U.S. Department of Health and Human Services
Assistant Secretary for Planning and Evaluation
Office of Disability, Aging and Long-Term Care Policy
EXITING THE MARKET:
UNDERSTANDING THE FACTORS
BEHIND CARRIERS’ DECISION TO
LEAVE THE LONG-TERM CARE
INSURANCE MARKET
July 2013
Office of the Assistant Secretary for Planning and Evaluation
The Office of the Assistant Secretary for Planning and Evaluation (ASPE) is the
principal advisor to the Secretary of the Department of Health and Human Services
(HHS) on policy development issues, and is responsible for major activities in the areas
of legislative and budget development, strategic planning, policy research and
evaluation, and economic analysis.
ASPE develops or reviews issues from the viewpoint of the Secretary, providing a
perspective that is broader in scope than the specific focus of the various operating
agencies. ASPE also works closely with the HHS operating divisions. It assists these
agencies in developing policies, and planning policy research, evaluation and data
collection within broad HHS and administration initiatives. ASPE often serves a
coordinating role for crosscutting policy and administrative activities.
ASPE plans and conducts evaluations and research--both in-house and through support
of projects by external researchers--of current and proposed programs and topics of
particular interest to the Secretary, the Administration and the Congress.
Office of Disability, Aging and Long-Term Care Policy
The Office of Disability, Aging and Long-Term Care Policy (DALTCP), within ASPE, is
responsible for the development, coordination, analysis, research and evaluation of
HHS policies and programs which support the independence, health and long-term care
of persons with disabilities--children, working aging adults, and older persons. DALTCP
is also responsible for policy coordination and research to promote the economic and
social well-being of the elderly.
In particular, DALTCP addresses policies concerning: nursing home and community-
based services, informal caregiving, the integration of acute and long-term care,
Medicare post-acute services and home care, managed care for people with disabilities,
long-term rehabilitation services, children’s disability, and linkages between employment
and health policies. These activities are carried out through policy planning, policy and
program analysis, regulatory reviews, formulation of legislative proposals, policy
research, evaluation and data planning.
This report was prepared under contract #HHSP23320100022WI between HHS’s
ASPE/DALTCP and Thomson Reuters. For additional information about this subject,
you can visit the DALTCP home page at http://aspe.hhs.gov/office_specific/daltcp.cfm
or contact the ASPE Project Officer, Samuel Shipley, at HHS/ASPE/DALTCP, Room
424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C.
20201. His e-mail address is: Samuel.Shipley@hhs.gov.

EXITING THE MARKET:
Understanding the Factors behind
Carriers’ Decision to Leave the
Long-Term Care Insurance Market
Marc A. Cohen, PhD
Chief Research and Development Officer
LifePlans, Inc.
Ramandeep Kaur, MA
Heller School, Brandeis University
Bob Darnell, ASA, MAAA
Independent Consultant
July 2013
Prepared for
Office of Disability, Aging and Long-Term Care Policy
Office of the Assistant Secretary for Planning and Evaluation
U.S. Department of Health and Human Services
Contract #HHSP23320100022WI
The opinions and views expressed in this report are those of the authors. They do not necessarily reflect
the views of the Department of Health and Human Services, the contractor or any other funding
organization.

i
TABLE OF CONTENTS
ACKNOWLEDGEMENTS ............................................................................................... vi
EXECUTIVE SUMMARY ................................................................................................ v
I. INTRODUCTION ....................................................................................................... 1
II. PURPOSE ................................................................................................................. 3
III. METHOD AND ANALYSIS ....................................................................................... 4
A. Published Information Sources .......................................................................... 4
B. Survey of Industry Executives ............................................................................ 5
IV. FINDINGS .................................................................................................................. 7
A. Entering the Long-Term Care Insurance Market ................................................ 7
B. Market Evolution .............................................................................................. 11
C. The Decision to Exit the Market ....................................................................... 27
D. Current Market Activity ..................................................................................... 41
E. Factors that Might Lead Companies to Re-Enter the Market ........................... 45
V. IMPLICATIONS ....................................................................................................... 50
VI. CONCLUSION ......................................................................................................... 54

ii
LIST OF FIGURES AND TABLES
FIGURE 1. Primary Motivations for Entering the Market .............................................. 8
FIGURE 2. Initial Business Strategy ............................................................................. 9
FIGURE 3. Evaluation of Most Volatile or Greatest Potential Future
Challenge at the Time of Market Entry..................................................... 10
FIGURE 4. New Sales of Individual Policies .............................................................. 16
FIGURE 5. Number of Insured Lives Covered by Year .............................................. 17
FIGURE 6. Annual Growth in Total Covered Lives..................................................... 18
FIGURE 7. Industry-Wide Actual Annualized Incurred Claims ................................... 20
FIGURE 8. Single Most Important Reason that the Company Left the
Market ...................................................................................................... 30
FIGURE 9. Moody’s Yield on Seasoned Corporate Bonds--All Industries,
AAA and Ten Year U.S. Treasury Note Yield Rate .................................. 32
FIGURE 10. Annual and Cumulative Loss-Ratio .......................................................... 37
FIGURE 11. Industry-Wide Actual Losses to Expected Losses ................................... 38
FIGURE 12. Industry Actual to Expected Annual Incurred Claims:
2009-2011 ................................................................................................ 39
FIGURE 13. Actions taken Prior to Leaving the Market ............................................... 40
FIGURE 14. Level of Concern about Selling the Product if In-Force Rates
had to be Raised ...................................................................................... 41
FIGURE 15. Market Indicators by Company Sales Status 2009 .................................. 45
FIGURE 16. Chance that the Company would begin Selling LTC
Insurance Again ....................................................................................... 46
FIGURE 17. Circumstances under which the Company would Consider
Re-Entering the Market ............................................................................ 49

iii
TABLE 1. Participating Companies ............................................................................... 5
TABLE 2. Characteristics of Policies Selling in the Market: 1990-2010 ...................... 13
TABLE 3. Characteristics of Individual LTC Insurance by Purchase Year .................. 21
TABLE 4. Key Pricing Assumptions in Developing LTC Insurance
Premiums ................................................................................................... 24
TABLE 5. Impact of Alternative Assumptions on Profitability of LTC
Insurance .................................................................................................... 25
TABLE 6. Distribution of Sample by Year of Market Exit ............................................ 28
TABLE 7. All of the Reasons Cited by Exiting the Market ........................................... 29
TABLE 8. Factors Influencing the Decision to Exit the Market .................................... 34
TABLE 9. Summary of Key Industry Parameters: 2000-2010 ..................................... 39
TABLE 10. Experience of 1995 Top Writers of Individual LTC Insurance in
2011 ........................................................................................................... 43
TABLE 11. Distribution of LTC Insurance Companies by Current Market
Status ......................................................................................................... 44
TABLE 12. Factors Potentially Influence the Decision to Re-Enter the Market ............. 47

iv
ACKNOWLEDGEMENTS
We would like to gratefully acknowledge the partial support that we received for the
survey development, analysis, and report writing for this project from the Office of the
Assistant Secretary for Planning and Evaluation (ASPE), U.S. Department of Health and
Human Services (HHS), Washington, D.C. and specifically our Project Officer, Sam
Shipley.
We would also like to thank all of the executives from long-term care insurance and
reinsurance companies who participate in this survey and set of unstructured
discussions who shared their views in a candid and honest manner.
As well, a number of individuals both inside and outside HHS provided valuable
input and insights into earlier drafts of this paper. We would like to thank Brian Burwell,
Eileen Tell, Al Schmitz, Jodi Anatole, Malcolm Cheung, Richard Frank and the staff of
ASPE for their important contributions to this report.
Of course any and all errors in this report are the sole responsibility of the authors.
v
EXECUTIVE SUMMARY
Throughout the 1980s and 1990s a growing number of private insurers began
providing insurance for long-term care (LTC). The market grew rapidly through the
early part of this decade. By 2003, however, growth in annual sales came to an abrupt
end and the market experienced a major decline. Whereas in 2002, there were 102
companies selling policies, by the end of the decade, there were roughly a dozen
companies still actively selling a meaningful number of policies in the market.
The sheer magnitude of the projected growth in the retiree population along with
the significant exposure to financial risk suggests that there still exists a business
opportunity for companies to provide LTC coverage. As well, there has been consistent
public policy effort in the form of state and federal tax incentives, Partnership Programs
across a growing number of states, and public awareness and education campaigns in
support of private insurance. All of this points to a strong desire on the part of public
policymakers that the private insurance market grows and prospers. Yet, this has
clearly not happened, and the question is, why not?
In this study we provide a systematic understanding of the growth and
development of the LTC insurance market with a particular focus on the reasons why
companies both entered and exited the market. We characterize the market and how it
has changed over time in terms of its size, product offerings, consumer characteristics,
regulatory framework, and financial performance. We also focus on firms’ initial
motivations for entering the market, their expectations and experience while in the
market, and ultimately why so many exited the market.
A review of industry data as well as structured interviews with executives and
decision makers from 26 major LTC insurance companies reveals the following key
selected findings:
Market Entry
About half of the companies entered the market because they believed it
represented a profitable opportunity. Others began providing the insurance to
demonstrate market leadership and to provide new products to their sales force
to keep them engaged and committed to selling the company’s other products.
More than half of companies were most concerned with the future claims risk or
the fact that the LTC risk had a “long-tail”.
Few companies were concerned with what turned out to be the two most
significant drivers of future poor financial performance -- the interest rate and
voluntary lapse rate assumptions built into the pricing of the product.

vi
During the first five years after market entry, roughly two-in-five companies
indicated that sales objectives had not been met and half indicated that either
underlying pricing objectives (25%) or initial profitability targets (25%) had not
been met.
Market Exit: Profitability Challenges
The issue of profitability is one of many factors related to why companies
entered the market but it is an absolutely central factor in understanding why
many of these same companies ultimately exited the market.
Product performance and more specifically, not hitting profit objectives was the
most cited reason for leaving the market.
High capital requirement to support the product was cited most frequently as the
single most important reason for market exit.
Other reasons for market exit related to challenges around marketing and sales,
risk management strategies, regulatory policy, and the lack of reinsurance
coverage.
The key drivers of profitability are embedded in the underlying pricing
assumptions used to develop premiums and are a function of company strategies
related to under-writing and claims management, product design, premium
structure, inflation adjustment rates, sales and marketing costs and investment
strategies.
Small variations in actual experience compared to expected performance of each
of the pricing assumptions can have a major impact on product profitability.
Since the late 1990s, all of these major determinants of premium and product
profitability have been going in the wrong direction: interest rates are
significantly lower than what was priced for, voluntary lapse rates are lower than
for any other insurance product, morbidity is somewhat worse than expected and
mortality is actually improving.
Regarding regulatory policy, the most cited factors having a moderate influence
on a company’s decision to exit the market have to do with the ability to obtain
rate increases in a timely manner or at all, as well as having the necessary
flexibility to engage in appropriate risk management activities.
The costs of regulatory compliance and the possibility that such compliance
encumbers product innovation were not seen as factors in the market exit
decision.

vii
Current Market Activity
Fewer than 15 companies are actively selling stand-alone LTC policies in 2012.
As of the end of 2011, policy sales for these companies were well below 1990
levels.
Market concentration has increased over the decade, with the top ten companies
now accounting for slightly more than two-thirds of covered lives and the top five
accounting for more than half of all policyholders.
Given the recent exodus of additional companies from the market, such
concentration is likely to grow.
While there has been variability in cumulative industry claims performance over
the last decade, recent data suggests that performance is deteriorating. Over the
past three years, new incurred claims are 112% higher than what was expected.
In 2010, annual premiums for companies still selling policies in the market totaled
$5.3 billion compared to $4.7 billion for those who exited the market and were
administering “closed-blocks” of business. On a cumulative premium basis,
however, closed-blocks represented 55% of all earned premiums.
By 2010, 55% of policyholders were being serviced by companies who had
exited the market.
Regarding claims, in 2010, closed-block companies represented 53% and 57%
of annual and cumulative total claims costs.
Factors that might lead Companies to Re-Enter the Market
About 42% of respondents affirmed their belief that the “door remained open” to
re-entering the market at some time in the future; however, only one-quarter
indicated that the chance was greater than 25% and the other 75% said that the
chance was very low or that it simply was not going to happen.
There were very few specific policy design changes or regulatory modifications
presented to respondents that would lead companies to definitely reconsider their
decision to exit the market.
The ability to file multiple premium schedules that would be based on alternative
levels of interest rates -- which in part helps to mitigate the investment (interest
rate) risk -- was cited most frequently as a change that would potentially lead to a
reconsideration of the decision.

viii
Expansion of combination-products to include LTC-disability, LTC-critical illness,
or others was viewed as something that might cause companies to think about
getting back into the market.
One-in-three respondents suggested that allowing policies to be funded with pre-
tax dollars also would lead them to potentially reconsider their decision.
In answer to a broad question about factors that would encourage a
reconsideration of the decision to exit the market, product structure changes
were cited most often as likely to have a meaningful influence; many of these had
to do with the level-funded nature of the product, the “long-tail risk”, and the fact
that the product is complicated.
Those citing regulatory requirements pointed to high capital requirements, as well
as a general sense that carriers needed to have more flexibility in product design.
Implications
Changes to the underlying funding structure of products should be considered
with designs that are less interest rate sensitive like term-priced products and
indexation of both premiums and benefits. These approaches make the product
more affordable for consumers and reduce the level of initial reserves that must
be set up by the company, which in turn eases the amount of capital required to
support the product.
Deploying more sophisticated investment strategies designed to hedge against
the inflation and interest rate risks can also help insurers protect underlying
product profitability.
Providing companies with more certainty regarding the anticipated actions of
state insurance departments vis-à-vis requested rate adjustments is also very
important to enhancing the attractiveness of the market.
By taking some of the most risky elements out of the product, high capital
requirements would no longer be justified which would remove a major barrier to
entry and help justify the deployment of capital to support the product.
Solutions to the challenge and cost of selling the product can include linking LTC
insurance to health insurance, simplifying the product, providing more support for
employer-sponsorship of insurance, educating the public about the risk and costs
of LTC, forcing active choice, and implementing targeted subsidies.
Provision of state-based organized reinsurance pools to provide a “back-stop” for
industry experience, may also encourage more suppliers to enter the market.

ix
Conclusions
The lessons learned about pricing and managing the risks associated with LTC
insurance from those who have left the market can help set the industry on a
more solid financial foundation and make entry for new carriers a more attractive
proposition.
Identifying strategies that produce a level of profitability attractive enough to draw
capital into the market is a key to assuring a robust and competitive market of
insurers.
Public policy and regulatory approaches designed to lower the cost of policies,
allow greater product funding-flexibility, support new forms of combination-
products, and encourage strategies that help to minimize risks outside of the
control of companies, could provide needed support for a market “re-set”.
1
I. INTRODUCTION
Paying for long-term care (LTC) continues to be one of the great financial risks
facing Americans during retirement. Current estimates suggest that the annual costs of
care in a nursing home are roughly $85,000 and that home health care can cost
upwards of $25,000 per year.
1
Given that one-in-five individuals can expect to spend
more than two years in need of care, this represents a significant financial risk. In 2010,
total spending for LTC was $208 billion or roughly 8% of all personal health care
spending.
2
For the most, part such care is provided and paid for by families whereas
the largest public payer of LTC services is the means-tested Medicaid program, which
pays more than 40% of costs. Medicaid is one of the fastest growing health programs
in the country, and is creating significant budgetary pressures on the states. Private
insurance covers a small -- less than 10% -- but growing share of LTC expenses.
Throughout the 1980s and 1990s a growing number of private insurers began
providing insurance for LTC, as an alternative to public coverage (i.e., Medicaid) or to
out-of-pocket payments by the elderly and their families. At first, such insurance
policies covered care provided only in a nursing home. Gradually, coverage expanded
to include payments for home care services, assisted living, adult day care, and other
community options. By the mid to late 1990s more than 100 companies were selling
policies to individuals and to individuals in group markets (i.e., employer settings).
3
Moreover, annual sales increased almost every year throughout the decade. In 1990,
380,000 individual policies were sold; by 2002, 755,000 policies were sold in that year.
4
In 2003, the pattern of annual increases in sales came to an abrupt end. In fact,
LTC policy sales began to decline rapidly. Between 2003 and 2009 individual policy
sales declined by 9% per year.
5
Thus, in 2009, fewer policies were sold than had been
sold in 1990. Moreover, while in 2002, there were 102 companies selling policies by
2009, most of these companies had exited the market; that is, they had stopped selling
new policies.
6
1
Mature Market Institute (2011). Market Survey of Long-Term Care Costs: The 2011 MetLife Market Survey of
Nursing Home, Assisted Living, Adult Day Services, and Home Care Costs. October.
2
O’Shaughnessy, CV. The Basics: National Spending for Long-Term Services and Supports. National Health
Policy Forum, 2012. http://www.nhpf.org/library/the-basics/Basics_LongTermServicesSupports_02-23-12.pdf.
Washington, DC.
3
America’s Health Insurance Plans (2004). Long-Term Care Insurance in 2002. Research Findings, Washington,
DC. June.
4
LifePlans, Inc. (2012). 2011 Long-Term Care Top Writers Survey Individual and Group Association Final Report,
Waltham, MA. March.
5
Ibid.
6
America’s Health Insurance Plans (2004). Long-Term Care Insurance in 2002. Research Findings, Washington,
DC. June.
2
The sheer magnitude of the projected growth in the retiree population -- from 12
million today to 27 million by 2050 -- along with the significant exposure to financial risk
suggests that a business opportunity exists for companies to provide LTC coverage. As
well, there has been consistent public policy support in the form of state and federal tax
incentives, Partnership Programs across a growing number of states, and public
awareness and education campaigns in support of private insurance. All of this points
to a strong desire on the part of public policymakers that the private insurance market
prospers and grows. Yet, this has clearly not happened, and in fact, the number of
companies actively selling LTC insurance continues to decline at a pace far in excess of
the small number of companies entering the market.

3
II. PURPOSE
The purpose of this study is to provide a systematic understanding of the growth
and development of the LTC insurance market with a particular focus on the reasons
why companies both entered and exited the market. We will characterize the market
and how it has changed over time in terms of its size, product offerings, consumer
characteristics, regulatory framework, and financial performance. We will also focus on
firms’ initial motivations for entering the market, their expectations and experience, and
ultimately why so many exited the market.
Specifically, we provide information on the following issues or questions:
1. What were the primary motivations and expectations of firms when they began
providing LTC insurance?
2. How has the market changed in terms of product, pricing, consumer profile,
regulatory environment, supplier characteristics, aggregate market
characteristics and performance indicators?
3. What are the primary reasons why companies who actively marketed LTC
insurance ceased selling policies?
4. What would be required for such companies to consider re-entering the market?
By addressing these issues we intend to paint a picture of the industry in terms of its
historical growth and development, as well as its current and future challenges.
4
III. METHOD AND ANALYSIS
In order to address these issues, we relied on a variety of sources of published
information as well as on new information provided by discussions with insurance
executives from 29 companies who had been in the market and chosen to exit.
A. Published Information Sources
We rely on data and information from America’s Health Insurance Plans (AHIP),
the Life Insurance Marketing and Research Association (LIMRA), industry analyst
reports from Moody’s and Standard & Poors, the academic research literature, and the
National Association of Insurance Commissioners (NAIC) Long-Term Care Experience
Reports for 2000, 2009, 2010 and 2011.
7,8,9,10,11
Reports from this latter source present
the most accurate information on key market parameters regarding premiums, claims,
growth of in-force business, as well as historical performance indicators like actual-to-
expected claims experience and data that enables calculation of measures of volatility
in performance. Almost all companies are required to file detailed data on an annual
basis with the NAIC, and such data is compiled and published in these annual reports.
These reports typically provide country-wide experience for companies. While the
forms are relatively consistent, there have been a number of changes in 2010. The
reports now provide additional information related to lapsation of policies but there is no
longer detailed durational loss-ratio information provided in these reports. Thus, after
2009, one can no longer track the year-by-year loss-ratio (incurred claims divided by
earned premiums) for a specific policy, based on how long that policy has been in-force.
Nevertheless, the data in these reports is extremely valuable and allows us to “size the
market” for companies still selling policies and for companies who exited the market.
An important caveat is that one of the large carriers to exit the market, Penn Treaty
Network America, is currently in rehabilitation status under the auspice of the State of
Pennsylvania. For this reason, the company was not required to provide data to the
7
National Association of Insurance Commissioners (2001). Long-Term Care Insurance Experience Reports for
2000.Kansas City, KS. November.
8
National Association of Insurance Commissioners (2010). Long-Term Care Insurance Experience Reports for
2009.Kansas City, KS. November.
9
National Association of Insurance Commissioners (2011). Long-Term Care Insurance Experience Reports for
2010.Kansas City, KS. November.
10
National Association of Insurance Commissioners (2012). Long-Term Care Insurance Experience Reports for
2011.Kansas City, KS. November.
11
While interim years were available from NAIC, in order to capture the trend over the decade, we focused
exclusively on these years.
5
NAIC in 2009 and 2010. We solicited such information directly from the company and
this allowed us to include their data with the aggregate NAIC reports.
B. Survey of Industry Executives
The second source of information was discussions with key executives who were
either directly involved in the decision making process relating to leaving the market, or
to those with intimate knowledge about their company’s decision to exit the market. The
instrument was administered in two ways: (1) in-person and telephonic interviews with
executives, and (2) a web-based survey that was sent to those individuals who did not
complete the in-person/telephonic interview. In total, executives from 29 companies
that have exited the market or exited specific market segments over the last 15 years
responded to the survey. Of these companies, three surveys were with executives from
reinsurance companies, and the other 26 from direct writers of LTC insurance. In-
person or telephonic interviews were completed with executives from16 companies and
the other 13 were completed on-line.
Executives from the following companies were interviewed and/or provided
responses to the survey.
TABLE 1. Participating Companies
Ability Re
Aetna
Allianz
American Family Mutual Insurance
Company
American Fidelity Assurance Company
CNA
Conseco
CUNA Mutual
Employers Reassurance Corp
Equitable
Great American Financial
Guardian--Berkshire
Hannover Life Reassurance Company of
America
Humana Insurance/Kanawha
John Hancock Group LTC Insurance
MetLife
Munich Re
Nationwide Financial
Penn Treaty
Physicians Mutual Insurance Company
Principal Financial Group
Prudential
RiverSource Life Insurance Company
Southern Farm Bureau Life
Standard Life and Accident Insurance
Company
Teachers Protective Mutual Life
Transamerica
a
Union Labor Life Insurance Company
UNUM
a. Note that Transamerica has since re-entered the market and the interview related to the
reasons for the initial decision to exit the market.
Based on an analysis of data for 2010 (and excluding Transamerica, which is now
back in the market), these companies represent slightly more than 95% of the total
earned premium and 90% of covered lives of companies among the top 100 of all
companies who have left the market. Thus, the results of the survey can be generalized
to the population of companies that have left the market.

6
The survey instrument itself typically resulted in an interview time of between 30
minutes to an hour. All data was captured and put into an analytic database so that
frequencies and cross-tabulations could be completed. Additional information from the
interviewees provided contextual information to many of the responses. This too is
included where appropriate. The survey results that are reported here focus exclusively
on the direct writers of LTC insurance; when appropriate, the issue of reinsurance is
addressed separately and responses from the three participating reinsurance
companies are reported.
Analytic Lens for Understanding Insurer Behavior
A primary focus of this study is to understand why firms have recently left the
market. Therefore, having a frame for understanding such behavior can be helpful in
interpreting the aggregate data as well as company-specific information. We use the
frame of “profit maximization” which posits that firms either enter a market or exit a
market depending on whether they are able to obtain a target return or profit level
commensurate with their expectations. Thus, the basic concept is that companies exist
and make decisions in order to maximize profits.
12
Clearly, the model of profit
maximization is a simplification of reality and assumes that profits are not the only
relevant goal of the firm. In fact, additional objectives may affect profits indirectly or be
equally as important such as sales maximization, public relations, gaining market share,
increasing the attractiveness of complementary products, acquiring power and prestige,
and other goals more related to managers maximizing their own utility rather than
insurer profit maximization. We do not ignore these other goals and in fact test their
validity by asking direct questions to the executives about the various motivations
underlying their decision making.
We begin by presenting information on why firms entered the market and then
present abridged summaries of key historical developments in the market focusing on
changes in product design, marketing and sales, risk management, consumer profiles,
and the regulatory framework that has developed over the past 30 years.
13
This is
followed by a discussion of why in recent years most firms have left the market. We
focus on a number of key issues affecting profitability such as pricing strategies, capital
requirements and distribution challenges. We conclude with an examination of the
factors that might influence firms to consider re-entering the market, and present some
specific actions that might encourage them do to so.
12
This theory of the firm parallels the theory of the consumer which states that consumers seek to maximize their
overall well-being (utility).
13
It is important to note that the information about firm entry to the market is based primarily on interviews with
companies that have since left the market. The exception is the presentation of some historical information on
Amex Life -- currently Genworth Financial.
7
IV. FINDINGS
A. Entering the Long-Term Care Insurance Market
LTC insurance has been selling in the marketplace for the better part of 30 years.
Early versions of the insurance were called “nursing home insurance.” This is because
such policies only covered care provided in nursing homes, primarily skilled facilities. In
the late 1970s, early 1980s there were a small number of companies providing such
coverage some of whom included Penn Treaty, Equitable, and Medico. They entered
the market at a time when expenditures on LTC were less than $20 billion which then
quickly grew to $30 billion in 1980 and over $70 billion within a decade.
14,15
Most of the
costs were borne by individuals and their families and already such care represented an
uncovered and potentially catastrophic expense. The problem of LTC financing was
recognized by policymakers who in the late 1980s debated a number of bills aimed at
paying for substantial LTC costs.
16
This occurred against the backdrop of more than 1.7
million private policies having been sold to individuals during that time.
Most of the firms providing nursing home products in the 1980s also distributed
other types of insurance. All were multi-line companies, the most prominent of which
was the Fireman’s Fund, which then became Amex Life in the late 1980s and G.E.
Capital and Genworth Financial (1990s). These early pioneers were motivated by the
perceived opportunity represented by demographic trends, but more importantly, the
sense that this coverage was not all that different from the Medicare Supplement
policies that were beginning to proliferate in the market. In some sense early nursing
home policies were viewed as a variant of such policies. This view, shaped early
approaches toward pricing, which will be discussed in a subsequent section.
We asked executives in the sample to recount why their company had initially
entered the market. Three of these companies began selling policies in the 1970s, ten
in the 1980s and almost all of the remainder in the 1990s. When these companies
entered the market most (73%) offered a nursing home-only policy -- many having
entered in the 1970s or 1980s -- and slightly more than half (57%) also offered
comprehensive policies covering both nursing home and home care services -- all
companies that entered the market in the late 1980s and early 1990s.
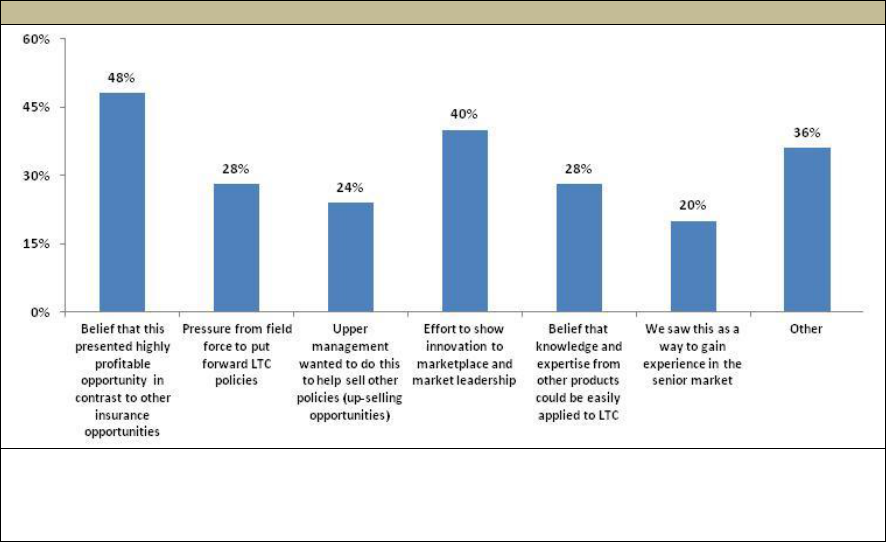
Consistent with our model of firm behavior, Figure 1 shows that almost half of the
companies entered the market because they believed it represented a profitable
14
Long-Term Care for the Elderly and Disabled (1977). Congressional Budget Office, Congress of the United
States, Washington, DC. February.
15
Health Care Financing Administration, Office of the Actuary, Data from the Office of National Health Statistics in
Health Care Financing Review, Fall 1994, Volume 16, Number 1.
16
Among others, these included the Mitchell Bill, which proposed paying for the care of individuals who stayed
more than two years in a nursing home and the Kennedy Bill which proposed paying for front-end LTC costs.
8
opportunity. However, profit maximization was not the only reason for entering this
market. Many companies felt that such a strategy supported efforts to show market
leadership and to provide new product to their sales force to keep them engaged and
committed to selling the company’s other products. During detailed discussions with
respondents, it was clear that compelling demographics and a perception of increasing
consumer need drove many companies to enter this market to take advantage of an
opportunity that they knew existed, even if they were not completely certain about how
to exploit it profitably. Not shown in the figure is the fact that among these companies
who left the market, 80% had senior management that was either supportive or very
supportive of the decision to initially enter the marketplace.
FIGURE 1. Primary Motivations for Entering the Market
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment of
the market.
NOTE: Numbers sum to more than 100% because respondents could check more than a single
motivation.
Even 30 years later, the need for a product addressing the catastrophic costs
associated with LTC needs persists. The consequence of demographic trends, a lack of
comprehensive public solutions, and an inadequate private market is that LTC remains
the largest unfunded health-related liability faced by elders during retirement. While
demographics and consumer need have remained constant over the period,
perceptions about the actual profit opportunity presented by this market have definitely
changed.
Figure 2 highlights the initial business strategy of companies and demonstrates
that for 40% of the companies that left the market, their initial business strategy was to
grow modestly in order to learn the business and improve their management of the
product over time. Only 16% had aspirations of becoming market leaders.
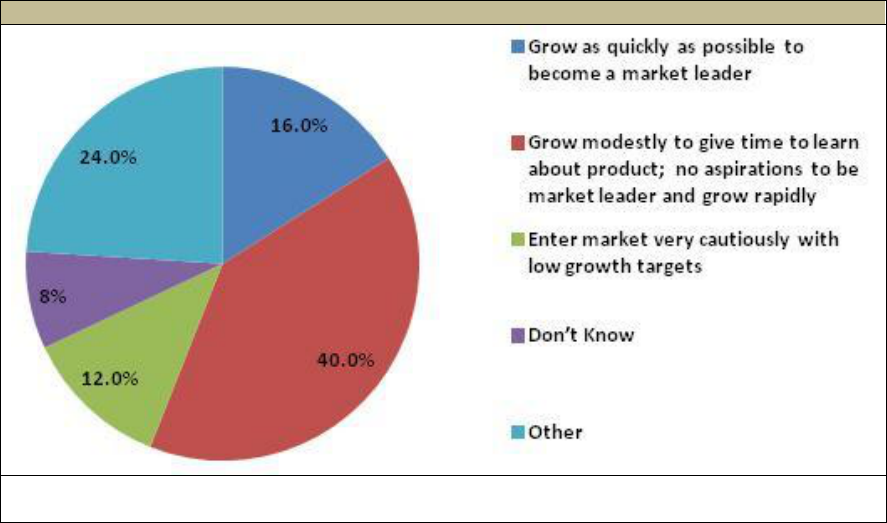
9
FIGURE 2. Initial Business Strategy
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment of
the market.
We also asked which business metric was viewed as the most important to
measuring the success of the endeavor during the first five years after market entry.
Slightly less than half (48%) of companies indicated that meeting sales targets was
most important. Profitability and meeting underlying pricing assumptions during the first
few years of sales were cited by fewer than 25% of respondents; this suggests that
there was a realistic understanding that given the long-term nature of the underlying
risk, as well as the relatively high initial costs associated with selling and underwriting
new policies, profit emergence and credible actuarial experience would be relatively
slow in developing. The first measurable goal would be sales.
Most companies tried to differentiate themselves from their competitors through
innovative product design as well as sales incentive plans. Some of the innovation
proved to be confusing for consumers, and in particular, competition related to the
benefit eligibility trigger. Some companies made eligibility for benefits dependant on the
ability to perform varying numbers of activities of daily living (ADLs) and instrumental
activities of daily living. It was nearly impossible for an individual to know which set of
conditions they were likely to meet 20 years into the future to qualify for insurance
payments. Benefit trigger standardization did not occur until the passage of the Health
Insurance Portability and Accountability Act (HIPAA) of 1996. Companies also
expanded coverage for more community services including caregiver support and
respite care, restoration of benefits, transportation services, and other ancillary benefits.
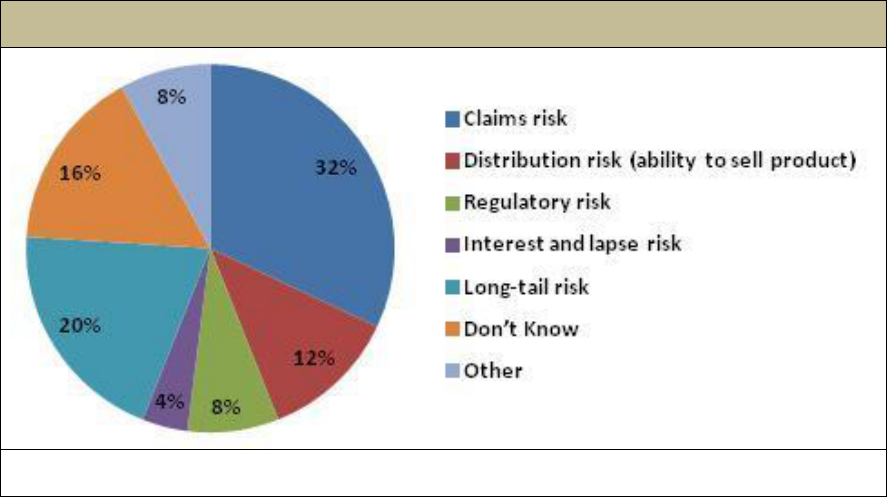
Figure 3 shows how companies evaluated the key risks associated with this
product. More than half of companies were most concerned with the future claims risk
or the fact that this risk had a “long-tail”. In other words, they were not certain how long
an individual with LTC needs would require paid services. A relatively high percentage
10
of policies had lifetime or uncapped benefit durations, which meant that they would pay
benefits for as long as someone had continued need -- which represented an uncapped
liability to the company.
FIGURE 3. Evaluation of Most Volatile or Greatest “Potential Future Challenge”
at the Time of Market Entry
SOURCE: Survey of executives from 25 LTC carriers who exited the market or exited segment of
the market.
It is somewhat ironic that few companies were concerned with what turned out to
be the two most significant drivers of future poor financial performance -- the interest
rate and voluntary lapse rate assumptions built into the product. Lower than expected
interest rates and voluntary lapse rates have forced almost all companies to seek rate
increases, and this may have contributed negatively to sales as well as to the reputation
of both the product and to a number of companies. As will be demonstrated in a
subsequent section, errors in these assumptions had a major negative impact on
product profitability.
We also asked companies which objectives were not met during the first five years
of market entry. Roughly two-in-five indicated that sales objectives had not been met
and half indicated that either underlying pricing objectives (25%) or initial profitability
targets (25%) had not been met. Thus, fairly early on, for a clear majority of these
companies, the key metrics established to judge whether the initial decision to enter the
market had been a good one, were not being met. Moreover, early undefined goals
may have led to later disappointments.
Since the time when most firms entered the market, the industry has experienced
a number of major changes, many of them directly and indirectly contributing to the
current picture of the industry. These include changes in product, risk management
strategy, sales approaches, and the regulatory and public policy environment. We
summarize these key trends in order to provide an historical view of industry
developments through the first decade of this century.

11
B. Market Evolution
1. Product Design
As mentioned, LTC insurance -- nursing home insurance -- has been selling in the
marketplace for the better part of 30 years. Thus, it may still be considered a relatively
new insurance product that continues to evolve. The implication is that one might
reasonably expect “wrong turns” along the way, as the product and industry adapts to
new information, changing market conditions, and accumulated actuarial experience.
Through the 1970s and up to the late 1980s, the coverage was linked to the structure of
Medicare coverage. Like many supplemental private health insurance policies, nursing
home insurance focused on what Medicare “did not cover”. Medicare paid for skilled
nursing home care for up to 100 days and private insurance began coverage when
Medicare ceased providing benefits. For this reason, early product configurations had
elimination periods (i.e., deductibles) that were typically defined as 100 days -- the
period of care that Medicare covered -- and the coverage was focused exclusively on
skilled nursing home care resulting from a prior three day hospitalization -- precisely in
line with Medicare policy. If care was initially considered to be “medically necessary”,
private insurance carriers would continue to pay benefits even when the need for skilled
care ceased and only custodial (i.e., maintenance) care was required. Thus, while
these early private policies “keyed off” of Medicare coverage, their innovation was that
they paid for custodial care, where Medicare did not. In essence, this extended
coverage from a limited amount of skilled nursing care (paid by Medicare) to a much
more generous amount of skilled and custodial nursing home care (paid by private
insurance and also by Medicaid for selected populations).
Early Medicaid policy also shaped the conception of LTC as synonymous with
nursing home care.
17
Over time, LTC -- and now long-term services and supports -- has
come to reflect the reality that the need for care, which is based on functional limitations
and/or cognitive impairment, requires a broader set of service responses. These
include home and community-based care and a variety of residential care settings such
as assisted living, adult day care and others.
Regarding the pricing of early policies, there was little basis on which to develop
an estimate for future morbidity (i.e., the chance that someone would develop a
condition that required use of LTC services) in the context of private insurance. In order
to price these early policies actuaries relied on national data sources like the 1977 and
1985 National Nursing Home Surveys. As they considered home care coverage, they
focused on the 1982, 1984, and 1994 National Long-Term Care Surveys for incidence
and continuance data; again, such data was not directly transferrable to the private
insurance context since it was neither insured data nor was the underlying population
17
Kemper, Peter (2010). Long-Term Services and Supports. The Basics: National Spending for Long-Term
Services and Supports. Presentation to the National Health Policy Forum, Washington, DC. June 18.
12
likely to reflect purchasers of insurance. For other pricing parameters, like voluntary
lapse rates and mortality, there was a reliance on the experience of Medicare
Supplement policies and standard mortality tables. For this reason, voluntary lapse
rates priced into initial policies were much higher than what they ultimately turned out to
be. (In fact, there is no other voluntary insurance product in the market that has
experienced lower voluntary lapse rates than what is found in LTC insurance policies.)
Policies were always sold as guaranteed renewable -- they could only be cancelled
for non-payment of premium -- and as level-funded. That is, while the premium charged
varied by age at purchase, once an individual purchased a policy, the premium was
designed to be level for life. Theoretically, an individual buying a policy at age 65 for a
premium of $1,000 per year could be expected to pay that same annual premium
throughout their lifetime, so long as the underlying pricing assumptions employed by the
actuaries were accurate. The level-funded nature of the product persists to this day,
and poses unique challenges to insurers. This will be discussed in a subsequent
section. Finally, almost all policies reimbursed the actual costs of care up to a daily
benefit maximum.
Relatively sluggish sales of LTC insurance policies in the 1980s suggested that the
then current product design was not going to reach a broader part of the public. Selling
insurance to cover something that no one wanted to access, except under the most
extreme of circumstances, did not seem to be an attractive value proposition for fueling
growth in the market. Moreover, Medicare, as well as certain Medicaid plans under
special waivers, began to pay for support services in peoples’ homes. Medicare
covered such services primarily when they were deemed to be medically necessary.
Medicaid also expanded its coverage for home and community-based care but still
severely restricted access to these services.
As agents and brokers came to play a larger role in the LTC product development
process, it was clear that for the coverage to sell, it needed to pay for custodial services
where people desired them most -- in their own homes. This presented a dilemma for
insurers because the primary risk management tool for managing claims was based on
policyholder behavior: no policyholder really wanted to go into a nursing home, and this
served as a brake on potential moral hazard and over-utilization of services. If policies
began covering services in settings that people desired, like the home, this “brake” on
moral hazard would disappear with the potential for making the underlying economics of
the product unsustainable.
It became clear that in order for the market to grow, the product would have to
cover home and community-based services in a manner that enabled insurers to
effectively manage what were viewed to be the primary risks of the product: adverse
selection and moral hazard. This was accomplished in part by changing the basis on
which benefits were paid from a medical necessity model to a functional and cognitive
impairment model. There had been a growing realization, encouraged by professionals
with geriatric experience who entered the industry or consulted with it, that measures of
13
functional abilities were most closely related to the need for covered services --
including home care.
In the mid to late 1980s and early 1990s, carriers began to provide limited
coverage for home and community-based care -- either through riders or as part of the
underlying basic policy design. They felt comfortable doing so because access to
insurance benefits was made contingent on an insureds inability to perform a certain
number of ADLs or the need for assistance due to a severe cognitive impairment.
These were more easily measurable and predictable benefit eligibility criteria. Also, a
number of third party assessment companies entered the market to assist insurers in
evaluating whether such deficits existed. It is not surprising, therefore, that consumer
demand, coupled with the sense that companies could manage the underlying risk,
fueled rapid growth in market share of comprehensive policies. This is clearly displayed
in Table 2, which highlights the changes in product design over the past 20 years.
TABLE 2. Characteristics of Policies Selling in the Market: 1990-2010
Policy Characteristics
Average
for 1990
Average
for 1995
Average
for 2000
Average
for 2005
Average
for 2010
Policy Type
Nursing Home-Only
63%
33%
14%
3%
1%
Nursing Home & Home
Care
37%
61%
77%
90%
95%
Home Care Only
---
6%
9%
7%
4%
Daily Benefit Amount for
Nursing Home Care
$72
$85
$109
$142
$153
Daily Benefit Amount for
Home Care
$36
$78
$106
$135
$152
Nursing Home-Only
Deductible Period
20 days
59 days
65 days
80 days
85 days
Integrated Policy
Deductible Period
---
46 days
47 days
81 days
90 days
Nursing Home Benefit
Duration
5.6 years
5.1 years
5.5 years
5.4 years
4.8 years
Inflation Protection
40%
33%
41%
76%
74%
Annual Premium
$1,071
$1,505
$1,677
$1,918
$2,283
SOURCE: LifePlans analysis of 8,099 policies sold in 2010, 8,208 policies sold in 2005, 5,407 policies
sold in 2000, 6,446 policies sold in 1995 and 14,400 policies in 1990. Reported in: Who Buys Long-Term
Care Insurance in 2010-2011? A Twenty-Year Study of Buyers and Non-Buyers (in the Individual Market),
AHIP, 2012.
Coverage limited to nursing home or institutional alternatives only has virtually
disappeared from the market. Deductible periods have increased and are roughly equal
to three months of care. Moreover, the percentage of individuals purchasing some level
of protection for increasing LTC costs is about three-in-four with roughly half buying
compound inflation protection.
The average daily nursing home benefit has increased significantly over the period
-- by an annual rate of roughly 4%. Given the mix of home care and nursing home
service use, this is roughly in line with the rate of inflation in these services over the
period; the $153 daily benefit amount in 2010 would cover 70% of the average daily
cost of nursing home, 155% of the daily cost of assisted living, and roughly eight hours

14
of home care a day seven days a week.
18
Over the period, there has been a decline in
the number of policies with unlimited benefits, a particularly risky policy design, given
the uncapped liability faced by the insurer. The desire of companies to move away from
this policy design stems in part from pressure by ratings agencies and fewer
reinsurance options.
19
It represents one of a number of actions insurers have taken to
“de-risk” the product.
Finally, annual premiums have increased significantly over the period, as policy
value has increased and as insurers have a body of credible experience on which to
make changes to a number of key underlying pricing assumptions. Clearly new policies
reflect a more conservative set of pricing assumptions, especially with respect to
interest rates and voluntary lapses. This will be discussed in more detail in a
subsequent section.
2. Marketing and Sales
Like other types of insurance, LTC insurance is sold in a variety of ways and
through a number of distribution channels. Most policies are sold by agents and
brokers directly to individuals. The distribution channel which is growing the most
quickly, however, is the employer group market. Here agents are able to market and
sell group policies to a large number of individuals, each of whom receives an individual
certificate of insurance under a group plan. In 2000, new individual sales accounted for
75% of the market and group sales -- primarily employer-sponsored -- represented only
25% of new sales. By 2010, new individual sales had fallen to 58% of the market and
group channels comprised 42% of new sales.
20,21
While most agents are independent -- this indicating that they can represent and
sell policies from a variety of insurers -- a number of companies do have what are called
“captive agents”. In these companies agents can only sell that company’s specific
policy. Only a very few companies have specialist LTC agents, whose sole focus is
selling LTC insurance policies. Currently there are fewer than 10,000 agents selling any
meaningful number of policies.
Commissions for LTC insurance tend to be “heaped”. This means that first-year
commissions relative to premiums are high -- 40%-60% of premium with some
companies approaching 100% -- and then they tend to drop down to between 5% and
18
Market Survey of Long-Term Care Costs (2010). The 2010 MetLife Market Survey of Nursing Home, Assisted
Living, Adult Day Services, and Home Care Costs. MetLife Mature Market Institute.
19
Moody’s: Long-Term Care Insurers Face Uncertain Future (2012). Moody’s Investor Service, Global Credit
Research, New York, NY. September 19.
20
Cohen, M. (2011). Financing Long-Term Care: The Private Insurance Market. Presentation to the National
Health Policy Forum, Washington, DC. April 15.
21
It is important to note that a number of companies exiting the market have transferred their group business to
other carriers and in some cases this may be counted as a “sale”, even if individuals purchased their coverage years
beforehand. Thus, some of the 42% of new sales could have been comprised of such takeover activity, which was
particularly prevalent in 2010-2012.

15
15% of ongoing renewal premiums.
22
This compensation structure does cause
significant first-year cash flow challenges for companies. Moreover, it delays the timing
of profit emergence as companies may be in a loss position for the first year after a
policy is sold.
The 1990s were characterized by companies competing for the allegiance of large
distribution forces by paying higher commissions to attract and encourage them to
represent and sell their, rather than competitors’, policies. This led to a situation where
the costs of the product increased and market share shifted rapidly between companies
as agent groups focused on selling the product that paid the highest commissions. The
higher commissions did not appear to draw enough new agents into the market to
effectively increase overall market size significantly over the past decade.
It is often said by industry participants that LTC insurance is not “bought” by
consumers, but rather, it is “sold” to consumers. Challenges related to individuals’ lack
of understanding about future risk, an incorrect belief that government will pay for LTC,
confusion about products, belief that other products already address the risk, its cost in
relation to the value that people believe it has, and a lack of belief in the underlying
value proposition have all contributed to the overall challenge of growing the market.
23,24
Even in the presence of such challenges, however, two-thirds of surveyed individuals
from the general population age 50 and over in 2010 indicated that they were aware of
companies that offer this insurance, and about 40% had been approached or had
considered purchasing it.
25
It often takes agents 2-3 visits to close a sale. Still agents are critical in the
process and are viewed very positively by buyers; in a study of buyers in 2000, more
than 90% reported that the agent they had dealt with was knowledgeable, explained the
product well, and helped them select a policy that met their needs. Moreover, after a
spouse, agents were seen to be the most important in individuals’ decision to purchase
a policy.
26
In terms of overall sales and market penetration, the first half of the 1990s
represented the fastest growth over the 20 year period and coincided with the
proliferation of policies covering home care and nursing home care. The precipitous
22
Note that for life insurance first-year commissions are commonly above 100% and the dollar value of annuity
commissions is often greater than the value of LTC commissions. Thus, LTC commissions are not out of line with
other voluntary insurance products.
23
Stevenson, D., Cohen, M., Tell, E. and Burwell, B. (2010). The Complementarity of Public And Private Long-
Term Care Coverage. Health Affairs, 29:1. January.
24
Brown, J.R., Coe, N.B., and Finkelstein, A. (2007). Medicaid Crowd-Out of Private Long-Term Care Insurance
Demand: Evidence from the Health and Retirement Survey. In J.M. Poterba, Ed., Tax Policy and the Economy, Vol.
21, pp.1-34.
25
Based on analysis of 500 individuals age 50 and over surveyed in 2010, 2005, and 2000 as well as 1,000
individuals age 55 and over surveyed in 1995 as reported in Who Buys Long-Term Care Insurance in 2010-2011? A
Twenty-Year Study of Buyers and Non-Buyers (in the Individual Market), AHIP, 2012.
26
Long-Term Care Insurance 2000: A Decade of Study of Buyers and Non-Buyers. The Health Insurance
Association of America, July 2000.
16
decline in sales in the early part of this century coincides with a growing number of
companies exiting the market, the general declines in the stock market which affected
demand, and the significant price increases in new policies offered by insurers.
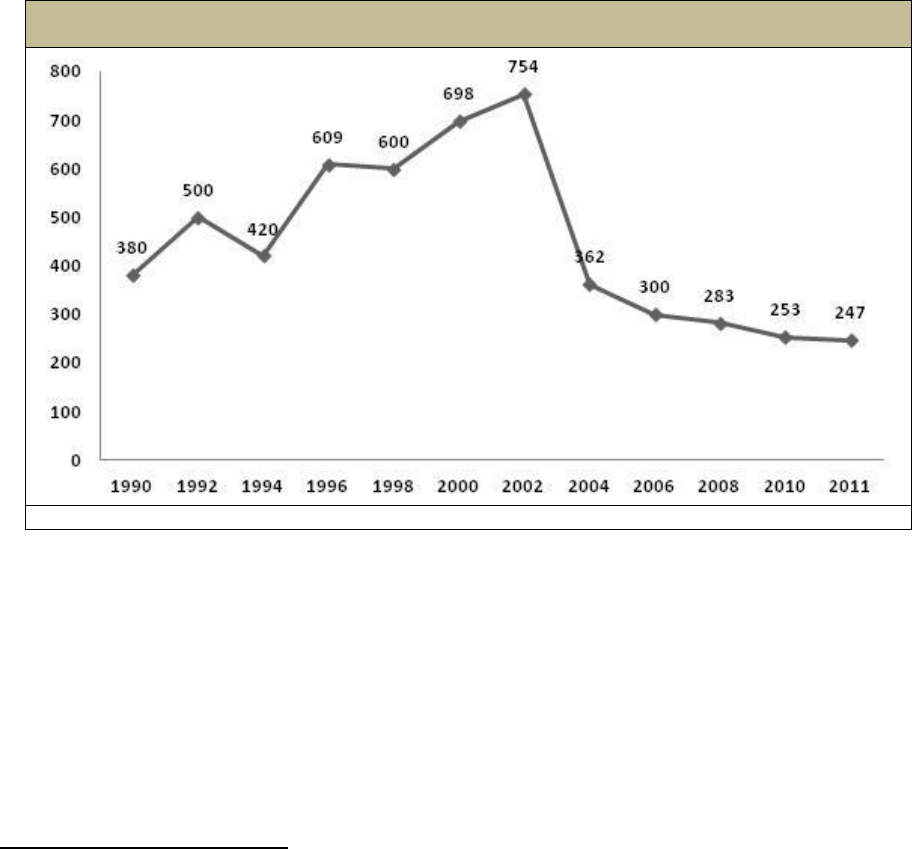
Figure 4 shows sales patterns for new individual policies over the past 20 years.
27
FIGURE 4. New Sales of Individual Policies
(thousands)
SOURCE: LifePlans analysis based on AHIP, LIMRA and LifePlans sales surveys, 2011.
Clearly, as policies became more attractive to consumers in the 1990s, the market
grew significantly both in terms of covered lives and insurance premium. It is also worth
noting that during the 1990s, there were minimal changes in the underlying pricing
assumptions of policies. In fact, between 1990 and 2000, the average value in policies
-- as measured by changes in average value of policy benefits -- increased more quickly
than the average premium during the period.
28
This trend foreshadowed a later criticism
and concern with LTC policies expressed by ratings agencies that early designs of
policies offered benefits that were too generous relative to factors like actual benefit
utilization.
29,30
27
Note that the decline in sales in 1994 coincided with the Clinton health care reform debates which included
provisions for expanded home and community-based care. This was seen to depress demand as potential buyers
waited to see whether or not the legislation would pass.
28
Authors calculations based on policy design data from more than 10,000 policies in 1990, 1995 and 2000 as
reported in Who Buys Long-Term Care Insurance in 1994? Profiles and Innovations in a Dynamic Market (2005).
Health Insurance Association of America, Washington, DC, and Who Buys Long-Term Care Insurance in 2005? A
Fifteen Year Study of Buyers and Non-Buyers (2006). America’s Health Insurance Plans, Washington, DC.
29
Bazer, L. (2012). An Outsiders View: The State of the LTCI Industry--Long Term Care from a Rating Agency
Perspective. Presentation at the 12th Annual Intercompany Long Term Care Insurance Conference, Las Vegas,
March. Moody’s: Long-Term Care Insurers Face Uncertain Future (2012). Moody’s Investor Service, Global
Credit Research, New York. September 19.
17
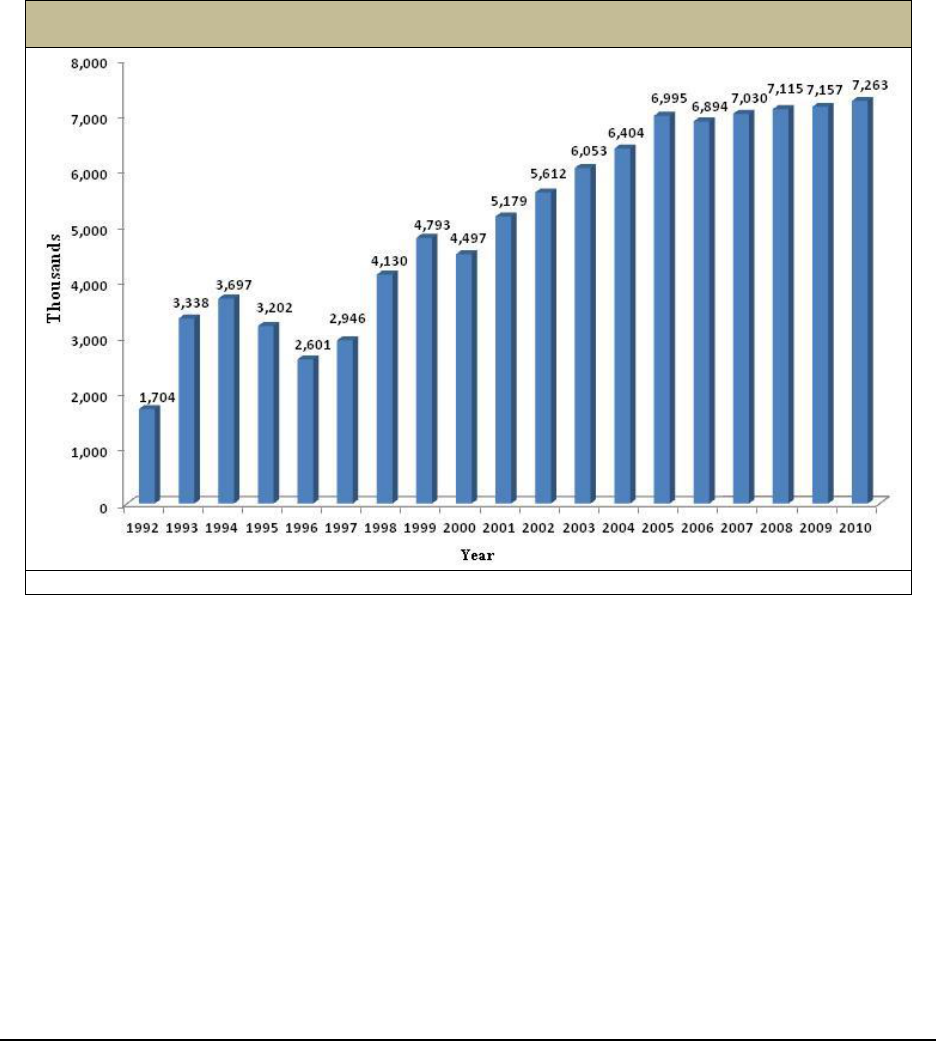
Figure 5 shows that in 2010, the total number of individuals with LTC insurance
coverage was 7.3 million. This does not represent all people who have ever had
policies, only those who still have them. Changes in covered lives reflect both growth in
annual sales as well as changes in the number of policyholders who maintain their
coverage over time.
FIGURE 5. Number of Insured Lives Covered by Year
(thousands)
SOURCE: NAIC Experience Reports, 2011.
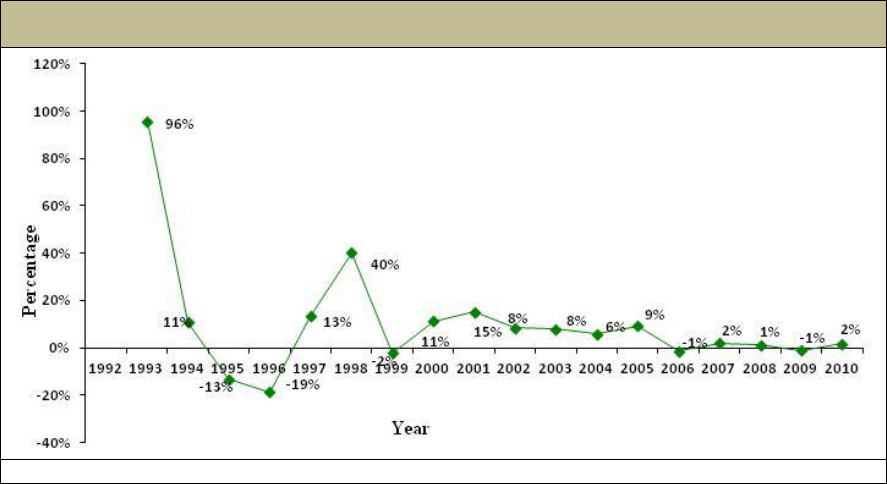
Figure 6 shows the annual change in covered lives over the period. As shown,
between 1992 and 2000 there was tremendous variation in the growth rate of covered
lives and after 2003, there has been a relatively steady yet small annual increase in
covered lives. Given the aging of the individuals with policies, this suggests that the
growth in sales throughout the decade has declined or been relatively flat.
30 Meyer, D. (2012). Why Get in? Why Get out? Ratings Agency Perspective on Long-Term Care. Fitch
Ratings, presentation at the 12th Annual Intercompany Long Term Care Insurance Conference, Las Vegas, March.
18
FIGURE 6. Annual Growth in Total Covered Lives
(thousands)
SOURCE: LifePlans analysis of NAIC data, 2010.
3. Risk Management
For first generation policies sold in the 1970s and 1980s, insurers were convinced
that because nursing homes were viewed as places of last resort to receive care, there
would be little moral hazard because it was well known that most people viewed nursing
home residency as a “dreaded event”. Not surprisingly, little attention was paid to
underwriting and claims management for these early policies. So long as an applicant
was not already in a nursing home, they could apply for coverage and would likely be
issued a policy. Given that the average age of new buyers at the time was 68, most
carriers still expected to see significant claims activity only 10-15 years in the future.
As companies began to market and sell comprehensive coverage they well
understood that the aversion to using nursing homes was no longer an impediment to
moral hazard; hence, companies felt a need to invest in more robust approaches to
managing the two primary risks associated with product performance that were
completely under their control: underwriting to guard against adverse selection, and
claims management, to protect against moral hazard.
In the early 1990s, insurers began to employ more vigorous approaches to the
underwriting of policies; these approaches focused on two broad dimensions: (1)
medical criteria; and (2) tools and requirements gathering. Regarding medical criteria,
the three domains on which companies focused their attention were the medical,
functional, and cognitive status of individuals. Risk managers tried to better identify
factors that put the individual at immediate or near term need for the services that were
being insured for, namely, human assistance required to compensate for an individual’s
inability to perform ADLs due to functional deficits or to cognitive issues. Diagnoses
were viewed as markers for current or future manifestations of functional need. Data
mining, as well as more comprehensive reviews of the medical literature resulted in the
19
development of detailed medical underwriting guides by companies. The information in
these guides was considered proprietary, since the ability to perform more effective risk
selection was seen as a competitive advantage for a company. At the same time,
cognitive testing was adopted in the early 1990s and became a standard business
practice. The availability of third party assessment companies serving the industry
significantly enhanced the ability of insurers to perform their risk management functions
both for underwriting and for claims management.
Companies also invested in more robust information gathering. The most common
tools included information provided from the application, telephone interviews, medical
records or attending physician statements, medical exams, in-person assessments and
pharmacy databases. Many of these tools are in use today. An analysis of underwriting
practices across the industry suggested that over the last decade, as companies have
been able to link their up-front underwriting strategies with back-end claims experience,
there has been a marked shift toward more conservative underwriting practices.
31
In
2009, underwriting rejection rates across the industry were at 19.4%. For applicants
under age 45, declination rates are below 10% whereas for those over age 80, rates
increase to more than two-in-five.
32
Regarding claims, insurers focused on managing three major types of risks
associated with a claim: (1) the incidence risk, which is the risk that someone becomes
disabled and requires LTC services covered by the policy; (2) the intensity risk, which
focuses on the level of service and associated expenditure required to compensate for
the individual’s functional or cognitive deficits; and (3) the continuance risk, the amount
of time that an individual would require paid services. Companies typically deploy --
through third party vendors -- nurses into the homes of claimants to measure whether
the benefit eligibility trigger has been met and these same nurses are also involved in
the development of care plans. These benefit assessments are fairly standard across
the industry, especially when someone is claiming home care or assisted living benefits.
For nursing home care, many companies rely on nursing notes or the Minimum
Dataset Survey to obtain the information necessary to adjudicate a claim. The latter is
an assessment that must be completed on all nursing home residents. Companies also
conduct regular follow-up with claimants to assure that they remain eligible for benefits
under the terms of the insurance contract. Over the last decade insurers have invested
significant resources into claims management systems and are far more active in terms
of helping claimants navigate the LTC system and get services in place.
33
31
Tolerating Risk: A Look at LTC Underwriting Strategies. Behind the Data, Issue 2, January 2011. LifePlans,
Inc., Waltham, MA.
32
Ibid.
33
U.S. Department of Health and Human Services, Office of Disability, Aging and Long-Term Care Policy (2008).
Private Long-Term Care Insurance: Following an Admission Cohort over 28 Months to Track Claim Experience,
Service Use and Transitions. Final Report. Washington, DC. April.
http://aspe.hhs.gov/daltcp/reports/2008/coht28mo.htm.
20
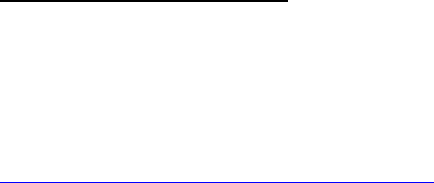
This investment is clearly warranted given the rapid growth in claims payments.
Figure 7 shows the growth in new claims over the period. The average growth in
annual incurred claims over the period is 13%. Although not shown in the figure,
through 2010, companies reported paying out on a cumulative basis over the last two
decades slightly less than $50 billion in incurred claims; on an annual basis, the liability
covered from private LTC insurance is roughly $6 billion, which is less than 5% of total
expenditures on LTC services in the United States.
FIGURE 7. Industry-Wide Actual Annualized Incurred Claims
SOURCE: NAIC Experience Reports, 2011.
NOTE: The growth in incurred claims in and of itself does not translate to underlying profitability
or performance for the industry, nor does its relationship to changes in earned premiums (which
are not shown in Figure 4) relate directly to profitability. Profitability is related in part to the actual
relationship between claims and premiums over the life of a policy.
4. Consumers of Long-Term Care Insurance
Roughly seven million individuals have a LTC insurance policy. The LTC
Financing Strategy Group estimated that penetration among individuals who are
considered to be suitable purchasers (i.e., have incomes in excess of $20,000 and are
not currently eligible for Medicaid) is 16% of the over age 65 group and about 5% of the
age 45-64 age group.
34
The profile of individuals purchasing LTC insurance has
changed dramatically over the last 20 years. As products have become more
comprehensive and costly, the proportion of middle income buyers of insurance has
declined. Table 3 summarizes key characteristics of buyers in the individual market.
The average age of buyers continues to decline, and most purchasers are working,
married college-educated and have significant levels of income and assets. In the
group market, the average age is roughly 46 years. Not shown in the table is the fact
that most people purchase the insurance to protect current consumption patterns (e.g.,
34
LTC Financing Strategy Group, 2008. Washington, DC.
21
maintain standard of living, avoid dependence, maintain affordability of services) rather
than to protect assets.
35
TABLE 3. Characteristics of Individual LTC Insurance by Purchase Year
Socio-Demographic
Characteristics
1990
1995
2000
2005
2010
Average Age
68
69
67
61
59
70 and over
42%
49%
40%
16%
8%
Percent Female
63%
61%
55%
57%
54%
Percent married
68%
62%
70%
75%
72%
Median Income
$27,000
$30,000
$42,500
$62,500
$87,500
% Greater than $50,000
21%
20%
42%
71%
77%
Median Assets
N.A.
$87,500
$225,000
$275,000
$325,000
% Greater than $75,000
53%
49%
77%
83%
82%
Percent College-Educated
33
36
47
61
71
Percent Employed
N.A.
23%
35%
71%
69%
SOURCE: Who Buys Long-Term Care Insurance in 2010-2011? A Twenty-Year Study of Buyers and
Non-Buyers (in the Individual Market), AHIP, 2012.
One of the ways policymakers have worked to expand the private insurance
market to reach middle income adults is to support Partnership Programs. These
programs -- which represent a partnership between state Medicaid programs and the
private insurance industry -- are designed to enable individuals who purchase qualified
LTC insurance policies to access Medicaid benefits without having to spend down their
assets to Medicaid levels, if and when their LTC insurance benefits are exhausted. A
growing number of states -- upwards of 45 by the end of 2012 -- have implemented
such programs.
36
Even so, few people age 50 and over -- less than 25% -- actually
know whether or not their state has a Partnership Program. However, the Program
does hold appeal: fully 45% of a random sample of individuals over age 50 indicated
that they would be likely to purchase a policy if their state participated in a Partnership
Program.
37
For individuals who have been approached by agents and choose not to buy a
policy, most cite cost as the primary impediment to purchase. Other far less prevalent
reasons typically include the difficulty of choosing a policy, a lack of confidence in
insurers to pay benefits as stated, and the desire to wait to see if better policies come
on the market.
38
5. Regulatory Framework and Public Policy
The first reported interest in developing a regulatory framework for private LTC
insurance was in 1985 when a series of conferences between legislators, regulators
and industry representatives were held; there was also growing interest in Congress in
35
Authors’ analysis of data summarized in AHIP Study of Buyers and Non-Buyers of Private LTC Insurance in
2010, Washington, DC.
36
Website on Partnership Programs: http://w2.dehpg.net/LTCPartnership.
37
Who Buys Long-Term Care Insurance in 2010-2011? A Twenty-Year Study of Buyers and Non-Buyers (in the
Individual Market), AHIP, 2012.
38
Ibid.

22
the area of nursing home insurance.
39
As a result of a sustained effort, NAIC adopted
the first Model Act in December 1986, followed by the first model regulation in 1987.
Many states adopted these model regulations. In fact, by 1989, more than two-thirds of
states had adopted the NAIC model act and/or regulation.
40
The model regulations
became the reference point for companies developing or modifying policies they were
selling -- or intended to sell -- in the marketplace. The model regulation provides
guidance and requirements related to many issues affecting the product including
capital requirements, pricing, marketing and sales, agent licensing and education, and
consumer protections, to name but a few.
In December 1988, the first attempt aimed at modifying insurance contracts
occurred. The regulation included prohibitions against prior hospitalization
requirements as a condition for receipt of institutional benefits and in 1989, the same
requirement was eliminated for home care benefits. It was not until 1995, however, that
a new section -- Section 27 -- was added to the Act that provided for standards on the
conditions under which insurance benefits would be paid. Regulators, consumer
representatives and the industry expressed widespread support for greater
standardization.
In 1998, the Senior Issues Task Force (which was part of the NAIC) was charged
with the task of reviewing the LTC Insurance Model Act and Regulation for compliance
with the HIPAA of 1996. Among other things, HIPAA set benefit eligibility standards for
tax-qualified LTC insurance policies. The federal requirement -- detailed in Section 213,
7702B and 4980C of the Internal Revenue Code -- was that benefits would be triggered
when the insured could not perform at least two of five ADLs, or had severe cognitive
impairment and six ADLs were specified in the Act. In 2000, an update to the Model
Regulation was completed which added a new section -- Section 28. The purpose of
this section was to assure that standards for qualified LTC insurance policies were
consistent with HIPAA.
Finally, there have been a number of changes at the NAIC level related to the
pricing of policies. Until the early part of this decade, insurers needed to certify that
policies were priced to achieve a 60% lifetime loss-ratio. This meant that at a statutory
interest rate (of 3.5%-4.5% depending on state) the policy had to pay out 60% in
benefits (claims payments) to consumers. As pricing became inadequate and insurers
had to increase rates, insurers had to certify that the pricing took into account
“moderately adverse conditions” and the minimum loss-ratio requirement was removed.
The intent was to assure that companies would not under-price their policies and that
premiums would be more stable over the life of the policy. To this day, the NAIC
remains the focal point for the regulation of LTC insurance.
The passage of HIPAA conferred favorable tax treatment to LTC policies that met
a series of standards set out in the law, the most important of which related to benefit
39
National Association of Insurance Commissioners (2009). Long-Term Care Insurance Model Act, Legislative
History, 640-21. October.
40
Ibid, 2009.

23
eligibility standards. HIPAA clarified the treatment of premiums for qualified plans as
medical expenses for individuals deducting medical expenses beyond 7.5% of their
gross income and by not taxing LTC insurance benefits up to certain limits. In addition
to standardizing policies, the law helped to signal to the market, that LTC insurance was
something that should be considered by the public. It appeared as a line item on every
federal income tax return.
On the other hand, few individuals actually purchasing the insurance would benefit
from the favorable tax treatment. This is because a policyholder would have to have
taxable income, very high medical expenses, and itemize expenses (rather than take
the standard deduction.)
41
The law did encourage states to begin to provide tax
deductions and exemptions for the purchase of insurance. In fact more than half the
states provide tax incentives for the purchase of LTC policies, and most of these are
linked to qualified policies.
42
Even so, there is little evidence that such policies have led
to a discernible effect on LTC insurance take-up rates. This is not too surprising given
that the value of incentives is fairly low compared to the costs of the policies
themselves.
43
There are a number of clear trends in the development of the industry in the 1990s
that laid the groundwork for many of the market exits that occurred in the subsequent
decade. These included the development of more comprehensive policies without
commensurate adjustments to premiums, pressure from agents to add benefit features
that served to confuse consumers and make the purchase decision more difficult, and a
likely underinvestment in risk management given the unknown nature of the morbidity
risk. While there was a rapidly developing regulatory infrastructure, many insurers felt
that the NAIC model act imposed requirements that added to the cost of the product
without a commensurate level of actual consumer benefit. Finally, tax benefits were
considered to be more ephemeral than real and were seen to have little impact on the
overall level of demand. Taken together, these factors all resulted in challenges to the
underlying profitability of the product, which is discussed in more detail below.
6. Long-Term Care Insurance Pricing and Profitability
The issue of profitability is one of many factors relating to why companies entered
the market but it is an absolutely central factor in understanding why many of these
same companies ultimately exited the market. Clearly, there was a belief that LTC
insurance could be priced and managed in a way that assured reasonable returns to
companies. The key drivers of profitability are embedded in the underlying pricing
assumptions used to develop premiums and are a function of company strategies
related to underwriting and claims management, product design, premium structure,
41
Baer, D. and O’Brien, E. (2010). Federal and State Income Tax Incentives for Private Long-Term Care Insurance.
AARP Public Policy Institute. Washington, DC.
42
Stevenson, D., Frank, R. and Tau, J. (2009). Private Long-Term Care Insurance and State Tax Incentives.
Inquiry 46:305-321. Fall.
43
Wiener, J.M., Tilly, J., and Goldenson, S.M. (2000). Federal and State Initiatives to Jump Start the Market for
Private Long-Term Care Insurance. Elder Law Journal 8(1):57-99.
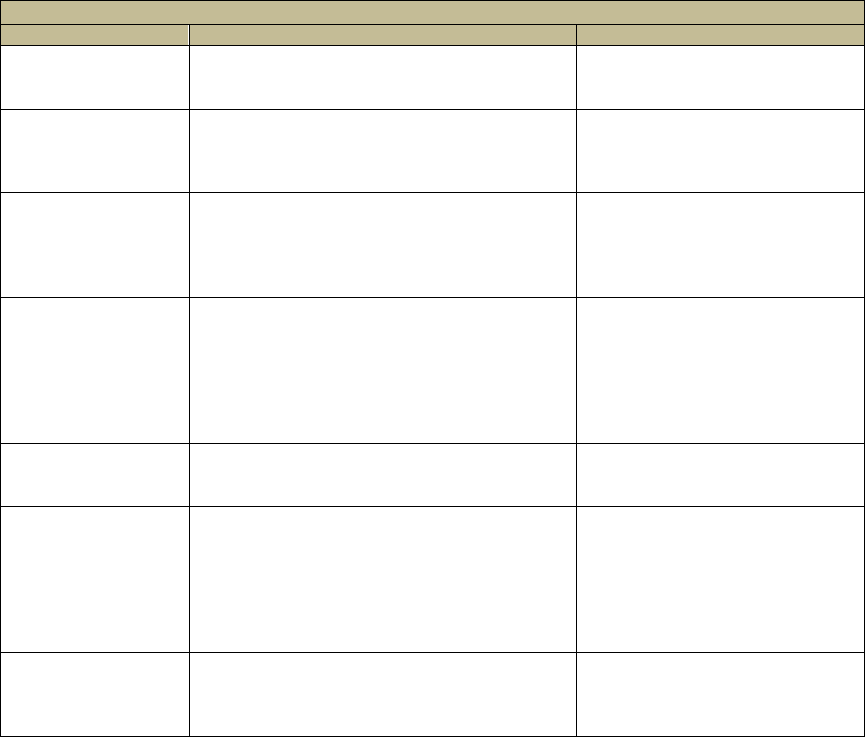
24
inflation adjustment rates, sales and marketing costs and investment strategies. Table
4 shows the key assumptions underlying the pricing of LTC insurance.
TABLE 4. Key Pricing Assumptions in Developing LTC Insurance Premiums
Pricing Parameter
Description
Typical Assumptions
Morbidity
The claims that are expected to be paid out
based on the specific benefit design of the
policy.
SOA Experience reports
National public data sources
Insured Experience.
Mortality
The underlying mortality table employed to
determine how long individuals who have
policies are expected to live and pay
premiums and collect benefits.
Annuitant mortality tables (e.g.,
1994, 2000).
Interest Rate
Because the product is level-funded, there is
a great deal of pre-funding occurring at early
durations of policy ownership and this is the
rate or return assumed on invested premiums
and risk-based capital (RBC).
1990s: 5% - 8%
2000s: 3% - 5%
Current: 2% - 4%
Voluntary Lapse
Rates
Not all individuals will hold their policies until
death. For a variety of reasons people may
cease paying premiums. High voluntary
lapse rates lead to lower premiums because
premium reserves from a lapsed policy are
retained by the company without related
future claim expenses.
1990s : 8% first year declining
to 4%
2000s: 6% first year declining
to 3%
Current: 4% first year declining
to 0.5%
Underwriting
Selection Effect
A group that is underwritten tends to be
healthier than a non-underwritten group and
this has a positive impact on the morbidity.
Claims reductions factors
typically wearing off within 5-7
years of policy issue.
Acquisition Costs
and Administration
These are the costs associated with
“producing” and servicing the policy and
include marketing and sales expenses
(commissions), underwriting, claims
management, ongoing policyholder billing
and premium collection and other
administrative expenses.
Sales costs typically greater than
60% of first year premiums and
then leveling out at lower levels.
Ongoing policyholder
administration and claims
management as a fixed per
policy fee or percent of premium.
Profit
This is the amount of load or additional
charge put into the product to assure an
adequate return for the insurer.
Profit measures including pre-tax
profits, post-tax profits, internal
rate of return (IRR), pricing to
lifetime loss-ratio.
Small variations in actual experience compared to expected performance of each
of the pricing assumptions can have a major impact on product profitability. In order to
demonstrate this, we developed a LTC insurance pricing model that allows us to
evaluate the impact of small changes in various pricing assumptions on overall product
profitability. Table 5 shows these impacts. Baseline profitability is defined as the
addition of a 10% margin on the premium that is generated to cover the present value of
all claims and expenses. Thus, the pre-tax profit margin is set at 10% of the premium.
What this model shows, for example, is that if a company assumed that it would be
able to earn 6.5% on its reserves, and instead, earned 5.5%, then depending on age,
premiums would have to increase between 5% and 10% to maintain the initial 10% level
of profitability as defined above. Again, depending on age, if the actual interest rate
earned on reserves was 5.5%, compared to the priced interest assumption of 6.5%,
then the profit margin would vary between 0.5% and 5.2%. This represents declines in
the margin of between 48% and 95%.
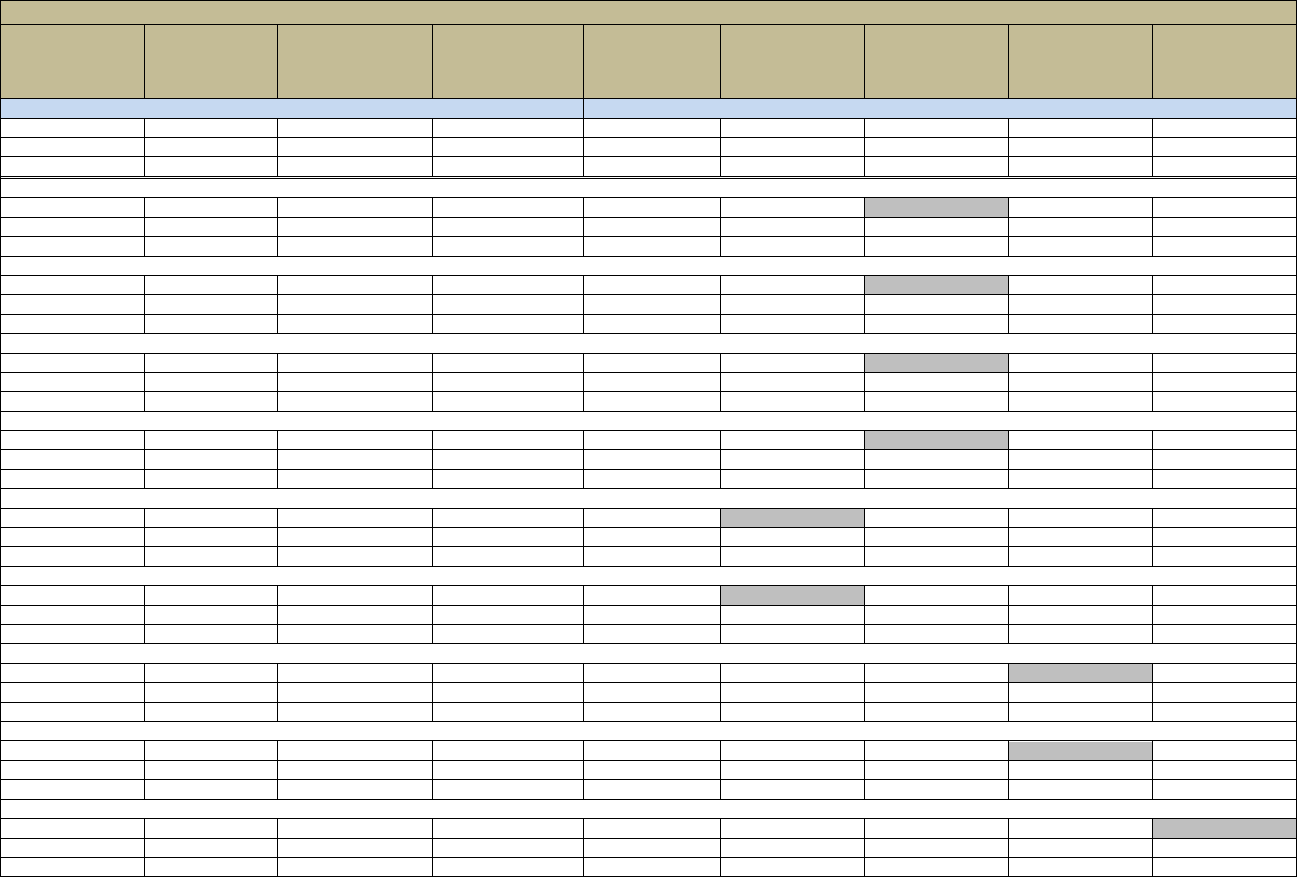
25
TABLE 5. Impact of Alternative Assumptions on Profitability of LTC Insurance
Change in
Profit Margin
(no change
in premium)
Profit Margin
(no change
in premium)
Required Change
in Premium Level
to Maintain
10% Profit Level
Premium
Needed to
Maintain
10% Profit Level
Age
Lapse
Interest
Morbidity
Mortality
BASE CASE
0%
10.0%
0%
$713
55
Standard
6.50%
Standard
Standard
0%
10.0%
0%
$1,379
65
0%
10.0%
0%
$2,149
70
-95%
0.5%
10%
$781
55
Actual
5.50%
Standard
Standard
-67%
3.3%
7%
$1,472
65
-48%
5.2%
5%
$2,252
70
-208%
-10.8%
21%
$861
55
Actual
4.50%
Standard
Standard
-142%
-4.2%
14%
$1,575
65
-100%
0.0%
10%
$2,364
70
-339%
-23.9%
34%
$955
55
Actual
3.50%
Standard
Standard
-224%
-12.4%
22%
$1,688
65
-156%
-5.6%
16%
$2,485
70
-492%
-39.2%
49%
$1,064
55
Actual
2.50%
Standard
Standard
-315%
-21.5%
31%
$1,813
65
-216%
-11.6%
22%
$2,614
70
102%
20.2%
-10%
$640
55
Better
6.50%
Standard
Standard
75%
17.5%
-7%
$1,276
65
54%
15.4%
-5%
$2,034
70
-52%
4.8%
5%
$750
55
Worse
6.50%
Standard
Standard
-39%
6.1%
4%
$1,433
65
-30%
7.0%
3%
$2,213
70
90%
19.0%
-9%
$649
55
Actual
6.50%
Lower
Standard
94%
19.4%
-9%
$1,250
65
96%
19.6%
-10%
$1,943
70
-90%
1.0%
9%
$777
55
Actual
6.50%
Higher
Standard
-94%
0.6%
9%
$1,509
65
-96%
0.4%
10%
$2,355
70
22%
12.2%
-2%
$697
55
Actual
6.50%
Standard
Higher
23%
12.3%
-2%
$1,347
65
21%
12.1%
-2%
$2,104
70

26
TABLE 5 (continued)
Change in
Profit Margin
(no change
in premium)
Profit Margin
(no change
in premium)
Required Change
in Premium Level
to Maintain
10% Profit Level
Premium
Needed to
Maintain
10% Profit Level
Age
Lapse
Interest
Morbidity
Mortality
-25%
7.5%
3%
$731
55
Actual
6.50%
Standard
Lower
-25%
7.5%
3%
$1,414
65
-22%
7.8%
2%
$2,196
70
SOURCE: LifePlans Long-Term Care Insurance Pricing Model, 2012.
Assumptions: 5 year policy; $100/ day; 10% margin; 60% minimum loss-ratio.
Better claims = 10% lower than priced; Worse claims = 10% higher than priced.
Better mortality = 10% higher than priced; Worse mortality = 10% lower than price.
Better lapse = 1 percentage point higher than priced; Worse = 1 percentage point lower than priced & year 7+ ultimate lapse rate of 0.25% versus 0.75%.
27
As shown, a percentage point difference in the underlying interest rate assumption
has a very major impact on underlying profitability. Moreover, the impact is most
pronounced at the younger ages. As well, even small errors on multiple assumptions
can lead to major changes in the product’s underlying profitability. Finally, the
assumptions are subject to a wide degree of volatility given changes in the provider
landscape, trends in disability rates, macro-economic policy vis-à-vis aggregate interest
rates, and other factors. Thus, it is not surprising that given the level-funded nature of
this product, along with the long-tail morbidity risk, the product is viewed as inherently
more risky than other insurance products, and regulated in a way that requires greater
levels of capital to support it.
Noteworthy is the fact that since the late 1990s, all of these major determinants of
premium and product profitability have been going in the wrong direction: interest rates
are significantly lower than what was priced for, voluntary lapse rates are lower than for
any other insurance product, morbidity is somewhat worse than expected and mortality
is actually improving. For these reasons, the prior decade saw a major exodus of
companies from the market, as returns on the product have been significantly below
expectation. More recently, major ratings agencies have highlighted the poor profit
results of companies and issued reports cautioning about the future of the industry.
44
C. The Decision to Exit the Market
With few exceptions, most companies that stopped selling LTC policies did so over
the past decade. Table 6 shows the distribution of companies by market exit year. It
shows that more than half of companies in the sample have exited the market (or
specific market segments) in the past eight years. The largest number of companies
exited the market in 2003 and 2010.
There does not seem to be any discernible difference between those companies
that chose to exit the market earlier rather than more recently. Most companies made
the decision to exit the market within a year of considering such a strategy and roughly
a quarter within six months. Thus, once these companies seriously began re-evaluating
the desirability of remaining active in the market, it did not take long for them to make a
final decision to leave the market.
44
Moody’s Investor Services. (2012). Special Comment: Long-Term Care Insurance: Sector Profile. September 18.
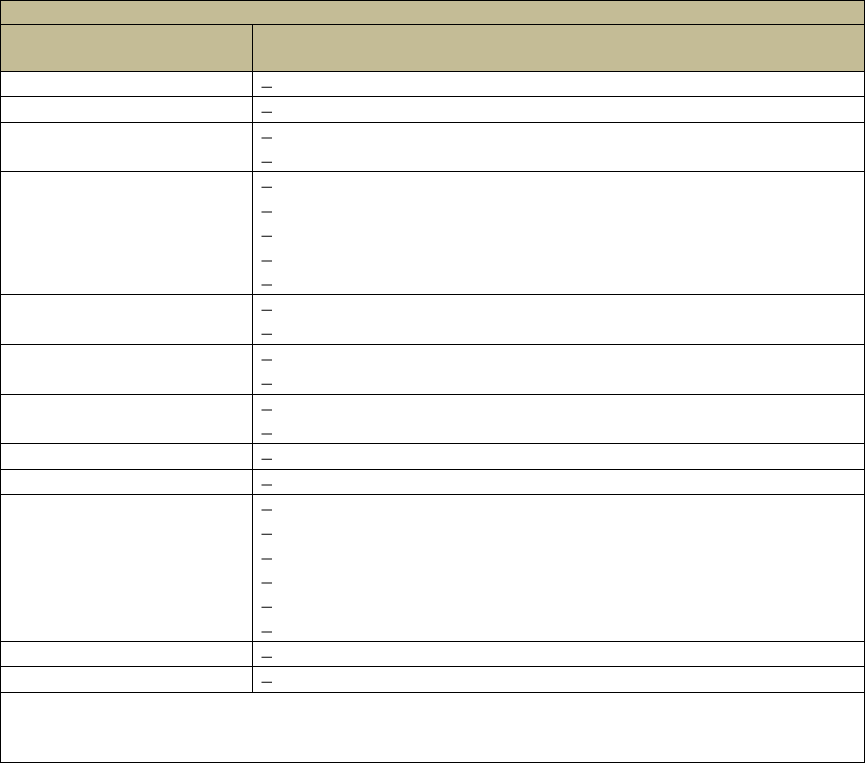
28
TABLE 6. Distribution of Sample by Year of Market Exit
Year of
Market Exit
Sample
1996
Principal Financial Group
2001
Nationwide
2002
American Fidelity Assurance Company
Standard Life & Accident Insurance Company
2003
American Family Mutual Insurance Company
CNA
Conseco
RiverSource Life Insurance Company
Union Labor Life Insurance Company
2004
Medico
Teachers Protective Mutual Life
2005
Humana Insurance/Kanawha
Transamerica (re-entry 2010)
2006
Aetna
Southern Farm Bureau Life
2008
Penn Treaty
2009
UNUM Individual
2010
Allianz
CUNA Mutual
Equitable
Great America Financial
John Hancock (group market)
MetLife
2011
Guardian--Berkshire
2012
Prudential, UNUM Group
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment
of the market and analysis of NAIC Experience Exhibit Reports from 2000, 2009, 2010 and
2011
We asked executives to highlight all of the reasons why the company left the
market (Table 7) and the single most important reason for doing so (Figure 8). In broad
terms the reasons can be related to profit, risk, internal management, sales and
distribution, public and regulatory policy, or other issues posing challenges to
companies.
As shown, product performance, that is, not hitting profit objectives was the most
cited reason for leaving the market. Incorrect assumptions about two underlying pricing
assumptions -- voluntary lapses and interest rates -- have had a lot to do with this and
have been key drivers behind the need of many companies to increase rates on
products. The concern about the ability to obtain needed rate increases from state
insurance departments was the second most cited reason for market exit. Slightly more
than half of respondents also cited high capital requirements as a reason for exiting the
market. It is noteworthy that only a single company cited an unfavorable public policy
environment specifically as a reason for exiting the market.
29
TABLE 7. All of the Reasons Cited for Exiting the Market
Reasons
Percent
Responses
Profit Issues
Product performance--not hitting profit objectives
69%
18
Product performance not hitting profit objectives
quickly
8%
2
High capital requirements
54%
14
Risk Issues
Concern about ability to get rate increases if
necessary
62%
16
New evaluation/assessment of the risk of product
and market
50%
13
Lack of confidence in ability to manage risk
42%
11
Could not get reinsurance or partner with whom to
share risk
19%
5
Internal Management Issues
Reputation Risk
23%
6
Pressure from Rating Agencies
23%
6
Pressure from Board of Directors
8%
2
New Senior Management not interested in the
product
39%
10
Sales and Distribution Issues
Too difficult to sell (consumer-related)
27%
7
Distribution issues (agent-related)
23%
6
Intense competition
15%
2
Regulatory/Public Policy Issues
New regulatory requirements
19%
5
Unfavorable public policy
4%
1
Other (please specify)
50%
13
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment
of the market.
Figure 8 highlights the point that a high capital requirement to support the product
was cited most frequently as the most important reason for market exit. Product
performance is the second most cited reason. Some of the other reasons cited include
a concern that a continued focus on LTC insurance detracted from other core products,
that tax qualification guidelines inhibited certain innovative product designs, and others.
In terms of classifying these reasons into major categories, slightly less than half are
related to profitability, about a quarter to risk issues and a quarter split out across the
other reasons.
It is important to note that some of the reasons -- particularly those related to
changes in the outlook of upper management -- are likely “intermediate” factors. That
is, if senior management wanted to exit the market, it was likely related to the fact that
business objectives were not being met, or they had a different evaluation of the risk,
etc. In some cases, it likely required a new CEO to take a fresh look at the business
which led to a market exit.
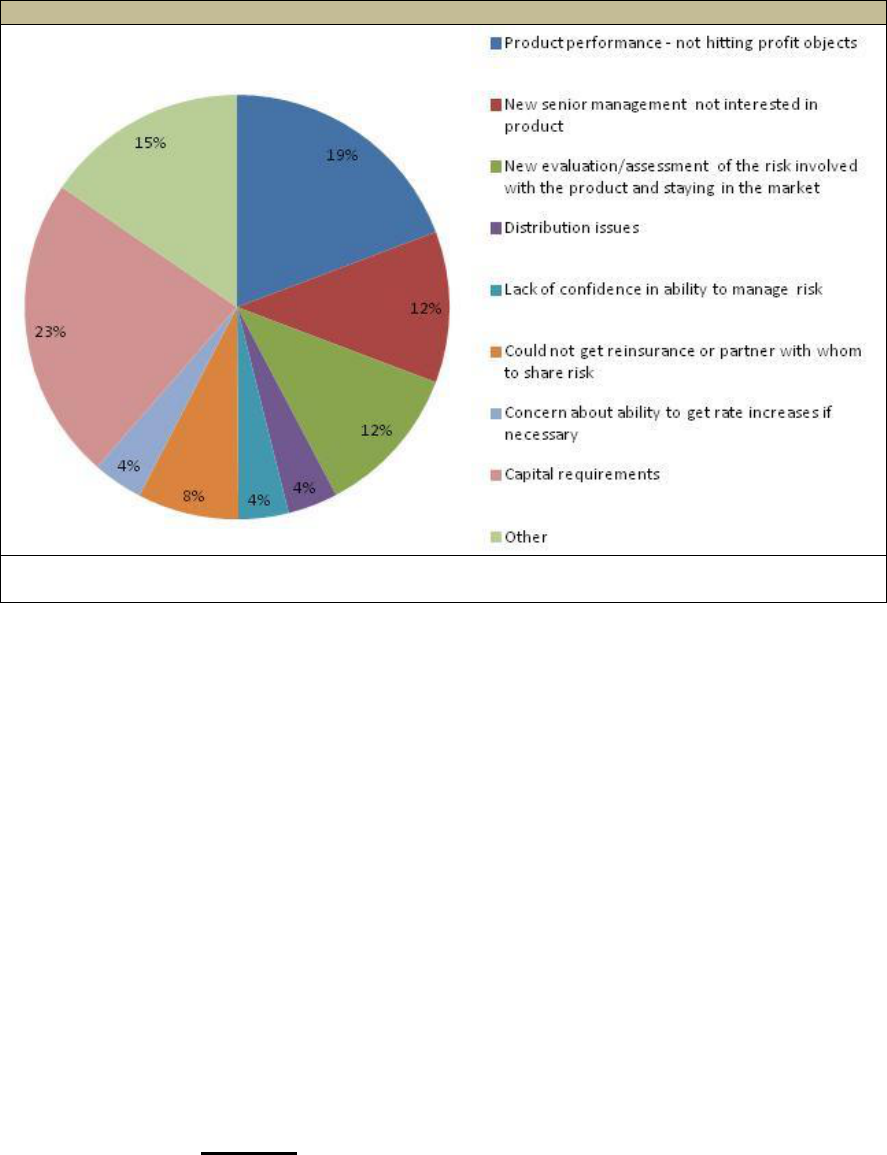
30
FIGURE 8. Single Most Important Reason that the Company Left the Market
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment of
the market.
Concerns related to capital requirements and rate increases may represent
something unique about the structure and regulatory requirements relating to LTC
insurance that have a major impact on profitability. LTC insurance is a guaranteed
renewable product which means that as long as an individual pays premiums, the
insurance company must continue to honor the coverage. Premiums are not
guaranteed, although they are designed to be level-funded over the life of the policy.
This means that if the actual experience of any of a number of underlying pricing
assumptions (claims, interest rate, mortality, voluntary lapse rates, etc.) varies from
what was anticipated, the financial viability of the product can be threatened, unless
there is an adjustment to rates.
Rate adjustments can only occur with the permission of individual state insurance
departments. Rate increases would typically be sought for policies that have been in
the market for enough time to gain credible experience. This means that policyholders
would typically be older and more likely to be on fixed incomes at the time that a
company might be seeking a rate adjustment. Given the sensitivity around increasing
rates for older policyholders, it is not surprising that companies are concerned about
their ability to raise rates; in fact, many companies have experienced significant
challenges obtaining the level of rate increases that they request, even when such
increases may be actuarially justified. For example, a company may request (and
require) a 35% rate increase, yet be allowed to adjust premiums by only 15%. This
does not mean that regulators have ignored requests for rate adjustments. With few
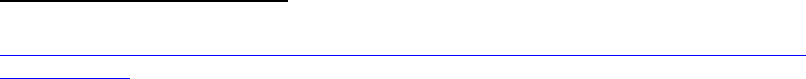
31
exceptions, most companies have increased rates on some if not all of their policy
series, and clearly the increases have been significant.
45
The failure to hit profitability targets as a reason to leave the market was pervasive
in the interviews with executives. Therefore it is important to understand what is meant
by profitability and how it is measured in evaluating the success of a product. Profit can
be defined differently by companies and the application of various standards affects
premium levels. Some of the more common profit standards include: (1) a pre-tax
measure (e.g., 10% of gross premium); (2) a post-tax measure (e.g., 5% of some level
of the RBC allocated to support the product); (3) pricing to a specific lifetime loss-ratio
standard (e.g., 60% at a conservative earnings or interest assumption); or (4) an IRR
(e.g., 15%). Even when all other assumptions are held constant, use of an alternative
profit standard can yield significant differences in premiums. For example, for a 62 year
old, everything else held constant, using a 10% pre-tax standard compared to a 15%
IRR calculation leads to a premium that is roughly 10% lower.
46
The post-tax profit
measure focuses on a target rate of return on RBC -- which is the level of capital that a
company is required to allocate to support the product.
The calculation behind the level of capital required to support insurance products
was set by the Risk-Based Capital for Insurers Model Act which went into effect in
1992/1993 for life and health companies. A company’s RBC is monitored by both state
regulators and A.M. Best or other rating agencies. State regulators use an RBC model
that is developed and maintained by the NAIC. The purpose is to require companies to
measure their capital allocation compared to a standard risk-based calculation of
needed capital.
47
In essence, the idea is to determine the minimum capitalization that is
appropriate to a company’s risks. While the exact formula will depend on the specific
type of insurance, in general there are four risk areas that are typically considered: C1 is
credit risk; C2 is pricing risk; C3 is interest rate risk, and; C4 is other business risks.
The key risks that are the focus of LTC insurance include C2 and C3.
At the core of the NAIC model is a formulaic approach to developing a “Company
Action Level (CAL)” of capital and then generally relating actual capital to this CAL. For
example, if a company’s CAL is $100M and its actual capital is $400M it would have a
400% RBC ratio. Regulators monitor this ratio and various actions generally result if
this ratio falls below certain target levels.
48
For many years, the RBC level on the C2
(i.e., pricing risk) had been to establish a level equal to 5% of claim reserves, plus $25
million of the first $50 million in premiums and 15% on all additional premium beyond
that. The formula now reflects a lower percentage (10% instead of 25%) applied to
45
California Department of Insurance Website relating to rate histories of LTC insurance companies.
http://www.insurance.ca.gov/0100-consumers/0060-information-guides/0050-health/ltc-rate-history-
guide/index.cfm.
46
Helwig, D. (2005). The Basics of Long-Term Care Insurance, New Orleans Life Spring Meeting, May 22-24,
Record, Volume 31, Number 1, Society of Actuaries.
47
Meilender, B. (2003). Risk Based Capital, 2003 Valuation Actuary Symposium, San Diego, CA. September 11-
12, 2003. Session 37 PD, Society of Actuaries, 2004.
48
Charsky, D., FSA and Nelson, R., FSA (2012). Personal Communication. December 28.
32
premiums and an additional component related to claims. The intent was to hold higher
levels of RBC as claims increased and to match the level of required capital to the
actual pattern of risk in the product.
Again, the capital requirements for LTC insurance are high relative to other
products such as health and life insurance. High capital requirements are due to the
long-term nature of the coverage and other “unknowns” which make the product
inherently more risky. Thus, the actual required capital is very high per dollar of earned
premium or reserves because of the perceived product risk, the long-term nature of the
guaranteed renewable coverage, and the fact that rating action impacts are muted as
policyholders continue to age.
49
Also, and in particular, with respect to policies with
inflation protection, the capital strain is often large in the early years of a policy because
sales commissions, underwriting and issue, taxes, and administrative expenses are
large relative to earned premium. For that reason, it is not uncommon for companies to
show financial losses in the first 2-3 years after a policy is sold and then show ever
increasing reserves for many years and continued losses. While claims may be low
during these initial years, expenses are high and for inflation policies, reserves high.
Thus, at the very least, for the product to be profitable over its lifetime, it must generate
returns that take account of the initial 1-3 years of expense-associated losses.
FIGURE 9. Moody’s Yield on Seasoned Corporate Bonds--All Industries, AAA and
Ten Year U.S. Treasury Note Yield Rate
49
Personal communication with Don Charsky, FSA President of Ability Re and Ray Nelson, FSA Senior Actuary at
Ability Re.

33
This would not be a major issue if the actual or expected returns on capital were
strong. However, that has rarely been the case. In addition to voluntary lapses being
lower than anticipated (resulting in premiums being lower than necessary), interest rates
have also been lower than anticipated, resulting in earnings on invested reserves that
are lower than anticipated. More specifically, an analysis of rates of return on Triple A
(AAA) corporate bonds and U.S. Treasure Notes over the last two decades highlights
why so many companies exited the market in the last 7-10 years -- yields on both types
of investments have experienced very major declines.
50
Between 1992 and 2002,
yields on Corporate Bonds were typically above 6.5% whereas in 2003, they began a
precipitous decline such that by 2010, they had fallen to below 5%. For Treasuries,
yields dropped to below 4%. The vast majority (85%) of companies that exited the
market did so from 2003 through 2010, which correlates closely to this decline in yields.
In addition to absolute declines in returns on invested capital, when carriers point
to required capital as a reason for exiting the market, they are also viewing constrained
capital in light of expected returns from other lines of business. If profits do not emerge
at either the rate or levels expected, then economic pressures will lead companies to
allocate such capital to products offering higher returns. The high “hurdle rate” needed
to justify the allocation of capital to the LTC insurance product line is particularly
sensitive to the interest rate environment, given the level-funded nature of the product.
While for most companies the primary motivations for leaving the market were
related to high capital requirements and the seeming inability to meet profit objectives,
many factors converged and played a role in the decision. Some of these were related
to challenges around marketing and sales, risk management strategies, regulatory
policy, the lack of reinsurance coverage and others. Executives were asked to indicate
whether a specific factor “Strongly influenced the decision to leave the market”,
“Somewhat influenced the decision to leave the market” or “Did not influence the
decision to leave the market at all”. Table 8 on the following page summarizes results.
There are a number of important points to be made about the data presented in
Table 8. First, consistent with prior results, the factors cited most often as having the
strongest influence on the decision to exit the market included high capital requirements
and pressure to reallocate capital to other more profitable business lines due to
profitability challenges. As well, roughly one-in-three respondents indicated that the
level-funded nature of the product made it particularly susceptible to investment risk
(i.e., interest earnings), and there were few ways to successfully mitigate this risk.
50
Note that not all companies hold assets in AAA bonds, but many of them do. In general and across various asset
classes in which companies typically invest, returns have declined over the period.
34
TABLE 8. Factors Influencing the Decision to Exit the Market
Factor
Strongly
Influenced
the Decision
Somewhat
Influenced
the Decision
Did Not
Influence
the Decision
Marketing and Sales
The required commission schedules to
attract agents made the product very
expensive.
---
19%
81%
It was difficult to recruit agents to sell the
product.
8%
8%
84%
The amount of agent training required by
regulations was excessive.
8%
8%
84%
LTC insurance was too difficult to sell.
8%
15%
77%
Marketing of and education about the
product became too costly.
---
15%
85%
Risk Management
Finding experienced actuaries became
difficult.
8%
12%
80%
Finding underwriters and claims
adjudicators who knew about LTC
insurance risk became difficult.
---
15%
85%
Underwriting and claims management
tools were not adequate to manage the
risk.
---
19%
81%
In a rapidly changing service environment
it became difficult to enforce original
provisions of the policy.
---
24%
76%
Denying claims became too much of a
reputation risk.
---
11%
89%
It became too difficult to mitigate
investment risk.
28%
24%
48%
There was too much bad publicity
regarding rate increases.
---
27%
73%
The costs associated with managing the
product became too high.
15%
43%
42%
Morbidity was worse than expected.
---
50%
50%
The incidence of fraudulent claims was too
high.
---
8%
92%
Regulatory Policy
Regulations encumbered product
development/innovation and sales.
15%
15%
70%
Regulations encumbered the ability to do
adequate risk management.
27%
35%
38%
The cost of regulatory compliance became
too high.
15%
19%
66%
State insurance departments would not
approve necessary rate increases (at all or
in a timely manner).
23%
31%
47%
We were concerned that the NAIC or state
insurance department would pass a model
regulation that would be applied to policies
retroactively.
12%
19%
69%
Availability of Reinsurance
It was difficult to acquire high value
reinsurance coverage.
15%
31%
54%
Requirements of the reinsurer were too
stringent for us.
15%
12%
73%
35
TABLE 8 (continued)
Factor
Strongly
Influenced
the Decision
Somewhat
Influenced
the Decision
Did Not
Influence
the Decision
Capital Costs and Profits
Capital requirements became too high
50%
15%
35%
High capital costs caused constant
pressure to reallocate capital to products
with more rapidly emerging profits
31%
12%
58%
Emergence of profits was too slow
35%
15%
50%
Level funding made the product too
dependent on interest earnings
35%
31%
34%
Other Factors
We were concerned that a negative rating
on LTC insurance business would
negatively affect other business lines
23%
38%
39%
Public policy was unsupportive of the
product
---
15%
85%
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment
of the market.
Second, issues relating to marketing and sales were not cited frequently as having
a major or even moderate influence on the decision. Third, finding skilled staff for
underwriting, claims and actuarial analysis has not played much of a role in the decision
nor have issues related to enforcing policy provisions in the context of a changing
provider landscape. In contrast, half of respondents indicated morbidity experience was
worse than they had anticipated and this influenced their decision to exit the market. On
a cumulative basis, most of these companies actual claims experience was better than
what was anticipated; that is, the actual-to-expected loss-ratio was less than 100%.
However, more recent claims experience suggested that claims costs were increasing
at a rate higher than expected, and that this did not bode well for projected future
profitability. (See Figure 11.)
Clearly, all of the activity related to risk management has costs which must be
absorbed or built into the underlying pricing of the product. As morbidity experience has
deteriorated for a growing number of companies, it is not surprising that companies are
investing significant resources in risk management -- not sales -- activities. Roughly
two-in-five respondents indicated that the costs associated with managing the product
have become too high and this has been one of the factors that has led them to exit the
market.
Regarding regulatory policy, the most cited factors having a moderate influence on
a company’s decision to exit the market have to do with the ability to obtain rate
increases in a timely manner or at all, as well as having the necessary flexibility to
engage in appropriate risk management activities; roughly one-in-three companies
indicated that this had a moderate impact on their decision. The costs of regulatory
compliance and the possibility that such compliance encumbers product innovation
were not seen as factors in the market exit decision.
A number of companies have reinsurance partners that enable them to share or
spread the underlying risks in the product. For some companies, the ability to obtain
36
reinsurance coverage is a pre-requisite to either entering or staying in the market. For
two of the companies, the difficulty of obtaining such coverage or of meeting the
requirements of the reinsurer proved to be very important to their decision to leave the
market. For roughly one-in-three carriers, the difficulty of obtaining such coverage had
some level of influence on their decision, but it was clearly not a dominant factor. It is
noteworthy that over the last five years the number of reinsurance companies providing
coverage for stand-alone LTC insurance policies has declined and that today, only 1-2
companies provide such coverage. Surveys of executives in these reinsurance
companies suggest that capital requirements and inadequate returns were primary
drivers of their exit from the market as well. The fact that these companies have also
exited the market reinforces findings about the inherent level of risk in the product (as it
is currently configured).
Finally, more than half of companies were concerned that a negative rating on their
LTC insurance business would adversely affect other business lines, and this played
some role in their decision to leave the market. This is because most writers of LTC
insurance are multi-line companies and for the most part this insurance represents a
small component of their overall portfolio. Again, it is worth mentioning that very few
companies felt that an unsupportive public policy played a role in their decision to exit
the market.
In addition to “missing” the interest and voluntary lapse assumptions, another
reason for falling short on profitability assumptions relates to morbidity. Companies
typically focus on two performance measures related to this parameter: the annual and
cumulative loss-ratio and the actual-to-expected loss-ratio. The loss-ratio focuses on
the relationship between claims and premiums and can be viewed on the basis of a
single year (e.g., claims incurred during the year compared to premiums earned during
the year) or on a cumulative basis (e.g., total claims incurred to date compared to total
premiums earned to date). The higher the loss-ratio, the greater are claims in relation
to earned premiums. Over the life of a group of policies, claims payments will ultimately
exceed the amount of annual premium payments; the difference is expected to be paid
for by the reserve that the company sets up. The reserve is funded in large part during
the years where annual premium exceeds the level of annual claims incurred. It is the
excess premium plus the interest earned on that excess premium that funds the future
gap between premiums and claims.
Figure 10 highlights the annual industry-wide loss-ratio as well as the cumulative
loss-ratio.
As expected, claims represent a growing percentage of premium payments over
time. This reflects both the aging of the in-force policyholder base as well as the
wearing off of the underwriting effect on morbidity. The slow-down in sales of new
policies -- with lower initial annual loss-ratios -- also contributes to the rate at which
such ratios are increasing for the industry. The growth in the loss-ratio does not
represent a problem for the industry so long as the premiums collected are sufficient to
fund the expected liabilities priced into the policy. What it does show is how claims are
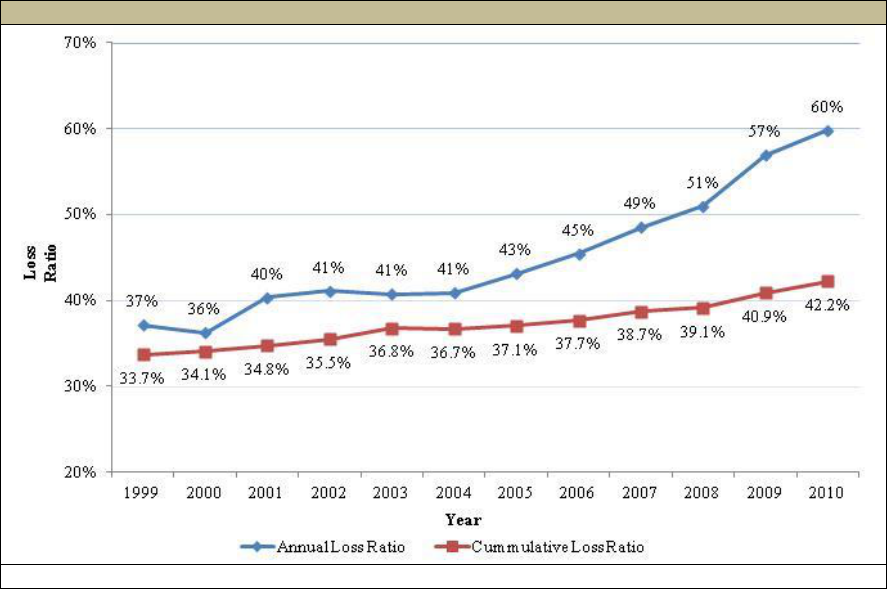
37
growing and this is typically compared to what the ratio was expected to be. Thus, the
most important performance measure is whether or not the actual incurred claims by a
company are in line with expected claims paid.
FIGURE 10. Annual and Cumulative Loss-Ratio
SOURCE: NAIC Experience Reports, 2011.
If a company anticipated that during a specific year its incurred claims compared
to its earned premiums would be 50%, and in fact the ratio of incurred claims to
premiums was actually 55%, this would indicate worse than anticipated experience.
The converse is also true: if a company expected to pay out in claims the equivalent of
50% of its earned premium, and instead paid out 45%, this would suggest better than
anticipated experience. An actual-to-expected ratio of 100% suggests experience is
exactly in line with what was anticipated.
The expected claims underlying the pricing in a policy represent the best estimate
for the amount of money that the insurer is going to need to pay out on an annual basis,
given the age, gender, marital status, and health status of policyholders. Typically
companies develop this “morbidity” or “claims cost” curve based on a set of
assumptions related to: (1) the probability of someone becoming disabled in a certain
year (incidence rate); (2) the probability that once disabled, an individual will require
paid care for a certain amount of time (continuance risk); (3) the intensity of care
required while the individual is disabled (intensity risk), and; (4) the level of service cost
in relation to the daily benefit chosen by the individual to pay for care. The claims cost
assumptions are a key input to the overall pricing of the policy -- see Table 4 -- and
once filed with the state, these assumptions become the basis on which reporting and
performance is monitored. If the actual experience does not conform to the initially
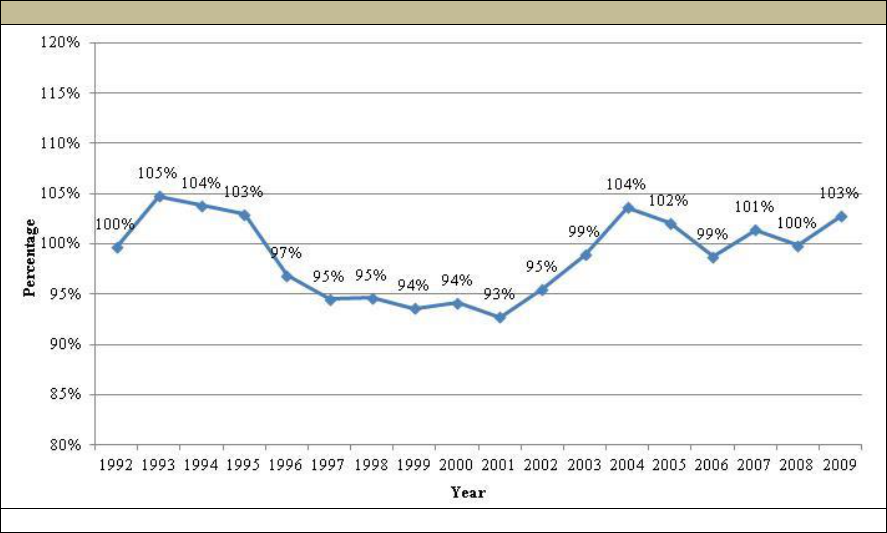
38
priced assumptions, companies can request rate relief from state insurance
departments and they would be required to file a new set of claims assumptions, which
would result in changes to premiums.
Figure 11 shows industry-wide average cumulative actual-to-expected losses
between 1992 and 2009.
FIGURE 11. Industry-Wide Actual Losses to Expected Losses
SOURCE: LifePlans Analysis of NAIC Experience Reports, 2010.
As shown, there has been variability in cumulative industry performance over the
last decade. If we focus exclusively on the last six years, in four of six of these years the
actual-to-expected loss experience has been over 100%; the average ratio over the
past six years has been 102%; this compares to a ratio of 95% in the preceding eight
years. Moreover, given this represents cumulative experience, for the ratio to increase
by three percentage points between 2008 and 2009 suggests that the annual
performance for that year must have been much worse than this.
As mentioned, in 2009 the NAIC changed its reporting format for companies and
experience tracking for the new format. Data in these reports is not directly comparable
to data from earlier reports because certain methodologies had changed regarding
calculation of the actual-to-expected loss percentages. In the context of the new
reporting, and as shown in Figure 12, based on recent data on the annual actual-to-
expected incurred claims, experience over the last three years has been worse than
what was priced for.
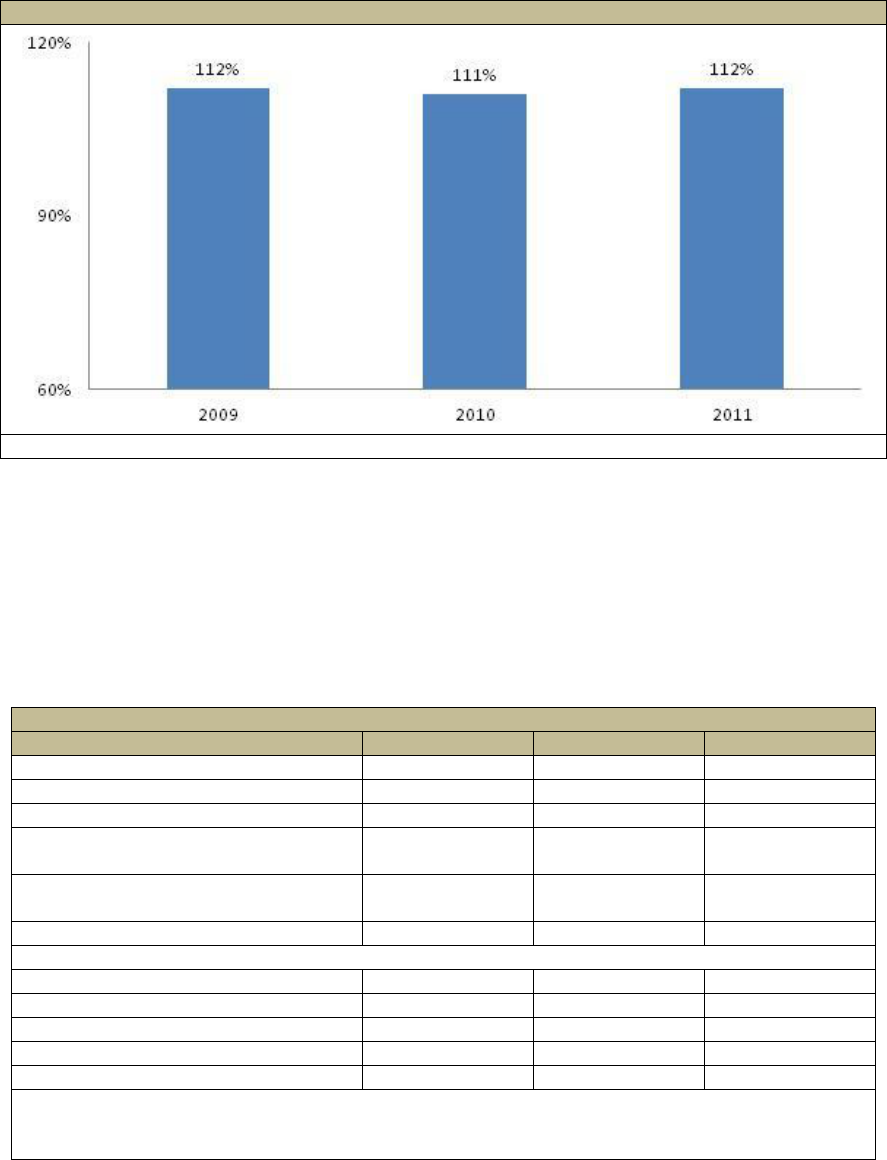
39
FIGURE 12. Industry Actual to Expected Annual Incurred Claims: 2009-2011
SOURCE: NAIC Experience Reports, 2012.
To obtain a summary view of industry change on key market indicators, we present
data from the beginning and end of the decade, including information on market
concentration. As shown in Table 9, market concentration has increased over the
decade, with the top ten companies now accounting for slightly more than two-thirds of
covered lives and the top five accounting for more than half of all policyholders. Given
the recent exodus of additional companies from the market, such concentration is likely
to grow.
TABLE 9. Summary of Key Industry Parameters: 2000-2010
Industry Parameter
2000
2010
Change
Earned Premium
$5,155,000
$10,614,816
106%
Incurred Claims
$1,870,000
$6,350,413
240%
Loss-Ratio
36%
60%
67%
Actual Losses Incurred to Premiums
Earned (%)
34%
42%
24%
Actual losses Incurred to Expected
Losses Incurred (cumulative)
94%
103%
a
10%
Number of Covered Lives
4,497,120
7,263,283
62%
Industry Concentration: Number of Covered Lives
Top 5
41%
55%
34%
Top 10
63%
69%
10%
Top 15
74%
78%
5%
Top 20
81%
84%
4%
Carrier with Largest Market Share
10%
15%
50%
SOURCE: LifePlans Analysis of NAIC Experience Reports, 2011.
a. The 103% figure is for 2009.
In addition to identifying the motivations for leaving the market, we also asked if
there were specific actions that were taken in support of staying in the market. Figure
13 shows that most companies changed product design and also changed rates on
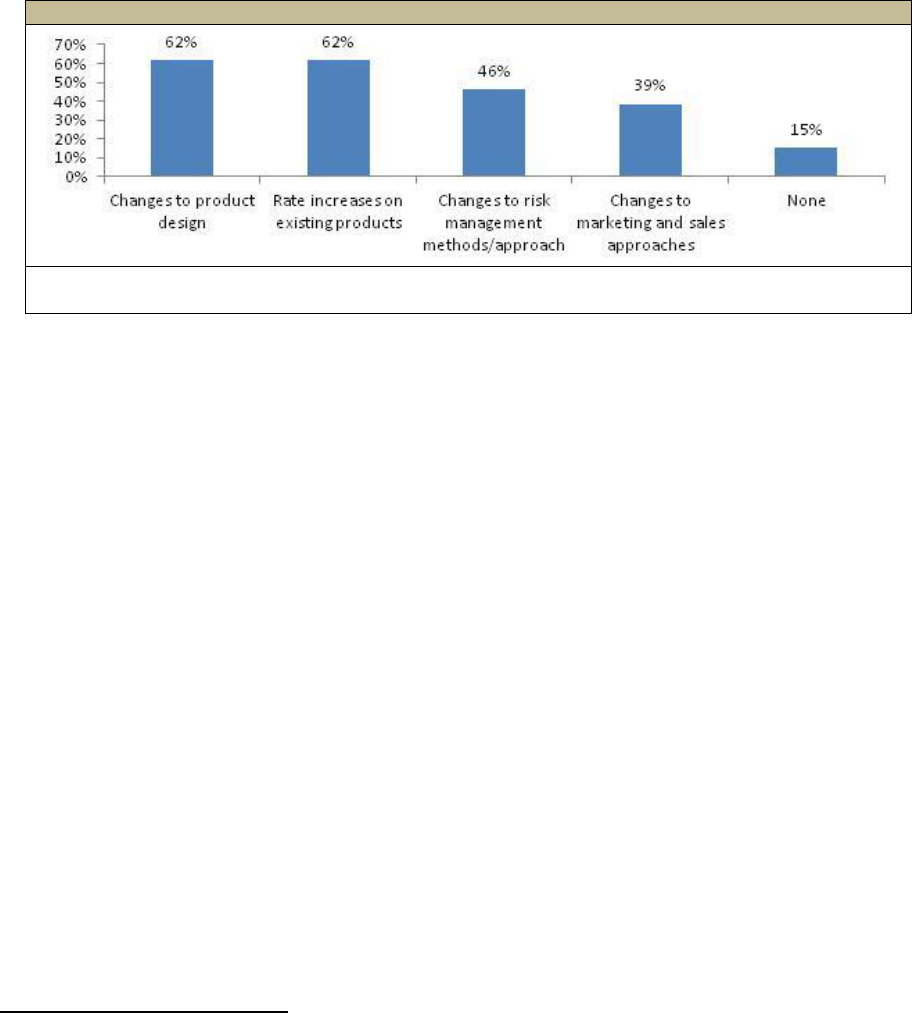
40
existing products. As well, more than two-in-five and one-third respectively changed
their risk management techniques and tried new approaches to marketing and sales.
Not shown in the figure is the fact only three of these companies (12%) have not raised
rates on existing policies. For the remainder of companies, roughly two-thirds raised
rates before they left the market. Only three companies left the market because of a
sense that they needed to raise rates and this would make ongoing sales extremely
difficult.
FIGURE 13. Actions taken Prior to Leaving the Market
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment of
the market.
Clearly, these actions represent most of the “levers” that a company can pull to
influence underlying product profitability. We know for example that companies
changed product designs, tightened up their approaches to underwriting and claims
management, and increased premiums. Some of these actions can only influence
performance on new policies issued (e.g., underwriting approach, marketing
approaches, and policy design changes) whereas others can also affect the
performance of older policies (e.g., rate increases and claims management strategies).
Although not explicitly addressed in this study, we also know that the specific
investment strategy vis-à-vis RBC and premium reserves has a major effect on
profitability. While companies have little control over general interest or inflation rates,
there are hedging strategies that can be undertaken to improve product performance.
Such strategies are important because insurers are paying fixed rates on forward
contracts; that is, premiums are received on an ongoing basis and they have to be
invested in assets that mature around the expected payout dates.
51
This can cause a
mismatch between future cash inflows and outflows because payouts can be influenced
by macro-economic trends that are outside of the control of the carrier.
Although few companies indicated that the need for rate increase activity is what
drove them to leave the market, there was general concern across companies about the
impact that this would have on sales. We asked respondents how concerned they were
with being able to continue selling the product if rates on the product had to be raised.
Figure 14 shows that roughly two-in-five respondents were somewhat or very
51
Helwig, D., Bhandula, R. and Barrett, N. (2007). Long-Term Care: Hedging Your Bet. Long-Term Care News,
Long-Term Care Insurance Section, Society of Actuaries. December.

41
concerned, and this had more to do with reputation risk and the impact on consumer
confidence than it did with losing business to a competitor.
FIGURE 14. Level of Concern about Selling the Product if In-force Rates
had to be Raised
SOURCE: Survey of executives from 26 LTC carriers who exited the market or exited segment
of the market.
D. Current Market Activity
Given the dramatic changes in market participation over the last decade, it is
challenging to obtain an accurate count of the total number of companies selling policies
in the marketplace. Some companies report sales of less than ten policies a year and
others show no policies in one year and then a small number of policy sales in a
subsequent year. In the year 2000, AHIP conducted a survey and found that 125
companies were selling policies in the marketplace; by 2002, however, this number had
fallen to 104 -- a 17% decline in just two years.
52
This survey has not been replicated
since 2002.
Today, the most reliable source of information on company-specific activity is
provided by the NAIC. Their most recent report, published in 2011, focuses on the top
100 companies reporting premium and claims information on any LTC insurance
policies that they have in-force in 2010. The report showed that fewer than 20
companies were actively selling stand-alone LTC policies in 2010; by 2012, only 11
companies were selling at least 2,500 new stand-alone individual or group policies
annually in the marketplace.
53,54
It is important to note that these figures do not include
companies that are selling various combination-products such as Life-LTC or Annuity-
52
America’s Health Insurance Plans (2004). Long-Term Care Insurance in 2002. Research Findings, Washington,
DC. June.
53
LifePlans, Inc. (2012). 2011 Long-Term Care Top Writers Survey Individual and Group Association Final
Report, Waltham, MA. March.
54
This figure is difficult to determine with precision. Broker World estimates that in 2010 there were 25 companies
selling stand-alone policies, but many of these were selling a very small number on an annual basis.

42
LTC products. These products still account for a very small -- but growing -- part of the
overall market. Some view such combination-products as the wave of the future for the
industry and the most promising way to increase the number of people covered by
insurance. Moreover, given some of the off-setting risks in these products, they may
also exhibit more premium stability over time, thus enhancing their attractiveness in the
market.
During 2012, companies writing at least 2,500 policies include:
55
Bankers Life and Casualty
Genworth Financial
John Hancock Financial Services (Individual Market)
Knights of Columbus
MassMutual Financial Group
MedAmerica Insurance Company
Mutual of Omaha
New York Life Insurance
Northwestern Long Term Care Insurance Company
Prudential
56
State Farm
TransAmerica Life Insurance
As of the end of 2011, policy sales for these companies totaled 223,000 which were
below 1990 levels.
Table 10 shows the top ten companies selling individual LTC policies in 1995 and
their status as of 2012.
57
Noteworthy is the fact that six of the companies are no longer
actively selling policies in the market and three have been acquired by others in the top
ten. Moreover, in 1995 these companies together sold slightly less than 300,000
policies, and by 2011, had experienced a net decline of 43% in annual policy sales.
55
Other companies include Auto-Owners Insurance Group, Blue Cross Blue Shield of Michigan (LifeSecure),
Country Life, Humana, United of Omaha, and United Security as reported in Brokers World, 2012.
56
Prudential announced its exit from the individual market but took applications through March 2012 and in July it
announced its exit from the group market but is taking applications through the middle of 2013.
57
We focus on the individual market due to data limitations associated with group carrier experience in the 1990s.
43
TABLE 10. Experience of 1995 Top Writers of Individual LTC Insurance in 2011
Company
# Policies
Sold 1995
# Policies
Sold 2011
Exit/
Acquisition Date
Aegon/Transamerica
22,000
7,095
Exited in 2005 and 2010 re-entry
CNA
24,000
0
Exited individual in 2000 and Group
in 2003 although continuing to take
enrollments on existing groups.
Bankers Life and
Casualty
38,800
10,948
In Market
American Travellers
(Conseco)
51,700
0
Exited in 1996
Amex/Genworth
58,100
90,190
In Market
IDS
24,000
0
Acquired by Genworth in 1995
John Hancock
16,700
20,586
In Market (2010 pause in Group
Market)
Penn Treaty
27,400
0
Exited in 2008
Fortis LTC
18,600
0
Acquired by John Hancock 2000
Travelers
18,000
0
Exited in 2000 and reinsured by
Genworth in 2000
Total
299,300
128,819
Currently, individuals with LTC insurance policies are either being serviced by
companies who continue to sell in the market or by those who have exited and are no
longer selling policies. The latter are considered to be in “closed-blocks”.
58
In order to
determine the size of the closed-block market, we analyzed and updated information
from the 2010 NAIC Experience Exhibit reports. Table 11 shows the current state of the
market for companies that comprise 95% of total market share, and are selling at least
2,500 policies a year. For the purposes of this analysis, we define a company as having
left the market to be one that ceases selling new policies to any part of the market or to
a particular market segment (e.g., group versus individual).
59
For companies that have
only pulled back from a specific market segment, all reported performance-based data
applies only to that market segment.
In general, company size, product offering, and geographic location do not
differentiate firms that have left the market versus those that have remained. In 2010,
annual premiums for companies still selling policies in the market totaled $5.3 billion
compared to $4.7 billion for those who exited the market and were administering
“closed-blocks” of business -- 53% compared to 47% of the total. On a cumulative
premium basis, however, closed-blocks represented 55% of all earned premiums.
Regarding claims, in 2010, closed-block companies represented 53% and 57% of
annual and cumulative total claims costs. As demonstrated below, just one year earlier,
the picture looked very different.
58
A “closed-block” means that while policyholders who hold policies continue to receive services from the
company, no new sales are occurring and hence, no additional individuals are being added to the risk pool.
59
A company may decide to exit one market segment but stay in another if it perceives greater risk or unique
challenges in a particular market segment. For example, the administrative burden of implementing rate increases in
the group market may be perceived as far greater than in the individual market, and therefore exiting this market
may be more attractive to some carriers.
44
TABLE 11. Distribution of LTC Insurance Companies by Current Market Status
Companies Still Selling in the Market
Companies Out of the Market
Bankers Life & Casualty Company
Genworth Life Insurance Company/
Genworth Life Insurance Company of New
York
John Hancock (individual policies)
Knights of Columbus
Massachusetts Mutual Life Insurance
Company
Medamerica Insurance Company/
Medamerica Insurance Company of New
York
Mutual of Omaha Insurance Company
New York Life Insurance Company
Northwestern Long Term Care Insurance
Company
State Farm Mutual Auto Insurance
Company
Thrivent Financial For Lutherans
Transamerica Life Insurance Company
Ability Insurance Company (Medico)
Aetna Life Insurance Company
Allianz Life Insurance Company of North
America
American Family
American Family Life Assurance Company
of Colorado
Continental Casualty Company
CUNA Mutual Insurance Society
First Unum Life Insurance Company
Guardian Life
Guarantee Trust Life Insurance Company
John Hancock Group
Kanawha Insurance Company
Lincoln Benefit Life Company
Metlife Insurance Company of Connecticut
Metropolitan Life Insurance Company
Monumental Life Insurance Company
Penn Treaty
Physicians Mutual Insurance Company
Provident Life & Accident Insurance
Company
Prudential Insurance Company of America
RiverSource Life Insurance Company
Senior Health Insurance Company of
Pennsylvania
Southern Farm Bureau Life Insurance
Company
Time Insurance Company
Union Security Insurance Company
United Teacher Assoc Insurance Company
Unum Life Insurance Company of America
WEA Insurance Corp
SOURCE: Analysis of NAIC Experience Exhibit Reports, 2011 and LifePlans Sales Survey
2012.
The 2009 NAIC Experience Exhibit Report is the last that contains detailed
information on actual-to-expected loss experience by company. In that year, 192
companies reported their individual claims experience. We extracted and analyzed
information from that study in order to determine whether or not the experience of
companies that left the market differed from those that remained in the market. At that
time, there were about 27 companies (among those reporting that year) that were
actively selling policies. The remainder administered closed-blocks or had negligible
sales. Figure 15 summarizes key market size and performance indicators for each of
these distinct segments in 2009. As indicated, quite a few companies left the market
between 2010-2012, so the picture would likely look different today than it did just a few
short years ago.

45
FIGURE 15. Market Indicators by Company Sales Status 2009
SOURCE: LifePlans Analysis of NAIC Experience Reports, 2010.
There are a number of important issues of note. First, in 2009, a majority of
individuals with LTC insurance policies were being serviced by companies selling
policies (75%). However, not shown in Figure 15 is the fact that by 2010 -- when
additional companies exited the market -- the percentage of policies serviced by
companies’ still selling policies in the market had fallen to 45%. Second, on a premium-
weighted basis, the actual-to-expected incurred claims experience in closed-blocks was
115% compared to 93% for companies still selling policies at that time. Thus,
experience was markedly worse for the companies that had already left the market, and
the impact on profitability was clearly negative. Finally, there was also somewhat
greater volatility in the cumulative actual-to-expected claims experience among
companies that exited the market. Volatility is an important performance indicator,
because the greater the level of volatility, the greater is the range of possible negative
(and positive) outcomes. Typically, when there is more variability in expected
outcomes, to attract capital, the return needs to be greater than for products or
industries with less volatile results. Taken together, these data suggest that unless
there are significant new entrants to the market, over time overall financial performance
will be increasingly dominated by the experience of closed-block companies, and such
experience to date, has been less positive than for companies still selling policies in the
market. To some degree, the relative difference in performance is not unsurprising
given that closed-blocks tend to derive from companies whose policies were sold many
years ago when there was less certainty around key pricing parameters affecting
premiums and claims.
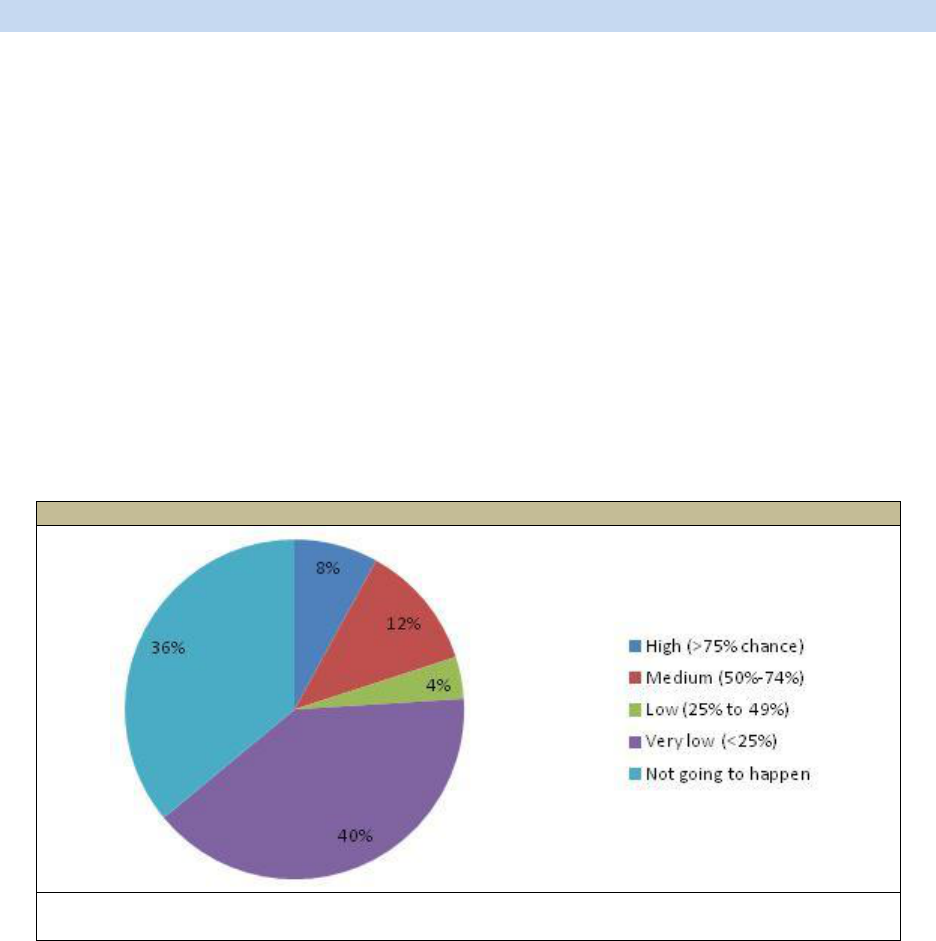
46
E. Factors that Might Lead Companies to Re-Enter the Market
Many of the same reasons that compelled companies to enter the LTC insurance
marketplace 20-30 years ago remain relevant today. Foremost among them is the fact
that LTC represents the single largest unfunded or uncovered liability during retirement
and demographic trends suggest a growing need for the product. Yet it is clear from the
data presented thus far, that a variety of factors have made the product in its current
form a difficult business proposition for companies. The underlying risk in the product,
which results in significant capital requirements and the need for a meaningful rate of
return on that capital make it difficult to generate an attractive level of profit at an
affordable price to support robust sales. We asked all respondents whether they
believed that their own company had left the door open to coming back into the market
at some point in the future. About 42% of respondents affirmed their belief that the
“door remained open”. When queried further, only one-quarter indicated that the
chance was greater than 25% and the other 75% said that the chance was very low or
that it simply was not going to happen. Not shown is that roughly one-third estimated
that if they returned to the market, it would be within the next five years.
FIGURE 16. Chance that the Company would begin Selling LTC Insurance Again
SOURCE: Survey of executives from 25 LTC carriers who exited the market or exited segment
of the market.
We also queried respondents on what might be needed to have them reconsider
their decision. We asked about regulatory, public or other policy design changes that
might make it more attractive for them to again develop and sell policies in this market.
More specifically, for a series of policy design and regulatory changes, we asked
whether the recommended change would “Definitely”, “Maybe”, “Probably Not”, or
“Definitely Not” influence their decision to reconsider entering the market. In the survey
instrument, background information was provided for each recommended change so
that the respondent knew precisely what was being asked. In Table 12, we paraphrase
the changes that were offered.
47
It is important to note that many of the changes that we asked about have been put
forward by industry advocates as positive and supportive of the private market. The
focus of our inquiry, however, was not on their desirability, but rather, whether they
would make a difference in the decision to re-enter the market. Thus, if a respondent
indicated that a particular change would “Definitely Not” make a difference regarding
market re-entry, this does not mean that the change would not be viewed positively or
important to efforts to support the private market.
TABLE 12. Factors Potentially Influence the Decision to Re-Enter the Market
Change
Would the Recommended Change Influence Company to
Reconsider Entering the Market?
Definitely
Maybe
Probably
Not
Definitely
Not
Undecided/
Other
Having premium rates vary by
interest rate. That is, having the
ability to file multiple sets of new
business premium rates the use of
which is automatically determined
by an external interest rate index for
new business premium rates and
in-force premium rates.
a
4%
36%
20%
36%
4%
Having premium rates vary by
interest rate. That is, having the
ability to file multiple sets of new
business premium rates the use of
which is automatically determined
by an external interest rate index.
4%
32%
24%
36%
4%
Allowing stand-alone LTC and/or
combination-products to be funded
with pre-tax dollars.
8%
25%
33%
29%
4%
Being able to offer other
combination-products for example,
disability income with LTC, or
critical illness with LTC rather than
just life and annuity combination-
products.
4%
28%
28%
40%
---
Being able to offer a Universal LTC
policy design which would allow for
premium flexibility, interest
crediting, cash values, age and/or
duration adjusted insurance
charges (current and guaranteed)
for LTC, and surrender charges.
8%
20%
24%
40%
8%
Allowing stand-alone LTC and
combination-products to be offered
in cafeteria plans.
---
21%
42%
38%
---
Changing the mandatory offer of 5%
compound inflation protection to a
mandatory offer of 2% inflation
protection.
---
20%
32%
40%
8%
Removing the requirement of
offering 5% compound inflation
protection on a combination-annuity
product.
---
16%
16%
52%
16%
Removing the requirement for a
minimum benefit period.
4%
8%
38%
42%
8%
Requiring all agents to get LTC
education to obtain their life/health
license and continuing education.
---
8%
36%
52%
4%
Changing the application to remove
questions about other health
coverage, financial questions, or
reconfirming benefit choices.
b
4%
4%
16%
72%
4%
Allowing longer Elimination Periods
like 180 day period.
---
4%
44%
48%
8%
48
TABLE 12 (continued)
Change
Would the Recommended Change Influence Company to
Reconsider Entering the Market?
Definitely
Maybe
Probably
Not
Definitely
Not
Undecided/
Other
Allowing Waiting Periods for those
who are insurable today, but want
benefits in later years or using a
Waiting Period as an underwriting
tool.
---
4%
36%
52%
8%
Allowing multiple policyholders to
share one pool of benefits so that
benefits are not "saved" but are
exhausted when used up,
regardless of who uses them.
---
---
20%
72%
8%
Last-survivor policies which would
pay benefits only after one spouse
had died.
---
---
28%
64%
8%
SOURCE: Survey of executives from 25 LTC carriers who exited the market or exited segment of the market.
NOTE: It is not always clear that a number of the policy designs are not currently allowed; however, there is enough
uncertainty about regulatory and tax treatment, that it might be the case that this represents a barrier.
a. This would enable the premiums that are paid by consumers to fluctuate based on a pre-determined schedule
which would be a function of a pegged interest rate. Multiple sets of rates would have to be approved by state
insurance departments.
b. The purpose is to simplify the application process, which is sometimes viewed as a barrier for consumers and also
can make it difficult for agents to sell the product.
As shown in Table 12, there are very few specific policy design changes or
regulatory modifications presented to respondents that would lead companies to
definitely reconsider their decision to exit the market. On the other hand, the ability to
file multiple business rates -- which in part helps to mitigate the investment (interest
rate) risk -- was cited most frequently as a change that would potentially lead to a
reconsideration of the decision. Filing multiple business rates would allow companies to
charge alternative premiums depending on the level of the interest rates and these
premiums would be pre-approved by state insurance departments. As well, expansion
of combination-products to include LTC-disability, LTC-critical illness, LTC-annuity
products, or others was viewed as something that might cause companies to think
about getting back into the market.
Noteworthy is the fact that one-in-three respondents suggested that allowing
policies to be funded with pre-tax dollars also would lead them to potentially reconsider
their decision. This is a lower percentage than those citing the ability to file multiple
rates which suggests that issues related to consumer demand are less important drivers
of the decision than are risk management issues; more specifically, risk management
on the investment side.
Respondents were given an additional opportunity to express what it might take for
them to consider returning to the market. They were asked to indicate the
circumstances under which they would consider doing so. They were provided with
broad categories and then requested to provide specific suggestions within each
category. The categories included changes to regulatory policy, distribution
approaches, policy design features, tax status, and consumer attitudes.
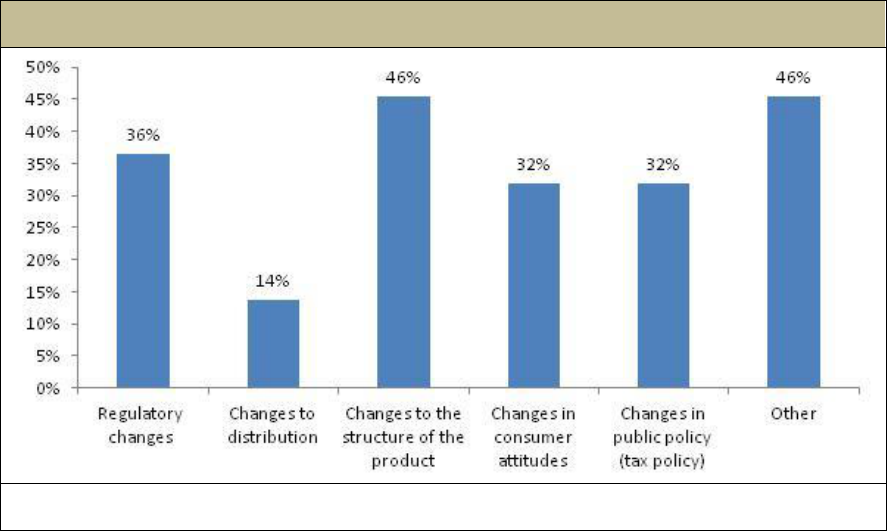
49
Figure 17 shows that product structure changes were cited most often as likely to
have a meaningful influence; many of these had to do with the level-funded nature of
the product, the “long-tail risk”, and the fact that the product is complicated. Those
citing regulatory requirements pointed to high capital requirements, as well as a general
sense that carriers needed to have more flexibility in product design. Finally, consumer
attitude changes that insurers felt might influence a decision to re-enter the market were
focused primarily on the need for additional education so that consumers would be
aware of the risks that they faced and how the product is designed to address this risk.
FIGURE 17. Circumstances under which the Company would Consider
Re-Entering the Market
SOURCE: Survey of executives from 25 LTC carriers who exited the market or exited segment of
the market.

50
V. IMPLICATIONS
By almost all measures, the private market for LTC insurance is not meeting the
initial expectations of companies that entered the market as well as current expectations
of those that continue to sell policies. Yet no one disputes the need for a product that
insures against the financial risk associated with LTC services nor is there an argument
about the fact that this need will increase over time. Even so, as companies have
entered the market to fill this need, most have fallen short on meeting sales and
profitability objectives and it is this latter failure that has driven most of them from the
market.
Clearly companies can do little to influence macro-economic trends affecting
interest rates and in fact, many companies have exited the market over the past seven
years because of the extremely low interest rate environment. Simply put, they could
not generate sufficient income on reserves and RBC to fund future liabilities. Yet there
are a number of actions that carriers can take to improve the overall profitability of
products. The results presented in this study suggest that the ability to generate a
reasonable level of profit is critical to assuring that companies remain in the market and
that new companies will find the market attractive.
First, change to the underlying funding structure of products should be considered.
Currently, products are level-funded, but they could be priced on a “term-basis”, much
like life insurance. This may be particularly relevant for individuals purchasing policies
at younger ages. For example, the premium could be set to cover the risk (expected
claim costs) over the term (e.g., one year) and there would be an understanding that
every year the premium would increase to cover the increase in expected claims. At a
certain point the premium would be fixed and level-funded, say at age 70 or 75. The
schedule may also include a small amount of pre-funding.
60
Because the annual
increase in premiums could approach 10%, in addition to limiting the age at which
premiums can be increased, it may also make sense to limit annual increases to smaller
amounts.
61
Such an approach minimizes the importance of interest earnings, makes the
product more affordable and attractive at younger ages and makes awareness of future
LTC risk more pervasive. This in turn, should help to reduce selling costs and
“mainstream” the product as part and parcel of a standard retirement plan. Results
presented here suggest that it may also draw companies back into the market.
60
This is similar to designing LTC insurance like Universal Life. An account value is credited with premiums and
interest earnings and charged with current insurance charges, withdrawals, and expenses. As the account value
increases, the net amount-at-risk decreases. The early pre-funding is available to the policyholder in the event of
lapse or early death.
61
Mohoric, E. (2013). Long-Term Care Product Design: Two Common-Sense Recommendations. Long-Term Care
News, Long-Term Care Insurance Section, Society of Actuaries. January.

51
A second approach involves indexing both premiums and benefits to account for
increases in the cost of services. Such an approach should be tied to actual changes in
the cost of LTC services which many companies track on an annual basis.
62
This
method has the virtue of reducing the uncertainty around the inflation risk, as well as
lowering initial premiums, since a fixed inflation adjustment (e.g., 5%) is not built into the
initial premium. It makes the product more affordable for consumers but even more
importantly, reduces the level of initial reserves that must be set up by the company,
which in turn eases the amount of capital required to support the product.
Clearly, a focus on restructuring the product is an important direction to consider
for the industry as well as for regulators, who have a great deal to say about what is and
is not acceptable in terms of product design. The industry will need to work with the
NAIC as well as consumer groups to assure acceptance of such designs. Even though
current regulations do not prohibit such approaches, insurers have not offered them in
part because of a concern about introducing additional complexity into the product.
Moreover, there is a legitimate concern that increasing premiums for people who are on
fixed incomes will cause them to drop their policies. Designs that begin with term or
indexed pricing, and then adjust the indexing rate downward at a certain point can
reduce these concerns. As well, new combination-product approaches are also
designed (in part) to lower the inherent risk in the product or even provide for off-setting
risks (mortality and morbidity) within a single product (e.g., annuity-LTC products).
Another strategy involves deploying more sophisticated investment strategies.
Even with major changes in product design, there will always be some need for an
investment strategy that maximizes returns on invested premiums and capital. While
companies have little control over general interest rates, there are mechanisms that can
minimize some of the risk associated with the mismatch between future cash inflows
and outflows. Helwig et al. (2007), identify a number of financial market innovations that
can mitigate interest and inflation risk in products. For example, a carrier can use what
is called a “Forward Interest Rate Swap” to lock in future interest rates; it then replaces
these contracts with assets funded by future premiums which can help to match the
asset/liability of their profile.
63
The same principle holds for Inflation Swaps; the carrier
pays a fixed inflation rate in exchange for the realized inflation rate for a period of time,
thus eliminating any uncertainty about future inflation. These strategies are designed to
hedge against the inflation and interest rate risks and they do require a level of
sophistication in managing investment portfolios.
Providing companies with more certainty regarding the anticipated actions of state
insurance departments vis-à-vis requested rate adjustments is also very important.
Many companies were uncertain how they would be treated by regulators when making
rate increase requests. While it is true that the vast majority of companies have
62
Both Genworth Financial and MetLife conduct annual cost of care surveys that track changes in the cost of key
LTC services including nursing home care, assisted living, and home health care.
63
Helwig, D., Bhandula, R. and Barrett, N. (2007). Long-Term Care: Hedging Your Bet. Long-Term Care News,
Long-Term Care Insurance Section, Society of Actuaries. December.

52
increased rates on exiting policyholders, in many cases the approved rate change is
less than what carriers demonstrated they required to cover anticipated losses, let alone
earn a minimum return on their investment. Insurance regulators must of course
balance insurer solvency and consumer protection, and it is not the role of insurance
regulators to guarantee a certain level of profit to companies. Nevertheless, the
concern about being able to obtain rate changes, when state-approved actuarial
assumptions have not been met, is real: the product is priced to be guaranteed
renewable but not non-cancellable.
64
This means that companies have approached this
market with the knowledge that if experience is not consistent with underlying pricing
assumptions -- all of which are reviewed and approved by state insurance departments
-- they have the ability to make adjustments prospectively. One approach to dealing
with this issue and viewed positively by many companies is the ability to file multiple
business rates that could be pre-approved and triggered when events occur outside of
the control of the individual company such as precipitous declines in interest rates. This
has the virtue of reducing the inherent risk in the product and thus may attract more
capital and firms into the marketplace.
By taking some of the most risky elements out of the product, one could argue that
relatively high capital requirements would no longer be justified. High capital
requirement have been both a major barrier to entry as well as a major reason why
companies have not been able to justify staying in the market. New arrangements with
reinsurers may also reduce some of the need for capital, but this would also require
changes in product to make the business opportunity attractive to reinsurers.
Finally, actions designed to reduce the costs of producing the product will enhance
profitability. The most important non-claims related cost is sales commissions. Many
view them as high today, in large part because of challenges in selling the product and
the need to attract more agents to sell LTC insurance. As noted, however, given the
challenges involved in selling the product, commissions are not out of line with what is
paid for other voluntary insurance products in the individual market. There are a variety
of reasons why it is difficult to sell the product and these have been outlined -- along
with potential solutions -- in Frank et al. (2013).
65
Some of the reasons relate to
household behaviors associated with savings, purchase of insurance, and health-
related behaviors (i.e., demand) and others with the efficiency of the private insurance
market (i.e., supply). Solutions include strategies linking LTC insurance to health
insurance, simplifying the product, providing more support for employer-sponsorship of
insurance, educating the public about the risk and costs of LTC, forcing active choice,
providing state-based organized reinsurance pools to provide a “back-stop” for industry
experience, implementing targeted subsidies, and others. All of these strategies are
64
A guaranteed renewable product in this context means that the insurer cannot cancel a policy if the individual
continues to pay premiums but the company does have the right to change premiums based on credible experience
for a class of individuals. A non-cancellable policy implies that the company cannot change premiums once they are
set, regardless of whether or not pricing assumptions are met.
65
See Frank, R., Cohen, M. and Mahoney, N. (2013). Making Progress: Expanding Risk Protection for Long-Term
Services and Supports through Private Long-Terms Care Insurance. Unpublished policy brief submitted to the
SCAN Foundation. January.
53
designed to increase demand -- both through lowering selling costs and through
changing peoples’ attitudes about the value of LTC insurance -- and help address risk
challenges facing the industry.
While not directly related to the central issue of product profitability, it is worth
noting again that a majority of policyholders are in closed-blocks of business. These
tend to perform less favorably than open blocks and in fact, a small number of large
companies are responsible for this experience among both closed and open blocks.
Thus, negative performance is to some degree skewed by a few companies and may
not represent the overall experience of the industry as a whole. Unless there is a
dramatic increase in new sales, the experience of these blocks will increasingly
characterize overall industry performance. Because such blocks may not represent
significant profit or growth opportunities for companies, it may become increasingly
difficult to attract necessary levels of investment to service the policyholders in these
blocks. As well, it may become increasingly difficult to attract and retain top risk
management talent to work with a segment of the business that has been deemed
unprofitable.
This poses potential risks to policyholders and challenges to regulators who may
face unique issues associated with closed-blocks of business. A certain level of
regulatory flexibility may be required to work through new and unknown issues. There
may be circumstances where carriers desire to take actions that will benefit consumers
as well as reduce costs or mitigate risks to the carrier, and it may not be clear whether
such actions are allowable under existing regulations. For example, adding no-cost
riders to policies that enable a more proactive approach to managing care, offering
policyholders the ability to change the underlying structure of benefits to keep premiums
more stable, supporting flexible approaches to applying alternate benefit provisions that
take account of changes in the service delivery environment and so on.

54
VI. CONCLUSION
Although the market has experienced a very major contraction in the number of
companies actively selling policies, it is worth noting that the LTC insurance market
covers more than seven million Americans and is larger than the individual disability
market. Significant reserves have been established to pay for future LTC costs and the
increasing flow of private insurance dollars to LTC providers is growing in importance.
As essential, there is a core of major insurers highly committed to this market and under
the right circumstances more carriers could be drawn back into the market.
While many early market entrants learned the “hard way” about what is required to
price and manage the risks in this product, there have been many valuable lessons
learned. Such lessons can help set the industry on a more solid financial foundation and
make entry for new carriers a more attractive proposition. Identifying strategies that
produce a level of profitability attractive enough to draw capital into the market is a key
to assuring that the growing demand for the product can be met by a robust and
competitive market of insurers. Public policy and regulatory approaches designed to
lower the cost of policies, allow greater product funding-flexibility, support new forms of
combination-products, and encourage strategies that help to minimize risks outside of
the control of companies, could provide needed support for a market “re-set”.
To obtain a printed copy of this report, send the full report title and your mailing
information to:
U.S. Department of Health and Human Services
Office of Disability, Aging and Long-Term Care Policy
Room 424E, H.H. Humphrey Building
200 Independence Avenue, S.W.
Washington, D.C. 20201
FAX: 202-401-7733
Email: [email protected]
NOTE: All requests must be in writing.
RETURN TO:
Office of Disability, Aging and Long-Term Care Policy (DALTCP) Home
http://aspe.hhs.gov/office_specific/daltcp.cfm
Assistant Secretary for Planning and Evaluation (ASPE) Home
http://aspe.hhs.gov
U.S. Department of Health and Human Services (HHS) Home
http://www.hhs.gov
