
PediatricMedulloblastoma
JeffBurkeen,MSIV(TexasA&M)
ShaliniMoningi,MSIV
AmandaWalker,MD
StephanieTerezakis,MD
JohnsHopkinsHospital
June10,2014

CasePresentation
• 9yopresentedtotheEDwith3monthhistory
ofintermittentheadacheassociatedwith
abdominalpainand vomiting
– HeadCTrevealeda3cmposteriorfossamass
with6mmtonsillarherniation
• PMH
– Anepisodeofileusat18months
– Otherwiseunremarkable
June10,2014
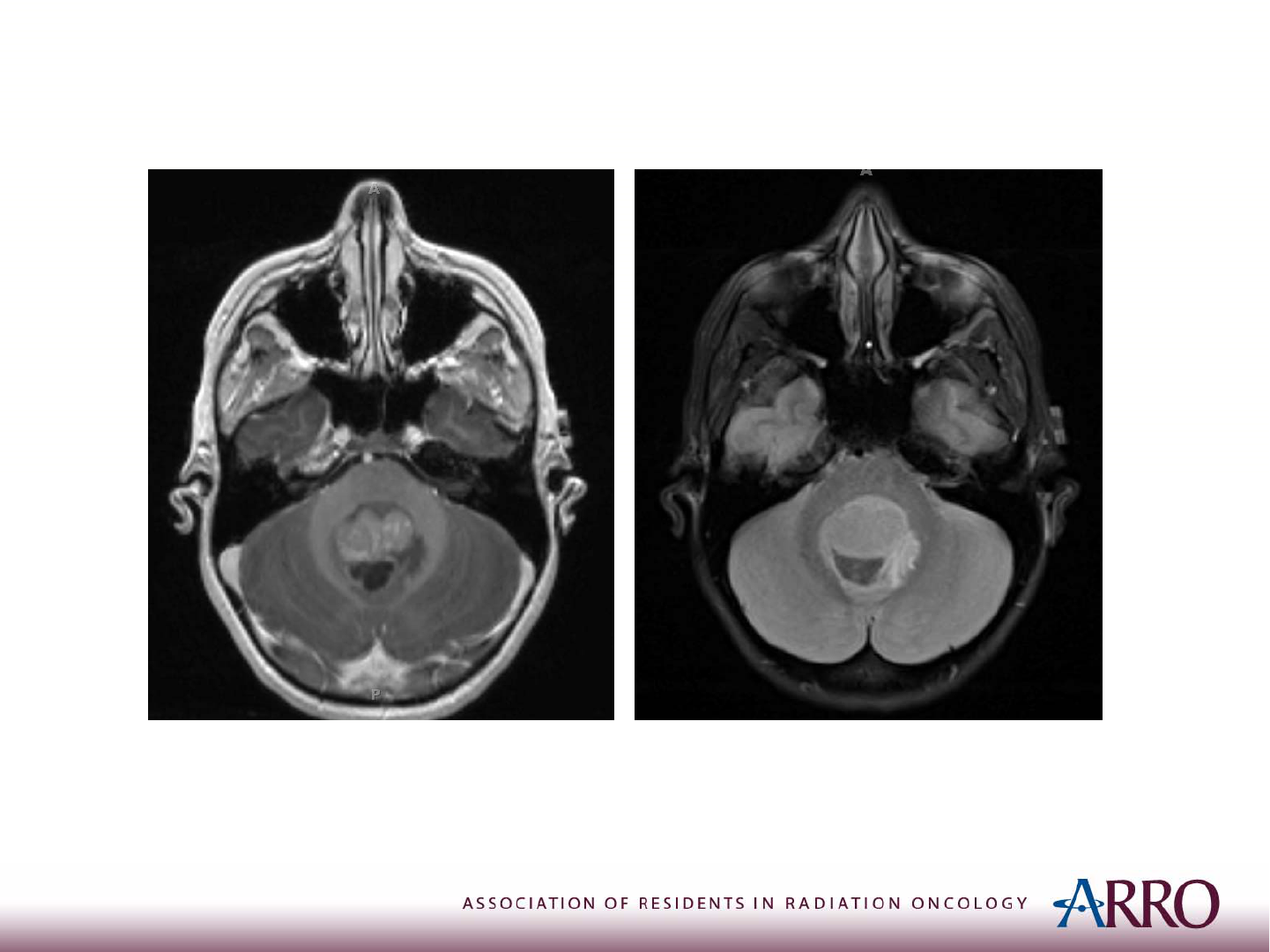
MRI
BrainMRIrevealedaheterogeneouslyenhancing2.4x2.2x3.0cm
massintheposteriorfossacenteredaroundthe4
th
ventricle.
T1postcontrast T2FLAIR
June10,2014
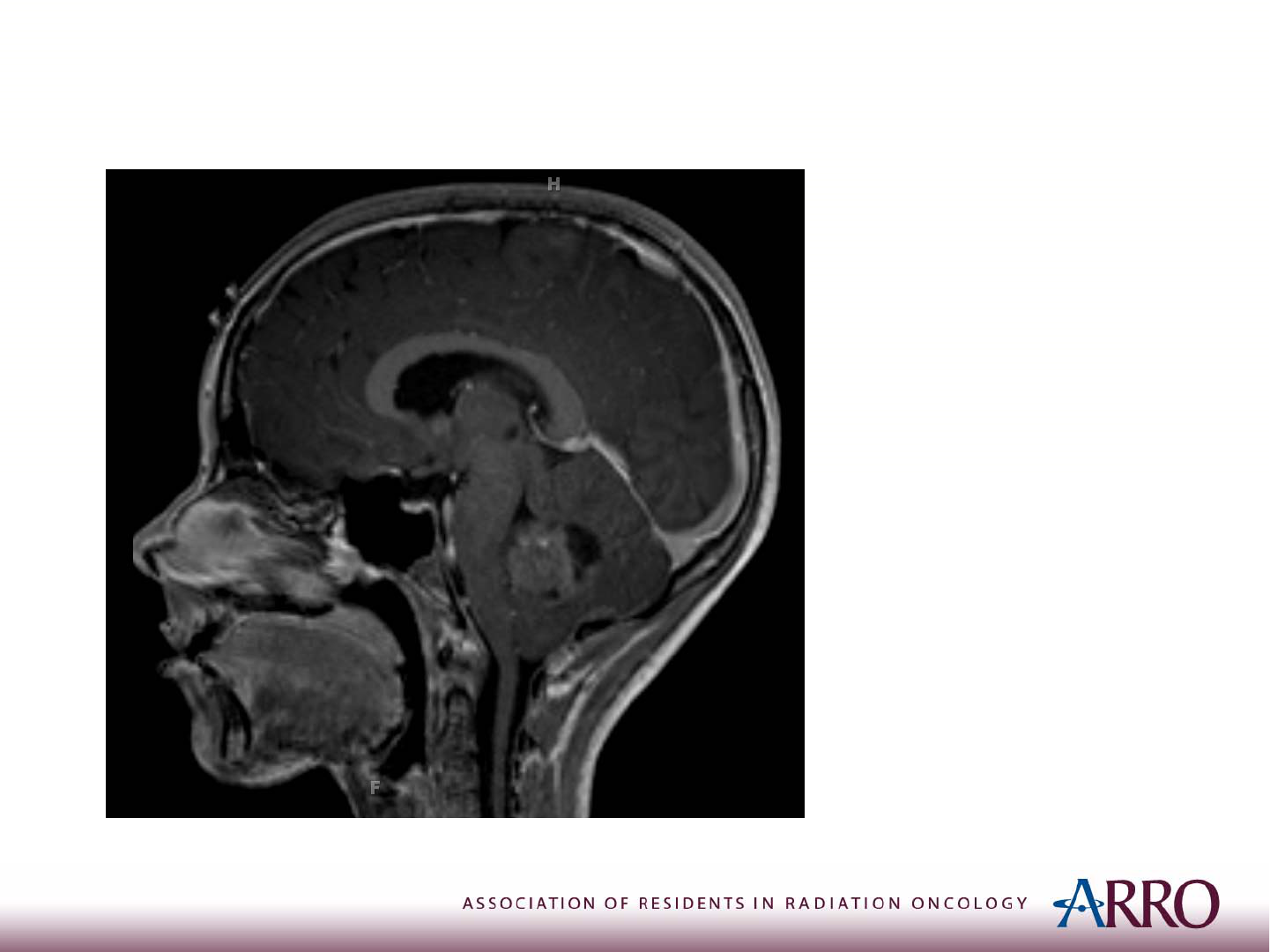
MRI
T1postcontrast
Therewasdescentof
cerebellartonsils
throughtheforamen
magnum(7mmbelow
planeoftheforamen
magnum)
Diffusionweighted
imaging(notshown)
revealedrestricted
diffusion,suggesting
highcellularity.
June10,2014

Treatment
• Surgicalresectionwasperformed
• MRIonPOD#1revealednoresidualdisease
• Pathology:medulloblastoma,gradeIV,withoutlarge
cell/anaplasticfeatures.Beta‐cateninstainingwas
negative
• CSFcytology>14dayspostopwasnegativeformalignant
cells
• Baselinelabs,audiometry,IQtestingwereallwithin
normallimits
• Diagnosis:StandardRiskMedulloblastoma
June10,2014

Epidemiology
• Mostcommonchildhoodmalignantbrain
tumor
• 20%ofpediatricCNS tumors
• ~550casesperyearintheUS
• Medianageofpresentationis5‐7yo
• 75%occurinchildren<15yo
• Morecommoninmales(~2:1)
June10,2014

Presentation
• Increasedintracranialpressure:headaches,nausea,
vomiting
• Cerebellarinvolvement:at axicgait
• Ininfants:lossofmilestones,increasedhead
circumference,headtiltduetoCNIVpalsy
• Clinicalexam:papilledema,nystagmus,CN
abnormalies(VImostcommon→"sengsun"sign
withdownwardgaze)
• 50‐75%have<3monthsofsymptoms
June10,2014

WorkUp
• Completehistory
• Completephysicalexamwithfocusonneurological
exam,fundusexam(forpapilledema)
• Labs:CBC,CMP
• Imaging:HeadCTandBrainMRI
• Ancillarytestspriortotreatment:
– Audiometry
– IQtesting
– SerumTSHandgrowthhormone
June10,2014

Workup:CSF
• 30‐40%haveCSFspreadatthetimeof
diagnosis
• CSFsamplingisrarelyobtainedprior to
surgerygiventheriskofherniationin the
settingofincreasedICP
• Ifnotobtainedpre‐operatively,mustwait10‐
14daysaftersurgerytoavoidfalse‐positive
findingsfromsurgicaldebris
June10,2014

ImagingRecommendations
• Pre‐opMRIbrainandspinalcord(post‐opspinecan
givefalsepositives)shouldbeperformed
• Timingofimagingisimportant:
– Post‐opMRIbrainwithin48hours
– IfMRIofspinenotperformedpre‐op,thenmust
wait10‐14daysaftersurgerytoavoidfalse
positives
June10,2014

TypicalImagingFindings
• CT:hyperdenseonnoncontrastCT(reflecting
highcellularity),enhanceswithcontrast
• MRI:welldefined,solid, T1hypointense,T2
hyperintensemass;oftencompresses4th
ventricle
June10,2014

DDxofposteriorfossamass inachild
• Medulloblastoma
• Astrocytoma(usuallypilocyticastrocytoma,
i.e.JPA)
• Ependymoma
• Atypicalteratoidrhabdoidtumor(ATRT)
June10,2014

Histology
• Smallroundbluecelltumor
• MostcommonembryonaltumoroftheCNS(others
includePNETs,ATRT)
• MolecularlydistinctfromPNETs
• 40%haveHomer‐Wrightrosettes
• Moststain+forneuron‐specificenolase,
synaptophysin,andnestin
June10,2014

Othersmallroundbluecelltumors
• LEARNNMR
– Lymphoma
– Ewing’s
– Acutelymphoblasticleukemia
– Rhabdomyosarcoma
– Neuroblastoma
– Neuroepithelioma
– Medulloblastoma
– Retinoblastoma
June10,2014

Histology‐ PrognosticFactors
Poorprognosis
• Largecell/anaplasticvariant
• DiploidDNA
• LOH17p
• p53mutation
• LowTrkC (tyrosinekinase
thatmediatesneuronal
differentiation)
• Her‐2Neu positive
Betterprognosis
• Desmoplasticvariant
• HighTrkCexpression
• β‐catenin
nucleopositivity
June10,2014

Histology
• Variantsofmedulloblastoma
– Classic:mostcommon
– Nodular/desmoplastic:bestprognosis,canbe
treatedwithsurgeryandchemotherapyalone
– Largecell/anaplastic:mostaggressive,always
treatunderhighriskparadigm
• Thistraditionalclassificationwilllikelybephasedout
infavorofmolecularclassification(nextslide)
June10,2014

PrognosticFactors
• Riskstratificationbasedonmolecularprofile
– Group1(~10%):Wnt/β‐cateninpathway,excellent
prognosis,5yrOS95%,usually“classic”histology
– Group2(~30%):Hedgehogpathway,goodprognosis,
peaksininfancyandyoungadults
– Group3(~25%):c‐MYCamplification,poorprognosis,5yr
OSonly50%
– Group4(~35%):neuronalsignature expression,peaksin
childhood,5yrOS50%
*Althoughbeingstudied,molecularanalysisisnotcurrentlypart ofroutine
pathologicev aluation
June10,2014

ModifiedChang’sStaging
• T1:tumor<3cmindiameter
• T2:tumor≥3cmindiameter
• T3a:tumor>3cmandwithextensionintoaqueduct
ofsylviusorforamenofluschka
• T3b:tumor>3cmandwithunequivocalextension
intobrainstem
• T4:tumor>3cmwithextensionpasttheaqueduct
ofsylviusorpastforamenmagnum
June10,2014

ModifiedChang’sStaging
• M0:noevidenceofgrosssubarachnoidor
hematogenousmetastases
• M1:microscopicCSFinvolvement
• M2:grossnodularseedingintracraniallybeyondthe
primarysite(incerebellar/cerebralsubarachnoid
space,3
rd
ventricle,orlateralventricle(s)
• M3:grossnodularseedingofspinalsubarachnoid
space
• M4:metastasesoutsidecerebrospinalaxis
June10,2014
RiskStratification
Features StandardRisk(2/3) HighRisk(1/3)
Age ≥3yearsold <3yearsold
Extentofresection <1.5cm
2
residual
diseaseafter
resection
Subtotalresection,
1.5cm
2
residualtumor
M‐stage* M0bycraniospinal
MRIandCSF
M+;leptomeningial
seeding
* Note: M stage is prognostic, T stage is not
June10,2014

Surgicaldefinitions
• Neartotalresection(NTR):<1.5cm
2
residual
tumoronpost‐opMRI
• Subtotalresection(STR):51‐90%resection
• Bxonly:<50%resection
– TumorbiopsyisNOTnecessary;patientsshouldgo
straighttosurgery
• 5‐yrEFSis worseinSTRvs.GTR/NTR
June10,2014

Surgeryrisks
• Posteriorfossasyndrome
– 10‐15%ofcases
– Mayoccur12‐24hourspostopandimprovesov er
severalmonths
– SAME
– Swallowingdysfunction
– Ataxia
– Mutism
– Emotionallability
June10,2014

PrincipalsofRadiation
• Inpatients>3yopost‐opRTwithconcurrent
vincristineisdeliveredtotheentirecraniospinalaxis
followedbyaposteriorfossaortumorbedboost
• Protontherapy,IMRT,or3‐Dconformaltherapyare
acceptabletreatmentmodalities
• Pre‐opandpostopMRIsofbrainandspineare
requiredforaccuratetargetvolumedelineation
June10,2014

PrincipalsofRadiation
• DoseofRTbaseduponriskgrouping:
– Standardriskpatientstreatedwith23.4Gyin13
fractionsfollowedbyposteriorfossa/tumorbed
boostto54‐56Gy
– Highriskpatientstreatedwith36‐39.6Gyin20‐22
fractionsfollowedbyposteriorfossaboostto54‐
56Gy
• Spinemetsalsoreceiveboostandfinaldosedepends
onlocation:
– 40‐45Gyatlevelofthecord
– 50.4Gyifbelowthecord
June10,2014

Chemotherapy
• Radiationisdeliveredwithconcurrentvincristine
• Adjuvantchemotherapyisstandardofcare
• Chemotherapycanalsobegivenforyoungerpatients
inordertodelayRT,asthetoxicityprofilefor
patients<3yowhogetradiationisworsethanfor
olderchildren
June10,2014

TreatmentParadigm‐
Standard risk
• Maxsaferesection RTwithconcurrent
weeklyvincristine adjuvantchemowith8
cyclesofcisplatin/CCNU(i.e.lomustine) /
vincristine
• RTisCSI23.4Gywithposteriorfossaortumor
bedboostto54Gy
• OSat5years:86%,EFS:81%(CCG/POG
A9961)
June10,2014

TreatmentParadigm‐
Highrisk(>3yo)
• SimilartostandardriskptsexceptRTisthe
following:
– CSIdoseis36Gy‐ 39.6Gyratherthan23.4Gy
– Entireposteriorfossaboostto54Gy
– RTwithconcurrentvincristinefollowedby
adjuvantchemotherapy(similar tostandardrisk)
• POG9031demonstratedthosewithM1
diseasehad5yrEFSof65%
June10,2014

Treatmentparadigm:<3yo
• Bydefinition,alwayshighriskif<3yo
• Surgeryfollowedbyintensivechemotherapyis
primarytreatment
• RTreservedforsalvagetherapy
June10,2014

CraniospinalIrradiation
• Goals:Achieveuniformdosethroughoutthe
subarachnoidspace
• Spinefield(s)deliveredwithPAbeam
• Cranialfieldsdeliveredwithopposedlaterals
• Cranialand spinefieldsmustbematched
– Thecollimatorandcouchmustberotatedduringdeliveryof
cranialfieldsinordertoaccountforbeamdivergence
• Movingjunction(i.e.gapand feather)isoftenused
betweenfieldstominimizeareasofpotential
underdose/overdose
June10,2014

CraniospinalIrradiation
• Specificapproachvariesbyinstitution
• Setup
• ProneorSupine
• Immobilizewithareproduciblesetup
– Body immobilizationwithalphacradle,vaclockbag,etc.
– Aquaplastmaskforheadimmobilization;neckhyperextended
toavoiddivergenceofPAbeamthroughmouth
– CTsim
– Anesthesiamayberequired
June10,2014

AdvantagestoPronevs.Supine
Prone
• Directvisualizationoflightfieldsforspinefieldsetup
(therapistsoftenpreferprone)
Supine
• Oftenmorecomfortableforthepatient;potentiallyless
movementduringtreatment
• Easyairwayaccessforpatientsrequiringsedation
June10,2014

TraditionalProneTechnique
• Simandplace spinefieldsfirst:
• SSDsetup(cranialfieldswillbeSAD)
• Borders
– Superior:C4‐C7(whileavoidingexitdosethroughoralca vity)
– Inferior:establishterminationofthecalsacasdeterminedby
MRI(~S2)andcover1‐2cminferiorly.
– Lateral:covertherecessesoftheentirevertebralbodieswith
atleast1cmmarginoneitherside.Mustcoverthesacral
foramina
(“spade”shape)
June10,2014

• Spinefield:
– Numberofspinefields
• Youngchildren:entirespinecanoftenbeencompassed
inonefield
• Inolderchildren,mayneedtwoadjacentfields
– TrytoavoidextendingSSDbecausethisincreasesexitdose
– Matchingadjacentspinalfields:Therewill beagapatthe
skinwithadjacentfieldbordersmatchingattheanterior
surfaceofthespinalcanal(someinstitutionsmatchatthe
depthofmid‐spinalcord)
TraditionalProneTechnique
June10,2014

• Brain anduppercervicalspinearetreated
withlateralfields
– SADsetup
– Placeisocenterinmidlineinsamecoronalplane
asspinefieldtoavoidant/postshiftsduring
treatment
– Musthavecover ageofcribriformplate(0.5–1cm
toblockedge)
– Trytominimizedosetoeyeandlens
TraditionalProneTechnique
June10,2014
• Brain anduppercervicalspinearetreated
withopposedlateralfields
TraditionalProneTechnique
• Borders
– Supandpost:flash
– 0.5‐1cmmarginon
cribriformplate(must
contour)
– 1cmmargininferiorto
middlecranialfossa
– 1cmmarginanteriorto
vertebralbodies
June10,2014

Techniqueformatchingbrainandspinefield:
• Inorderforthecranialfieldtomatchdiverging
spinefields,thecollimatormustrotate
• Angleofcollimatorrotationcanbecalculated
withthefollowingequation:
θ
coll
=arctan(L
1
/2*SSD)
L
1
=lengthofposteriorspinefield
SSD=sourcetosurfacedistanceofposteriorspinefield
TraditionalProneTechnique
June10,2014

Techniqueformatchingbrainandspinefield:
• Inorderforthespinefieldtomatchdiverging
cranialfields,couchmustrotatetowardthe
gantry
• Angleof“couchkick”canbecalculatedwiththe
followingequation:
θ
couch
=arctan(L
2
/2*SAD)
L
2
=lengthoflateralcranialfield
SAD=sourcetoaxisdistanceoflateralcranialfield
TraditionalProneTechnique
June10,2014
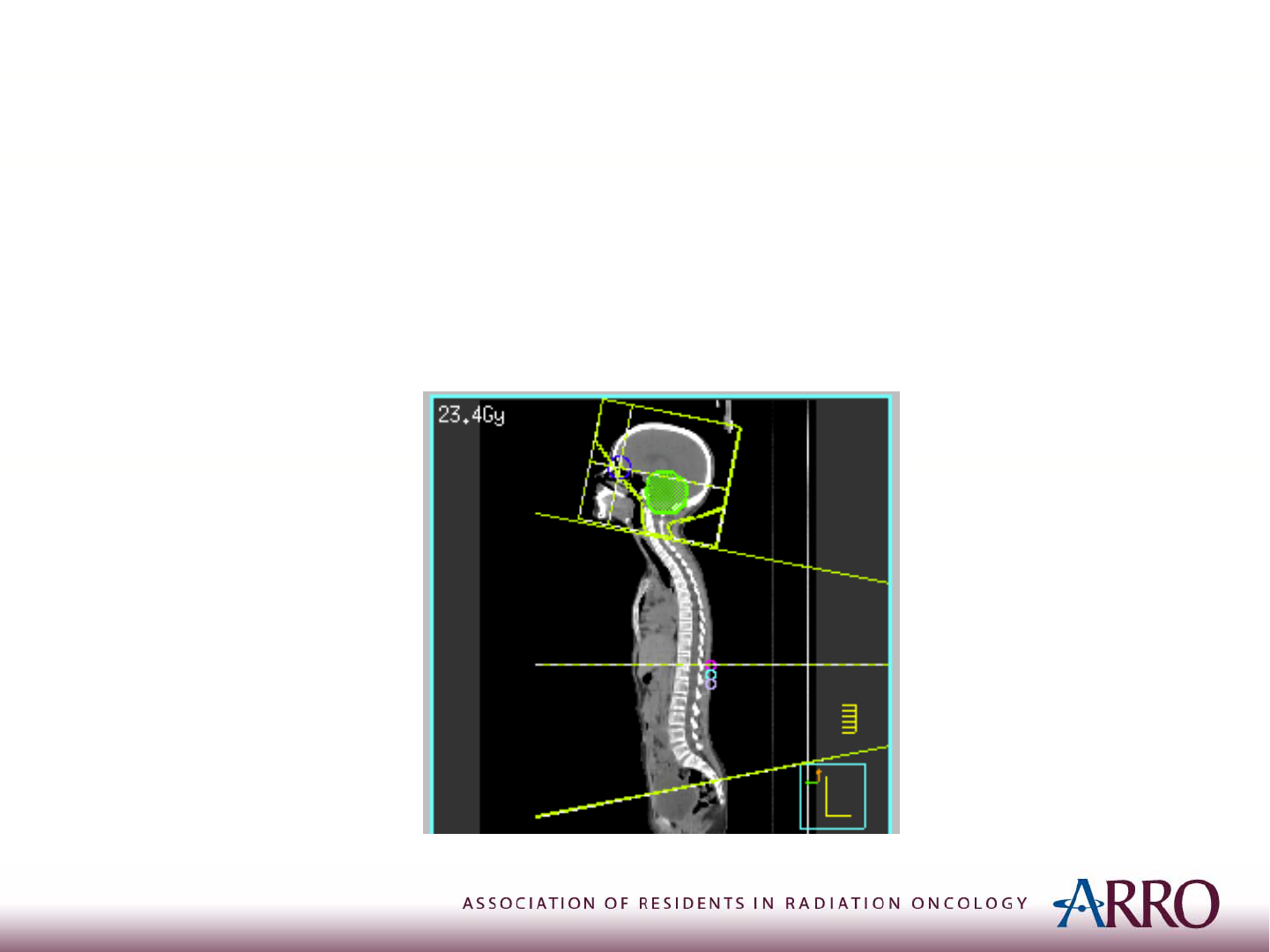
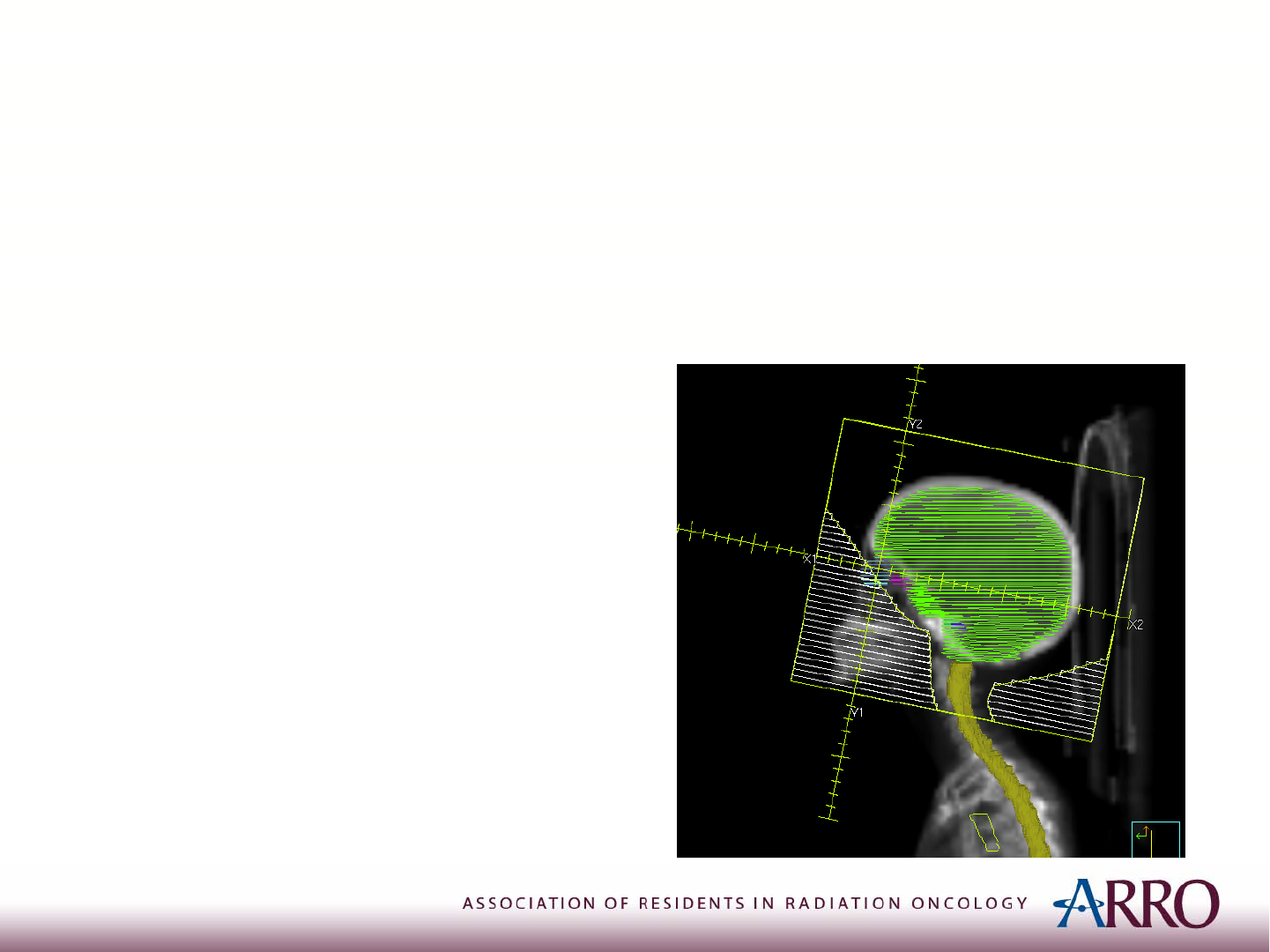
TheCase:CSI
• OurpatientwastreatedCSIto23.4Gyinthe
supineposition
June10,2014

The“gapandfeather”technique
• Ratherthanrotatingthecouchtomatchdivergenceofcranial
beam,agapof0.5cmisplacedbetweenthebrainandspine
fieldeachday(collimatorisstillrotated).
• Feathering“spreadsout”thecoldspotatthegapbetween
thebrainandspinefields,aswellasanycoldspotsinthecord
duetoskingapwhenmorethanonespinefieldisrequired.
• Featheringisaccomplishedwiththeuseofasymmetricjaws.
– Forcranialfields:opencaudalborderofcranialfieldby
1cmeachday,cycleevery3days.
– Forspinefields:shiftisocenter(s)caudallyby1cmforeach
day;adjustblocksforeachdayaccordingly.
June10,2014
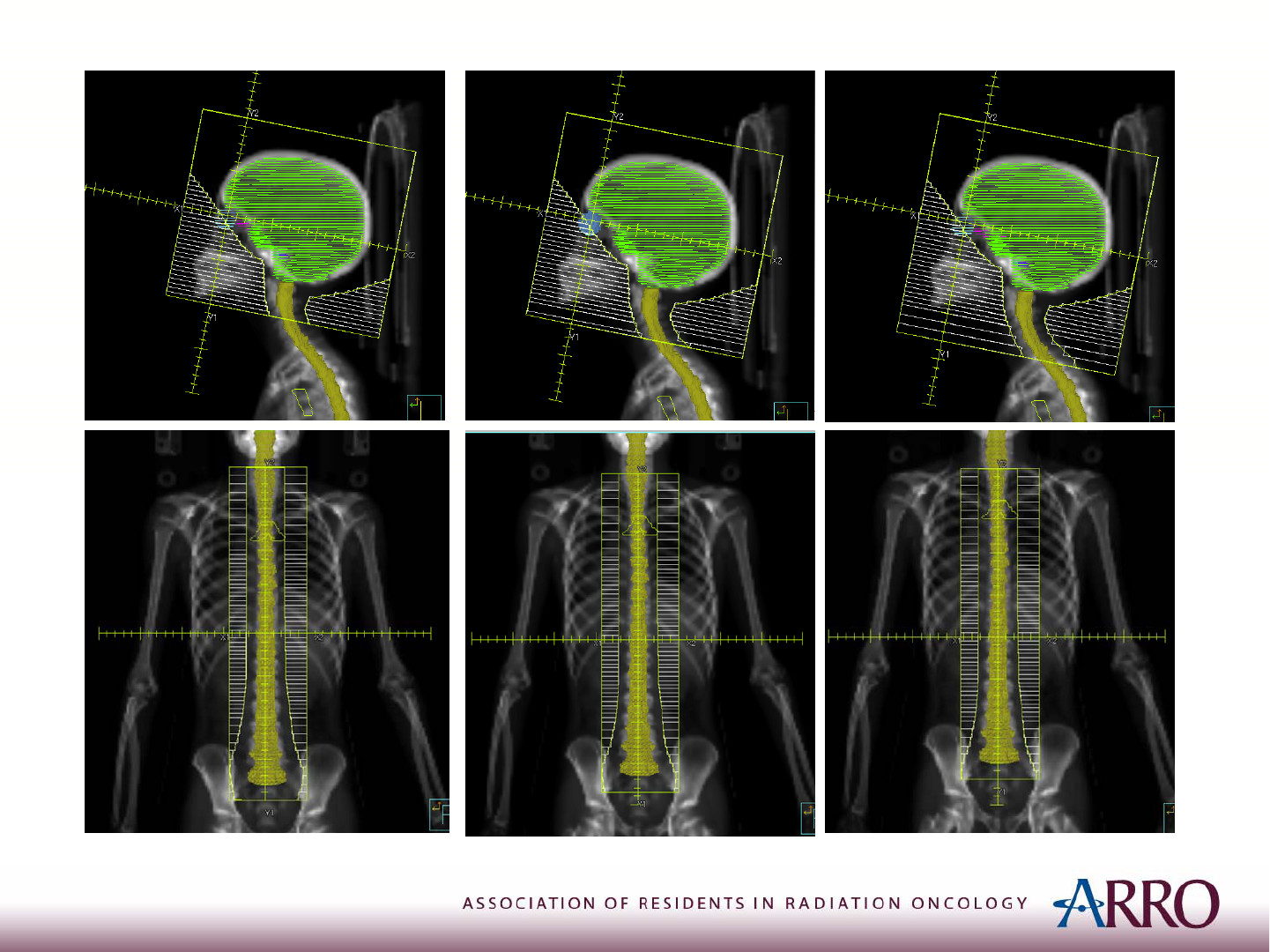
Day3
6/10/2014
Day2Day1
June10,2014

TheCase:TumorBedBoost
AfterCSIto23.4Gy,patientreceivedlimitedtargetboosttotumorbed
withIMRTphotonstoatotaldoseof54Gy
• GTV:
– tumorbed+grossresidualdisease,includingT1signal
abnormalitywithandwithoutcontrast
– Donotincludesurgicaldefectsvisibleonpost‐opMRIthatdid
not
containdiseaseonpre‐opMRI
• CTV:
– GTV+1–1.5cm
– excludingbone,tentorium,andentiretyofbrainstem(however,
brainstemimmediatelyadjacenttotumorbedshouldbe
includedasthisisanareaofpotentialmicroscropicdisease)
• PTV:
– CTV+3–5mm
June10,2014

StandardRisk:TumorBed vs.Posterior
FossaBoost
• CurrentCOGprotocol(ACNS0331)iscomparing
posteriorfossaboostvs.tumorbedboostin
standardriskpatients
• However,thereisevidenceavailabletosupport
limitingtheboostvolumetothetumorbed
– Fa ilurerateswithinposteriorfossaaftertumorbedboost
arecomparabletohistoricalexperiencewithtreating
entireposteriorfossa
• Woldenetal.,JCO,2003(PMID:12915597)
• Merchantetal.,IJROBP,2008(PMID:17892918)
June10,2014

Posteriorfossaboost
• CTV=entireposteriorfossa,includingbrainstem
• PTV=CTV+3‐5mm(excludepituitaryunless
involved)
• BonyLandmarks
– Superior:1cmabovethemidpointofalinedrawn
betweentheforamenmagnumandthevertex
– Anterior:posteriorclinoidsandanteriorC1(the
pituitaryshouldbeblockedunlessinvolved)
–
Inferior:C1‐C2junction
– Posterior:internaloccipitalprotuberance
June10,2014

RTlateeff ects
• DecreasedIQ
• Decreasedgrowth
• Ototoxicity
• Hypopituitarism
• Secondarymalignancy
June10,2014

FactorsfordeclineinIQafterCSI
• Age<7yo(mostimporant)
• Higherdose (36Gyvs.23.4Gy)
• HigherIQatbaseline
• Femalegender
June10,2014

References
June10,2014
1) Lee,N.L.,Lu,J.J.TargetVolumeandFieldSetup:APracticalGuideforConformalandIntensity‐ModulatedRadiationTherapy
(2013).
2) HansenE.K.,Roche,M.HandbookofEvidence‐BasedRadiationOncology. 2
nd
Ed.(2010).
3) Gajjaretal.Medulloblastomainveryyoungchildren:outcomeofdefinitivecraniospinalirradiationfollowingincomplete
responsetochemotherapy(1994). JCO.12:1212‐1216.
4) Miralbell.Radiotherapyinpediatricmedulloblastoma:qualityassessmentofPediatricOncologyGroupTrial903(2006).IJROBP.
64(5):1325‐30.
5) Thomasetal.Low‐stagemedulloblastoma:finalanalysisoftrialcomparing
standard‐dosewithreduced‐doseneuraxisirradiation
(2000).JCO.18(16):3004‐11.
6) Zeltzeretal.Metastasisstage,adjuvanttreatment,andresidualtumorareprognosticfactorsformedulloblastomainchildren:
conclusionsfromtheChildren’sCancerGroup921randomizedphaseIIIstudy(1999).JCO.17(3):832‐845.
7) Packeretal.PhaseIIIstudyofcraniospinal
radiationtherapyfollowedbyadjuvantchemotherapyfornewlydiagnosedaverage‐
riskmedulloblastoma(2006).JCO.24(25):4204‐8.
8) Monjeetal.Hedgehogs,flies,wnts,andMYCs:thetimehascomeformanythingsinmedulloblastoma(2011).JCO.29(11):1395‐
8.
9) Woldenetal.Patternsoffailureusingaconformalradiationtherapytumorbedboost
formedulloblastoma(2003).JCO.21
(16):3079‐83.
10) Merchantetal.Multi‐inst itutionalprospectivetrialofreduced‐dosecraniospinalirradiation(23.4Gy)followedbyconformal
posteriorfossa(36Gy)andprimarysiteirradiation(55.8Gy)anddose‐intensivechemotherapyforaverage‐riskmedulloblastoma
(2008).IJROBP.70(3):782‐7.
11) Risetal.Intellectualoutcome
afterreduced‐doseradiationtherapyplusadjuvantchemotherapyformedulloblastoma:a
Children’sCancerGroupstudy(2001).JCO.19(15):3470‐76.
12) Armstrongetal.Evaluationofmemoryimpairmentinagingadultsurvivorsofchildhoodacutelymphoblasticleukemiatreated
withcranialradiotherapy(2013).JNCI.105(12):899‐907.
