PAYMENT POLICY
Page 1 of 19
Psychotherapy
Policy Number: SC14P0043A2 Effective Date: May 1, 2018
Last Update: April 6, 2021
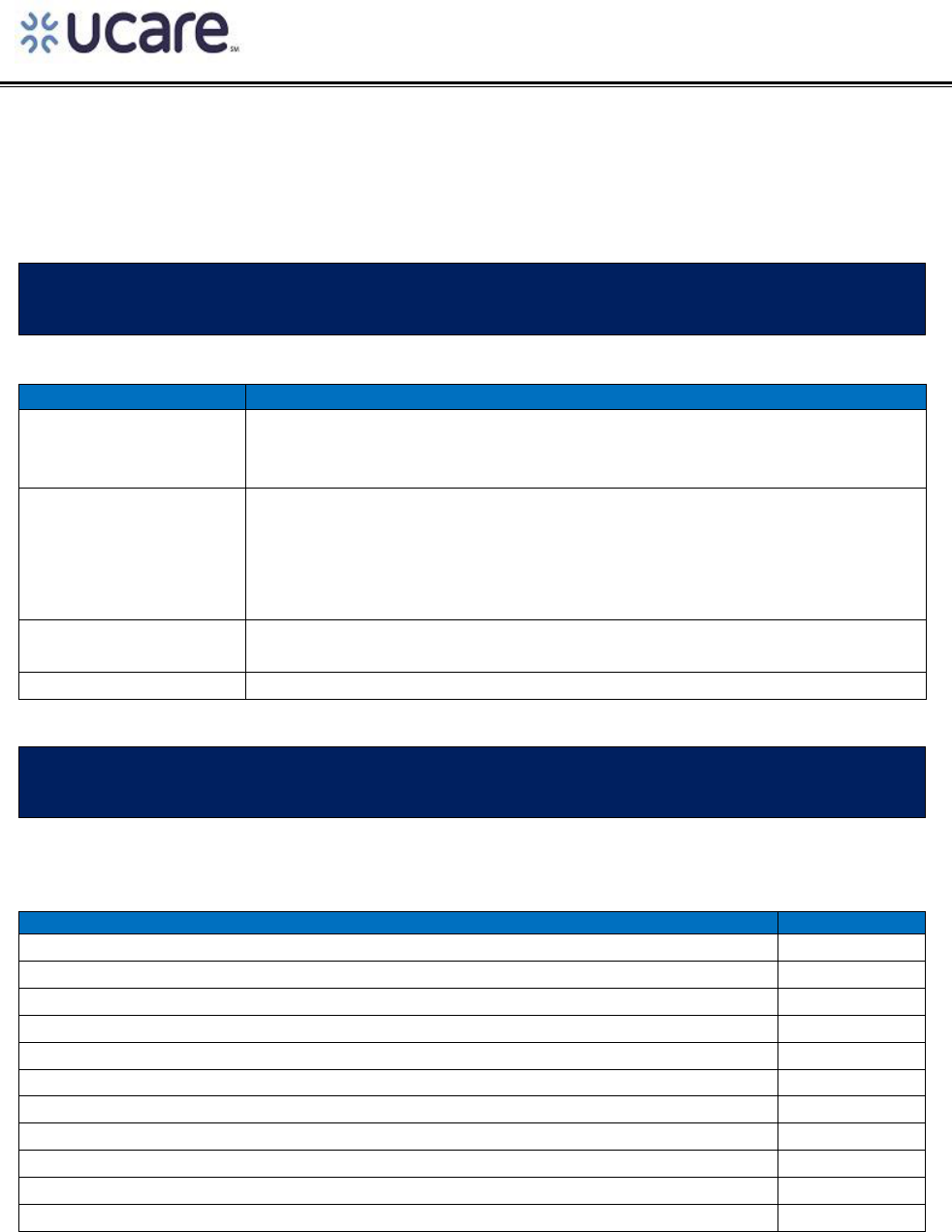
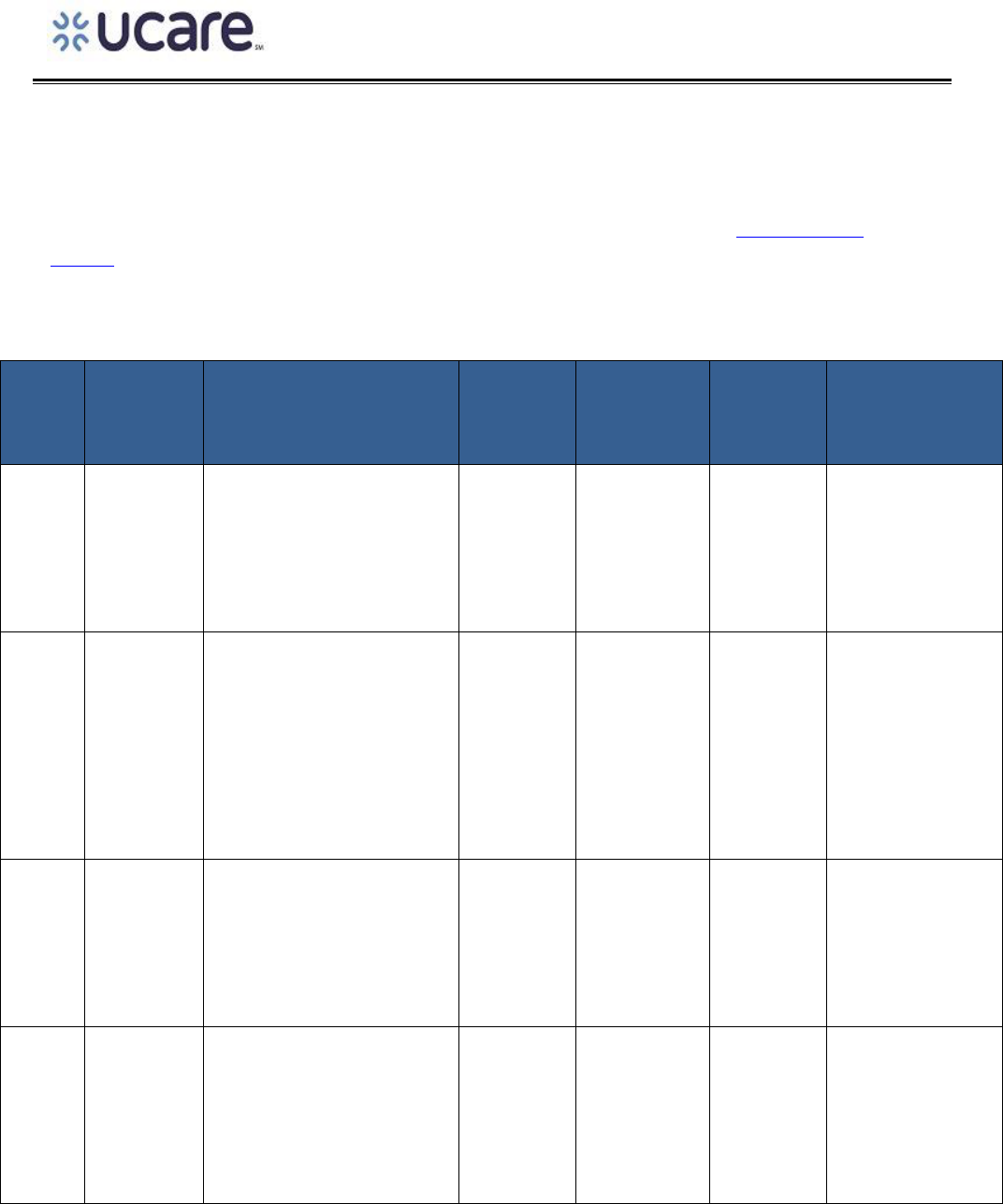
PAYMENT POLICY HISTORY
DATE
SUMMARY OF CHANGE
April 6, 2021
The psychotherapy policy was moved to an updated UCare format. As a
result, some of the information may have been reformatted. In addition,
an annual update was completed. No changes were made to the policy.
August 28, 2019
Information regarding comparison to the DHS MH Procedure CPT® or
HCPCS Codes and Rates Chart and UCare fee schedules was removed from
the document. The UCare Provider Manual contains information regarding
how and when UCare updates fee schedules. A link to the UCare Provider
Manual continues to be available within the document.
5/1/2019
Annual policy review. The links within the Policy and the UCare logo were
updated.
5/1/2018
The psychotherapy policy was implemented by UCare.
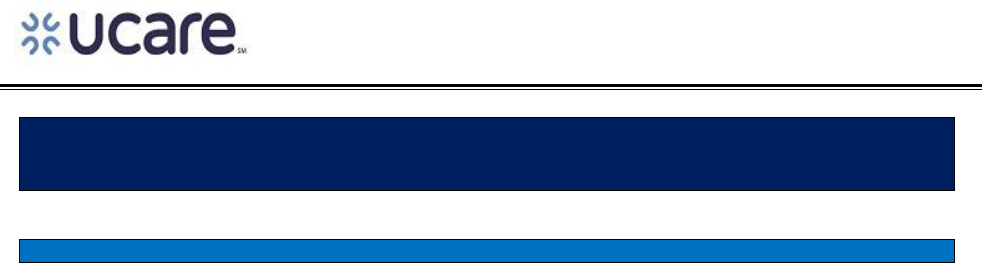
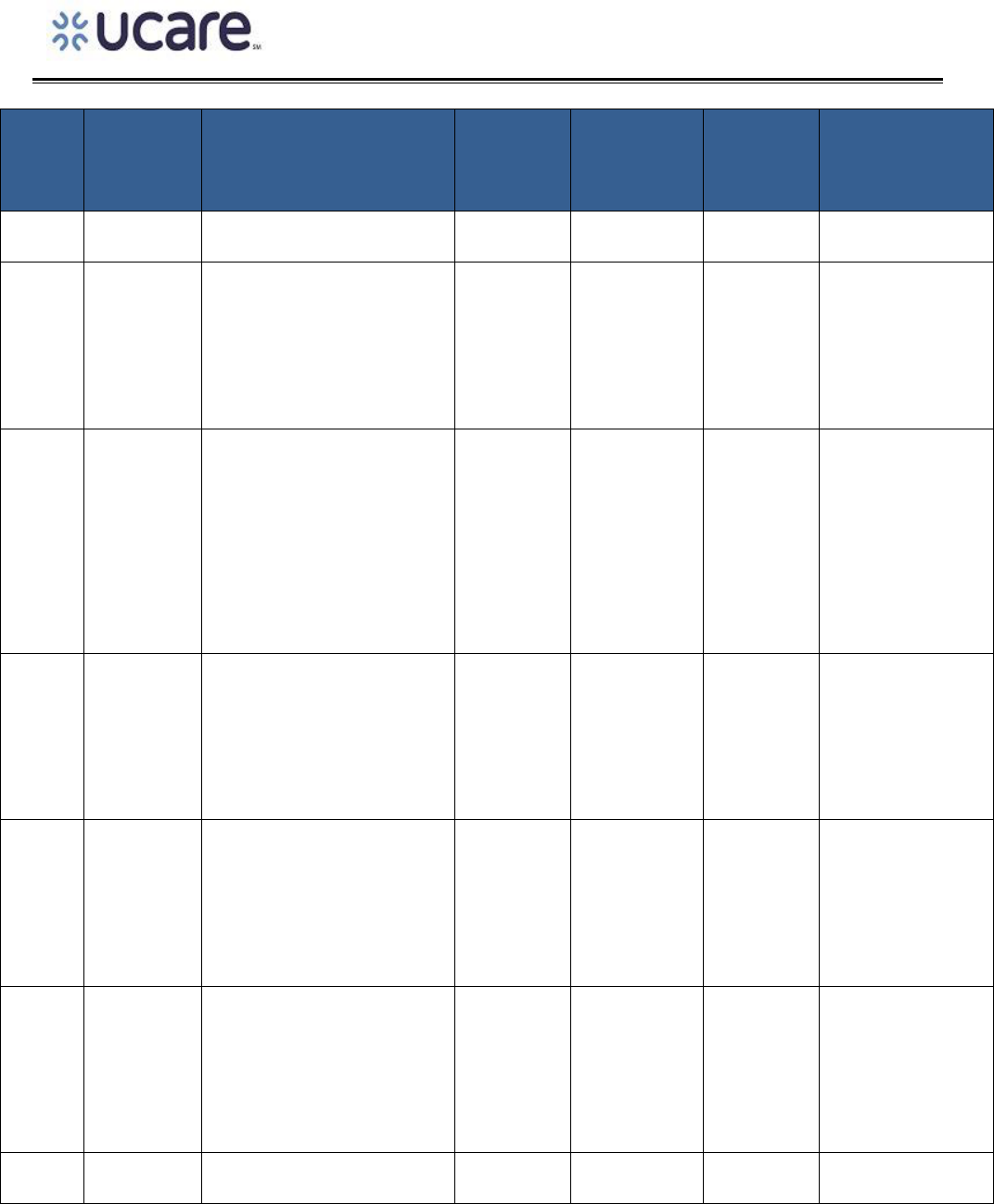
APPLICABLE PRODUCTS
This policy applies to the products checked below:
UCARE PRODUCT
APPLIES TO
UCare MinnesotaCare
√
UCare Minnesota Senior Care Plus (MSC+)
√
UCare Prepaid Medical Assistance (PMAP)
√
UCare Connect
√
UCare Connect + Medicare (When MHCP is the primary payer)
√
UCare Minnesota Senior Health Options (MSHO) (When MHCP is the primary payer)
√
UCare Medicare Plans
UCare EssentiaCare
UCare Medicare M Health Fairview & North Memorial
UCare Individual & Family Plans
UCare Individual & Family Plans M Health Fairview
PAYMENT POLICY
Page 2 of 19
TABLE OF CONTENTS
TABLE OF CONTENTS PAGE
Table of Contents
PAYMENT POLICY HISTORY ........................................................................................................................... 1
APPLICABLE PRODUCTS ................................................................................................................................ 1
TABLE OF CONTENTS ..................................................................................................................................... 2
PAYMENT POLICY OVERVIEW ....................................................................................................................... 5
POLICY DEFINITIONS ..................................................................................................................................... 5
ENROLLEE ELIGIBILITY CRITERIA.................................................................................................................... 6
ELIGIBLE PROVIDERS OR FACILITIES .............................................................................................................. 7
Provider ................................................................................................................................................. 7
Facility ................................................................................................................................................... 7
Other and/or Additional Information ................................................................................................... 7
EXLUDED PROVIDER TYPES ........................................................................................................................... 7
MODIFIERS, CPT, HCPCS, AND REVENUE CODES .......................................................................................... 8
General Information ............................................................................................................................. 8
Modifiers ............................................................................................................................................... 8
CPT and/or HCPCS Code(s) .................................................................................................................... 8
Revenue Codes ...................................................................................................................................... 9
PAYMENT INFORMATION ............................................................................................................................. 9
Payment Guidelines .............................................................................................................................. 9
Time Based Services ............................................................................................................................ 13
BILLING REQUIREMENTS AND DIRECTIONS ................................................................................................ 13
General Information ........................................................................................................................... 13
Billing Guidelines ................................................................................................................................. 16
PRIOR AUTHORIZATI0N, NOTIFICATION AND THRESHOLD INFORMATION ............................................... 17
Prior Authorization, Notification, and Threshold Requirements ........................................................ 17

PAYMENT POLICY
Page 3 of 19
RELATED PAYMENT POLICY INFORMATION ................................................................................................ 18
SOURCE DOCUMENTS AND REGULATORY REFENCES ................................................................................. 18
DISCLAIMER................................................................................................................................................. 18

PAYMENT POLICY
Page 4 of 19
This page was intentionally left blank

PAYMENT POLICY
Page 5 of 19
PAYMENT POLICY INSTRUCTIONS
A payment policy assists in determining provider reimbursement for specific covered services. To
receive payment, the provider must be in a contractual relationship with UCare and provide services to a
member enrolled in one of UCare’s products. This payment policy is intended to provide a foundation
for system configuration, work instructions, call scripts, and provider communications. A payment
policy describes the rules for payment, which include applicable fee schedules, additional payment rules
by regulatory bodies, and contractual terms. This policy is a general guideline and may be superseded
by specific provider contract language.
PAYMENT POLICY OVERVIEW
This Policy outlines the professional payment and billing guidelines associated with psychotherapy
services.
POLICY DEFINITIONS
TERM
NARRATIVE DESCRIPTION
Diagnostic Assessment
Means functional face-to-face evaluation resulting in a complete
written assessment that includes clinical considerations and severity of
the client's general physical, developmental, family, social, psychiatric,
and psychological history and current condition. The Diagnostic
Assessment will also note strengths, vulnerabilities, and needed mental
health services.
Family Member
Means a person identified by the patient (or patient’s parent or
guardian) as being important to the patient’s mental health and may
include, but is not limited to parents, children, spouse, committed
partners, and ex-spouses, person related by blood or adoption, or
persons who are presently residing together as a family unit. Shift staff
or other facility staff members at the patient’s residence are not
considered a Family Member.
Mental Health Practitioner
Qualified as a Clinical
Trainee
Means a mental health practitioner working as a clinical trainee who
meets the following criteria:
• Be complying with requirements for licensure or board
certification as a mental health professional including

PAYMENT POLICY
Page 6 of 19
TERM
NARRATIVE DESCRIPTION
supervised practice in the delivery of mental health services for
the treatment of mental illness
• Be a student in a bona fide field placement or internship under
a program leading to completion of the requirements for
licensure as a mental health professional
The clinical trainee’s clinical supervision experience helps the
practitioner gain knowledge and skills necessary to practice effectively
and independently. The experience gained by the clinical trainee during
supervision may include:
• Direct practice
• Treatment team collaboration
• Continued professional learning
• Job management
Psychotherapy
Means a planned and structured, face-to-face treatment of a patient’s
mental illness that is provided using the psychological, psychiatric or
interpersonal method most appropriate to the needs of the patient
according to current community standards of mental health practice
and is directed to accomplish measurable goals and objectives specified
in the patient’s individual treatment plan (ITP).
Notification
Means the process of informing UCare or their delegates of a specific
medical treatment or service prior to billing for certain services.
Services that require notification are not subject to review for medical
necessity but must be medically necessary and covered within the
member’s benefit set. If claims are submitted to UCare and no
notification has been received from the provider, the claim will be
denied.
Prior Authorization
Means an approval by UCare or their delegates prior to the delivery of a
specific service or treatment. Prior authorization requests require a
clinical review by qualified, appropriate professionals to determine if
the service or treatment is medically necessary. UCare requires certain
services to be authorized before services begin. Services provided
without an authorization will be denied.
ENROLLEE ELIGIBILITY CRITERIA
THIS SECTION OF THE POLICY PROVIDES INFORMATION THAT IS SPECIFIC TO THE
UCARE MEMBER, INCLUDING INFORMATION ABOUT THE CRITERIA THE MEMBER MUST
MEET IN ORDER FOR THE SERVICE(S) IN THE POLICY TO BE ELIGIBLE FOR PAYMENT

PAYMENT POLICY
Page 7 of 19
For services to be covered by UCare the patient must be actively enrolled in one of the UCare products
listed above.
ELIGIBLE PROVIDERS OR FACILITIES
OUTLINED BELOW IS THE SPECIFIC CRITERIA A PROVIDER MUST MEET IN ORDER FOR THE
SERVICE(S) IN THIS POLICY TO BE ELIGIBLE FOR PAYMENT. THE SERVICE(S) IN THE
POLICY TO BE ELIGIBLE FOR PAYMENT
Provider
Psychotherapy may be provided by:
• Clinical nurse specialist in mental health (CNS)
• Licensed independent clinical social worker (LICSW)
• Licensed marriage and family therapist (LMFT)
• Licensed professional clinical counselor (LPCC)
• Licensed psychologist (LP)
• Psychiatric nurse practitioner (NP)
• Psychiatrist
• Mental health practitioners working as clinical trainees under the supervision of a mental health
professional.
Facility
This policy outlines payment for professional services.
Other and/or Additional Information
Not applicable.
EXLUDED PROVIDER TYPES
OUTLINED BELOW IS INFORMATION REGARDING PROVIDERS WHO ARE NOT ELIGIBLE
TO FURNISH THE SERVICE(S) LISTED IN THIS POLICY.
Not applicable.
PAYMENT POLICY
Page 8 of 19
MODIFIERS, CPT, HCPCS, AND REVENUE CODES
General Information
The Current Procedural Terminology (CPT®) HCPCS, and Revenue codes listed in this policy are for
reference purposes only. Including information in this policy does not imply that the service described
by a code is a covered or non-covered health service. The inclusion of a code does not imply any right to
reimbursement or guarantee of claim payment.
Modifiers
The modifiers listed below are not intended to be a comprehensive list of all modifiers. Instead, the
modifiers listed are those that must be appended to the CPT® / HCPCS codes listed below. Based on the
service(s) provided, and the circumstances surrounding those services it may, based on correct coding,
be appropriate to append an additional modifier(s) to the CPT® / HCPCS code.
When a service requires multiple modifiers, the modifiers must be submitted in the order listed
below. If it is necessary to add additional modifiers they should be added after the modifiers listed
below.
MODIFIER(S)
NARRATIVE DESCRIPTION
HN
For purposes of this policy, the –HN modifier indicates services were furnished
by a Mental Health Practitioner or qualified Clinical Trainee when licensing and
supervision requirements are met.
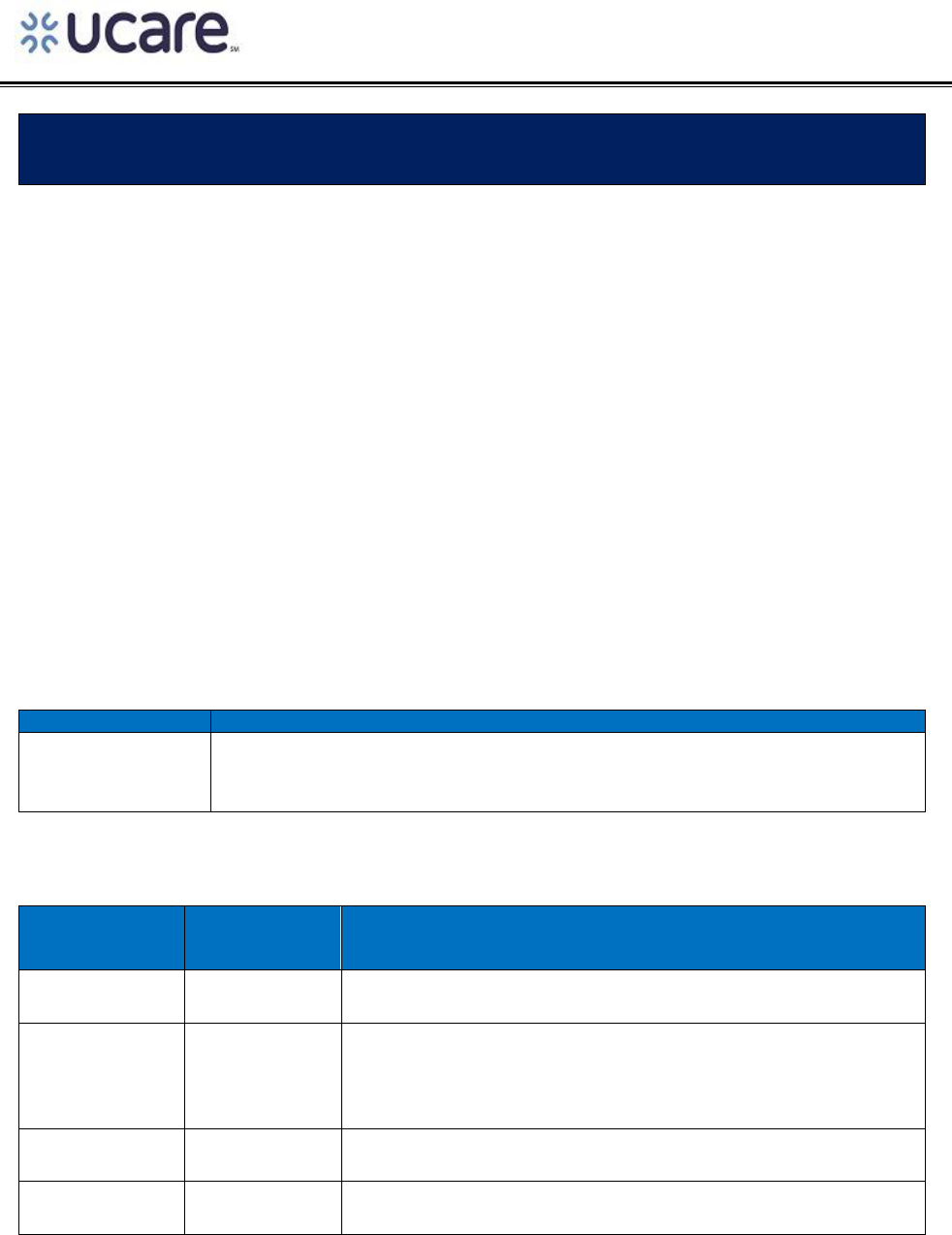
CPT and/or HCPCS Code(s)
CPT AND/OR
HCPCS
CODE(S)
MODIFIER(S)
NARRATIVE DESCRIPTION
90832
Psychotherapy (with patient or family member or both), 30
minutes
90833
Psychotherapy, 30 minutes with patient or family member or
both when performed with an evaluation and management
service (List separately in addition to the code for primary
procedure (E&M code))
90834
Psychotherapy (with patient or family member or both), 45
minutes
90836
Psychotherapy, 45 minutes with patient or family member or
both when performed with an evaluation and management
PAYMENT POLICY
Page 9 of 19
CPT AND/OR
HCPCS
CODE(S)
MODIFIER(S)
NARRATIVE DESCRIPTION
service (List separately in addition to the code for primary
procedure (E&M code))
90837
Psychotherapy (with patient or family member or both),
90838
Psychotherapy, 60 minutes with patient or family member or
both when performed with an evaluation and management
service (List separately in addition to the code for primary
procedure (E&M code))
90839
Psychotherapy for Crisis
90840
Psychotherapy for Crisis (add on-code code to 90839)
90846
Family psychotherapy (without the patient present), 50 minutes
90847
Family psychotherapy (conjoint psychotherapy) (with patient
present), 50 minutes
90849
Multiple-family group psychotherapy
90853
Group psychotherapy (other than of a multiple-family group)
90875
Individual psychophysiological therapy incorporating
biofeedback, with psychotherapy, 30 minutes
90876
Individual psychophysiological therapy incorporating
biofeedback, with psychotherapy, 45 minutes
99354
Prolonged service code for psychotherapy services (add on to
90837)
CPT® is a registered trademark of the American Medical Association.
Revenue Codes
PAYMENT INFORMATION
Payment Guidelines
UCare follows MHCP guidelines when applying Master’s prepared provider reductions to eligible mental
health services. Master’s level reductions are not applied to mental health services when they are
furnished:
• In a Community Mental Health Center (CMHC)
• By a Mental Health Practitioner qualified to work as a clinical trainee.
PAYMENT POLICY
Page 10 of 19
The reduction percentage listed below is applied when mental health services are furnished. If clinical
services like Evaluation and Management services are provided to a patient by an eligible provider, the
clinical reduction applicable to that provider specialty will be applied to the service.
Additional information regarding UCare fee schedule updates can be found in the UCare Provider
Manual (Section 10-20 Fee Schedule Updates).
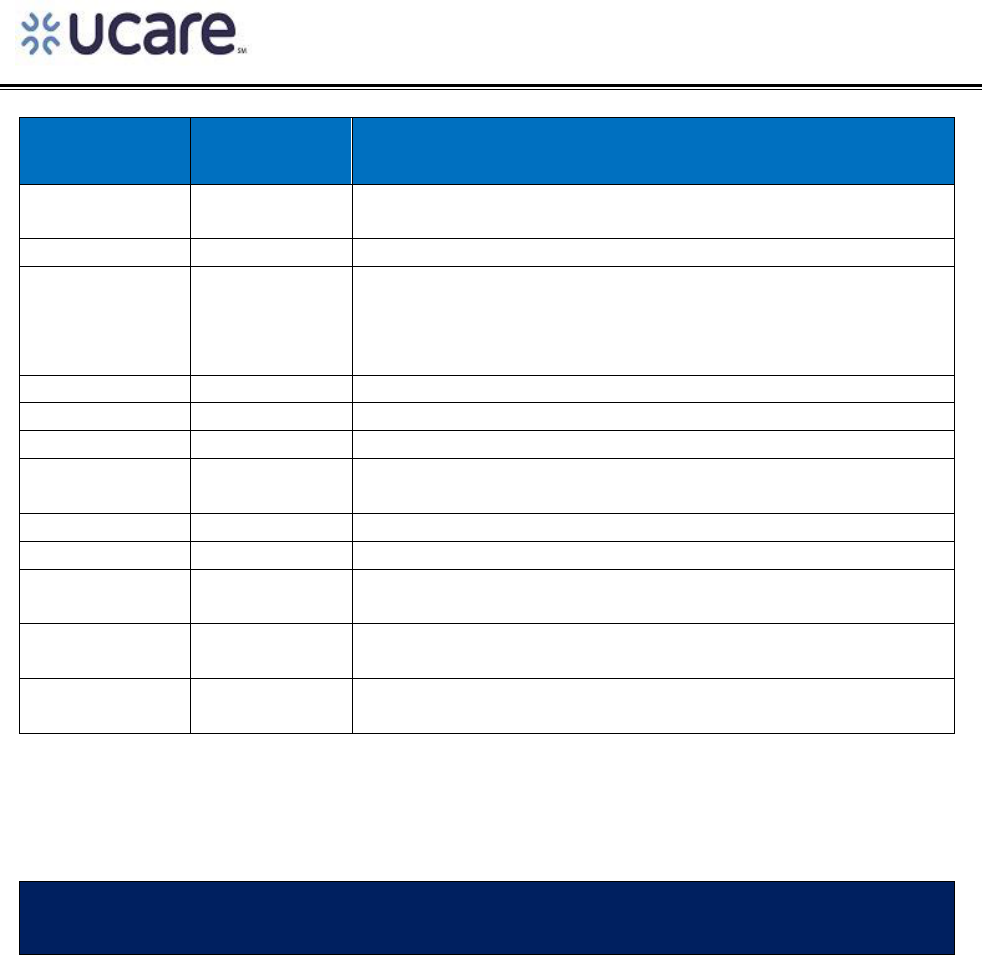
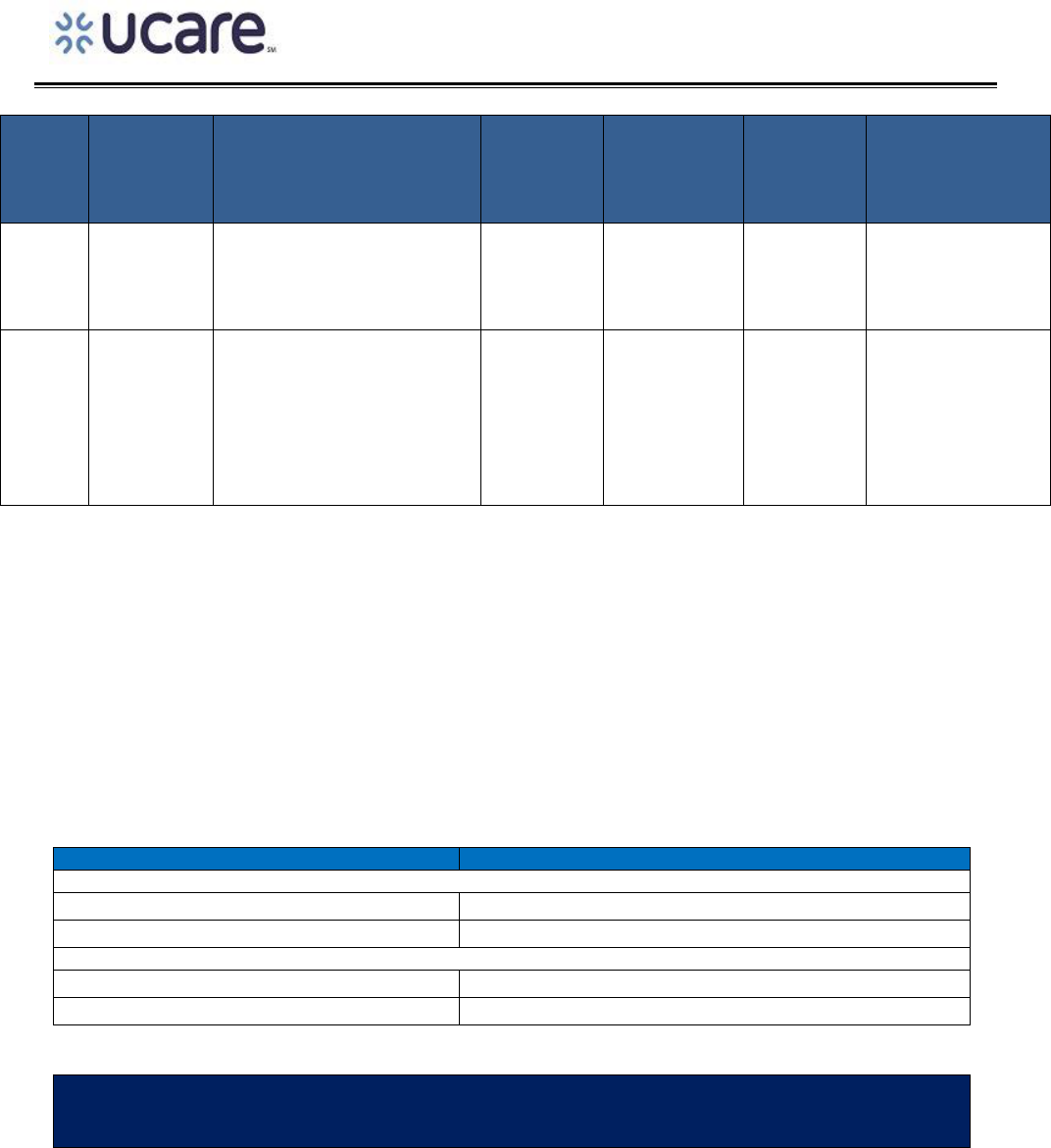
The grid below identifies whether the Master’s level provider reduction and/or 23.7% increase applies
to service(s) associated with Psychotherapy.
CPT®
or
HCPCS
CODES
MODIFIER
NARRATIVE
DESCRIPTION
UNIT OF
SERVICE
APPLY
MASTER’S
LEVEL
REDUCTION
DOES
23.7%
INCREASE
APPLY
PROVIDERS
ELIGIBLE TO
PERFORM
SERVICE
90832
Psychotherapy (with
patient or family member
or both), 30 minutes
30 Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90833
Psychotherapy, 30 minutes
with patient or family
member or both when
performed with an
evaluation and
management service (List
separately in addition to
the code for primary
procedure (E&M code))
30 Minutes
Yes
Yes
• Psychiatrist
• NP
• CNS-MH-MH
90834
Psychotherapy (with
patient or family member
or both), 45 minutes
45 Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90836
Psychotherapy, 45 minutes
with patient or family
member or both when
performed with an
evaluation and
management service (List
separately in addition to
45 Minutes
Yes
Yes
• Psychiatrist
• NP
• CNS-MH-MH
PAYMENT POLICY
Page 11 of 19
CPT®
or
HCPCS
CODES
MODIFIER
NARRATIVE
DESCRIPTION
UNIT OF
SERVICE
APPLY
MASTER’S
LEVEL
REDUCTION
DOES
23.7%
INCREASE
APPLY
PROVIDERS
ELIGIBLE TO
PERFORM
SERVICE
the code for primary
procedure (E&M code))
90837
Psychotherapy (with
patient or family member
or both), 60 minutes
60 Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90838
Psychotherapy, 60 minutes
with patient or family
member or both when
performed with an
evaluation and
management service (List
separately in addition to
the code for primary
procedure (E&M code))
60 Minutes
Yes
Yes
• Psychiatrist
• NP
• CNS-MH-MH
90839
Psychotherapy for Crisis
60 Minutes
Yes
Yes
• CNS-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90840
Psychotherapy for Crisis
(add on-code code to
90839)
30 Minutes
Yes
Yes
• CNS-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90846
Family psychotherapy
(without the patient
present), 50 minutes
Per Session
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90847
Family psychotherapy
(conjoint psychotherapy)
Per Session
Yes
Yes
• CNS-MH-MH
• LICSW

PAYMENT POLICY
Page 12 of 19
CPT®
or
HCPCS
CODES
MODIFIER
NARRATIVE
DESCRIPTION
UNIT OF
SERVICE
APPLY
MASTER’S
LEVEL
REDUCTION
DOES
23.7%
INCREASE
APPLY
PROVIDERS
ELIGIBLE TO
PERFORM
SERVICE
(with patient present), 50
minutes
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90849
Multiple-family group
psychotherapy
Per Session
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90853
Group psychotherapy
(other than of a multiple-
family group)
Per Session
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90875
Individual
psychophysiological
therapy incorporating
biofeedback, with
psychotherapy, 30 minutes
20 - 30
Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90876
Individual
psychophysiological
therapy incorporating
biofeedback, with
psychotherapy, 45 minutes
45 – 50
Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
90785
Interactive Complexity Add-
On Service
Individual
psychophysiological
therapy incorporating
biofeedback training by any
modality (face-to-face with
the patient), with
Yes
Yes
• CNS-MH
• NP
• Psychiatrist
PAYMENT POLICY
Page 13 of 19
CPT®
or
HCPCS
CODES
MODIFIER
NARRATIVE
DESCRIPTION
UNIT OF
SERVICE
APPLY
MASTER’S
LEVEL
REDUCTION
DOES
23.7%
INCREASE
APPLY
PROVIDERS
ELIGIBLE TO
PERFORM
SERVICE
psychotherapy (e.g., insight
oriented, behavior
modifying or supportive
psychotherapy); 30 minutes
99354
Pronged E&M or
psychotherapy service(s)
beyond the typical service
time of the primary
procedure. (List separately
in addition to 90837)
30 Minutes
Yes
Yes
• CNS-MH-MH
• LICSW
• LMFT
• LPCC
• LP
• NP
• Psychiatrist
Time Based Services
When billing for services that include time as part of their definition, follow HCPCS and CPT guidelines to
determine the appropriate unit(s) of service to report. Based on current guidelines, providers must
spend more than half the time of a time-based code performing the service to report the code. If the
time spent results in more than one- and one-half times the defined value of the code, and no additional
time increment code exists, round up to the next whole number. Outlined below are the billable units
of service based on whether the description of the service includes the unit of measurement of 15
minutes or 60 minutes:
MINUTES
BILLABLE UNITS
Fifteen (15) Minute Increments
0 – 7 minutes
0 (no billable unit of service)
8 – 15 minutes
1 (unit of billable service)
Sixty (60) Minute Increments
0 – 30 minutes
0 (no billable unit of service)
31 – 60 minutes
1 (unit of billable service)
BILLING REQUIREMENTS AND DIRECTIONS
General Information

PAYMENT POLICY
Page 14 of 19
Psychotherapy (with patient or family member or both)
These codes should be used for services when:
• The patient, family member or both are present.
• Therapy includes some time without the patient (but the patient must be present for a
significant amount of the psychotherapy time).
• Therapy includes hypnotherapy (conducted by a mental health professional or qualified clinical
trainee trained in hypnotherapy). Do not bill hypnotherapy separately.
• Therapy includes individual psychophysiological therapy incorporating biofeedback, with
psychotherapy
• Appropriate the interactive complexity add-on (CPT® code 90785) service may be billed in
addition to psychotherapy.
Evaluation and Management (E&M) with Psychotherapy (patient or family or both)
These codes should be used when:
• Psychotherapy is performed in addition to E&M services.
• The time spent on E&M activities and psychotherapy are necessary and distinct services.
• Appropriate interactive complexity add-on (CPT® code 90785) service may be billed in addition
to psychotherapy.
Family Psychotherapy
These codes should be used when:
• The patient and one or more family members participation in therapy is necessary to accomplish
the patient’s treatment goals.
• In the opinion of the treating provider the patient’s absence from the family psychotherapy
session is necessary to carry out the patient’s treatment plan.
Family members do not need to be enrolled with UCare or MHCP to participate in family psychotherapy.
Multiple Family Group Psychotherapy
• Multiple family group psychotherapy is designed for at least two, but no more than five families.
• The focus of multiple family group psychotherapy is to meet the treatment needs of the patient
as outlined in their treatment plan.
• If it is the opinion of the treating provider that the patient’s absence from the family
psychotherapy session is necessary to carry out the patient’s treatment plan, document the
length of time and reason for the patient’s absence in the medical record. In addition, also
document reason(s) for a family member’s exclusion from family psychotherapy.

PAYMENT POLICY
Page 15 of 19
Group Psychotherapy
• Group psychotherapy is appropriate for individuals who because of the nature of their
emotional, behavioral, or social dysfunctions can benefit from treatment in a group setting.
• One mental health professional may provide services for a group of 3 - 8 patients
• When the size of the group is 9 – 12 patients, two Mental Health Professionals must be present.
• For group psychotherapy the group may not exceed 12 patients and is not dependent on the
number of UCare enrollees or MHCP patients participating the group.
• When appropriate, the interactive complexity add-on (CPT® code 90785) service may be billed in
addition to psychotherapy.
Interactive Complexity
It is appropriate to add-on CPT® code 90785 when any of the following circumstances exist during the
visit:
• Communication difficulties among participants complicate care delivery related to issues such
as:
o High anxiety
o High reactivity
o Repeated questions
o Disagreement
o Caregiver emotions or behaviors that interfere with implementing the treatment plan
o Discovery or discussion of evidence relating to an event that must be reported to a third
party. This may include events such as abuse or neglect that require a mandatory report
to the state agency
• It is necessary to overcomes communication barriers by using any of the following methods:
o Play equipment
o Physical devices
o An interpreter
o A translator
• For patients who are not fluent in the same language as the mental health provider.
• For patient who have not developed or have lost the skills needed to use or understand typical
language.
Diagnostic Assessment and Diagnosis Requirements
Eligible patients must have a diagnosis of mental illness as determined by a diagnostic assessment. A
new patient may receive up to three (3) sessions of a combination of individual or group psychotherapy
or family psychoeducation prior to completion of the patient’s diagnostic assessment.

PAYMENT POLICY
Page 16 of 19
Billing Guidelines
The services outlined below must be submitted using the 837P format or the electronic equivalent.
CPT® or
HCPCS
CODES
MODIFIER
NARRATIVE DESCRIPTION
BILLING GUIDELINES
90832
Psychotherapy (with patient or
family member or both), 30
minutes
E&M with psychotherapy may only be billed by:
• Clinical nurse specialist – MH (CNS-MH-
MH)
• Psychiatric Nurse Practitioner (NP)
• Psychiatrist
CPT® Code 90785 (Interactive complexity) may
reported in addition to the following services:
• Psychotherapy (CPT® codes 90832,
90834, 90837)
• Psychotherapy performed with an E&M
service (90833, 90836, 90938)
CPT® code 90849 may be billed for each family
participating in the multi-family group session.
This coded should not be billed for each family
member participating in the therapy session
90834
Psychotherapy (with patient or
family member or both), 45
minutes
90837
Psychotherapy (with patient or
family member or both), 60
minutes
90833
Psychotherapy, 30 minutes with
patient or family member or
both when performed with an
evaluation and management
service (List separately in
addition to the code for primary
procedure (E&M code))
90836
Psychotherapy, 45 minutes with
patient or family member or
both when performed with an
evaluation and management
service (List separately in
addition to the code for primary
procedure (E&M code))
90838
Psychotherapy, 60 minutes with
patient or family member or
both when performed with an
evaluation and management
service (List separately in
addition to the code for primary
procedure (E&M code))
90875
Individual psychophysiological
therapy incorporating
biofeedback, with
psychotherapy, 30 minutes
90876
Individual psychophysiological
therapy incorporating
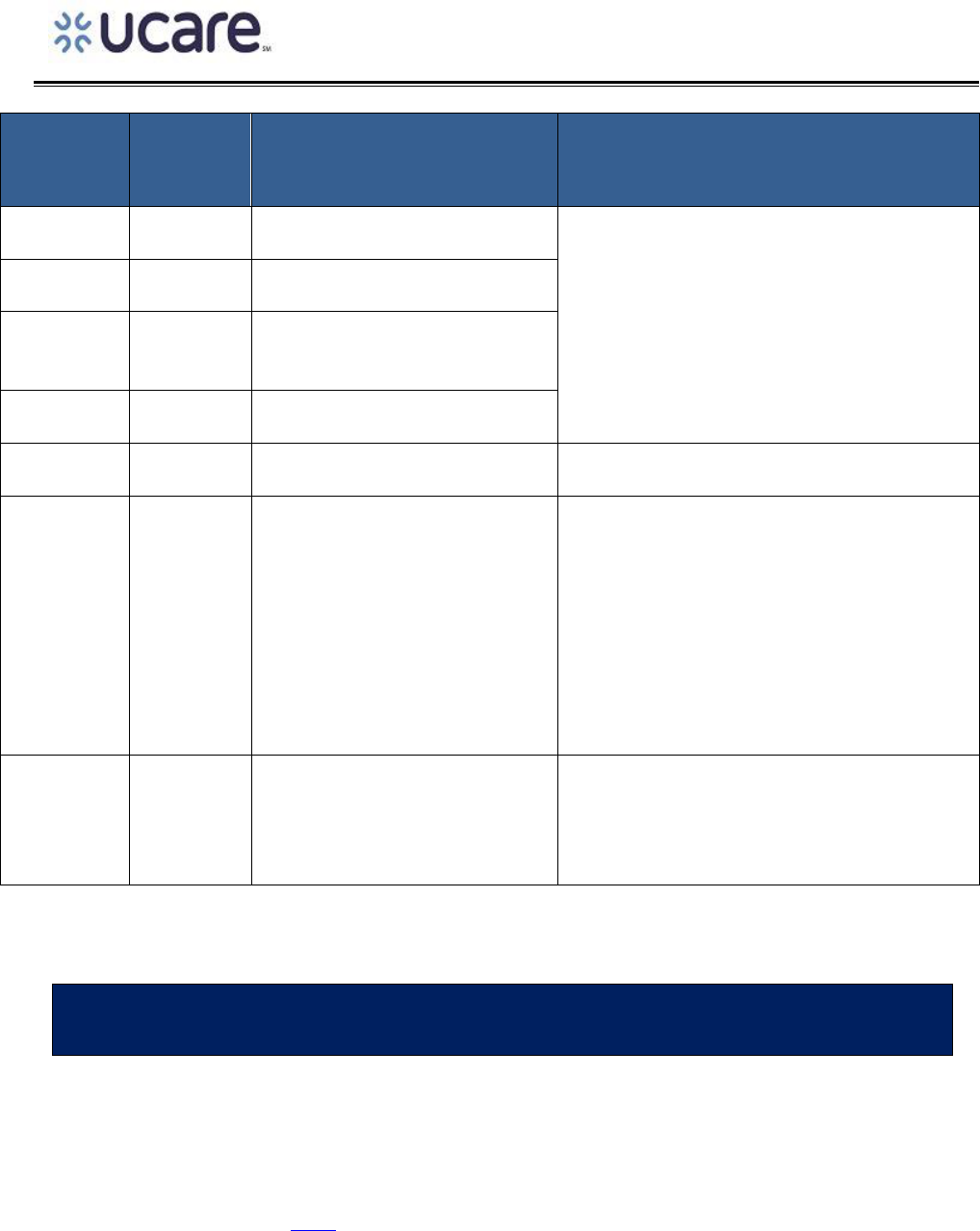
PAYMENT POLICY
Page 17 of 19
CPT® or
HCPCS
CODES
MODIFIER
NARRATIVE DESCRIPTION
BILLING GUIDELINES
biofeedback, with
psychotherapy, 45 minutes
90846
Family psychotherapy (without
the patient present), 50 minutes
90847
Family psychotherapy (conjoint
psychotherapy) (with patient
present), 50 minutes
90849
Multiple-family group
psychotherapy
90853
Group psychotherapy (other
than of a multiple-family group)
When appropriate, 90875 Interactive Complexity
add-on service may be billed in addition to 90853
90785
Interactive Complexity Add-On
Service
Individual psychophysiological
therapy incorporating
biofeedback training by any
modality (face-to-face with the
patient), with psychotherapy
(e.g., insight oriented, behavior
modifying or supportive
psychotherapy); 30 minutes
99354
Pronged E&M or psychotherapy
service(s) beyond the typical
service time of the primary
procedure. (List separately in
addition to 90837)
PRIOR AUTHORIZATI0N, NOTIFICATION AND THRESHOLD INFORMATION
Prior Authorization, Notification, and Threshold Requirements
Psychotherapy services do not require at prior authorization. UCare does update its’ authorization,
notification, and threshold requirements from time-to-time. The most current prior authorization
requirements can be found here.

PAYMENT POLICY
Page 18 of 19
RELATED PAYMENT POLICY INFORMATION
OUTLINED BELOW ARE OTHER POLICIES THAT MAY RELATE TO THIS POLICY AND/OR
MAY HAVE AN IMPACT ON THIS POLICY.
POLICY NUMBER
POLICY TITLE
UCare payment policies are updated from time to time. The most current UCare payment policies can
be found here.
SOURCE DOCUMENTS AND REGULATORY REFENCES
LISTED BELOW ARE LINKS TO CMS, MHCP, AND STATUTORY AND REGULATORY
REFERENCES USED TO CREATE THIS POLICY
MHCP Provider Manual, Mental Health Services, Psychotherapy
Minnesota Statutes 144.292, subdivision 2 and 7 (Minnesota Health Records Act – patient access and
exception
Minnesota Statutes 245.4871, subdivision 11a (Diagnostic assessment)
Minnesota Rules 9505.0372 (Psychotherapy services)
Minnesota Rules 9505.0371 Subp. 7 (Individual Treatment Plan)
Code of Federal Regulations, title 45, section 164, parts 501 (45 CFR 164.501) (Psychotherapy notes)
Code of Federal Regulations title 45, section 160, parts 203 (45 C.F.R. 160.203 (b) ) (Release of Privacy)
DISCLAIMER
“Payment Policies assist in administering payment for UCare benefits under UCare’s health benefit
Plans. Payment Policies are intended to serve only as a general reference resource regarding UCare’s
administration of health benefits and are not intended to address all issues related to payment for
health care services provided to UCare members. When submitting claims, all providers must first
identify member eligibility, federal and state legislation or regulatory guidance regarding claims
submission, UCare provider participation agreement contract terms, and the member-specific Evidence
of Coverage (EOC) or other benefit document. In the event of a conflict, these sources supersede the
Payment Policies. Payment Policies are provided for informational purposes and do not constitute

PAYMENT POLICY
Page 19 of 19
coding or compliance advice. Providers are responsible for submission of accurate and compliant
claims. In addition to Payment Policies, UCare also uses tools developed by third parties, such as the
Current Procedural Terminology (CPT®*), InterQual guidelines, Centers for Medicare and Medicaid
Services (CMS), the Minnesota Department of Human Services (DHS), or other coding guidelines, to
assist in administering health benefits. References to CPT® or other sources in UCare Payment Policies
are for definitional purposes only and do not imply any right to payment. Other UCare Policies and
Coverage Determination Guidelines may also apply. UCare reserves the right, in its sole discretion, to
modify its Policies and Guidelines as necessary and to administer payments in a manner other than as
described by UCare Payment Policies when necessitated by operational considerations.”
