches to address health issues (Wright et al.,2009,2010). After some
debate, the ICPHR chose PHR as a neutral umbrella term that can encompass different national
and regional traditions. Through consolidating existing knowledge and reaching agreement on
common terminology and principles, the ICPHR seeks to strengthen the role of PHR in interven-
tion design and decision making on health issues and thus to provide a means for people most
affected by health problems to inuence how these problems are addressed in society. This includes
developing guidelines for conducting and evaluating PHR, describing which forms of theory and
evidence are produced by this approach, and nding a means for conducting systematic reviews of
the PHR literature in order to contribute to the body of international knowledge on health.
Some examples of the projects initiated by members of the ICPHR include the following: a
position paper on ethics has been published on the website and ethics case studies are being col-
lected from members in several countries for a book publication. ICPHR members are also devel-
oping position papers on empowerment, the training of professionals in participatory research,
and the relationship between PHR and implementation science. An international conference on
impact in PHR was held in Germany, resulting in special issues in two journals examining the
various effects of participation over the course of PHR projects. The ICPHR has also developed
a continuing education course that has been offered in English, German, and Portuguese and is
being piloted in an online version. And the project Kids in Action is drawing people of all ages
together from several countries who are interested in children’s participation in health research.
In its rst position paper (ICPHR,2013) the ICPHR sought to identify some of the central
characteristics of participatory approaches to health research that cut across various cultures.
The paper has since been translated into several languages and is used for promoting critical
thinking in the teaching and practice of PHR. Many people engaged in PHR nd the position
paper too long and complicated to be used in their work. To address this problem, Tina Cook
from the United Kingdom distilled the eleven primary characteristics into short statements that
are meant to describe the unique qualities of PHR. These statements are not necessarily specic
to research on health issues but rather can be applied to participatory research more generally.
ENSURING QUALITY: INDICATIVE CHARACTERISTICS
OF PARTICIPATORY (HEALTH) RESEARCH
The following criteria can be used when reecting on the quality of participatory research projects.
Participatory
The goal of PHR is to maximize the participation of those whose life or work is the subject
of the research in all stages of the research process, including the formulation of the research
question and goal, the development of a research design, the selection of appropriate methods
for data collection and analysis, the implementation of the research, the interpretation of the
results, and the dissemination of the ndings. Such participation is the core, dening principle
of PHR, setting this type of research apart from other approaches in the health eld. Whatever
Appendix 3 353
model is used to describe participation in the research process, the goal of PHR is to provide
the opportunity for all participants to be equitably involved to the maximum degree possible
throughout the research.
Locally Situated
PHR is grounded in the reality of daily life and work in a specic place and time. The issue being
researched must be located in the social system, which is likely to adopt the changes that result
from the research process. This is the strength of PHR and results in the further development of
local knowledge. It is this local dimension that often presents the greatest challenge to funders
and policy makers as well as to those who assume that their generalized knowledge (“scientic”
or “professional” knowledge, in the usual sense) is superior.
A Collective Research Process
In PHR the research process is typically conducted by a group representing the various stake-
holders taking part in the study. This group can include engaged citizens, members of civil
society (e.g., nongovernmental organizations), health and social welfare professionals, health
organizations, academic researchers, and policy makers. Any one of these stakeholders can ini-
tiate and lead a study. The title participatory researcher or coresearcher is not reserved for the
academics but rather designates all members of the research group. The leadership role con-
sists of facilitating a shared decision-making group process for developing, implementing, ana-
lyzing, and disseminating the research.
PHR Projects Are Collectively Owned
Consistent with the previously named principles, the ownership of the research lies in the hands
of the group conducting the study. The group needs to decide how best to report on the ndings
of the research in order to meet the set goals.
Aims for Transformation through Human Agency
PHR follows the explicit goal of creating positive social change as a result of the research pro-
cess for those persons whose life or work is the focus of the research. Typical research goals are
as follows:
■ Improving the health of a specic group of people
■ Addressing the social determinants of health by improving living standards
■ Addressing the political determinants of health by changing repressive or restrictive policy
■ Improving the quality of services by addressing organizational issues
A quality criterion for PHR is supporting transformation processes that go beyond the span
of the research project so as to contribute to lasting change in the interest of better health. Sus-
tainable change is promoted, for example, by involving a broad coalition of stakeholders in the
research, setting up structures for sustained learning and action as part of the research process,
and providing skills training for local people to carry on the initiatives launched during the
research once the project is completed.
354 Appendix 3
Promotes Critical Reflexivity
Critical reexivity means considering how power and powerlessness affect the daily lives and
practice of those whose life or work is the focus of the research. It requires professionals to
question their roles and their knowledge based on power differentials between themselves and
service users and based on the expertise gained through life experiences and the social disad-
vantages faced by people without professional health qualications.
Produces Knowledge That Is Local, Collective, Cocreated,
Conversational, and Diverse
Knowledge produced by health research is typically by and for an academic audience. Often
highly technical in methodology and reporting, the knowledge can be difcult to diffuse to
policy makers, practitioners, community leaders, and others who could use the information to
make change. Knowledge produced through PHR is accessible to different audiences, espe-
cially for whom the work has direct impact.
Strives for a Broad Impact
An explicit intention of PHR is to bring about social change. Social learning (learning together
and from each other) is a fundamental dimension of the PHR process, and the continual cycle
of “look, reect, act” underpins the dynamics of developing a connected knowing. Interactive
processes engage people in transformative learning, that is, changes in the way they see the
world and themselves. This generates an intention of being able to act based on their experience
during the research and the research ndings, thus having a wider impact.
Produces Local Evidence Based on Broad Understandings of Generalizability
The generation of local evidence can accumulate over time, strengthening the ability of local
participants to take effective action. Transfer of interventions from one locality to the next is
about understanding the contextual conditions in the new setting, how they differ from the
setting in which the knowledge was produced, and reecting on the consequences.
Follows Specific Validity Criteria
■ Participatory validity: extent to which stakeholders take an active part in research process
■ Intersubjective validity: extent to which the research is viewed as being credible and mean-
ingful by the stakeholders from a variety of perspectives
■ Contextual validity: extent to which the research relates to the local situation
■ Catalytic validity: extent to which the research is useful in presenting new possibilities for
social action
■ Ethical validity: extent to which the research outcomes and the changes exerted on people
by the research are sound and just
■ Empathic validity: extent to which the research has increased empathy among the participants
Is a Dialectical Process Characterized by Messiness?
As knowledge and action strategies generated by PHR arise out of a collective research process
characterized by dialogue among participants with different perspectives on the subject under
Appendix 3 355
study, this does not necessarily result in a consensual view. It may reveal and promote several
different views resulting in different ways of addressing the issue at hand. The occurrence of
this messiness is a fundamental characteristic of PHR and its nonlinear, multifocused research
process and outcomes that cannot be characterized prior to the study. The rigor in PR lies in the
extent the research is facilitated so as to make possible new, transformative insights that offer
fresh approaches for action.
REFERENCES
International Collaboration for Participatory Health Research (ICPHR). (2013, May). Position paper 1: What is participatory
health research? Berlin, Germany: International Collaboration for Participatory Health Research. Retrieved from www.
icphr.org/uploads/2/0/3/9/20399575/ichpr_position_paper_1_dention_-_version_may_2013.pdf
Wright, M. T., Gardner, B., Roche, B., von Unger, H., & Ainlay, C. (2010). Building an international collaboration on par-
ticipatory health research. Progress in Community Health Partnerships: Research, Education, and Action, 4(1), 31–36.
Wright, M. T., Roche, B., von Unger, H., Block, M., & Gardner, B. (2009). A call for an international collaboration on partic-
ipatory research for health. Health Promotion International, 25(1), 115–122.
APPENDIX
4
CULTURAL HUMILITY
REFLECTIONS AND RELEVANCE FOR CBPR
VIVIAN CHÁVEZ
The words humanity and humility come from being tied to the earth and the
soil. Unpretentious. Being able to tell the truth and acknowledging that to tell
the truth is to allow suffering to speak. There is no real talk or engagement with
the truth about our lives, individually, collectively, nationally, or globally without
allowing suffering to speak.
Cornel West, Keynote, AmeriCAn PubliC HeAltH AssoCiAtion meeting, Denver (2010)
In their seminal essay, “Cultural Humility versus Cultural Competence,” Tervalon and Murray-
Garcia (1998) reframed the discourse of health disparities and institutional inequities in med-
icine. The authors dened cultural humility as “a lifelong commitment to self- evaluation and
critique, to redressing the power imbalances in the physician-patient dynamic, and to devel-
oping mutually benecial and non-paternalistic partnerships with communities on behalf of
individuals and dened populations” (p.123). Cultural humility is a rich multifaceted construct
that reects key dimensions of CBPR thinking, behavior, and actions and recognizes the perva-
siveness of culture in every research encounter (see BoxA4.1). Now cited in 894 related pub-
lications, cultural humility is recognized as a resource in a number of elds including public
358 Appendix 4
health (Chávez et al., 2008; Fleckman et al., 2015; Minkler,2012; Rajaram & Bockrath,2011;
US Department of Health and Human Services,2009; Wallerstein & Duran,2010; Yonas et al.,
2006); psychology (Gallardo,2014; Hook et al., 2013;); social work (Fisher-Borne, Cain, &
Martin,2014; Hyde,2012; also Appendix 1; Ortega & Coulborn,2011); nursing (Faronda, Bap-
tiste, Reinholdt, & Ousman, 2016); community development (Rice, 2007; Ross, 2010); and
spiritual formation (Owen et al., 2014).
Although denitions play an important role in enhancing collaboration between and
within disciplines, solidarity, more than cognitive understanding, is required. Cultural humility
is an embodied approach that expands the frame from traditional understandings of race and
ethnicity to include the culture of building alliances between groups and individuals from
diverse backgrounds, genders, sexual orientation, (dis)ability, educational levels, immigration
status and other socioeconomic and social-identity indicators. “Humility, and not so much the
discrete mastery traditionally implied by the static notion of competence, captures most accu-
rately what researchers need to model” (Tervalon & Murray-Garcia,1998, p. 120). Cultural
humility takes into account the uidity of culture and challenges individuals and institutions
to address inequalities (Fisher-Borne et al., 2014). The concept came out of the social injus-
tices experienced by Rodney King in 1992 when people all over the world watched videotaped
images of an African American man brutally beaten by the Los Angeles police. “At Children’s
Hospital, Oakland, we started talking about our own private Rodney Kings, the circumstances
where families felt they were not being taken care of in a respectful way. That was a big part
of our work, being certain that we were living up to the principles; that given the composition
of the faculty and given the composition of the patients, the faculty (alone) could not teach
about the issues of culture and race, difference and income” (see Chávez,2012 [video]). As
the National Partnership for Action to End Health Disparities (2015) notes, cultural compe-
tence is part of the evolutionary process toward cultural humility. Ultimately, “experiencing
with the community the factors at play in dening health priorities, research activities and
community-informed advocacy activities require that we recognize that foci of expertise
with regard to health can indeed reside outside of the academic center” (Tervalon & Murray-
Garcia,1998, p. 122).
Faronda and her colleagues (2016) provide a concept analysis for cultural humility based
on use of the term in articles published between 2009 and 2014. They note that the movement
toward cultural humility implies social and personal transformation and not only skills and
information about various cultures. “Cultural humility involves a change in overall perspective.
Box A4.1 Principles Guiding Cultural Humility That Resonate with Principles
of CBPR
■ Lifelong learning and critical self-reection
■ Recognize and change power imbalances
■ Develop mutually benecial partnerships
■ Institutional accountability
Appendix 4 359
Cultural humility is a way of being. Employing cultural humility means being aware of power
imbalances and being humble in every interaction with every individual” (Faronda et al., 2016,
p. 214). On a similar note, Rajaram and Bockrath (2011) advocate for integration of reective
inquiry of researcher’s social location in systems of privilege and oppression to extend beyond
mastery of knowledge and communication skills to a deeper understanding of the underlying
sociopolitical and economic processes of power and privilege that create, support, and maintain
existing health disparities.
TEACHING CBPR WITH CULTURAL HUMILITY
Strong CBPR partnerships reect three levels of cultural humility: intrapersonal, interpersonal,
and institutional. Through community dialogue, the relationship-based character of cultural
humility has the potential to open courageous conversations and offer healing to communities
of practice. At the intrapersonal level, researchers, teachers, and students of CBPR engage
in critical self-reection and awareness of biases and limitations. They commit to a lifelong
learning process that includes “not knowing” and deference to multiple sources of knowledge.
This key aspect of the model is difcult given academic training in having “expert knowledge”
at all times. The place of humility is a full-bodied experience that requires recognition of how
each of us is socialized by the cultures of the university, health department, hospital, or other
professional workplaces. We embody structures and may contribute to making invisible and
exploiting others through our positions of privilege without intention because of lack of aware-
ness. Instructors are prepared to design classroom activities that provoke emotional responses
necessary to expand students’ comfort zone and explore bias in an open environment without
reacting or defending.
The interpersonal level is the level of partnership in which issues of race, ethnicity, class,
gender, disability, and other forms of hierarchy present in academia and the health professions
risk being replicated at community gatherings, one-on-one, or in CBPR partnerships. Building
alliances across differences and having a commitment to redress power imbalances need an
action plan and adequate time dedicated to develop, implement, and evaluate the intended
actions. Approaching community members as peers starts with recognizing students as col-
leagues and partnering with them in their education. Even when CBPR researchers come
from working class backgrounds or are people of color, of the same gender identity, religion,
age group, and so on, we must be aware of the varied historical experiences of powerless-
ness, poverty, racism, trauma, and privilege. Peer learning promotes a culture of collaboration
and cooperation that takes practice and is a key component of the hidden or implicit curric-
ulum for CBPR.
At the institutional level, organization(s) sponsoring CBPR recognize and value the
dynamic terrain of culture. Currently, a third of the US population is composed of racial-ethnic
“minorities,” and in some communities the word minority itself is a misnomer. The institu-
tion is thus committed to an ongoing examination of stafng patterns and equitable hiring,
training, and advancement practices that are representative and drawn from the communities
being served. Antidiscrimination policies are followed, updated, and revised to reect culturally
appropriate language. There is a supportive environment for professional development in the
areas of unlearning oppression and examining privilege.
360 Appendix 4
CONCLUSION
Humility is an elusive concept with ethical dimensions emphasized by spiritual practices
worldwide. An expanded denition of health includes spirituality as the fourth dimension of
health (World Health Organization, 1991) and emphasizes social engagement and mindful-
ness. Freire was a deeply spiritual human being who believed in humility to be an act of soli-
darity (Boyd,2012; Darder,2000). Freire’s solidarity was not simply a cognitive decision but a
spiritual transformation that brings one into identication and common struggle with those who
have less power. Freire himself said, “dialogue cannot exist without humility” (Freire,1970,
p. 79). Given the centrality of authentic dialogue and collaboration between partners in CBPR
to understand, study, and address community-identied problems, cultural humility is a basic
requirement.
“Denitions are vital points for the imagination,” says bell hooks, in All about Love (2000,
p. 14). “A good denition marks our starting point and lets us know where we want to end up.
As we move toward our desired destination we chart the journey, creating a map.” Reversing
the starting point, I end with an open-ended denition of cultural humility and an invitation
for readers to keep nding its meaning, particularly in relation to CBPR. Genuine, high-level
CBPR can move cultural humility from idea to embodied practice. Cultural humility is a daily
practice of self-study, openness to understanding others’ cultures, and developing skills to deal
with and redress power imbalances. Often, it means changing organizational policy to reect
these commitments while building relationships based on mutual trust and a shared commit-
ment to equity and social justice.
REFERENCES
Boyd D. (2012). The critical spirituality of Paulo Freire. International Journal of Lifelong Education, 31(6), 759–778.
Chávez, V. (2012). Cultural humility: People, principles & practices [Video]. CES4Health.info. Retrieved from www.
ces4health.info/nd-products/view-product.aspx?code=XT4NJRJP
Chávez, V., Duran, B., Baker, Q., Avila, M., & Wallerstein, N. (2008). The dance of race and privilege in community-based
participatory research. In M Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From
process to outcomes (2nd ed.). San Francisco, CA: Jossey-Bass.
Darder, A. (2000). Teaching as an act of love: Reections on Paulo Freire and his contributions to our lives. Unpublished
manuscript. Retrieved September 1, 2016, from www.darder.org/publications/darderarticles
Faronda, C., Baptiste, D. L., Reinholdt, M., & Ousman, K. (2016). Cultural humility: A concept analysis. Journal of Trans-
cultural Nursing, 27(3), 210–217.
Fisher-Borne, M., Cain, J. M., & Martin, S. (2014). From mastery to accountability: Cultural humility as an alternative to
cultural competence. Social Work Education: The International Journal, 334(2).
Fleckman, J., Corso, M., Ramirez, S., Begalieva, M., & Johnson, C. (2015). Intercultural competency in public health: A call
for action to incorporate training into public health education. Frontiers in Public Health, 3, 210.
Freire, P. (1970). Pedagogy of the oppressed. New York, NY: Herder and Herder.
Gallardo, M. (2014). Developing cultural humility: Embracing race, privilege and power. Thousand Oaks, CA: Sage.
Hook, J., Davis, D., Owen, J., Worthington, E., & Utsey, S. (2013). Cultural humility: Measuring openness to culturally
diverse clients. Journal of Counseling and Psychology, 60(3), 353–366.
hooks, b. (2000). All about love. New York, NY: Harpers Collins.
Hyde, C. (2012) Challenging ourselves: Critical self-reection on power and privilege. In M. Minkler (Ed.), Community orga-
nizing and community building for health and welfare (3rd ed.). Rutgers, NJ: Rutgers University Press.
Appendix 4 361
Minkler, M. (Ed.). (2012). Community organizing and community building for health and welfare (3rd ed.). New Brunswick,
NJ: Rutgers University Press.
National Partnership for Action to End Health Disparities. (2015). Cultural competency; What is it and why is it necessary.
Southeastern Health Equity Council. Retrieved September 1, 2016, from http://region4.npa-rhec.org/in-the-spotlight/
resourceguidewhitepaper
Ortega, R., & Coulborn, F. (2011). Training child welfare workers from an intersectional cultural humility perspective: A par-
adigm shift. Child Welfare, 90(5), 27–49.
Owen, J., Jordan, T., Turner, D., Davis, D., Hook, J., & Leach M. (2014). Therapists’ multicultural orientation: Client per-
ceptions of cultural humility, spiritual/religious commitment, and therapy outcomes. Journal of Psychology and The-
ology, 42(1).
Rajaram, S., & Bockrath, S. (2011). Cultural competence: New conceptual insights into its limits and potential for addressing
health disparities. Journal of Health Disparities Research and Practice, 7(5), 82–89.
Rice, M. (2007). A post-modern cultural competency framework for public administration and public service delivery.
International Journal of Public Sector Management, 20(7), 622–637.
Ross, L. (2010) Notes from the eld: Learning cultural humility through critical incidents and central challenges in
community-based participatory research. Journal of Community Practice, 18, 315–335.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in dening phy-
sician training outcomes in multicultural education. Journal of Healthcare for the Poor and Underserved, 9(2), 117–125.
US Department of Health and Human Services. (2009). Transforming the face of health professions through cultural
and linguistic competence education: The role of the HRSA Centers of Excellence. Retrieved from www.hrsa.gov/
culturalcompetence/cultcompedu.pdf
Wallerstein, N., & Duran, B. (2010). Community-based participatory research contributions to intervention research: The
intersection of science and practice to improve health equity. American Journal of Public Health, 100(Suppl 1), S40–S46.
World Health Organization. (1991). Issue 9290211407. Chapter 4: The Spiritual Dimension. Retrieved from http://new.
worldlibrary.net/wplbn0000152157-world-health-organization-publication--year-1991--issue-9290211407--chapter-
4-by-world-health-organization.aspx?
Yonas, M., Jones, N., Eng, E., Vines, A., Aronson, R. E., Grifth, D. M., White, B., & DuBose, M. (2006). The art and sci-
ence of integrating undoing racism with CBPR: Challenges of pursuing NIH funding to investigate cancer care and racial
equity. Journal of Urban Health, 83(6), 1004–1012.
APPENDIX
5
FUNDING IN CBPR IN
US GOVERNMENT AND
PHILANTHROPY
LAURA C. LEVITON AND LAWRENCE W. GREEN
Although academic-community partnerships can thrive and grow based on mutual commit-
ment to address community priorities and health inequities, actual funding for CBPR and
community-engaged research remains essential. Resources are needed for program implemen-
tation, research costs, and opportunities for community members to be involved in the research
enterprise. Sharing budgets, between universities and community agencies or associations, is in
fact one of the identied promising practices that best exemplify power sharing and collabora-
tive decision making. The history and growth of federal and foundation funding illustrates this
importance.
GOVERNMENT
The US federal government has supported the use of CBPR in grants, contracts, centers, and
systematic reviews for close to three decades. Although it has never been the dominant approach
to research and evaluation, multiple government agencies have recognized the importance
of CBPR for its underlying democratic and social justice underpinnings and for its utility in
engaging communities to obtain better data, analysis, and interpretation of ndings. It remains
to be seen how federal policies in the new administration might include CBPR. The Community-
Campus Partnerships for Health at https://ccph.memberclicks.net/ tracks federal opportunities
for funding in CBPR-related projects.
364 Appendix 5
Mercer and Green (2008) reported on the history of US federal CBPR funding in the sec-
ond edition of this book.
1
As they noted, there was a gradual shift in community participa-
tion from “downstream to upstream involvement of people in the continuum of research to
policy and practice” (p. 400). Initially, people’s engagement in research had a decided utilitarian
point of view. People’s cooperation in implementing programs produced superior results; then
it emerged that community-engaged advocacy and planning had better outcomes, and today
it is abundantly clear that community participation is important to the meaningful translation
of research in local circumstances. By 2016, some agencies have added requirements in their
application guidelines for community participants in research to be identied and others require
letters of commitment from representatives of the community organizations or groups par-
ticipating.
The rst signicant milestone for CBPR involved the Prevention Research Centers (PRCs)
funded by the Centers for Disease Control and Prevention (CDC). When Congress created the
PRCs in 1988, it mandated that each university-based PRC was to engage its communities in
collaborative development and execution of research projects (Mercer & Green,2008). In 1998
an Institute of Medicine (now National Academy of Medicine) committee evaluated the experi-
ence of the thirteen centers funded during that rst decade. “The broad mission of the Preven-
tion Research Centers...can be achieved only through the sustained cooperation of a diverse
array of professionals and nonprofessionals who have roles in inuencing the health of com-
munities, who have competing goals and priorities, and who have little history of engaging in
long-term cooperative efforts” (Green,1997, p. v). Though community participation was found
to be a shortcoming of most centers, the committee recommended additional funding of PRCs
with requirements for community engagement. The PRCs, in turn, became a major source of
subsequent grant applications to CDC for CBPR projects in the following decade.
In 1995, the National Institute of Environmental Health Sciences (NIEHS) became the rst
of the National Institutes of Health to support CBPR by that name when it funded fteen CBPR
projects at about $6.1 million per year (Mercer & Green, 2008). Among the NIH Institutes,
NIEHS had been under the greatest pressure to undertake PR, owing to public concern about the
reliability of environmental research—a skepticism brought on by Love Canal and other pollution
disasters in which residents perceived government scientists as protecting industry or failing to
represent community knowledge, concerns, and perspectives in their environmental research.
From 2002 through 2005, NIEHS sponsored a federal interagency working group (IWG)
on CBPR, with active participation from eleven federal agencies. The purpose of this IWG
was to strengthen communication among federal agencies with an interest in supporting CBPR
methodologies in biomedical research, education, health care delivery, or policy. One of the
IWG’s most important products was a funding announcement titled “Community Participation
in Research,” cosponsored by the NIH, AHRQ (Agency for Healthcare Research and Quality),
and CDC. The goal was to support research on health promotion, disease prevention, and health
disparities that was jointly conducted by communities and researchers. In 2008 this announce-
ment was replaced with two NIH announcements of funding for “community participation in
research targeting the medically underserved,” and a co-funding initiative by NIH and CDC for
“community participation in research” (Mercer & Green,2008).
Since that time, federal funders have increased their investments in CBPR, including mul-
tiple National Institutes of Health, at least ve areas of CDC, the US Department of Agriculture
Appendix 5 365
(USDA, for prevention of obesity), Environmental Protection Agency (EPA), Housing and Urban
Development (HUD), Health Resources and Services Administration (HRSA), and the AHRQ.
Beginning in 2006, applications for the NIH Clinical Science Translational Research
Awards required community-engagement cores, which opened new initiatives within schools
of medicine and academic health centers. Since 2010, the Patient Centered Outcomes Research
Institute (PCORI) has mandated greater stakeholder involvement in research, including patients
and families. Similarly, the Affordable Care Act (ACA) focus on eliminating disparities relies
on community-engaged research to align academic health centers with community priorities
and build bidirectional capacity, especially among hard-to-reach populations. NIH funding of
interdisciplinary team science centers has increased community partner involvement as part
of these teams. A specic Program Announcement (PA-13–209) from the National Institute of
Nursing Research is succeeding to advance the science of measures and metrics of community
engagement.
A collaboration of the Indian Health Service and NIH, the Native American Research for
Centers in Health (NARCH), is now on its tenth call and has spurred the generation of CBPR
and tribal participatory research grants in Indian country to such an extent that multiple insti-
tutes launched an RO1—https://grants.nih.gov/grants/guide/pa-les/PAR-14–260.htm—that
has successfully encouraged Native scholars and others working in Indian country to apply for
RO1 intervention grants, all with a CBPR focus.
The consequences of participatory research for health-related goals now extend beyond those
key agencies when one considers the “Health in All Policies” approach: that health is affected
by a variety of systems and policies that might benet from CBPR. Consider these examples:
■ Problem-oriented policing prevents violent crime, uses data, and is best done with community
participation in problem-solving (National Institute of Justice, www.crimesolutions.
gov/PracticeDetails.aspx?ID=32).
■ The Federal Reserve promotes community development investments in low- to moderate-
income communities. Community development corporations (CDCs) and community
development nancial institutions (CDFIs) nance important changes in the built environ-
ment that are conducive to health, often use data for selection of investments, and are best
done with community participation (www.federalreserve.gov/communitydev/cdf.htm).
PHILANTHROPY
The W.K. Kellogg Foundation led the way in philanthropic contributions to CBPR in the early
1990s, with its Community Health Scholars program (Chapter19). In the present day, founda-
tions of all sizes use CBPR approaches on a regular basis, including some of the largest, such
as the Kresge and Annie Casey Foundations, and smaller ones with a consistent commitment to
CBPR, such as the Liberty Hill Foundation of Los Angeles. Grantmakers in Health (www.gih.
org/) and the Foundation Center (http://foundationcenter.org/) can help the reader nd resources
for CBPR projects.
Some of the strongest proponents of CBPR in the present day are the health-focused
conversion foundations, such as the California Endowment, the Colorado Trust, and the Portland-
based Northwest Health Foundation. This is understandable given that these foundations use
366 Appendix 5
what is arguably public money, derived from converting nonprot insurance companies and
health care institutions to private, for-prot organizations. As such, the founding documents for
their very existence often stipulate community involvement. As part of their mission, therefore,
many conversion foundations feel a distinct requirement to be responsive to underserved and
marginalized communities. CBPR offers a good vehicle for doing so.
For illustration, we will focus on the CBPR investments of the Robert Wood Johnson
Foundation (RWJF). RWJF is not a conversion foundation: similar to other private foundations
it is accountable only to its board of trustees and the Internal Revenue Service. At over $10 bil-
lion in assets, in 2017 it is among the largest private foundations in the country and the largest
domestic foundation devoted to improving health and health care. RWJF sometimes supports
CBPR, although it is usually for a utilitarian motivation, as opposed to viewing CBPR as a
central vehicle for democratic process or social justice in research and evaluation. Nevertheless,
some past investments in CBPR are noteworthy. For example, the Clinical Scholars Program
recently had a training specialization on CBPR. The evaluation of the RWJF Allies Against
Asthma was based in CBPR (Butterfoss et al.,2006). The African American Childhood Obe-
sity Research Network (AACORN; http://aacorn.org/) uses CBPR as part of its founding prin-
ciples. Salud America!, the research network to prevent childhood obesity in Latino children,
formulated its entire research agenda by consulting a nationwide network of Latino community
leaders and researchers about their communities’ priorities, and community partners were
required for each project (Leviton & Lavizzo-Mourey,2013—the results of initial funding can
be seen in a special 2013 supplement of the American Journal of Preventive Medicine).
RWJF is now shifting its focus to “Building a Culture of Health” to improve the upstream
social, economic, and environmental forces creating health (www.rwjf.org/en/culture-of-
health/2015/11/measuring_what_matte.html). This new focus is compatible with the principles
of CBPR. Although CBPR will not likely be the primary approach used in research and evalua-
tion, it has an important new place at the table. For example, RWJF’s new predoctoral program,
Health Policy Research Scholars (www.healthpolicyresearch-scholars.org), will train using
the principles of CBPR. Interdisciplinary Research Leaders (www.interdisciplinaryresearch-
leaders.org) involve cross-disciplinary teams that must include a community partner and will
focus on actions to address these upstream factors affecting health. New “research pillar pro-
grams” (www.rwjf.org/en/how-we-work/grants/grantees/r-e-l-signature-programs.html) fund
efforts to cast light on actionable changes in systems, policies, and the environment that can
better address the drivers of health.
In sum, the Culture of Health and other foundation initiatives have the opportunity to dem-
onstrate the importance of community voice as equal partners within the research enterprise.
Foundations are important stakeholders, along with the public sector, in ensuring resources are
available for partnerships to be effective in their research and actions for a more healthful and
equitable society.
NOTE
1. We gratefully acknowledge the contributions of Shawna Mercer to the information provided in
this appendix.
Appendix 5 367
REFERENCES
Butterfoss, F. B., Gilmore, L. A., Krieger, J. W., Lachance, L. L., Lara, M., Meurer, J. R., Orians, C. E., Peterson, J. W., Rose,
S. W., & Rosenthal, M. P. (2006). From formation to action: How allies against asthma coalitions are getting the job done.
Health Promotion Practice, 7(2), 34S–43S.
Green, L. W. (1997). Preface. In M. A. Stoto, L. W. Green, & L. A. Bailey (Eds.), Linking research and public health prac-
tice: A review of CDC’s program of Centers for Research and demonstration of health promotion and disease prevention.
Washington, DC: National Academy Press.
Leviton, L. C., & Lavizzo-Mourey, R. (2013). A research network to prevent obesity among Latino children. American
Journal of Preventive Medicine, 44(3S3), S173–S174.
Mercer, S. L., & Green, L. W. (2008). Appendix B: Federal funding and support for participatory research in public health and
health care. In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process to
outcomes (2nd ed., pp. 399–406). San Francisco, CA: Jossey-Bass.
APPENDIX
6
REALIST EVALUATION
AND REVIEW FOR
COMMUNITY-BASED
PARTICIPATORY RESEARCH
WHAT WORKS, FOR WHOM, UNDER WHAT
CIRCUMSTANCES, AND HOW?
JUSTIN JAGOSH
Realist methodology (including realist evaluation and realist review) is a relatively new approach
that can help in the study of how CBPR partnerships achieve research and improvement goals.
The complex dynamics of partnership relations play a signicant role in determining outcomes.
Key efforts include building and strengthening trust and overcoming mistrust; establishing equi-
table roles and decision making; determining the research agenda; consenting on who will own
data; converging on research methods, ethics, and analysis; accepting or challenging academic
and institutional demands and restrictions; and resolving concerns over potential stigma from
research evidence.
In a large systematic realist review of the CBPR literature conducted from 2009 to 2013,
I worked with a team of CBPR and realist methodology experts at the University Center for
370 Appendix 6
Participatory Research at McGill (PRAM) to understand what benets, if any, accrue from
participatory research.
1
The use of realist methodology was found to be benecial in concep-
tualizing how CBPR outcomes accrue and in testing causal pathways from collaboration to
outcomes. Resulting publications include a rationale for using a realist review for participatory
research (Macaulay et al.,2011); protocol to identify, select, appraise, and synthesize literature
(Jagosh et al.,2011); results (Jagosh et al.,2012,2015; Macaulay et al.,2014); and reections
for CBPR assessment (Jagosh et al.,2014).
This appendix provides a brief overview of how realist methodology can be applied to
CBPR assessment.
WHAT IS REALIST METHODOLOGY AND WHY IS IT ADVANTAGEOUS?
Realist methodology is a theory-driven inquiry that has the goal of understanding “what works,
for whom, under what circumstances, and how” (Pawson, 2013; Pawson & Tilley, 1997).
Realist evaluation is for primary data collection and analysis, whereas realist review (also
known as realist synthesis) is a secondary, literature-based analysis. Realist methodology uses
the context-mechanism-outcome (CMO) conguration to provide explanatory insight and
theory for the nature of programs and how they work in context.
A realist line of inquiry involves a series of iteratively derived steps:
1. Establishing initial research or evaluation questions that involve inquiry along the lines of
what works, for whom, under what circumstances, and how.
2. Constructing candidate program or middle-range theories that provide a hypothesis or set
of hypotheses that may explain how the program (or aspects of the program) work, given
Definitions
Context: Any element in the environment, background, physical setting, or socio-demography
that, although not formally a part of the program, has a causal impact on outcomes
Mechanism: The host of resources created or offered through a program and the responses to
those resources by program participants
Outcomes: The interaction of contextual elements with the mechanisms; outcomes can be
proximal or final, intended or unintended
Middle-range theory: An implicit or explicit explanatory theory that can be used to explain specific
elements of the program or how program logic manifests in implementation; middle-range means
that it can be tested with the observable data and is not abstract to the point of addressing larger
social or cultural forces (i.e., grand theories); this theory is sought at the outset and examined
iteratively throughout the review (Jagosh et al.,2015)
Appendix 6 371
variations in context. The theories can be formulated by the researchers or adopted from
the preexisting theoretical and empirical literature.
3. Developing data collection protocols. For realist evaluation, this means determining who
to include in the study sample and developing survey instruments and qualitative guides.
For realist synthesis, this involves tools to identify, select, and appraise the literature.
4. Analyzing data using context-mechanism-outcome congurations.
5. Synthesizing and integrating data analysis with program and middle-range theory. The
product of the evaluation or synthesis is an evidence-informed program or middle-range
theories about what works, for whom, under what circumstances, and how.
The advantage of using realist methodology for CBPR is to help unpack the complex causal
pathway from the relationship and activities of academic, community, and other stakeholders
to the intended and unintended outcomes. The success of CBPR relies heavily on relationship
dynamics given numerous inuences from the research setting, geopolitical history of collab-
oration, and preexistence (or not) of social capital, human resources, support infrastructure,
and other assets (Trickett & Ryerson Espino,2004). Members of CBPR projects often expe-
rience shifting perceptions of power and ownership over the duration of a project, especially
in long-term partnerships. Thus, applying empirical measurement to understand the dynamics
of collaboration and testing their causal impacts on outcomes is challenging because, in realist
terms, the underpinning causes of outcomes happen through the relatively intangible and shift-
ing thoughts, feelings, and motivations of CBPR stakeholders over time. Alternatively, realist
methodology is advantageous because it offers program and middle-range theory development
and testing of CMO congurations that produce evidence-informed CBPR theories to guide
future partnership development and work processes. These theories should be subject to ongoing
scrutiny and testing in new contexts and conditions.
For example, a written memorandum of understanding (MOU) is commonly introduced
in early stages to establish roles and responsibilities. Such early agreements may help estab-
lish trust for certain communities at certain times, but alternatively they can foster mistrust
if community members are not ready to engage at that level or if such contracts are pushed
preemptively without providing time and space to discuss what equity in partner roles means.
A realist investigation of the impact of an MOU could start by constructing potential theories
about how an MOU might work in a context that may rival or complement each other. Then
those theories would be used to gather and analyze evidence for a clearer understanding of
when, at what point, for which communities, and in what circumstances that the MOU would
serve to strengthen coalitions or otherwise create mistrust.
Similarly, the process of choosing research topics can affect partnership functioning and
outcomes. If academic researchers approach communities with predetermined funding or topics,
this may affect community buy in and have a ripple effect on outcomes. If the predetermined
topic coincides with community interests, there may be increased community motivation. If
the topic has less community relevance, however, community partners may perceive they are
“doing a favor” for academics, which may affect their investment.
372 Appendix 6
EXEMPLIFYING REALIST METHODOLOGY WITH THE PRAM REVIEW
The PRAM review was conducted with a core team of researchers and decision-making part-
ners. Our research questions were as follows:
1. What benets or constraints emerge from the collaborative undertaking of health-related
research by researchers and those affected by the issues under study or by those who would
apply the research results?
2. How can the collaborative research process be theorized and evaluated?
3. How do variations in the program’s context and mechanisms inuence the process and
outcomes of collaborative health research (Jagosh et al.,2012)?
The rst stages of the review involved identifying, selecting, and appraising key litera-
ture from the CBPR eld using a series of iteratively developed identication, selection, and
appraisal tools (Jagosh et al.,2011). Concurrent with that effort was locating a suitable middle-
range theory that could explain how CBPR creates impacts. After an extensive literature search
and vetting numerous theories (Jagosh et al.,2014), we settled on “partnership synergy,” origi-
nally not developed for CBPR, which is dened as combining perspectives, resources, and skills
of a group of people to “create something new and valuable together—a whole that is greater
than the sum of its individual parts” (Lasker, Weiss, & Miller,2001, p. 184). We found that the
theory was broad enough to account for the heterogeneity of CBPR partnerships but specic
enough to help explain why partnerships form and how they produce outcomes over time.
Our ndings advanced understanding of partnership synergy within CBPR and dem-
onstrated that genuine forms of CBPR that involved equitable co-governance of all stake-
holders tended to (1) generate culturally sound and logistically appropriate research; (2)
increase recruitment and retention of study participants; (3) develop capacity of community
and academic stakeholders; (4) create productive conicts, disagreements, and resolutions; (5)
increase synergy and trust among partners over time; (6) sustain projects during funding gaps;
and (7) produce systemic changes and unanticipated projects and activity (Jagosh et al.,2012).
The theory of partnership synergy provided a conceptual currency that served to explain how
long-term partnerships were able to achieve these impacts through relationship trust that was
established, tested, and maintained over time. We came to rene the theory of partnership
synergy by adding a dimension of time to show that the kinds of outcomes achieved from
long-term maturation of working relationships was much greater than at the outset of collabo-
ration (Jagosh et al.,2015).
An additional feature of our renement of the theory of partnership synergy was incorpo-
rating the concept of the ripple effect inspired from the work of Hawe, Shiell, and Riley (2009).
We linked CMO congurations to each other, with the outcomes of one CMO conguration
becoming the context for a subsequent phase in the partnership in a ripple-effect pattern (Jagosh
et al.,2015). The advantage of using this is that it served to explain how trust and synergy were
built over time and in stages.
Appendix 6 373
CHALLENGES TO USING THE REALIST APPROACH
The main challenge of using realist methodology is that it takes much longer than a traditional
review because of the time required to account for complex context-mechanism-outcome inter-
actions and to locate middle-range theories that can explain the data. The heterogeneity within
the CBPR literature presents a further challenge to constructing relevant middle-range theories
and incorporating different types of partnerships within one review. Another challenge is in
understanding mechanisms. For our review, we dened mechanisms as the resources offered by
partnerships and how they were responded to by all stakeholders, which we determined to be
trust-building and sustainability over time (Jagosh et al.,2015).
Quality appraisal typically means the scrutiny of methods used to produce ndings to
ensure the trustworthiness of the evidence. However, using realist-review methodology, we
took a different approach to appraisal. Rather than critically appraising every method used in
published CBPR literature, we examined the extent to which there was adequate description
of participatory processes and contexts (often in introductions and discussion sections) suit-
able for realist synthesis. We also contacted authors by e-mail to solicit further information
and subsequently interviewed key stakeholders in partnerships retained in the review for
further theory validation. Evidence synthesis often requires a mind-set shift and can take
time to undertake with condence. We suggest conducting a realist project with someone
with prior experience and triangulating data using a realist review and evaluation methods.
CONCLUSION
Choosing to use realist methodology can be a rewarding process with the potential of providing
valuable guidance about how context affects the application of mechanisms corresponding to
CBPR principles and practice, which in turn affect outcomes. With the many dimensions of het-
erogeneity, the assessment can be complex and time-consuming. The specic realist inquiry, how-
ever, of how, for whom, and under what circumstances can serve the CBPR agenda and assist in
unpacking the complexity of partnership dynamics for improving research and health outcomes.
ACKNOWLEDGMENTS
The development of realist methodology for CBPR assessment has come from the sustained
thinking during the PRAM review (2009–2013). I would like to acknowledge the following coin-
vestigators in building capacity in this area: Drs. Paula Bush, Margaret Cargo, Lawrence W. Green,
Trish Greenhalgh, Carol Herbert, Ann Macaulay, Pierre Pluye, Jon Salsberg, and Geoff Wong.
NOTE
1. Funding by Canadian Institutes of Health Research Knowledge Synthesis Grant and further CIHR
postdoctoral fellowship.
374 Appendix 6
REFERENCES
Hawe, P., Shiell, A., & Riley, T. (2009). Theorising interventions as events in systems. American Journal of Community
Psychology, 43(3–4), 267–276.
Jagosh, J., Bush, P. L., Macaulay, A., Salsberg, J., Greenhalgh, T., Wong, G., Cargo, M., Green, L. W., Herbert, C. P., & Pluye,
P. (2015). A realist evaluation of community-based participatory research: Partnership synergy, trust building and related
ripple effects. BMC Public Health, 15(725), 1–11.
Jagosh, J., Macaulay, A. C., Pluye, P., Salsberg, J., Bush, P. L., Henderson, J., Sirett, E., Wong, G., Cargo, M., Herbert, C. P.,
Seifer, S. D., Green, L. W., & Greenhalgh, T. (2012). Uncovering the benets of participatory research: Implications of a
realist review for health research and practice. Milbank Quarterly, 90(2), 311–346.
Jagosh, J., Pluye, P., Macaulay, A. C., Salsberg, J., Henderson, J., Sirett, E., Bush, P. L., Seller, R., Wong, G., Greenhalgh, T.,
Cargo, M., Herbert, C. P., Seifer, S. D., & Green, L. W. (2011). Assessing the outcomes of participatory research: Protocol
for identifying, selecting, appraising, and synthesizing the literature for realist review. Implementation Science, 6(24).
Jagosh, J., Pluye, P., Wong, G., Cargo, M., Salsberg, J., Bush, P. L., Herbert, C. P., Green, L. W., Greenhalgh, T., & Macaulay,
A. C. (2014). Critical reections on realist review: Insights from customizing the methodology to the needs of participa-
tory research assessment. Research Synthesis Methods, 5(2), 131–141.
Lasker, R. D., Weiss, E. S., & Miller, R. (2001). Partnership synergy: A practical framework for studying and strengthening
the collaborative advantage. The Millbank Quarterly, 79(2), 179–205.
Macaulay, A. C., Jagosh, J., Pluye, P., Bush, P. L., & Salsberg, J. (2014). Quantitative methods in participatory research:
Being sensitive to issues of scientic validity, community safety, and the academic-community relationship. Nouvelles
Pratiques Sociales, 25(2), 159–172.
Macaulay, A. C., Jagosh, J., Seller, R., Henderson, J., Cargo, M., Greenhalgh, T., Wong, G., Salsberg, J., Green, L. W.,
Herbert, C. P., & Pluye, P. (2011). Assessing the benets of participatory research: A rationale for a realist review. Global
Health Promotion, 18(2), 45–48.
Pawson, R. (2013). The science of evaluation: A realist manifesto. London, UK: Sage.
Pawson, R., & Tilley, N. (1997). Realistic evaluation. London, UK: Sage.
Trickett, E. J., & Ryerson Espino, S. L. (2004). Collaboration and social inquiry: Multiple meanings of a construct and its role
in creating useful and valid knowledge. American Journal of Community Psychology, 34(1), 1–69.
APPENDIX
7
PARTNERSHIP RIVER OF LIFE
CREATING A HISTORICAL TIME LINE
SHANNON SANCHEZ-YOUNGMAN AND NINA WALLERSTEIN
The River of Life is a reective tool to describe the life journey for partnerships (or coalitions
or organizations). Its purpose is to uncover the histories and inuences that motivate individual
and organizational partners to promote community empowerment, greater social participation
in the research process, and community transformation for health equity. Building on the work
of Paulo Freire, the exercise is premised on the process of dialogue and reection wherein
participants reect and document the critical and signicant moments of their partnership and
empowerment work.
This exercise offers the opportunity for people committed to community organizing and
change to construct a communal narrative about their origins, their histories of struggle, their
successes, and their challenges. Through a process of co-creation, participants create conscious
meanings of the ebbs and ows of their research and social justice work. As a critical reection,
it offers the opportunity for participants to give voice to the collective narratives that sustain
their partnership. Through guided questions and by using the metaphor of a river, the exercise
is designed to trigger community and academic partners to actively acknowledge, celebrate, cri-
tique, change, and sustain the processes, goals, and results of their health equity work.
Beyond reecting on internal partnership dynamics, community and academic partners
may also use the exercise to delve into the cultural, institutional, political, economic, and gov-
ernmental context that enables or inhibits them to create effective collective action strategies.
© 2016, Engage for Equity, Nina Wallerstein, Center for Participatory Research, University of New Mexico.
376 Appendix 7
© 2016, Engage for Equity, Nina Wallerstein, Center for Participatory Research, University of New Mexico.
From this external vantage point, the River of Life is a historical and contextual exercise in
which participants are free to consider how past historical events, histories of community orga-
nizing, broader political-economic structures that inuence social conditions, and the receipt of
grant funding or the arrival or departure of partnership members create opportunities and chal-
lenges to advance multiple social justice agendas. For example, in the Research for Improved
Health study (described in Chapters6 and17), one case study site used the narrative of the
River of Life to identify how the legacy of the civil rights movement informed their current
strategies to challenge governmental and health institutions for a more equitable distribution of
resources to communities of color in an urban area.
By reecting on the connections between external conditions and their impact on their part-
nerships or organizations, the River of Life also helps partnerships recognize and clarify mul-
tiple goals, successes, and opportunities for change. In sum, we have found that this exercise
is a powerful tool for partnerships to learn from each other and to assess where the partnership
came from, what progress has been made, and what directions people might begin to talk about
for their future. As a caution, if partners nd themselves in intense dialogue around longstand-
ing conditions of powerlessness, discrimination, or historical trauma, then it may be important
to follow up the exercise with personal support for individuals, as well as ongoing community
building. The exercise itself, however, which brings people together to name and portray their
partnership’s strengths, has facilitated people as a team to identify their successes and therefore
to nd ways to support their own healing.
Though the exercise is presented here as a collective exercise, the University of New
Mexico Center for Participatory Research has also used this tool successfully as an individual
exercise for students, community members working together, or community groups to learn
about each other’s histories and values. If done as an individual exercise, the facilitator needs to
remind people to take care of themselves and draw and present only issues or times in their lives
that they will feel comfortable sharing.
PARTNERSHIP RIVER OF LIFE HISTORICAL TIME LINE EXERCISE
Objectives
To facilitate partnership (or organizational) reection regarding the following:
1. The history and inuences that motivate partners (as individuals or from organizations) to
work together in their partnership or participatory research projects, coalitions, or organi-
zations to promote community empowerment, social participation, and health equity
2. The goals, processes, and results of your partnership work
Time
Few minutes for individual team member reection (step 1)
45 minutes for teamwork (steps 2 through 4)
15 minutes to reect and report back (steps 5 and 6)
Appendix 7 377
© 2016, Engage for Equity, Nina Wallerstein, Center for Participatory Research, University of New Mexico.
Materials
■ Sheets of paper
■ Plenty of colored markers
■ Scissors, magazines, construction paper, and glue
■ Flipchart or butcher paper
Procedure
Explain that a river is an important symbol in many cultures; it symbolizes life and change for
many people, and it is stimulating to think about the river, nature, and what it represents. Every
river has headwaters or springs (beginnings of the partnership or organization) and times or places
where the river is owing well (partners are working well together). Sometimes partnerships
have a calm period where the river smooths out into a wide pool. Other times the partnership
has obstacles or challenges, which can be represented by boulders, rapids, and waterfalls. There
are times when bodies of water join through tributaries (new resources, mentors, or new mem-
bers) or a stream branches off from the main river (members leave or new separate partnerships
are formed).
Step 1. Each member of the partnership reects independently about him- or herself and
the partnership in terms of a river and answers these questions: How and why did you join?
What is important to know about your community and how and why you started working
together? What important events and changes have you seen?
Step 2. Lay out a long sheet of paper (or two ipcharts taped together) and other art supplies
(markers, crayons, construction paper, glue) so that together you can draw your partnership
river of life. Construction paper can also be used to cut out images (e.g., hearts to show
positive moments or good river ow and boulders or rocks to show obstacles).
Step 3. Draw the river of life for your partnership. Discuss the beginnings, the inuences,
the obstacles, and the peaceful moments, because these are key aspects for the work and
the commitment to change in the communities and across partnerships and coalitions.
Start where you think it’s important to start, which could be before the partnership began
or historical moments that led to the formation of the partnership.
If it helps, write these instructions on a ipchart:
Start where you think it is important to start, such as a historical moment before the partnership
began, when you received funding, and so on.
Draw important or influential stages.
Draw key tributaries coming in, or tributaries leaving.
What were factors that facilitated the work?
What were obstacles that were challenging?
Where are you headed?
378 Appendix 7
© 2016, Engage for Equity, Nina Wallerstein, Center for Participatory Research, University of New Mexico.
Step 4. Make a historical time line with dates of months, years (or decades) below the
river of life. Relate important historic events within the community, region, state, or nation-
ally that might inuence what is currently happening in your partnership (or coalition or
organization), and consider whether this has had an impact on your partnership’s life.
Step 5. Stand back and admire your River of Life and answer the following questions:
1. What stood out for you while doing this collective process? (Any general thoughts
about what you learned or feelings this exercise raised?)
2. What were/are some of the facilitators you identified that were important for your
partnership?
3. What were/are some of the challenges or obstacles you have faced in terms of moving
forward in a good way with your partners?
4. Were there important external events that made a difference?
5. When do you think you could use the River of Life tool in your own work?
Step 6. If there are multiple teams or partnerships (or individuals) creating rivers at the
same time, you will need enough time for the sharing of journeys and discussion of simi-
larities and differences within different contexts and experiences. If time is limited, share
specic rivers in groups of two to four (for ten minutes), and use the questions in step 5 for
a larger group discussion of similarities and differences.
See facilitation guide and examples of Rivers of Life at: http://cpr.unm.edu/research-projects/cbpr-project/facilitation_tools
.html

APPENDIX
8
PURPOSING A
COMMUNITY-GROUNDED
RESEARCH ETHICS
TRAINING INITIATIVE
CYNTHIA PEARSON AND VICTORIA SÁNCHEZ
Historical unethical research practices have often generated community mistrust for research
(discussed further in Chapters14–16). To compound this history, academic research and institu-
tional or ethical review boards (IRBs and ERBs) often lack familiarity with diverse community’s
specic risks and benets, hampering the review of culturally ethical research protocols. As a
result, practitioners of community-based participatory research (CBPR) and community-engaged
research (CEnR) have raised questions about how well standard research ethics training ts with
the principles and practices of CBPR and CEnR (Anderson et al.,2012). Specically, the absence
of culturally relevant human subject research education for community partners has been noted
as an ongoing barrier to CBPR and CEnR. Currently, online ethics training for federally funded
research has not been written for community research partners (Anderson et al.,2012), nor does
it address research ethics issues unique to diverse cultural and environmental contexts.
The Collaborative IRB Training Initiative (CITI,2000), the developer of online modules
used most frequently to meet the NIH requirement for research ethics training, offers a potential
380 Appendix 8
gateway into ethical and respectful CBPR or CEnR partnerships. However, many community
members and academics have identied CITI’s critical gaps in ethical training pertinent to
many stigmatized communities (e.g., men who sleep with men [MSM]) (Anderson et al.,2012;
Pearson, Parker, Fisher, & Moreno,2014) and ethnically and racially diverse (E-RD) commu-
nities. These gaps have included (1) ethics topics and examples relevant to stigmatized and
E-RD populations; (2) clear, simple language; and (3) community-level oversight, risk, and
benet concerns (Cochran et al.,2008; Pearson et al.,2014).
IRBs have the authority to determine what constitutes sufcient training for those engaged
in research (US Department of Health and Human Services,2009) and thus can facilitate
community-grounded, culturally centered human research ethics training that moves beyond
meeting only institutional research requirements.
There has been increasing interest in the importance of culturally based ethical research.
Nationally, several research conferences and academic institutes have hosted workshops on the
conduct of ethical research in Indian country, and several IRB directors are seeking expertise
and understanding in diverse community viewpoints for their boards. Internationally as well,
leading organizations from Kenya (e.g., Kenya CDC, national ethical review boards, and the
research policy council) are reaching out to develop a training that will highlight specic con-
cerns when conducting HIV/AIDS research with MSM population in areas where human rights
are constrained (i.e., when political and cultural norms outlaw same-sex relationships). All of
which highlight a growing community and funder interest in obtaining relevant and community-
specic ethical training materials.
This appendix presents the issues to consider in what would constitute an alternative ethics
training, provides a short case study of the development of a new CITI module for Indigenous
populations, and identies resources of other academic and community institutions that use
alternative research ethics training for community research partners.
In developing an alternative research ethics training for community partners, the key is to
start with listening and learning from community partners to determine specic processes and
content for translating research ethics content that reects community history, experience, and
culture. Essential to implementation of a culturally grounded ethic’s training program is obtaining
organizational commitment and leadership support in order to facilitate acceptability, credibility,
and sustainability. As others have pointed out: “changing institutional culture starts with the lead-
ership and commitment of top decision-makers” (Michener et al.,2012, p. 2). Researchers who
have successfully implemented alternative research ethics training have worked in collaboration
with their IRB leadership to implement their training. From a review of several of these modules
as well as from the following case study, here we provide a summary of key considerations:
■ Content. Although topics for any human subject research training will include the core
ethical principles of respect for persons, beneficence, and justice, how these principles are
applied will vary based on a culture’s values and belief systems and likely change over time.
■ Risk and benefits. The concept of individual risk and benefit may include community risk
and benefit; understanding the balance between the two should be clearly articulated.
Community-identified risk and benefits may vary greatly across communities.
■ Validity and acceptance. To ensure validity as well as community and institutional
acceptance, the training should be constructed with representatives from all three entities,
Appendix 8
381
for example, community members or leaders, researchers, and the academic IRB. CEnR
and CBPR researchers would help facilitate change within the university system and work
with community research partners to determine specific processes and content for trans-
lating research ethics content that reflects community history, experience, and culture
(Michener et al.,2012).
■ Training delivery. Online training has been the norm; however, in-person training or a
hybrid may enhance efficacy and feasibility for populations less connected to the Internet.
■ Literacy. Originally trainings were developed specifically for members of the scientific
community, written at a college level, and contained examples from laboratory settings
with little or no direct relevance to CBPR or CEnR. The few training approaches developed
specifically for community training in human subjects protections and research were often
narrow in scope, focusing on responsibilities of project field staff members, techniques
for primary data collection, and policy advocacy and missed the opportunity to develop
research literacy in understanding human subjects protection. As the case study illustrates,
complex regulations can be presented in lay terms, thus expanding reach for the under-
standing of the conduct of human subjects research for community members (Carroll-Scott
et al.,2012; Goodman, Dias, & Stafford,2010).
■ Assessing training outcomes. Assessment may include group discussion or posttests. In
some cases, the academic partner who conducts the training attests that the community
partners completed the training, understood the material, and are able to apply the concepts
to their research project.
CASE STUDY: ETHICAL TRAINING FOR HEALTH WITH
INDIGENOUS COMMUNITIES
Pearson et al. (2014) used a CEnR process to adapt the CITI-certied human subjects training
module on assessing risk and benets from a Pacic Northwest AI/AN perspective. They pre-
pared materials for panel review including mapping the modules’ core components to the code
of federal regulations. Three expert panels, one each of AI/AN community members, scientists,
and ethicists (n=11), identied consent, risk and benet, and condentiality as primary areas
needing adaptation to meet cultural perspectives and concerns.
The community panel decided to adapt the assessing risk and benets module because it
covered the area in which research has created the most harm and mistrust. A total of sixty-
two changes in four categories: (1) “cultural relevance” included reference to AI/AN culture
and laws (n=12); (2) “claried concepts” included removing jargon, simplifying language, or
expanding explanations (n= 22); (3) “human subjects relevance” addressed breaches of ethics
that occur often, such as misuse of data or are more reective of events in AI/AN communities
versus a technologically advanced setting (n=11); and (4) “community protection,” providing
community-level risk and benets to address a critical gap in ethical training pertinent to AI/AN
communities (n=17).
After adapting the module in a two-arm randomized clinical trial, followed by debrieng
interviews, they evaluated module acceptability and feasibility (i.e., relevance of materials, self-
efcacy in applying concepts, and satisfaction) and understandability of module (test scores)
382 Appendix 8
among forty AI/AN reservation-based community members. Participants who took the adapted
module as compared to those who took the standard module reported higher scores on relevance
of the material (82.7 versus 65.8, t=3.06, p<0.01), overall satisfaction (81.4 versus 69.4, t=2.10,
p<0.05), module mean quiz scores (75.7 versus 62.9, t=2.15, p<0.05), and a trend toward higher
research self-efcacy (76.3 versus 68.1, t=1.71, p<0.10). CITI requires the quiz to be taken until
a passing score is reached (˜80 percent). Pearson et al. (2014) calculated quiz scores based on rst
try and found that 65 percent of respondents in the adapted module group passed as compared to
35 percent in the control group (X
2
=3.6, p=.058). In debrieng interviews (n=30), respondents
reported that examples in the adapted module highlight potential risks for research that resonated
with their lived experience, were interested in sharing the culturally adapted module with their
tribe, and stressed the utility of the material in health care and social service settings outside of
the research arena. One person said,“I’m ready to jump into research...I’m really glad I did
this.” One respondent also suggested the training would be good for academic researchers, “for
non-Indians coming into a reservation, I thought it would be good for them to do this training.
People coming out don’t know about the sensitivity of elders and the damage they could be
doing. Researchers are wanting to do something good, but could cause harm unintentionally.”
Literacy, however, remained a concern. Although the adapted module was at a high school
level, respondents expressed difculty with the vocabulary, long sentences, and the time needed
to understand the materials. This preliminary study demonstrates the acceptability of an adapted
training, the feasibility of identifying core ethical concerns across diverse rural and urban
tribal entities, the need to simplify language, and the utility of including community voice in
adapting the CITI training materials and increasing potential for research partnerships with
community members.
Following the pilot, community members spoke of the value a full certication curric-
ulum would provide. Thus the investigators obtained funding from NIH for the Ethical Training
for Health with Indigenous Communities (ETHICS). ETHICS expands the pilot to a national
randomized control trial among ve hundred American Indian and Alaska Natives. The national
study will evaluate whether a culturally developed human subjects training curriculum (as com-
pared to the CITI standard social behavioral curriculum) increases research ethics knowledge,
research review efcacy, and trust in research and researchers. Findings from this study will be
released in summer 2017, and the curriculum is scheduled for immediate dissemination through
CITI as a full certication curriculum in their basic package at no additional charge to their
more than six thousand subscribers. Moreover, the Department of Health and Human Services
Administration for Children & Family Ofce of Planning, Research & Evaluation (OPRE) will
soon provide open access to their national data on AI/AN children, their families, teachers,
and providers. OPRE is proposing, prior to accessing the data, researchers take the ETHICS
training. OPRE believes it will help sensitize researchers to the unique consideration when
working with AI/AN communities.
This case study represents one alternative training mechanism that teaches concepts from
the Belmont Report and the CFR 45SS on the conduct of ethical research with human sub-
jects from a community’s values. It offers an example of how to address ethical challenges
in conducting research with stigmatized and E-RD populations who face health disparities by
Appendix 8
383
increasing informed IRB panels and academic partners and community involvement in research
oversight, design, implementation, and dissemination.
Other academic institutions and community-based organizations have developed, tested,
and implemented alternative research ethics training for community research members and
partners including the University of Pittsburgh (Yonas et al.,2016); University of Colorado
(Westfall et al.,2016); the University of North Carolina at Chapel Hill (http://research.unc.
edu/ofces/human-research-ethics/getting-started/training/ccm3_019063/); Harvard University
(https://catalyst.harvard.edu/programs/regulatory/cenr.html); and the University of Michigan
(Solomon & Piechowski,2011). These curricula blend training in core ethical principles with
community experiences with research through stories and case studies.
The signicance of these initiatives lies in the potential to enhance IRB reviews, academic
scholars’ sensitivity in working with stigmatized and E-RD communities, and community par-
ticipation in research through local or online community-driven research ethics training that
highlights the cultural, policy, and environmental context of diverse communities.
These kinds of initiatives with community and academic partners will have a high impact
by contributing to the development of CEnR capacity within national and international com-
munities, facilitating more inclusive and ethical research aimed at reducing health disparities.
From a CBPR or CEnR perspective, research ethics training with community research part-
ners builds on a commitment to trust and respect, bidirectional learning, capacity building, and
developing shared language and meaning. The extension of the research partnership into ethics
training is a central ingredient to democratize knowledge and promote social justice within the
research enterprise.
Examples of Online Resources
■ Campus Community Partnerships for Health (CCPH). Reengaging Ethics: Ethical Issues in
Engaged Research. https://ccph.memberclicks.net/research-ethics
■ Training and Resources in Research Ethics Evaluation (TRREE) and regulation of health
research involving human participant. TRREE focused primarily, but not exclusively, on
the needs of African countries. http://elearning.trree.org/
■ Family Health International (FHI). Designed and developed for an international audience
of researchers and research ethics committee members. www.fhi360.org/sites/default/les/
media/documents/Research%20Ethics%20Training%20Curricula.pdf
■ Harvard Catalyst/Harvard CTSC. Provides resources for investigators, community partners,
and IRB. https://catalyst.harvard.edu/programs/regulatory/cenr.html
■ University of Michigan—Research Ethics Training for Community Research Partners.
http://inventions.umich.edu/technologies/4768_research-ethics-training-for-community-
research-partners
■ University of Pittsburgh/CTCC—Introduction to Community Partnered Research Ethics
Training (CPRET). www.ctsi.pitt.edu/cpret.shtml
■ UNC Chapel Hill—Alternative Training for Special Circumstances. http://research.unc.
edu/ofces/human-research-ethics/getting-started/training/ccm3_019063/
384 Appendix 8
REFERENCES
Anderson, E. E., Solomon, S., Heitman, E., DuBois, J. M., Fisher, C. B., Kost, R. G.,...Ross, L. F. (2012). Research ethics
education for community-engaged research: A review and research agenda. Journal of Empirical Research on Human
Research Ethics, 7(2), 3–19. doi:10.1525/jer.2012.7.2.3
Carroll-Scott, A., Toy, P., Wyn, R., Zane, J. I., & Wallace, S. P. (2012). Results from the Data & Democracy initiative to enhance
community-based organization data and research capacity. American Journal of Public Health, 102(7), 1384–1391.
CITI. (2000). Collaborative institutional training initiative: Social and behavioral sciences human subjects training. Miami,
Florida. Retrieved from www.citiprogram.org/aboutus.asp?language=english
Cochran, P. A., Marshall, C. A., Garcia-Downing, C., Kendall, E., Cook, D., McCubbin, L., & Gover, R. M. (2008). Indig-
enous ways of knowing: Implications for participatory research and community. American Journal of Public Health,
98(1), 22–27.
Goodman, M. S., Dias, J. J., & Stafford, J. D. (2010). Increasing research literacy in minority communities: CARES fellows
training program. Journal of Empirical Research on Human Research Ethics, 5(4), 33–41. doi:10.1525/jer.2010.5.4.33
Michener, M., Cook, J., Ahmed, S. M., Yonas, M. A., Coyne-Beasley, T., & Aguilar-Gaxiola, S. (2012). Aligning the goals
of community-engaged research: Why and how academic health centers can successfully engage with communities to
improve health. Academic Medicine, 87(3), 285–291.
Pearson, C. R., Parker, M., Fisher, C. B., & Moreno, C. (2014). Capacity building from the inside out: Development and
evaluation of a CITI ethics certication training module for American Indian and Alaska Native community. Journal of
Empirical Research on Human Research Ethics (JERHRE), 9(1), 46–57. doi:10.1525/jer.2014.9.1.46
Solomon, S., & Piechowski, P. J. (2011). Developing community partner training: Regulations and relationships. Journal of
Empirical Research on Human Research Ethics (JERHRE), 6(2), 23–30. doi:https://doi.org/10.1525/jer.2011.6.2.23
US Department of Health and Human Services. (2009). Code of federal regulations, Title 45 Public Welfare, Part 46, Protec-
tion of Human Services, Subpart A Basic HHS Policy for Protection of Human Research Subjects. Rockville, MD: Author.
Westfall, J. M., Zittleman, L., Felzien, M., Ringel, M., Lakin, A., & Nease, D. (2016). Institutional review board training
when patients and community members are engaged as researchers. Family Practice, 10, 1–4. doi:https://doi.org/10.1093/
fampra/cmw112
Yonas, M. A., Jaime, M. C., Barone, J., Valenti, S., Documét, P., Ryan, C. M., & Miller, E. (2016). Community partnered
research ethics training in practice: A collaborative approach to certication. Journal of Empirical Research on Human
Research Ethics (JERHRE), 11(2), 97–105. doi:10.1177/1556264616650802
APPENDIX
9
PARTNERSHIP AGREEMENTS
A PRACTICAL GUIDE TO DEVELOPING DATA
SHARING, OWNERSHIP, AND PUBLISHING
AGREEMENTS
PATRICIA RODRÍGUEZ ESPINOSA AND AL RICHMOND
Advances in CBPR and community-engaged research are accompanied by a commitment to
create processes and procedures that fully engage all partners, including community leaders
and community-based organizations (CBOs) in the work, from concept design to dissemina-
tion. This appendix explores myriad opportunities to formalize partnership relationships and
provides guidance that can facilitate meaningful and authentic engagement on the part of all
partners. The information provided is not prescriptive but serves to capture the core values asso-
ciated with partnership agreements and documents.
Although not all partnerships have formal agreements, and some partnerships may decide
that shared guiding values are sufcient, at some point partnerships may want to consider signed
agreements on specic issues such as data sharing and ownership. In the national Research
for Improved Health study, use of formal agreements emerged as a promising practice in its
association with greater resource sharing as well as power sharing in research (see Chapter17).
Whether or not partnerships choose to create a formal agreement, members of academic-
community research partnerships have the opportunity and responsibility to work together col-
laboratively to protect, store, and share their data and disseminate ndings in a way that is
consistent with their partnership values and with the needs of their partners. The principles from
386 Appendix 9
Community Campus Partnerships for Health might be useful starting points for partnerships to
articulate their own values (https://ccph.memberclicks.net/principles-of-partnership).
This appendix provides suggested topics for agreements, that is, mission, partner respon-
sibilities, data, addition of new investigators or students, and dissemination and coauthorship.
As partnerships evolve, agreements can serve as a foundation for guiding decisions and can
be revisited periodically. This appendix is not meant to be fully comprehensive of all possible
sections; however, we hope to offer examples of major sections to consider and resources that
can prompt partnership dialogue and decisions. Included are URLs intended to serve as more
concrete examples.
PURPOSE
A purpose statement offers a partnership the opportunity to document the participants’ com-
mitment to working equitably and providing an introduction to sections that follow. It may
dene terms, such as data, meaning primary source information gathered in a project, or
that “sharing or disseminating data” may take any forms, such as community or professional
presentations, media communications, reports, grants, manuscripts, and information
on websites.
AGREEMENT INTRODUCTION
This section underscores topics typically found in introductions of formal agreements along
with some sample language.
Mission and Vision
Agreements oftentimes emphasize core missions of promoting health equity, social justice, and
contributing to the knowledge and science of CBPR. Partnerships can benet from dialogues
and formal discussions regarding goals and values of the project.
Project Values and Principles
Agreements are often an expression of the principles of CBPR in the research. The data sharing,
data storage, publication, and dissemination of the research results might follow generally
accepted principles, which include but are not limited to the following:
■ Anonymity of individuals and partnerships. The research results will be presented in an
aggregated or grouped manner. Partnerships and communities have the right to decide if
they want to be identied or not in the research results. Community and academic partners
must agree to be identied.
■ Privacy and condentiality. All information collected from individual participants and part-
nerships will remain private and condential.
■ Respect. The cultural and intellectual integrity of any participating partnerships or proj-
ects must be respected in all publications and disseminations. Further discussion on what
respect might mean for different partnerships is encouraged at the beginning of the concep-
tualization of agreements.
Appendix 9
387
Respective Responsibilities
Many agreements include primary responsibilities for each partner or stakeholder group
involved in the collaboration. Listing these responsibilities, in design, implementation of
research or intervention, and data collection and analysis, can help organize efforts and reduce
the risk of misunderstandings about deliverables or expectations. A key consideration is offering
ample collaborative and equitable involvement of all partners in different phases of the project.
Although some partners might be primarily responsible for certain areas (e.g., academic part-
ners responsible for data analysis based on in-house expertise), it is important to encourage
community partners to get involved throughout the research. Agreements can serve to formalize
these efforts. Involving community partners in data interpretation and dissemination is key to
translation and use of ndings.
DATA-RELATED CHALLENGES
Ethical and other responsibilities involved in data collection and management make this a core
section(s) in many agreements. For instance, who owns the data and what are the repercussions
of that choice? If community partners own the data, can academic partners use it for publishing
to support their promotion and tenure? Will data be aggregated or de-indentied, and who will
have access to the raw de-identied data? How will data be shared with the community or the
public? What are federal responsibilities?
Involvement in Data Collection
For formal research projects, data collection procedures must comply with institutional review
boards (IRBs) (e.g., at the university, the community, or tribe). In addition to specifying who is
involved in data collection efforts, it is useful to establish procedures for adding new team mem-
bers, who need to comply with IRB guidelines.
Data Ownership and Data Sharing
Data ownership, sharing, and use agreements are especially important for partnerships with
multiple teams (e.g., community, academic, tribes) in order to avoid potential conicts. This
becomes extremely important for small communities and for those who might face stigma or
other negative consequences as a result of research participation or particular ndings.
Case example: The Research for Improved Health study, in one of our tribal case studies, found
that our agreement was insufcient for interview data. The university had assumed sharing of aggre-
gated data, but after data collection, the tribe assumed the raw data would be stored with the tribe.
The consent form, however, did not include sharing of individual raw data beyond the person inter-
viewed. After multiple discussions, the team decided to re-consent the participants, with detailed
data-sharing modications, to allow sharing and storage of data with the tribe. Although this team
was able to reach an agreement, ethical concerns such as this one are not uncommon.
Data Storage
For projects collecting identiable data, agreements should detail guidelines for protecting par-
ticipants’ condentially. For instance, will personally identiable data be stored? What steps are
388 Appendix 9
taken to prevent loss of condentiality (e.g., password protection or encryption)? Often, only
few team members have access to identiable data. Detailing their responsibilities, including
sharing de-identied data, and communicating these processes to the larger team, would be in
this section.
Procedures for Project Modifications
Given the uid nature of CBPR projects, it is not uncommon for modications to happen as
the project develops. Partnerships can use agreements to establish processes for future modi-
cations, such as new data collection efforts or new proposals based on ndings. Establishing
guidelines for modications might include the creation of a subcommittee or appointing an
individual who can oversee and approve the modications, clarifying what needs to be sub-
mitted, and communicating clearly to the partnership these processes.
PUBLICATION, WRITING, AND GENERAL DISSEMINATION
Dissemination can be dened broadly, for example, as peer review venues as well as classroom
or community presentations, media releases, monographs, policy briefs, white papers, and so
on. Dissemination efforts can last many years and continue long after a research study has con-
cluded data collection. Given the diversity of dissemination products, the long time frame, and
different backgrounds of partners, this can be particularly difcult to navigate. Considerations
should be made for (1) equitable or collaborative involvement of all partners and (2) honoring
partnership and project values and goals when considering dissemination products. For a com-
prehensive example of dissemination, see Engage for Equity in “Examples of Agreements” at
the end of this appendix.
General Dissemination
It can be useful to think about project goals and responsibilities (and to whom) when drafting
this section. For instance, dissemination responsibilities may include funding agencies (e.g.,
NIH), communities involved in the research, and other stakeholders. After considering differ-
ent responsibilities, it can be useful to clarify individual party responsibilities for developing
needed products. Principal investigators are often responsible for facilitating these efforts, with
many agreements including formal sections on the role of principal investigator.
Publications, Review Processes, and Opportunity for Collaborative Dissemination
This section can be used as starting points for discussion on publication and writing. We have
found it helpful and transparent to create subcommittees, such as a publications committee.
Although there are other options, we do encourage partnerships to establish a formal process for
reviewing publications and for ensuring opportunities for all partners to participate and receive
credit for their contributions.
Publications and Writing Teams The approval process needs to be consistent with relevant
IRB, tribal government, NIH, or university policies and usual and customary academic stan-
dards pertaining to scholarly publications. Partnerships can discuss potential topics rst. Or,
Appendix 9
389
the PI or publications committee could be designated to be approached by team members inter-
ested in potential topics and then can broker avoiding similar or overlapping papers, submitting
papers to the same journal, or publishing articles in an illogical sequence.
The agreement can specify what should be submitted to the PI or publications committee
(or both), that is, an abstract, desired journal (or other form of publication), lead authors and
coauthors, list of information or data requested, and time line for completion. The approving
body will return comments and a decision within a specied period of time. If the committee
does not return a decision within the time frame, specify the responsibility of the lead author
to follow up with the PI. It is helpful to establish a process by which all team members are
informed of current opportunities to get involved in different dissemination efforts. For in-
stance, a newsletter or a document with ongoing writing efforts can be circulated at regular time
intervals to invite partners to join the writing teams.
Criteria for Authorship Consensus among the lead author and coauthors pertaining to roles and
responsibilities should be obtained at the earliest planning stages of the manuscript. Agreements
can detail the criteria required to qualify for authorship. For instance:
■ Individuals who contribute substantially to the manuscript’s concept, design, data analysis,
or implications
■ Individuals who provide essential expertise (e.g., academic, Indigenous knowledge, histor-
ical, cultural relevancy)
■ Individuals who review or make substantive comments or edits on at least one draft
Authorship conditions can be included, such as modications of author order based on
actual work, approvals by all authors within a set time frame, and so on. Lead author responsi-
bilities can be delineated with nal draft to the PI(s) for review.
Student Authorship For students using project data to satisfy graduation requirements such
as thesis or dissertations, further guidelines can be developed that take into consideration data
sharing and dissemination of their work.
Planning and Development of a Manuscript When considering the selection, journals that
pose the least difculty for community access should be explored rst. If a decision is made to
publish in a journal with signicant barriers to community access, the authors should identify
ways to make the information accessible to community members.
Publication Guidelines Acknowledgment All those who contributed to the research project,
but do not meet the authorship criteria, may be included in the acknowledgment section of the
manuscript. Partnerships can write out an acknowledgment paragraph that might include advi-
sory council members, core staff members, and so on, as well as funding sources.
RESOLVING GRIEVANCES
A process for acknowledging and resolving grievances is oftentimes included. Partnerships
should consider nominating a person or group for arbitration. A process, with time lines, should
390 Appendix 9
take into account the ability of parties to engage in meaningful communication to resolve the
dispute, followed by other steps, including potential termination of the agreement.
TERMINATION
Conditions for termination of the partnership can be included, such as approval by all parties,
and stipulations regarding ongoing data sharing, ownership, and dissemination.
AGREEMENT PERIOD
It is useful to include dates under which the agreement will be in effect and can include review
of the agreement once the initial approval period expires.
OTHER SECTIONS TO CONSIDER
An appendix listing those parties referred to in the agreement, subcommittee membership, and
advisory boards may be helpful.
EXAMPLE AGREEMENTS
For comprehensive example, see Engage for Equity (E2):
http://cpr.unm.edu/common/new-engage-for-equity-data-publish-agreements-2017-.pdf
For comprehensive tribal examples, see the Indigenous Wellness Research Institute (IWRI):
http://health.iwri.org/tribal-colleges-universities-drug-and-alcohol-problems-and-
solutions-study/
Community-Campus Partnerships for Health (Appendix E in the CBPR Curriculum) has an
extensive list of agreements:
https://ccph.memberclicks.net/index.php?option=com_content&view=article&id=169:cbpr-
curriculum-appendix-e&catid=31:cbpr-curriculum
Project Values and Principles
https://depts.washington.edu/ccph/pdf_les/MOU10.pdf
See Research for Improved Health: Project Code of Ethics and Integrity: http://cpr.unm.edu/
research-projects/cbpr-project/RIH.html
Respective Responsibilities
http://catalyst.harvard.edu/pdf/chirp/Appendix%20F%20-%20Memorandum%20of%
20Agreement.pdf
Data Related
www.ucdenver.edu/research/CCTSI/community-engagement/resources/Documents/
DataSharingCreatingAgreements.pdf
health.iwri.org/wp-content/uploads/2016/02/Sample-Data-Sharing-Agmt.docx
Appendix 9
391
www.reading.ac.uk/ssc/resource-packs/akf-surveypack/Session13-DataOwnership/
FilesForCourseFolders/Template-DataOwnershipAgreement.pdf
Publication, Writing, and Dissemination
www.maine.edu/pdf/PublishingAgreementStandard.pdf
http://blogs.harvard.edu/infolaw/les/2009/05/authors_publishing_intro-tka1.pdf
www.copylaw.com/new_articles/collab.html
www.detroiturc.org/images/PDFs/URCDisseminationGuidelines.pdf
Student Involvement
http://health.iwri.org/wp-content/uploads/2016/01/NCAI-UNM-UW-NARCH-V-Research-for-
Improved-Health-Protocol-for-Student-Involvement-in-the-Research-Team.pdf
Grievances
www.calpelra.org/pdf/von%20Kalinowski,%20Judy.pdf
http://ucnet.universityofcalifornia.edu/labor/bargaining-units/k8/docs/k8_2015–2016_23_
grievance-procedure.pdf
Termination
https://seeingcollaborations.les.wordpress.com/2014/10/template-of-memorandum-of-
understanding-for-mutual-aid-research-in-disasters-5–1–12.docx
APPENDIX
10
INSTRUMENTS AND
MEASURES FOR EVALUATING
COMMUNITY ENGAGEMENT
AND PARTNERSHIPS
NINA WALLERSTEIN
As noted throughout this book, over the last decades, evaluation evidence has grown, showing
that CBPR and community-engaged research (CEnR) partnerships have contributed to health and
health equity improvements. Intervention studies, experimental and quasi-experimental design
trials, case studies, CBPR policy analyses, as well as systematic reviews and meta-analyses
have showcased engagement and collaborative practices that have contributed to a range of out-
comes. These outcomes have included short-term increased partner synergy and culture-centered
interventions; intermediate outcomes, such as increased community capacities, sustainability
of projects and partnerships, health behavior changes, and shared power in research between
community, agency, and academic stakeholders; as well as more long-term policy changes, trans-
formed conditions, and health status outcomes.
Although partnerships have often focused on evaluating outcomes of their research project
aims, increasingly they are adopting qualitative and quantitative evaluation methods to assess
their partnership or engagement practices. This appendix identies measurement tools and
instruments that have been published or available on public websites that may prove useful
to partnerships to strengthen capacity and practices in evaluation and collective reection.
Because of the vast diversity of individual evaluation tools for specic projects, it is not meant
to be comprehensive but identies various resources in the eld.
394 Appendix 10
A few early reviews of literature on collaboration deserve special mention. Granner and
Sharpe (2004) published the rst summary of measurement tools on coalitions. This summary
identied 26 articles and 146 measurement scales in multiple categories, including member
and organizational characteristics, group processes and functioning, and impacts. The American
Journal of Preventive Medicine published a supplement in 2008, led by Daniel Stokols and
colleagues, which included articles on measures of team science as a result of the National
Cancer Institute (NCI) investment in transdisciplinary research centers (Hall et al., 2008;
Mâsse et al.,2008). This further led to an NCI-hosted team science tool kit on the web that
includes collaboration measures (www.teamsciencetoolkit.cancer.gov/Public/searchAdvResult
.aspx?st=a&sid=2).
The Research for Improved Health (RIH) study (discussed in Chapters6 and17) conducted
a literature review from 2002 to 2008 of measures of coalitions, inter-agency partnerships,
community-academic partnerships, CBPR, and other community-engaged research. Forty-six
instruments were identied with 224 individual measures, which tracked along constructs from
the CBPR conceptual model (Sandoval et al.,2011). Partnering processes had the largest number
of identied measures, including instruments such as the widely used Wilder Collaboration tool
(http://wilderresearch.org/tools/c/index.php; Mattessich, Murray-Close, & Monsey,2001).
This RIH study then went on to integrate some of these published measures (such as
Khodyakov et al.,2011; Lasker, Weiss, & Miller,2001) with newly created ones, such as align-
ment with CBPR engagement principles, to assess partnering practices and outcomes in two
Internet surveys of two hundred federally funded research partnerships in 2009 (see Chapter17).
Scales from these survey instruments have been validated (Oetzel et al.,2015; Wallerstein et al.,
under review; Chapter5). The measures themselves are provided in Excel spreadsheets and in
pdf form on the Center for Participatory Research, University of New Mexico (UNM-CPR),
website (http://cpr.unm.edu/research-projects/cbpr-project/research-for-improved-health.html)
for partnerships to use or adapt for their own needs. The matrix of the variables used in these
scales was published by CES4Health (Pearson et al.,2014).
In addition, the RIH study included a number of qualitative evaluation and reection tools
including historical time lines and Rivers of Life (Appendix 7), and open-ended focus group
and interview guides for in-depth case studies are also available at UNM-CPR (see http://cpr
.unm.edu/research-projects/cbpr-project/index.html). Realist methodology has contributed impor-
tant analytic methodologies for theorizing from the data (see Appendix 6).
A follow-up UNM-CPR Engage for Equity study (2015–2020), with ve other university
and community partners and a think tank of CBPR practitioners, has rened these instruments
(also translating them into Spanish). A new Internet survey has been conducted with close to
two hundred federally funded partnerships in 2015 to provide additional validation and under-
standing of promising practices contributing to multiple outcomes. The CBPR model is being
used as a reection tool for visioning and assessing where partnerships have been and where
they’re headed. See http://cpr.unm.edu/research-projects/cbpr-project/facilitation_tools.html
for facilitation planning and evaluation visioning guides, among other tools.
Some constructs, such as trust, have received much attention because of the importance of
relationships in CBPR. Trust, however, has been difcult to measure because of its dynamic
nature and its history of being seen as a binary construct. The Centers for Disease Control pub-
lished one of the rst trust tool surveys (www.cdc.gov/prc/pdf/partnershiptrusttoolsurvey.pdf).
Appendix 10
395
Lucero and colleagues in the Research for Improved Health study have tested a new trust
typology measure with qualitative and quantitative evidence (Lucero et al.,2016; see Chapter5).
Jagosh and colleagues, using a qualitative approach of realist evaluation, have identied trust
and synergy as important pathways within CBPR (see Appendix 6).
Over the course of the last several decades, many established CBPR centers have developed
their own qualitative and quantitative methods and instruments, including the well-regarded
and long-standing Detroit Community-Academic Urban Research Center (www.detroiturc.org/
resources/urc-cbpr-tools.html; Israel, Eng, Schulz, & Parker,2013). The University of Kansas
Community Tool Box (Appendix 11) has provided substantial evaluation expertise to collabo-
ratives with innovative tracking tools to enable communities to conduct self-evaluations. Green
and colleagues rst published in 1995 (and later amended) their reliability-tested guidelines for
funders, evaluators, and partnerships to assess the extent projects were using participatory cri-
teria at all stages of the research process (Mercer et al.,2008; http://lgreen.net/guidelines.html).
Colleagues at the University of California, Los Angeles, the RAND Corporation, and
Healthy African American Families and others have developed strategies and measures
to assess the added value of participation in mental health services research (Khodyakov
et al.,2011,2013; Ngo et al.,2016; see Chapters10 and17). The core practice of alignment
with CBPR or community engagement principles has been assessed by multiple teams (Braun
et al,2012; Goodman et al.,2017; Oetzel et al.,2015).
The network of Clinical Translational Science Awardees (CTSAs) since 2006 has sup-
ported greater interest in community engagement across academic health centers. The CTSA
Community Engagement Key Functions Committee rst produced a community engagement
infrastructure logic model, with a call to identify measures that could be shared across sites
(Eder et al., 2013). In 2016, NIH’s National Center for Advancing Translational Science, which
currently supports the CTSAs, charged their more recently formed Collaboration and Engage-
ment Domain Task Force to identify existing measures of collaboration and team science quality
and collaboration outcomes, including measures of community engagement and team science,
to share across academic health centers. The work group
1
that formed started with a review of
the literature and found, similar to Granner and Sharpe (2004) and Sandoval et al. (2011), a
greater focus on group dynamics, with only some measures having rigorous validity or reli-
ability data. Social network analyses also have been growing as a newer measure of engagement
processes and outcomes (Franco et al.,2015).
The NCI has continued their interest in measures with their interactive Grid-Enabled Mea-
sures (GEM) website (www.gem-beta.org/Public/Home.aspx), a “collaborative tool containing
behavioral, social science, and other relevant scientic measures” that includes measures and
constructs on dissemination and implementation, community collaboration, CBPR, and CEnR.
Ongoing “Research to Reality” NCI-sponsored webinars continue to share community engage-
ment methods and measures (Glasgow & Stange, 2017). While distinct, measures from the
Consolidated Framework for Implementation Research may also be useful (see http://www
.crguide.org/quant.html; Lewis et al,2015).
In summary, there are a number of approaches for evaluation in CBPR contexts, processes,
impact on research, and outcomes. Previous evaluation tools tended to be locally developed
and thus lacked some psychometric validation because sample sizes were small by design.
More recent tools have been developed with large samples of partnerships and have strong
396 Appendix 10
measurement validity. In addition, recent tools have also moved beyond a focus on group
dynamics to other domains in the CBPR conceptual model, including contextual issues and
strategies that affect intervention and research design, such as level of community involve-
ment in research steps, intervention t to culture, and partnership synergy in working together.
A broader array of outcomes is also being collected in addition to specic research outcomes.
Intermediate capacity, policy changes, and sustainability outcomes are being seen as important,
as are the larger outcomes of community transformations to improve health and health equity.
Finally, qualitative methods are being recognized as equally important to triangulate with
the quantitative data. Mixed methods are needed to produce a rich picture and understandings
of the depth and breadth of partnering and engagement processes that contribute to outcomes.
Probably most importantly, however, is the recognition that participatory processes are dynamic
and ever-changing, and partnerships need to identify what practices may be most important for
them to assess and strengthen as they move forward toward their own outcomes and goals of
promoting health equity (Brennan Ramirez, Baker & Metzler,2008, pg. 82). All these develop-
ments are welcome for advancing our understanding and practice of CBPR.
NOTE
1. With ndings to be published by Developing Measures of Collaboration Workgroup led by Beth
Tigges, PhD (University of New Mexico), Usha Menon, PhD (University of Arizona), and Doriane
Miller, MD (University of Chicago). See Collaboration/Engagement Domain Task Force for other
resources: https://ctsacentral.org/articles/?article=Collaboration%20Engagement.
REFERENCES
Braun, K. L., Nguyen, T. T., Tanjasiri, S. P., Campbell, J., Heiney, S. P., Brandt, H. M., Smith, S. A., Blumenthal,
D.S., Hargreaves, M., Coe, K., Ma, G. X., Kenerson, D., Patel, K., Tsark, J., & Hébert, J. R. (2012). Operationalization of
community-based participatory research principles: Assessment of the National Cancer Institute’s community network
programs. American Journal of Public Health, 102(6), 1195–1203.
Brennan Ramirez, L. K., Baker, E. A., & Metzler, M. (2008). Promoting health equity: A resource to help communities
address social determinants of health. Atlanta: US Department of Health and Human Services, Centers for Disease
Control and Prevention. https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/tools/pdf/sdoh-
workbook.pdf, Accessed, June, 2017.
Eder, M., Carter-Edwards, L., Hurd, T. C., Rumala, B. B., & Wallerstein, N. (2103). A logic model for community engage-
ment within the CTSA Consortium: Can we measure what we model? Academic Medicine, 88(9), 1430–1436.
Franco, Z. E., Ahmed, S. M., Maurana, C. A., DeFino, M. C., & Brewer, D. D. (2015). A social network analysis of 140
community-academic partnerships for health: Examining the healthier Wisconsin partnership program. Clinical and
Translational Science, 8, 311–319. doi:10.1111/cts.12288
Glasgow, R. E., & Stange, K. C. (2107, May). How engaged are we? Measuring community engagement and partnership.
Research to Reality. Retrieved from https://researchtoreality.cancer.gov/discussions/how-engaged-are-we-measuring-
community-engagement-and-partnership
Goodman, M., Sanders Thompson, V., Johnson, C. A., Gennarelli, R., Drake, B. F., Bajwa, P., Witherspoon, M., & Bowen,
D. (2017). Evaluating community engagement in research: Quantitative measure development. Journal of Community
Psychology, 45(1),17–32.
Granner, M. L., & Sharpe, P. A. (2004). Evaluating community coalition characteristics and functioning: A summary of
measurement tools. Health Education Research, 19, 514–532.
Appendix 10
397
Hall, K. L., Stokols, D., Moser, R. P., Taylor, B. K., Thornquist, M. D., Nebeling, L. C.,...Jeffery, R. W. (2008). The collaboration
readiness of transdisciplinary research teams and centers: Findings from the National Cancer Institute’s TREC year-one eval-
uation study. American Journal of Preventive Medicine, 35(2S), S161–S172. doi:10.1016/j.amepre.2008.03.035
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (Eds.). (2013). Methods in community-based participatory research for
health: From processes to outcomes (2nd ed.). San Francisco, CA: Jossey-Bass.
Jagosh, J., Bush, P. L., Macaulay, A., Salsberg, J., Greenhalgh, T., Wong, G., Cargo, M., Green, L. W., Herbert, C. P., & Pluye,
P. (2015). A realist evaluation of community-based participatory research: Partnership synergy, trust building and related
ripple effects. BMC Public Health, 15(725), 1–11.
Khodyakov, D., Stockdale, S., Jones, A., Mango, J., Jones, F., & Lizaola, E. (2013). On measuring community participation in
research. Health Education Behavior, 40(3), 346–354.
Khodyakov, D., Stockdale, S., Jones, F., Ohito, E., Jones, A., Lizaola, E., et al. (2011). An exploration of the effect of
community engagement in research on perceived outcomes of partnered mental health services projects. Society and
Mental Health, 1(3), 185–199.
Lasker, R., Weiss, E., & Miller, R. (2001). Partnership synergy: A practical framework for studying and strengthening the
collaborative advantage. The Milbank Quarterly, 79, 179–205.
Lewis, C. C., Fischer, S., Weiner, B., Stanick, C., Kim, M., & Martinez, R. (2015). Outcomes for implementation science:
An enhanced systematic review of instruments using evidence-based rating criteria, Implementation Science, 10:155,
DOI: 10.1186/s13012-015-0342-x
Lucero, J., Wallerstein, N., Duran, B., Alegria, M., Greene-Moton, E., Israel, B., Kastelic, S., Magarati, M., Oetzel, J.,
Pearson, C., Schulz, A., Villegas, M., & White Hat, E. (2016). Development of a mixed methods investigation of process
and outcomes of community based participatory research. Journal of Mixed Methods. doi:10.1177/1558689816633309
Mâsse, L. C., Moser, R. P., Stokols, D., Taylor, B. K., Marcus, S. E., Morgan, G. D.,...Trochim, W. M. (2008). Measuring
collaboration and transdisciplinary integration in team science. American Journal of Preventive Medicine, 35(2S),
S151–S160. doi:10.1016/j.amepre.2008.05.020
Mattessich, P., Murray-Close, M., & Monsey, B. (2001). Wilder collaboration factors inventory. St. Paul, MN: Wilder Research.
Mercer, S., Green, L. W., Cargo, M., Potter, M., Daniel, M., Olds, R. S., & Reed-Gross, E. (2008). Appendix C: Reliability-
tested guidelines for assessing participatory research projects. In W. Minkler & N. Wallerstein (Eds.), Community-based
participatory research for health: From processes to outcomes (2nd ed.). San Francisco, CA: Jossey-Bass.
Ngo, V. K., Sherbourne, C., Chung, B., Tang, L., Wright, A. L., Whittington, Y., Wells, K., & Miranda, J. (2016). Community
engagement compared with technical assistance to disseminate depression care among low-income, minority women:
A randomized controlled effectiveness study. American Journal of Public Health, 106(10), 1833–1841.
Oetzel, J. G., Zhou, C., Duran, B., Pearson, C., Magarati, M., Lucero, J., Wallerstein, N., & Villegas, M. (2015). Establish-
ing the psychometric properties of constructs in a community-based participatory research conceptual model. American
Journal of Health Promotion, 29, e188–e202.
Pearson, C., Duran, B., Martin, D., Lucero, J., Sandoval, J., Oetzel, J., Tafoya, G., Belone, L., Avila, M., Wallerstein, N., &
Hicks, S. (2014, December). CBPR variable matrix: Research for improved health in academic-community partnerships.
CES4Health.info. Retrieved from http://ces4health.info/nd-products/view-product.aspx?code=FWYC2L2T
Sandoval, J. A., Lucero, J., Oetzel, J., Avila, M., Belone, L., Mau, M., Pearson, C., Tafoya, G., Duran, B., Rios, L. I., &
Wallerstein, N. (2011). Process and outcome constructs for evaluating community-based participatory research projects:
A matrix of existing measures. Health Education Research, 27, 680–690. doi:10.1093/her/cyr087
Stokols, D., Hall, K. L., Taylor, B. K., & Moser, R. P. (2008). The science of team science: Overview of the eld and introduc-
tion to the supplement. American Journal of Preventive Medicine, 35(2S), S77–S89.
Wallerstein, N., Oetzel, J., Duran, B., Magarati, M., Pearson, C., Belone, L., Davis, J., Dewindt, L., Lucero, J., Ruddock, C.,
Sutter, E., Villegas, M., & Dutta, M. (under review). Conceptualizing and measuring the culture-centered approach in
community based participatory research. Social Science & Medicine.
APPENDIX
11
PARTICIPATORY MONITORING
AND EVALUATION OF
COMMUNITY HEALTH
INITIATIVES USING THE
COMMUNITY CHECK BOX
EVALUATION SYSTEM
STEPHEN FAWCETT, JERRY SCHULTZ, VICKI COLLIE-AKERS, CHRISTINA HOLT,
JOMELLA WATSON-THOMPSON, AND VINCENT FRANCISCO
How do we see and reflect on what community health initiatives are
accomplishing and use the information to enhance progress?
Comprehensive community health initiatives are challenging to evaluate; they are complex,
dynamic, unfolding, with their effects on outcomes often delayed. For an evaluation approach
to be useful and used, it needs to be able to document the unfolding of key activities (the inter-
vention) over time, characterize and report the information in meaningful ways, and examine
possible associations between activities and indicators of success. Consistent with principles of
400 Appendix 11
community-based participatory research (CBPR) (Fawcett, Collie-Akers, Schultz, & Cupertino,
2013; Minkler & Wallerstein, 2008), a participatory evaluation system should make it easier
for community and evaluation partners to (1) document activities and indicators of success, (2)
reect on patterns in the data (e.g., factors related to a marked increase in community or sys-
tems changes), and (3) use the information for decision making and adjustments.
BACKGROUND AND TECHNICAL SUPPORTS FOR MONITORING AND
EVALUATION
Since the early 1990s, the Work Group for Community Health and Development at the Univer-
sity of Kansas (http://communityhealth.ku.edu) has developed and implemented supports for
participatory evaluation using the Community Check Box Evaluation System, an online docu-
mentation and support system (Fawcett & Schultz, 2008). This evaluation system has been used
with a variety of community health initiatives, including those to prevent chronic diseases, com-
municable diseases, adolescent pregnancy, substance abuse, violence, child abuse, and limited
access to health care (e.g., Collie-Akers et al., 2013; Fawcett et al., 1997, 2013, 2015; Paine-
Andrews et al., 2002; Watson-Thompson et al., 2013).
Each customized Community Check Box integrates tools for participatory evaluation with
supports for systematic reection and making adjustments. It includes tools to make the follow-
ing easier:
■ Documenting activities and importing of indicators of success
■ Graphing key measures (e.g., development activities, resources generated, services
provided, community and systems change, indicators of population-level outcomes)
■ Shared sensemaking (i.e., using embedded questions to reect on the data—what are we
seeing and what does it mean, e.g., in patterns of activity over time, distribution of activities
by goal area)
■ Reporting to stakeholders (e.g., about activities, outcomes, factors affecting success,
lessons learned)
The Community Check Box also features integrated supports for reection and action
curated from the content of the Community Tool Box (CTB) (http://ctb.ku.edu). For instance,
if review of data for an initiative suggests that “there is not enough improvement in outcomes,”
the Check Box user is prompted to ask questions of the situation (e.g., “Are changes in place
long enough to make a difference?”). Links are also provided to Tool Box resources to support
improvement (e.g., tool kits and troubleshooting guides for evaluation and sustainability).
Selected supports are curated from the Community Tool Box’s more than seven thousand
pages of free resources for building healthy communities. Reaching more than 5 million unique
users annually, these include CTB open source content for (1) learning skills (e.g., conducting
listening sessions), (2) doing the work (e.g., assessing needs and resources), (3) solving prob-
lems (e.g., not enough participation), and (4) implementing processes for change (e.g., imple-
menting effective interventions).
This report outlines a protocol for participatory monitoring and evaluation, sensemaking,
and adjustments made easier by the Community Check Box Evaluation System.
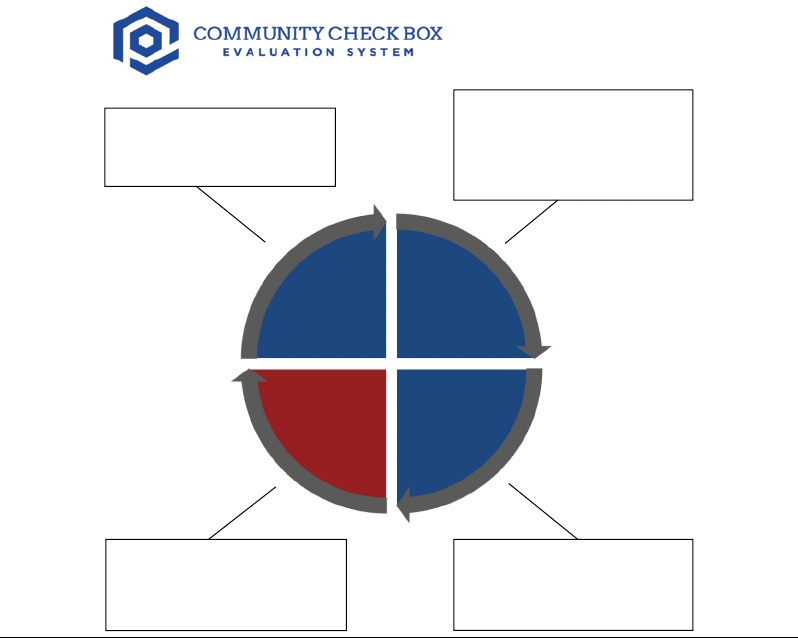
Appendix 11
401
PROTOCOL FOR PARTICIPATORY MONITORING AND EVALUATION
As depicted in FigureA11.1, the Community Check Box Evaluation System enables a four-step
process to do the following:
1. Capture instances of key activities implemented in the effort. Methods used include report-
ing of activities by implementers, interviews with key informants (i.e., people knowledge-
able about the initiative), and review of documents (e.g., progress reports). This results in
identied instances of activities and relevant details (i.e., what was done, when, by whom,
toward what goal).
2. Code by type of activity using denitions and scoring instructions to ensure consistency
of entries. For instance, typical initiative activities and outputs may include development
activities (e.g., action plans), services provided (e.g., delivery of programs), resources gen-
erated (e.g., new grants), and community or systems changes (e.g., new or expanded pro-
grams, policies, environmental changes).
2. Capture: documenting
activities related to the
effort
1. Code: classifying by types
of activity (e.g.,
development activities,
community and system
changes)
CodeCapture
4. Communicate: using
activity listings, graphic
displays, and participation
in sensemaking
3. Characterize: by relevant
attributes (e.g., goal
addressed, sector in which
implemented)
CharacterizeCommunicate
FIGURE A11.1 Protocol for Participatory Monitoring and Evaluation Using the
Community Check Box Evaluation System
402 Appendix 11
3. Characterize the activity by attributes important-to-understanding implementation.
For instance, documented community or system changes may be characterized by (a)
goal addressed (e.g., infant mortality, poverty, and jobs); (b) strategy used (e.g., mod-
ifying access, policy change); (c) estimated reach (e.g., low—less than 5 percent of
population); (d) duration (e.g., one-time event, ongoing); (e) target group (e.g., children,
marginalized group); (f) sector in which implemented (e.g., schools, government); and
other attributes.
4. Communicate and dialogue about progress. For instance, community and evaluation part-
ners can use summary activity listings, online graphs, and reection questions to report,
critically review, and make sense of the data (see FigureA11.2).
PARTICIPATORY SENSEMAKING AND ADJUSTMENTS
A hallmark of CBPR and other participatory approaches is that community and research
partners have shared roles in collecting and analyzing data. As an example, we used the
check box in a participatory monitoring and evaluation (M&E) project with partners at the
World Health Organization Regional Ofce for Africa. They were interested in examining
the implementation and effects of Ebola response activities in an outbreak area in Libe-
ria. We used the Community Check Box (CCB) Evaluation System to support participatory
sensemaking by pairing (1) graphs of activities and outcomes (see the graph at the left in
FigureA11.2) with (2) CCB questions to guide systematic reection (see the text box at the
right of FigureA11.2).
Shared sensemaking among community and evaluation partners focused on three reection
questions:
1. What are we seeing? For instance, for this M&E of the Ebola response effort, the line graph
of cumulative activities (see FigureA11.2) showed a marked increase in Ebola response
activities over time, with an acceleration (steeper curve) and sustained activity from late
June 2014 through October 2014.
2. What does it mean? In dialogue, WHO regional ofce partners noted that this increase
in Ebola response activity was associated with a bending of the curve in the incidence
of Ebola virus disease in this affected county (by mid-August 2014) and in achieving
zero (by November 2014). Marked acceleration in Ebola response activities (late June
2014) was associated with several factors (see FigureA11.2, boxes with arrows show-
ing date of onset), for instance, WHO staff member engagement and development of
action plans.
3. What are the implications for adjustment? The WHO regional ofce for Africa lead-
ership team reviewed the M&E data and associated sensemaking to identify areas for
future adjustment and improvement. For instance, the group recommended ensuring early
deployment of WHO staff members and other supports suggested during the sensemak-
ing dialogue.
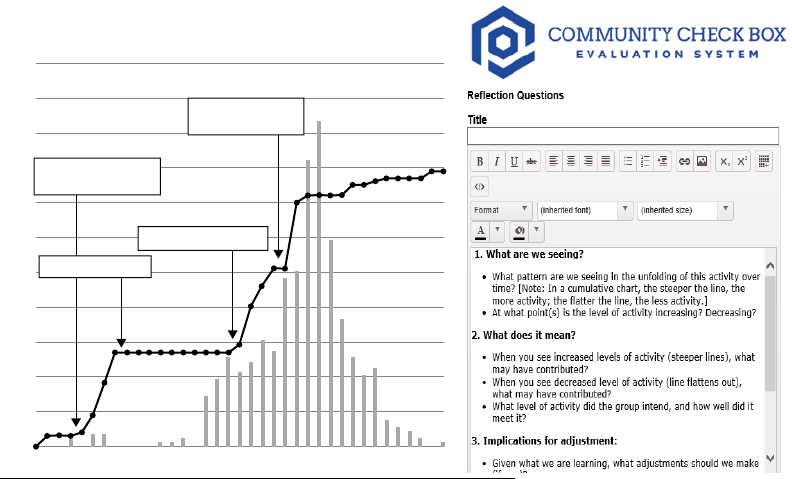
Appendix 11
403
CONCLUSION
Adherence to CBPR principles—especially fostering co-learning and capacity building among all
partners—is a particular strength of this approach. In supporting participatory sensemaking, this
evaluation approach strengthens the capabilities of community and research partners to systemat-
ically reect on what is happening—what we are seeing, its meaning, and implications for adjust-
ment. By making documentation and reporting easier and more transparent, this evaluation system
creates opportunities for shared learning, communication, and accountability. Through coding of
key implementation activities and outcomes, it enables attention to core evaluation questions such
as whether the initiative is bringing about community and environmental change and whether these
changes are associated with improvements in indicators of population health and health equity.
By enabling characterization of activities by key attributes, we can more effectively estimate
the dose of comprehensive community initiatives (i.e., the amount and type of interventions
implemented) and their contribution to population health improvement (Fawcett, Collie-Akers,
Schultz, & Kelley, 2015). Our hope is that such participatory evaluation approaches can
strengthen the capacity of community and research partners to understand and improve efforts
to build healthier and more just communities.
110
100
County-level action
plans developed
WHO confirms Ebola
outbreak
WHO staff on ground
90
80
70
60
50
40
30
20
10
0
Feb-14 Mar-14 Apr-14 May-14
New cases of Ebola Ebola Response Activities
Jun-14 Jul-14 Aug-14 Sep-14 Oct-14
Activities halted
Using Community Check Box Reflection Questions (What are we seeing? Meaning? Adjustments?)
to dialogue with partners about key events [in boxes] that are associated with increased or decreased
implementation activity and related improvement or worsening of outcomes.
FIGURE A11.2 Participatory Sensemaking
404 Appendix 11
REFERENCES
Collie-Akers, V. L., Fawcett, S. B., & Schultz, J. A. (2013). Measuring progress of collaborative action in a community health
effort. Revista Panamericana de Salud Pública/Pan American Journal of Public Health, 34(6), 422–428.
Fawcett, S. B., Collie-Akers, V., Schultz, J. A., & Cupertino, P. (2013). Community-based participatory research within the
Latino Health for All Coalition. Journal of Prevention and Intervention in the Community, 41(3), 142–154.
Fawcett, S. B., Collie-Akers, V., Schultz, J., & Kelley, M. (2015). Measuring community programs and policies in the Healthy
Communities Study. American Journal of Preventive Medicine, 49(4), 636–641.
Fawcett, S. B., Lewis, R. K., et al. (1997). Evaluating community coalitions for the prevention of substance abuse: The case
of Project Freedom. Health Education and Behavior, 26(6), 812–828.
Fawcett, S. B., & Schultz, J. A. (2008). Supporting participatory evaluation using the Community Tool Box online documen-
tation system. In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health: From process
to outcomes (2nd ed., pp. 419–424). San Francisco, CA: Jossey-Bass.
Fawcett, S. B., Sepers, C. E., Jones, J., Jones, L., & McKain, W. (2015). Participatory evaluation of a community mobilization
effort to enroll residents of Wyandotte County, Kansas residents through the Affordable Care Act. American Journal of
Public Health, 105(S3), S433–S437.
Minkler, M., & Wallerstein, N. (Eds.). (2008). Community-based participatory research for health: From process to outcomes
(2nd ed.). San Francisco, CA: Jossey-Bass.
Paine-Andrews, A., Fisher, J. L., Berkley-Patton, J., Fawcett, S. B., Williams, E. L., Lewis, R. K., & Harris, K. J. (2002).
Analyzing the contribution of community change to population health outcomes in an adolescent pregnancy prevention
initiative. Health Education and Behavior, 29(2), 183–193.
Watson-Thompson, J., Jones, M. D., Colvin, J. D., McClendon-Cole, T., Schober, D. J., & Johnson, A. M. (2013). Supporting
a community-based participatory evaluation approach to violence prevention in Kansas City. Journal of Prevention and
Intervention in the Community, 41(3), 155–166. doi:10.1080/10852352.2013.788342
APPENDIX
12
POWER MAPPING
A USEFUL TOOL FOR UNDERSTANDING THE
POLICY ENVIRONMENT AND ITS APPLICATION
TO A LOCAL SODA TAX INITIATIVE
JENNIFER FALBE, MEREDITH MINKLER, ROBIN DEAN, AND JANA CORDEIERO
Power mapping is increasingly used by CBPR partnerships and community-based organizations
to better understand local or regional policy environments for a particular issue or legisla-
tion they hope to see passed (or defeated). Best used in small groups of ve or six members,
this power-mapping exercise is helpful for identifying key organizational, community, and
individual players; their stance on the issue; and their relative strength and inuence (Ritas, Ni,
Halpin, & Minkler,2008).
Policy mapping is particularly useful in cases of “strange bedfellows,” for example, when an
organization that has historically favored measures promoting public health takes an uncharacter-
istic opposing stand on a health-promoting measure. As illustrated in the following, the acceptance
of donations or other support from an industry or group opposing the measure may be behind such
unexpected reversals.
After briey describing how to make and use a power map, we turn to a case study of a
coalition’s efforts to pass a soda tax ballot measure in San Francisco in 2014 and again in 2016.
We demonstrate how understanding where key community, organizational, and government and
other actors stood helped partially explain the measure’s initial failure, as well as how changes
in the initiative and its support strategies may have helped a subsequent measure succeed.

406 Appendix 12
MAKING AND USING A POWER MAP
First, select the specic policy measure your group wants to help pass or defeat, for example,
a state legislative initiative to increase the smoking age from eighteen to twenty-one or a city
council proposal to ban the shipping of coal from its port.
As a group, do the following:
1. Identify the policy target(s): the individuals and organizations with the power to make a
particular change happen
2. Identify the other key players in this situation: the individuals, organizations, or commu-
nities that may be affected by the problem or policy or that have the potential to inuence
the situation. Keep in mind that as change becomes imminent, many people will be drawn
into the issue who did not know or care about it before. Try to anticipate who this will be.
3. On a sheet of paper, write your policy objective at the top. Label the left side supporters,
the middle undecided (or divided), and the right side opposition. Indicate on this page
your targets (depicted as circles) and key players (squares), according to where they fall
along the spectrum. As illustrated in FigureA12.1, for visual reference use larger squares
and circles to indicate more powerful targets and players, or those with more at stake, and
smaller ones to indicate those who are weaker or less affected by the outcome.
In your mapping, remember that many considerations go into decisions about relative
power (depicted in the size of the squares or circles), among them the target’s or player’s
Policy goal or objective: ______________________
Supporters
Neutral or cannot comment
Opposition
Targets with
power to
make change
Players
affected by
problem or
policy or
having the
potential to
influence the
situation
FIGURE A12.1 Creating a Power Map
Source: Reprinted from Ritas, Ni, Halpin, and Minkler (2008).
Appendix 12
407
scope (size), resources (staff, money, lobbyists), skills, and access, as well as how intensely
the issue affects each target or player (e.g., is it a burning or tangential issue?). A small
group that cares deeply about an issue and has great resources and organization may be
more effective than a larger group with few resources or poor organization or one that feels
less strongly (Ritas et al.,2008). When possible, allow the circles and squares to overlap
where interests overlap. However, because some supporters may share interests with those
opposed to your policy, nding areas of (sometimes unspoken) overlap between supporters
may not always be possible (Ritas et al.,2008).
4. Particularly important in an election or decision year is to nd out what campaign con-
tributions, donations, or perks may have been received in current or recent years and by
which player(s) in a position of inuence. This step typically is not included in an initial
power map and often takes place subsequently because there is usually a time lag between
when campaign contributions are made and when they are publicly disclosed. However,
when available, campaign contribution information may be useful in updating the map and
considering strategic choices. Such information may serve as an important reality check or
point of leverage in your group’s efforts.
5. Given your current knowledge base, choose the three most important individuals and orga-
nizations to inuence. Consider the following:
■ Is it more important now to strengthen your allies, persuade those who are neutral, or
weaken the opposition?
■ Is it time to approach a target or to work with key players?
■ Can we get more information to increase the map’s accuracy? If so, where, when, and how?
Questions for reection: For the policy you have chosen, was it easier to identify supporters
or sources of opposition? Why or why not? Were there surprises when considering potential
overlapping interests? If your group decided the time was right to approach a key target or
player, what are useful next steps?
ILLUSTRATION OF POLICY MAPPING REGARDING A LOCAL SODA TAX
INITIATIVE
Reducing consumption of sugar-sweetened beverages (SSBs) is a major public health priority
because its consumption increases the risk of obesity, diabetes, and heart disease (Hu,2013).
Based on the success of tobacco taxation in reducing smoking, public health experts have called
for SSB taxes (so-called soda taxes) to reduce consumption and raise revenues for public health
programs (Brownell et al.,2009). Mexico implemented a soda tax in 2014, and in the wake of
dozens of unsuccessful attempts in the United States, Berkeley, California, became the rst US
jurisdiction to pass a soda tax in 2014. Berkeley’s successful passage has since been followed
by Philadelphia, Oakland, San Francisco, Albany, Boulder, and Cook County in 2016. A com-
prehensive junk food and soda tax passed the Navajo Nation Council in 2015, after three years
of education and organizing campaigns. As predicted from economic models, Mexico’s and
Berkeley’s soda taxes resulted in reduced consumption of SSBs (Colchero, Popkin, Rivera, &
Ng,2016; Falbe et al., 2016), especially in lower-income households, which bear the brunt of
diet-related chronic disease.

408 Appendix 12
In November 2014, at the same time that Berkeley passed a soda tax, San Francisco
residents took to the polls for a vote on a two-cent-per-ounce tax on the distributors of sug-
ary drink. Tax revenues were to be allocated to physical activity and nutrition programs, child
dental care, and healthy food and drinks access for those most at risk for chronic diseases. Three
city supervisors who crafted the measure did so by consulting with advocates, academics, and
experts. Because the measure designated specic revenue allocations, it needed a two-thirds
majority to pass under California tax law, unlike Berkeley’s general soda tax, which required
only a simple majority.
One group of soda tax advocates’ assessment of support, opposition, and neutrality vis-à-
vis the tax informed the power map shown in FigureA12.2. These power dynamics are based on
advocates’ knowledge and information gleaned from policy makers, news media, public health
research, and advocacy and philanthropic organizations.
Before the initiative was on the ballot, advocates had a good understanding of its key sup-
porters, opponents, and neutral players and had learned from soda tax attempts in other cit-
ies that the beverage industry would use tremendous nancial and political resources to ght
the measure. However, the pro-tax advocates were unsure which organizations the industry
could sway. San Francisco’s rst Chinese American mayor, who was extremely popular in the
Chinese community, was neutral from the start of the campaign. Advocates were unsure if his
silence was the result of the city previously having received funds from the beverage industry,
his close relationship with the business community, or competing political priorities. Without
the mayor’s support and signicant resources, advocates knew they needed to gain support and
build their power base through endorsements from the city’s many education, health, youth-
serving, and political Democratic groups that publish voter guides. Throughout the campaign,
the mayor remained neutral, likely resulting in failure to garner support from Chinese voters.
Further, opposition funding appeared to sway the positions of some other key players.
Supporters Neutral or cannot comment Opposition
Most city
supervisors
Mayor
Voters
Chamber of Commerce
Healthy Retail
coalition
SF Unified
School District
and PTAs
City departments
Beverage
industry
Large LGBT
organization
SF Council of
Merchants
and many
store owners
Many public
health and
health care
organizations
Large, progressive
medical organization
Targets with
power to
make change
Players
affected by
problem or
policy or
having the
potential to
influence
situation
City
Supervisor
FIGURE A12.2 Power Map for San Francisco Soda Tax 2014
Appendix 12
409
At the start of the campaign, a city supervisor’s vote to place the initiative on the ballot
suggested he was a supporter. However, when his comments at a board of supervisor’s meet-
ing mirrored arguments from the No campaign, advocates were unsure where to place him.
This supervisor was strongly supported by a progressive LGBT group, which was actively
campaigning for his election to a higher ofce. That group had received $70,000 early in
the election year from the American Beverage Association (ABA)–funded opposition. ABA
support was evident from the many mailers advocating for this candidate and against the soda
tax measure. This infusion of campaign funds, and its apparent inuence, led advocates to
move the supervisor from “supporter” to “opponent” on the power map.
Although two other city supervisors and some Democratic clubs also received ABA funds,
because of their perceived minimal inuence, they were not included on the map.
The inability of some likely and potentially powerful supporters to take a stand on the tax
also may have hurt the measure’s chances. For example, the SF Health Commission—the gov-
erning policy body of the San Francisco Department of Public Health (SFDPH) whose mem-
bers are appointed by the mayor—passed a resolution supporting public health efforts to reduce
soda consumption (SFDPH, 2014). By law, however (and unlike elected ofcials), city and
state employees are not permitted to advocate for ballot initiatives, so they could not mention
the soda tax initiative in their resolution. Experts from a well-respected public university, who
also are state employees, were largely silent and had indeed received warnings from the univer-
sity prohibiting activity in political campaigns.
Yet even nongovernmental employees sometimes failed to take a stand. The heads of some
community-based organizations with city contracts thus were concerned that those contracts
might be at risk if they supported the soda tax given the mayor’s neutrality. Finally, a large and
progressive medical organization, whose support could have provided credibility to help sway
voters, also remained silent for reasons that are unclear.
The 2014 San Francisco soda tax measure never had unanimous support from key political
leaders, and this case illustrates how the opposition’s money eroded some of the political support
it did have. Creating and periodically updating a power map can track this support, help explain
why an initiative is succeeding or failing, and inform course corrections.
However, power mapping also has limitations. Even with periodic updates, it cannot account
for all factors operative in the success or failure of political campaigns. Along with the money-
inuenced shifting power dynamics, several other factors inuenced the SF soda tax measure’s
initial failure. These included lack of funds to ght an opponent with seemingly unlimited resources
(soda tax advocates were outspent thirty-one to one), the two-thirds vote threshold for passage, and
a coalition that was narrower and less diverse than desirable. Finally, the ABA-funded opposition
harnessed one of the city’s most urgent concerns—cost of living—in campaign materials. By con-
trast, Philadelphia’s passage of a soda tax in June 2016 was helped, in part, by strong leadership
from the mayor but also by its focus on connecting tax-generated revenue to an issue of great local
concern: early childhood education. Further, it required passage by only the city council.
MOVING TO VICTORY THE SECOND TIME AROUND
As San Francisco supporters embarked on a subsequent soda tax measure for November
2016, they pushed to get and retain mayoral support and endorsements from a wide range of
410 Appendix 12
education, health, civic, and political groups and individuals, which helped balance the power
and resources of the beverage industry. The ultimate victory of the 2016 soda tax measure by
62 percent of the vote (www.sfelections.org/results/20161108/) also had to do with ordinance
revisions proposing a general tax (requiring only a simple majority to pass in California), cou-
pled with the establishment of an advisory committee to make recommendations to the city
on funding of programs to reduce the consumption of sugary drinks. This echoed the structure
of Berkeley’s successful Measure D. Thus far, the Berkeley city council has acted on its advi-
sory commission’s recommendations to fund school, community, and city programs focused
on nutrition and health promotion (www.takepart.com/article/2016/04/25/soda-public-health).
Despite the soda tax’s passage, the overwhelming opposition and resources of the ABA
illustrate the incredibly difcult odds soda tax supporters faced. Indeed, the industry spent over
$28 million to defeat 2016 soda taxes in three Bay Area (https://cspinet.org/resource/big-sodas-
spending-spree-ght-public-health-measures)!
CONCLUSION
As illustrated by the soda tax case study, power mapping is a useful tool for CBPR partnerships
and advocacy groups wishing to better understand the political lay of the land on particular leg-
islation. Periodic mapping updates, and the inclusion of diverse mapping partners with unique
knowledge, can broaden and deepen the evolving story. Meanwhile, supplementing mapping
with ongoing analysis of other make-or-break factors for passage of a new measure, ideally with
the help of policy mentors and other knowledgeable insiders and community leaders, may pro-
vide the most realistic knowledge base for informing subsequent action.
REFERENCES
Brownell, K. D., Farley, T., Willett, W. C., et al. (2009). The public health and economic benets of taxing sugar-sweetened
beverages. New England Journal of Medicine, 361(16), 1599–1605.
Colchero, M. A., Popkin, B. M., Rivera, J. A., & Ng, S. W. (2016). Beverage purchases from stores in Mexico under the excise
tax on sugar sweetened beverages: Observational study. BMJ, 352, h6704.
Falbe, J., Thompson, H. R., Becker, C. M., Rojas, N., McCulloch, C. E., & Madsen, K. A. Impact of the Berkeley excise tax
on sugar-sweetened beverage consumption. American Journal of Public Health, 106(10), 1865–1871.
Hu, F. B. (2013). Resolved: There is sufcient scientic evidence that decreasing sugar-sweetened beverage consumption will
reduce the prevalence of obesity and obesity-related diseases. Obesity Review, 14(8), 606–619.
Ritas, C., Ni, A., Halpin, H., & Minkler, M. (2008). Using CBPR to promote policy change. In M. Minkler & N. Wallerstein
(Eds.), Community-based participatory research for health: From process to outcomes (2nd ed., p. 461). San Francisco,
CA: Jossey-Bass.
San Francisco Department of Public Health (SFDPH). (2014). Health Commission Resolution 11–2. Retrieved from www
.sfdph.org/dph/les/hc/HCRes/Resolutions/2014/Sugar%20Beverages%20Jan%202014rev.pdf

APPENDIX
13
CBPR INTERACTIVE
ROLE-PLAYS
THREE SCENARIOS
MICHELE POLACSEK AND GAIL DANA-SACCO
An interactive online teaching tool provides an ideal environment within which to develop a
virtual community where students and faculty members can dene problems through dialogue,
practice solutions, and engage in disciplined self-reection and critical thinking. This digital
learning space provides real-life-like opportunities to apply knowledge gained though other
CBPR course materials. Short ten- to fteen-minute interactive scenarios paused for discussion
and replay or longer improvised scenarios lasting up to thirty minutes or more could be used
in a classroom setting or as a synchronous or asynchronous online teaching tool. This tool is
particularly suited to digitally inclined students, who may have little opportunity or time to
practice interacting with community research projects or when faculty members are reticent to
overburden a community with student learners.
We envision a game with ve CBPR modules (community-based practice, dening the
issue, partnering with the community, the research process and its transformative power, and
action planning), each of which can stand alone or be presented in sequence. Each module
will provide students with opportunities to attain cross-cutting and module-specic learning
objectives.
The use of interchangeable avatars or digital characters (e.g., minority population, majority
population, gender identity, race, SES) enables students to take on and personally experience
412 Appendix 13
diverse characters, promoting cultural competence, cultural humility, and empathy. Faculty
members, acting as “provocateur,” facilitate the problem-based learning by establishing param-
eters, posing questions, and actively participating with students in the learning environment.
Further development of this approach will require substantial investments. If you are inter-
ested in partnering in this venture please contact Giant Otter at http://giantotter.com or Michele
Polacsek at the University of New England, 716 Stevens Avenue, Portland, ME 04103. One
screenshot of the game with sample characters and dialogue is included.
SAMPLE MODULE 1: CONDUCTING CBPR RESEARCH ON INTIMATE
PARTNER VIOLENCE IN A HIGH SCHOOL WITH A SIGNIFICANT NEW
IMMIGRANT POPULATION
The following is an example of a situation in which community and academic partners are
called to action to address a public health issue. The exible format in which multiple charac-
ters and roles can be created encourages reection and discussion. Background, sample roles,
and instructions are included.
Background for Module 1
Urban high school ofcials have determined that there is a high reported rate of intimate partner
violence (IPV) among the local high school students as reported on a recent Youth Behavioral
Risk Factor Survey (YBRFS). There appears to be a higher prevalence in schools with higher
new immigrant populations. This high school serves a population composed of a signicant
number of new immigrant families as well as a well-established working class white majority.
Because of the preliminary YBRFS ndings and recent inux of new immigrants, school of-
cials are open to an invitation from a well-established community service organization to
partner with a local university to develop and provide health education materials for an IPV-
prevention campaign.
Sample Roles, Characteristics, and Cue Card Instructions for Module 1
1. University faculty member (second-generation East Indian female)—You are working
with a limited time frame because students are available for one semester only. You’re
eager to move the project forward. You have experience studying IPV but no experience
with the new immigrant population. You have partnered with this community service orga-
nization once before.
2. Community service organization staff member (Hispanic female)—You are a long-standing
community activist with deep experience in IPV and extensive knowledge of the transi-
tions this community has experienced over the last thirty years or so.
3. School guidance counselor (white female)—You are very familiar with the IPV issues
that have surfaced. They conrm what you know anecdotally, and you’re eager to nd
solutions.
4. School principal (white male)—You recognize that IPV is a problem, but you’re
concerned that ndings don’t reect well on the school and that racial stereotyping will
fuel tensions.

Appendix 13
413
5. High school student 1 (white male)—You’ve been an active student leader and are looking
to end your senior year with several commitments including a social service project.
Although not known to others, your family currently experiences IPV.
6. High school student 2 (new immigrant female)—You understand the stresses experienced
by new immigrant families, including reluctance to access public safety resources because
of fear of deportation.
7. University student 1 (mixed-race female)—You have personal experience with family
issues involving substance use and IPV. You have completed two internships addressing
these issues. You’re convinced that substance abuse is most often a driver of IPV. You come
from a well-resourced family and have had many opportunities throughout your life to
further your education and have traveled extensively outside the United States.
8. University student 2 (white female)—You’ve organized a get-out-the-vote campaign
among your peers in your home community. You are sensitive to the potential challenges
of working with this issue within the new immigrant population. You come from a modest
working-class background and have no international experience.
9. Parent or school board member (white female)—You are a long-standing member of the
school board and your children grew up in the district and attended the school here. You’re
not sure that the nding of greater substance use among white students is accurate.
Instructions for Students
As you participate, ensure that you attend to relevant CBPR principles. For successful CBPR,
reective practice is essential. Think critically about your role as a researcher and the implica-
tions of your experience and your social status and relative positions of power and privilege in
these interactions (as indicated in the introductory chapters of this book).
Scenario 1: Developing Consensus on a Research Agenda
Setting for Scenario 1
High school classroom
Learning Objectives for Scenario 1
1. Identify key challenges of race-ethnicity and social privilege in the research process.
2. Name the essential elements of conflict management in meetings.
3. Describe the benefits of an inclusive approach to stakeholder participation in CBPR.
Background for Scenario 1
A university faculty member is visiting the school to discuss the YBRFS findings and decide next
steps with the school principal, the guidance counselor, and a community service organization
staff member. She proposes a pilot project in this high school to further investigate factors
associated with IPV among high school students in order to understand how best to intervene.
A peer leader group in the high school, represented by a student in the meeting, will inform the
process and perhaps participate in the research. The group discusses how best to proceed.
(Continued )

414 Appendix 13
Scenario 2: Research Team Meeting
Setting for Scenario 2
At a café or restaurant
Learning Objectives for Scenario 2
1. Name key elements of successful community partnerships in CBPR.
2. Recognize and name own social privilege.
3. Describe how social privilege can bias research processes and outcomes.
4. Demonstrate understanding of complexities of race-ethnicity and social privilege in the research process.
5. Demonstrate effective group or meeting process in CBPR.
Background for Scenario 2
The faculty member reports back preliminary plans and concerns about the project and any next
steps that have already been decided in an initial meeting at the high school. The research team
comes up with two aims: to conduct more research among students to compare factors associ-
ated with IPV in the established and new immigrant populations and to develop recommenda-
tions for interventions based on YBRFS and formative research data. The team develops a
formative research strategy. A short survey with ten questions is developed. An equal number of
respondents will be drawn from volunteers in eleventh- and twelfth-grade health classes.
Characters in Scenario 2
University faculty member, university student 1, and university student 2
Discussion Questions for Scenario 2
1. How does the research team make decisions that are responsive to community concerns?
2. What considerations does the research team need to take into account with regard to developing
community partnerships?
3. What does the research team need to keep in mind to maximize community partner engagement?
Characters in Scenario 1
University faculty member, community service organization staff member, school guidance
counselor, school principal, high school student 1, and high school student 2
Discussion Questions for Scenario 1
1. What steps does the research team take next?
2. How are the important stakeholders identified and involved in this process?
3. What are the challenges that the research team faces?
4. What challenges do the community members face?
5. What challenges do the students face?
6. What decision-making process should be used to establish the research agenda?
Scenario 1 (CONTINUED)
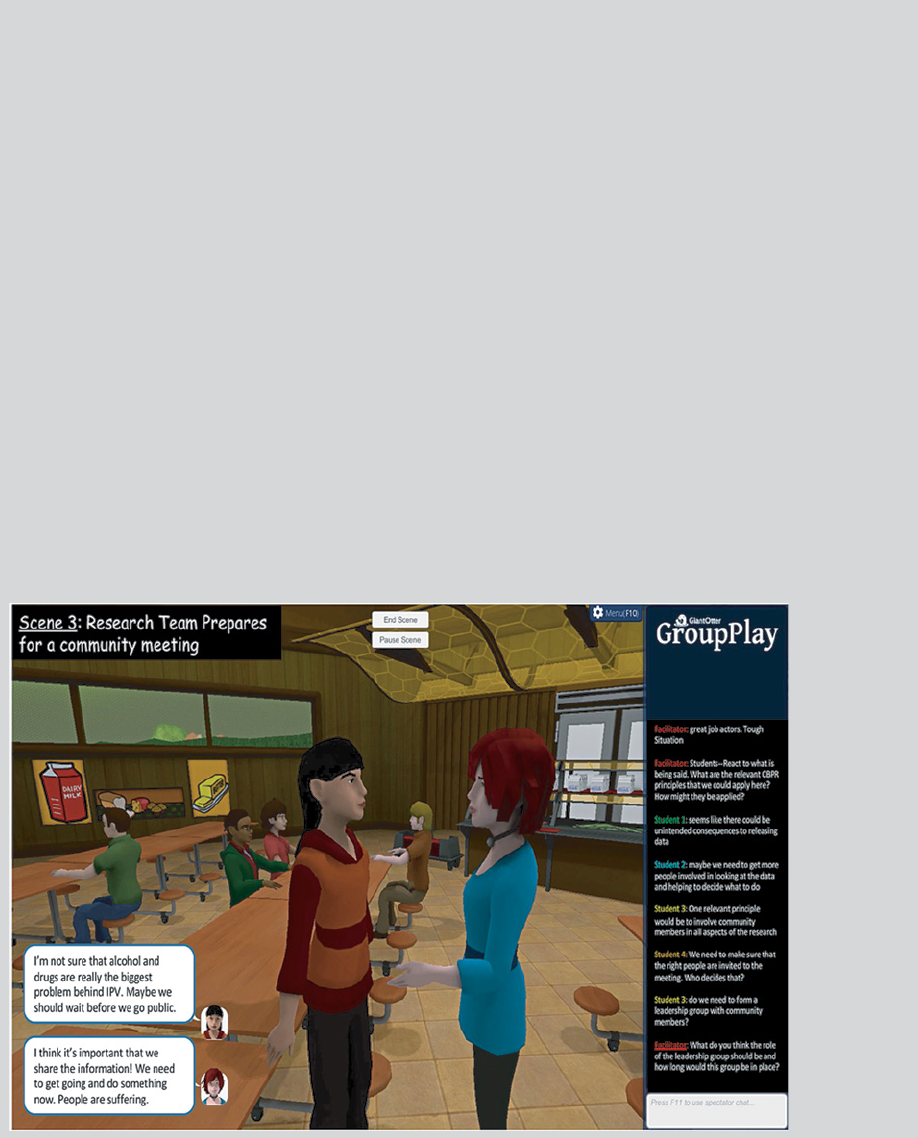
Appendix 13
415
Scenario 3: Research Team Prepares for a Community Meeting
Setting for Scenario 3
School cafeteria
Learning Objectives for Scenario 3
1. Demonstrate understanding of the role of researcher in the CBPR process.
2. Name structural considerations important to a successful CBPR process.
3. Describe ethical considerations working with sensitive information.
Scenario 3 (After the formative research process has taken place)
The research team, at the invitation of the school, plans to attend a community meeting in the school
to report the results of the study. The study does not confirm earlier indicators of a higher incidence
of IPV in the new immigrant community. The research also demonstrates differing associations with
IPV in the two populations studied. Among whites, substance use is associated with IPV. Among new
immigrants, IPV seems to be more associated with economic status of the family. There is a
reluctance to report incidence of IPV within both populations but for different reasons.
Characters in Scenario 3
University faculty member, community service organization staff members, school guidance
counselor, high school student 1 and high school student 2, university student 1 and university
student 2, parent or school board member.
In the following screen shot, the two university students are discussing strategy for the upcoming
community meeting.
(Continued )
416 Appendix 13
Discussion Questions for Scenario 3
1. How should the research team interact with people at the community meeting?
2. Is the group meeting too fast? Are there other steps that need to be taken before the community
meeting?
3. How does the research team develop the recommendations using a CBPR approach?
4. What steps should the team take to involve the appropriate stakeholders in interpreting the
research results and developing an action plan?
Avatar interaction continues as long as the facilitator deems useful. Faculty members and
students have the opportunity to participate as characters or facilitators. Avatar interaction may be
halted at any time to allow for group discussion and recommendations for improvement.
This virtual reality approach provides an innovative pedagogical tool to practice CBPR in a
dynamic, interactive environment, which can be used in a wide variety of settings.
Scenario 3 (CONTINUED)
What a pleasure to be able to share a few thoughts on reading this third edition of Community-
Based Participatory Research for Health. It is a joy to see that Nina Wallerstein and Meredith
Minkler are continuing their productive, insightful, and inspirational leadership in this critically
important role of understanding health and justice within a framework of knowledge democ-
racy. That framework, and this book, are inclusive of each and all of our bodies and diversities,
including the diversities of the knowledge of the earth and the rest of nature. It makes us happy
that Nina and Meredith have found Bonnie Duran and John G. Oetzel with whom to curate this
important new edition. Perhaps most impressive is the fact that this book continues a passion-
ate call for justice, inclusion, change, and democracy. The editors and contributors emphat-
ically reject the idea that the highest standards in health research can be reached only when
detached from the bias of community, our bodies, inequality, racism, or poverty. In some places,
they even challenge the domination of the Western canon of white-male scientic knowledge,
providing examples from women’s knowledge, Indigenous knowledge, knowledge of the street-
involved, and others.
The two of us met in the mid-1970s. Budd had been working in Tanzania in the eld of
adult education. He met Paulo Freire there in 1971 and continued a friendship with him over a
lifetime. But it was the group of Tanzanian and expatriate researchers working together at the
time to explore what they were calling non-colonial research methods who rst articulated the
concept of participatory research (Hall,1975,2005). Rajesh fell into what we both began calling
participatory research during the course of doing his eldwork with Indigenous farmers in
southern Rajasthan, also in the mid-1970s. He discovered that in spite of his elite level of educa-
tion at the best universities in India and the United States, the women and men of the villages in
Rajasthan were vastly more knowledgeable in every aspect of rural agricultural life than he was.
The two of us found others in Latin America, Europe, North America, and Asia who were
challenging the dominant research paradigms of the time, including Nina Wallerstein, Barbara
Israel, and Meredith Minkler from the health eld and John Gaventa, Peter Park, and John
Hurst from social movement elds in the United States. We were fortunate to have the organiza-
tional structure of the International Council for Adult Education to provide a home for the rst
International Participatory Research Network, a network that Rajesh coordinated for most of
the years between 1978 and 1992.
Why do we mention this? We mention this because in those days, nearly all of the support
for CBPR (and its many other names) came from outside the academy. The idea that knowledge
of persons living with HIV/AIDS, of women’s movements, of Indigenous peoples, of peas-
ant farmers in Brazil, and of the homeless could be recognized, valued, or drawn on to make
improvements in the lives of people was heretical. CBPR was not taught in universities back
AFTERWORD
BUDD HALL AND RAJESH TANDON
418 Afterword
then. When many of us were invited in those early days to give talks about these kinds
of ideas we were even shouted down. Our ideas were shared excitedly in the democracy
movements in the Philippines, South Africa, Nicaragua, and the Black and Latino com-
munities in the United States, but a book on CBPR for health could not have been pub-
lished at the time.
That was forty years ago. As a result of a refusal to separate the ideas of knowledge
and justice, evidence and passion, and the body and the world, particularly in the eld of
public health and health care, we have a third edition of a book that takes our collective
hopes that much further ahead. This book is a wonderful addition to the state of the eld
largely in the United States, although there are some global chapters. Yet, the knowledge
democracy movement is exploding around the world in ways that we could never have
imagined forty years ago. Our jointly shared UNESCO chair was created in 2012 to
support the building of capacity of CBPR in the Global South and the excluded North. We
work with many global networks of higher education institutions on issues of community-
university engagement, decolonization of higher education, knowledge democracy, and
the question of how to facilitate learning for a new generation of CBPR workers (Hall,
Tandon, & Tremblay,2015).
Challenges remain, many of which are touched on in the chapters of this book.
Inequality in the United States and in other parts of the world has grown dramatically
over the past forty years. This results in more health inequities for many more people.
Violence against women is a global threat ranging from the rape stories in India to the
campuses of elite universities of the United States and Canada. Indigenous peoples’ land
continues to be pillaged for resource extraction that benets only the very richest. Black
Lives Matter in the United States, Idle No More in Canada, the Latin American African
Descendants movement, and others illustrate the continued use of race to exclude and
marginalize. Sixty million people have been forced from their homes because of war and
violence and live precarious lives as refugees and outsiders.
We draw these matters to readers’ attention to underscore the importance of not only
multiplying and carrying on the kinds of work in CBPR shared in this book but also to
continue to deepen our understanding of how knowledge, organizing, speaking out, and
co-learning can contribute to healthy, just, sustainable, and joyful lives for each person in
this glorious, troubled, and perplexing world.
REFERENCES
Hall, B. L. (1975). Participatory research: An approach for change. Convergence, 8(2), 24–31.
Hall, B. L. (2005). From the cold? Reections on participatory research 1970–2005. Convergence, 38(1), 5–24.
Hall, B. L., Tandon, R., & Tremblay, C. (Eds.). (2015). Strengthening community-university research partnerships:
Global perspectives. Victoria, BC, Canada: University of Victoria.
INDEX
Page numbers in italics refer to illustrations.
A
AA. See Asian American communities
AAGA. See Arab American Grocers’
Association
Academic Researcher’s Guide for Pre-
and Post-Award Grants Management
When Conducting Community Engaged
Research, 119
Accountability for Cancer Care through
Undoing Racism and Equity (ACCURE)
benets of, 118
breast and lung cancer treatment outcome
measurements, 117
CBPR principles to prepare for resubmitting
application, 111
community and academic member balance
within, 119
early stage lung cancer treatment
rates and, 118
HEET sessions for, 113–114, 114, 118
intervention components of, 114
navigator job duties for, 114–115
post-award period of, 119
power and authority analysis, 112–113
racial gap in treatment narrowed by, 116
results and lessons learned, 116, 116–118
study design components of, 111–112
system change study of, 111–116
transparency intervention component, 112
vision of, 119
action research, 7, 19, 20
Action Research Network of the Americas, 20
active feminist research, 25
African-American communities, with
CBPR, 107–122
Agency of Health Care Research and Quality,
9, 78, 144
AI/AN. See American Indian/Alaska
Native tribe
Alaska Native communities, breast milk bio-
monitoring among, 220–221
Alegria, Margarita, 138
Alzheimer’s disease, 219
American Indian/Alaska Native (AI/AN)
tribe, 85, 204
CBPR principles and research ethics in,
207–214, 213
community voice of, 211
culture and, 212
health knowledge disparity in, 209
knowledge integration and action
within, 212
leadership within, 211–212
research idea discussion and, 210
research projects serving, 86
American Sign Language (ASL), 158
IRB and, 164
training skills of, 164
American Society for Thoracic Radiation
Oncology (ASTRO), 116
AMOS Health and Hope, 89, 91
CHW and staff training for, 260
community-driven priorities of, 261
context of, 260
lessons learned by, 261
participatory evaluation practiced by, 262
Participatory evaluation process
and, 260–261
partnership for, 261
T-PE approach of, 260
420 Index
antiracism
approaches for, 48–49
frameworks for, 49
training for, 108–109, 118–120
antiracism training, in Greensboro, CBPR
and, 108–109
Appadurai, Arjun, 311
Arab American Grocers’ Association
(AAGA), 297
Asian American communities (AA)
CBPR in, 175–185
CHW role in, 178
diversity of, 175
rst- and second-generation, 185
opportunities and future considerations
for, 184–185
small groups of, 184
ASL. See American Sign Language
ASTRO. See American Society for Thoracic
Radiation Oncology
Athi Water Services Board, 332
authority, ACCURE analysis of, 112–113
B
Balazs, C. L., 9
Banks, S., 228, 233
ban-the-box measure, 310
Baquero, Barbara, 236
Bardach, E., 282
Barnett, Steven, 139
Bayview Hunters Point neighborhood, 294
apple map data of, 295
no-smoking signs in, 295–296
Belmont Report, 216
principle implementation of, 217
Belone, Lorenda (NARCH scholar),
236, 266–267
benecence principle, Belmont
Report and, 217
Black Lives Matter, 306, 307
Black Panthers Party, 52
Boal, Augusto, 25
bounded empowerment, 99
Brody, Julia Green, 204
Bronx HealthREACH, 87, 88
Brown, Phil, 204
Burke, N., 285
Burt, R. S., 64
C
CAAA. See Detroit Community-
Academic Urban Research Center-afliated
Community Action Against Asthma
CAB. See community advisory board
Cacari-Stone, Lisa, 274, 295, 296, 302
The California Endowment/Policylink, 280
Camerer, C., 64
Cancer Care and Racial Equity Study
(CCARES), research ndings of, 110
cancer centers, as equal partners in system
change research for health equity, 110–111
cancer journey diagram, 113
cancer survival, racial disparities in, 107–108
Cazenave, N. A., 50, 56
CBOs. See community-based organizations
CBPR (community-based participatory
research)
antiracist and power-equalizing interven-
tions for, 48
application of, 3–4
authentic partnership within, 21
bridges built from, 274–275
case studies for, 52–55
communities wary of, 61
community-academic partnership
and, 132–133
as community driven, 9, 176–177
community representation in, 22
context, 245
core principles of, 7–8
cultural humility and, 24, 357–362
denition of, 32–35
differential consciousness and, 133
dominant cultural explanations
within, 24–25
as dynamic tool, 74, 133
Index
421
effectiveness of, 9–11
emancipatory approach of, 19
empirical rationale for, 238
empowerment strategies in, 10
engagement of, 138
equity and equanimity from, 133
evaluation measures and metrics, 238–239,
246–247, 369–374, 393–398, 399–404
federal and foundation funding for, 5,
315, 363–368
feminism, post-structuralism, and
postcolonialism dimensions of, 24–25
Freirian goals, 20, 25–26
GHDC approach of, 110–111
growth of, 4
health inequities addressed by, 31–32
historical traditions of, 19–20
humanity in, 26
human subject protection and, 204
(see also IRB)
immigrant communities and, 176–177
institutions leading, 20
IRB review of projects, 221–222
IRBs and, 21, 207, 210, 216–226, 227–228,
244, 310–311, 315
IRB training for communities, 379–384
“know-do” gap bridged by, 279, 279
knowledge democracy and, 22–23, 26
limits of, 26
listening-dialogue-reection
approach to, 25–26
manipulation of community by, 8–9
mapping, 323, 333, 334–335
mixed-method evaluation for, 6
model development of, 78
mutuality needed for, 132
new and continuing challenges and
opportunities for, 4–5
Northern tradition of, 18
participant interests and, 20
participation and, 20–21
pathways model of, 275
policy-focused efforts of, 278, 303
policy making link with, 280–283, 295–301
policy model of, 281
positivism critiques of, 22
potency of, 274
power and privilege in, 51
power relations and, 23–24
praxis, 211
problem-solving utilitarian of, 19
publications of, 5–6
race and diversity in, 45–47
racism exploration and, 48–49, 52, 57–58
racism reinscription in, 55–56
realist evaluation, 369–374
reciprocal capacity building and, 144
researcher and community relationship
within, 23–24
researcher team for, 18
respect for persons, 217
RSD and, 160–161
scientic rigor of, 6
Southern tradition of, 18
subgroup inclusion and, 208
support for, 5
systematic review of, 9
systemic processes of, 19
tensions embraced within, 133
term variations of, 7
three Rs for, 215–216, 216
training opportunities for, 271
transformative potential of, 216
tyrannies proposed of, 21
usage of, 77–78
utilitarian usage of, 6
visibility of, 12
CBPR, for health equity policy making,
277–292, 284
analysis tools for, 288–289, 405–410
electoral strategies, 287
legal actions, 286
policy principles, 283–284
power mapping, 405–410
strategy selection and, 285–286
studies and moratoriums, 286–287
422 Index
target identication and, 287
useful perception needed for, 277–278
voluntary agreements, 286
CBPR, in health care settings, 141–155
advancement of, 142–143
benets of, 154
continuing education credits, 150
CPIC, 150–155
DREAM Project, 153–154
engagement and, 145
evidence-based research and, 141
implementation of, 145–147
methodological challenges of, 145
patient-centered research and, 141–142
PCORI, 152–153
principles of, 143–144
recommendations for, 154
research partnerships and, 145
shared analysis, interpretation, and dissemi-
nation of results, 149–150
study designs pros and cons, 146–148
training and resource manuals for,
149–150
vignettes for, 150–155
CBPR, realist review of, 237, 369–374
CBPR, with African-American communities,
107–122
CBPR, with American Indian/Alaska Native
communities, 107–120
CBPR, with Asian American commu-
nities, 175–185
case studies for, 177–183
opportunities and future considerations
for, 184–185
relevance of, 176–177
CBPR, with Deaf communities
CCA and, 165–166
common values found within, 166
cultivate relationships within, 166
diversity among, 158
early experiences and, 158
health surveys for, 161
historical events relevant to, 170–171
intervention development for, 161–162
introduction to, 157–158
lessons learned for, 166–168
online resources related to, 168–170
recognize strengths of, 167–168
research designs for, 161–162
shared ownership with, 166
CBPR, with Latino communities, 50, 52–53,
123–134, 189–200, 268–269, 280, 305,
307, 312, 315–316, 350
CBPR conceptual model, 80, 237–238,
280–281
academic literature and research on,
78–79
adapting and expanding of, 89–91
CBPR model visioning guide, 91, 246–247
characteristic variability within, 85
context domain of, 81, 81
creation of, 78–84
dynamic characteristics of, 79, 89
evaluation measures, 393–398
focus group research for, 84–86
intervention and research domain of, 81,
83, 83
material structural pathway for, 88
ongoing collective reection of, 79
outcome domain of, 81, 83–84, 83
partnership capacity pathway for, 88
partnership process domain of,
81–82, 82
partnership river of life/historical time-
line, 375–378
scientic methodology and research
design of, 210
self-created plans of, 89–91
successful outcome processes of, 89
testing and strengthening of, 84–88, 87
as visioning and planning tool, 91
CBPR/E. See community-based participatory
research and evaluation
CBPR ethics
beyond IRB regulations, 203–204,
216, 217–218
democratizing, 215–223
tension with, 223
CBPR evaluation measures, 246–247,
369–374, 393–398, 399–404
Index
423
CBPR facilitation tools
CBPR model visioning guide, 91, 246–247
partnership river of life, 375–378
CBPR life cycle
community protocol honor and, 229–230
conclusion on, 232–233
ethics and, 227–228
exchange plan and, 231
governance as stewardship, 229–230
groundwork for, 228–229
project implementation, 230–231
PRs and, 230–231
work sharing and ending of, 231–232
CBPR logic model, 237
CBPR principles, 31, 41, 142
American Indian/Alaska Native, 207–214
building on community strengths and
resources, 32, 143
disseminating ndings and knowledge,
34, 144, 211
embracing cultural humility, 34–35, 144
emphasizing public health problems/deter-
minants of health and disease, 33, 144
facilitating partnership in research and
power-sharing, 33, 143
integrating and achieving balance between
research and action, 33, 143
International Collaboration for Participatory
Health Research, 351–356
involving system development, 34, 144
Latino border communities, 350
LGBT, 345–350
partnership formal agreements, 385–392
promoting co-learning and capacity
building, 33, 143
recognizing community as unit of
identity, 32, 143
requiring long-term process and sustainabil-
ity, 34, 144
CBPR principles issues
alignment and misalignment, 123–140
“community” dened by each partner-
ship, 35–36
continual evaluation of principles, 41
creating collaborative and equitable, 36–37
culture and, 208–209
establishing dissemination
procedures, 38–39
ethics during application of, 210–211
limitations of principles to dictate research
design, 40
matching principles to partnerships, 35
partnership participation, 37–38
partnership size appropriate for
community, 39–40
power and privilege, 337–344
recognizing value priorities of
community, 38
working with cultural diversity of
partners, 39
CBPR processes, 281, 282
CBPR racism inscription, 55
community capacity building, 56
equitable distribution of funding, 56–57
researcher identity and positionality,
57–58
scholars of color and, 57
CBPR socio-ecologic framework
adapting and expanding model, 89–91
creating model, 78–84
testing and strengthening model, 84–88
CBPR trust development
building behaviors for, 62
foundation of, 61
limitation of, 62
as outcome, 62
study background for, 62–63
CCA. See culture-centered approach
CCARES. See Cancer Care and Racial
Equity Study
CCC. See Community Capacitation Center
CCISCO. See Contra Costa Interfaith Sup-
porting Community Organization
CDC. See Centers for Disease Control and
Prevention
CE. See community engagement
CeaseFire program, police involved
with, 308–309
CEDAPS. See Center for Health Promotion
CEnR. See community-engaged research
424 Index
Center for Health Promotion (CEDAPS), 276,
323, 335n1–3
government involvement crucial
needed for, 327
lessons from mapping, 326–327
local leaders needed for, 327
location-specic approaches to, 326–327
methodology, 324–325
technical partners and back-up plans
required for, 328
tensions and delays caused in, 327
Center for Participatory Research at the
University of New Mexico (UNM-CPR),
team reections of, 54–55
Center for the Study of Asian American
Health (CSAAH), 139
action commitment and, 178–179
asset-based approach of, 179–180
equity promoted in partnerships of,
178
internal structures building sustainabil-
ity, 180–181
multi-sectorial approach of, 179
phase 1 of, 177
phase 2 of, 179
principles guiding, 177
social determinants of health per-
spective, 179
Centers for Disease Control and Prevention
(CDC), 5, 86, 190
Centro de Promoção da Saúde (CEDAPS).
See Center for Health Promotion
CEP. See community engagement planning
CERI. See community engagement in
research index
CES. See community engagement survey
CEW. See Oregon Community Education
Worker Program
“Charging and Sentencing Policy” (Justice
Department), 308
CHCC. See Cone Health Cancer Center
ChiCAS intervention, 195
Chinese Progressive Association of San
Francisco (CPA), 181–183
Chouinard, J. A., 252
CHSP. See Community Health
Scholars Program
CHW. See community health worker
City University of New York (CUNY), 311
civic engagement, 282
Civil Rights Act of 1964, 108
civil rights movement
environmental movement and, 124
US health care racial barriers eradi-
cated by, 107
clinical performance reports (CPRs), race-
specic, 115–116
Clinical Translational Science Awards
(CTSAs), 5
Cochran Collaborative Review, 150
codes, development of, 25
Collaborative Action Research Group, 20
collaborative utilization-focused research, 18
collateral consequences, 307
Commission on Social Justice for the San
Francisco Archdiocese, 12
Common Rule, regarding human subjects
research, 207–208
communication, community capacity building
and, 163–164
communication issues
hidden transcripts, 23–24
translating culture, 245
Communities United for Police Reform
(CPR), 313
community
dening of, 36
engagement of, 205
IRBs represented by, 222–223
partnership dening, 35–36
real-time data use by, 262
representation of, 36
research relationship of, 19–20
strengths and resources within, 32
tribal IRBs and, 222–223
as unit of identity, 32, 210
value priorities identied by, 38–39
voice of, 211
Index
425
community-academic partnership,
61, 238, 246
humility within, 132–133
Community-Academic Research Network,
40
community advisory board (CAB),
152
community-based organizations (CBOs),
153, 257, 321
community-based participatory
research. See CBPR
community-based participatory research and
evaluation (CBPR/E), 258
Community Benets District, 296
Community-Campus Partnerships for
Health, 89
Community Capacitation Center (CCC)
year 1 evaluation proposal, 258
year 2 evaluation, 259
community capacity building,
56–57, 256, 302
CBPR, 144
communication and, 163–164
LRA and, 56
RPRC/NCDHR and, 163–164
Tenderloin Healthy Corner Store
Coalition, 301
community consent, 221
community empowerment, 211
community-engaged research
(CEnR), 5, 8, 61
effectiveness of, 9–11
race and diversity in, 45–47
community engagement (CE), 238
interviews for measurement of, 239
partnerships inuenced by, 239
community engagement continuum,
7–8, 137–138
Community Engagement Core of the
University of New Mexico, 8
community engagement in research index
(CERI), 22
models for activities in, 239
community engagement planning (CEP), 151
community engagement survey (CES), 240
culture-centeredness and, 243
partnership context domain for, 242
partnership dynamics domain for, 243
partnership outcomes, 243
Community Health Scholars Program
(CHSP), 3, 267–268
scholar and contribution of, 269–270
community health worker (CHW),
153, 176, 236
in AA communities, 178
AMOS Health and Hope training, 260
community involvement in research, 239
community-partnered participatory research
(CPPR), 151
Community Partners in Care (CPIC),
138, 150–151
data analysis and, 149
Community Strategies for Sustainability and
Justice (CSSJ), 53
Cone Health Cancer Center (CHCC), 110
condentiality, IRB and, 217–218
consensus rule, 37
consent requirements, 210
community, 221
Contra Costa Interfaith Supporting
Community Organization (CCISCO),
309
Cooke, B., 21
coproducing knowledge, 138
Corburn, Jason, 276
Cornwall, A., 4, 23
“The Counted,” 308
Cousins, J. B., 252
covert racism, 50
CPA. See Chinese Progressive Association of
San Francisco
CPIC. See Community Partners in Care
CPPR. See community-partnered
participatory research
CPR. See Communities United for
Police Reform
CPRs. See clinical performance reports
CR. See critical-reective trust
426 Index
criminal justice reform, 275
broader public health approach
for, 307–308
collateral consequences and, 307
efforts for, 315
focus groups on, 315–316
lessons learned on, 316–317
through PAR, 305–317
racial disparities within, 305–306
critical consciousness, 25, 129
critical reection, 166
critical-reective (CR) trust, 63, 64–65
partnerships in, 64
CSAAH. See Center for the Study of Asian
American Health
CSSJ. See Community Strategies for Sustain-
ability and Justice
CTSAs. See Clinical Translational
Science Awards
cultural humility, 24, 210, 284–285, 357–362
CBPR principles and, 34–35
cultural translation, 54
culture
CBPR principles issues and, 208–209
health behaviors affected by, 209
health understanding and, 209
as multidimensional, 208–209
culture-centered approach (CCA), 22,
89, 138, 243
culture-centeredness, 89, 138, 243
CBPR praxis and, 211
measurement of, 245
as partnership project development, 245
research beneting from, 208
culture-centeredness approach (CCA), Deaf
communities and, 165–166
CUNY. See City University of New York
Cyril, S., 9
D
Deaf communities. See also CBPR, with Deaf
communities
CCA and, 165–166
common values found within, 166
cultivate relationships within, 166
diversity among, 158
early experiences and, 158
health surveys for, 161
intervention development for, 161–162
introduction to, 157–158
lessons learned for, 166–168
other language minority populations
compared to, 158–160
recognize strengths of, 167–168
research designs for, 161–162
shared ownership with, 166
Deaf Health Community Committee
(DHCC), 167
Deaf moms and infant care project, 167
Deaf Weight Wise (DWW), 161
consent signature form, 165
delayed-start design of, 162
inclusion criteria used by, 164
informed consent information for, 162
intervention, 162
Deaf Wellness Center (DWC), 164
de Las Nueces, D., 10
Department of Children, Youth, and Their
Families (San Francisco), 103
Detroit Community-Academic Urban
Research Center (Detroit URC),
32, 35, 42n1
collaborative, equitable partner-
ship of, 36–37
consensus rule and, 37
equitable distribution of resources, 37
membership criteria for, 40
shared inuence and equity of, 37
Detroit Community-Academic Urban
Research Center-afliated Community
Action Against Asthma (CAAA), 38, 39
Detroit URC. See Detroit Community-
Academic Urban Research Center
Deutsch, M., 67
Deveaux, M., 23
Devia, C., 285
deVuono-Powell, Saneta, 275, 305, 309, 318
Index
427
Diabetes, Research, Education, and Action
for Minorities (DREAM) Project, 153–154
differential consciousness, 133
disease determinant, 33
dissemination process, 34
procedure establishment, 38–39
distributive justice, 283–284
Drahota, A., 10
DREAM Coalition, 178
DREAM Project. See Diabetes, Research,
Education, and Action for Minor-
ities Project
Dream Teens, 102
Dressler, W. W., 208
Duran, Bonnie, 24, 78, 84, 244, 247
Dutta, Mohan J., 22, 138
DWC. See Deaf Wellness Center
DWW. See Deaf Weight Wise
E
East Side Village Health Worker Partner-
ship, 37–40
“Effectiveness of DECIDE in Patient-
Provider Communication, Therapeutic
Alliance & Care Continuation,” 152
EHC. See Environmental Health Coalition
Eikeland, O., 228
EJ. See environmental justice
electronic medical record (EMR), 115
Elwood, W. N., 208
empowerment
benets of, 253
evaluation and, 252
EMR. See electronic medical record
Eng, Eugenia (Geni), 109, 111
ENGAGED for CHANGE, 191, 192
intervention development and, 189
strategy for, 139–140
“Engage for Equity study,” 89, 394
environmental activism
civil rights movement and, 124
racism and, 125
social class interest in, 125
in SV, 125–126
Environmental Health Coalition (EHC), 280
environmental health research
biomedical-driven, 220
chemical exposure reporting and, 218–220
reporting-back process, 220
study participants right to know, 218–220
environmentalism, 125, 131
environmental justice (EJ), 48, 274
divergent tactics for, 129–130
Environmental Protection Agency, US, 9
epistemicide, 22
epistemology, 259
equity lens, 285
Espino, S. L. R., 20
ethics. See also research ethics
CBPR life cycle and, 227–228
democratizing oversight of, 221–222
ethnic enclaves, 176
ethnicity, racism and, 49
evaluation
empowerment and, 252
as political, 252
research compared to, 252
on specic program, 252
evidenced-based research, 141
exchange plan, 231
F
faculty of color, academic positions for,
236, 265–271
CBPR approach of, 270–271
KHSP and CHSP, 267–270
NARCH, 266–267
faith-based organizations (FBOs), 153
Fals-Borda, Orlando, 20
Family Listening/Circle Program
(FL/CP), 267
Farley, T. A., 293
Feagin, 49
feminism theory, CBPR dimensions of, 24–25
Fernandes, Walter, 253
Feuerstein, M. T., 256
Fine, M., 25
FJLs. See food justice leaders
428 Index
FL/CP. See Family Listening/Circle Program
Flicker, Sarah, 204
Floyd v. City of New York, 312
food insecurity, description of prob-
lem, 293–294
food justice leaders (FJLs), 275, 294
HRSF and, 299
store relationship with, 298, 302
Tenderloin Healthy Corner Store Coalition
and, 296–297
food stamps, 300
“food swamps,” 286
formal agreements, 65
Foucault, M., on power relations, 23
Frankfurt School theorists, 253
Freire, Paulo, 10, 79, 253
praxis and, 25–26
on reality, 19–20
functional trust, 63
partnerships and, 65–66
funding, equitable distribution of, 56–57
funding, U.S. government and founda-
tions, 358–363
equitable distribution of, 56–57
G
Gaventa, John, 23, 253
geographic information system
(GIS), 282, 321
George, S. M., 208
“Get Ready for Equity” (Burke), 285
GHDC. See Greensboro Health Disparities
Collaborative
Gibbs, Lisa, 89
GIS. See geographic information system
global health policy, 321–336
Global South, 253
challenges and opportunities for, 333–335
community-driven mapping of, 321–322
Nairobi/Kenya mapping case
study, 328–334
Rio de Janiero case study, 321–328
Google Earth, 329
Google Maps, 276, 295, 332
governance, as stewardship, 229–230
Green, L. W., 4, 363–368
Greensboro Health Disparities Collaborative
(GHDC), 75
antiracism training in, 108–109, 118–120
cancer journey diagram by, 113
CBPR approach by, 110–111
vision of, 119
grid of resources for intervention
development (GRID), 191
Grifth, Derek M. (CHSP and KHSP
contributor), 236, 269–270
Guta, Adrian, 204
H
HAAF. See Healthy African
American Families
Habermas, J., 20–21, 21
Hall, Budd, 3
Harvard University, 274
Havasupai Diabetes Study,
208
Hawthorne Community Education
Center, 247
HC. See health committee
Healing Home, 232
Healing of the Canoe, 87
health care equity education and training
(HEET), 111, 113–114, 114
health care settings. See CBPR, in health
care settings
health committee (HC), 261
health disparities research, 18
health equity, cancer centers as equal partners
in system change research for, 110–111
Health Equity Summit (2013), 301
health inequities, distribution of,
47
health outcomes, 10
Healthy African American Families
(HAAF), 150
Healthy Environments Partnership, 38
Index
429
healthy policy making, 321
HealthyRetail SF (HRSF) model, 298
FJLs and, 299
implementation of, 299
heath care settings, CBPR in, 141–155,
143–144
HEET. See health care equity education
and training
hidden transcripts, 23
Highlander School for Research and
Education, 253
HIV prevention, youth leadership for, 230
HOLA group, logic model from,
196, 197–198
Horton, Myles, 253
HPV. See human papillomavirus screening
HRSF. See HealthyRetail SF model
human papillomavirus (HPV) screening, 209
Hyde, Cheryl A., 38
I
ICPHR. See International Collaboration for
Participatory Health Research
IHS. See Indian Health Service
IMF. See International Monetary Fund
Immigrant and Refugee Community Organi-
zation (IRCO), 258
immigrant communities, CBPRs and, 176–
178, 180–181, 415
Improving Children’s Lives Initiative, 103
Indian Health Service (IHS), 5, 207, 220, 265
indigenous research, IRB challenges related
to, 220–221
Indigenous Rights Protection Act, 221
Indigenous-transformative paradigm, 85, 245
Individual Burden of Illness Index for
Depression, 142
inequality, 19
“Insider/Outsider: Our Ascribed and
Achieved Identities as Researchers”
UNM-CPR, 54
InSTEDD, 324
Institute of Medicine (IOM), 5, 109, 265
institutional racism, 75, 107
institutional review board (IRB), 21,
112, 207–233
of ASL, 164
breast milk biomonitoring among Alaska
Native communities, 220–221
CBPR ethics beyond, 203–204,
216, 217–218
of CBPR projects, 221–222
challenges and obstacles created by, 218
community representation and, 222–223
community training, 379–384
condentiality and, 217–218
conicts of interest and, 222
indigenous research and, 220–221
NIH rules for, 222
protocol review of, 221
situations addressed by, 222
tribal, 220, 222–223
university, 221
internal validity, 252
International Collaboration for Participatory
Health Research (ICPHR), 103, 351–356
International Council for Adult Education, 20
International Monetary Funds (IMF), 260
International Participatory Research
Network, 20
Internet surveys, 236
intervention development
activity and material pretest, 196, 199
CBPR partnerships experience
with, 190–191
community needs, priorities, and asset
assessment, 193–194
conceptual or logic model design, 196
craft activities and materials, 196
evolution of, 191
intervention team establishment and, 193
lack of, 189
literature and data gathering, 193
pilot test administering, 199
pilot test feedback, 199
pilot test implementation process, 199
430 Index
priority generation and renement, 195–196
success of, 199–200
theory evaluation and incorpora-
tion, 195–196
intervention team, 193
IOM. See Institute of Medicine
IRB. See institutional review board
IRCO. See Immigrant and Refugee
Community Organization
Islam, Nadia, 139
Israel, Barbara, 7, 32–41, 79, 229, 334
J
Jagosh, Justin, 10, 238, 369–374
jails. See prisons and jails
Jewkes, R., 4
Jones, Camara, 49, 285
Journal of Health Care for the Poor and
Underserved, 315
Journal of Urban Health, 315
Justice Department, 308
justice principle, Belmont Report and, 217
K
Kagawa-Singer, M., 208, 209
Kalusugan Coalition, 179
Kastelic, Sarah, 84–85
KBT. See knowledge-based trust
Kellogg Health Scholars Program
(KHSP), 267
scholar and contribution of, 268–270
key informant survey (KIS), 240
project descriptive measures, 242
key outcomes
conceptualizing, 243–244
promising practices, 244–245
KHSP. See Kellogg Health Scholars Program
KHSP scholar, 236, 268–269
Kids in Action network (ICPHR), 103
Kingdon, J. W., 275, 282, 295, 302
KIS. See key informant survey
“know-do” gap, 279
CBPR bridging, 279
knowledge, co-producing, 138
knowledge-based trust (KBT), 66
knowledge democracy, 22–23, 26
power relations and, 23
Kothari, U., 21
Krieger, N., 309
Kwon, S. C., 176
L
Labor Occupational Health Program, UC
Berkeley, 181–183
Latin America, T-PE in, 253
Latina transgender women, photovoice
project for, 194, 194–195
Latino communities
intervention development case study
in, 190–200
partnership development within, 190–200
lesbian, gay, bisexual, and transgender
(LGBT), 190, 345–350
Lewin, Kurt, 19
LGBT. See lesbian, gay, bisexual, and
transgender
Library of Medicine, 9
linguistic racial accommodation (LRA),
49, 50–51, 56
listening-dialogue-action-reection approach,
25. See also Freire, Paulo
Longest, B. B., Jr., 282
long-term process, of CBPR, 34
LRA. See linguistic racial accommodation
Lucero, Julie E., 46, 85
M
macro-contextual factors, 282
majority rule, 37
Manning, Matthew, 116, 118
Mapeamento Digital Liderado por
Adolescentes e Jovens (Youth-Led Digital
Mapping), 323
mapping, 100
CBPR, 323, 333, 334–335
CEDAPS lessons, 326–327
community health concerns and, 334
democratic process of, 322
Index
431
new technologies for, 333
partnerships for, 333
place and, 322
relational view of, 322–323
Rio de Janeiro case study and, 323–326
social capital bonding and bridging, 334
MapServer, 332
Markow, Therese Ann, 207
Massachusetts General Hospital, 138, 152
mass incarceration. See also prisons and jails
harsher sentencing laws and, 306
public health and, 306–307
rehabilitative failures for, 306–307
Mathare collaboration, 328
sanitation and women’s health, 331
Mathare Zonal Plan, 331–332
Mayo Clinic, 247
McTaggart, R., 26
memoranda of understanding (MOU),
37, 286
Men on the Move, 87
men who have sex with men (MSM),
140, 190, 195
methodology
CBPR, in health care settings, chal-
lenges of, 145
CBPR conceptual model and, 210
CEDAPS, 324–325
decolonizing, 254
for Rio de Janeiro mapping case
study, 323–325
“Methodology 101 Training Booklet and
Resource Guide” (PCORI), 149
microaggression, 50
in partnership, 53–54
in WOEIP, 53–54
micro-insults, 50
micro-invalidation, 50
Mindful Eating Group, 164
Minkler, Meredith, 4, 8, 38, 95, 144, 181,
183, 274, 280, 283, 302
MJP. See Morris Justice Project
model minority myth, 176
Moriarty, Pia, 12
Morrello-Frosch, Rachel, 9, 204
Morris Justice Project (MJP), 286, 311–315
back-pocket reports by, 312
employment and development of, 312
equity, health and safety, 316
formation of, 311
judge’s community advisory board and, 314
poster made by, 313
process of, 311
role of, 312–313
sidewalk science of, 312
Moses Cone Memorial Hospital, 108
Moses Cone-Wesley Long Community
Health Foundation, 109
MOU. See memoranda of understanding
MSM. See men who have sex with men
multidirectional learning, 77
Murray-Garcia, J., 34
N
Nagar, R., 24
Nairobi, Kenya mapping case study,
328–334, 329
collaborative analysis and policy
for, 331–332
community mobilization, 330–331
potential displacement, 330
sanitation and women’s health, 331
visible images of, 329–330
NARCH. See Native American Research
Centers for Health
National Academy of Sciences, 219, 285
National Cancer Institute, 86
National Center for Deaf Health Research
(NCDHR), 139, 157
capacity building, 163–164
growth of, 164
National Center for Minority Health and
Health Disparities (NCMHD), 62, 177
National Congress of American Indians
Policy Research Center (NCAI PRC), 84
policy making mission of, 85
432 Index
National Environment Management Author-
ity, Kenyan (NEMA), 329
National Indian Child Welfare Association
(NICWA), 89
National Institute of Environmental Health
Science (NIEHS), 5, 123–124
National Institute of Mental Health Affective
Disorders Work Group, 142
National Institute of Minority Health and
Health Disparities (NIMHD), 5, 78
National Institute of Nursing Research
(NINR), 89
National Institutes of Health (NIH), 5, 108, 222
National Research Center for Excellence
in Asian American Communities, creat-
ing and sustaining multiple partnerships
within, 177–178
National Secretary of Health, 102
National Technical Institute for the Deaf
(NTID), 160
National Youth Service (NYS), 332
Native American Research Centers for Health
(NARCH), 5, 62, 84, 265
indigenous scholar’s contribution to, 266–267
purpose and funding of, 266
Native American Youth and Family
Association (NAYA), 258
Native Hawaiian and Pacic Islanders
(NHPIs), 175
NAYA. See Native American Youth and
Family Association
NCAI PRC. See National Congress of
American Indians Policy Research Center
NCDHR. See National Center for Deaf
Health Research
NCMHD. See National Center for Minority
Health and Health Disparities
NEMA. See National Environment
Management Authority, Kenyan
neutral trust, 63
partnership and, 66
New York Police Department (NYPD), 311
police stops dropping, 314–315
quotas needed by, 312
stop-and-frisk by, 315
NHPIs. See Native Hawaiian and
Pacic Islanders
Nicaragua, 252
NIEHS. See National Institute of Environ-
mental Health Science
NIH. See National Institutes of Health
NIMHD. See National Institute of Minority
Health and Health Disparities
North American Primary Care Group, 5
Northern tradition, of CBPR, 18
Northington-Gamble, V., 278
NTID. See National Technical Institute
for the Deaf
NYPD. See New York Police Department
NYS. See National Youth Service
O
objects of study, 19
OBSSR. See Ofce of Behavioral and Social
Science Research
Oetzel, John G., 18, 37, 88, 229,
236, 243, 246
OEWD. See Ofce of Economic and Work-
force Development
Ofce of Behavioral and Social Science
Research (OBSSR), 5
Ofce of Childhood and Adolescence, 102
Ofce of Economic and Workforce
Development (OEWD), 297
Ofce of Neighborhood Safety
(Richmond), 309
Old Town National City (OTNC), 280
ontology, 259
Open Notes project, 220
OpenStreetMap, 332
oppression, systemic racism and, 49–50
Oregon Community Education Worker
Program (CEW)
background and lead partners for,
257–258
context of, 258
deepening participatory process, 259–260
T-PE initial steps, 258–259
OTNC. See Old Town National City
Ozer, Emily J., 97
Index
433
P
Pacic Institute (PI), 52
Panteli, N., 65
PAR. See participatory action research
Parajón, Gustavo, 260
Parajón, L. C., 251–264
Park, A. N., 9
Parker, Myra, 204
Parsons, Talcott, 19
participation, Venn diagram approach to, 40
participatory action research (PAR),
7, 20, 275
authenticity of, 21
criminal justice reform through, 305–317
participatory evaluation, 251
application of ndings, 257
contextual factors of, 254
data collection and, 256
decolonizing, 253–254
development of, 259–260
feedback and interpretation, 257
key steps in, 255
power and, 253
progress tracking, 256
as range of collaborative
approaches, 252–253
results communication, 257
subject and topic agreement with, 256
team building for, 255–256
participatory evaluation team
capacity building, 255
core team for, 255
relationship constituencies, 255
roles and multiple mechanisms
for, 255–256
participatory research context, 282
participatory starting points, 181–182, 186
Partnered Research Center for Quality Care
(PRC), 238
partnership
agreements, 385–393
best practices chosen by, 235–236
CBPR principles applicable to, 35
CE inuencing, 239
community-academic, 61
“community” dened by, 35–36
consensus rule compared to
majority rule, 37
in CR trust, 64
cultural diversity within, 39
culture-centeredness development and,
245
deductive approach to, 246–247
diversity of, 39
equitable and collaborative, 33
expansion of, in intervention
development, 191–193
functional trust and, 65–66
high-functioning, 73–74
for mapping, 333
microaggression in, 53–54
neutral trust and, 66
proxy trust and, 65
structures of, 244
Partnership Evaluation Study (PES), 238
logic model development for, 239
The Partnership Project (TPP), 108
partnership synergy
as middle-range theory, 238
study of, 238–239
Patient Centered Outcomes Research Institute
(PCORI), 5, 142, 149, 152
Patient Protection and Affordable
Care Act, 77
Payne-Sturges, D., 9
PCORI. See Patient Centered Outcomes
Research Institute
peer researchers (PRs), 230–231
power sharing and, 231
women’s CBR study and, 231
People of Color Summit of Environmental
Justice, 125
People’s Institute for Survival and Beyond
(PISAB), 108
racial analysis by, 109
PES. See Partnership Evaluation Study
Photovoice project, 194, 194–195
PI. See Pacic Institute; principal investigator
PISAB. See People’s Institute for Survival
and Beyond
434 Index
place
contingent and contested characteris-
tics of, 323
distance in relation to, 322
mapping and, 322
relational view on, 322–323
police
aggressive, 306, 316
brutality, 308
CeaseFire program and, 308–309
policy making
academic research and, 278–279
CBPR link between, 280–283, 295–301
formation stage, 282–283
knowledge transmission and, 278
research before attempting, 302
three streams in, 295
policy stream, 295
opportunity window and, 298–299
politics stream, 295
advocacy contributions and,
296–297
postcolonialism theory, CBPR
dimension of, 24–25
post-structuralism theory, CBPR
dimension of, 24–25
power
ACCURE analysis of, 112–113
analysis of, 288
in CBPR, 51
contextual factors, 254
participatory evaluation and, 253
privilege and, 51
repressive, 23
UNM-CPR reections on, 54–55
of youth voices, 301
power mapping, 288
power relations
CBPR and, 23–24
Foucault on, 23
knowledge democracy and, 23
power sharing, 33
of adults and youth, 97–98
PRs and, 231
practical participatory evaluation (P-PE),
252
praxis, Freire and, 25–26
PRC. See Partnered Research Center for
Quality Care
Prevention Institute, 316
Prewitt, K., 278
principal investigator (PI), 126, 240
discredited knowledge of, 129, 130
prisons and jails, overcrowding of,
305–306
privilege
in CBPR, 51
power and, 51
problem stream, grassroots coalition
creation, 295–296
procedural justice, 283–284
program improvement, 252
Progress in Community Health Part-
nerships, 62
Progressive Workers Alliance (PWA), 183
Project CHARGE, 178
proxy mistrust, 65
proxy trust, 63
partnerships and, 65
PRs. See peer researchers
Psyhinfo, 95
public health, mass incarceration
and, 306–307
public housing, police and, 307
Public Laboratory for Open Technology and
Science, 325
Public Science Project (CUNY),
102–103, 312
public transcripts, 23
Pullman Porters’ Union, 52
PWA. See Progressive Workers Alliance
Q
qualitative data, 39
interview guides for, 241
measures and tools for, 240–241
quantitative outcomes, 244
Quinn, S. C., 8
Index
435
R
Racial Equity Institute (REI), 109
racism, 4, 8–9, 107–120, 307, 309, 316
beyond and within, 51
CBPR exploration and, 48–49, 52, 57–58
CBPR reinscription of, 55–56
covert, 50
cumulative effect of, 47–48
environmental movement and, 123,
125, 127, 130
ethnicity and, 49
recognition of, 51
systemic, 49–50, 56
unconscious, 48, 52
understanding of, 49
UNM-CPR reections on, 54–55
whites beneting from, 48–49
racism framework
covert and microaggression, 50
LRA, 50–51
three-tiered, Camara Jones, 49
white racial, 49–50
Rahman, M. A., 254
randomized control trial (RCT),
111, 153, 211
RDHTF. See Rochester Deaf Health
Task Force
reach, 215, 216
“Ready for Kindergarten (R4K) Collabo-
rative,” 257
reality, Freire on, 19–20
Reentry Success Center, 310
reexivity, 17, 52, 132–133, 246–247,
354, 375–378
REI. See Racial Equity Institute
relationships, 244
with constituencies, 256
relevance, 215, 216
RePORTER, 242
reporting back, guidelines for, 219
repressive power, 23
research, evaluation compared to, 252
Researchers for Fair Policing (RFP), 314
research ethics, issues regarding, 207
Research for Improved Health (RIH), 63,
68–69, 236
case studies, 86–87
CES and, 242–243
cross-sectional survey for, 240
data collection elements, 240
evaluation measures and tools,
246–247, 394–395
ndings organized by, 243
historical development interview for, 241–242
instruments for, 247
interviews for, 241–242
key outcomes for, 87–88, 243–244
KIS for, 242
measures, 394–395
planning tool for, 246
quantitative outcomes, 87–88, 244
sampling frame for, 85–87, 240
structure and governance for, 245–246
study methods of, 84–86, 239–240
workshop and we-based tools for, 247–248
“Research for Improved Health: A Study of
Community-Academic Partnerships” (RIH),
77–94, 237–250
research-intervention, 244
respect for persons principle
Belmont Report and, 217
CBPR and, 217
RFP. See Researchers for Fair Policing
Rhodes, Scott D., 139
Rifkin, S., 22
rigor, 215, 216
RIH. See Research for Improved Health;
“Research for Improved Health: A Study of
Community-Academic Partnerships”
Rio de Janeiro mapping case study, 324, 326
lessons learned from, 326–328
methodologies for, 323–325
success of, 325–326
RIT. See Rochester Institute of Technology
Rochester Community Health Part-
nership, 247
Rochester Deaf Health Task Force
(RDHTF), 161
436 Index
Rochester Healthy Community Partnership,
Minnesota, 89
Rochester Institute of Technology (RIT), 160
Rochester Prevention Research Center
(RPRC), 157
capacity building, 163–164
growth of, 164
logo communication aid for, 162–163, 163
Rochester School for the Deaf (RSD), CBPR
and, 160–161
role-based trust, 63, 66–67
role-play, 411–416
Roth, N. L., 65
Rousseau, D. M., 64
RPRC. See Rochester Prevention
Research Center
RSD. See Rochester School for the Deaf
S
Safe Return Project (SR), 309–311, 316–317
ban-the-box measure and, 310
effective work of, 311
goal of, 309
interview training for, 310
organizational partners for, 309–310
policy and political stage of, 310
Sandoval, C., 124
The San Francisco Chinatown Restaurant
Worker Health and Safety Study, 180–181
CBPR principle application and adapta-
tions, 182–183
co-learning opportunities for, 182
participatory starting points of, 181–182
policy and community capacity out-
comes and, 183
research context of, 181
setting and partnership of, 181
worker leadership development
and, 182–183
sanitation, women’s health and, 331
scaling up, 26
Schwandt, T. A., 278
SDI. See Shack/Slum Dwellers International
Seifer, S. D., 9
self-assessment, 247
SEM. See structural equation model
Sessions, Jeff, 305
Shack/Slum Dwellers International (SDI),
Mathare collaboration and, 328
Shapiro, S. P., 65
Shonkoff, J. P., 278
Shor, Ira, 26
sidewalk science, 275, 312
Simkins, George, Jr., 108
Simkins v. Cone Health, 108
Sirin, S., 25
Sisters Network Greensboro (SNG), 111
cancer journey diagram by, 113
Sitkin, S. B., 64, 65
Smith, Linda Tuhiwai, 254
SNG. See Sisters Network Greensboro
Snow, John, 321
social ecology, of research use, 278–279
social trauma, 309
Social Venture Partners (SVP), 258
Sockalingam, S., 65
Southeast Food Access (SEFA), 294, 302
Southern tradition, of CBPR, 18
South Valley (SV)
community resilience in, 131–132
critical consciousness and, 129
political advocacy within, 128–129
sociocultural relations and environmental
activism in, 125–126
sociopolitical history of, 125–126
South Valley Partners for Environmental
Justice (SVPEJ), 75, 87
community PI discredited, 129, 130
divergent tactics for EJ, 129–130
divergent worldviews of, 127–129
funding for, 123–124
goals of, 126
lessons learned from, 132–133
linearity lacking, 130
methods of, 126–127
misalignment of, 126
partners of, 126
policy goal challenges, 124
Index
437
power asymmetries within, 131
ruptures in ways of knowing, 130–131
status-quo reinforced by, 131
tensions and fractures within, 127–132
Speaking Truth on Coming Home, 310
SR. See Safe Return Project
stewardship, 203–204
Stone, D., 278
stop-and-frisk policy, 286, 315
Straf, M. L., 278
Strategies to Reach and Implement the
Vision of Health Equity (STRIVE)
program, 179
structural equation model (SEM), 87
study participant protection
oversight of, 216–218
results uncertainty and, 218–220
right to know, 218–220
suicide, 307
Sullivan Commission, 107
SurveyMonkey, 101
surveys
CES, 240, 242
health, 161
KIS, 240, 242
sustainability, 34
SV. See South Valley
SVP. See Social Venture Partners
SVPEJ. See South Valley Partners for
Environmental Justice
Swarr, A., 24
Sykes, R., 293
systemic racism, 56
oppression and, 49–50
systems development, 34
T
Taking Action! Building Aboriginal Youth
Leadership for HIV Prevention, 230
Tandon, Rajesh, 3, 176, 253
Teeth Tales, 89
CBPR model of, 90
The Tenderloin District
alcohol and tobacco density in, 294
apple map data of, 295
no-smoking signs in stores, 295–296
Tenderloin Healthy Corner Store
Coalition, 294–295
capacity building in, 301
challenges of, 302
community support for, 297
education provided by, 298–299
FJLs and, 296–297
healthy retail feasibility and, 297–298
partnership dynamics of, 301
policy implementation, monitoring, and
evaluation of, 299–300
precursor to, 294
success of, 300–301, 303
Tenderloin Neighborhood Development
Corporation (TNDC), 294
Tervalon, M., 34
theater of the oppressed, 25
Themba, Makani N., 285
Thomas, S. B., 8
Thompson, B., 10
three-tired racism framework, 49
TNDC. See Tenderloin Neighborhood
Development Corporation
Tobacco-Related Disease Research
Program, 300
Torre, María Elena, 312
T-PE. See transformative participatory
evaluation
TPP. See The Partnership Project
transformational research, 216
transformative participatory evaluation
(T-PE), 252, 253
continuing education for, 261
as cyclical, 254
process for, 254–255
purpose and commitment to, 254–255
as skill building, 262
translational research, 216
Trans PULSE Project, 229
Travers, Robb, 204
tribal institutional review boards, 220
community and, 222–223
438 Index
Tribal Nation, 87
Trickett, E. J., 6, 10, 20
Trump administration, 305, 317
punitive measures of, 308
trust, 61
cognitive-based, 64
continual development of, 66
critical-reective, 63, 64–65
decit suspicion, 63
early development of, 65
functional, 63
identication-based, 64
investigation and measurement of,
62, 69
neutral, 63
proxy, 63
role-based, 63, 66–67
social and types of, 68
trust decit suspicion, 63
historical context of, 67
as personality trait, 67
trust typology model, 63–65
characteristics for, 63
community consultation for, 64–65
operationalization of, 68–69
RIH and, 68–69
variations within, 69
Tuskegee syphilis study, 8, 216
21st Century Policing, 314
U
UC Berkeley-SF Peer Resources
Project, 98, 102
UNEP. See United Nations Environmental
Programme
Unequal Treatment (IOM), 109
UNICEF, 276
United Nations Environmental Programme
(UNEP), 329
UNITED SIKHS, 180
United States, environmental justice
in, 124–125
University of California, 276
University of Nairobi, 276, 330
University of Pittsburgh Medical Center
(UPMC), 111
University of Washington Indigenous Well-
ness Research Institute (UW IWRI), 78
UNM-CPR. See Center for Participatory
Research at the University of New Mexico
UPMC. See University of Pittsburgh Med-
ical Center
UW IWRI. See University of Washington
Indigenous Wellness Research Institute
V
ventriloquy, 25
Vietnamese Youth Development Center
(VYDC), 294, 297
Vines, Anissa, 109
Viramundo (nongovernmental organization),
100–101
Voces y Manos (YPAR project), 99, 101–102
voices, 25
Voices of Youth Maps, 324, 324
VYDC. See Vietnamese Youth
Development Center
W
Wage Theft Ordinance Task Force, 183
Wallerstein, Nina, 4, 7, 18, 21, 22, 25, 48, 57,
62, 78, 84, 144, 208, 238, 253, 279, 288
Webber, S. S., 65
West Oakland Environmental Indicators
Project (WOEIP)
case study of, 48, 52–54
microaggression in, 53–54
white racial frame, 49
whites, racism beneting, 48–49
Wiggins, Noelle, 236
window of opportunity, 298–299
W.K. Kellogg Foundation, 3, 265,
267–268, 280
WOEIP. See West Oakland Environmental
Indicators Project
women’s CBR study, 231
women’s health, sanitation and, 331
World Health Organization, 21
World Social Science Report, 19
Index
439
Y
Youth-Led Digital Mapping, 323
youth-led participatory action
research (YPAR)
adult-youth power sharing from, 97
balancing research and action with, 98
benets from, 96–98
challenges for, 103
complexity of, 100
equality and positive development
promoted by, 74–75
focus of, 95
key principles of, 96–98
knowledge creators from, 98
as multidimensional, 96, 104
phases and support resources for,
98–104
power of, 301
youth development inuenced by, 97
YPAR Hub, 98, 100
YPAR phases, 104
data analysis and interpretation, 101–102
issue selection, 98–99
reporting back and taking action from
outcomes, 102–103
research design and methods as, 100–101
scaling, embedding, and institutionalizing
change, 103
topic constraint and, 99
Yuen, T., 9
